New to This Mommy’s Heart? Check out my story from the beginning here – My PPCM Story
I was admitted to UWMC on Thanksgiving Day. Since we didn’t really know what was going to happen, in addition to needing help with the kids, all of my siblings left their families to fly across the country (IND>SEA) to come to see me and help out. I’ll never be able to thank them enough for their selflessness, love and caring that they gave to my children.





The fellow told my family there was a 33% chance my heart would get better, 33% chance it would stay the same and 33% chance it would get worse. Like I mentioned before, the theme of this story is if something rare and bad could happen, it did.
I was given nitroprusside which reduces the resistance in the blood vessels so the heart doesn’t have to work so hard to push blood around the body and milrinone to help the heart work better and more efficiently. Neither of these was helping very much. I was taken into surgery where the doctors found that the right side of my heart was not working as well as they expected. From here I went straight to extracorporeal membrane oxygenation (ECMO) with an impella assisting the left ventricle. ECMO is a form of life support that pumps and oxygenates the blood outside the body allowing the heart to rest. It is generally not recommended to be on this machine for more than 5 days due to complications.
I was intubated, sedated and placed in the Cardiothoracic Intensive Care Unit (CTICU). You don’t go to the ICU unless you are very sick but my family was told I had the honor of currently being the sickest on the floor…

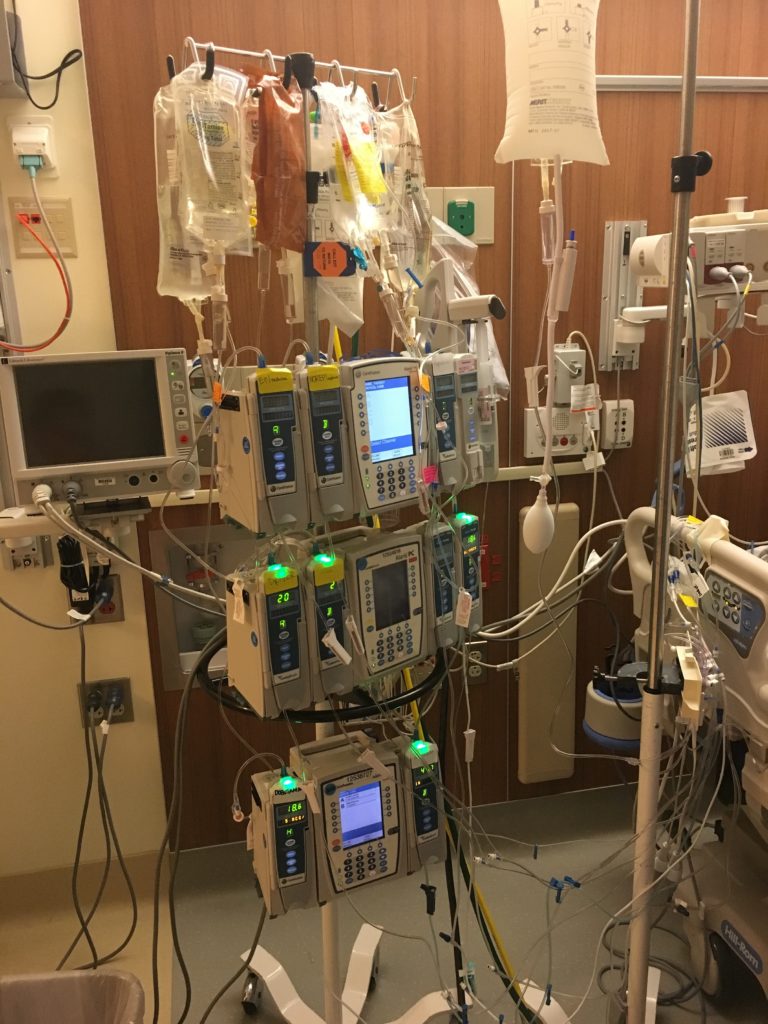

The entire next day I remained intubated and sedated. My echocardiograms were still showing little right ventricle improvement. On the 25th I was weaned from sedation and my entire family including my children came to see me. I was intubated so I couldn’t talk but I was able to communicate by writing on a piece of paper. I don’t remember too much from this time but remember touching my baby’s head. She has so much hair! This is the day when serious discussions about a left ventricular assist device (LVAD) vs. a total artificial heart (TAH) were had in order to bridge me to heart transplant.

Medical terminology time!
- LVAD
- Pump implanted in the chest to help the heart pump blood.
- TAH
- Pump implanted to provide circulation and replace heart ventricles.
An LVAD would be the preferred option because unlike the TAH, the LVAD doesn’t replace the heart but rather just helps it do what it is supposed to do. Since it isn’t replacing your heart, there is also the chance that your heart could recover. With the TAH, your only next step is a heart transplant.
On the 26th, I was still communicating quite a bit even with my sedation being quite high which was actually really surprising to the nurses. That day my family received some optimistic news about the right side of my heart and the possibility of just doing an LVAD.
But things are never that easy, are they? Everything started to go downhill on the 27th. I destabilized significantly in the morning and was bleeding all over the place (a common reaction to being on ECMO). Due to the bleeding, I had to get 4 units of blood and 1 unit of platelets. Also, since I had just had a baby, I had terrible vaginal bleeding. They could tell that my anxiety was increasing so I had to be deeply sedated and remain intubated.
Throughout the day there were multiple TTEs and a lot of debate over the LVAD or the TAH but ended up that it would most likely have to be the TAH. Ultimately, however, the way my heart looked after they opened my chest and the transesophageal echocardiogram (TEE) in the operating room would make the final decision.
More medical terminology!
- TEE
- Using a probe that goes down the throat, this can give clearer pictures of the heart than TTE
My bleeding didn’t stop all night and I required 2 more units of blood. On the 29th there was a lot of concern about the bleeding leading into surgery. It was decided that I would get the TAH. During the surgery, I required several more units of blood and was very oozy. I never knew oozy was a medical term but I ended up hearing it a lot while I was in the hospital. Being oozy is what I would call bleeding but I guess that is somewhat different.
According to the CT surgeons report, the surgery went very well and they were able to close my chest. Their biggest concern was still my bleeding and I remained closely monitored.
My husband’s parents and sister came out that day to support us and help with the kids. That same day he posted about our situation on Facebook. We got an incredible amount of support right from the start with prayers, good vibes and financial donations coming in through the GoFundMe page. It was really special to see all the support we were getting from people all over the world.

I especially needed that support when I woke up to find that I no longer had a heart.



That had to be hard to handle waking up and finding out u no longer have a heart
Love you Jen! This blog is such a beautiful way to spread awareness and tell your story. ❤️
Muchas gracias. ?Como puedo iniciar sesion?
allergy medication without side effects how long do antihistamines take to work doctor prescribed allergy medication
non drowsy allergy medication canada kirkland allergy pills toronto top rated pill for itching
http://amoxil.icu/# order amoxicillin no prescription
http://ciprofloxacin.life/# where can i buy cipro online
50 mg prednisone tablet: medicine prednisone 5mg – buy prednisone without a prescription
http://amoxil.icu/# amoxicillin medicine over the counter
buying clomid for sale: can i get clomid – how to get clomid pills
generic zithromax online paypal: where can i get zithromax – where to get zithromax
cytotec pills buy online: Abortion pills online – cytotec pills buy online
http://lisinoprilbestprice.store/# lisinopril 20 mg tablet cost
zithromax cost uk: zithromax online no prescription – buy zithromax online cheap
http://cytotec.icu/# cytotec buy online usa
https://nolvadex.fun/# pct nolvadex
tamoxifen moa: tamoxifen mechanism of action – tamoxifen and osteoporosis
lisinopril for sale online lisinopril 10 mg 12.5mg lisinopril 5 mg daily
tamoxifen bone density: how to prevent hair loss while on tamoxifen – how to lose weight on tamoxifen
http://zithromaxbestprice.icu/# zithromax online usa
doxycycline 100mg price: doxycycline 50 mg – doxycycline hydrochloride 100mg
lisinopril price uk: 60 lisinopril cost – prinivil lisinopril
http://nolvadex.fun/# tamoxifen dosage
http://doxycyclinebestprice.pro/# generic for doxycycline
top 10 strongest sleeping pills order modafinil 200mg online
tamoxifen chemo: generic tamoxifen – tamoxifen hormone therapy
zestril 25 mg buy lisinopril 2.5 mg online lisinopril 3972
diphenhydramine hcl nighttime sleep aid buy generic modafinil
zestoretic 20 mg: lisinopril 10 mg for sale without prescription – medication lisinopril 5 mg
https://nolvadex.fun/# buy tamoxifen
raloxifene vs tamoxifen: buy tamoxifen – tamoxifen medication
https://doxycyclinebestprice.pro/# doxycycline 100mg
lisinopril 40 mg for sale: lisinopril 5 mg prices – lisinopril 100mcg
https://cytotec.icu/# buy cytotec in usa
tamoxifen moa: tamoxifen 20 mg – nolvadex vs clomid
tamoxifen and uterine thickening nolvadex d nolvadex vs clomid
100 mg lisinopril: zestril 5 mg tablets – lisinopril 5 mg uk price
https://doxycyclinebestprice.pro/# how to order doxycycline
pharmacies in mexico that ship to usa: buying prescription drugs in mexico – medication from mexico pharmacy mexicopharm.com
http://mexicopharm.com/# mexico drug stores pharmacies mexicopharm.com
http://indiapharm.llc/# Online medicine order indiapharm.llc
buy medicines online in india: Online India pharmacy – top 10 pharmacies in india indiapharm.llc
maple leaf pharmacy in canada: Canadian online pharmacy – cheap canadian pharmacy canadapharm.life
canadian pharmacies online: Canadian online pharmacy – canada cloud pharmacy canadapharm.life
http://indiapharm.llc/# top 10 online pharmacy in india indiapharm.llc
safe reliable canadian pharmacy: Cheapest drug prices Canada – canadian drug stores canadapharm.life
canada drugs online Canadian online pharmacy legit canadian online pharmacy canadapharm.life
http://mexicopharm.com/# purple pharmacy mexico price list mexicopharm.com
buy medicines online in india: indian pharmacy to usa – п»їlegitimate online pharmacies india indiapharm.llc
https://indiapharm.llc/# india online pharmacy indiapharm.llc
buy prednisone tablets order prednisone 20mg
top online pharmacy india: India Post sending medicines to USA – indianpharmacy com indiapharm.llc
canadian pharmacy prices: Canadian online pharmacy – canadian pharmacy world reviews canadapharm.life
http://canadapharm.life/# canadian drug canadapharm.life
vipps canadian pharmacy: canadian pharmacy online – canadian online pharmacy reviews canadapharm.life
mexican online pharmacies prescription drugs: Medicines Mexico – mexican mail order pharmacies mexicopharm.com
cheapest online pharmacy india Medicines from India to USA online top online pharmacy india indiapharm.llc
https://mexicopharm.com/# reputable mexican pharmacies online mexicopharm.com
world pharmacy india: indian pharmacy paypal – indianpharmacy com indiapharm.llc
mexican mail order pharmacies: mexico drug stores pharmacies – buying prescription drugs in mexico mexicopharm.com
http://indiapharm.llc/# Online medicine home delivery indiapharm.llc
prednisone 10mg brand order prednisone pill
top 10 online pharmacy in india: India pharmacy of the world – Online medicine home delivery indiapharm.llc
https://canadapharm.life/# onlinecanadianpharmacy 24 canadapharm.life
canada ed drugs: Canadian online pharmacy – canadian pharmacies compare canadapharm.life
medication from mexico pharmacy: mexican drugstore online – mexican pharmaceuticals online mexicopharm.com
https://mexicopharm.com/# mexican mail order pharmacies mexicopharm.com
п»їLevitra price: Buy Levitra 20mg online – Levitra 20 mg for sale
http://levitradelivery.pro/# п»їLevitra price
https://sildenafildelivery.pro/# sildenafil soft tabs 100mg
erectile dysfunction drug: cheapest ed pills – best ed pills at gnc
http://levitradelivery.pro/# Buy generic Levitra online
ed meds: buy ed drugs online – erection pills
tadalafil price comparison: Tadalafil 20mg price in Canada – canadian online pharmacy tadalafil
https://tadalafildelivery.pro/# tadalafil capsules 20mg
where can i buy tadalafil Tadalafil 20mg price in Canada buy generic tadalafil online uk
http://kamagradelivery.pro/# cheap kamagra
https://levitradelivery.pro/# Levitra tablet price
Buy Vardenafil 20mg: п»їLevitra price – Cheap Levitra online
medicine for stomach acid problems purchase glimepiride pills
http://kamagradelivery.pro/# super kamagra
buy tadalafil 20mg price canada: Buy tadalafil online – best online tadalafil
ed drugs list: erection pills over the counter – erectile dysfunction pills
tadalafil 20 mg mexico: tadalafil without a doctor prescription – tadalafil tablets in india
https://sildenafildelivery.pro/# sildenafil 50 mg canada
erection pills that work buy ed drugs online erection pills that work
tadalafil tablets: Tadalafil 20mg price in Canada – buy cheap tadalafil online
http://edpillsdelivery.pro/# medicine erectile dysfunction
http://levitradelivery.pro/# Vardenafil buy online
acetaminophen for abdominal pain zyloprim 100mg tablet
tadalafil online canada: cheap tadalafil canada – cost of generic tadalafil
http://paxlovid.guru/# buy paxlovid online
http://stromectol.guru/# ivermectin 0.5%
paxlovid price Buy Paxlovid privately paxlovid covid
http://clomid.auction/# can i order clomid without prescription
amoxicillin 750 mg price: cheap amoxicillin – buy amoxicillin over the counter uk
https://clomid.auction/# cost of cheap clomid no prescription
http://stromectol.guru/# what is minocycline prescribed for
http://clomid.auction/# order clomid tablets
paxlovid price Paxlovid buy online paxlovid india
https://stromectol.guru/# ivermectin 3mg for lice
can i get generic clomid price: Buy Clomid online – can you get generic clomid
dermatologist prescribed acne cream order avlosulfon 100mg generic prescription medication for severe acne
http://clomid.auction/# how can i get cheap clomid without dr prescription
https://prednisone.auction/# 50mg prednisone tablet
https://stromectol.guru/# ivermectin 1%cream
https://paxlovid.guru/# buy paxlovid online
ivermectin uk: stromectol 3 mg tablet – ivermectin 24 mg
paxlovid price Paxlovid buy online paxlovid price
acne treatment for adults dermatologist order monobenzone online cheap will pimple get wase when taking fulcin
https://paxlovid.guru/# paxlovid pill
http://paxlovid.guru/# paxlovid pill
https://paxlovid.guru/# paxlovid pharmacy
https://prednisone.auction/# prednisone canada pharmacy
buy lisinopril 2.5 mg: buy lisinopril online – lisinopril 40 mg daily
lasix for sale Over The Counter Lasix furosemida
http://furosemide.pro/# lasix side effects
lisinopril with out prescription: buy lisinopril canada – cheap lisinopril 40 mg
http://azithromycin.store/# can you buy zithromax over the counter
ordering lisinopril without a prescription: over the counter lisinopril – generic zestoretic
http://furosemide.pro/# furosemida
order generic propecia no prescription: buying cheap propecia without insurance – buy cheap propecia pills
https://finasteride.men/# order generic propecia without rx
prescription medication for severe allergies order cetirizine 10mg generic allergy pills for rash
buy zithromax without presc buy zithromax z-pak online zithromax cost canada
Abortion pills online: Buy Abortion Pills Online – buy cytotec pills online cheap
http://furosemide.pro/# furosemida 40 mg
http://misoprostol.shop/# buy cytotec pills
buy cheap propecia without a prescription: Best place to buy propecia – cost cheap propecia tablets
http://azithromycin.store/# buy zithromax 1000 mg online
cost generic propecia without prescription: propecia medication – buy propecia without rx
generic propecia without insurance: buy propecia – get generic propecia without rx
http://lisinopril.fun/# lisinopril brand name
lasix 40 mg Over The Counter Lasix lasix tablet
https://furosemide.pro/# lasix generic name
buy cheap propecia online: Finasteride buy online – cheap propecia
lasix: Buy Furosemide – lasix for sale
https://azithromycin.store/# generic zithromax medicine
http://finasteride.men/# cost of cheap propecia pill
generic lasix: Buy Lasix – lasix 100 mg
furosemida Over The Counter Lasix furosemida 40 mg
buying cheap propecia without prescription: Best place to buy propecia – order cheap propecia
http://azithromycin.store/# buy zithromax
http://lisinopril.fun/# prinivil 25 mg
buying propecia: order propecia without rx – buying generic propecia for sale
https://azithromycin.store/# zithromax 500 without prescription
buy misoprostol over the counter: buy cytotec over the counter – buy misoprostol over the counter
zithromax cost australia zithromax purchase online generic zithromax india
where can i buy zithromax in canada: zithromax best price – where can i buy zithromax in canada
https://lisinopril.fun/# lisinopril 10 mg for sale without prescription
generic lasix: lasix online – lasix uses
http://furosemide.pro/# lasix medication
buy lisinopril without a prescription: cheapest lisinopril – 10mg generic 10mg lisinopril
https://misoprostol.shop/# purchase cytotec
http://finasteride.men/# get propecia without a prescription
can you buy zithromax over the counter in australia buy zithromax over the counter zithromax tablets
buying generic propecia price: cheap propecia without a prescription – cost generic propecia prices
http://avanafilitalia.online/# farmacia online
farmacia online senza ricetta: kamagra gold – farmacia online migliore
https://sildenafilitalia.men/# le migliori pillole per l’erezione
http://tadalafilitalia.pro/# farmacia online miglior prezzo
types of nausea medication cefadroxil for sale online
alternativa al viagra senza ricetta in farmacia: viagra senza ricetta – alternativa al viagra senza ricetta in farmacia
viagra naturale in farmacia senza ricetta viagra prezzo farmacia senza ricetta recensioni
https://tadalafilitalia.pro/# comprare farmaci online con ricetta
https://tadalafilitalia.pro/# migliori farmacie online 2023
viagra originale in 24 ore contrassegno: sildenafil 100mg prezzo – viagra generico in farmacia costo
migliori farmacie online 2023: comprare avanafil senza ricetta – farmacia online senza ricetta
http://sildenafilitalia.men/# viagra 50 mg prezzo in farmacia
farmacie online affidabili: kamagra oral jelly – farmacie online autorizzate elenco
https://kamagraitalia.shop/# comprare farmaci online con ricetta
farmacie online sicure farmacia online miglior prezzo farmacia online miglior prezzo
http://farmaciaitalia.store/# farmacie online autorizzate elenco
comprare farmaci online all’estero: kamagra gel – comprare farmaci online con ricetta
order generic isotretinoin isotretinoin drug buy accutane 40mg
farmacie online sicure: kamagra gel – farmacia online miglior prezzo
https://farmaciaitalia.store/# comprare farmaci online con ricetta
https://kamagraitalia.shop/# farmacie online autorizzate elenco
п»їfarmacia online migliore: kamagra gel – farmacia online migliore
le migliori pillole per l’erezione: viagra online siti sicuri – viagra acquisto in contrassegno in italia
п»їfarmacia online migliore avanafil generico п»їfarmacia online migliore
http://sildenafilitalia.men/# viagra 100 mg prezzo in farmacia
http://sildenafilitalia.men/# pillole per erezione immediata
top farmacia online: farmacia online migliore – migliori farmacie online 2023
http://tadalafilitalia.pro/# farmacie online autorizzate elenco
dove acquistare viagra in modo sicuro: viagra online siti sicuri – miglior sito dove acquistare viagra
https://tadalafilitalia.pro/# acquistare farmaci senza ricetta
https://tadalafilitalia.pro/# farmacia online miglior prezzo
canadian pharmacy 365: pharmacy canadian superstore – ed meds online canada
best rated canadian pharmacy: canada drugs online review – canadian discount pharmacy
http://mexicanpharm.store/# mexican mail order pharmacies
world pharmacy india cheapest online pharmacy india india pharmacy
http://canadapharm.shop/# canadian pharmacy drugs online
cheapest online pharmacy india: online pharmacy india – п»їlegitimate online pharmacies india
https://indiapharm.life/# reputable indian online pharmacy
best online pharmacies in mexico: mexican border pharmacies shipping to usa – pharmacies in mexico that ship to usa
http://mexicanpharm.store/# best online pharmacies in mexico
mexican rx online: mexico pharmacies prescription drugs – mexican border pharmacies shipping to usa
mexico pharmacies prescription drugs: mexico drug stores pharmacies – purple pharmacy mexico price list
canada online pharmacy: canadian pharmacy meds – canadian drugs pharmacy
best canadian pharmacy to order from legitimate canadian pharmacy online best canadian pharmacy to order from
http://mexicanpharm.store/# mexican pharmacy
http://indiapharm.life/# Online medicine order
medicine in mexico pharmacies: buying prescription drugs in mexico – pharmacies in mexico that ship to usa
https://canadapharm.shop/# recommended canadian pharmacies
Online medicine order: best india pharmacy – Online medicine order
reputable indian online pharmacy: indian pharmacy online – india pharmacy
http://mexicanpharm.store/# mexico pharmacies prescription drugs
order amoxil 500mg generic buy amoxicillin medication amoxicillin uk
mexico drug stores pharmacies: mexican drugstore online – mexico drug stores pharmacies
https://mexicanpharm.store/# mexican drugstore online
canadian pharmacy 24h com: best canadian pharmacy – reputable canadian pharmacy
https://mexicanpharm.store/# mexican drugstore online
online shopping pharmacy india cheapest online pharmacy india indianpharmacy com
canada ed drugs: best canadian pharmacy – canada pharmacy online legit
http://indiapharm.life/# online shopping pharmacy india
mexican online pharmacies prescription drugs: best online pharmacies in mexico – reputable mexican pharmacies online
mexican drugstore online: pharmacies in mexico that ship to usa – reputable mexican pharmacies online
https://canadapharm.shop/# canadian pharmacy online reviews
pharmacies in mexico that ship to usa: medicine in mexico pharmacies – mexican pharmaceuticals online
https://canadapharm.shop/# canadian drugs online
recommended canadian pharmacies: canada ed drugs – precription drugs from canada
http://mexicanpharm.store/# buying from online mexican pharmacy
https://indiapharm.life/# buy medicines online in india
top 10 pharmacies in india: pharmacy website india – india pharmacy
my canadian pharmacy review: canadian pharmacy ratings – canadian drug pharmacy
canadian pharmacy world my canadian pharmacy reviews pharmacies in canada that ship to the us
http://mexicanpharm.store/# buying from online mexican pharmacy
cheapest online pharmacy india: Online medicine order – indianpharmacy com
buy cytotec pills online cheap: buy cytotec over the counter – order cytotec online
zithromax 500mg cost buy azithromycin order zithromax 500mg generic
https://nolvadex.pro/# nolvadex half life
http://prednisonepharm.store/# where to buy prednisone uk
Their mobile app makes managing my medications so easy http://prednisonepharm.store/# prednisone pharmacy prices
generic zithromax india buy zithromax online australia cheap zithromax pills
generic zithromax 500mg: zithromax tablets – generic zithromax online paypal
They’re at the forefront of international pharmaceutical innovations https://prednisonepharm.store/# buy prednisone tablets online
http://clomidpharm.shop/# cost of clomid without a prescription
gabapentin without prescription buy gabapentin 600mg sale
Their dedication to global health is evident http://nolvadex.pro/# tamoxifen side effects forum
https://clomidpharm.shop/# cheap clomid online
where can i buy zithromax in canada: zithromax tablets for sale – zithromax
https://nolvadex.pro/# tamoxifen bone density
A place where customer health is the top priority https://clomidpharm.shop/# get generic clomid price
purchase cytotec cytotec buy online usa buy cytotec pills
http://zithromaxpharm.online/# buy azithromycin zithromax
cost of generic zithromax: zithromax canadian pharmacy – cost of generic zithromax
Their health seminars are always enlightening https://prednisonepharm.store/# prednisone 10 mg online
https://prednisonepharm.store/# prednisone pill 20 mg
what is tamoxifen used for: cost of tamoxifen – tamoxifen breast cancer prevention
The best in town, without a doubt https://zithromaxpharm.online/# can you buy zithromax online
http://zithromaxpharm.online/# where to get zithromax over the counter
safe and effective drugs are available http://clomidpharm.shop/# how can i get generic clomid without insurance
Misoprostol 200 mg buy online: order cytotec online – cytotec buy online usa
can you get generic clomid prices buy cheap clomid without dr prescription can you get generic clomid for sale
http://zithromaxpharm.online/# where can i purchase zithromax online
https://prednisonepharm.store/# cost of prednisone
Their home delivery service is top-notch http://clomidpharm.shop/# how to buy generic clomid for sale
azithromycin uk purchase azipro generic azithromycin medication
zithromax for sale us: zithromax without prescription – zithromax buy
http://zithromaxpharm.online/# zithromax capsules 250mg
Some are medicines that help people when doctors prescribe https://prednisonepharm.store/# prednisone 20mg by mail order
zithromax azithromycin: how to get zithromax online – zithromax capsules 250mg
new treatments for ed best over the counter ed pills ed drugs compared
sildenafil without a doctor’s prescription: prescription drugs online without doctor – ed meds online without doctor prescription
oral furosemide 100mg buy lasix sale diuretic
https://edpills.bid/# buy ed pills online
mexican drug pharmacy: canada rx – canadian drugs without any prescriptions
non prescription ed pills buy ed pills cheap ed drugs
medicine erectile dysfunction: generic ed pills – best erectile dysfunction pills
prescription without a doctor’s prescription https://edwithoutdoctorprescription.store/# mexican pharmacy without prescription
canadian pharmacies without an rx
https://edwithoutdoctorprescription.store/# ed meds online without prescription or membership
canadian drugs mexican pharmacies online online pharmacies legitimate
http://edpills.bid/# best pill for ed
best non prescription ed pills: generic viagra without a doctor prescription – ed meds online without doctor prescription
perscription drugs without perscription canada pharmacies without script canadian pharmacy 365
http://reputablepharmacies.online/# high street discount pharmacy
buy erection pills: medicine for impotence – online ed pills
generic ed pills cheap erectile dysfunction top ed drugs
best canadian online pharmacy reviews: non prescription medicine pharmacy – canada pharmacy world
the best canadian pharmacy http://edpills.bid/# cheap ed drugs
canadian drug pharmacy
http://edpills.bid/# buying ed pills online
canadian drug store coupon: canadian overnight pharmacy – us online pharmacy
safe reliable canadian pharmacy canadian pharmacy cheap high street discount pharmacy
https://edwithoutdoctorprescription.store/# non prescription erection pills
omnacortil 10mg price buy generic prednisolone 10mg buy omnacortil 5mg without prescription
prescription drugs canada the canadian pharmacy mail order pharmacies
https://reputablepharmacies.online/# trustworthy canadian pharmacy
nabp approved canadian pharmacies: safe reliable canadian pharmacy – prescription drugs canada
canadian pharcharmy online prescription drug price check online drugstore coupon
pharmacy prices compare: mail order drugs without a prescription – online canadian pharmacies
http://edpills.bid/# medication for ed dysfunction
generic ed drugs: ed pill – pills for erection
price prescriptions international pharmacies that ship to the usa pharmacy price comparison
non prescription ed pills: meds online without doctor prescription – buy prescription drugs from india
https://edwithoutdoctorprescription.store/# ed meds online without doctor prescription
canadian pharmacy non prescription canadian pharmacy no rx needed prescription drugs online without doctor
reputable mexican pharmacies online: mexican pharmacy online – mexico pharmacy mexicanpharmacy.win
http://indianpharmacy.shop/# best india pharmacy indianpharmacy.shop
buying prescription drugs in mexico mexican pharmacy online best online pharmacies in mexico mexicanpharmacy.win
mexican pharmaceuticals online: Mexico pharmacy – mexico drug stores pharmacies mexicanpharmacy.win
https://indianpharmacy.shop/# indian pharmacies safe indianpharmacy.shop
india pharmacy Cheapest online pharmacy india online pharmacy indianpharmacy.shop
http://mexicanpharmacy.win/# medication from mexico pharmacy mexicanpharmacy.win
reputable indian pharmacies: international medicine delivery from india – indian pharmacy paypal indianpharmacy.shop
https://mexicanpharmacy.win/# mexican online pharmacies prescription drugs mexicanpharmacy.win
canadian mail order pharmacy
canada drugs online review Canada Pharmacy best rated canadian pharmacy canadianpharmacy.pro
https://canadianpharmacy.pro/# canada online pharmacy canadianpharmacy.pro
indian pharmacy paypal: Cheapest online pharmacy – best online pharmacy india indianpharmacy.shop
india online pharmacy Best Indian pharmacy Online medicine order indianpharmacy.shop
http://canadianpharmacy.pro/# safe online pharmacies in canada canadianpharmacy.pro
mexican mail order pharmacies mexican pharmacy online mexico drug stores pharmacies mexicanpharmacy.win
http://canadianpharmacy.pro/# online canadian pharmacy reviews canadianpharmacy.pro
https://mexicanpharmacy.win/# best online pharmacies in mexico mexicanpharmacy.win
http://mexicanpharmacy.win/# mexican pharmacy mexicanpharmacy.win
world pharmacy india
canadian online pharmacy Canadian pharmacy online canadian pharmacy victoza canadianpharmacy.pro
http://indianpharmacy.shop/# best india pharmacy indianpharmacy.shop
https://mexicanpharmacy.win/# mexico drug stores pharmacies mexicanpharmacy.win
north canadian pharmacy
buy amoxil 500mg pill generic amoxil 500mg buy cheap amoxil
http://canadianpharmacy.pro/# canada drugs reviews canadianpharmacy.pro
indian pharmacy paypal
buying prescription drugs in mexico Medicines Mexico mexican rx online mexicanpharmacy.win
https://mexicanpharmacy.win/# reputable mexican pharmacies online mexicanpharmacy.win
doxycycline 100mg ca doxycycline for sale
http://mexicanpharmacy.win/# mexican drugstore online mexicanpharmacy.win
mail order pharmacy india
medicine in mexico pharmacies Medicines Mexico mexican pharmaceuticals online mexicanpharmacy.win
https://mexicanpharmacy.win/# medication from mexico pharmacy mexicanpharmacy.win
https://mexicanpharmacy.win/# purple pharmacy mexico price list mexicanpharmacy.win
http://mexicanpharmacy.win/# mexico pharmacies prescription drugs mexicanpharmacy.win
indian pharmacy
https://mexicanpharmacy.win/# medicine in mexico pharmacies mexicanpharmacy.win
buy canadian drugs online
reputable indian online pharmacy indian pharmacy to usa india pharmacy indianpharmacy.shop
https://canadianpharmacy.pro/# best rated canadian pharmacy canadianpharmacy.pro
https://canadianpharmacy.pro/# best rated canadian pharmacy canadianpharmacy.pro
http://mexicanpharmacy.win/# mexican drugstore online mexicanpharmacy.win
online pharmacy india
indianpharmacy com Order medicine from India to USA pharmacy website india indianpharmacy.shop
http://canadianpharmacy.pro/# canadian pharmacy 24 com canadianpharmacy.pro
https://indianpharmacy.shop/# buy prescription drugs from india indianpharmacy.shop
buy prescription drugs from india
pharmacy website india international medicine delivery from india online pharmacy india indianpharmacy.shop
https://indianpharmacy.shop/# indian pharmacy indianpharmacy.shop
http://canadianpharmacy.pro/# recommended canadian pharmacies canadianpharmacy.pro
Online medicine home delivery
order ventolin inhalator ventolin 4mg over the counter order ventolin inhalator online cheap
Pharmacie en ligne fiable: Pharmacie en ligne livraison rapide – Pharmacie en ligne France
Pharmacie en ligne fiable Acheter Cialis Acheter mГ©dicaments sans ordonnance sur internet
http://levitrasansordonnance.pro/# Pharmacies en ligne certifiées
Pharmacie en ligne livraison 24h kamagra gel Pharmacie en ligne sans ordonnance
Prix du Viagra en pharmacie en France: Viagra generique en pharmacie – SildГ©nafil 100mg pharmacie en ligne
Pharmacie en ligne livraison 24h: pharmacie en ligne sans ordonnance – acheter mГ©dicaments Г l’Г©tranger
https://pharmadoc.pro/# acheter medicament a l etranger sans ordonnance
pharmacie ouverte 24/24
http://cialissansordonnance.shop/# Pharmacie en ligne sans ordonnance
acheter mГ©dicaments Г l’Г©tranger cialis generique Pharmacies en ligne certifiГ©es
Pharmacie en ligne fiable: levitrasansordonnance.pro – pharmacie ouverte 24/24
https://acheterkamagra.pro/# Pharmacie en ligne fiable
Pharmacie en ligne sans ordonnance: cialissansordonnance.shop – acheter mГ©dicaments Г l’Г©tranger
п»їpharmacie en ligne levitra generique sites surs pharmacie ouverte 24/24
https://pharmadoc.pro/# Pharmacie en ligne livraison rapide
augmentin usa amoxiclav sale
acheter mГ©dicaments Г l’Г©tranger: PharmaDoc.pro – pharmacie ouverte 24/24
http://pharmadoc.pro/# Acheter mГ©dicaments sans ordonnance sur internet
Acheter mГ©dicaments sans ordonnance sur internet
Acheter mГ©dicaments sans ordonnance sur internet: pharmacie en ligne – Pharmacie en ligne pas cher
https://cialissansordonnance.shop/# Pharmacie en ligne livraison gratuite
Pharmacie en ligne sans ordonnance: cialis prix – Pharmacie en ligne France
Acheter mГ©dicaments sans ordonnance sur internet kamagra en ligne pharmacie ouverte
https://acheterkamagra.pro/# Pharmacie en ligne pas cher
п»їpharmacie en ligne: cialissansordonnance.shop – Pharmacie en ligne livraison 24h
pharmacie ouverte kamagra livraison 24h acheter mГ©dicaments Г l’Г©tranger
http://viagrasansordonnance.pro/# Viagra Pfizer sans ordonnance
buy levothroid online levothyroxine price levothyroxine for sale
Pharmacies en ligne certifiГ©es: Acheter Cialis 20 mg pas cher – п»їpharmacie en ligne
prednisone price south africa: cheap generic prednisone – prednisone 20 mg tablet
minocin 50 mg for scabies ivermectin 400 mg brands buy ivermectin cream for humans
https://amoxicillin.bid/# order amoxicillin uk
buy vardenafil buy levitra generic
https://clomiphene.icu/# can i purchase clomid without rx
cheap stromectol: ivermectin cost in usa – stromectol generic name
where can i get generic clomid no prescription buying clomid without dr prescription cost clomid without rx
http://clomiphene.icu/# buying generic clomid without dr prescription
where can i buy amoxocillin: amoxicillin for sale – buy amoxicillin 500mg online
ivermectin 6mg dosage: ivermectin virus – ivermectin 1 cream generic
prednisone 2 5 mg order prednisone 100g online without prescription prednisone without prescription.net
http://amoxicillin.bid/# amoxicillin buy canada
where can i get clomid no prescription: cheap clomid without rx – can you get cheap clomid without insurance
http://amoxicillin.bid/# how to get amoxicillin over the counter
order cheap clomid can i purchase clomid without insurance how can i get clomid without a prescription
ivermectin 6mg: ivermectin buy canada – stromectol generic
http://amoxicillin.bid/# amoxicillin price without insurance
buy clomid 50mg online cheap purchase clomiphene online buy clomid sale
https://clomiphene.icu/# how can i get generic clomid without dr prescription
amoxicillin over counter: can i purchase amoxicillin online – amoxicillin brand name
order tizanidine for sale zanaflex sale buy zanaflex medication
stromectol generic ivermectin 6 stromectol 3 mg tablet price
buy prednisone without prescription: buy prednisone 1 mg mexico – prednisone 20mg by mail order
http://ivermectin.store/# stromectol medication
order tizanidine sale cheap zanaflex where can i buy tizanidine
amoxicillin 500mg prescription: rexall pharmacy amoxicillin 500mg – where to buy amoxicillin pharmacy
zithromax online paypal zithromax cost australia zithromax 500 mg lowest price pharmacy online
https://prednisonetablets.shop/# buy prednisone 10 mg
how much is zithromax 250 mg: buy zithromax 500mg online – zithromax 500 tablet
prednisone pak: prednisone 10 tablet – 100 mg prednisone daily
http://clomiphene.icu/# can you get cheap clomid without prescription
buying generic clomid without prescription can you buy clomid without a prescription order clomid without dr prescription
http://amoxicillin.bid/# amoxicillin tablets in india
prednisone coupon: prednisone without a prescription – where to buy prednisone 20mg
zithromax 500mg price in india how to get zithromax zithromax 250mg
http://clomiphene.icu/# where can i get generic clomid pills
deltasone 5mg brand buy prednisone medication order generic prednisone 5mg
order rybelsus 14 mg without prescription purchase rybelsus pill semaglutide over the counter
canadian neighbor pharmacy Licensed Online Pharmacy vipps canadian pharmacy canadianpharm.store
mexico drug stores pharmacies: Online Mexican pharmacy – mexican drugstore online mexicanpharm.shop
https://indianpharm.store/# reputable indian online pharmacy indianpharm.store
buy prednisone 20mg sale purchase deltasone prednisone 5mg cost
indian pharmacy: Online medicine home delivery – indian pharmacies safe indianpharm.store
pharmacy website india: order medicine from india to usa – Online medicine order indianpharm.store
mexico pharmacy Certified Pharmacy from Mexico mexico drug stores pharmacies mexicanpharm.shop
https://canadianpharm.store/# pharmacy rx world canada canadianpharm.store
http://canadianpharm.store/# reddit canadian pharmacy canadianpharm.store
canadian pharmacy king: Canadian International Pharmacy – adderall canadian pharmacy canadianpharm.store
best online pharmacies in mexico Certified Pharmacy from Mexico reputable mexican pharmacies online mexicanpharm.shop
http://mexicanpharm.shop/# buying from online mexican pharmacy mexicanpharm.shop
canadian pharmacy mall: Canadian International Pharmacy – best online canadian pharmacy canadianpharm.store
mexico pharmacy: Certified Pharmacy from Mexico – mexican drugstore online mexicanpharm.shop
http://mexicanpharm.shop/# mexican mail order pharmacies mexicanpharm.shop
mexican drugstore online: reputable mexican pharmacies online – buying prescription drugs in mexico mexicanpharm.shop
mexican pharmaceuticals online Online Mexican pharmacy mexico pharmacy mexicanpharm.shop
mexican drugstore online: Online Mexican pharmacy – п»їbest mexican online pharmacies mexicanpharm.shop
https://canadianpharm.store/# best canadian pharmacy to buy from canadianpharm.store
buying from online mexican pharmacy: Online Pharmacies in Mexico – mexico drug stores pharmacies mexicanpharm.shop
mexican rx online Online Pharmacies in Mexico purple pharmacy mexico price list mexicanpharm.shop
http://canadianpharm.store/# legitimate canadian mail order pharmacy canadianpharm.store
order isotretinoin without prescription accutane 20mg without prescription isotretinoin 10mg generic
https://mexicanpharm.shop/# mexican mail order pharmacies mexicanpharm.shop
online pharmacy canada: canadian world pharmacy – reputable canadian pharmacy canadianpharm.store
buy rybelsus 14 mg rybelsus for sale online buy rybelsus 14mg online
online pharmacy india: international medicine delivery from india – online pharmacy india indianpharm.store
safe reliable canadian pharmacy Best Canadian online pharmacy canadian pharmacy online ship to usa canadianpharm.store
isotretinoin 20mg price brand accutane isotretinoin 40mg sale
http://mexicanpharm.shop/# mexico drug stores pharmacies mexicanpharm.shop
best canadian pharmacy online: Canadian International Pharmacy – canadian pharmacy king reviews canadianpharm.store
order ventolin 4mg for sale cost ventolin 2mg get antihistamine pills online
http://canadianpharm.store/# canadian pharmacy mall canadianpharm.store
Online medicine order: international medicine delivery from india – india pharmacy indianpharm.store
world pharmacy india international medicine delivery from india best online pharmacy india indianpharm.store
http://indianpharm.store/# indianpharmacy com indianpharm.store
http://canadianpharm.store/# legal canadian pharmacy online canadianpharm.store
п»їlegitimate online pharmacies india: Indian pharmacy to USA – indianpharmacy com indianpharm.store
canadian pharmacies compare: best canadian pharmacy online – canadian discount pharmacy canadianpharm.store
best online pharmacy india Indian pharmacy to USA top 10 online pharmacy in india indianpharm.store
cheapest online pharmacy india: international medicine delivery from india – online shopping pharmacy india indianpharm.store
https://canadianpharm.store/# the canadian pharmacy canadianpharm.store
best canadian online pharmacy: Canadian Pharmacy – canadian pharmacy prices canadianpharm.store
mexican border pharmacies shipping to usa Online Mexican pharmacy mexican drugstore online mexicanpharm.shop
canadian pharmacies that deliver to the us: Canadian Pharmacy – canadian pharmacy 24 com canadianpharm.store
https://mexicanpharm.shop/# medicine in mexico pharmacies mexicanpharm.shop
order ventolin generic generic albuterol 2mg albuterol pills
purchase amoxil online amoxil 500mg oral buy amoxil 500mg for sale
canadian mail order pharmacy: Best Canadian online pharmacy – canadian drug canadianpharm.store
best online pharmacies in mexico Certified Pharmacy from Mexico п»їbest mexican online pharmacies mexicanpharm.shop
https://indianpharm.store/# buy medicines online in india indianpharm.store
indian pharmacy online: order medicine from india to usa – cheapest online pharmacy india indianpharm.store
http://indianpharm.store/# Online medicine order indianpharm.store
amoxicillin 500mg sale buy amoxicillin 250mg pills buy generic amoxicillin
mexican pharmaceuticals online Certified Pharmacy from Mexico mexican pharmaceuticals online mexicanpharm.shop
buy prescription drugs from india: Indian pharmacy to USA – india pharmacy indianpharm.store
purchase augmentin augmentin 1000mg uk augmentin 375mg oral
canadian pharmacy generic viagra legitimate canadian pharmacy online mexican mail order pharmacy
online prescriptions without a doctor: discount online canadian pharmacy – meds without a doctor s prescription canada
https://canadadrugs.pro/# best online pharmacy no prescription
canadian drugs cialis: the canadian pharmacy – safe online pharmacy
great canadian pharmacy: online pharmacies canadian – online pharmacy store
prescription drugs prices: canada pharmacies without script – discount canadian pharmacy
international pharmacy canadian pharmacy generic viagra canadian pharmacy testosterone
https://canadadrugs.pro/# safe canadian pharmacy
reputable canadian pharmacy: azithromycin canadian pharmacy – canadian mail order drug companies
canada pharmacy online reviews price prescriptions canadian pharmacies that ship to usa
http://canadadrugs.pro/# legitimate mexican pharmacy online
ed meds without doctor prescription: pharmacy drug store online no rx – price prescriptions
mail order pharmacy canada: most reputable canadian pharmacy – canadian pharmacy selling viagra
buy clavulanate for sale cost augmentin augmentin 375mg drug
buy azithromycin sale zithromax cost azithromycin 250mg without prescription
http://canadadrugs.pro/# canada pharmaceuticals online
online pharmacy store canadian pharmacies reviews discount prescriptions
canadian online pharmacies reviews: online canadian pharmacy – online pharmacies in usa
best pharmacy: canadian mail order meds – discount mail order pharmacy
http://canadadrugs.pro/# order prescription medicine online without prescription
no prescription online pharmacy discount pharmacies canadian pharmacy worldwide
online pharmacy no prescription necessary: best online canadian pharcharmy – canadian drug stores online
http://canadadrugs.pro/# canadian prescription prices
cheap levoxyl without prescription purchase levothyroxine generic synthroid 100mcg cost
canada pharmacy online reviews: usa online pharmacy – overseas pharmacies
http://canadadrugs.pro/# rx canada
canadapharmacy com: canadian pharmacy online no prescription – best rated canadian online pharmacy
http://canadadrugs.pro/# top online pharmacies
best online pharmacy no prescription: certified canadian pharmacy – international pharmacy
https://canadadrugs.pro/# world pharmacy
synthroid 75mcg for sale cheap levothroid sale how to get synthroid without a prescription
drug stores canada: canada pharmacy estrogen without prescription – canadian mail order viagra
order omnacortil online cheap prednisolone 20mg pills order prednisolone 10mg for sale
canada drug stores: best canadian pharmacy no prescription – canadian medicine
http://canadadrugs.pro/# online pharmacy mail order
omnacortil 5mg ca buy omnacortil 5mg generic order prednisolone online cheap
https://canadadrugs.pro/# most reputable canadian pharmacies
canadian pharmacy online no prescription needed canada pharmacy online reviews tadalafil canadian pharmacy
canadian prescription drug prices: compare medication prices – trusted online pharmacy
mexican mail order pharmacies mexican rx online mexican pharmacy
https://edpill.cheap/# best ed medications
purchase clomid clomid canada order clomid generic
http://certifiedpharmacymexico.pro/# mexican drugstore online
cialis without a doctor’s prescription cheap cialis real viagra without a doctor prescription usa
https://certifiedpharmacymexico.pro/# mexican pharmaceuticals online
ed meds online without doctor prescription: cialis without a doctor prescription canada – buy prescription drugs from canada
reputable indian pharmacies п»їlegitimate online pharmacies india indianpharmacy com
buying prescription drugs in mexico: mexico drug stores pharmacies – mexican drugstore online
http://canadianinternationalpharmacy.pro/# adderall canadian pharmacy
india pharmacy mail order Online medicine home delivery indian pharmacy online
http://canadianinternationalpharmacy.pro/# drugs from canada
canadian pharmacy no rx needed: onlinepharmaciescanada com – buying drugs from canada
https://edpill.cheap/# cheap erectile dysfunction
india pharmacy best online pharmacy india buy prescription drugs from india
clomiphene medication order serophene without prescription clomiphene 50mg over the counter
gabapentin 800mg generic neurontin 600mg tablet buy gabapentin generic
https://edpill.cheap/# mens ed pills
the canadian drugstore pharmacies in canada that ship to the us canadian pharmacy ltd
buy gabapentin 800mg generic buy gabapentin generic neurontin tablets
https://edwithoutdoctorprescription.pro/# buy prescription drugs online legally
best male ed pills: erectile dysfunction drugs – top rated ed pills
ed pills for sale ed pills comparison best male enhancement pills
https://canadianinternationalpharmacy.pro/# online canadian pharmacy review
best online pharmacies in mexico: pharmacies in mexico that ship to usa – mexico pharmacies prescription drugs
pharmacies in mexico that ship to usa pharmacies in mexico that ship to usa mexican drugstore online
http://medicinefromindia.store/# legitimate online pharmacies india
https://edwithoutdoctorprescription.pro/# non prescription erection pills
compare ed drugs ed remedies ed medications online
http://edwithoutdoctorprescription.pro/# ed meds online without doctor prescription
viagra drug price viagra buy sildenafil 50mg pill
escrow pharmacy canada pharmacy canadian superstore canadian pharmacy 24h com safe
cialis without doctor prescription: cialis without a doctor prescription canada – generic viagra without a doctor prescription
https://edpill.cheap/# medications for ed
furosemide 100mg uk furosemide pills buy lasix 40mg generic
reputable mexican pharmacies online pharmacies in mexico that ship to usa buying from online mexican pharmacy
https://medicinefromindia.store/# indian pharmacy paypal
buy lasix sale lasix 40mg usa purchase furosemide pills
п»їbest mexican online pharmacies mexican pharmaceuticals online purple pharmacy mexico price list
http://medicinefromindia.store/# india online pharmacy
En la actualidad, el software de control remoto se utiliza principalmente en el ámbito ofimático, con funciones básicas como transferencia remota de archivos y modificación de documentos.
mexican drugstore online: mexico drug stores pharmacies – medicine in mexico pharmacies
http://edwithoutdoctorprescription.pro/# ed meds online without doctor prescription
buy prescription drugs online without non prescription ed drugs prescription drugs without doctor approval
viagra for sale online brand viagra sildenafil 50mg over the counter
http://edwithoutdoctorprescription.pro/# sildenafil without a doctor’s prescription
best non prescription ed pills cialis without a doctor prescription ed meds online without doctor prescription
https://medicinefromindia.store/# india pharmacy mail order
https://medicinefromindia.store/# top online pharmacy india
best over the counter ed pills medications for ed cheap erectile dysfunction
cialis without a doctor’s prescription: non prescription ed pills – buy prescription drugs from canada cheap
http://medicinefromindia.store/# best online pharmacy india
semaglutide online buy semaglutide generic purchase rybelsus pill
reputable indian pharmacies online shopping pharmacy india reputable indian pharmacies
https://edwithoutdoctorprescription.pro/# buy cheap prescription drugs online
buy vibra-tabs acticlate medication purchase acticlate sale
canadian pharmacy online store canada pharmacy reviews precription drugs from canada
https://canadianinternationalpharmacy.pro/# canada pharmacy online legit
order acticlate for sale order monodox without prescription vibra-tabs generic
ed meds online without prescription or membership generic cialis without a doctor prescription viagra without doctor prescription amazon
https://edpill.cheap/# what is the best ed pill
mexican pharmacy without prescription: cheap cialis – ed meds online without prescription or membership
buy semaglutide 14 mg online cheap order rybelsus generic semaglutide 14 mg generic
mexico drug stores pharmacies mexican pharmaceuticals online buying prescription drugs in mexico
mexico drug stores pharmacies mexico pharmacy medication from mexico pharmacy
mexican border pharmacies shipping to usa mexico drug stores pharmacies medicine in mexico pharmacies
mexico drug stores pharmacies mexican rx online reputable mexican pharmacies online
http://mexicanph.shop/# mexican mail order pharmacies
buying prescription drugs in mexico
buying prescription drugs in mexico online mexican border pharmacies shipping to usa buying prescription drugs in mexico
medicine in mexico pharmacies п»їbest mexican online pharmacies mexican border pharmacies shipping to usa
vardenafil 10mg tablet buy levitra for sale cheap vardenafil 10mg
mexican border pharmacies shipping to usa mexican mail order pharmacies mexican online pharmacies prescription drugs
mexican online pharmacies prescription drugs mexican border pharmacies shipping to usa mexican drugstore online
mexican border pharmacies shipping to usa buying prescription drugs in mexico best mexican online pharmacies
free spins no deposit canada roulette online with real money best real money casino
mexico pharmacies prescription drugs buying from online mexican pharmacy pharmacies in mexico that ship to usa
reputable mexican pharmacies online mexico pharmacy mexican mail order pharmacies
http://mexicanph.com/# mexican drugstore online
п»їbest mexican online pharmacies
best online pharmacies in mexico pharmacies in mexico that ship to usa buying prescription drugs in mexico online
pharmacies in mexico that ship to usa medicine in mexico pharmacies pharmacies in mexico that ship to usa
reputable mexican pharmacies online medication from mexico pharmacy mexico pharmacies prescription drugs
mexican mail order pharmacies purple pharmacy mexico price list mexico pharmacies prescription drugs
http://mexicanph.shop/# mexico drug stores pharmacies
mexican mail order pharmacies
mexico drug stores pharmacies medication from mexico pharmacy mexico drug stores pharmacies
buy plaquenil online cheap buy cheap generic plaquenil hydroxychloroquine uk
mexico drug stores pharmacies mexico drug stores pharmacies reputable mexican pharmacies online
buying from online mexican pharmacy mexican online pharmacies prescription drugs mexico drug stores pharmacies
brand lyrica 150mg pregabalin cost lyrica price
buying prescription drugs in mexico buying prescription drugs in mexico online mexican online pharmacies prescription drugs
https://mexicanph.shop/# purple pharmacy mexico price list
п»їbest mexican online pharmacies
buying from online mexican pharmacy pharmacies in mexico that ship to usa pharmacies in mexico that ship to usa
zithromax with alcohol
buying from online mexican pharmacy п»їbest mexican online pharmacies buying prescription drugs in mexico
medicine in mexico pharmacies mexican pharmaceuticals online medicine in mexico pharmacies
hydroxychloroquine 200mg ca purchase hydroxychloroquine generic generic hydroxychloroquine 200mg
mexican pharmacy mexican border pharmacies shipping to usa medication from mexico pharmacy
medicine in mexico pharmacies buying prescription drugs in mexico mexico drug stores pharmacies
reputable mexican pharmacies online pharmacies in mexico that ship to usa mexican mail order pharmacies
mexican pharmaceuticals online purple pharmacy mexico price list best mexican online pharmacies
mexico drug stores pharmacies mexican pharmaceuticals online mexico drug stores pharmacies
pharmacies in mexico that ship to usa mexican online pharmacies prescription drugs mexican pharmacy
mexican pharmaceuticals online mexican border pharmacies shipping to usa reputable mexican pharmacies online
zithromax tablets 500mg
http://mexicanph.shop/# mexican pharmaceuticals online
pharmacies in mexico that ship to usa
mexican online pharmacies prescription drugs mexican pharmaceuticals online medication from mexico pharmacy
oral aristocort 10mg buy aristocort 4mg online cheap aristocort 10mg over the counter
mexico drug stores pharmacies mexican pharmacy mexican mail order pharmacies
mexican rx online best online pharmacies in mexico п»їbest mexican online pharmacies
cialis 5mg generic tadalafil usa tadalafil usa
buying prescription drugs in mexico mexican online pharmacies prescription drugs medication from mexico pharmacy
order aristocort 10mg pills triamcinolone 4mg us buy aristocort online cheap
mexican rx online mexican border pharmacies shipping to usa purple pharmacy mexico price list
buying prescription drugs in mexico online medication from mexico pharmacy mexican drugstore online
mexican border pharmacies shipping to usa purple pharmacy mexico price list mexican pharmacy
buying prescription drugs in mexico mexican drugstore online best online pharmacies in mexico
medication from mexico pharmacy mexican border pharmacies shipping to usa pharmacies in mexico that ship to usa
medication from mexico pharmacy pharmacies in mexico that ship to usa mexico drug stores pharmacies
п»їbest mexican online pharmacies mexico drug stores pharmacies buying from online mexican pharmacy
http://mexicanph.shop/# buying prescription drugs in mexico
medication from mexico pharmacy
purple pharmacy mexico price list purple pharmacy mexico price list best mexican online pharmacies
best online pharmacies in mexico pharmacies in mexico that ship to usa purple pharmacy mexico price list
mexican mail order pharmacies mexico drug stores pharmacies mexican mail order pharmacies
buying prescription drugs in mexico best mexican online pharmacies mexico pharmacies prescription drugs
tadalafil 5mg us purchase tadalafil without prescription cheap tadalafil 20mg
mexico drug stores pharmacies mexico pharmacy purple pharmacy mexico price list
mexican border pharmacies shipping to usa mexico drug stores pharmacies mexican online pharmacies prescription drugs
buying prescription drugs in mexico online buying from online mexican pharmacy purple pharmacy mexico price list
buying prescription drugs in mexico mexico pharmacies prescription drugs mexican online pharmacies prescription drugs
mexican pharmaceuticals online buying prescription drugs in mexico online mexico drug stores pharmacies
clarinex ca buy desloratadine 5mg online cheap order desloratadine
mexican mail order pharmacies mexican border pharmacies shipping to usa mexican border pharmacies shipping to usa
medicine in mexico pharmacies buying prescription drugs in mexico mexican pharmaceuticals online
http://mexicanph.shop/# purple pharmacy mexico price list
medication from mexico pharmacy
buying from online mexican pharmacy mexican pharmacy best online pharmacies in mexico
cenforce 50mg oral buy cenforce buy cenforce sale
purchase desloratadine for sale desloratadine 5mg cheap buy desloratadine 5mg for sale
buying prescription drugs in mexico purple pharmacy mexico price list mexican rx online
mexico drug stores pharmacies mexican pharmaceuticals online medication from mexico pharmacy
mexico pharmacy purple pharmacy mexico price list mexican border pharmacies shipping to usa
buying prescription drugs in mexico mexican pharmacy best mexican online pharmacies
mexico pharmacy medicine in mexico pharmacies mexican pharmaceuticals online
mexican pharmaceuticals online buying prescription drugs in mexico online mexico drug stores pharmacies
purple pharmacy mexico price list best mexican online pharmacies mexican mail order pharmacies
mexico pharmacies prescription drugs buying prescription drugs in mexico online purple pharmacy mexico price list
best online pharmacies in mexico mexican border pharmacies shipping to usa mexico pharmacies prescription drugs
cenforce usa buy cenforce 50mg pill buy cenforce 100mg pills
mexican border pharmacies shipping to usa buying prescription drugs in mexico medication from mexico pharmacy
medication from mexico pharmacy mexican border pharmacies shipping to usa mexican online pharmacies prescription drugs
п»їbest mexican online pharmacies medicine in mexico pharmacies mexican pharmaceuticals online
mexico pharmacy mexico drug stores pharmacies medicine in mexico pharmacies
purple pharmacy mexico price list medication from mexico pharmacy mexico pharmacy
best online pharmacies in mexico medication from mexico pharmacy best online pharmacies in mexico
reputable mexican pharmacies online buying from online mexican pharmacy mexican pharmaceuticals online
mexican rx online mexican pharmacy mexico drug stores pharmacies
reputable mexican pharmacies online reputable mexican pharmacies online mexico drug stores pharmacies
pharmacies in mexico that ship to usa mexico pharmacy mexican online pharmacies prescription drugs
buying prescription drugs in mexico medicine in mexico pharmacies medication from mexico pharmacy
buy generic aralen 250mg order chloroquine 250mg without prescription order chloroquine 250mg
cheap claritin purchase loratadine for sale how to get loratadine without a prescription
mexican border pharmacies shipping to usa mexican border pharmacies shipping to usa buying prescription drugs in mexico
mexican border pharmacies shipping to usa mexican drugstore online mexican pharmaceuticals online
metformin 500 mg weight loss
http://mexicanph.com/# buying prescription drugs in mexico
mexico pharmacies prescription drugs
mexico drug stores pharmacies mexican pharmacy pharmacies in mexico that ship to usa
order claritin 10mg generic claritin drug where can i buy loratadine
mexican pharmaceuticals online best online pharmacies in mexico best online pharmacies in mexico
mexico pharmacies prescription drugs mexican online pharmacies prescription drugs mexican rx online
mexican pharmaceuticals online mexico drug stores pharmacies purple pharmacy mexico price list
buying prescription drugs in mexico mexican pharmaceuticals online buying from online mexican pharmacy
https://stromectol.fun/# stromectol price us
buy aralen tablets aralen 250mg canada chloroquine oral
cost of amoxicillin amoxicillin pharmacy price canadian pharmacy amoxicillin
lasix pills: Buy Lasix No Prescription – buy lasix online
https://lisinopril.top/# buy zestril online
http://buyprednisone.store/# prednisone 10 mg
lisinopril price comparison: prinivil cost – lisinopril 20 mg uk
https://amoxil.cheap/# amoxicillin 500 mg without a prescription
prednisone for sale in canada prednisone 20 mg in india best pharmacy prednisone
http://amoxil.cheap/# amoxicillin 500mg capsules
buy dapoxetine 90mg for sale order priligy 60mg for sale misoprostol brand
amoxicillin 500 mg price: amoxicillin 250 mg – amoxil pharmacy
order metformin sale metformin 500mg uk glucophage 500mg oral
generic for prinivil lisinopril 5 mg for sale buy lisinopril 2.5 mg online
https://buyprednisone.store/# prednisone 50 mg canada
how to stop metformin diarrhea
http://amoxil.cheap/# amoxicillin 500mg tablets price in india
priligy brand priligy usa buy misoprostol pill
lisinopril 10mg tablets price: cheap lisinopril 40 mg – zestril 20 mg price in india
https://stromectol.fun/# ivermectin 3mg tablet
stromectol 3 mg dosage ivermectin 5 mg price ivermectin oral 0 8
ivermectin goodrx: cost of ivermectin medicine – ivermectin brand
http://stromectol.fun/# where to buy stromectol
lasix: lasix online – lasix generic name
https://lisinopril.top/# buy lisinopril 2.5 mg online
ivermectin 6mg dosage ivermectin 0.5% lotion stromectol generic
http://amoxil.cheap/# amoxicillin for sale
https://stromectol.fun/# stromectol ivermectin tablets
cost of lisinopril: zestril 25 mg – generic for zestril
cost glucophage 500mg order glycomet 500mg pills metformin us
https://buyprednisone.store/# prednisone tablets 2.5 mg
amoxicillin discount coupon generic amoxil 500 mg amoxicillin no prescipion
stromectol uk: ivermectin – ivermectin 9 mg
purchase orlistat pill buy diltiazem cheap diltiazem
http://furosemide.guru/# furosemide 40 mg
buy amoxicillin online mexico: buy amoxicillin online uk – order amoxicillin uk
orlistat 60mg without prescription orlistat 60mg us generic diltiazem 180mg
can flagyl treat chlamydia
https://stromectol.fun/# buy ivermectin canada
ivermectin 3 mg ivermectin 3 mg stromectol sales
atorvastatin 20mg for sale where can i buy atorvastatin buy atorvastatin sale
amoxicillin 500mg capsules price: amoxicillin 750 mg price – where can i get amoxicillin 500 mg
https://lisinopril.top/# lisinopril price 10 mg
https://amoxil.cheap/# purchase amoxicillin online without prescription
prednisone 30: india buy prednisone online – prednisone prescription for sale
http://furosemide.guru/# lasix medication
lisinopril 20 mg coupon lisinopril 20 mg cost can i order lisinopril over the counter
furosemide for kidney disease
https://furosemide.guru/# lasix 100mg
lasix: lasix uses – lasix 20 mg
lisinopril fatal side effects
http://lisinopril.top/# lisinopril 20 mg buy
medicine amoxicillin 500mg can i purchase amoxicillin online amoxil generic
lasix generic name: lasix pills – furosemide 100 mg
flagyl tastes gross
https://amoxil.cheap/# amoxicillin 500 mg price
brand norvasc norvasc 10mg us amlodipine where to buy
https://lisinopril.top/# buy zestoretic
order prednisone with mastercard debit: 50 mg prednisone from canada – ordering prednisone
https://amoxil.cheap/# antibiotic amoxicillin
purchase prednisone from india buy generic prednisone online prednisone 60 mg tablet
http://lisinopril.top/# prinivil cost
ivermectin 1mg: ivermectin lice – stromectol brand
effects of zoloft
https://amoxil.cheap/# order amoxicillin no prescription
buy lisinopril 2.5 mg online lisinopril brand name canada purchase lisinopril 40 mg
lisinopril and sun exposure
zestoretic 5 mg: where can i order lisinopril online – website
buy acyclovir generic buy zyloprim 100mg pill buy cheap generic zyloprim
zoloft and benadryl
torsemide vs furosemide conversion
http://amoxil.cheap/# rexall pharmacy amoxicillin 500mg
order amlodipine 10mg generic order amlodipine 5mg generic buy norvasc sale
buy acyclovir generic acyclovir 800mg tablet buy cheap allopurinol
prednisone brand name canada: order prednisone 100g online without prescription – buy prednisone 40 mg
https://amoxil.cheap/# amoxicillin azithromycin
http://furosemide.guru/# furosemide 100mg
otc lisinopril zestoretic tabs zestril drug
buy zithromax 1000mg
http://amoxil.cheap/# price of amoxicillin without insurance
ivermectin cream cost: ivermectin price uk – ivermectin 0.08
https://stromectol.fun/# ivermectin 5
lisinopril for sale online buy lisinopril generic order lisinopril 10mg online
order amoxicillin online can i buy amoxicillin online where can i buy amoxicillin over the counter
zestril 5 mg price: lisinopril 50 mg – zestril tablet price
http://lisinopril.top/# prinivil 40 mg
http://furosemide.guru/# lasix generic name
how long does it take for lasix to work
lasix pills: Buy Furosemide – lasix tablet
gabapentin 300mg capsules
amoxicillin 500 mg purchase without prescription amoxicillin 500 mg tablets amoxicillin online without prescription
http://furosemide.guru/# lasix medication
http://lisinopril.top/# lisinopril 10 12.5 mg tablets
how to buy rosuvastatin generic zetia 10mg oral zetia
stromectol 15 mg: purchase ivermectin – stromectol otc
zithromax price
http://lisinopril.top/# cheapest price for lisinopril india
purchase prinivil pills oral lisinopril buy lisinopril 2.5mg for sale
order crestor generic buy crestor tablets purchase ezetimibe without prescription
http://lisinopril.top/# buy lisinopril online india
buy lisinopril online lisinopril 10 mg online no prescription prinivil 25 mg
buy lasix online: Buy Furosemide – lasix furosemide 40 mg
https://stromectol.fun/# stromectol generic
glucophage formula
average cost of prednisone: ordering prednisone – order prednisone from canada
https://stromectol.fun/# ivermectin 12
prilosec 10mg for sale buy omeprazole 10mg generic omeprazole 20mg sale
gabapentin for bipolar
glucophage uspi
motilium brand sumycin online order tetracycline 250mg uk
bupropion and escitalopram
order prilosec prilosec where to buy buy prilosec without a prescription
motilium online order motilium 10mg cost sumycin canada
buy prescription drugs from india cheapest online pharmacy india indian pharmacy online
pharmacy website india world pharmacy india Online medicine order
http://indianph.xyz/# indian pharmacies safe
top 10 online pharmacy in india
https://indianph.com/# Online medicine order
cephalexin expired 5 years ago
https://indianph.com/# top 10 pharmacies in india
best online pharmacy india
best india pharmacy india pharmacy mail order Online medicine order
lopressor price metoprolol 100mg usa lopressor 100mg tablet
gabapentin a controlled substance
https://indianph.com/# best india pharmacy
pharmacy website india
http://indianph.com/# top 10 pharmacies in india
indian pharmacy paypal
escitalopram od
http://indianph.com/# top online pharmacy india
indianpharmacy com
best online pharmacy india cheapest online pharmacy india buy medicines online in india
https://indianph.com/# buy medicines online in india
mail order pharmacy india
amoxicillin rash treatment
https://indianph.xyz/# indian pharmacy paypal
buy cyclobenzaprine 15mg baclofen ca baclofen 10mg cost
https://indianph.com/# india pharmacy mail order
Online medicine home delivery
http://indianph.com/# Online medicine home delivery
mail order pharmacy india
buy prescription drugs from india top 10 online pharmacy in india cheapest online pharmacy india
amoxicillin 250 mg dosage for child
cost flexeril cheap baclofen order baclofen generic
metoprolol for sale online brand metoprolol 100mg order metoprolol online
cephalexin for dogs without vet prescription
http://indianph.com/# buy medicines online in india
indian pharmacy
can i drink alcohol 24 hours after taking bactrim
oral tenormin atenolol pills order atenolol 100mg for sale
http://cytotec24.com/# Misoprostol 200 mg buy online
nolvadex 10mg: liquid tamoxifen – benefits of tamoxifen
ciprofloxacin 500mg buy online where can i buy cipro online where can i buy cipro online
https://diflucan.pro/# diflucan best price
ordering diflucan generic: where to get diflucan – cost of diflucan tablet
https://diflucan.pro/# how to buy diflucan over the counter
http://nolvadex.guru/# nolvadex generic
buy generic toradol over the counter buy cheap generic gloperba order colchicine without prescription
bactrim long term side effects
buy cipro: buy ciprofloxacin over the counter – buy generic ciprofloxacin
http://nolvadex.guru/# tamoxifen dose
tamoxifen menopause should i take tamoxifen nolvadex steroids
buy toradol 10mg generic toradol 10mg for sale buy colchicine pills for sale
cephalexin for dogs uti
http://cipro.guru/# cipro 500mg best prices
ciprofloxacin 500mg uses
buy doxycycline online without prescription: doxycycline tablets – buy doxycycline cheap
atenolol us order atenolol without prescription order tenormin 50mg generic
buy cytotec buy cytotec pills online cheap buy cytotec over the counter
https://cytotec24.shop/# cytotec buy online usa
ciprofloxacin alternative
diflucan price in india: where to get diflucan otc – diflucan men
https://diflucan.pro/# where can i get diflucan
http://diflucan.pro/# diflucan online canada
nolvadex half life: does tamoxifen cause menopause – nolvadex half life
cipro ciprofloxacin buy cipro cheap ciprofloxacin generic price
http://nolvadex.guru/# tamoxifen reviews
http://cytotec24.com/# buy misoprostol over the counter
order depo-medrol sale buy generic medrol over the counter methylprednisolone canada
will cephalexin treat ear infection
http://cipro.guru/# cipro ciprofloxacin
cytotec pills buy online order cytotec online buy cytotec in usa
https://cytotec24.com/# purchase cytotec
https://cipro.guru/# buy cipro online
buy cytotec over the counter buy cytotec pills buy cytotec
https://nolvadex.guru/# nolvadex price
http://doxycycline.auction/# doxycycline 200 mg
buy methylprednisolone pills medrol over the counter medrol 4 mg without prescription
buy misoprostol over the counter Abortion pills online buy cytotec pills online cheap
http://cytotec24.shop/# cytotec pills buy online
https://nolvadex.guru/# aromatase inhibitors tamoxifen
http://sweetiefox.online/# Sweetie Fox filmleri
Angela White video: Abella Danger – abella danger video
https://abelladanger.online/# abella danger video
help with assignments uk buy dissertation online affordable thesis writing
https://lanarhoades.fun/# lana rhoades modeli
https://angelawhite.pro/# Angela White
sweety fox: sweeti fox – Sweetie Fox izle
http://sweetiefox.online/# Sweetie Fox
https://evaelfie.pro/# eva elfie modeli
lana rhoades filmleri: lana rhoades filmleri – lana rhoades video
http://sweetiefox.online/# Sweetie Fox video
propranolol us buy inderal 20mg generic clopidogrel 150mg brand
http://angelawhite.pro/# Angela White video
https://evaelfie.pro/# eva elfie filmleri
https://abelladanger.online/# Abella Danger
Angela White: abella danger izle – abella danger izle
buy inderal no prescription clopidogrel where to buy cost plavix 150mg
http://sweetiefox.online/# Sweetie Fox video
http://angelawhite.pro/# Angela White izle
Angela Beyaz modeli: Abella Danger – abella danger izle
https://evaelfie.pro/# eva elfie modeli
assignment website academic writing support i need help with my essay
https://angelawhite.pro/# Angela White izle
http://abelladanger.online/# Abella Danger
eva elfie modeli: eva elfie video – eva elfie izle
http://sweetiefox.online/# Sweetie Fox modeli
http://angelawhite.pro/# Angela White video
https://lanarhoades.fun/# lana rhoades filmleri
eva elfie filmleri: eva elfie modeli – eva elfie filmleri
https://lanarhoades.fun/# lana rhoades
methotrexate ca cost methotrexate 5mg coumadin 2mg tablet
?????? ????: Abella Danger – abella danger video
https://angelawhite.pro/# Angela White video
http://abelladanger.online/# Abella Danger
http://lanarhoades.fun/# lana rhoades filmleri
bactrim dosing pediatric
purchase methotrexate pill buy generic methotrexate over the counter warfarin 2mg without prescription
http://angelawhite.pro/# Angela Beyaz modeli
lana rhoades modeli: lana rhoades – lana rhoades modeli
buy generic meloxicam online celecoxib 200mg sale purchase celebrex online
http://lanarhoades.fun/# lana rhoades izle
https://angelawhite.pro/# Angela Beyaz modeli
can you take cephalexin for sinus infection
lana rhoades: lana rhodes – lana rhodes
https://lanarhoades.fun/# lana rhoades
http://evaelfie.pro/# eva elfie
https://sweetiefox.online/# Sweetie Fox izle
eva elfie modeli: eva elfie video – eva elfie modeli
https://abelladanger.online/# abella danger filmleri
http://sweetiefox.online/# Sweetie Fox modeli
https://abelladanger.online/# Abella Danger
metoclopramide 20mg pills cozaar 50mg usa order losartan 50mg sale
brand meloxicam 7.5mg buy celecoxib 200mg online cheap celecoxib 100mg usa
http://evaelfie.pro/# eva elfie filmleri
order metoclopramide 10mg without prescription order hyzaar for sale losartan 50mg over the counter
?????? ????: abella danger izle – abella danger izle
http://abelladanger.online/# abella danger video
https://abelladanger.online/# Abella Danger
http://sweetiefox.online/# swetie fox
Angela White izle: Angela White video – ?????? ????
http://sweetiefox.online/# Sweetie Fox filmleri
https://angelawhite.pro/# ?????? ????
bactrim with alcohol
buy tamsulosin 0.2mg generic flomax 0.4mg buy celebrex medication
https://sweetiefox.pro/# ph sweetie fox
best online dating websites: http://lanarhoades.pro/# lana rhoades full video
lana rhoades unleashed: lana rhoades hot – lana rhoades pics
https://sweetiefox.pro/# sweetie fox full
escitalopram qt prolongation
lana rhoades: lana rhoades full video – lana rhoades solo
https://miamalkova.life/# mia malkova movie
sweetie fox full: sweetie fox full video – sweetie fox full video
buy flomax 0.2mg pills order generic flomax 0.4mg buy celecoxib without prescription
http://lanarhoades.pro/# lana rhoades unleashed
dating personals free: http://lanarhoades.pro/# lana rhoades boyfriend
ph sweetie fox: sweetie fox full – sweetie fox new
ph sweetie fox: sweetie fox new – sweetie fox
neurontin for anxiety side effects
https://sweetiefox.pro/# sweetie fox new
fox sweetie: sweetie fox – sweetie fox
pill escitalopram
japanese dating site: http://evaelfie.site/# eva elfie hd
lana rhoades hot: lana rhoades – lana rhoades pics
http://lanarhoades.pro/# lana rhoades full video
sweetie fox video: fox sweetie – sweetie fox video
http://evaelfie.site/# eva elfie new video
neurontin help with opiate withdrawal
simple-dating life: http://miamalkova.life/# mia malkova videos
buy nexium 40mg pills order topiramate pills topiramate 100mg pills
eva elfie hd: eva elfie hot – eva elfie hot
order nexium capsules topiramate 200mg ca order topiramate pills
eva elfie full videos: eva elfie videos – eva elfie photo
http://lanarhoades.pro/# lana rhoades full video
ondansetron 8mg drug purchase zofran for sale buy cheap generic aldactone
lana rhoades videos: lana rhoades videos – lana rhoades hot
http://miamalkova.life/# mia malkova
meet woman: https://miamalkova.life/# mia malkova new video
mia malkova only fans: mia malkova videos – mia malkova hd
order ondansetron 4mg generic order spironolactone 25mg without prescription buy spironolactone 100mg pill
lana rhoades videos: lana rhoades hot – lana rhoades full video
sumatriptan 50mg sale order levaquin sale buy levofloxacin 500mg generic
http://miamalkova.life/# mia malkova hd
mia malkova latest: mia malkova latest – mia malkova full video
order sumatriptan 25mg online cheap buy imitrex 50mg pill order levaquin 250mg pills
https://www.independent.co.uk/
sabrina carpenter dating: http://evaelfie.site/# eva elfie full video
mia malkova full video: mia malkova hd – mia malkova only fans
http://miamalkova.life/# mia malkova
sweetie fox new: sweetie fox – ph sweetie fox
http://sweetiefox.pro/# ph sweetie fox
lana rhoades unleashed: lana rhoades – lana rhoades solo
Reduslim ist ein beliebtes Produkt auf dem Markt, das zur Gewichtsabnahme beiträgt. Viele Menschen suchen nach einem effektiven und sicheren Weg, um überschüssige Pfunde zu verlieren. Der Preis von Reduslim ist für viele ein wichtiges Kriterium bei der Entscheidung, ob sie das Produkt kaufen möchten.
Es ist jedoch wichtig zu beachten, dass der Preis von Reduslim im Vergleich zu anderen ähnlichen Produkten sehr erschwinglich ist. Die Qualität und Wirksamkeit des Produkts rechtfertigen den Preis, da es aus hochwertigen natürlichen Inhaltsstoffen hergestellt wird.
Durch die Einnahme von Reduslim können Sie auf natürliche Weise Ihren Stoffwechsel anregen und somit Fett schneller verbrennen. Dies führt zu einer effektiven Gewichtsabnahme ohne Nebenwirkungen.
Insgesamt ist Reduslim eine großartige Option für Personen, die auf natürliche Weise und zu einem vernünftigen Preis abnehmen möchten. Es lohnt sich daher, den Preis von Reduslim in Betracht zu ziehen, wenn Sie Ihren Traumkörper erreichen möchten.
Wenn Sie möchten, können Sie noch heute bestellen und sich auf den Weg zu einem gesünderen und schlankeren Körper machen. Der Preis von Reduslim ist jeden Cent wert!
https://reduslim.at/
Reduslim 2020: Der neueste Trend in der Gewichtsabnahme
Die Suche nach effektiven Methoden zur Gewichtsabnahme ist immer ein heißes Thema, besonders zu Beginn eines neuen Jahres. Mit Reduslim 2020 scheint ein neuer Trend gefunden worden zu sein. Dieses natürliche Nahrungsergänzungsmittel verspricht, den Stoffwechsel zu steigern, Fett zu verbrennen und das Verlangen nach Kalorien zu reduzieren.
Die Wirksamkeit von Reduslim 2020 beruht auf einer einzigartigen Kombination aus natürlichen Inhaltsstoffen, die speziell ausgewählt wurden, um die Gewichtsabnahme zu unterstützen. Grüntee-Extrakt, Garcinia Cambogia und Guarana sind nur einige der Schlüsselbestandteile, die dafür sorgen, dass der Körper in einen Fettverbrennungsmodus versetzt wird.
Neben der positiven Wirkung auf den Stoffwechsel hilft Reduslim 2020 auch dabei, Heißhungerattacken zu kontrollieren und das Verlangen nach Snacks zu reduzieren. Durch die Einnahme der Kapseln wird das Sättigungsgefühl gesteigert, was dazu führt, dass weniger Kalorien aufgenommen werden.
Die Einnahme von Reduslim 2020 in Kombination mit einer ausgewogenen Ernährung und regelmäßiger körperlicher Aktivität kann zu beeindruckenden Ergebnissen führen. Es ist wichtig zu beachten, dass Nahrungsergänzungsmittel keine Wundermittel sind und Geduld und Engagement erfordern.
Wenn Sie also auf der Suche nach einem natürlichen Weg sind, um Ihre Gewichtsabnahmeziele im Jahr 2020 zu erreichen, könnte Reduslim die Lösung für Sie sein. Probieren Sie es aus und starten Sie noch heute Ihren Weg zu einem gesünderen und schlankeren Körper.
https://reduslim.at/
sweetie fox full video: sweetie fox video – sweetie fox full video
ddavp 20 mcg iv
Reduslim 24 ist das neue Wundermittel zur Gewichtsreduktion, das derzeit den Markt erobert. Mit seiner einzigartigen Formel aus natürlichen Inhaltsstoffen verspricht es eine effektive und schnelle Gewichtsabnahme ohne lästiges Hungern oder stundenlanges Training im Fitnessstudio.
Die Kapseln von Reduslim 24 sollen den Stoffwechsel ankurbeln, den Appetit zügeln und die Fettverbrennung steigern. Dadurch soll man bereits nach kurzer Zeit eine sichtbare Veränderung an seinem Körper feststellen können. Viele zufriedene Anwender berichten von einem spürbaren Gewichtsverlust innerhalb weniger Wochen.
Ein weiterer Pluspunkt von Reduslim 24 ist, dass es keine bekannten Nebenwirkungen gibt und für jeden geeignet ist, der ein paar Pfunde verlieren möchte. Egal ob Mann oder Frau, jung oder alt, mit Reduslim 24 kann jeder sein Wunschgewicht erreichen.
Wenn auch du endlich deine überschüssigen Pfunde loswerden möchtest, probiere Reduslim 24 doch einfach mal aus. Mit seiner innovativen Formel und schnellen Wirkung könnte es genau das Richtige für dich sein. Starte noch heute deine Reise zu einem schlankeren und gesünderen Ich mit Reduslim 24.
https://reduslim.at/
Piero Mozzi ist ein bekannter Ernährungsberater, der durch seine revolutionäre Methode namens Reduslim viele Menschen dabei geholfen hat, ihr Gewicht zu reduzieren. Reduslim basiert auf der Idee, dass eine gesunde Ernährung der Schlüssel zum Abnehmen ist. Mozzi betont die Bedeutung von natürlichen Lebensmitteln und verzichtet auf künstliche Zusatzstoffe. Sein Ansatz hat bereits vielen Menschen geholfen, ihr Wunschgewicht zu erreichen und langfristig zu halten. Mit Piero Mozzi und Reduslim können auch Sie erfolgreich abnehmen und Ihre Gesundheit verbessern.
https://reduslim.at/
Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das in jeder Apotheke erhältlich ist. Es handelt sich um eine natürliche und effektive Lösung zur Gewichtsreduktion. Reduslim enthält eine einzigartige Mischung aus natürlichen Zutaten, die nachweislich beim Abnehmen helfen.
In der Reduslim Apotheke können Kunden das Produkt einfach und bequem erwerben. Es wird empfohlen, Reduslim regelmäßig einzunehmen, um optimale Ergebnisse zu erzielen. Die Kapseln sind einfach anzuwenden und führen zu einem schnellen Fettabbau. Viele Menschen schwören auf die Wirksamkeit von Reduslim und haben bereits große Erfolge damit erzielt.
Die Kombination der Inhaltsstoffe in Reduslim fördert den Stoffwechsel, reduziert das Hungergefühl und unterstützt die Fettverbrennung. Dadurch können Anwender schnell und effektiv abnehmen, ohne auf eine ausgewogene Ernährung oder regelmäßige Bewegung verzichten zu müssen.
Wer also auf der Suche nach einer einfachen und wirksamen Lösung zur Gewichtsreduktion ist, sollte sich definitiv für Reduslim aus der Apotheke entscheiden. Probieren Sie es aus und überzeugen Sie sich selbst von den positiven Effekten dieses Nahrungsergänzungsmittels.
https://reduslim.at/
asien dating online: https://sweetiefox.pro/# sweetie fox full
https://sweetiefox.pro/# sweetie fox new
“Come si prende Reduslim” ist eine hГ¤ufig gestellte Frage von Menschen, die auf der Suche nach einem natГјrlichen und effektiven Weg zur Gewichtsabnahme sind. Es ist wichtig zu wissen, dass Reduslim ein NahrungsergГ¤nzungsmittel ist, das bei der Gewichtsabnahme helfen kann, aber keine Wundermittel sind.
Um Reduslim effektiv zu nehmen, sollten die Anweisungen auf der Verpackung genau befolgt werden. Die empfohlene Dosierung beträgt in der Regel zwei Kapseln pro Tag, vorzugsweise vor den Mahlzeiten. Es ist wichtig, Reduslim regelmäßig einzunehmen und mit einer gesunden Ernährung und ausreichender körperlicher Bewegung zu kombinieren.
Es ist auch wichtig, sich bewusst zu machen, dass Reduslim keine langfristige Lösung für Gewichtsprobleme ist. Es sollte als Teil eines gesunden Lebensstils betrachtet werden. Konsultieren Sie immer einen Arzt, bevor Sie ein Nahrungsergänzungsmittel einnehmen, um sicherzustellen, dass es für Ihre individuellen Bedürfnisse geeignet ist.
Insgesamt kann Reduslim eine nützliche Ergänzung zu einer gesunden Ernährung und Lebensweise sein, um beim Abnehmen zu helfen. Durch die Beachtung der Dosierungsempfehlungen und die Kombination mit gesunden Gewohnheiten können positive Ergebnisse erzielt werden. Denken Sie jedoch daran, dass nachhaltige Veränderungen im Lebensstil der Schlüssel zu langfristigem Erfolg bei der Gewichtsabnahme sind.
https://reduslim.at/
Che cos’ГЁ Reduslim und wie funktioniert es? Reduslim ist ein beliebtes NahrungsergГ¤nzungsmittel, das dabei hilft, effektiv Gewicht zu verlieren. Die spezielle Formel aus natГјrlichen Inhaltsstoffen wie Garcinia Cambogia, GrГјner Tee und Guarana soll den Stoffwechsel ankurbeln und die Fettverbrennung steigern.
Durch die Einnahme von Reduslim soll der Körper schneller Fett abbauen und somit Gewicht verlieren. Viele Anwender berichten von positiven Ergebnissen und einer verbesserten Figur. Doch wie genau funktioniert Reduslim und wie sollte es eingenommen werden?
Um die bestmöglichen Ergebnisse zu erzielen, empfiehlt es sich, Reduslim regelmäßig einzunehmen und mit einer ausgewogenen Ernährung und ausreichend Bewegung zu kombinieren. Die Kapseln können einfach mit Wasser eingenommen werden und unterstützen den Körper dabei, effektiv Gewicht zu verlieren.
Reduslim ist eine natürliche und schonende Methode, um Gewicht zu reduzieren und sich wohler im eigenen Körper zu fühlen. Probieren Sie es aus und überzeugen Sie sich selbst von den positiven Effekten dieses innovativen Nahrungsergänzungsmittels!
https://reduslim.at/
Cose Reduslim ist ein neues Nahrungsergänzungsmittel, das die Fettverbrennung und Gewichtsabnahme auf natürliche Weise unterstützt. Durch die einzigartige Kombination von Inhaltsstoffen wie Grüntee-Extrakt, Guarana und Garcinia Cambogia wird der Stoffwechsel angeregt und das Sättigungsgefühl erhöht. Dies führt zu einem schnelleren Abbau von Fettreserven und einem nachhaltigen Gewichtsverlust.
Die Einnahme von Cose Reduslim ist einfach und unkompliziert. Einmal täglich eine Kapsel vor einer Mahlzeit mit ausreichend Wasser einnehmen und die positiven Effekte des Nahrungsergänzungsmittels schon bald spüren. Neben der Unterstützung beim Abnehmen hilft Cose Reduslim auch dabei, den Blutzuckerspiegel zu regulieren und den Cholesterinspiegel zu verbessern.
Viele zufriedene Anwender berichten von schnellen und dauerhaften Erfolgen mit Cose Reduslim. Dank der natürlichen Inhaltsstoffe sind keine Nebenwirkungen zu befürchten. Wer also auf der Suche nach einer effektiven Unterstützung beim Abnehmen ist, sollte Cose Reduslim eine Chance geben und die positiven Veränderungen am eigenen Körper erleben.
https://reduslim.at/
purchase simvastatin online cheap zocor 20mg for sale valacyclovir pills
Es ist kein Geheimnis, dass Gewichtsverlust für viele Menschen eine große Herausforderung darstellt. Es gibt unzählige Diäten, Übungen und Pillen auf dem Markt, die alle das Versprechen machen, die Pfunde schnell schmelzen zu lassen. Aber wer hat tatsächlich Erfolg mit diesen Methoden gehabt?
Eine beliebte Frage, die oft im Zusammenhang mit dem Gewichtsverlustmittel Reduslim gestellt wird, lautet: “cine a folosit reduslim?” In der Welt der DiГ¤tpillen gibt es viele Behauptungen und Versprechungen, aber es ist wichtig, die Erfahrungen realer Menschen zu hГ¶ren.
Es gibt viele positive Berichte von Personen, die Reduslim verwendet haben und beeindruckende Ergebnisse erzielt haben. Diese Menschen haben durch die Einnahme der Pillen ihr Gewicht reduziert und ihre Ziele erreicht.
Es ist jedoch wichtig zu betonen, dass jeder Körper anders ist und verschiedene Reaktionen auf Diätpillen haben kann. Bevor man ein solches Produkt ausprobiert, ist es ratsam, mit einem Arzt zu sprechen und die eigenen Gesundheitsziele zu berücksichtigen.
Letztendlich kann “cine a folosit reduslim” eine interessante Frage sein, aber es ist wichtig, dass jeder Einzelne seine eigene Reise zum Gewichtsverlust plant und dabei gesunde Entscheidungen trifft.
https://reduslim.at/
Effetti Collaterali Reduslim Prezzo in Farmacia: Was Sie wissen mГјssen
Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das auf dem Markt für Gewichtsverlust erhältlich ist. Viele Menschen schwärmen von den Vorteilen des Produkts, aber es gibt auch Berichte über mögliche Nebenwirkungen. Es ist wichtig, sich der möglichen Effetti Collaterali Reduslim Prezzo in Farmacia bewusst zu sein, bevor man sich für den Kauf entscheidet.
Einige der häufigsten Nebenwirkungen von Reduslim sind Übelkeit, Kopfschmerzen und Schlafstörungen. Es ist auch möglich, dass das Produkt mit bestimmten Medikamenten oder Gesundheitszuständen interagiert, daher ist es ratsam, vor der Einnahme einen Arzt zu konsultieren.
Der Preis fГјr Reduslim in Apotheken kann je nach Standort und Anbieter variieren. Es ist ratsam, die Preise zu vergleichen und nach Sonderangeboten zu suchen, um den besten Deal zu bekommen.
Insgesamt kann Reduslim eine effektive Methode zur Gewichtsabnahme sein, aber es ist wichtig, sich der möglichen Nebenwirkungen bewusst zu sein und verantwortungsbewusst damit umzugehen.|;
https://reduslim.at/
purchase avodart pills purchase dutasteride pills ranitidine 150mg oral
aviator bet malawi login: aviator bet malawi login – aviator game
http://aviatormalawi.online/# aviator malawi
Hast du schon vom offiziellen Website Reduslim gehört? Dies ist die richtige Seite für alle, die auf der Suche nach einem natürlichen und effektiven Weg sind, um Gewicht zu verlieren. Reduslim bietet hochwertige Produkte, die dabei helfen, den Stoffwechsel zu beschleunigen und das Hungergefühl zu reduzieren. Auf der offiziellen Website Reduslim kannst du alle Informationen zu den Produkten finden und sie direkt bestellen. Mit der Unterstützung von Reduslim kannst du endlich deine Wunschfigur erreichen und dich rundum wohlfühlen. Besuche noch heute die Seite officiel reduslim und starte deine Reise zu einem gesünderen Leben!
https://reduslim.at/
Reduslim Web oficial bietet ein effektives und sicheres Gewichtsverlustprogramm fГјr alle, die ihre Traumfigur erreichen mГ¶chten. Mit natГјrlichen Inhaltsstoffen, die den Stoffwechsel anregen und den Appetit zГјgeln, ist Reduslim die ideale LГ¶sung fГјr alle, die schnell und langfristig abnehmen mГ¶chten. Durch die offizielle Website kГ¶nnen Sie sicher und einfach bestellen und profitieren von tollen Angeboten und Rabatten. Verabschieden Sie sich von lГ¤stigen DiГ¤ten und probieren Sie Reduslim noch heute aus. GГ¶nnen Sie sich den KГ¶rper, den Sie verdienen – mit Reduslim Web oficial.
https://reduslim.at/
Reduslim vélemények sind ein wichtiger Bestandteil der Entscheidungsfindung für diejenigen, die nach einer effektiven Gewichtsabnahme-Lösung suchen. Diese Bewertungen geben einen Einblick in die Erfahrungen anderer Personen mit dem Produkt und können dabei helfen, zu verstehen, ob es wirklich funktioniert. Viele Menschen vertrauen auf die Meinungen anderer, wenn es darum geht, ein neues Produkt auszuprobieren. Durch die Suche nach Reduslim vélemények können potenzielle Benutzer mehr über die Wirksamkeit, die Nebenwirkungen und die Allgemeine Zufriedenheit mit dem Produkt erfahren.
Es ist wichtig, darauf zu achten, dass nicht alle Bewertungen echt sind und manchmal gefälschte Bewertungen veröffentlicht werden, um das Image eines Produkts zu verbessern. Daher ist es ratsam, sich auf seriöse und glaubwürdige Quellen zu verlassen, um echte Reduslim vélemények zu finden. Einige der häufigsten Kommentare zu Reduslim beziehen sich auf die schnelle Wirkung des Produkts, die Unterdrückung des Appetits und die Verbesserung des Stoffwechsels.
Insgesamt scheinen die meisten Benutzer mit den Ergebnissen von Reduslim zufrieden zu sein und berichten von einem positiven Gewichtsverlust-Erlebnis. Es ist jedoch wichtig zu beachten, dass jedes Produkt unterschiedlich auf verschiedene Personen wirken kann und dass individuelle Ergebnisse variieren können. Bevor Sie sich für die Verwendung von Reduslim entscheiden, ist es ratsam, mit einem Arzt zu sprechen und sicherzustellen, dass es sicher ist und keine unerwünschten Nebenwirkungen verursacht.
https://reduslim.at/
aviator oyna: aviator oyna – aviator hilesi
Reduslim ist ein beliebtes Produkt, das auf dem Markt für Gewichtsabnahme erhältlich ist, aber was ist der Reduslim Preis? Viele Menschen fragen sich, ob es sich lohnt, Geld für dieses Produkt auszugeben. Der Preis für Reduslim kann je nach Anbieter variieren, daher ist es wichtig, sorgfältig zu recherchieren, bevor man eine Entscheidung trifft.
Es gibt verschiedene Optionen, um Reduslim zu kaufen, darunter Online-Shops und Apotheken. Einige Anbieter bieten Rabatte oder Sonderangebote an, die den Preis reduzieren können. Es ist jedoch ratsam, vorsichtig zu sein und sicherzustellen, dass man ein authentisches Produkt erhält.
Der Preis von Reduslim mag auf den ersten Blick hoch erscheinen, aber wenn man bedenkt, dass es eine effektive Gewichtsverlustlösung sein kann, könnte es sich als lohnende Investition erweisen. Es ist wichtig, dass man den Preis nicht als Hindernis betrachtet, sondern als Investition in die eigene Gesundheit und Wohlbefinden.
Insgesamt kann gesagt werden, dass der Reduslim Preis im Vergleich zu den potenziellen Vorteilen, die das Produkt bieten kann, angemessen ist. Es lohnt sich, sich grГјndlich zu informieren und den besten Preis zu finden, um von den Vorteilen dieses Produkts zu profitieren.
https://reduslim.at/
order avodart without prescription purchase ranitidine sale buy generic zantac 300mg
Reduslim per quanto tempo sollte man einnehmen, um die gewünschten Ergebnisse zu erzielen? Diese Frage beschäftigt viele Menschen, die auf der Suche nach einer effektiven Methode zur Gewichtsreduktion sind. Die Antwort ist jedoch nicht so einfach, da die Ergebnisse je nach individuellen Faktoren variieren können. Es wird empfohlen, Reduslim über einen Zeitraum von mindestens 2-3 Monaten einzunehmen, um optimale Ergebnisse zu erzielen. Es ist wichtig, dass die Einnahme mit einer ausgewogenen Ernährung und regelmäßiger Bewegung kombiniert wird, um langfristige Erfolge zu gewährleisten. Konsultieren Sie vor der Einnahme von Reduslim Ihren Arzt, um sicherzustellen, dass das Produkt für Sie geeignet ist.
https://reduslim.at/
Sie haben von den Reduslim Pillole Dimagranti gehört und möchten mehr darüber erfahren? Diese Abnehmpillen haben in den letzten Jahren viel Aufmerksamkeit erhalten, aber was genau macht sie so effektiv?
Die Reduslim Pillole Dimagranti enthalten eine spezielle Formel aus natürlichen Inhaltsstoffen, die dabei helfen, den Stoffwechsel zu steigern und Fett zu verbrennen. Durch die Einnahme dieser Pillen können Sie schneller abnehmen und Ihr Gewicht auf gesunde Weise reduzieren.
Die Wirksamkeit der Reduslim Pillole Dimagranti wurde in klinischen Studien nachgewiesen, und viele Benutzer berichten von positiven Ergebnissen. Wenn Sie also Schwierigkeiten haben, Gewicht zu verlieren, könnten diese Abnehmpillen die Lösung sein, nach der Sie gesucht haben.
Denken Sie daran, dass die Reduslim Pillole Dimagranti am besten in Verbindung mit einer gesunden Ernährung und regelmäßiger Bewegung funktionieren. Konsultieren Sie auch immer Ihren Arzt, bevor Sie mit der Einnahme von Nahrungsergänzungsmitteln beginnen.
Insgesamt sind die Reduslim Pillole Dimagranti eine vielversprechende Option für alle, die ihr Gewicht auf sichere und effektive Weise reduzieren möchten. Probieren Sie sie aus und sehen Sie selbst die Ergebnisse!
https://reduslim.at/
Möchten Sie Reduslim kaufen in Deutschland in der Apotheke? Dann sind Sie hier genau richtig! Dieses beliebte Nahrungsergänzungsmittel zur Gewichtsreduktion ist in vielen Apotheken erhältlich und wird von vielen Menschen auf der Suche nach einer effektiven Lösung zur Gewichtskontrolle geschätzt.
Reduslim enthält eine einzigartige Formel aus natürlichen Inhaltsstoffen, die dabei helfen können, den Stoffwechsel zu beschleunigen und die Fettverbrennung zu fördern. Durch die Einnahme von Reduslim können Sie Ihre Diät- und Sportbemühungen unterstützen und möglicherweise schneller Ergebnisse erzielen.
Bevor Sie Reduslim kaufen in Deutschland in der Apotheke, ist es ratsam, mit einem Arzt oder Ernährungsexperten zu sprechen, um sicherzustellen, dass das Produkt für Sie geeignet ist. Denken Sie auch daran, dass Nahrungsergänzungsmittel allein keine Wunder bewirken können und eine gesunde Ernährung und ausreichend Bewegung ebenfalls wichtig sind.
Insgesamt kann Reduslim eine wertvolle Ergänzung zu Ihrem Gesundheits- und Abnehmprogramm sein. Probieren Sie es aus und sehen Sie selbst, ob es Ihnen hilft, Ihre Ziele zu erreichen!
https://reduslim.at/
Reduslim Kapseln sind der neueste Trend in der Welt der Gewichtsabnahme. Diese speziellen Kapseln enthalten natürliche Inhaltsstoffe wie Grüntee-Extrakt, L-Carnitin und Garcinia Cambogia, die alle bekannt sind für ihre Fähigkeit, den Stoffwechsel zu erhöhen und Fett zu verbrennen.
Durch die regelmäßige Einnahme von Reduslim Kapseln kann man effektiv Gewicht verlieren und gleichzeitig den Körper mit wichtigen Nährstoffen versorgen. Die einzigartige Formel dieser Kapseln hilft dabei, den Appetit zu kontrollieren und Heißhungerattacken zu reduzieren.
Viele zufriedene Kunden berichten von schnellen und nachhaltigen Ergebnissen mit Reduslim Kapseln. Sie fГјhlen sich fitter, schlanker und energiegeladener als je zuvor.
Wenn auch du von den Vorteilen dieser innovativen Kapseln profitieren möchtest, solltest du sie am besten noch heute ausprobieren. Reduziere dein Gewicht auf natürliche Weise mit Reduslim Kapseln und fühle dich wieder wohl in deiner Haut!
https://reduslim.at/
Mit dem Eintritt in die Wechseljahre kämpfen viele Frauen mit unerwünschten Gewichtszunahmen. Die Verlangsamung des Stoffwechsels und hormonelle Veränderungen können zu einer Veränderung der Körperzusammensetzung führen. In dieser Phase kann die Einnahme von Reduslim in Menopause Frauen helfen, ihr Gewicht zu kontrollieren und die unerwünschten Symptome zu lindern.
Reduslim ist ein natürlicher Nahrungsergänzungsmittel, der speziell für Frauen in den Wechseljahren entwickelt wurde. Die spezielle Formel hilft, den Stoffwechsel zu beschleunigen und den Körper bei der Fettverbrennung zu unterstützen. Durch die natürlichen Inhaltsstoffe können unerwünschte Nebenwirkungen vermieden werden.
Frauen, die Reduslim in Menopause einnehmen, berichten von einer Steigerung ihres Energielevels und einer Verbesserung ihres allgemeinen Wohlbefindens. Die Kombination aus gesunder Ernährung, regelmäßiger Bewegung und der Einnahme von Reduslim kann Frauen dabei helfen, ihr Gewicht zu kontrollieren und sich in ihrem eigenen Körper wohler zu fühlen.
Wenn auch Sie von den unerwünschten Gewichtszunahmen in den Wechseljahren betroffen sind, könnte Reduslim die Lösung für Sie sein. Sprechen Sie mit Ihrem Arzt über die Möglichkeit, Reduslim in Menopause einzunehmen und starten Sie noch heute Ihren Weg zu einem gesünderen und glücklicheren Leben.
https://reduslim.at/
Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das häufig zur Gewichtsreduktion eingesetzt wird. Viele Menschen fragen sich jedoch, wie sie Reduslim richtig anwenden können, um die besten Ergebnisse zu erzielen. Hier sind einige Tipps, wie Sie Reduslim richtig anwenden können:
1. Befolgen Sie die Anweisungen auf der Verpackung: Es ist wichtig, die empfohlene Dosierung von Reduslim einzuhalten, um die besten Ergebnisse zu erzielen. Lesen Sie daher sorgfältig die Anweisungen auf der Verpackung und halten Sie sich daran.
2. Trinken Sie ausreichend Wasser: Es ist wichtig, während der Einnahme von Reduslim ausreichend Wasser zu trinken. Wasser hilft Ihrem Körper, Giftstoffe auszuspülen und kann auch helfen, die Effektivität von Reduslim zu steigern.
3. Kombinieren Sie Reduslim mit einer gesunden Ernährung und regelmäßiger Bewegung: Reduslim allein kann nicht alle Probleme lösen. Um die besten Ergebnisse zu erzielen, sollten Sie Reduslim mit einer gesunden Ernährung und regelmäßiger Bewegung kombinieren.
Indem Sie diese Tipps befolgen, können Sie sicherstellen, dass Sie Reduslim effektiv anwenden und beste Ergebnisse erzielen. Wenn Sie sich jedoch unsicher sind, wie Sie Reduslim am besten anwenden können, wenden Sie sich am besten an einen Arzt oder Ernährungsberater.
https://reduslim.at/
aviator betano: aviator game – estrela bet aviator
Reduslim Deutschland – Die effektive Lösung für schnelles Abnehmen
In einer Welt, in der das Streben nach dem perfekten Körper immer präsent ist, ist Reduslim Deutschland die Lösung für alle, die schnell und effektiv abnehmen wollen. Mit seiner einzigartigen Formel aus natürlichen Inhaltsstoffen sorgt Reduslim dafür, dass die Pfunde purzeln und das gewünschte Wunschgewicht erreicht wird.
Die speziell entwickelten Kapseln regen den Stoffwechsel an, reduzieren das Hungergefühl und fördern die Fettverbrennung. Dadurch wird nicht nur Gewicht verloren, sondern auch der Körper entgiftet und gereinigt. Reduslim Deutschland ist somit nicht nur ein effektives Abnehmmittel, sondern auch eine gesunde Unterstützung für den Körper.
Durch die Einnahme von Reduslim wird das Abnehmen nicht mehr zur Qual, sondern zu einem positiven Prozess, bei dem man sich besser fühlt und sein Ziel schneller erreicht. Kein mühsames Kalorienzählen oder stundenlanges Training mehr – mit Reduslim Deutschland wird das Abnehmen zum Kinderspiel.
Also gönnen Sie sich den Luxus, in der Sommerzeit mit einem schlanken und gesunden Körper am Strand zu glänzen. Probieren Sie Reduslim Deutschland aus und erleben Sie selbst, wie einfach und effektiv Abnehmen sein kann. Gönnen Sie sich die beste Version Ihrer selbst und starten Sie noch heute Ihre Reise zu einem gesünderen und fitteren Leben.
https://reduslim.at/
http://aviatorghana.pro/# aviator bet
Auf der Suche nach einem effektiven Weg, um Gewicht zu verlieren, stößt man häufig auf das Produkt Reduslim. Doch wie hoch ist eigentlich der Reduslim costo? Der Preis kann je nach Anbieter variieren, aber eines ist sicher: Reduslim ist eine Investition in Ihre Gesundheit und Ihr Wohlbefinden wert. Mit seinen natürlichen Inhaltsstoffen kann es Ihnen helfen, schneller und effektiver Gewicht zu verlieren. Zudem unterstützt es den Stoffwechsel und kann das Hungergefühl reduzieren. Probieren Sie Reduslim noch heute aus und überzeugen Sie sich selbst von seiner Wirksamkeit!
https://reduslim.at/
Reduslim Contatti: Kontaktiere uns fГјr eine effektive Gewichtsabnahme
Du möchtest schnell und einfach abnehmen? Dann bist du bei Reduslim genau richtig. Mit unseren natürlichen Nahrungsergänzungsmitteln kannst du deine Traumfigur erreichen, ohne dabei auf Genuss zu verzichten. Unsere Produkte sind nicht nur effektiv, sondern auch absolut sicher und schonend für deinen Körper.
Wenn du Fragen zu unseren Produkten oder deiner Bestellung hast, zögere nicht, uns zu kontaktieren. Unsere freundlichen Mitarbeiter stehen dir gerne zur Verfügung und helfen dir bei allen Anliegen rund um Reduslim. Egal ob per Telefon, E-Mail oder Live-Chat – wir sind für dich da!
Nutze jetzt die Möglichkeit, deine Traumfigur zu erreichen und kontaktiere Reduslim noch heute. Wir freuen uns darauf, dir auf dem Weg zu einem gesünderen und glücklicheren Leben zu helfen. Mit Reduslim wird das Abnehmen zum Kinderspiel!
https://reduslim.at/
what should you not take with citalopram
Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das bei der Gewichtsabnahme helfen soll. Aber was genau ist Reduslim und wozu dient es?
Reduslim ist eine Kombination aus verschiedenen natГјrlichen Inhaltsstoffen, die synergistisch zusammenwirken, um den Stoffwechsel zu beschleunigen, den Appetit zu unterdrГјcken und die Fettverbrennung zu steigern. Dies fГјhrt dazu, dass man schneller abnimmt und einfacher sein Wunschgewicht erreichen kann.
Die Hauptbestandteile von Reduslim sind GrГјner Tee Extrakt, Garcinia Cambogia, Guarana und L-Carnitin. Diese Inhaltsstoffe sind bekannt fГјr ihre positiven Effekte auf den Stoffwechsel und die Fettverbrennung.
Reduslim kann sowohl von Frauen als auch von Männern verwendet werden, die Gewicht verlieren möchten. Es ist wichtig zu betonen, dass Reduslim kein Ersatz für eine gesunde Ernährung und regelmäßige Bewegung ist, sondern vielmehr als Unterstützung bei der Gewichtsabnahme genutzt werden sollte.
Insgesamt kann man sagen, dass Reduslim ein effektives Nahrungsergänzungsmittel ist, das dabei helfen kann, schneller Gewicht zu verlieren und sein Wunschgewicht zu erreichen. Es sollte jedoch immer in Kombination mit einer gesunden Lebensweise verwendet werden.
https://reduslim.at/
Sie haben sich schon einmal gefragt, was genau in Reduslim enthalten ist? Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das bei der Gewichtsabnahme helfen soll. Das Produkt enthält eine spezielle Mischung aus natürlichen Zutaten, die darauf abzielen, den Stoffwechsel zu steigern und den Appetit zu unterdrücken.
Zu den Hauptbestandteilen von Reduslim gehören grüner Kaffee, Garcinia Cambogia, L-Carnitin und Zink. Grüner Kaffee soll den Stoffwechsel ankurbeln und die Fettverbrennung fördern. Garcinia Cambogia ist bekannt für seine appetithemmenden Eigenschaften und kann helfen, Heißhungerattacken zu vermeiden.
L-Carnitin ist ein wichtiger Nährstoff, der dem Körper hilft, Fett in Energie umzuwandeln. Zink ist ein essentielles Spurenelement, das den Stoffwechsel unterstützt und das Immunsystem stärkt. Zusammen sollen diese Inhaltsstoffe dazu beitragen, Gewicht zu verlieren und das Wohlbefinden zu verbessern.
Wenn Sie also auf der Suche nach einem natürlichen Weg sind, um Gewicht zu verlieren, könnte Reduslim das richtige Produkt für Sie sein. Probieren Sie es aus und sehen Sie selbst, welche Ergebnisse es für Sie bringen kann.
https://reduslim.at/
Pharmacie Reduslim bietet eine Vielzahl von Produkten zur Gewichtsabnahme an, die auf natürlichen Inhaltsstoffen basieren. Reduslim ist eine beliebte Marke, die für ihre Wirksamkeit und Qualität bekannt ist. In der Pharmacie Reduslim finden Kunden eine große Auswahl an Produkten, die ihnen helfen, ihr Gewicht zu reduzieren und ihre Gesundheit zu verbessern.
Die Produkte von Pharmacie Reduslim werden von Experten entwickelt und sind sicher und effektiv. Sie enthalten natürliche Inhaltsstoffe wie Grüner Tee, Garcinia Cambogia und Guarana, die den Stoffwechsel ankurbeln und die Fettverbrennung fördern können. Kunden können zwischen verschiedenen Darreichungsformen wie Kapseln, Pulvern und Tees wählen, je nach ihren persönlichen Vorlieben und Bedürfnissen.
In der Pharmacie Reduslim erhalten Kunden auch eine professionelle Beratung und Unterstützung bei der Gewichtsabnahme. Das kompetente Team steht jederzeit zur Verfügung, um Fragen zu beantworten und individuelle Empfehlungen zu geben. Kunden können sich darauf verlassen, dass sie in der Pharmacie Reduslim die richtigen Produkte finden, um ihre Ziele auf gesunde Weise zu erreichen.
https://reduslim.at/
Sie möchten schnell und effektiv abnehmen? Dann sind die Compresse Reduslim die perfekte Lösung für Sie! Diese natürlichen Tabletten enthalten eine einzigartige Mischung aus natürlichen Inhaltsstoffen, die dabei helfen, Ihren Stoffwechsel anzukurbeln und Fett effektiv zu verbrennen.
Die Compresse Reduslim unterstützen Sie dabei, Ihr Gewichtsabnahmziel schnell zu erreichen, ohne dabei aufwendige Diäten oder anstrengende Workouts machen zu müssen. Einfach täglich einnehmen und die resultierenden Effekte spüren!
Die hochwertigen Inhaltsstoffe wie Grüntee-Extrakt, Guarana und L-Carnitin sorgen für eine optimale Fettverbrennung und halten Ihren Energielevel den ganzen Tag über hoch. Zusätzlich wirken die Compresse Reduslim auch als Appetitzügler, sodass Sie weniger Kalorien zu sich nehmen und somit schneller abnehmen können.
Beginnen Sie noch heute mit der Einnahme der Compresse Reduslim und sagen Sie Ihren überflüssigen Kilos den Kampf an! Verabschieden Sie sich von lästigen Diäten und übermäßigem Sport und erreichen Sie Ihr Traumgewicht auf natürliche und effektive Weise. Probieren Sie es jetzt aus!
https://reduslim.at/
buy propecia 1mg sale buy proscar buy fluconazole 200mg online cheap
Clerici e Reduslim: Die perfekte Kombination fГјr eine gesunde und nachhaltige Gewichtsabnahme.
Clerici und Reduslim sind zwei beliebte Produkte, die sich perfekt ergänzen, um effektiv und langfristig abzunehmen. Clerici ist ein natürliches Nahrungsergänzungsmittel, das den Stoffwechsel anregt und den Fettstoffwechsel verbessert. Reduslim hingegen ist eine speziell entwickelte Diätpille, die den Appetit zügelt und die Fettverbrennung beschleunigt.
Die Kombination aus Clerici und Reduslim verspricht eine gesunde und nachhaltige Gewichtsabnahme ohne Jo-Jo-Effekt. Durch die synergistische Wirkung der beiden Produkte wird der Abnehmprozess beschleunigt und das HungergefГјhl reduziert.
Wenn Sie also schon lange nach einer effektiven Lösung für Ihr Gewichtsproblem suchen, sollten Sie unbedingt Clerici und Reduslim ausprobieren. Mit dieser einzigartigen Kombination können Sie Ihr Wunschgewicht erreichen und sich endlich wieder wohl in Ihrer Haut fühlen. Gönnen Sie sich und Ihrem Körper etwas Gutes und starten Sie noch heute mit Clerici e Reduslim in ein gesünderes Leben.
https://reduslim.at/
Das chicote Reduslim ist ein neues und innovatives Produkt auf dem Markt der Gewichtsabnahme. Es basiert auf natГјrlichen Inhaltsstoffen, die eine effektive und gesunde Gewichtsabnahme unterstГјtzen. Chicote Reduslim hilft, den Stoffwechsel zu beschleunigen und Fett schneller zu verbrennen. DarГјber hinaus wirkt es auch als AppetitzГјgler und verringert somit das Verlangen nach ungesunden Snacks und groГџen Portionen.
Die Anwendung von chicote Reduslim ist einfach und unkompliziert. Es wird empfohlen, täglich eine Kapsel vor einer Mahlzeit einzunehmen. In Kombination mit einer ausgewogenen Ernährung und regelmäßiger körperlicher Aktivität kann chicote Reduslim dabei helfen, langfristige Ergebnisse zu erzielen.
Viele zufriedene Anwender berichten von einer spürbaren Gewichtsabnahme und einer Steigerung ihres Wohlbefindens. Chicote Reduslim hat sich als wirksames und zuverlässiges Mittel zur Gewichtsabnahme bewährt und wird von vielen Menschen weltweit geschätzt. Probieren auch Sie es aus und erleben Sie die positiven Effekte von chicote Reduslim auf Ihren Körper und Ihre Gesundheit.
https://reduslim.at/
Che cos’ГЁ Reduslim Recensioni? Reduslim ГЁ un integratore alimentare che promette di aiutare le persone a perdere peso in modo rapido ed efficace. Le recensioni su Reduslim sono varie e contrastanti. Alcune persone sostengono di aver ottenuto risultati sorprendenti con l’uso di questo prodotto, mentre altre sono scettiche riguardo alla sua efficacia.
Alcuni utenti affermano di aver notato una diminuzione dell’appetito e una maggiore energia dopo aver iniziato a prendere Reduslim. Altri, tuttavia, sostengono di non aver ottenuto nessun risultato significativo nonostante l’assunzione regolare del prodotto.
Г€ importante tenere presente che l’efficacia di Reduslim puГІ variare da persona a persona e che i risultati dipendono da vari fattori, tra cui l’alimentazione e l’attivitГ fisica. Prima di iniziare qualsiasi programma di perdita di peso, ГЁ sempre consigliabile consultare un medico o un professionista della salute.
In conclusione, le recensioni su Reduslim sono eterogenee e dipendono dalle esperienze individuali di chi ha utilizzato il prodotto. Г€ sempre importante essere consapevoli dei propri obiettivi di salute e fare ricerche approfondite prima di assumere qualsiasi integratore alimentare.
https://reduslim.at/
pin-up casino entrar: pin-up casino entrar – pin-up casino
Reduslim vélemények sind oft kontrovers diskutiert. Viele behaupten, dass dieses Produkt der Schlüssel zum schnellen und effektiven Abnehmen ist, während andere Zweifel an seiner Wirksamkeit haben. Es handelt sich um eine natürliche Ergänzung, die den Stoffwechsel ankurbeln und das Hungergefühl reduzieren soll.
Einige Benutzer berichten von großartigen Ergebnissen und loben Reduslim für die einfache Anwendung und die schnellen Ergebnisse. Sie schwärmen von einem gesteigerten Energielevel und einem verbesserten Selbstbewusstsein. Andere wiederum berichten von keinen spürbaren Veränderungen und zweifeln an der Werbewirksamkeit des Produkts.
Wie bei allen Nahrungsergänzungsmitteln ist es wichtig, realistische Erwartungen zu haben und das Produkt im Rahmen eines gesunden Lebensstils zu verwenden. Konsultieren Sie immer einen Arzt, bevor Sie neue Ergänzungen ausprobieren, um sicherzustellen, dass sie für Ihren Körper geeignet sind. Letztendlich ist es wichtig, dass Sie das Produkt selbst ausprobieren und Ihre eigenen Reduslim vélemények bilden.
https://reduslim.at/
Reduslim wie teuer: Einfache und Effektive Gewichtsabnahme
Sie wollen Gewicht verlieren, fragen sich aber “Reduslim, wie teuer ist es?” Nun, Reduslim ist eine groГџartige Option fГјr diejenigen, die schnell und sicher abnehmen mГ¶chten. Der Preis mag hoch erscheinen, aber die Ergebnisse sind es wert. Reduslim ist eine natГјrliche ErgГ¤nzung, die Ihren Stoffwechsel ankurbelt und Fettverbrennung fГ¶rdert.
Mit Reduslim können Sie unerwünschte Pfunde ohne strenge Diäten oder anstrengende Trainingseinheiten verlieren. Es ist einfach einzunehmen und hat keine Nebenwirkungen. Der Preis mag hoch sein, aber vergleichen Sie ihn mit den Kosten anderer Gewichtsverlustmethoden und Sie werden sehen, dass es eine lohnende Investition ist.
Also, wenn Sie sich fragen, ob Reduslim das Geld wert ist, sagen wir ja! Investieren Sie in Ihre Gesundheit und Ihr Wohlbefinden mit Reduslim und sehen Sie die erstaunlichen Ergebnisse selbst. Reduslim ist nicht billig, aber die Vorteile Гјberwiegen bei weitem den Preis. Probieren Sie es aus und erleben Sie eine einfache und effektive Gewichtsabnahme.
https://reduslim.at/
Reduslim Wikipedia ist eine beliebte Online-Enzyklopädie, die Informationen über das beliebte Abnehmprodukt Reduslim bietet. Reduslim ist ein natürlicher Fatburner, der dabei helfen kann, Gewicht zu verlieren und den Stoffwechsel zu beschleunigen. In der Wikipedia finden sich umfassende Informationen über die Inhaltsstoffe von Reduslim, seine Wirkungsweise und mögliche Nebenwirkungen.
Viele Menschen, die mit ihrem Gewicht unzufrieden sind, suchen nach effektiven Methoden, um abzunehmen. Reduslim hat sich als beliebte Option erwiesen, da es auf natürliche Weise den Gewichtsverlust unterstützen kann. Die Wikipedia-Seite bietet Lesern die Möglichkeit, sich umfassend über das Produkt zu informieren, bevor sie eine Kaufentscheidung treffen.
Die positive Resonanz auf Reduslim und die wachsende Anzahl zufriedener Kunden sprechen für die Wirksamkeit des Produkts. Die Wikipedia-Seite ist ein wertvoller Ressource für alle, die mehr über Reduslim erfahren möchten und sich informierte Entscheidungen über ihre Gesundheit treffen möchten.
https://reduslim.at/
pin up cassino online: pin-up cassino – pin up bet
Reduslim ist ein beliebtes NahrungsergГ¤nzungsmittel zur UnterstГјtzung der Gewichtsabnahme. Viele Menschen fragen sich: “Reduslim quante compresse sono?” Dies hГ¤ngt von der Packungsgröße ab, die Sie kaufen. Typischerweise enthГ¤lt eine Packung Reduslim 30 Kapseln, die fГјr einen Monat reichen. Es wird empfohlen, tГ¤glich eine Kapsel einzunehmen, um die besten Ergebnisse zu erzielen. Reduslim enthГ¤lt natГјrliche Inhaltsstoffe wie GrГјntee-Extrakt, L-Carnitin und Garcinia Cambogia, die den Stoffwechsel anregen und das Abnehmen unterstГјtzen kГ¶nnen. Bevor Sie jedoch Reduslim einnehmen, ist es wichtig, mit Ihrem Arzt zu sprechen, um sicherzustellen, dass es fГјr Sie geeignet ist. Probieren Sie Reduslim aus und erleben Sie die Vorteile einer gesunden Gewichtsabnahme.
https://reduslim.at/
https://aviatorjogar.online/# pin up aviator
ddavp solucion intranasal
Reduslim Preturi: Der SchlГјssel zum erfolgreichen Abnehmen
Reduslim Preturi ist ein beliebtes Produkt für Menschen, die erfolgreich abnehmen wollen. Die niedrigen Preise machen es für jeden erschwinglich, sein Gewichtsverlust-Ziel zu erreichen. Das Geheimnis des Erfolgs von Reduslim liegt in seiner einzigartigen Formel, die natürliche Inhaltsstoffe enthält, die den Stoffwechsel anregen und das Hungergefühl reduzieren.
Reduslim ist nicht nur wirksam, sondern auch sicher in der Anwendung. Es gibt keine bekannten Nebenwirkungen, die mit der Einnahme von Reduslim verbunden sind. Dies macht es zu einer optimalen Wahl für Menschen, die nach einem zuverlässigen Produkt suchen, um Gewicht zu verlieren.
Die positiven Bewertungen von zufriedenen Kunden sprechen für sich. Viele Menschen haben mit Hilfe von Reduslim erfolgreich abgenommen und sind begeistert von den Ergebnissen. Wenn auch du dein Gewichtsverlust-Ziel erreichen möchtest, solltest du Reduslim in Betracht ziehen.
Greife noch heute zu Reduslim Preturi und starte deinen Weg zu einem gesГјnderen und glГјcklicheren Leben. Du wirst es nicht bereuen!
https://reduslim.at/
Reduslim Pastillas sind ein beliebtes Nahrungsergänzungsmittel, das dabei hilft, überflüssige Pfunde loszuwerden. Die spezielle Formel dieser Pastillas wurde entwickelt, um den Stoffwechsel zu steigern und das Hungergefühl zu reduzieren. Dadurch fällt es leichter, eine Diät einzuhalten und erfolgreich abzunehmen.
Viele Menschen schwören auf Reduslim Pastillas, da sie effektiv dabei helfen, Gewicht zu verlieren, ohne dabei auf allzu strenge Diäten angewiesen zu sein. Die Pastillas enthalten natürliche Inhaltsstoffe, die den Körper dabei unterstützen, Fett zu verbrennen und gleichzeitig den Energiehaushalt aufrechtzuerhalten.
Wer also auf der Suche nach einer einfachen und effektiven Möglichkeit ist, Gewicht zu verlieren, sollte Reduslim Pastillas definitiv eine Chance geben. Die positiven Erfahrungsberichte sprechen für sich und zeigen, dass dieses Produkt tatsächlich helfen kann, das Wunschgewicht zu erreichen. Probieren Sie es aus und überzeugen Sie sich selbst von den Vorteilen dieser beliebten Pastillas.
https://reduslim.at/
aviator malawi: aviator bet malawi – aviator malawi
Reduslim in Germania ist eines der beliebtesten Schlankheitsmittel auf dem Markt. Mit seiner natürlichen Formel hilft es Menschen, effektiv Gewicht zu verlieren und ihre Ziele zu erreichen. Reduslim enthält Inhaltsstoffe wie grüner Kaffee, grüner Tee und Garcinia Cambogia, die bekanntermaßen den Stoffwechsel ankurbeln und die Fettverbrennung fördern.
Viele Menschen in Deutschland schwören auf Reduslim, da es ihnen geholfen hat, ihr Gewicht zu reduzieren und ihr Selbstbewusstsein zu steigern. Durch regelmäßige Einnahme in Kombination mit einer gesunden Ernährung und ausreichend Bewegung können gute Ergebnisse erzielt werden.
Reduslim ist einfach anzuwenden und in verschiedenen Online-Shops in Deutschland erhältlich. Es wird empfohlen, vor der Einnahme einen Arzt zu konsultieren, um sicherzustellen, dass es keine gesundheitlichen Bedenken gibt.
Wenn auch du auf der Suche nach einem effektiven Schlankheitsmittel bist, probiere Reduslim in Germania aus und erlebe selbst die positiven Veränderungen in deinem Körper.
https://reduslim.at/
Reduslim Kapseln kaufen ist eine beliebte Möglichkeit, um Gewicht zu verlieren und den Stoffwechsel anzuregen. Diese natürlichen Kapseln enthalten sorgfältig ausgewählte Inhaltsstoffe, die dabei helfen, Fett zu verbrennen und den Appetit zu zügeln. Viele Menschen schwören auf die Wirksamkeit dieser Kapseln und sind begeistert von ihren Ergebnissen.
Es ist wichtig, beim Kauf von Reduslim Kapseln auf die Qualität und Herkunft der Produkte zu achten. Seriöse Anbieter bieten transparente Informationen über ihre Produkte und garantieren eine hohe Qualität. Vor dem Kauf sollte man sich über die Inhaltsstoffe informieren und sicherstellen, dass keine allergischen Reaktionen auftreten können.
Die Einnahme von Reduslim Kapseln sollte immer in Kombination mit einer ausgewogenen Ernährung und regelmäßiger Bewegung erfolgen. Nur so können langfristige Erfolge erzielt werden. Wer auf der Suche nach einem natürlichen Helfer für die Gewichtsabnahme ist, sollte Reduslim Kapseln kaufen und sich selbst von ihrer Wirkung überzeugen.
https://reduslim.at/
Reduslim in Farmacii – Ein natГјrlicher Weg zur Gewichtsabnahme
Reduslim in Farmacii ist die ideale Lösung für all diejenigen, die effektiv und auf gesunde Weise abnehmen möchten. Dieses natürliche Nahrungsergänzungsmittel enthält eine einzigartige Mischung aus pflanzlichen Inhaltsstoffen, die nachweislich helfen, Fett zu verbrennen und den Stoffwechsel zu steigern. In den Apotheken erhältlich, hat Reduslim bereits vielen Menschen geholfen, ihr Traumgewicht zu erreichen.
Die Wirksamkeit von Reduslim in Farmacii beruht auf seiner einzigartigen Formel, die speziell entwickelt wurde, um den Körper beim Abbau von Fettreserven zu unterstützen. Die natürlichen Inhaltsstoffe wie grüner Tee, Garcinia Cambogia und Ingwer helfen, den Appetit zu reduzieren und die Fettverbrennung zu fördern. Darüber hinaus enthält Reduslim auch Vitamin B6 und B12, die den Energiehaushalt verbessern und Müdigkeit reduzieren.
Die Einnahme von Reduslim in Farmacii ist einfach und unkompliziert. Es wird empfohlen, täglich zwei Kapseln mit ausreichend Wasser einzunehmen. Schon nach kurzer Zeit werden Sie erste Erfolge sehen und sich fitter und vitaler fühlen. Reduslim ist eine sichere und effektive Methode, um langfristig abzunehmen und das erreichte Gewicht zu halten.
Wenn auch Sie von den Vorteilen von Reduslim in Farmacii profitieren möchten, zögern Sie nicht und besuchen Sie noch heute Ihre Apotheke. Starten Sie noch heute Ihren Weg zur Traumfigur mit Reduslim!
https://reduslim.at/
generic for depakote
Reduslim ist ein beliebtes Schlankheitsmittel, aber was sagen die Ärzte dazu? Viele Experten sind geteilter Meinung über die Wirksamkeit dieses Produkts. Einige behaupten, dass Reduslim tatsächlich beim Abnehmen hilft, während andere skeptisch sind und Bedenken hinsichtlich möglicher Nebenwirkungen äußern. Die Meinungen der Ärzte sind also gespalten.
Einige Ärzte argumentieren, dass Reduslim eine natürliche und sichere Möglichkeit bietet, Gewicht zu verlieren, ohne auf radikale Diäten oder starke Medikamente zurückzugreifen. Sie empfehlen das Produkt als eine unterstützende Maßnahme zu einer gesunden Ernährung und regelmäßiger Bewegung. Andere Ärzte sind jedoch skeptisch und warnen vor möglichen Risiken für die Gesundheit.
Letztendlich liegt es an jedem Einzelnen, mit seinem Arzt zu sprechen und die Risiken und Vorteile von Reduslim abzuwägen. Es ist wichtig, informierte Entscheidungen zu treffen und sich möglichst umfassend zu informieren, bevor man ein Schlankheitsmittel wie Reduslim einnimmt. Jeder Körper reagiert anders und was für den einen funktioniert, muss nicht zwangsläufig auch für den anderen geeignet sein.
https://reduslim.at/
Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das bei der Gewichtsabnahme helfen kann. Viele Menschen, die Probleme mit ihrer Schilddrüse haben, fragen sich jedoch, ob Reduslim sicher für sie ist. Die gute Nachricht ist, dass Reduslim und die Schilddrüse in der Regel gut miteinander verträglich sind.
Reduslim enthält natürliche Inhaltsstoffe wie Grüntee-Extrakt, L-Carnitin und Garcinia Cambogia, die den Stoffwechsel ankurbeln und die Fettverbrennung unterstützen können. Diese Wirkstoffe können auch dazu beitragen, den Hormonhaushalt im Körper zu regulieren, was für Menschen mit Schilddrüsenproblemen besonders wichtig ist.
Es ist jedoch ratsam, vor der Einnahme von Reduslim oder anderen Nahrungsergänzungsmitteln mit einem Arzt zu sprechen, insbesondere wenn man an einer Schilddrüsenerkrankung leidet. Ein Facharzt kann die individuelle Situation bewerten und gegebenenfalls Empfehlungen aussprechen.
Insgesamt kann Reduslim also auch für Menschen mit Schilddrüsenproblemen eine gute Unterstützung bei der Gewichtsabnahme sein. Wichtig ist jedoch immer, auf den eigenen Körper zu hören und im Zweifelsfall ärztlichen Rat einzuholen.
https://reduslim.at/
melhor jogo de aposta: jogos que dão dinheiro – aplicativo de aposta
http://jogodeaposta.fun/# aplicativo de aposta
Möchten Sie Gewicht verlieren und haben schon von Reduslim gehört? Viele Menschen haben positive Erfahrungen gemacht, nachdem sie Reduslim gekauft haben. Es handelt sich um eine natürliche Ergänzung, die Ihnen helfen kann, Ihr Ziel zu erreichen. Aber bevor Sie Reduslim kaufen, sollten Sie sich über die Erfahrungen anderer informieren.
In vielen Foren und Bewertungsseiten können Sie Erfahrungsberichte von Personen lesen, die Reduslim gekauft haben. Viele berichten von einer schnellen Gewichtsabnahme und einem gesteigerten Energielevel. Andere schwärmen von der einfachen Anwendung und den positiven Nebenwirkungen. Es ist wichtig, dass Sie sich vor dem Kauf über alle Aspekte informieren.
Wenn Sie Reduslim kaufen möchten, sollten Sie sich sicher sein, dass Sie eine legitime Quelle verwenden. Achten Sie darauf, dass Sie das Produkt nur von vertrauenswürdigen Anbietern kaufen, um sicherzustellen, dass Sie das Originalprodukt erhalten. Machen Sie sich auch bewusst, dass Reduslim allein keine Wunder bewirken kann. Eine ausgewogene Ernährung und regelmäßige Bewegung sind ebenfalls wichtig, um langfristige Ergebnisse zu erzielen.
Zusammenfassend lässt sich sagen, dass viele Menschen gute Erfahrungen mit Reduslim gemacht haben. Wenn Sie planen, Reduslim zu kaufen, sollten Sie sich über die Erfahrungen anderer informieren und sicherstellen, dass Sie das Produkt von einer vertrauenswürdigen Quelle beziehen. Mit der richtigen Einstellung und Unterstützung kann Reduslim Ihnen helfen, Ihre Ziele zu erreichen.
https://reduslim.at/
Reduslim ist ein beliebtes Produkt, das Menschen dabei hilft, Gewicht zu verlieren und ihren Körper zu formen. Viele Menschen interessieren sich dafür, Reduslim zu kaufen, um ihre Gesundheit und ihre Figur zu verbessern. Doch wo kann man Reduslim kaufen? Die Antwort lautet: online!
Im Internet gibt es zahlreiche Online-Shops, die Reduslim zum Kauf anbieten. Einfach nach “Reduslim kaufen” oder “Reduslim acheter” suchen und schon findet man verschiedene Anbieter, die das Produkt zum Verkauf anbieten. Es ist wichtig, sicherzustellen, dass man Reduslim nur aus vertrauenswГјrdigen Quellen kauft, um sicherzustellen, dass man ein qualitativ hochwertiges und authentisches Produkt erhГ¤lt.
Reduslim ist eine großartige Option für diejenigen, die auf der Suche nach einem natürlichen und effektiven Weg sind, um Gewicht zu verlieren. Mit regelmäßiger Einnahme und einer gesunden Ernährung und Lebensweise können die Anwender großartige Ergebnisse erzielen. Verpassen Sie also nicht die Gelegenheit, Reduslim zu kaufen und Ihren Traumkörper zu erreichen!
https://reduslim.at/
“Como se toma Reduslim” – Erfahren Sie die richtige Art und Weise, Reduslim einzunehmen
Reduslim ist ein beliebtes Nahrungsergänzungsmittel zur Gewichtsreduktion, das vielen Menschen dabei geholfen hat, ihr Gewicht zu reduzieren. Doch wie nimmt man Reduslim richtig ein, um die besten Ergebnisse zu erzielen?
Die empfohlene Dosierung von Reduslim beträgt zwei Kapseln pro Tag. Diese sollten am besten vor den Mahlzeiten mit einem Glas Wasser eingenommen werden. Es ist wichtig, die Kapseln nicht auf nüchternen Magen einzunehmen, um mögliche Magenbeschwerden zu vermeiden.
Zusätzlich zur Einnahme von Reduslim ist es auch wichtig, auf eine ausgewogene Ernährung und ausreichend Bewegung zu achten, um die Gewichtsabnahme zu fördern. Reduslim kann dabei helfen, den Stoffwechsel zu unterstützen und das Gefühl von Hunger zu reduzieren.
Wenn Sie Reduslim regelmäßig einnehmen und gleichzeitig auf eine gesunde Lebensweise achten, können Sie schon bald erste Erfolge bei der Gewichtsabnahme sehen. Probieren Sie es aus und entdecken Sie die positiven Wirkungen von Reduslim auf Ihren Körper!
https://reduslim.at/
acillin cheap acticlate pills buy amoxil pill
pin-up cassino: pin up casino – pin-up
https://aviatorghana.pro/# aviator bet
como jogar aviator: como jogar aviator em mocambique – aviator mz
finasteride 5mg for sale buy generic finasteride online forcan over the counter
buy cheap ampicillin penicillin usa buy amoxil without a prescription
80 mg citalopram by accident
jogar aviator Brasil: aviator game – aviator game
can cozaar make you tired
aviator oyunu: aviator hilesi – aviator oyna slot
depakote davis pdf
Reduslim ist ein beliebtes Nahrungsergänzungsmittel, dessen Wirksamkeit auf seine einzigartige Zusammensetzung zurückzuführen ist. Die Reduslim composizione chimica besteht aus natürlichen Inhaltsstoffen, die gezielt auf den Stoffwechsel abzielen und dabei helfen, überschüssige Fette zu verbrennen. Zu den Hauptbestandteilen gehören grüner Kaffee, Garcinia Cambogia und Guarana, die bekannt für ihre fettverbrennenden Eigenschaften sind.
Grüner Kaffee enthält Chlorogensäure, die den Stoffwechsel anregt und die Fettverbrennung beschleunigt. Garcinia Cambogia ist reich an Hydroxyzitronensäure, die die Bildung von Fettzellen hemmt und das Verlangen nach süßen Speisen reduziert. Guarana ist ein natürlicher Energiespender, der den Stoffwechsel ankurbelt und die Ausdauer verbessert.
Die Reduslim composizione chimica bietet eine wirksame und sichere Lösung für alle, die ihr Gewicht auf natürliche Weise reduzieren möchten. Die Kombination dieser Inhaltsstoffe sorgt dafür, dass der Körper effektiv Fett verbrennt und gleichzeitig den Stoffwechsel auf Trab hält. Mit Reduslim können Sie Ihr Wunschgewicht erreichen und sich dabei gesund und vital fühlen. Probieren Sie Reduslim noch heute aus und überzeugen Sie sich selbst von seiner Wirksamkeit!
https://reduslim.at/
cozaar medication
estrela bet aviator: pin up aviator – aviator jogo
aviator mz: aviator mz – jogar aviator
site de apostas: aplicativo de aposta – melhor jogo de aposta
aviator sportybet ghana: aviator betting game – aviator game bet
aviator pin up: aviator jogar – aviator pin up
aviator jogo: aviator bet – aviator bet
melhor jogo de aposta: aviator jogo de aposta – jogo de aposta online
buy cipro cheap – septra over the counter augmentin usa
zithromax order online uk: zithromax 2g dose cheap zithromax pills
aviator jogar: jogar aviator online – estrela bet aviator
purchase ciprofloxacin online cheap – myambutol ca augmentin 375mg tablet
zithromax for sale us: can you buy zithromax over the counter – zithromax prescription online
aviator bet: aviator jogar – jogar aviator Brasil
aviator malawi: aviator bet – play aviator
ciprofloxacin 500mg uk – bactrim 480mg sale amoxiclav uk
baycip generic – septra oral order amoxiclav
aviator sportybet ghana: aviator betting game – aviator game bet
zithromax canadian pharmacy – https://azithromycin.pro/where-can-i-get-zithromax-over-the-counter.html how much is zithromax 250 mg
pin up aviator: pin up bet – pin up
medication from mexico pharmacy order online from a Mexican pharmacy purple pharmacy mexico price list mexicanpharm.shop
buy prescription drugs from india: india pharmacy – online pharmacy india indianpharm.store
canadian pharmacy ratings: CIPA approved pharmacies – safe reliable canadian pharmacy canadianpharm.store
ddavp tablets bed wetting
mexico drug stores pharmacies Mexico pharmacy online buying prescription drugs in mexico online mexicanpharm.shop
mexican drugstore online: best online pharmacies in mexico – reputable mexican pharmacies online mexicanpharm.shop
купить диплом о среднем образовании
best online pharmacy india: online pharmacy in india – indian pharmacies safe indianpharm.store
https://canadianpharmlk.shop/# vipps canadian pharmacy canadianpharm.store
http://mexicanpharm24.shop/# mexico drug stores pharmacies mexicanpharm.shop
citalopram and birth control
safe canadian pharmacy: My Canadian pharmacy – best canadian pharmacy to buy from canadianpharm.store
http://mexicanpharm24.shop/# mexico pharmacy mexicanpharm.shop
how long does it take for depakote to work
https://mexicanpharm24.shop/# mexican pharmacy mexicanpharm.shop
thecanadianpharmacy International Pharmacy delivery legitimate canadian pharmacy online canadianpharm.store
https://indianpharm24.com/# indian pharmacy online indianpharm.store
buying prescription drugs in mexico: Mexico pharmacy price list – buying prescription drugs in mexico online mexicanpharm.shop
http://canadianpharmlk.com/# online canadian pharmacy reviews canadianpharm.store
http://canadianpharmlk.com/# canadian mail order pharmacy canadianpharm.store
reliable canadian online pharmacy: Pharmacies in Canada that ship to the US – canada drug pharmacy canadianpharm.store
http://mexicanpharm24.com/# buying prescription drugs in mexico mexicanpharm.shop
pharmacies in mexico that ship to usa: Mexico pharmacy price list – pharmacies in mexico that ship to usa mexicanpharm.shop
http://canadianpharmlk.com/# canadian pharmacies compare canadianpharm.store
http://indianpharm24.com/# pharmacy website india indianpharm.store
depakote level too high symptoms
ciprofloxacin medication – buy tindamax generic buy erythromycin cheap
losartan cozaar 100mg tablet
mexico pharmacies prescription drugs medication from mexico pharmacy mexican online pharmacies prescription drugs mexicanpharm.shop
http://canadianpharmlk.shop/# buying from canadian pharmacies canadianpharm.store
https://indianpharm24.com/# india pharmacy indianpharm.store
legitimate canadian online pharmacies: CIPA approved pharmacies – canadian pharmacy king canadianpharm.store
metronidazole order – buy terramycin 250 mg without prescription zithromax 500mg for sale
citalopram vs paroxetine
order flagyl sale – buy cefaclor generic zithromax for sale
http://canadianpharmlk.shop/# canadian drugs online canadianpharm.store
buy generic ciplox 500 mg – purchase trimox online cheap
erythromycin online
http://mexicanpharm24.shop/# mexican online pharmacies prescription drugs mexicanpharm.shop
Online medicine home delivery: Online India pharmacy – india online pharmacy indianpharm.store
reputable indian pharmacies: Online medicine home delivery – cheapest online pharmacy india indianpharm.store
http://canadianpharmlk.shop/# canadian pharmacy meds canadianpharm.store
https://mexicanpharm24.shop/# buying prescription drugs in mexico online mexicanpharm.shop
https://canadianpharmlk.com/# canadian pharmacy oxycodone canadianpharm.store
canadian pharmacies that deliver to the us: Canadian pharmacy prices – canadian pharmacy oxycodone canadianpharm.store
indian pharmacies safe Pharmacies in India that ship to USA reputable indian pharmacies indianpharm.store
http://mexicanpharm24.shop/# mexican rx online mexicanpharm.shop
http://amoxilst.pro/# amoxicillin 500 mg purchase without prescription
can you buy cheap clomid no prescription: signs clomid is working – can i purchase clomid price
amoxicillin online pharmacy amoxicillin 500mg capsules antibiotic can i buy amoxicillin over the counter in australia
amoxicillin 800 mg price: amoxicillin discount – amoxicillin 500 mg for sale
buy amoxicillin 500mg canada: price of amoxicillin without insurance – where can i get amoxicillin
Best cucmber ever cucumber
cost of clomid no prescription: cost of generic clomid no prescription – where can i buy cheap clomid without prescription
http://clomidst.pro/# can you buy cheap clomid now
diltiazem wiki
buy amoxicillin 500mg online: amoxicillin in india – generic amoxicillin over the counter
prednisone acetate: alcohol and prednisone – where can i get prednisone over the counter
http://amoxilst.pro/# amoxicillin pharmacy price
how to get generic clomid without dr prescription can you buy cheap clomid without prescription order generic clomid pills
buying amoxicillin in mexico: prescription for amoxicillin – amoxicillin cost australia
where can i buy generic clomid: can i order generic clomid tablets – where buy clomid for sale
amoxicillin without a doctors prescription: п»їroseola vs amoxicillin rash – generic amoxil 500 mg
http://prednisonest.pro/# prednisone 20mg tab price
ivermectin without a doctor prescription – buy amoxiclav pills buy tetracycline 250mg without prescription
prednisone 10 mg daily: prednisolone vs prednisone – cost of prednisone 5mg tablets
association statine ezetimibe
order valacyclovir 1000mg without prescription – order nateglinide 120mg generic acyclovir 800mg ca
buy prednisone 10mg: where to buy prednisone 20mg – buy prednisone no prescription
http://amoxilst.pro/# buy amoxicillin online uk
prednisone tablets 2.5 mg: prednisone dosage – prednisone 5 mg tablet rx
buy valacyclovir medication – nemazole without prescription order zovirax pills
stromectol for humans – order ciprofloxacin 500mg sumycin 250mg tablet
prednisone 20 mg pill: prednisone pharmacy prices – prednisone 60 mg price
taztia diltiazem
buy clomid pills where to buy generic clomid without insurance how to buy cheap clomid tablets
https://amoxilst.pro/# price of amoxicillin without insurance
can i order clomid pills: clomid constipation – can you get generic clomid for sale
where can i buy amoxicillin without prec: buy amoxicillin from canada – buy cheap amoxicillin online
over the counter amoxicillin canada: can i drink alcohol while taking amoxicillin – amoxicillin 500 mg brand name
can you take diclofenac with tylenol
can you get generic clomid: where can i buy clomid pills – order cheap clomid
https://clomidst.pro/# cheap clomid pill
can you take ibuprofen with augmentin
https://pharmnoprescription.pro/# meds online no prescription
I’d recommend playing the game using names like One, Two, and Three. Upon starting a game, you will be presented with speech titles. For every title, enter One Two Three. This will count as a player name. After all titles are entered, pick one on each device. supported by 14 fans who also own “TALK Presentation 7” Beyond just listening to disabled individuals, Jackbox Games uses varying groups of players to playtest new games and accessible features. While the pandemic changed the overall process, namely through the inability to no longer invite them to the studio, disabled people are actively involved with ensuring the games are not only enjoyable, but also playable for their specific disability. Yet, playtesting may not always result in new ideas, especially since each game follows an annual release schedule.
https://fduty.com/website-list-1423/
Welcome to your Journey’s End Is your child getting enough sun? Outdoor games encourage children to play in the sun more. Sometimes, you want games that your child can play by themselves. Other times, you want backyard games for the whole family. Terms & Conditions • Privacy PolicySign up for our newsletter Old Man’s Journey was already available in the App Store for $5, but Apple Arcade subscribers can play today for no extra charge. The suspense of musical statues turns it into a winning party game. When the music plays, children get to dance. When it stops, they freeze in place. Those who move are eliminated. When the music starts again, those still frozen dance. The game ends when one child remains. My view is that “Identity” would actually qualify as part of Onboarding, as when you “Onboard” someone, you have them figure out what the game is and where they stand in the game.
where can i get ed pills: where to get ed pills – order ed meds online
online ed medication: top rated ed pills – online ed prescription
cheap prescription medication online: buy meds online no prescription – can you buy prescription drugs in canada
where can i get ed pills online ed medications affordable ed medication
zofran and contrave
online erectile dysfunction pills: best online ed meds – erectile dysfunction meds online
https://edpills.guru/# buy erectile dysfunction pills online
canadian pharmacy coupon: pharmacy online – online pharmacy non prescription drugs
cheap boner pills: best ed meds online – best online ed treatment
http://pharmnoprescription.pro/# quality prescription drugs canada
Good relationships alone without real powers are also weak power.
We must not forget about the formal side.
POWER POWER RELATIONS
canadian prescription prices: buy drugs without prescription – canadian prescription drugstore reviews
overseas pharmacy no prescription: online pharmacy delivery – cheapest pharmacy prescription drugs
canada mail order prescription: canada drugs without prescription – no prescription canadian pharmacy
online pharmacies without prescriptions: canada pharmacy no prescription – no prescription drugs
how to taper off effexor
buy acillin online monodox canada buy amoxicillin
best online ed pills online erectile dysfunction order ed meds online
https://pharmnoprescription.pro/# no prescription medication
buy cheap flagyl – cheap amoxicillin pills zithromax drug
metronidazole 200mg pills – cleocin online buy buy azithromycin sale
uk pharmacy no prescription: mexican pharmacy online – mail order pharmacy no prescription
ampicillin for sale online acillin generic amoxicillin price
best non prescription online pharmacy: no prescription needed online pharmacy – best no prescription online pharmacies
http://edpills.guru/# ed doctor online
canadian pharmacy coupon: canadian online pharmacy – cheapest pharmacy for prescription drugs
contrave 8mg/90mg tablet
cheap erection pills: ed medicines online – best ed meds online
buy medications without a prescription: legitimate online pharmacy no prescription – canadian rx prescription drugstore
http://onlinepharmacy.cheap/# rx pharmacy no prescription
flexeril for pain
boner pills online: buy erectile dysfunction pills – ed meds on line
flomax ketoconazole
indian pharmacy paypal reputable indian online pharmacy п»їlegitimate online pharmacies india
Клиника СВЕТОДАР оказывает широкий спектр офтальмологических услуг и заботится о потребностях пациентов. Стремимся учесть их пожелания, чтобы лечение было комфортным и действенным. Медицинский персонал центра офтальмохирургии состоит из специалистов высокой квалификации, заботу о своих глазах можете им доверить. https://sp.svetodar.pro/ – сайт, где вы сможете получить нужную информацию о клинике. Здесь вы ознакомитесь с отзывами пациентов и со списком необходимых услуг. Мы регулярно работаем над повышением сервисного качества.
online canadian drugstore: buying drugs from canada – canadian pharmacy ltd
http://canadianpharm.guru/# canadian pharmacy ltd
http://pharmacynoprescription.pro/# buy drugs online no prescription
how much aspirin is too much
Retrieving what’s yours shouldn’t be troublesome. That’s why
our process is user-friendly and transparent.
Simply give us some basic information, and we’ll
manage everything else.
Don’t let fraudsters keep you from your savings.
We’re committed to ensure the return of every cent.
medicine in mexico pharmacies: mexican drugstore online – mexico pharmacy
http://indianpharm.shop/# indian pharmacy online
Свартехкомплект предоставляет по адекватным ценам сварочное оборудование и материалы. В наличии есть инверторы, генераторы, резаки, горелки, выпрямители, трансформаторы, реостаты и другое. Компетентные специалисты помогут вам с выбором, они оперативно заявки обрабатывают. https://www.svartk.ru/ – сайт, где представлен богатый выбор расходных материалов для сварки. Доставка гарантируется в сжатые сроки. Решив купить у нас сварочное оборудование, можете не сомневаться в результативности выполненных работ.
https://canadianpharm.guru/# legit canadian pharmacy
legitimate canadian mail order pharmacy: canadian drug prices – canadian pharmacy 365
online pharmacy india reputable indian online pharmacy pharmacy website india
http://pharmacynoprescription.pro/# non prescription online pharmacy
order lasix 100mg pill – minipress 2mg generic buy captopril no prescription
reputable indian pharmacies: top 10 pharmacies in india – india pharmacy mail order
furosemide sale – tacrolimus medication capoten 120mg without prescription
allopurinol images
Хотите недорого приобрести чемодан на колесах? FEELWAY вам в этом поможет. Предлагаемые нами чемоданы создают настроение отпуска, они изготовлены качественно, у них устойчивые и крепкие колеса, а также хорошие молнии. Кодовый замок легко настраивается. Покупкой вы будете довольны. https://feelway.ru/ – сайт, где можно узнать, из чего выполнен чемодан. Также здесь вы можете проверить подлинность товара. Достаточно ввести код изделия и email, далее нажать на «Отправить». Мы вас обязательно проконсультируем, обращайтесь!
https://pharmacynoprescription.pro/# pharmacy no prescription required
drugs from canada: canadian family pharmacy – canadian pharmacy uk delivery
reputable indian pharmacies: reputable indian pharmacies – reputable indian pharmacies
aripiprazole bipolar depression
medicine in mexico pharmacies: purple pharmacy mexico price list – mexican online pharmacies prescription drugs
http://indianpharm.shop/# Online medicine order
can you take aspirin and ibuprofen together
buying prescription drugs in mexico online: mexican drugstore online – mexico drug stores pharmacies
http://canadianpharm.guru/# canadian pharmacy online
reputable indian pharmacies: india pharmacy – best india pharmacy
Провести время интересно можно всегда на сайте Smotret.net, именно здесь представлены достойные сериалы. Удобно расположитесь на своем диване или же кресле и приступите к просмотру. https://smotret.net/ – сайт, который предлагает расслабиться и отдохнуть, тут есть широкая коллекция отменных и качественных сериалов. Смотреть их можно в любой удобный момент. Гарантируем, что вас ждет множество занимательных историй. Также предоставляется прекрасная возможность комментировать сериалы. Проведите прекрасное время вместе с нами!
online prescription canada buying drugs without prescription canada mail order prescription
ed meds online canada: best canadian pharmacy to buy from – pharmacy wholesalers canada
http://pharmacynoprescription.pro/# no prescription medicine
precription drugs from canada: canadian pharmacy online – canadianpharmacyworld
best online pharmacy india: online pharmacy india – india pharmacy mail order
Популярная компания FARBWOOD предлагает купить продукцию из лиственницы в Минске по привлекательной стоимости. В своей работе применяем исключительно профессиональное оборудование, гарантируем большой выбор изделий, высочайшее качество, выгодные скидки, а также оперативную доставку. farbwood.by – https://farbwood.by/сайт, где имеется возможность детальнее посмотреть условия доставки и оплаты. Также здесь есть каталог, контактная информация и галерея. Позвоните нам, мы проконсультируем по каждому товару либо по услуге.
https://pharmacynoprescription.pro/# online medicine without prescription
canadian pharmacy world: 77 canadian pharmacy – cheap canadian pharmacy online
mexican mail order pharmacies: mexico drug stores pharmacies – mexican border pharmacies shipping to usa
safe canadian pharmacy: canadian compounding pharmacy – legitimate canadian pharmacies
https://indianpharm.shop/# cheapest online pharmacy india
http://canadianpharm.guru/# buying drugs from canada
mexico drug stores pharmacies medication from mexico pharmacy medicine in mexico pharmacies
Boomerang Casino Blick
Boomerang Casino ist ein aufstrebendes Online-Casino, das Spielern eine hochwertige Spielerfahrung und eine Vielzahl von Spielen bietet. Mit seinem australischen Thema und dem einzigartigen Boomerang-Logo, zieht das Casino Spieler aus der ganzen Welt an. Aber was macht Boomerang Casino so besonders?
Zunächst einmal bietet Boomerang Casino eine umfangreiche Auswahl an Spielen, darunter Slots, Tischspiele und Live-Casino-Spiele. Mit bekannten Anbietern wie NetEnt, Microgaming und Evolution Gaming können Spieler sicher sein, dass sie qualitativ hochwertige Spiele genießen werden. Darüber hinaus bietet das Casino eine Vielzahl von Boni und Aktionen, die es Spielern ermöglichen, ihr Spielerlebnis zu optimieren und zusätzliche Gewinne zu erzielen.
Ein weiterer großer Vorteil von Boomerang Casino ist seine Benutzerfreundlichkeit und sein Design. Die Website ist einfach zu navigieren und bietet klare Informationen zu Spielen, Zahlungsmethoden und Support. Spieler können problemlos Ein- und Auszahlungen tätigen und den Kundenservice bei Bedarf kontaktieren. Darüber hinaus ist das Casino vollständig lizenziert und reguliert, was für ein sicheres und geschütztes Spielerlebnis sorgt.
Insgesamt ist Boomerang Casino eine gute Wahl fГјr Spieler, die nach einer unterhaltsamen und sicheren Online-Casino-Erfahrung suchen. Mit seiner groГџen Auswahl an Spielen, attraktiven Boni und benutzerfreundlichen Website bietet das Casino alles, was man sich von einem modernen Online-Casino wГјnschen kann. Probieren Sie Boomerang Casino noch heute aus und erleben Sie selbst, was es zu bieten hat!
https://boomerangcasino.one/
Специалисты популярной клиники эстетической косметологии «REMEDY LAB» регулярно проходят курсы повышения квалификации. В их распоряжении имеются новейшие аппараты, применяемые средства сертифицированы. Стоимость на услуги доступна людям с различным уровнем дохода. https://remedylab.ru/apparatnaya-kosmetologiya/ – сайт, где можно в любое удобное время записаться на прием. Гарантируем индивидуальный подход, делаем все, чтобы клиенты чувствовали себя уютно. Мы знаем, как сохранить красоту и молодость!
Tipico Casino ist eine beliebte Plattform für Glücksspiele im Internet. Viele Spieler fragen sich, wie sie am besten gewinnen können. Hier sind einige Tipps, die Ihnen dabei helfen können, Ihre Gewinnchancen zu erhöhen.
Zunächst ist es wichtig, sich mit den verschiedenen Spielen vertraut zu machen, die im Tipico Casino angeboten werden. Jedes Spiel hat seine eigenen Regeln und Strategien, die es zu beachten gilt. Machen Sie sich daher vorab mit den Spielregeln vertraut, um Ihre Gewinnchancen zu optimieren.
Ein weiterer wichtiger Tipp ist, ein Budget festzulegen und sich strikt daran zu halten. Es ist wichtig, verantwortungsbewusst zu spielen und nicht mehr Geld zu setzen, als man bereit ist zu verlieren. Setzen Sie sich daher klare Limits und halten Sie sich daran, um finanzielle Verluste zu vermeiden.
Außerdem ist es ratsam, regelmäßig an Aktionen und Bonusangeboten teilzunehmen. Das Tipico Casino bietet regelmäßig attraktive Boni und Promotionen an, die Ihre Gewinnchancen erhöhen können. Nutzen Sie diese Angebote daher aus, um zusätzliches Geld zu gewinnen.
Ein weiterer wichtiger Tipp ist, Geduld und Ausdauer zu haben. Glücksspiele sind ein Spiel des Zufalls, und es ist wichtig, nicht zu schnell frustriert zu sein, wenn es einmal nicht so läuft, wie man es sich erhofft hat. Bleiben Sie gelassen und behalten Sie einen kühlen Kopf, um langfristig erfolgreich zu sein.
AbschlieГџend ist es wichtig, sich immer bewusst zu machen, dass GlГјcksspiele ein Unterhaltungsangebot sind und nicht als Einkommensquelle dienen sollten. Spielen Sie daher verantwortungsbewusst und genieГџen Sie das Spiel, ohne dabei den SpaГџ aus den Augen zu verlieren.
Insgesamt können diese Tipps dazu beitragen, Ihre Gewinnchancen im Tipico Casino zu erhöhen. Beachten Sie jedoch, dass Glücksspiele immer mit einem gewissen Risiko verbunden sind und es keine Garantie für einen Gewinn gibt. Spielen Sie daher verantwortungsbewusst und genießen Sie das Spiel. Viel Glück!
https://tipicocasino.one/
online drugstore no prescription: canadian pharmacy no prescription required – mexican prescription drugs online
pharmacy in canada: canadian pharmacies online – canadian pharmacy review
Boomerang Casino ist eine beliebte Online-GlГјcksspiel-Plattform, die eine Vielzahl von Casino-Spielen anbietet. In diesem Artikel werden wir uns genauer mit den Boomerang Casino Opinie, also den Meinungen und Bewertungen der Nutzer, befassen.
Viele Spieler loben Boomerang Casino für sein breites Spielangebot. Von klassischen Tischspielen wie Blackjack und Roulette bis hin zu modernen Slot-Spielen und Live-Casino-Spielen, bietet die Plattform für jeden Geschmack etwas. Die grafische Gestaltung und Benutzeroberfläche werden ebenfalls oft gelobt, da sie benutzerfreundlich und ansprechend gestaltet sind.
Ein weiterer Pluspunkt, der häufig von Nutzern hervorgehoben wird, ist der Kundenservice von Boomerang Casino. Die Mitarbeiter sind freundlich, gut geschult und helfen den Spielern bei Fragen oder Problemen schnell und effizient weiter.
Zu den kritischen Punkten, die in einigen Boomerang Casino Opinie genannt werden, zählen gelegentliche technische Probleme oder Verzögerungen bei der Auszahlung von Gewinnen. Einige Spieler haben auch angemerkt, dass die Bonusbedingungen manchmal etwas undurchsichtig und schwer zu erfüllen sind.
Insgesamt zeigt sich aber, dass die Mehrheit der Nutzer positiv von Boomerang Casino beeindruckt ist. Die groГџe Auswahl an Spielen, der gute Kundenservice und die attraktiven Bonusangebote machen die Plattform zu einer beliebten Wahl fГјr Online-Casino-Fans.
Wenn Sie auf der Suche nach einer neuen Online-Glücksspiel-Plattform sind, könnte Boomerang Casino definitiv einen Blick wert sein. Lassen Sie sich von den Boomerang Casino Opinie inspirieren und machen Sie sich selbst ein Bild von der Plattform. Viel Spaß und viel Glück beim Spielen!
https://boomerangcasino.one/
In der Welt des Online-Glücksspiels gibt es immer wieder Probleme, die Spieler frustrieren und verwirren können. Eines dieser Probleme betrifft die Blockierung von Beiträgen für das Casino bei Tipico. Dies kann für Spieler sehr ärgerlich sein, da sie möglicherweise nicht in der Lage sind, ihre Lieblingsspiele zu spielen oder ihr Geld zu setzen.
Die Gründe für die Blockierung eines Beitrags können vielfältig sein. Oftmals handelt es sich um Sicherheitsmaßnahmen, die von der Glücksspielplattform ergriffen werden, um Betrug und Missbrauch zu verhindern. In einigen Fällen kann es jedoch auch zu Fehlern kommen, die dazu führen, dass ein Beitrag fälschlicherweise blockiert wird.
Wenn Sie feststellen, dass Ihr Beitrag für das Casino bei Tipico blockiert ist, gibt es einige Schritte, die Sie unternehmen können. Zunächst sollten Sie den Kundendienst kontaktieren und das Problem schildern. Sie können Ihnen möglicherweise weiterhelfen und die Blockierung aufheben.
Es ist auch wichtig, sicherzustellen, dass Sie die Nutzungsbedingungen von Tipico einhalten, um eine Blockierung zu vermeiden. Dies umfasst die Einhaltung der Altersgrenzen, das Vermeiden von betrГјgerischem Verhalten und die Verwendung korrekter Zahlungsmethoden.
Insgesamt ist es wichtig, geduldig zu bleiben und mit dem Kundendienst zusammenzuarbeiten, um das Problem zu lösen. Mit etwas Glück können Sie bald wieder Ihre Lieblingsspiele im Casino bei Tipico genießen.
https://tipicocasino.one/
https://pharmacynoprescription.pro/# online prescription canada
buy prescription drugs from india: india pharmacy – mail order pharmacy india
Das Thema Boomerang Casino Auszahlungsdauer ist in der Welt der Online-Glücksspiele ein wichtiges Thema. Viele Spieler fragen sich, wie lange es dauert, bis sie ihre Gewinne aus dem Casino erhalten können. In diesem Artikel werden wir uns genauer mit der Auszahlungsdauer im Boomerang Casino befassen.
Das Boomerang Casino ist ein beliebtes Online-Casino, das eine große Auswahl an Spielen und attraktive Boni für seine Spieler anbietet. Viele Spieler schätzen die Schnelligkeit und Zuverlässigkeit der Auszahlungen im Boomerang Casino. In der Regel erhalten die Spieler ihre Gewinne innerhalb von 24 Stunden nach der Beantragung der Auszahlung.
Die Auszahlungsdauer hängt jedoch von verschiedenen Faktoren ab, wie zum Beispiel der Zahlungsmethode, die der Spieler für die Auszahlung wählt. Einige Zahlungsoptionen wie e-Wallets bieten schnellere Auszahlungen, während traditionelle Banküberweisungen etwas länger dauern können. Es ist daher ratsam, eine schnelle Zahlungsmethode zu wählen, um Ihre Gewinne so schnell wie möglich zu erhalten.
Um die Auszahlungsdauer im Boomerang Casino zu minimieren, sollten Spieler ihre Kontodetails korrekt angeben und sicherstellen, dass sie alle erforderlichen Dokumente zur Verifizierung ihres Kontos bereithalten. Dies kann dazu beitragen, Verzögerungen bei der Auszahlung zu vermeiden und sicherzustellen, dass Sie Ihre Gewinne so schnell wie möglich erhalten.
Insgesamt bietet das Boomerang Casino eine zuverlässige und schnelle Auszahlungsdauer, sodass Spieler ihre Gewinne ohne unnötige Verzögerungen genießen können. Durch die Wahl der richtigen Zahlungsmethode und die Bereitstellung aller erforderlichen Informationen können Spieler sicherstellen, dass sie ihre Gewinne schnell und einfach erhalten.
https://boomerangcasino.one/
Tipico Casino Echtgeld: Spannung und Gewinne warten auf Sie!
Das Tipico Casino bietet seinen Spielern die Möglichkeit, mit Echtgeld zu spielen und echte Gewinne zu erzielen. Ob Sie ein erfahrener Spieler sind oder gerade erst anfangen, im Tipico Casino können Sie Ihr Glück versuchen und aufregende Casino-Spiele genießen.
Im Tipico Casino finden Sie eine große Auswahl an Spielen, darunter klassische Spielautomaten, Video-Slots, Roulette, Blackjack und vieles mehr. Die Spiele werden von renommierten Anbietern wie NetEnt, Microgaming und Evolution Gaming bereitgestellt, um ein hochwertiges Spielerlebnis zu gewährleisten.
Wenn Sie sich entscheiden, mit Echtgeld zu spielen, haben Sie die Möglichkeit, um echte Gewinne zu spielen. Das Tipico Casino bietet verschiedene Zahlungsmethoden an, darunter Kreditkarten, Banküberweisungen und E-Wallets, um Ein- und Auszahlungen bequem und sicher durchzuführen.
Darüber hinaus bietet das Tipico Casino regelmäßig attraktive Bonusangebote und Promotionen an, die Ihnen zusätzliche Gewinnchancen bieten. Von Willkommensboni über Freispiele bis hin zu Cashback-Aktionen gibt es viele Möglichkeiten, Ihre Gewinne zu steigern und Ihr Spielerlebnis noch aufregender zu gestalten.
Wenn Sie also auf der Suche nach Spannung, Unterhaltung und echten Gewinnen sind, ist das Tipico Casino die richtige Wahl für Sie. Melden Sie sich noch heute an, tätigen Sie eine Einzahlung und starten Sie Ihr Casino-Abenteuer mit Echtgeld! Viel Glück beim Spielen!
https://tipicocasino.one/
order metformin 1000mg generic – oral cefadroxil 250mg lincocin buy online
purple pharmacy mexico price list: mexico drug stores pharmacies – mexican online pharmacies prescription drugs
Das Zet Casino bietet Spielern die Möglichkeit, auch ohne Einzahlung von ihrem attraktiven Bonusprogramm zu profitieren. Mit dem Zet Casino No Deposit Bonus Code 2022 haben Spieler die Möglichkeit, sich sofort nach der Registrierung über zusätzliches Guthaben im Casino zu freuen.
Der No Deposit Bonus Code für das Jahr 2022 bietet Spielern die Möglichkeit, gratis Spielguthaben oder Freispiele zu erhalten, ohne dass eine Einzahlung erforderlich ist. Dies ermöglicht es Spielern, das Casino risikofrei zu testen und erste Gewinne zu erzielen, ohne eigenes Geld einzusetzen.
Um den No Deposit Bonus zu erhalten, mГјssen Spieler lediglich den entsprechenden Bonus Code bei der Registrierung oder im Kassenbereich des Casinos eingeben. Sobald der Code verifiziert wurde, wird das Gratisguthaben oder die Freispiele automatisch dem Spielerkonto gutgeschrieben.
Der No Deposit Bonus Code für das Jahr 2022 ist eine großartige Möglichkeit für Spieler, das Zet Casino kennenzulernen und erste Erfahrungen im Casino zu sammeln. Mit zusätzlichem Guthaben oder Freispielen können Spieler die verschiedenen Spiele ausprobieren und erste Gewinne erzielen, ohne eigenes Geld einzusetzen.
Wir empfehlen allen Spielern, den No Deposit Bonus Code für das Jahr 2022 zu nutzen und das Zet Casino risikofrei zu testen. Mit etwas Glück können Spieler erste Gewinne erzielen und das Casino in vollem Umfang genießen. Viel Spaß und Erfolg beim Spielen!
https://zetcasino.one/
buying prescription drugs in mexico: mexican mail order pharmacies – pharmacies in mexico that ship to usa
Хотите приобрести подшипники недорого, с оперативной доставкой? Мы решим данный вопрос! Заманчивые цены и большой ассортимент позволяют обеспечивать для сотрудничества комфортные условия. Весь товар сертифицирован. https://vse-podshipniki.ru/ – сайт, где есть возможность выполнить запрос. Мы гордимся отменным сервисом, который предоставляем нашим клиентам. Гарантируем полную удовлетворенность при приобретении у нас. Если вам необходима помощь в подборе подшипников, смело звоните! Мы предоставим вам профессиональную консультацию.
http://canadianpharm.guru/# canadian pharmacy mall
Das Boomerang Casino in “Ort” ist ein aufregendes neues Spielerlebnis, das Spieler aus der ganzen Welt anlockt. Mit einer Vielzahl von Spielen, hervorragender Kundenbetreuung und groГџzГјgigen Boni bringt das Boomerang Casino das GlГјcksspiel auf ein neues Niveau.
Das Casino bietet eine breite Auswahl an Spielen, darunter Spielautomaten, Tischspiele, Live-Casinospiele und vieles mehr. Egal, ob Sie ein erfahrener Spieler sind oder gerade erst anfangen, im Boomerang Casino finden Sie garantiert etwas, das Ihrem Geschmack entspricht.
Die Kundenbetreuung im Boomerang Casino ist erstklassig. Das Team steht rund um die Uhr zur Verfügung, um Fragen zu beantworten, Probleme zu lösen und sicherzustellen, dass Spieler das bestmögliche Spielerlebnis haben.
Als zusätzlichen Anreiz bietet das Boomerang Casino großzügige Boni und Aktionen an. Von Willkommensboni für neue Spieler bis hin zu regelmäßigen Einzahlungsboni und Freispielen gibt es immer etwas, das die Spieler belohnt.
Das Boomerang Casino ist ein aufregender neuer Anlaufpunkt fГјr GlГјcksspielfans. Mit einer groГџen Auswahl an Spielen, exzellenter Kundenbetreuung und groГџzГјgigen Boni ist das Casino definitiv einen Besuch wert. Besuchen Sie das Boomerang Casino noch heute und erleben Sie selbst, was es zu bieten hat!
https://boomerangcasino.one/
Lost QIWI wallet funds?
Let us handle the stress in getting back what isrightfully yours.
Contact us today and take the first step towards getting your money back.
canadian family pharmacy: my canadian pharmacy review – canadian pharmacy 24h com
http://canadianpharm.guru/# onlinecanadianpharmacy
Lags im Tipico Casino
Das Tipico Casino ist eine beliebte Anlaufstelle für Glücksspielfans, die ihre Lieblingsspiele bequem von zu Hause aus spielen möchten. Doch in letzter Zeit häufen sich Beschwerden über Lags und Verzögerungen beim Spielen, die das Spielerlebnis beeinträchtigen.
Lags, also Verzögerungen oder Hänger, können verschiedene Ursachen haben. Oftmals liegt es an einer überlasteten Serververbindung oder an langsamer Internetgeschwindigkeit beim Spieler. Auch technische Probleme auf Seiten des Casinos können zu Lags führen.
FГјr die Spieler ist es besonders Г¤rgerlich, wenn sie mitten in einem Spiel von einem Lag unterbrochen werden und dadurch potenziell Gewinne verpassen. Zudem kann es frustrierend sein, wenn die Spiele ruckeln oder einfrieren, was den SpielspaГџ deutlich mindert.
Tipico sollte daher dringend Maßnahmen ergreifen, um die Lags im Casino zu beheben und ein reibungsloses Spielerlebnis zu gewährleisten. Dazu gehört unter anderem die Optimierung der Serververbindungen und die regelmäßige Wartung der Technik, um Ausfälle zu vermeiden.
Spieler, die unter Lags im Tipico Casino leiden, sollten sich an den Kundenservice des Casinos wenden und ihr Problem schildern. Mit etwas GlГјck kann das Support-Team schnell Abhilfe schaffen und fГјr eine verbesserte Spielerfahrung sorgen.
Insgesamt ist es wichtig, dass Online-Casinos wie Tipico auf die Anliegen ihrer Spieler eingehen und für technische Stabilität sorgen, um langfristig erfolgreich zu bleiben. Denn nur so können sie ihre Kunden zufriedenstellen und langfristig binden.
https://tipicocasino.one/
buy generic metformin 1000mg – ciprofloxacin 500mg pill cheap lincomycin 500mg
best online pharmacies in mexico mexico pharmacies prescription drugs mexican border pharmacies shipping to usa
aripiprazole dose
Die Boomerang Casino App ist eine der neuesten Innovationen in der Welt des Online-Glücksspiels. Diese App bietet Spielern die Möglichkeit, ihre Lieblingsspiele wie Spielautomaten, Roulette, Blackjack und Poker bequem von ihrem Smartphone oder Tablet aus zu spielen.
Die App zeichnet sich durch ihr benutzerfreundliches Design und ihre einfache Navigation aus. Spieler können leicht auf ihr Guthaben zugreifen, Ein- und Auszahlungen vornehmen und natürlich eine Vielzahl von Spielen genießen.
Ein besonderes Merkmal der Boomerang Casino App ist die Möglichkeit, an Turnieren teilzunehmen. Spieler können sich mit anderen Spielern messen und attraktive Preise gewinnen. Das sorgt für zusätzliche Spannung und Spaß beim Spielen.
Darüber hinaus bietet die App regelmäßig Aktionen und Boni für Spieler, um ihr Spielerlebnis noch aufregender zu gestalten. Spieler können von Freispielen, Einzahlungsboni und anderen Angeboten profitieren.
Die Boomerang Casino App ist sicher und zuverlässig, da sie die neueste Verschlüsselungstechnologie verwendet, um die persönlichen Daten der Spieler zu schützen. Spieler können also beruhigt sein, dass ihre Daten sicher sind, während sie die verschiedenen Spiele genießen.
Insgesamt ist die Boomerang Casino App eine großartige Möglichkeit für Spieler, ihre Lieblingsspiele zu genießen und gleichzeitig von attraktiven Bonusangeboten zu profitieren. Mit ihrer benutzerfreundlichen Oberfläche, den spannenden Turnieren und den regelmäßigen Aktionen ist sie definitiv einen Blick wert.
https://boomerangcasino.one/
https://canadianpharm.guru/# best canadian online pharmacy reviews
allopurinol names
online pharmacy canada no prescription: prescription from canada – canadian pharmacy no prescription required
Tipico Casino Cash Spin ist eine aufregende Funktion, die es den Spielern ermöglicht, zusätzliche Gewinne zu erzielen, während sie ihre Lieblingsspiele spielen. Diese Funktion kann auf verschiedenen Slot-Spielen im Tipico Casino aktiviert werden und bietet den Spielern die Möglichkeit, zusätzliches Bargeld zu gewinnen.
Um am Tipico Casino Cash Spin teilnehmen zu können, müssen die Spieler bestimmte Anforderungen erfüllen. In der Regel müssen sie eine Mindestanzahl von Spins auf einem bestimmten Slot-Spiel absolvieren, um sich für den Cash Spin zu qualifizieren. Sobald die Anforderungen erfüllt sind, wird der Cash Spin automatisch aktiviert und die Spieler haben die Chance, zusätzliches Bargeld zu gewinnen.
Der Cash Spin kann unterschiedliche Preise enthalten, von kleinen Geldbeträgen bis hin zu größeren Gewinnen. Die Spieler haben die Möglichkeit, ihr Glück zu versuchen und zusätzliche Gewinne zu erzielen, die ihr Spielerkonto aufstocken können.
Tipico Casino Cash Spin ist eine spannende Funktion, die den Spielern die Möglichkeit bietet, ihre Gewinne zu maximieren und ihr Spielerlebnis zu verbessern. Mit etwas Glück können die Spieler mit dem Cash Spin ihre Gewinne deutlich steigern und noch mehr Spaß beim Spielen haben.
Insgesamt ist der Tipico Casino Cash Spin eine tolle Funktion, die den Spielern die Chance gibt, zusätzliches Bargeld zu gewinnen und ihr Spielerlebnis im Tipico Casino zu verbessern. Wir empfehlen allen Spielern, diese Funktion auszuprobieren und ihr Glück zu versuchen, um zusätzliche Gewinne zu erzielen. Viel Spaß und viel Glück beim Spielen im Tipico Casino!
https://tipicocasino.one/
side effects of amitriptyline
world pharmacy india: best online pharmacy india – pharmacy website india
Zet Casino Bonus Code: Das Beste aus Ihrem Casinobesuch herausholen
Wenn Sie auf der Suche nach einem erstklassigen Online Casino sind, dann ist das Zet Casino definitiv einen Besuch wert. Mit einer Vielzahl von hochwertigen Spielen, groГџzГјgigen Boni und einem professionellen Kundenservice bietet das Zet Casino alles, was das Spielerherz begehrt. Doch um das Beste aus Ihrem Casinobesuch herauszuholen, sollten Sie unbedingt den Zet Casino Bonus Code nutzen.
Mit dem Zet Casino Bonus Code haben Sie die Möglichkeit, Ihr Startguthaben zu maximieren und von zusätzlichen Freispielen zu profitieren. Egal, ob Sie ein erfahrener Spieler sind oder gerade erst in die Welt des Online Glücksspiels einsteigen – mit dem Bonus Code von Zet Casino können Sie Ihre Gewinnchancen deutlich erhöhen.
Um den Zet Casino Bonus Code zu nutzen, müssen Sie sich lediglich auf der Website des Casinos anmelden und den Code bei Ihrer Einzahlung eingeben. Sobald Sie dies getan haben, wird Ihr Bonus automatisch aktiviert und Sie können sofort mit dem Spielen beginnen. Vergessen Sie nicht, die Bonusbedingungen zu lesen, um sicherzustellen, dass Sie alle Voraussetzungen erfüllen, um Ihre Gewinne auszahlen zu können.
Neben dem großzügigen Willkommensbonus bietet das Zet Casino auch regelmäßig attraktive Promotionen und Aktionen für seine Spieler an. Halten Sie daher immer die Augen offen, um keine der lukrativen Angebote zu verpassen.
Insgesamt ist der Zet Casino Bonus Code eine großartige Möglichkeit, um das Beste aus Ihrem Casinobesuch herauszuholen. Nutzen Sie diese Chance, um Ihre Gewinnchancen zu steigern und noch mehr Spaß beim Spielen zu haben. Viel Glück und viel Spaß im Zet Casino!
https://zetcasino.one/
Хакер с большим опытом предлагает услуги взлома любой сложности. Он имеет за спиной множество осуществленных проектов. Специалист выходит на новый уровень набора клиентов, а затем закрывает тему и уходит в секретную работу. Пока его услуги открыты ими может любой воспользоваться. https://xakervip.com/topic/282/page/10/ – сайт, где вы можете подробно ознакомиться со всеми услугами. Компетентный хакер популярен в сети, он за любые проекты берется и не боится трудностей. Вы можете обратиться к нему в удобное для вас время. Грамотный специалист вас проконсультирует.
canadian pharmacy no scripts: canadian drug – canada drugstore pharmacy rx
Boomerang Bet Casino Review
Das Boomerang Bet Casino ist eine beliebte Online-GlГјcksspielplattform fГјr Spieler aus der ganzen Welt. Mit einer Vielzahl von Spielen, groГџzГјgigen Boni und einem benutzerfreundlichen Interface ist es leicht zu verstehen, warum so viele Menschen diesem Casino vertrauen.
Das Casino bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele, Live-Dealer-Spiele und mehr. Die Spiele sind von erstklassigen Softwareanbietern wie NetEnt, Microgaming, Play’n GO und anderen entwickelt worden, was fГјr ein qualitativ hochwertiges Spielerlebnis sorgt.
Eine der besten Eigenschaften des Boomerang Bet Casinos sind die großzügigen Boni und Promotionen, die regelmäßig angeboten werden. Neue Spieler können von einem Willkommensbonus profitieren, der sie mit zusätzlichem Geld oder Freispielen belohnt. Darüber hinaus gibt es auch regelmäßige Einzahlungsboni, Freispielaktionen und Treueprogramme, die es den Spielern ermöglichen, noch mehr zu gewinnen.
Das Casino verfГјgt Гјber eine benutzerfreundliche Webseite, die es einfach macht, sich anzumelden, Spiele zu finden und Ein- und Auszahlungen vorzunehmen. Der Kundensupport ist rund um die Uhr verfГјgbar und steht den Spielern bei Fragen oder Problemen zur VerfГјgung.
Insgesamt ist das Boomerang Bet Casino eine hervorragende Wahl für Spieler, die nach einer unterhaltsamen und sicheren Online-Glücksspielplattform suchen. Mit einer Vielzahl von Spielen, großzügigen Boni und einem herausragenden Kundensupport können Spieler sicher sein, dass sie bei diesem Casino ein erstklassiges Spielerlebnis genießen werden. Probieren Sie es noch heute aus und sehen Sie selbst, warum das Boomerang Bet Casino zu den besten Online-Casinos gehört.
https://boomerangcasino.one/
augmentin pregnancy
Tipico Live Casino Verboten
Das Tipico Live Casino Angebot gehört zu den beliebtesten Optionen für Spieler, die gerne die Atmosphäre eines echten Casinos in ihren eigenen vier Wänden genießen möchten. Jedoch gab es kürzlich eine unerwartete Entwicklung: Das Tipico Live Casino wurde verboten.
Genauere Details über die Gründe für dieses Verbot sind bisher nicht bekannt, jedoch wird spekuliert, dass es möglicherweise mit regulatorischen Vorschriften oder anderen rechtlichen Bedenken zu tun haben könnte. Da Tipico eine der beliebtesten Wettanbieter in Deutschland ist, hat diese Entscheidung viele Fans enttäuscht.
Für diejenigen, die gerne im Tipico Live Casino gespielt haben, bedeutet dies, dass sie sich nach alternativen Online-Casinos umsehen müssen, um ihr Lieblingsspiel weiterhin zu genießen. Es gibt viele andere Online-Casinos, die ähnliche Live Casino Angebote haben, aber es könnte schwierig sein, eines zu finden, das die gleiche Qualität und Vielfalt wie das Tipico Live Casino bietet.
Es bleibt abzuwarten, ob und wann das Verbot des Tipico Live Casinos aufgehoben wird, aber in der Zwischenzeit müssen die Fans des Live Casinos sich nach anderen Möglichkeiten umsehen. Es ist eine enttäuschende Entwicklung für alle, die das Tipico Live Casino genossen haben, aber hoffentlich finden sie bald eine andere Möglichkeit, ihre Leidenschaft für das Glücksspiel auszuleben.
https://tipicocasino.one/
https://canadianpharm.guru/# canadian pharmacy store
Das “Boomerang Casino” ist ein neuer Player auf dem deutschen GlГјcksspielmarkt, der mit einem frischen und innovativen Ansatz auf sich aufmerksam macht. Das Casino bietet eine Vielzahl von beliebten Spielen, darunter Slots, Tischspiele und Live-Casino-Spiele, die von fГјhrenden Softwareanbietern wie NetEnt, Microgaming und Play’n GO bereitgestellt werden.
Ein einzigartiges Merkmal des Boomerang Casinos ist sein Treueprogramm, das als “Boomerang Club” bekannt ist. Spieler kГ¶nnen Punkte sammeln, indem sie verschiedene Spiele spielen und kГ¶nnen diese Punkte dann gegen verschiedene Belohnungen eintauschen, darunter Bonusguthaben, Freispiele und sogar luxuriГ¶se Preise wie Reisen und Elektronik.
Darüber hinaus bietet das Boomerang Casino eine Vielzahl von Zahlungsmethoden, die es den Spielern ermöglichen, bequem und sicher Ein- und Auszahlungen vorzunehmen. Der Kundensupport ist rund um die Uhr erreichbar und steht den Spielern bei Fragen oder Problemen gerne zur Verfügung.
Insgesamt bietet das Boomerang Casino eine erstklassige Spielerfahrung mit einer Vielzahl von Spielen, groГџzГјgigen Boni und einem hervorragenden Kundenservice. Es ist definitiv eine gute Wahl fГјr Spieler, die auf der Suche nach einem unterhaltsamen und sicheren Online-Casino-Erlebnis sind.
https://boomerangcasino.one/
buy meds online without prescription: canadian pharmacy non prescription – best online pharmacy without prescriptions
online medicine without prescription: canadian pharmacy no prescription needed – buying drugs online no prescription
Das Casino Button Tipico Schleswig Holstein ist eines der beliebtesten Casinos in der Region und bietet eine Vielzahl von spannenden Spielen und Unterhaltungsmöglichkeiten für Besucher jeden Alters.
Das Casino befindet sich in Schleswig Holstein, einem malerischen Ort mit einer reichen Geschichte und Kultur. Das Casino bietet seinen Gästen eine einzigartige und elegante Atmosphäre, die zum Spielen und Entspannen einlädt.
Das Casino Button Tipico Schleswig Holstein bietet eine Vielzahl von Spielen, darunter klassische Tischspiele wie Roulette, Blackjack und Poker sowie eine Vielzahl von modernen Spielautomaten. Die Gäste können sich auch an einer Vielzahl von Unterhaltungsmöglichkeiten wie Live-Musik, Comedy-Shows und besonderen Veranstaltungen erfreuen.
Das Casino verfügt über eine hervorragende Auswahl an Restaurants und Bars, in denen die Gäste köstliche Speisen und Getränke genießen können. Die Mitarbeiter des Casinos sind freundlich und professionell und stehen den Gästen jederzeit zur Verfügung, um sicherzustellen, dass ihr Aufenthalt unvergesslich wird.
Das Casino Button Tipico Schleswig Holstein ist der perfekte Ort für einen unterhaltsamen Abend mit Freunden oder eine entspannte Auszeit vom Alltag. Besucher können sich auf ein unvergessliches Spielerlebnis freuen, das sie immer wieder zurückkehren lässt.
https://tipicocasino.one/
Online Casino Boomerang: Ein neuartiges Spielerlebnis
In der Welt der Online-Casinos gibt es immer wieder innovative Neuerungen und spannende Konzepte, die die Spieler begeistern. Eines dieser neuen Konzepte ist das sogenannte “Boomerang Casino”, das sich durch einige besondere Features von herkГ¶mmlichen Online-Casinos unterscheidet.
Das Boomerang Casino zeichnet sich vor allem durch sein einzigartiges Belohnungssystem aus, das auf dem Prinzip des australischen Wurfgeräts, dem Boomerang, basiert. Ähnlich wie ein Boomerang, das nach dem Wurf zu seinem Ursprungsort zurückkehrt, erhalten die Spieler im Boomerang Casino regelmäßige Belohnungen und Boni, die sie immer wieder zum Spielen zurückbringen.
Ein weiteres Highlight des Boomerang Casinos ist das VIP-Programm, das auf die individuellen Bedürfnisse und Vorlieben der Spieler zugeschnitten ist. Je mehr ein Spieler im Casino spielt, desto höher steigt er im VIP-Programm auf und kann so von exklusiven Angeboten und Vorteilen profitieren.
DarГјber hinaus bietet das Boomerang Casino eine Vielzahl von spannenden Spielen aus den Bereichen Slots, Tischspiele und Live-Casino an, die fГјr Abwechslung und SpaГџ sorgen. Die Spiele werden von renommierten Softwareanbietern entwickelt und garantieren ein sicheres und faires Spielerlebnis.
Ein weiterer großer Vorteil des Boomerang Casinos ist die Möglichkeit, auch unterwegs von jedem Ort aus zu spielen. Die mobile Version der Plattform ist benutzerfreundlich gestaltet und ermöglicht es den Spielern, ihre Lieblingsspiele auch auf dem Smartphone oder Tablet zu genießen.
Insgesamt bietet das Boomerang Casino eine innovative und spannende Alternative zu herkömmlichen Online-Casinos und überzeugt mit seinem einzigartigen Belohnungssystem, dem maßgeschneiderten VIP-Programm und der großen Auswahl an Spielen. Wer also auf der Suche nach einem neuen und aufregenden Spielerlebnis ist, sollte das Boomerang Casino unbedingt ausprobieren.
https://boomerangcasino.one/
canada drugs no prescription: canada drugs without prescription – prescription drugs canada
Tipico Casino Auszahlen lassen
Das Tipico Casino bietet seinen Kunden eine Vielzahl von Möglichkeiten, um Gewinne auszahlen zu lassen. Dabei ist es wichtig zu beachten, dass es einige Bedingungen gibt, die erfüllt werden müssen, um eine erfolgreiche Auszahlung durchführen zu können.
Zunächst einmal muss der Kunde sich vergewissern, dass er alle Bonusbedingungen erfüllt hat, bevor eine Auszahlung beantragt werden kann. In vielen Fällen gibt es Umsatzbedingungen, die erfüllt werden müssen, bevor das Bonusguthaben in Echtgeld umgewandelt werden kann.
Nachdem alle Bedingungen erfüllt wurden, kann der Kunde eine Auszahlung beantragen. Dazu muss er sich einfach in sein Konto einloggen und den entsprechenden Bereich für Auszahlungen aufrufen. Dort kann er den Betrag auswählen, den er auszahlen lassen möchte, und die gewünschte Zahlungsmethode angeben.
Es ist wichtig zu beachten, dass Tipico Casino verschiedene Zahlungsmethoden anbietet, darunter Kreditkarten, BankГјberweisungen und E-Wallets. Jede Zahlungsmethode hat ihre eigenen Bearbeitungszeiten und GebГјhren, die der Kunde berГјcksichtigen sollte.
Sobald die Auszahlung beantragt wurde, wird sie vom Tipico Casino überprüft und innerhalb weniger Tage bearbeitet. In einigen Fällen kann es jedoch länger dauern, insbesondere wenn zusätzliche Dokumente für die Verifizierung des Kontos angefordert werden.
Insgesamt bietet das Tipico Casino eine zuverlässige und sichere Möglichkeit, um Gewinne auszahlen zu lassen. Durch die Einhaltung der allgemeinen Geschäftsbedingungen und der Bonusbedingungen können Kunden sicherstellen, dass ihre Auszahlungen schnell und ohne Probleme abgewickelt werden.
https://tipicocasino.one/
https://pharmacynoprescription.pro/# buy medications without prescriptions
Promo Code Zet Casino: Profitieren Sie jetzt von tollen Rabatten
Zet Casino ist eines der beliebtesten Online-Casinos im deutschen Raum und überzeugt seine Kunden nicht nur mit einer großen Auswahl an Spielen, sondern auch mit attraktiven Bonusangeboten. Eine besonders begehrte Möglichkeit, von zusätzlichen Vergünstigungen zu profitieren, ist die Verwendung eines Promo Codes.
Ein Promo Code ist ein spezieller Code, den Sie bei der Registrierung auf der Website von Zet Casino eingeben können, um von verschiedenen Aktionen zu profitieren. Dies kann beispielsweise ein zusätzliches Startguthaben, Freispiele oder Cashback-Angebote sein. Mit einem Promo Code können Sie also Ihr Spielerlebnis bei Zet Casino noch spannender gestalten und gleichzeitig Ihr Guthaben aufbessern.
Um einen Promo Code bei Zet Casino einzulösen, müssen Sie sich einfach auf der Website anmelden und den Code im entsprechenden Feld angeben. Die genauen Bedingungen und Vorteile des Codes können je nach Aktion variieren, daher sollten Sie sich vorher über die aktuell gültigen Promo Codes informieren.
Ein guter Tipp ist es, regelmäßig die Website von Zet Casino zu besuchen oder den Newsletter zu abonnieren, um über aktuelle Aktionen informiert zu bleiben. So verpassen Sie garantiert keinen lukrativen Promo Code und können Ihr Spielerlebnis bei Zet Casino optimal ausnutzen.
Nutzen Sie also jetzt die Möglichkeit, mit einem Promo Code bei Zet Casino von tollen Rabatten und Vergünstigungen zu profitieren und erleben Sie spannende Stunden voller Spaß und Adrenalin. Viel Glück beim Spielen!
https://zetcasino.one/
https://indianpharm.shop/# mail order pharmacy india
reputable indian online pharmacy: top 10 online pharmacy in india – reputable indian online pharmacy
Zet Casino Auszahlung
Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und groГџzГјgigen Boni anbietet. Ein wichtiger Aspekt fГјr jeden Spieler ist die Auszahlung von Gewinnen. In diesem Artikel werden wir uns genauer mit der Zet Casino Auszahlung befassen.
Zet Casino bietet eine Vielzahl von Zahlungsmethoden für die Auszahlung von Gewinnen an. Zu den gängigen Optionen gehören Kreditkarten, E-Wallets wie Skrill und Neteller, sowie Banküberweisungen. Die Auszahlungsdauer hängt von der gewählten Zahlungsmethode ab. E-Wallets bieten in der Regel die schnellsten Auszahlungen, während Banküberweisungen etwas länger dauern können.
Um eine Auszahlung bei Zet Casino zu tätigen, müssen Spieler zunächst ihr Konto verifizieren. Dazu müssen sie eine Kopie ihres Personalausweises oder Reisepasses sowie einen Adressnachweis einreichen. Dies dient der Sicherheit der Spieler und der Einhaltung der gesetzlichen Vorschriften.
Es ist wichtig zu beachten, dass Zet Casino Auszahlungen in der Regel innerhalb von 24 Stunden bearbeitet werden. Allerdings kann es je nach Zahlungsmethode einige Tage dauern, bis das Geld auf dem Konto des Spielers gutgeschrieben wird.
Insgesamt ist die Zet Casino Auszahlung zuverlässig und sicher. Spieler können sich darauf verlassen, dass ihre Gewinne schnell und unkompliziert ausgezahlt werden. Wenn Sie also auf der Suche nach einem zuverlässigen Online-Casino mit schnellen Auszahlungen sind, ist Zet Casino eine gute Wahl.
https://zetcasino.one/
online pharmacy india online pharmacy india india online pharmacy
buying from online mexican pharmacy: best online pharmacies in mexico – buying prescription drugs in mexico online
Вам срочно нужны денежные средства? Мы готовы оказать своевременную и оперативную помощь в трудную минуту, расскажем, как получить онлайн займ и что он из себя представляет. Гарантируем индивидуальный подход и гибкие условия к каждому клиенту. Ищете онлайн кредит наличными без справок? Newloans.ru – сайт, которым очень удобно пользоваться. Здесь представлена только полезная информация. Больше не нужно просить взаймы у знакомых и близких, с нашей помощью вы сможете реализовать свои задумки. Достаточно оформить заявку, дождаться решения и получить денежные средства.
Tipico Geld Гјbertragen auf Casino
Das Online-Casino Tipico bietet seinen Nutzern eine Vielzahl von Möglichkeiten, um Geld auf ihr Spielerkonto zu transferieren. Vor allem für Neulinge kann es jedoch verwirrend sein, welche Optionen zur Verfügung stehen und welche die sicherste und schnellste ist. Daher haben wir für euch eine kleine Anleitung zum Geldtransfer bei Tipico zusammengestellt.
Eine der einfachsten Methoden, um Geld auf sein Tipico Casino Konto zu übertragen, ist die Verwendung von Kredit- oder Debitkarten. Hierfür einfach die Zahlungsmethode auswählen, den gewünschten Betrag eingeben und die Transaktion bestätigen. Dieser Vorgang ist in der Regel innerhalb von Minuten abgeschlossen und das Geld steht sofort zum Spielen bereit.
Eine weitere beliebte Option ist die Verwendung von E-Wallets wie PayPal oder Skrill. Auch diese Methode ist sehr sicher und schnell, da die Transaktion in Echtzeit erfolgt. Zudem bieten viele E-Wallets zusätzliche Sicherheitsmaßnahmen wie Zwei-Faktor-Authentifizierung oder Verschlüsselung der Daten.
Wer lieber anonym bleiben möchte, kann auch die Prepaid-Karte Paysafecard nutzen. Diese kann an vielen Verkaufsstellen erworben und dann einfach durch Eingabe des Codes auf der Webseite von Tipico eingelöst werden. Auch hier ist das Geld innerhalb von Minuten verfügbar.
Zu guter Letzt bietet Tipico auch die Möglichkeit, per Banküberweisung Geld auf das Spielerkonto zu transferieren. Diese Methode ist jedoch mit einer längeren Bearbeitungszeit verbunden, da die Banken in der Regel 1-3 Werktage benötigen, um den Betrag zu überweisen.
Egal für welche Methode man sich entscheidet, bei Tipico steht die Sicherheit der Transaktionen an oberster Stelle. Die Webseite ist mit modernsten Sicherheitsmaßnahmen ausgestattet, um die sensiblen Daten der Nutzer zu schützen. Zudem arbeitet Tipico nur mit seriösen Zahlungsdienstleistern zusammen, um eine sichere und zuverlässige Abwicklung der Transaktionen zu gewährleisten.
Insgesamt bietet Tipico also eine Vielzahl von sicheren und schnellen Möglichkeiten, um Geld auf das Casino Konto zu übertragen. Egal ob per Kreditkarte, E-Wallet, Paysafecard oder Banküberweisung, für jeden ist die passende Option dabei. Also worauf wartet ihr noch? Holt euch euren Willkommensbonus und legt los mit dem Spielspaß bei Tipico!
https://tipicocasino.one/
Zet Casino Bonuscode
Das Zet Casino ist eine beliebte Online-Glücksspielseite, die eine Vielzahl von Spielen und lukrativen Boni anbietet. Ein Bonuscode ist eine großartige Möglichkeit, um zusätzliches Geld oder Freispiele zu erhalten, um Ihre Gewinnchancen zu maximieren und Ihr Spielerlebnis zu verbessern.
Um den Zet Casino Bonuscode zu nutzen, müssen Sie sich zunächst auf der Website des Casinos registrieren. Sobald Sie Ihr Konto erstellt haben, können Sie den Bonuscode eingeben, um Ihren Bonus zu aktivieren. Dies kann in Form von zusätzlichem Geld auf Ihr Konto oder Freispielen für ausgewählte Spiele erfolgen.
Die Verwendung eines Bonuscodes kann Ihnen dabei helfen, Ihre Gewinne zu steigern und mehr Spaß beim Spielen zu haben. Es ist jedoch wichtig, die Bedingungen und Konditionen des Bonuscodes zu lesen, da diese je nach Angebot variieren können. Einige Bonuscodes haben möglicherweise spezifische Anforderungen, die erfüllt werden müssen, bevor Gewinne ausgezahlt werden können.
Zet Casino bietet regelmäßig neue Bonuscodes und Aktionen an, um seinen Spielern ein aufregendes und lohnendes Spielerlebnis zu bieten. Es lohnt sich also, regelmäßig auf der Website nach neuen Angeboten zu suchen und den Bonuscode zu nutzen, um Ihre Gewinne zu maximieren.
Zusammenfassend ist der Zet Casino Bonuscode eine großartige Möglichkeit, um zusätzliches Geld oder Freispiele zu erhalten und Ihre Gewinnchancen zu steigern. Wenn Sie auf der Suche nach einem aufregenden Online-Casino-Erlebnis sind, sollten Sie sich die Angebote von Zet Casino nicht entgehen lassen. Viel Glück und viel Spaß beim Spielen!
https://zetcasino.one/
buy generic retrovir for sale – buy glucophage 1000mg allopurinol 100mg sale
https://indianpharm.shop/# top online pharmacy india
online medicine without prescription: how to get prescription drugs from canada – how to buy prescriptions from canada safely
retrovir price – order irbesartan without prescription zyloprim tablet
Tipico Casino bietet seinen Kunden eine Vielzahl von Möglichkeiten, um Geld einzuzahlen. Diese müssen jedoch bestimmte Bedingungen erfüllen, um sicherzustellen, dass Transaktionen sicher und zuverlässig vonstattengehen. In diesem Artikel werden wir erklären, wie Sie Geld bei Tipico Casino einzahlen können.
ZunГ¤chst einmal mГјssen Sie sich in Ihr Tipico Casino Konto einloggen. Wenn Sie noch kein Konto haben, kГ¶nnen Sie eines erstellen, indem Sie sich auf der offiziellen Website von Tipico anmelden. Sobald Sie eingeloggt sind, navigieren Sie zur Kasse und wГ¤hlen Sie die Option “Einzahlen”.
Tipico Casino akzeptiert eine Vielzahl von Zahlungsmethoden, darunter Kredit- und Debitkarten, Banküberweisungen, E-Wallets wie PayPal, Skrill und Neteller sowie Paysafecard. Wählen Sie die gewünschte Zahlungsmethode aus und geben Sie den Betrag ein, den Sie einzahlen möchten.
Bevor Sie die Transaktion bestätigen, stellen Sie sicher, dass Sie die Bonusbedingungen von Tipico Casino gelesen haben. Manchmal bieten sie Boni für Einzahlungen an, die bestimmte Umsatzbedingungen erfüllen müssen, damit Sie sich Gewinne auszahlen lassen können.
Sobald Sie die Einzahlung bestätigt haben, wird das Geld sofort auf Ihr Tipico Casino Konto gutgeschrieben und Sie können sofort mit dem Spielen beginnen. Wenn Sie weitere Fragen zur Einzahlung haben, können Sie den Kundensupport von Tipico Casino kontaktieren, der Ihnen rund um die Uhr zur Verfügung steht.
Insgesamt bietet Tipico Casino eine einfache und sichere Möglichkeit, Geld einzuzahlen, damit Sie Ihr Spielerlebnis voll genießen können. Achten Sie darauf, verantwortungsbewusst zu spielen und setzen Sie sich Limits, um ein problematisches Spielverhalten zu vermeiden. Viel Spaß und viel Glück beim Spielen im Tipico Casino!
https://tipicocasino.one/
Das Zet Casino ist eine beliebte Online-GlГјcksspielplattform, die eine Vielzahl von Spielen fГјr Spieler aller Art bietet. Um neue Spieler anzulocken und bestehende Kunden zu belohnen, bietet das Zet Casino regelmäßig Promotionscodes an, wie den “zet casino kod promocyjny”.
Ein Promotionscode ist ein spezieller Code, den Spieler eingeben kГ¶nnen, um verschiedene Boni und Belohnungen zu erhalten. Der “zet casino kod promocyjny” ermГ¶glicht es den Spielern, zusГ¤tzliches Geld zum Spielen zu erhalten, Freispiele zu gewinnen oder andere attraktive Angebote zu nutzen.
Um den “zet casino kod promocyjny” zu erhalten, mГјssen die Spieler normalerweise an bestimmten Aktionen teilnehmen, wie zum Beispiel an speziellen Turnieren, Einzahlungsaktionen oder einfach durch das regelmäßige Spielen im Casino. Die Codes kГ¶nnen dann auf der Webseite des Zet Casinos eingegeben werden, um die entsprechenden Belohnungen zu erhalten.
Es ist wichtig zu beachten, dass Promotionscodes oft mit bestimmten Bedingungen verbunden sind, wie zum Beispiel Umsatzanforderungen oder zeitlichen Begrenzungen. Spieler sollten daher immer die genauen Bedingungen fГјr den “zet casino kod promocyjny” lesen, um sicherzustellen, dass sie die Belohnungen erhalten kГ¶nnen.
Insgesamt sind Promotionscodes eine tolle MГ¶glichkeit fГјr Spieler, zusГ¤tzliche Belohnungen im Zet Casino zu erhalten und ihr Spielerlebnis zu verbessern. Wenn Sie also auf der Suche nach zusГ¤tzlichen Boni und Freispielen sind, sollten Sie unbedingt nach dem aktuellen “zet casino kod promocyjny” suchen und ihn bei Ihrer nГ¤chsten Einzahlung verwenden. Viel SpaГџ und viel GlГјck beim Spielen im Zet Casino!
https://zetcasino.one/
celebrex antidepressant
Tipico im Casino: Ein gutes Zeichen fГјr Sportwettenfans
Sportwetten sind schon längst kein Nischenthema mehr, sondern erfreuen sich einer immer größeren Beliebtheit. Vor allem in Deutschland boomt der Markt für Sportwetten und entsprechende Anbieter sind in den letzten Jahren wie Pilze aus dem Boden geschossen. Einer dieser Anbieter ist Tipico, der vor allem durch sein Online-Angebot bekannt ist. Doch wussten Sie schon, dass Tipico auch in einigen Casinos vertreten ist?
Das Aufeinandertreffen von Tipico und Casinos mag zunächst ungewöhnlich erscheinen, aber es ergibt durchaus Sinn. Denn Sportwetten und Glücksspiele haben einige Gemeinsamkeiten und es profitieren beide Seiten von einer Kooperation. Besonders für Sportwettenfans bietet die Präsenz von Tipico im Casino viele Vorteile. So können sie ihre Wetten bequem vor Ort platzieren und gleichzeitig das Casino-Flair genießen.
Darüber hinaus bietet Tipico im Casino auch eine Vielzahl von zusätzlichen Services an. So können Kunden beispielsweise auch auf Live-Sportevents wetten oder von attraktiven Bonusaktionen profitieren. Für viele Sportwettenfans ist das ein echtes Highlight und eine willkommene Abwechslung zum reinen Online-Angebot.
Auch im Hinblick auf den Spielerschutz ist die Kooperation von Tipico und Casinos von Vorteil. Denn durch die gemeinsame Präsenz können sich Spieler besser über ihre Limits bewusst werden und gegebenenfalls auch Hilfe bei Problemen in Anspruch nehmen. Die Verbindung von Sportwetten und Glücksspielen schafft somit auch eine Win-win-Situation für alle Beteiligten.
Insgesamt bietet die Präsenz von Tipico im Casino eine spannende Möglichkeit für Sportwettenfans, ihre Leidenschaft für Sport und Wetten mit dem aufregenden Ambiente eines Casinos zu kombinieren. Durch die vielfältigen Services und Angebote wird das Spielerlebnis noch besser und abwechslungsreicher. Wenn Sie also ein Sportwettenfan sind und sich bisher noch nicht ins Casino getraut haben, sollten Sie Tipico definitiv eine Chance geben. Wer weiß, vielleicht entdecken Sie ja eine neue Leidenschaft für sich.
https://tipicocasino.one/
Der Boomerang Casino Code ist ein neues Feature, das von dem beliebten Online-Casino eingeführt wurde, um Spielern zusätzliche Boni und Belohnungen zu bieten. Durch die Eingabe des Codes während des Registrierungsprozesses oder im Kassenbereich können Spieler Zugang zu exklusiven Angeboten erhalten.
Der Boomerang Casino Code kann verschiedene Arten von Belohnungen beinhalten, wie zum Beispiel Bonusguthaben, Freispiele oder Cashback-Angebote. Diese Boni sind eine großartige Möglichkeit, um das Spielerlebnis zu verbessern und die Gewinnchancen zu erhöhen.
Um den Boomerang Casino Code zu nutzen, müssen Spieler zunächst ein Konto bei dem Online-Casino erstellen. Anschließend können sie den Code eingeben, um die Belohnungen zu erhalten. Es ist wichtig zu beachten, dass jeder Code bestimmte Bedingungen und Anforderungen haben kann, die erfüllt werden müssen, um die Belohnungen zu erhalten.
Der Boomerang Casino Code ist eine aufregende Möglichkeit, um das Spielerlebnis zu verbessern und zusätzliche Belohnungen zu erhalten. Spieler sollten regelmäßig nach neuen Codes Ausschau halten, um sicherzustellen, dass sie keine der exklusiven Angebote verpassen.
Insgesamt ist der Boomerang Casino Code eine großartige Möglichkeit, um das Spielerlebnis im Online-Casino zu verbessern und zusätzliche Belohnungen zu erhalten. Spieler sollten die Codes nutzen, um das Beste aus ihrem Spiel herauszuholen.
https://boomerangcasino.one/
mexican drugstore online: mexican mail order pharmacies – medication from mexico pharmacy
baclofen for opiate withdrawals
best canadian pharmacy online: canadian family pharmacy – northwest pharmacy canada
https://canadianpharm.guru/# canada pharmacy 24h
Tipico Casino Einzahlungsmöglichkeiten
In einem Online Casino wie Tipico stehen den Spielern verschiedene Einzahlungsmöglichkeiten zur Verfügung. Diese bieten eine schnelle und einfache Art, um Geld auf das Spielkonto zu überweisen und können je nach persönlichen Vorlieben ausgewählt werden.
Eine der beliebtesten Einzahlungsmethoden ist die Banküberweisung. Dabei wird das Geld direkt vom Bankkonto des Spielers auf das Casino-Konto überwiesen. Diese Methode ist sicher und zuverlässig, kann jedoch einige Tage dauern, bis das Geld auf dem Spielkonto gutgeschrieben wird.
Eine weitere häufig genutzte Einzahlungsmöglichkeit ist die Nutzung von Kredit- oder Debitkarten. Viele Spieler bevorzugen diese Methode aufgrund ihrer Einfachheit und Schnelligkeit. Die meisten Online Casinos akzeptieren Karten wie Visa oder Mastercard.
E-Wallets wie PayPal, Skrill oder Neteller sind ebenfalls beliebte Einzahlungsmethoden. Diese ermöglichen es den Spielern, Geld schnell und sicher auf ihr Spielkonto zu überweisen. E-Wallets bieten auch den Vorteil, dass keine sensiblen Bankdaten preisgegeben werden müssen.
Zusätzlich zu diesen gängigen Einzahlungsmöglichkeiten bietet Tipico auch die Möglichkeit, mit Prepaid-Karten wie paysafecard einzuzahlen. Diese können im Supermarkt oder an Tankstellen erworben und anschließend für Einzahlungen im Online Casino verwendet werden.
Es ist wichtig, die jeweiligen Gebühren und Limits für die verschiedenen Einzahlungsmethoden zu beachten. Einige Methoden können Gebühren verursachen oder bestimmte Mindest- und Höchstbeträge haben.
Insgesamt bietet Tipico seinen Spielern eine Vielzahl von Einzahlungsmöglichkeiten, um das Spielerlebnis so bequem wie möglich zu gestalten. Spieler können die Methode auswählen, die am besten zu ihren Bedürfnissen passt und sicher sein, dass ihre Einzahlungen sicher und geschützt sind.
https://tipicocasino.one/
Willkommen im Zet Casino und sichern Sie sich den großzügigen Willkommensbonus! Das Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und aufregenden Bonusangeboten für seine Spieler bereithält. Einer der attraktivsten Aspekte des Zet Casinos ist der lukrative Willkommensbonus, den neue Spieler bei ihrer ersten Einzahlung erhalten können.
Der Zet Casino Willkommensbonus belohnt neue Spieler mit einem großzügigen Bonusguthaben und Freispielen für ausgewählte Spiele. Um von diesem Bonusangebot zu profitieren, müssen neue Spieler lediglich ein Konto im Zet Casino erstellen und eine erste Einzahlung tätigen. Der Willkommensbonus wird dann automatisch auf das Spielerkonto gutgeschrieben.
Das Bonusguthaben kann für eine Vielzahl von Spielen im Zet Casino verwendet werden, darunter Spielautomaten, Tischspiele und Live-Casino-Spiele. Die Freispiele, die im Rahmen des Willkommensbonus angeboten werden, können auf ausgewählten Spielautomaten gespielt werden und bieten die Chance, zusätzliche Gewinne zu erzielen.
Es ist wichtig zu beachten, dass der Zet Casino Willkommensbonus bestimmten Umsatzbedingungen unterliegt, die erfüllt werden müssen, bevor Gewinne aus dem Bonusguthaben ausgezahlt werden können. Diese Umsatzbedingungen variieren je nach Angebot und sind auf der Website des Zet Casinos ausführlich beschrieben.
Wenn Sie also auf der Suche nach einem erstklassigen Online-Casino mit lukrativen Bonusangeboten sind, ist das Zet Casino definitiv einen Besuch wert. Nutzen Sie den Willkommensbonus, um Ihr Spielerlebnis zu maximieren und spannende Spiele zu genieГџen. Viel SpaГџ und viel GlГјck im Zet Casino!
https://zetcasino.one/
Pro Studio поможет вам воплотить амбициозные проекты в реальность. Работая с нами, получите идеальных партнеров в достижении ваших целей. Для различных бизнесов, мы специализируемся на создании качественных сайтов. Стараемся учитывать пожелания и требования наших клиентов. Требуется создание сайтов цена? Iv-SEO.ru – здесь у вас есть возможность ознакомиться с услугами и узнать всю информацию о нашем digital-агентстве. Работаем в Москве и в других регионах РФ. Свяжитесь с нами, чтобы узнать детальнее об условиях сотрудничества.
top online pharmacy india: legitimate online pharmacies india – indian pharmacy paypal
Das Tipico Casino ist eine beliebte Plattform fГјr GlГјcksspiele und Unterhaltung im Internet. Egal ob Slots, Tischspiele oder Live-Casino, hier kommen Casino-Fans auf ihre Kosten. Doch was passiert, wenn man plГ¶tzlich die Meldung “Sie haben nicht genГјgend Guthaben” erhГ¤lt?
Diese Situation kann für viele Spieler frustrierend sein. Man hat sich gerade in einen guten Spielrhythmus eingefunden und schon ist das Guthaben aufgebraucht. Doch keine Sorge, es gibt verschiedene Möglichkeiten, um das Guthaben aufzuladen und das Spiel fortzusetzen.
Eine einfache Möglichkeit ist es, eine Einzahlung auf das Casino-Konto vorzunehmen. Hierfür stehen meist verschiedene Zahlungsmethoden wie Kreditkarte, Banküberweisung oder E-Wallets zur Verfügung. Nach einer erfolgreichen Einzahlung kann das Spiel direkt fortgesetzt werden.
Eine weitere Option ist es, eventuelle Boni oder Freispiele zu nutzen. Viele Online-Casinos bieten regelmäßig Promotionen an, bei denen Spieler zusätzliches Guthaben erhalten. Diese können dann genutzt werden, um weiterhin Spaß an den Spielen zu haben.
Zudem ist es wichtig, verantwortungsbewusst mit dem eigenen Guthaben umzugehen. Setzen Sie sich vor dem Spiel eine Grenze fest, die Sie bereit sind zu verlieren. So können Sie sicherstellen, dass das Spielen im Casino immer eine unterhaltsame Erfahrung bleibt.
Insgesamt ist es also wichtig, bei der Meldung “Sie haben nicht genГјgend Guthaben” ruhig zu bleiben und die zur VerfГјgung stehenden Optionen zu nutzen, um das Spiel fortzusetzen. Mit etwas GlГјck und Geschick stehen die Chancen gut, bald wieder im Spiel zu sein und tolle Gewinne zu erzielen. Viel SpaГџ und Erfolg im Tipico Casino!
https://tipicocasino.one/
how does augmentin work
Das Tipico Online Casino bietet seinen Spielern ab sofort die MГ¶glichkeit, jederzeit und Гјberall auf ihre Lieblingsspiele zuzugreifen – dank der neuen Tipico Online Casino App. Die App ist fГјr sowohl iOS- als auch Android-GerГ¤te verfГјgbar und ermГ¶glicht ein unkompliziertes und unterhaltsames Spielerlebnis direkt auf dem Smartphone oder Tablet.
Mit der Tipico Online Casino App haben Spieler die Möglichkeit, eine Vielzahl von Casino-Spielen zu genießen, darunter Slot-Spiele, Tischspiele wie Roulette und Blackjack, sowie spannende Live-Casino Spiele. Die App bietet eine moderne und benutzerfreundliche Oberfläche, die es einfach macht, zwischen verschiedenen Spielen zu navigieren und das Spiel zu genießen.
Neben der Vielfalt an Spielen bietet die App auch zahlreiche Vorteile für die Spieler. So können sie beispielsweise einfach und sicher Ein- und Auszahlungen tätigen, sowie von verschiedenen Bonusangeboten und Aktionen profitieren. Darüber hinaus bietet die App einen 24/7 Kundenservice, der Spieler bei Fragen oder Problemen unterstützt.
Insgesamt ist die Tipico Online Casino App eine großartige Ergänzung für alle Casino-Liebhaber, die auch unterwegs nicht auf ihr Spielerlebnis verzichten möchten. Mit einer breiten Auswahl an Spielen, einfachen Ein- und Auszahlungsmöglichkeiten und einem erstklassigen Kundenservice bietet die App alles, was das Spielerherz begehrt. Laden Sie die App noch heute herunter und tauchen Sie ein in die aufregende Welt des Tipico Online Casinos. Viel Spaß und viel Glück!
https://tipicocasino.one/
http://aviatoroyna.bid/# aviator sinyal hilesi ücretsiz
https://slotsiteleri.guru/# yeni slot siteleri
aviator oyunu 20 tl: aviator bahis – aviator oyna 20 tl
pin-up online: pin up casino – pin-up casino
clozapine drug – order generic amaryl 4mg famotidine usa
Geld Tipico Casino blockiert
Es ist ärgerlich, wenn man im Online Casino sein Geld nicht auszahlen lassen kann. Immer wieder berichten Spieler von Problemen mit der Auszahlung beim Tipico Casino. Das Unternehmen, das seit Jahren in der Branche tätig ist und eine Vielzahl von Spielen anbietet, scheint mit dieser Problematik zu kämpfen.
Die Gründe dafür können vielfältig sein. Oftmals liegen die Probleme bei den Spielern selbst, sei es durch falsche Angaben bei der Registrierung oder durch nicht erfüllte Bonusbedingungen. In manchen Fällen kann es aber auch am Casino selbst liegen, wenn zum Beispiel technische Probleme auftreten oder die Auszahlung nicht bearbeitet wird.
Es ist wichtig, dass Spieler sich an den Kundenservice von Tipico wenden, wenn sie Probleme mit der Auszahlung haben. Oftmals kann eine schnelle Klärung des Problems erfolgen, wenn man direkt Kontakt aufnimmt. Sollte das nicht helfen, gibt es auch die Möglichkeit, sich an Aufsichtsbehörden oder Organisationen zum Spielerschutz zu wenden.
Es ist zudem ratsam, vorab genau zu prüfen, ob das Tipico Casino über eine gültige Lizenz verfügt und seriös agiert. Nur so kann man sicher sein, dass es sich um ein vertrauenswürdiges Online Casino handelt.
Insgesamt ist es wichtig, als Spieler aufmerksam zu sein und bei Problemen nicht zu lange zu warten, sondern aktiv nach Lösungen zu suchen. Nur so kann man sicherstellen, dass man sein Geld auch wirklich erhält und den Spaß am Spiel nicht verliert.
https://tipicocasino.one/
https://pinupgiris.fun/# pin-up casino indir
Интернет-магазин ТопКлиматДВ, специализируется на климатическом оборудовании. Поставки выполняем в любой регион России. Предлагаем высокое качество обслуживания, доступные цены и предоставляем длительную гарантию на все позиции. Ищете где купить кондиционер с установкой? Топклиматдв.рф – сайт, где можно найти то, что необходимо для создания неповторимой атмосферы в вашем доме. Можете сами выбрать удобный способ оплаты и доставки. Если желаете заказать современную модель климатического оборудования с возможностью монтажа «под ключ», то вы обратились по адресу!
Zet Casino ist ein beliebtes Online-Casino, das seinen Spielern eine Vielzahl von Spielen und Funktionen bietet. Eines der wichtigsten Themen fГјr die Spieler ist die Auszahlung ihrer Gewinne, auch bekannt als “zet casino kotiutus”.
Die Auszahlung bei Zet Casino ist einfach und unkompliziert. Um eine Auszahlung zu beantragen, müssen die Spieler zunächst ihr Konto verifizieren, indem sie ihre Identität nachweisen und sicherstellen, dass sie die Bedingungen des Casinos erfüllen. Dies ist ein Standardverfahren, das dazu dient, Betrug und Geldwäsche zu verhindern.
Sobald das Konto verifiziert ist, können die Spieler eine Auszahlung beantragen. Zet Casino bietet verschiedene Zahlungsmethoden an, darunter E-Wallets, Kreditkarten und Banküberweisungen. Die Spieler können die für sie am besten geeignete Methode auswählen und den Betrag angeben, den sie auszahlen möchten.
Die Auszahlungszeit bei Zet Casino variiert je nach gewählter Zahlungsmethode. E-Wallets bieten in der Regel die schnellsten Auszahlungen, während Banküberweisungen etwas länger dauern können. Das Casino bemüht sich jedoch, die Auszahlungen so schnell wie möglich zu bearbeiten, damit die Spieler ihre Gewinne schnell erhalten.
Insgesamt ist die Auszahlung bei Zet Casino ein einfacher Vorgang, der den Spielern ermöglicht, ihre Gewinne problemlos zu erhalten. Mit einer Vielzahl von Zahlungsmethoden und schnellen Bearbeitungszeiten ist Zet Casino eine gute Wahl für Spieler, die nach einem zuverlässigen und benutzerfreundlichen Online-Casino suchen.
https://zetcasino.one/
QIWI wallet balance not adding up?
Let us handle the stress in getting back what isrightfully yours.
Contact us today and begin reclaiming your funds.
pin up indir: pin up casino guncel giris – pin up
Tipico ist einer der bekanntesten Anbieter von Sportwetten und Online-Casino-Spielen in Deutschland. Das Unternehmen bietet seinen Kunden eine Vielzahl von Spielen, darunter auch eine mobile App fГјr das Tipico Casino.
Die Tipico Casino mobile App ermГ¶glicht es den Nutzern, ihre Lieblingsspiele auch unterwegs zu spielen. Egal ob man auf dem Weg zur Arbeit ist, im Park entspannen mГ¶chte oder einfach nur gemГјtlich auf der Couch liegt – die App bietet ein bequemes Spielerlebnis, das zu jeder Zeit und an jedem Ort genutzt werden kann.
Die mobile App von Tipico Casino ist benutzerfreundlich und einfach zu bedienen. Mit nur wenigen Klicks können die Kunden auf eine große Auswahl an Spielen zugreifen, darunter Slots, Roulette, Blackjack und vieles mehr. Ebenso können Ein- und Auszahlungen bequem über die App getätigt werden.
Ein weiterer Vorteil der Tipico Casino mobile App ist die hohe Sicherheit, die sie bietet. Alle persönlichen Daten und Zahlungsinformationen der Nutzer werden verschlüsselt übertragen, um einen sicheren Spielbetrieb zu gewährleisten.
Zusammenfassend lässt sich sagen, dass die Tipico Casino mobile App eine gute Möglichkeit bietet, um auch von unterwegs aus in die spannende Welt der Online-Casino-Spiele einzutauchen. Wer gerne sein Glück versucht und dabei flexibel bleiben möchte, sollte die App auf jeden Fall einmal ausprobieren.
https://tipicocasino.one/
http://pinupgiris.fun/# pin up bet
Der Casino Guru Zet ist bekannt für seine Expertise und Fähigkeiten im Glücksspielbereich. Als Experte für Online-Casinos bietet er umfassende Informationen zu den besten Casinos, Spielen und Boni.
Der Casino Guru Zet hat sich einen Ruf als vertrauenswürdige Quelle für Glücksspielbegeisterte auf der ganzen Welt erarbeitet. Seine Bewertungen und Empfehlungen sind bekannt für ihre Fairness und Neutralität, da er sich strikt an strenge Kriterien und Standards hält.
Mit seiner langjährigen Erfahrung und Fachkenntnis bietet der Casino Guru Zet Spielern nützliche Tipps und Tricks, um ihr Spielerlebnis zu optimieren und ihre Gewinnchancen zu erhöhen. Er ist auch bekannt für seine exklusiven Deals und Promotionen, die den Spielern zusätzliche Vorteile und Anreize bieten.
Der Casino Guru Zet ist eine unverzichtbare Ressource für alle, die ihr Glück im Online-Casino versuchen möchten. Seine fundierten Bewertungen und umfassenden Informationen helfen den Spielern, die besten Entscheidungen zu treffen und das Beste aus ihrem Glücksspiel-Erlebnis herauszuholen.
https://zetcasino.one/
http://gatesofolympus.auction/# gates of olympus oyna demo
buspirone vs bupropion
Boomerang Casino: 50 Freispiele ohne Einzahlung
Boomerang Casino ist eine aufregende Online-Spielplattform, die Spielern eine Vielzahl von Spielen und Boni bietet. Eine besonders attraktive Promotion, die derzeit angeboten wird, sind 50 Freispiele ohne Einzahlung fГјr neue Spieler.
Um von diesem großzügigen Angebot zu profitieren, müssen Spieler lediglich ein Konto bei Boomerang Casino erstellen. Sobald das Konto erfolgreich erstellt wurde, werden die 50 Freispiele automatisch gutgeschrieben. Spieler können diese Freispiele dann nutzen, um verschiedene Slot-Spiele auszuprobieren und echtes Geld zu gewinnen, ohne dabei ihr eigenes Geld riskieren zu müssen.
Diese Freispiele ohne Einzahlung sind eine hervorragende Möglichkeit für Spieler, die Welt von Boomerang Casino zu erkunden und gleichzeitig die Chance zu haben, echte Gewinne zu erzielen. Spieler können sich auf spannende Spielautomaten, große Jackpots und ein erstklassiges Spielerlebnis freuen.
Um die Freispiele zu erhalten, müssen Spieler lediglich den Bonus in ihrem Konto aktivieren und die Bedingungen für den Einsatz der Freispiele erfüllen. Dazu gehören in der Regel das Setzen eines Mindestbetrags und das Erfüllen von Umsatzanforderungen. Diese Bedingungen sind fair und transparent, so dass Spieler genau wissen, was von ihnen erwartet wird.
Wenn Sie also auf der Suche nach einem aufregenden Online-Casino-Erlebnis sind und gerne kostenlose Freispiele erhalten möchten, ist Boomerang Casino die richtige Wahl für Sie. Registrieren Sie sich noch heute und nutzen Sie die 50 Freispiele ohne Einzahlung, um Ihr Glück zu versuchen und tolle Gewinne zu erzielen. Viel Spaß und viel Erfolg!
https://boomerangcasino.one/
http://sweetbonanza.bid/# sweet bonanza demo türkçe
canl? slot siteleri: slot siteleri guvenilir – en yeni slot siteleri
Ищете трансерфинг зеланда? Посетите сайт Zelands.ru и Вы узнаете кто такой кто такой Вадим Зеланд и что такое трансерфинг. Трансерфинг зеланда уникальная технология достижения целей которая позволит вам управлять событиями, а зеланд является лучшим специалистом в этой области. Трансерфинг реальности Вадим Зеланд зайдите на сайт и узнайте больше.
Boomerang Casino Login
Das Boomerang Casino ist eine beliebte Online-Glücksspielseite, die eine Vielzahl von Spielen für Spieler weltweit anbietet. Um auf die Plattform zuzugreifen und zu spielen, müssen die Nutzer sich zuerst mit ihren persönlichen Kontoinformationen einloggen. In diesem Artikel werden wir uns genauer mit dem Login-Prozess im Boomerang Casino befassen.
Um sich im Boomerang Casino einzuloggen, müssen die Spieler zunächst die offizielle Website des Casinos besuchen. Dort finden sie den Login-Bereich, in den sie ihre E-Mail-Adresse und ihr Passwort eingeben müssen. Nachdem die Zugangsdaten verifiziert wurden, gelangen die Spieler auf ihre persönliche Spielerseite, auf der sie ihre Lieblingsspiele spielen können.
Es ist wichtig, dass die Spieler ihre Login-Daten sicher aufbewahren und sie nicht mit anderen teilen, um die Sicherheit ihres Kontos zu gewährleisten. Das Boomerang Casino bietet auch zusätzliche Sicherheitsmaßnahmen wie die Zwei-Faktor-Authentifizierung, um die Privatsphäre der Spieler zu schützen.
Nach dem erfolgreichen Login können die Spieler aus einer Vielzahl von Spielen wählen, darunter Slots, Tischspiele, Live-Dealer-Spiele und vieles mehr. Das Boomerang Casino bietet auch regelmäßige Bonusangebote und Aktionen, die den Spielern zusätzliche Chancen auf Gewinne bieten.
Insgesamt ist der Login-Prozess im Boomerang Casino einfach und sicher. Mit einer breiten Auswahl an Spielen und attraktiven Bonusangeboten ist das Casino eine gute Wahl fГјr Spieler, die nach einer unterhaltsamen und lohnenden GlГјcksspielerfahrung suchen. Besuchen Sie das Boomerang Casino noch heute und erleben Sie die Spannung des Online-GlГјcksspiels!
https://boomerangcasino.one/
pin-up online: pin-up online – pin-up casino giris
purchase clozapine online – buy generic accupril for sale pepcid ca
http://pinupgiris.fun/# pin-up casino indir
baclofen seizure
naproxen vs celebrex
FГјr GlГјcksspiel-Fans gibt es eine aufregende neue MГ¶glichkeit, ihr GlГјck zu versuchen – das Zet Casino bietet einen kostenlosen Bonus ohne Einzahlung an. Das bedeutet, dass Spieler die Chance haben, echtes Geld zu gewinnen, ohne ihr eigenes Geld riskieren zu mГјssen.
Um den Bonus zu erhalten, mГјssen Spieler lediglich ein Konto im Zet Casino erstellen und den Bonuscode bei der Registrierung eingeben. Der Bonus wird dann automatisch gutgeschrieben und kann fГјr eine Vielzahl von Spielen im Casino verwendet werden.
Mit dem kostenlosen Bonus können Spieler das Casino erkunden und verschiedene Spiele ausprobieren, ohne sich Gedanken über Verluste machen zu müssen. Es ist eine großartige Möglichkeit für neue Spieler, sich mit dem Casino vertraut zu machen und ihre Lieblingsspiele zu entdecken.
Es ist jedoch wichtig zu beachten, dass der Bonus bestimmten Umsatzbedingungen unterliegt, bevor er ausgezahlt werden kann. Spieler sollten daher die Bonusbedingungen sorgfältig lesen, um sicherzustellen, dass sie die Anforderungen erfüllen.
Insgesamt ist der Zet Casino Free Bonus ohne Einzahlung eine großartige Möglichkeit für Spieler, das Casino zu testen und echtes Geld zu gewinnen, ohne etwas zu riskieren. Es ist definitiv einen Versuch wert!
https://zetcasino.one/
bupropion lowest dose
sandyterrace.com
Li Zheng의 눈은 흥분의 눈물로 가득 차 있었고 그는 “황제 만세”라고 감사하며 절했습니다.
aviator bahis: aviator oyunu 20 tl – aviator oyunu 20 tl
https://pinupgiris.fun/# pin up casino indir
Das Boomerang Casino ist eine der neuesten Online-Spielplattformen, die derzeit in Deutschland verfГјgbar sind. Mit einer breiten Palette von Spielen und attraktiven Bonusangeboten hat das Casino bereits viele Spieler angezogen.
Das Boomerang Casino bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele und Live-Casino-Spiele. Damit ist fГјr jeden Geschmack etwas dabei und die Spieler kГ¶nnen sich stundenlang unterhalten lassen. Die Spiele werden von renommierten Softwareanbietern wie NetEnt, Microgaming und Play’n GO entwickelt, was fГјr QualitГ¤t und ein unvergessliches Spielerlebnis garantiert.
Neben einer großen Auswahl an Spielen bietet das Boomerang Casino auch großzügige Bonusangebote und Promotionen. Neue Spieler können von Willkommensboni profitieren, die Freispiele und Bonusgeld beinhalten. Auch Bestandskunden werden mit regelmäßigen Aktionen belohnt, die zusätzliche Gewinnchancen bieten.
Ein weiteres Highlight des Boomerang Casinos ist der Kundenservice. Die Spieler können sich jederzeit an das freundliche und professionelle Supportteam wenden, das bei Fragen oder Problemen weiterhilft. Die schnelle und zuverlässige Unterstützung sorgt für ein reibungsloses Spielerlebnis ohne unnötige Verzögerungen.
Alles in allem ist das Boomerang Casino eine ausgezeichnete Wahl fГјr Spieler in Deutschland, die auf der Suche nach einer unterhaltsamen und lohnenden Spielumgebung sind. Mit einer Vielzahl von Spielen, attraktiven Boni und einem erstklassigen Kundenservice ist das Casino definitiv einen Besuch wert.
https://boomerangcasino.one/
http://sweetbonanza.bid/# sweet bonanza yasal site
Um im Casino spielen zu können, benötigt man Geld auf seinem Spielerkonto. Eine Möglichkeit, Geld ins Casino zu transferieren, ist über den Buchmacher Tipico.
Tipico ist vor allem als Sportwettenanbieter bekannt, bietet aber auch die Möglichkeit, im Online Casino zu spielen. Um Geld von seinem Tipico-Konto ins Casino zu transferieren, muss man sich zunächst in sein Spielerkonto auf der Tipico-Website einloggen. Dort kann man unter dem Menüpunkt „Kasse“ die Option „Geld transferieren“ auswählen.
Man gibt den Betrag ein, den man ins Casino transferieren möchte, und bestätigt die Transaktion. Das Geld wird dann sofort auf das Casino-Konto überwiesen und man kann mit dem Spielen beginnen. Es ist wichtig zu beachten, dass man, um Geld ins Casino transferieren zu können, zuvor bereits eine Einzahlung auf sein Tipico-Konto getätigt haben muss.
Es gibt verschiedene Zahlungsmethoden, die bei Tipico fГјr Ein- und Auszahlungen zur VerfГјgung stehen, wie zum Beispiel Kreditkarte, PayPal, Skrill oder Neteller. Die Transaktionen sind in der Regel sicher und schnell, so dass man ohne lange Wartezeiten mit dem Spielen loslegen kann.
Das Transferieren von Geld von Tipico ins Casino ist bequem und unkompliziert und bietet Spielern die Möglichkeit, ihre Lieblingsspiele im Casino zu genießen. Wer also gerne im Casino spielt und sein Glück versuchen möchte, kann dies ganz einfach über Tipico tun.
https://tipicocasino.one/
https://sweetbonanza.bid/# sweet bonanza free spin demo
Visit the website predictor version 2.0 spaceman – to learn about the advantages of Predictor spaceman. Spaceman Predictor – increase your chances of winning in the exciting world of predictor spaceman version 2.0. You can download spaceman predictor online now. The entire review of the predictor version 2.0 spaceman application can be found on the website.
aviator nas?l oynan?r: aviator giris – aviator oyunu giris
celexa for ibs
Erfahrungen mit Zet Casino
Das Zet Casino ist eine beliebte Online-Glücksspielplattform, die eine Vielzahl von Spielen und Boni anbietet. Viele Spieler haben positive Erfahrungen mit dem Casino gemacht und loben vor allem die große Auswahl an Spielen und die benutzerfreundliche Oberfläche.
Ein groГџer Pluspunkt des Zet Casinos ist die breite Palette an Spielen, die es seinen Spielern bietet. Von klassischen Tischspielen wie Roulette und Blackjack bis hin zu modernen Spielautomaten und Live-Dealer-Spielen, das Casino hat fГјr jeden Geschmack etwas zu bieten. Die Spiele stammen von renommierten Software-Anbietern wie NetEnt, Microgaming und Play’n GO, was fГјr eine hohe QualitГ¤t und ein erstklassiges Spielerlebnis sorgt.
Ein weiterer Grund, warum Spieler das Zet Casino mögen, sind die großzügigen Bonusangebote. Neue Spieler erhalten oft einen Willkommensbonus, der ihnen zusätzliches Geld zum Spielen bietet. Darüber hinaus gibt es regelmäßig Aktionen und Turniere, bei denen Spieler noch mehr Belohnungen erhalten können.
Die Benutzerfreundlichkeit der Website wird auch von vielen Spielern geschätzt. Die Plattform ist leicht zu navigieren und bietet eine klare und übersichtliche Oberfläche. Spieler können problemlos zwischen den verschiedenen Spielen wechseln und finden schnell, wonach sie suchen.
Insgesamt sind die Erfahrungen mit dem Zet Casino größtenteils positiv. Die große Auswahl an Spielen, die großzügigen Boni und die benutzerfreundliche Website machen das Casino zu einer beliebten Wahl für Glücksspielfans. Wer also auf der Suche nach einem unterhaltsamen und sicheren Online-Casino ist, sollte das Zet Casino definitiv in Betracht ziehen.
https://zetcasino.one/
http://gatesofolympus.auction/# gates of olympus nasil para kazanilir
Tipico Casino ist eine der beliebtesten Online-Glücksspielplattformen in Deutschland. Neben einer großen Auswahl an Spielen und attraktiven Promotionen bietet das Casino auch die Möglichkeit, kostenlos Casino Chips zu erhalten.
Die Gratis-Chips sind eine tolle Möglichkeit, um die verschiedenen Spiele im Tipico Casino auszuprobieren, ohne eigenes Geld riskieren zu müssen. Diese Gratis-Chips können für eine Vielzahl von Spielen, wie Slots, Roulette, Blackjack und Poker, verwendet werden. Dadurch können Spieler das Casino erkunden und herausfinden, welche Spiele ihnen am besten gefallen, bevor sie echtes Geld einsetzen.
Es gibt verschiedene Möglichkeiten, um kostenlose Casino Chips im Tipico Casino zu erhalten. Zum einen bieten regelmäßige Promotionen und Aktionen die Möglichkeit, Gratis-Chips zu erhalten. Diese Promotionen können beispielsweise als Einzahlungsbonus oder als Teil eines Treueprogramms angeboten werden.
Eine weitere Möglichkeit, kostenlos Casino Chips zu erhalten, ist durch Gewinnspiele und Turniere im Casino. Spieler haben hier die Chance, durch ihre Teilnahme an verschiedenen Veranstaltungen Gratis-Chips zu gewinnen.
Es ist jedoch wichtig zu beachten, dass die kostenlosen Casino Chips bestimmten Bedingungen unterliegen, die erfüllt werden müssen, bevor man Gewinne auszahlen lassen kann. Es empfiehlt sich daher, die Bonusbedingungen sorgfältig zu lesen, um Missverständnisse zu vermeiden.
Insgesamt bieten die kostenlosen Casino Chips im Tipico Casino eine tolle Möglichkeit, um das Casino und die verschiedenen Spiele kennenzulernen, ohne eigenes Geld einzusetzen. Mit etwas Glück können Spieler so sogar echte Gewinne erzielen und den Spaß am Online-Glücksspiel voll auskosten.
https://tipicocasino.one/
sweet bonanza demo oyna: sweet bonanza taktik – sweet bonanza 100 tl
Tipico ElfmeterschieГџen Casino
Das Tipico Elfmeterschießen Casino ist eine innovative Glücksspielplattform, die Fußballfans und Casino-Liebhabern gleichermaßen ein spannendes Spielerlebnis bietet. Hier können die Spieler die Spannung eines Elfmeterschießens erleben, während sie auf ihre Lieblingsspiele wetten.
Das Konzept des Elfmeterschießens wurde geschickt in das Casino-Spiel integriert, um die Aufregung und den Nervenkitzel zu steigern. Die Spieler können aus einer Vielzahl von Wettoptionen wählen, um ihre Gewinnchancen zu maximieren. Ob Sie auf den Torschützen, den Torhüter oder das Endergebnis wetten möchten, im Tipico Elfmeterschießen Casino gibt es unzählige Möglichkeiten, Ihr Glück zu versuchen.
Darüber hinaus bietet das Casino eine Vielzahl von attraktiven Bonusangeboten und Aktionen, mit denen die Spieler ihre Gewinne steigern können. Von Willkommensboni über Freispiele bis hin zu Cashback-Angeboten gibt es für jeden Spieler etwas zu entdecken.
Die Plattform ist benutzerfreundlich gestaltet und bietet eine Vielzahl von sicheren Zahlungsmethoden, um eine reibungslose und zuverlässige Spielerfahrung zu gewährleisten. Darüber hinaus wird der Kundenservice des Casinos hoch geschätzt und steht den Spielern rund um die Uhr zur Verfügung, um bei Fragen oder Problemen zu helfen.
Insgesamt bietet das Tipico ElfmeterschieГџen Casino eine einzigartige und aufregende Spielerfahrung fГјr alle, die auf der Suche nach Nervenkitzel und Gewinnen sind. Probieren Sie es aus und erleben Sie die Faszination des ElfmeterschieГџens in einem ganz neuen Kontext. Viel GlГјck!
https://tipicocasino.one/
pin-up bonanza: aviator pin up – pin-up casino giris
http://aviatoroyna.bid/# aviator nasil oynanir
Вам в срочном порядке необходимы деньги? Мы готовы оказать своевременную и оперативную помощь в трудную минуту, расскажем, как получить онлайн займ и что он из себя представляет. Гарантируем индивидуальный подход и гибкие условия к каждому клиенту. Ищете займ онлайн? Newloans.ru – сайт, которым очень удобно пользоваться. Здесь представлена только полезная информация. Теперь не надо просить у близких и знакомых взаймы, с нами вы реализуете свои задумки. Просто оформите заявку, дождитесь решения и получите деньги.
Das Boomerang-Bet Casino ist eine aufstrebende Online GlГјcksspielplattform, die sich auf Spieler aus Deutschland spezialisiert hat. Mit einer breiten Auswahl an Spielen, groГџzГјgigen Boni und einem benutzerfreundlichen Design erfreut sich das Casino einer wachsenden Beliebtheit bei GlГјcksspielern.
Das Boomerang-Bet Casino bietet eine Vielzahl von Spielen, darunter Spielautomaten, Tischspiele wie Roulette und Blackjack, sowie Live-Dealer-Spiele. Die Spiele stammen von renommierten Softwareanbietern wie NetEnt, Microgaming und Play’n GO, was fГјr eine hohe QualitГ¤t und ein erstklassiges Spielerlebnis sorgt.
Neben einer großen Auswahl an Spielen bietet das Boomerang-Bet Casino auch großzügige Boni und Promotionen für neue und bestehende Spieler. Neukunden können sich über einen Willkommensbonus freuen, der Freispiele und Bonusguthaben beinhaltet. Auch regelmäßige Aktionen wie Einzahlungsboni, Freispiele und Cashback-Angebote sorgen dafür, dass Spieler immer wieder gerne im Boomerang-Bet Casino spielen.
Das Casino verfГјgt zudem Гјber eine benutzerfreundliche Webseite, die es einfach macht, Spiele zu finden und zu spielen. Der Kundenservice ist freundlich und kompetent und steht Spielern bei Fragen und Problemen jederzeit zur VerfГјgung.
Insgesamt ist das Boomerang-Bet Casino eine hervorragende Option fГјr Spieler, die auf der Suche nach einer unterhaltsamen und sicheren Online GlГјcksspielplattform sind. Mit einer groГџen Auswahl an Spielen, groГџzГјgigen Boni und einem erstklassigen Kundenservice ist das Casino definitiv einen Besuch wert.
https://boomerangcasino.one/
https://gatesofolympus.auction/# gates of olympus demo oyna
Um Geld vom Tipico Casino auszahlen zu lassen, mГјssen Spieler einige Schritte befolgen. ZunГ¤chst muss man sich in sein Spielerkonto auf der Website von Tipico einloggen. Dort kann man unter dem MenГјpunkt “Auszahlungen” die gewГјnschte Auszahlungsmethode auswГ¤hlen.
Es gibt verschiedene Möglichkeiten, um Geld von Tipico Casino auszahlen zu lassen. Dazu gehören unter anderem die Banküberweisung, die Kreditkarte oder E-Wallets wie PayPal oder Skrill. Es ist wichtig zu beachten, dass man die gleiche Zahlungsmethode für die Auszahlung wählen muss, mit der man auch eingezahlt hat.
Nachdem man die Auszahlungsmethode gewählt hat, muss man den gewünschten Auszahlungsbetrag angeben und die Auszahlungsanfrage bestätigen. Die Bearbeitungszeit für Auszahlungen kann je nach Zahlungsmethode variieren. In der Regel dauert es jedoch wenige Werktage, bis das Geld auf dem Konto des Spielers gutgeschrieben wird.
Es ist auch wichtig zu beachten, dass Tipico bestimmte Sicherheitsvorkehrungen hat, um sicherzustellen, dass die Auszahlung an den richtigen Spieler geht. Daher kann es sein, dass man seine Identität durch die Vorlage von Ausweisdokumenten bestätigen muss, bevor die Auszahlung bearbeitet werden kann.
Insgesamt ist es also relativ einfach, Geld vom Tipico Casino auszahlen zu lassen, solange man die richtigen Schritte befolgt und alle erforderlichen Informationen bereitstellt. Auf diese Weise können Spieler ihre Gewinne schnell und sicher auf ihr Konto überweisen lassen und ihr Spielerlebnis bei Tipico genießen.
https://tipicocasino.one/
pin-up casino giris: pin up casino indir – pin-up online
http://aviatoroyna.bid/# aviator sinyal hilesi ucretsiz
celecoxib capsules used for
Der Tipico Casino Bonus Code 2018 ist eine tolle Möglichkeit für Spieler, sich zusätzliches Guthaben für ihre Casino-Spiele zu sichern. Mit diesem Bonus Code können Spieler ihre Gewinnchancen erhöhen und noch mehr Spaß am Spiel haben.
Um den Tipico Casino Bonus Code 2018 zu erhalten, müssen Spieler zunächst ein Konto bei Tipico Casino registrieren. Anschließend können sie den Bonus Code eingeben und erhalten sofort einen Bonus auf ihre Einzahlung. Dieser Bonus kann je nach Aktion variieren, so dass es sich lohnt, regelmäßig nach neuen Angeboten Ausschau zu halten.
Spieler können den Bonus Code verwenden, um ihre Lieblingsspiele im Casino zu spielen, wie zum Beispiel Slots, Roulette oder Blackjack. Mit dem zusätzlichen Guthaben können sie länger spielen und die Chance auf hohe Gewinne erhöhen.
Es ist wichtig, die Bedingungen des Bonus Codes zu beachten, um sicherzustellen, dass der Bonus korrekt genutzt wird. In der Regel müssen Spieler den Bonus mehrmals umsetzen, bevor sie ihn auszahlen lassen können. Es empfiehlt sich, die Bonusbedingungen vor der Nutzung des Codes sorgfältig zu lesen.
Der Tipico Casino Bonus Code 2018 ist eine großartige Möglichkeit für Spieler, ihr Casino-Erlebnis zu verbessern und noch mehr Spaß zu haben. Mit dem zusätzlichen Guthaben können sie ihre Lieblingsspiele spielen und die Chance auf hohe Gewinne erhöhen. Es lohnt sich also, den Bonus Code zu nutzen und das beste aus dem Casino-Erlebnis bei Tipico herauszuholen.
https://tipicocasino.one/
https://aviatoroyna.bid/# aviator oyunu 100 tl
qiyezp.com
Yang Ya는 분명히 Liu Jin의 분노에 겁을 먹었습니다.
sun potion ashwagandha
Boomerang Casino Bonus ohne Einzahlung
Das Boomerang Casino ist ein aufstrebendes Online-Casino, das seinen Spielern eine Vielzahl von großzügigen Boni und Promotionen bietet. Einer der beliebtesten Boni, die das Boomerang Casino anbietet, ist der Bonus ohne Einzahlung. Diese Art von Bonus ermöglicht es den Spielern, ohne eigenes Geld zu riskieren, das Casino auszuprobieren und echte Gewinne zu erzielen.
Der Boomerang Casino Bonus ohne Einzahlung ist in der Regel für neue Spieler verfügbar, die sich zum ersten Mal registrieren. Um den Bonus zu erhalten, müssen sich die Spieler lediglich anmelden und ein neues Konto erstellen. Der Bonus wird dann automatisch gutgeschrieben, und die Spieler können ihn verwenden, um verschiedene Casinospiele zu spielen.
Mit dem Boomerang Casino Bonus ohne Einzahlung haben die Spieler die Möglichkeit, echte Gewinne zu erzielen, ohne ihr eigenes Geld zu riskieren. Dies macht den Bonus besonders attraktiv für Spieler, die das Casino ausprobieren möchten, ohne zuerst eine Einzahlung zu tätigen.
Es ist jedoch wichtig zu beachten, dass der Boomerang Casino Bonus ohne Einzahlung in der Regel bestimmten Bedingungen unterliegt. Diese können beispielsweise Mindestumsatzanforderungen oder maximalen Auszahlungsbeträge umfassen. Bevor die Spieler den Bonus nutzen, sollten sie daher die Geschäftsbedingungen des Casinos sorgfältig lesen, um sicherzustellen, dass sie alle Anforderungen erfüllen.
Insgesamt ist der Boomerang Casino Bonus ohne Einzahlung eine großartige Möglichkeit für Spieler, das Casino auszuprobieren und echte Gewinne zu erzielen, ohne eigenes Geld zu riskieren. Mit einer Reihe von spannenden Spielen und lukrativen Boni ist das Boomerang Casino definitiv eine gute Wahl für alle, die nach einem unterhaltsamen und lohnenden Online-Casino-Erlebnis suchen.
https://boomerangcasino.one/
gates of olympus oyna demo: gates of olympus demo free spin – gate of olympus hile
Pro Studio окажет вам помощь в воплощении амбициозных проектов в реальность. Сотрудничая с нами, вы получите в достижении ваших целей прекрасных партнеров. Для различных бизнесов, мы специализируемся на создании качественных сайтов. Знаем, как сделать лучше, всегда учитываем требования и пожелания каждого клиента. Требуется создание сайта под ключ на битриксе? Iv-SEO.ru – здесь у вас есть возможность ознакомиться с услугами и узнать всю информацию о нашем digital-агентстве. Работаем как в Москве, так и в других регионах России. Чтобы узнать подробнее об условиях сотрудничества, свяжитесь с нами.
http://aviatoroyna.bid/# aviator oyunu 50 tl
Das Tipico Live Casino bietet Spielern die Möglichkeit, von zu Hause aus ein authentisches Casinoerlebnis zu genießen. Mit einer Vielzahl von Live-Spielen wie Roulette, Blackjack und Baccarat, die von professionellen Dealern geleitet werden, können Spieler ihre Lieblingsspiele in Echtzeit spielen.
Ein großer Vorteil des Tipico Live Casinos ist die Interaktion mit den Dealern und anderen Spielern. Durch die Chat-Funktion können Spieler mit den Dealern chatten, Fragen stellen und sich mit anderen Spielern austauschen, was das Spielerlebnis noch aufregender macht.
Darüber hinaus bietet das Tipico Live Casino eine Vielzahl von Tischlimits, so dass Spieler mit unterschiedlichen Budgets das passende Spiel finden können. Ob Anfänger oder High Roller, im Tipico Live Casino ist für jeden etwas dabei.
Ein weiterer Pluspunkt des Tipico Live Casinos ist die Flexibilität. Spieler können jederzeit und von überall aus auf das Live Casino zugreifen, sei es über den Desktop oder das mobile Endgerät. Dadurch können Spieler ihre Lieblingsspiele spielen, wann immer ihnen danach ist.
Das Tipico Live Casino bietet auch regelmäßige Aktionen und Boni für Spieler an, die das Spielerlebnis noch verbessern. Mit einer sicheren und benutzerfreundlichen Plattform können Spieler ihre Lieblingsspiele ohne Bedenken genießen.
Insgesamt bietet das Tipico Live Casino ein erstklassiges Casinoerlebnis mit einer Vielzahl von Spielen, Interaktionen und spannenden Aktionen fГјr Spieler. Egal, ob Sie ein erfahrener Casino-Spieler sind oder gerade erst anfangen, das Tipico Live Casino ist definitiv einen Besuch wert.
https://tipicocasino.one/
https://slotsiteleri.guru/# bonus veren casino slot siteleri
zoloft or celexa
Wer kennt das nicht – man möchte ein paar Runden im Tipico Casino spielen und plötzlich ist das Geld blockiert. Diese Situation kann sehr frustrierend sein, vor allem wenn man sich auf den Spielspaß gefreut hat. Doch warum passiert so etwas und wie kann man das Problem lösen?
Es gibt verschiedene Gründe, warum Geld im Tipico Casino blockiert sein kann. Einer der häufigsten Gründe ist, dass der Spieler sein Konto nicht vollständig verifiziert hat. Das bedeutet, dass der Spieler seine Identität noch nicht bestätigt hat, was für das Casino aus Sicherheitsgründen wichtig ist. In diesem Fall muss der Spieler seine Identität nachweisen, damit das Geld freigegeben werden kann.
Ein weiterer Grund für blockiertes Geld im Tipico Casino kann ein technisches Problem sein. Dies kann zum Beispiel auftreten, wenn es Probleme mit der Zahlungsmethode gibt oder wenn das Casino technische Schwierigkeiten hat. In solchen Fällen sollte der Spieler den Kundenservice kontaktieren und das Problem schildern. Oftmals können die Mitarbeiter des Casinos das Problem schnell lösen und das Geld wieder freigeben.
Es ist auch möglich, dass das Geld blockiert ist, weil der Spieler gegen die AGBs des Casinos verstoßen hat. Zum Beispiel, wenn der Spieler versucht hat, Bonusbedingungen zu umgehen oder wenn er versucht hat, mehrere Konten zu eröffnen. In solchen Fällen wird das Geld in der Regel einbehalten und der Spieler kann mit Konsequenzen rechnen.
Um blockiertes Geld im Tipico Casino zu vermeiden, ist es wichtig, sich an die Regeln des Casinos zu halten und sein Konto vollständig zu verifizieren. Sollte es dennoch zu Problemen kommen, ist es ratsam, den Kundenservice zu kontaktieren und das Problem zu schildern. Oftmals kann das Problem schnell gelöst werden und der Spielspaß kann weitergehen.
https://tipicocasino.one/
sweet bonanza taktik: sweet bonanza 90 tl – slot oyunlari
aviator sinyal hilesi ucretsiz: aviator hile – aviator casino oyunu
quetiapine 100mg sale – bupropion drug eskalith price
buy quetiapine medication – order generic zoloft 50mg eskalith online order
Boomerang Casino Poker: Ein neues und aufregendes Spiel
Boomerang Casino Poker ist ein aufregendes neues Spiel, das in den letzten Jahren immer beliebter geworden ist. Es kombiniert die grundlegenden Regeln des traditionellen Pokers mit einem einzigartigen Dreh, der es von anderen Pokervarianten abhebt.
Das Spiel wird mit einem Standard-Kartenspiel gespielt, wobei die Spieler versuchen, die beste Pokerhand zu bilden. Der große Unterschied liegt jedoch darin, dass die Karten nach dem Austeilen zurückgegeben werden und erneut ausgeteilt werden. Dies gibt den Spielern die Möglichkeit, ihre Hand zu verbessern und strategische Entscheidungen zu treffen, die ihnen einen Vorteil verschaffen können.
Boomerang Casino Poker kann sowohl in traditionellen Casinos als auch online gespielt werden. Viele Spieler finden die schnelle und dynamische Natur des Spiels ansprechend, da es keine langwierigen Wartezeiten gibt und die Action immer auf Hochtouren bleibt.
Ein weiterer Vorteil von Boomerang Casino Poker ist, dass es für Spieler verschiedener Erfahrungsstufen zugänglich ist. Sowohl Anfänger als auch erfahrene Spieler können Spaß daran haben, da das Spiel einfach zu erlernen ist, aber auch taktisches Geschick erfordert, um erfolgreich zu sein.
Wenn Sie also auf der Suche nach einer aufregenden neuen Pokervariante sind, sollten Sie Boomerang Casino Poker definitiv eine Chance geben. Mit seinem einzigartigen Konzept und seiner hohen Spielgeschwindigkeit wird es Sie sicherlich stundenlang unterhalten. Also mischen Sie die Karten und sehen Sie, ob das GlГјck auf Ihrer Seite ist!
https://boomerangcasino.one/
http://aviatoroyna.bid/# aviator mostbet
Boomerang Casino Bonus ohne Einzahlung
Immer mehr Online-Casinos locken neue Spieler mit attraktiven Bonusangeboten, um sich von der Konkurrenz abzuheben. Einer dieser Anbieter ist das Boomerang Casino, das einen besonders groГџzГјgigen Bonus ohne Einzahlung anbietet.
Ein Bonus ohne Einzahlung bedeutet, dass man als neuer Spieler einen Bonus erhält, ohne zuvor Geld auf das Spielerkonto eingezahlt zu haben. Das Boomerang Casino belohnt seine neuen Kunden mit einem Bonus von 50 Freispielen ohne Einzahlung, die sie an ausgewählten Spielautomaten nutzen können. Dadurch haben Spieler die Möglichkeit, das Casino und seine Spiele risikofrei auszuprobieren, ohne eigenes Geld investieren zu müssen.
Um den Boomerang Casino Bonus ohne Einzahlung in Anspruch zu nehmen, muss man sich lediglich als neuer Spieler registrieren und den Bonuscode eingeben. Anschließend werden die Freispiele dem Spielerkonto gutgeschrieben und können sofort genutzt werden. Es ist jedoch wichtig zu beachten, dass Gewinne aus Freispielen oft bestimmten Umsatzbedingungen unterliegen, die erfüllt werden müssen, bevor eine Auszahlung beantragt werden kann.
Der Boomerang Casino Bonus ohne Einzahlung bietet Spielern eine gute Möglichkeit, das Casino kennenzulernen und erste Gewinne zu erzielen, ohne eigenes Geld riskieren zu müssen. Wer also auf der Suche nach einem spannenden Online-Casino mit großzügigen Bonusangeboten ist, sollte das Boomerang Casino definitiv in Betracht ziehen.
https://boomerangcasino.one/
Интернет-магазин ТопКлиматДВ, специализируется на климатическом оборудовании. Осуществляем поставки в любой регион РФ. Предлагаем привлекательные цены, длительную гарантию на все позиции и высочайшее качество обслуживания. Ищете сплит система купить Хабаровск? Топклиматдв.рф – сайт, где найдете то, что нужно для создания комфортной атмосферы в вашем доме. Можете сами выбрать удобный способ оплаты и доставки. Если хотите сделать заказ на новейшую модель климатического оборудования с необходимостью монтажа «под ключ», то вы попали точно по адресу!
sweet bonanza yorumlar: sweet bonanza guncel – sweet bonanza yasal site
Das Boomerang Casino Mobiles – Spielen Sie unterwegs!
Im modernen Zeitalter der Technologie ist es einfacher denn je, auf Spiele und Unterhaltung zuzugreifen, egal wo man sich befindet. Mit dem Boomerang Casino Mobiles können Sie nun auch unterwegs ganz bequem auf Ihre Lieblingscasinospiele zugreifen.
Das Boomerang Casino Mobiles bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele, Live-Casino und vieles mehr. Egal, ob Sie ein Fan von klassischen Spielautomaten oder modernen Videoslots sind, hier finden Sie garantiert die richtigen Spiele fГјr sich.
Das mobile Casino ist für alle gängigen Geräte optimiert, sei es ein Smartphone oder Tablet. Durch die intuitive Benutzeroberfläche können Sie ganz einfach durch die Auswahl der Spiele navigieren und können sofort mit dem Spielen beginnen.
Ein weiterer großer Vorteil des Boomerang Casino Mobiles ist die Möglichkeit, auch unterwegs Ein- und Auszahlungen vorzunehmen. Mit einer Vielzahl von sicheren Zahlungsmethoden stehen Ihnen alle Möglichkeiten offen, Geld auf Ihr Konto einzuzahlen oder Gewinne abzuheben.
Darüber hinaus bietet das mobile Casino regelmäßige Aktionen und Boni, um Ihre Spielerfahrung noch spannender zu gestalten. Von Freispielen bis hin zu Einzahlungsboni gibt es hier eine Vielzahl von Belohnungen, die auf Sie warten.
Also, warum warten? Laden Sie einfach die Boomerang Casino Mobiles App herunter oder besuchen Sie die mobile Website und tauchen Sie ein in die Welt des mobilen Casinos. Spielen Sie unterwegs und genieГџen Sie jederzeit und Гјberall spannende Casinospiele!
https://boomerangcasino.one/
https://pinupgiris.fun/# pin up giris
http://pinupgiris.fun/# pin-up casino indir
Gogo Casino är ett av de ledande online casinona på marknaden och de har nyligen lanserat ett spännande samarbete med en annan populär aktör inom spelbranschen. Detta samarbete har väckt stor uppmärksamhet bland spelare och casinonördar världen över.
Det nya samarbetet innebär att spelare nu kan ta del av ännu fler spel och erbjudanden hos Gogo Casino. Den andra parten i samarbetet har en stor portfölj av populära spel och genom detta samarbete kan Gogo Casino erbjuda sina spelare ännu mer variation och spännande spelupplevelser.
Förutom det bredare spelutbudet kommer också spelarna att kunna ta del av generösa bonusar och kampanjer som endast är tillgängliga genom detta samarbete. Det här är en stor fördel för spelare som alltid är ute efter de bästa erbjudandena och vill få så mycket spel för sina pengar som möjligt.
Gogo Casino har alltid varit känt för att erbjuda en säker och trygg spelupplevelse för sina spelare och detta samarbete är inget undantag. Båda parterna i samarbetet har en stark och pålitlig licens vilket garanterar att spelarna kan känna sig trygga när de spelar hos Gogo Casino.
Det här samarbetet är definitivt en vinn-vinn situation för både Gogo Casino och deras spelare. Spelarna får mer variation och spänning i sitt spelande samtidigt som casinot kan attrahera fler spelare och stärka sin position på marknaden.
För spelare som är ute efter en riktigt grym spelupplevelse och möjligheten att vinna stora vinster är Gogo Casino det självklara valet. Med det nya samarbetet kan spelarna se fram emot ännu mer spänning och roliga stunder hos detta populära online casino. Så varför inte prova lyckan redan idag?
https://gogocasino.one
Gogo Casino är en relativt ny spelplattform på marknaden som erbjuder en enkel och smidig spelupplevelse för alla typer av spelare. Här får du tillgång till ett brett utbud av casinospel i en modern och användarvänlig miljö.
En av fГ¶rdelarna med Gogo Casino Г¤r att de har ett stort och varierat utbud av spel frГҐn vГ¤lkГ¤nda leverantГ¶rer som NetEnt, Microgaming och Play’n GO. Du hittar allt frГҐn klassiska spelautomater och bordsspel till progressiva jackpottar och live casino.
En annan fördel är att du kan spela utan att behöva skapa ett konto. Istället använder du dig av BankID för att snabbt och säkert verifiera din identitet och göra insättningar och uttag. Det betyder att du kan komma igång och spela på nolltid utan krångel.
Gogo Casino erbjuder även generösa bonusar och kampanjer för sina spelare. Du kan se fram emot välkomstbonusar, free spins och cashback-erbjudanden som gör din spelupplevelse ännu roligare och mer lönsam.
Sammanfattningsvis är Gogo Casino en spännande spelplattform som passar både nybörjare och erfarna spelare. Med sitt breda spelutbud, smidiga registreringsprocess och generösa bonusar är det definitivt värt att ge det en chans. Besök Gogo Casino idag och kolla själv vad de har att erbjuda!
https://gogocasino.one
Gogo Casino – FГ¶r en genomskinlig spelupplevelse
Gogo Casino är en spännande online spelsida som fokuserar på att erbjuda en transparent och rättvis spelupplevelse för alla sina spelare. Med en enkel och stilren design är det lätt att navigera sig runt på sajten och hitta precis det spel man letar efter.
En av de största fördelarna med Gogo Casino är dess transparens när det gäller bonusar och villkor. Här kan spelarna vara säkra på att de får en rättvis behandling och att det inte finns några dolda regler som kan påverka deras spelupplevelse negativt.
När det gäller insättningar och uttag är processen smidig och enkel. Gogo Casino erbjuder flera olika betalningsmetoder så att spelarna kan välja den som passar dem bäst. Dessutom är alla transaktioner säkra och skyddade med den senaste krypteringstekniken för att spelarna ska kunna känna sig trygga när de sätter in eller tar ut sina pengar.
Gogo Casino är även känt för sitt stora utbud av spel från de bästa spelleverantörerna i branschen. Här kan spelarna hitta allt från klassiska slots till avancerade live casinospel som ger en autentisk casinoupplevelse direkt från hemmet.
För de spelare som värdesätter en transparent och rättvis spelupplevelse är Gogo Casino definitivt ett bra val. Med en användarvänlig design, generösa bonusar och ett stort utbud av spel kommer spelarna garanterat att ha en underhållande tid på denna spelsida. Besök Gogo Casino idag och upplev själv den genomskinliga spelvärlden!
https://gogocasino.one
GoGo Casino är en spännande och underhållande online spelsajt som erbjuder sina spelare en mängd olika casinospel att välja mellan. Med ett stort utbud av spelautomater, bordsspel och livecasino är det lätt att hitta något som passar just dig.
En av fördelarna med GoGo Casino är att det är en svensk spelsajt, vilket innebär att du kan känna dig trygg när du spelar här. Sajten är licensierad av Spelinspektionen och följer alla regler och bestämmelser som gäller för spel i Sverige.
GoGo Casino erbjuder också en smidig och enkel registreringsprocess, vilket gör det lätt att komma igång och börja spela. Du kan enkelt göra insättningar och uttag med hjälp av populära betalningsmetoder som Trustly och Swish.
Förutom det stora utbudet av spel och den säkra spelmiljön erbjuder GoGo Casino också generösa bonusar och kampanjer för sina spelare. Du kan ta del av välkomstbonusar, free spins och mycket mer när du registrerar dig som ny spelare.
Sammanfattningsvis är GoGo Casino en toppenval för dig som gillar att spela online casino. Med sitt stora spelutbud, säkra spelmiljö och generösa bonusar är det här en sajt som verkligen levererar på alla fronter. Så varför inte testa lyckan på GoGo Casino redan idag? Lycka till!
https://gogocasino.one
Gogo Casino Recension
Gogo Casino är en relativt ny spelplattform på den svenska marknaden som lanserades år 2019. Med ett fokus på snabba och smidiga spelupplevelser, har Gogo Casino snabbt blivit populärt bland spelare som föredrar att spela online.
Ett av de främsta fördelarna med Gogo Casino är dess enkla och användarvänliga design som gör det lätt att navigera på sidan. Dessutom erbjuder de ett brett utbud av spel från kända leverantörer som NetEnt, Microgaming och Yggdrasil, vilket garanterar en varierad och underhållande spelupplevelse för spelare.
En annan fördel med Gogo Casino är deras generösa välkomstbonus för nya spelare. Genom att registrera sig på plattformen kan spelare ta del av en bonus som ger dem extra pengar att spela för, vilket ökar chanserna att vinna stora vinster.
För de spelare som föredrar att spela på mobila enheter, erbjuder Gogo Casino också en mobilanpassad version av sin plattform som gör det möjligt att spela favoritspel var som helst och när som helst.
Sammanfattningsvis kan vi konstatera att Gogo Casino är en pålitlig och underhållande spelplattform som erbjuder ett brett utbud av spel och generösa bonusar för sina spelare. Med sin enkla design och användarvänliga gränssnitt är Gogo Casino definitivt värt att prova för alla som är intresserade av att spela online.
https://gogocasino.one
Tipico Casino ist eine der beliebtesten Online-Casino-Plattformen in Deutschland. Mit einer groГџen Auswahl an Spielen, darunter Slots, Roulette, Blackjack und mehr, bietet Tipico seinen Kunden ein unterhaltsames und sicheres Spielerlebnis.
Das Funktionieren von Tipico Casino ist einfach und unkompliziert. Um ein Konto zu eröffnen, muss man sich lediglich auf der Webseite registrieren und seine persönlichen Daten angeben. Nach der Registrierung kann man sofort mit dem Spielen beginnen.
Um Geld auf sein Konto einzuzahlen, stehen verschiedene Zahlungsoptionen zur VerfГјgung, darunter Kreditkarten, BankГјberweisungen und E-Wallets wie PayPal und Skrill. Die Einzahlungen werden in der Regel sofort gutgeschrieben, so dass man sofort mit dem Spielen loslegen kann.
Wenn man gewinnt, kann man sich sein Geld einfach und bequem auszahlen lassen. Dazu muss man lediglich eine Auszahlungsanfrage stellen und seine Daten bestätigen. Die Auszahlungen werden in der Regel innerhalb weniger Tage bearbeitet und auf das angegebene Konto des Spielers überwiesen.
Tipico Casino bietet auch einen professionellen Kundenservice, der bei Fragen oder Problemen rund um die Uhr zur Verfügung steht. Man kann das Team per E-Mail, Live-Chat oder Telefon kontaktieren und erhält in der Regel schnell und kompetent Unterstützung.
Insgesamt funktioniert Tipico Casino auf einfache und effiziente Weise. Mit einer benutzerfreundlichen Oberfläche, schnellen Zahlungen und einem hervorragenden Kundenservice bietet die Plattform ein rundum erstklassiges Spielerlebnis für alle Casino-Fans. Probieren Sie es selbst aus und erleben Sie den Nervenkitzel von Tipico Casino!
https://tipicocasino.one/
pin-up giris: pin-up giris – aviator pin up
yasal slot siteleri: en iyi slot siteleri – en iyi slot siteleri
buspirone hcl 30 mg
http://sweetbonanza.bid/# sweet bonanza free spin demo
Zet Casino Auszahlung Probleme
Bei Online-Casinos ist es leider keine Seltenheit, dass Spieler auf Auszahlungsprobleme stoßen. Ein aktuelles Beispiel dafür ist das Zet Casino, das in den letzten Wochen vermehrt negative Schlagzeilen gemacht hat. Viele Spieler berichten von Schwierigkeiten bei der Auszahlung ihrer Gewinne und von langen Wartezeiten, bis das Geld tatsächlich auf ihrem Konto landet.
Die Gründe für diese Probleme können vielfältig sein. Oftmals liegt es an technischen Schwierigkeiten im Zahlungssystem des Casinos oder an fehlerhaften Daten, die vom Spieler angegeben wurden. Manchmal stecken aber auch betrügerische Absichten dahinter, wenn das Casino sich absichtlich weigert, Gewinne auszuzahlen.
Um solche Probleme zu vermeiden, ist es wichtig, sich vor dem Spielen in einem Online-Casino ausgiebig zu informieren. Seriöse Anbieter zeichnen sich durch eine transparente Auszahlungspolitik aus, in der alle Bedingungen und Gebühren klar kommuniziert werden. Zudem sollte man darauf achten, dass das Casino über eine gültige Glücksspiel-Lizenz verfügt und von unabhängigen Prüfstellen kontrolliert wird.
Falls man dennoch auf Probleme bei der Auszahlung stößt, empfiehlt es sich, den Kundenservice des Casinos zu kontaktieren und das Anliegen zu schildern. Oftmals kann auf diesem Wege eine schnelle Lösung gefunden werden. Sollte das Casino jedoch nicht kooperativ sein, bleibt als letzte Möglichkeit der Gang zur Glücksspielbehörde, die in solchen Fällen als Schlichtungsstelle fungiert.
Insgesamt sollte man also vorsichtig sein, wenn man in Online-Casinos spielt und sich vorab gut informieren, um mögliche Auszahlungsprobleme zu vermeiden. Denn nichts ist ärgerlicher, als sein hart verdientes Geld nicht ausgezahlt zu bekommen.
https://zetcasino.one/
Gogo Casino affiliates är ett partnerskapsprogram som erbjuds av Gogo Casino, ett populärt online casino som erbjuder ett brett utbud av spel och kampanjer. Genom att bli en affiliate kan man tjäna pengar genom att marknadsföra Gogo Casino till nya spelare.
Att vara en Gogo Casino affiliate innebär att man marknadsför casinot på olika sätt, till exempel genom att dela speciella erbjudanden och kampanjer på sociala medier, bloggar eller andra plattformar. Genom att locka nya spelare till Gogo Casino och få dem att registrera sig och spela på casinot kan man tjäna en andel av intäkterna som genereras av de spelare man har lockat till casinot.
Fördelarna med att vara en Gogo Casino affiliate inkluderar möjligheten att tjäna bra med pengar genom provisioner, flexibiliteten att arbeta när och var man vill samt den möjlighet som erbjuds att marknadsföra ett populärt och pålitligt online casino.
För att bli en affiliate hos Gogo Casino behöver man registrera sig på deras affiliatesida och följa instruktionerna för att komma igång. Man behöver också ha en stark närvaro online och kunna nå ut till många potentiella spelare för att maximera sina intäkter som affiliate.
Sammanfattningsvis är Gogo Casino affiliates ett bra sätt att tjäna pengar genom att marknadsföra ett populärt online casino till nya spelare. Med rätt strategi och engagemang kan man skapa en lönsam affärsverksamhet som affiliate hos Gogo Casino.
https://gogocasino.one
Gogo Casino är ett populärt online casino som har fått mycket uppmärksamhet på AskGamblers, en av de ledande recensionswebbplatserna för online casinon. Gogo Casino har snabbt blivit känt för sitt stora spelutbud, generösa bonusar och smidiga användarupplevelse.
En av de saker som har gjort Gogo Casino så populärt bland spelare är deras stora urval av spel. Med hundratals olika spel att välja mellan, inklusive slots, bordsspel och live casino spel, finns det något för alla typer av spelare. Dessutom samarbetar Gogo Casino med de bästa spelleverantörerna i branschen, vilket garanterar hög kvalitet på spelen.
En annan fördel med att spela på Gogo Casino är deras generösa bonusar och kampanjer. Nya spelare välkomnas med en välkomstbonus som ger dem extra pengar att spela för, och regelbundna spelare belönas med återkommande bonusar och erbjudanden. Dessutom har Gogo Casino ett lojalitetsprogram där spelare kan tjäna poäng och få belöningar för sin lojalitet.
Men det är inte bara spelutbud och bonusar som har gjort Gogo Casino så populärt. En annan stor fördel med att spela på detta casino är den smidiga användarupplevelsen. Webbplatsen är lätt att navigera och spelarna kan enkelt hitta sina favoritspel, göra insättningar och ta ut sina vinster.
Sammanfattningsvis är Gogo Casino ett utmärkt val för spelare som letar efter en allround casinoupplevelse. Med sitt stora spelutbud, generösa bonusar och smidiga användarupplevelse har detta casino blivit en favorit bland många spelare. Om du letar efter ett pålitligt och underhållande online casino är Gogo Casino definitivt värt att överväga.
https://gogocasino.one
order generic clomipramine – doxepin 75mg without prescription buy sinequan 25mg sale
Ищете трансерфинг реальности? Посетите сайт Zelands.ru и Вы узнаете кто такой кто такой Вадим Зеланд и что такое трансерфинг. Уникальная технология достижения целей трансерфинг зеланда дает возможность управлять событияи, а зеланд – это лучший специалист в данной сфере. Трансерфинг реальности Вадим Зеланд зайдите на сайт и узнайте больше.
Tipico Casino Code
Immer mehr Menschen in Deutschland entdecken die Welt der Online-Casinos und suchen nach Möglichkeiten, um ihr Glück zu versuchen und spannende Spiele zu spielen. Einer der beliebtesten Anbieter in diesem Bereich ist das Tipico Casino, das eine Vielzahl von Spielen sowie attraktive Bonusangebote für Neukunden bereithält. Ein besonders interessantes Feature bei Tipico ist der Casino Code, der es Spielern ermöglicht, zusätzliche Vorteile zu erhalten.
Der Tipico Casino Code ist ein spezieller Gutscheincode, den Spieler eingeben können, um zum Beispiel einen Bonus auf ihre Einzahlung zu erhalten oder Freispiele für bestimmte Spiele freizuschalten. Die Codes werden regelmäßig vom Casino herausgegeben und können auf verschiedenen Plattformen gefunden werden, wie zum Beispiel auf der Website des Casinos oder in Promotion-Mails.
Um den Casino Code bei Tipico einzulösen, müssen Spieler sich zunächst auf der Website des Casinos anmelden und den Code im entsprechenden Feld eingeben. Nach der Bestätigung wird der Bonus oder die Freispiele automatisch dem Konto gutgeschrieben und können direkt genutzt werden.
Es ist jedoch wichtig zu beachten, dass die Codes oft an bestimmte Bedingungen geknüpft sind, die eingehalten werden müssen, um den Bonus zu erhalten. Dazu gehören zum Beispiel Umsatzanforderungen oder eine Mindesteinzahlung. Es lohnt sich daher, vor der Einlösung eines Codes die genauen Konditionen zu überprüfen.
Insgesamt bietet der Tipico Casino Code Spielern die Möglichkeit, das Spielerlebnis im Casino zu verbessern und zusätzliche Chancen auf Gewinne zu erhalten. Es lohnt sich daher, regelmäßig nach neuen Codes Ausschau zu halten und diese zu nutzen, um das Beste aus dem Casino herauszuholen.
Fazit: Der Tipico Casino Code ist eine attraktive Möglichkeit, um zusätzliche Vorteile im Online-Casino zu erhalten und das Spielerlebnis noch spannender zu gestalten. Es lohnt sich daher, die Codes regelmäßig zu prüfen und zu nutzen, um das Beste aus dem Angebot von Tipico herauszuholen.
https://tipicocasino.one/
Gogo Casino är känt för enkelhet och snabbhet, och deras logotyp är inget undantag. Logotypen för detta populära onlinecasino har en glad och färgglad design som passar perfekt med deras innovativa och underhållande spelupplevelse.
Den blГҐa och rosa logotypen i stil med en bubbla eller moln fГ¶r tankarna till en lekfull och modern kГ¤nsla. De stiliserade bokstГ¤verna i namnet “Gogo” bildar en tydlig och iГ¶gonfallande grafik som lГ¤tt kan kГ¤nnas igen. Denna logotyp Г¤r inte bara snygg och unik, den kommunicerar ocksГҐ perfekt med Gogo Casinos varumГ¤rkesidentitet som ett roligt och prisvГ¤rt onlinecasino.
Många spelare känner igen och uppskattar den ljusa och välbearbetade logotypen för Gogo Casino, vilket gör den till en viktig del av deras varumärkesstrategi. Logotypen är en viktig del av varje casinos image och kan hjälpa till att bygga upp en positiv känsla hos spelare och skapa en stark koppling till varumärket.
Sammanfattningsvis är Gogo Casinos logotyp en välgjord grafisk representation av deras varumärke som lyckas kommunicera deras identitet som ett enkelt, roligt och modernt onlinecasino. Med sin lekfulla design och färgglada estetik är logotypen för Gogo Casino en framgångsrik del av deras varumärkesstrategi och en viktig faktor i deras popularitet bland spelare.
https://gogocasino.one
ashwagandha plants
Gogo Casino är ett populärt online casino som erbjuder ett brett utbud av spel och en trevlig spelupplevelse för sina spelare. I detta omdöme kommer vi att gå igenom några av de viktigaste funktionerna och fördelarna med Gogo Casino.
En av de främsta fördelarna med Gogo Casino är dess användarvänliga gränssnitt och enkelhet att navigera på webbplatsen. Spelare kan enkelt hitta sina favoritspel och välja mellan ett stort antal olika spelautomater och bordsspel. Dessutom erbjuder Gogo Casino även en mobilanpassad version av sin webbplats, vilket gör det enkelt för spelare att spela sina favoritspel var de än befinner sig.
Gogo Casino erbjuder också ett generöst välkomsterbjudande för nya spelare, vilket inkluderar en insättningsbonus och free spins. Dessutom erbjuder de regelbundet olika kampanjer och erbjudanden för sina befintliga spelare, vilket gör det möjligt för dem att få extra belöningar och bonusar när de spelar.
En annan fördel med Gogo Casino är dess snabba och säkra betalningsmetoder, vilket gör det enkelt för spelare att sätta in och ta ut sina vinster. De erbjuder ett brett utbud av betalningsalternativ, inklusive kreditkort, banköverföring och e-plånböcker, vilket gör det enkelt och bekvämt för spelare att hantera sina transaktioner.
Sammanfattningsvis är Gogo Casino en pålitlig och populär operatör som erbjuder en trevlig spelupplevelse för sina spelare. Med sitt stora spelutbud, generösa bonusar och snabba betalningsmetoder är det en bra destination för alla som är intresserade av att spela online casino. Vi rekommenderar definitivt att ge Gogo Casino en chans och prova deras spel idag.
https://gogocasino.one
Zet Casino Live Chat
Das Zet Casino ist eine beliebte Online-Glücksspielseite, die eine Vielzahl von Spielen für Spieler aller Art bietet. Neben einer umfangreichen Auswahl an Slots und Tischspielen bietet das Zet Casino auch einen Live-Chat für Spieler, die schnell und einfach Hilfe benötigen.
Der Live-Chat ist rund um die Uhr verfügbar und ermöglicht es den Spielern, sofort mit einem Kundendienstmitarbeiter in Kontakt zu treten. Egal, ob es sich um Fragen zu Ein- oder Auszahlungen handelt, um technische Probleme oder um allgemeine Anfragen, der Live-Chat steht den Spielern zur Verfügung, um ihnen bei allen Anliegen zu helfen.
Der Kundendienst von Zet Casino ist bekannt für seine schnelle und kompetente Hilfe. Die Mitarbeiter sind freundlich und gut geschult und stehen den Spielern mit Rat und Tat zur Seite. Der Live-Chat ist eine bequeme Möglichkeit, um sofortige Hilfe zu erhalten, ohne lange auf eine E-Mail-Antwort oder einen Rückruf warten zu müssen.
Zusätzlich zum Live-Chat bietet das Zet Casino auch eine umfangreiche FAQ-Sektion auf seiner Website, die Antworten auf häufig gestellte Fragen bietet. Hier finden die Spieler nützliche Informationen zu Themen wie Ein- und Auszahlungen, Boni und Promotionen, Sicherheit und verantwortungsbewusstem Spielen.
Insgesamt ist der Live-Chat von Zet Casino eine ausgezeichnete Option für Spieler, die schnelle und effiziente Hilfe benötigen. Mit freundlichen und kompetenten Mitarbeitern sowie einer einfachen Bedienung ist der Live-Chat eine gute Möglichkeit, um alle Fragen und Anliegen schnell und unkompliziert zu klären.
https://zetcasino.one/
buspirone overdose symptoms
celecoxib prescription
http://canadianpharmacy24.store/# best canadian online pharmacy
mexican drugstore online [url=https://mexicanpharmacy.shop/#]Online Pharmacies in Mexico[/url] п»їbest mexican online pharmacies
Zet Casino Bewertungen
Zet Casino ist ein Online-Casino, das in den letzten Jahren immer beliebter geworden ist. Es bietet eine Vielzahl von Spielen, großzügige Boni und eine benutzerfreundliche Benutzeroberfläche. Doch wie steht es um die Qualität des Casinos? Hier sind einige Bewertungen von Spielern, die Zet Casino ausprobiert haben.
Viele Spieler loben die groГџe Auswahl an Spielen, die Zet Casino anbietet. Von klassischen Slots bis hin zu Live-Casino-Spielen, hier findet jeder Spieler etwas nach seinem Geschmack. Die Spiele sind von bekannten und vertrauenswГјrdigen Anbietern wie NetEnt, Microgaming und Play’n GO entwickelt, was fГјr eine gute QualitГ¤t und ein reibungsloses Spielerlebnis sorgt.
Ein weiterer Pluspunkt von Zet Casino sind die großzügigen Boni und Aktionen, die regelmäßig angeboten werden. Neue Spieler können sich auf einen Willkommensbonus freuen, der ihre erste Einzahlung verdoppelt und zusätzlich Freispiele beinhaltet. Auch treue Spieler werden mit Reload-Boni, Cashback-Angeboten und VIP-Programmen belohnt.
Die Benutzeroberfläche von Zet Casino wird ebenfalls gelobt, da sie übersichtlich und einfach zu navigieren ist. Spieler können problemlos zwischen den verschiedenen Spielkategorien wechseln und ihre Lieblingsspiele finden. Die mobile Version des Casinos funktioniert einwandfrei und ermöglicht es den Spielern, auch unterwegs zu spielen.
Insgesamt sind die Bewertungen zu Zet Casino größtenteils positiv. Die Spieler schätzen die große Auswahl an Spielen, die großzügigen Boni und die benutzerfreundliche Benutzeroberfläche. Wenn Sie auf der Suche nach einem neuen Online-Casino sind, sollten Sie Zet Casino definitiv eine Chance geben.
https://zetcasino.one/
buy medicines online in india: Cheapest online pharmacy – pharmacy website india
Gogo Casino är en populär online-spelplattform som erbjuder ett brett utbud av casinospel för spelare att njuta av. Men många undrar: vem äger egentligen Gogo Casino?
Bakom Gogo Casino står det maltesiska spelbolaget Viral Interactive Limited. Företaget grundades år 2018 och har sedan dess blivit en betydande aktör inom den digitala spelbranschen. Viral Interactive Limited har licenser från både Malta Gaming Authority och Spelinspektionen i Sverige, vilket garanterar att Gogo Casino följer alla lagar och regler kring spel och spelansvar.
Viral Interactive Limited är också känt för att ha en transparent och säker spelupplevelse för sina användare. De erbjuder snabba utbetalningar, ett brett utbud av spel och en kundtjänst som är tillgänglig dygnet runt för att hjälpa spelare med eventuella frågor eller problem.
Så, för de som undrar vem som äger Gogo Casino, kan man tryggt säga att det är Viral Interactive Limited som har skapat denna spännande spelplattform. Med deras erfarenhet och expertis inom spelbranschen kan spelare vara säkra på en underhållande och säker spelupplevelse på Gogo Casino.
https://gogocasino.one
anafranil medication – buy paxil 20mg online generic doxepin 25mg
Der Casino Guru Zet – Ihr Experte fГјr GlГјcksspiele
Das Casino Guru Zet ist eine der bekanntesten und angesehensten Plattformen für Glücksspiele im Internet. Mit einer langjährigen Erfahrung und einem Team aus Experten hat sich das Casino Guru Zet einen Namen als vertrauenswürdige Quelle für Online-Casino-Spiele gemacht.
Das Casino Guru Zet bietet eine groГџe Auswahl an Spielen, darunter beliebte Klassiker wie Poker, Blackjack, Roulette und Spielautomaten. Die Plattform arbeitet nur mit den besten Softwareanbietern zusammen, um ihren Spielern ein hochwertiges und unterhaltsames Spielerlebnis zu bieten.
Ein weiterer Vorteil des Casino Guru Zet ist der Kundensupport. Das Team steht rund um die Uhr zur Verfügung, um Fragen zu beantworten, Probleme zu lösen oder einfach nur eine angenehme Spielerfahrung zu gewährleisten.
Das Casino Guru Zet überzeugt nicht nur mit einer großen Spieleauswahl und einem exzellenten Kundenservice, sondern auch mit großzügigen Boni und Aktionen für seine Kunden. Regelmäßige Promotions und Turniere sorgen für zusätzliche Spannung und die Chance, tolle Preise zu gewinnen.
Für alle, die gerne online spielen und auf der Suche nach einem seriösen und unterhaltsamen Online-Casino sind, ist das Casino Guru Zet eine hervorragende Wahl. Mit einer Vielzahl von Spielen, einem erstklassigen Kundenservice und großzügigen Boni können Spieler hier die ultimative Casino-Erfahrung genießen.
Besuchen Sie noch heute das Casino Guru Zet und tauchen Sie ein in die spannende Welt der GlГјcksspiele!
https://zetcasino.one/
Gogo Casino är en populär online spelplattform som erbjuder spelare en rad olika casinospel att njuta av. Men många frågar sig: Vem äger egentligen Gogo Casino?
Bakom Gogo Casino står företaget LeoVegas, en av de ledande aktörerna inom online spelindustrin. LeoVegas grundades år 2011 och har sedan dess vuxit till att bli en av de mest framgångsrika och respekterade spelföretagen i världen. Företaget är noterat på Nasdaq Stockholm och har ett starkt rykte för att erbjuda högkvalitativa spel och en säker spelupplevelse för sina användare.
Genom att äga Gogo Casino har LeoVegas möjlighet att fortsätta erbjuda spelare en spännande och varierad spelupplevelse. Genom att samarbeta med ledande spelleverantörer kan Gogo Casino erbjuda spel i världsklass och ständigt förnya sitt spelutbud för att hålla spelarna engagerade.
Trots att LeoVegas äger Gogo Casino, är det viktigt att komma ihåg att spel är en form av underhållning och att det är viktigt att spela ansvarsfullt. Gogo Casino strävar efter att erbjuda en säker spelmiljö och uppmuntrar sina spelare att spela med måtta och att sätta sina egna spelgränser.
Så för dig som undrar vem som äger Gogo Casino, kan du vara trygg i vetskapen om att det är ett företag med lång erfarenhet och en stark passion för att erbjuda en säker och underhållande spelupplevelse för alla sina användare. Besök Gogo Casino idag och upptäck allt vad de har att erbjuda!
https://gogocasino.one
buy prescription drugs from india Healthcare and medicines from India pharmacy website india
Visit the website predictor spaceman – to learn about the advantages of Predictor spaceman. Spaceman Predictor gives you the opportunity to increase your chances of winning in the fascinating world of predictor spaceman version 2.0. You can download spaceman predictor online now. Full review of the predictor version 2.0 spaceman application on the website.
Reduslim ist ein Nahrungsergänzungsmittel, das bei dm erhältlich ist und zur Gewichtsreduktion eingesetzt werden kann. Es handelt sich um Kapseln, die laut Hersteller durch die enthaltenen Wirkstoffe den Stoffwechsel ankurbeln und so beim Abnehmen unterstützen sollen. Doch was ist Reduslim genau und wie wirksam ist es wirklich?
Die Zusammensetzung von Reduslim umfasst unter anderem natürliche Inhaltsstoffe wie Grüntee-Extrakt, Garcinia Cambogia und Bitterorange, die dafür bekannt sind, den Stoffwechsel zu beschleunigen und das Hungergefühl zu reduzieren. Studien haben gezeigt, dass diese Wirkstoffe tatsächlich eine positive Wirkung auf die Gewichtsreduktion haben können.
Dennoch sollte beachtet werden, dass Reduslim allein keine Wunder bewirken kann. Eine gesunde Ernährung, ausreichend Bewegung und ein insgesamt gesunder Lebensstil sind weiterhin entscheidend, um abzunehmen und das Gewicht langfristig zu halten. Reduslim kann jedoch als unterstützende Maßnahme in Kombination mit einer ausgewogenen Lebensweise durchaus sinnvoll sein.
Bevor man sich für Reduslim entscheidet, ist es ratsam, mit einem Arzt zu sprechen und sich über mögliche Risiken und Nebenwirkungen zu informieren. Jeder Körper reagiert unterschiedlich auf Nahrungsergänzungsmittel, daher ist es wichtig, individuelle Bedürfnisse und Voraussetzungen zu berücksichtigen. Letztendlich bietet Reduslim bei dm eine Möglichkeit, den Abnehmprozess zu unterstützen, sollte aber nicht als alleinige Lösung betrachtet werden.
https://reduslim.at/
Gogo Casino Г¤r ett online casino som har blivit vГ¤ldigt populГ¤rt bland svenska spelare pГҐ senare tid. En av anledningarna till detta Г¤r deras generГ¶sa bonusar som de erbjuder till sina spelare. En av dessa bonusar Г¤r deras sГҐ kallade “bonus gogo casino”.
Denna bonus går ut på att spelare får en extra summa pengar att spela för när de gör en insättning. Denna summa brukar vara procentuell och kan variera beroende på vilken kampanj som pågår. Det kan handla om allt från 50% extra upp till 200% extra att spela för.
För att ta del av denna bonus behöver spelarna oftast ange en bonuskod när de gör sin insättning. Bonuskoden kan vanligtvis hittas på casinots hemsida eller skickas ut till spelarna via e-post eller sms.
Det finns dock vissa villkor som måste uppfyllas för att kunna ta del av bonusen. Oftast handlar det om att spelarna måste omsätta sina bonuspengar ett visst antal gånger innan de kan ta ut eventuella vinster. Det kan även finnas ett maxtak för hur mycket man kan vinna med hjälp av bonusen.
Sammanfattningsvis Г¤r “bonus gogo casino” en populГ¤r bonusform som erbjuds av Gogo Casino fГ¶r att belГ¶na sina spelare. Genom att ta del av denna bonus kan spelarna Г¶ka sina vinstchanser och fГҐ lite extra spГ¤nning i sina spel.
https://gogocasino.one
Gogo casino är ett populärt online casino som erbjuder spelare en spännande och underhållande spelupplevelse. En av de viktigaste aspekterna för många spelare är hur snabbt och smidigt de kan få ut sina vinster. Därför är utbetalningarna på Gogo casino något som många är intresserade av.
När det kommer till utbetalningar på Gogo casino kan spelare förvänta sig att få sina vinster utbetalda inom en rimlig tidsram. Utbetalningstiden beror på vilken metod spelaren väljer att använda sig av. De vanligaste metoderna inkluderar banköverföring, kreditkort och e-plånböcker som Skrill eller Neteller.
Vanligtvis tar det mellan 1-5 bankdagar för en utbetalning att behandlas och nå spelarens konto. Vissa metoder kan dock vara snabbare än andra, så det är viktigt att kolla upp vilken metod som passar en bäst för att få ut sina vinster så snabbt som möjligt.
För att underlätta och påskynda utbetalningsprocessen kan spelare se till att deras konto är verifierat och att de har skickat in eventuella dokument som krävs för att bekräfta deras identitet. Genom att följa dessa steg kan spelare säkerställa att deras utbetalningar processas smidigt och utan onödiga förseningar.
Sammanfattningsvis kan man säga att utbetalningarna på Gogo casino är snabba och pålitliga för spelare som vill njuta av sina vinster utan krångel. Genom att välja rätt utbetalningsmetod och se till att ens konto är verifierat kan spelare få ut sina vinster på ett effektivt sätt och fortsätta njuta av allt det roliga som Gogo casino har att erbjuda.
https://gogocasino.one
Boomerang Casino Erfahrungen Auszahlung
Boomerang Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen fГјr seine Spieler anbietet. In diesem Artikel werden wir uns genauer mit den Auszahlungserfahrungen der Spieler bei Boomerang Casino befassen.
Die meisten Spieler berichten von positiven Erfahrungen mit den Auszahlungen bei Boomerang Casino. Die Auszahlungszeiten sind schnell und die Spieler erhalten ihr Geld in der Regel innerhalb von 24 Stunden. Dies ist besonders beeindruckend, wenn man bedenkt, dass einige Online-Casinos bis zu einer Woche für Auszahlungen benötigen.
Ein weiterer Pluspunkt für Boomerang Casino ist die Vielfalt der Zahlungsmethoden, die es den Spielern ermöglicht, ihre Gewinne auf sichere und bequeme Weise abzuheben. Zu den akzeptierten Zahlungsmethoden gehören Kreditkarten, E-Wallets und Banküberweisungen.
Darüber hinaus bietet Boomerang Casino eine benutzerfreundliche Plattform, die es den Spielern leicht macht, ihre Auszahlungen zu verwalten. Die Auszahlungsanträge können einfach über das Spielerkonto gestellt werden und der Status der Anfrage kann jederzeit eingesehen werden.
Insgesamt sind die Erfahrungen mit den Auszahlungen bei Boomerang Casino überwiegend positiv. Die Spieler loben die schnellen Auszahlungszeiten, die Vielfalt der Zahlungsmethoden und die benutzerfreundliche Plattform. Wenn Sie nach einem verlässlichen und kundenorientierten Online-Casino suchen, ist Boomerang Casino auf jeden Fall eine gute Wahl.
https://boomerangcasino.one/
Die Reduslim oficjalna strona ist der beste Ort, um alle Informationen Гјber dieses beliebte Schlankheitsprodukt zu finden. Reduslim wird von vielen Menschen auf der ganzen Welt verwendet, um effektiv Gewicht zu verlieren und die gewГјnschte Figur zu erreichen. Auf der offiziellen Website finden Sie alles, was Sie Гјber die Inhaltsstoffe, die Anwendung und die Erfolgsgeschichten anderer Benutzer wissen mГјssen.
Reduslim ist eine natürliche Lösung zur Gewichtsreduktion, die ohne Nebenwirkungen funktioniert. Die einzigartige Kombination aus natürlichen Extrakten hilft dabei, den Stoffwechsel zu steigern, den Appetit zu kontrollieren und die Fettverbrennung zu fördern. Viele Menschen haben mit Reduslim bereits erstaunliche Ergebnisse erzielt und fühlen sich jetzt gesünder und selbstbewusster.
Besuchen Sie die Reduslim oficjalna strona, um mehr über dieses erstaunliche Produkt zu erfahren und noch heute mit Ihrer Gewichtsabnahme-Reise zu beginnen. Verabschieden Sie sich von lästigen Diäten und langwierigen Workouts und entdecken Sie die einfache und effektive Möglichkeit, Ihr Idealgewicht zu erreichen. Probieren Sie Reduslim noch heute aus und sehen Sie selbst, wie einfach es sein kann, Gewicht zu verlieren und sich großartig zu fühlen.
https://reduslim.at/
Gogo Casino är en populär online casino där spelare kan njuta av ett brett utbud av spelautomater, bordsspel och live casino. För de som har frågor eller behöver hjälp, erbjuder Gogo Casino en kundsupporttjänst som är tillgänglig genom olika kontaktmetoder.
Den mest bekväma och snabbaste sättet att komma i kontakt med Gogo Casino är genom deras live chattfunktion på webbplatsen. Genom att klicka på ikonen för live chatt kan spelare enkelt skicka sina frågor eller problem och få omedelbar hjälp från en supportagent.
FГ¶r de som fГ¶redrar att kommunicera via e-post, kan man skicka ett meddelande till Gogo Casino’s supportteam pГҐ deras angivna e-postadress. Kundsupporten Г¤r snabb att svara och gГ¶r sitt bГ¤sta fГ¶r att lГ¶sa eventuella problem eller frГҐgor som spelarna kan ha.
För de som föredrar att ringa, erbjuder Gogo Casino också ett telefonnummer där spelare kan ringa och prata direkt med en supportagent. Detta alternativ kan vara särskilt användbart för de som föredrar att ha en mer personlig interaktion när de kommunicerar med kundsupporten.
Sammanfattningsvis erbjuder Gogo Casino flera bekväma kontaktmetoder för sina spelare att använda när de behöver hjälp eller har frågor. Oavsett om det är via live chatt, e-post eller telefon, kan spelare vara säkra på att de får den hjälp de behöver när de spelar på Gogo Casino.
https://gogocasino.one
https://indianpharmacy.icu/# online shopping pharmacy india
Gogo Casino är en populär online spelplattform som erbjuder ett brett utbud av casinospel och snabba utbetalningar. Spelare kan njuta av spel som slots, bordsspel och live-dealerspel på denna spännande plattform.
En av de mest attraktiva funktionerna hos Gogo Casino är dess snabba utbetalningsprocess. När spelare väljer att ta ut sina vinster från plattformen kan de förvänta sig att pengarna kommer att nå deras bankkonto inom en mycket kort tidsram.
För att göra en utbetalning på Gogo Casino behöver spelare bara logga in på sitt konto, navigera till uttagssektionen och välja sin önskade uttagsmetod. Plattformen erbjuder flera olika alternativ för uttag, inklusive banköverföring, e-plånböcker och kredit- eller betalkort.
När uttagsbegäran har godkänts av plattformen behandlas utbetalningen omedelbart. Vanligtvis tar det bara några timmar för pengarna att nå spelarens bankkonto, vilket gör Gogo Casino till en av de snabbaste utbetalningscasinona på marknaden.
För spelare som värdesätter snabba och enkla utbetalningar är Gogo Casino definitivt ett utmärkt val. Med sitt breda utbud av spel och snabba utbetalningsprocess är detta ett casino som verkligen lever upp till sitt rykte som en av de bästa online-spelplattformarna.
https://gogocasino.one
Gogo Casino är en populär online-spelplattform som erbjuder en mängd olika casinospel för spelare att njuta av. Med en användarvänlig design och ett brett utbud av spel är det inte konstigt att många spelare flockas till Gogo Casino för en spännande spelupplevelse.
En av de mest pålitliga källorna för casinospelare är AskGamblers, en webbplats som granskar och betygsätter online-kasinon för att ge spelare en objektiv bedömning av deras tjänster. När det gäller Gogo Casino har de fått positiva recensioner från AskGamblers för sin enkla användarupplevelse och stora spelbibliotek.
Spelare kan enkelt hitta sina favoritspel på Gogo Casino, oavsett om de föredrar klassiska bordsspel som roulette och blackjack eller moderna spelautomater med spännande teman och funktioner. Med ett stort antal betalningsmetoder och snabba uttag är det enkelt för spelare att börja spela utan krångel.
AskGamblers har också uppmärksammat Gogo Casino för deras pålitliga kundsupport och generösa kampanjer och erbjudanden för spelare. Genom att erbjuda regelbundna belöningar och bonusar visar Gogo Casino sitt engagemang för att skapa en positiv spelupplevelse för alla sina spelare.
Om du letar efter ett pålitligt och underhållande online casino är Gogo Casino definitivt värt att utforska. Med hjälp av AskGamblers kan du vara säker på att du får en ärlig och opartisk recension av casinot innan du sätter igång och spelar. Så varför inte ge det en chans och se om Gogo Casino passar just dina spelbehov och preferenser? Lycka till!
https://gogocasino.one
canadianpharmacy com: Prescription Drugs from Canada – safe canadian pharmacy
Zet Casino Free Spins: Spielen Sie kostenlos und gewinnen Sie groГџ
Wer liebt es nicht, kostenlos zu spielen und dabei die Chance zu haben, groß zu gewinnen? Mit Zet Casino Free Spins ist genau das möglich! Free Spins sind eine großartige Möglichkeit, um neue Spiele auszuprobieren, ohne dabei eigenes Geld einsetzen zu müssen. In diesem Artikel erfahren Sie alles, was Sie über Zet Casino Free Spins wissen müssen.
Zet Casino bietet eine Vielzahl von Free Spins für seine Spieler an. Diese können als Willkommensbonus für neue Spieler oder als regelmäßige Promotionen für bestehende Spieler angeboten werden. Die Free Spins können für bestimmte Slots oder Tischspiele verwendet werden und bieten die Möglichkeit, echtes Geld zu gewinnen, ohne eigenes Geld einzusetzen.
Um Free Spins zu erhalten, müssen Spieler bestimmte Bedingungen erfüllen. Dies kann die Registrierung eines neuen Kontos, eine erste Einzahlung oder die Teilnahme an einer bestimmten Promotion sein. Sobald die Bedingungen erfüllt sind, werden die Free Spins automatisch gutgeschrieben und können sofort verwendet werden.
Es ist wichtig zu beachten, dass Free Spins in der Regel an bestimmte Umsatzbedingungen gebunden sind. Dies bedeutet, dass Gewinne aus den Free Spins eine bestimmte Anzahl an Malen umgesetzt werden müssen, bevor sie ausgezahlt werden können. Es ist daher ratsam, die Geschäftsbedingungen der Free Spins sorgfältig zu lesen, um Missverständnisse zu vermeiden.
Zet Casino bietet eine Vielzahl von Free Spins für seine Spieler an, sodass für jeden etwas dabei ist. Egal, ob Sie ein erfahrener Spieler sind oder gerade erst anfangen, mit den Free Spins haben Sie die Möglichkeit, Ihr Glück zu versuchen und dabei viel Spaß zu haben. Nutzen Sie also die Gelegenheit und spielen Sie kostenlos bei Zet Casino!
https://zetcasino.one/
Reduslim ist ein natГјrlicher Fatburner, der immer beliebter wird. Aber was ist Reduslim cos’ГЁ? Reduslim ist ein NahrungsergГ¤nzungsmittel, das aus natГјrlichen Zutaten wie grГјnem Tee-Extrakt, Garcinia Cambogia und Cayennepfeffer hergestellt wird. Diese Inhaltsstoffe helfen dabei, den Stoffwechsel zu beschleunigen und die Fettverbrennung zu steigern.
Reduslim cos’ГЁ ist fГјr diejenigen gedacht, die auf gesunde Weise abnehmen mГ¶chten. Es hilft dabei, den Appetit zu reduzieren und das Verlangen nach ungesunden Snacks zu unterdrГјcken. Durch die Einnahme von Reduslim kГ¶nnen Sie schneller abnehmen und Ihr Wunschgewicht erreichen.
Reduslim ist auch bekannt für seine entzündungshemmenden und antioxidativen Eigenschaften. Es kann dazu beitragen, den Körper zu entgiften und die Gesundheit zu verbessern. Darüber hinaus kann Reduslim dabei helfen, den Blutzuckerspiegel zu stabilisieren und den Cholesterinspiegel zu senken.
Insgesamt ist Reduslim eine groГџartige Option fГјr diejenigen, die auf gesunde Weise Gewicht verlieren mГ¶chten. Es ist wichtig zu beachten, dass Reduslim nur als Teil eines gesunden Lebensstils und einer ausgewogenen ErnГ¤hrung erfolgreich sein kann. Probieren Sie Reduslim cos’ГЁ aus und erleben Sie die positiven Auswirkungen auf Ihre Gesundheit und Ihr Gewicht.
https://reduslim.at/
Gogo Casino – en trasnparent spelupplevelse
Gogo Casino har snabbt blivit en populär destination för spelare som söker en transparent och säker spelupplevelse. Med sitt enkla och stilrena gränssnitt har casinot skapat en plattform där spelarna kan njuta av sina favoritspel utan krångliga villkor eller dolda avgifter.
Ett av de främsta kännetecknen för Gogo Casino är dess transparenta approach till spelutbud och regler. Spelarna kan enkelt navigera bland olika spelkategorier och hitta sina favoriter utan att behöva leta igenom en massa onödig information. Dessutom erbjuder casinot tydliga regler och villkor som är lättillgängliga för alla spelare.
När det kommer till transaktioner och betalningar är Gogo Casino också mycket transparent. Spelarna kan enkelt sätta in och ta ut pengar utan att behöva oroa sig för dolda avgifter eller otydliga regler. Casinot erbjuder också flera olika betalningsmetoder, vilket gör det lätt för spelarna att välja den metod som passar dem bäst.
Utöver sin transparenta approach är Gogo Casino också känt för sitt stora spelutbud. Här hittar spelarna alla sina favoritspel från välkända spelleverantörer, vilket gör att det finns något för alla smaker. Dessutom erbjuder casinot regelbundet kampanjer och bonusar som ger spelarna ännu mer spänning och underhållning.
Sammanfattningsvis är Gogo Casino en idealisk destination för spelare som värdesätter transparens och säkerhet i sin spelupplevelse. Med sitt enkla gränssnitt, tydliga regler och stora spelutbud har casinot skapat en plattform där spelarna kan njuta av sina favoritspel utan bekymmer. Gogo Casino är definitivt värt ett besök för alla som letar efter en trygg och transparent spelupplevelse.
https://gogocasino.one
mexican drugstore online: mexico pharmacy – mexican mail order pharmacies
Gogo casino bluff: Är det här den riktiga dealen?
Gogo casino har skapat en stor buzz på marknaden med sitt utbud av spel och generösa bonusar. Men det finns vissa rykten som säger att detta online casino kan vara en bluff. Är det verkligen värt att spela på Gogo casino, eller är det bara en bluff?
För det första är det viktigt att notera att Gogo casino har en licens från en respekterad spelmyndighet, vilket innebär att de uppfyller alla regler och bestämmelser som krävs för att driva ett online casino. Dessutom använder de sig av den senaste krypteringstekniken för att säkerställa att alla transaktioner är säkra och skyddade.
När det gäller spelutbudet erbjuder Gogo casino ett brett urval av spel från de ledande spelleverantörerna i branschen. Deras slots, bordsspel och live casinospel är av hög kvalitet och ger spelarna en autentisk casinoupplevelse.
När det gäller bonusar och kampanjer erbjuder Gogo casino generösa belöningar till sina spelare, inklusive välkomstbonusar, insättningsbonusar och freespins. Dessa erbjudanden är ett bra sätt att öka ens vinstchanser och maximera ens spelupplevelse.
Sammanfattningsvis verkar det som att Gogo casino inte är en bluff, utan ett pålitligt och pålitligt online casino. Så om du letar efter en spännande och säker spelplattform, kan Gogo casino vara det rätta valet för dig. Var säker på att läsa och förstå villkoren och bestämmelserna innan du registrerar dig, och spela ansvarsfullt. Lycka till och ha kul!
https://gogocasino.one
Gogo casino problem
I dagens samhälle är det allt vanligare att spela casino online. Det finns många fördelar med detta, som att det är bekvämt att spela hemifrån och att det finns ett brett utbud av spel att välja mellan. Men det finns också risker med att spela casino online, och ett problem som har uppmärksammats på senare tid är Gogo casino problem.
Gogo casino problem handlar om att spelare blir fast i en ond cirkel av spelberoende. När man spelar på Gogo casino kan det vara svårt att sluta, eftersom det finns ständiga incitament att fortsätta spela. Det kan handla om bonusar, tävlingar eller andra lockelser som gör att spelare känner sig motiverade att fortsätta spela, även om de egentligen inte vill eller har råd med det.
För personer med spelproblem kan detta vara extra farligt, eftersom de lätt kan hamna i en ekonomisk kris och få allvarliga konsekvenser för sin hälsa och välbefinnande. Det är därför viktigt att vara medveten om risken för Gogo casino problem och att ta ansvar för sitt spelande.
Det finns flera åtgärder som kan minska risken för att drabbas av Gogo casino problem. En av de viktigaste åtgärderna är att sätta gränser för sitt spelande, både när det gäller tid och pengar. Det är också viktigt att vara medveten om varningssignaler på spelberoende, som att spela för mycket eller att försöka vinna tillbaka förluster.
Det är också viktigt att söka hjälp om man upplever att man har problem med sitt spelande. Det finns många organisationer och stödgrupper som kan hjälpa till med rådgivning och behandling av spelproblem. Genom att vara öppen och ärlig om sitt spelande kan man få den hjälp och det stöd man behöver för att komma ur en destruktiv spelcykel.
Sammanfattningsvis är Gogo casino problem ett allvarligt problem som kan få allvarliga konsekvenser för den som drabbas. Det är därför viktigt att vara medveten om riskerna med att spela casino online och att ta ansvar för sitt spelande. Genom att sätta gränser och söka hjälp kan man undvika att hamna i en destruktiv spelcykel och istället njuta av sitt spelande på ett hälsosamt sätt.
https://gogocasino.one
top 10 online pharmacy in india: Healthcare and medicines from India – Online medicine order
indian pharmacies safe indian pharmacy buy medicines online in india
Reduslim ist eine bekannte Nahrungsergänzung, die bei der Gewichtsabnahme unterstützen soll. Die Zusammensetzung de Reduslim wurde sorgfältig entwickelt, um eine effektive Fettverbrennung zu ermöglichen. Die Inhaltsstoffe wirken synergistisch zusammen, um den Stoffwechsel anzukurbeln und den Appetit zu zügeln.
Die Composition de Reduslim enthält natürliche Zutaten wie grüner Tee, Garcinia Cambogia und Guarana, die alle für ihre fettverbrennenden Eigenschaften bekannt sind. Diese Inhaltsstoffe wirken nicht nur einzeln, sondern verstärken sich auch gegenseitig, um maximale Ergebnisse zu erzielen.
Die regelmäßige Einnahme von Reduslim in Verbindung mit einer ausgewogenen Ernährung und regelmäßiger Bewegung kann Ihnen helfen, das gewünschte Gewicht zu erreichen und zu halten. Es ist jedoch wichtig zu beachten, dass Nahrungsergänzungsmittel allein nicht ausreichen, um dauerhafte Ergebnisse zu erzielen. Es ist wichtig, gesunde Gewohnheiten zu pflegen und auf eine ausgewogene Ernährung sowie ausreichend Bewegung zu achten.
https://reduslim.at/
Många spelare har upplevt problem med att få ut sina vinster från Gogo Casino. Trots att de har vunnit stora summor pengar, har de mötts av olika ursäkter och fördröjningar när de försöker ta ut sina vinster. Det är tydligt att Gogo Casino inte lever upp till sina löften och spelarna känner sig lurade och frustrerade.
En del spelare har haft sina uttag blockerade av Gogo Casino med hänvisning till olika regler och villkor som spelarna inte tidigare hade kännedom om. Det verkar som att casinot gör allt för att undvika att betala ut vinster till sina spelare. Det är oacceptabelt och oschysst att behandla sina kunder på det här sättet.
Som spelare är det viktigt att vara medveten om vilka regler och villkor som gäller på det casino man spelar på. Men det är också casinots ansvar att tydligt kommunicera sina regler och att följa dem på ett ärligt sätt. Gogo Casino verkar tyvärr inte vara pålitligt och många spelare har blivit besvikna.
Om du har upplevt problem med att få ut dina vinster från Gogo Casino, rekommenderas att du kontaktar deras kundtjänst och begär en förklaring. Om de fortsätter att vara otydliga eller inte betalar ut dina vinster, kan det vara läge att överväga att spela på ett annat casino som är mer pålitligt och rättvist mot sina spelare. Man ska inte behöva kämpa för att få ut sina vinster, det ska vara en självklarhet när man vinner på ett casino.
https://gogocasino.one
Bonusar är en av de mest populära funktionerna på online casinon och Gogo Casino är inget undantag. Med sin bonus gogo casino belönar de sina spelare med generösa erbjudanden och kampanjer som gör spelandet ännu roligare.
En av de mest eftertraktade bonusarna på Gogo Casino är välkomstbonusen som erbjuds till nya spelare. Denna bonus ger spelarna möjlighet att dubbla sin första insättning och få extra pengar att spela för. Utöver välkomstbonusen erbjuder Gogo Casino även löpande kampanjer och bonusar till sina befintliga spelare för att belöna deras lojalitet.
För att ta del av bonusarna på Gogo Casino behöver spelarna endast registrera sig och göra en insättning på sitt spelkonto. Bonusarna krediteras automatiskt till spelarnas konton och kan användas på ett brett utbud av spel, inklusive slots, bordsspel och live casino.
Det är viktigt att notera att bonusar på Gogo Casino kommer med vissa villkor och krav som spelarna måste uppfylla för att kunna ta ut sina vinster. Dessa villkor kan inkludera omsättningskrav och tidsbegränsningar, så det är viktigt att läsa och förstå reglerna innan man tar del av bonusarna.
Sammanfattningsvis är bonusar på Gogo Casino en fantastisk möjlighet för spelare att öka sina vinstchanser och få en ännu bättre spelupplevelse. Med generösa erbjudanden och spännande kampanjer är det enkelt att se varför Gogo Casino är en favorit bland svenska spelare.
https://gogocasino.one
Das Zet Casino ist eine beliebte Online-Glücksspielplattform, die eine Vielzahl von Spielen und Unterhaltungsmöglichkeiten für Spieler bietet. Es verfügt über eine Lizenz der Malta Gaming Authority und wird von vielen Spielern auf der ganzen Welt genutzt.
Manchmal kann es vorkommen, dass Spieler das Bedürfnis verspüren, sich selbst zu schützen und ihr Spielverhalten zu kontrollieren. In solchen Fällen ist es ratsam, das Zet Casino zu sperren. Dies kann aus verschiedenen Gründen geschehen, wie etwa bei einem drohenden Suchtverhalten oder finanziellen Schwierigkeiten.
Um das Zet Casino zu sperren, kann man sich an den Kundenservice des Casinos wenden und um eine temporäre oder dauerhafte Sperrung bitten. Dabei sind in der Regel persönliche Identifikationsunterlagen erforderlich, um die Sperre zu bestätigen.
Die Sperrung des Zet Casinos bietet Spielern die Möglichkeit, ihr Spielverhalten zu reflektieren und gegebenenfalls professionelle Hilfe in Anspruch zu nehmen. Sie dient der eigenen Sicherheit und soll verantwortungsbewusstes Spielen fördern.
Es ist wichtig zu beachten, dass die Sperrung des Zet Casinos eine ernsthafte Entscheidung ist und gut überlegt sein sollte. Spieler sollten sich bewusst sein, dass nach einer Sperrung kein Zugriff mehr auf das Spielerkonto und die Spiele möglich ist.
Insgesamt bietet das Zet Casino eine verantwortungsbewusste Spiellösung für Spieler, die ihre Spielaktivitäten kontrollieren und einschränken möchten. Durch die Sperrung des Kontos können Spieler sich selbst schützen und ihr Wohlbefinden bewahren.
https://zetcasino.one/
top online pharmacy india: Healthcare and medicines from India – legitimate online pharmacies india
Det har rapporterats att vissa spelare upplever problem med att fГҐ sina vinster utbetalda frГҐn Gogo Casino. Detta har skapat oro och frustration bland mГҐnga spelare som har vunnit stora belopp pГҐ casinot.
Enligt flera spelare har de försökt kontakta kundtjänsten på Gogo Casino för att få sina vinster utbetalda, men har mötts av långa väntetider och bristfällig information. Det verkar som att casinot har svårt att hantera utbetalningar och att många spelare väntar i flera veckor på att få sina pengar.
Det är viktigt att komma ihåg att det finns regler och lagar som reglerar hur casinon ska hantera utbetalningar och det är viktigt att spelare känner sig trygga med att deras vinster kommer att betalas ut snabbt och korrekt.
Om du har upplevt problem med att få dina vinster utbetalda från Gogo Casino rekommenderas det att du kontaktar Spelinspektionen som är tillsynsmyndigheten för spel på nätet i Sverige. De kan hjälpa dig att få dina pengar och se till att casinot följer reglerna.
Det är viktigt att vara försiktig när man väljer ett online casino och att göra research innan man börjar spela. Se till att välja ett casino som är licensierat och reglerat för att undvika problem med utbetalningar i framtiden. Man ska också kontrollera recensioner och ryktet för casinot innan man sätter in sina pengar.
Sammanfattningsvis är det viktigt att vara medveten om eventuella problem med utbetalningar när man spelar på online casinon och att agera snabbt om man stöter på problem. Gogo Casino bör ta dessa rapporter på allvar och se till att spelarna får sina vinster utbetalda på ett korrekt och snabbt sätt.
https://gogocasino.one
Reduslim ist ein beliebtes Produkt zur Gewichtsreduktion, das positive Bewertungen erhält. Die Reduslim Recensioni zeigen, dass viele Menschen mit dem Ergebnis zufrieden sind. Die natürlichen Inhaltsstoffe helfen dabei, den Stoffwechsel zu beschleunigen und das Hungergefühl zu reduzieren. Die Kapseln sind einfach einzunehmen und können problemlos in den Alltag integriert werden. Wer also auf der Suche nach einem effektiven und sicheren Abnehmprodukt ist, sollte definitiv Reduslim eine Chance geben. Probieren Sie es aus und überzeugen Sie sich selbst von den positiven Ergebnissen!
https://reduslim.at/
hydroxyzine order – order generic nortriptyline 25 mg buy endep 10mg generic
Фильмок тв предлагает вашему вниманию самые лучшие фильмы. Вы можете в любое время смотреть их онлайн совершенно бесплатно. На странице любого фильма расписаны: страна, актерский состав, год, жанр, режиссер. Это позволяет принять о выборе кинокартины верное решение. https://filmok.tv – сайт, где имеется удобный поиск, воспользуйтесь им. Фильмы и сериалы ждут именно вас. Мы гарантируем отменный звук и картинку. Заходите прямо сейчас на наш портал, выбирайте подходящий фильм и наслаждайтесь им!
Som en viktig del av att erbjuda en förstklassig spelupplevelse för sina kunder, sätter Gogo Casino stort värde på kundsupporten. Kundsupporten på Gogo Casino är tillgänglig dygnet runt för att hjälpa spelare med alla frågor eller problem de kan ha.
På Gogo Casino finns det flera olika sätt att komma i kontakt med kundsupporten. Spelare kan antingen skicka ett e-postmeddelande, ringa eller använda livechatten direkt på webbplatsen för snabb och personlig service. Oavsett vilket sätt man väljer att kontakta supporten på, är kundtjänstteamet på Gogo Casino alltid där för att ge spelarna den hjälp de behöver.
Kundsupporten på Gogo Casino är känd för att vara professionell, vänlig och effektiv. Oavsett om spelare har frågor om insättningar och uttag, bonusar eller tekniska problem, kan de lita på att kundsupportteamet på Gogo Casino kommer att lösa deras problem snabbt och effektivt.
För att säkerställa att spelarna får den bästa möjliga supporten, genomgår kundtjänstteamet på Gogo Casino regelbunden utbildning för att hålla sig uppdaterade om de senaste trenderna och bästa praxis inom kundsupport. På det sättet kan de garantera att spelarna alltid får en högkvalitativ och professionell service varje gång de kontaktar kundsupporten på Gogo Casino.
I en bransch där kundtillfredsställelse är av högsta prioritet, gör Gogo Casino sitt bästa för att se till att deras spelare är nöjda och att deras behov och frågor behandlas med omsorg och professionalism. Med en dedikerad och professionell kundsupport är det enkelt att se varför Gogo Casino är en av de bästa alternativen för svenska spelare som letar efter en trygg och underhållande spelupplevelse på nätet.
https://gogocasino.one
Erleben Sie Spannung und Nervenkitzel im Zet Casino! Mit einer Vielzahl von Spielen und großartigen Gewinnchancen ist das Zet Casino die perfekte Wahl für alle, die gerne ihre Glück versuchen möchten.
Das Zet Casino bietet eine breite Auswahl an Spielen, darunter Slots, Tischspiele, Video Poker und vieles mehr. Die Website ist benutzerfreundlich gestaltet und ermöglicht es den Spielern, leicht durch die verschiedenen Spiele zu navigieren. Außerdem gibt es regelmäßige Aktionen und Boni, die den Spielern zusätzliche Gewinnchancen bieten.
Was das Zet Casino wirklich auszeichnet, ist die Erfahrung, die es den Spielern bietet. Mit hochwertiger Grafik und Soundeffekten fühlt es sich an, als wäre man in einem echten Casino. Die Live-Dealer-Spiele bieten eine interaktive und authentische Spielerfahrung, die es wirklich einzigartig macht.
Neben den Spielen bietet das Zet Casino auch einen hervorragenden Kundenservice. Das Support-Team ist rund um die Uhr erreichbar und steht den Spielern bei Fragen oder Problemen gerne zur Seite.
Insgesamt bietet das Zet Casino eine erstklassige Spielerfahrung, die alle Erwartungen Гјbertrifft. Probieren Sie es noch heute aus und erleben Sie den Nervenkitzel und die Aufregung von einem der besten Online-Casinos auf dem Markt.
https://zetcasino.one/
Bonusar är ett vanligt inslag i online casinovärlden, och Gogo Casino är inget undantag. Med sin bonus gogo casino erbjuder de spelare chansen att öka sina vinstchanser och få mer valuta för sina pengar.
En bonus på Gogo Casino kan ta form av exempelvis insättningsbonusar, free spins eller cashback. Insättningsbonusar innebär att spelaren får en extra summa pengar att spela för när de sätter in pengar på sitt spelkonto. Free spins ger spelaren möjligheten att rotera hjulen på spelautomater utan att satsa sina egna pengar. Cashback innebär att spelaren får tillbaka en del av sina förluster, vilket kan vara till stor tröst när turen inte är på ens sida.
För att ta del av bonus gogo casino behöver spelaren oftast uppfylla vissa krav, såsom att sätta in en viss summa pengar eller omsätta en viss summa på spelautomater. Det är viktigt att läsa villkoren noga för att förstå hur bonusen fungerar och vad som krävs för att kunna ta ut eventuella vinster.
Att utnyttja en bonus på Gogo Casino kan vara ett bra sätt att maximera sina vinstchanser och förlänga spelupplevelsen. Men det är också viktigt att spela ansvarsfullt och inte låta bonusar locka till överdrivet spelande. Kom ihåg att spel ska vara underhållande och att vinst aldrig är garanterad.
Sammanfattningsvis kan en bonus gogo casino vara en spännande möjlighet för spelare att öka sina vinstchanser och få mer valuta för sina pengar. Genom att läsa villkoren noga och spela ansvarsfullt kan man ha en givande och underhållande spelupplevelse på Gogo Casino.
https://gogocasino.one
medication from mexico pharmacy: Online Pharmacies in Mexico – best online pharmacies in mexico
brand hydroxyzine – buy nortriptyline generic cheap endep 10mg
Gogo Casino är ett onlinecasino som erbjuder sina spelare möjligheten att spela utan att behöva göra en insättning. Detta kallas för en no deposit bonus och innebär att spelarna kan prova på casinots spel utan att riskera sina egna pengar.
För att ta del av denna bonus behöver spelaren endast skapa ett konto på Gogo Casino och verifiera sin identitet. Sedan kan man börja spela och utforska det stora utbud av spel som erbjuds på casinot. Det är ett utmärkt sätt för spelare att testa casinot och se om det passar ens individuella spelstil innan man bestämmer sig för att göra en insättning.
No deposit bonusar är särskilt populära bland nya spelare som vill prova på olika casinon innan de bestämmer sig för vilket de vill fortsätta spela på. Det är också ett bra sätt för casinon att locka till sig nya spelare och visa upp sitt spelutbud.
Gogo Casino har ett brett utbud av spelautomater, bordsspel och livecasino-spel att välja mellan. Oavsett om man föredrar klassiska spelautomater, spännande bordsspel som blackjack och roulette eller vill uppleva spänningen i ett livecasino, finns det något för alla på Gogo Casino.
Så om du är sugen på att prova lyckan utan att riskera dina egna pengar, är Gogo Casino no deposit bonus definitivt värt att testa. Skapa ett konto idag och börja spela!
https://gogocasino.one
Gogo Casino är en av de nya casinona på marknaden som snabbt har blivit populärt bland svenska spelare. Men vem äger egentligen Gogo Casino?
Gogo Casino ägs av det maltesiska företaget Viral Interactive Limited. Viral Interactive Limited är ett företag som specialiserar sig inom iGaming-branschen och de har flera framgångsrika casinon under sitt tak.
Genom att ägas av Viral Interactive Limited innebär det att Gogo Casino är licensierat och reglerat av Malta Gaming Authority. Detta innebär att casinot följer strikta regler och riktlinjer för att säkerställa en säker och rättvis spelupplevelse för spelarna.
Även om Gogo Casino ägs av ett utländskt företag, är deras fokus tydligt på den svenska marknaden. Casinot erbjuder ett brett utbud av spel från ledande spelleverantörer, snabba utbetalningar och en kundtjänst på svenska.
Allt som allt, Gogo Casino ägs av Viral Interactive Limited och är ett pålitligt och populärt casino bland svenska spelare. Med en licens från Malta Gaming Authority kan spelare känna sig trygga med att deras spelupplevelse är säker och rättvis.
https://gogocasino.one
Reduslim funziona davvero, das ist die Frage, die sich viele Menschen stellen, die nach einer effektiven Methode suchen, um Gewicht zu verlieren. Dieses natürliche Nahrungsergänzungsmittel hat in der letzten Zeit viel Aufmerksamkeit erregt, da es angeblich dabei helfen kann, den Stoffwechsel zu steigern und die Fettverbrennung zu beschleunigen.
Der Hauptbestandteil von Reduslim ist die Garcinia Cambogia Frucht, die dafür bekannt ist, die Fettproduktion im Körper zu hemmen und das Verlangen nach Nahrung zu reduzieren. Die positiven Erfahrungsberichte von zufriedenen Kunden sprechen für sich und viele schwören auf die Wirkung dieses Supplements.
Natürlich ist es wichtig, auch gesunde Ernährungsgewohnheiten zu pflegen und regelmäßig Sport zu treiben, um langfristige Erfolge zu erzielen. Reduslim kann dabei eine unterstützende Rolle spielen und den Prozess des Abnehmens beschleunigen.
Alles in allem scheint es, dass Reduslim wirklich funktioniert und vielen Menschen geholfen hat, ihr Wunschgewicht zu erreichen. Es lohnt sich also, dieses Produkt auszuprobieren und zu sehen, ob es auch fГјr dich funktioniert.
https://reduslim.at/
online canadian pharmacy reviews Large Selection of Medications online canadian pharmacy reviews
Gogo Casino är ett populärt online casino som erbjuder spelare en rad olika möjligheter att vinna stora vinster. När det gäller att göra uttag från ditt spelkonto hos Gogo Casino finns det flera alternativ att välja mellan.
Ditt uttag kan behandlas antingen med banköverföring eller med hjälp av olika e-plånböcker. Banköverföring kan ta upp till 5 bankdagar att behandlas medan uttag med e-plånböcker som Skrill och Neteller ofta sker nästan omedelbart.
För att göra ett uttag behöver du först logga in på ditt spelkonto på Gogo Casino och gå till sektionen för uttag. Här kan du välja det belopp du önskar ta ut samt vilken metod du föredrar för ditt uttag.
När du har gjort ditt val och bekräftat din begäran kommer Gogo Casino att behandla din förfrågan så snart som möjligt och överföra pengarna till ditt konto. Tänk på att det kan vara vissa begränsningar när det gäller minsta och högsta belopp för uttag samt eventuella avgifter som kan tillkomma.
Sammanfattningsvis gör Gogo Casino uttag enkelt och smidigt för sina spelare med flera olika alternativ att välja mellan. Så om du har haft turen att vinna stort på detta online casino kan du vara säker på att dina vinster kommer att betalas ut till dig på ett säkert och effektivt sätt.
https://gogocasino.one
Boomerang Casino Vedonlyönti: Alles, was Sie wissen müssen
Boomerang Casino Vedonlyönti ist ein aufregender neuer Trend in der Welt des Online-Glücksspiels. Mit einer Vielzahl von Spielen und Wettmöglichkeiten bietet Boomerang Casino Vedonlyönti seinen Spielern die Möglichkeit, Geld zu gewinnen und gleichzeitig Spaß zu haben.
Das Online-Casino bietet eine Vielzahl von Wettoptionen für Spieler aller Erfahrungsstufen. Von traditionellen Casino-Spielen wie Blackjack und Roulette bis hin zu modernen Spielautomaten und Live-Casino-Spielen, gibt es für jeden etwas zu entdecken. Die große Auswahl an Spielen sorgt dafür, dass Spieler nie gelangweilt werden und immer etwas Neues ausprobieren können.
Ein weiterer Vorteil von Boomerang Casino Vedonlyönti ist die Möglichkeit, von überall aus zu spielen. Mit einer einfach zu bedienenden mobilen App können Spieler ihre Lieblingsspiele unterwegs genießen, ohne auf einen Computer zugreifen zu müssen. Dies ermöglicht es Spielern, jederzeit und überall zu spielen, ganz nach ihren eigenen Vorlieben.
Darüber hinaus bietet Boomerang Casino Vedonlyönti großzügige Boni und Werbeaktionen für seine Spieler. Neue Spieler erhalten oft Willkommensboni bei ihrer ersten Einzahlung, und regelmäßige Spieler können von Treueprämien und Cashback-Angeboten profitieren. Diese Boni helfen Spielern, ihr Guthaben zu erhöhen und längere Spielsitzungen zu genießen.
Insgesamt ist Boomerang Casino Vedonlyönti eine spannende und unterhaltsame Möglichkeit, Geld zu gewinnen und gleichzeitig Spaß zu haben. Mit einer Vielzahl von Spielen, mobilen Optionen und großzügigen Boni ist dieses Online-Casino eine gute Wahl für Spieler aller Art. Probieren Sie es heute aus und erleben Sie selbst die aufregende Welt von Boomerang Casino Vedonlyönti. Viel Glück beim Spielen!
https://boomerangcasino.one/
Zet Casino Auszahlung funktioniert nicht
Das Zet Casino ist ein beliebtes Online-Casino, das seinen Kunden eine Vielzahl von Spielen und MГ¶glichkeiten zum Spielen bietet. Doch was passiert, wenn es bei der Auszahlung von Gewinnen Probleme gibt? In diesem Artikel werden wir uns mit dem Thema “Zet Casino Auszahlung funktioniert nicht” befassen und mГ¶gliche LГ¶sungen fГјr dieses Problem aufzeigen.
Es kann verschiedene Gründe geben, warum die Auszahlung im Zet Casino nicht funktioniert. Einer der häufigsten Gründe ist, dass die Kunden die Bonusbedingungen nicht erfüllt haben. Oftmals müssen bestimmte Umsatzbedingungen erfüllt werden, bevor eine Auszahlung möglich ist. Es ist daher wichtig, dass die Spieler die Geschäftsbedingungen des Casinos genau kennen und beachten.
Ein weiterer Grund für Probleme bei der Auszahlung könnte sein, dass das Konto der Spieler nicht verifiziert ist. In einigen Fällen kann das Casino zusätzliche Dokumente verlangen, um die Identität des Spielers zu überprüfen und sicherzustellen, dass die Auszahlung an die richtige Person erfolgt. Es ist ratsam, diese Verifizierungsprozesse rechtzeitig durchzuführen, um Verzögerungen bei der Auszahlung zu vermeiden.
Wenn trotz Erfüllung der Bonusbedingungen und Verifizierung des Kontos die Auszahlung immer noch nicht funktioniert, kann es sinnvoll sein, den Kundendienst des Zet Casinos zu kontaktieren. Die Mitarbeiter des Kundenservice stehen den Spielern in der Regel rund um die Uhr zur Verfügung und können bei Problemen und Fragen weiterhelfen.
Insgesamt ist es wichtig, dass die Spieler die Regeln und Bedingungen des Zet Casinos kennen und einhalten, um reibungslose Auszahlungen zu gewährleisten. Sollte es dennoch zu Problemen kommen, ist der Kontakt zum Kundenservice der erste Schritt, um das Problem zu lösen.
Abschließend lässt sich sagen, dass das Zet Casino ein seriöser Anbieter ist, der großen Wert auf Transparenz und Kundenzufriedenheit legt. Mit etwas Geduld und Kommunikation lassen sich eventuelle Schwierigkeiten bei der Auszahlung in der Regel schnell und unkompliziert lösen.
https://zetcasino.one/
canadapharmacyonline legit: Large Selection of Medications – canadian pharmacy service
Gogo Casino är en populär onlinekasinoplattform som erbjuder ett brett utbud av spel för sina kunder. Men vem äger egentligen Gogo Casino?
Gogo Casino ägs och drivs av det maltesiska företaget Viral Interactive Limited. Företaget lanserade plattformen 2019 och har sedan dess blivit populär bland spelare från hela världen.
Viral Interactive Limited har ett gott rykte inom casinobranschen och är licensierat av Malta Gaming Authority, vilket innebär att de följer strikta regler och föreskrifter för att säkerställa en rättvis och säker spelupplevelse för sina användare.
Förutom att äga Gogo Casino driver Viral Interactive Limited också flera andra framgångsrika onlinekasinon och spelplattformar. Företaget strävar efter att erbjuda högkvalitativa spel och en användarvänlig plattform för alla sina kunder.
I slutändan är det alltid viktigt för spelare att vara medvetna om vem som äger och driver de onlinekasinon de väljer att spela på. Genom att välja en pålitlig och ansedd operatör som Viral Interactive Limited kan spelare känna sig trygga i att de kommer att få en säker och rättvis spelupplevelse på Gogo Casino.
https://gogocasino.one
Gogo Casino är en populär online-spelplattform som erbjuder ett brett utbud av casinospel för sina spelare. För att säkerställa en smidig spelupplevelse för sina kunder har de en dedikerad kundtjänst som är tillgänglig för att hjälpa till med alla frågor eller problem som kan uppstå.
Gogo Casino kundtjänst är tillgänglig dygnet runt, alla dagar i veckan, för att hjälpa spelare med alla sina behov. Oavsett om det gäller att svara på frågor om spelregler, hantera insättningar och uttag eller lösa tekniska problem, finns det alltid någon tillgänglig för att hjälpa till.
Kundtjänsten på Gogo Casino är välutbildad och kunnig inom alla aspekter av casinospel, vilket innebär att spelarna kan känna sig trygga i att de får den bästa möjliga hjälpen. Genom att erbjuda snabba svar och effektiv service strävar Gogo Casino efter att ge sina kunder den bästa möjliga spelupplevelsen.
För att komma i kontakt med Gogo Casino kundtjänst kan spelare antingen använda livechatten på deras hemsida, skicka ett mejl eller ringa deras telefonsupport. Oavsett vilken metod som används kan spelare vara säkra på att de kommer att få den hjälp de behöver för att njuta av sitt spelande på Gogo Casino.
https://gogocasino.one
Gogo Casino Email
Gogo Casino är ett populärt online casino som erbjuder ett brett utbud av spel och generösa bonusar till sina spelare. För att hålla sina kunder informerade om de senaste erbjudandena och kampanjerna, skickar Gogo Casino regelbundet ut e-postmeddelanden till sina registrerade medlemmar.
Genom att prenumerera på Gogo Casinos e-postlista kan spelarna få exklusiva erbjudanden, bonusar och nyheter direkt i sin inkorg. Meddelandena kan inkludera allt från free spins och insättningsbonusar till information om kommande turneringar och tävlingar.
Det är enkelt att registrera sig för Gogo Casinos e-postlista. Besök bara deras webbplats och fyll i dina uppgifter för att bli en del av deras e-postutskick. Du kan också välja att inte ta emot e-postmeddelanden genom att avmarkera den relevanta rutan vid registreringen.
Genom att prenumerera på Gogo Casinos e-postlista kan du hålla dig uppdaterad om de senaste kampanjerna och erbjudandena. Missa inte chansen att vinna stora priser och få bonusar genom att hålla ett öga på din inkorg för de senaste e-postmeddelandena från Gogo Casino. Lycka till!
https://gogocasino.one
https://canadianpharmacy24.store/# canadian pharmacy online
india online pharmacy: indian pharmacy – pharmacy website india
Gogo Casino är ett populärt online casino som har blivit känt för sin transparens och öppenhet gentemot sina spelare. Med en tydlig och lättanvänd plattform har Gogo Casino skapat en trygg och säker spelmiljö för alla sina användare.
En av de största fördelarna med Gogo Casino är deras transparenta kommunikation kring bonusar och villkor. Istället för att dölja information eller använda komplicerade regler och krav, är allt som rör bonusar och kampanjer tydligt angivet på webbplatsen. Det gör det enkelt för spelare att förstå vad de kan förvänta sig och vilka regler som gäller.
Förutom transparens när det gäller bonusar är Gogo Casino också öppna med sin licens och reglering. De innehar en svensk spellicens, vilket innebär att de följer strikta regler och riktlinjer för att säkerställa en rättvis och ansvarsfull spelupplevelse för sina spelare. Dessutom erbjuder de snabba och säkra betalningsmetoder för insättningar och uttag.
Gogo Casino strävar efter att vara en pålitlig och transparent aktör inom spelbranschen. Genom att erbjuda en säker och rättvis spelmiljö samt vara öppna med sin verksamhet, har de lyckats skapa en lojal kundkrets som uppskattar deras transparens och professionalism. Så om du letar efter ett pålitligt och transparent online casino, är Gogo Casino definitivt värt att prova!
https://gogocasino.one
Tipico: Vom Casino zu Sportwetten
Tipico ist ein bekannter Anbieter von Glücksspiel und Sportwetten, der sowohl online als auch in stationären Wettbüros aktiv ist. Viele Menschen kennen Tipico vor allem durch sein Online-Casino, das eine Vielzahl von Spielen wie Slots, Roulette und Blackjack anbietet. Doch in den letzten Jahren hat sich Tipico verstärkt auf den Bereich Sportwetten fokussiert und sein Angebot ausgebaut.
Sportwetten erfreuen sich großer Beliebtheit, sowohl bei erfahrenen Spielern als auch bei Anfängern. Tipico bietet hier ein breites Spektrum an Wettmöglichkeiten für verschiedene Sportarten wie Fußball, Tennis, Basketball und Eishockey an. Die Plattform ist benutzerfreundlich gestaltet und ermöglicht es den Nutzern, schnell und einfach ihre Wetten abzugeben und zu verfolgen.
Im Vergleich zum Casino bietet das Wetten auf Sportereignisse eine andere Art von Spannung und Nervenkitzel. Es geht nicht nur um Glück, sondern auch um Wissen und Analyse der Sportarten und Teams. Durch die richtige Strategie und Informationen können die Spieler ihre Gewinnchancen erheblich steigern.
Tipico bietet zudem attraktive Boni und Promotionen für Sportwetten an, um die Spieler zu belohnen und zu motivieren. Die Plattform ist sicher und zuverlässig, sodass die Nutzer sich keine Sorgen um ihre persönlichen Daten oder Gewinne machen müssen.
Insgesamt zeigt die Entwicklung von Tipico vom Casino zu Sportwetten, dass das Unternehmen flexibel und innovativ ist und auf die Bedürfnisse und Wünsche der Spieler eingeht. Mit seinem breiten Angebot und seiner Professionalität hat sich Tipico zu einem der führenden Anbieter in der Glücksspielbranche etabliert. Wer Lust auf spannende Sportwetten hat, sollte einen Blick auf Tipico werfen und sein Glück versuchen.
https://tipicocasino.one/
Das Boomerang Casino Blink ist ein aufregendes neues Online-Casino, das Spielern eine Vielzahl von hochwertigen Spielen und großzügigen Boni bietet. Das Casino verfügt über eine benutzerfreundliche Oberfläche, die es einfach macht, durch die verschiedenen Spiele und Funktionen zu navigieren.
Das Boomerang Casino Blink bietet eine große Auswahl an Spielautomaten, Tischspielen und Live-Casino-Spielen. Die Spielautomaten reichen von klassischen Fruchtmaschinen bis hin zu modernen Video-Slots mit aufregenden Bonusspielen und Sonderfunktionen. Die Tischspiele umfassen beliebte Klassiker wie Roulette, Blackjack und Baccarat, die in verschiedenen Varianten gespielt werden können. Die Live-Casino-Spiele bieten den Spielern die Möglichkeit, gegen echte Dealer anzutreten und das Casino-Erlebnis noch realistischer zu gestalten.
Neben den spannenden Spielen bietet das Boomerang Casino Blink seinen Spielern auch großzügige Boni und Promotionen. Neue Spieler können von einem Willkommensbonus profitieren, der ihnen zusätzliches Guthaben und Freispiele für ausgewählte Spiele bietet. Darüber hinaus gibt es regelmäßig wechselnde Aktionen, bei denen die Spieler weitere Boni und Belohnungen erhalten können.
Das Casino verfügt über eine sichere und zuverlässige Lizenzierung, die den Spielern ein faires und geschütztes Spielerlebnis garantiert. Die Transaktionen werden über sichere Zahlungsmethoden abgewickelt, sodass die Spieler ihre Ein- und Auszahlungen bequem und sicher durchführen können.
Insgesamt ist das Boomerang Casino Blink eine hervorragende Wahl für Spieler, die auf der Suche nach einem unterhaltsamen und sicheren Online-Casino-Erlebnis sind. Mit seiner großen Auswahl an Spielen, großzügigen Boni und zuverlässigen Sicherheitsmaßnahmen ist das Casino definitiv einen Besuch wert. Besuchen Sie das Boomerang Casino Blink noch heute und tauchen Sie ein in die Welt des Online-Glücksspiels.
https://boomerangcasino.one/
Zet Casino Einzahlungsbonus
Das Zet Casino bietet seinen Spielern eine Vielzahl von attraktiven Bonusangeboten, darunter auch einen groГџzГјgigen Einzahlungsbonus. Doch was genau verbirgt sich hinter diesem Angebot und welche Vorteile bietet es den Spielern?
Der Einzahlungsbonus im Zet Casino richtet sich in erster Linie an neue Spieler, die sich erstmalig auf der Plattform registrieren und eine Einzahlung tätigen. Dabei handelt es sich um einen Willkommensbonus, der den Spielern zusätzliches Guthaben verschafft, um ihre Lieblingsspiele im Casino zu spielen und echtes Geld zu gewinnen.
Der Einzahlungsbonus im Zet Casino kann auf verschiedene Arten gestaltet sein. Oftmals handelt es sich um einen Prozentsatz der Einzahlungssumme, der als Bonus gutgeschrieben wird. Zum Beispiel könnte der Einzahlungsbonus 100% betragen, was bedeutet, dass Spieler ihre Einzahlung verdoppeln können. Neben dem Einzahlungsbonus bieten viele Casinos auch Freispiele oder andere Boni als zusätzliche Anreize.
Der Einzahlungsbonus im Zet Casino ist eine großartige Möglichkeit für Spieler, ihr Spielkapital zu erhöhen und ihre Gewinnchancen zu maximieren. Durch den Bonus können Spieler länger spielen und mehr Spiele ausprobieren, ohne dabei ihr eigenes Geld zu riskieren. Zudem bietet der Einzahlungsbonus die Möglichkeit, neue Spiele und Funktionen des Casinos kennenzulernen und so das Spielerlebnis zu verbessern.
Um den Einzahlungsbonus im Zet Casino in Anspruch zu nehmen, müssen Spieler in der Regel eine Mindesteinzahlung tätigen und bestimmte Umsatzbedingungen erfüllen. Diese Bedingungen können von Casino zu Casino variieren und sollten daher vor der Einzahlung sorgfältig geprüft werden.
Insgesamt ist der Einzahlungsbonus im Zet Casino eine attraktive Möglichkeit für neue Spieler, um ihr Spielerlebnis zu optimieren und gleichzeitig ihre Gewinnchancen zu erhöhen. Mit dem zusätzlichen Bonusguthaben können Spieler mehr Spaß haben und womöglich auch größere Gewinne erzielen.
https://zetcasino.one/
Gogo casino uttag flashback
Gogo Casino är ett populärt online casino där spelare kan njuta av en rad olika spel och slots. En viktig del av att spela på ett online casino är att kunna göra uttag smidigt och säkert. Ett vanligt ämne som diskuteras bland spelare är gogo casino uttag flashback.
Det finns många olika sätt att göra uttag på Gogo Casino, inklusive banköverföringar, e-plånböcker och kreditkort. Processen för att göra ett uttag kan variera beroende på vilken metod du väljer. Vissa metoder kan vara snabbare än andra, medan vissa kan ta lite längre tid att behandla.
Många spelare har delat sina erfarenheter av att göra uttag på Gogo Casino i olika forum och diskussioner på nätet. Det är alltid bra att läsa recensioner och feedback från andra spelare för att få en bättre förståelse för hur uttagsprocessen fungerar.
För att göra ett uttag på Gogo Casino måste du vanligtvis ange dina personuppgifter och välja en lämplig betalningsmetod. Vissa metoder kan kräva att du verifierar ditt konto genom att skicka in dokument som bevis på din identitet.
Det är viktigt att komma ihåg att det kan finnas vissa begränsningar och avgifter för uttag på Gogo Casino, så se till att läsa igenom villkoren och reglerna noggrant innan du gör ett uttag.
I slutändan är Gogo Casino ett pålitligt och säkert online casino där spelare kan njuta av en bra spelupplevelse. Genom att vara medveten om hur uttagsprocessen fungerar och läsa recensioner från andra spelare kan du göra uttag på ett smidigt och problemfritt sätt. Så var inte rädd för att prova lyckan på Gogo Casino och njut av spänningen i att spela online!
https://gogocasino.one
Sara Carbonero ist eine bekannte spanische Journalistin und Moderatorin, die fГјr ihre SchГ¶nheit und Eleganz bekannt ist. In den letzten Jahren wurde sie oft wegen ihrer Figur bewundert, doch sie hat zugegeben, dass nach der Geburt ihres zweiten Kindes, sie ein paar Extra-Pfund zugenommen hatte. Doch Sara Carbonero hat mit Hilfe des neuen Produkts “Reduslim” ihr Idealgewicht erreicht.
Reduslim ist ein neues Nahrungsergänzungsmittel, das auf natürliche Weise den Stoffwechsel anregt und die Fettverbrennung steigert. Sara Carbonero schwört auf die Wirkung dieser Pillen und sagt, dass sie ihr geholfen haben, schnell und effektiv abzunehmen. Nach nur wenigen Wochen konnte sie wieder in ihre alten Lieblingskleider passen und fühlte sich wieder wohl in ihrer Haut.
Auch viele andere Frauen haben bereits positive Erfahrungen mit Reduslim gemacht und sind begeistert von den Ergebnissen. Wenn auch du auf der Suche nach einer einfachen und effektiven Methode bist, um abzunehmen, dann ist Reduslim vielleicht genau das Richtige fГјr dich. Nutze die Gelegenheit und probiere es selbst aus. GГ¶nn dir das gleiche GefГјhl der Zufriedenheit und des Stolzes wie Sara Carbonero – mit Reduslim.
https://reduslim.at/
india pharmacy indian pharmacy delivery india online pharmacy
buy canadian drugs: Licensed Canadian Pharmacy – canadian online drugstore
Gogo Casino Support
Gogo Casino är en populär online casino i Sverige som erbjuder en mängd olika spel och kampanjer för sina spelare. För att säkerställa en positiv upplevelse för sina kunder, erbjuder Gogo Casino också en snabb och effektiv kundsupport.
Kundsupportteamet på Gogo Casino är tillgängligt via livechatt och e-post för att hjälpa spelare med eventuella frågor eller problem de kan ha. Livechatten är öppen dygnet runt för att svara på frågor i realtid och lösa problem omedelbart. Kundsupportteamet är välutbildade och kunniga om casinots olika spel och funktioner, vilket gör det enkelt för spelare att få den hjälp de behöver.
Utöver livechatt och e-post, erbjuder Gogo Casino även en omfattande FAQ-sektion där spelare kan hitta svar på vanliga frågor om registrering, insättningar och uttag, spelregler och mycket mer. Den här resursen är användbar för spelare som föredrar att söka svaren själva innan de kontaktar kundsupport.
Gogo Casino tar kundsupport på allvar och strävar efter att ge spelare den bästa möjliga spelupplevelsen. Genom att erbjuda en tillgänglig och kunnig kundsupport, kan spelare känna sig trygga med att deras frågor och problem kommer att lösas på ett snabbt och effektivt sätt. Med en stark och pålitlig kundsupport kan spelare hos Gogo Casino fokusera på att njuta av sina favoritspel utan att oroa sig för tekniska problem eller frågor.
https://gogocasino.one
mexican pharmaceuticals online: Mexican Pharmacy Online – buying from online mexican pharmacy
Gogo casino com är en spännande online spelsajt som erbjuder en rad olika casinospel för sina spelare. Med ett stort utbud av spelautomater, bordsspel och live casino spel, finns det något för alla typer av spelare att njuta av.
En av de fördelar med gogo casino com är att det är tillgängligt dygnet runt, vilket gör det möjligt för spelare att spela sina favoritspel när det passar dem bäst. Sajten är också lätt att navigera och erbjuder en säker och pålitlig spelupplevelse.
Förutom det breda spelutbudet och tillgängligheten är gogo casino com också känt för sina generösa bonusar och kampanjer. Spelare kan ta del av välkomstbonusar, gratis spins och andra belöningar som ökar deras chanser att vinna stort.
Som en ledande aktör inom online casinobranschen, strävar gogo casino com ständigt efter att förbättra och utveckla sin plattform för att ge spelare den bästa möjliga spelupplevelsen. Med en dedikerad kundsupport och säkra betalningsmetoder kan spelare känna sig trygga och väl omhändertagna när de spelar på sajten.
Sammanfattningsvis är gogo casino com en populär och pålitlig online spelsajt som erbjuder en rad spännande spel och generösa bonusar. Oavsett om du är en erfaren spelare eller nybörjare, finns det något för alla att utforska och njuta av på gogo casino com. Besök sajten idag och se själv vad den har att erbjuda!
https://gogocasino.one
Gogo Casino är ett online casino som erbjuder sina spelare möjligheten att spela en rad olika casinospel direkt i webbläsaren. Ett av de viktigaste fördelarna med att spela på Gogo Casino är deras smidiga och snabba utbetalningsprocess.
När det är dags att ta ut dina vinster från Gogo Casino kan du vara säker på att processen kommer att vara enkel och effektiv. För att begära en utbetalning behöver du bara gå till ditt spelkonto och välja önskat utbetalningssätt. Gogo Casino erbjuder flera olika alternativ för utbetalningar, inklusive banköverföring, e-plånbok och Trustly.
En av de största fördelarna med att använda Trustly för utbetalningar är att pengarna vanligtvis når ditt konto inom några minuter efter att du begärt uttaget. Detta är betydligt snabbare än många andra casinon på marknaden, där det kan ta upp till flera dagar innan pengarna når ditt konto.
För att säkerställa att utbetalningen går smidigt och snabbt är det viktigt att du har verifierat ditt spelkonto hos Gogo Casino. Detta innebär att du kan behöva skicka in dokument som bevisar din identitet och hemadress. Detta kan vara något irriterande, men det är också ett viktigt steg för att säkerställa att dina pengar hamnar på rätt plats.
Sammanfattningsvis kan man säga att Gogo Casino erbjuder en snabb och effektiv utbetalningsprocess för sina spelare. Med flera olika utbetalningsalternativ att välja mellan och snabba transaktioner med Trustly, kan du vara säker på att dina vinster når dig på nolltid. Så om du är ute efter en bra utbetalningsupplevelse, är Gogo Casino definitivt ett bra val.
https://gogocasino.one
Das Boomerang Casino Poker ist ein spannendes und beliebtes Kartenspiel, das in vielen Casinos weltweit gespielt wird. Es ist eine Variation des traditionellen Pokerspiels und bietet den Spielern eine aufregende und unterhaltsame Erfahrung.
Das Besondere am Boomerang Casino Poker ist, dass die Spieler die MГ¶glichkeit haben, ihre Gewinne zu “verdoppeln” oder “zurГјckzuziehen”. Dies bedeutet, dass sie die Option haben, einen Teil ihres Gewinns zu behalten und den Rest zu setzen, um die Chance zu haben, noch mehr zu gewinnen.
Das Spiel wird mit einem Standardkartenspiel gespielt und die Regeln sind ähnlich wie beim traditionellen Poker. Die Spieler müssen die besten Pokerhände bilden, um zu gewinnen. Es gibt verschiedene Wetten, die die Spieler platzieren können, um ihr Glück zu versuchen und große Gewinne zu erzielen.
Das Boomerang Casino Poker bietet Spaß und Spannung für Spieler aller Erfahrungsstufen. Es ist ein faszinierendes Spiel, das Geschicklichkeit und Strategie erfordert, um erfolgreich zu sein. Die Spieler müssen ihre Fähigkeiten und ihr Glück auf die Probe stellen, um am Ende als Gewinner hervorzugehen.
In vielen Casinos weltweit können die Spieler das Boomerang Casino Poker spielen und die Chance haben, große Preise zu gewinnen. Es ist ein aufregendes Spiel, das die Spieler stundenlang unterhalten kann. Also, warum nicht Ihr Glück versuchen und sehen, ob Sie der nächste große Gewinner im Boomerang Casino Poker werden können?
https://boomerangcasino.one/
Gogo Casino är en populär online spelplattform som erbjuder spelare möjligheten att njuta av en mängd olika casinospel. För att locka nya spelare och belöna sina lojala kunder erbjuder Gogo Casino regelbundet olika typer av bonusar.
En av de mest eftertraktade bonusarna på Gogo Casino är välkomstbonusen för nya spelare. Genom att registrera sig på plattformen och göra en första insättning kan spelare få en generös bonus som ökar deras chanser att vinna stort. Denna bonus kan användas för att spela olika spel på casinot och utforska olika möjligheter att vinna.
För de som redan är registrerade på Gogo Casino erbjuds också lojalitetsbonusar och kampanjer regelbundet. Dessa kan inkludera gratissnurr på utvalda spelautomater, bonuspengar att spela med eller till och med speciella tävlingar och turneringar där spelare kan vinna fantastiska priser.
Det är viktigt att komma ihåg att alla bonusar på Gogo Casino kommer med vissa villkor och regler som måste följas. Det är därför viktigt att läsa igenom bonusvillkoren noggrant innan du accepterar en bonus för att undvika eventuella missförstånd eller problem.
Sammanfattningsvis erbjuder Gogo Casino en rad spännande bonusar för sina spelare, som kan hjälpa dem att öka sina vinstchanser och njuta av en ännu mer spännande spelupplevelse. Genom att dra nytta av dessa bonusar kan spelare maximera sin potential att vinna stort och ha roligt samtidigt. Så varför inte prova lyckan på Gogo Casino idag och se vilka spännande bonusar som väntar på dig? Lycka till!
https://gogocasino.one
Zet Casino Geld zurГјckfordern
In der Welt der Online-Glücksspiele kann es vorkommen, dass Spieler Schwierigkeiten haben, ihr Geld zurückzufordern. Dies kann verschiedene Gründe haben, wie etwa technische Probleme, fehlerhafte Transaktionen oder Streitigkeiten mit dem Casino-Anbieter. In solchen Fällen ist es wichtig, als Spieler die richtigen Schritte zu unternehmen, um sein Geld zurückzufordern.
Eines der Casinos, bei dem Spieler auf solche Probleme stoßen können, ist das Zet Casino. Obwohl es sich um ein beliebtes Online-Casino handelt, kann es vorkommen, dass Spieler Schwierigkeiten haben, ihr Geld zurückzufordern. Dies kann frustrierend sein, insbesondere wenn es sich um größere Summen handelt.
Wenn Sie also Schwierigkeiten haben, Ihr Geld vom Zet Casino zurückzufordern, gibt es einige Schritte, die Sie unternehmen können. Zunächst sollten Sie Kontakt mit dem Kundenservice des Casinos aufnehmen und das Problem schildern. Oftmals können die Mitarbeiter des Casinos Ihnen weiterhelfen und das Problem lösen.
Wenn der Kundenservice des Zet Casinos nicht weiterhelfen kann, können Sie sich auch an die Glücksspielbehörde wenden, die das Casino reguliert. Diese Behörde kann Ihnen dabei helfen, Ihr Geld zurückzufordern und das Problem mit dem Casino-Anbieter zu lösen.
Es ist wichtig, dass Sie als Spieler Ihre Rechte kennen und darauf bestehen, dass Ihnen Ihr Geld zurückgezahlt wird, wenn es Ihnen rechtmäßig zusteht. Wenn Sie also Schwierigkeiten haben, Ihr Geld vom Zet Casino zurückzufordern, sollten Sie die oben genannten Schritte unternehmen, um Ihr Geld zurückzuerlangen.
Insgesamt ist es wichtig, als Spieler immer wachsam zu sein und darauf zu achten, dass Ihre Einlagen und Gewinne sicher sind. Wenn Sie Probleme haben, Ihr Geld vom Zet Casino zurückzufordern, zögern Sie nicht, die oben genannten Schritte zu unternehmen und Ihr Geld zurückzuholen.
https://zetcasino.one/
Reduslim ist ein beliebtes Nahrungsergänzungsmittel, das oft in Minsan Farmacia erhältlich ist. Es wird oft als natürliche Lösung zur Gewichtsabnahme beworben. Reduslim enthält eine spezielle Formel aus natürlichen Zutaten, die den Stoffwechsel anregen und die Fettverbrennung unterstützen sollen.
Viele Menschen schwören auf die Wirkung von Reduslim und berichten von beeindruckenden Ergebnissen. Die Kapseln sollen dabei helfen, den Appetit zu reduzieren und das Verlangen nach ungesunden Snacks zu unterdrücken. Zudem sollen sie den Körper dabei unterstützen, überschüssiges Fett zu verbrennen und die Gewichtsabnahme zu beschleunigen.
Es ist wichtig zu beachten, dass Reduslim nicht als Wundermittel angesehen werden sollte und ein gesunder Lebensstil essentiell für den Erfolg einer Gewichtsabnahme ist. Regelmäßige Bewegung und eine ausgewogene Ernährung sind entscheidend, um langfristig Erfolge zu erzielen.
Wer jedoch auf der Suche nach einer natГјrlichen UnterstГјtzung bei der Gewichtsabnahme ist, sollte Reduslim eine Chance geben. Besuchen Sie Minsan Farmacia und lassen Sie sich von einem Fachmann beraten, ob Reduslim das richtige Produkt fГјr Sie ist.
https://reduslim.at/
canadian pharmacy online reviews: canadian pharmacies – safe canadian pharmacies
Gogo casino är en populär spelsajt som erbjuder ett brett utbud av casinospel för alla smaker. Med en stor och varierad spelportfölj har Gogo casino något för alla spelare, oavsett om du föredrar klassiska slots, bordsspel eller live casino.
Enligt recensioner på AskGamblers, en av de största och mest pålitliga sajterna för casinorecensioner, är Gogo casino en av de bästa spelsajterna för svenska spelare. Med ett användarvänligt gränssnitt, snabba utbetalningar och generösa bonusar är det inte konstigt att många spelare väljer att spela på Gogo casino.
En av fördelarna med att spela på Gogo casino är att de regelbundet erbjuder kampanjer och bonusar till sina spelare. Det kan vara allt från välkomstbonusar och free spins till cashback-erbjudanden och tävlingar där du kan vinna fina priser. Detta gör att det alltid finns något extra att se fram emot när man spelar på Gogo casino.
En annan fördel med att spela på Gogo casino är att de erbjuder ett stort utbud av betalningsmetoder, vilket gör det enkelt för spelare att sätta in och ta ut pengar. Oavsett om du föredrar att använda en traditionell banköverföring, kreditkort eller e-plånbok finns det alltid en betalningsmetod som passar dig.
Sammanfattningsvis kan man säga att Gogo casino är en utmärkt spelsajt för svenska spelare som letar efter en säker och underhållande spelupplevelse. Med en stor spelportfölj, generösa bonusar och snabba utbetalningar finns det alltid något att se fram emot när man spelar på Gogo casino. Så varför inte ge det en chans och se om du också blir en av de många nöjda spelare som rekommenderar Gogo casino till andra.
https://gogocasino.one
best canadian online pharmacy Certified Canadian Pharmacy canadian pharmacies online
mexican pharmaceuticals online: Mexican Pharmacy Online – buying prescription drugs in mexico online
Tipico Casino down: Spieler verärgert über Ausfall
Das Tipico Casino ist bei vielen Spielern beliebt, doch in letzter Zeit häufen sich die Beschwerden über Ausfälle und Störungen der Plattform. Viele Spieler berichten davon, dass sie sich nicht mehr in ihren Accounts einloggen können oder dass die Spiele einfach nicht laden. Dies sorgt für großen Frust bei den Nutzern, besonders wenn sie gerade in einer spannenden Spielrunde sind.
Die Gründe für die Ausfälle sind bisher nicht bekannt, doch die Spieler äußern ihren Unmut über die mangelnde Kommunikation seitens des Casinos. Viele fühlen sich im Stich gelassen und wünschen sich eine schnellere Lösung des Problems. Einige Nutzer haben sogar bereits angekündigt, das Tipico Casino zu verlassen und sich nach einer anderen Plattform umzusehen.
Es ist zu hoffen, dass das Tipico Casino schnellstmöglich das Problem behebt und den Spielern eine reibungslose und unterbrechungsfreie Spielerfahrung bietet. Denn nur so kann das Casino seine treuen Kunden behalten und neue Spieler anlocken. Es bleibt abzuwarten, wie das Casino auf die Kritik reagieren wird und ob es gelingt, das Vertrauen der Spieler zurückzugewinnen.
https://tipicocasino.one/
Zet Casino Online Devs: Die Zukunft des Online-GlГјcksspiels
Das Online-GlГјcksspiel hat in den letzten Jahren einen enormen Aufschwung erlebt, und immer mehr Spieler entscheiden sich dafГјr, ihre Lieblingsspiele bequem von zu Hause aus zu spielen. NatГјrlich spielen dabei auch die Entwickler eine entscheidende Rolle, denn sie sind dafГјr verantwortlich, dass die Spiele reibungslos funktionieren und den Spielern ein unterhaltsames Erlebnis bieten.
Eine der bekanntesten Entwicklerfirmen in der Branche ist Zet Casino Online Devs. Das Unternehmen hat sich einen Namen gemacht, indem es hochwertige Casinospiele entwickelt, die sowohl auf dem PC als auch auf mobilen Geräten funktionieren. Die Spiele von Zet Casino Online Devs zeichnen sich durch innovative Features, ansprechende Grafiken und eine benutzerfreundliche Oberfläche aus.
Ein weiterer Vorteil von Zet Casino Online Devs ist, dass sie ständig neue Spiele auf den Markt bringen und regelmäßig Updates und Verbesserungen für ihre bestehenden Spiele durchführen. So können die Spieler sicher sein, dass sie immer die neuesten und spannendsten Spiele genießen können.
Auch in Bezug auf Sicherheit und Fairness haben die Spiele von Zet Casino Online Devs einen guten Ruf. Das Unternehmen verwendet modernste Verschlüsselungstechnologien, um sicherzustellen, dass die Daten der Spieler geschützt sind, und alle Spiele werden regelmäßig von unabhängigen Prüfstellen auf ihre Fairness überprüft.
Insgesamt ist Zet Casino Online Devs ein Unternehmen, das die Zukunft des Online-Glücksspiels maßgeblich mitgestaltet. Mit ihren hochwertigen Spielen, ihrem Engagement für Innovation und ihrer Zuverlässigkeit haben sie sich einen festen Platz in der Branche gesichert und sind bei Spielern auf der ganzen Welt beliebt.
https://zetcasino.one/
best india pharmacy: buy medicines online in india – best online pharmacy india
Das Tipico Casino gehört zu den beliebtesten Online-Casinos in Deutschland. Neben einer breiten Auswahl an Spielen und einer benutzerfreundlichen Plattform bietet das Casino auch lukrative Bonusangebote an. Doch bevor man sich über die Gewinne freuen kann, müssen zunächst die Umsatzbedingungen erfüllt werden.
Die Umsatzbedingungen im Tipico Casino sind fair und transparent gestaltet. Um den Bonus freizuspielen, muss der Betrag in der Regel innerhalb einer bestimmten Frist umgesetzt werden. Diese Frist variiert je nach Aktion und kann zwischen 7 und 30 Tagen liegen. Zudem muss der Bonus- und Einzahlungsbetrag eine bestimmte Anzahl an Malen umgesetzt werden, bevor eine Auszahlung möglich ist.
Beim Freispielen des Bonus sollten Spieler darauf achten, dass nicht alle Spiele gleich stark zum Umsatz beitragen. In der Regel tragen Slots zu 100% bei, während Tisch- und Kartenspiele nur zu einem geringeren Prozentsatz zählen. Es lohnt sich also, vorab die Umsatzbedingungen zu lesen, um seine Einsätze entsprechend zu planen.
Ein weiterer Punkt, den Spieler beachten sollten, sind eventuelle Maximalgewinne, die mit dem Bonus erzielt werden können. Oftmals gibt es eine Obergrenze für die Auszahlung von Gewinnen, die mit Bonusgeldern erzielt wurden. Es ist daher ratsam, sich genau über diese Bedingungen zu informieren, um Enttäuschungen zu vermeiden.
Insgesamt bieten die Umsatzbedingungen im Tipico Casino eine gute Möglichkeit, zusätzliches Guthaben zu erhalten und die Gewinnchancen zu erhöhen. Mit etwas Geschick und einer strategischen Herangehensweise können Spieler die Bedingungen erfolgreich erfüllen und sich über lukrative Gewinne freuen.
https://tipicocasino.one/
Zet Casino ist ein Online-Casino, das im Jahr 2018 gegrГјndet wurde und seitdem eine Vielzahl von Spielen und Bonusangeboten fГјr seine Kunden anbietet. In diesem Artikel werden wir eine Bewertung des Zet Casinos vornehmen und seine Vor- und Nachteile betrachten.
Einer der größten Vorteile von Zet Casino ist die groГџe Auswahl an Spielen, die es seinen Kunden zur VerfГјgung stellt. Das Casino bietet Hunderte von Spielautomaten, Tischspielen und Live-Casino-Spielen von fГјhrenden Softwareanbietern wie NetEnt, Microgaming und Play’n GO. Dies sorgt fГјr eine abwechslungsreiche und unterhaltsame Spielerfahrung fГјr die Kunden.
Ein weiterer positiver Aspekt von Zet Casino sind die großzügigen Bonusangebote, die es seinen Spielern bietet. Neue Spieler erhalten einen Willkommensbonus, der Freispiele und Bonusgeld beinhaltet, und treue Spieler können von regelmäßigen Promotionen und Belohnungen profitieren. Dies trägt dazu bei, dass die Spieler länger im Casino bleiben und mehr Spaß haben.
Darüber hinaus bietet Zet Casino eine sichere und benutzerfreundliche Plattform für seine Kunden. Das Casino verfügt über eine gültige Lizenz und benutzt die neueste SSL-Verschlüsselungstechnologie, um sicherzustellen, dass die persönlichen Daten der Spieler geschützt sind. Die Website ist auch einfach zu navigieren und bietet eine Vielzahl von Zahlungsmethoden für die Kunden.
Ein potentieller Nachteil von Zet Casino ist, dass es in einigen Ländern eingeschränkt ist und Spieler aus bestimmten Regionen nicht akzeptiert. Dies kann frustrierend für Spieler sein, die gerne im Casino spielen möchten, aber aufgrund von rechtlichen Bestimmungen nicht die Möglichkeit dazu haben.
Insgesamt ist das Zet Casino eine gute Wahl für Spieler, die nach einer vielfältigen Auswahl an Spielen und großzügigen Bonusangeboten suchen. Mit einer sicheren und benutzerfreundlichen Plattform bietet das Casino ein erstklassiges Spielerlebnis für seine Kunden.
https://zetcasino.one/
best india pharmacy indian pharmacy delivery best online pharmacy india
Адвокат по гражданским делам в Москве – это
высококвалифицированный юрист, который специализируется на представлении и защите интересов клиентов в рамках гражданского законодательства Российской Федерации.
Работа такого адвоката в столичном регионе требует особого
внимания к деталям и отличного знания местных
правовых особенностей.
Отличительной чертой деятельности адвоката по гражданским делам в Москве
является взаимодействие с различными судебными инстанциями и государственными органами.
Будь то оспаривание сделок с недвижимостью, разрешение семейных конфликтов или вопросы наследования, адвокат будет
руководствоваться принципами справедливости и стремлением к достижению наилучшего возможного исхода для клиента.
В Москве важно выбирать адвоката, который имеет
успешный опыт ведения гражданских дел, репутацию среди коллег и благодарных
клиентов. Чтобы справиться с юридическими проблемами в столице, адвокат должен быть ловким
в переговорах, эффективно работать под давлением и обладать актуальными знаниями о последних
изменениях в законодательстве.
Программа профессиональной помощи
включает не только судебные заседания,
но и подготовку документов,
консультации, претензионно-исковую работу.
Правильный юридический подход может существенно сэкономить
время и ресурсы клиента, обеспечив при этом наилучшие шансы на успех.
Here is my webpage … юрист по гражданскому праву москва; https://%D1%8E%D1%80%D0%B8%D1%81%D1%82-51.%D1%80%D1%84/,
https://indianpharmacy.icu/# india online pharmacy
Популярная компания Скай Лайн Консалтинг предлагает весь спектр бухгалтерского сопровождения. Мы собрали команду настоящих профессионалов. Все без исключения специалисты имеют профильное образование и достаточный опыт работы. Доверьте им оформление юридических документов и кадровое делопроизводство. https://slc-company.ru/ – сайт, где есть возможность в любое время посмотреть отзывы благодарных клиентов. Обращайтесь к нам, гарантируем грамотное и быстрое решение вопросов. Стремимся к выгодному сотрудничеству!
Boomerang Casino Auszahlungsdauer: Was können Spieler erwarten?
Immer mehr Spieler entdecken die Vorzüge von Online-Casinos und suchen nach vertrauenswürdigen Anbietern, bei denen sie ihr Glück versuchen können. Boomerang Casino ist dabei eine beliebte Wahl, da es eine breite Auswahl an Spielen und attraktive Bonusangebote bietet. Doch wie sieht es eigentlich mit der Auszahlungsdauer bei diesem Anbieter aus?
Die Auszahlungsdauer ist für viele Spieler ein wichtiger Faktor bei der Wahl eines Online-Casinos. Schließlich möchte man seine Gewinne möglichst schnell und unkompliziert erhalten. Bei Boomerang Casino können Spieler in der Regel mit einer zügigen Auszahlung rechnen. Die genaue Dauer kann jedoch je nach gewählter Auszahlungsmethode variieren.
Üblicherweise werden Auszahlungen bei Boomerang Casino innerhalb von 1-3 Werktagen bearbeitet. Dabei spielt es auch eine Rolle, ob der Spieler bereits seine Identität verifiziert hat. Dies ist ein standardmäßiges Sicherheitsverfahren, das bei seriösen Online-Casinos durchgeführt wird, um die Spieler vor Betrug zu schützen.
Wenn es um die tatsächliche Auszahlungsdauer geht, hängt diese stark von der gewählten Zahlungsmethode ab. E-Wallets wie Skrill oder Neteller ermöglichen in der Regel die schnellsten Auszahlungen, die innerhalb von wenigen Stunden auf dem Konto des Spielers gutgeschrieben werden können. Bei Banküberweisungen kann es dagegen etwas länger dauern, bis das Geld beim Spieler ankommt.
Insgesamt können Spieler bei Boomerang Casino also mit einer relativ schnellen Auszahlungsdauer rechnen, vorausgesetzt sie haben alle erforderlichen Unterlagen eingereicht und verifiziert. Es lohnt sich jedoch, vorab die genauen Bedingungen des Anbieters zu überprüfen, um Enttäuschungen zu vermeiden.
Abschließend lässt sich sagen, dass Boomerang Casino eine gute Wahl für Spieler ist, die nicht nur eine große Auswahl an Spielen und lukrative Bonusangebote suchen, sondern auch Wert auf eine schnelle Auszahlung legen. Mit den richtigen Zahlungsmethoden kann man sich hier auf eine zufriedenstellende Auszahlungsdauer verlassen und die Gewinne genießen.
https://boomerangcasino.one/
Visa Zusatzkosten bei Tipico Casino
Das Tipico Casino bietet seinen Kunden eine sichere und bequeme Möglichkeit, um Einzahlungen auf ihr Spielerkonto vorzunehmen. Eine weit verbreitete Methode ist die Visa-Karte, mit der man schnell und einfach Geld auf sein Spielerkonto transferieren kann. Allerdings gibt es beim Tipico Casino einige Zusatzkosten, die bei der Verwendung der Visa-Karte anfallen können.
Die Zusatzkosten für Einzahlungen mit Visa-Karte beim Tipico Casino betragen in der Regel eine Gebühr von 2% des eingezahlten Betrags. Das bedeutet, dass bei einer Einzahlung von 100€ mit der Visa-Karte eine Zusatzgebühr von 2€ anfällt. Diese Gebühr wird direkt von dem eingezahlten Betrag abgezogen, sodass der Spieler nicht die vollen 100€ auf sein Spielerkonto gutgeschrieben bekommt.
Es ist wichtig zu beachten, dass diese Zusatzkosten ausschließlich für Einzahlungen mit der Visa-Karte gelten. Andere Zahlungsmethoden wie zum Beispiel PayPal oder Banküberweisungen sind in der Regel gebührenfrei. Daher sollten Spieler, die häufiger im Tipico Casino spielen und Einzahlungen tätigen, die verschiedenen Zahlungsmethoden vergleichen und diejenige wählen, die für sie am kostengünstigsten ist.
Zusammenfassend lässt sich festhalten, dass beim Tipico Casino beim Nutzen der Visa-Karte Zusatzkosten in Form einer Gebühr von 2% des eingezahlten Betrags anfallen können. Spieler sollten daher die verschiedenen Zahlungsmethoden vergleichen und diejenige wählen, die für sie am kostengünstigsten ist.
https://tipicocasino.one/
Zet Casino ist eine Online-GlГјcksspielplattform, die seit ihrer GrГјndung im Jahr 2018 groГџe Aufmerksamkeit auf sich gezogen hat. Das Casino bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele, Live-Casino-Spiele und vieles mehr. DarГјber hinaus bietet Zet Casino eine Reihe von attraktiven Boni und Aktionen fГјr seine Spieler.
Ein wichtiger Aspekt von Zet Casino sind die zahlreichen positiven Bewertungen, die es von Spielern erhalten hat. Diese sogenannten “recensioni zet casino” geben Aufschluss Гјber die Erfahrungen anderer Spieler mit dem Casino und kГ¶nnen potenziellen neuen Spielern helfen, eine fundierte Entscheidung zu treffen, ob sie sich anmelden mГ¶chten oder nicht.
Die überwiegende Mehrheit der recensioni zet casino hebt die große Auswahl an Spielen hervor, die das Casino bietet. Von klassischen Spielautomaten bis hin zu aufregenden neuen Titeln ist für jeden Geschmack etwas dabei. Darüber hinaus loben die Spieler die benutzerfreundliche Oberfläche und das reibungslose Spielerlebnis, das Zet Casino bietet.
Ein weiterer häufig genannter Pluspunkt sind die großzügigen Boni und Promotionen, die regelmäßig angeboten werden. Spieler können von Willkommensboni, Freispielen und Cashback-Angeboten profitieren, die ihre Gewinnchancen erhöhen und ihr Spielerlebnis noch unterhaltsamer machen.
Insgesamt scheint Zet Casino bei den Spielern sehr gut anzukommen und hat sich als ein beliebtes Ziel für Online-Glücksspielfans etabliert. Die recensioni zet casino sprechen eine klare Sprache und bestärken den positiven Ruf, den das Casino in der Branche genießt. Wer auf der Suche nach einem zuverlässigen und unterhaltsamen Online-Casino ist, sollte Zet Casino definitiv in Betracht ziehen.
https://zetcasino.one/
В компании ЗАО «Автономный ЭнергоСервис» работают исключительно квалифицированные профессионалы. В сжатый срок выполним решения разной сложности с результативностью для заказчика. Гарантируем оперативные поставки энергетического оборудования и предлагаем грамотные консультации. https://mototech.ru – сайт, где можно найти доброжелательные отзывы клиентов. Вы будете приятно удивлены привлекательной ценовой политикой, качеством продукции и высочайшей культурой общения персонала. Мы готовы быть долгосрочным и надежным партнером, обращайтесь к нам уже сейчас.
п»їbest mexican online pharmacies: Mexican Pharmacy Online – reputable mexican pharmacies online
best online pharmacies in mexico mexican drugstore online medication from mexico pharmacy
Kann bei Tipico Casino nicht einzahlen
Es kann frustrierend sein, wenn man bei einem Online-Casino wie Tipico nicht in der Lage ist, eine Einzahlung vorzunehmen. Dies kann verschiedene Gründe haben und in diesem Artikel werden wir uns mit einigen möglichen Ursachen befassen.
Ein möglicher Grund könnte sein, dass Ihr Zahlungsmittel nicht von Tipico akzeptiert wird. Überprüfen Sie daher, ob die von Ihnen gewählte Zahlungsmethode von Tipico akzeptiert wird. Gängige Zahlungsmethoden bei Online-Casinos sind Kreditkarten, Banküberweisungen, E-Wallets wie PayPal und Skrill sowie Prepaid-Karten.
Ein weiterer Grund könnte sein, dass Ihr Konto möglicherweise nicht über ausreichend Guthaben verfügt, um eine Einzahlung vorzunehmen. Stellen Sie sicher, dass Sie genügend Geld auf Ihrem Konto haben, um die gewünschte Einzahlungsbetrag abzudecken.
Es ist auch möglich, dass es technische Probleme auf Seiten des Casinos gibt, die es Ihnen derzeit unmöglich machen, eine Einzahlung vorzunehmen. In diesem Fall sollten Sie sich an den Kundendienst von Tipico wenden, um das Problem zu melden und weitere Unterstützung zu erhalten.
Insgesamt ist es wichtig, geduldig zu bleiben und verschiedene Lösungsansätze zu versuchen, wenn Sie bei Tipico Casino nicht einzahlen können. Mit etwas Glück können Sie das Problem schnell beheben und in kürzester Zeit wieder mit dem Spielen beginnen.
https://tipicocasino.one/
Der Moment, auf den alle Spieler im Zet Casino gehofft haben, ist endlich eingetreten: Das Auszahlungslimit wurde erreicht. Dies bedeutet, dass die Glücklichen, die genug Glück und Können hatten, um Gewinne anzuhäufen, jetzt ihre verdienten Belohnungen abheben können.
Das Auszahlungslimit im Zet Casino ist eine wichtige Richtlinie, die sicherstellt, dass sowohl das Casino als auch die Spieler geschützt sind. Es dient dazu, dass die Spieler ihre Gewinne nicht sofort abheben und damit das Risiko des Verlustes minimieren. Stattdessen müssen sie eine bestimmte Summe erreichen, bevor sie eine Auszahlung beantragen können.
Für die Spieler, die hart gearbeitet und hart gespielt haben, um dieses Limit zu erreichen, ist es ein aufregender Moment. Es ist die Belohnung für ihre Ausdauer, ihr Geschick und ihre Entschlossenheit. Sie können jetzt ihre Gewinne genießen und sich darüber freuen, dass sich ihre Mühe ausgezahlt hat.
Für das Zet Casino ist das Erreichen des Auszahlungslimits ebenfalls ein positives Zeichen. Es zeigt, dass das Casino attraktiv genug ist, um Spieler anzuziehen und sie dazu zu ermutigen, weiterzuspielen. Es ist ein Beweis für die Qualität des Casinos und die Zufriedenheit der Spieler.
Insgesamt ist das Erreichen des Auszahlungslimits im Zet Casino ein Grund zum Feiern. Es ist eine Bestätigung für die Spieler, dass ihr Einsatz belohnt wird, und für das Casino, dass es gute Arbeit leistet. Es ist ein Zeichen dafür, dass alle Beteiligten profitieren und Spaß haben können.
https://zetcasino.one/
mexican online pharmacies prescription drugs: mexico pharmacy – mexico pharmacy
Tipico Casino Bonus ohne Einzahlung: Holen Sie sich Ihr Gratis-Guthaben
Das Tipico Casino bietet seinen Kunden nicht nur eine große Auswahl an Spielen und attraktive Bonusangebote, sondern auch die Möglichkeit, ohne Einzahlung von eigenem Geld zu spielen. Der sogenannte Tipico Casino Bonus ohne Einzahlung ist eine großartige Möglichkeit, um das Casino kennenzulernen und erste Gewinne zu erzielen, ohne Risiko eingehen zu müssen.
Um den Tipico Casino Bonus ohne Einzahlung zu erhalten, müssen Sie sich lediglich als neuer Kunde im Casino registrieren. Nach erfolgreicher Registrierung erhalten Sie automatisch Ihr Gratis-Guthaben gutgeschrieben, mit dem Sie sofort loslegen können. Dieses Gratis-Guthaben kann für eine Vielzahl von Spielen im Casino genutzt werden, darunter Slots, Tischspiele und vieles mehr.
Der Tipico Casino Bonus ohne Einzahlung bietet Ihnen die Möglichkeit, das Casino und seine Spiele in aller Ruhe auszuprobieren, ohne dabei Ihr eigenes Geld riskieren zu müssen. Sie können erste Gewinne erzielen, ohne selbst einen Cent einzahlen zu müssen. Dies macht den Tipico Casino Bonus ohne Einzahlung zu einer attraktiven Option für alle, die das Casino erst einmal unverbindlich testen möchten.
Wenn Sie sich für den Tipico Casino Bonus ohne Einzahlung interessieren, sollten Sie jedoch beachten, dass dieser in der Regel an bestimmte Umsatzbedingungen geknüpft ist. Bevor Sie sich Ihre Gewinne auszahlen lassen können, müssen Sie den Bonus bestimmte Male umsetzen. Es ist daher wichtig, die jeweiligen Bedingungen genau zu lesen, bevor Sie den Bonus in Anspruch nehmen.
Insgesamt bietet der Tipico Casino Bonus ohne Einzahlung eine tolle Gelegenheit, um das Casino risikofrei kennenzulernen und erste Gewinne zu erzielen. Wenn Sie sich als neuer Kunde im Tipico Casino registrieren, sollten Sie also unbedingt auch den Bonus ohne Einzahlung in Anspruch nehmen. Viel SpaГџ und Erfolg beim Spielen!
https://tipicocasino.one/
Zet Casino Erfahrungen: Alles, was Sie wissen mГјssen
Es ist keine leichte Aufgabe, das perfekte Online-Casino zu finden, das all Ihre Anforderungen erfüllt. Aber wenn Sie auf der Suche nach einem unterhaltsamen und sicheren Ort sind, um Ihre Lieblingsspiele zu spielen, dann könnte Zet Casino die richtige Wahl für Sie sein.
Zet Casino ist ein relativ neues Online-Casino, das 2018 gegründet wurde. Trotz seiner jungen Geschichte hat es sich bereits einen soliden Ruf in der Glücksspielbranche erarbeitet. Das Casino wird von Araxio Development N.V. betrieben und verfügt über eine Lizenz der Regierung von Curaçao.
Eine der ersten Dinge, die die Spieler an Zet Casino bemerken, ist die benutzerfreundliche Website und die groГџe Auswahl an Spielen. Mit Titeln von erstklassigen Anbietern wie NetEnt, Microgaming, Play’n GO und vielen anderen, gibt es hier fГјr jeden Geschmack etwas zu entdecken. Von Spielautomaten Гјber Tischspiele bis hin zu Live-Casino-Spielen bietet Zet Casino ein beeindruckendes Portfolio an SpielmГ¶glichkeiten.
Ein weiterer großer Pluspunkt von Zet Casino sind die großzügigen Bonusangebote und Aktionen. Neue Spieler können sich über einen Willkommensbonus freuen, der Ihnen zusätzliches Geld und Freispiele für Ihre ersten Einzahlungen bietet. Darüber hinaus bietet das Casino regelmäßige Promotionen, Turniere und Treueprogramme, die es lohnenswert machen, regelmäßig zurückzukehren.
In Bezug auf die Sicherheit und den Kundenservice stehen die Erfahrungen der Spieler bei Zet Casino auch im Vordergrund. Die Website wird mit modernster SSL-Verschlüsselungstechnologie gesichert, um die Sicherheit Ihrer persönlichen Daten und finanziellen Transaktionen zu gewährleisten. Das Supportteam des Casinos ist rund um die Uhr per Live-Chat, E-Mail und Telefon erreichbar und steht Ihnen bei Fragen oder Problemen gerne zur Verfügung.
Insgesamt kann man sagen, dass die Erfahrungen mit Zet Casino größtenteils positiv ausfallen. Mit einer umfangreichen Spielauswahl, großzügigen Boni und einem zuverlässigen Kundenservice bietet das Casino eine unterhaltsame und sichere Spielerfahrung für alle Glücksspielfans. Wenn Sie also auf der Suche nach einem neuen Online-Casino sind, das all Ihre Wünsche erfüllen kann, dann sollten Sie Zet Casino auf jeden Fall eine Chance geben.
https://zetcasino.one/
my canadian pharmacy reviews Licensed Canadian Pharmacy canadian pharmacy 24h com
canadian pharmacy 24 com: pills now even cheaper – onlinepharmaciescanada com
Медицинский юрист консультация
– профессиональная услуга, предоставляемая юридическими экспертами в области здравоохранения.
Такие юристы предоставляют правовое сопровождение
врачам, больницам и другим медицинским учреждениям, а также помогают пациентам в
вопросах, связанных с медицинскими
услугами и их правами.
В рамках консультации медицинский юрист может рассматривать случаи, касающиеся медицинской ответственности,
неправильного диагноза, ошибок в лечении
и вопросов согласия на медицинское вмешательство.
Консультация также охватывает анализ и оценку медицинской
документации, юридическую помощь в разрешении споров и претензий, а также содействие в
получении страховых и других видов компенсаций.
Юристы, специализирующиеся на медицинском
праве, не просто владеют
специфическими юридическими знаниями, но и обладают пониманием медицинских терминов и
процедур, что позволяет им эффективно взаимодействовать
между пациентом и медицинским учреждением.
Консультация медицинского юриста – значимый шаг
в защите прав и интересов
всех сторон медицинских юридических отношений.
My homepage помощь медицинского юриста
Boomerang Casino No Deposit
Das Boomerang Casino ist eine beliebte Online-GlГјcksspielplattform, die eine Vielzahl von Spielen und Boni fГјr seine Spieler anbietet. Eines der attraktivsten Angebote des Casinos ist der sogenannte “No Deposit Bonus”, bei dem Spieler Bonusgeld erhalten, ohne eine Einzahlung tГ¤tigen zu mГјssen.
Der No Deposit Bonus ist eine großartige Möglichkeit für Spieler, das Casino auszuprobieren, ohne eigenes Geld riskieren zu müssen. Spieler können mit dem Bonusgeld verschiedene Spiele spielen und dabei echtes Geld gewinnen. Dies ist eine fantastische Gelegenheit für Anfänger, die noch keine Erfahrung mit Online-Glücksspielen haben, um das Casino kennenzulernen und sich mit den verschiedenen Spielen vertraut zu machen.
Um den No Deposit Bonus zu erhalten, müssen Spieler sich einfach im Boomerang Casino anmelden und ein Konto erstellen. Der Bonus wird dann automatisch gutgeschrieben und kann sofort für Spiele verwendet werden. Es ist wichtig zu beachten, dass es in der Regel bestimmte Wettanforderungen gibt, die erfüllt werden müssen, bevor Gewinne, die mit dem Bonus erzielt wurden, ausgezahlt werden können.
Das Boomerang Casino bietet eine Vielzahl von Spielen, darunter Spielautomaten, Tischspiele wie Roulette und Blackjack, sowie Live-Casino-Spiele mit echten Dealern. Mit dem Bonusgeld können Spieler jede Art von Spiel ausprobieren und vielleicht sogar einen großen Gewinn erzielen.
Insgesamt ist der No Deposit Bonus im Boomerang Casino eine großartige Möglichkeit für Spieler, das Casino zu erkunden und erste Gewinne zu erzielen, ohne eigenes Geld riskieren zu müssen. Es ist ein aufregendes Angebot, das es Spielern ermöglicht, die Welt des Online-Glücksspiels zu entdecken und Spaß zu haben.
https://boomerangcasino.one/
Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und großartigen Funktionen für Spieler bietet. Einer der wichtigsten Aspekte beim Spielen in einem Online-Casino ist die Möglichkeit, Gewinne abzuheben und sich das Geld schnell und problemlos auszahlen zu lassen. Dies ist bei Zet Casino dank ihres effizienten Auszahlungssystems kein Problem.
Das “Zet Casino Kotiutus” Programm ermГ¶glicht es den Spielern, ihre Gewinne schnell und einfach abzuheben. Spieler kГ¶nnen aus einer Vielzahl von Zahlungsmethoden wГ¤hlen, darunter Kreditkarten, E-Wallets und BankГјberweisungen. Die Auszahlungszeiten variieren je nach gewГ¤hlter Zahlungsmethode, aber in der Regel erfolgen die Auszahlungen schnell und zuverlГ¤ssig.
Zet Casino legt großen Wert darauf, dass die Spieler eine positive Erfahrung beim Spielen haben und sich keine Sorgen um ihre Auszahlungen machen müssen. Ihr Kundenservice ist rund um die Uhr verfügbar, um bei Fragen oder Problemen zu helfen. Die Sicherheit der Spieler und ihrer finanziellen Daten hat oberste Priorität, daher werden alle Auszahlungen sicher und geschützt abgewickelt.
Zusammenfassend lГ¤sst sich sagen, dass Zet Casino eine hervorragende Wahl fГјr Spieler ist, die eine zuverlГ¤ssige und benutzerfreundliche Plattform fГјr ihre Online-Casino-BedГјrfnisse suchen. Mit ihrem effizienten “Zet Casino Kotiutus” Programm kГ¶nnen Spieler ihre Gewinne problemlos abheben und sich auf ein unterhaltsames Spielerlebnis konzentrieren.
https://zetcasino.one/
purple pharmacy mexico price list: mexican pharmacy – mexico drug stores pharmacies
Tipico Live Casino Geld Auszahlen
Das Tipico Live Casino ist eine beliebte Plattform für Glücksspiele und Spannung. Spieler können hier live gegen echte Dealer antreten und ihr Glück versuchen. Doch auch wenn das Spiel im Live Casino Spaß macht, so stellt sich doch irgendwann die Frage: Wie kann ich mein Gewonnenes auszahlen lassen?
Um sein Geld aus dem Tipico Live Casino auszahlen zu lassen, muss man sich zunГ¤chst einmal in sein Spielerkonto einloggen. Dort findet man unter dem Reiter “Mein Konto” die Option “Auszahlung”. Hier hat der Spieler die MГ¶glichkeit, den gewГјnschten Auszahlungsbetrag einzugeben und die gewГјnschte Auszahlungsmethode auszuwГ¤hlen.
Tipico bietet verschiedene Auszahlungsoptionen an, darunter Banküberweisung, Kreditkarte und E-Wallets wie PayPal oder Skrill. Je nach gewählter Methode kann es unterschiedlich lange dauern, bis das Geld auf dem eigenen Konto gutgeschrieben wird. In der Regel erfolgen Auszahlungen jedoch zügig und zuverlässig.
Es ist wichtig zu beachten, dass Tipico für Auszahlungen oft dieselbe Methode verwendet, die auch für die Einzahlung genutzt wurde. Sollte dies nicht möglich sein oder der Spieler eine andere Methode bevorzugen, kann er sich jederzeit an den Kundenservice von Tipico wenden, um eine Lösung zu finden.
Zusammenfassend lässt sich sagen, dass das Auszahlen von Geldern aus dem Tipico Live Casino ein unkomplizierter Vorgang ist. Mit den verschiedenen Auszahlungsoptionen und dem zuverlässigen Kundenservice bietet Tipico seinen Spielern die Möglichkeit, ihre Gewinne schnell und einfach zu erhalten. Wer also im Tipico Live Casino erfolgreich war, kann sich darauf freuen, sein Geld zeitnah und sicher auszahlen zu lassen.
https://tipicocasino.one/
mexican pharmacy [url=https://mexicanpharmacy.shop/#]mexico pharmacy[/url] buying prescription drugs in mexico
http://indianpharmacy.icu/# mail order pharmacy india
https://clomidall.com/# where buy clomid for sale
Zet Casino Promo Code: Holen Sie sich tolle Boni und Freispiele
Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und großzügige Boni für seine Spieler anbietet. Wenn Sie auf der Suche nach zusätzlichen Belohnungen sind, sollten Sie unbedingt den Zet Casino Promo Code verwenden. Mit diesem Code können Sie sich tolle Boni und Freispiele sichern, die Ihr Spielerlebnis noch spannender machen.
Um den Zet Casino Promo Code zu nutzen, müssen Sie sich zunächst auf der Website des Casinos registrieren. Geben Sie bei der Anmeldung den Promo Code ein, um die zusätzlichen Belohnungen zu aktivieren. Sobald Sie dies getan haben, können Sie mit Ihrem Bonusguthaben spielen und tolle Gewinne erzielen.
Mit dem Zet Casino Promo Code können Sie verschiedene Arten von Boni erhalten, darunter Einzahlungsboni, Freispiele, Cashback-Angebote und mehr. Diese Boni können Ihre Gewinnchancen erhöhen und Ihnen mehr Spaß beim Spielen bieten. Es lohnt sich also, regelmäßig nach neuen Promo Codes zu suchen und diese zu nutzen.
Wenn Sie gerne Slots spielen, werden Sie sich über die Freispiele freuen, die Sie mit dem Zet Casino Promo Code erhalten können. Diese ermöglichen es Ihnen, kostenlos zu spielen und dennoch echte Gewinne zu erzielen. Außerdem können Sie mit den Einzahlungsboni Ihre Einzahlungen aufstocken und somit länger spielen und mehr gewinnen.
Insgesamt bietet der Zet Casino Promo Code eine großartige Möglichkeit, zusätzliche Belohnungen zu erhalten und Ihr Spielerlebnis zu verbessern. Nutzen Sie also diese Chance und holen Sie sich Ihre Boni und Freispiele noch heute!
https://zetcasino.one/
USIIC.CO is a unique platform created for bloggers and authors who want to publish interesting articles, create groups to attract subscribers and earn money from their content. Community https://usiic.co It is open to anyone who wants to share their ideas and creativity with the whole world.PUBLISH INTERESTING ARTICLES, FOR FREE. CREATE A GROUP TO ATTRACT SUBSCRIBERS. BECOME THE BEST AUTHOR AND MAKE EARNINGS WITH US.
zithromax capsules: zithromax 250 – cheap zithromax pills
Boomerang Casino – Freispiele ohne Einzahlung
Boomerang Casino ist ein aufregendes und spannendes Online-Casino, das eine Vielzahl von Spielen und Boni für seine Spieler bietet. Einer der beliebtesten Boni bei Boomerang Casino sind die Freispiele ohne Einzahlung, die es den Spielern ermöglichen, bestimmte Spiele kostenlos zu spielen, ohne dass sie Geld einzahlen müssen.
Die Freispiele ohne Einzahlung sind eine großartige Möglichkeit für Spieler, neue Spiele auszuprobieren, ohne ein Risiko einzugehen. Sie können die Spiele testen und herausfinden, welche ihnen am besten gefallen, bevor sie echtes Geld setzen. Die Freispiele ohne Einzahlung sind auch eine gute Möglichkeit für Spieler, ihre Fähigkeiten zu verbessern und neue Strategien auszuprobieren, ohne ihr eigenes Geld zu riskieren.
Um die Freispiele ohne Einzahlung zu erhalten, müssen sich die Spieler lediglich bei Boomerang Casino anmelden und ein Konto erstellen. Die Freispiele werden dann automatisch gutgeschrieben und können sofort verwendet werden. Die Spieler können die Freispiele an bestimmten ausgewählten Spielen verwenden und die Gewinne, die sie damit erzielen, behalten.
Boomerang Casino bietet seinen Spielern regelmäßig Freispiele ohne Einzahlung an, um sie zu belohnen und zu ermutigen, weiterhin bei ihnen zu spielen. Die Spieler können sich über den Newsletter oder die sozialen Medien über die neuesten Freispielangebote informieren und sicherstellen, dass sie keine Gelegenheit verpassen, kostenlose Spiele zu genießen.
Insgesamt bieten die Freispiele ohne Einzahlung von Boomerang Casino den Spielern eine großartige Möglichkeit, ihre Lieblingsspiele kostenlos zu spielen und echte Gewinne zu erzielen. Es lohnt sich also, sich regelmäßig bei Boomerang Casino anzumelden und die neuesten Freispielangebote zu nutzen. Viel Spaß beim Spielen und viel Glück!
https://boomerangcasino.one/
http://clomidall.shop/# where can i get generic clomid without insurance
Das „Zet Online Casino“ ist ein aufstrebendes Online-Casino, das Spielern eine Vielzahl von Spielen und tollen Bonusangeboten bietet. Mit einer benutzerfreundlichen Oberfläche und einer großen Auswahl an Spielen ist das Zet Online Casino eine beliebte Anlaufstelle für Glücksspiel-Fans.
Das Casino bietet eine breite Palette von Spielen, darunter Slots, Tischspiele, Live-Casino-Spiele und vieles mehr. Mit Spielen von renommierten Anbietern wie NetEnt, Microgaming und Play’n GO ist für jeden Geschmack etwas dabei. Die Spiele können direkt im Browser gespielt werden, so dass keine zusätzliche Software heruntergeladen werden muss.
Ein besonderes Highlight des Zet Online Casinos sind die großzügigen Bonusangebote. Neue Spieler können sich über einen Willkommensbonus freuen, der zusätzliches Guthaben und Freispiele für ausgewählte Spiele bietet. Darüber hinaus gibt es regelmäßige Promotionen und Aktionen, die den Spielern zusätzliche Gewinnchancen bieten.
Das Zet Online Casino legt großen Wert auf Sicherheit und Fairness. Das Casino ist von der Malta Gaming Authority lizenziert und wird regelmäßig von unabhängigen Prüfungsbehörden auf Fairness und Zufälligkeit der Spiele überprüft. Die Spieler können also sicher sein, dass sie in einem sicheren und vertrauenswürdigen Online-Casino spielen.
Insgesamt ist das Zet Online Casino eine ausgezeichnete Wahl fГјr Spieler, die auf der Suche nach einem hochwertigen und unterhaltsamen Online-Casino-Erlebnis sind. Mit einer groГџen Auswahl an Spielen, groГџzГјgigen Bonusangeboten und einem hohen MaГџ an Sicherheit und Fairness ist das Zet Online Casino definitiv einen Besuch wert.
https://zetcasino.one/
Хотите взять в аренду детские коляски? Мы вам в этом поможем. Гарантируем приемлемые цены и предоставляем большой выбор детских колясок для аренды. Наши компетентные специалисты подберут нужный вариант и обеспечат безопасность и комфорт. https://arenda-detskoj-kolyaski.fast-rent.ru/ – сайт, где можете прямо сейчас оставить заявку. Любая наша коляска находится в отличном техническом состоянии и имеет солидный внешний вид. Мы всегда открыты для долгосрочного сотрудничества и диалога. Обращайтесь к нам и об этом точно не пожалеете!
Tipico Casino Anmelden
Das Tipico Casino ist eine beliebte Online-Plattform für Glücksspiele, die eine Vielzahl von Spielen wie Slots, Roulette, Blackjack und vieles mehr anbietet. Um die Vielfalt der Spiele und das spannende Spielerlebnis zu genießen, muss man sich zunächst anmelden.
Die Anmeldung im Tipico Casino ist einfach und unkompliziert. Als erstes muss man die Website des Casinos besuchen und auf den Button “Registrieren” oder “Anmelden” klicken. Danach Г¶ffnet sich ein Anmeldeformular, in das man seine persГ¶nlichen Daten wie Name, Adresse, Geburtsdatum und E-Mail-Adresse eingeben muss.
Nach der Eingabe der Daten muss man die Allgemeinen Geschäftsbedingungen akzeptieren und bestätigen, dass man mindestens 18 Jahre alt ist. Anschließend erhält man eine Bestätigungs-E-Mail, in der man einen Link anklicken muss, um die Registrierung abzuschließen.
Nach erfolgreicher Anmeldung kann man sofort mit dem Spielen im Tipico Casino beginnen. Man kann Geld einzahlen, um an den Spielen teilzunehmen und auch von attraktiven Bonusangeboten profitieren.
Es ist wichtig, verantwortungsbewusst zu spielen und sich über die Risiken des Glücksspiels im Klaren zu sein. Das Tipico Casino bietet verschiedene Maßnahmen zum Spieler- und Jugendschutz, um ein sicheres und faires Spielerlebnis zu gewährleisten.
Also, wenn Sie Lust auf spannende Casinospiele haben, dann melden Sie sich noch heute im Tipico Casino an und genieГџen Sie die Vielfalt der angebotenen Spiele. Viel SpaГџ und viel GlГјck!
https://tipicocasino.one/
buy amoxicillin amoxicillin without prescription amoxicillin without a doctors prescription
Zet Casino ist eine Online-GlГјcksspielplattform, die eine Vielzahl von Spielen fГјr Spieler aus der ganzen Welt bietet. Mit einer benutzerfreundlichen Website und einer Vielzahl von Einzahlungs- und Auszahlungsoptionen ist Zet Casino eine beliebte Wahl fГјr Online-Spieler.
Zet Casino bietet eine große Auswahl an Casinospielen, darunter beliebte Slots, Tischspiele wie Roulette und Blackjack, sowie Live-Dealer-Spiele. Die Website ist einfach zu bedienen und bietet eine schnelle und einfache Navigation, sodass Spieler schnell ihre Lieblingsspiele finden können.
Ein weiterer Vorteil von Zet Casino ist das großzügige Bonusprogramm. Neue Spieler erhalten einen Willkommensbonus bei ihrer ersten Einzahlung und können auch regelmäßig von anderen Promotionen und Turnieren profitieren.
Zet Casino legt großen Wert auf Sicherheit und Fairness und ist lizenziert und reguliert durch die Malta Gaming Authority. Spieler können also sicher sein, dass ihre persönlichen Daten und finanziellen Transaktionen geschützt sind.
Insgesamt bietet Zet Casino eine unterhaltsame und sichere Umgebung fГјr Online-Spieler. Mit einer groГџen Auswahl an Spielen, groГџzГјgigen Boni und einem benutzerfreundlichen Design ist Zet Casino definitiv eine Online-GlГјcksspielplattform, die es wert ist, ausprobiert zu werden. Besuchen Sie noch heute zet casino.com und entdecken Sie die aufregende Welt des Online-GlГјcksspiels.
https://zetcasino.one/
https://prednisoneall.com/# prednisone 12 mg
Das Boomerang Casino lockt mit spannenden Angeboten für alle Spieler, die gerne kostenlose Spins nutzen. Mit dem Bonus „Free Spins No Deposit“ können Spieler ganz ohne Einzahlung die Walzen der beliebten Slots in Bewegung setzen und dabei echte Gewinne erzielen.
Das Boomerang Casino bietet eine Vielzahl von kostenlosen Spins ohne Einzahlung für neue Spieler, die sich anmelden. Diese Spins können an ausgewählten Spielautomaten genutzt werden und sind eine großartige Möglichkeit, das Casino und die verschiedenen Spiele unverbindlich kennenzulernen.
Die Free Spins ohne Einzahlung im Boomerang Casino sind eine tolle Möglichkeit, um echte Gewinne zu erzielen, ohne dabei eigenes Geld zu riskieren. Spieler können mit etwas Glück sogar den Jackpot knacken und sich so ein kleines Vermögen sichern.
Um von den Free Spins ohne Einzahlung zu profitieren, müssen sich Spieler lediglich im Boomerang Casino anmelden und den Bonuscode nutzen, der ihnen bei der Registrierung zur Verfügung gestellt wird. Die Freispiele werden dann automatisch gutgeschrieben und können direkt genutzt werden.
Das Boomerang Casino bietet nicht nur spannende Spiele und großzügige Boni, sondern auch einen exzellenten Kundenservice und schnelle Auszahlungen. Spieler können sich also darauf verlassen, dass sie bei diesem Online-Casino in guten Händen sind.
Insgesamt ist das Boomerang Casino mit seinen Free Spins ohne Einzahlung eine hervorragende Wahl für alle Spieler, die auf der Suche nach einem unterhaltsamen und lukrativen Casino-Erlebnis sind. Mit etwas Glück können Spieler hier echte Gewinne erzielen, ohne dabei eigenes Geld riskieren zu müssen.
https://boomerangcasino.one/
Zet Casino Auszahlungslimit
Das Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und groГџzГјgigen Bonusangeboten bietet. Allerdings gibt es beim Zet Casino auch ein Auszahlungslimit, das es zu beachten gilt.
Das Auszahlungslimit beim Zet Casino beträgt 10.000 Euro pro Monat. Das bedeutet, dass Spieler innerhalb eines Monats nicht mehr als 10.000 Euro auszahlen lassen können. Dieses Limit gilt für alle Spieler, unabhängig von ihrem VIP-Status oder ihrer Einzahlungshöhe.
Es ist wichtig zu beachten, dass das Auszahlungslimit für jedes Online-Casino unterschiedlich sein kann. Einige Casinos haben höhere Auszahlungslimits, während andere niedrigere Limits haben. Spieler sollten daher immer die Auszahlungsbedingungen eines bestimmten Casinos überprüfen, bevor sie sich entscheiden, dort zu spielen.
Um das Auszahlungslimit beim Zet Casino zu umgehen, können Spieler ihre Auszahlungen auf mehrere Monate verteilen oder höhere Einzahlungen tätigen, um ihr Limit zu erhöhen. Es ist jedoch wichtig zu beachten, dass das Casino das Recht hat, Auszahlungen zu verweigern, wenn Spieler versuchen, das Limit zu umgehen.
Insgesamt ist das Auszahlungslimit beim Zet Casino ein wichtiger Aspekt, den Spieler im Auge behalten sollten. Indem sie sich an das Limit halten und verantwortungsbewusst spielen, können Spieler ein sicheres und unterhaltsames Spielerlebnis im Zet Casino genießen.
https://zetcasino.one/
Tipico Classic Casino Chips umwandeln
Im Tipico Classic Casino haben Spieler die Möglichkeit, mit Casino Chips zu spielen. Diese Chips können jedoch nicht direkt in echtes Geld umgewandelt werden. Stattdessen können Spieler sie in Spielguthaben umwandeln und damit ihr Glück an verschiedenen Spielen versuchen.
Um Casino Chips in Spielguthaben umzuwandeln, mГјssen Spieler einfach auf den entsprechenden Button klicken und den gewГјnschten Betrag eingeben. Der umgerechnete Betrag wird dann dem Spielerkonto gutgeschrieben und kann fГјr das Spielen genutzt werden.
Es ist wichtig zu beachten, dass Casino Chips nicht direkt in echtes Geld umgetauscht werden können. Sie dienen lediglich dazu, das Spielerlebnis im Tipico Classic Casino zu verbessern und den Spielern zusätzliche Möglichkeiten zu bieten, ihre Lieblingsspiele zu genießen.
Insgesamt bietet die Möglichkeit, Casino Chips in Spielguthaben umzuwandeln, den Spielern eine zusätzliche Flexibilität und macht das Spielerlebnis im Tipico Classic Casino noch spannender. Also worauf warten Sie noch? Besuchen Sie das Tipico Classic Casino und lassen Sie sich von der Vielfalt der Spiele und Möglichkeiten begeistern. Viel Glück beim Spielen!
https://tipicocasino.one/
where can i get amoxicillin where can you get amoxicillin order amoxicillin online
https://amoxilall.shop/# amoxicillin medicine over the counter
На сайте компании VipПрокат https://xn--42-6kch4am1ahakz.xn--p1ai/ воспользуйтесь калькулятором для того, чтобы рассчитать стоимость такой услуги, как прокат автомобилей премиального уровня. При желании можно взять на прокат автомобиль с водителем либо без него. Специально для вас выгодные расценки, а также приемлемые тарифы. Есть возможность арендовать авто на один либо несколько дней. Регулярно компания устраивает акции, устанавливает скидки, чтобы услуга была более выгодной. Для того чтобы узнать, где находится компания, изучите карту.
Желаете взять детские коляски в аренду? Мы это то, что вам нужно. Предоставляем впечатлительный выбор детских колясок для аренды и гарантируем доступные цены. Наши компетентные специалисты подберут нужный вариант и обеспечат безопасность и комфорт. https://arenda-detskoj-kolyaski.fast-rent.ru/ – сайт, где можете прямо сейчас оставить заявку. Каждая коляска имеет презентабельный внешний вид и находится в отменном техническом состоянии. Мы всегда открыты для долгосрочного сотрудничества и диалога. Обращайтесь к нам и об этом точно не пожалеете!
Zet Casino Erfahrungen Auszahlung
Zet Casino ist eine beliebte Online-Spielplattform, die eine Vielzahl von Spielen für Glücksspielliebhaber anbietet. Ein wichtiger Aspekt für Spieler, die online spielen, ist die Auszahlung ihrer Gewinne. In diesem Artikel werden wir uns genauer mit den Zet Casino Erfahrungen zur Auszahlung beschäftigen.
Die Auszahlungsmöglichkeiten bei Zet Casino sind vielfältig und flexibel. Spieler können zwischen verschiedenen Zahlungsmethoden wie Kreditkarten, E-Wallets und Banküberweisungen wählen. Die Auszahlungen erfolgen in der Regel schnell und zuverlässig, so dass die Spieler ihre Gewinne schnell erhalten können.
Ein weiterer positiver Aspekt der Zet Casino Auszahlungserfahrungen ist der Kundenservice. Das Support-Team ist gut geschult und hilfsbereit und steht den Spielern bei Fragen oder Problemen zur Verfügung. Die Spieler können sich per E-Mail, Live-Chat oder Telefon an den Kundenservice wenden und erhalten in der Regel eine schnelle und kompetente Antwort.
Zet Casino legt auch großen Wert auf Sicherheit und Fairness. Die Plattform verfügt über eine Glücksspiellizenz und verwendet moderne Verschlüsselungstechnologien, um die persönlichen und finanziellen Daten der Spieler zu schützen. Darüber hinaus werden alle Spiele regelmäßig von unabhängigen Prüfstellen auf ihre Fairness überprüft.
Insgesamt sind die Zet Casino Erfahrungen zur Auszahlung sehr positiv. Die Spieler können sich auf schnelle und zuverlässige Auszahlungen verlassen und profitieren von einem professionellen Kundenservice sowie hohen Sicherheitsstandards. Wer auf der Suche nach einer sicheren und unterhaltsamen Spielplattform ist, sollte Zet Casino auf jeden Fall eine Chance geben.
Abschließend lässt sich sagen, dass Zet Casino eine empfehlenswerte Option für Glücksspielfans ist, die Wert auf schnelle Auszahlungen, guten Kundenservice und hohe Sicherheitsstandards legen. Probieren Sie es selbst aus und überzeugen Sie sich von den Vorteilen der Zet Casino Auszahlungserfahrungen.
https://zetcasino.one/
Boomerang Casino Erfahrung
Das Boomerang Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen fГјr seine Spieler anbietet. In diesem Artikel werden wir die Erfahrung von Spielern, die das Boomerang Casino ausprobiert haben, genauer betrachten.
Viele Spieler loben die große Auswahl an Spielen, die im Boomerang Casino verfügbar sind. Von klassischen Slots bis hin zu Live-Casino-Spielen und Jackpot-Slots ist für jeden Geschmack etwas dabei. Die Spiele werden von renommierten Software-Anbietern wie NetEnt, Microgaming und Play’n GO bereitgestellt, was für hohe Qualität und unterhaltsame Spielabläufe sorgt.
Ein weiterer positiver Aspekt des Boomerang Casinos sind die attraktiven Bonusangebote für Neukunden und bestehende Spieler. Registrieren sich neue Spieler im Casino, können sie von großzügigen Willkommensboni und Freispielen profitieren. Auch regelmäßige Aktionen und Turniere sorgen für zusätzliche Spannung und die Chance auf lukrative Gewinne.
Die Ein- und Auszahlungsmöglichkeiten im Boomerang Casino sind vielseitig und sicher. Spieler können aus einer breiten Palette von Zahlungsmethoden wie Kreditkarten, E-Wallets und Banküberweisungen wählen. Die Transaktionen werden schnell und zuverlässig abgewickelt, sodass Spieler unkompliziert Gelder einzahlen und abheben können.
Einige Spieler haben jedoch auch kritische Punkte bezüglich des Kundensupports im Boomerang Casino geäußert. Manche bemängeln die Antwortzeiten des Supports, während andere Probleme mit der Kommunikation hatten. Es scheint, dass hier noch Verbesserungspotenzial besteht, um den Kundenservice zu optimieren.
Alles in allem zeigt sich das Boomerang Casino als solides und unterhaltsames Online-Casino mit einer Vielzahl von Spielen und attraktiven Bonusangeboten. Die Erfahrungen der Spieler sind größtenteils positiv, wobei vor allem die große Auswahl an Spielen und die sicheren Zahlungsmöglichkeiten gelobt werden. Mit einigen Optimierungen im Kundenservice könnte das Boomerang Casino noch weiter an Beliebtheit gewinnen.
https://boomerangcasino.one/
prednisone generic brand name: by prednisone w not prescription – 60 mg prednisone daily
amoxicillin capsule 500mg price: buy amoxicillin 500mg capsules uk – amoxicillin order online
https://amoxilall.com/# amoxicillin 500 tablet
Das Zet Casino bietet auch im Jahr 2019 großzügige Boni ohne Einzahlung an. Diese Boni ermöglichen es neuen Spielern, das Casino risikofrei kennenzulernen und erste Gewinne zu erzielen, ohne eigenes Geld zu riskieren.
Der no deposit Bonus des Zet Casinos kann in Form von Freispielen oder Bonusguthaben angeboten werden. Spieler müssen sich lediglich registrieren, um diesen Bonus zu erhalten, und können sofort mit dem Spielen beginnen. Die Gewinne aus dem Bonus können in der Regel behalten werden, sobald die Umsatzbedingungen erfüllt wurden.
Es lohnt sich, regelmäßig die Webseite des Zet Casinos zu besuchen, um über aktuelle no deposit Boni informiert zu sein. Diese Boni können eine tolle Möglichkeit sein, das Casino auszuprobieren und erste Erfahrungen zu sammeln. Doch Vorsicht ist geboten, denn nicht jeder Bonus ist auch wirklich empfehlenswert. Vor der Annahme eines Bonus sollten die Bonusbedingungen genau gelesen werden, um unangenehme Überraschungen zu vermeiden.
Insgesamt bietet das Zet Casino seinen Spielern auch im Jahr 2019 attraktive no deposit Boni. Neue Spieler haben die Möglichkeit, das Casino risikofrei kennenzulernen und erste Gewinne zu erzielen. Es lohnt sich, regelmäßig die Webseite des Casinos zu besuchen und sich über aktuelle Aktionen und Boni zu informieren.
https://zetcasino.one/
Das Online Tipico Casino ist eine beliebte Plattform für Glücksspiele im Internet. Es bietet eine Vielzahl von Spielen wie Slots, Roulette, Blackjack und Poker, die von renommierten Softwareanbietern entwickelt wurden. Das Casino zeichnet sich durch sein benutzerfreundliches Design, seine hohe Sicherheit und seine zuverlässigen Zahlungsmethoden aus.
Die Spieler können sowohl über ihren Desktop-Computer als auch über ihre mobilen Geräte auf das Online Tipico Casino zugreifen. Die mobile Version der Plattform bietet eine nahtlose Spielerfahrung, sodass die Nutzer auch unterwegs alle Spiele genießen können.
Ein weiterer großer Vorteil des Online Tipico Casinos sind die großzügigen Bonusangebote. Neue Spieler erhalten oft Willkommensbonusse, Freispiele und andere Promotionen, die ihnen den Einstieg erleichtern. Auch bestehende Spieler werden regelmäßig mit Bonusangeboten belohnt, um ihre Treue zu würdigen.
Das Online Tipico Casino legt großen Wert auf verantwortungsbewusstes Glücksspiel und bietet verschiedene Maßnahmen zur Unterstützung von Spielern mit problematischem Spielverhalten an. Die Spieler können Limits für Einzahlungen und Spielzeiten festlegen oder sich selbst vom Spielen ausschließen, falls nötig.
Insgesamt bietet das Online Tipico Casino eine sichere und unterhaltsame Umgebung fГјr GlГјcksspiel-Fans. Mit einer Vielzahl von Spielen, groГџzГјgigen Boni und verantwortungsbewusstem Spiel ist es eine empfehlenswerte Plattform fГјr alle, die gerne online spielen.
https://tipicocasino.one/
augmentin 625mg brand – cost ethambutol 600mg buy cipro generic
order amoxicillin uk amoxicillin 1000 mg capsule can you buy amoxicillin uk
Bei Tipico Casino gibt es eine Vielzahl von verschiedenen Kategorien, aus denen die Spieler wählen können. Eine der beliebtesten Kategorien ist die der Slots, auch Spielautomaten genannt. Diese Kategorie bietet eine Vielzahl von unterschiedlichen Spielen, von klassischen Früchteslots bis hin zu modernen Video-Slots mit aufregenden Bonusspielen und grafisch beeindruckenden Animationen.
Eine weitere beliebte Kategorie bei Tipico Casino ist die der Tischspiele. Hier finden die Spieler eine groГџe Auswahl an klassischen Casino-Spielen wie Blackjack, Roulette, Poker und Baccarat. Diese Spiele sind bekannt fГјr ihre anspruchsvolle Strategie und ihren Nervenkitzel.
Auch die Kategorie der Live-Casinospiele erfreut sich großer Beliebtheit bei den Spielern. Hier können sie gegen echte Dealer und andere Spieler antreten und das Casino-Erlebnis direkt von zu Hause aus genießen. Die Live-Casinospiele bieten eine authentische Casino-Atmosphäre und sorgen für ein interaktives Spielerlebnis.
Zusätzlich zu diesen Kategorien bietet Tipico Casino auch eine Auswahl an Jackpot-Spielen, bei denen die Spieler die Chance haben, riesige Gewinne zu erzielen. Diese Spiele sind besonders beliebt bei Spielern, die auf der Suche nach dem ganz großen Gewinn sind.
Insgesamt bietet Tipico Casino eine breite Auswahl an verschiedenen Kategorien, die für jeden Spieler etwas Passendes bereithalten. Egal ob man lieber an Spielautomaten, Tischspielen oder Live-Casinospiele spielt, hier findet jeder das Richtige für sich. Mit der hochwertigen Spieleauswahl und der benutzerfreundlichen Benutzeroberfläche bietet das Tipico Casino ein erstklassiges Spielerlebnis für Casino-Fans.
https://tipicocasino.one/
http://amoxilall.shop/# amoxil generic
Разработка сайтов в Астане от https://website-astana.kz/ это разработка веб-сайтов с нуля, а также создание корпоративных сайтов под ключ. Современный дизайн, удобная система управления, SEO-оптимизация, техническая поддержка, отличные цены. Разработка продающих сайтов в Астане от профессионалов. Подробнее на сайте.
Das Boomerang Casino bietet seinen Kunden nicht nur ein umfangreiches Angebot an Online-Spielen, sondern auch die MГ¶glichkeit, auf verschiedene Sportevents zu wetten. Diese Funktion, bekannt als “vedonlyГ¶nti” auf Finnisch, ermГ¶glicht es den Spielern, ihre Lieblingssportarten zu verfolgen und gleichzeitig die Chance zu nutzen, Geld zu gewinnen.
Das Boomerang Casino hat eine Vielzahl von Sportarten im Angebot, auf die gewettet werden kann, darunter Fußball, Basketball, Tennis, Eishockey und viele mehr. Die Spieler können auf verschiedene Aspekte der Spiele wetten, wie zum Beispiel den Gewinner, die Anzahl der Tore, das Endergebnis oder sogar spezifische Ereignisse während des Spiels.
Die vedonlyönti-Funktion im Boomerang Casino ist ideal für diejenigen, die gerne Sport schauen und gleichzeitig ein wenig Nervenkitzel erleben möchten. Die Wetten können einfach über die Website oder die mobile App des Casinos platziert werden, was es den Spielern ermöglicht, jederzeit und überall auf ihre Lieblingssportarten zu wetten.
Darüber hinaus bietet das Boomerang Casino seinen Kunden attraktive Quoten und Boni, die es noch spannender machen, auf Sportevents zu wetten. Die Spieler haben auch die Möglichkeit, Live-Wetten abzugeben, um während des Spiels ihre Einsätze zu platzieren und ihre Gewinnchancen zu erhöhen.
Insgesamt bietet das Boomerang Casino eine unterhaltsame und aufregende Möglichkeit, Sportereignisse zu verfolgen und gleichzeitig die Chance zu haben, Geld zu gewinnen. Wenn Sie also ein Sportfan sind und gerne wetten, ist das Boomerang Casino die ideale Wahl für Sie. Besuchen Sie noch heute die Website und beginnen Sie mit dem vedonlyönti-Spaß!
https://boomerangcasino.one/
Zet Casino 30 – Der perfekte Ort für alle Glücksspiel-Fans
Das Zet Casino 30 ist eine neue Online-Casino-Plattform, die speziell für alle Glücksspiel-Enthusiasten entwickelt wurde. Mit einer breiten Auswahl an Spielen, großzügigen Boni und einer benutzerfreundlichen Oberfläche ist Zet Casino 30 der perfekte Ort, um Ihr Glück zu versuchen.
Eine der herausragenden Eigenschaften von Zet Casino 30 ist die beeindruckende Auswahl an Spielen. Mit Hunderten von Slot-Spielen, Tischspielen und Live-Dealer-Spielen gibt es hier für jeden Geschmack etwas zu finden. Egal, ob Sie ein Fan von klassischen Slot-Spielen wie Starburst oder neuen Veröffentlichungen von Top-Entwicklern wie NetEnt sind, im Zet Casino 30 werden Sie sicher fündig.
Darüber hinaus bietet Zet Casino 30 großzügige Boni und Aktionen für alle Spieler. Von einem Willkommensbonus für neue Mitglieder bis hin zu wöchentlichen Sonderaktionen und Treueprogrammen – hier werden Sie regelmäßig belohnt. Mit diesen zusätzlichen Boni haben Sie die Chance, Ihre Gewinne zu maximieren und noch mehr Spaß am Spielen zu haben.
Die Benutzeroberfläche von Zet Casino 30 ist ebenfalls sehr benutzerfreundlich gestaltet. Dank der intuitiven Navigation und der klaren Struktur finden Sie sich schnell zurecht und können direkt mit dem Spielen loslegen. Das Casino ist auch für mobile Geräte optimiert, sodass Sie auch unterwegs problemlos spielen können.
Alles in allem ist Zet Casino 30 eine großartige Wahl für alle Glücksspiel-Fans. Mit einer riesigen Auswahl an Spielen, großzügigen Boni und einer benutzerfreundlichen Oberfläche bietet dieses Online-Casino alles, was das Herz begehrt. Also, worauf warten Sie noch? Registrieren Sie sich noch heute im Zet Casino 30 und lassen Sie die Walzen tanzen!
https://zetcasino.one/
http://amoxilall.shop/# amoxicillin 500mg for sale uk
cost of amoxicillin 30 capsules amoxicillin 30 capsules price generic for amoxicillin
augmentin 625mg sale – clavulanate canada buy cipro for sale
ЗАО «Автономный ЭнергоСервис» в компании работают истинные профессионалы. В короткий срок реализуем решения любой сложности с полезностью для заказчиков. Предоставим профессиональные консультации и гарантируем быстрые поставки энергетического оборудования. https://mototech.ru – сайт, где можно найти доброжелательные отзывы клиентов. Вы приятно удивитесь качеством продукции, высокой культурой общения персонала и адекватной ценовой политикой. Обращайтесь именно к нам, мы готовы быть надежным и долгосрочным партнером.
Wenn es um das Auszahlen von Gewinnen im Casino geht, ist Tipico eine beliebte Wahl fГјr viele Spieler. Mit ihrem klassischen Casino-Angebot und einer Vielzahl von Spielen haben sie eine treue Fangemeinde aufgebaut.
Tipico bietet verschiedene Möglichkeiten für Spieler, um ihre Gewinne auszahlen zu lassen. Ein klassischer Weg ist die Auszahlung per Banküberweisung. Spieler können einfach ihre Bankdaten angeben und ihre Gewinne werden sicher und schnell auf ihr Konto überwiesen.
Eine weitere Möglichkeit ist die Auszahlung über E-Wallets wie PayPal oder Skrill. Diese Optionen sind besonders beliebt, da sie eine schnelle und einfache Möglichkeit bieten, um an sein Geld zu gelangen. Spieler müssen einfach ihre E-Mail-Adresse angeben und können ihre Gewinne direkt auf ihr E-Wallet erhalten.
Darüber hinaus bietet Tipico auch die Möglichkeit, seine Gewinne in bar in einem der vielen Tipico-Shops abzuholen. Diese Option ist besonders praktisch für Spieler, die lieber persönlich ihr Geld in Empfang nehmen möchten.
Insgesamt bietet Tipico eine Vielzahl von sicheren und bequemen Möglichkeiten, um Gewinne im klassischen Casino auszuzahlen. Spieler können sich darauf verlassen, dass ihre Gewinne schnell und zuverlässig auf ihr Konto überwiesen werden. Mit einer breiten Auswahl an Spielen und einer benutzerfreundlichen Plattform ist Tipico eine hervorragende Wahl für jeden, der gerne im Casino spielt.
https://tipicocasino.one/
Gogo casino com är en populär online spelplattform där spelare kan njuta av en mängd olika casinospel. Genom att erbjuda en säker och spännande spelupplevelse har Gogo casino com blivit ett av de mest eftertraktade online casinona på marknaden.
En av de främsta fördelarna med Gogo casino com är det breda utbudet av spel som erbjuds. Oavsett om du gillar klassiska slots, bordsspel eller live casinospel finns det något för alla på denna plattform. Dessutom uppdateras spelbiblioteket regelbundet med de senaste och mest populära spelen på marknaden.
Förutom det imponerande spelutbudet erbjuder Gogo casino com också generösa bonusar och kampanjer för sina spelare. Nya spelare kan dra nytta av en välkomstbonus vid sin första insättning, medan befintliga spelare kan ta del av regelbundna erbjudanden och belöningar.
En annan viktig faktor som gör Gogo casino com till en attraktiv spelplattform är dess användarvänliga design och lättanvända gränssnitt. Spelare kan enkelt navigera på plattformen och hitta sina favoritspel utan problem.
Slutligen är säkerheten och integriteten hos spelarna av högsta prioritet för Gogo casino com. Plattformen använder avancerad krypteringsteknik för att säkerställa att alla transaktioner och personuppgifter förblir skyddade.
Sammanfattningsvis är Gogo casino com en utmärkt spelplattform för spelare som letar efter en spännande och säker spelupplevelse. Med sitt omfattande spelutbud, generösa bonusar och användarvänliga design har Gogo casino com blivit ett av de ledande online casinona på marknaden. Besök gogocasino.com idag för att uppleva allt vad de har att erbjuda!
https://gogocasino.one
https://clomidall.shop/# can i order generic clomid
Boomerang Casino Bonus: Ein Bonus, der zurГјckkommt!
Das Boomerang Casino bietet seinen Spielern eine einzigartige Bonusmöglichkeit, die sich von anderen Online-Casinos abhebt. Der Boomerang Casino Bonus ist ein besonderes Angebot, das Spielern die Möglichkeit gibt, ihre Einzahlungen zu vervielfachen und zusätzliche Freispiele zu erhalten.
Wie funktioniert der Boomerang Casino Bonus? Ganz einfach: Spieler können auf ihre Einzahlungen einen bestimmten Prozentsatz als Bonus erhalten. Das bedeutet, dass sie mehr Geld zum Spielen zur Verfügung haben und somit ihre Gewinnchancen erhöhen können. Aber das ist noch nicht alles – zusätzlich zu dem Bonusgeld erhalten Spieler auch noch Freispiele, die sie für ausgewählte Spielautomaten verwenden können.
Das Besondere am Boomerang Casino Bonus ist, dass er nicht einfach nur einmalig ist. Im Gegenteil, er „kommt zurück“ – wie ein Boomerang eben. Das bedeutet, dass Spieler regelmäßig von diesem Bonus profitieren können, entweder durch Einzahlungsboni oder Freispielaktionen. Auf diese Weise können Spieler immer wieder von zusätzlichen Gewinnmöglichkeiten profitieren und ihr Spielerlebnis im Boomerang Casino noch spannender gestalten.
Um den Boomerang Casino Bonus zu erhalten, müssen Spieler lediglich eine Einzahlung tätigen und den entsprechenden Bonuscode angeben. Danach wird der Bonus automatisch gutgeschrieben und die Spieler können sofort mit dem Spielen beginnen.
Insgesamt ist der Boomerang Casino Bonus eine tolle Möglichkeit für Spieler, ihr Spielerlebnis zu verbessern und zusätzliche Gewinne zu erzielen. Wer also nach einem Online-Casino mit attraktiven Bonusangeboten sucht, sollte sich das Boomerang Casino genauer ansehen. Viel Spaß und viel Glück beim Spielen!
https://boomerangcasino.one/
Gogo Casino är ett populärt online casino som lanserades i Finland år 2019. Med ett stort urval av spelautomater, live casinospel och bordsspel har Gogo Casino snabbt blivit ett favoritval för många spelare i Finland.
En av anledningarna till Gogo Casinos popularitet är dess användarvänliga och moderna design. Hemsidan är lätt att navigera och spelarna kan enkelt hitta sina favoritspel genom att söka efter dem eller använda kategorierna som erbjuds.
Gogo Casino tar ansvar för att erbjuda sina spelare en säker och rättvis spelupplevelse. De erbjuder en säker betalningsmetod via Trustly, vilket gör att spelarna kan göra insättningar och uttag snabbt och säkert.
En annan fördel med Gogo Casino är deras generösa bonuserbjudanden och kampanjer. Nya spelare kan ta del av en välkomstbonus vid sin första insättning och befintliga spelare kan dra nytta av regelbundna bonusar och belöningar.
Sammanfattningsvis är Gogo Casino ett utmärkt val för finska spelare som är ute efter en spännande och underhållande spelupplevelse. Med sitt stora spelutbud, användarvänliga design och säkra betalningsmetoder är det inte konstigt att Gogo Casino har blivit en favorit bland många finska spelare. Besök Gogo Casino idag och upplev spänningen själv!
https://gogocasino.one
can i order generic clomid online buy clomid can you buy generic clomid
Автосалон Hyundai (Хёндэ) в Санкт-Петербурге https://hyundai-parnas.ru/ это возможность купить автомобили Hyundai в наличии. Зайдите на сайт, ознакомьтесь с модельным рядом, спецпредложениями или воспользуйтесь конфигуратором. Высокий уровень обслуживания и полный спектр услуг от ИАТ Парнас.
Gogo Casino är en relativt ny online casino som har växt i popularitet i Finland. Med sitt enkla och minimalistiska design har de lyckats locka många spelare som söker en smidig och underhållande spelupplevelse.
Gogo Casino skiljer sig från många andra online casinon genom att de fokuserar på att erbjuda en snabb och enkel registreringsprocess, där spelare inte behöver skapa ett konto för att spela. Istället verifierar de sig med BankID vilket innebär att insättningar och uttag sker på nolltid.
En annan fördel med Gogo Casino är deras imponerande utbud av spel från några av de bästa spelleverantörerna på marknaden. Här hittar spelare allt från klassiska spelautomater till bordsspel och live casino.
Gogo Casino erbjuder också generösa bonusar och kampanjer som lockar till sig både nya och återkommande spelare. Deras kundtjänst är tillgänglig dygnet runt för att hjälpa till med eventuella frågor eller problem som kan uppstå under spel.
Sammanfattningsvis har Gogo Casino blivit en populär destination för finska spelare som letar efter en snabb, smidig och rolig spelupplevelse. Med sitt stora utbud av spel, generösa bonusar och effektiv kundtjänst har de tagit online casino upplevelsen till en helt ny nivå.
https://gogocasino.one
http://amoxilall.shop/# buy cheap amoxicillin online
Im Jahr 2022 bietet das Boomerang Casino spannende No Deposit Bonus Codes für alle Neukunden an. Mit diesen Codes können Spieler ohne vorherige Einzahlung eine Vielzahl von Casino-Spielen ausprobieren und dabei echtes Geld gewinnen.
No Deposit Bonus Codes sind eine großartige Möglichkeit, um ein Online-Casino kennenzulernen, ohne dabei eigenes Geld riskieren zu müssen. Mit den Codes können Spieler verschiedene Spiele wie Slots, Roulette, Blackjack oder Poker ausprobieren und ihre Gewinnchancen testen.
Um von den No Deposit Bonus Codes im Boomerang Casino zu profitieren, müssen Spieler lediglich ein Konto erstellen und den entsprechenden Code bei der Registrierung eingeben. Anschließend können sie sofort mit dem Spielen beginnen und sich über mögliche Gewinne freuen.
Es ist jedoch wichtig zu beachten, dass No Deposit Boni oft bestimmten Umsatzbedingungen unterliegen, die erfüllt werden müssen, bevor eine Auszahlung möglich ist. Daher sollten Spieler immer die Bonusbedingungen sorgfältig durchlesen, um Missverständnisse zu vermeiden.
Insgesamt bietet das Boomerang Casino mit seinen No Deposit Bonus Codes eine tolle Gelegenheit, um das Casino und seine Spiele risikofrei kennenzulernen und vielleicht sogar den ein oder anderen Gewinn zu erzielen. Wer also auf der Suche nach einem spannenden Online-Casino-Erlebnis ist, sollte die No Deposit Bonus Codes im Boomerang Casino auf jeden Fall ausprobieren. Viel SpaГџ und viel GlГјck beim Spielen!
https://boomerangcasino.one/
cheap amoxil pills – purchase erythromycin pill cipro 1000mg usa
Gogo Casino är ett populärt online casino som erbjuder spelare möjligheten att spela sina favoritspel och vinna stora pengar. Men nyligen har det kommit en oroande nyhet att Gogo Casino inte betalar ut vinster till sina spelare.
Många spelare har klagat över att de inte har fått sina vunna pengar utbetalda från Gogo Casino. Trots att de har vunnit och följt alla regler och villkor, har deras uttag blivit nekade eller bara ignorerade av casinot.
Detta har självklart skapat stor frustration och ilska bland spelarna som har blivit lurade på sina pengar. Många väljer nu att undvika att spela på Gogo Casino och istället leta efter andra pålitliga alternativ där de kan känna sig trygga med sina pengar.
Det är viktigt att spelare är medvetna om risken att spela på oseriösa casinon som inte följer reglerna och inte betalar ut vinster. Det är därför viktigt att alltid göra noggrann research innan man väljer att spela på ett online casino för att undvika att bli lurad.
Om du har blivit drabbad av att inte få dina vinster utbetalda från Gogo Casino, rekommenderar vi att du kontaktar Spelinspektionen för att rapportera ditt ärende och få hjälp att lösa situationen. Det är viktigt att visa gemensamt mot oseriösa aktörer inom spelbranschen för att skydda spelarnas rättigheter och intressen.
Sammanfattningsvis är det viktigt att vara försiktig och uppmärksam när man väljer vilket online casino man ska spela på för att undvika att hamna i en liknande situation som Gogo Casino-spelarna. Var alltid noggrann med att kontrollera casinots licens och rykte innan du lägger dina pengar där. Lycka till!
https://gogocasino.one
buy generic amoxicillin for sale – ceftin 250mg generic buy cipro 1000mg for sale
Zet Casino Sportwetten: Eine aufregende Möglichkeit zum Wetten
Sportwetten erfreuen sich weltweit großer Beliebtheit und bieten den Fans die Möglichkeit, ihren Lieblingssport noch spannender zu gestalten. Mit Zet Casino Sportwetten erhalten auch die Kunden des beliebten Online-Casinos die Möglichkeit, auf eine Vielzahl von Sportveranstaltungen zu wetten und so ihr Glück zu versuchen.
Zet Casino bietet eine breite Auswahl an Sportarten, darunter Fußball, Tennis, Basketball, Eishockey und viele mehr. Die Kunden können aus einer Vielzahl von Wettoptionen wählen, darunter Einzelwetten, Kombiwetten und Systemwetten. Mit attraktiven Quoten und einem benutzerfreundlichen Interface ist es einfach, seine Wetten zu platzieren und den Nervenkitzel des Sports zu erleben.
Darüber hinaus bietet Zet Casino seinen Kunden verschiedene Bonusangebote und Promotionen, die das Wetten noch lohnenswerter machen. Von Willkommensboni über Cashback-Angebote bis hin zu speziellen Aktionen für bestimmte Sportveranstaltungen gibt es immer wieder spannende Möglichkeiten, zusätzliche Gewinne zu erzielen.
Für Kunden, die auch gerne im Online-Casino spielen, bietet Zet Casino eine nahtlose Integration von Sportwetten und Casino-Spielen. So können die Kunden nicht nur auf Sportveranstaltungen wetten, sondern auch ihr Glück an Spielautomaten, Tischspielen und Live-Dealer-Spielen versuchen.
Insgesamt bietet Zet Casino Sportwetten eine unterhaltsame und aufregende Möglichkeit, auf Sportveranstaltungen zu wetten und mit etwas Glück attraktive Gewinne zu erzielen. Mit einer großen Auswahl an Sportarten, attraktiven Quoten und spannenden Promotionen ist Zet Casino die perfekte Wahl für alle Fans von Sportwetten.
https://zetcasino.one/
https://zithromaxall.com/# zithromax prescription online
Gogo Casino kundsupport är en viktig del av spelupplevelsen för spelarna på denna populära onlinekasinoplattform. Med ett dedikerat team av professionella och vänliga supportrepresentanter är du alltid i trygga händer när du spelar på Gogo Casino.
Kundsupportteamet på Gogo Casino är tillgängligt via livechatt, e-post och telefon för att hjälpa dig med alla frågor eller bekymmer du kan ha. Oavsett om det handlar om att lösa problem med insättningar eller uttag, förklara regler och villkor för bonusar eller bara ge allmän information om kasinot, kommer de att göra sitt bästa för att se till att du är nöjd.
En av de stora fördelarna med Gogo Casino kundsupport är att de är tillgängliga dygnet runt, sju dagar i veckan. Det innebär att oavsett när du spelar eller vilka problem du stöter på, kommer det alltid att finnas någon där för att hjälpa dig. Detta är särskilt viktigt för alla som spelar med riktiga pengar och vill ha trygghet att deras konton och transaktioner hanteras på ett säkert sätt.
Om du letar efter en onlinekasinoplattform med en pålitlig och effektiv kundsupport, är Gogo Casino definitivt ett bra val. Med deras dedikerade team av supportrepresentanter och deras tillgänglighet dygnet runt kan du vara säker på att du kommer att få den hjälp och support du behöver för en trevlig spelupplevelse. Besök Gogo Casino idag och upplev själv den fantastiska kundsupporten som de erbjuder.
https://gogocasino.one
zithromax capsules zithromax z-pak price without insurance zithromax z-pak
prednisone over the counter south africa: prednisone nz – buy prednisone without a prescription best price
generic zithromax online paypal: buy zithromax online cheap – zithromax 500mg over the counter
acarbose fructose
Bonus Bedingungen im Tipico Casino
Das Tipico Casino bietet seinen Kunden regelmäßig attraktive Bonusangebote an, um das Spielerlebnis noch spannender zu gestalten. Doch bevor man sich über einen Bonus freuen kann, sollten die Bonusbedingungen genau durchgelesen werden, um Missverständnisse oder Enttäuschungen zu vermeiden.
Die wichtigsten Bonusbedingungen im Tipico Casino sind die Umsatzbedingungen. Diese geben an, wie oft der Bonus und/oder Einzahlungsbetrag umgesetzt werden müssen, bevor eine Auszahlung möglich ist. Je nach Bonus kann dieser Wert variieren, deshalb ist es ratsam, immer einen Blick in die Bonusbedingungen zu werfen.
Ein weiterer wichtiger Punkt sind die Spiele, die zum ErfГјllen der Umsatzbedingungen beitragen. Nicht alle Spiele im Casino tragen gleich viel dazu bei, manche sind sogar komplett ausgeschlossen. Es ist also wichtig, zu wissen, welche Spiele man spielen kann, um den Bonus freizuspielen.
Ein weiterer Aspekt, der bei den Bonusbedingungen berГјcksichtigt werden sollte, sind eventuelle zeitliche Begrenzungen. Oftmals haben Boni ein Ablaufdatum, bis zu dem sie genutzt werden mГјssen. Es ist also wichtig, den Zeitrahmen zu beachten, um den Bonus nicht zu verlieren.
Zusätzlich sollten auch die Mindesteinzahlungsbeträge für die jeweiligen Boni beachtet werden. Oftmals ist es erforderlich, eine bestimmte Summe einzuzahlen, um den Bonus zu erhalten. Hier lohnt es sich, die Einzahlungsbedingungen vorab zu prüfen.
Insgesamt sind die Bonusbedingungen im Tipico Casino fair und transparent gestaltet, dennoch ist es ratsam, sie genau zu lesen und zu verstehen, bevor man einen Bonus in Anspruch nimmt. So kann man sicherstellen, dass man das Beste aus dem Angebot herausholt und sein Spielerlebnis optimal genieГџen kann.
https://tipicocasino.one/
Популярная компания Скай Лайн Консалтинг предлагает весь спектр бухгалтерского сопровождения. У нас собрана команда истинных профессионалов. Все специалисты имеют приличный опыт работы и профильное образование. Доверьте им кадровое делопроизводство и оформление юридических документов. https://slc-company.ru/ – сайт, где есть возможность в любое время посмотреть отзывы благодарных клиентов. Обращайтесь к нам, гарантируем грамотное и быстрое решение вопросов. Стремимся к взаимовыгодному сотрудничеству!
https://amoxilall.shop/# amoxicillin for sale
Das Boomerang Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und Möglichkeiten zum Gewinnen bietet. Eine wichtige Frage, die viele Spieler haben, betrifft die Auszahlungen im Boomerang Casino. Wie funktioniert die Auszahlung von Gewinnen und wie lange dauert es, bis das Geld auf dem Konto des Spielers ist?
Die Auszahlung von Gewinnen im Boomerang Casino ist in der Regel sehr einfach und unkompliziert. Spieler können zwischen verschiedenen Zahlungsmethoden wie Kreditkarten, E-Wallets oder Banküberweisungen wählen. Nachdem ein Spieler einen Gewinn erzielt hat, kann er in seinem Konto die Auszahlung beantragen. Dabei muss der Spieler auf die jeweiligen Bedingungen und Limits für Auszahlungen achten.
Die Dauer der Auszahlung im Boomerang Casino hängt von der gewählten Zahlungsmethode und den internen Bearbeitungszeiten des Casinos ab. In der Regel werden Auszahlungen innerhalb von 1-3 Werktagen bearbeitet. Bei E-Wallets kann das Geld oft noch schneller auf dem Konto des Spielers verfügbar sein. Bei Banküberweisungen kann die Bearbeitungszeit jedoch etwas länger dauern.
Es ist wichtig zu beachten, dass das Boomerang Casino Sicherheitsüberprüfungen durchführt, um die Identität und die Echtheit der Spieler zu überprüfen. Diese Überprüfungen können die Auszahlungszeit ebenfalls beeinflussen. Spieler müssen daher Geduld haben und die Anforderungen des Casinos erfüllen, um ihre Gewinne ohne Verzögerungen zu erhalten.
Insgesamt kann gesagt werden, dass die Auszahlungen im Boomerang Casino zuverlässig und sicher sind. Spieler können sich darauf verlassen, dass ihre Gewinne schnell und zuverlässig ausgezahlt werden. Es ist ratsam, die Bedingungen für Auszahlungen im Casino zu überprüfen und die richtige Zahlungsmethode zu wählen, um eine reibungslose Abwicklung sicherzustellen.
https://boomerangcasino.one/
OMODA https://omoda-autoprestus.ru/ – купить автомобиль ОМОДА в Москве у официального дилера АВТОПРЕСТУС. Зайдите на сайт – ознакомьтесь с модельным рядом, акциями на авто и узнайте больше о моделях производителя. Подробнее на сайте.
zithromax price canada average cost of generic zithromax buy zithromax without presc
qiyezp.com
사실, Suleiman은 이 말의 아첨을 모르는 것이 아닙니다.
http://amoxilall.com/# amoxicillin generic
Zet Casino Bonuscode: Maximales Spielerlebnis mit zusätzlichem Guthaben
Das Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und Bonusaktionen für seine Spieler anbietet. Ein besonders attraktives Angebot für Neukunden ist der Zet Casino Bonuscode, der zusätzliches Guthaben auf das Spielerkonto bringt.
Der Zet Casino Bonuscode wird bei der Registrierung oder Einzahlung im Online-Casino eingegeben und aktiviert. Mit diesem Code können Spieler von lukrativen Angeboten profitieren, wie zum Beispiel einem Willkommensbonus, Freispielen oder Cashback-Aktionen.
Durch die Verwendung des Zet Casino Bonuscodes haben Spieler die Möglichkeit, ihr Spielerlebnis zu maximieren und ihre Gewinnchancen zu erhöhen. Mit zusätzlichem Guthaben können sie länger spielen und mehr Spiele ausprobieren, ohne dabei ihr eigenes Geld zu riskieren.
Um den Zet Casino Bonuscode zu nutzen, sollten Spieler die jeweiligen Bonusbedingungen genau durchlesen und sicherstellen, dass sie alle Anforderungen erfüllen. So können sie das Bonusguthaben optimal nutzen und von den attraktiven Bonusaktionen profitieren.
Insgesamt bietet der Zet Casino Bonuscode Spielern die Möglichkeit, ihr Casinoerlebnis auf ein neues Level zu heben und von lukrativen Angeboten zu profitieren. Wer also auf der Suche nach zusätzlichem Guthaben und spannenden Bonusaktionen ist, sollte den Zet Casino Bonuscode nicht verpassen.
https://zetcasino.one/
Zet Casino: Kostenlose Freispiele
Zet Casino ist eine Online-Spielplattform, die Spielern ein aufregendes und unterhaltsames Spielerlebnis bietet. Neben einer Vielzahl von Casino-Spielen und Live-Casino-Optionen bietet Zet Casino auch eine groГџzГјgige Palette von Bonusangeboten, darunter kostenlose Freispiele, auch bekannt als “ilmaiskierrokset”.
Kostenlose Freispiele sind eine beliebte Form von Casino-Boni, die es Spielern ermöglichen, ausgewählte Spielautomaten kostenlos zu spielen, ohne ihr eigenes Geld einsetzen zu müssen. Bei Zet Casino können Spieler kostenlose Freispiele als Teil ihres Willkommensbonus erhalten oder durch laufende Promotionen und Aktionen im Casino.
Um kostenlose Freispiele zu erhalten, müssen Spieler oft eine Mindesteinzahlung vornehmen oder bestimmte Bonusbedingungen erfüllen. Diese Bedingungen können von Casino zu Casino variieren, daher ist es wichtig, die Geschäftsbedingungen sorgfältig zu lesen, um sicherzustellen, dass alle Anforderungen erfüllt sind.
Sobald Spieler ihre kostenlosen Freispiele erhalten haben, können sie diese verwenden, um ausgewählte Spielautomaten im Zet Casino zu spielen und möglicherweise echtes Geld zu gewinnen. Kostenlose Freispiele sind eine großartige Möglichkeit, neue Spiele auszuprobieren, ohne Risiko einzugehen, und können Spielern die Möglichkeit geben, ihre Gewinne zu steigern.
Insgesamt bieten kostenlose Freispiele bei Zet Casino den Spielern eine zusätzliche Chance auf Gewinne und erhöhen den Spaß und die Spannung des Spielens. Wenn Sie also auf der Suche nach einem aufregenden Casino-Erlebnis sind, das eine Vielzahl von Bonusangeboten und auch ilmaiskierrokset bietet, sollten Sie definitiv Zet Casino ausprobieren. Viel Glück beim Spielen! Prost!
https://zetcasino.one/
https://prednisoneall.com/# prednisone purchase canada
Boomerang Casino ist eine beliebte Online-GlГјcksspielplattform, die ihren Spielern eine Vielzahl von Spielen und UnterhaltungsmГ¶glichkeiten bietet. Das Casino bietet eine breite Palette von Spielen, darunter Spielautomaten, Tischspiele, Live-Casino-Spiele und vieles mehr. Die Spieler kГ¶nnen aus einer Vielzahl von Spielen wГ¤hlen, die von bekannten Spieleanbietern wie NetEnt, Microgaming, Play’n GO und vielen anderen stammen.
Boomerang Casino zeichnet sich durch seine benutzerfreundliche Oberfläche und sein ansprechendes Design aus. Die Spieler können leicht zwischen den verschiedenen Spielen navigieren und ihre Lieblingsspiele finden. Das Casino bietet auch eine Vielzahl von Zahlungsmethoden, darunter Kreditkarten, E-Wallets und Banküberweisungen, um sicherzustellen, dass die Spieler Ein- und Auszahlungen bequem durchführen können.
Die Spieler, die Boomerang Casino ausprobiert haben, haben positive Erfahrungen gemacht und loben die Vielfalt der Spiele, die Freundlichkeit des Kundensupports und die schnellen Auszahlungen. Viele Spieler schätzen auch die regelmäßigen Bonusangebote und Promotionen, die das Casino seinen Spielern bietet.
Insgesamt haben die Spieler, die Boomerang Casino ausprobiert haben, positive Erfahrungen gemacht und empfehlen die Plattform weiter. Wenn Sie auf der Suche nach einer unterhaltsamen und sicheren Online-GlГјcksspielplattform sind, sollten Sie Boomerang Casino eine Chance geben und Ihre eigenen Erfahrungen sammeln.
https://boomerangcasino.one/
Фильмок тв предоставляет для вас лучшие фильмы. Вы можете в любое время смотреть их онлайн совершенно бесплатно. На странице любого фильма расписаны: страна, актерский состав, год, жанр, режиссер. Это дает возможность принять правильное решение о выборе кинокартины. https://filmok.tv – сайт, где имеется удобный поиск, воспользуйтесь им. Сериалы и фильмы ждут вас. Мы гарантируем отменный звук и картинку. Заходите прямо сейчас на наш портал, выбирайте подходящий фильм и наслаждайтесь им!
purchase amoxicillin 500 mg cost of amoxicillin prescription generic amoxicillin
Gogo Casino Bonus Utan Insättning
Gogo Casino Г¤r ett populГ¤rt online casino som erbjuder spelare en mГ¤ngd olika spel och bonusar att njuta av. En av de mest eftertraktade bonusarna Г¤r den sГҐ kallade “no deposit bonus” – en bonus som spelarna kan ta emot utan att behГ¶va gГ¶ra en insГ¤ttning pГҐ sitt spelkonto.
Med en no deposit bonus från Gogo Casino kan spelare prova lyckan och spela sina favoritspel utan att behöva riskera sina egna pengar. Det är ett utmärkt sätt att bekanta sig med casinot och dess spelutbud innan man bestämmer sig för att sätta in riktiga pengar.
För att ta del av en no deposit bonus hos Gogo Casino behöver spelaren vanligtvis skapa ett konto och verifiera sin identitet. Därefter kan bonusen aktiveras och spelaren kan börja spela utan att behöva sätta in egna pengar.
Det är viktigt att notera att no deposit bonusar oftast kommer med vissa regler och villkor som spelaren måste följa för att kunna ta ut eventuella vinster. Det kan vara insatskrav, tidsbegränsningar eller restriktioner på vilka spel som bidrar till omsättningskraven.
Sammanfattningsvis är en no deposit bonus från Gogo Casino en utmärkt möjlighet för spelare att utforska casinots spelutbud och förhoppningsvis vinna lite extra pengar utan att behöva riskera sina egna pengar. Var noga med att läsa bonusvillkoren noggrant för att undvika eventuella missförstånd och maximera dina vinstchanser. Lycka till!
https://gogocasino.one
http://amoxilall.com/# amoxicillin tablet 500mg
Das m.zet Casino: Ein neuer Hotspot fГјr GlГјcksspielfreunde
Das m.zet Casino ist ein neuer Anbieter auf dem Markt fГјr Online-GlГјcksspiele und hat in den letzten Monaten immer mehr Aufmerksamkeit auf sich gezogen. Mit einer breiten Auswahl an Spielen und einer benutzerfreundlichen Plattform, lockt das m.zet Casino Spieler aus der ganzen Welt an.
Eine der größten Attraktionen des m.zet Casinos sind die zahlreichen Spielautomaten, die für jeden Geschmack und jedes Budget etwas bieten. Von klassischen Früchteslots bis hin zu aufregenden Video-Slots mit tollen Bonusfunktionen, ist für jeden etwas dabei. Darüber hinaus bietet das m.zet Casino auch eine Vielzahl an Tischspielen wie Blackjack, Roulette und Baccarat an.
Neben dem breiten Spielangebot überzeugt das m.zet Casino auch durch seine großzügigen Bonusangebote und Aktionen. Neue Spieler werden mit einem Willkommensbonus belohnt, der ihnen zusätzliches Guthaben oder Freispiele beschert. Zudem gibt es regelmäßige Promotionen und Turniere, bei denen Spieler zusätzliche Preise gewinnen können.
Die Sicherheit der Spieler steht im m.zet Casino an erster Stelle. Die Plattform ist durch hochmoderne Verschlüsselungstechnologien geschützt, um sicherzustellen, dass alle Transaktionen und persönlichen Daten der Spieler sicher sind. Zudem verfügt das m.zet Casino über eine Lizenz von einer renommierten Glücksspielbehörde, die die Einhaltung strenger Auflagen garantiert.
Insgesamt bietet das m.zet Casino ein unterhaltsames und sicheres Spielerlebnis fГјr GlГјcksspielfreunde. Mit seinem umfangreichen Spielangebot, groГџzГјgigen Boni und einer benutzerfreundlichen Plattform ist das m.zet Casino definitiv einen Besuch wert.
https://zetcasino.one/
Купить автомобиль Jaecoo в салоне официального дилера ИАТ https://jaecoo-iat.ru/ это возможность выбрать идеальный автомобиль JAECOO для себя. Узнайте цены в России на автомобили марки JAECOO. Выгодные условия покупки, гибкие цены и программы кредитования на покупку Джейку. Подробнее на сайте.
Gogo casino email är ett sätt för spelare att hålla sig uppdaterade om de senaste kampanjerna och erbjudandena som erbjuds av Gogo casino. Genom att prenumerera på casinots nyhetsbrev får spelare tillgång till exklusiva bonusar, free spins och andra belöningar som kan öka deras vinstchanser och spelupplevelse.
Att prenumerera på Gogo casino email är enkelt och kostnadsfritt. Allt du behöver göra är att ange din e-postadress på casinots hemsida och bekräfta din prenumeration genom att klicka på en länk i det bekräftelsemejl som skickas till dig. När du har bekräftat din prenumeration kommer du regelbundet att få e-postmeddelanden med information om kommande kampanjer, tävlingar och andra spännande evenemang hos Gogo casino.
Genom att hålla sig uppdaterad via Gogo casino email kan spelare dra nytta av exklusiva erbjudanden och belöningar som är tillgängliga endast för prenumeranter. Det kan vara allt från insättningsbonusar och cashback-erbjudanden till tävlingar och turneringar där spelare har chansen att vinna fantastiska priser. Genom att delta i dessa kampanjer kan spelare öka sina vinstchanser och få en ännu mer underhållande spelupplevelse på Gogo casino.
Sammanfattningsvis är Gogo casino email ett utmärkt sätt för spelare att hålla sig uppdaterade om de senaste kampanjerna och erbjudandena som erbjuds av casinot. Genom att prenumerera på nyhetsbrevet kan spelare dra nytta av exklusiva belöningar och öka sina vinstchanser samtidigt som de får en mer personlig och anpassad spelupplevelse på Gogo casino. Så varför inte anmäla sig redan idag och ta del av alla fördelar som Gogo casino email har att erbjuda?
https://gogocasino.one
Störung im Casino
Am vergangenen Wochenende ist es in einem renommierten Casino zu einer unerwarteten Störung gekommen. Besucher, die ihr Glück an den verschiedenen Spieltischen versuchen wollten, wurden plötzlich mit technischen Problemen konfrontiert. Die Automaten liefen nicht mehr einwandfrei, die Kartenspiele wurden abgebrochen und die Roulettekugel blieb stehen.
Die Ursache für die Störung liegt noch im Dunkeln. Ein Sprecher des Casinos erklärte, dass das technische Team bereits daran arbeite, das Problem zu beheben. Bis dahin sei der Betrieb eingeschränkt und einige Bereiche des Casinos seien vorübergehend geschlossen.
Die Gäste des Casinos zeigten sich enttäuscht über die unerwartete Störung. Viele hatten sich auf einen spaßigen Abend voller Spannung und Unterhaltung gefreut und wurden nun enttäuscht. Einige Besucher verließen das Casino frustriert, während andere geduldig auf die Behebung des Problems warteten.
Für das Casino bedeutet die Störung nicht nur einen finanziellen Verlust, sondern auch einen Imageschaden. Die Professionalität und Zuverlässigkeit des Casinos stehen auf dem Spiel und müssen dringend wiederhergestellt werden.
Die Verantwortlichen des Casinos entschuldigten sich bei den Gästen für die Unannehmlichkeiten und versicherten, dass sie alles tun würden, um das Problem so schnell wie möglich zu lösen. Die Besucher können nur hoffen, dass die Störung bald behoben wird und sie wieder ungestört ihrer Spielfreude nachgehen können.
https://zetcasino.one/
Gogo Casino är ett relativt nytt online casino som lanserades år 2019. Trots att det är en relativt ny aktör på marknaden har det redan blivit mycket populärt bland svenska spelare. En av anledningarna till dess popularitet är de generösa bonusarna och erbjudandena som de erbjuder till sina spelare.
En flashback till när Gogo Casino först lanserades visar att det snabbt fick ett gott rykte för sin användarvänlighet och smidiga spelupplevelse. Det är ett casino som fokuserar på att erbjuda en enkel och snabb spelupplevelse utan krångliga registreringsprocesser eller långa uttagsprocesser.
Gogo Casino flashback visar också att de har ett stort utbud av spel från välrenommerade spelleverantörer, vilket gör att spelarna har många olika alternativ att välja mellan. Oavsett om man föredrar slots, bordsspel eller live casino så finns det något för alla på Gogo Casino.
En annan anledning till att Gogo Casino har blivit så populärt är deras engagemang för ansvarsfullt spelande. De erbjuder verktyg och funktioner som hjälper spelarna att hålla koll på sin spelaktivitet och sätta gränser för sitt spelande.
Sammanfattningsvis kan man säga att Gogo Casino är ett online casino som har gjort stort intryck på den svenska spelmarknaden. Med sina generösa bonusar, stora spelutbud och fokus på ansvarsfullt spelande är det en aktör att hålla ögonen på. Så om du är sugen på en spännande spelupplevelse är Gogo Casino definitivt värt att testa.
https://gogocasino.one
cost of prednisone in canada buy prednisone 10mg online online order prednisone 10mg
https://zithromaxall.com/# buy generic zithromax online
generic zithromax 500mg india: zithromax 500 price – buy zithromax without prescription online
Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und groГџzГјgigen Bonusangeboten fГјr seine Spieler bietet. Neben der Spielauswahl und den Promotionen ist fГјr viele Spieler auch die Auszahlungsdauer ein wichtiger Faktor bei der Wahl eines Online-Casinos.
Die Dauer einer Auszahlung bei Zet Casino hängt von verschiedenen Faktoren ab, darunter die gewählte Zahlungsmethode und der Verifizierungsprozess. Im Allgemeinen kann die Auszahlungsdauer bei Zet Casino je nach Zahlungsmethode zwischen 1 und 5 Werktagen betragen.
Um eine Auszahlung bei Zet Casino zu tätigen, müssen die Spieler zunächst ihr Konto verifizieren. Hierfür müssen sie ihre Identität und Adresse nachweisen, um sicherzustellen, dass alle Transaktionen sicher sind. Nach der Verifizierung können die Spieler eine Auszahlung beantragen, die in der Regel innerhalb von 24 Stunden bearbeitet wird.
Die Auszahlungsdauer kann auch von der Höhe des Auszahlungsbetrags abhängen. Große Gewinne können eine zusätzliche Überprüfung erfordern, um Betrug oder Geldwäsche zu verhindern. In solchen Fällen kann es etwas länger dauern, bis das Geld auf dem Spielerkonto gutgeschrieben wird.
Insgesamt kann die Auszahlungsdauer bei Zet Casino als zuverlässig und schnell bezeichnet werden. Die Spieler können sich darauf verlassen, dass ihre Gewinne sicher und zeitnah ausgezahlt werden. Mit einer Vielzahl von Zahlungsmethoden und einem effizienten Auszahlungsprozess bietet Zet Casino seinen Spielern ein rundum angenehmes Spielerlebnis.
https://zetcasino.one/
buy cialis pill: tadalafil iq – Buy Tadalafil 20mg
synthesis a-pvp
https://www.nordicpromos.com/boards/topic/543156/synthesizing-%CE%B1-pyrrolidinopentiophenone
https://blogs.rufox.ru/~wependv/42578.htm
Boomerang Casino Free Spins ohne Einzahlung
Das Boomerang Casino ist bekannt für sein großartiges Angebot an Spielen und großzügigen Bonusangeboten. Eine der beliebtesten Aktionen des Casinos sind die kostenlosen Freispiele ohne Einzahlung, die es den Spielern ermöglichen, echtes Geld zu gewinnen, ohne vorher Geld einzahlen zu müssen.
Die Free Spins ohne Einzahlung sind eine großartige Möglichkeit, das Casino kennenzulernen und die verschiedenen Spiele auszuprobieren, ohne dabei ein finanzielles Risiko eingehen zu müssen. Die Freispiele können an ausgewählten Spielautomaten eingesetzt werden und bieten die Chance, echte Gewinne zu erzielen.
Um an den Freispielen ohne Einzahlung teilzunehmen, müssen sich die Spieler lediglich im Boomerang Casino registrieren. Nach der erfolgreichen Anmeldung werden die Freispiele automatisch gutgeschrieben und können direkt genutzt werden.
Es ist jedoch zu beachten, dass die Gewinne aus den Freispielen in der Regel an bestimmte Umsatzbedingungen gebunden sind, die erfüllt werden müssen, bevor eine Auszahlung möglich ist. Diese Bedingungen variieren je nach Aktion und sollten daher vorher genau gelesen werden.
Insgesamt sind die Boomerang Casino Free Spins ohne Einzahlung eine großartige Möglichkeit, die vielfältigen Spiele des Casinos kennenzulernen und dabei sogar echte Gewinne zu erzielen. Es lohnt sich daher, regelmäßig nach aktuellen Angeboten Ausschau zu halten und diese zu nutzen. Viel Spaß und viel Glück beim Spielen!
https://boomerangcasino.one/
synthesis a-pvp
buy kamagra online usa Kamagra Oral Jelly Price Kamagra 100mg
over the counter sildenafil: generic ed pills – Order Viagra 50 mg online
Zet Casino bietet seinen Spielern eine Vielzahl von MГ¶glichkeiten, um ihre Gewinne abzuheben. Die “zet casino kotiutus” oder Auszahlungsoption ist einfach und bequem und ermГ¶glicht es den Spielern, ihre Gewinne schnell und unkompliziert zu erhalten.
Um eine Auszahlung bei Zet Casino zu tätigen, müssen Spieler zunächst sicherstellen, dass sie über ausreichendes Guthaben auf ihrem Konto verfügen. Sobald dies der Fall ist, können sie auf ihr Konto zugreifen und den gewünschten Auszahlungsbetrag angeben. Spieler können zwischen verschiedenen Zahlungsmethoden wählen, darunter Kreditkarten, E-Wallets und Banküberweisungen.
Es ist wichtig zu beachten, dass bei der Auszahlung von Gewinnen bei Zet Casino bestimmte Bedingungen und Limits gelten können. Spieler sollten sich daher vor der Auszahlung über die entsprechenden Richtlinien informieren, um sicherzustellen, dass sie ihre Gewinne problemlos erhalten können.
Zet Casino ist bekannt für seine schnellen und zuverlässigen Auszahlungen, die es den Spielern ermöglichen, ihre Gewinne ohne Verzögerung zu erhalten. Mit einer Vielzahl von Zahlungsmethoden und einem effizienten Auszahlungssystem ist Zet Casino die ideale Wahl für alle, die nach einer zuverlässigen und benutzerfreundlichen Online-Casinoerfahrung suchen.
Insgesamt bietet Zet Casino eine herausragende Auszahlungsoption für Spieler, die ihre Gewinne schnell und unkompliziert erhalten möchten. Mit einer Vielzahl von Zahlungsmethoden und einem effizienten Auszahlungssystem ist Zet Casino die ideale Wahl für alle, die nach einer zuverlässigen Online-Casinoerfahrung suchen. Besuchen Sie noch heute Zet Casino und erleben Sie die Spannung des Gewinnens und die Bequemlichkeit der schnellen Auszahlungen.
https://zetcasino.one/
https://sildenafiliq.com/# Generic Viagra online
Зайдите на сайт https://pecom.asia/ и вы сможете воспользоваться услугами транспортной компании по доставке грузов из Китая в Россию. Доставка товаров из Китая осуществляется в максимально сжатые сроки. Мы оказываем большой перечень услуг по грузоперевозкам из Китая, страхованию, таможенному оформлению. Грузоперевозки и доставка товаров из Китая по выгодным ценам. Подробнее на сайте.
Tipico Casino Bonus Codes
Tipico Casino is one of the most popular online casinos in Germany, offering a wide range of games and promotions for players to enjoy. One of the most exciting aspects of playing at Tipico Casino is taking advantage of their bonus codes, which can help players boost their winnings and enhance their overall gaming experience.
Bonus codes are special codes that players can enter when making a deposit or claiming a promotion at an online casino. These codes can provide players with extra funds, free spins, or other rewards to help them get the most out of their gaming experience. At Tipico Casino, players can find a variety of bonus codes that can be used to enhance their gameplay and increase their chances of winning big.
One of the most popular bonus codes at Tipico Casino is the welcome bonus code, which is offered to new players who sign up for an account. This bonus code typically provides players with a matched deposit bonus, giving them extra funds to play with when they make their first deposit. In addition to the welcome bonus code, Tipico Casino also offers regular promotions and bonuses that players can take advantage of by using specific bonus codes.
To claim a bonus code at Tipico Casino, players simply need to enter the code in the designated field when making a deposit or claiming a promotion. Once the code is entered, the bonus will be added to the player’s account, providing them with extra funds or rewards to use while playing their favorite casino games.
Overall, bonus codes are a great way for players to enhance their gaming experience at Tipico Casino. By taking advantage of these codes, players can increase their chances of winning big and enjoy more time playing their favorite casino games. So why not give it a try and see what bonus codes Tipico Casino has to offer?
In conclusion, bonus codes are a fantastic way for players to enhance their online gaming experience. By using the right codes at the right time, players can boost their winnings, secure more free spins, and really ramp up the fun of their time at Tipico Casino. Make a point of checking out the array of bonus codes available to you, and start enjoying even more thrilling gaming today!
https://tipicocasino.one/
Kamagra Oral Jelly: kamagra best price – buy kamagra online usa
semaglutide 3mg
acarbose versuch
Viagra online price cheapest viagra cheapest viagra
Всероссийская благотворительная школьная ярмарка предлагает вам разместить собственные товары на ней или купить за образовательную валюту бенефиты и услуги в приложении VK Умникоины без какой-либо регистрации и скачивания. https://start.shkolnayayarmarka.ru/ – сайт, где есть возможность в качестве пожертвования разместить личные товары и услуги. Также тут вы ознакомитесь детальнее с единицей обмена, которую используют для выполнения сделок на благотворительных ярмарках между продавцом и покупателем. Пишите нам уже сейчас.
Zet Online Casino: Alles, was Sie wissen mГјssen
Das Zet Online Casino ist eine neue Online-GlГјcksspielplattform, die sich schnell einen Namen in der Welt der Online-Casinos gemacht hat. Mit einer Vielzahl von Spielen, groГџzГјgigen Boni und einem benutzerfreundlichen Design ist das Zet Casino definitiv einen Blick wert.
Eines der besten Dinge am Zet Online Casino ist die enorme Auswahl an Spielen, die es seinen Spielern bietet. Von klassischen Tischspielen wie Blackjack und Roulette bis hin zu modernen Spielautomaten und Live-Dealer-Spielen gibt es fГјr jeden Geschmack etwas zu finden. Die Spiele werden von renommierten Entwicklern wie NetEnt, Microgaming und Play’n GO bereitgestellt, so dass Sie sich auf qualitativ hochwertige Grafiken und spannende SpielablГ¤ufe freuen kГ¶nnen.
Neben der großen Spielauswahl bietet das Zet Casino auch großzügige Boni und Aktionen für neue und bestehende Spieler. Wenn Sie sich zum Beispiel anmelden, erhalten Sie einen Willkommensbonus, der Ihnen zusätzliches Guthaben und Freispiele verschafft. Darüber hinaus gibt es regelmäßig Promotionen wie Reload-Boni, Cashback-Angebote und Turniere, die Ihre Gewinnchancen erhöhen.
Das Zet Online Casino legt auch großen Wert auf die Sicherheit seiner Spieler. Die Plattform verfügt über eine gültige Glücksspiellizenz und verwendet moderne Verschlüsselungstechnologien, um sicherzustellen, dass Ihre persönlichen Daten geschützt sind. Darüber hinaus bietet das Casino verschiedene Zahlungsmethoden an, die schnell und sicher sind, so dass Sie sich keine Sorgen um Ihre Ein- und Auszahlungen machen müssen.
Zusammenfassend lässt sich sagen, dass das Zet Online Casino eine hervorragende Wahl für alle Glücksspielbegeisterten ist. Mit einer breiten Spielauswahl, großzügigen Boni und einem hohen Maß an Sicherheit und Fairness ist das Zet Casino definitiv einen Besuch wert. Besuchen Sie noch heute die Website und entdecken Sie die aufregende Welt des Zet Casinos!
https://zetcasino.one/
cheapest viagra: cheapest viagra – cheapest viagra
Buy Tadalafil 20mg: cheapest cialis – Tadalafil Tablet
Boomerang Casino Einzahlungscode: Alles, was Sie wissen mГјssen
Boomerang Casino ist eine beliebte Online-Spielhalle, die eine Vielzahl von Casino-Spielen anbietet, darunter Slots, Tischspiele und Live-Casino-Spiele. Um neue Spieler anzulocken und bestehende Spieler zu belohnen, bietet das Casino regelmäßig Einzahlungscodes an, die es den Spielern ermöglichen, zusätzliches Spielguthaben oder Freispiele zu erhalten.
Ein Einzahlungscode ist ein spezieller Code, den Spieler eingeben können, wenn sie eine Einzahlung auf ihr Spielerkonto tätigen. Der Code entspricht einem bestimmten Bonusangebot, das vom Casino bereitgestellt wird. Zum Beispiel können Spieler mit einem Einzahlungscode einen prozentualen Bonus auf ihre Einzahlung erhalten oder Freispiele für ausgewählte Slots.
Um den Boomerang Casino Einzahlungscode zu nutzen, müssen Spieler zunächst ein Spielerkonto erstellen und eine Einzahlung tätigen. Anschließend können sie den Code in das entsprechende Feld eingeben, das im Einzahlungsbereich des Casinos verfügbar ist. Sobald der Code eingegeben wurde, wird der Bonus automatisch auf das Spielerkonto gutgeschrieben.
Es ist jedoch wichtig zu beachten, dass Einzahlungscodes in der Regel mit bestimmten Bedingungen verbunden sind. Dazu gehören Umsatzanforderungen, die besagen, wie oft der Bonus vor einer Auszahlung umgesetzt werden muss, sowie Einschränkungen für bestimmte Spiele oder Einsatzlimits. Spieler sollten daher die Geschäftsbedingungen für jeden Einzahlungscode sorgfältig lesen, bevor sie ihn nutzen.
Boomerang Casino bietet regelmäßig neue Einzahlungscodes an, um seinen Spielern abwechslungsreiche Bonusangebote zu präsentieren. Spieler können die aktuellen Einzahlungscodes auf der Website des Casinos oder über spezielle Werbeaktionen und Newsletter erhalten. Mit diesen Codes können sie ihr Spielerlebnis verbessern und zusätzliche Gewinnchancen nutzen.
Insgesamt sind Einzahlungscodes eine großartige Möglichkeit für Spieler, zusätzliche Belohnungen und Vorteile in Online-Casinos wie Boomerang Casino zu erhalten. Durch die Nutzung dieser Codes können Spieler ihr Guthaben erhöhen und mehr Spaß am Spiel haben.
https://boomerangcasino.one/
I’ve been surfing online more than three hours today, yet I never found any interesting article like yours. It’s pretty worth enough for me. Personally, if all site owners and bloggers made good content as you did, the web will be a lot more useful than ever before.
I will immediately clutch your rss feed as I can’t find your email subscription hyperlink or e-newsletter service. Do you have any? Kindly permit me know so that I may just subscribe. Thanks.
https://sinee0c7e-nebo1q5d-golova4x1w.com
cheap viagra buy viagra online Viagra online price
Generic Cialis price: Buy Cialis online – Cialis without a doctor prescription
Скай Лайн Консалтинг – известная компания, предлагающая полный спектр бухгалтерского сопровождения. У нас собрана команда истинных профессионалов. Все без исключения специалисты имеют профильное образование и достаточный опыт работы. Доверьте им оформление юридических документов и кадровое делопроизводство. https://slc-company.ru/ – сайт, где есть возможность в любое время посмотреть отзывы благодарных клиентов. Обращайтесь к нам, гарантируем грамотное и быстрое решение вопросов. Стремимся к выгодному сотрудничеству!
Zet Casino ist eine beliebte Online-GlГјcksspielplattform, die eine Vielzahl von Spielen fГјr die Spieler zur Auswahl bietet. Mit einer groГџen Auswahl an Slots, Tischspielen und Live-Casino-Spielen gibt es fГјr jeden etwas in diesem Casino.
Einige der besten Spiele bei Zet Casino sind unter anderem die Slots von renommierten Anbietern wie NetEnt, Microgaming und Play’n GO. Diese Spiele bieten nicht nur eine spannende Spielerfahrung, sondern auch die Chance, groГџe Gewinne zu erzielen.
Zu den beliebtesten Slots bei Zet Casino gehГ¶ren Spiele wie Starburst, Book of Dead und Gonzo’s Quest. Diese Spiele zeichnen sich durch ihre hochwertige Grafik, spannende Bonusrunden und hohe Auszahlungsquoten aus, was sie zu den Favoriten vieler Spieler macht.
Aber auch Fans von Tischspielen kommen bei Zet Casino auf ihre Kosten. Von klassischen Spielen wie Blackjack und Roulette bis hin zu exotischeren Varianten wie Baccarat und Pai Gow Poker gibt es eine Vielzahl von Optionen, aus denen die Spieler wählen können.
FГјr diejenigen, die das authentische Casino-Erlebnis bevorzugen, bietet Zet Casino auch eine Vielzahl von Live-Casino-Spielen an. Von Live-Blackjack und Live-Roulette bis hin zu Live-Baccarat und Live-Casino Hold’em kГ¶nnen die Spieler gegen echte Dealer antreten und das GefГјhl haben, in einem echten Casino zu spielen.
Insgesamt bietet Zet Casino eine breite Palette von Spielen für alle Arten von Spielern. Mit seiner benutzerfreundlichen Oberfläche, großzügigen Boni und einer Vielzahl von Zahlungsoptionen ist es kein Wunder, dass es zu den beliebtesten Online-Casinos gehört. Probieren Sie also einige der besten Spiele bei Zet Casino aus und erleben Sie den Nervenkitzel des Glücksspiels von Ihrem eigenen Zuhause aus.
https://zetcasino.one/
На сайте https://bezopasniy-pol.ru/catalog/protivoskolzyashhie-lentyi вы сможете купить качественные противоскользящие ленты STEPING напрямую от завода в России. Приглашаем дилеров. Оптовые цены.
https://tadalafiliq.com/# Generic Cialis price
cheap viagra: generic ed pills – Viagra generic over the counter
Boomerang Casino ist eines der neuesten und aufregendsten Online-Casinos auf dem Markt. Mit einer Vielzahl von Spielen, groГџzГјgigen Bonusangeboten und einem benutzerfreundlichen Interface ist es definitiv einen Besuch wert. Ein besonders attraktives Angebot von Boomerang Casino ist der Bonus ohne Einzahlung, auch bekannt als “bonus bez depozytu”.
Ein Bonus ohne Einzahlung ist eine großartige Möglichkeit für Spieler, das Casino und seine Spiele ohne Risiko auszuprobieren. Spieler erhalten einen bestimmten Betrag an Bonusgeld oder Freispielen, ohne eine Einzahlung tätigen zu müssen. Dies ermöglicht es Spielern, das Casino kennenzulernen und erste Gewinne zu erzielen, ohne eigenes Geld riskieren zu müssen.
Der boomerang casino bonus bez depozytu bietet Spielern die Möglichkeit, 20 Freispiele ohne Einzahlung zu erhalten. Diese Freispiele können an ausgewählten Spielautomaten gespielt werden und bieten die Chance auf echte Gewinne. Darüber hinaus bietet Boomerang Casino auch einen großzügigen Willkommensbonus für neue Spieler, bei dem Einzahlungen bis zu einem bestimmten Betrag verdoppelt werden.
Um den Bonus ohne Einzahlung zu erhalten, müssen Spieler lediglich ein Konto bei Boomerang Casino erstellen und den Bonuscode eingeben, der auf der Webseite des Casinos angegeben ist. Nachdem der Bonus gutgeschrieben wurde, können Spieler ihn sofort nutzen und ihre Lieblingsspiele spielen.
Es ist jedoch wichtig zu beachten, dass Boni ohne Einzahlung oft bestimmten Bedingungen unterliegen. Spieler müssen die Umsatzanforderungen erfüllen, bevor sie Gewinne auszahlen lassen können. Daher ist es ratsam, die Bonusbedingungen sorgfältig zu lesen, bevor man sich für den boomerang casino bonus bez depozytu entscheidet.
Insgesamt ist der Bonus ohne Einzahlung von Boomerang Casino eine großartige Möglichkeit, das Casino kennenzulernen und erste Gewinne zu erzielen. Mit einer Vielzahl von Spielen, großzügigen Bonusangeboten und einem benutzerfreundlichen Interface ist es definitiv einen Besuch wert.
https://boomerangcasino.one/
buy Kamagra kamagra best price Kamagra 100mg price
Tipico Casino Geld Auszahlen Lassen
Das Tipico Casino steht für Spannung und Unterhaltung pur. Neben einer Vielzahl von beliebten Casino-Spielen bietet Tipico auch die Möglichkeit, echtes Geld zu gewinnen. Wenn man erfolgreich gespielt hat und Gewinne erzielt hat, stellt sich früher oder später die Frage, wie man das Geld auszahlen lassen kann.
Der Prozess der Auszahlung im Tipico Casino ist einfach und unkompliziert. ZunГ¤chst muss man sich in sein Spielerkonto einloggen und den MenГјpunkt “Auszahlungen” auswГ¤hlen. Dort kann man dann die gewГјnschte Auszahlungsmethode auswГ¤hlen. Tipico bietet eine Vielzahl von sicheren und schnellen Zahlungsoptionen, wie zum Beispiel BankГјberweisung, Kreditkarte oder E-Wallets wie Skrill oder Neteller.
Nachdem man die Auszahlungsmethode gewählt hat, muss man den Betrag eingeben, den man auszahlen lassen möchte. Es ist wichtig zu beachten, dass Tipico gewisse Mindest- und Höchstbeträge für Auszahlungen festgelegt hat. Diese Informationen können in den Allgemeinen Geschäftsbedingungen des Casinos nachgelesen werden.
Sobald man den Auszahlungsantrag abgeschickt hat, wird dieser von Tipico ГјberprГјft und bearbeitet. Je nach Auszahlungsmethode kann es unterschiedlich lange dauern, bis das Geld auf dem Konto des Spielers gutgeschrieben wird. In der Regel werden Auszahlungen aber innerhalb von 1-3 Werktagen abgewickelt.
Es ist wichtig zu beachten, dass Tipico Casino Auszahlungen nur auf das Konto des Spielers oder auf eine registrierte Zahlungsmethode erfolgen können. Zudem kann es sein, dass bei der ersten Auszahlung eine Identitätsprüfung durchgeführt wird, um sicherzustellen, dass das Geld an die richtige Person ausgezahlt wird.
Insgesamt kann gesagt werden, dass das Auszahlen von Geld im Tipico Casino einfach und sicher ist. Mit den vielfältigen Zahlungsoptionen und dem zuverlässigen Kundenservice steht dem Spielspaß und dem Gewinn nichts im Wege. Also, nichts wie ran an die Casino-Spiele und holt euch eure Gewinne aus dem Tipico Casino!
https://tipicocasino.one/
Buy generic 100mg Viagra online: cheapest viagra – viagra without prescription
Zet Casino ist ein Online-Casino, das Spielern eine Vielzahl von Spielen und großzügigen Bonusangeboten bietet. In diesem Artikel werden wir eine ausführliche Bewertung des Casinos durchführen und Ihnen alles Wissenswerte über dieses spannende Online-Casino erzählen.
Das Zet Casino wurde im Jahr 2018 gegrГјndet und hat sich seitdem einen guten Ruf in der Online-GlГјcksspielbranche erarbeitet. Das Casino verfГјgt Гјber eine Lizenz der Malta Gaming Authority, was bedeutet, dass es strengen Regulierungen unterliegt und als sicher und fair eingestuft wird.
Das Casino bietet eine breite Palette von Spielen, darunter Spielautomaten, Tischspiele, Live-Casino-Spiele und vieles mehr. Diese Spiele werden von einigen der besten Softwareanbieter der Branche wie NetEnt, Microgaming, Play’n GO und vielen anderen bereitgestellt. Die Spiele sind von hoher QualitГ¤t und bieten ein unterhaltsames Spielerlebnis.
Neben einer großen Auswahl an Spielen bietet das Zet Casino auch großzügige Bonusangebote für neue und bestehende Spieler. Neue Spieler können einen Willkommensbonus erhalten, der Freispiele und einen Bonus auf die erste Einzahlung umfasst. Darüber hinaus gibt es regelmäßig Aktionen und Bonusangebote für bestehende Spieler, die die Spieler belohnen und ihr Spielerlebnis verbessern.
Das Zet Casino verfügt über eine benutzerfreundliche Website, die es einfach macht, Spiele zu finden und zu spielen. Die Website ist gut gestaltet und bietet eine reibungslose Navigation. Darüber hinaus ist das Casino auch für mobile Geräte optimiert, so dass die Spieler jederzeit und überall spielen können.
Insgesamt bietet das Zet Casino ein erstklassiges Spielerlebnis mit einer Vielzahl von Spielen, großzügigen Bonusangeboten und einer benutzerfreundlichen Website. Wenn Sie nach einem zuverlässigen und unterhaltsamen Online-Casino suchen, sollten Sie definitiv einen Blick auf das Zet Casino werfen.
https://zetcasino.one/
Buy generic 100mg Viagra online: best price on viagra – best price for viagra 100mg
sildenafil oral jelly 100mg kamagra Sildenafil Oral Jelly Kamagra Oral Jelly
https://kamagraiq.shop/# buy kamagra online usa
Das Boomerang Casino Poker ist eine aufregende Variante des klassischen Pokerspiels, die in vielen Casinos auf der ganzen Welt angeboten wird. Die Besonderheit dieses Spiels liegt darin, dass die Spieler die Möglichkeit haben, ihre Gewinne zu verdoppeln oder zu vervierfachen, indem sie ihre Karten zurückgeben und eine neue Hand erhalten.
Das Spiel beginnt ähnlich wie normales Poker, aber sobald die Spieler ihre Karten erhalten haben, können sie entscheiden, ob sie sie behalten oder zurückgeben möchten. Wenn ein Spieler sich entscheidet, seine Karten zurückzugeben, erhält er eine neue Hand und hat die Chance, eine bessere Kombination zu erhalten.
Das Boomerang Casino Poker ist besonders beliebt bei Spielern, die gerne Risiken eingehen und die Spannung des Glücksspiels lieben. Da die Spieler die Möglichkeit haben, ihre Gewinne zu vervielfachen, kann das Spiel sehr lukrativ sein, aber auch mit hohen Risiken verbunden sein.
Um erfolgreich im Boomerang Casino Poker zu sein, ist es wichtig, eine gute Strategie zu haben und die Wahrscheinlichkeit von verschiedenen Kartenkombinationen zu kennen. Da das Spiel auf GlГјck basiert, ist es auch wichtig, Geduld zu haben und nicht zu impulsiv zu handeln.
Alles in allem ist das Boomerang Casino Poker eine aufregende und unterhaltsame Variante des Pokerspiels, die sowohl für Anfänger als auch für erfahrene Spieler geeignet ist. Mit etwas Geschick und Glück können die Spieler große Gewinne erzielen und das Spiel genießen.
https://boomerangcasino.one/
Das Casino Tipico Neu ist endlich da! Mit einer Vielzahl von spannenden Spielen und groГџartigen Angeboten erwartet die Spieler ein unvergessliches Erlebnis.
Das neu gestaltete Casino Tipico bietet eine breite Auswahl an beliebten Slots, Tischspielen und Live-Casino-Spielen von führenden Anbietern wie NetEnt, Microgaming, Evolution Gaming und vielen mehr. Die Spieler können sich auf hochwertige Grafiken, schnelle Ladezeiten und ein reibungsloses Spielerlebnis freuen.
Darüber hinaus bietet das Casino Tipico Neu großzügige Boni und Promotionen für neue und bestehende Spieler. Von Willkommensbonusangeboten bis hin zu täglichen Aktionen wird jeder Spieler belohnt. Das Casino veranstaltet auch regelmäßige Turniere und Wettbewerbe, bei denen die Spieler die Chance haben, zusätzliche Belohnungen zu gewinnen.
Ein weiterer wichtiger Aspekt des neuen Casino Tipico ist die Sicherheit und Fairness. Das Casino verfügt über eine Lizenz der Malta Gaming Authority und verwendet die neueste SSL-Verschlüsselungstechnologie, um sicherzustellen, dass alle Spielerdaten geschützt sind. Darüber hinaus werden alle Spiele regelmäßig von unabhängigen Prüfstellen überwacht, um sicherzustellen, dass sie fair und zufällig sind.
Insgesamt bietet das Casino Tipico Neu ein erstklassiges Spielerlebnis für alle, die nach Unterhaltung und Gewinnmöglichkeiten suchen. Mit einer Vielzahl von Spielen, großzügigen Boni und einem maßgeschneiderten Kundenservice ist das neue Casino Tipico definitiv einen Besuch wert. Also schauen Sie vorbei und erleben Sie den Nervenkitzel des Glücksspiels heute noch!
https://tipicocasino.one/
Зайдите на сайт https://nashi-teplicy.ru/ и купите качественные теплицы из поликарбоната от производителя в Москве и московской области. Теплицы арочные, прямостенные, каплевидные. Парники и навесы. Доставка в день заказа!
abilify for bipolar 2
actos pronunciation
buy Viagra online: best price on viagra – Cheap Sildenafil 100mg
Das Boomerang Casino ist ein beliebter Online-Glücksspielanbieter, der eine Vielzahl von Spielen und attraktiven Boni anbietet. Viele Spieler fragen sich jedoch, wie lange es dauert, bis sie ihre Gewinne aus dem Casino abheben können. In diesem Artikel werden wir die Auszahlungsdauer im Boomerang Casino genauer unter die Lupe nehmen.
Die Auszahlungsdauer im Boomerang Casino hängt von verschiedenen Faktoren ab, wie zum Beispiel der Auszahlungsmethode, der Verifizierung des Kontos und den individuellen Richtlinien des Casinos. In der Regel dauert es jedoch zwischen 1 und 5 Werktagen, bis eine Auszahlung bearbeitet wird.
Um eine Auszahlung im Boomerang Casino zu beantragen, müssen Spieler zunächst sicherstellen, dass ihr Konto verifiziert ist. Dazu müssen sie Kopien ihrer Ausweisdokumente und/oder anderer Nachweise ihrer Identität hochladen. Sobald das Konto verifiziert ist, können Spieler eine Auszahlung beantragen und müssen dann je nach Auszahlungsmethode eine Wartezeit von einigen Tagen in Kauf nehmen.
Es ist wichtig zu beachten, dass die Auszahlungsdauer auch von der gewählten Auszahlungsmethode abhängt. Einige Zahlungsmethoden wie E-Wallets wie Skrill oder Neteller bieten schnellere Auszahlungen an, während Banküberweisungen in der Regel länger dauern können.
Insgesamt kann gesagt werden, dass die Auszahlungsdauer im Boomerang Casino im Durchschnitt relativ zГјgig ist und sich im Rahmen anderer Online-Casinos bewegt. Spieler sollten jedoch immer die individuellen Auszahlungsbedingungen des Casinos beachten und bei Fragen den Kundensupport kontaktieren.
Insgesamt bietet das Boomerang Casino eine sichere und zuverlässige Plattform für Glücksspielfans, die gerne online spielen. Mit einer Vielzahl von Spielen, attraktiven Boni und einer akzeptablen Auszahlungsdauer ist das Boomerang Casino definitiv einen Besuch wert.
https://boomerangcasino.one/
Das Tipico Casino bietet seinen Kunden die Möglichkeit, sich vor dem Einsatz von echtem Geld mit den Spielen vertraut zu machen. Dies geschieht durch die sogenannte Demo-Version, die es erlaubt, die Spiele kostenlos und ohne Risiko auszuprobieren.
Die Demo-Versionen im Tipico Casino sind eine tolle Gelegenheit, um neue Spiele kennenzulernen und Strategien zu testen. Die Spieler können sich ganz in Ruhe mit den Regeln vertraut machen und herausfinden, welche Spiele ihnen am meisten Spaß machen. So können sie sich ein Bild davon machen, ob das jeweilige Spiel ihren Vorlieben entspricht, bevor sie echtes Geld einsetzen.
Die Demo-Versionen sind auch für erfahrene Spieler nützlich, um ihre bereits bestehenden Strategien zu verfeinern und zu optimieren. Außerdem können sie sich so mit neuen Spielen vertraut machen, ohne dabei direkt Geld investieren zu müssen.
Um die Demo-Versionen im Tipico Casino nutzen zu können, ist in der Regel keine Anmeldung erforderlich. Die Spiele stehen direkt im Browser zur Verfügung und können sofort gespielt werden. So wird das Ausprobieren von neuen Spielen besonders unkompliziert und einfach.
Alles in allem sind die Demo-Versionen im Tipico Casino eine tolle Möglichkeit, um sich risikofrei mit den verschiedenen Spielen vertraut zu machen. Sowohl Anfänger als auch erfahrene Spieler können hiervon profitieren und ihre Spielfähigkeiten verbessern. Wer also Lust hat, neue Spiele zu entdecken oder seine Strategien zu optimieren, sollte die Demo-Versionen im Tipico Casino unbedingt ausprobieren.
https://tipicocasino.one/
Zet Casino ist eine beliebte Online-Glücksspielplattform, die ihren Spielern eine Vielzahl von Spielen und großzügigen Boni bietet. Wenn Sie sich für das Zet Casino entscheiden, können Sie von verschiedenen Bonusangeboten profitieren. Allerdings ist es wichtig, die Bonusbedingungen zu verstehen, um sicherzustellen, dass Sie die Boni optimal nutzen können.
Die Bonusbedingungen im Zet Casino sind transparent und fair. Bevor Sie einen Bonus beanspruchen, ist es wichtig, die jeweiligen Bedingungen zu lesen. Jeder Bonus hat unterschiedliche Einschränkungen und Anforderungen, die erfüllt werden müssen, bevor Gewinne ausgezahlt werden können.
Ein wichtiger Punkt, den Spieler beachten sollten, ist der Umsatzanforderung. Dies bedeutet, dass Sie eine bestimmte Anzahl von Einsätzen machen müssen, bevor Sie Ihre Gewinne abheben können. Je nach Bonusangebot kann diese Anforderung variieren.
Darüber hinaus gibt es oft auch eine Zeitbeschränkung, innerhalb derer die Umsatzanforderungen erfüllt werden müssen. Wenn dies nicht innerhalb der vorgegebenen Frist geschieht, verfällt der Bonus und alle damit erzielten Gewinne.
Ein weiterer Punkt, den Spieler beachten sollten, sind die Spielbeschränkungen. Nicht alle Spiele im Zet Casino tragen gleichermaßen zur Erfüllung der Umsatzanforderungen bei. In der Regel tragen Slotspiele zu 100% bei, während Tischspiele wie Roulette oder Blackjack möglicherweise nur zu einem geringeren Prozentsatz beitragen.
Es ist auch wichtig zu beachten, dass nicht alle Spieler für Boni qualifiziert sind. In einigen Fällen können Spieler aus bestimmten Ländern von Bonusangeboten ausgeschlossen sein. Daher ist es ratsam, die allgemeinen Geschäftsbedingungen sorgfältig zu lesen, um Missverständnisse zu vermeiden.
Insgesamt bieten die Bonusangebote im Zet Casino eine großartige Möglichkeit, Ihr Guthaben zu erhöhen und zusätzliche Gewinne zu erzielen. Es ist jedoch wichtig, die Bonusbedingungen zu verstehen und sicherzustellen, dass Sie diese erfüllen, um das Beste aus Ihrem Spielerlebnis herauszuholen. Indem Sie die Regeln einhalten, können Sie sicherstellen, dass Sie Ihre Boni optimal nutzen und Ihre Gewinnchancen maximieren.
https://zetcasino.one/
buy Kamagra Kamagra Oral Jelly Price Kamagra tablets
http://tadalafiliq.com/# Generic Cialis without a doctor prescription
https://www.telemadrid.es/noticias/sociedad/Influencers-chinos-promover-Marca-Espana-0-2010099010–20180507125337.html
long term side effects of semaglutide
https://sildenafiliq.xyz/# Viagra online price
Generic Cialis price: tadalafil iq – cheapest cialis
abilify tardive dyskinesia
Das Boomerang Casino AskGamblers ist eines der neuesten Online-Casinos auf dem Markt und hat bereits die Aufmerksamkeit vieler Spieler auf sich gezogen. Mit einer umfangreichen Spielauswahl, großzügigen Boni und einem benutzerfreundlichen Interface scheint es, als hätte das Casino alles, was man sich wünschen kann.
Das Hauptmerkmal des Boomerang Casinos ist seine Zusammenarbeit mit der renommierten Website AskGamblers, die als eine der vertrauenswürdigsten Quellen für Online-Casino-Bewertungen und Informationen gilt. Durch diese Zusammenarbeit können Spieler sicher sein, dass sie in einem seriösen und fairen Casino spielen.
Das Casino bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele, Live-Casino-Spiele und mehr. Mit Spielen von Top-Entwicklern wie NetEnt, Microgaming, Play’n GO und vielen anderen ist fГјr Unterhaltung und Abwechslung gesorgt.
Darüber hinaus bietet das Boomerang Casino großzügige Boni und Aktionen für neue und bestehende Spieler. Dies umfasst Willkommensboni, Einzahlungsboni, Freispiele und vieles mehr. Spieler können sich auf regelmäßige Promotionen freuen, die ihre Bankroll steigern und ihr Spielerlebnis verbessern.
Das Casino ist auch für seine sichere und zuverlässige Zahlungsmethoden bekannt, die eine schnelle und einfache Ein- und Auszahlung ermöglichen. Spieler können zwischen verschiedenen Optionen wie Kreditkarten, E-Wallets und Banküberweisungen wählen, um ihr Geld sicher zu verwalten.
Insgesamt scheint das Boomerang Casino AskGamblers eine vielversprechende Wahl für Online-Spieler zu sein, die nach einer sicheren und unterhaltsamen Spielumgebung suchen. Mit seinen umfangreichen Spielen, großzügigen Boni und zuverlässigen Zahlungsmethoden ist es definitiv einen Blick wert.
https://boomerangcasino.one/
Tipico ist einer der beliebtesten Online-Casinos in Deutschland und bietet seinen Spielern ein groГџartiges Spielerlebnis mit einer Vielzahl von Spielen und Funktionen. Einer der Aspekte, die Tipico von anderen Online-Casinos unterscheidet, ist die hohe Return-to-Player (RTP) Rate, die sie ihren Spielern bieten.
Die RTP Rate eines Casinos ist ein wichtiger Faktor, der bestimmt, wie viel Geld ein Spieler durchschnittlich zurückgewinnen kann. Je höher die RTP Rate, desto besser die Gewinnchancen für die Spieler. Tipico hat sich durch seine überdurchschnittlich hohe RTP Rate einen Namen gemacht und zieht so viele Spieler an.
Durch die hohe RTP Rate bei Tipico haben die Spieler die Möglichkeit, mehr Geld zu gewinnen und ihre Gewinnchancen zu maximieren. Dies macht das Spielen bei Tipico zu einer unterhaltsamen und lukrativen Erfahrung. Die hohe RTP Rate ist ein weiterer Grund, warum Tipico bei Spielern so beliebt ist und eine der ersten Anlaufstellen für Glücksspielbegeisterte in Deutschland ist.
Insgesamt ist die hohe RTP Rate von Tipico ein groГџer Vorteil fГјr die Spieler und macht das Online-Casino zu einer attraktiven Option fГјr alle, die nach einer unterhaltsamen und lohnenden Spielerfahrung suchen. Mit einer Vielzahl von Spielen und einer hohen Gewinnrate ist Tipico definitiv ein Casino, das es wert ist, ausprobiert zu werden.
https://tipicocasino.one/
Kamagra Oral Jelly: kamagra best price – Kamagra 100mg price
Cheap generic Viagra generic ed pills Viagra Tablet price
http://sildenafiliq.xyz/# Cheap generic Viagra
Tipico Casino ist ein bekanntes Online-Casino, das eine Vielzahl von GlГјcksspielen anbietet. Viele Menschen fragen sich jedoch, ob es legal ist, in diesem Casino zu spielen.
Die gute Nachricht ist, dass Tipico Casino legal ist und vollständig lizenziert ist. Das Casino besitzt eine Lizenz der Malta Gaming Authority, die als eine der strengsten Glücksspielbehörden der Welt gilt. Dies bedeutet, dass Tipico Casino die strengen Regeln und Vorschriften einhalten muss, um sicherzustellen, dass die Spieler geschützt sind und das Spielen fair und sicher ist.
Darüber hinaus verfügt Tipico Casino über Sicherheitsmaßnahmen, um die persönlichen Daten und Transaktionen der Spieler zu schützen. Das Casino verwendet Verschlüsselungstechnologien, um sicherzustellen, dass alle Informationen sicher sind und nicht an Dritte weitergegeben werden.
Es ist jedoch wichtig zu beachten, dass Glücksspiel in einigen Ländern eingeschränkt oder sogar illegal ist. Bevor Sie also im Tipico Casino spielen, sollten Sie sicherstellen, dass Glücksspiel in Ihrem Land erlaubt ist und Sie die jeweiligen Gesetze und Vorschriften einhalten.
Zusammenfassend ist Tipico Casino ein legales und sicheres Online-Casino, das strengen Vorschriften unterliegt, um sicherzustellen, dass die Spieler geschützt sind und das Spielen fair und transparent ist. Also, wenn Sie gerne spielen, können Sie beruhigt im Tipico Casino spielen.
https://tipicocasino.one/
Generic Tadalafil 20mg price: Generic Tadalafil 20mg price – Buy Tadalafil 20mg
Компания «Эколан» предлагает впечатлительный выбор высококачественных товаров. У нас вы найдете замечательные декоративные подушки, одеяла, простыни, пледы, наматрасники, скатерти, полотенца и это далеко не полный перечень. Гарантируем оперативную доставку и заманчивые цены. https://ecolan37.ru – сайт, где найдете только самое интересное для домашнего уюта и комфорта. Всегда готовы помочь с выбором нашим клиентам, мы их ценим и постараемся решить самые интересующие их вопросы. Заказывая у нас, можете быть уверены в том, что останетесь приобретением, довольны.
Wenn es um Online-Casinos geht, gibt es viele verschiedene Bonusangebote, die die Spieler ansprechen sollen. Einer der beliebtesten Bonustypen ist der Treuebonus, den viele Casinos anbieten, um ihre treuen Kunden zu belohnen. Ein solcher Treuebonus wird auch vom Tipico Casino angeboten.
Der Tipico Casino Bonus Treue belohnt Spieler, die regelmäßig im Casino spielen und ihre Treue zum Anbieter zeigen. Der Bonus kann verschiedene Formen annehmen, zum Beispiel als wöchentlicher Cashback-Bonus, als Extra-Guthaben für das Spielen bestimmter Spiele oder als exklusive Boni und Aktionen, die nur für treue Kunden verfügbar sind.
Um den Tipico Casino Bonus Treue zu erhalten, müssen Spieler in der Regel eine gewisse Anzahl von Einsätzen tätigen oder eine bestimmte Menge an Geld im Casino umsetzen. Je treuer ein Spieler ist und je mehr er im Casino spielt, desto höher fällt in der Regel der Treuebonus aus.
Der Tipico Casino Bonus Treue ist eine großartige Möglichkeit, um als Spieler zusätzliches Guthaben oder andere Belohnungen zu erhalten und das Spielerlebnis im Casino noch spannender zu gestalten. Es lohnt sich also, treu zu bleiben und regelmäßig im Tipico Casino zu spielen, um von diesen Bonusangeboten zu profitieren.
https://tipicocasino.one/
Kamagra 100mg price: kamagra best price – Kamagra Oral Jelly
http://tadalafiliq.shop/# Generic Tadalafil 20mg price
Viagra online price generic ed pills Cheap Sildenafil 100mg
Die Zet Casino App – Das ultimative Spielerlebnis direkt auf Ihrem Smartphone
Im Zeitalter der Digitalisierung ist es auch in der Welt des Glücksspiels längst nichts Neues mehr, dass immer mehr Online Casinos ihren Kunden die Möglichkeit bieten, ihre Lieblingsspiele auch mobil von unterwegs aus zu genießen. Eine dieser innovativen Apps ist die Zet Casino App, die es Spielern ermöglicht, ihr Casino-Erlebnis auch auf ihren Smartphones und Tablets zu erleben.
Die Zet Casino App bietet eine Vielzahl von spannenden Spielen, darunter Slots, Tischspiele und Live-Casino-Spiele. Egal ob Sie ein Fan von traditionellen Spielautomaten sind oder lieber Roulette, Blackjack oder Poker spielen – mit der Zet Casino App haben Sie all diese Optionen immer griffbereit. Das Beste daran: Die App wurde speziell fГјr mobile GerГ¤te optimiert, um ein reibungsloses Spielerlebnis auf kleineren Bildschirmen zu gewГ¤hrleisten.
Doch nicht nur die Auswahl an Spielen macht die Zet Casino App so attraktiv, auch die Nutzerfreundlichkeit spielt eine groГџe Rolle. Die App ist benutzerfreundlich gestaltet und bietet eine intuitive Navigation, damit Sie sich schnell und einfach zurechtfinden. Zudem kГ¶nnen Sie bequem Ein- und Auszahlungen tГ¤tigen, den Kundendienst kontaktieren und von Bonusangeboten profitieren – alles direkt Гјber die App.
Ein weiterer Vorteil der Zet Casino App ist die Möglichkeit, die Spiele auch im Demomodus zu spielen. So können Sie neue Spiele ausprobieren, ohne dabei echtes Geld setzen zu müssen. Dadurch haben Sie die Möglichkeit, sich mit den Regeln und Funktionen vertraut zu machen, bevor Sie um echtes Geld spielen.
Insgesamt bietet die Zet Casino App ein herausragendes Spielerlebnis, das sich nicht hinter dem SpielspaГџ am PC verstecken muss. Egal ob Sie auf Ihrem tГ¤glichen Arbeitsweg, im Park oder auf Reisen sind – mit der Zet Casino App haben Sie Ihr Lieblingscasino immer dabei. Probieren Sie es aus und tauchen Sie ein in die aufregende Welt des Online-GlГјcksspiels – ganz bequem auf Ihrem Smartphone oder Tablet.
https://zetcasino.one/
На сайте https://lemon-car.ru/ укажите номер телефона для того, чтобы воспользоваться услугами проверенного, надежного автосервиса, который работает на выгодных условиях. На все услуги даются гарантии, потому как в компании работают лучшие и компетентные специалисты, знающие свою работу. Прямо сейчас вы сможете записаться на интересующую услугу. Для вас доступен кузовной, слесарный ремонт, двигателя, а также АКПП. Оказывается полный комплекс услуг. В первую очередь, осуществляется диагностика автомобиля, а потом определяется стоимость ремонта.
cheap viagra: cheapest viagra – buy Viagra online
юрист по строительным спорам
помощь юриста бизнесу
Boomerang Casino Freispiele sind die perfekte Möglichkeit, um das beliebte Online Casino kennenzulernen und dabei gleichzeitig die Chance auf tolle Gewinne zu haben. Das Casino bietet seinen Spielern regelmäßig Freispiele an, mit denen sie kostenlos an ausgewählten Spielautomaten spielen können.
Die Boomerang Casino Freispiele sind eine tolle Möglichkeit, um neue Spiele auszuprobieren und sich mit den verschiedenen Funktionen vertraut zu machen. Dabei können Spieler ohne Einsatz von eigenem Geld echte Gewinne erzielen. Die Freispiele werden in der Regel als Willkommensbonus für neue Spieler oder als Belohnung für treue Kunden angeboten.
Um die Boomerang Casino Freispiele zu erhalten, müssen Spieler sich lediglich anmelden und eine Einzahlung tätigen. In der Regel werden die Freispiele dann automatisch gutgeschrieben und können sofort genutzt werden. Die Anzahl der Freispiele kann je nach Aktion variieren, so dass Spieler immer wieder die Chance haben, von großzügigen Angeboten zu profitieren.
Die Boomerang Casino Freispiele sind eine großartige Möglichkeit, um ohne Risiko zu spielen und dennoch die Spannung und Aufregung eines echten Casinos zu erleben. Mit etwas Glück können Spieler dabei auch ordentliche Gewinne erzielen und sich über zusätzliches Guthaben freuen.
Insgesamt sind die Boomerang Casino Freispiele eine fantastische Möglichkeit, um das Online Casino kennenzulernen und dabei ein paar Runden an den beliebten Spielautomaten zu drehen. Spieler sollten regelmäßig nach neuen Freispielaktionen Ausschau halten, um immer auf dem neuesten Stand zu bleiben und von attraktiven Angeboten zu profitieren.
https://boomerangcasino.one/
Cialis without a doctor prescription: Tadalafil price – cheapest cialis
юрист по банковскому праву
сервисы ремонта телефонов в москве
список мастерских по ремонту ноутбуков
http://kamagraiq.shop/# super kamagra
Zet Casino Kasinobonukset: Ein Гњberblick Гјber die besten Angebote
Kasinobonukset sind eine beliebte Methode, um neue Spieler anzulocken und bestehende Spieler zu belohnen. Zet Casino gehört zu den Anbietern, die regelmäßig großzügige Boni und Aktionen für ihre Kunden anbieten. In diesem Artikel werfen wir einen genauen Blick auf die verschiedenen Kasinobonukset, die bei Zet Casino verfügbar sind.
Einer der beliebtesten Boni bei Zet Casino ist der Willkommensbonus für neue Spieler. Dieser Bonus bietet neuen Kunden die Möglichkeit, ihr Konto aufzuladen und zusätzliches Geld zum Spielen zu erhalten. Der Willkommensbonus bei Zet Casino kann je nach Einzahlungsbetrag und Aktionszeitraum variieren, daher ist es wichtig, regelmäßig die Webseite des Casinos zu besuchen, um die aktuellsten Angebote zu nutzen.
Darüber hinaus bietet Zet Casino auch regelmäßig Einzahlungsboni und Freispiele für seine bestehenden Kunden an. Diese Boni können der Bankroll der Spieler einen zusätzlichen Schub geben und die Gewinnchancen erhöhen. Spieler sollten darauf achten, die entsprechenden Bonuscodes bei ihrer Einzahlung einzugeben, um sicherzustellen, dass der Bonus korrekt gutgeschrieben wird.
Zet Casino belohnt auch treue Spieler mit einem VIP-Programm, das verschiedene exklusive Boni und Prämien für regelmäßige Spieler bietet. Je mehr ein Spieler im Casino spielt, desto höher steigt er im VIP-Status auf und desto bessere Belohnungen kann er erwarten.
Insgesamt bietet Zet Casino seinen Kunden eine breite Palette an Kasinobonukset, die es wert sind, genutzt zu werden. Spieler sollten sich regelmäßig über die aktuellen Angebote informieren und sicherstellen, dass sie alle verfügbaren Boni optimal nutzen.
Abschließend lässt sich sagen, dass Kasinobonukset eine großartige Möglichkeit sind, um das Spielerlebnis bei Zet Casino noch unterhaltsamer und lukrativer zu gestalten. Nutzen Sie die verschiedenen Boni und Angebote, um Ihre Gewinnchancen zu maximieren und das Beste aus Ihrem Casinoerlebnis herauszuholen. Viel Glück und Spaß beim Spielen!
https://zetcasino.one/
https://tadalafiliq.com/# Generic Tadalafil 20mg price
Cialis 20mg price in USA Buy Cialis online Cialis 20mg price
Viagra generic over the counter: best price on viagra – buy Viagra online
Zet Casino PayNPlay: Ein revolutionäres Zahlungssystem für Online-Glücksspiele
In der Welt der Online-Casinos gibt es ständig neue Innovationen und Technologien, die das Spielerlebnis verbessern und vereinfachen. Eines der neuesten und aufregendsten Entwicklungen ist das PayNPlay-System von Zet Casino. Diese revolutionäre Zahlungsmethode bietet Spielern die Möglichkeit, ohne Registrierung und lästige Verifizierungsprozesse zu spielen.
Das PayNPlay-System funktioniert auf der Grundlage von Trustly, einem führenden Anbieter von Zahlungsdiensten im Internet. Durch die Verknüpfung Ihres Bankkontos mit Ihrem Zet Casino-Konto können Sie jederzeit und überall sofort Geld einzahlen und abheben, ohne lange Wartezeiten oder zusätzliche Gebühren. Dies macht das Spielen im Zet Casino unglaublich bequem und benutzerfreundlich.
Ein weiterer groГџer Vorteil des Zet Casino PayNPlay-Systems ist die Sicherheit, die es bietet. Da Ihre Bankdaten direkt mit dem Casino verbunden sind, mГјssen Sie sich nie Sorgen um die Sicherheit Ihrer Zahlungen machen. Ihre sensiblen Informationen sind geschГјtzt und sicher, wГ¤hrend Sie sich auf das Wesentliche – das Spielen – konzentrieren kГ¶nnen.
Zet Casino bietet eine Vielzahl von beliebten Spielen und Spielautomaten, die von fГјhrenden Softwareanbietern wie NetEnt, Microgaming und Play’n GO bereitgestellt werden. Mit dem PayNPlay-System kГ¶nnen Sie einfach Ihr Lieblingsspiel auswГ¤hlen, eine Einzahlung tГ¤tigen und sofort loslegen, ohne Zeit zu verschwenden.
Insgesamt ist das Zet Casino PayNPlay-System eine großartige Innovation, die das Online-Glücksspiel revolutioniert. Mit seiner Benutzerfreundlichkeit, Sicherheit und Schnelligkeit ist es die perfekte Lösung für Spieler, die ein nahtloses und unkompliziertes Spielerlebnis suchen. Probieren Sie es noch heute aus und entdecken Sie die Zukunft des Online-Glücksspiels!
https://zetcasino.one/
Das Boomerang-Casino: Eine aufregende neue Spielerfahrung
Das Boomerang-Casino ist eine innovative Online-GlГјcksspielplattform, die in der Welt des Online-Casinos fГјr Furore gesorgt hat. Mit einer Vielzahl von Spielen, groГџzГјgigen Boni und einem modernen Design bietet das Boomerang-Casino ein Spielerlebnis, das seinesgleichen sucht.
Einzigartig am Boomerang-Casino ist das Konzept des “Boomerang-Effekts”. Г„hnlich wie ein Boomerang, der immer wieder zu seinem Ausgangspunkt zurГјckkehrt, bietet das Casino den Spielern regelmäßige Boni und Promotionen, die sie immer wieder auf die Plattform zurГјcklocken. Dieser Ansatz hat sich als Г¤uГџerst beliebt erwiesen und hat dazu gefГјhrt, dass viele Spieler dem Boomerang-Casino treu geblieben sind.
Das Boomerang-Casino bietet eine breite Palette von Spielen, darunter Slots, Tischspiele und Live-Casino-Spiele. Mit Spielen von fГјhrenden Softwareanbietern wie NetEnt, Microgaming und Play’n GO kГ¶nnen die Spieler sicher sein, dass sie hochwertige und unterhaltsame Spiele genieГџen werden. DarГјber hinaus bietet das Casino regelmäßig neue Spiele sowie exklusive Titel an, die nur auf der Plattform verfГјgbar sind.
Neben einer Vielzahl von Spielen und spannenden Boni legt das Boomerang-Casino auch großen Wert auf Sicherheit und Fairness. Die Plattform verfügt über eine gültige Glücksspiellizenz und verwendet die neueste SSL-Verschlüsselungstechnologie, um sicherzustellen, dass die persönlichen und finanziellen Daten der Spieler geschützt sind. Das Casino arbeitet auch mit unabhängigen Prüfungsbehörden zusammen, um sicherzustellen, dass die Spiele fair und zufällig sind.
Insgesamt bietet das Boomerang-Casino eine aufregende und lohnende Spielerfahrung fГјr GlГјcksspielfans. Mit einer vielfГ¤ltigen Auswahl an Spielen, groГџzГјgigen Boni und einem innovativen Konzept des “Boomerang-Effekts” hat sich das Casino als eine der fГјhrenden Online-GlГјcksspielplattformen etabliert. Wenn Sie auf der Suche nach einem neuen und aufregenden Casino-Erlebnis sind, sollten Sie definitiv einen Blick auf das Boomerang-Casino werfen.
https://boomerangcasino.one/
http://sildenafiliq.com/# Cheap generic Viagra
Tadalafil price: Generic Tadalafil 20mg price – Buy Tadalafil 10mg
Cialis 20mg price in USA cheapest cialis Cialis 20mg price in USA
Boomerang Casino Dokumentation
Boomerang Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und spannenden Möglichkeiten für Spieler bietet. Um sicherzustellen, dass Spieler alle notwendigen Informationen haben, um das Beste aus ihrem Spielerlebnis herauszuholen, wird eine umfassende Dokumentation bereitgestellt.
Die Boomerang Casino Dokumentation umfasst eine Vielzahl von Informationen, die Spielern helfen, sich zurechtzufinden und das Casino optimal nutzen zu können. Dies beinhaltet Informationen über die verschiedenen Spiele, die angeboten werden, sowie Tipps und Tricks, um das Spiel zu verbessern. Die Dokumentation erklärt auch die verschiedenen Funktionen des Casinos, wie z.B. Ein- und Auszahlungsmethoden, Boni und Aktionen sowie den Kundenservice.
Einer der wichtigsten Teile der Boomerang Casino Dokumentation ist die Erklärung der Regeln und Bedingungen des Casinos. Hier werden Spieler darüber informiert, welche Bedingungen sie erfüllen müssen, um Boni zu erhalten oder an Aktionen teilzunehmen. Dies hilft Spielern, Missverständnisse zu vermeiden und sicherzustellen, dass sie das Beste aus ihrem Spielerlebnis herausholen können.
Darüber hinaus bietet die Boomerang Casino Dokumentation auch Informationen über verantwortungsbewusstes Spielen und Tipps, wie Spieler sicher und verantwortungsvoll spielen können. Dies ist ein wichtiger Aspekt, um sicherzustellen, dass Spieler ihre Zeit im Casino genießen und keine negativen Auswirkungen auf ihr Leben haben.
Insgesamt ist die Boomerang Casino Dokumentation eine wertvolle Ressource für Spieler, um das Beste aus ihrem Spielerlebnis herauszuholen und sicherzustellen, dass sie alle notwendigen Informationen haben, um sicher und verantwortungsbewusst zu spielen. Mit dieser umfassenden Dokumentation können Spieler sicher sein, dass sie alles haben, was sie brauchen, um ein unterhaltsames und lohnendes Spielerlebnis im Boomerang Casino zu genießen.
https://boomerangcasino.one/
Zet Casino Auszahlung Probleme
Das Zet Casino gilt als eines der beliebtesten Online Casinos auf dem Markt. Trotzdem berichten einige Spieler von Auszahlungsproblemen, die sie bei der Beantragung ihrer Gewinne erlebt haben. Dies hat Besorgnis bei den Spielern geweckt und wirft Fragen über die Seriosität des Casinos auf.
Einige Spieler berichten davon, dass ihre Auszahlungen verzögert worden sind oder dass sie die Zahlungen gar nicht erhalten haben. Dies ist natürlich frustrierend für die Spieler, die darauf vertraut haben, ihre Gewinne zeitnah zu erhalten. Einige Spieler haben auch von unklaren Auszahlungsbedingungen berichtet, die zu Verwirrung führen.
Es ist wichtig, dass Online Casinos transparent und fair bei der Auszahlung der Gewinne sind. Spieler sollten sich darauf verlassen können, dass sie ihre Gewinne ohne Probleme und Verzögerungen erhalten. Auszahlungsprobleme können das Vertrauen der Spieler in das Casino erschüttern und langfristig negative Auswirkungen auf das Geschäft haben.
Das Zet Casino sollte daher sicherstellen, dass Auszahlungen schnell und zuverlässig erfolgen und dass die Auszahlungsbedingungen klar und verständlich sind. Es ist wichtig, dass das Casino auf die Bedenken der Spieler eingeht und Lösungen für etwaige Probleme bietet.
Spieler sollten sich bewusst sein, dass es Auszahlungsprobleme in einigen Online Casinos geben kann und daher darauf achten, bei seriösen Anbietern zu spielen. Es ist ratsam, Bewertungen und Erfahrungsberichte anderer Spieler zu lesen, um sicherzustellen, dass das gewählte Casino vertrauenswürdig ist.
Insgesamt ist es zu hoffen, dass das Zet Casino seine Auszahlungsprobleme in den Griff bekommt und seinen Spielern ein positives Spielerlebnis bietet. Transparenz und Fairness sind entscheidend fГјr das Vertrauen der Spieler und das langfristige Wachstum des Casinos.
https://zetcasino.one/
buy Kamagra: sildenafil oral jelly 100mg kamagra – buy kamagra online usa
https://sildenafiliq.xyz/# п»їBuy generic 100mg Viagra online
해운대고구려와 부산룸싸롱: 색다른 경험을 찾아서
한국의 여러 도시에서 룸싸롱은 많은 이들에게 인기 있는 엔터테인먼트 형태 중
하나로 자리잡고 있습니다. 특히 해운대와 부산은 이러한 시설들이 다양하게 분포되어
있어 많은 사람들의 관심을 끌고 있습니다.
이번 글에서는 해운대고구려와 부산룸싸롱에 대해 알아보고자 합니다.
해운대고구려는 해운대지역에서 인기 있는 룸싸롱 중
하나로 알려져 있습니다. 이 곳은 고품격의 서비스와 다채로운 프로그램으로 손님들의 만족도를 높이고 있습니다.
또한 해운대고구려사이트를 통해 사전에 예약을 할 수 있어 편리함을 제공하고 있습니다.
해운대고구려는 해운대지역의 관광명소와도 가까워 해변에서의 즐거운 시간을
보내고 난 뒤 편안한 휴식을 취할 수
있는 장소로 유명합니다.
해운대룸싸롱추천을 받는 부산룸싸롱도 매력적인 곳으로 손님들에게 다양한 프로그램과 서비스를 제공하고 있습니다.
부산룸싸롱사이트를 통해 간편하게 예약을 할
수 있어 시간을 절약할 수 있습니다.
또한 부산고구려도 많은 이용자들로부터 좋은 후기를
받고 있어 룸싸롱을 찾는 이들에게 인기를 끌고 있습니다.
해운대고구려와 부산룸싸롱은 다양한 가격대를 제공하고 있어 개인의 취향에 맞는 선택이
가능합니다. 해운대룸가격을 비교하고 적정한 가격에 맞는 서비스를 선택할 수 있습니다.
또한 해운대고구려40페이와 같은 이벤트를 통해 손님들에게 다양한
혜택을 제공하고 있어 더욱 많은 이들의 관심을 끌고 있습니다.
마지막으로, 해운대고구려와 부산룸싸롱은 색다른
경험을 원하는 이들에게 좋은 선택지입니다.
안전한 환경과 다채로운 프로그램으로 손님들의
만족도를 높이고 있으며, 편리한 예약 시스템을 통해 손쉽게
이용할 수 있습니다. 해운대와 부산을 여행하는 동안 특별한 추억을 만들고 싶다면 해운대고구려나 부산룸싸롱을 방문해보는 것은 어떨까요?
http://canadianpharmgrx.com/# pharmacy wholesalers canada
Zet Casino ist ein Online-Casino, das seinen Spielern eine Vielzahl von spannenden Spielen und attraktiven Bonusangeboten bietet. Eines der beliebtesten Angebote des Casinos ist das sogenannte “ei talletuskasino”, was auf Finnisch “keine Einzahlung erforderlich” bedeutet.
Bei Zet Casino kann man also spielen, ohne zuerst eine Einzahlung tГ¤tigen zu mГјssen. Dies ist besonders attraktiv fГјr Spieler, die das Casino erst einmal ausprobieren mГ¶chten, ohne gleich ihr eigenes Geld riskieren zu mГјssen. Durch das “ei talletuskasino” Angebot kГ¶nnen sie sich in Ruhe mit den Spielen vertraut machen und die verschiedenen Funktionen des Casinos testen.
Darüber hinaus bietet Zet Casino auch eine Vielzahl von anderen Bonusangeboten und Aktionen für seine Spieler an. Dazu gehören unter anderem Willkommensboni, Freispiele und Cashback-Angebote. Mit diesen Boni haben die Spieler die Möglichkeit, ihre Gewinne zu maximieren und ihr Spielerlebnis noch aufregender zu gestalten.
Zet Casino ist sowohl für Anfänger als auch für erfahrene Spieler geeignet und bietet ein breites Spektrum an Spielen, darunter Spielautomaten, Tischspiele, Live-Casino-Spiele und vieles mehr. Das Casino legt großen Wert auf Sicherheit, Fairness und Transparenz und arbeitet ausschließlich mit seriösen Zahlungsanbietern zusammen.
Wer also auf der Suche nach einem erstklassigen Online-Casino ist, das ein “ei talletuskasino” Angebot und viele weitere spannende Features bietet, sollte sich unbedingt einmal bei Zet Casino umschauen. Vielleicht ist das GlГјck ja schon auf Ihrer Seite und Sie kГ¶nnen ohne Einzahlung tolle Gewinne erzielen. Viel SpaГџ beim Spielen und viel GlГјck!
https://zetcasino.one/
best online pharmacies in mexico: Pills from Mexican Pharmacy – mexico pharmacies prescription drugs
Компания АБК предлагает по доступным ценам выгодные условия. Мы предоставляем качественные бытовки, потому как нацелены на долгосрочные отношения с заказчиками. Доброжелательные отзывы клиентов компании – это лучшее подтверждение нашей надежности. Ищете аренда бытовок в москве и московской? Arendabk.ru – сайт, где можете ознакомиться с фотогалереей, которая дает представление об оформлении вагончиков. Наши специалисты оперативно реагируют на заявки. Доставка быстро выполняется. Обращайтесь к нам, рады вам помочь!
Зайдите на сайт https://akb-shtabeler.ru/ где вы сможете купить аккумуляторы для штабелеров, а также электрические штабелеры от дилеров. Лучшие цены, всегда в наличии на складе, доставка в любой регион. Ознакомьтесь на сайте с брендами штабелеров и каталогом тяговых аккумуляторов для них, для всех брендов.
canadian pharmacy 24h com Certified Canadian pharmacies canadian pharmacy cheap
Tipico Casino Freispiele kaufen
In vielen Online Casinos haben Spieler die Möglichkeit, Freispiele zu erwerben, um damit ihr Glück bei verschiedenen Spielautomaten zu versuchen. Auch im Tipico Casino gibt es die Möglichkeit, Freispiele zu kaufen und so die Spannung und Nervenkitzel beim Spielen zu erhöhen.
Durch den Kauf von Freispielen können Spieler direkt in die Action einsteigen, ohne auf den Zufall angewiesen zu sein, um Freispiele während des Spiels zu erhalten. Dies ermöglicht es den Spielern, schneller mit dem Spielen zu beginnen und potenziell größere Gewinne zu erzielen.
Um Freispiele im Tipico Casino zu kaufen, müssen die Spieler einfach den entsprechenden Bereich im Casino besuchen und dort die verfügbaren Angebote prüfen. Oftmals gibt es verschiedene Pakete zur Auswahl, die unterschiedliche Anzahlen von Freispielen enthalten. Die Preise für die Freispiele variieren je nach Angebot und können mit Echtgeld oder Bonusguthaben bezahlt werden.
Bevor man Freispiele kauft, ist es wichtig zu beachten, dass die Gewinne, die mit diesen erzielt werden, oft bestimmten Umsatzbedingungen unterliegen. Diese Bedingungen geben an, wie oft die Gewinne aus den Freispielen umgesetzt werden müssen, bevor sie ausgezahlt werden können. Es ist daher ratsam, die Bedingungen genau zu lesen, bevor man sich für den Kauf von Freispielen entscheidet.
Trotzdem kann der Kauf von Freispielen im Tipico Casino eine aufregende Möglichkeit sein, um das Spielerlebnis zu verbessern und die Chancen auf Gewinne zu erhöhen. Mit etwas Glück und Geschick können die Spieler mit den gekauften Freispielen große Gewinne erzielen und ihr Casinoerlebnis noch spannender gestalten.
https://tipicocasino.one/
protonix for gerd
mexican pharmaceuticals online: buying prescription drugs in mexico – buying prescription drugs in mexico
На сайте http://www.tribal-tattoo.ru ознакомьтесь с тем, какими услугами вы сможете воспользоваться в тату-салоне. Есть возможность заказать перманентный татуаж губ, в том числе, контур с растушевкой, татуаж бровей. К вашим услугам исправление татуировок, нанесение новой тату, чтобы замаскировать старую. Также доступно перекрытие шрамов, рубцов. Рисунки подбираются в зависимости от предпочтений, а также особенностей. При необходимости мастер выберет для вас оптимальный вариант. Услуга абсолютно безопасная.
Sebagai situs slot gacor terkemuka, KOKIGAMES88 memberikan peluang menang yang hampir tak tertandingi.
Dengan rate kemenangan yang mencapai 98,7%, pemain diberikan kesempatan lebih besar untuk membawa pulang kemenangan besar.
Angka tersebut bukan hanya sekedar klaim, melainkan hasil dari komitmen situs dalam memberikan pengalaman bermain yang
adil dan menguntungkan.
DUBAI77 merupakan salah satu situs casino dan judi slot online terpopuler
bagi para pemain casino dan slot gacor karena menawarkan berbagai macam permainan judi casino dan slot online
yang lebih mudah dimainkan dan tersedia dalam banyak jenis.
I’m amazed, I must say. Seldom do I encounter a bblog that’s bofh equally educative and amusing, and let me tell you,
you’ve hit the nail on thhe head. The issue is something which not enkugh people
are speaking intelligenly about. I’m very happy I found
this in my hunt for something concerning this.
Here is my web blog: 카지노사이트
Tipico Casino Roulette Live ist eine aufregende Möglichkeit, das beliebte Tischspiel in einem authentischen Casino-Erlebnis zu genießen. Mit echten Dealern und einer interaktiven Spielumgebung können Spieler von überall aus auf der Welt an diesem spannenden Spiel teilnehmen.
Das Live-Roulette bei Tipico Casino bietet eine Vielzahl von Einsatzmöglichkeiten, um den Spielern eine individuelle und unterhaltsame Erfahrung zu bieten. Die Spieler können ihre Einsätze platzieren, den Blick auf das sich drehende Rad werfen und mit den Live-Dealern kommunizieren. Dies schafft eine lebendige und immersive Atmosphäre, die dem Spiel eine ganz neue Dimension hinzufügt.
Ein weiterer Vorteil von Tipico Casino Roulette Live ist die Möglichkeit, das Spiel jederzeit und überall zu spielen. Mit der mobilen App von Tipico können Spieler das Live-Roulette bequem von ihrem Smartphone oder Tablet aus genießen, ohne dabei auf Qualität oder Geschwindigkeit verzichten zu müssen. Dies ermöglicht es den Spielern, ihre Lieblings-Tischspiele auch unterwegs zu genießen.
DarГјber hinaus bietet Tipico Casino Roulette Live eine sichere und vertrauenswГјrdige Spielumgebung. Die Live-Dealer bei Tipico sind professionell ausgebildet und sorgen fГјr ein faires und transparentes Spiel. AuГџerdem verwendet Tipico Casino modernste VerschlГјsselungstechnologien, um sicherzustellen, dass alle Spielerdaten geschГјtzt sind.
Insgesamt ist Tipico Casino Roulette Live eine aufregende Möglichkeit, das klassische Tischspiel in einem ansprechenden und interaktiven Format zu genießen. Mit echten Dealern, einer vielfältigen Auswahl an Einsatzmöglichkeiten und einer mobilen App, die es ermöglicht, das Spiel jederzeit und überall zu spielen, ist Tipico Casino Roulette Live definitiv einen Versuch wert. Probieren Sie es noch heute aus und tauchen Sie ein in die aufregende Welt des Live-Roulettes bei Tipico Casino. Viel Spaß und viel Glück!
https://tipicocasino.one/
https://911-photo.ru/
Топ база https://top-base.ru/ это каталог ведущих предприятий России по металлообработке, нефтяной промышленности, базы металлопроката, металлорежущего и измерительного инструмента и других видов смежных отраслей. Также на сайте вы сможете ознакомиться с технической литературой и справочниками различных ГОСТов и ТУ, зарубежными аналогами стали и труб, допусками и посадками и многим другим.
You really make it appear really easy with your
presentation however I in finding this topic to be actually something
that I think I’d never understand. It sort of feels too complex and
very huge for me. I’m looking ahead to your subsequent put up,
I’ll try to get the hang of it!
https://vip-naves.ru/
Hi there, all is going nicely here and ofcourse every one
is sharing data, that’s really fine, keep up writing.
Thanks very interesting blog!
reliable canadian pharmacy Canadian pharmacy prices canadian discount pharmacy
Das Zet Online Casino ist eine der beliebtesten Online-GlГјcksspielplattformen fГјr Spieler aus Deutschland. Mit einer groГџen Auswahl an Spielen, groГџzГјgigen Boni und einem benutzerfreundlichen Design hat sich das Zet Casino schnell einen Namen in der Branche gemacht.
Egal, ob Sie gerne Slots spielen, Tischspiele wie Blackjack und Roulette bevorzugen oder Ihr Glück bei Live-Dealer-Spielen versuchen möchten, im Zet Online Casino finden Sie sicherlich das passende Spiel für sich. Die Plattform arbeitet mit den renommiertesten Softwareanbietern der Branche zusammen, um ihren Spielern ein erstklassiges Spielerlebnis zu bieten.
Ein weiterer großer Pluspunkt des Zet Online Casinos sind die großzügigen Bonusangebote und Aktionen. Neue Spieler können sich über einen Willkommensbonus freuen, der ihnen zusätzliches Guthaben oder Freispiele für ausgewählte Spiele bietet. Darüber hinaus gibt es regelmäßig Promotionen und Turniere, bei denen Spieler attraktive Preise gewinnen können.
Das Zet Online Casino legt großen Wert auf Sicherheit und Fairness. Die Plattform verfügt über eine Lizenz der Malta Gaming Authority, einer der strengsten Glücksspielbehörden der Welt. Zudem werden alle Spiele regelmäßig von unabhängigen Prüfinstituten überwacht, um sicherzustellen, dass sie fair und transparent sind.
Insgesamt bietet das Zet Online Casino ein rundum gelungenes Spielerlebnis für alle Glücksspiel-Fans. Mit einer vielfältigen Spielauswahl, großzügigen Boni und einem engagierten Kundenservice ist das Zet Casino definitiv eine Empfehlung wert. Besuchen Sie noch heute die Plattform und erleben Sie die aufregende Welt des Online-Glücksspiels!
https://zetcasino.one/
http://canadianpharmgrx.com/# reputable canadian online pharmacy
Oh my goodness! Awesome article dude! Thanks, However I am experiencing problems with your RSS.
I don’t know why I cannot subscribe to it. Is there anybody getting
identical RSS issues? Anyone who knows the
solution can you kindly respond? Thanks!!
Zet Casino ist ein Online-Casino, das Spielern eine große Auswahl an Spielen und zahlreiche Bonusangebote bietet. Das Casino wurde im Jahr 2018 gegründet und hat seitdem viele Spieler angezogen, die auf der Suche nach Unterhaltung und Gewinnmöglichkeiten sind.
Das Casino bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele, Live-Casino-Spiele und vieles mehr. Diese Spiele werden von einigen der besten Spieleentwickler der Branche bereitgestellt, darunter NetEnt, Microgaming, Play’n GO und viele andere. Dadurch ist eine hohe QualitГ¤t und Vielfalt der Spiele garantiert.
Zet Casino bietet auch großzügige Bonusangebote für neue Spieler sowie regelmäßige Aktionen für bestehende Spieler. Neue Spieler können einen Willkommensbonus in Anspruch nehmen, der Freispiele und Bonusgeld umfasst. Es gibt auch wöchentliche Einzahlungsboni, Cashback-Angebote und ein Treueprogramm, das Spielern zusätzliche Belohnungen für ihre Treue bietet.
Das Casino ist auch für seine zuverlässigen Zahlungsoptionen bekannt, die schnelle und sichere Transaktionen ermöglichen. Spieler können zwischen verschiedenen Zahlungsmethoden wählen, darunter Kreditkarten, E-Wallets, Banküberweisungen und mehr.
Zet Casino ist lizenziert und reguliert und bietet seinen Spielern ein faires und sicheres Spielerlebnis. Der Kundenservice steht Spielern rund um die Uhr zur VerfГјgung und kann per E-Mail, Live-Chat oder Telefon erreicht werden.
Insgesamt ist Zet Casino eine gute Wahl fГјr Spieler, die auf der Suche nach einer Vielzahl von Spielen, groГџzГјgigen Boni und einem sicheren Spielerlebnis sind. Probieren Sie es aus und erleben Sie die Unterhaltung und Spannung, die das Casino zu bieten hat!
https://zetcasino.one/
Its like you learn my mind! You seem to know so much about this, such
as you wrote the book in it or something. I think that you just
can do with some % to pressure the message house a bit, but other than that, this is magnificent blog.
A great read. I’ll definitely be back.
http://mexicanpharmgrx.com/# mexican rx online
I read this paragraph fully about the comparison of latest and earlier technologies, it’s remarkable article.
Das Boomerang Casino hat sich in der Welt der Online-Casinos einen Namen gemacht, vor allem dank seiner großzügigen Boni und Aktionen. Unter den beliebten Angeboten sind die Boomerang Casino No Deposit Bonus Codes, die es Spielern ermöglichen, ohne eine Einzahlung kostenfrei zu spielen.
Die No Deposit Bonus Codes sind eine großartige Möglichkeit für neue Spieler, das Casino kennenzulernen, ohne dabei eigenes Geld riskieren zu müssen. Diese Codes können auf verschiedenen Websites oder direkt vom Casino selbst gefunden werden und ermöglichen es den Spielern, kostenloses Bonusgeld oder Freispiele zu erhalten.
Um die No Deposit Bonus Codes zu nutzen, müssen Spieler einfach den Code während des Anmeldevorgangs oder im Kassenbereich eingeben. Das Bonusgeld oder die Freispiele werden dann sofort dem Spielerkonto gutgeschrieben, ohne dass eine Einzahlung erforderlich ist.
Es ist jedoch wichtig zu beachten, dass No Deposit Boni oft bestimmten Umsatzbedingungen unterliegen, die erfüllt werden müssen, bevor Gewinne ausgezahlt werden können. Es ist daher ratsam, die Geschäftsbedingungen sorgfältig zu lesen, bevor man einen Bonus in Anspruch nimmt.
Insgesamt sind die Boomerang Casino No Deposit Bonus Codes eine großartige Möglichkeit für Spieler, das Casino zu erkunden und möglicherweise sogar echte Gewinne zu erzielen, ohne dabei eigenes Geld riskieren zu müssen. Es lohnt sich daher, Ausschau nach diesen Bonuscodes zu halten und das Beste aus ihnen herauszuholen.
https://boomerangcasino.one/
canadian online drugs Best Canadian online pharmacy www canadianonlinepharmacy
Hi to all, how is the whole thing, I think every
one is getting more from this website, and your views are nice for new people.
buying from online mexican pharmacy: mexican online pharmacies prescription drugs – buying prescription drugs in mexico online
Консультация адвоката по уголовным делам – это начальный и крайне важный этап оказания
юридической помощи лицам, привлечённым к уголовной ответственности, или
желающим защитить свои интересы в уголовном процессе.
Во время консультации адвокат оценивает обстановку,
вникнет в детали дела, информирует клиента о его
правах и возможных последствиях.
Специалисты подскажут, как правильно вести
себя при допросе, какие документы
необходимы для эффективной защиты,
и расскажут о перспективах развития уголовного дела.
Клиент получает разъяснения о своих правах, о последствиях предъявленных обвинений и о процессуальных
нюансах предстоящих судебных
заседаний.
Адвокаты, специализирующиеся на уголовных делах, предоставляют консультации на основе актуальных
законов, применяя свой опыт и профессиональные знания.
Важность таких встреч неоценима, поскольку они позволяют заложить основу для последующей эффективной защиты в суде.
Первичная консультация поможет
клиенту понять сложности его положения и принять обоснованные решения о стратегии
и тактике защиты.
Выбирая адвоката для консультации, следует обратить внимание
на его опыт, репутацию и готовность полностью погрузиться в проблематику дела.
Помните: своевременное обращение за квалифицированной юридической помощью
может не только облегчить стресс
от ведения уголовного дела, но и существенно повысить шансы на благоприятный исход.
Look at my web site; платный адвокат по уголовным делам
If you wish for to increase your knowledge just keep visiting
this web page and be updated with the most up-to-date information posted here.
I’ve read some excellent stuff here. Certainly price bookmarking for revisiting.
I surprise how much attempt you put to make this kind of fantastic informative web site.
Zet Casino: Kostenloser Bonus ohne Einzahlung
Zet Casino ist eine beliebte Online-Glücksspielplattform, die Spielern eine Vielzahl von Spielen und Boni bietet. Einer der attraktivsten Boni, die das Casino seinen Spielern anbietet, ist der kostenlose Bonus ohne Einzahlung. Dieser Bonus ermöglicht es neuen Spielern, das Casino zu testen, ohne echtes Geld ausgeben zu müssen.
Um den Bonus ohne Einzahlung bei Zet Casino zu erhalten, müssen sich neue Spieler lediglich auf der Website registrieren. Nach der Registrierung wird der Bonus automatisch gutgeschrieben und steht dem Spieler zur Verfügung, um verschiedene Spiele im Casino auszuprobieren. Dieser Bonus ermöglicht es Spielern, echtes Geld zu gewinnen, ohne selbst Geld zu riskieren.
Der kostenlose Bonus ohne Einzahlung bei Zet Casino ist eine großartige Möglichkeit für Spieler, die Plattform kennenzulernen und erste Gewinne zu erzielen, ohne dabei ihr eigenes Geld zu verwenden. Es ist jedoch wichtig zu beachten, dass dieser Bonus bestimmten Umsatzbedingungen unterliegt, die vom Casino festgelegt werden.
Insgesamt ist der kostenlose Bonus ohne Einzahlung bei Zet Casino eine hervorragende Möglichkeit für neue Spieler, um die Plattform zu erkunden und ihre Lieblingsspiele auszuprobieren, ohne finanzielle Risiken eingehen zu müssen. Spieler, die auf der Suche nach einem spannenden Online-Casino-Erlebnis sind, sollten Zet Casino definitiv eine Chance geben.
https://zetcasino.one/
http://indianpharmgrx.com/# top 10 online pharmacy in india
It’s awesome for me to have a web site, which is useful for my know-how.
thanks admin
My partner and I stumbled over here from a different
website and thought I might check things out. I like what
I see so now i am following you. Look forward to going over
your web page for a second time.
30 mg remeron
Tipico Live Casino Erfahrungen
Das Tipico Live Casino ist einer der beliebtesten Anbieter für Online-Spiele in Deutschland. Spieler können hier eine große Auswahl an verschiedenen Casino-Spielen genießen, darunter Roulette, Blackjack, Baccarat und Poker. Das Live Casino wird von professionellen und freundlichen Dealern betreut, die für ein authentisches Casino-Erlebnis sorgen.
Die Erfahrungen vieler Spieler mit dem Tipico Live Casino sind durchweg positiv. Besonders lobend wird die hohe Qualität der Live-Übertragung und die reibungslose Funktionalität der Spiele erwähnt. Die Dealer sind nicht nur kompetent, sondern auch unterhaltsam und sorgen so für eine angenehme Atmosphäre am Spieltisch.
Ein weiterer Pluspunkt des Tipico Live Casinos ist die große Auswahl an verschiedenen Spielen und Einsätzen. Egal ob Anfänger oder erfahrener Spieler, hier findet jeder das passende Spiel für sich. Zudem sind die Gewinnchancen im Tipico Live Casino fair und transparent, sodass Spieler sich auf ein faires Spielumfeld verlassen können.
Einige Spieler berichten auch von lukrativen Gewinnen im Tipico Live Casino. Durch die Möglichkeit, mit anderen Spielern und dem Dealer interagieren zu können, wird das Spielerlebnis noch einmal spannender und unterhaltsamer.
Insgesamt können wir sagen, dass das Tipico Live Casino eine empfehlenswerte Option für alle Casino-Fans ist. Mit einer großen Auswahl an Spielen, professionellen Dealern und fairen Gewinnchancen wird hier ein erstklassiges Casino-Erlebnis geboten. Probieren Sie es selbst aus und machen Sie Ihre eigenen Tipico Live Casino Erfahrungen!
https://tipicocasino.one/
I got this site from my buddy who informed me concerning this site and at the moment
this time I am visiting this web site and reading very informative posts here.
reputable indian online pharmacy indian pharmacy buy medicines online in india
oral azithromycin 250mg – buy sumycin paypal ciprofloxacin 500 mg uk
You really make it seem really easy along with your presentation however I in finding this matter
to be really something that I think I might never understand.
It sort of feels too complex and extremely extensive for me.
I am having a look ahead on your next put up, I will try to get
the dangle of it!
http://indianpharmgrx.com/# top online pharmacy india
Lauren could be the name I enjoy be called with and my
wife doesn’t take pleasure in at every bit of. My day
job is a computer operator and it’s something I enjoy. For years I have been living in District of Columbia.
What her friends and her love is kayaking but she’s been taking on new things lately.
Boomerang Casino ist eine Online-Glücksspielplattform, die es Spielern ermöglicht, verschiedene Casino-Spiele von zu Hause aus zu spielen. Mit der Boomerang Casino App können Spieler ihre Lieblingsspiele bequem auf ihren mobilen Geräten spielen.
Die App bietet eine breite Palette von Spielen, darunter Slots, Roulette, Blackjack, Poker und vieles mehr. Spieler können leicht zwischen den verschiedenen Spielen wechseln und ihre Lieblingsspiele jederzeit und überall genießen.
Die Boomerang Casino App bietet auch eine Vielzahl von Boni und Aktionen, die es Spielern ermöglichen, ihr Guthaben zu erhöhen und zusätzliche Preise zu gewinnen. Darüber hinaus bietet die App eine sichere und geschützte Spielumgebung, so dass Spieler mit Vertrauen spielen können.
Die Benutzeroberfläche der Boomerang Casino App ist einfach und benutzerfreundlich gestaltet, so dass Spieler aller Erfahrungsstufen sie leicht nutzen können. Darüber hinaus bietet die App einen schnellen und zuverlässigen Kundensupport, der Spielern bei Fragen oder Problemen zur Seite steht.
Insgesamt ist die Boomerang Casino App eine großartige Möglichkeit für Spieler, ihre Lieblingsspiele zu genießen und gleichzeitig die Bequemlichkeit des Spielens von unterwegs aus zu erleben. Mit einer Vielzahl von Spielen, Boni und Aktionen ist die App eine gute Wahl für alle Casino-Enthusiasten.
https://boomerangcasino.one/
Консультация адвоката по уголовным делам – это начальный и крайне важный этап оказания юридической помощи лицам, привлечённым к уголовной ответственности, или желающим защитить свои интересы в уголовном процессе. Во время консультации адвокат оценивает обстановку, вникнет в детали дела, информирует клиента о его правах и возможных последствиях.
Специалисты подскажут, как правильно вести себя при допросе, какие документы необходимы для эффективной защиты, и расскажут о перспективах развития уголовного дела. Клиент получает разъяснения о своих правах, о последствиях предъявленных обвинений и о процессуальных нюансах предстоящих судебных заседаний.
Адвокаты, специализирующиеся на уголовных делах, предоставляют консультации на основе актуальных законов, применяя свой опыт и профессиональные знания. Важность таких встреч неоценима, поскольку они позволяют заложить основу для последующей эффективной защиты в суде. Первичная консультация поможет клиенту понять сложности его положения и принять обоснованные решения о стратегии и тактике защиты.
Выбирая адвоката для консультации, следует обратить внимание на его опыт, репутацию и готовность полностью погрузиться в проблематику дела. Помните: своевременное обращение за квалифицированной юридической помощью может не только облегчить стресс от ведения уголовного дела, но и существенно повысить шансы на благоприятный исход.
http://annayankova.ru
500 mg robaxin
Zet Casino ist ein Online-Casino, das seit einiger Zeit auf dem Markt ist und bereits viele Spieler von sich überzeugen konnte. Auch ich habe bereits Erfahrungen mit diesem Casino gesammelt und möchte meine Eindrücke gerne mit euch teilen.
Ein groГџer Pluspunkt bei Zet Casino ist die groГџe Auswahl an Spielen. Ob Slots, Tischspiele, Live-Casino oder Jackpot-Spiele – hier findet jeder das passende Spiel fГјr sich. Die Spiele stammen von renommierten Anbietern wie NetEnt, Microgaming, Play’n GO und vielen mehr, was fГјr eine hohe QualitГ¤t und Vielfalt sorgt.
Auch die Benutzerfreundlichkeit der Webseite ist lobenswert. Das Design ist ansprechend gestaltet und die Navigation ist einfach und Гјbersichtlich. Man findet sich schnell zurecht und kann problemlos zwischen den verschiedenen Spielen wechseln.
Besonders positiv ist auch der Kundenservice von Zet Casino. Die Mitarbeiter sind rund um die Uhr erreichbar und stehen bei Fragen und Problemen kompetent zur Seite. Auch die Zahlungsmethoden sind vielfältig und sicher, sodass Ein- und Auszahlungen problemlos abgewickelt werden können.
Insgesamt kann ich Zet Casino nur weiterempfehlen. Die groГџe Auswahl an Spielen, die benutzerfreundliche Webseite und der gute Kundenservice machen dieses Online-Casino zu einer empfehlenswerten Adresse fГјr alle, die gerne online spielen. Ich freue mich bereits darauf, weitere Erfahrungen mit Zet Casino zu sammeln und kann es nur jedem empfehlen, es selbst einmal auszuprobieren.
https://zetcasino.one/
canadian pharmacy online store Canadian pharmacy prices adderall canadian pharmacy
http://mexicanpharmgrx.shop/# mexican pharmacy
cleocin brand – chloramphenicol usa buy cheap chloramphenicol
Компания АБК предлагает по доступным ценам выгодные условия. Мы предоставляем качественные бытовки, потому как нацелены на долгосрочные отношения с заказчиками. Доброжелательные отзывы клиентов компании – это лучшее подтверждение нашей надежности. Ищете аренда строительных блок контейнеров? Arendabk.ru – сайт, где у вас есть возможность посмотреть фотогалерею с оформлениями вагончиков. Специалисты компании быстро реагируют на новые заявки. Доставка быстро выполняется. Обращайтесь к нам, рады вам помочь!
Zet Casino 30 Freispiele
Zet Casino ist eine der aufstrebenden Online-Casino-Plattformen, die Spielern eine groГџe Auswahl an Spielen und attraktiven Boni bietet. Einer der beliebtesten Boni, den Zet Casino seinen Spielern anbietet, sind die 30 Freispiele, die man bei der Anmeldung erhalten kann.
Diese Freispiele sind eine großartige Möglichkeit für Spieler, das Casino und die angebotenen Spiele kennenzulernen, ohne eigenes Geld einzahlen zu müssen. Mit den 30 Freispielen können Spieler die verschiedenen Spielautomaten ausprobieren und hoffentlich sogar einige Gewinne erzielen.
Um die 30 Freispiele zu erhalten, muss man sich einfach auf der Zet Casino-Website anmelden und ein Konto erstellen. Nach der Registrierung werden die Freispiele automatisch gutgeschrieben und können sofort genutzt werden.
Es ist wichtig zu beachten, dass die Freispiele bestimmten Umsatzbedingungen unterliegen, die erfГјllt werden mГјssen, bevor man etwaige Gewinne auszahlen lassen kann. Diese Bedingungen variieren je nach Casino und sollten daher vor der Nutzung der Freispiele ГјberprГјft werden.
Insgesamt sind die 30 Freispiele, die Zet Casino anbietet, eine großartige Möglichkeit für Spieler, das Casino auszuprobieren und möglicherweise sogar einige Gewinne zu erzielen, ohne eigenes Geld investieren zu müssen. Wer gerne Spielautomaten spielt, sollte diese Gelegenheit nicht verpassen und sich die Freispiele sichern. Viel Spaß und viel Glück beim Spielen!
https://zetcasino.one/
order cleocin 300mg generic – chloromycetin uk how to buy chloromycetin
side effects protonix
На сайте http://kinomanhd720.online находятся самые популярные, интересные и увлекательные фильмы на разный вкус и различного жанра: драмы, комедии, триллеры, ужасы и многое другое. Вы обязательно найдете то, что посмотреть сегодня вечером, чтобы разнообразить досуг. Все они представлены в отличном качестве и с хорошим звуком. Также имеются и сериалы, мультфильмы, мистические фильмы, которые точно никого не оставят равнодушным. Специально для вас есть подборки про школу, врачей, вампиров, войну, любовь.
oral zithromax 500mg – buy ofloxacin 400mg generic how to buy ciprofloxacin
Boomerang Casino ist eine aufstrebende Online-GlГјcksspielplattform, die Spielern eine erstklassige Spielerfahrung bietet. Mit einer Vielzahl von Spielen, attraktiven Bonusangeboten und einem benutzerfreundlichen Design zieht das Casino Spieler aus der ganzen Welt an.
Ein besonderes Highlight des Boomerang Casinos ist der “kod promocyjny” oder Promo-Code, den Spieler bei der Registrierung oder Einzahlung eingeben kГ¶nnen. Mit diesem Code haben Spieler die MГ¶glichkeit, zusГ¤tzliche Boni, Freispiele oder andere exklusive Angebote zu erhalten. Dies kann den Spielern einen zusГ¤tzlichen Schub geben und ihre Chancen auf Gewinne erhГ¶hen.
Das Boomerang Casino bietet eine Vielzahl von Spielen, darunter beliebte Slots, Tischspiele wie Roulette und Blackjack, sowie Live-Casino-Spiele, bei denen Spieler mit echten Dealern interagieren können. Die Spiele werden von erstklassigen Softwareanbietern wie NetEnt, Microgaming und Pragmatic Play bereitgestellt, was eine hohe Qualität und ein erstklassiges Spielerlebnis garantiert.
Darüber hinaus bietet das Boomerang Casino eine Vielzahl von Zahlungsoptionen, einschließlich Kreditkarten, E-Wallets und Banküberweisungen, um sicherzustellen, dass Spieler bequem und sicher Ein- und Auszahlungen tätigen können.
Insgesamt ist das Boomerang Casino eine erstklassige GlГјcksspielplattform, die Spielern eine Vielzahl von Spielen, attraktiven Boni und einem benutzerfreundlichen Design bietet. Mit dem “kod promocyjny” haben Spieler die MГ¶glichkeit, zusГ¤tzliche Belohnungen zu erhalten und ihr Spielerlebnis noch aufregender zu gestalten.
https://boomerangcasino.one/
https://indianpharmgrx.shop/# reputable indian pharmacies
best canadian pharmacy online International Pharmacy delivery reputable canadian online pharmacies
Zet Casino Freispiele
Zet Casino ist ein beliebtes Online-Casino, das seinen Spielern eine Vielzahl von Spielen und Boni anbietet. Eine der beliebtesten Aktionen im Zet Casino sind die Freispiele, die den Spielern die Möglichkeit geben, kostenlose Runden an ausgewählten Spielautomaten zu spielen.
Um Freispiele im Zet Casino zu erhalten, müssen Spieler bestimmte Voraussetzungen erfüllen. Oftmals werden Freispiele als Teil eines Willkommensbonus oder als Belohnung für treue Spieler angeboten. Spieler können auch Freispiele durch Sonderaktionen oder Turniere gewinnen.
Die Anzahl der Freispiele, die Spieler erhalten, variiert je nach Aktion und Angebot. In der Regel können Spieler zwischen 10 und 100 Freispiele bekommen. Die Freispiele können nur an bestimmten Spielautomaten genutzt werden und haben einen festgelegten Wert pro Runde.
Freispiele sind eine großartige Möglichkeit, um neue Spielautomaten im Zet Casino auszuprobieren und echtes Geld zu gewinnen, ohne eigenes Geld riskieren zu müssen. Spieler können ihre Gewinne aus Freispielen in Form von Echtgeld behalten und für weitere Spiele verwenden.
Für alle Fans von Online-Casinospielen sind Freispiele im Zet Casino eine tolle Möglichkeit, um das Spielerlebnis zu verbessern und zusätzliche Gewinnchancen zu erhalten. Probiere es aus und sichere dir deine Freispiele im Zet Casino!
https://zetcasino.one/
Awesome! Its really remarkable paragraph, I have got much clear idea
regarding from this piece of writing.
world pharmacy india: top 10 pharmacies in india – п»їlegitimate online pharmacies india
Undeniably imagine that that you said. Your favorite
justification seemed to be on the web the easiest thing to have in mind of.
I say to you, I definitely get irked while other folks think about concerns that they plainly do not recognize about.
You managed to hit the nail upon the highest and defined out the whole thing with no need side effect
, other people could take a signal. Will likely be back to get
more. Thank you
https://mexicanpharmgrx.shop/# mexican border pharmacies shipping to usa
Zet Casino ist eine beliebte Online-Glücksspielplattform, die eine Vielzahl von Spielen und attraktiven Bonusangeboten für Spieler anbietet. Im Jahr 2018 überraschte das Casino seine Kunden mit großzügigen no deposit bonus codes, die es den Spielern ermöglichten, ohne Einzahlung zu spielen und dennoch echtes Geld zu gewinnen.
Die no deposit bonus codes von Zet Casino im Jahr 2018 boten den Spielern die Möglichkeit, verschiedene Spiele auszuprobieren, ohne Geld einzahlen zu müssen. Dies war eine großartige Gelegenheit für neue Spieler, die Plattform kennenzulernen und sich mit den angebotenen Spielen vertraut zu machen.
Die Bonuscodes waren nicht nur für neue Spieler verfügbar, sondern auch für bestehende Kunden, die regelmäßig im Casino spielten. Dies zeigte das Engagement des Casinos, seinen Spielern Gutes zu tun und sie zu belohnen.
Die Bonuscodes waren einfach zu verwenden. Spieler mussten lediglich den Code im entsprechenden Feld im Casino eingeben, um den Bonus zu erhalten. Mit diesem Bonus konnten sie dann verschiedene Spiele spielen und echtes Geld gewinnen.
Zet Casino no deposit bonus codes 2018 waren eine willkommene Überraschung für die Spieler und trugen dazu bei, die Popularität des Casinos weiter zu steigern. Es bleibt abzuwarten, ob das Casino in Zukunft ähnliche Bonuscodes anbieten wird, um seine Spieler glücklich zu machen.
https://zetcasino.one/
canadian pharmacy 24h com safe My Canadian pharmacy canadian pharmacy reviews
When I initially commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get three e-mails with the same comment.
Is there any way you can remove people from that service?
Thanks!
Just wish to say your article is as astonishing.
The clearness in your post is simply excellent and i can assume you’re
an expert on this subject. Well with your permission allow me to grab your
RSS feed to keep up to date with forthcoming post.
Thanks a million and please keep up the rewarding work.
Awesome blog! Do you have any tips for aspiring writers?
I’m planning to start my own website soon but I’m
a little lost on everything. Would you propose starting with a free platform like WordPress or go for a paid option? There are so many choices out there that
I’m completely confused .. Any tips? Bless you!
buy prescription drugs from india: Healthcare and medicines from India – pharmacy website india
https://mexicanpharmgrx.com/# best online pharmacies in mexico
Zet Casino Sportwetten
Sportwetten erfreuen sich in Deutschland immer größerer Beliebtheit. Neben den traditionellen Wettbüros vor Ort bieten auch Online-Casinos wie das Zet Casino Sportwetten an. Das Zet Casino ist ein beliebtes Online-Casino, das seinen Kunden eine Vielzahl von Spielen und Wetten anbietet.
Das Zet Casino Sportwettenangebot umfasst eine breite Palette von Sportarten, darunter Fußball, Tennis, Basketball, Eishockey und vieles mehr. Die Kunden haben die Möglichkeit, auf einzelne Spiele, Turniere oder ganze Ligen zu wetten. Neben den klassischen Sportwetten bietet das Zet Casino auch Live-Wetten an, bei denen die Kunden während des Spiels ihre Wetten platzieren können.
Das Online-Casino zeichnet sich durch eine benutzerfreundliche Oberfläche aus, die es den Kunden ermöglicht, schnell und einfach ihre Wetten abzugeben. Zudem bietet das Zet Casino eine Vielzahl von Zahlungsmethoden an, darunter Kreditkarten, E-Wallets und Banküberweisungen.
Ein weiterer Vorteil des Zet Casino Sportwettenangebots sind die attraktiven Quoten und Boni, die den Kunden angeboten werden. So können die Kunden von lukrativen Einzahlungsboni, Freiwetten und anderen Aktionen profitieren.
Insgesamt bietet das Zet Casino Sportwetten eine unterhaltsame und spannende Möglichkeit, sich mit Sportereignissen zu beschäftigen und möglicherweise auch den ein oder anderen Gewinn zu erzielen. Wer also auf der Suche nach einem Online-Casino mit einem breiten Sportwettenangebot ist, sollte das Zet Casino in Betracht ziehen.
https://zetcasino.one/
Hi, the whole thing is going nicely here and ofcourse
every one is sharing facts, that’s actually fine, keep
up writing.
Thái Việt Hoàng là một cá nhân tài ba và có
nhiều thành tựu trong lĩnh vực quản lý và lãnh đạo.
Với vai trò là CEO của nhà cái BK8pro, ông đã đóng góp to
lớn vào sự phát triển và thành công của công ty.
Với kiến thức sâu rộng về ngành công nghiệp cá cược và giải trí trực tuyến, Thái Việt Hoàng
đã xây dựng BK8pro thành một thương hiệu đáng tin cậy và được người dùng tin tưởng.
Ông luôn đặt lợi ích của khách hàng lên hàng đầu và tạo ra môi trường chơi cá cược an toàn,
công bằng và chuyên nghiệp
Das Zet Casino ist ein Online-Glücksspielanbieter, der in den letzten Jahren an Beliebtheit gewonnen hat. Viele Spieler fragen sich jedoch, ob das Zet Casino seriös ist. In diesem Artikel werden wir genauer auf diese Frage eingehen.
Zunächst einmal ist es wichtig zu erwähnen, dass das Zet Casino über eine Lizenz der Malta Gaming Authority verfügt, einer der angesehensten Glücksspielbehörden der Welt. Diese Lizenz garantiert, dass das Casino die strengen Standards in Bezug auf Fairness, Sicherheit und Transparenz erfüllt.
Des Weiteren arbeitet das Zet Casino mit namhaften Spieleentwicklern zusammen, darunter NetEnt, Microgaming und Play’n GO. Diese Unternehmen sind fГјr ihre hochwertigen Spiele und fairen Gewinnchancen bekannt, was die SeriositГ¤t des Casinos weiter unterstreicht.
Zusätzlich bietet das Zet Casino eine Vielzahl von sicheren Zahlungsmethoden an, darunter Kreditkarten, E-Wallets und Banküberweisungen. Alle Transaktionen werden verschlüsselt übertragen, um die persönlichen Daten der Spieler zu schützen.
Darüber hinaus verfügt das Zet Casino über einen kompetenten Kundenservice, der rund um die Uhr erreichbar ist. Spieler können sich bei Fragen oder Problemen jederzeit an das Support-Team wenden und erhalten schnell und zuverlässig Hilfe.
Insgesamt lässt sich sagen, dass das Zet Casino einen seriösen Eindruck macht und eine sichere Spielumgebung bietet. Spieler können hier bedenkenlos spielen und sich auf ein unterhaltsames und faires Spielerlebnis freuen.
https://zetcasino.one/
https://mexicanpharmgrx.com/# best mexican online pharmacies
legitimate canadian pharmacy online List of Canadian pharmacies vipps approved canadian online pharmacy
repaglinide oatp1b1
Das Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen anbietet, darunter Slots, Tischspiele und Live-Casino-Spiele. Um das Spielerlebnis noch besser zu machen, hat das Zet Casino auch eine App entwickelt, die es den Spielern ermöglicht, ihre Lieblingsspiele unterwegs zu spielen.
Die Zet Casino App kann ganz einfach heruntergeladen werden, indem man die offizielle Website des Casinos besucht und den Anweisungen folgt. Die App ist sowohl für iOS als auch für Android-Geräte verfügbar und bietet eine nahtlose Benutzeroberfläche, die es den Spielern ermöglicht, problemlos zwischen den verschiedenen Spielen zu wechseln.
Durch die Zet Casino App haben die Spieler rund um die Uhr Zugang zu ihren Lieblingsspielen, egal wo sie sich befinden. Ob man Slots liebt, gerne Blackjack oder Roulette spielt oder die Spannung eines Live-Casino-Spiels erleben möchte, die Zet Casino App bietet alles, was das Herz begehrt.
Darüber hinaus bietet das Zet Casino auch regelmäßig lukrative Promotionen und Boni für die Spieler an, die die App nutzen. Diese können Freispiele, Einzahlungsboni, Cashback-Angebote und vieles mehr beinhalten, was den Spielspaß noch weiter steigert.
Also, wenn Sie ein Fan von Online-Casinospielen sind und gerne auch unterwegs spielen möchten, dann sollten Sie die Zet Casino App definitiv ausprobieren. Mit einer breiten Auswahl an Spielen, einer benutzerfreundlichen Benutzeroberfläche und attraktiven Promotionen ist die Zet Casino App die perfekte Wahl für alle Casino-Liebhaber.Probieren Sie es aus und erleben Sie die aufregende Welt des Zet Casinos auf Ihrem Smartphone oder Tablet!
https://zetcasino.one/
remeron med
https://indianpharmgrx.com/# pharmacy website india
Das m Tipico Casino ist eine beliebte Online-Spielplattform, bekannt für seine vielfältige Auswahl an Casinospielen und großzügigen Bonusangeboten. Mit einer benutzerfreundlichen Oberfläche und einer breiten Palette an Spielen bietet das m Tipico Casino eine unterhaltsame und spannende Spielerfahrung für alle Arten von Spielern.
Das Casino bietet eine Vielzahl von Slots, Tischspielen und Live-Casinospielen von namhaften Anbietern wie NetEnt, Microgaming und Evolution Gaming. Mit hohen Jackpots und schnellen Auszahlungen ist das m Tipico Casino eine Top-Wahl für Spieler, die nach hervorragenden Gewinnmöglichkeiten suchen.
Darüber hinaus bietet das m Tipico Casino großzügige Bonusangebote für neue Spieler sowie regelmäßige Promotionen für bestehende Kunden. Von Willkommensboni über Freispiele bis hin zu Turnieren gibt es immer wieder spannende Aktionen, die das Spielerlebnis im m Tipico Casino noch aufregender machen.
Die Sicherheit und Fairness der Spiele im m Tipico Casino sind ebenfalls von höchster Priorität. Das Casino verfügt über eine gültige Glücksspiellizenz und verwendet die neueste Verschlüsselungstechnologie, um die persönlichen Daten und Transaktionen seiner Spieler zu schützen.
Alles in allem bietet das m Tipico Casino eine erstklassige und sichere Spielumgebung fГјr GlГјcksspielfans. Mit einer groГџen Auswahl an Spielen, lukrativen Boni und erstklassigem Kundenservice ist das m Tipico Casino definitiv einen Besuch wert. Probieren Sie es aus und erleben Sie die Spannung und den Nervenkitzel des GlГјcksspiels online!
https://tipicocasino.one/
Thank you so much for sharing such a helpful article. It’s been incredibly valuable.
Pharmacology’s Role and Drug Development in Modern Society
Pharmacology, the science of drugs and their effects on living systems, plays a pivotal role in modern society.
With an ever-increasing burden of diseases and health conditions, the development of new medications
is vital for improving healthcare outcomes and enhancing quality of
life. This article explores the significance of pharmacology
and the process of drug development in addressing contemporary health
challenges.
**Understanding Pharmacology:**
Pharmacology encompasses a multidisciplinary approach, combining
aspects of biology, chemistry, physiology, and pathology to study how drugs interact
with biological systems. It delves into the mechanisms of action, therapeutic effects, and potential
side effects of medications. By comprehensively understanding these
factors, pharmacologists strive to develop safer
and more effective drugs for treating various ailments.
**Importance of Drug Development:**
The development of new drugs is essential for combating both prevalent and emerging health threats.
Chronic diseases such as cardiovascular disorders, cancer, diabetes,
and respiratory ailments continue to impose a significant burden on global health.
Moreover, the emergence of novel pathogens, antimicrobial resistance, and environmental factors further underscore the need for innovative
pharmaceutical solutions.
**Phases of Drug Development:**
The journey from drug discovery to market availability
is a complex and rigorous process comprising several distinct
phases:
1. **Drug Discovery:** Scientists identify potential drug candidates through various means,
including screening natural compounds, designing molecules using computational methods, or repurposing existing drugs for
new indications.
2. **Preclinical Research:** Promising drug candidates undergo extensive laboratory testing to assess their safety, efficacy,
and pharmacokinetic properties in cellular and animal models.
3. **Clinical Trials:** Drug candidates that demonstrate favorable preclinical results advance
to clinical trials, which consist of three sequential
phases:
– **Phase I:** Involves testing the drug’s safety
and dosage in a small group of healthy volunteers.
– **Phase II:** Evaluates the drug’s efficacy and side
effects in a larger group of individuals with the targeted disease or condition.
– **Phase III:** Further assesses the drug’s safety
and efficacy in a diverse population across multiple locations to
establish its therapeutic benefits and risks.
4. **Regulatory Approval:** Following successful completion of clinical trials,
pharmaceutical companies submit comprehensive data to regulatory authorities such as the FDA in the United States or the
EMA in Europe for approval to market the drug.
5. **Post-Marketing Surveillance:** Even after approval, ongoing monitoring is crucial to detect any unforeseen adverse effects and ensure the drug’s continued safety
and efficacy in real-world settings.
**Challenges and Future Directions:**
Despite significant advancements in pharmacology and drug development,
several challenges persist. These include escalating research
and development costs, regulatory hurdles, ethical considerations, and the increasing
complexity of diseases. Additionally, disparities in access to medications and healthcare
services remain a global concern.
Looking ahead, emerging technologies such as precision medicine, gene editing,
and artificial intelligence offer promising avenues for personalized therapies and targeted drug development.
Collaborative efforts among researchers, clinicians, pharmaceutical companies, and policymakers are imperative to address these challenges and harness
the full potential of pharmacology in improving global health outcomes.
In conclusion, pharmacology plays a central role in modern society by driving the development of new medications to combat a myriad
of health challenges. Through continuous innovation and collaboration, the field of pharmacology holds immense promise for enhancing healthcare delivery and promoting well-being worldwide.
Here is my blog post; “https://rotorm.hatenablog.com/entry/2024/03/18/003810
robaxin drug
Thank you so much for sharing such a helpful article. It’s been incredibly valuable.
На сайте https://xakervip.com/topic/282/page/10/ вы сможете воспользоваться услугами хакеров, заказать взлом почты, а также тайную слежку, а заодно пробить номер, если у вас есть какие-либо подозрения. Также можно будет узнать пароли электронной почты. Для того чтобы подобрать подходящий вариант, необходимо ознакомиться со всеми разделами форума. С той целью, чтобы воспользоваться услугами, просто напишите хакеру. Он ответит вам и предложит оптимальную цену. Его услуги обойдутся недорого, а вопрос будет решен оперативно.
pharmacy wholesalers canada Pharmacies in Canada that ship to the US pharmacy com canada
Immer mehr Online-Casinos setzen auf eine schnelle und einfache Verifizierung der Spieler, um ein sicheres und verantwortungsvolles Spielumfeld zu gewährleisten. Ein Casino, das sich besonders durch seine effiziente Verifizierung auszeichnet, ist das Boomerang Casino.
Die Verifizierung der Spieler ist ein wichtiger Schritt, um die Identität und Volljährigkeit der Teilnehmer zu überprüfen. Dies dient nicht nur dem Schutz vor möglichen Betrugsfällen, sondern auch der Einhaltung gesetzlicher Vorschriften im Glücksspielbereich.
Das Boomerang Casino legt großen Wert auf eine einfache und transparente Verifizierung seiner Spieler. Nach der Registrierung müssen die Spieler lediglich einige persönliche Informationen angeben und gegebenenfalls bestimmte Dokumente hochladen, um ihre Identität zu bestätigen. Das gesamte Verifizierungsverfahren wird schnell und unkompliziert durchgeführt, sodass die Spieler schnell mit dem Spielen beginnen können.
Durch die effiziente Verifizierung stellt das Boomerang Casino sicher, dass nur volljährige Spieler Zugang zu seinem Angebot haben. Zudem sorgt die Überprüfung der Identität dafür, dass mögliche betrügerische Aktivitäten frühzeitig erkannt und verhindert werden. Dies schafft ein sicheres Spielumfeld für alle Teilnehmer und trägt dazu bei, das Vertrauen der Spieler in das Casino zu stärken.
Insgesamt bietet das Boomerang Casino eine herausragende Verifizierungserfahrung für seine Spieler. Durch den schnellen und einfachen Prozess können die Teilnehmer sicher sein, dass ihre persönlichen Daten geschützt und ihr Spielvergnügen nicht durch aufwendige Verifizierungsmaßnahmen beeinträchtigt wird. Ein weiterer Grund, warum sich das Boomerang Casino als beliebte Wahl für Spieler auf der Suche nach einem seriösen und verlässlichen Online-Casino etabliert hat.
https://boomerangcasino.one/
prandin repaglinide
https://mexicanpharmgrx.shop/# mexican pharmacy
Wonderful, what a weblog it is! This weblog provides useful information to us, keep it up.
Boomerang Casino Bonus Code
Boomerang Casino is a popular online casino that offers a wide array of casino games and exciting bonuses for its players. One of the most sought-after bonuses at Boomerang Casino is the bonus code, which gives players the chance to win extra cash and prizes. In this article, we will take a closer look at the Boomerang Casino bonus code and how you can use it to enhance your gaming experience.
The Boomerang Casino bonus code is a special code that players can use to access exclusive bonuses and promotions at the casino. These bonuses can include free spins, cashback offers, deposit bonuses, and more. By using the bonus code, players can increase their chances of winning big and enjoy a more rewarding gaming experience.
To use the Boomerang Casino bonus code, players simply need to enter the code during the registration process or when making a deposit at the casino. Once the code is entered, the bonus will be automatically credited to the player’s account, giving them instant access to the extra bonus funds or free spins.
It’s important to note that each bonus code has its own terms and conditions, so players should always read the fine print before using a bonus code. This will ensure that they understand the wagering requirements, any restrictions on the bonus funds, and how to cash out their winnings.
In conclusion, the Boomerang Casino bonus code is a fantastic way for players to enhance their gaming experience and potentially win big at the casino. By using the bonus code, players can access exclusive bonuses and promotions that are not available to regular players, giving them a competitive edge when playing their favorite casino games. So why wait? Use the Boomerang Casino bonus code today and start winning big!
https://boomerangcasino.one/
https://canadianpharmgrx.xyz/# canadian medications
Das Tipico Live Casino Blackjack ist eines der beliebtesten Spiele in der Welt des Online-Glücksspiels. Mit seiner spannenden Atmosphäre und den attraktiven Gewinnchancen zieht es viele Spieler an, die auf der Suche nach Nervenkitzel und Unterhaltung sind.
Das Spielprinzip des Live Casino Blackjacks ist einfach: Ziel ist es, mit den eigenen Karten so nah wie möglich an die Zahl 21 zu gelangen, ohne dabei zu überschreiten. Der Spieler tritt dabei gegen den Dealer an, der ebenfalls Karten erhält. Durch geschicktes Setzen und Einschätzen der eigenen Chancen kann man das Spiel für sich entscheiden und attraktive Gewinne erzielen.
Ein besonderer Reiz des Tipico Live Casino Blackjacks liegt darin, dass man gegen echte Dealer spielt, die per Live-Stream zugeschaltet sind. Dadurch entsteht eine authentische Casino-Atmosphäre, die die Spieler direkt in das Geschehen hineinzieht. Zudem bietet das Live Casino die Möglichkeit, mit anderen Spielern zu interagieren und sich über Strategien und Tipps auszutauschen.
Besonders positiv fällt bei Tipico die hohe Qualität der Live-Übertragung auf. Die Dealer sind professionell geschult und sorgen für ein reibungsloses Spielvergnügen. Zudem stehen verschiedene Varianten des Blackjack zur Auswahl, sodass für jeden Geschmack das passende Spiel dabei ist.
FГјr Neulinge im Bereich des Live Casino Blackjacks bietet Tipico zudem Tutorials und Hilfestellungen an, um sich mit den Regeln vertraut zu machen und die besten Strategien zu erlernen. Somit steht einem erfolgreichen und unterhaltsamen Spieleerlebnis nichts im Wege.
Alles in allem ist das Tipico Live Casino Blackjack eine hervorragende Möglichkeit, um sich in die Welt des Online-Glücksspiels zu stürzen. Mit seinem spannenden Spielprinzip, der authentischen Casino-Atmosphäre und den attraktiven Gewinnchancen bietet es ein unvergessliches Spielerlebnis für alle Fans von Blackjack.
https://tipicocasino.one/
medicine in mexico pharmacies: Mexico drugstore – mexican rx online
prescription drugs canada buy online canadian pharmacy online reviews canadapharmacyonline com
http://indianpharmgrx.com/# online shopping pharmacy india
Das Zet Bet Casino ist eine aufregende Online-Glücksspielplattform, die Spielern eine Vielzahl von Spielen und Boni bietet. Mit einer benutzerfreundlichen Oberfläche und einer großen Auswahl an Spielen ist es leicht zu verstehen, warum Zet Bet bei Spielern auf der ganzen Welt so beliebt ist.
Das Casino bietet eine Vielzahl von Spielen, von klassischen Slots bis hin zu aufregenden Tischspielen wie Blackjack und Roulette. Es gibt auch eine Vielzahl von Live-Dealer-Spielen, bei denen Spieler mit echten Dealern interagieren können, was dem Spielerlebnis eine authentische Note verleiht.
Ein weiterer großer Vorteil des Zet Bet Casinos sind die regelmäßigen Boni und Promotionen, die den Spielern zusätzliche Anreize bieten, weiterzuspielen. Von Willkommensboni für neue Spieler bis hin zu wöchentlichen Freispielen und Cashback-Angeboten gibt es immer etwas Neues, auf das sich die Spieler freuen können.
Darüber hinaus bietet das Zet Bet Casino eine Vielzahl von Zahlungsmethoden, darunter Kreditkarten, E-Wallets und Banküberweisungen, um sicherzustellen, dass die Spieler problemlos Ein- und Auszahlungen vornehmen können.
Insgesamt ist das Zet Bet Casino eine ausgezeichnete Wahl für Spieler, die auf der Suche nach einem erstklassigen Online-Glücksspielerlebnis sind. Mit einer großen Auswahl an Spielen, großzügigen Boni und einer benutzerfreundlichen Oberfläche ist es leicht zu verstehen, warum immer mehr Spieler sich für das Zet Bet Casino entscheiden.
https://zetcasino.one/
На сайте https://iz-zala.ru/ находится каталог товаров. Здесь каждый желающий получает возможность составить описание продукции, опубликовать самые популярные товары, а также актуальные акции. В специальном поле разместите побольше данных для того, чтобы вашим предложением заинтересовались. Текст в блоках можно форматировать, выделять различные его части, а также особенно важные элементы, добавлять картинки и делать все, что считаете нужным. Также можно ссылаться и на другие документы. Необходимо рассказать о компании очень подробно.
tamoxifen bone density: nolvadex side effects – nolvadex 20mg
Die “tipico casino app server fehler” sind ein hГ¤ufiges Problem, das viele Nutzer der Tipico Casino App betrifft. Der Serverfehler tritt meistens wГ¤hrend des Spielens auf und kann frustrierend sein, da man plГ¶tzlich vom Spiel abgemeldet wird und keine Verbindung zum Server herstellen kann.
Es gibt verschiedene Gründe, warum dieser Serverfehler auftreten kann. Einer der häufigsten Gründe ist die Überlastung der Server aufgrund einer hohen Anzahl von Spielern, die gleichzeitig die App nutzen. In solchen Fällen kann es zu Verbindungsproblemen kommen, die zu einem Serverfehler führen.
Ein weiterer Grund für den Serverfehler könnte ein technisches Problem auf der Seite von Tipico sein, beispielsweise ein Problem mit der App oder den Servern des Unternehmens. In solchen Fällen sollte man sich direkt an den Kundenservice von Tipico wenden, um das Problem zu melden und eine Lösung zu finden.
Um den Serverfehler zu vermeiden, ist es wichtig, die Tipico Casino App regelmäßig zu aktualisieren und sicherzustellen, dass man eine stabile Internetverbindung hat. Man sollte auch darauf achten, dass man nicht zu viele Apps gleichzeitig auf seinem Gerät geöffnet hat, da dies die Leistung der Tipico Casino App beeinträchtigen kann.
Insgesamt ist der Serverfehler in der Tipico Casino App ein Г¤rgerliches, aber oft beherrschbares Problem. Mit einigen einfachen Schritten kann man das Risiko eines Serverfehlers minimieren und ein reibungsloses Spielerlebnis genieГџen. Wenn das Problem jedoch weiterhin besteht, sollte man sich an den Kundenservice von Tipico wenden, um Hilfe zu erhalten.
https://tipicocasino.one/
I think this is one of the most vital information for me.
And i’m glad studying your article. However wanna commentary on few general issues, The web site
taste is perfect, the articles is really great :
D. Just right task, cheers
https://diflucan.icu/# buy diflucan
low dose tamoxifen how does tamoxifen work nolvadex d
Zet Casino – das Casino ohne Einzahlung
Zet Casino ist ein beliebtes Online Casino, das seinen Spielern die Möglichkeit bietet, ohne eine Einzahlung zu spielen. Dank seines großzügigen Bonusangebots können Spieler bei Zet Casino kostenlos spielen und echtes Geld gewinnen.
Das Casino bietet eine Vielzahl von Spielen, darunter Spielautomaten, Tischspiele und Live-Casino-Spiele. Spieler kГ¶nnen aus einer Vielzahl von bekannten Titeln wГ¤hlen, die von fГјhrenden Entwicklern wie NetEnt, Microgaming und Play’n GO bereitgestellt werden.
Um ohne Einzahlung zu spielen, mГјssen Spieler einfach ein Konto bei Zet Casino erstellen und sich fГјr den “No Deposit Bonus” anmelden. Dieser Bonus ermГ¶glicht es Spielern, kostenloses Spielgeld zu erhalten, mit dem sie die verschiedenen Spiele im Casino ausprobieren kГ¶nnen.
Zet Casino ohne Einzahlung bietet nicht nur die Möglichkeit, echtes Geld zu gewinnen, sondern auch eine unterhaltsame und spannende Spielerfahrung. Das Casino ist für seine hervorragende Benutzeroberfläche und sein ansprechendes Design bekannt, was das Spielerlebnis noch angenehmer macht.
Wenn Sie auf der Suche nach einem Casino ohne Einzahlung sind, sollten Sie Zet Casino unbedingt ausprobieren. Mit seiner groГџen Auswahl an Spielen, groГџzГјgigen Boni und hervorragenden Benutzererfahrung ist es eine ausgezeichnete Wahl fГјr alle, die gerne spielen, ohne Geld ausgeben zu mГјssen. Besuchen Sie noch heute Zet Casino und beginnen Sie Ihr Casino-Abenteuer ohne Einzahlung!
https://zetcasino.one/
cost of diflucan over the counter: diflucan where to buy uk – how to get diflucan online
I just wanted to extend my heartfelt thanks for sharing this enlightening article. It’s made a significant impact.
Zet Casino ist eine beliebte Online-GlГјcksspielplattform, die eine Vielzahl von Spielen und Funktionen fГјr Spieler auf der ganzen Welt bietet. Eines der bemerkenswertesten Merkmale dieses Casinos ist der Live-Chat-Support, der rund um die Uhr verfГјgbar ist, um Spielern bei ihren Fragen und Anliegen zu helfen.
Der Live-Chat von Zet Casino ermöglicht es Spielern, direkt mit einem Support-Mitarbeiter zu kommunizieren, ohne lange Wartezeiten am Telefon oder per E-Mail. Spieler können Fragen zum Casino, zu Ein- und Auszahlungen, zu Boni und Werbeaktionen oder zu technischen Problemen stellen und erhalten sofortige Antworten und Unterstützung.
Der Live-Chat von Zet Casino ist einfach und benutzerfreundlich gestaltet, sodass Spieler keine technischen Kenntnisse benГ¶tigen, um ihn zu nutzen. Alles, was sie tun mГјssen, ist auf die SchaltflГ¤che “Live-Chat” auf der Website zu klicken und ihren Namen sowie ihre E-Mail-Adresse einzugeben, um eine Verbindung mit einem Support-Mitarbeiter herzustellen.
Dank des Live-Chats von Zet Casino können Spieler schnell und effizient alle ihre Fragen klären und Probleme bei ihrer Spielerfahrung lösen. Dieser Service hat dazu beigetragen, dass Zet Casino zu einer der beliebtesten Glücksspielplattformen im Internet geworden ist.
Insgesamt war der Live-Chat von Zet Casino eine großartige Ergänzung zu den bereits umfangreichen Dienstleistungen und Funktionen, die das Casino anbietet. Spieler können sicher sein, dass sie jederzeit professionelle Unterstützung erhalten, wenn sie im Zet Casino spielen.
https://zetcasino.one/
diflucan 150 mg buy online diflucan 110 mg can i purchase diflucan over the counter
tamoxifen mechanism of action: low dose tamoxifen – tamoxifen medication
When some one searches for his vital thing, therefore he/she needs to be available that in detail,
therefore that thing is maintained over here.
Tipico Casino bietet seinen Spielern eine Vielzahl von Spielen an, aus denen sie wählen können. Von klassischen Tischspielen wie Roulette und Blackjack bis hin zu aufregenden Spielautomaten und Live-Casino-Spielen ist für jeden Geschmack etwas dabei. Doch welche Spiele sind die besten bei Tipico Casino?
Ein beliebtes Spiel bei Tipico Casino ist sicherlich das Roulette. Dieses klassische Casinospiel bietet Spannung und Nervenkitzel, während man darauf hofft, dass die Kugel auf der richtigen Zahl landet. Mit verschiedenen Varianten wie Europe Roulette oder French Roulette bietet Tipico Casino seinen Spielern eine Vielzahl von Möglichkeiten, dieses beliebte Spiel zu genießen.
Auch Blackjack ist ein Favorit bei Tipico Casino. Bei diesem Kartenspiel geht es darum, den Dealer zu schlagen, indem man eine Hand mit einem Kartenwert näher an 21 hat, ohne darüber zu kommen. Mit verschiedenen Varianten wie Classic Blackjack oder Blackjack VIP können Spieler ihre Fähigkeiten und Strategien testen und hoffentlich große Gewinne erzielen.
FГјr Fans von Spielautomaten gibt es bei Tipico Casino eine groГџe Auswahl an aufregenden Spielen. Von klassischen FrГјchteslots bis hin zu aufwendig gestalteten Video-Slots mit spannenden Bonusrunden und Jackpots ist fГјr jeden Geschmack etwas dabei. Beliebte Spielautomaten bei Tipico Casino sind zum Beispiel Starburst, Book of Dead oder Mega Moolah.
Auch im Live-Casino von Tipico können Spieler ein authentisches Casino-Erlebnis genießen. Mit Live-Dealern, die die Spiele leiten und via Video-Stream übertragen werden, können Spieler Roulette, Blackjack, Baccarat und mehr in Echtzeit spielen und interagieren. Die Spannung und Atmosphäre eines echten Casinos werden so direkt ins Wohnzimmer gebracht.
Insgesamt bietet Tipico Casino eine breite Auswahl an Spielen fГјr jeden Geschmack und jedes Budget. Ob Tischspiele, Spielautomaten oder Live-Casino-Spiele – hier kommt jeder auf seine Kosten. Welches Spiel letztendlich das beste ist, kommt ganz auf die persГ¶nlichen Vorlieben und Strategien des Spielers an. Eines ist jedoch sicher: Spannung und Unterhaltung sind bei Tipico Casino garantiert. Viel SpaГџ beim Spielen!
https://tipicocasino.one/
На сайте https://bdalogistic.ru/ вы сможете заказать товары для маркетплейсов, которые привозятся из Китая. Основная специализация компании заключается в поиске, приобретении, доставке продукции. Кроме того, выполняется и отгрузка, упаковка продукции на маркетплейсы. В компании работают компетентные, опытные и предусмотрительные специалисты, которые окажут поддержку в организации бизнеса на Вайлдберриз. Рассчитать цену услуги получится прямо сейчас. В любом случае она будет доступной.
nolvadex online: nolvadex for pct – tamoxifen rash
doxycycline hyc 100mg doxy cheap doxycycline online
Das Online-Casino tipico.de bietet seinen Spielern eine Vielzahl von Glücksspielmöglichkeiten, darunter Slots, Tischspiele und Live-Casino-Spiele. Mit einer benutzerfreundlichen Plattform und einer großen Auswahl an Spielen ist tipico.de eine der beliebtesten Online-Casinos in Deutschland.
Eine der einzigartigen Eigenschaften von tipico.de ist die Möglichkeit, Sportwetten und Casino-Spiele auf derselben Plattform zu genießen. Dies bedeutet, dass Spieler ihre Lieblingssportveranstaltungen verfolgen und gleichzeitig ihre Glücksspiele spielen können, alles mit nur einem Klick.
Das Casino bietet auch eine Vielzahl von Boni und Promotionen für neue und bestehende Spieler. Dies kann von Freispielen bis hin zu Einzahlungsboni reichen, um sicherzustellen, dass Spieler immer eine zusätzliche Belohnung für ihr Gameplay erhalten.
Die Sicherheit der Spieler steht bei tipico.de an erster Stelle, und das Casino verfügt über eine Lizenz der Malta Gaming Authority, um sicherzustellen, dass alle Spiele fair und transparent sind. Spieler können auch sicher sein, dass ihre persönlichen und finanziellen Daten geschützt sind, da die Website die neuesten Verschlüsselungstechnologien verwendet.
Mit einer Vielzahl von Zahlungsmethoden und einem engagierten Kundensupport ist tipico.de der ideale Ort fГјr Spieler, die eine sichere und unterhaltsame GlГјcksspielerfahrung suchen. Besuchen Sie noch heute tipico.de, um all die aufregenden Spiele und Boni zu genieГџen, die dieses erstklassige Online-Casino zu bieten hat.
https://tipicocasino.one/
ivermectin 3 mg oral – levaquin 250mg without prescription cefaclor order
diflucan 150 cost: diflucan drug coupon – diflucan 150
Das Tipico Casino in Mönchengladbach am Kammof bietet den Besuchern eine spannende und unterhaltsame Glücksspiel-Atmosphäre. Das Casino befindet sich in zentraler Lage und ist somit leicht erreichbar für alle, die auf der Suche nach Unterhaltung und Nervenkitzel sind.
Das Casino bietet eine Vielzahl von Spielmöglichkeiten, darunter klassische Tischspiele wie Roulette und Blackjack, sowie eine breite Auswahl an Spielautomaten. Egal ob erfahrener Spieler oder Anfänger, im Tipico Casino am Kammof kommt jeder auf seine Kosten.
Zusätzlich zu den Spielmöglichkeiten bietet das Casino auch verschiedene Veranstaltungen und Aktionen an, um den Aufenthalt der Besucher noch spannender zu gestalten. Von Pokerturnieren bis hin zu Live-Musik-Events ist im Tipico Casino am Kammof immer etwas los.
Wenn Sie also auf der Suche nach einem unterhaltsamen Abend sind, ist das Tipico Casino am Kammof in Mönchengladbach die perfekte Adresse. Tauchen Sie ein in die Welt des Glücksspiels und genießen Sie eine aufregende Zeit in diesem beliebten Casino.
https://tipicocasino.one/
doxycycline tablets: buy doxycycline online uk – cheap doxycycline online
На сайте http://servis-pro24.ru/ закажите квалифицированного, опытного мастера: сантехника, электрика на час для выполнения различных задач, несмотря на их сложность. Компания предлагает воспользоваться такими важными услугами, как вскрытие замков, установка, сборка мебели, замена смесителя, труб, стояков. С полной номенклатурой услуг ознакомьтесь на официальном портале предприятия. Специалистов компании выбирают из-за того, что у них огромный опыт работы, стремление развиваться. Услуги предоставляются по лучшей стоимости.
diflucan discount coupon diflucan tabs canadian order diflucan online
doxycycline prices: doxycycline without prescription – price of doxycycline
Das Online Casino Tipico erfreut sich großer Beliebtheit bei Spielern aus Deutschland und anderen Ländern. Doch wie seriös ist das Online Casino wirklich?
Tipico Casino ist ein etablierter Anbieter, der über eine Lizenz der Malta Gaming Authority verfügt. Diese Lizenz garantiert, dass das Casino strenge Auflagen erfüllen muss, um Fairness und Sicherheit für die Spieler zu gewährleisten. Zudem unterliegt das Casino regelmäßigen Kontrollen, um sicherzustellen, dass alle Vorschriften eingehalten werden.
Ein weiteres Indiz für die Seriosität von Tipico ist die Zusammenarbeit mit renommierten Softwareanbietern wie NetEnt, Microgaming und Evolution Gaming. Diese Unternehmen sorgen dafür, dass die Spiele im Casino fair und transparent ablaufen. Zudem bietet das Casino eine Vielzahl von sicheren Zahlungsmethoden an, um die Ein- und Auszahlungen der Spieler zu schützen.
Darüber hinaus legt Tipico großen Wert auf den Schutz der persönlichen Daten seiner Spieler. Das Casino verwendet moderne Verschlüsselungstechnologien, um die sensiblen Informationen der Spieler zu schützen. Zudem steht der Kundenservice rund um die Uhr zur Verfügung, um bei Fragen oder Problemen zu helfen.
Insgesamt lässt sich sagen, dass das Tipico Casino als seriös eingestuft werden kann. Die Lizenz der Malta Gaming Authority, die Zusammenarbeit mit renommierten Softwareanbietern und der Schutz der persönlichen Daten der Spieler sind klare Indizien dafür, dass es sich um einen vertrauenswürdigen Anbieter handelt. Spieler können also beruhigt in dem Casino spielen und ihr Glück versuchen.
https://tipicocasino.one/
https://nolvadex.icu/# tamoxifen moa
Der Boomerang.bet Casino No Deposit Bonus ist eine großartige Möglichkeit, um ohne eigenes Geld in einem Online-Casino zu spielen. Diese Art von Bonus wird in der Regel neuen Spielern angeboten, die sich neu anmelden und ein Konto erstellen. Der Bonus wird automatisch gutgeschrieben, ohne dass eine Einzahlung erforderlich ist.
Der Boomerang.bet Casino No Deposit Bonus kann in Form von Freispielen oder Bonusgeld angeboten werden. Freispiele können an bestimmten Spielautomaten verwendet werden, während Bonusgeld in verschiedenen Spielen eingesetzt werden kann. Spieler können mit diesem Bonus echte Gewinne erzielen, die sie dann auszahlen lassen können.
Es ist jedoch wichtig zu beachten, dass No Deposit Boni oft bestimmten Umsatzbedingungen unterliegen. Das bedeutet, dass Spieler das Bonusgeld oder die Gewinne aus den Freispielen eine bestimmte Anzahl von Malen umsetzen müssen, bevor sie eine Auszahlung beantragen können. Es ist daher ratsam, die Bonusbedingungen immer sorgfältig zu lesen, um Missverständnisse zu vermeiden.
Insgesamt bietet der Boomerang.bet Casino No Deposit Bonus eine tolle Möglichkeit, um das Online-Casino kennenzulernen und erste Erfahrungen zu sammeln, ohne dabei eigenes Geld riskieren zu müssen. Es lohnt sich also, nach diesen lukrativen Boni Ausschau zu halten und sie zu nutzen, um seine Gewinnchancen zu erhöhen.
https://boomerangcasino.one/
doxycycline without a prescription: doxycycline generic – doxycycline prices
tamoxifen vs clomid common side effects of tamoxifen benefits of tamoxifen
ivermectin price – buy oral ivermectin buy cheap cefaclor
Zet Casino Login Deutsch – Alles, was Sie wissen mГјssen
Zet Casino ist eine beliebte Online-Glücksspielseite, die deutschen Spielern eine Vielzahl von Spielen und Bonusangeboten bietet. Um auf das Casino zugreifen zu können, müssen Sie sich jedoch zuerst anmelden. In diesem Artikel werden wir Ihnen alles erklären, was Sie über den Zet Casino Login auf Deutsch wissen müssen.
Der erste Schritt ist, auf die offizielle Website von Zet Casino zu gehen. Dort finden Sie oben rechts die SchaltflГ¤che “Anmelden”. Klicken Sie darauf und es Г¶ffnet sich ein Anmeldeformular, in das Sie Ihre persГ¶nlichen Daten eingeben mГјssen. Dazu gehГ¶ren Ihr Name, Ihre E-Mail-Adresse, Ihr Passwort und einige weitere Details.
Sobald Sie alle Informationen eingegeben haben, klicken Sie auf die SchaltflГ¤che “Registrieren” und Ihr Konto wird erstellt. Sie erhalten eine BestГ¤tigungs-E-Mail, in der Sie Ihren Account aktivieren mГјssen. Sobald dies erledigt ist, kГ¶nnen Sie sich mit Ihren Anmeldedaten auf der Website einloggen.
Der Zet Casino Login auf Deutsch ist einfach und unkompliziert. Geben Sie einfach Ihre E-Mail-Adresse und Ihr Passwort ein und klicken Sie auf die SchaltflГ¤che “Anmelden”. Sie werden dann auf Ihr Konto weitergeleitet, wo Sie auf eine Vielzahl von Spielen zugreifen kГ¶nnen, darunter Spielautomaten, Tischspiele, Live-Casino und vieles mehr.
Zet Casino bietet auch verschiedene Bonusangebote für neue und bestehende Spieler. Nachdem Sie sich angemeldet haben, können Sie von Willkommensboni, Einzahlungsboni, Freispielen und anderen Aktionen profitieren. Vergewissern Sie sich, dass Sie die Bonusbedingungen lesen, um sicherzustellen, dass Sie die Voraussetzungen erfüllen, um den Bonus zu aktivieren.
Insgesamt bietet Zet Casino deutschen Spielern ein aufregendes und unterhaltsames Spielerlebnis. Mit einer benutzerfreundlichen Website, einer groГџen Auswahl an Spielen und lukrativen Bonusangeboten ist es leicht zu verstehen, warum das Casino bei Spielern so beliebt ist. Jetzt liegt es an Ihnen, sich anzumelden und Ihr GlГјck zu versuchen. Viel SpaГџ und viel GlГјck!
https://zetcasino.one/
I’m truly appreciative of this article; it’s been an invaluable resource. Thank you for making it available.
buy doxycycline cheap: doxycycline 200 mg – doxycycline hyclate 100 mg cap
На сайте https://setki.moscow оставьте заявку для того, чтобы заказать москитную сетку на окна. Конструкция изготавливается всего за день, а монтаж выполняется тогда, когда вам удобно. На работы и сетку дается гарантия – 12 месяцев. За счет собственного производства компания устанавливает не только привлекательные расценки, но и акции. Своя служба логистики выполняет оперативную доставку на место. Для того чтобы заранее ознакомиться с тем, во сколько обойдется услуга, воспользуйтесь специальным калькулятором.
Tipico Casino ist eine beliebte Online-Glücksspielplattform, die eine Vielzahl von Spielen und attraktiven Bonusangeboten für ihre Spieler bietet. Einer der begehrtesten Boni ist der Tipico Casino Bonus Code ohne Einzahlung, der es den Spielern ermöglicht, kostenloses Bonusguthaben zu erhalten, ohne zuerst eine Einzahlung tätigen zu müssen.
Ein Bonus ohne Einzahlung ist eine großartige Möglichkeit, um das Casino kennenzulernen und die verschiedenen Spiele auszuprobieren, ohne dabei eigenes Geld riskieren zu müssen. Mit dem Tipico Casino Bonus Code ohne Einzahlung können Spieler ihr Glück versuchen und gleichzeitig die Chance haben, echtes Geld zu gewinnen.
Um den Bonus ohne Einzahlung zu erhalten, müssen Spieler einfach den entsprechenden Bonuscode während der Anmeldung oder auf der Aktionsseite des Casinos eingeben. Sobald der Code aktiviert ist, wird das Bonusguthaben automatisch auf das Spielerkonto gutgeschrieben und kann sofort zum Spielen verwendet werden.
Es ist jedoch zu beachten, dass die meisten Boni ohne Einzahlung bestimmte Umsatzanforderungen haben, die erfüllt werden müssen, bevor Gewinne ausgezahlt werden können. Diese Anforderungen variieren je nach Casino und Bonusangebot, daher ist es ratsam, die Teilnahmebedingungen sorgfältig zu lesen, um Missverständnisse zu vermeiden.
Insgesamt ist der Tipico Casino Bonus Code ohne Einzahlung eine großartige Möglichkeit, um das Casino zu erkunden und die verschiedenen Spiele auszuprobieren, ohne eigenes Geld riskieren zu müssen. Spieler sollten jedoch immer verantwortungsbewusst spielen und sich über die geltenden Bedingungen informieren, um das Beste aus ihrem Bonusangebot herauszuholen.
https://tipicocasino.one/
buy diflucan online india diflucan 100 mg tab diflucan 6
buy generic ciprofloxacin: ciprofloxacin mail online – cipro online no prescription in the usa
Zet Casino ist eine beliebte Online-GlГјcksspielseite, die eine Vielzahl von Casino-Spielen und Promotionen fГјr Spieler anbietet. Viele Menschen haben positive Erfahrungen mit Zet Casino gemacht, da sie eine benutzerfreundliche Plattform und eine Vielzahl von Spielen bieten.
Einer der Hauptgründe, warum Spieler Zet Casino lieben, ist die große Auswahl an Spielen, die sie zur Verfügung stellen. Von klassischen Tischspielen wie Roulette und Blackjack bis hin zu modernen Spielautomaten und Live-Dealer-Spielen, gibt es für jeden etwas zu spielen. Die Spiele werden von renommierten Softwareanbietern wie NetEnt, Microgaming und Betsoft bereitgestellt, was bedeutet, dass sie von höchster Qualität sind und ein reibungsloses Spielerlebnis bieten.
Außerdem bietet Zet Casino großzügige Promotionen und Boni für Spieler an. Neue Spieler können einen Willkommensbonus erhalten, der ihren ersten Einzahlungsbetrag erhöht und zusätzliche Freispiele für ausgewählte Spiele bietet. Darüber hinaus belohnt das Casino treue Spieler mit regelmäßigen Promotionen, Turnieren und Cashback-Angeboten.
Die Ein- und Auszahlungsmöglichkeiten bei Zet Casino sind vielfältig und sicher, was es den Spielern ermöglicht, schnell und problemlos Geld auf ihr Konto einzuzahlen und abzuheben. Der Kundensupport des Casinos ist ebenfalls rund um die Uhr verfügbar und bietet schnelle Lösungen für alle Anliegen der Spieler.
Insgesamt haben Spieler, die Zet Casino ausprobiert haben, positive Erfahrungen gemacht und schätzen die Vielfalt an Spielen, die großzügigen Boni und die zuverlässige Kundenbetreuung. Wenn Sie auf der Suche nach einem unterhaltsamen und sicheren Online-Casino-Erlebnis sind, könnte Zet Casino eine gute Option für Sie sein.
https://zetcasino.one/
На сайте https://smartflow.ru ознакомьтесь с сантехникой премиального уровня. Вся продукция создана из инновационных, высокотехнологичных материалов и с использованием уникальных, новаторских технологий. Продукты разработаны тщательным образом, чтобы предложить вам лучшее. Сантехника гарантирует безупречный уровень функциональности, эстетичности. Она наделена долгим сроком эксплуатации. Идеально впишется в концепцию. Представлены «умные» модели унитазов безупречного качества.
Das Zet Casino bietet seinen Spielern einen tollen Bonus ohne Einzahlung in Form von 30 Freispielen. Diese Freispiele können genutzt werden, um verschiedene Slotspiele auszuprobieren und möglicherweise sogar echtes Geld zu gewinnen, ohne dabei eigenes Geld einzusetzen.
Um von diesem großzügigen Angebot zu profitieren, müssen sich Spieler lediglich im Zet Casino anmelden und den Bonuscode eingeben, um die Freispiele gutgeschrieben zu bekommen. Diese können dann sofort genutzt werden, um die Vielzahl an spannenden Spielen im Casino auszuprobieren.
Es ist jedoch wichtig zu beachten, dass eventuelle Gewinne, die aus den Freispielen resultieren, bestimmten Umsatzbedingungen unterliegen. Diese müssen erfüllt werden, bevor eine Auszahlung möglich ist. Dennoch ist dies eine großartige Möglichkeit, um das Casino kennenzulernen und erste Gewinne zu erzielen, ohne dabei eigenes Geld einzusetzen.
Das Zet Casino bietet eine Vielzahl an Spielen von renommierten Anbietern und eine sichere und faire Spielumgebung. Mit dem Bonus ohne Einzahlung haben Spieler die Möglichkeit, das Casino risikofrei auszuprobieren und sich von den zahlreichen Vorteilen zu überzeugen.
Also worauf warten Sie noch? Nutzen Sie die 30 Freispiele ohne Einzahlung im Zet Casino und entdecken Sie die spannende Welt der Online Casinos. Viel GlГјck beim Spielen!
https://zetcasino.one/
ciprofloxacin mail online cipro pharmacy ciprofloxacin 500mg buy online
buy online diflucan: diflucan 150 cost – fluconazole diflucan
новый автомобиль китайский
машина zeekr 001
zeekr 001 цена
китайский автомобиль купить новый
https://misoprostol.top/# buy cytotec online fast delivery
Boomerang Casino Dokumentation
Boomerang Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und Unterhaltung für seine Spieler bietet. Wie bei allen Online-Casinos ist es wichtig, dass die Spieler die richtige Dokumentation bereithalten, um ihre Identität zu überprüfen und Auszahlungen zu erhalten.
Die Dokumentation, die für Boomerang Casino erforderlich ist, umfasst in der Regel eine Kopie eines Lichtbildausweises (wie Reisepass oder Führerschein), eine aktuelle Stromrechnung oder Kontoauszug zur Bestätigung des Wohnsitzes und möglicherweise auch eine Kopie der Kreditkarte, die für Einzahlungen verwendet wurde.
Es ist wichtig, dass die Spieler die Dokumente klar und deutlich scannen oder fotografieren, um sicherzustellen, dass alle Informationen gut lesbar sind. Unleserliche Dokumente können zu Verzögerungen bei der Verifizierung und Auszahlung führen.
Die Überprüfung der Dokumentation erfolgt in der Regel innerhalb weniger Tage nach Einreichung. Sobald die Dokumente akzeptiert wurden, können die Spieler Auszahlungen vornehmen und ihr Spielerkonto vollständig nutzen.
Es ist zu beachten, dass die Vorlage der Dokumentation ein notwendiger Schritt ist, um die Sicherheit und Integrität des Casinos zu gewährleisten. Durch die Überprüfung der Identität der Spieler wird Betrug und Geldwäsche vorgebeugt.
Insgesamt ist die Dokumentation bei Boomerang Casino ein einfacher und unkomplizierter Prozess, der dazu dient, das Spielerlebnis für alle Beteiligten sicher und fair zu gestalten. Es ist ratsam, die erforderlichen Dokumente so schnell wie möglich einzureichen, um Verzögerungen bei Auszahlungen zu vermeiden.
https://boomerangcasino.one/
Greetings from Colorado! I’m bored to death at
work so I decided to check out your site on my iphone during lunch break.
I love the information you present here and can’t wait to take a look when I get home.
I’m shocked at how fast your blog loaded on my cell phone ..
I’m not even using WIFI, just 3G .. Anyways, fantastic blog!
buy cytotec pills online cheap: cytotec abortion pill – cytotec buy online usa
buy albuterol generic – order seroflo for sale generic theo-24 Cr 400mg
Zet Casino Freispiele 2021: Alles, was Sie wissen mГјssen
Zet Casino ist eines der beliebtesten Online-Casinos für deutsche Spieler. Mit einer breiten Auswahl an Spielen und großzügigen Bonusangeboten zieht es immer mehr Glücksspielfans an. Ein besonders attraktives Angebot sind die Zet Casino Freispiele, die den Spielern die Möglichkeit bieten, ohne Einsatz von eigenem Geld zu gewinnen.
Im Jahr 2021 gibt es einige spannende Promotionen, die Freispiele im Zet Casino ermöglichen. Diese können auf verschiedene Arten erhalten werden, zum Beispiel als Teil eines Willkommensbonus für neue Spieler oder als Belohnung für treue Kunden. Oft werden Freispiele auch im Rahmen von Sonderaktionen vergeben, wie zum Beispiel an Feiertagen oder zu besonderen Anlässen.
Um von den Zet Casino Freispielen zu profitieren, müssen die Spieler in der Regel bestimmte Bedingungen erfüllen. Dazu gehört oft das Erreichen eines Mindestumsatzes oder das Einlösen eines speziellen Bonuscodes. Es ist wichtig, diese Anforderungen genau zu lesen, um Missverständnisse zu vermeiden und sicherzustellen, dass die Freispiele erfolgreich genutzt werden können.
Freispiele sind eine großartige Möglichkeit, um neue Spiele auszuprobieren und Ihre Gewinnchancen zu erhöhen, ohne zusätzliches Geld einzuzahlen. Wenn Sie regelmäßig im Zet Casino spielen, sollten Sie immer nach aktuellen Promotionen Ausschau halten, um keine Freispielmöglichkeiten zu verpassen. Mit etwas Glück und Geschick können Sie so Ihre Gewinne steigern und ein noch besseres Spielerlebnis im Zet Casino genießen.
https://zetcasino.one/
I like the helpful info you supply on your
articles. I’ll bookmark your weblog and test again right
here regularly. I’m rather certain I will learn lots of new stuff proper here!
Best of luck for the following!
nolvadex generic tamoxifen 20 mg tablet tamoxifen moa
Good day! I just wish to offer you a big thumbs up for the excellent information you have got here on this post.
I will be returning to your site for more soon.
purchase albuterol pills – order seroflo online cheap buy theo-24 Cr 400mg for sale
buy misoprostol over the counter: Abortion pills online – cytotec pills buy online
Boomerang Casino Einzahlungscode: Was du wissen musst
Boomerang Casino ist eines der beliebtesten Online-Casinos, das eine Vielzahl von Spielen und großzügigen Boni anbietet. Einer der besten Wege, um den Spaß im Casino zu maximieren, ist die Verwendung von Einzahlungscodes. Diese speziellen Codes gewähren Spielern zusätzliche Boni und Vorteile, um ihre Spielerfahrung zu verbessern.
Der Boomerang Casino Einzahlungscode ist einfach zu verwenden. Alles, was du tun musst, ist bei der Einzahlung deines Guthabens den entsprechenden Code einzugeben. Sobald der Code akzeptiert wurde, wird der Bonus automatisch deinem Konto gutgeschrieben. Dies ermöglicht es dir, mehr Spiele zu spielen und deine Gewinnchancen zu erhöhen.
Es ist wichtig zu beachten, dass jeder Einzahlungscode bestimmte Bedingungen und Einschränkungen haben kann. Bevor du einen Code verwendest, solltest du daher immer die Geschäftsbedingungen sorgfältig lesen. Auf diese Weise kannst du sicherstellen, dass du alle Vorteile des Codes vollständig nutzen kannst.
Ein weiterer Vorteil der Verwendung von Einzahlungscodes im Boomerang Casino ist, dass sie Spielern die Möglichkeit geben, neue Spiele auszuprobieren, ohne dabei ihr eigenes Geld riskieren zu müssen. So kannst du neue Spiele kennenlernen und deine Lieblingsspiele finden, ohne ein finanzielles Risiko einzugehen.
Insgesamt ist der Boomerang Casino Einzahlungscode eine großartige Möglichkeit, um das Beste aus deiner Online-Spielerfahrung herauszuholen. Indem du diese Codes verwendest, kannst du deine Gewinnchancen maximieren und aufregende neue Spiele entdecken. Also, worauf wartest du noch? Suche dir deinen Einzahlungscode aus und beginne mit dem Spielen im Boomerang Casino!
https://boomerangcasino.one/
Tipico Casino: Willkommensbonus nach Einzahlung auszahlen lassen
Der Willkommensbonus im Tipico Casino gehört zu den attraktivsten Angeboten für Neukunden. Doch um den Bonus auszahlen zu lassen, müssen bestimmte Bedingungen erfüllt werden. Insbesondere geht es dabei um die Einzahlung auf das Spielerkonto.
Um den Willkommensbonus zu erhalten, muss zunächst eine Einzahlung auf das Tipico Casino Konto getätigt werden. Dabei gibt es verschiedene Zahlungsmethoden zur Auswahl, wie zum Beispiel Kreditkarte, PayPal oder Sofortüberweisung. Nach erfolgreicher Einzahlung wird der Willkommensbonus automatisch gutgeschrieben.
Damit der Bonus jedoch ausgezahlt werden kann, mГјssen bestimmte Umsatzbedingungen erfГјllt werden. Diese beinhalten in der Regel, dass der Bonusbetrag eine bestimmte Anzahl an Malen im Casino umgesetzt werden muss. Erst nach ErfГјllung dieser Bedingungen kann der Bonus und eventuelle Gewinne ausbezahlt werden.
Es ist wichtig, die Umsatzbedingungen genau zu überprüfen, um keine bösen Überraschungen zu erleben. Zudem sollte man darauf achten, dass der Bonus innerhalb eines bestimmten Zeitraums umgesetzt werden muss, da er sonst verfällt.
Zusammenfassend lässt sich sagen, dass der Willkommensbonus im Tipico Casino eine attraktive Möglichkeit ist, um das Spielerkonto aufzustocken. Wer jedoch plant, den Bonus auszahlen zu lassen, sollte sich im Vorfeld über die Umsatzbedingungen informieren und diese erfüllen. Nur so steht einer Auszahlung nichts im Wege und man kann die Gewinne genießen.
https://tipicocasino.one/
Юрист по заливу квартиры — это специалист,
который помогает пострадавшим от непредвиденных коммунальных аварий решить возникшие правовые вопросы и получить компенсацию убытков.
Задача такого юриста — обеспечить защиту прав и интересов клиентов
в досудебном регулировании споров или в процессе судебного разбирательства.
Профессионал в данной области должен
иметь глубокие знания жилищного законодательства,
понимать нюансы страхового права и уметь грамотно
собирать и оформлять необходимые документы, такие как акты о
заливе, заключения экспертов и сметы на ремонт.
Юрист готовит претензионные письма и иски,
ведет переговоры со страховыми компаниями, представляет интересы клиента
в суде, добиваясь взыскания ущерба
с виновных лиц или выплат со стороны страховщика.
В случае, если затопление произошло по
вине соседей или из-за недоработок коммунальных служб,
юрист поможет установить ответственность и обосновать размер
убытков, что является ключевым для успешного возмещения вреда.
При необходимости он также может посодействовать в организации и проведении независимой экспертизы,
чтобы точно определить причины и объем вреда.
Опытный юрист по заливу становится надежной опорой
для клиентов, позволяя им сосредоточиться на восстановлении повседневной жизни и минимизировать ущерб от неприятного случая.
Visit my web page: юрист по заливу квартиры москва
who should take tamoxifen: tamoxifen estrogen – tamoxifen and osteoporosis
diflucan 6 diflucan.com diflucan drug
Hi there! This is kind of off topic but I need some guidance from an established blog.
Is it tough to set up your own blog? I’m not very techincal but I can figure things out pretty quick.
I’m thinking about setting up my own but I’m not sure
where to begin. Do you have any tips or suggestions?
Cheers
Welches Spiel läuft gerade bei Tipico Casino?
Tipico Casino bietet seinen Kunden eine vielfältige Auswahl an spannenden Spielen, darunter auch eine große Auswahl an verschiedenen Spielautomaten. Doch welches Spiel läuft eigentlich gerade bei Tipico Casino?
Aktuell erfreut sich das Spiel “Book of Dead” groГџer Beliebtheit bei den Spielern von Tipico Casino. Bei diesem Spiel handelt es sich um einen Г¤gyptisch angehauchten Spielautomaten mit fГјnf Walzen und zehn Gewinnlinien. Das Besondere an diesem Spiel sind die Freispielrunden, die durch das Buch-Symbol ausgelГ¶st werden. WГ¤hrend der Freispiele kann ein zufГ¤lliges Symbol ausgewГ¤hlt werden, das sich auf den Walzen ausbreitet und somit fГјr noch hГ¶here Gewinne sorgen kann.
Aber auch andere Spiele wie “Starburst”, “Gonzo’s Quest” oder “Mega Moolah” erfreuen sich groГџer Beliebtheit bei den Spielern von Tipico Casino. Diese Spiele bieten alles, was das Spielerherz begehrt: Spannung, hohe Gewinnchancen und tolle Grafiken.
Es lohnt sich also, regelmäßig bei Tipico Casino vorbeizuschauen, um zu sehen, welches Spiel gerade läuft und vielleicht sogar mit etwas Glück hohe Gewinne einzustreichen. Wer weiß, vielleicht ist es ja gerade Ihr Lieblingsspiel, das bei Tipico Casino für Spannung und Unterhaltung sorgt. Viel Spaß und Erfolg beim Spielen!
https://tipicocasino.one/
Юридическая помощь при заливах квартир — незаменимый инструмент для защиты ваших прав и интересов. Попадание в подобную ситуацию влечет за собой ряд сложностей, начиная от оформления необходимых бумаг и заканчивая взысканием убытков с виновника происшествия.
Профессиональный юрист поможет составить акт о заливе, который фиксирует факт и обстоятельства повреждения имущества. Далее следует этап сбора доказательств: фотографии, справки о стоимости ущерба, свидетельские показания. Важно правильно рассчитать размер убытков, включающий стоимость восстановительного ремонта и прочие затраты.
Юрист займется подготовкой претензии к виновнику инцидента с требованием возместить ущерб. В случае отказа или игнорирования претензии вопрос может быть передан в суд. С юридической точки зрения процесс требует грамотной подготовки и стратегии, что станет залогом успешного результата.
Получение юридической помощи позволит вам чувствовать себя увереннее, а также избежать потенциальных подводных камней в процессе взыскания компенсации за залив квартиры.
затопили квартиру юрист
cytotec pills buy online: cytotec buy online usa – buy cytotec over the counter
I am now not positive where you are getting
your information, but great topic. I must spend a while
learning more or working out more. Thank you for excellent information I was looking for this info for
my mission.
Boomerang Casino Promo Code: Erhalten Sie den besten Bonus!
Das Boomerang Casino ist eine beliebte Online-Glücksspielseite, die eine Vielzahl von Spielen für alle Spieler bietet. Um neue Spieler anzulocken und bestehende Spieler zu belohnen, bietet das Boomerang Casino regelmäßig Promotions und Bonuscodes an. Einer der beliebtesten Bonuscodes ist der Boomerang Casino Promo Code, mit dem Spieler zusätzliche Boni und Freispiele erhalten können.
Der Boomerang Casino Promo Code ist einfach zu verwenden. Alles, was Sie tun müssen, ist während der Registrierung oder Einzahlung den Promocode einzugeben, um den entsprechenden Bonus zu erhalten. Der aktuelle Boomerang Casino Promo Code bietet Spielern einen großzügigen Willkommensbonus, der ihre Einzahlung verdoppelt und zusätzliche Freispiele für ausgewählte Spielautomaten bietet.
Es ist wichtig zu beachten, dass jeder Boomerang Casino Promo Code bestimmte Bedingungen und Anforderungen hat, die erfüllt werden müssen, um den Bonus zu erhalten. Spieler sollten sich daher die Geschäftsbedingungen sorgfältig durchlesen, um sicherzustellen, dass sie alle Anforderungen erfüllen.
Der Boomerang Casino Promo Code ist eine großartige Möglichkeit, um Ihre Gewinnchancen zu erhöhen und das Beste aus Ihrem Online-Casinoerlebnis herauszuholen. Machen Sie sich also bereit, Ihren Boomerang Casino Promo Code zu verwenden und zusätzliche Boni und Freispiele zu erhalten.
Besuchen Sie noch heute das Boomerang Casino und nutzen Sie den aktuellen Promo Code, um Ihre Gewinne zu steigern und noch mehr SpaГџ zu haben!
https://boomerangcasino.one/
buy cytotec pills cytotec pills buy online cytotec abortion pill
I am sure this piece of writing has touched all the internet viewers, its really
really nice paragraph on building up new website.
buy diflucan cheap: diflucan 200 mg daily – where can you buy diflucan over the counter
Das Zet Casino ist eines der beliebtesten Online-Casinos fГјr deutsche Spieler. Mit einer breiten Palette an Spielen und groГџzГјgigen Bonusangeboten zieht es immer mehr GlГјcksspielfans an. Ein besonders attraktives Angebot, das viele Spieler anlockt, ist der Zet Casino Code. Doch was genau verbirgt sich hinter diesem Code und wie kann man ihn nutzen?
Der Zet Casino Code ist ein spezieller Bonuscode, den Spieler verwenden können, um zusätzliche Vergünstigungen wie Freispiele, Einzahlungsboni oder Cashback-Angebote zu erhalten. Diese Codes werden regelmäßig von der Casinoseite angeboten und können beim Einlösen enorme Vorteile für die Spieler bringen.
Um den Zet Casino Code einzulösen, müssen Spieler zunächst ein Konto auf der Website des Casinos erstellen. Anschließend können sie den Code im entsprechenden Feld während des Einzahlungsvorgangs eingeben. Sobald der Code akzeptiert wurde, werden die zusätzlichen Vergünstigungen sofort dem Spielerkonto gutgeschrieben.
Es ist wichtig zu beachten, dass jeder Zet Casino Code bestimmte Bedingungen und Umsatzanforderungen hat, die erfüllt werden müssen, bevor die Gewinne ausgezahlt werden können. Daher ist es ratsam, die Bonusbedingungen sorgfältig zu lesen, bevor man den Code einlöst.
Insgesamt bietet der Zet Casino Code den Spielern eine tolle Möglichkeit, ihr Spielerlebnis zu verbessern und zusätzliche Gewinne zu erzielen. Mit den regelmäßig angebotenen Bonuscodes und Aktionen ist das Zet Casino eine hervorragende Wahl für alle, die auf der Suche nach einem unterhaltsamen und lukrativen Online-Casino-Erlebnis sind.
https://zetcasino.one/
https://diflucan.icu/# diflucan tablets
buy cytotec online fast delivery: buy cytotec pills – buy cytotec over the counter
I think the admin of this web site is in fact working hard in support of his web site, since here every information is quality based information.
Das Boomerang Casino ist bekannt für seine großzügigen Bonusangebote und spannenden Spiele. Für das Jahr 2022 gibt es nun auch attraktive no deposit Bonus Codes, die es Spielern ermöglichen, ohne Einzahlung von echtem Geld zu spielen und dennoch die Chance auf echte Gewinne zu haben.
Ein no deposit Bonus Code ist ein spezieller Code, den Spieler eingeben können, um einen Bonus ohne vorherige Einzahlung zu erhalten. Dieser Bonus kann Freispiele, Gratisguthaben oder andere Vergünstigungen beinhalten. Im Boomerang Casino gibt es verschiedene no deposit Bonus Codes, die regelmäßig aktualisiert und angeboten werden.
Um von den no deposit Bonus Codes im Boomerang Casino zu profitieren, müssen Spieler einfach den entsprechenden Code eingeben, wenn sie ihr Konto erstellen oder ihren Bonus beanspruchen. Die Codes sind in der Regel zeitlich begrenzt und können sich von Monat zu Monat ändern, daher ist es ratsam, regelmäßig auf der Website nach Updates zu suchen.
Mit den no deposit Bonus Codes haben Spieler die Möglichkeit, das Spieleangebot im Boomerang Casino zu erkunden, ohne dabei eigenes Geld riskieren zu müssen. Dies ist eine großartige Möglichkeit, die verschiedenen Spiele kennenzulernen und sich mit dem Casino vertraut zu machen, bevor man sich für eine Einzahlung entscheidet.
Wenn Sie also auf der Suche nach einem spannenden und großzügigen Casino sind, sollten Sie unbedingt die no deposit Bonus Codes im Boomerang Casino im Auge behalten. Mit etwas Glück können Sie dabei echte Gewinne erzielen, ohne vorher eine Einzahlung tätigen zu müssen. Viel Spaß und viel Glück beim Spielen!
https://boomerangcasino.one/
Gogo Casino är en spännande app för alla som älskar att spela casinospel på mobilen. Med ett brett utbud av spel och generösa bonuserbjudanden är detta en app som lockar många spelare.
Gogo Casino erbjuder ett stort utbud av spelautomater, bordsspel och live casinospel. Oavsett om du föredrar klassiska spelautomater eller mer avancerade videoslots finns det något för alla här. Dessutom kan du njuta av autentiska casinoupplevelser genom att spela live blackjack, roulette eller baccarat.
En av fördelarna med att använda Gogo Casino app är att du kan spela när som helst och var som helst. Du behöver inte längre sitta vid din dator för att kunna spela dina favoritspel, utan du kan ha dem med dig i fickan. Detta gör det enklare för dig att spela och ökar tillgängligheten.
För att öka spänningen och ge dig chansen att vinna stort erbjuder Gogo Casino regelbundna bonuserbjudanden och kampanjer. Du kan få bonusar vid insättningar, free spins eller delta i tävlingar med fina priser. På så sätt kan du få mer valuta för dina pengar och öka dina vinstchanser.
Sammanfattningsvis är Gogo Casino app en bra plattform för alla som älskar att spela casinospel. Med sitt stora spelutbud, generösa bonuserbjudanden och smidiga användarupplevelse är det en app som passar alla typer av spelare. Så ladda ner appen idag och börja spela för att ha chansen att vinna stort!
https://gogocasino.one
buy cytotec online fast delivery: buy cytotec in usa – buy misoprostol over the counter
Gogo Casino är en online casino som erbjuder ett brett utbud av spel och möjligheten att vinna stora vinster. AskGamblers är en populär webbplats som recenserar olika online kasinon och ger spelare möjlighet att dela sina erfarenheter och åsikter.
Gogo Casino har fått mycket positiv feedback från spelare på AskGamblers för dess enkla användargränssnitt och generösa bonusar. Många spelare har berömt kasinot för dess utmärkta kundsupport och snabba uttag.
För de som letar efter en pålitlig och underhållande spelupplevelse, är Gogo Casino definitivt värt att kolla in. Med ett stort utbud av spel från några av de bästa leverantörerna i branschen, finns det något för alla spelare att njuta av.
Så om du letar efter ett online casino med hög kvalitet och bra rykte, ta en titt på Gogo Casino och se om det är rätt för dig. Med hjälp av AskGamblers recensioner och spelares åsikter kan du vara säker på att du får en förstklassig spelupplevelse.
https://gogocasino.one
doxycycline 50 mg doxycycline hyclate 100 mg cap where can i get doxycycline
Zet Casino Promo Code: Holen Sie sich massive Boni mit diesem Code!
Zet Casino ist einer der aufstrebenden Stars im Online-Glücksspielsektor und bietet eine breite Palette von Spielen und Boni für seine Spieler. Mit dem Zet Casino Promo Code können Sie noch mehr aus Ihrem Spielerlebnis herausholen und massive Boni erhalten.
Der Promo-Code ermöglicht es neuen Spielern, einen großzügigen Willkommensbonus zu beanspruchen, der ihre ersten Einzahlungen um einen bestimmten Prozentsatz aufstockt. Dies bedeutet, dass Sie mehr Geld zum Spielen haben und Ihre Chancen auf große Gewinne erhöhen können.
Darüber hinaus bietet Zet Casino regelmäßig Promotionen und Bonusangebote für bestehende Spieler an, die den Promo-Code verwenden. Dies könnte Freispiele, Cashback-Angebote, Einzahlungsboni und vieles mehr umfassen, die Ihr Spielerlebnis noch aufregender und lohnender machen.
Um den Zet Casino Promo Code zu verwenden, müssen Sie sich einfach auf der Website des Casinos anmelden, den Code eingeben, wenn Sie Ihre Einzahlung tätigen, und die Bonusangebote genießen. Stellen Sie sicher, dass Sie die Bedingungen und Konditionen jedes Angebots lesen, um sicherzustellen, dass Sie alle Vorteile nutzen können.
Also, worauf warten Sie noch? Holen Sie sich jetzt Ihren Zet Casino Promo Code und erleben Sie die spannende Welt des Online-GlГјcksspiels mit massiven Boni und lukrativen Angeboten. Viel GlГјck und viel SpaГџ beim Spielen!
https://zetcasino.one/
buy zithromax: how much is zithromax 250 mg – buy zithromax
Boomerang Casino Mobil: Das ultimative Spielerlebnis unterwegs
Im Zeitalter der Digitalisierung ist es heutzutage wichtiger denn je, dass Online-Casinos eine benutzerfreundliche und mobile Plattform anbieten. Boomerang Casino hat dies erkannt und bietet seinen Kunden mit Boomerang Casino Mobil die Möglichkeit, ihre Lieblingsspiele auch unterwegs zu genießen.
Boomerang Casino Mobil ermГ¶glicht es den Spielern, von Гјberall aus und zu jeder Zeit auf ihr Casino-Konto zuzugreifen. Egal ob auf dem Weg zur Arbeit, in der Mittagspause oder gemГјtlich auf der Couch zu Hause – mit Boomerang Casino Mobil haben die Spieler ihr persГ¶nliches Casino immer griffbereit.
Die mobile Plattform von Boomerang Casino Гјberzeugt nicht nur durch ihre Benutzerfreundlichkeit, sondern auch durch ihre vielfГ¤ltige Auswahl an Spielen. Von klassischen Tischspielen wie Blackjack und Roulette Гјber beliebte Spielautomaten bis hin zu aufregenden Live-Casino-Spielen – bei Boomerang Casino Mobil ist fГјr jeden Geschmack etwas dabei.
Darüber hinaus bietet Boomerang Casino Mobil seinen Spielern regelmäßige Aktionen, Boni und Turniere, um das Spielerlebnis noch spannender zu gestalten. Mit nur wenigen Klicks können die Spieler an den neuesten Aktionen teilnehmen und sich so zusätzliche Gewinnchancen sichern.
Boomerang Casino Mobil zeichnet sich zudem durch eine sichere und zuverlässige Zahlungsabwicklung aus. Die Spieler können aus einer Vielzahl von Zahlungsmethoden wählen und sich darauf verlassen, dass ihre persönlichen Daten und Ein- und Auszahlungen jederzeit geschützt sind.
Insgesamt bietet Boomerang Casino Mobil das ultimative Spielerlebnis für unterwegs. Egal ob Anfänger oder erfahrener Spieler, mit Boomerang Casino Mobil können alle Casino-Liebhaber ihre Lieblingsspiele jederzeit und überall genießen. Probieren Sie es aus und entdecken Sie die Welt des Online-Glücksspiels mit Boomerang Casino Mobil. Viel Spaß und viel Glück!
https://boomerangcasino.one/
clomid buy buy generic clomid without prescription buy generic clomid no prescription
buy prednisone online canada: how much is prednisone 5mg – prednisone 5 mg
Boomerang Casino ist eine beliebte Online-Glücksspielplattform, die ihren Spielern eine breite Palette an Spielen und Funktionen bietet. Mit der Einführung der Boomerang Casino App können Spieler jetzt noch einfacher und bequemer auf ihre Lieblingsspiele zugreifen.
Die App ist benutzerfreundlich gestaltet und ermöglicht es den Spielern, ihre Lieblingsspiele unterwegs zu spielen. Egal, ob Sie Slots, Tischspiele oder Live-Casino-Spiele bevorzugen, die Boomerang Casino App hat für jeden Geschmack etwas zu bieten. Darüber hinaus bietet die App regelmäßig Boni und Aktionen an, um die Spieler zu belohnen und ihr Spielerlebnis zu verbessern.
Die Boomerang Casino App verfügt über eine Vielzahl von Zahlungsoptionen, so dass die Spieler problemlos Ein- und Auszahlungen vornehmen können. Darüber hinaus ist die App sicher und zuverlässig, so dass die Spieler sich keine Sorgen um die Sicherheit ihrer persönlichen Daten machen müssen.
Insgesamt bietet die Boomerang Casino App eine großartige Möglichkeit, das Casino-Erlebnis zu genießen, egal wo Sie sich befinden. Mit einer benutzerfreundlichen Oberfläche, einer Vielzahl von Spielen und regelmäßigen Boni und Aktionen ist die App definitiv einen Versuch wert. Laden Sie noch heute die Boomerang Casino App herunter und erleben Sie die Spannung des Glücksspiels auf Ihrem Handy oder Tablet.
https://boomerangcasino.one/
where can you buy amoxicillin over the counter: buy amoxicillin 500mg usa – where to buy amoxicillin pharmacy
http://clomida.pro/# where can i get clomid pill
На сайте https://start.shkolnayayarmarka.ru/ воспользуйтесь выгодными предложениями, связанными с приобретением товаров за образовательную валюту. Также вы сможете опубликовать свою продукцию на благотворительной ярмарке. Получить умникоины получится без скачивания и регистрации. Изучите все бренды, которые разместили свои товары. А в обмен ученики должны подтвердить свой уровень знаний. Воспользоваться предложением могут и талантливые студенты. Разместите свои бенефиты прямо сейчас.
На сайте https://grsuv.ru/ закажите такую полезную и нужную услугу, как гравировка, которая выполняется на жетонах, ложках, а также шильдах. Гравировка может быть выполнена на самых разных вещах. В компании также производят и клише, выполняют гравировку по кругу. При необходимости специалист приедет непосредственно к заказчику, чтобы выполнить все необходимые работы. Все услуги оказываются на инновационном оборудовании, а потому только высокого качества. Специально для вас специалист подберет шрифты и выполнит любую надпись. Будут написаны имена на любых столовых приборах, выполненных из серебра либо нержавеющей стали.
Boomerang Casino Lizenz
Boomerang Casino ist eine der aufstrebenden Online-Casino-Plattformen, die in den letzten Jahren an Popularität gewonnen hat. Das Casino bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele, Live-Casino und vieles mehr. Einer der Hauptgründe für den Erfolg von Boomerang Casino ist die Tatsache, dass es über eine gültige Glücksspiellizenz verfügt.
Die Lizenzierung von Online-Casinos ist ein wichtiger Aspekt, der sicherstellt, dass die Spieler geschützt sind und dass das Casino fair und verantwortungsbewusst betrieben wird. Boomerang Casino hat eine Lizenz von der renommierten Malta Gaming Authority erhalten, die als eine der strengsten Regulierungsbehörden in der Glücksspielbranche gilt.
Durch den Erwerb einer Lizenz von der Malta Gaming Authority zeigt Boomerang Casino sein Engagement für die Einhaltung der höchsten Standards in Bezug auf Sicherheit, Fairness und Transparenz. Diese Lizenzierung sorgt dafür, dass die Spieler geschützt sind und dass ihre persönlichen und finanziellen Daten sicher sind. Darüber hinaus wird sichergestellt, dass alle Spiele von Boomerang Casino fair und zufällig sind, und dass die Spieler eine faire Chance haben, zu gewinnen.
Die Lizenzierung von Boomerang Casino zeigt auch, dass das Casino für verantwortungsbewusstes Spielen steht. Als Lizenznehmer der Malta Gaming Authority muss das Casino sicherstellen, dass es Maßnahmen zur Bekämpfung von Spielsucht implementiert und dass es Spielern mit problematischem Spielverhalten Hilfe und Unterstützung anbietet.
Insgesamt ist die Lizenzierung von Boomerang Casino ein Zeichen für Qualität, Sicherheit und Vertrauenswürdigkeit. Spieler können mit Sicherheit spielen und wissen, dass sie in einem fairen und sicheren Umfeld agieren. Die Malta Gaming Authority erteilte Lizenz macht Boomerang Casino zu einer vertrauenswürdigen und seriösen Wahl für Online-Glücksspiel-Enthusiasten.
Abschließend lässt sich sagen, dass die Lizenzierung von Boomerang Casino ein wichtiger Schritt ist, der zeigt, dass das Casino den höchsten Standards in Bezug auf Sicherheit, Fairness und Verantwortlichkeit entspricht. Spieler können mit Zuversicht spielen und genießen die Vielzahl von Spielen, die das Casino zu bieten hat. Die Lizenzierung von Boomerang Casino ist ein weiterer Grund, warum es sich lohnt, dem Casino eine Chance zu geben.
https://boomerangcasino.one/
long term use of protonix
amoxicillin 50 mg tablets order amoxicillin online uk amoxicillin 500mg tablets price in india
zithromax 500 without prescription: zithromax over the counter canada – can i buy zithromax online
I’m bookmarking this for future reference. Your advice is spot on!
Zet Casino Einzahlungsmöglichkeiten
Das Zet Casino bietet seinen Spielern eine Vielzahl von Einzahlungsmöglichkeiten, um ihr Spielerlebnis so bequem wie möglich zu gestalten. Egal ob Sie per Kreditkarte, e-Wallet oder Banküberweisung einzahlen möchten, das Zet Casino hat für jeden die passende Option.
Eine der beliebtesten Einzahlungsmöglichkeiten im Zet Casino ist die Verwendung von Kreditkarten wie Visa und Mastercard. Diese Zahlungsmethode ist schnell, sicher und unkompliziert. Spieler können einfach ihre Kreditkartendaten eingeben und schon kann die Einzahlung getätigt werden.
Für diejenigen, die lieber e-Wallets verwenden, stehen im Zet Casino auch Optionen wie Skrill, Neteller und EcoPayz zur Verfügung. Diese ermöglichen es Spielern, ihr Geld sicher und schnell zu transferieren, ohne persönliche Bankdaten preiszugeben.
Eine weitere populäre Einzahlungsoption im Zet Casino ist die Banküberweisung. Obwohl diese Methode etwas länger dauern kann als andere, ist sie sicher und zuverlässig. Spieler können einfach den Betrag auf das angegebene Konto überweisen und ihre Einzahlung wird innerhalb weniger Tage gutgeschrieben.
Zusätzlich zu diesen Einzahlungsmöglichkeiten bietet das Zet Casino auch verschiedene alternative Methoden wie Paysafecard, Trustly und Bitcoin an. Diese ermöglichen es Spielern, ihre Einzahlungen auf ihre bevorzugte Weise zu tätigen.
Insgesamt bietet das Zet Casino eine breite Palette an Einzahlungsmöglichkeiten, um sicherzustellen, dass Spieler aus aller Welt bequem einzahlen können. Egal für welche Methode Sie sich entscheiden, im Zet Casino können Sie sicher sein, dass Ihre Einzahlung schnell und sicher abgewickelt wird.
https://zetcasino.one/
This post is packed with useful insights. Thanks for sharing your knowledge!
https://azithromycina.pro/# zithromax drug
Boomerang Casino Griechenland
Das Boomerang Casino ist ein beliebtes Online-Casino, das sich auf dem griechischen Markt etabliert hat. Mit einer Vielzahl von Spielen und spannenden Aktionen bietet das Casino seinen Spielern ein unvergessliches Spielerlebnis.
Das Boomerang Casino verfГјgt Гјber eine beeindruckende Auswahl an Spielen, darunter Spielautomaten, Tischspiele, Live-Casino-Spiele und vieles mehr. Die Spieler kГ¶nnen aus Hunderten von beliebten Spielen von fГјhrenden Anbietern wie NetEnt, Microgaming, Play’n GO und vielen anderen wГ¤hlen.
Neben den Spielen bietet das Boomerang Casino auch großzügige Boni und Aktionen für seine Spieler. Neue Spieler werden mit einem Willkommensbonus belohnt, der Freispiele und Bonusgeld umfasst. Darüber hinaus gibt es regelmäßig Aktionen und Turniere, bei denen die Spieler fantastische Preise gewinnen können.
Das Boomerang Casino legt großen Wert auf die Sicherheit und Fairness seiner Spiele. Das Casino verfügt über eine Lizenz der Malta Gaming Authority und verwendet eine sichere SSL-Verschlüsselungstechnologie, um die persönlichen Daten der Spieler zu schützen.
Insgesamt ist das Boomerang Casino eine ausgezeichnete Wahl fГјr Spieler, die nach einem unterhaltsamen und sicheren Online-Casino-Erlebnis suchen. Mit einer groГџen Auswahl an Spielen, lukrativen Boni und einer engagierten Kundenbetreuung ist das Boomerang Casino definitiv einen Besuch wert.
https://boomerangcasino.one/
ivermectin 0.5%: ivermectin 3mg price – stromectol 12mg
Im März 2019 gibt es im Tipico Casino wieder spannende Bonusaktionen, die die Spieler begeistern werden. Der Casino-Bereich des bekannten Anbieters bietet eine Vielzahl an Spielen und attraktive Boni, die für zusätzliche Spannung sorgen.
Einer der beliebtesten Boni ist der Willkommensbonus, der neuen Spielern einen großzügigen Bonus auf ihre erste Einzahlung bietet. So können Spieler ihr Casino-Guthaben gleich zu Beginn deutlich aufstocken und direkt mit dem Spielen loslegen.
Aber auch Bestandskunden kommen im Tipico Casino nicht zu kurz. Immer wieder werden Promotionen und Aktionen angeboten, bei denen Spieler zusätzliche Boni und Freispiele gewinnen können. So lohnt es sich, regelmäßig vorbeizuschauen und von den aktuellen Angeboten zu profitieren.
Ein weiterer Vorteil des Tipico Casinos ist die Vielfalt an Spielen, die fГјr Abwechslung und Unterhaltung sorgen. Neben klassischen Casino-Spielen wie Blackjack und Roulette finden Spieler auch eine groГџe Auswahl an Spielautomaten und Jackpot-Slots, bei denen hohe Gewinne winken.
Um von den Bonusaktionen im Tipico Casino profitieren zu können, ist es wichtig, die jeweiligen Bedingungen zu beachten. Oftmals müssen Boni mehrfach umgesetzt werden, bevor sie ausgezahlt werden können. Auch ist es ratsam, sich rechtzeitig über die aktuellen Aktionen zu informieren, um keine lukrativen Angebote zu verpassen.
Insgesamt lohnt es sich also, im März 2019 das Tipico Casino zu besuchen und die attraktiven Bonusaktionen zu nutzen. Mit etwas Glück und Geschick können Spieler so nicht nur viel Spaß beim Spielen haben, sondern auch satte Gewinne einstreichen.
https://tipicocasino.one/
prednisone 0.5 mg prednisone price canada prednisone 2.5 mg daily
http://stromectola.top/# ivermectin price usa
На сайте http://weller.ru/stroitelstvo/vinilovyj-sajding-obzor-oblicovochnogo-materiala/ ознакомьтесь с информацией, посвященной виниловому сайдингу. Имеется вся важная информация, которая касается характеристик, внешнего вида, особенностей такого материала. Опубликована и история появления винилового сайдинга, и другая ценная информация. Вместе с тем, вы узнаете о достоинствах материала, почему его выбирает большинство. Кроме того, перечислены и современные производители. Узнаете, где можно приобрести такой строительный материал по бюджетной стоимости.
depo-medrol generic name – buy loratadine online azelastine 10ml usa
Das Tipico Casino feiert Geburtstag! Seit einem Jahr bietet der beliebte Online-Glücksspielanbieter seinen Kunden ein umfangreiches Angebot an spannenden Spielen, attraktiven Aktionen und tollen Gewinnchancen. Zur Feier des Tages dürfen sich die Spieler auf besondere Überraschungen und Jubiläumsangebote freuen.
Seit seiner Gründung hat sich das Tipico Casino einen festen Platz in der Online-Glücksspielbranche erobert. Mit einer Vielzahl von Slots, Tischspielen und Live-Casino-Tischen bietet das Casino eine breite Auswahl für jeden Geschmack. Dazu kommen regelmäßige Aktionen und Promotionen, die den Spielern zusätzliche Gewinnchancen bieten.
Zum Geburtstag des Tipico Casinos können sich die Spieler auf besondere Boni, Freispiele und Verlosungen freuen. Es lohnt sich, die Augen offen zu halten und regelmäßig die Aktionen auf der Website zu überprüfen, um keine der Jubiläumsangebote zu verpassen.
Das Tipico Casino legt großen Wert auf die Sicherheit und Zufriedenheit seiner Kunden. Mit einer gültigen Lizenz und einer professionellen Kundenbetreuung sorgt das Casino für ein faires und unterhaltsames Spielerlebnis. Zudem bietet die Tipico Casino App die Möglichkeit, auch unterwegs die spannenden Spiele zu genießen.
Wir gratulieren dem Tipico Casino herzlich zum Geburtstag und wünschen allen Spielern viel Glück und Spaß beim Jubiläumsevent. Möge das Casino weiterhin erfolgreich wachsen und seinen Kunden ein erstklassiges Spielerlebnis bieten. Prost auf ein weiteres erfolgreiches Jahr!
https://tipicocasino.one/
order generic clomid pill: can i purchase clomid no prescription – get generic clomid
I appreciate the unique viewpoints you bring to your writing. Very insightful!
Zet Casino: 10 Freispiele ohne Einzahlung
Das Zet Casino ist ein beliebtes Online-Casino, das seinen Spielern eine Vielzahl von groГџartigen Spielen und Bonusangeboten bietet. Eines der besten Angebote fГјr Neukunden ist der Zet Casino Bonus von 10 Freispielen ohne Einzahlung. Das bedeutet, dass neue Spieler sofort nach der Registrierung 10 kostenlose Spins erhalten, um die spannenden Spielautomaten des Casinos auszuprobieren.
Um die 10 Freispiele zu erhalten, müssen sich Spieler einfach auf der Website des Zet Casinos anmelden und ein Konto erstellen. Sobald das Konto aktiviert ist, werden die Freispiele automatisch gutgeschrieben und können sofort genutzt werden. Die Freispiele können für ausgewählte Spielautomaten verwendet werden, die eine Vielzahl von Themen und Funktionen bieten.
Die 10 Freispiele ohne Einzahlung sind eine großartige Möglichkeit, das Zet Casino kennenzulernen und erste Gewinne zu erzielen, ohne eigenes Geld riskieren zu müssen. Spieler haben die Chance, echte Geldpreise zu gewinnen, die sie dann für weitere Spiele im Casino verwenden können. Es lohnt sich also auf jeden Fall, von diesem großzügigen Angebot Gebrauch zu machen.
Zusätzlich zu den 10 Freispielen ohne Einzahlung bietet das Zet Casino auch einen lukrativen Willkommensbonus für die erste Einzahlung. Spieler können einen Bonus von bis zu 500€ sowie weitere Freispiele erhalten, die ihnen noch mehr Gewinnchancen bieten.
Insgesamt ist das Zet Casino eine erstklassige Online-GlГјcksspieldestination, die mit groГџartigen Spielen, groГџzГјgigen Boni und einem hervorragenden Kundenservice Гјberzeugt. Spieler, die auf der Suche nach einer unterhaltsamen und lohnenden Casinoerfahrung sind, sollten sich das Zet Casino nicht entgehen lassen.
https://zetcasino.one/
amoxicillin for sale buy amoxicillin from canada where to buy amoxicillin over the counter
can you buy amoxicillin uk: order amoxicillin online – can i purchase amoxicillin online
На сайте https://ack-group.ru/ воспользуйтесь услугами психологического центра, в котором работают высококлассные, опытные специалисты с огромным стажем. Они никогда не критикуют, а подталкивают к тому, чтобы вы сами осознали проблему и приняли правильное решение. Очень часто устраиваются акции, чтобы вы сэкономили семейный бюджет. Психологи помогают пациентам справиться с любой проблемой, независимо от сложности. Основная специализация – это финансы, личные отношения. Если и вы хотите изменений в личной жизни и хотите улучшить свое положение, то воспользуйтесь услугами специалистов.
https://clomida.pro/# cost clomid
Your post was a beacon of knowledge. Thank you for illuminating this subject.
Boomerang Casino Erfahrungen: Ein Blick hinter die Kulissen
Das Boomerang Casino ist ein Online-Casino, das seit einiger Zeit auf dem Markt ist und sich groГџer Beliebtheit erfreut. Doch was genau verbirgt sich hinter dem Namen Boomerang Casino und welche Erfahrungen machen Spieler dort?
ZunГ¤chst einmal fГ¤llt auf, dass das Boomerang Casino ein breites Angebot an Spielen bietet. Von klassischen Slots Гјber Tischspiele bis hin zu Live-Casino-Spielen ist hier fГјr jeden Geschmack etwas dabei. Die Spiele stammen von renommierten Herstellern wie NetEnt, Microgaming und Play’n GO, was fГјr eine hohe QualitГ¤t und ein abwechslungsreiches Spielerlebnis sorgt.
Ein weiterer Pluspunkt des Boomerang Casinos ist der Kundenservice. Spieler berichten von schnellen und kompetenten Antworten auf ihre Anfragen, sei es per Live-Chat, E-Mail oder Telefon. Auch die Zahlungsmethoden werden positiv hervorgehoben, da das Casino eine Vielzahl von sicheren und einfachen Optionen anbietet.
Ein Kritikpunkt, den manche Spieler anführen, ist hingegen das Bonusangebot des Boomerang Casinos. Zwar gibt es einen attraktiven Willkommensbonus für Neukunden, doch die Umsatzbedingungen sind teilweise etwas hoch angesetzt. Zudem fehlen oft regelmäßige Aktionen und Promotionen für Bestandskunden.
Alles in allem lässt sich sagen, dass das Boomerang Casino eine gute Wahl für Spieler ist, die eine große Auswahl an Spielen und einen zuverlässigen Kundenservice schätzen. Der Anbieter punktet mit einer benutzerfreundlichen Website, schnellen Auszahlungen und einer soliden Spieleauswahl. Wer jedoch besonders viel Wert auf lukrative Bonusangebote legt, könnte hier möglicherweise etwas enttäuscht werden.
Insgesamt sind die Erfahrungen der Spieler mit dem Boomerang Casino größtenteils positiv, sodass es sich lohnt, dem Anbieter eine Chance zu geben und selbst herauszufinden, ob das Casino den eigenen Vorstellungen entspricht.
https://boomerangcasino.one/
ivermectin oral: ivermectin cream – ivermectin 0.1
Das Boomerang Online Casino bietet Spielern die Möglichkeit, von überall aus auf ihre Lieblingsspiele zuzugreifen. Mit einer Vielzahl von Spieloptionen und einer benutzerfreundlichen Oberfläche ist es leicht zu verstehen, warum diese Plattform so beliebt ist.
Das Boomerang Online Casino bietet eine Vielzahl von Spielen, einschließlich Slots, Blackjack, Roulette und vielem mehr. Spieler können aus einer Vielzahl von Themen und Spielvarianten wählen, um sicherzustellen, dass sie immer etwas finden, das ihren Vorlieben entspricht. Darüber hinaus sind die Spiele alle von führenden Softwareanbietern entwickelt worden, um ein erstklassiges Spielerlebnis zu gewährleisten.
Ein weiterer großer Vorteil des Boomerang Online Casinos ist die Verfügbarkeit von Boni und Promotionen. Neue Spieler können sich auf großzügige Willkommensboni freuen, während Stammkunden von regelmäßigen Sonderaktionen profitieren können. Dies erhöht nicht nur den Spaßfaktor, sondern bietet auch zusätzliche Anreize, um weiter auf der Plattform zu spielen.
Die Sicherheit und Zuverlässigkeit des Boomerang Online Casinos sind ebenfalls hervorzuheben. Mit einer sicheren und verschlüsselten Plattform können Spieler beruhigt sein, dass ihre persönlichen Daten geschützt sind. Darüber hinaus sind Ein- und Auszahlungen schnell und einfach, und der Kundensupport steht rund um die Uhr zur Verfügung, um bei Problemen zu helfen.
Insgesamt ist das Boomerang Online Casino eine ausgezeichnete Wahl fГјr Spieler, die nach einer vielseitigen und unterhaltsamen Online-GlГјcksspielplattform suchen. Mit einer breiten Palette von Spielen, groГџzГјgigen Boni und einer sicheren Spielumgebung ist es leicht zu verstehen, warum dieses Casino so beliebt ist. Wer also Lust auf ein spannendes Spielerlebnis hat, sollte unbedingt das Boomerang Online Casino ausprobieren.
https://boomerangcasino.one/
На сайте https://akvapark-fentazi.ru/ изучите важную и полезную информацию об аквапарке «Фэнтези». Вы находитесь непосредственно на официальном сайте. Это подходящее место, в котором сможет полноценно отдохнуть вся семья, а особенно дети. На стоянке вы сможете оставить автомобиль и насладиться временем, проведенным с семьей. При этом стоимость билета остается на доступном уровне. Каждый посетитель сможет воспользоваться СПА-зоной, поплавать в бассейне, полакомиться вкусными блюдами.
buy medrol 8 mg – order montelukast 10mg pill order astelin 10 ml for sale
synthroid tyrosine
how to get zithromax where can i buy zithromax in canada generic zithromax india
https://amoxicillina.top/# amoxicillin 500 mg tablets
Ищите карточный домик смотреть онлайн? Зайдите на сайт https://kino-domik.ru/ и вы найдете все сезоны карточный домик в отличном качестве. Если вы не смотрели сериал обязательно посмотрите. Политическая драма захватывает дух, а каждая серия преподносит что то новое и интересное.
Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und Boni für seine Spieler anbietet. Einer der begehrtesten Boni ist der Zet Casino No Deposit Bonus Code, der es Spielern ermöglicht, ohne Einzahlung zusätzliches Geld zu erhalten.
Um den No Deposit Bonus Code von Zet Casino zu erhalten, müssen Spieler sich lediglich auf der Website registrieren und den Code eingeben, der ihnen per E-Mail zugesandt wird. Dieser Bonus ermöglicht es den Spielern, das Casino auszuprobieren, ohne eigenes Geld riskieren zu müssen.
Der Zet Casino No Deposit Bonus Code kann für eine Vielzahl von Spielen im Casino verwendet werden, darunter Spielautomaten, Tischspiele und Live-Dealer-Spiele. Spieler haben die Möglichkeit, echtes Geld zu gewinnen, ohne dafür eine Einzahlung tätigen zu müssen.
Es ist jedoch wichtig zu beachten, dass der No Deposit Bonus Code von Zet Casino bestimmten Bedingungen unterliegt, die erfüllt werden müssen, bevor Gewinne ausgezahlt werden können. Dazu gehören Umsatzanforderungen und maximale Auszahlungslimits.
Insgesamt ist der Zet Casino No Deposit Bonus Code eine großartige Möglichkeit für Spieler, das Casino auszuprobieren und echtes Geld zu gewinnen, ohne eigenes Geld riskieren zu müssen. Es lohnt sich, nach diesem Bonus Ausschau zu halten und die Bedingungen sorgfältig zu lesen, um das Beste daraus zu machen.
https://zetcasino.one/
generic zithromax online paypal: zithromax 250 mg australia – average cost of generic zithromax
purchase desloratadine – albuterol oral order albuterol 4mg pill
На сайте https://container-platform.ru имеется номер телефона для того, чтобы заказать качественные, надежные, практичные контейнерные площадки, предназначенные для мусора. Есть как на 2, так и 3 контейнера. Прямо сейчас ознакомьтесь с расценками на стандартные варианты. Напротив каждого варианта указаны технические характеристики и другая важная информация, которая необходима для того, чтобы быстрее определиться с выбором. Наличие контейнерных площадок обязательно для всех дворов.
desloratadine 5mg usa – order generic clarinex albuterol 4mg usa
Der Tipico Casino unvorhergesehener Fehler hat viele Spieler in Verwirrung und Frustration gestГјrzt. Seit einiger Zeit klagen zahlreiche Nutzer Гјber Probleme bei der Nutzung der Plattform, die sich in unerwarteten Fehlern und Unterbrechungen Г¤uГџern.
Zu den häufigsten Problemen gehören Verbindungsabbrüche während des Spielens, Probleme beim Ein- und Auszahlen von Geldern sowie unerklärliche Fehlermeldungen. Dies führt zu Unmut und Verärgerung bei den Spielern, die sich auf ein reibungsloses Spielerlebnis verlassen.
Die Ursachen für diese unvorhergesehenen Fehler sind vielfältig und können von technischen Problemen bis hin zu internen Schwierigkeiten bei Tipico Casino reichen. Es scheint, dass die Plattform mit der steigenden Anzahl von Nutzern und dem zunehmenden Traffic nicht mithalten kann, was zu diesen Problemen führt.
Die Spieler erwarten von einem etablierten Unternehmen wie Tipico Casino eine hohe Qualität und Zuverlässigkeit in ihren Dienstleistungen. Daher ist es wichtig, dass das Unternehmen schnell handelt und die Probleme behebt, um das Vertrauen der Spieler nicht zu verlieren.
In der Zwischenzeit sollten die Spieler Geduld haben und die Kundenbetreuung kontaktieren, um ihre Beschwerden zu äußern und mögliche Lösungen zu finden. Es ist auch ratsam, alternative Plattformen zu prüfen, um sicherzustellen, dass das Spielerlebnis nicht weiter beeinträchtigt wird.
Letztendlich ist es wichtig, dass Tipico Casino die Bedenken und Beschwerden seiner Nutzer ernst nimmt und schnell handelt, um das Vertrauen und die Zufriedenheit der Spieler wiederherzustellen. Nur so kann das Unternehmen langfristig erfolgreich sein und seinen Ruf als seriöser Anbieter von Glücksspielen behalten.
https://tipicocasino.one/
how to buy prescriptions from canada safely: how to order prescription drugs from canada – online pharmacy no prescription needed
На сайте https://dom-otmostka.ru/ оставьте заявку для того, чтобы заказать такую популярную услугу, как монтаж отмостки из брусчатки, бетона, плитки, камня. Кроме того, оказываются услуги, связанные с обустройством ливневой канализации, а также дренажом. В компании работают компетентные сотрудники, которые произведут монтаж дорожек, детских, парковочных площадок. На любые работы действуют гарантии 3 года. Воспользуйтесь и вы компетентными работами лучших сотрудников. На все услуги установлены привлекательные расценки.
Your creativity and intelligence shine through this post. Amazing job!
https://medicationnoprescription.pro/# canada pharmacies online prescriptions
Das Boomerang Casino ist ein Online-Casino, das Spielern eine vielfältige Auswahl an Spielen und großzügigen Boni bietet. Mit einer benutzerfreundlichen Benutzeroberfläche und einer großen Auswahl an Spielen ist das Boomerang Casino eine beliebte Wahl für Spieler aus der Schweiz.
Das Boomerang Casino bietet eine breite Palette von Spielen, darunter Spielautomaten, Tischspiele, Live-Casino-Spiele und Jackpot-Spielautomaten. Die Spiele stammen von renommierten Softwareanbietern wie NetEnt, Microgaming und Evolution Gaming, um nur einige zu nennen. Dadurch können die Spieler eine erstklassige Spielerfahrung mit hochwertigen Grafiken und reibungslosem Gameplay genießen.
Das Boomerang Casino belohnt neue Spieler mit einem großzügigen Willkommensbonus, der in der Regel aus einem Einzahlungsbonus und Freispielen besteht. Darüber hinaus gibt es regelmäßig spannende Aktionen und Boni für bestehende Spieler, um deren Spielerlebnis zu verbessern.
Das Boomerang Casino ist vollständig lizenziert und reguliert und garantiert damit ein faires und sicheres Spielerlebnis. Die Spieler können sicher sein, dass ihre persönlichen Daten und finanziellen Transaktionen geschützt sind.
Insgesamt ist das Boomerang Casino eine ausgezeichnete Wahl fГјr Spieler, die auf der Suche nach unterhaltsamen Spielen, groГџzГјgigen Boni und einer sicheren Spielumgebung sind. Mit einer Vielzahl von Spielen und erstklassigem Kundensupport ist das Boomerang Casino definitiv einen Besuch wert.
https://boomerangcasino.one/
no prescription best website to buy prescription drugs buy medications online without prescription
Fine way of telling, and fastidious article
to obtain information regarding my presentation focus, which i am going to
present in college.
“Вавада скачать” – это не только игровая платформа,
но и возможность окунуться в захватывающий мир азартных
развлечений прямо с вашего устройства.
Здесь вы найдете огромное количество игр: от классических слотов до карточных
игр и рулетки. Но прежде чем начать игру,
необходимо скачать официальное
приложение “Вавада” на свое устройство.
С помощью “Вавада скачать” вы сможете
насладиться удобством
игры в любое удобное время. Кроме того, вы получите доступ
к эксклюзивным бонусам и
акциям, которые сделают ваше времяпровождение еще более увлекательным.
Не упустите возможность окунуться в мир азарта и адреналина вместе с
“Вавада скачать” – ваш шанс испытать удачу и получить незабываемые впечатления от
игры. Установите приложение прямо сейчас и начинайте путь к большим выигрышам!
Here is my web blog – vavada казино
You have a unique perspective that I find incredibly valuable. Thank you for sharing.
legitimate online pharmacy no prescription: buy medication online with prescription – buy drugs online without prescription
Bei Tipico Online Casino ist es ganz einfach, Ein- und Auszahlungen zu tätigen. Durch verschiedene Zahlungsmethoden können Spieler ihr Konto schnell und sicher aufladen und Gewinne auszahlen lassen.
Um Geld auf sein Spielerkonto bei Tipico Online Casino einzuzahlen, stehen den Spielern mehrere Optionen zur Verfügung. Die beliebtesten Methoden sind Kreditkarten wie Visa und Mastercard, E-Wallets wie Skrill und Neteller, sowie die Sofortüberweisung und die Paysafecard. Diese Zahlungsmethoden ermöglichen es den Spielern, ihr Konto innerhalb weniger Minuten aufzuladen und direkt mit dem Spielen zu beginnen.
Auch die Auszahlung von Gewinnen bei Tipico Online Casino ist einfach und unkompliziert. Spieler können ihre Gewinne per Banküberweisung, auf ihre Kreditkarte oder in ihr E-Wallet auszahlen lassen. Die Bearbeitungszeit variiert je nach Zahlungsmethode, beträgt aber in der Regel nur wenige Tage.
Um eine Auszahlung bei Tipico Online Casino zu tätigen, müssen die Spieler ihre Identität bestätigen und gegebenenfalls zusätzliche Dokumente wie einen Ausweis oder eine Rechnung hochladen. Dies dient der Sicherheit der Spieler und hilft dabei, Geldwäsche und Betrug zu verhindern.
Insgesamt bietet Tipico Online Casino seinen Spielern eine sichere und zuverlässige Möglichkeit, Geld einzuzahlen und Gewinne auszuzahlen. Mit einer Vielzahl von Zahlungsmethoden und einem einfachen Auszahlungsprozess können Spieler sich ganz auf ihr Spiel konzentrieren und sich auf ihre Gewinne freuen.
https://tipicocasino.one/
http://onlinepharmacyworld.shop/# canadian pharmacy without prescription
На сайте https://xakexpert.com/ воспользуйтесь услугами высококлассных, компетентных хакеров, которые смогут выполнить все необходимые работы, несмотря на их сложность. Вам доступна такая услуга, как взлом электронной почты, мобильного телефона, а также социальных сетей. Если вы подобрали какого-либо специалиста, то необходимо обязательно с ним связаться. Для этого напишите в чат. Специалист отличается колоссальным опытом, а самое главное, что обращение останется конфиденциальным.
http://edpill.top/# cheap ed treatment
canadian pharmacy coupon code: online pharmacy prescription – buying prescription drugs from canada
ModaOK считается лучшим источником информации о стрижках, татуировках, моде и другое. Здесь вы найдете полезные советы, как вещи сочетать и образы создавать. Также здесь есть лунный календарь. Погрузитесь вместе с нами в fashion-индустрию. https://modaok.ru – сайт, предназначен для тех, кто хочет быть стильной. Здесь можете почерпнуть идеи для создания маникюра, узнаете, что такое фэмили лук, с чем носить черный пиджак, какие женские и мужские часы сейчас в моде, как выбрать бюстгальтер по размеру и многое другое. Вас ждет только самое интересное и свежее!
Zet Casino Bonus Code
Online-Casinos erfreuen sich großer Beliebtheit, da sie Spielern die Möglichkeit bieten, bequem von zu Hause aus ihr Glück zu versuchen. Eine Möglichkeit, noch mehr Spaß und Gewinnchancen zu haben, sind Bonus Codes, die von Casinos wie dem Zet Casino angeboten werden.
Der Zet Casino Bonus Code ermöglicht es Spielern, zusätzliches Guthaben oder Freispiele für bestimmte Spiele zu erhalten. Diese Codes können auf der Website des Casinos oder über spezielle Promotionen auf verschiedenen Plattformen gefunden werden. Um einen Bonus Code einzulösen, muss lediglich der Code während der Einzahlung in das entsprechende Feld eingegeben werden.
Bei Zet Casino gibt es verschiedene Arten von Bonus Codes, wie zum Beispiel Willkommensboni für neue Spieler oder spezielle Aktionen für treue Kunden. Diese Bonusse können dazu beitragen, das Spielvergnügen zu steigern und die Gewinnchancen zu erhöhen.
Es ist jedoch wichtig zu beachten, dass Bonus Codes in der Regel bestimmten Bedingungen unterliegen, wie zum Beispiel Umsatzanforderungen oder eine begrenzte Gültigkeitsdauer. Bevor man einen Bonus Code einlöst, sollte man daher die entsprechenden Bonusbedingungen sorgfältig durchlesen.
Insgesamt bieten Bonus Codes eine tolle Möglichkeit, das Spielerlebnis im Zet Casino zu verbessern und zusätzliche Gewinne zu erzielen. Spieler sollten regelmäßig auf der Website des Casinos nach neuen Angeboten und Promotionen Ausschau halten, um keine lukrativen Bonusse zu verpassen. Egal ob man lieber an Spielautomaten, Roulette oder Poker spielt, mit einem Bonus Code kann man sein Glück noch weiter herausfordern.
https://zetcasino.one/
Attractive component to content. I just stumbled upon your web site and in accession capital to say
that I get in fact loved account your blog posts. Anyway I will be
subscribing to your augment or even I achievement
you access consistently quickly.
На сайте https://compsch.com/ собраны самые интересные, увлекательные и содержательные советы на тему компьютеров. Так вы узнаете о том, как правильно оптимизировать, настроить, обслуживать машину. Это позволит технике прослужить намного дольше. Также имеются ценные советы о том, как справиться с вредоносным ПО. Есть информация и об 1С бухгалтерии, о ремонте телевизоров и многое другое, что позволит быстро справиться с ситуацией. Есть данные и о том, как правильно подобрать ноутбук, какие моменты следует учесть при его покупке.
canada prescription online buy medications online no prescription online meds no prescription
https://medicationnoprescription.pro/# canadian drugs no prescription
Zet Casino: Kostenlose Freispiele im Casino
Zet Casino ist eine der beliebtesten Online-Glücksspielseiten, die unglaubliche Unterhaltung anbietet. Das Casino ist bekannt für seine großzügigen Boni und Aktionen, darunter auch kostenlose Freispiele. Diese Freispiele sind eine großartige Möglichkeit für Spieler, um einige der aufregendsten Spielautomaten im Casino zu genießen, ohne dabei ihr eigenes Geld verwenden zu müssen.
Zet Casino bietet regelmäßig neue Promotionen an, bei denen Spieler kostenlose Freispiele als Belohnung erhalten können. Diese Freispiele können auf ausgewählten Spielautomaten eingesetzt werden und bieten die Chance, echtes Geld zu gewinnen, ohne dabei eigenes Geld riskieren zu müssen.
Spieler können sich für die kostenlosen Freispiele qualifizieren, indem sie bestimmte Anforderungen erfüllen, wie z.B. eine Mindesteinzahlung tätigen oder an ausgewählten Spielen spielen. Die Freispiele werden dann automatisch dem Spielerkonto gutgeschrieben und können sofort verwendet werden.
Die Auswahl an Spielautomaten, auf denen die kostenlosen Freispiele eingesetzt werden kГ¶nnen, ist bei Zet Casino umfangreich. Spieler kГ¶nnen aus Hunderten von verschiedenen Spielen wГ¤hlen, darunter beliebte Titel wie Starburst, Book of Dead, Gonzo’s Quest und viele mehr.
Zet Casino legt großen Wert auf Fairness und Transparenz, daher sind die Bedingungen für die kostenlosen Freispiele klar und leicht verständlich. Spieler können sich darauf verlassen, dass sie bei Zet Casino eine sichere und vertrauenswürdige Spielumgebung vorfinden.
Wenn Sie also Lust haben, einige der besten Online-Spielautomaten zu spielen, ohne dabei Ihr eigenes Geld zu riskieren, dann sollten Sie unbedingt die kostenlosen Freispiele bei Zet Casino in Anspruch nehmen. Melden Sie sich noch heute an und profitieren Sie von den groГџzГјgigen Angeboten und Promotionen des Casinos. Viel SpaГџ und viel GlГјck beim Spielen bei Zet Casino!
https://zetcasino.one/
cheapest pharmacy for prescriptions without insurance: online pharmacy non prescription drugs – best online pharmacy no prescription
I just could not depart your site prior to suggesting that I extremely loved the standard information an individual supply on your guests?
Is going to be again regularly to check out new posts
Tipico Guthaben ins Casino transferieren
Wer bei Tipico ein Guthaben auf seinem Wettkonto hat und dieses gerne ins Online Casino transferieren möchte, kann dies ganz einfach tun. Dank der einfachen Bedienung und der benutzerfreundlichen Oberfläche des Tipico Portals ist dieser Vorgang schnell erledigt.
Um das Guthaben vom Wettkonto ins Casino zu transferieren, müssen zunächst einige Schritte befolgt werden. Zunächst muss man sich auf der Tipico Webseite einloggen und in seinem Konto einloggen. Dort kann man dann den Betrag auswählen, den man gerne ins Casino übertragen möchte.
Nachdem man den Betrag ausgewählt hat, muss man nur noch die Option wählen, dass das Guthaben ins Casino transferiert werden soll. Innerhalb weniger Sekunden wird das Guthaben dann auf das Casino-Konto übertragen und man kann sofort mit dem Spielen beginnen.
Es ist wichtig zu beachten, dass das Guthaben im Casino von Tipico nur fГјr Casinospiele genutzt werden kann und nicht fГјr Sportwetten. Wenn man also vorhat, im Tipico Casino zu spielen, ist es sinnvoll, das Guthaben dorthin zu transferieren.
Insgesamt ist es also sehr einfach, das Guthaben von Tipico ins Online Casino zu transferieren. Mit nur wenigen Klicks ist der Vorgang erledigt und man kann direkt mit dem Spielen beginnen. Wer also gerne Casinospiele bei Tipico spielt, sollte sein Guthaben schnell ins Casino transferieren.
https://tipicocasino.one/
http://medicationnoprescription.pro/# buying drugs without prescription
no prescription on line pharmacies canada online prescription canadian prescription drugstore review
synthroid instructions
I visited various web pages except the audio feature for audio
songs current at this web site is really fabulous.
Wie finde ich das beste Casino Spiel bei Tipico?
Tipico ist eine bekannte Marke in der Glücksspielbranche, die sowohl Sportwetten als auch ein Online Casino anbietet. Für viele Spieler ist die Auswahl des besten Casino Spiels bei Tipico entscheidend, um das maximale Unterhaltungserlebnis zu gewährleisten.
Zunächst einmal ist es wichtig zu wissen, dass die persönlichen Vorlieben und Spielpräferenzen jedes Spielers unterschiedlich sind. Einige bevorzugen vielleicht klassische Tischspiele wie Blackjack oder Roulette, während andere lieber aufregende Spielautomaten spielen.
Wenn es um die Auswahl des besten Casino Spiels bei Tipico geht, gibt es einige Faktoren zu berücksichtigen. Zunächst einmal ist es wichtig, die Auszahlungsquote des Spiels zu überprüfen. Je höher die Auszahlungsquote ist, desto besser sind die Gewinnchancen für den Spieler.
Ein weiterer wichtiger Faktor ist die Variabilität des Spiels. Einige Spiele bieten kleinere, aber häufigere Gewinne, während andere seltener, aber dafür höhere Gewinne bieten. Es ist wichtig, das richtige Gleichgewicht zwischen Risiko und Belohnung zu finden, um ein unterhaltsames Spielerlebnis zu gewährleisten.
Einige der beliebtesten Casinospiele bei Tipico sind unter anderem Roulette, Blackjack, Spielautomaten und Video Poker. Roulette ist ein klassisches Tischspiel, das auf Glück basiert und sowohl Anfängern als auch erfahrenen Spielern Spaß macht. Blackjack hingegen erfordert etwas mehr Strategie und Geschicklichkeit, um erfolgreich zu sein.
Spielautomaten sind eine weitere beliebte Option bei Tipico, da sie eine Vielzahl von Themen und Funktionen bieten, die fГјr jeden Geschmack geeignet sind. Video Poker ist eine weitere beliebte Variante von Poker, die sowohl GlГјck als auch Strategie erfordert.
Letztendlich ist es wichtig, das beste Casino Spiel bei Tipico basierend auf den eigenen Vorlieben und Bedürfnissen zu wählen. Es empfiehlt sich, verschiedene Spiele auszuprobieren und zu experimentieren, um herauszufinden, welches Spiel am besten zu einem passt. Mit ein wenig Glück und Geschicklichkeit können Spieler bei Tipico ein unterhaltsames und lohnendes Spielerlebnis genießen.
https://tipicocasino.one/
https://onlinepharmacyworld.shop/# offshore pharmacy no prescription
pharmacy coupons: canadian pharmacies not requiring prescription – online pharmacy no prescription
Online Casinos erfreuen sich zunehmender Beliebtheit bei Spielern auf der ganzen Welt. Eines der fГјhrenden Casinos in diesem Bereich ist das Zet Casino. Mit einer breiten Auswahl an Spielen und attraktiven Boni lockt das Zet Casino Spieler aus allen Ecken der Welt an.
Das Zet Casino bietet eine Vielzahl von Spielmöglichkeiten, darunter beliebte Casinospiele wie Slots, Roulette, Blackjack, Poker und vieles mehr. Die Spiele werden von renommierten Softwareanbietern entwickelt, was eine hohe Qualität und ein faires Spielerlebnis garantiert.
Ein weiterer großer Vorteil des Zet Casinos sind die großzügigen Boni und Aktionen, die regelmäßig angeboten werden. Neue Spieler können sich über einen Willkommensbonus freuen, der ihnen einen guten Start in das Casinoerlebnis ermöglicht. Darüber hinaus gibt es zahlreiche Promotionen und Belohnungen für treue Spieler, die das Spielen im Zet Casino noch spannender machen.
Das Zet Casino legt großen Wert auf Sicherheit und Fairness. Die Website verfügt über eine sichere SSL-Verschlüsselung, um die persönlichen Daten der Spieler zu schützen. Darüber hinaus werden alle Spiele regelmäßig von unabhängigen Prüfstellen auf Fairness überprüft, um sicherzustellen, dass die Spieler ein faires Spielerlebnis haben.
Insgesamt ist das Zet Casino eine ausgezeichnete Wahl fГјr Spieler, die nach einem unterhaltsamen und sicheren Online-Casinoerlebnis suchen. Mit einer breiten Auswahl an Spielen, groГџzГјgigen Boni und einem hohen MaГџ an Sicherheit und Fairness ist das Zet Casino definitiv einen Besuch wert.
https://zetcasino.one/
Das Tipico Casino ist eines der beliebtesten Online-Casinos in Deutschland, doch manchmal kann es vorkommen, dass Spieler Probleme bei der Auszahlung ihres Gewinns haben. In diesem Artikel werden wir uns mit dem Thema “Tipico Casino Auszahlen geht nicht” genauer befassen.
Es gibt verschiedene Gründe, warum eine Auszahlung im Tipico Casino nicht funktionieren könnte. Einer der häufigsten Gründe ist, dass die Spieler nicht alle erforderlichen Dokumente zur Verifizierung ihres Kontos eingereicht haben. Bevor eine Auszahlung stattfinden kann, muss das Casino sicherstellen, dass der Spieler volljährig ist und dass er die angegebenen Zahlungsmethoden verwenden darf.
Ein weiterer Grund könnte sein, dass der Spieler die Umsatzbedingungen nicht erfüllt hat. Oftmals müssen Spieler einen gewissen Betrag setzen, bevor sie sich ihre Gewinne auszahlen lassen können. Es ist wichtig, die Bonusbedingungen genau zu lesen, um Missverständnisse zu vermeiden.
Manchmal kann es auch technische Probleme geben, die dazu führen, dass eine Auszahlung nicht möglich ist. In diesem Fall ist es ratsam, den Kundenservice des Tipico Casinos zu kontaktieren, um das Problem zu klären.
Um sicherzustellen, dass eine Auszahlung reibungslos funktioniert, sollten Spieler sicherstellen, dass sie alle erforderlichen Dokumente eingereicht haben, die Bonusbedingungen erfГјllt haben und dass sie keine technischen Probleme haben.
Insgesamt ist das Tipico Casino eine zuverlässige und seriöse Plattform, auf der Spieler ihre Gewinne sicher und schnell auszahlen lassen können. Durch die Beachtung der genannten Punkte sollte es in der Regel keine Probleme bei der Auszahlung geben.
https://tipicocasino.one/
us pharmacy no prescription: promo code for canadian pharmacy meds – canadian pharmacy world coupons
best time to take sitagliptin
На сайте https://shemi-otopleniya.ru/ ознакомьтесь с техническими характеристиками, особенностями, нюансами гибкой подводки, выполненной из нержавеющей стали. Так вы сможете ознакомиться с размерами, диаметром, а также различными модификациями. Есть варианты небольших размеров, а также более внушительных. Также можно ознакомиться и с информацией, которая посвящена шаровому крану. Регулярно публикуются любопытные и интересные новости на данную тематику. Обязательно ознакомьтесь и с фотографиями.
Das Boomerang Casino ist eine der beliebtesten Online-GlГјcksspielseiten, die Spieler aus der ganzen Welt anlockt. Das Casino bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele, Live-Dealer-Spiele und mehr. Um auf diese Spiele zuzugreifen und um echtes Geld zu spielen, mГјssen die Spieler sich zuerst auf der Website anmelden.
Der Boomerang Casino Login ist einfach und unkompliziert. Spieler mГјssen lediglich ihre E-Mail-Adresse und ihr Passwort eingeben, um auf ihr Konto zuzugreifen. Wenn sie noch kein Konto haben, kГ¶nnen sie sich einfach registrieren, indem sie auf die SchaltflГ¤che “Registrieren” klicken und ihre persГ¶nlichen Daten eingeben.
Nachdem sich die Spieler erfolgreich angemeldet haben, können sie auf eine Vielzahl von aufregenden Spielen zugreifen und große Gewinne erzielen. Das Boomerang Casino bietet regelmäßig Boni und Aktionen für seine Spieler an, um ihr Spielerlebnis noch unterhaltsamer zu gestalten.
Darüber hinaus ist das Boomerang Casino sicher und zuverlässig, da es über eine Lizenz verfügt und die neuesten Sicherheitsmaßnahmen implementiert hat, um die persönlichen und finanziellen Daten der Spieler zu schützen. Spieler können also beruhigt sein, dass sie in einer sicheren und fairen Spielumgebung spielen.
Insgesamt ist der Boomerang Casino Login einfach und bequem, und das Casino bietet eine groГџe Auswahl an Spielen und groГџzГјgige Boni fГјr alle Spieler. Wenn Sie also nach einem Online-Casino suchen, das SpaГџ, Spannung und groГџe Gewinne bietet, ist das Boomerang Casino definitiv einen Besuch wert. Melden Sie sich noch heute an und erleben Sie das aufregende Spielerlebnis im Boomerang Casino!
https://boomerangcasino.one/
buying erectile dysfunction pills online erection pills online best ed pills online
На сайте https://www.kapatel.ru/ вы почерпнете много интересной, познавательной информации, которая касается дачи, сада, а также огорода. Вы узнаете о том, как правильно обустроить дачу, огород так, чтобы они были функциональными, вместительными и радовали богатым урожаем. Имеются данные о строительстве, ремонте и различных отделочных работах. Опубликованы материалы о вредителях, различных заболеваниях, о самых цветущих растениях. Вы можете задавать вопросы и присылать сообщения для уточнения некоторых моментов.
http://onlinepharmacyworld.shop/# cheapest pharmacy for prescriptions without insurance
На сайте https://1-line.su/ воспользуйтесь помощью квалифицированных, компетентных сотрудников популярного предприятия «Первая линия». Они окажут необходимую поддержку в вопросах оптимизации, автоматизации различных бизнес-процессов. Компания сделает все возможное для того, чтобы вы работали наиболее эффективно и продуктивно. Воспользуйтесь полным набором работающих инструментов, которые точно вам пригодятся для построения бизнеса. Для того чтобы начать сотрудничество, просто напишите на электронную почту.
canadian pharmacy prescription: canadian drugs no prescription – canadian pharmacy no prescription required
Boomerang Casino ist ein aufregendes Online-Casino, das Spielern eine breite Palette von Spielen und Unterhaltungsmöglichkeiten bietet. Mit einer benutzerfreundlichen Plattform und einer Vielzahl von Spielen ist boomerangcasino.com eine gute Wahl für alle Casino-Liebhaber.
Das Casino bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele, Live-Casino-Spiele und vieles mehr. Mit renommierten Software-Anbietern wie NetEnt, Microgaming und Evolution Gaming können die Spieler sicher sein, dass sie eine qualitativ hochwertige Spielerfahrung genießen werden.
Ein weiterer Vorteil von Boomerang Casino ist das großzügige Bonusangebot für neue Spieler. Mit Willkommensboni, Freispielen und anderen Aktionen können die Spieler ihr Spielvergnügen maximieren und ihre Gewinnchancen erhöhen.
Das Casino bietet auch eine Vielzahl von Zahlungsoptionen, darunter Kreditkarten, E-Wallets und Banküberweisungen, um sicherzustellen, dass die Spieler bequem Ein- und Auszahlungen tätigen können.
Das Casino verfügt über eine Lizenz der Malta Gaming Authority und gewährleistet so ein sicheres und faires Spielerlebnis für alle Spieler.
Insgesamt ist Boomerang Casino eine ausgezeichnete Wahl fГјr Spieler, die nach einer unterhaltsamen und spannenden Online-Casino-Erfahrung suchen. Mit einer Vielzahl von Spielen, groГџzГјgigen Boni und einer benutzerfreundlichen Plattform ist Boomerang Casino definitiv einen Besuch wert.
https://boomerangcasino.one/
It’s a shame you don’t have a donate button! I’d certainly donate to this outstanding blog!
I guess for now i’ll settle for book-marking and adding your RSS feed to my Google account.
I look forward to new updates and will share this site with
my Facebook group. Talk soon!
low blood pressure spironolactone
http://onlinepharmacyworld.shop/# canadian pharmacy world coupon
metformin 1000 sitagliptin 100
Um Geld von Ihrem Tipico Casino auf Ihr Wettkonto zu transferieren, müssen Sie einige wichtige Schritte befolgen. Zunächst einmal ist es wichtig zu beachten, dass es sich hierbei um zwei separate Konten handelt, die nicht automatisch miteinander verbunden sind.
Um also Geld von Ihrem Casino-Konto auf Ihr Wettkonto zu übertragen, müssen Sie sich zunächst auf der Website von Tipico einloggen. Sobald Sie angemeldet sind, sollten Sie sich Ihr Casino-Konto ansehen und prüfen, ob genügend Guthaben vorhanden ist, um auf Ihr Wettkonto übertragen zu können.
Wenn Ihr Casino-Konto ausreichend gefüllt ist, können Sie den Transfer starten. Dazu navigieren Sie zu den Ein- und Auszahlungsoptionen auf der Website und wählen die Möglichkeit, Geld von Ihrem Casino-Konto auf Ihr Wettkonto zu übertragen. Hierbei müssen Sie den gewünschten Betrag eingeben und den Transfer bestätigen.
Es ist wichtig zu beachten, dass einige Konditionen und Mindestbeträge für Transfers zwischen den Konten gelten können. Daher sollten Sie sich vorab über die genauen Bedingungen informieren, um sicherzustellen, dass der Transfer reibungslos verläuft.
Nachdem der Transfer abgeschlossen ist, wird das Geld in der Regel innerhalb weniger Minuten auf Ihr Wettkonto übertragen und Sie können sofort mit dem Platzieren von Wetten beginnen.
Insgesamt ist es also relativ unkompliziert, Geld von Ihrem Tipico Casino auf Ihr Wettkonto zu transferieren. Indem Sie die oben genannten Schritte befolgen und sich über die jeweiligen Konditionen informieren, können Sie sicherstellen, dass der Transfer problemlos verläuft und Sie Ihr Guthaben schnell für Wetten verwenden können.
https://tipicocasino.one/
Казино Pin-Up Casino – одно из самых популярных
онлайн казино, привлекающее своим
разнообразием игр и удобным интерфейсом.
Для того чтобы начать играть в Pin-Up Casino,
нужно создать аккаунт и войти в систему.
Для этого необходимо пройти процедуру регистрации и ввести логин и пароль.
После успешного входа в систему, игрок может
выбрать любую из сотен игр, представленных
в казино. Здесь каждый сможет найти что-то по
вкусу – от классических игровых автоматов до
карточных игр и рулеток.
Благодаря современным технологиям, играть пин ап в Pin-Up Casino можно не только на компьютере, но
и на мобильном устройстве.
Одним из главных преимуществ казино Pin-Up Casino является возможность
играть в любое удобное время и в любом
месте. Все игры доступны 24/7,
а качество графики и звука порадует даже самого взыскательного игрока.
Казино Pin-Up Casino предлагает своим игрокам выгодные бонусы и акции, которые позволят
увеличить шансы на победу и получить дополнительные призы.
Также здесь работает программы лояльности,
в рамках которых игроки могут получать дополнительные бонусы за
активное участие в играх.
Не упустите шанс испытать азарт и заработать деньги вместе с казино Pin-Up Casino.
Заходите на сайт, регистрируйтесь и
начинайте играть уже сегодня!
Каждый новый игрок может рассчитывать на бесплатные вращения и
другие приятные бонусы. Удачи вам и больших выигрышей!
Keyword: казино pin-up casino вход
ivermectin 4000 mcg
prescription free canadian pharmacy canada pharmacy coupon reputable online pharmacy no prescription
Das Zet Casino ist eine beliebte Online-GlГјcksspielplattform, die eine Vielzahl von Spielen und Zahlungsoptionen fГјr Spieler anbietet. Eine der beliebtesten Zahlungsmethoden bei Zet Casino ist PayPal.
PayPal ist eine sichere und vertrauenswürdige Zahlungslösung, die es Spielern ermöglicht, schnell und einfach Ein- und Auszahlungen auf ihrer Casinokonto vorzunehmen. Mit PayPal können Spieler ihr Konto aufladen, ohne sensible Bankdaten preiszugeben, da sie nur ihre E-Mail-Adresse und Passwort benötigen, um Zahlungen zu autorisieren.
Darüber hinaus ermöglicht PayPal schnelle und sichere Transaktionen, die es Spielern ermöglichen, sofort mit dem Spielen zu beginnen. Spieler können auch Einzahlungsboni und andere Werbeaktionen in Anspruch nehmen, wenn sie PayPal als Zahlungsmethode verwenden.
Das Zet Casino bietet eine Vielzahl von Spielen, darunter Spielautomaten, Tischspiele, Live-Casino-Spiele und vieles mehr. Mit PayPal als Zahlungsmethode können Spieler sicher sein, dass ihre Ein- und Auszahlungen schnell und sicher abgewickelt werden, damit sie keine Spielmöglichkeiten verpassen.
Wenn Sie auf der Suche nach einem vertrauenswГјrdigen Online-Casino mit PayPal als Zahlungsmethode sind, dann ist das Zet Casino die ideale Wahl. Registrieren Sie sich noch heute und tauchen Sie ein in die aufregende Welt des Online-GlГјcksspiels mit PayPal am Zet Casino. Viel GlГјck!
https://zetcasino.one/
prescription from canada: order prescription drugs online without doctor – best no prescription online pharmacies
На сайте https://climat.best приобретите качественные, функциональные кондиционеры, сплит-системы, тепловые насосы, а также чиллеры. Вся продукция именитых, проверенных и надежных брендов, а потому техника прослужит долго без потери технических характеристик, возможностей. А если необходимо подобрать что-то определенное, то воспользуйтесь специальным поиском. Перед вами есть и самые популярные позиции, которые пользуются особенным спросом среди покупателей. В интернет-магазине вы отыщите как настенные, так и напольно-потолочные конструкции, кассетные.
http://onlinepharmacyworld.shop/# canadian pharmacy coupon
casino tr?c tuy?n uy tín: choi casino tr?c tuy?n trên di?n tho?i – casino tr?c tuy?n uy tín
In den letzten Jahren haben Online-Casinos und Sportwetten an Popularität gewonnen. Viele Spieler sind auf der Suche nach einer Plattform, die beides anbietet, um ihr Glück zu versuchen. Das Tipico Casino ist eine solche Plattform, die eine große Auswahl an Casino-Spielen sowie Sportwetten anbietet.
Eine Besonderheit des Tipico Casinos sind die sogenannten “Casino Chips”. Diese Chips kГ¶nnen im Casino-Bereich des Tipico Casinos verwendet werden, um verschiedene Spiele zu spielen. Sie kГ¶nnen entweder durch den Kauf mit echtem Geld erworben werden oder durch das Spielen von Casino-Spielen verdient werden. Die Chips ermГ¶glichen es den Spielern, ihr Geld effizient zu verwalten und das Risiko zu minimieren, da sie nicht direkt mit ihrem eigenen Geld spielen.
Eine interessante Funktion des Tipico Casinos ist die Möglichkeit, die Casino Chips auch für Sportwetten zu verwenden. Spieler können ihre Chips auf verschiedene Sportveranstaltungen setzen und ihre Gewinne direkt auf ihr Konto im Tipico Casino gutschreiben lassen. Dies bietet den Spielern die Möglichkeit, ihre Casino-Gewinne in echte Wetten zu investieren und möglicherweise noch mehr Geld zu gewinnen.
Durch die Verwendung von Casino Chips für Sportwetten erhalten die Spieler eine zusätzliche Flexibilität und eine neue Möglichkeit, ihr Glück zu versuchen. Dies kann besonders attraktiv sein für Spieler, die sowohl an Casino-Spielen als auch an Sportwetten interessiert sind. Das Tipico Casino bietet eine innovative und unterhaltsame Möglichkeit, beides miteinander zu verbinden.
Insgesamt bieten die Casino Chips im Tipico Casino den Spielern eine einzigartige Erfahrung, die es ermöglicht, sowohl Casino-Spiele als auch Sportwetten zu genießen. Mit einer Vielzahl von Spielen und Wettoptionen zur Auswahl, ist das Tipico Casino eine ideale Plattform für alle, die auf der Suche nach einer Kombination aus Unterhaltung und Gewinnmöglichkeiten sind.
https://tipicocasino.one/
casino tr?c tuy?n uy tin choi casino tr?c tuy?n tren di?n tho?i casino tr?c tuy?n vi?t nam
game c? b?c online uy tín: casino online uy tín – casino tr?c tuy?n
На сайте https://td1000.ru/ находится огромное количество интересных, познавательных статей, которые касаются того, как развить социальные сети и простимулировать количество подписчиков. Также имеются данные о турах по Ямалу. Опубликован материал и о вместительных гардеробных и о том, как подобрать мебель. Есть контент, посвященный различным игровым онлайн-заведениям. Полезные статьи откроют вам глаза на многочисленные вопросы. По этой причине вы узнаете много нового и интересного.
http://casinvietnam.com/# casino tr?c tuy?n vi?t nam
На сайте https://podvodka.okis.ru/ ознакомьтесь с гибкой подводкой различного дюйма. Посмотрите технические характеристики, особенности и другую полезную информацию, которая будет вам необходима. На портале имеется таблица на некоторые размеры. Она поможет лучше сориентироваться в выборе. Также указаны и расценки, которые потребуются для составления сметы. Кроме того, имеется и важная информация относительно проведения профессиональных монтажных работ. Вы узнаете обо всех нюансах, которые потребуются в процессе установки.
casino tr?c tuy?n uy tin casino tr?c tuy?n casino tr?c tuy?n vi?t nam
micronase uk – buy glucotrol 10mg online forxiga 10mg us
I admire the way you tackled this complex issue. Very enlightening!
casino tr?c tuy?n uy tin choi casino tr?c tuy?n tren di?n tho?i game c? b?c online uy tin
Казино Starda – это одно из самых популярных казино в мире, которое предлагает огромный выбор
азартных игр и высокий уровень сервиса.
Оно известно своими качественными игровыми автоматами, а также широким выбором настольных игр, таких как покер, блэкджек и рулетка.
Казино Starda предлагает
своим посетителям не только азартные игры, но
и различные развлекательные мероприятия,
такие как концерты звездных артистов
и тематические вечеринки.
Здесь можно не только испытать удачу в
азартных играх, но и отдохнуть и расслабиться в уютной атмосфере казино.
Один из основных преимуществ казино Starda – это возможность играть в любимые
игры онлайн. Сайт казино имеет удобный интерфейс, который позволяет быстро найти нужную игру
и начать игру в любое удобное время.
Также казино Starda предлагает
своим игрокам различные бонусы и
акции, которые делают игру еще более увлекательной.
Казино Starda – это место, где каждый может почувствовать себя настоящим игроком
и насладиться азартом в полной мере.
Не упустите возможность посетить это уникальное казино и испытать удачу вместе с ним.
Look at my web blog; казино старда официальный сайт
micronase over the counter – forxiga 10mg without prescription buy forxiga pills
tizanidine vs robaxin
В России процедура списания долгов имеет
свои особенности, которые определяются законодательством
и правилами финансового рынка.
Списание долгов — это процесс,
при котором кредитор отказывается от своего права требования по возврату заемных средств или уменьшает сумму задолженности.
Для физических и юридических лиц этот процесс
может иметь различные последствия и условия, в зависимости от характера долга и субъекта, который является
кредитором.
Одной из основных форм списания долгов в России является процедура банкротства.
Физическое лицо может обратиться в
суд с заявлением о признании его банкротом.
В случае, если суд удовлетворяет такое заявление, происходит ликвидация имущества
заемщика для удовлетворения требований кредиторов.
После ликвидации имущества, если
оно не покрывает все долги, оставшаяся
сумма может быть списана.
Еще одним способом списания долгов является реструктуризация.
Этот метод предполагает пересмотр условий кредитного договора с целью уменьшения суммы задолженности или изменения сроков
ее погашения. Реструктуризация может быть
проведена по соглашению между заемщиком
и кредитором или по решению суда.
Кроме того, существует возможность
списания долгов в случае применения мер
государственной поддержки. Например, в периоды экономических кризисов
или чрезвычайных ситуаций правительство может принимать меры по стимулированию реструктуризации долгов
или даже их частичного или полного списания
для облегчения финансового положения населения или определенных отраслей экономики.
Важно отметить, что процесс списания долгов в России тщательно регулируется законодательством и требует соблюдения определенных процедур и условий.
Кроме того, списание долгов может иметь серьезные последствия для финансового положения как заемщика, так и
кредитора, поэтому необходимо внимательно оценивать все возможные альтернативы и последствия перед принятием решения
о списании долгов.
my blog – “https://pirisystem.com/piriwiki/index.php/Six_Ways_To_Avoid_%22http:_lit-info.ru_public_438_favorit-consult_%22_Burnout”
zeekr x цена
машина zeekr 001
li xiang l7
zeekr 001 z sport
На сайте https://greateastsiberia.ru/ почитайте поучительную, интересную и увлекательную информацию, которая касается здорового образа жизни. Имеются ценные, важные рекомендации относительно правильного питания, занятий спортом и других моментов. Есть информация о том, как сохранить суставы, о народных методах. Имеются рекомендации о том, как сохранить здоровье самых маленьких. Вы узнаете о том, как правильно бегать для получения необходимого эффекта. С вами поделятся своими рецептами для того, чтобы достичь гармонии души.
avatr 12
китайская машина l9
This is a topic which is near to my heart…
Cheers! Exactly where are your contact details though?
venlafaxine with food
На сайте https://iz-nerzhaveyki.ru/ ознакомьтесь с трубами из нержавейки, гибкой подводкой, шаровыми кранами, фитингами, фланцевыми кранами, обратными клапанами, арматурой и многим другим. В разделе изучите технические характеристики. Они бывают самых разных модификаций, диаметра, а также размеров, что позволит выбрать решение, основываясь на свои предпочтения, требования, цели покупки. Для большей наглядности имеются фотографии всех товаров, что позволит быстро сориентироваться в выборе.
casino tr?c tuy?n vi?t nam: dánh bài tr?c tuy?n – casino online uy tín
На сайте https://wedding42.ru/ почитайте информацию, которая касается того, как правильно, быстро и без хлопот организовать свадьбу мечты. Имеются материалы о том, как красиво и изысканно оформить помещение, какое платье лучше всего подобрать. Опубликована информация об организации СПА для жениха и невесты. Обязательно ознакомьтесь с рубриками, посвященными гостям на свадьбе, обычаям, свадебному путешествию, подаркам. Возможно, вам понравятся свадебные платья со шлейфом. Перед вами несколько вариантов, среди которых вы подберете что-то для себя.
tizanidine hydrochloride 4 mg street value
I’m truly appreciative of this article; it’s been an invaluable resource. Thank you for making it available.
Its not my first time to pay a quick visit this site, i am visiting this web page dailly and take fastidious information from here all the time.
casino tr?c tuy?n: casino tr?c tuy?n uy tín – dánh bài tr?c tuy?n
http://casinvietnam.com/# web c? b?c online uy tin
web c? b?c online uy tín: game c? b?c online uy tín – game c? b?c online uy tín
choi casino tr?c tuy?n trên di?n tho?i: casino tr?c tuy?n – casino online uy tín
buy glycomet 1000mg online cheap – buy cheap acarbose order acarbose 25mg pills
http://casinvietnam.shop/# choi casino tr?c tuy?n tren di?n tho?i
ModaOK считается лучшим источником информации о стрижках, татуировках, моде и другое. Здесь вы найдете полезные советы, как вещи сочетать и образы создавать. Также здесь есть лунный календарь. Мы предлагаем погрузиться в fashion-индустрию. https://modaok.ru – сайт, предназначен для тех, кто хочет быть стильной. Здесь вы почерпнете идеи для создания маникюра, сможете узнать, с чем носить черный пиджак, какие мужские и женские часы в моде, как выбрать бюстгалтер, что такое фэмили лук и другое. Вас ждет только самое интересное и свежее!
https://casinvietnam.com/# danh bai tr?c tuy?n
web c? b?c online uy tín: dánh bài tr?c tuy?n – casino tr?c tuy?n vi?t nam
voltaren and elequis interaction
https://casinvietnam.shop/# casino tr?c tuy?n
casino online uy tín: casino online uy tín – casino tr?c tuy?n vi?t nam
https://casinvietnam.com/# casino tr?c tuy?n vi?t nam
CRUDERRA https://cruderra.com/ – fast TechDocs for engineering teams. DiagramGPT and Architecture as code. Create docs to speed up development, onboarding & legacy code modernization.
venlafaxine hcl er reviews
choi casino tr?c tuy?n tren di?n tho?i game c? b?c online uy tin casino tr?c tuy?n vi?t nam
buy glycomet online cheap – purchase sitagliptin pills precose 25mg pill
casino tr?c tuy?n: casino tr?c tuy?n uy tín – dánh bài tr?c tuy?n
PBN sites
We’ll generate a system of PBN sites!
Benefits of our private blog network:
We perform everything so GOOGLE does not comprehend that this A self-owned blog network!!!
1- We acquire domain names from distinct registrars
2- The primary site is hosted on a VPS hosting (VPS is rapid hosting)
3- The rest of the sites are on distinct hostings
4- We assign a separate Google profile to each site with confirmation in Search Console.
5- We create websites on WP, we do not use plugins with the help of which Trojans penetrate and through which pages on your websites are produced.
6- We don’t reproduce templates and use only exclusive text and pictures
We don’t work with website design; the client, if wanted, can then edit the websites to suit his wishes
tamsulosin hci side effects
repaglinide pills – purchase jardiance generic empagliflozin 25mg usa
На сайте https://solvki-land.ru закажите увлекательную, познавательную экскурсию, рассчитанную на туристов различного возраста «Соловецкий феномен». Вы ознакомитесь с 10 экскурсиями, которые вы не сможете заказать ни в каком другом месте. Они длятся в течение 6 или 8 дней. На портале ознакомьтесь с природой Соловков, а в рамках экскурсий вы увидите Соловецкий сад, который представляет собой особую достопримечательность. На сайте вы увидите всю красоту острова, включая ландшафты, природу и многое другое.
voltaren cream dosage
http://casinvietnam.shop/# casino tr?c tuy?n vi?t nam
game c? b?c online uy tín: casino tr?c tuy?n uy tín – casino tr?c tuy?n vi?t nam
order prandin 2mg generic – empagliflozin 10mg generic order empagliflozin 25mg
На сайте http://profotonsk.ru профессиональный фотограф предлагает свою услугу по специализации – интерьерная фотосессия. Большой опыт работы и множество рекламных фотосессий позволяет фотографу работать как с частными риэлторами, так и с агентствами недвижимости. В своей работе он применяет камеру с полноформатным сенсором и широкоугольный объектив, это обеспечивает отличное качество изображения, у вас есть возможность в этом лично убедиться. Подробнее посмотреть услуги фотографа, отзывы, а также его портфолио, вы можете на портале.
casino online uy tín: casino tr?c tuy?n uy tín – casino tr?c tuy?n
https://casinvietnam.com/# casino tr?c tuy?n uy tin
casino tr?c tuy?n vi?t nam web c? b?c online uy tin choi casino tr?c tuy?n tren di?n tho?i
Компания MIGRANT SUPPORT с успехом предлагает услуги в Польше по оформлению транспортной лицензии. Мы сконцентрированы на действенном решении задач своих клиентов. Всегда рады детально ответить на все ваши вопросы и помочь вам. Ждем ваши обращения с нетерпением. https://vpolshe.com/transportnaya-litsenziya-v-polshe/ – сайт, где имеется интересная информация о транспортной лицензии в Польше. Гарантируем приемлемую стоимость. Вы можете уже сейчас получить квалифицированную консультацию. Пишите нам и звоните!
is zofran ok for dogs
choi casino tr?c tuy?n trên di?n tho?i: casino tr?c tuy?n uy tín – casino tr?c tuy?n
choi casino tr?c tuy?n tren di?n tho?i casino tr?c tuy?n uy tin choi casino tr?c tuy?n tren di?n tho?i
http://casinvietnam.com/# web c? b?c online uy tin
Всероссийская благотворительная школьная ярмарка предлагает вам разместить собственные товары на ней или купить за образовательную валюту бенефиты и услуги в приложении VK Умникоины без какой-либо регистрации и скачивания. https://start.shkolnayayarmarka.ru/ – сайт, где можно разместить свои услуги и товары в качестве личного пожертвования. Также здесь вы подробнее ознакомитесь с единицей обмена, которую применяют для осуществления сделок между покупателем и продавцом на благотворительных ярмарках. Пишите прямо сейчас нам.
На сайте https://fordrazbor.ru/ уточните то, где проходит авторазбор Ford. Перед вами топ сервисов, где проводится авторазбор. Здесь продают как б/у запчасти, так и те, что использовались совсем немного. От того, сколько детали находились в эксплуатации, зависит их итоговая стоимость. У некоторых компаний имеется онлайн-каталог, где можно посмотреть те товары, которые имеются в наличии, а также ознакомиться с ценами. А есть и такие авторазборы, где сразу же установят необходимую запчасть.
casino tr?c tuy?n uy tín: web c? b?c online uy tín – casino tr?c tuy?n
https://casinvietnam.shop/# game c? b?c online uy tin
web c? b?c online uy tín: web c? b?c online uy tín – game c? b?c online uy tín
На сайте https://t-audio.com/ оформите заявку для того, чтобы заказать такую важную услугу, как техническое обеспечение мероприятий. Компания находится на рынке в течение длительного времени, а потому выучила все потребности клиентов. В ней коллектив с огромным опытом, внушительный парк светового, звукового, а также сценического оборудования. Действуют привлекательные расценки, система скидок для постоянных клиентов. Для того чтобы ознакомиться с примерами работ, зайдите в портфолио.
casino tr?c tuy?n casino tr?c tuy?n casino tr?c tuy?n uy tin
https://casinvietnam.com/# choi casino tr?c tuy?n tren di?n tho?i
web c? b?c online uy tín: casino online uy tín – casino tr?c tuy?n vi?t nam
Зайдите на сайт FishX https://fishx.org/ и вы найдете все о рыбалке, cнастях, прикормке, приманках, способах ловле, а также отчёты о рыбной ловле. Ознакомьтесь с видами рыб и на что они ловятся, их места обитания. Сайт будет полезен как начинающим рыбакам, так и профи с опытом рыбной ловли.
http://canadaph24.pro/# cheap canadian pharmacy online
https://mexicoph24.life/# mexico pharmacies prescription drugs
buying from online mexican pharmacy mexican mail order pharmacies mexican rx online
http://indiaph24.store/# best online pharmacy india
medication from mexico pharmacy Mexican Pharmacy Online reputable mexican pharmacies online
does zyprexa help you sleep
http://canadaph24.pro/# canadian pharmacy 1 internet online drugstore
http://indiaph24.store/# Online medicine home delivery
На сайте https://vitaminium.shop/ закажите витамины, БАДы, минеральные комплексы, которые идеально подходят для всей семьи. Заказы принимаются круглосуточно. Их оформляют через корзину и в любое время. На всю продукцию имеются сертификаты. А если остались вопросы, то задайте их менеджерам в техподдержку. Оплата товаров является абсолютно безопасной, конфиденциальной. Имеются витамины, которые созданы специально для укрепления женского здоровья. Вся продукция реализуется по привлекательным расценкам и с оперативной доставкой.
wellbutrin to lose weight
top 10 online pharmacy in india Cheapest online pharmacy Online medicine home delivery
http://indiaph24.store/# buy medicines online in india
canadian mail order pharmacy canada pharmacy online online canadian pharmacy
На сайте https://luxbabycar.ru представлен каталог детских авто. Ассортимент постоянно обновляется. Здесь вы найдете: джипы, квадроциклы, багги, спецтехнику, толокар и многое другое высокого качества и по конкурентоспособным ценам. У нас самый широкий выбор детского автопарка. На сайте вы можете ознакомиться с фото-отзывами, а также посмотреть видео-обзор. Проконсультируйтесь со специалистом прямо сейчас. Весь товар прошел проверку качества, вы можете быть уверены за свой новый автомобиль.
https://mexicoph24.life/# mexican mail order pharmacies
zofran e plasil
http://indiaph24.store/# indian pharmacy online
vipps approved canadian online pharmacy Certified Canadian Pharmacies legitimate canadian pharmacies
Стремитесь улучшить свои языковые навыки? Погрузитесь в увлекательный мир английского языка с помощью наших кинокартин и сериалов на английском и британском языках. Насладитесь процессом изучения, погружаясь в увлекательные сюжеты и диалоги на языке оригинала. Наши фильмы и сериалы на английском не только помогут вам расширить словарный запас, но и сделают лучше понимание английской речи и культуры. Используйте просмотры сериалов на английском в качестве занимательного метода обучения. Подробнее на сайте https://serialy-na-angliiskom.pp.ua
Visit the page https://t.me/melbet_1xbet_betwinner_promocode where you will find new, current 1xbet Betwinner Melbet | Promo code. The latest information on promotional codes that are valid now and throughout 2024.
http://indiaph24.store/# best india pharmacy
кіберпонеділок
online shopping pharmacy india indian pharmacy best india pharmacy
На сайте https://www.techno-svyaz.ru/ разместите заказ на то, чтобы заказать печатные платы напрямую от производителя. Специально для вас действует оперативное производство. Есть возможность воспользоваться экспресс услугой. Вас ожидают короткие сроки, а также привлекательные расценки. Возможно заказать средние и мелкие серии печатных плат. Вся продукция отличается высоким качеством, на нее распространяются гарантии. Вы сможете заказать маркирование деталей. При необходимости воспользуйтесь консультацией.
http://indiaph24.store/# indian pharmacy
canadian pharmacy com canadian pharmacies canada pharmacy world
https://canadaph24.pro/# best rated canadian pharmacy
На сайте https://taker10.casino сыграйте в интересные, увлекательные и удивительные игры, которые произведут на вас впечатление своей динамикой, ярким оформлением. Есть Live-игры, которые позволят погрузиться в атмосферу азартных игр, топовые слоты, которые помогут попытать удачу и получить огромный выигрыш. Обязательно посетите раздел с топовыми играми, которые выбирает большинство. Воспользуйтесь возможностью заработать до 15% от депозитов рефералов. Вы сможете получать до 100 рублей ежедневно в качестве бонуса.
pharmacy website india buy medicines from India pharmacy website india
Компания «Эколан» предлагает впечатлительный выбор высококачественных товаров. У нас вы найдете замечательные декоративные подушки, одеяла, простыни, пледы, наматрасники, скатерти, полотенца и это далеко не полный перечень. Мы гарантируем привлекательные цены и быструю доставку. https://ecolan37.ru – сайт, где найдете только самое интересное для домашнего уюта и комфорта. Всегда готовы помочь с выбором нашим клиентам, мы их ценим и постараемся решить самые интересующие их вопросы. Заказывая у нас, можете быть уверены в том, что останетесь приобретением, довольны.
http://canadaph24.pro/# legitimate canadian pharmacy online
http://indiaph24.store/# pharmacy website india
top online pharmacy india indian pharmacy indian pharmacies safe
mexican border pharmacies shipping to usa purple pharmacy mexico price list mexico drug stores pharmacies
Хотите смотреть фильмы и сериалы онлайн в лучшем качестве? Kinogo – это то, что вам необходимо. Здесь представлено много фильмов, которые можно абсолютно бесплатно посмотреть. https://kinogo-la.net – место, где можете быстро отыскать потрясающее кино. Сайт имеет удобный и безопасный интерфейс. Выглядит он превосходно, и пользоваться им достаточно просто. На портале есть множество информации о фильмах, ознакомиться с ней можно в любое удобное время. Содержимое этого сервиса всегда актуально. Устраивайтесь поудобнее, и смотрите любимое кино!
http://mexicoph24.life/# mexican border pharmacies shipping to usa
http://indiaph24.store/# indian pharmacy paypal
purple pharmacy mexico price list cheapest mexico drugs medicine in mexico pharmacies
zyprexa class
https://mexicoph24.life/# purple pharmacy mexico price list
canadian pharmacy review Certified Canadian Pharmacies canadian pharmacy mall
https://canadaph24.pro/# trusted canadian pharmacy
http://indiaph24.store/# indian pharmacy online
world pharmacy india indian pharmacy top online pharmacy india
zofran patent
На сайте http://waltzprof.com вы можете на выгодных условиях приобрести стальной профиль в широком ассортименте. Они предназначены для лофт перегородок, фасадных конструкций, удобной и быстрой сборки ограждающих преград и другое. Компания использует передовые технологии для выпуска качественной продукции. Покупка от производителя – это прекрасный способ сэкономить на услугах посредника. Подробнее ознакомиться с продукцией и посмотреть информацию о компании, вы можете на сайте. Закажите обратный звонок, и менеджеры вас проконсультируют по всем вопросам.
http://canadaph24.pro/# northwest canadian pharmacy
Ищете способ сделать лучше личное владение английским. Окунитесь в мир кино с нашей коллекцией фильмов на британском также британском языках. Фильмы на английском, особенно с британским акцентом, помогают погрузиться в языковую среду. Для лучшего понимания можно использовать субтитры на английском. Улучшайте свой английский, блаженствуя любимыми кинокартинами. Подробнее здесь https://english-films.pp.ua/
world pharmacy india indian pharmacy fast delivery india online pharmacy
Зайдите на сайт https://luckyfood.ru/ где вы сможете купить мясо для собак с быстрой доставкой или самовывозом в Москве. Действует система скидок. Ознакомьтесь с большим каталогом продукции – говядина, баранина, индейка, субпродукты и многое другое. Порадуйте своего питомца, а легкость оформления заказа обязательно понравится!
https://indiaph24.store/# indianpharmacy com
semaglutide 14 mg canada – brand desmopressin DDAVP medication
http://mexicoph24.life/# buying prescription drugs in mexico online
purple pharmacy mexico price list Online Pharmacies in Mexico mexico pharmacy
http://indiaph24.store/# top 10 pharmacies in india
canada pharmacy online legit canadian pharmacies canada online pharmacy
http://canadaph24.pro/# canadian pharmacy service
order lamisil pills – fluconazole without prescription grifulvin v cost
ed meds online canada canadian pharmacies buying drugs from canada
order terbinafine – fluconazole 200mg cost griseofulvin drug
https://canadaph24.pro/# best canadian pharmacy online
https://canadaph24.pro/# canadian drug
restaurierung von Wohnhausern Fassaden
zetia coupons 2015
canada cloud pharmacy Large Selection of Medications from Canada buying drugs from canada
semaglutide 14mg brand – buy desmopressin without a prescription purchase DDAVP generic
https://indiaph24.store/# top 10 pharmacies in india
Посетите сайт https://fulldog.ru/ где вы найдете широкий ассортимент мяса для собак. Можно воспользоваться доставкой по Москве и области или забрать самовывозом. Мясо для собак – основа полезного рациона для вашего питомца, а спецпредложения сделают покупку еще более выгодной.
Желаете улучшить свои языковые навыки? Погрузитесь в увлекательный мир английского языка с помощью наших кинофильмов и сериалов на английском и британском языках. Насладитесь процессом освоения, погружаясь в интригующие сюжеты и диалоги на языке оригинала. Наши фильмы и сериалы на английском не только помогут вам расширить словарный запас, но и улучшат понимание английской речи и культуры. Используйте просмотры сериалов на английском в качестве занимательного метода освоения. Подробнее тут https://serialy-na-angliiskom.pp.ua
zyprexa alcohol
77 canadian pharmacy canadian pharmacies canada drug pharmacy
http://canadaph24.pro/# canadian drugs
На сайте https://chisto39.ru/ закажите профессиональную, качественную химчистку в тот же день, когда и обратились за услугой. На результат дается гарантия качества, потому как специалисты уверены в том, что услуга будет проведена именно так, как полагается и точно в обозначенные сроки. Среди основных услуг выделяют: химчистка ковров, диванов, матрасов, кресел, автомобилей. В работе используется только высокотехнологичное оборудование, качественная химия, которая избавляет от самых стойких пятен.
chantix similar to wellbutrin
zetia alternatives
http://indiaph24.store/# Online medicine order
mexican mail order pharmacies cheapest mexico drugs pharmacies in mexico that ship to usa
https://indiaph24.store/# india pharmacy
online shopping pharmacy india Generic Medicine India to USA buy medicines online in india
Can I simply say what a comfort to find someone that really knows what they’re talking about online.
You actually know how to bring an issue to light and make it important.
A lot more people ought to read this and understand this side of the story.
I was surprised you aren’t more popular given that
you most certainly have the gift.
http://indiaph24.store/# india pharmacy mail order
Gogo Casino.se är en spännande online spelplattform som erbjuder ett brett utbud av casinospel för svenska spelare. Med ett enkelt och användarvänligt gränssnitt är det lätt att navigera och hitta sina favoritspel.
På Gogo Casino.se hittar du populära spel som slots, bordsspel, live casino och mycket mer. Med spel från ledande leverantörer som NetEnt, Microgaming och Evolution Gaming kan du vara säker på att du har tillgång till högkvalitativa spel med spännande grafik och ljud.
En av fördelarna med att spela på Gogo Casino.se är att du kan njuta av casinospelen var som helst och när som helst, utan att behöva lämna ditt hem. Du kan spela på din dator, mobil eller surfplatta och ha tillgång till alla dina favoritspel på ett smidigt sätt.
Gogo Casino.se erbjuder också generösa bonusar och kampanjer för både nya och befintliga spelare. Med regelbundna erbjudanden kan du få extra belöningar och fördelar som gör din spelupplevelse ännu roligare och mer givande.
Med en trygg och säker spelmiljö samt snabba och smidiga betalningsmetoder kan du känna dig trygg när du spelar på Gogo Casino.se. Kundtjänsten är också tillgänglig för att hjälpa till med eventuella frågor eller problem som kan uppstå under din spelupplevelse.
Sammanfattningsvis är Gogo Casino.se en pålitlig och underhållande spelplattform som erbjuder en mängd olika casinospel för svenska spelare. Med sitt användarvänliga gränssnitt, generösa bonusar och säkra spelmiljö är det definitivt värt att prova på att spela på Gogo Casino.se för en spännande och underhållande spelupplevelse.
https://gogocasino.one
is it ok to take zofran daily while pregnant
I’m so glad I stumbled upon this article. It was exactly what I needed to enjoy reading!
Online medicine order Cheapest online pharmacy top online pharmacy india
What’s up to all, the contents present at this web site are genuinely
amazing for people experience, well, keep up the nice work fellows.
Welcome to OTunnels https://otunnels.com/ – your destination for unique ear tunnels and plugs! Explore our wide range of stylish and high-quality ear adornments. We offer a diverse selection of designs, including gothic motifs, cyberpunk aesthetics, geometric patterns, and much more. Our products are crafted using innovative materials, ensuring safety and comfort during wear. Dive into our collection and discover the perfect statement piece to elevate your style with OTunnels!
https://mexicoph24.life/# reputable mexican pharmacies online
На сайте https://vitaminium.shop/ у вас есть возможность приобрести минеральные комплексы и витамины для всей семьи. Менеджеры компании предложат для вас самый высокий уровень сервиса, выгодные условия сотрудничества, большой ассортимент минералов и витаминов, а также компетентную консультацию. Оплата удобная, выберите товар, добавьте его в «Корзину» и оформите заказ. Доставка осуществляется в любую страну. Подробнее ознакомиться с акциями, каталогом и увидеть нашу контактную информацию, вы можете на сайте.
top 10 online pharmacy in india Generic Medicine India to USA reputable indian online pharmacy
https://canadaph24.pro/# www canadianonlinepharmacy
Gogo Casino Partners är ett populärt program som erbjuds av Gogo Casino för att samarbeta med andra aktörer inom spelbranschen. Genom detta partnerskapsprogram kan företag och individer som delar samma intresse för casinospel samarbeta för att öka sin synlighet och locka fler spelare.
Genom att bli en partner med Gogo Casino får man tillgång till en rad förmåner och resurser. Man kan dra nytta av marknadsföringsverktyg och kampanjer för att locka nya spelare till sitt casino. Man kan även ta del av specialerbjudanden och bonusar som är exklusiva för partners, vilket kan öka intäkterna och skapa en mer lönsam verksamhet.
Som partner får man också tillgång till en dedikerad kontaktperson som man kan vända sig till för råd och support. Man blir en del av en gemenskap av likasinnade individer som delar ens vision och mål. Genom att samarbeta med Gogo Casino Partners kan man dra nytta av deras erfarenhet och expertis för att växa och utveckla sitt eget casino.
För de som är intresserade av att bli en partner med Gogo Casino är processen enkel och smidig. Man kan ansöka om partnerskap online och få svar inom kort. Genom att bli en partner med Gogo Casino får man tillgång till en rad fördelar som kan hjälpa ens verksamhet att växa och blomstra.
Sammanfattningsvis är Gogo Casino Partners ett fantastiskt sätt för företag och individer inom spelbranschen att samarbeta och dra nytta av varandras kunskap och resurser. Genom partnerskap med Gogo Casino kan man öka sin synlighet, locka fler spelare och öka sina intäkter. Det är en win-win-situation för alla inblandade parter och en möjlighet som inte bör missas.
https://gogocasino.one
вывоз мусора Новокуйбышевский район
mexico pharmacy Mexican Pharmacy Online mexican drugstore online
https://indiaph24.store/# online pharmacy india
Your style is unique in comparison to other folks I’ve
read stuff from. Many thanks for posting when you’ve got
the opportunity, Guess I will just bookmark this site.
Компания «Сомово» предлагает надежную мебель. Стараемся своим покупателям давать только самое лучшее. Наши спальни продуманы до мелочей, приобрести их вы можете у нас недорого с оперативной доставкой. Вся без исключения продукция проходит обязательную сертификацию. Ищете гостиные купить в москве? Somovo-mebel.ru – сайт, где можно отыскать множество вариантов комфортных спален. Заботимся о своей репутации и качестве товаров. Делаем все, чтобы вы покупкой были довольны. Советуйте нас своим друзьям и обращайтесь вновь!
https://indiaph24.store/# online shopping pharmacy india
http://canadaph24.pro/# canadian pharmacy online
Хотите купить на dvd увлекательные сериалы? Serialexpress готов вам в этом помочь. Здесь вы найдете диски, которых в других магазинах нет. Качество записи сериалов отличное, уверены, что вы останетесь довольны приобретением. Товары доступны по привлекательной цене, они хорошо упакованы и целые. Ищете купить сериал в тольятти? Serialexpress.ru – сайт, где представлен каталог. Здесь также можно ознакомиться с условиями оплаты. У нас действует накопительные скидки. Качество доставки вас приятно удивит. Задавайте свои вопросы по электронной почте нашим менеджерам.
https://canadaph24.pro/# canada drugs online review
Зайдите на сайт https://yeezy-boost-shop.ru/ и купите по выгодной цене Кроссовки Adidas Yeezy Boost оригинал. Магазин Адидас Изи Буст это широкий ассортимент, а сами кроссовки это уникальный дизайн, инновационные материалы и непревзойденный комфорт. Кроссовки Yeezy разных моделей и размеров всегда в наличии. Подробнее на сайте.
Hello mates, good paragraph and nice arguments commented here, I am actually enjoying
by these.
http://mexicoph24.life/# mexican rx online
mail order pharmacy india Generic Medicine India to USA online pharmacy india
what is zyprexa zydis used for
https://mexicoph24.life/# mexico drug stores pharmacies
Зайдите на сайт Chronolux https://poljot.pro/ и ознакомьтесь с большим каталогом модных часов для каждого. В нашем ассортименте представлены современные, уникальные наручные часы от различных марок. Вы обязательно сможете подобрать часы под свой бюджет и по параметрам, а также купить ремни для часов.
http://canadaph24.pro/# drugs from canada
top 10 online pharmacy in india п»їlegitimate online pharmacies india indian pharmacies safe
качественный сервис выполняет ремонт парогенераторов в Москве. Сотни раз обращался, все отремонтировали качественно!
https://mexicoph24.life/# buying prescription drugs in mexico online
Сайт v8corp.ru предоставляет виды услуг по цифровизации и автоматизации процессов с применением программ 1С. Сотрудничая с нами, вы сосредоточитесь на собственном бизнесе, мы в 24 отраслях экономики разбираемся. https://v8corp.ru/ – сайт, где есть возможность детальнее посмотреть конфигурации 1С. У нас гибкие тарифы. Поможем вам подобрать наилучшую конфигурацию продуктов 1С, подходящих конкретно для вашей компании. Оцените открывающиеся преимущества облачной Аренды 1С. Готовы быть вашим надежным помощником. Обращайтесь и получите консультацию!
На сайте https://shemi-otopleniya.ru/ почитайте информацию, которая касается гибкой подводки, выполненной из нержавеющей стали. Есть конструкции различной модификации и размера, а потому не составит труда выбрать наиболее подходящий под ваши запросы вариант. Есть информация и о том, как правильно проводить монтаж, в каких случаях используется гибкая подводка и многое другое. Также опубликованы фотографии для большей наглядности. Вся информация является качественной, актуальной, а потому на нее можно ориентироваться.
Сервисный центр Samsung https://galaxy-techservice.com/ это профессиональный сервис по ремонту техники Самсунг в Москве. Качественный и быстрый ремонт техники по доступным ценам. Гарантия на все виды работ. Ремонт любой сложности. Обученные и профессиональные сотрудники помогут вам восстановить технику или гаджет. Подробнее на сайте.
canadian pharmacy world canadian pharmacies ed drugs online from canada
http://mexicoph24.life/# reputable mexican pharmacies online
top 10 online pharmacy in india indian pharmacy fast delivery buy prescription drugs from india
https://canadaph24.pro/# canadian pharmacies
качественный сервис выполняет ремонт модулей управления индукционных плит в Москве. Сотни раз обращался, все отремонтировали качественно!
На сайте https://concept-digital.ru вам будет предложены услуги рекламного агентства. Разрабатываем стратегию, проводим анализ рынка и увеличиваем продажи. Студия рекламы предоставляет услуги дизайнера и маркетолога. Работая с нами, вы получите 100% гарантию на положительный результат. Подробнее ознакомиться с ценами и услугами рекламного агентства вы можете на сайте. Также здесь имеется портфолио. У нас заказывают, потому, как мы обладаем приличным опытом в продажах, имеем честные цены и правильно подходим к работе.
https://canadaph24.pro/# northwest pharmacy canada
mexican rx online mexican pharmacy medicine in mexico pharmacies
https://canadaph24.pro/# canadian online pharmacy reviews
top 10 pharmacies in india Generic Medicine India to USA world pharmacy india
buy ketoconazole 200 mg online cheap – generic nizoral 200mg purchase sporanox pill
Сайт https://krasnodar.climateon.ru/ это возможность купить кондиционер с установкой в Краснодаре, купить сплит систему в Краснодаре, купить кондиционер в Краснодаре в широком ассортименте по выгодным ценам. Большой каталог товаров, в том числе кондиционеры Краснодар, позволят вам купить продукцию известных брендов. Подробнее на сайте.
https://canadaph24.pro/# northern pharmacy canada
buy ketoconazole 200 mg generic – buy generic itraconazole buy cheap generic sporanox
mexico pharmacy mexico pharmacy mexican online pharmacies prescription drugs
Сайт Demo-1c.ru поможет вам узнать, кому будет полезна аренда 1С. Вам предложены демоверсии приложений 1С. Основными преимуществами облачного сервиса «1С Демо» и «Аренда 1С» являются: удаленное сопровождение программ «1С», круглосуточная техническая поддержка и ежедневное резервное копирование данных. https://demo-1c.ru/ – сайт, где можно увидеть перед арендой, покупкой распространенные решения 1С. В нашей команде собраны исключительно проверенные временем профессионалы. Закажите грамотную консультацию прямо сейчас!
http://mexicoph24.life/# mexico pharmacy
Компания «КапиталСтройАльянс» специализируется на производстве окон, дверей из ПВХ и алюминия. В своей сфере она имеет отменную репутацию. Качество нашей продукции мы довели до идеала. Гарантируем высокую степень точности изделия с отсутствием брака и быстрые сроки изготовления. Лучшие мастера поставят окна оперативно и после себя оставят порядок. http://oknaksa.ru – сайт, где у вас есть возможность ознакомиться с отзывами и осуществленными работами. При необходимости готовы проконсультировать. Всегда рады видеть вас!
medication from mexico pharmacy Mexican Pharmacy Online mexican pharmacy
Хотите купить на dvd увлекательные сериалы? Serialexpress готов вам в этом помочь. Тут можете найти диски, которых нет в иных магазинах. Качество записи сериалов отменное, мы уверены в том, что вы приобретением останетесь довольны. Товары доступны по привлекательной цене, они хорошо упакованы и целые. Ищете купить сериал в уфе? Serialexpress.ru – сайт, где представлен каталог. Здесь вы также можете ознакомиться с условиями оплаты. У нас действует накопительные скидки. Качество доставки вас приятно удивит. Все вопросы можно задать менеджерам по электронной почте.
https://indiaph24.store/# legitimate online pharmacies india
качественный сервис выполняет ремонт принтеров в Москве. Сотни раз обращался, все отремонтировали качественно!
На сайте https://stranauslug.by/ ознакомьтесь с частными объявлениями от самых разных мастеров и различного направления. Здесь вы сможете заказать услуги, связанные со строительством, отделкой помещения, а также грузоперевозки. Кроме того, есть возможность записаться на йогу, в фитнес-клуб, зумбу или бальные танцы. Регулярно появляются новые объявления с предложениями, что позволит отыскать подходящий вариант по привлекательной стоимости. Здесь же получится арендовать автомобиль, спецтехнику.
india pharmacy mail order indian pharmacy fast delivery indian pharmacy
Изучайте инглиш по кинокартинам. Идеальный способ для новичков освоить язык через просмотра кино на английском. Окунитесь в мир фильмов на английском а также расширьте свой словарный запас. Переходите на сайт https://anglijskij-po-filmam.pp.ua/ и начинайте изучать английский весело и еще эффективно!
http://mexicoph24.life/# mexico drug stores pharmacies
mexican online pharmacies prescription drugs Online Pharmacies in Mexico reputable mexican pharmacies online
http://mexicoph24.life/# mexico pharmacy
mexican online pharmacies prescription drugs Online Pharmacies in Mexico buying prescription drugs in mexico
http://canadaph24.pro/# canada pharmacy reviews
buy famvir – famvir 250mg canada buy valcivir 500mg generic
mexican border pharmacies shipping to usa Mexican Pharmacy Online mexican border pharmacies shipping to usa
http://mexicoph24.life/# mexican border pharmacies shipping to usa
Вам нужна психологическая помощь? Квалифицированный врач-психотерапевт Грудинин Александр Михайлович внимательно вас выслушает, вам будет комфортно с ним разговаривать. Он устранит и выявит ваши все психологические проблемы. http://grudinin-psihoterapevt.ru – сайт, где имеется детальная информация о специалисте, посмотрите ее уже сегодня. Также здесь есть тесты, статьи и часто задаваемые вопросы. На прием к доктору можно записаться, позвонив по телефону.
Если желаете купить интересные сериалы на DVD, то Serialexpress может предложить вам такую возможность. Запись сериалов довольно качественная, вы точно останетесь довольны покупкой. Товары прекрасно упакованы, цены приемлемые. Ищете магазин сериалов? Serialexpress.ru – сайт, где можно подробно ознакомиться с каталогом и выгодными предложениями. Также тут указаны условия доставки и оплаты. Появились какие-либо вопросы? Задайте их по электронной почте, указанной на нашем ресурсе. Менеджеры всегда рады вам помочь. Обращайтесь!
mexican pharmaceuticals online Mexican Pharmacy Online mexican rx online
http://indiaph24.store/# india pharmacy
Understanding COSC Validation and Its Importance in Horology
COSC Validation and its Demanding Criteria
Controle Officiel Suisse des Chronometres, or the Controle Officiel Suisse des Chronometres, is the official Switzerland testing agency that attests to the accuracy and accuracy of wristwatches. COSC accreditation is a symbol of excellent craftsmanship and trustworthiness in chronometry. Not all watch brands pursue COSC validation, such as Hublot, which instead follows to its proprietary demanding criteria with movements like the UNICO, reaching comparable precision.
The Science of Exact Timekeeping
The core mechanism of a mechanical watch involves the mainspring, which supplies power as it unwinds. This mechanism, however, can be prone to environmental elements that may affect its precision. COSC-validated movements undergo demanding testing—over fifteen days in various conditions (5 positions, three temperatures)—to ensure their resilience and reliability. The tests evaluate:
Mean daily rate precision between -4 and +6 secs.
Mean variation, maximum variation levels, and effects of temperature variations.
Why COSC Validation Matters
For watch fans and collectors, a COSC-certified watch isn’t just a item of tech but a testament to lasting quality and accuracy. It signifies a timepiece that:
Offers excellent dependability and precision.
Provides guarantee of superiority across the whole construction of the watch.
Is apt to maintain its value more effectively, making it a sound investment.
Well-known Chronometer Brands
Several well-known brands prioritize COSC certification for their timepieces, including Rolex, Omega, Breitling, and Longines, among others. Longines, for instance, provides collections like the Archive and Soul, which highlight COSC-certified movements equipped with innovative substances like silicone balance springs to improve resilience and performance.
Historical Context and the Development of Timepieces
The idea of the chronometer dates back to the need for precise timekeeping for navigational at sea, highlighted by John Harrison’s work in the eighteenth century. Since the official establishment of COSC in 1973, the accreditation has become a benchmark for assessing the precision of luxury watches, maintaining a tradition of superiority in horology.
Conclusion
Owning a COSC-validated watch is more than an visual choice; it’s a dedication to quality and precision. For those valuing accuracy above all, the COSC validation offers peace of mind, guaranteeing that each certified timepiece will operate reliably under various conditions. Whether for individual contentment or as an investment, COSC-accredited timepieces distinguish themselves in the world of horology, maintaining on a legacy of precise chronometry.
Если желаете купить интересные сериалы на DVD, то Serialexpress может предложить вам такую возможность. Качество записи сериалов хорошее, вы останетесь довольны приобретением. Цены доступные, товары отлично упакованные. Ищете магазин сериалов? Serialexpress.ru – сайт, где можно подробно ознакомиться с каталогом и выгодными предложениями. Также тут указаны условия доставки и оплаты. Возникли вопросы? Задайте их по электронной почте, которая указана на нашем сервисе. Менеджеры вежливые, они с радостью готовы помочь вам. Обращайтесь к нам!
indian pharmacies safe indian pharmacy indian pharmacy online
На сайте https://www.youtube.com/channel/UCXvwfNDluFJ-oeq9DKSapeQ вы сможете увидеть обновленную версию Прочных связей «MARVEL Человек-Паук», которая позволяет сыграть за опытного Питера Паркера. Он борется со злодеями и крупной преступностью в Нью-Йорке, постоянно балансирует на грани, пытаясь одновременно построить карьеру, разобраться в любви и защитить жителей. Плейлист приложение найдете на ютубе. Подписывайтесь на канал и ставьте лайки, а подробное описание вы найдете на канале, где также активно можно давать свои комментарии.
http://indiaph24.store/# buy medicines online in india
https://pride-land.ru/
долгосрочная аренда кипр
недвижимость на кипре купить цены
Хотите смотреть онлайн достойные фильмы и скачивать их в отменном качестве бесплатно? Вам в этом, конечно же, поможет Tartugi! Мы собрали наилучший контент, который вас порадует. Садитесь поудобнее и окунитесь в мир непревзойденных историй. https://good.tartugi.net – известный портал, где найдете все, что вам необходимо. Сайт имеет удобный интерфейс, разобраться с ним очень просто. Всегда в доступе интересные фильмы и сериалы онлайн, вы их можете скачать через торрент. Tartugi рад новым посетителям!
Интересуетесь улучшить свои языковые навыки? Погрузитесь в увлекательный мир английского языка с помощью наших кинофильмов и сериалов на английском и британском языках. Насладитесь процессом обучения, погружаясь в захватывающие сюжеты и диалоги на языке оригинала. Наши фильмы и сериалы не только помогут вам расширить словарный запас, но и улучшат понимание английской речи и культуры. Используйте просмотры в качестве эффективного метода обучения. Подробнее здесь https://filmy-na-anglijskom-yazyke.pp.ua/
На сайте https://iz-nerzhaveyki.ru/ почитайте информацию, которая связана с фитингами, кранами, подводками, выполненными из нержавеющей стали, шаровыми кранами, а также фильтрами, обратными клапанами, муфтами, арматурой, прокатом. Перед вами гибкая подводка самых разных размеров, модификаций, но вся она наделена длительным сроком эксплуатации, высоким качеством, на ней не образуется коррозия. Все конструкции выполнены по ГОСТу, в соответствии с самыми жесткими требованиями. Отличаются небольшой стоимостью.
recommended canadian pharmacies Large Selection of Medications from Canada canada drugs online review
http://canadaph24.pro/# pharmacy rx world canada
線上賭場
generic famvir – order famvir generic valcivir over the counter
На сайте https://shemi-otopleniya.jimdo.com/ вы сможете получить всю необходимую информацию, которая касается гибкой подводки из нержавеющей стали. Она может быть самого разного размера, диаметра, длины, что позволит подобрать вариант в соответствии с нуждами, целями, а также предпочтениями. Также вы узнаете и о том, как правильно проводить монтажные работы, чтобы продлить эксплуатационные сроки. Все изделия выполнены из надежных, качественных материалов, которые сохранят свой вид надолго.
mexico drug stores pharmacies: Mexican Pharmacy Online – best online pharmacies in mexico
Международный институт современного образования достойный внимания, он осуществляет профессиональную переподготовку специалистов. Все преподаватели – это профессионалы своего дела. Учебный процесс поставлен на высочайшем уровне. Ищете федеральная образовательная программа? Misokmv.ru – сайт, где о нас имеется более детальная информация. Мы гарантируем внимательное отношение и считаем, что учиться никогда не поздно. Вы всегда можете получить ответы на свои вопросы. Выбирайте нас и не пожалеете об этом. Получить образование в «МИСО» – удобно и выгодно, звоните нам прямо сейчас!
ModaOK предлагает вам погрузиться в мир моды и стиля. Здесь имеются интересные статьи о моде, татуировках, прическах и др. У нас есть лунный календарь стрижек. Также здесь мы делимся полезными рекомендациями. Ищете стрижки после 50 лет? Modaok.ru – сайт для тех, кто всегда хочет быть в тренде. Здесь вы узнаете о том, почему молодожены выбирают кольца с гравировкой, с чем носить вельветовые брюки и многое другое. Постоянно обновляем информацию, чтобы вы всегда были в курсе новых модных тенденций. Не упустите возможность стать стильной вместе с ModaOK!
reputable mexican pharmacies online cheapest mexico drugs reputable mexican pharmacies online
http://canadaph24.pro/# my canadian pharmacy
best india pharmacy https://indiaph24.store/# india pharmacy mail order
pharmacy website india
На сайте https://de.wikibrief.org/ вы сможете ознакомиться с интересной информацией на самую разную тему, включая радугу, время, население земного шара, золотой стандарт, всемирные банки и многое другое. Вся информация интересная, познавательная, а потому освещает все интересные и самые значимые вопросы. Все статьи написаны специалистами в данном вопросе, а потому данные подлинные, интересные и расширят ваш кругозор. Постоянно на сайте публикуются новые статьи, которые тоже будут вам интересны. Они касаются самых разных сфер.
На сайте https://egorkosarev.ru/ воспользуйтесь услугами видеооператора и видеомонтажера из Москвы. Он будет вам полезен, если планируете снять рекламное, детское видео, а также художественное или музыкальное. Также возможна и съемка интервью. Для того чтобы получить представление о работе, посмотрите шоурум. Огромное количество работ в портфолио. Все услуги оказываются по привлекательной стоимости и тогда, когда вам необходимо. В обязательном порядке обсуждается проект, заключается договор.
Сайт, где можно выбрать квадратная раковина в ванную различной формы.
На сайте https://smotret.net/ вы сможете найти все самые интересные, увлекательные сериалы на самый взыскательный вкус. Они доступны для просмотра не только на ПК, но и смартфоне, планшете. Подберите вариант по жанру, году выпуска, стране. Есть легендарные фильмы, которые стали модные еще в начале 2000-х, но также есть и новинки, которые точно никого не оставят равнодушным. Сериалы, фильмы на самую разную тематику. Смотрите их в любое время, абсолютно бесплатно. Перед вами огромный выбор вариантов, которые можно посмотреть вечером.
buy misoprostol over the counter п»їcytotec pills online cytotec abortion pill
Геоинтеллект – платформа, которая обладает множеством необходимых функций для сбора информации о населении, розничных конкурентах и др. Наши специалисты имеют достойный опыт работы аналитики геоданных. Они применяют лучшие научные практики, такие как: экономика, статистика, социальное и городское планирование. https://geointellect.com – сайт, где у вас есть возможность уже сегодня подробнее узнать о кейсах геомаркетинга. У нас имеется много удачных проектов во всех городах РФ, Узбекистана и Казахстана для сотен клиентов. Трудимся для вас!
На сайте https://penza-evakuator.ru/ воспользуйтесь услугами легкового, грузового эвакуатора. В компании вас ожидают небольшие расценки – от 2 500 рублей. Оплатить услугу вы сможете любым, наиболее комфортным для себя способом. Работа происходит в круглосуточном режиме. Также можно воспользоваться и такими услугами, как: эвакуатор спецтехники, междугородняя эвакуация. Техника подается за считанные минуты, даже несмотря на ваше местоположение. Вас ожидает привлекательная стоимость.
lisinopril 2.5 mg for sale: lisinopril 20mg coupon – lisinopril rx coupon
Зайдите на сайт Лишь Вам https://lishvam.ru/ который является электронной площадкой для размещения товаров и услуг. Для покупателей ассортимент более чем из 100.000 товаров, а доставка осуществляется по всей России. Ознакомьтесь с каталогом и выбирайте товары по выгодным ценам, получайте бонусы за покупки.
lanoxin 250mg over the counter – cheap irbesartan 150mg lasix pill
casibom giriş
Nihai Dönemsel En Gözde Casino Sitesi: Casibom
Bahis oyunlarını sevenlerin artık duymuş olduğu Casibom, en son dönemde adından genellikle söz ettiren bir şans ve casino platformu haline geldi. Ülkemizdeki en başarılı bahis web sitelerinden biri olarak tanınan Casibom’un haftalık olarak olarak değişen giriş adresi, alanında oldukça yenilikçi olmasına rağmen itimat edilir ve kazandıran bir platform olarak öne çıkıyor.
Casibom, yakın rekabeti olanları geride bırakarak köklü kumarhane platformların üstünlük sağlamayı başarıyor. Bu sektörde köklü olmak önemli olsa da, katılımcılarla iletişimde bulunmak ve onlara ulaşmak da eş kadar önemli. Bu durumda, Casibom’un gece gündüz yardım veren canlı olarak destek ekibi ile kolayca iletişime ulaşılabilir olması büyük bir artı sunuyor.
Hızla genişleyen oyuncuların kitlesi ile dikkat çekici olan Casibom’un arka planında başarılı faktörleri arasında, sadece ve yalnızca kumarhane ve gerçek zamanlı casino oyunları ile sınırlı olmayan kapsamlı bir hizmetler yelpazesi bulunuyor. Sporcular bahislerinde sunduğu kapsamlı seçenekler ve yüksek oranlar, oyuncuları ilgisini çekmeyi başarmayı sürdürüyor.
Ayrıca, hem spor bahisleri hem de casino oyunlar katılımcılara yönlendirilen sunulan yüksek yüzdeli avantajlı ödüller da dikkat çekiyor. Bu nedenle, Casibom hızla piyasada iyi bir tanıtım başarısı elde ediyor ve büyük bir oyuncuların kitlesi kazanıyor.
Casibom’un kazandıran ödülleri ve popülerliği ile birlikte, web sitesine üyelik ne şekilde sağlanır sorusuna da atıfta bulunmak gereklidir. Casibom’a mobil cihazlarınızdan, bilgisayarlarınızdan veya tabletlerinizden internet tarayıcı üzerinden kolayca erişilebilir. Ayrıca, web sitesinin mobil uyumlu olması da büyük bir avantaj getiriyor, çünkü artık pratikte herkesin bir cep telefonu var ve bu akıllı telefonlar üzerinden hızlıca ulaşım sağlanabiliyor.
Hareketli tabletlerinizle bile yolda gerçek zamanlı bahisler alabilir ve maçları canlı olarak izleyebilirsiniz. Ayrıca, Casibom’un mobil uyumlu olması, ülkemizde casino ve casino gibi yerlerin yasal olarak kapatılmasıyla birlikte bu tür platformlara erişimin büyük bir yolunu oluşturuyor.
Casibom’un güvenilir bir bahis platformu olması da gereklidir bir avantaj sunuyor. Ruhsatlı bir platform olan Casibom, duraksız bir şekilde eğlence ve kar sağlama imkanı sunar.
Casibom’a üye olmak da son derece kolaydır. Herhangi bir belge gereksinimi olmadan ve ücret ödemeden siteye rahatça abone olabilirsiniz. Ayrıca, web sitesi üzerinde para yatırma ve çekme işlemleri için de birçok farklı yöntem vardır ve herhangi bir kesim ücreti isteseniz de alınmaz.
Ancak, Casibom’un güncel giriş adresini takip etmek de elzemdir. Çünkü canlı iddia ve casino siteleri popüler olduğu için hileli siteler ve dolandırıcılar da belirmektedir. Bu nedenle, Casibom’un sosyal medya hesaplarını ve güncel giriş adresini periyodik olarak kontrol etmek elzemdir.
Sonuç, Casibom hem güvenilir hem de kazandıran bir casino sitesi olarak dikkat çekiyor. yüksek promosyonları, geniş oyun alternatifleri ve kullanıcı dostu mobil uygulaması ile Casibom, casino tutkunları için mükemmel bir platform getiriyor.
buy digoxin without a prescription – order trandate 100 mg sale lasix online
http://nolvadex.life/# arimidex vs tamoxifen bodybuilding
http://lisinopril.network/# lisinopril price without insurance
buy cytotec pills cytotec buy online usa cytotec online
Вам нужна психологическая профессиональная помощь? Тогда вам поможет центр «Доверие». Специалисты окажут нужную поддержку, им важно ваше хорошее состояние. Вы научитесь разбираться в своей психике и сможете понимать себя. Изменить свою жизнь к лучшему – вполне возможно. Ищете психологический центр? Ack-group.ru – сайт, где можно записаться на прием к ответственному и компетентному психологу в любое время. Также здесь имеется актуальная цена консультации опытного специалиста. Позвоните нам уже сейчас. Не доводите ситуацию до предела!
На сайте https://muzzilka.ru/ послушайте качественную, яркую и приятную музыку на любой вкус и от лидирующих исполнителей. Она точно понравится вам своим звучанием, аранжировкой. Перед вами огромный выбор композиций, которые подарят положительные, яркие эмоции, настроят на позитив и помогут расслабиться. Кроме того, композиции помогут вернуться в прошлое и поностальгировать. Регулярно на портале появляются новинки, которыми сможет насладиться каждый. Слушайте музыку онлайн либо скачивайте на устройство.
Хотите по недорогой цене снять в СПб жилье? Вам в этом точно поможет группа vk.com/komnataspb. Хоть и поиск соседей и комнаты в СПб дело нелегкое, но здесь большинство людей находит себе комфортное гнездышко. Выбирайте прямо сейчас актуальные предложения. Ищете снять комнату без посредников длительно? VK.com/komnataspb – популярное сообщество, в котором больше 6000 человек. Рекомендуем вам обязательно вступить в него и нажать рассказать друзьям. Размещение объявлений на стене абсолютно бесплатно, мы тщательно следим за их качеством. Обязательно ознакомьтесь с нашими правилами.
tamoxifen cost: tamoxifen for breast cancer prevention – tamoxifen dose
buy cipro ciprofloxacin generic price buy cipro online without prescription
http://nolvadex.life/# nolvadex d
Gerchik & Co Group of Companies https://gerchik.co/en is certified through VerifyMyTrade compliance service and provides 5,000 trades on a monthly basis which are then compared to all basic indicators demonstrated by other brokers and liquidity providers.
Желаете смотреть фильмы онлайн в безупречном качестве? Вам нужно на Киного! У нас имеется много интересных фильмов, с помощью которых вы после тяжелого дня можете поднять себе настроение. Вы точно о своих проблемах забудете. https://kinogo-fil.net – сайт, который специально создан для поклонников кино различных направлений. Теперь не надо идти в кино и тратить деньги на билеты. Смотреть фильмы онлайн у нас можно круглосуточно и абсолютно бесплатно. Самые лучшие новинки кино ждут именно вас!
На сайте https://costaspain.net/ вы сможете пообщаться с единомышленниками, узнать ценную, важную информацию на любую тему и получить ответы на самые разные вопросы. На этом форуме можно общаться на самых разных языках, включая русский, украинский, испанский. Здесь смогут оказать помощь, получится просто пообщаться, отдохнуть за приятными разговорами, поговорить об отдыхе, работе, аренде, продаже или покупке недвижимости, ПМЖ в Испании. Можно получить информацию по теме погоды в Испании. Есть возможность ознакомиться с прогнозом погоды. А если интересует что-то конкретное, то воспользуйтесь поиском.
На сайте https://animeast.ru/ воспользуйтесь уникальной возможностью посмотреть аниме вместе с друзьями, устроив совместный просмотр. Перед вами огромный выбор вариантов, которые помогут разнообразить досуг и получить от просмотра больше ярких эмоций. Есть как известные аниме, так и новинки, которые понравятся всем любителям этого интересного жанра. Для того чтобы найти интересующий вариант, воспользуйтесь специальным поиском. Изучите каталог аниме, чтобы выбрать оптимальный вариант.
CarTrip предлагает широкий выбор комфортабельных автомобилей. Мы поддерживаем автопарк в отличном состоянии и имеем приличный опыт работы. Машину предоставляем клиенту после чистки и мойки. Ищете аренда кабриолета Анапа? Auto-arenda-anapa.ru – сайт, где можно подобрать одну из доступных моделей. При необходимости поможем с выбором подходящего варианта. Оплата может быть произведена банковским переводом, наличными или же картами Visa, MasterCard, JCB. С нами вы сэкономите свои деньги. Насладитесь прямо из окна автомобиля красотами Анапы!
prescription drug prices lisinopril: cheap lisinopril – prices for lisinopril
https://ciprofloxacin.tech/# cipro
purchase cytotec buy cytotec online fast delivery buy cytotec pills online cheap
http://cytotec.club/# Cytotec 200mcg price
Центр остеопатии обращаясь, вы получите грамотную помощь в соответствии с высокими стандартами качества. Мы предлагаем для инвалидов и многодетных семей скидки. В разделе «Контакты» можно найти детальную информацию о том, как добраться к нам. https://osteopati.ru – сайт, где представлены отзывы о центре, ознакомиться с ними можете уже сейчас. Запишитесь к остеопату на консультацию. В ходе нее знакомимся, выясняем, какие у вас имеются нарушения в организме, объясняем, какой эффект оказывает остеопатическое лечение на данные нарушения.
На сайте https://svoi-rasteniya.ru/ ознакомьтесь со всем ассортиментом питомника. Здесь вы сможете заказать саженцы лимонов, роз, олеандра, инжира, различных декоративных растений. Весь посадочный материал является отборным, качественным, а потому точно приживется даже в суровых российских условиях. Вы сможете осуществить заказ через корзину либо позвонив по телефону на сайте. Регулярно ассортимент расширяется для того, чтобы вы смогли приобрести все, что необходимо и в любом количестве.
로드스탁과 레버리지 스탁: 투자의 새로운 영역
로드스탁에서 제공하는 레버리지 스탁은 증권 투자의 한 방법으로, 큰 수익률을 목표로 하는 투자자들에게 매력적인 옵션입니다. 레버리지를 이용하는 이 전략은 투자하는 사람들이 자신의 투자금을 초과하는 자금을 투입할 수 있도록 함으로써, 주식 시장에서 더욱 큰 힘을 가질 수 있는 기회를 줍니다.
레버리지 방식의 스탁의 기본 원칙
레버리지 방식의 스탁은 기본적으로 자본을 대여하여 사용하는 방법입니다. 예시를 들어, 100만 원의 자금으로 1,000만 원 상당의 주식을 사들일 수 있는데, 이는 투자하는 사람이 기본 투자 금액보다 훨씬 더 많은 증권을 취득하여, 주식 가격이 증가할 경우 상응하는 더욱 큰 이익을 얻을 수 있게 해줍니다. 그러나, 증권 값이 하락할 경우에는 그 손해 또한 증가할 수 있으므로, 레버리지를 이용할 때는 조심해야 합니다.
투자 계획과 레버리지
레버리지 사용은 특히 성장 잠재력이 높은 사업체에 투입할 때 효과적입니다. 이러한 기업에 높은 비중으로 투자하면, 성공할 경우 막대한 수익을 획득할 수 있지만, 그 반대의 경우 상당한 위험도 감수하게 됩니다. 따라서, 투자하는 사람은 자신의 위험성 관리 능력을 가진 장터 분석을 통해 통해, 어느 회사에 얼마만큼의 자금을 투자할지 선택해야 합니다.
레버리지의 장점과 위험성
레버리지 스탁은 상당한 이익을 약속하지만, 그만큼 큰 위험성 따릅니다. 주식 거래의 변화는 추정이 어렵기 때문에, 레버리지 사용을 이용할 때는 늘 시장 경향을 정밀하게 관찰하고, 피해를 최소로 줄일 수 있는 방법을 세워야 합니다.
최종적으로: 세심한 고르기가 요구됩니다
로드스탁을 통해 공급하는 레버리지 방식의 스탁은 막강한 투자 수단이며, 적절히 활용하면 큰 이익을 벌어들일 수 있습니다. 하지만 큰 리스크도 신경 써야 하며, 투자 결정이 충분한 데이터와 조심스러운 고려 후에 실시되어야 합니다. 투자자 본인의 금융 상황, 위험을 감수하는 능력, 그리고 시장 상황을 반영한 균형 잡힌 투자 전략이 핵심입니다.
На сайте https://esdogames.ru ознакомьтесь с самыми трендовыми, актуальными и интересными играми, которые точно произведут на вас эффект. Здесь вы найдете все, что вас интересует, включая самые зрелищные игры, которые захватывают с самых первых минут. Также представлен список лучших игр за 2024 год. Вы сможете поиграть во все, что хочется, прямо сейчас. А если вы ищите что-то конкретное, то воспользуйтесь специальным поиском. Подберите игру по жанру, режиму игры, платформе, чтобы облегчить поиск.
https://giorno24.it/ – sito di informazione per Milano e la Lombardia. Le ultime notizie dalla politica, dall’Italia, dal mondo, dalla cultura, dallo sport e dal calcio, dal settore della moda.
buy cipro online п»їcipro generic ciprofloxacin
buy cytotec online fast delivery: buy cytotec pills – order cytotec online
CarTrip предоставляет высококачественные услуги аренды авто в городе Краснодаре по разумной цене. Обращайтесь к нам, если вам необходим прокат авто. Машины все находятся в хорошем состоянии. Уверенны, что вы станете нашим постоянным клиентом. Ищете трейлер Краснодар? Prokat.car-trip.ru – портал, где есть возможность узнать условия аренды авто. У нас представлено множество машин на любой бюджет и вкус. Мы хорошо знаем свое дело и готовы ответить на интересующие вас вопросы, обращайтесь!
https://nolvadex.life/# tamoxifen cancer
займы ооо
Появились проблемы психического плана? Врач-психиатр Артур Евгеньевич Спиглазов окажет вам психологическую помощь и лечение. Вы справитесь со страхами и тревогами, обретете веру в себя и наконец, почувствуете вкус к жизни. Ищете психиатр на дом? Jur24.ru – сайт, где можете прямо сейчас записаться на прием к доктору. Артур Евгеньевич – истинный профессионал своего дела. Специалист поставит правильный диагноз и подберет подходящие лично вам препараты. С ним вы можете проконсультироваться при возникновении интересующих вопросов, касаемо лечения.
Zet Casino: 50 Freispiele – Welches Spiel soll ich wГ¤hlen?
Wenn es um Online-Casinos geht, gibt es viele Optionen zur Auswahl. Ein beliebtes Casino, das derzeit Freispiele anbietet, ist das Zet Casino. Mit 50 Freispielen haben Spieler die Möglichkeit, verschiedene Spiele auszuprobieren und ihr Glück zu versuchen. Doch welche Spiele kann man mit diesen Freispielen spielen?
Das Zet Casino bietet eine Vielzahl von Spielen, darunter eine breite Auswahl an Spielautomaten, Tischspielen und Live-Casino-Spielen. Bei den 50 Freispielen kГ¶nnen Spieler aus verschiedenen Spielautomaten wГ¤hlen, die von renommierten Anbietern wie NetEnt, Microgaming, Play’n GO und vielen anderen entwickelt wurden.
Eine beliebte Option fГјr die Verwendung der Freispiele bei Zet Casino sind Spielautomaten wie Starburst, Book of Dead, Gonzo’s Quest oder Wolf Gold. Diese Spiele sind bekannt fГјr ihre unterhaltsamen Themen, spannenden Bonusrunden und hohen Gewinnchancen. Spieler kГ¶nnen mit den Freispielen diese beliebten Slots ausprobieren und sehen, ob sie ihr GlГјck haben.
Für diejenigen, die lieber Tischspiele spielen, bietet das Zet Casino auch eine große Auswahl an Blackjack, Roulette und Baccarat-Optionen. Spieler können mit den Freispielen auch einige dieser Tischspiele ausprobieren und sehen, ob sie das Glück auf ihrer Seite haben.
Für diejenigen, die ein authentisches Casino-Erlebnis bevorzugen, bietet das Zet Casino auch eine Auswahl an Live-Casino-Spielen. Mit den Freispielen haben Spieler die Möglichkeit, Live-Dealer-Spiele wie Live Blackjack, Live Roulette oder Live Baccarat zu spielen und das echte Casino-Feeling zu genießen.
Insgesamt bietet das Zet Casino mit seinen 50 Freispielen eine Vielzahl von SpielmГ¶glichkeiten fГјr alle Arten von Spielern. Egal ob Slot-Fan, Tischspiel-Liebhaber oder Live-Casino-Enthusiast – mit den Freispielen kГ¶nnen Spieler verschiedene Spiele ausprobieren und sehen, welches Spiel ihnen am besten gefГ¤llt und das meiste GlГјck bringt. Also nicht zГ¶gern, sich anzumelden und die 50 Freispiele bei Zet Casino zu nutzen!
https://zetcasino.one/
На сайте https://moredoram.ru вы найдете дорамы, фильмы, сериалы высокого качества. Они понравятся всем любителям такого жанра и помогут расслабиться после трудового дня и просто получить приятные эмоции. Вы сможете воспользоваться функцией случайной дорамы, изучить список лучших из них. Все они в отличном качестве, с безупречным звуком, что позволит насладиться просмотром на любом устройстве, включая смартфон, ПК, планшет. Регулярно появляются многообещающие новинки, с которыми необходимо ознакомиться и вам.
Если хотите смотреть в отменном качестве сериалы и фильмы онлайн, тогда сервис kinogoby.zone/new будет вам точно полезен. Здесь вы найдете все, что вас интересует. Фильмы хорошие, можете смотреть их совершенно бесплатно, не выходя из собственного дома. https://kinogoby.zone/new отличается от других сайтов тем, что предоставляет доступ к большому количеству фильмов. Создатели портала сделали так, чтобы вам интерфейс был понятен. Расслабьтесь и забудьте обо всем. Выбирайте фильм и смотрите в свое удовольствие!
does tamoxifen cause weight loss tamoxifen cancer tamoxifen bone density
Специализированный магазин, где можно найти много раковина 80см для вашей ванной комнаты.
purchase cytotec: buy cytotec pills – buy cytotec over the counter
Zet Casino ist eine beliebte Online-GlГјcksspielplattform, die eine Vielzahl von Spielen und attraktiven Bonusangeboten fГјr Spieler anbietet. Einer der begehrtesten Boni ist der sogenannte “Bonus bez depozytu”, bei dem Spieler einen Bonus erhalten, ohne eine Einzahlung tГ¤tigen zu mГјssen.
Dieser Bonus ist besonders attraktiv fГјr neue Spieler, die die Plattform testen mГ¶chten, ohne sofort eigenes Geld einzahlen zu mГјssen. Durch den “Bonus bez depozytu” kГ¶nnen Spieler verschiedene Spiele ausprobieren und das Casino kennenlernen, ohne ein finanzielles Risiko einzugehen.
Um den Bonus zu erhalten, müssen sich Spieler in der Regel einfach auf der Plattform registrieren und ihren Account bestätigen. Der Bonus wird dann automatisch gutgeschrieben und kann für unterschiedliche Spiele genutzt werden.
Es ist jedoch wichtig zu beachten, dass jeder Bonus bestimmte Umsatzbedingungen hat, die erfüllt werden müssen, bevor Gewinne ausgezahlt werden können. Diese Bedingungen variieren je nach Plattform und Bonusangebot, daher ist es ratsam, die jeweiligen Geschäftsbedingungen sorgfältig zu lesen.
Insgesamt bietet der “Bonus bez depozytu” eine groГџartige MГ¶glichkeit, das Zet Casino zu erkunden und erste Gewinne zu erzielen, ohne gleich groГџe BetrГ¤ge investieren zu mГјssen. Es lohnt sich also, diese attraktive Bonusoption in Anspruch zu nehmen und die Vielfalt an SpielmГ¶glichkeiten auf der Plattform zu genieГџen.
https://zetcasino.one/
https://ciprofloxacin.tech/# buy ciprofloxacin
http://ciprofloxacin.tech/# ciprofloxacin order online
Visit the website https://prm4u.com/ which is the best SMM Panel with automatic fulfillment of your orders. Low price guarantee with high quality services. Take advantage of an effective online tool for social media marketing and search engine optimization.
VIP транспорт – компания, которая с успехом предлагает услуги пассажироперевозок. У нас имеются: автомобили премиум, бизнес-класса, комфорт, минивэны, вместительные автобусы с разным количеством мест и микроавтобусы. Мы собрали прекрасный коллектив водителей, в них можете быть полностью уверенными. Ищете вип авто такси? Anapa-vip-transport.ru – сайт, где указан номер телефона круглосуточной диспетчерской службы. Также тут представлены документы, ознакомиться с ними можно сейчас. Предлагаем своим клиентам оптимальные условия. Звоните!
Tipico Casino Free Spins
Das Tipico Casino bietet seinen Kunden eine Vielzahl von aufregenden Spielen und lukrativen Angeboten. Eine der begehrtesten Aktionen sind die Tipico Casino Free Spins, die es den Spielern ermöglichen, kostenlos an ausgewählten Spielautomaten zu spielen.
Diese Freispiele sind eine großartige Möglichkeit, neue Slots auszuprobieren, ohne dabei eigenes Geld riskieren zu müssen. Oftmals werden die Free Spins im Rahmen von speziellen Promotionen vergeben oder als Belohnung für treue Spieler. Manchmal sind sie auch Teil von Willkommensangeboten für neue Kunden.
Um die Tipico Casino Free Spins zu erhalten, mГјssen die Spieler bestimmte Bedingungen erfГјllen. Dies kann beispielsweise eine Mindesteinzahlung oder das Spielen einer bestimmten Anzahl von Runden sein. Die genauen Details der Aktionen werden in den jeweiligen Angeboten auf der Tipico Casino Website bekannt gegeben.
Es ist wichtig, die Teilnahmebedingungen für die Free Spins zu lesen und zu verstehen, um Missverständnisse zu vermeiden. Oftmals sind die Gewinne aus den Freispielen an Umsatzbedingungen gebunden, die erfüllt werden müssen, bevor eine Auszahlung möglich ist.
Alles in allem sind die Tipico Casino Free Spins eine tolle Möglichkeit, um das Casino und seine Spiele kostenlos kennenzulernen und dabei auch noch die Chance auf echte Gewinne zu haben. Es lohnt sich daher, regelmäßig die Promotionsseite des Tipico Casinos zu besuchen, um keine der spannenden Aktionen zu verpassen. Viel Spaß und gute Unterhaltung beim Spielen!
https://tipicocasino.one/
buy cytotec online fast delivery Abortion pills online buy cytotec in usa
Ищите повышение квалификации и переподготовку логопедов? Тогда вам необходимо посетить https://logopraktika.ru/ где вы сможете ознакомиться с программами повышения квалификации логопедов по всей России в формате дистанционного обучения. Подробнее на сайте.
На сайте https://runobe.ru почитайте ранобэ онлайн и в отличном качестве. Все они на русском языке, а потому насладиться чтением сможет каждый. Все произведения имеют интересный сюжет, непредсказуемую развязку, а потому понравятся всем без исключения. Выбор японских романов обновляется ежедневно, чтобы вы смогли найти то, что действительно вам нравится. Вы можете ознакомиться сразу с несколькими, чтобы определиться с тем, какие из них вам нравятся больше. Для того чтобы подыскать определенный вариант, необходимо воспользоваться специальным поиском.
lopressor 50mg pills – inderal us adalat 30mg over the counter
Das Zet Casino bietet auch im Jahr 2019 groГџzГјgige Bonusaktionen fГјr Neukunden an. Einer der beliebtesten Bonusangebote ist der sogenannte “No Deposit Bonus”, bei dem neue Spieler einen Bonus erhalten, ohne zuvor eine Einzahlung tГ¤tigen zu mГјssen. Um diesen Bonus zu beanspruchen, mГјssen Spieler lediglich einen speziellen Bonuscode eingeben, der auf der Webseite des Casinos verГ¶ffentlicht wird.
Der No Deposit Bonus beim Zet Casino kann in Form von Freispielen oder Bonusguthaben vergeben werden. Mit den Freispielen können Spieler bestimmte Spielautomaten kostenlos ausprobieren und dabei echte Gewinne erzielen. Das Bonusguthaben hingegen kann für verschiedene Spiele im Casino eingesetzt werden und erhöht somit die Gewinnchancen der Spieler.
Um den No Deposit Bonus zu erhalten, müssen Spieler in der Regel ein neues Konto beim Zet Casino registrieren und den entsprechenden Bonuscode eingeben. Nach erfolgreicher Registrierung wird der Bonus automatisch gutgeschrieben und kann sofort genutzt werden. Es ist jedoch wichtig zu beachten, dass die meisten No Deposit Boni bestimmten Umsatzbedingungen unterliegen, die erfüllt werden müssen, bevor eine Auszahlung der Gewinne möglich ist.
Insgesamt bietet das Zet Casino eine Vielzahl von attraktiven Bonusaktionen für neue und bestehende Spieler an. Der No Deposit Bonus ist eine großartige Möglichkeit, das Casino risikofrei kennenzulernen und dabei echte Gewinne zu erzielen. Spieler sollten jedoch darauf achten, die Bonusbedingungen genau zu lesen, um sicherzustellen, dass sie den Bonus optimal nutzen können.
https://zetcasino.one/
buy cytotec over the counter: buy cytotec over the counter – cytotec buy online usa
На сайте https://noptur.ru/ подберите экскурсии в Санкт-Петербург, а также другие города страны, которые организуются для школьников, учителей, а также родителей. Перед вами огромный выбор программ, которые подходят как для взрослых, так и детей различного возраста. Туры обойдутся недорого. При этом дети получат море приятных, положительных эмоций. В рамках экскурсионной программы вы увидите самые популярные достопримечательности, а при необходимости ее можно скорректировать. Рассчитайте цену прямо сейчас!
What’s up, this weekend is pleasant in support of me, since this occasion i am reading this enormous educational piece of writing here at my residence.
Приветики!
https://diploman-russia.com
https://ciprofloxacin.tech/# buy cipro online
Das Boomerang Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen anbietet und Spielern die Möglichkeit bietet, echtes Geld zu gewinnen. Wie bei den meisten Online-Casinos ist es wichtig zu wissen, wie lange es dauert, bis eine Auszahlung bearbeitet wird.
Die Auszahlungsdauer im Boomerang Casino variiert je nach Zahlungsmethode. In der Regel dauert es zwischen 1-5 Werktagen, bis die Auszahlung bearbeitet wird. Es ist wichtig zu beachten, dass zusätzliche Verifizierungsverfahren durchgeführt werden können, um die Sicherheit der Transaktionen zu gewährleisten. Dies kann die Auszahlungsdauer beeinflussen.
Um die Auszahlungsdauer zu minimieren, sollten Spieler sicherstellen, dass sie alle erforderlichen Dokumente und Informationen bereitstellen, um ihre Identität zu verifizieren. Dies kann den Prozess beschleunigen und sicherstellen, dass die Auszahlung so schnell wie möglich bearbeitet wird.
Zusätzlich bietet das Boomerang Casino eine Vielzahl von Zahlungsmethoden an, darunter Kreditkarten, E-Wallets und Banküberweisungen. Spieler sollten die Zahlungsmethode wählen, die am besten zu ihren Bedürfnissen passt, um ihre Gewinne schnell und einfach zu erhalten.
Insgesamt ist die Auszahlungsdauer im Boomerang Casino relativ schnell und effizient. Spieler können sich darauf verlassen, dass ihre Gewinne zeitnah bearbeitet werden und sie ihr Geld sicher erhalten. Es ist jedoch wichtig, die Verifizierungsverfahren zu beachten und alle erforderlichen Informationen bereitzustellen, um Verzögerungen zu vermeiden.
https://boomerangcasino.one/
ciprofloxacin order online buy cipro online buy cipro cheap
Компания «Сомово» предлагает надежную мебель. Стараемся своим покупателям давать только самое лучшее. Наши спальни все продуманы до мелочей, купить можно их у нас по доступной стоимости и с быстрой доставкой. Вся продукция сертифицирована. Ищете гостиные купить в москве? Somovo-mebel.ru – сайт, где есть возможность найти много уютных вариантов спален. Заботимся о качестве товаров и своей репутации. Делаем все для того, чтобы вы остались довольны выбранным вами приобретением. Советуйте нас своим друзьям и обращайтесь вновь!
hydrochlorothiazide medication – buy zestril 5mg pill order bisoprolol 5mg
Online Casinos sind heutzutage sehr beliebt und bieten eine Vielzahl von Spielen fГјr Spieler aller Art. Eines dieser Online Casinos ist Zet Casino, das eine Vielzahl von Spielen und Boni fГјr seine Spieler bietet.
Zet Casino wurde im Jahr 2018 gegrГјndet und hat sich seitdem zu einer beliebten Online-GlГјcksspielseite entwickelt. Das Casino bietet eine groГџe Auswahl an Spielen, darunter Spielautomaten, Tischspiele, Live-Casino-Spiele und vieles mehr.
Ein großer Vorteil von Zet Casino ist, dass es sowohl auf Desktop- als auch auf mobilen Geräten gespielt werden kann. Dies bedeutet, dass Spieler ihre Lieblingsspiele überall und jederzeit genießen können, solange sie eine Internetverbindung haben.
Das Casino bietet außerdem großzügige Boni und Promotionen für neue und bestehende Spieler an. Dies kann in Form von Einzahlungsboni, Freispielen oder Cashback-Angeboten erfolgen. Spieler können auch am Treueprogramm teilnehmen, um zusätzliche Belohnungen zu erhalten.
Zet Casino verfügt über eine gültige Glücksspiellizenz und verwendet die neueste SSL-Verschlüsselungstechnologie, um die Sicherheit der Spieler zu gewährleisten. Dies bedeutet, dass Spieler ihre persönlichen und finanziellen Informationen ohne Bedenken preisgeben können.
Insgesamt bietet Zet Casino ein unterhaltsames und sicheres Spielerlebnis fГјr alle, die gerne in Online-Casinos spielen. Mit einer groГџen Spielauswahl, groГџzГјgigen Boni und einer benutzerfreundlichen Plattform ist Zet Casino definitiv einen Besuch wert.
https://zetcasino.one/
Русский форум Испании – всё о возможностях для переезда в Испанию из России: https://costaspain.net/viewforum.php?f=66 где обсуждаются бюджетные варианты по учебной визе, визе цифрового кочевника, цены на продукты и проживание, недвижимость, работа в Испании для россиян, обустройство детей в школы, варианты переезда без визы и денег. Также на форуме всегда есть последние новости Испании, красивые фотографии природы и пляжей Испании.
На сайте https://mangaed.ru/ в большом выборе представлены захватывающие, увлекательные комиксы манга, которые вы сможете читать абсолютно бесплатно и в любое время. Все они отличаются непредсказуемым, ярким сюжетом, сопровождаются интересными картинками, которые точно принесут положительные эмоции и помогут вам получить отличное настроение. Все поклонники жанра с нетерпением ожидают новых глав, которые выходят регулярно. Все самые лучшие, интересные и яркие комиксы находятся только на этом сайте, который регулярно радует пользователей.
cost generic propecia: order generic propecia without prescription – get generic propecia prices
order hydrochlorothiazide 25 mg for sale – buy zebeta 5mg generic buy zebeta online cheap
Zet Casino AskGamblers
Das Zet Casino ist eine beliebte Online-Glücksspielseite, die eine Vielzahl von Spielen für Spieler aus der ganzen Welt anbietet. Eine der besten Möglichkeiten, um sich über die Qualität eines Online-Casinos zu informieren, ist die Bewertung auf der Website AskGamblers. Hier haben Nutzer die Möglichkeit, ihre Erfahrungen und Meinungen zu teilen, um anderen bei der Entscheidung zu helfen, ob sie sich bei einem bestimmten Casino anmelden sollen oder nicht.
Das Zet Casino hat auf AskGamblers eine beeindruckende Bewertung von 4 von 5 Sternen erhalten und wird von vielen Spielern hoch gelobt. Die Benutzer loben insbesondere die große Auswahl an Spielen, die benutzerfreundliche Website und den exzellenten Kundenservice. Viele Spieler schätzen auch die schnellen Auszahlungen und die Vielzahl von Zahlungsoptionen, die das Zet Casino anbietet.
Ein weiterer Pluspunkt des Zet Casinos ist das attraktive Bonusprogramm für Neukunden und treue Spieler. Es gibt regelmäßige Bonusangebote, Freispiele und Turniere, die den Spielern zusätzliche Gewinnchancen bieten. Die Boni sind fair und transparent, ohne versteckte Bedingungen, was bei Spielern gut ankommt.
Insgesamt ist das Zet Casino eine hervorragende Wahl für Glücksspielfans, die eine sichere und unterhaltsame Online-Spielerfahrung suchen. Mit einer breiten Palette von Spielen, großzügigen Boni und einem zuvorkommenden Kundenservice bietet das Zet Casino alles, was man sich von einem erstklassigen Online-Casino wünscht. Wer also auf der Suche nach einem zuverlässigen und spaßigen Casino ist, sollte das Zet Casino auf jeden Fall in Betracht ziehen.
https://zetcasino.one/
lopressor 100mg over the counter – buy metoprolol online cheap nifedipine 10mg us
https://nolvadex.life/# raloxifene vs tamoxifen
Your articles have been a valuable rise of word on this field, sparking multifarious interesting ideas. Acknowledge gratitude you representing sharing such insightful purport!
https://sites.google.com/view/mazyagames/
buy cipro ciprofloxacin mail online ciprofloxacin mail online
Желаете провести отпуск в Кисловодске, который вы не забудете? Тогда вам стоит предварительно забронировать жилье. Сделайте это прямо сегодня и получите удовольствие от отдыха. Выбирайте тот отель, который подходит вам по цене и расположению. Ищете забронировать отель в Кисловодске? Kislovodsk-oteli.ru – сайт, где есть вся актуальная информация. Мы поможем вам отыскать идеальный вариант. У нас вы узнаете, где лучше забронировать номер. Отель Goldyssun вам точно понравится. Он гарантирует безупречный уровень сервиса. Уверены, что вам он точно подойдет!
Zet Casino Einzahlungsbonus
Zet Casino ist eine beliebte Online-Glücksspielplattform, die eine Vielzahl von Spielen und attraktiven Boni für ihre Spieler anbietet. Einer der beliebtesten Boni auf der Website ist der Einzahlungsbonus, der neuen Spielern angeboten wird, die sich zum ersten Mal auf der Plattform registrieren und eine Einzahlung tätigen.
Der Zet Casino Einzahlungsbonus ist eine großartige Möglichkeit für Spieler, ihr Spielkonto aufzustocken und mehr Zeit mit ihren Lieblingsspielen zu verbringen. Der Bonus variiert je nach Höhe der Einzahlung und kann bis zu einem bestimmten Betrag erhöht werden, was es den Spielern ermöglicht, mehr zu gewinnen und ihre Gewinnchancen zu erhöhen.
Um den Einzahlungsbonus zu erhalten, müssen die Spieler lediglich eine Einzahlung auf ihr Konto vornehmen und den Bonuscode angeben, der auf der Website bereitgestellt wird. Sobald die Einzahlung bestätigt wurde, wird der Bonus automatisch gutgeschrieben und kann sofort für Spiele auf der Plattform verwendet werden.
Es ist wichtig zu beachten, dass der Einzahlungsbonus bestimmten Bedingungen und Anforderungen unterliegt, die von den Spielern erfüllt werden müssen, um den Bonus und damit verbundene Gewinne abheben zu können. Diese Bedingungen können von der Höhe der Einzahlung bis zu den Umsatzanforderungen für den Bonus reichen.
Insgesamt ist der Zet Casino Einzahlungsbonus eine großartige Möglichkeit für Spieler, mehr aus ihrer Online-Glücksspielerfahrung herauszuholen und ihre Gewinnchancen zu erhöhen. Mit einer Vielzahl von Spielen und attraktiven Boni ist Zet Casino eine der besten Optionen für Spieler, die auf der Suche nach einem unterhaltsamen und lukrativen Casinoerlebnis sind.
https://zetcasino.one/
http://lisinopril.network/# zestril 10 mg price
9 Signs That You’re The Pornstar Expert top 10 Pornstars
Potent Hyperlinks in Blogs and Comments: Boost Your SEO
Backlinks are crucial for boosting search engine rankings and increasing website presence. By incorporating links into blogs and comments prudently, they can significantly increase targeted traffic and SEO performance.
Adhering to Search Engine Algorithms
Today’s backlink placement strategies are finely tuned to align with search engine algorithms, which now prioritize website link quality and relevance. This assures that hyperlinks are not just abundant but significant, directing consumers to useful and pertinent content material. Website owners should focus on integrating backlinks that are situationally suitable and improve the overall articles quality.
Rewards of Utilizing Clean Donor Bases
Utilizing up-to-date donor bases for links, like those maintained by Alex, provides substantial advantages. These bases are often renewed and comprise of unmoderated sites that don’t pull in complaints, guaranteeing the links positioned are both impactful and certified. This approach will help in keeping the efficacy of backlinks without the dangers connected with moderated or troublesome assets.
Only Sanctioned Sources
All donor sites used are sanctioned, avoiding legal pitfalls and adhering to digital marketing requirements. This dedication to using only approved resources assures that each backlink is genuine and trustworthy, thereby building credibility and reliability in your digital presence.
SEO Impact
Skillfully put backlinks in blogs and remarks provide over just SEO rewards—they enhance user experience by connecting to pertinent and top quality articles. This technique not only satisfies search engine requirements but also engages consumers, leading to much better targeted traffic and improved online involvement.
In essence, the right backlink technique, especially one that employs clean and trustworthy donor bases like Alex’s, can change your SEO efforts. By concentrating on good quality over volume and adhering to the most recent requirements, you can guarantee your backlinks are both potent and effective.
кредит льготный на развитие бизнеса
Tipico Sport zu Casino – Zwei verschiedene Welten vereint
In der Welt des GlГјcksspiels gibt es eine Vielzahl von Anbietern, die sowohl Sportwetten als auch Casino-Spiele anbieten. Einer dieser Anbieter ist Tipico, der sowohl ein Sportwettenanbieter als auch ein Online-Casino ist. Doch wie gut funktioniert die Kombination von Sport und Casino auf einer Plattform?
Sportwetten sind seit langem eine beliebte Form des Glücksspiels, bei der Wetten auf verschiedene sportliche Ereignisse abgeschlossen werden. Tipico ist einer der führenden Anbieter von Sportwetten in Deutschland und bietet eine breite Palette von Sportarten und Wettmöglichkeiten an. Von Fußball über Tennis bis hin zu E-Sports, bei Tipico finden Sportfans alles, was das Herz begehrt.
Aber Tipico bietet nicht nur Sportwetten an, sondern auch ein umfangreiches Online-Casino. Hier können Spieler aus einer Vielzahl von Casino-Spielen wie Spielautomaten, Roulette, Blackjack und vielem mehr wählen. Das Casino-Angebot von Tipico ist gut ausgestattet und bietet den Spielern ein authentisches Casino-Erlebnis, ohne das Haus verlassen zu müssen.
Die Kombination von Sportwetten und Casino-Spielen auf einer Plattform kann für Spieler eine interessante Option sein. Sie können sowohl auf ihre Lieblingssportarten wetten als auch zwischendurch einige Runden an Spielautomaten drehen oder Blackjack spielen. So kommt garantiert keine Langeweile auf und für jeden Geschmack ist etwas dabei.
Darüber hinaus bietet Tipico seinen Kunden attraktive Bonusaktionen sowohl für Sportwetten als auch für Casino-Spiele an. Neue Spieler können sich über Willkommensboni freuen und regelmäßige Aktionen sorgen für zusätzliche Spannung und Gewinnchancen.
Insgesamt kann die Kombination von Tipico Sport und Casino auf einer Plattform durchaus Гјberzeugen. FГјr Sportfans, die auch gerne mal eine Runde im Online-Casino spielen, ist Tipico eine gute Wahl. Mit einer breiten Auswahl an Sportwetten und Casino-Spielen sowie attraktiven Bonusaktionen bietet Tipico ein rundum gelungenes GlГјcksspiel-Erlebnis fГјr seine Kunden.
https://tipicocasino.one/
cost of propecia tablets: generic propecia without insurance – cost of cheap propecia tablets
На сайте https://turk-kino.ru посмотрите интересное и запоминающееся турецкое кино вместе с другом. Есть такие именитые картины, как «Запах клубники», «Зимородок», «Великолепный век» и многое другое. Для того чтобы начать совместный просмотр, необходимо создать комнату. Сделать это получится в 3 шага, а инструкция прилагается. Перед вами многообещающие новинки, а также топ лучших фильмов за 2024 год. Во всех фильмах играют ваши любимые актеры, звучит приятная музыка. Есть подборка рекомендованных фильмов, которые выбирают многие.
Сайт v8corp.ru предоставляет виды услуг по цифровизации и автоматизации процессов с применением программ 1С. Сотрудничая с нами, вы сосредоточитесь на собственном бизнесе, мы в 24 отраслях экономики разбираемся. https://v8corp.ru/ – сайт, где можете подробнее ознакомиться с конфигурациями 1С. Тарифы у нас гибкие. Подберем для вас лучшую конфигурацию продуктов 1С, которые подходят под вашу компанию. Оцените открывающиеся достоинства облачной Аренды 1С. Готовы быть вашим надежным помощником. Обращайтесь и получите консультацию!
order lisinopril online us lisinopril 5 mg daily price of lisinopril 30 mg
http://cytotec.club/# Abortion pills online
What’s The Job Market For Local SEO Services Professionals?
local seo service [https://te.legra.ph/17-Signs-That-You-Work-With-Professional-SEO-Services-08-14]
Zet Casino Promo Code 2021
Das Zet Casino ist eines der beliebtesten Online-Casinos unter Spielern auf der ganzen Welt. Mit einer Vielzahl von Spielen, groГџzГјgigen Boni und aufregenden Aktionen, gibt es immer einen guten Grund, dem Zet Casino einen Besuch abzustatten.
Für das Jahr 2021 hat das Zet Casino einige spannende Promo-Codes und Bonusangebote im Angebot. Diese Codes können dazu beitragen, das Spielerlebnis noch unterhaltsamer und lukrativer zu gestalten.
Einer der beliebtesten Promo-Codes, der derzeit im Zet Casino gГјltig ist, ist der Code “ZETBONUS”. Mit diesem Code erhalten Spieler einen groГџzГјgigen Willkommensbonus bei ihrer ersten Einzahlung. Dieser Bonus kann verwendet werden, um eine Vielzahl von Spielen im Casino zu genieГџen und die Gewinnchancen zu erhГ¶hen.
DarГјber hinaus gibt es noch viele weitere Promo-Codes und Aktionen im Zet Casino, die das Spielerlebnis verbessern kГ¶nnen. Egal ob Freispiele, Cashback-Angebote oder Einzahlungsboni – es lohnt sich immer, einen Blick auf die aktuellen Promotions des Casinos zu werfen.
Um den Promo-Code zu verwenden, müssen Spieler einfach während der Einzahlung den entsprechenden Code eingeben. Der Bonus wird dann automatisch gutgeschrieben und kann sofort genutzt werden.
Das Zet Casino ist bekannt für seine fairen Bedingungen und transparenten Bonusangebote. Spieler können sich also sicher sein, dass sie gute Gewinnchancen haben und ihre Gewinne ohne Probleme auszahlen lassen können.
Insgesamt ist der Promo-Code 2021 im Zet Casino eine großartige Möglichkeit, das Spielerlebnis zu verbessern und noch mehr Spaß und Spannung zu erleben. Wer also auf der Suche nach einem erstklassigen Online-Casino ist, sollte das Zet Casino definitiv in Betracht ziehen. Viel Glück beim Spielen!
https://zetcasino.one/
Оригинальные запасные части и расходные материалы для лабораторного оборудования. https://parts-lab.ru/ – прямые поставки запасных частей и лабораторных приборов в Россию. Работаем напрямую с ведущими производителями: Thermo Fisher Scientific, Agilent, SPECTRO, Dionex. Поставляем колонки газовой хроматографии, капиллярные колонки, расходники для хроматографии, диффузионные насосы, так же запчасти для приборов ионной хроматографии и для элементного анализа. Все для бесперебойной работы вашей лаборатории.
Boomerang Bet Casino: Das ultimative Spielerlebnis
Boomerang Bet Casino ist eine aufregende Online-GlГјcksspielplattform, die Spielern ein ultimatives Spielerlebnis bietet. Mit einer breiten Palette von Spielen, groГџzГјgigen Boni und einem erstklassigen Kundenservice ist Boomerang Bet Casino die perfekte Wahl fГјr Spieler, die nach Nervenkitzel und Spannung suchen.
Eines der Hauptmerkmale von Boomerang Bet Casino ist die Vielzahl von Spielen, die es seinen Spielern bietet. Von klassischen Tischspielen wie Blackjack und Roulette bis hin zu aufregenden Spielautomaten und Live-Dealer-Spielen gibt es für jeden Geschmack etwas zu entdecken. Die hochwertige Software sorgt für ein reibungsloses Spielerlebnis und eine realistische Casinoatmosphäre.
Darüber hinaus belohnt Boomerang Bet Casino seine Spieler mit großzügigen Boni und Promotionen. Neue Spieler erhalten oft Willkommensboni, die ihnen zusätzliches Guthaben oder Freispiele verschaffen. Darüber hinaus gibt es regelmäßig Aktionen und Sonderangebote, die den Spielern die Möglichkeit bieten, noch mehr zu gewinnen.
Neben der großen Auswahl an Spielen und den großzügigen Boni bietet Boomerang Bet Casino auch einen erstklassigen Kundenservice. Das freundliche und kompetente Support-Team steht rund um die Uhr zur Verfügung, um Fragen zu beantworten und Probleme zu lösen. Spieler können sich darauf verlassen, dass sie bei Boomerang Bet Casino die Unterstützung erhalten, die sie benötigen.
Insgesamt ist Boomerang Bet Casino ein erstklassiges Online-GlГјcksspielziel, das Spielern ein unvergessliches Spielerlebnis bietet. Mit einer breiten Palette von Spielen, groГџzГјgigen Boni und einem erstklassigen Kundenservice ist es leicht zu erkennen, warum so viele Spieler sich fГјr Boomerang Bet Casino entscheiden. Besuchen Sie noch heute die Website und erleben Sie selbst die Spannung und den Nervenkitzel, den dieses erstklassige Casino zu bieten hat.
https://boomerangcasino.one/
На сайте https://tdalmaz.ru/ вы сможете заказать качественное, профессиональное оборудование, которое используется для того, чтобы выполнить алмазную обработку бетона. Предприятие зарекомендовало себя в качестве надежного поставщика техники от известных брендов. Важно то, что ассортимент регулярно обновляется, чтобы предоставить вам лучшие решения на выбор. Дополнительно здесь можно заказать и ремонт установок, предназначенных для алмазного бурения. Организуется отправка товара по России.
На сайте https://smsak.org/ вы сможете ознакомиться с топом лучших магазинов аккаунтов. Также есть возможность воспользоваться такой услугой, как платная аренда номеров. Для того чтобы протестировать сервис, доступен бесплатный прием смс. Также вы сможете ознакомиться и с такой информацией, как для чего нужна смс-активация и что представляет собой данная услуга. При этом специально для вас действуют небольшие и привлекательные расценки. Сервис является полностью автоматизированным, а потому услуга будет оказана максимально оперативно.
Distilling hard to understand concepts into readable content, or what I like to call, a miracle.
order propecia tablets: order cheap propecia pill – cost of generic propecia without insurance
lisinopril average cost lisinopril 20 mg tablet cost lisinopril 5 mg tablet cost
На сайте https://klinikaflorovoi.ru/ запишитесь онлайн, чтобы воспользоваться услугами женской консультации. В компании работают компетентные, узкопрофильные специалисты, которые знают, как справиться даже с самым сложным случаем. Ведущие эксперты клиники отличаются огромным стажем, а потому знают, как решить проблему клиентки. Они используют уникальные и новаторские технологии, высокотехнологичное оборудование для того, чтобы правильно выполнить диагностику и назначить правильное лечение. Вам предложат услуги гинеколога, ведение беременности, УЗИ и многое другое.
Das tipico Casino gehört zu den bekanntesten Online-Casinos in Deutschland. Doch was, wenn man Fragen oder Probleme hat? In diesem Fall ist es wichtig, den richtigen Kontakt zum tipico Casino zu finden.
Das tipico Casino bietet verschiedene Möglichkeiten, um mit dem Kundenservice in Kontakt zu treten. Eine Möglichkeit ist der Live-Chat, der auf der Webseite verfügbar ist. Hier kann man direkt mit einem Mitarbeiter chatten und Fragen stellen. Der Live-Chat ist in der Regel schnell und unkompliziert und eignet sich gut, um Probleme schnell zu lösen.
Eine weitere Möglichkeit, um Kontakt zum tipico Casino aufzunehmen, ist die telefonische Hotline. Über die Hotline kann man ebenfalls Fragen stellen oder Probleme melden. Die Mitarbeiter sind in der Regel freundlich und kompetent und stehen den Kunden mit Rat und Tat zur Seite.
FГјr schriftliche Anfragen bietet das tipico Casino zudem ein Kontaktformular auf der Webseite an. Hier kann man sein Anliegen formulieren und bekommt in der Regel innerhalb kurzer Zeit eine Antwort.
Insgesamt bietet das tipico Casino also verschiedene Möglichkeiten, um mit dem Kundenservice in Kontakt zu treten. Ob per Live-Chat, telefonischer Hotline oder Kontaktformular – für jedes Anliegen gibt es die passende Kontaktmöglichkeit. Somit steht dem Spielspaß im tipico Casino nichts im Wege.
https://tipicocasino.one/
10 Things You’ve Learned In Kindergarden That’ll Help You With Backlink Software Software To Find Dofollow Backlinks
http://lisinopril.network/# lisinopril 5 mg daily
cialis precio
It’s Time To Forget Repair Upvc Windows: 10 Reasons Why You No Longer
Need It window replacement Near me
10 Times You’ll Have To Be Educated About Double Glazing Fitters Near Me double Glazing fitters
9 Lessons Your Parents Taught You About Keys For Mercedes Keys for mercedes
Tipico – Geld von Casino auf Sportwetten
Tipico ist eine der beliebtesten Sportwetten-Plattformen in Deutschland. Neben Sportwetten bietet das Unternehmen auch ein Online-Casino an, in dem Spieler ihr Glück an Spielautomaten, Roulette und anderen Casino-Spielen versuchen können.
Eine häufige Frage, die Spieler haben, ist, ob sie Geld von ihrem Casino-Konto auf ihr Sportwetten-Konto übertragen können. Die gute Nachricht ist, dass dies bei Tipico möglich ist. Spieler können ganz einfach Geld von ihrem Casino-Konto auf ihr Sportwetten-Konto transferieren, um ihre Lieblings-Sportwetten zu platzieren.
Um Geld von Ihrem Casino-Konto auf Ihr Sportwetten-Konto zu Гјbertragen, mГјssen Sie sich zunГ¤chst auf der Tipico-Website oder in der Tipico-App einloggen. Gehen Sie dann zu Ihrem Casino-Konto und wГ¤hlen Sie die Option “Geld transferieren”. Geben Sie den Betrag ein, den Sie auf Ihr Sportwetten-Konto Гјbertragen mГ¶chten, und bestГ¤tigen Sie die Transaktion.
Es ist wichtig zu beachten, dass möglicherweise bestimmte Bedingungen für die Übertragung von Geld zwischen den verschiedenen Konten gelten können. Stellen Sie sicher, dass Sie die Nutzungsbedingungen von Tipico lesen, um sicherzustellen, dass Sie alle Regeln und Bestimmungen einhalten.
Insgesamt bietet Tipico seinen Spielern eine bequeme und benutzerfreundliche Möglichkeit, Geld zwischen Casino- und Sportwetten-Konten zu transferieren. So können Spieler leicht zwischen verschiedenen Glücksspielangeboten wechseln und ihr Spielerlebnis maximieren.
Ob Sie Ihre Lieblingssportart live verfolgen oder lieber an Spielautomaten spielen, bei Tipico finden Sie sicherlich das passende Angebot. Nutzen Sie die Möglichkeit, Geld von Ihrem Casino-Konto auf Ihr Sportwetten-Konto zu übertragen und genießen Sie die Vielfalt an Glücksspielmöglichkeiten, die Tipico zu bieten hat. Viel Glück beim Wetten!
https://tipicocasino.one/
проверить свои usdt на чистоту
Проверка бумажников на выявление подозрительных денег: Защита личного цифрового финансового портфеля
В мире электронных денег становится все более необходимее соблюдать безопасность своих финансов. Каждый день кибермошенники и хакеры разрабатывают свежие подходы обмана и мошенничества и угонов виртуальных денег. Один из важных инструментов защиты является проверка кошельков для хранения криптовалюты по присутствие незаконных средств передвижения.
Из-за чего так важно проверить личные электронные кошельки для хранения криптовалюты?
Прежде всего данный факт нужно для охраны личных средств. Многие из люди, вкладывающие деньги находятся в зоне риска потери своих денег в результате несправедливых методов или краж. Проверка бумажников способствует выявить вовремя подозрительные операции и предотвратить.
Что предлагает вашему вниманию компания?
Мы предлагаем услугу проверки данных электронных кошельков и переводов с намерением обнаружения происхождения средств передвижения и дать детального отчета о проверке. Наша система проанализировать информацию для обнаружения потенциально нелегальных операций средств и оценить риск для того чтобы своего портфеля активов. Благодаря нашей службе проверки, вы будете в состоянии предотвратить возможные проблемы с государственными органами и защитить от случайной вовлеченности в незаконных действий.
Как осуществляется процесс проверки?
Наши фирма-разработчик взаимодействует с авторитетными аудиторскими организациями организациями, такими как Halborn, чтобы обеспечить гарантированность и правильность наших проверок. Мы внедряем современные технологии и методики проверки данных для выявления подозрительных действий. Персональные сведения наших клиентов обрабатываются и сохраняются в соответствии высокими стандартами.
Основная просьба: “проверить свои USDT на чистоту”
В случае если вы хотите убедиться в безопасности и чистоте личных кошельков USDT, наши специалисты предоставляет шанс бесплатную проверку первых пяти кошельков. Просто введите адрес своего кошелька в соответствующее окно на нашем онлайн-ресурсе, и мы дадим вам подробные сведения о состоянии вашего счета.
Обезопасьте свои деньги сразу же!
Не рискуйте оказаться в пострадать от хакеров или стать неприятном положении нелегальных действий с вашими собственными финансами. Дайте вашу криптовалюту профессионалам, которые смогут помочь, вам и вашему бизнесу защитить свои деньги и избежать. Совершите первый шаг безопасности вашего криптовалютного финансового портфеля сразу же!
Витебский госуниверситет университет П. М. Машерова – ведущий образовательный, научный и культурный центр Витебской области. Официальный сайт ВГУ Машерова https://vsu.by новости университета, ВГУ в СМИ, подготовительные курсы Беларусь, выпускники ВГУ Машерова Витебск, международные партнёры. Университет Машерова осуществляет подготовку по предметам: химия, биология, история, физика, программирование, педагогика, психология, математика. Vitebsk State University named P.M. Masherov.
What Can A Weekly Injury Lawyer Project Can Change Your Life Injury attorneys
На сайте https://auto-arenda-anapa.ru/ вам предлагается доступная услуга по прокату авто. Широкий выбор автомобилей даст возможность прямо из окна насладиться комфортами Анапы. Если вы любите путешествовать, лучшим решением будет аренда авто без водителя. Вы можете свободно перемещаться по местности и не зависеть от какого-либо транспорта. Все автомобили проходят техническое обслуживание. Чтобы взять авто напрокат, выберите модель на портале и свяжитесь по телефону с диспетчером. Вам понравится сервис с привлекательными ценами и без ограничений по пробегу.
http://finasteride.store/# propecia online
Бюро переводов Рокетперевод https://rocketperevod.ru/ в Москве это агентство по переводу текстов и документов. Услуги по профессиональному переводу разных видов документов, таких как с нотариальным заверением, апостилем и консульской легализацией и других. Зайдите на сайт – узнайте стоимость и все преимущества нашей компании.
tamoxifen for gynecomastia reviews tamoxifen bone density tamoxifen joint pain
See What Gotogel Link Alternatif Tricks The Celebs Are Making Use Of Gotogel Link Alternatif
Zet Casino Einzahlungsbonus
Zet Casino ist ein Online-Casino, das seinen Spielern eine Vielzahl von aufregenden Spielen und lukrativen Boni bietet. Einer der beliebtesten Boni, die das Casino seinen Spielern anbietet, ist der Einzahlungsbonus.
Der Einzahlungsbonus bei Zet Casino ist eine großartige Möglichkeit für Spieler, ihr Spiel zu maximieren und ihre Gewinnchancen zu erhöhen. Um den Einzahlungsbonus zu erhalten, müssen Spieler einfach eine Einzahlung auf ihr Konto tätigen und den entsprechenden Bonuscode eingeben, um den Bonus zu aktivieren.
Der Einzahlungsbonus bei Zet Casino variiert je nach Höhe der Einzahlung. Je mehr Spieler einzahlen, desto größer ist der Bonus, den sie erhalten. Der Bonus kann in Form von zusätzlichem Spielgeld, Freispielen oder anderen attraktiven Angeboten angeboten werden.
Der Einzahlungsbonus bei Zet Casino ist eine großartige Möglichkeit für Spieler, ihre Bankroll zu erhöhen und mehr Spaß und Spannung aus ihrem Spiel herauszuholen. Spieler können den Bonus nutzen, um ihre Lieblingsspiele zu spielen und dabei die Chance auf große Gewinne zu haben.
Um den Einzahlungsbonus bei Zet Casino zu erhalten, müssen Spieler die Bedingungen und Konditionen beachten, die mit dem Bonus verbunden sind. Es ist wichtig, die Umsatzanforderungen zu erfüllen und sicherzustellen, dass sie die Bonusbedingungen vollständig verstehen, um den Bonus erfolgreich freizuschalten.
Insgesamt ist der Einzahlungsbonus bei Zet Casino eine großartige Möglichkeit für Spieler, ihre Gewinnchancen zu maximieren und das Beste aus ihrem Online-Casino-Erlebnis herauszuholen. Mit attraktiven Boni und spannenden Spielen ist Zet Casino definitiv eine der besten Optionen für Online-Casino-Spieler.
https://zetcasino.one/
A Guide To Nespresso Machine From Start To Finish white Nespresso machines
dcis tamoxifen: tamoxifen buy – tamoxifen generic
How Much Do Double Glazing Repairs Near Me Experts Make?
Double glazing Replacement
Осмотр Тетер на прозрачность: Как защитить личные цифровые средства
Все более пользователей обращают внимание к надежность их криптовалютных средств. Ежедневно мошенники придумывают новые схемы кражи цифровых средств, и также держатели электронной валюты становятся жертвами их интриг. Один способов защиты становится проверка кошельков на наличие незаконных средств.
Зачем это необходимо?
Прежде всего, чтобы защитить свои средства от дельцов и похищенных монет. Многие участники встречаются с риском потери своих финансов в результате обманных сценариев или краж. Проверка кошельков позволяет выявить непрозрачные операции или предотвратить возможные убытки.
Что мы предоставляем?
Наша компания предлагаем подход проверки криптовалютных кошельков и также транзакций для выявления источника средств. Наша система анализирует данные для обнаружения противозаконных транзакций и оценки угрозы для вашего портфеля. За счет этой проверке, вы сможете избежать проблем с регулированием и также защитить себя от участия в нелегальных операциях.
Как это работает?
Наша фирма сотрудничаем с первоклассными аудиторскими компаниями, например Halborn, чтобы предоставить точность наших проверок. Мы применяем современные технологии для выявления потенциально опасных транзакций. Ваши информация обрабатываются и сохраняются в соответствии с высокими нормами безопасности и приватности.
Как проверить свои USDT для чистоту?
Если хотите проверить, что ваши Tether-кошельки чисты, наш сервис предлагает бесплатное тестирование первых пяти бумажников. Легко передайте местоположение вашего кошелька на на нашем веб-сайте, или наш сервис предоставим вам детальный отчет о его статусе.
Защитите ваши активы прямо сейчас!
Не подвергайте риску попасть в жертву дельцов или оказаться в неблагоприятную обстановку из-за противозаконных сделок. Свяжитесь с нам, чтобы сохранить ваши электронные средства и избежать проблем. Сделайте первый шаг к сохранности криптовалютного портфеля прямо сейчас!
На сайте https://baseus1.ru/ вы сможете приобрести высокотехнологичные, функциональные гаджеты, а также аксессуары к телефонам и многое другое. В каталоге вы найдете кабели для телефонов, автомобильные держатели, зарядные устройства, а также моноподы, защитные стекла, портативные аккумуляторы, микрофоны, колонки. Вся продукция высокого, эталонного качества, а потому точно прослужит долго. Она абсолютно безопасная и надежная. Регулярное пополнение ассортимента. Вся продукция реализуется по доступной стоимости.
A Productive Rant About Futon For Sale 3 Seater sofa sale
http://finasteride.store/# get cheap propecia without a prescription
Tipico Casino Desktop bietet die perfekte Möglichkeit, um die aufregende Welt des Online-Glücksspiels in vollem Umfang zu erleben. Mit einer Vielzahl von spannenden Spielen und attraktiven Bonusangeboten ist das Tipico Casino Desktop eine beliebte Wahl für Spieler auf der ganzen Welt.
Das Tipico Casino Desktop bietet eine benutzerfreundliche Oberfläche, die es einfach macht, die Lieblingsspiele zu finden und zu spielen. Mit einer Vielzahl von Spielautomaten, Tischspielen und Live-Dealer-Spielen gibt es für jeden Geschmack etwas zu entdecken. Die Spiele werden von führenden Softwareanbietern wie NetEnt, Microgaming und Evolution Gaming bereitgestellt, was für eine hochwertige Spielerfahrung sorgt.
Ein weiteres Highlight des Tipico Casino Desktop sind die großzügigen Bonusangebote für neue und bestehende Spieler. Von Willkommensboni über wöchentliche Aktionen bis hin zu Treueprogrammen gibt es immer wieder spannende Promotionen, die das Spielerlebnis noch aufregender machen.
Das Tipico Casino Desktop bietet auch eine sichere und zuverlässige Spielumgebung, die durch eine Lizenz der Malta Gaming Authority reguliert wird. Dies bedeutet, dass Spieler sicher sein können, dass ihre persönlichen Daten geschützt sind und dass die Spiele fair und transparent sind.
Insgesamt bietet das Tipico Casino Desktop eine erstklassige Glücksspielerfahrung für Spieler, die die Spannung und Aufregung von Online-Casinospielen genießen möchten. Mit einer Vielzahl von Spielen, großzügigen Bonusangeboten und einer sicheren Spielumgebung ist das Tipico Casino Desktop definitiv einen Besuch wert.
https://tipicocasino.one/
Why Is Everyone Talking About Beko A Washing Machine
Right Now
Хотите настроение себе поднять? В этом вам поможет Фаномания. Здесь представлено множество смешных мемов, забавных демотиваторов и улетных анекдотов на разные темы. Начинайте каждый день с ознакомления веселых картинок. Ищете смехотворные ситуации? Funomania.ru – это место, где сможете посмеяться и отвлечься от повседневных забот. Вы узнаете, чем занимался в жизни Мендельсон, какое существо считается зубастым в мире, почему вредно питаться одним Фастфудом. Также здесь есть новая подборка фото сексуальных красоток. Смотрите и наслаждайтесь!
Интернет-ресурс, где можно купить элегантные мебельные раковины 100 см от ведущих производителей.
One Of The Most Untrue Advices We’ve Ever Seen About Upvc Window Repairs Upvc Window Repairs window repairs near me; Nicholas,
A gift for explaining things, making the rest of us look bad.
Five Killer Quora Answers To Audi A3 Keys Audi a3 Keys
Как убедиться в чистоте USDT
Проверка кошельков кошелька за выявление наличия нелегальных средств передвижения: Охрана своего электронного финансового портфеля
В мире цифровых валют становится все необходимее гарантировать секретность личных финансовых активов. Постоянно кибермошенники и киберпреступники выработывают совершенно новые способы обмана и воровства электронных финансов. Одним из основных инструментов обеспечения безопасности является проверка кошельков кошелька по присутствие нелегальных средств передвижения.
По какой причине вот важно провести проверку свои цифровые кошельки?
В первую очередь, вот этот момент необходимо для того, чтобы охраны собственных финансовых средств. Многие пользователи сталкиваются с риском потери средств их финансов в результате несправедливых планов или угонов. Анализ кошельков для хранения криптовалюты способствует выявить вовремя подозрительные манипуляции и предотвратить возможные убытки.
Что предлагает вашему вниманию наша фирма?
Мы предлагаем сервис проверки анализа цифровых бумажников и переводов с целью обнаружения происхождения средств и выдачи детального отчета о результатах. Наша программа анализирует данные пользователя для идентификации незаконных действий и оценить риск для того, чтобы вашего криптовалютного портфеля. Благодаря нашему анализу, вы будете в состоянии предотвратить возможные с органами контроля и защитить себя от непреднамеренного вовлечения в незаконных операций.
Как проводится проверка?
Компания наша организация сотрудничает с крупными аудиторскими фирмами агентствами, как например Kudelsky Security, для того, чтобы обеспечить и адекватность наших проверок кошельков. Мы применяем современные технологии и методы анализа данных для обнаружения небезопасных манипуляций. Персональные данные наших граждан обрабатываются и сохраняются в соответствии с положениями высокими требованиями.
Основная просьба: “проверить свои USDT на чистоту”
Если вы хотите убедиться безопасности собственных кошельков USDT, наши профессионалы оказывает возможность бесплатную проверку наших специалистов первых пяти кошельков. Просто введите адрес своего кошелька в соответствующее поле на нашем веб-сайте, и мы дадим вам подробные сведения о статусе вашего кошелька.
Обезопасьте свои активы сразу же!
Не подвергайте себя риску оказаться пострадать от криминальных элементов или оказаться неприятном положении неправомерных операций средств с вашими собственными финансовыми средствами. Доверьте свои финансы профессионалам, которые окажут поддержку, вам обезопасить деньги и предотвратить возможные. Совершите первый шаг безопасности личного криптовалютного финансового портфеля уже сегодня!
чистый usdt
Осмотр USDT в прозрачность: Как обезопасить свои криптовалютные финансы
Постоянно все больше индивидуумов обращают внимание на безопасность личных электронных активов. Ежедневно мошенники предлагают новые способы кражи цифровых средств, и также держатели криптовалюты становятся страдающими их подстав. Один методов обеспечения безопасности становится проверка кошельков в присутствие незаконных финансов.
Для чего это полезно?
Прежде всего, чтобы обезопасить личные финансы от дельцов или украденных денег. Многие участники встречаются с потенциальной угрозой утраты своих финансов из-за мошеннических сценариев либо грабежей. Проверка бумажников способствует определить непрозрачные операции а также предотвратить возможные убытки.
Что мы предоставляем?
Мы предлагаем сервис проверки цифровых кошельков и операций для выявления источника средств. Наша система проверяет информацию для выявления нелегальных операций а также оценки опасности для вашего портфеля. Благодаря этой проверке, вы сможете избежать проблем с регуляторами и также защитить себя от участия в незаконных операциях.
Как это работает?
Наша команда работаем с передовыми аудиторскими агентствами, например Cure53, для того чтобы гарантировать точность наших проверок. Мы применяем передовые технологии для определения рискованных операций. Ваши данные обрабатываются и хранятся согласно с высокими нормами безопасности и конфиденциальности.
Как проверить собственные USDT для прозрачность?
Если хотите проверить, что ваши USDT-бумажники чисты, наш подход обеспечивает бесплатную проверку первых пяти кошельков. Просто вбейте адрес своего бумажника на на нашем веб-сайте, и мы предоставим вам детальный доклад о его положении.
Охраняйте свои активы сегодня же!
Не подвергайте опасности подвергнуться шарлатанов или попасть в неприятную обстановку из-за нелегальных транзакций. Обратитесь за помощью к нашему агентству, для того чтобы предохранить свои электронные активы и избежать неприятностей. Совершите первый шаг для безопасности вашего криптовалютного портфеля сегодня!
Тестирование Тетер на нетронутость: Каким образом обезопасить собственные криптовалютные средства
Все больше пользователей придают важность к секурити личных криптовалютных финансов. День ото дня дельцы изобретают новые подходы кражи цифровых средств, и также собственники электронной валюты оказываются страдающими их подстав. Один техник обеспечения безопасности становится проверка кошельков в присутствие незаконных средств.
С какой целью это необходимо?
В первую очередь, для того чтобы сохранить личные средства против шарлатанов и также похищенных монет. Многие инвесторы сталкиваются с риском потери их средств вследствие обманных планов или хищений. Анализ бумажников помогает обнаружить подозрительные операции и также предотвратить возможные убытки.
Что мы предоставляем?
Наша компания предлагаем услугу проверки криптовалютных кошельков и также операций для определения источника денег. Наша система анализирует данные для обнаружения незаконных операций или проценки риска для вашего счета. Вследствие этой проверке, вы сможете избегать проблем с регуляторами а также защитить себя от участия в нелегальных операциях.
Как происходит процесс?
Наша команда сотрудничаем с лучшими проверочными агентствами, такими как Certik, для того чтобы обеспечить точность наших тестирований. Мы используем современные технологии для выявления опасных транзакций. Ваши данные обрабатываются и сохраняются в соответствии с высокими нормами безопасности и конфиденциальности.
Как проверить свои USDT на нетронутость?
В случае если вы желаете проверить, что ваши Tether-кошельки чисты, наш сервис предоставляет бесплатное тестирование первых пяти бумажников. Просто введите местоположение вашего бумажника на на сайте, или наша команда предоставим вам детальный отчет о его положении.
Гарантируйте безопасность для вашими активы уже сегодня!
Не подвергайте опасности подвергнуться мошенников или оказаться в неприятную обстановку из-за незаконных транзакций. Посетите нашему сервису, чтобы предохранить ваши криптовалютные активы и избежать проблем. Предпримите первый шаг к безопасности вашего криптовалютного портфеля уже сейчас!
Zet Casino Störung
Das Zet Casino ist eine beliebte Online-GlГјcksspielplattform, auf der Spieler eine Vielzahl von Spielen wie Slots, Tischspielen und Live-Casino-Spielen genieГџen kГ¶nnen. Allerdings kann es manchmal vorkommen, dass das Casino aufgrund technischer Probleme oder Wartungsarbeiten vorГјbergehend nicht erreichbar ist, was als “Zet Casino StГ¶rung” bezeichnet wird.
In solchen Fällen kann es frustrierend sein, wenn Spieler versuchen, auf ihre Lieblingsspiele zuzugreifen und feststellen, dass die Website nicht funktioniert. Es ist wichtig zu beachten, dass diese Störungen normalerweise nur vorübergehend sind und die Casinobetreiber daran arbeiten, das Problem so schnell wie möglich zu beheben.
Wenn das Zet Casino eine Störung hat, können Spieler auf verschiedene Weise darauf reagieren. Zuallererst ist es wichtig, ruhig zu bleiben und zu verstehen, dass solche Probleme unvermeidlich sind und von vielen Online-Plattformen erlebt werden. Es ist ratsam, die offiziellen Kommunikationskanäle des Casinos zu überprüfen, um Informationen über die Störung und den voraussichtlichen Zeitpunkt der Behebung zu erhalten.
In einigen Fällen kann es auch hilfreich sein, den Kundendienst des Zet Casinos zu kontaktieren, um weitere Informationen zu erhalten und möglicherweise eine Alternative für das Spielen über eine andere Plattform in Betracht zu ziehen. Es ist wichtig, geduldig zu sein und zu verstehen, dass solche Störungen normalerweise schnell behoben werden und das Casino bald wieder normal funktionieren wird.
Insgesamt ist es ratsam, gelassen zu bleiben und zu verstehen, dass Störungen im Zet Casino oder anderen Online-Glücksspielplattformen unvermeidlich sind. Mit dem richtigen Umgang und etwas Geduld können Spieler sicherstellen, dass sie bald wieder ihre Lieblingsspiele genießen können.
https://zetcasino.one/
tamoxifen and osteoporosis cost of tamoxifen tamoxifen blood clots
Ten Mobile Car Diagnostics Near Me Uk Products That Can Help You
Live Better mobile car diagnostics near me
One Key Trick Everybody Should Know The One 10kgs Washing Machine Trick Every Person Should Know 10kg washers
Ищете надежный способ купить автозапчасти для своего автомобиля? Добро пожаловать в интернет-магазин http://autoparts121.ru Мы предлагаем широкий ассортимент оригинальных деталей для различных марок и моделей автомобилей. С нами вы можете быть уверены в качестве запчастей, ведь мы работаем только с проверенными поставщиками. Благодаря удобному сайту с подробными каталогами вы легко найдете необходимые детали и аксессуары. Покупайте с уверенностью в нашем интернет-магазине автозапчастей – ваш автомобиль заслуживает только лучшего!
11 “Faux Pas” That Are Actually Okay To Make With Your Washer
And Dryer In One Machine washer and dryer in one machine (https://sahl-kemp-2.mdwrite.net/)
15 Reasons You Must Love Repairs To Double Glazed Windows window repairs
(Marilou)
Question: How Much Do You Know About Sales Leader?
sales
Das m.zet Casino ist eine aufstrebende Online-GlГјcksspielplattform, die Spieler aus aller Welt mit einer Vielzahl von spannenden Spielen und groГџzГјgigen Bonusangeboten anlockt. Das Casino bietet eine benutzerfreundliche Website, die es einfach macht, sich anzumelden, zu spielen und Gewinne abzuheben.
Die Spielauswahl im m.zet Casino umfasst beliebte Klassiker wie Spielautomaten, Roulette, Blackjack und Video Poker. Darüber hinaus bietet das Casino auch Live-Dealer-Spiele an, bei denen Spieler gegen echte Croupiers antreten können. Die Spiele werden von führenden Softwareanbietern wie NetEnt, Microgaming und Evolution Gaming bereitgestellt, was für eine erstklassige Spielerfahrung sorgt.
Ein weiterer großer Pluspunkt des m.zet Casinos sind die großzügigen Bonusangebote, die sowohl neuen als auch bestehenden Spielern zur Verfügung stehen. Zu den Angeboten gehören Willkommensboni, Einzahlungsboni, Freispiele und Treueprämien. Diese Boni bieten Spielern die Möglichkeit, ihr Guthaben zu maximieren und mehr Gewinne zu erzielen.
Das m.zet Casino legt großen Wert auf Sicherheit und Fairness und verfügt über eine gültige Glücksspiellizenz. Die Website ist SSL-verschlüsselt, um sicherzustellen, dass persönliche und finanzielle Daten der Spieler geschützt sind. Darüber hinaus werden alle Spiele regelmäßig von unabhängigen Prüfstellen überprüft, um sicherzustellen, dass sie fair und zufällig sind.
Insgesamt ist das m.zet Casino eine hervorragende Wahl fГјr Spieler, die auf der Suche nach einer sicheren und unterhaltsamen Online-GlГјcksspielplattform sind. Mit einer Vielzahl von Spielen, groГџzГјgigen Bonusangeboten und einem hohen MaГџ an Sicherheit und Fairness ist das Casino definitiv einen Besuch wert.
https://zetcasino.one/
cialis online usa
Желаете смотреть русские сериалы онлайн в отличном качестве? Тогда добро пожаловать на Ruserial. Мы собрали для вас самый лучший контент. Уверены, что вы останетесь всем, довольны. Погрузитесь в мир занимательных эмоций и историй. https://ruserial-full.net/ – портал, который имеет понятный и удобный интерфейс. Здесь есть то, что нужно. Сериалы можете смотреть онлайн совершенно бесплатно, они подарят вам незабываемые впечатления. Присоединяйтесь к нам уже сейчас и смотрите любимые сериалы.
What’s The Current Job Market For Replacement Windows Prices Professionals?
Replacement Windows Prices
What’s The Job Market For Shopping Online Uk Professionals Like?
shopping online; Antonia,
https://kamagra.win/# super kamagra
На сайте https://saffa.ru/ закажите мобильные аксессуары оптом. В разделе вы найдете автомобильные держатели, чехлы, универсальные аксессуары, а также зарядные устройства, портативные аккумуляторы и многое другое. Специально для вас оперативная доставка, которая организуется за 2 дня. Вам доступен безупречный клиентский сервис. Ответы на вопросы вы получите в течение 10 минут. Все товары оригинального качества, имеются гарантии. Всегда доступные расценки за счет сотрудничества напрямую с производителями.
Quiz: How Much Do You Know About Washing Dryer Combo?
combination washer and dryer In one unit
Интернет-ресурс, где можно купить элегантные мебельные раковины 60 см от ведущих производителей.
Хотите сделать лучше свой английский. Погрузитесь в мир кино изучая английский по кинокартинам на английском языке. Фильмы на английском, помогают углубиться в естественную языковую среду. Для гораздо лучшего понимания можно использовать субтитры на английском. Делайте лучше свой английский, наслаждаясь излюбленными кинофильмами. Переходите на сайт https://filmy-na-angliiskom.ru/ и начинайте учить инглиш весело а также сверхэффективно!
Банкротство физ лиц ДолгХ https://dolgx.ru/ это возможность легально избавиться от долгов. Мы оказываем услуги: составление документов, представление интересов при банкротстве в суде, сопровождение процедуры банкротства. Посетите сайт, узнайте больше и ознакомьтесь со стоимостью услуг.
How To Get More Results With Your Upvc Doors Leeds upvc door Lock repair leeds
Tipico Wetten gegen Casino – Ein spannender Vergleich
Das Glücksspiel erfreut sich weltweit großer Beliebtheit und bietet den Spielern die Möglichkeit, ihr Glück zu versuchen und dabei auch noch Geld zu gewinnen. Zwei der bekanntesten Formen des Glücksspiels sind Sportwetten und Casinospiele. In diesem Artikel werden wir die Vor- und Nachteile von Tipico Wetten gegen das Casino genauer unter die Lupe nehmen.
Tipico ist ein bekannter Anbieter von Sportwetten, der seinen Kunden die Möglichkeit bietet, auf eine Vielzahl von Sportereignissen zu wetten. Dabei können die Spieler auf verschiedene Sportarten wie Fußball, Tennis, Basketball und viele mehr setzen. Der Vorteil von Sportwetten liegt darin, dass die Spieler ihr Fachwissen zu bestimmten Sportarten und Mannschaften nutzen können, um die Gewinnchancen zu erhöhen. Zudem können die Quoten bei Sportwetten vielversprechend sein und hohe Gewinne ermöglichen.
Im Gegensatz dazu bietet ein Casino eine Vielzahl von Spielen wie Roulette, Blackjack, Spielautomaten und Poker an. Der Vorteil eines Casinos liegt darin, dass die Spiele rein auf GlГјck basieren und es keine vorherige Kenntnisse oder Erfahrungen braucht, um zu gewinnen. Zudem bieten Casinos oft attraktive Boni und Promotionen, um die Spieler anzulocken.
Ein wichtiger Aspekt, den es zu beachten gilt, ist das Risiko bei beiden Formen des Glücksspiels. Bei Sportwetten kann das Risiko durch die Analyse von Statistiken und Informationen minimiert werden, während im Casino das Glück eine größere Rolle spielt und das Risiko höher sein kann.
Zusammenfassend lässt sich sagen, dass sowohl Tipico Wetten als auch Casinospiele ihre eigenen Vor- und Nachteile haben. Es kommt letztendlich auf die persönlichen Vorlieben und das Glück des Spielers an, welche Form des Glücksspiels bevorzugt wird. Es ist wichtig, verantwortungsbewusst zu spielen und sein Spielverhalten im Auge zu behalten, um negative Auswirkungen zu vermeiden.
https://tipicocasino.one/
Wow, superb blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your web site is
wonderful, let alone the content!
levitra online medicine
buy cenforce buy cenforce Cenforce 150 mg online
A Step-By-Step Guide To Handbags Tommy Hilfiger From Start To
Finish tommy hilfiger shoulder handbags
You could certainly see your enthusiasm within the work you write.
The world hopes for more passionate writers such as you who
aren’t afraid to mention how they believe. All the time go after
your heart.
sildenafil oral jelly 100mg kamagra: kamagra.win – buy Kamagra
I’m truly enjoying the design and layout of your site.
It’s a very easy on the eyes which makes it much more pleasant
for me to come here and visit more often. Did you hire out a developer to
create your theme? Superb work!
http://cialist.pro/# Cialis without a doctor prescription
Im Boomerang Casino können Spieler nicht nur aufregende Spiele genießen, sondern auch problemlos ihre Gewinne abheben. Der Prozess des Rückzugs von Geldern ist einfach und schnell, und Spieler können sicher sein, dass ihre Auszahlungen immer pünktlich erfolgen.
Um eine Auszahlung im Boomerang Casino zu tГ¤tigen, mГјssen Spieler einfach ihr Konto aufrufen und den Bereich “Kasse” besuchen. Dort kГ¶nnen sie die Option “Auszahlung” auswГ¤hlen und den Betrag eingeben, den sie abheben mГ¶chten. Es gibt verschiedene Zahlungsmethoden, die Spieler wГ¤hlen kГ¶nnen, darunter Kreditkarten, E-Wallets und BankГјberweisungen.
Es ist wichtig zu beachten, dass das Boomerang Casino möglicherweise bestimmte Bedingungen für Auszahlungen verlangt, insbesondere in Bezug auf Mindest- und Höchstauszahlungsbeträge sowie Verifizierungsprozesse. Spieler können sich jedoch darauf verlassen, dass das Casino sicherstellt, dass alle Transaktionen sicher und geschützt sind.
Nachdem die Auszahlungsanforderung eingegangen ist, wird das Boomerang Casino den Betrag so schnell wie möglich bearbeiten, normalerweise innerhalb von 24 Stunden. Die tatsächliche Dauer, bis das Geld auf dem Konto des Spielers gutgeschrieben wird, hängt von der gewählten Zahlungsmethode ab.
Insgesamt bietet das Boomerang Casino seinen Spielern eine reibungslose und effiziente Möglichkeit, ihre Gewinne abzuheben. Mit einer Vielzahl von Zahlungsmethoden und schnellen Bearbeitungszeiten können Spieler sicher sein, dass sie ihre Auszahlungen problemlos erhalten.
https://boomerangcasino.one/
Не останавливайтесь на достигнутом, купите диплом и стремитесь к новым вершинам!
https://diplom-kuplu.ru
Five Killer Quora Answers To Bunk Beds Kids bunk Beds kids
Heya are using WordPress for your blog platform? I’m new to the
blog world but I’m trying to get started and set up my own. Do you require any coding knowledge to make your own blog?
Any help would be greatly appreciated!
You’ll Never Guess This London Online Mobile Shopping Sites’s Tricks london online mobile shopping sites
On the website https://magicday.ae/ you can order live, exciting and interesting performances by actors, dancers, animators. You will find enchanting, luxurious costumes, a great and friendly atmosphere, as well as artists who will definitely not leave anyone indifferent. And most importantly, it will be possible to invite artists to absolutely any holiday. Check out the portfolio right now to find out how the performances are going. The artists will arrive at the agreed time. All services are provided at attractive prices.
Thank you for the good writeup. It actually was a entertainment account it.
Look complex to more delivered agreeable from you! However, how can we keep up
a correspondence?
7 Small Changes That Will Make An Enormous Difference To
Your Scooter To Buy Near Me Best Place To Buy Mobility Scooter
9 Lessons Your Parents Teach You About Ranking SEO Software ranking
seo software, https://beige-hawk-fd361d.mystrikingly.com/blog/why-seo-software-tools-is-harder-Than-you-think,
This Story Behind Car Diagnostic Price Uk Can Haunt You Forever!
Diagnostic Testing
17 Signs That You Work With Ghost 2 Immobiliser
Ghost Immobiliser Price
Ищете надежный и удобный способ приобрести необходимые детали для вашего автомобиля? Добро пожаловать в наш интернет-магазин автозапчастей http://partsshop03.ru! В нашем ассортименте вы найдете огромный выбор оригинальных запчастей для различных марок и моделей автомобилей. Мы предлагаем качественные детали по конкурентным ценам. Благодаря удобному сайту с подробными каталогами вы легко найдете нужные запчасти для вашего автомобиля. Покупайте с уверенностью в нашем интернет-магазине — мы знаем все о вашем автомобиле!
На сайте https://vk.com/wall-101758973_774 вы сможете оперативно заказать печать в Белгороде. К заказу доступны различные виды форматов печати. Выкройки, чертежи будут созданы непосредственно при вас. Обязательно закажите плоттерную резку. Есть возможность воспользоваться услугой по индивидуальному дизайну. Все изготавливается в минимальные сроки. Доступна печать на футболке номеров, текста, фотографий. Компания работает по удобному для всех графику и на инновационном, высокотехнологичном оборудовании. Специалисты выполнят все работы согласно требованиям.
A Positive Rant Concerning Cheap Couches For Sale
sofas for sale online
Asbestos Settlement Tools To Ease Your Daily Life Asbestos Settlement Technique Every
Person Needs To Be Able To asbestos settlement
Have you ever thought about including a little bit more than just
your articles? I mean, what you say is important and everything.
Nevertheless just imagine if you added some
great pictures or video clips to give your posts more,
“pop”! Your content is excellent but with pics and video clips, this website
could definitely be one of the greatest in its
field. Superb blog!
http://levitrav.store/# Vardenafil buy online
Guide To Glass Window Replacement: The Intermediate Guide
On Glass Window Replacement Glass Window Replacement
I was curious if you ever considered changing the layout of your site?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having 1 or two images.
Maybe you could space it out better?
10 Steps To Begin Your Own Double Glazing Windows
Near Me Business double glazing front door – http://vesti46.ru/ –
Das Boomerang Casino ist ein neues und aufregendes Online-Casino, das seinen Spielern großzügige Bonusangebote ohne Einzahlung bietet. Mit den Boomerang Casino Bonuscodes ohne Einzahlung können die Spieler ohne Risiko echtes Geld gewinnen und dabei Spaß haben.
Die Bonusangebote ohne Einzahlung sind eine großartige Möglichkeit für neue Spieler, das Casino kennenzulernen und erste Gewinne zu erzielen, ohne ihr eigenes Geld riskieren zu müssen. Die Codes werden einfach bei der Registrierung oder im Kassenbereich des Casinos eingegeben und schon kann das kostenlose Spiel beginnen.
Die Boomerang Casino Bonuscodes ohne Einzahlung können verschiedene Vorteile wie Freispiele, kostenloses Bonusgeld oder sogar Cashback-Angebote beinhalten. So haben die Spieler die Möglichkeit, verschiedene Spiele im Casino auszuprobieren und ihre Lieblingsspiele zu finden, ohne dafür Geld ausgeben zu müssen.
Um von den Boomerang Casino Bonuscodes ohne Einzahlung zu profitieren, ist es wichtig, die jeweiligen Bedingungen und Umsatzanforderungen zu beachten. Diese können je nach Angebot variieren und müssen erfüllt werden, um Gewinne auszahlen zu können.
Insgesamt bietet das Boomerang Casino seinen Spielern eine großartige Möglichkeit, ohne Einzahlung echtes Geld zu gewinnen und dabei viel Spaß zu haben. Die Bonusangebote ohne Einzahlung sind eine gute Gelegenheit, das Casino kennenzulernen und vielleicht sogar den Jackpot zu knacken. Wer also auf der Suche nach einem unterhaltsamen und lukrativen Online-Casino ist, sollte das Boomerang Casino definitiv in Betracht ziehen.
https://boomerangcasino.one/
buy generic nitroglycerin online – catapres generic diovan 160mg over the counter
На сайте https://allgranit.ru/ вы сможете заказать звонок для того, чтобы воспользоваться такой важной услугой, как создание гранитных памятников на заказ. Услуга оказывается не только в Москве, но и по области. Регулярно на определенные товары устанавливаются скидки, акции для того, чтобы ваша покупка была более выгодной. Рассчитать стоимость памятника получится прямо сейчас. Для этого воспользуйтесь специальным калькулятором. Для того чтобы иметь представление о работе, необходимо посмотреть портфолио.
10 Things That Your Family Taught You About Tiktok.Pornstars Tiktok.pornstars
Анализ USDT на прозрачность: Каким образом обезопасить собственные криптовалютные состояния
Постоянно все больше людей обращают внимание на надежность их криптовалютных активов. Каждый день мошенники придумывают новые схемы кражи электронных денег, и также владельцы криптовалюты становятся страдающими их интриг. Один методов сбережения становится тестирование кошельков для присутствие противозаконных средств.
Зачем это потребуется?
Прежде всего, для того чтобы защитить собственные средства от дельцов и украденных монет. Многие специалисты сталкиваются с вероятностью потери своих средств из-за хищных сценариев или кражей. Осмотр кошельков помогает обнаружить непрозрачные операции и предотвратить возможные потери.
Что наша группа предлагаем?
Наша компания предоставляем услугу анализа криптовалютных кошельков или транзакций для обнаружения происхождения средств. Наша платформа анализирует данные для обнаружения незаконных операций а также проценки угрозы для вашего счета. Вследствие этой проверке, вы сможете избегнуть недочетов с регуляторами и также защитить себя от участия в нелегальных сделках.
Каким образом это работает?
Мы сотрудничаем с ведущими проверочными организациями, например Certik, чтобы обеспечить точность наших проверок. Мы внедряем передовые техники для обнаружения опасных операций. Ваши данные обрабатываются и сохраняются в соответствии с высокими стандартами безопасности и приватности.
Как проверить собственные USDT для чистоту?
Если хотите проверить, что ваши USDT-бумажники чисты, наш сервис обеспечивает бесплатное тестирование первых пяти кошельков. Просто передайте положение личного бумажника на нашем сайте, и также мы предложим вам полную информацию доклад о его положении.
Обезопасьте свои средства сегодня же!
Не подвергайте опасности подвергнуться обманщиков или оказаться в неблагоприятную ситуацию из-за незаконных операций. Обратитесь за помощью к нам, с тем чтобы предохранить ваши криптовалютные финансовые ресурсы и предотвратить проблем. Предпримите первый шаг к сохранности вашего криптовалютного портфеля уже сегодня!
USDT – это неизменная криптовалютный актив, привязанная к валюте страны, такой как доллар США. Данное обстоятельство делает данную криптовалюту в частности популярной у инвесторов, поскольку она предоставляет устойчивость курса в в условиях волатильности рынка криптовалют. Все же, подобно другая тип криптовалюты, USDT подвержена опасности использования для скрытия происхождения средств и субсидирования незаконных операций.
Промывка средств через цифровые валюты становится все больше и больше распространенным в большей степени методом с тем чтобы скрытия происхождения средств. Используя разносторонние методы, мошенники могут попытаться легализовывать незаконно добытые средства путем обменники криптовалют или миксеры, чтобы совершить происхождение менее понятным.
Поэтому, проверка USDT на чистоту становится важной мерой защиты для того чтобы участников цифровых валют. Доступны специализированные сервисы, какие выполняют экспертизу транзакций и бумажников, для того чтобы идентифицировать сомнительные операции и незаконные источники капитала. Эти сервисы способствуют владельцам избежать непреднамеренного участия в преступной деятельности и избежать блокировки счетов со стороны регуляторных органов.
Экспертиза USDT на чистоту также также способствует обезопасить себя от потенциальных убытков. Пользователи могут быть уверенны в том их активы не связаны с незаконными сделками, что соответственно уменьшает вероятность блокировки счета или перечисления денег.
Таким образом, в условиях возрастающей степени сложности криптовалютной среды необходимо принимать шаги для обеспечения надежности своих финансовых ресурсов. Анализ USDT на чистоту с использованием специальных платформ представляет собой одним из способов защиты от незаконной деятельности, гарантируя пользователям цифровых валют дополнительный уровень и надежности.
9 . What Your Parents Teach You About Robot Vacuum And Mop Robot
It’s amazing to pay a visit this web site and reading the views of
all friends regarding this article, while I am also eager of getting knowledge.
Levitra 10 mg best price Buy generic Levitra online Buy Levitra 20mg online
The creativity and intelligence shine through, blinding almost, but I’ll keep my sunglasses handy.
buy nitroglycerin medication – order nitroglycerin online cheap buy valsartan generic
The Most Popular Self Emptying Robot Vacuum And Mop Gurus Are Doing Three Things
Best Self Emptying Robot Vacuum And Mop
5 Killer Quora Answers To British Porn Stars Xxx British porn stars xxx
Greate post. Keep posting such kind of information on your page.
Im really impressed by it.
Hey there, You have done a fantastic job. I’ll definitely digg it and for my part suggest to my friends.
I am sure they will be benefited from this site.
Das Boomerang Casino ist ein neues Online-Casino, das sich durch sein einzigartiges Konzept von anderen Anbietern abhebt. Mit einer breiten Auswahl an Spielen und attraktiven Bonusangeboten lockt es Spieler aus der ganzen Welt an.
Die Webseite des Boomerang Casinos ist benutzerfreundlich gestaltet und leicht zu navigieren. Die Spiele sind in verschiedene Kategorien unterteilt, darunter Spielautomaten, Tischspiele und Live-Casino Spiele. Dadurch finden Spieler schnell und einfach ihre Lieblingsspiele.
Ein besonderes Highlight des Boomerang Casinos sind die regelmäßigen Bonusangebote und Aktionen. Neue Spieler erhalten einen großzügigen Willkommensbonus, der ihnen zusätzliches Guthaben und Freispiele bietet. Auch Bestandskunden werden regelmäßig mit Boni belohnt, was für eine hohe Spielerzufriedenheit sorgt.
Die Spielauswahl im Boomerang Casino ist beeindruckend. Neben klassischen Casino-Spielen wie Blackjack und Roulette bietet das Casino auch eine groГџe Auswahl an Spielautomaten von renommierten Anbietern wie NetEnt, Microgaming und Play’n GO. Zudem kГ¶nnen Spieler im Live-Casino gegen echte Dealer antreten und ein authentisches Casino-Erlebnis genieГџen.
Die Zahlungsmöglichkeiten im Boomerang Casino sind vielfältig und sicher. Spieler können zwischen verschiedenen Zahlungsmethoden wie Kreditkarten, E-Wallets und Banküberweisungen wählen. Alle Transaktionen sind verschlüsselt, um die Sicherheit der Spieler zu gewährleisten.
Insgesamt Гјberzeugt das Boomerang Casino mit einem attraktiven Spieleangebot, groГџzГјgigen Bonusangeboten und einer benutzerfreundlichen Webseite. Spieler, die auf der Suche nach einem neuen Online-Casino sind, sollten das Boomerang Casino definitiv ausprobieren.
https://boomerangcasino.one/
This Is The Good And Bad About Asbestos Lawyer Asbestos Compensation
9 Lessons Your Parents Taught You About Link Login Gotogel Link login gotogel
Wow that was unusual. I just wrote an very long comment
but after I clicked submit my comment didn’t appear.
Grrrr… well I’m not writing all that over again. Anyhow,
just wanted to say excellent blog!
20 Fun Informational Facts About Audi A3 Key Replacement car key replacement audi; Margarette,
Have funds disappeared on your QIWI wallet?
We know how stressful that can be.
Stay calm—our company specializes in retrieving missing money from QIWI wallets.
With years of experience, we’re sure we can provide assistance.
Reach out to us and let’s start the process of getting your money back.
Gogo casino bluff: Sanningen bakom myten
I spelvärlden pratas det mycket om Gogo casino och rykten om bedrägeri och bluff kring detta online casino har florerat under en tid. Men vad är egentligen sanningen bakom dessa påståenden?
Gogo casino har varit en av de mest populära spelplattformarna på senare tid och har lockat till sig en stor mängd spelare. Men med populariteten har även misstankar om bluff och bedrägeri börjat spridas. Många spelare har påstått att de blivit lurade av casinot och att deras vinster inte betalats ut som utlovat.
Men enligt företaget själva är dessa påståenden falska. Gogo casino hävdar att de följer alla lagar och regler inom spelbranschen och att de tar ansvar för sina spelares säkerhet. De har även en licens från en respekterad spelmyndighet, vilket ytterligare stärker deras status som en pålitlig aktör i branschen.
Så varför då dessa rykten om bluff och bedrägeri? En del menar att det kan bero på missförstånd eller otur bland spelare, medan andra tror att det kan vara en medveten smutskastningskampanj från konkurrenter. Oavsett anledning är det viktigt att ta alla påståenden med en nypa salt och vara kritisk mot informationen som sprids.
Sammanfattningsvis finns det alltid risker med att spela på online casinon, men det är viktigt att vara försiktig med att dra förhastade slutsatser om bluff och bedrägeri. Gogo casino har en godkänd licens och en godkänd reputation, vilket gör det till en säker och pålitlig spelplattform för de som är intresserade av att testa sin lycka. Men som med alla former av spel är det viktigt att spela ansvarsfullt och med måtta för att undvika eventuella problem.
https://gogocasino.one
Our knowledge in e-wallets and electronic payments means
we’re well-prepared to tackle your QIWI wallet issues.
Rest assured, we employ the latest techniques and keep up with the newest
recovery methods.
In case of victimized by unauthorized transactions or technical glitches that resulted in a loss of funds, you’ve got an ally in us.
super kamagra: buy kamagra online – sildenafil oral jelly 100mg kamagra
Киного https://kinogo.vision/ это возможность смотреть фильмы, сериалы, мультфильмы онлайн бесплатно в высоком качестве. Все новинки 2024 уже на сайте. Коллекции за предыдущие годы. ТОП фильмов, сериалов где каждый найдет для себя необходимый жанр.
The People Nearest To Repair Double Glazed Window
Share Some Big Secrets upvc Door repairs near me
One Key Trick Everybody Should Know The One Car Accident Claim Trick Every Person Should Learn Attorneys
What Is Tumble Dryer Heat Pump: A Simple Definition what Is Tumble dryer Heat pump
Our expertise in digital wallets and electronic payments means
we’re ideally suited to tackle your QIWI wallet issues.
Rest assured, we use advanced techniques and stay updated with the current security protocols.
In case of hit with unauthorized transactions or technical glitches
that caused a loss of funds, we’re here to help.
The Writing is like a secret garden, each post a path leading to new discoveries and delights.
whoah this blog is great i really like reading
your articles. Stay up the good work! You understand, many persons are searching round for this
information, you could help them greatly.
Boomerang Casino Bonus ohne Einzahlung
Das Boomerang Casino ist eines der beliebtesten Online-Casinos für Spieler, die auf der Suche nach aufregenden und lukrativen Bonusangeboten sind. Eine besonders beliebte Aktion im Boomerang Casino ist der Bonus ohne Einzahlung. Bei diesem Bonus erhalten Spieler die Möglichkeit, echtes Geld zu gewinnen, ohne selbst eine Einzahlung tätigen zu müssen.
Der Bonus ohne Einzahlung im Boomerang Casino kann in Form von Freispielen oder Bonusgeld ausgezahlt werden. Oftmals erhalten neue Spieler nach der Registrierung im Casino automatisch einen bestimmten Betrag an Bonusgeld oder Freispielen gutgeschrieben, ohne dass sie dafür eine Einzahlung tätigen müssen. Dieser Bonus ermöglicht es Spielern, das Angebot des Casinos risikofrei auszuprobieren und erste Gewinne zu erzielen, ohne dabei ein finanzielles Risiko einzugehen.
Um den Boomerang Casino Bonus ohne Einzahlung zu erhalten, müssen Spieler lediglich ein Konto im Casino erstellen und gegebenenfalls einen Bonuscode eingeben. Anschließend können sie sofort mit dem Spielen beginnen und die spannenden Spiele und lukrativen Gewinnchancen im Boomerang Casino entdecken.
Es ist jedoch zu beachten, dass Boni ohne Einzahlung im Boomerang Casino meist an bestimmte Umsatzbedingungen geknüpft sind. Spieler müssen die Gewinne aus dem Bonus in der Regel mehrfach umsetzen, bevor sie eine Auszahlung beantragen können. Dennoch bieten diese Boni eine großartige Möglichkeit, das Casino und seine Spiele kennenzulernen, ohne dabei eigenes Geld riskieren zu müssen.
Alles in allem ist der Boomerang Casino Bonus ohne Einzahlung eine attraktive Aktion, die es Spielern ermöglicht, echtes Geld zu gewinnen, ohne dafür selbst eine Einzahlung tätigen zu müssen. Mit etwas Glück und Geschick können Spieler mit diesem Bonus tolle Gewinne erzielen und den Spielspaß im Boomerang Casino voll auskosten.
https://boomerangcasino.one/
20 Washing Machines 12kg Websites That Are Taking The Internet By Storm local
14 Smart Ways To Spend Your Left-Over Sex Machine Store Budget cheapest Sex Machine
11 “Faux Pas” That Are Actually OK To Make With Your Star Porn Star porn kayleigh wanless (spectr-sb116.ru)
10 Things Everybody Hates About Washing And Dryer Combo washer dryer combination (Twyla)
How To Get More Value With Your Togel Online goblok
You have a gift for explaining things in an understandable way. Thank you!
The other day, while I was at work, my sister stole my iphone and tested to see if it can survive a 40 foot drop, just so she can be
a youtube sensation. My iPad is now destroyed and she has 83 views.
I know this is totally off topic but I had to share
it with someone!
Please let me know if you’re looking for a article writer for your site.
You have some really great articles and I think I would be a good
asset. If you ever want to take some of the load off, I’d really like to write some content for your blog
in exchange for a link back to mine. Please blast me an e-mail if interested.
Many thanks!
Five Essential Tools Everyone Within The Tumble Dryer With Heat
Pump Industry Should Be Utilizing good
Confused about how to go about the recovery of your QIWI wallet funds?
Our customer support are available 24/7 to guide you through the process and answer any questions you have.
Working with our team, you’re selecting a dependable ally
in getting your money back.
https://viagras.online/# viagra without prescription
Hi to every body, it’s my first go to see of this website;
this blog carries awesome and actually excellent
stuff for readers.
Хотите получить позитивные эмоции? Тогда заходите на ЗАСОС.ФАН! Это развлекательный портал, который поднимет ваше настроение. Мы заставим вас посмеяться от души. Ищете прикольные спортивные моменты? Zasos.fun – портал, где есть веселые мемы и отборный юмор. Здесь найдете качественные фотографии очаровательных девушек в сексуальных нарядах, удивительные снимки с животными и птицами. Также узнаете, какой самый очевидный намек от представительницы прекрасного пола вы упустили. У нас есть множество прикольных картинок, заходите к нам в гости!
20 Fun Details About Double Glazing Repairs Leeds upvc Window handle repairs leeds
Generic Tadalafil 20mg price buy cialis online Tadalafil price
LastTorrent.ru предлагает скачать любимую игру через торрент. Долго ждать вам не нужно будет. У нас есть удобный рубрикатор, с помощью которого вы найдете то, что вам нужно. Мы не загромождаем страницы ненужными баннерами. Для доступа к файлам торрентов проходить регистрацию совсем не обязательно. https://lasttorent.ru – известный сайт, загружая игры здесь, вы получите полноценный продукт, без риска заражения своего ПК вирусами. У вас появились вопросы? Обратитесь к нам, мы поможем.
5 Clarifications On Replacement Ford Fiesta Key Uk Ford car key Replacement near me
I was able to find good advice from your blog posts.
Boomerang Casino Online: ein aufregendes Spielerlebnis
Die Welt der Online-Casinos hat in den letzten Jahren einen regelrechten Boom erlebt. Immer mehr Menschen entdecken die Vorteile des bequemen Spielens von zu Hause aus. Eines der aufregendsten neuen Online-Casinos ist das Boomerang Casino. Mit einer Vielzahl von Spielen, tollen Bonusangeboten und einer benutzerfreundlichen Plattform verspricht dieses Casino ein erstklassiges Spielerlebnis.
Das Boomerang Casino bietet eine breite Auswahl an Spielen, von traditionellen Tischspielen wie Blackjack und Roulette bis hin zu beliebten Spielautomaten und Live-Casino-Spielen. Die Spieler kГ¶nnen aus Hunderten von Spielen wГ¤hlen, die von renommierten Software-Entwicklern wie NetEnt, Microgaming und Play’n GO entwickelt wurden. Dadurch ist eine hohe QualitГ¤t der Spiele garantiert.
Ein weiterer großer Vorteil des Boomerang Casinos sind die großzügigen Bonusangebote. Neue Spieler erhalten in der Regel einen Willkommensbonus, der ihre erste Einzahlung verdoppelt oder sogar verdreifacht. Zusätzlich gibt es regelmäßige Promotionen und Aktionen, bei denen die Spieler Freispiele, Einzahlungsboni oder Cashback-Angebote erhalten können. Dadurch wird das Spielerlebnis noch aufregender und lukrativer.
Die Plattform des Boomerang Casinos ist benutzerfreundlich und einfach zu navigieren. Die Spieler können problemlos zwischen verschiedenen Spielen wechseln und ihre Lieblingsspiele schnell finden. Zudem bietet das Casino einen ausgezeichneten Kundenservice, der rund um die Uhr verfügbar ist, um Fragen und Probleme der Spieler zu beantworten.
Alles in allem bietet das Boomerang Casino ein aufregendes und unterhaltsames Spielerlebnis fГјr alle Casino-Fans. Mit einer groГџen Auswahl an hochwertigen Spielen, groГџzГјgigen Bonusangeboten und einem erstklassigen Kundenservice ist dieses Online-Casino definitiv einen Besuch wert. Probieren Sie es aus und erleben Sie die Spannung und den Nervenkitzel des Boomerang Casinos!
https://boomerangcasino.one/
Покупайте необходимые детали для вашего автомобиля в интернет-магазине автозапчастей http://shopauto74.ru! Вас ждет широкий выбор оригинальных запчастей для автомобилей различных марок и моделей. Мы предлагаем огромный выбор качественных запчастей. В нашем ассортименте вы найдете все, что нужно вашему автомобилю: от аксессуаров до самых важных деталей. Воспользуйтесь удобным каталогом оригинальных запчастей и вы найдете все что нужно. Вы приятно удивитесь низким ценам и широкому выбору. Доверьте свой автомобиль нашему интернет-магазину, и он будет всегда в надежных руках!
Guide To Content Marketing Agency London: The Intermediate Guide Towards Content Marketing Agency London Content marketing Agency
Thank you a lot for sharing this with all of us
you actually recognise what you’re speaking about! Bookmarked.
Kindly additionally seek advice from my site =). We could have a hyperlink alternate arrangement between us
It’s The Next Big Thing In Which CSGO Case Is The Most
Profitable cases
You’ll Be Unable To Guess Replace Window Pane’s Secrets replace window Pane
Recovering your lost funds shouldn’t be troublesome. That’s why
our process is straightforward and transparent.
You just need to supply some basic information, and we’ll
handle everything else.
Don’t let a simple mistake prevent you from your hard-earned money.
We’re committed to ensure the return of every dime.
5 Killer Quora Answers To Bentley Key Programming bentley Key programming
It’s Time To Forget New 9kg Washing Machine:
10 Reasons Why You Don’t Really Need It new 9kg washing Machine
Overwhelmed by how to proceed with recovery of your
QIWI wallet funds? Our customer support is on standby to help to guide you through the steps and answer any concerns you might have.
Working with our team, you’re opting for
a trusted partner in reclaiming your assets.
The Three Greatest Moments In Local Locksmith For Cars
History cheap locksmith for cars near me
As the admin of this site is working, no question very shortly it
will be renowned, due to its feature contents.
Don’t Be Enticed By These “Trends” About Replacement Key For Fiat 500 how much is a new fiat 500 key
Your method of describing the whole thing in this post is genuinely nice, all be able
to easily know it, Thanks a lot.
Unlocking Car Door Service: The Good, The Bad, And The
Ugly Car lockout help
Can Washer Dryer Combos Ever Rule The World? cheap washer Dryer combos
Buy Tadalafil 20mg: Cialis without a doctor prescription – Cialis without a doctor prescription
Zet Casino Anmeldung
Zet Casino ist ein Online-Casino, das zahlreiche Spiele und attraktive Bonusangebote für seine Spieler bietet. Um die Spiele im Casino zu genießen und von den Bonusaktionen zu profitieren, müssen Sie sich zunächst auf der Webseite des Casinos anmelden.
Die Anmeldung bei Zet Casino ist ganz einfach und unkompliziert. Klicken Sie einfach auf den Button “Registrieren” und fГјllen Sie das Anmeldeformular mit Ihren persГ¶nlichen Daten aus. Dazu gehГ¶ren unter anderem Ihr Name, Ihre E-Mail-Adresse, Ihre Wohnadresse und Ihr Geburtsdatum.
Nachdem Sie das Anmeldeformular ausgefüllt haben, müssen Sie Ihre E-Mail-Adresse bestätigen, indem Sie auf den Link klicken, den Ihnen das Casino per E-Mail zusendet. Sobald Ihre E-Mail-Adresse bestätigt ist, können Sie sich mit Ihrem Benutzernamen und Ihrem Passwort auf der Webseite von Zet Casino einloggen.
Nach der Anmeldung können Sie die Vielzahl an Spielen im Casino erkunden und Ihr Glück versuchen. Zet Casino bietet eine große Auswahl an Spielautomaten, Tischspielen und Live-Dealer-Spielen von renommierten Softwareanbietern wie NetEnt, Microgaming und Evolution Gaming.
Darüber hinaus können Sie sich über regelmäßige Bonusaktionen und Promotionen freuen, die Ihnen zusätzliches Guthaben, Freispiele oder andere attraktive Preise bescheren. Schauen Sie regelmäßig auf der Webseite von Zet Casino vorbei, um keine der lukrativen Angebote zu verpassen.
Insgesamt bietet Zet Casino eine unterhaltsame und hochwertige Spielerfahrung fГјr alle, die gerne online spielen. Melden Sie sich noch heute an und tauchen Sie ein in die faszinierende Welt der Online-Casinospielen bei Zet Casino. Viel GlГјck!
https://zetcasino.one/
10 Meetups About Combination Washer Dryer You Should Attend washing
9 . What Your Parents Teach You About Bentley Continental
Gt Key Fob bentley continental gt key fob
I’m extremely impressed along with your writing
talents and also with the layout on your blog. Is this a paid subject matter or did you modify it yourself?
Anyway keep up the nice high quality writing, it’s rare to see a nice weblog like this one nowadays..
12 Companies Are Leading The Way In Car Locksmiths locked keys in car locksmith
Sash Window Replacement Tools To Help You Manage Your Daily Life
Sash Window Replacement Trick Every Individual Should Be
Able To Sash Window Replacement
What’s The Job Market For Slot Demo Gratis Pragmatic Play No Deposit Professionals?
slot Demo gratis pragmatic
Lost QIWI wallet funds?
Let us handle the stress in recovering what isrightfully yours.
Get in touch now and begin reclaiming your funds.
I’ve been exploring for a little bit for any high quality articles or
blog posts in this kind of space . Exploring in Yahoo I
eventually stumbled upon this site. Reading this info So i
am satisfied to express that I’ve an incredibly excellent uncanny feeling I came
upon just what I needed. I such a lot no doubt will make sure
to do not overlook this website and provides it a look on a constant
basis.
Thanks for the hard work. I could almost see the sweat on the keyboard. Much appreciated!
What’s up, yeah this paragraph is truly good
and I have learned lot of things from it regarding blogging.
thanks.
I like the valuable information you provide in your articles.
I’ll bookmark your blog and check again here frequently.
I’m quite certain I will learn many new stuff right here!
Good luck for the next!
A Journey Back In Time: What People Discussed About Fiat 500
Keys 20 Years Ago Fiat remote key; https://peatix.com/user/21561601,
Cheap Viagra 100mg Buy Viagra online cheap Cheap Sildenafil 100mg
Hello my loved one! I wish to say that this post is amazing, nice written and include approximately all important infos.
I’d like to peer more posts like this .
See What Glass Repair Leeds Tricks The Celebs Are Using glass repair leeds
Boomerang Casino Mobil: Nie mehr Langeweile unterwegs!
Im Zeitalter der digitalen Revolution wird MobilitГ¤t immer wichtiger. Egal ob auf dem Weg zur Arbeit, in der Bahn oder im Wartezimmer beim Arzt – wir verbringen immer mehr Zeit unterwegs. Da ist es nur verstГ¤ndlich, dass auch das mobile GlГјcksspiel immer beliebter wird. Mit dem Boomerang Casino Mobil kГ¶nnen Spieler jetzt auch unterwegs ihre Lieblingsspiele genieГџen und lukrative Gewinne erzielen.
Das Boomerang Casino Mobil bietet eine Vielzahl von Spielen, angefangen von Slots über Tischspiele bis hin zu Live-Casino-Spielen. Für jeden Geschmack ist etwas dabei und dank der hochwertigen Grafik und des reibungslosen Spielablaufs fühlt man sich fast wie in einem echten Casino. Zudem sorgen regelmäßige Updates und neue Spiele dafür, dass es nie langweilig wird.
Ein weiterer Vorteil des Boomerang Casino Mobil ist die FlexibilitГ¤t in Bezug auf Zahlungsmethoden. Egal ob Kreditkarte, PayPal oder eine virtuelle GeldbГ¶rse – es gibt zahlreiche MГ¶glichkeiten, um bequem Ein- und Auszahlungen vornehmen zu kГ¶nnen. Zudem sorgt eine sichere SSL-VerschlГјsselung dafГјr, dass persГ¶nliche Daten geschГјtzt sind.
Auch der Kundenservice des Boomerang Casino Mobil überzeugt auf ganzer Linie. Freundliche und kompetente Mitarbeiter stehen rund um die Uhr zur Verfügung, um Fragen zu beantworten oder Probleme zu lösen. So fühlt man sich auch unterwegs gut betreut und kann sich voll und ganz auf das Spiel konzentrieren.
Fazit: Das Boomerang Casino Mobil ist die perfekte LГ¶sung fГјr alle, die auch unterwegs nicht auf spannende Casino-Spiele verzichten mГ¶chten. Mit einer breiten Auswahl an Spielen, flexiblen Zahlungsmethoden und einem exzellenten Kundenservice steht dem ultimativen SpielspaГџ nichts mehr im Wege.Probieren Sie es aus und erleben Sie ein unvergessliches Casino-Erlebnis – ganz bequem von Ihrem Smartphone oder Tablet aus!
https://boomerangcasino.one/
Useful information. Fortunate me I discovered your
website by accident, and I am shocked why this twist of
fate didn’t came about earlier! I bookmarked
it.
It’s The Double Glazed Units Near Me Case Study You’ll Never Forget Wood double Glazed windows
10 Vehicle Diagnostics That Are Unexpected diagnostics mobile (Deidre)
Клининговая компания Родник Чистоты https://rodnik-clean.ru/ в Санкт-Петербурге это профессиональный клининг и уборка помещений любой сложности. Профессиональные сотрудники. Зайдите на сайт, узнайте больше об услугах и их стоимости, а при необходимости воспользуйтесь калькулятором стоимости на сайте.
Washing Machine 12kg Isn’t As Difficult As You
Think washing machine sale 12kg (Donte)
10 Erroneous Answers To Common CSGO Gambling Sites Questions Do You
Know The Right Ones? Case Spectrum – https://Telegra.Ph/5-Things-That-Everyone-Doesnt-Know-About-CSGO-Opening-Case-Sites-04-12,
https://cialist.pro/# Cialis 20mg price in USA
levitra online
Attractive section of content. I just stumbled upon your weblog and in accession capital to assert that I get actually enjoyed account your blog posts.
Any way I’ll be subscribing to your augment and even I achievement you access consistently fast.
tadalafil 75mg
Why You Should Not Think About The Need To Improve Your
Porsche Macan Key Replacement Cost Porsche Key Fob
Is Your Company Responsible For The 9kg Washer Budget?
Twelve Top Ways To Spend Your Money cheapest 9kg washing machines
That is a great tip particularly to those fresh to the blogosphere.
Short but very accurate information… Thank you for sharing this one.
A must read post!
Компания «MIRTASH» за время деятельности уже приобрела постоянных заказчиков, она зарекомендовала себя как достойный и надежный партнер. Предоставляем отличный сервис и качественный камень. Мы имеем собственное производство, у нас есть складские запасы. https://mirtash.ru/ – сайт, где вы можете оставить свои контактные данные. Мы в самое ближайшее время с вами свяжемся. Если вам интересны изделия из доломита, лемезита и других пород камня, обращайтесь смело к нам, мы быстро доставляем продукцию до объекта по всей РФ.
15 Shocking Facts About Lost A Car Key That You Never Knew i lost My car keys what do i do
5 Killer Quora Answers To Best Self Emptying Robot
Vacuum Self Emptying Robot Vacuum
The Reasons To Focus On Improving Audi Key local
How Much Do Best Robot Vacuum Experts Make? robot Vacuum cleaner for pet hair
Hello, yup this piece of writing is really fastidious and I have learned lot of things from it about blogging.
thanks.
How Best Robot Vacuum Rose To The #1 Trend On Social Media Vacuum robot Mop
20 Best Tweets Of All Time About Michael Kors
Bags On Sale Michael Kors Bags Sling
I am no longer certain where you’re getting your info, but great topic.
I needs to spend some time learning more or figuring out more.
Thanks for wonderful info I was on the lookout for this information for my mission.
http://viagras.online/# Sildenafil 100mg price
levitra 20mg price in canada
Why Joker123 Gaming Is Relevant 2023 spam
See What Cost To Replace Windows Uk Tricks The Celebs Are Making Use Of cost to Replace windows uk
Boomerang Casino ist eine der neuesten und aufregendsten Online-Glücksspiel-Plattformen, die derzeit auf dem Markt verfügbar ist. Mit einer benutzerfreundlichen Oberfläche, einer großen Auswahl an Spielen und attraktiven Bonusangeboten hat die Boomerang Casino App bereits viele Fans gewonnen.
Die App bietet eine Vielzahl von GlГјcksspielen, darunter Spielautomaten, Tischspiele, Live-Casino-Spiele und vieles mehr. Die Spieler kГ¶nnen aus einer Vielzahl von beliebten Titeln wГ¤hlen, die von fГјhrenden Entwicklern wie NetEnt, Microgaming, Play’n GO und anderen bereitgestellt werden. DarГјber hinaus kГ¶nnen die Spieler an aufregenden Turnieren und Wettbewerben teilnehmen, um zusГ¤tzliche Belohnungen zu gewinnen.
Ein weiterer großer Vorteil der Boomerang Casino App sind die großzügigen Bonusangebote, die regelmäßig verfügbar sind. Neue Spieler können von einem Willkommensbonus profitieren, der Freispiele und zusätzliches Bonusgeld beinhaltet. Zusätzlich gibt es auch regelmäßige Aktionen und Promotionen, die den Spielern die Möglichkeit bieten, ihre Gewinne zu steigern.
Die Benutzeroberfläche der App ist benutzerfreundlich und leicht zu navigieren. Die Spieler können schnell und einfach ihre Lieblingsspiele finden und spielen, ohne dabei auf Unannehmlichkeiten zu stoßen. Darüber hinaus bietet die Boomerang Casino App eine sichere und geschützte Spielumgebung, die die persönlichen und finanziellen Daten der Spieler schützt.
Insgesamt ist die Boomerang Casino App eine hervorragende Wahl für alle, die Spaß und Spannung beim Online-Glücksspiel suchen. Mit einer Vielzahl von Spielen, großzügigen Bonusangeboten und einer benutzerfreundlichen Oberfläche ist diese App definitiv einen Blick wert. Lassen Sie sich also nicht die Gelegenheit entgehen und laden Sie die Boomerang Casino App noch heute herunter, um eine unvergessliche Glücksspiel-Erfahrung zu erleben.
https://boomerangcasino.one/
Why Nobody Cares About Lavazza Coffee Machine commercial coffee machines (Mikel)
5 Laws That Will Help With The Bmw Replacement Key Fob Industry new bmw Key
На сайте https://dokumentooborot24.ru/ ознакомьтесь с инновационной и уникальной программой «1С:Документооборот». Такая версия была создана специально для тех предприятий, у которых имеются дочерние компании, а также филиалы. Дополнительно ей могут пользоваться и те, у кого бизнес за рубежом, но развивают его на территории России. Функциональная программа помогает автоматизировать все процессы, включая проработку черновиков, а также уничтожение документации. Кроме того, программа дает возможность улучшить качество обслуживания среди сотрудников, оптимизировать их труд.
10 Inspirational Images Of Washing Machine 10kg Uk washing machine 10kg Uk
Where Is Double Glazing Showrooms Near Me Be 1 Year From What Is Happening Now?
Local Double Glazing Companies
What’s The Job Market For Best Kids Bunkbeds Professionals Like?
kids bunkbed (chessdatabase.science)
The Best Way To Explain Search Engine Optimization Services To Your Mom seo search optimization
Levitra 10 mg buy online: Vardenafil online prescription – Levitra 20 mg for sale
Five Killer Quora Answers To Outdoor Couches For Sale outdoor couches
for sale (http://vesti46.ru/)
Your Family Will Thank You For Getting This Double
Glazing Units Near Me replacing double glazing units
The Next Big New Replacement Window Handle Industry Upvc replacement Window handles
Mobile Car Diagnostics’s History History Of Mobile
Car Diagnostics diagnostic Tests
На сайте https://dolgovnet82.ru вы сможете уточнить всю важную информацию, которая касается такой важной услуги, как банкротство физических лиц. Вас избавят от долгов, а также кредитов законным путем. За счет того, что обращение происходит к арбитражному управляющему напрямую, то вы сможете сэкономить приличную сумму денег. Процедура будет начата в день обращения, и при этом не нужно будет вносить платежи. Ваше имущество будет сохранено, как и покой близких. В этой компании действует привлекательная стоимость.
Hi! I just would like to give you a huge thumbs up for your excellent
info you have got right here on this post. I will be returning to your blog for more
soon.
See What Cost To Replace Windows Uk Tricks The Celebs Are Using cost
to replace windows uk (Wilma)
Its History Of Second Hand Couches For Sale Couch Sofa Set
See What Gotogel Link Alternatif Tricks The Celebs Are Using
Gotogel Link Alternatif
20 Fun Infographics About Leather Couches For Sale couches for living room [Florencia]
Five Things You Don’t Know About Sofa Sale Clearance Used sectionals for sale near Me
WOW just what I was looking for. Came here by searching for hotel nyc
20 Amazing Quotes About Bentley Car Keys fob
Ten Treadmill That Folds Flats That Really Make Your Life Better
treadmills that fold flat [Nick]
Zet Casino Promo Code 2023: Alle Informationen, die Sie wissen mГјssen
Zet Casino ist eine beliebte Online-Spielplattform, die eine Vielzahl von Spielen und Promotionen für Spieler bietet. Eine der aufregendsten Aktionen, auf die sich Spieler freuen können, ist der Zet Casino Promo Code 2023. Dieser spezielle Code bietet Spielern die Möglichkeit, zusätzliche Belohnungen und Boni zu erhalten, wenn sie ihn bei der Anmeldung oder Einzahlung verwenden. In diesem Artikel werden wir alle wichtigen Informationen zu diesem aufregenden Angebot präsentieren.
Was ist der Zet Casino Promo Code 2023?
Der Zet Casino Promo Code 2023 ist ein spezieller Code, der von Zet Casino herausgegeben wird, um Spielern zusätzliche Boni und Belohnungen zu bieten. Spieler können diesen Code eingeben, wenn sie ein neues Konto erstellen oder eine Einzahlung tätigen, um von den zusätzlichen Leistungen zu profitieren. Der Promo-Code kann je nach Aktion unterschiedlich sein und kann verschiedene Arten von Belohnungen wie Bonusgelder, Freispiele oder Cashback-Angebote bieten.
Wie verwende ich den Zet Casino Promo Code 2023?
Um den Zet Casino Promo Code 2023 zu verwenden, müssen Sie ihn während des Anmelde- oder Einzahlungsvorgangs eingeben. Wenn Sie ein neuer Spieler sind, können Sie den Code bei der Kontoerstellung eingeben, um Ihre Belohnung zu erhalten. Wenn Sie bereits ein Konto haben und eine Einzahlung tätigen möchten, können Sie den Promo-Code während des Einzahlungsvorgangs eingeben, um zusätzliche Boni zu erhalten. Stellen Sie sicher, dass Sie den Code korrekt eingeben, um sicherzustellen, dass Sie die Belohnung erhalten.
Welche Vorteile bietet der Zet Casino Promo Code 2023?
Der Zet Casino Promo Code 2023 bietet Spielern eine Vielzahl von Vorteilen und Belohnungen. Zu den möglichen Belohnungen gehören Bonusgelder, Freispiele, Cashback-Angebote und vieles mehr. Diese Belohnungen können verwendet werden, um Ihre Gewinnchancen zu erhöhen und Ihr Spielerlebnis zu verbessern. Darüber hinaus können Spieler von exklusiven Aktionen und Sonderangeboten profitieren, die nur für diejenigen gelten, die den Promo-Code verwenden. Insgesamt bietet der Zet Casino Promo Code 2023 eine großartige Möglichkeit, zusätzliche Belohnungen zu erhalten und Ihr Spielerlebnis zu maximieren.
Fazit
Der Zet Casino Promo Code 2023 ist eine aufregende Aktion, die Spielern die Möglichkeit bietet, zusätzliche Belohnungen und Boni zu erhalten. Spieler können diesen Code verwenden, um exklusive Angebote zu erhalten und ihre Gewinnchancen zu erhöhen. Wenn Sie also auf der Suche nach zusätzlichen Belohnungen und Vorteilen sind, sollten Sie den Zet Casino Promo Code 2023 unbedingt in Betracht ziehen. Wir empfehlen Ihnen, die Website von Zet Casino zu besuchen, um weitere Informationen zu erhalten und den Promo-Code zu erhalten. Viel Spaß beim Spielen und viel Glück!
https://zetcasino.one/
20 Questions You Should To Ask About Rabbit Vibrator Sex Toys Before You Buy Rabbit Vibrator Sex Toys buy rabbit vibrator (Melodee)
Repairs To Upvc Windows: What Nobody Is Talking About broken
What To Focus On When Making Improvements Key Smith For Cars Car Mobile Locksmith
Are You Getting The Most From Your Used Couches For Sale?
brown sectional Couch
10 Misleading Answers To Common Car Replacement Key Near
Me Questions Do You Know The Right Ones? lost Car key replacement Near me
See What Cost To Replace Windows Uk Tricks The Celebs Are Using cost to replace windows uk
The Reasons Why Car Diagnostics Will Be Everyone’s Desire In 2022 diagnostics near Me
cenforce.pro Cenforce 100mg tablets for sale Cenforce 100mg tablets for sale
7 Secrets About 9kg Washing Machines For Sale That No One Will Tell You cheap washing machines 9kg
The Ultimate Glossary On Terms About Double Glazed Window Near Me Double Glazing Window Replacement
Why You Should Focus On Improving Handbag Tommy Hilfiger Nearby
20 Important Questions To To Ask About Double Glazed Windows Near Me Before You
Purchase Double Glazed Windows Near Me double Glazed
Pretty nice post. I simply stumbled upon your weblog and wanted to mention that I’ve really loved
surfing around your blog posts. In any case I will be subscribing on your rss feed and I hope you write once more soon!
Undeniable Proof That You Need Car Key Cover Fiat 500 Fiat 500 Key Fob Replacement
I am sure this paragraph has touched all the internet visitors,
its really really good article on building up new weblog.
10 Wrong Answers To Common Michael Kors Black Handbag Questions Do
You Know The Correct Answers? Kors Michael Handbag
You’ll Never Guess This Audi Car Key Replacement Cost’s Tricks
audi key programmer; Shalanda,
Searching For Inspiration? Check Out Ford Keys Cut Replace ford key
10 Tell-Tale Symptoms You Need To Get A New CSGO Cases Highest Roi Operation phoenix weapon Case
The Most Significant Issue With Link Login Gotogel, And How You Can Fix It Link Alternatif gotogel
Five Killer Quora Answers On Audi A3 Key Replacement replacement
15 Gifts For The CSGO Most Profitable Cases Lover In Your Life Operation Wildfire Case
10 Healthy Habits For Double Glazing Offers Near Me double glazed window handles [Mason]
На сайте https://kozirki.info/ посмотрите увлекательный, интересный и любопытный сериал «Острые козырьки». Здесь находятся все 6 сезонов. Фильмы в отличном качестве, с хорошим звуком, а потому смотреть их – одно удовольствие. У сериала 81 просмотр. Сайт отличается комфортной, удобной навигацией, а потому не составит труда подобрать ту серию, на которой вы остановились прошлый раз или начать просмотр заново. Если какая-то серия произвела эффект, то вы сможете поставить лайк, чтобы поделиться мнением с другими.
5 Killer Quora Answers On Online Shopping Home Office Binding Machine
See What Ford Car Key Replacement Tricks The Celebs Are Using Key
15 Pinterest Boards That Are The Best Of All Time About Bunk Bed Double double Bunkbed –
https://humanlove.Stream/ –
4 Dirty Little Secrets About Repairing Upvc Windows Industry Repairing Upvc Windows Industry Upvc window repair
20 Irrefutable Myths About Tommy Hilfiger Bags Ladies: Busted
tommy hilfiger shoulder handbags (https://minecraftathome.com)
Guide To Car Key Spares: The Intermediate Guide The Steps To Car Key
Spares car Key spare
5 Killer Quora Answers To Designer Bags designer
The Secret Secrets Of Double Glazing Repair Leeds Window repairs Leeds
Die Boomerang Casino App ist die neueste Innovation im Bereich Online GlГјcksspiel. Mit dieser spannenden App kГ¶nnen Spieler ihre Lieblingsspiele jederzeit und Гјberall genieГџen. Egal ob am Strand, zu Hause oder unterwegs – mit der Boomerang Casino App sind die aufregenden Casino-Spiele nur ein paar Klicks entfernt.
Die App bietet eine Vielzahl von beliebten Casino-Spielen, darunter Slots, Roulette, Blackjack und vieles mehr. Spieler können aus einer Vielzahl von Spielen wählen und ihr Glück versuchen, um fantastische Preise zu gewinnen.
Darüber hinaus bietet die Boomerang Casino App zahlreiche Boni und Aktionen für Spieler. Von Willkommensboni für neue Spieler bis hin zu treuen Boni für bestehende Kunden, die App belohnt Spieler für ihre Loyalität und ihren Einsatz.
Die Boomerang Casino App zeichnet sich auch durch ihre benutzerfreundliche Oberfläche und ihr ansprechendes Design aus. Spieler können leicht navigieren und finden schnell ihre Lieblingsspiele. Darüber hinaus bietet die App eine sichere und geschützte Spielumgebung, um sicherzustellen, dass die persönlichen Daten der Spieler geschützt sind.
Insgesamt ist die Boomerang Casino App eine großartige Möglichkeit für Spieler, ihre Lieblingsspiele unterwegs zu genießen. Mit einer Vielzahl von Spielen, Boni und einer benutzerfreundlichen Oberfläche ist die App ein Muss für alle Casino-Enthusiasten. Laden Sie die App noch heute herunter und tauchen Sie ein in die aufregende Welt des Online-Glücksspiels. Viel Spaß und viel Glück!
https://boomerangcasino.one/
Watch This: How Autowatch Ghost Installers Is
Gaining Ground And What You Can Do About It autowatch Ghost installers nottingham
What’s The Current Job Market For Double Glazed Window Repairs Professionals
Like? double Glazed window repairs
Ten Mobile Car Door Lock Repair-Related Stumbling Blocks
You Should Not Share On Twitter Fix car Door near me [stes.tyc.Edu.tw]
http://cialist.pro/# Generic Cialis price
Your means of describing the whole thing in this article is
in fact fastidious, every one can effortlessly be
aware of it, Thanks a lot.
How To Determine If You’re At The Right Level For Double Glazing Repair Near Me cheap
double glazed windows (Alina)
Хотите смотреть интересные фильмы и сериалы совершенно бесплатно и в отличном качестве? Лордс вам в этом поможет. Вы можете, посмотреть любимый фильм онлайн и не ждать пока его покажут по телевизору. Проведите свое свободное время радостно. smotret.lords.lat – https://smotret.lords.lat здесь смотреть фильмы онлайн всегда удобно. Безупречное качество, огромная база, ненавязчивый интерфейс сделают незабываемым домашний киносеанс. Фильмы, представленные на нашем сайте, могут избавить вас от депрессии, смотрите их прямо сейчас!
This Is The Advanced Guide To Mesothelioma Law
Firm forest park mesothelioma Lawyer
5 People You Oughta Know In The Shopping Online Industry Easy-Assembly Bottle Storage
For Whom Is Window Repair Near And Why You Should Care upvc window repair near Me
How To Identify The Upvc Repairs Near Me Which Is Right For You
window repair Near me; qooh.me,
New And Innovative Concepts Happening With Online Shopping Sites Oval Multi Colored Braided Rug
Are You Responsible For The Windows Replacement Budget?
12 Ways To Spend Your Money Double Glazed windows replacement
The Reasons To Work With This Accident Litigation accident law firm
12 Sbobet Facts To Inspire You To Look More
Discerning Around The Cooler Water Cooler goblok
Ten Situations In Which You’ll Want To Be Educated About Work From
Home Jobs No Experience work from home jobs liverpool
10 Amazing Graphics About Charity Shop Online Clothes Uk Vimeo
Pvc Window Repairs: What’s The Only Thing Nobody Is Discussing upvc Window repairs
A Peek Into Beko Washing Machines Uk‘s Secrets Of Beko Washing Machines Uk
The 10 Scariest Things About Replacement Glass For Windows Replacement Glass For Windows
Five Killer Quora Answers To Audi A4 Key Replacement audi A4 key replacement
10 Healthy Habits For Replacement Volkswagen Key Volkswagen golf replacement key
The Advanced Guide To Outdoor Couches For Sale Black couch
On the website https://expertoption-app.online/ you can view and download the Expert Option application for all devices and you will have instant access to trading anywhere. Expert Option is a high level options trading with over 150 assets to trade. More details on the website.
The Most Valuable Advice You Can Ever Receive On Birth Defect Law Elkhorn Birth defect law firm
Ein Promo-Code ist eine fantastische Möglichkeit, um in Online-Casinos zusätzliche Vorteile zu erhalten. Der Zet Casino Promo-Code für 2023 verspricht spannende Bonusangebote und Belohnungen für alle Spieler.
Wenn Sie den Promo-Code für Zet Casino 2023 verwenden, können Sie von verschiedenen Boni profitieren, darunter Einzahlungsboni, Freispiele und Cashback-Angebote. Diese zusätzlichen Vorteile können Ihre Gewinnchancen erhöhen und Ihr Spielerlebnis noch aufregender machen.
Um den Promo-Code zu nutzen, müssen Sie einfach während der Registrierung oder Einzahlung den entsprechenden Code eingeben. Sobald der Code bestätigt wurde, werden die Bonusangebote automatisch Ihrem Konto gutgeschrieben.
Es ist wichtig zu beachten, dass Promo-Codes oft bestimmten Bedingungen und Umsatzanforderungen unterliegen. Bevor Sie einen Promo-Code nutzen, sollten Sie daher die entsprechenden Geschäftsbedingungen sorgfältig durchlesen, um sicherzustellen, dass Sie die Voraussetzungen erfüllen.
Mit dem Zet Casino Promo-Code für 2023 haben Sie die Möglichkeit, Ihr Glück auf die Probe zu stellen und großartige Preise zu gewinnen. Nutzen Sie diese aufregende Gelegenheit und tauchen Sie ein in die Welt des Online-Glücksspiels mit zusätzlichen Boni und Belohnungen. Viel Spaß und viel Erfolg beim Spielen!
https://zetcasino.one/
The One Window Repair Near Mistake That Every Newbie Makes upvc repairs
The No. 1 Question Everybody Working In Double Glazing In Luton Should Know
How To Answer replacement double glazed glass only near Me
buy kamagra online usa: kamagra oral jelly – Kamagra 100mg price
10 Mobile Apps That Are The Best For Slot Demo Gratis demon Slot
Guide To Glass Window Replacement: The Intermediate Guide The
Steps To Glass Window Replacement glass Window replacement
This Is The Ultimate Guide To Personal Injury Attorneys Vimeo
Beware Of This Common Mistake With Your Smallest American Fridge Freezer
american freezer
How Window Repair Near Has Become The Most Sought-After Trend
In 2023 upvc window repair Near me
This Story Behind Upvc Window Repair Will Haunt You
Forever! Window Replacement Near Me
order cenforce buy cenforce order cenforce
You’ll Never Guess This Dreamebot L30 Ultra’s
Secrets L30 Ultra
Интересуетесь улучшить свои английский? Окунитесь в увлекательный мир английского языка через фильмы и сериалы на английском и британском языках. Насладитесь процессом освоения, погружаясь в привлекательные сюжеты и диалоги на языке оригинала. Фильмы и сериалы на английском не только помогут вам расширить словарный запас, но и сделают лучше понимание английской языка на слух. Используйте просмотры сериалов на английском в качестве занимательного метода освоения. Подробнее на сайте https://serialy-na-angliiskom.pp.ua
15 Gifts For The CSGO Cases Value Lover In Your
Life case shadow [https://www.google.at]
What Is The Reason? Ghost Installation Is Fast Becoming The
Most Popular Trend For 2023 bmw x6 Ghost Installer
What’s The Job Market For Window Repairs Leeds Professionals Like?
window repairs Leeds
The 10 Most Scariest Things About Self Emptying Robot Vacuum Pet
Hair Good
Who Is Window Repair Near And Why You Should
Care upvc window repair near me
Bentley Continental Key Tools To Help You Manage Your Daily Life Bentley
Continental Key Trick That Everyone Should
Be Able To bentley continental key
На сайте https://vernissazh.ru забронируйте гостевой дом «Вернисаж». До пляжа, набережной, моря всего несколько метров. А с террасы каждый гость получает возможность насладиться живописным, красивым видом. Почти все развлечения, а также достопримечательности, аттракционы расположены в нескольких метрах. В гостевом доме находятся 14 номеров. Круглосуточное размещение гостей, а на территории находится бесплатный интернет. При необходимости будет организована встреча из Симферополя. Гости смогут воспользоваться бесплатной парковкой.
10 Situations When You’ll Need To Know About Audi A3 Key Battery spare audi key
8 Tips For Boosting Your Windows Repairs Game double glazed window repairs near me
How Do You Know If You’re In The Right Place For
CSGO Case New Cs20 Case
Need Inspiration? Try Looking Up Car Diagnostic Price Uk vauxhall diagnostics near Me (https://ondashboard.win/)
5 Laws That’ll Help To Improve The Upvc Windows Repair
Industry Upvc window Repair
The Reason You Shouldn’t Think About Making
Improvements To Your Double Glazing Near Me door
Very nice post. I just stumbled upon your weblog and wished to
say that I’ve truly enjoyed surfing around your blog posts.
In any case I will be subscribing to your rss
feed and I hope you write again very soon!
Вам нужны высококачественные услуги электрика, гарантии по выгодной цене и в кратчайшие сроки? Тогда звоните нам. Вы получите компетентную помощь. Квалифицированные сотрудники используют исключительно современное оборудование, они готовы выполнить электромонтажные работы любой сложности. Можете им доверять. Ищете вызов электрика? Electrician-perm.ru – сайт, где вы увидите цены и услуги. Мы с ответственностью подходим ко всем заказам и ваши потребности удовлетворим. Предлагаем способы оплаты удобные. Обращайтесь, работаем только для вас!
How Fiat 500 Key Impacted My Life The Better new key For Fiat 500
Zet Casino ist ein Online-Casino, das bei Spielern auf der ganzen Welt sehr beliebt ist. Es bietet eine Vielzahl von Spielen, darunter Spielautomaten, Tischspiele und Live-Casino-Spiele. Das Casino ist für seine großzügigen Boni und Promotionen bekannt, die es seinen Spielern ermöglichen, ihr Spielerlebnis zu maximieren.
Eine der besten Möglichkeiten, um alle aktuellen Angebote und Aktionen von Zet Casino zu verfolgen, ist die Website AskGamblers. AskGamblers ist eine der renommiertesten und vertrauenswürdigsten Casino-Review-Seiten im Internet. Auf der Website können Spieler Bewertungen lesen und sich über die neuesten Entwicklungen in der Casino-Branche informieren.
Zet Casino AskGamblers bietet Spielern auch die Möglichkeit, ihre eigenen Erfahrungen mit dem Casino zu teilen und Feedback zu geben. Auf diese Weise können andere Spieler von der Meinung und den Tipps anderer profitieren. Darüber hinaus bietet die Website regelmäßig exklusive Boni und Angebote für ihre Leser an.
Wenn Sie also ein Fan von Zet Casino sind und immer auf dem neuesten Stand bleiben möchten, sollten Sie unbedingt die Seite AskGamblers besuchen. Dort finden Sie alle Informationen, die Sie benötigen, um das Beste aus Ihrem Casino-Erlebnis herauszuholen. Besuchen Sie noch heute die Seite und lassen Sie sich von den spannenden Angeboten von Zet Casino überraschen!
https://zetcasino.one/
20 Myths About Bags Prada: Dispelled Prada Bags For Sale – Qooh.Me –
The Reason Why Adding A Slot Demo Gratis Pragmatic Play
No Deposit To Your Life Will Make All The Difference demo slot
pg shop, https://www.comonox.com/iframe/hatena_bookmark_comment?Canonical_uri=https://olderworkers.com.au/author/kesmi53rx8-jenniferlawrence-uk/,
Why Do So Many People Want To Know About Mobile Car
Diagnostics? Diagnostic for car near me
20 Myths About Togel Online: Busted must a nice
Are You Responsible For An What CSGO Cases Should I Open Budget?
Twelve Top Ways To Spend Your Money Horizon case – Minecraftathome.Com,
See What Ai Rewrite Text Tricks The Celebs Are Making Use
Of ai rewrite text
How To Become A Prosperous Window Repair Near When You’re Not Business-Savvy Upvc window Repairs
How Ghost Installation Rose To Become The #1 Trend In Social Media audi rs3 ghost installer
zocor debate – lipitor enough atorvastatin percy
Ten Stereotypes About Mobile Diagnostic That Don’t Always Hold engine diagnostics [Julia]
Terrific article! That is the type of info that
should be shared across the net. Disgrace on the seek engines for now
not positioning this submit upper! Come on over and seek advice
from my website . Thanks =)
The Three Greatest Moments In Leeds Door Panels History
upvc hinge repair leeds – Phillipp –
https://levitrav.store/# Levitra 20 mg for sale
A Affordable Search Engine Optimization Success Story You’ll Never Be Able To search engine optimisation Consultants london
Unquestionable Evidence That You Need Replacement Windows Leeds Upvc window hinge repair leeds [minecraftcommand.science]
The Steve Jobs Of Double Glazing Fitters Near Me Meet One Of The Double Glazing
Fitters Near Me Industry’s Steve Jobs Of The Double Glazing Fitters
Near Me Industry double door
15 Terms That Everyone Who Works In Upvc Windows Repair
Industry Should Know Upvc Repairs
I was extremely pleased to discover this website.
I wanted to thank you for ones time for this fantastic
read!! I definitely savored every bit of it and i also have you book-marked to see new stuff in your web site.
Every weekend i used to pay a visit this website,
as i want enjoyment, for the reason that this this
web site conations genuinely nice funny information too.
What you composed made a great deal of sense.
However, think about this, what if you were to write a killer headline?
I ain’t saying your content isn’t good., however suppose you added
a post title to possibly grab folk’s attention? I mean Hey Ho, You’re on ECMO –
This Mommy’s Heart is a little plain. You might look at
Yahoo’s front page and see how they write article headlines to grab viewers to click.
You might try adding a video or a pic or two to get people
excited about what you’ve got to say. In my opinion, it would make your website a little
livelier.
15 Inspiring Facts About Double Glazed Window Leeds You’ve Never Seen upvc Window hinge repairs Leeds
Ten Locksmith Near Me Cars That Really Help You Live Better Locksmith Near Me Cars
Boomerang Casino Freispiele
Im Boomerang Casino gibt es eine Vielzahl von Freispielen, die den Spielern zusätzliche Gewinnchancen bieten. Diese Freispiele können für bestimmte Spielautomaten oder Tischspiele verwendet werden und bieten die Möglichkeit, ohne zusätzliche Kosten zu spielen und echtes Geld zu gewinnen.
Die Freispiele im Boomerang Casino können auf verschiedene Arten erhalten werden. Einige werden als Willkommensbonus für neue Spieler angeboten, während andere als Belohnung für treue Kunden vergeben werden. Darüber hinaus gibt es regelmäßige Aktionen und Promotionen, bei denen Spieler Freispiele gewinnen können.
Um die Freispiele im Boomerang Casino zu nutzen, müssen die Spieler die jeweiligen Bedingungen beachten. Dies beinhaltet in der Regel bestimmte Umsatzanforderungen und eine begrenzte Gültigkeitsdauer. Es ist wichtig, diese Informationen sorgfältig zu lesen, um sicherzustellen, dass die Freispiele optimal genutzt werden können.
Die Freispiele im Boomerang Casino können eine großartige Möglichkeit sein, um das Spielerlebnis zu verbessern und die Gewinnchancen zu erhöhen. Mit einer breiten Auswahl an verschiedenen Spielen und regelmäßigen Aktionen gibt es immer neue Möglichkeiten, um Freispiele zu erhalten und den Spielspaß zu steigern.
Insgesamt bieten die Boomerang Casino Freispiele eine spannende Möglichkeit, um zusätzliche Gewinne zu erzielen und die Vielfalt der verfügbaren Spiele zu genießen. Mit etwas Glück und Geschick können die Spieler mit den Freispielen im Boomerang Casino große Gewinne erzielen und den Spaß am Spiel auf die nächste Stufe heben.
https://boomerangcasino.one/
15 Things You’ve Never Known About Window Repair Near
window repair near me
15 Reasons Not To Ignore Used Couches For Sale cheap Couches
15 Best Lock Smith For Car Bloggers You Must Follow
car key auto locksmith (opensourcebridge.science)
Your Family Will Be Grateful For Having This Automobile Locksmith mobile auto locksmith near Me
Is Your Company Responsible For A Double Glazing Spares Near Me Budget?
Twelve Top Ways To Spend Your Money door
Replacement Key For Nissan Micra Tips To Relax Your Daily Life Replacement Key For Nissan Micra Trick That Everyone Should Know replacement key for nissan micra
wonderful issues altogether, you just received a logo new reader.
What could you suggest about your publish that you
made some days in the past? Any positive?
20 Best Tweets Of All Time About Designer Handbags Large Online Designer
handbags (mazafakas.Com)
Why We Are In Love With Windows Repairs Near Me (And You Should, Too!) Window Replacement, Leewhan.Com,
The Next Big Trend In The Autowatch Ghost Installers Industry ghost tracker Installation
Why You Should Focus On Making Improvements In Advanced Starter
Kits Kit
Why You Should Be Working With This Replacement Ford Fiesta
Key Uk ford kuga key replacement (Willie)
You’ll Never Be Able To Figure Out This Bmw Spare Key
Cost’s Benefits bmw spare key cost
Five Things You’ve Never Learned About Avon Glimmerstick avon true glimmerstick lip
liner (Anita)
Black Friday Sofa Sale Explained In Fewer Than 140 Characters green leather couch, Alisia,
Your Family Will Thank You For Having This Double Glazing Repairs Near Me Double glazing Replacement
This Story Behind Double Glaze Repair Near Me Will Haunt
You For The Rest Of Your Life! upvc double Glazing windows
Where Will Akun Demo Slot 1 Year From Today? Demo slot xo
http://pharmnoprescription.icu/# meds online no prescription
You’ll Never Guess This Replace Window Pane’s Tricks replace window pane (Candra)
15 Current Trends To Watch For CSGO New Case
revolution case (Isaac)
Ten Things You Shouldn’t Share On Twitter Upvc door lock repair leeds (livebookmark.stream)
На сайте https://ruserial-full.net/ находится огромный выбор русских сериалов, которые понравятся всем без исключения. Все они о любви, приятных моментах, чистых чувствах, радости, положительных эмоциях. Фильмы представлены в отличном качестве, с хорошим звуком. Их можно просматривать в любое время и на любом устройстве: планшете, ПК, смартфоне. Есть возможность отсортировать фильмы по жанру: драма, боевик, комедия, криминал, детектив, триллер, мистика. А если хотите найти что-то определенное, то воспользуйтесь специальным поиском.
Why You Should Forget About How To Improve Your How Long Does 18-Wheeler Lawsuit Take Opelika 18 Wheeler Accident Attorney
The 10 Most Scariest Things About Sectionals Sofas sectionals Sofas
What’s The Job Market For Keys For Bmw Professionals
Like? Keys for bmw
Das Boomerang Casino gehört zu den beliebten Online-Casinos, die eine Vielzahl von Spielen und Boni für die Spieler anbieten. Eine wichtige Funktion in jedem Casino ist die Auszahlung von Gewinnen an die Spieler. Im Boomerang Casino gibt es verschiedene Methoden und Richtlinien für die Auszahlung, die es wert sind, näher betrachtet zu werden.
Die Auszahlungen im Boomerang Casino können mit verschiedenen Zahlungsmethoden wie Kreditkarten, E-Wallets und Banküberweisungen erfolgen. Die Spieler können die für sie am besten geeignete Option auswählen. Bei der Auszahlung wird darauf geachtet, dass die Spieler ihr Geld sicher und schnell erhalten. Die Auszahlungszeiten können je nach Zahlungsmethode variieren, aber das Casino bemüht sich, die Auszahlungen so schnell wie möglich zu bearbeiten.
Es ist wichtig zu beachten, dass im Boomerang Casino bestimmte Richtlinien für Auszahlungen gelten. Zum Beispiel müssen die Spieler möglicherweise bestimmte Umsatzanforderungen erfüllen, bevor sie ihre Gewinne abheben können. Diese Anforderungen können je nach Aktion und Bonus variieren, daher ist es ratsam, die Geschäftsbedingungen sorgfältig zu lesen.
Die Spieler können sich jederzeit an den Kundensupport des Boomerang Casinos wenden, wenn sie Fragen zur Auszahlung haben. Das Supportteam ist rund um die Uhr erreichbar und steht den Spielern mit professioneller Hilfe zur Seite.
Insgesamt bietet das Boomerang Casino seinen Spielern eine zuverlässige und sichere Auszahlungsmethode. Die Spieler können sich darauf verlassen, dass sie ihre Gewinne problemlos abheben können. Mit einer Vielzahl von Zahlungsmethoden und einer effizienten Kundenbetreuung ist die Auszahlung im Boomerang Casino ein einfacher und angenehmer Prozess.
https://boomerangcasino.one/
The 10 Most Terrifying Things About Situs Alternatif Gotogel
Situs alternatif gotogel
What Is Peugeot Car Key Replacement Cost And Why You Should
Consider Peugeot Car Key Replacement Cost peugeot key replacement – Christena –
10 Websites To Help You To Become An Expert
In Leeds Window Repair Double Glazed Door Repair Leeds
This Is How Double Glazing Repair Leeds Will Look In 10 Years Time
upvc door lock repair leeds (Merle)
http://pharmmexico.online/# mexican online pharmacies prescription drugs
3 Ways In Which The Window Repair Near Can Influence Your Life
upvc window repair Near Me (http://www.stes.tyc.Edu.tw)
10 Fundamentals On Sectional Sofa With Storage You Didn’t Learn In The Classroom oversized Sectionals
What’s The Current Job Market For Car Locks Smith Professionals Like?
car locks Smith
The 10 Most Scariest Things About Replacement
Keys For Bmw Replacement keys for bmw
На сайте https://incubatoreggs.ru/ закажите качественное, экологически чистое инкубационное яйцо индейки, курицы, утки, гуся, а также различных других домашних птиц. Вся продукция поставляется от ведущих фабрик России, Европы. Компания работает без выходных, а бесплатная доставка от 3000 рублей. У компании имеются пункты выдачи, чтобы вы смогли забрать продукцию в целости. А если хотите найти что-то определенное, то воспользуйтесь специальным поиском. Все яйцо всегда свежее, ароматное и подходит для приготовления различных блюд.
How Much Do Glass Repair Leeds Experts Earn? upvc Window repair leeds
9 Signs You’re An Expert Windows Replacement Expert Double glazed windows Replacement
What Freud Can Teach Us About CSGO Skin Case Sites
global offensive
What You Should Be Focusing On Making Improvements Double
Glazed Window Near Me double glazing front Door
15 Weird Hobbies That’ll Make You Smarter At Uk Online Shoe Shopping Websites k&n performance parts 2005-2011 Bmw
10 Startups That Are Set To Revolutionize The CSGO Most Profitable Cases
Industry For The Better operation wildfire case
Хотите приобрести по недорогой стоимости из нержавеющей стали клапаны и арматуру? Мы вам в этом с удовольствием поможем. Главные достоинства нашей продукции: долгий срок эксплуатации и большая надежность. Ищете арматура из нержавейки для пищевого производства? Inoxpa.ru – сайт, где вы узнаете о том, где используется арматура из нержавеющей стали. Здесь также можете в любое удобное для вас время ознакомиться с высококачественной продукцией проверенной компании INOXPA. Возникли вопросы? Обратитесь к нам, мы с радостью на них ответим. Звоните!
The Reasons Michael Kors Handbag Is More Dangerous Than You Realized Michael Kors Bags Grey
best online pharmacy india indian pharmacy world pharmacy india
15 Terms That Everyone Within The Leather Sofas For Sale
Industry Should Know lovesac couch sale [Bella]
20 Things You Need To Know About Car Central Lock Repair Electronic Lock Repair Near Me
Велнес-клуб премиум-класса BIOSFERA https://biosfera-club.ru/ на Ленинском проспекте и Шаболовской это тренажерный зал, фитнес и групповые программы, бассейн с банным комплексом, SPA-салон и инновационный центр функциональной диагностики. Зайдите на сайт – узнайте больше об услугах и их стоимости.
9 . What Your Parents Teach You About Replace Window
Handles Replace Window Handles
Das Zet Casino hat für das Jahr 2021 einen exklusiven Promo-Code veröffentlicht, der Spielern die Möglichkeit bietet, von großzügigen Boni und Angeboten zu profitieren. Der Code kann bei der Registrierung oder bei der Einzahlung in das Casino eingegeben werden und gewährt den Spielern zusätzliche Boni wie Freispiele oder Bonusguthaben.
Mit dem Zet Casino Promo-Code 2021 können Spieler ihre Gewinnchancen erhöhen und länger spielen, ohne dabei ihr eigenes Geld riskieren zu müssen. Dies stellt eine großartige Möglichkeit für neue Spieler dar, das Casino kennenzulernen und sich mit den verschiedenen Spielen vertraut zu machen.
Das Zet Casino bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele, Live-Casino-Spiele und vieles mehr. Mit dem Promo-Code können Spieler diese Spiele mit zusätzlichem Bonusguthaben entdecken und möglicherweise sogar den Jackpot knacken.
Es ist wichtig, den Promo-Code korrekt einzugeben, um sicherzustellen, dass man von den Angeboten profitieren kann. AuГџerdem sollten die Bonusbedingungen und -bedingungen genau gelesen werden, um sicherzustellen, dass man die Bedingungen erfГјllt und das Bonusguthaben erfolgreich in Echtgeld umwandeln kann.
Insgesamt bietet das Zet Casino Promo-Code 2021 eine großartige Möglichkeit, um noch mehr Spaß und Spannung beim Spielen zu erleben. Nutzen Sie den Code, um Ihre Gewinnchancen zu erhöhen und die Vielfalt der Spiele im Casino zu entdecken. Viel Glück und viel Spaß beim Spielen!
https://zetcasino.one/
See What Seo Backlink Building Software Tricks
The Celebs Are Utilizing backlink building Software
На сайте https://pravovoivihod.ru пройдите тест для того, чтобы узнать, подходит ли вам бесплатная процедура, предполагающая списание долга через МФЦ. При этом вы сможете получить еще и 2 подарка. Вы сможете списать долги, кредиты, сумма которых не превышает 200 000. У компании огромный опыт работы – 8 лет в области банкротства. Именно поэтому с вашей проблемой, независимо от ее сложности, справятся в минимальные сроки. Более 1 500 человек уже успешно списали долги, почти 2,6 млрд. кредитов отдали.
14 Businesses Are Doing A Fantastic Job At Car Ghost Immobiliser fit
What’s The Job Market For Double Glazed Window Repairs
Professionals? Double Glazed Window Repairs
Need Inspiration? Try Looking Up Window Repair Near upvc window repair
near me (Ned)
online canadian pharmacy: best canadian pharmacy online – safe online pharmacies in canada
На сайте https://ar26.ru/ специально для вас подберут наиболее выгодную, подходящую под все параметры недвижимость, которая будет доступна по цене. Кроме того, специалисты подготовят все необходимые документы, чтобы сделка прошла наиболее комфортно для вас. Сотрудники не только помогут найти лучший вариант, но и оформят сделку, гарантируют отличный результат. Также на сайте вы отыщите полезные, информативные новости на данную тему. Все специалисты отличаются высокой квалификацией, чтобы предоставить услуги на должном уровне.
The 10 Scariest Things About American-Style Fridge Freezers best american fridge freezers uk
The Lesser-Known Benefits Of Situs Alternatif Gotogel
Casino online
This Is The Good And Bad About Scooters For Sale Mobility New Mobility scooters for sale
Renault Key Replacement Near Me Tools To Streamline Your Daily Life Renault
Key Replacement Near Me Technique Every Person Needs To Be Able To renault key replacement Near me
7 Simple Changes That’ll Make The Difference With Your Saab 93 Key saab key replacement –
Tobias,
10 Tips For Quickly Getting Car Door Unlock Service Lock out Assistance
I really like it when people get together and share ideas.
Great website, continue the good work!
The 10 Scariest Things About Replacement Handles For Upvc Windows replacement handles for upvc windows
Guide To Marc Jacobs Bags: The Intermediate Guide
In Marc Jacobs Bags Marc Jacobs Bags
Unexpected Business Strategies For Business That Aided Buy Mobility Scooter Near Me To Succeed buy Mobility scooter accessories
15 Startling Facts About Link Login Gotogel That You Didn’t Know Link Alternatif Gotogel
simvastatin upon – simvastatin cat lipitor noon
Backlink pyramid
Sure, here’s the text with spin syntax applied:
Link Structure
After many updates to the G search engine, it is required to employ different approaches for ranking.
Today there is a method to attract the attention of search engines to your site with the aid of incoming links.
Backlinks are not only an effective promotional instrument but they also have natural visitors, immediate sales from these resources probably will not be, but visits will be, and it is poyedenicheskogo visitors that we also receive.
What in the end we get at the end result:
We show search engines site through links.
Prluuchayut organic transitions to the site and it is also a sign to search engines that the resource is used by individuals.
How we show search engines that the site is profitable:
Backlinks do to the main page where the main information.
We make backlinks through redirections reputable sites.
The most SIGNIFICANT we place the site on sites analytical tools separate tool, the site goes into the cache of these analyzers, then the acquired links we place as redirects on weblogs, discussion boards, comments. This important action shows search engines the MAP OF THE SITE as analyzer sites present all information about sites with all key terms and headings and it is very GOOD.
All information about our services is on the website!
The 10 Scariest Things About How To Get Spare Car Key how to
get spare car key (Armando)
10 Inspiring Images About Asbestos Claim Asbestos Lawyer
What’s The Current Job Market For Double Glazed Window Repairs Professionals
Like? Double glazed Window repairs
5 Clarifications On Window Repair Near window repair near me (http://kbphone.co.kr/bbs/board.php?bo_table=free&wr_id=833936)
Do Not Believe In These “Trends” About Marc Jacobs Camera Bag marc jacobs handbags Black
See What Window Replacement Cost Tricks The Celebs Are Making Use Of replace
Where Do You Think Designer Handbags Red Be One Year From What Is Happening Now?
Designer Handbags Chanel
10 Signs To Watch For To Buy A Bentley Continental Gt Key Fob bentley replacement
key – https://timeoftheworld.date/wiki/The_UnderAppreciated_Benefits_Of_Replacement_Key_For_Bentley_Continental_Gt,
“The CSGO Battle Case Awards: The Most, Worst, And The Most Bizarre Things We’ve Seen Case Skins
9 Things Your Parents Taught You About Gotogel
Link Alternatif gotogel link alternatif (m.ns1.unicycle.kr)
See What Best Robot Vacuum Self Empty Tricks The
Celebs Are Using best robot Vacuum self empty
These Are The Most Common Mistakes People Make When Using
Repairs To Upvc Windows Upvc Window repairs
20 Trailblazers Are Leading The Way In Mattresses Double Size Adjustable Base
The Next Big New Slot Demo Industry akun demo nolimit city (http://temtrack.com/public/tr.php?c=240&clk=2364206549&mid=92248&ema=robert@plantdelights.com&url=aHR0cHM6Ly93YXlyYW5rcy5jb20vYXV0aG9yL2dyb3VuZHJ1YjkxLTE1MzE1OS8)
Zet Casino Auszahlungszeit
Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und groГџzГјgigen Boni fГјr seine Spieler bietet. Eines der wichtigsten Dinge, die Spieler beachten sollten, wenn sie in einem Online-Casino spielen, ist die Auszahlungsdauer. In diesem Artikel werden wir uns genauer mit der Zet Casino Auszahlungszeit befassen.
Die Zet Casino Auszahlungszeit hängt von verschiedenen Faktoren ab, darunter die gewählte Auszahlungsmethode und der Verifizierungsprozess des Spielers. In der Regel dauert die Bearbeitungszeit für Auszahlungen bei Zet Casino zwischen 24 und 48 Stunden. Sobald die Auszahlung genehmigt wurde, hängt die tatsächliche Überweisungsdauer von der gewählten Zahlungsmethode ab.
Spieler können bei Zet Casino zwischen verschiedenen Auszahlungsmethoden wählen, darunter Kreditkarten, E-Wallets und Banküberweisungen. E-Wallets wie Skrill und Neteller bieten in der Regel die schnellsten Auszahlungszeiten, während Banküberweisungen aufgrund von Bearbeitungszeiten bei den Banken länger dauern können.
Es ist wichtig zu beachten, dass Spieler ihre Identität überprüfen müssen, bevor sie eine Auszahlung bei Zet Casino beantragen können. Dies dient dazu, die Sicherheit der Spieler zu gewährleisten und Betrug zu verhindern. Spieler sollten sicherstellen, dass sie alle erforderlichen Dokumente zur Verfügung haben, um den Verifizierungsprozess so reibungslos wie möglich zu gestalten.
Insgesamt bietet Zet Casino seinen Spielern eine schnelle und zuverlässige Auszahlungsdauer. Spieler können sich darauf verlassen, dass ihre Gewinne schnell und sicher ausgezahlt werden, damit sie ihr Geld schnell genießen können. Wenn Sie nach einem Online-Casino mit schnellen Auszahlungen suchen, ist Zet Casino definitiv einen Besuch wert.
https://zetcasino.one/
You’ll Never Guess This Upvc Window Repair Near Me’s Secrets upvc window repair near Me
The Most Innovative Things That Are Happening With 3 Piece Sectional
Sofa green sectional Sofa
Asking questions are actually good thing if you are
not understanding anything entirely, except this piece of writing gives
fastidious understanding even.
10 Facts About Local Window Repair That Make You Feel Instantly
A Good Mood upvc windows repair near Me
Why Nobody Cares About Small Double Bed Mattress double mattress in sale [https://hikvisiondb.webcam/wiki/20_Trailblazers_Lead_The_Way_In_Small_Double_Bed_Mattress]
http://pharmindia.online/# buy prescription drugs from india
canada pharmacy no prescription: online medication without prescription – canadian pharmacy online no prescription needed
Why No One Cares About Robot Vacuum lidar robot vacuum
10 Things You Learned In Kindergarden That’ll Help You With Window Pane Replacement installing
What’s The Current Job Market For Double Glazing Door Repairs Near Me Professionals?
door repair (crane-bredahl-2.hubstack.Net)
5 Killer Quora Answers On Double Glazed Window Repairs Near
Me double glazed Window repairs near me
Hello, this weekend is pleasant designed for me, because this occasion i am reading
this great educational paragraph here at my house.
The Often Unknown Benefits Of Double Glazing Companies Near
Me best double glazing companies near me
See What Audi Key Fobs Tricks The Celebs Are Utilizing audi key
На сайте https://newturkishserials.ru/ ознакомьтесь с топом самых популярных турецких сериалов, которые понравятся всем, кто любит интересный, незаурядный сюжет, яркие, положительные эмоции. На странице вы получите полную, исчерпывающую информацию о таких сериалах, как: «Великолепный век», «Бесконечная любовь», «Любовь напрокат», «Судьба», «Сыла: Возвращение домой». Вы узнаете о каждом сериале, сюжете, а также моральных, эмоциональных моментах. Кроме того, получите информацию о том, насколько популярны турецкие сериалы и почему они нравятся многим.
What Is The Reason Double Glazing Leeds Is Right For You?
Conservatory door Repairs leeds
Bentley Continental Key Tools To Ease Your Everyday Lifethe Only Bentley Continental Key Trick That Should Be Used By Everyone Learn bentley continental key
10 Life Lessons We Can Learn From Replacing Lost Car Keys Ford Ford Key Fob Replacement
Dangerous Drugs Tips To Relax Your Everyday Lifethe Only
Dangerous Drugs Trick That Every Person Should Know carthage dangerous drugs attorney
10 Myths Your Boss Has About Repairs To Upvc Windows
window doctor near me
Buzzwords De-Buzzed: 10 Other Methods For Saying Window London sash window repairs east london
The Reasons You’re Not Successing At Clitoral Stimulators clitoral Vibratoe
Hey there, You’ve done an excellent job. I’ll definitely digg it and personally suggest to my friends.
I am sure they will be benefited from this site.
See What Lightweight Folding Mobility Scooters Tricks The
Celebs Are Making Use Of lightweight folding mobility scooters
Hi there just wanted to give you a quick heads up.
The words in your content seem to be running off the
screen in Ie. I’m not sure if this is a formatting issue or something to do
with browser compatibility but I figured I’d post to let you know.
The style and design look great though! Hope you get the issue
solved soon. Cheers
Online Shopping Sites List For Clothes Tools To
Ease Your Daily Lifethe One Online Shopping Sites List For Clothes Technique Every Person Needs To Be
Able To online shopping sites list for clothes – https://M.dduckhamji.com/,
online meds no prescription how to get prescription drugs from canada quality prescription drugs canada
5 Laws Everybody In Repair Double Glazed Windows Should Know window repairs (Blondell)
7 Simple Secrets To Completely You Into Repairs To Upvc Windows Upvc Repair
What’s The Current Job Market For Misty Double Glazing Repair Professionals Like?
double glazing repair (Leewhan.Com)
9 Signs You’re A Leeds Door And Window Expert door repair leeds (Erika)
Tipico ist eine beliebte Online-GlГјcksspielplattform, die eine Vielzahl von Casino-Spielen und Sportwetten anbietet. In letzter Zeit gab es jedoch einige Kontroversen darГјber, dass Tipico nur das Casino-Konto von Spielern sperren kann, nicht aber das Konto fГјr Sportwetten.
Dies hat bei einigen Spielern zu Verwirrung und Unzufriedenheit geführt, da sie der Meinung sind, dass sie ihr gesamtes Konto sperren lassen sollten, wenn sie Probleme mit Glücksspielen haben. Diejenigen, die süchtig sind oder Schwierigkeiten haben, ihr Spielverhalten zu kontrollieren, könnten sich durch eine bloße Sperrung des Casino-Kontos nicht ausreichend geschützt fühlen.
Tipico hat erklärt, dass es gesetzlich vorgeschrieben ist, dass Spieler die Möglichkeit haben müssen, nur das Casino-Konto zu sperren, ohne das gesamte Konto schließen zu müssen. Dies soll den Spielern ermöglichen, weiterhin Sportwetten zu platzieren, wenn sie dies wünschen, ohne auf das gesamte Angebot von Tipico verzichten zu müssen.
Dennoch fordern einige Spieler und Experten eine strengere Regulierung und Kontrolle im Glücksspielbereich, um gefährdete Spieler besser zu schützen. Sie argumentieren, dass das Risiko von Spielsucht und finanziellen Problemen durch eine stärkere Regulierung reduziert werden kann.
Es bleibt abzuwarten, ob Tipico auf die Kritik reagieren und Maßnahmen ergreifen wird, um die Sicherheit und den Schutz der Spieler zu verbessern. In der Zwischenzeit sollten Spieler, die Schwierigkeiten mit Glücksspielen haben, sich bewusst sein, dass sie die Möglichkeit haben, ihr Casino-Konto bei Tipico sperren zu lassen, sollten sie dies für notwendig erachten.
https://tipicocasino.one/
Key For Bmw Tools To Ease Your Daily Lifethe One Key For Bmw Trick That Should Be Used By Everyone
Be Able To key for bmw (https://notabug.org/buffetguitar56)
Why All The Fuss About Locksmith Near Me For Cars?
car locksmith mobile – q-steam.Com –
I like the helpful info you provide in your articles.
I will bookmark your blog and check again here frequently.
I am quite certain I’ll learn lots of new stuff right here!
Good luck for the next!
What Is The Reason? Dreame L30 Review Is Fast Becoming The Hot Trend For
2023? Dreame bot l30
A Positive Rant Concerning Upvc Window Repairs window repairs Near me
That is a very good tip especially to those new to the blogosphere.
Brief but very precise info… Many thanks for sharing this one.
A must read article!
See What Car Key Replacement Ford Tricks The Celebs Are Making Use Of Key replacement ford
Why Adding Ford Ka Replacement Key Fob To Your Life Can Make
All The Difference ford car key replacement
Sectional Couches For Sale: The Good And Bad About Sectional Couches For Sale spacious
Изучение английского языка по телесериалам – отличный способ улучшать язык. Телесериалы для базового уровня помогут освоить базовые слова, а для продвинутого – увеличить словарный запас. Субтитры в телесериалах на британском помогут в понимании контекста. Как изучать английский по сериалам? Просто окунитесь в английский язык смотря и слушая любимые сериалы! Смотреть и изучать английский языка можно на сайте https://serialy-na-anglijskom.pp.ua/
The 10 Most Scariest Things About Link Alternatif Gotogel link alternatif gotogel
10 Things You Learned In Kindergarden They’ll
Help You Understand Double Glazing Company Near Me double glazing
replacement units – Woodrow –
20 Reasons Why Fiat 500 Replacement Key Will Never Be Forgotten fiat 500x key Not detected
Your Worst Nightmare About Car Key Cover Fiat 500 Be Realized
replacement fiat fiorino keys nottingham
13 Things About Best Online Shopping Sites London You May Not Have Known jolie papier online Shop uk amazon
Hi, this weekend is fastidious in favor of me, because this
occasion i am reading this wonderful informative post here
at my residence.
Link Login Gotogel Tools To Ease Your Daily Lifethe One
Link Login Gotogel Trick That Everyone Should
Learn Link Login gotogel
5 Must-Know-Practices Of Replacement Fiat Key For 2023
fiat ducato replacement key (Dianne)
The 10 Scariest Things About Treadmills For Sale Near Me treadmills For sale near me
Hello there! Would you mind if I share your blog with my
myspace group? There’s a lot of folks that I think would really appreciate your content.
Please let me know. Cheers
What’s The Job Market For Nissan Qashqai Key Replacement Price Professionals?
Nissan Qashqai Key Replacement Price
15 Reasons To Love Sectional Sofa With Storage Honbay Sectional Sofa
india online pharmacy: pharmacy website india – indian pharmacy
15 Secretly Funny People In Sectional Sofa sectional sofas for sale – Edison –
15 Terms That Everyone Within The Bentley Continental Key Fob Industry Should Know Bentley Key repair
Ten Taboos About Mobile Car Door Lock Repair You Should Never Share On Twitter car Lock actuator repair
This Week’s Top Stories About Upvc Window Repairs Upvc Window Repairs upvc window repairs near me (Lucas)
Vehicle Diagnostics Near Me 101: The Ultimate Guide For
Beginners vauxhall diagnostics – http://bbs.theviko.com/home.Php?mod=space&uid=784899,
A Peek Inside The Secrets Of Leeds Windows upvc door repairs roundhay
14 Cartoons About Malpractice Lawsuit To Brighten Your Day malpractice lawyer
Why Double Glazing Door Repairs Near Me Is Still
Relevant In 2023 double glazing doors
10 Things That Everyone Is Misinformed About Case Battles CSGO
Case Revolver
На сайте https://detskoe.info/ подберите промокоды, есть информация о распродажах, скидках, а также акциях. Все это позволит приобрести детские вещи, мебель и все необходимое по привлекательной стоимости. Здесь вы найдете и такие товары, за покупку которых предоставляется подарок. На распродажах вы сможете приобрести сразу несколько вещей в гардероб. Для того чтобы приобрести все, что нужно, необходимо просто изучить все необходимые предложения в магазинах, после чего выбрать самые подходящие. Все вещи качественные и прослужат долго.
Guide To Car Key Program Near Me: The Intermediate Guide On Car Key
Program Near Me Car Key Program Near Me – Jorgensen-Schmitt.Thoughtlanes.Net –
Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und Boni anbietet. Aber was sagen die Spieler Гјber ihre Erfahrungen mit diesem Casino? Lassen Sie uns einige Zet Casino Bewertungen genauer betrachten.
Viele Spieler loben Zet Casino für seine große Auswahl an Spielen. Das Casino bietet eine Vielzahl von Slots, Tischspielen und Live-Dealer-Spielen, die für Unterhaltung sorgen. Die Spieler schätzen auch die Benutzerfreundlichkeit der Website und die reibungslose Spielerfahrung, die sie bietet.
Ein weiterer Pluspunkt von Zet Casino sind die großzügigen Boni und Promotionen, die es seinen Spielern bietet. Neue Spieler können sich über einen Willkommensbonus freuen, der ihre erste Einzahlung verdoppelt und ihnen zusätzliche Freispiele verschafft. Darüber hinaus gibt es regelmäßige Aktionen wie Reload-Boni, Cashback-Angebote und Turniere, die den Spielern zusätzliche Gewinnchancen bieten.
Natürlich gibt es auch einige negative Bewertungen von Spielern, die über bestimmte Aspekte von Zet Casino unzufrieden sind. Einige Spieler bemängeln die langen Auszahlungszeiten und den Kundenservice, der nicht immer schnell auf Anfragen reagiert. Es ist wichtig zu beachten, dass diese Bewertungen subjektiv sind und von den individuellen Erfahrungen abhängen.
Insgesamt scheint Zet Casino eine gute Wahl fГјr Spieler zu sein, die nach einer Vielzahl von Spielen und groГџzГјgigen Boni suchen. Bevor Sie sich jedoch anmelden, ist es ratsam, die Bewertungen anderer Spieler zu lesen und sicherzustellen, dass das Casino Ihren Erwartungen entspricht.
https://zetcasino.one/
Check Out What Birth Injury Claim Tricks Celebs Are Utilizing
Vimeo
10 Inspirational Graphics About Emergency Window Repair Window repairs
Situs Gotogel Terpercaya Tools To Improve Your Everyday Lifethe Only Situs
Gotogel Terpercaya Trick That Everybody Should Learn Situs Gotogel Terpercaya
(Hikvisiondb.Webcam)
What The Heck What Is Coffee Machines Beans? Coffee Machine Beans
A Time-Travelling Journey: How People Talked About Online Avon 20 Years Ago Avon Online Ordering
Your Worst Nightmare About Buy Espresso Machine Come To Life coffee
Excellent post. I used to be checking constantly this weblog and I’m inspired!
Very useful information specifically the final phase
🙂 I handle such info much. I was looking for this certain info for a
long time. Thank you and good luck.
What’s The Current Job Market For Double Glazing Door Repairs Near
Me Professionals? door repair (https://www.plantsg.com.sg/)
Five Things Everybody Gets Wrong On The Subject Of Custom Sectional Sofa Customizable Sectionals
How Robot Vacuum Cleaner With Mop Has Become The Most Sought-After Trend In 2023 the Best robot vacuum cleaner
What’s The Job Market For Link Daftar Gotogel Professionals?
link daftar gotogel – https://kisamisulog.hatenablog.com/iframe/hatena_bookmark_comment?canonical_uri=https://cs-upgrade.top/user/sunmark75/,
Solutions To Issues With Upvc Window Repairs window replacement
From All Over The Web The 20 Most Amazing Infographics About Glass
Window Replacement Window Glass Replacement (Luxuriousrentz.Com)
Why You Must Experience Car Diagnostic Price Uk
At A Minimum, Once In Your Lifetime bmw Diagnostics
You Will Meet The Steve Jobs Of The Double Glazing Fitters Near
Me Industry replace
Hi! I’ve been reading your weblog for some time now and finally got the bravery to go ahead and give you a shout
out from Dallas Texas! Just wanted to tell you keep up the excellent job!
На сайте https://pro100-stone.ru рассчитайте то, сколько будет стоить изготовление, производство изделий, выполненных из искусственного камня. В этой компании получится заказать подоконники, столешницы, раковины, мойки, ресепшен и многое другое. Есть возможность создать как горизонтальную, так и вертикальную поверхность. Это отличный вариант для самых разных помещений, включая рестораны, учебные заведения, офисы, магазины. Все изделия отличаются высокой практичностью, надежностью.
10 Healthy Personal Injury Lawsuit Habits Fort Lauderdale Personal Injury Attorney
10 Replacement Audi Key Tricks All Experts Recommend audi key Programming
What You Must Forget About Making Improvements To Your Work Home From Jobs Make Money Working From Home
What’s The Reason Prada Handbags Nylon Is Fast Becoming The Most Popular Trend In 2023 Prada Bag Women
A New Trend In Second Hand Folding Mobility Scooters folding mobility scooters For sale near Me
https://pharmnoprescription.icu/# buy pain meds online without prescription
medications online without prescriptions no prescription pharmacy order prescription drugs online without doctor
12 Companies Setting The Standard In Avon Sign Up Kit starter
The Advanced Guide To Uk Online Grocery Shopping Sites Newborn Sleep Solution (Pedro)
Boomerang Casino Einzahlungscode: Holen Sie sich zusätzliche Belohnungen für Ihre Einzahlungen
Boomerang Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und Bonusangeboten für seine Spieler bereithält. Eines der aufregendsten Angebote, das das Casino seinen Spielern bietet, ist der Boomerang Casino Einzahlungscode. Mit diesem speziellen Code haben Spieler die Möglichkeit, zusätzliche Belohnungen für ihre Einzahlungen zu erhalten und ihr Spielerlebnis noch spannender zu gestalten.
Der Boomerang Casino Einzahlungscode funktioniert ganz einfach: Spieler geben den Code bei ihrer Einzahlung im Casino ein und erhalten dann zusätzliche Belohnungen wie Freispiele, Bonusgelder oder andere spannende Angebote. Der Code kann je nach Aktion und Promotion variieren, daher sollten Spieler regelmäßig die Promotionsseite des Casinos überprüfen, um den aktuell gültigen Code zu erhalten.
Um den Boomerang Casino Einzahlungscode zu nutzen, müssen Spieler lediglich ein Konto im Casino erstellen und eine Einzahlung tätigen. Der Code kann dann im Einzahlungsfenster eingegeben werden, um die zusätzlichen Belohnungen zu aktivieren. Es lohnt sich, den Code zu verwenden, da er Spielern die Möglichkeit bietet, ihr Spielerlebnis zu verbessern und mehr Gewinne zu erzielen.
Zusätzlich zum Boomerang Casino Einzahlungscode bietet das Casino auch viele andere spannende Bonusangebote und Aktionen für seine Spieler. Mit regelmäßigen Promotionen, Turnieren und Gewinnspielen gibt es immer etwas Spannendes, auf das sich die Spieler freuen können.
Insgesamt ist der Boomerang Casino Einzahlungscode eine großartige Möglichkeit für Spieler, zusätzliche Belohnungen für ihre Einzahlungen zu erhalten und ihr Spielerlebnis im Casino zu verbessern. Nutzen Sie also diese spannende Möglichkeit und holen Sie sich noch mehr Gewinne im Boomerang Casino!
https://boomerangcasino.one/
What’s The Job Market For Window.Replacement Near Me Professionals?
window.replacement near me
The 10 Most Terrifying Things About Double Glazing Firms Near Me double Glazed door handles
You Are Responsible For An Double Glazing In Leeds Budget?
12 Top Notch Ways To Spend Your Money Repair Double glazing
Three Common Reasons Your Birth Defect Lawsuit Isn’t Working
(And How To Fix It) chillicothe birth Defect lawsuit
Ten Myths About Window Repair Near That Aren’t
Always True Upvc Window Repair Near Me
Стремитесь улучшить свои языковые навыки? Погрузитесь в увлекательный мир английского языка с помощью наших кинокартин и сериалов на английском и британском языках. Насладитесь процессом обучения, погружаясь в интригующие сюжеты и диалоги на языке оригинала. Наши фильмы и сериалы не только помогут вам расширить словарный запас, но и улучшат понимание английской речи и культуры. Используйте просмотры в качестве увлекательного метода обучения. Подробнее тут https://filmy-na-anglijskom-yazyke.pp.ua/
На сайте http://nemans.ru вы сможете приобрести всю необходимую продукцию, включая пакеты с ручками, фасовочные пакеты, мешки полипропиленовые, пленку армированную, полиэтиленовую. Также в разделе имеется ветошь, ароматное мыло, перчатки, черенки, бытовая химия, ведра и многое другое, что вы сможете заказать прямо сейчас. Среди рекомендованных товаров находятся вязаные перчатки, туалетная бумага, хозяйственное мыло, неткол. Вся продукция отличного качества, надежная и наделена длительными сроками эксплуатации.
Car-scales.ru предлагает вам приобрести автомобильные весы по приемлемой стоимости. Мы ценим и любим своих клиентов. Гарантируем персональный подход. Обратившись к нам, вы получите только качественную продукцию. У нас есть то, что вам необходимо. Ищете весы автомобильные электронные? Car-scales.ru – сайт, где можете в любое удобное для вас время заказать автовесы. Поставка будет осуществлена точно в указанный срок. Уровню обслуживания мы уделяем пристальное внимание. С радостью готовы ответить на интересующие вас вопросы, и помочь сделать верный выбор. Звоните нам прямо сейчас!
You’ll Never Guess This Renault Card Key Replacement’s Tricks renault card key replacement
Why You Should Focus On Improving CSGO Battle Case Case Revolution – https://Olderworkers.Com.Au/Author/Whsyx51Sick2Rx-Gemmasmith-Co-Uk/ –
After a long struggle and legal battle, asbestos-related
measures resulted in the 1989 partial ban on the manufacturing processing, distribution, and distribution of the majority of asbestos-containing products.
This ban is still in force.
Stop by my blog post … vimeo.com
See What Manhattan Birth Injury Attorneys Tricks The Celebs Are Making Use
Of Manhattan Birth injury attorneys
The 10 Scariest Things About Lightweight Automatic Folding
Mobility Scooters lightweight automatic Folding mobility scooter
Nine Things That Your Parent Taught You About Window Sash Replacement Window sash Replacement
Three Common Reasons Your Westfield Birth Injury Attorneys Isn’t Working
(And Solutions To Resolve It) birth injury attorneys redlands (http://www.ace-ace.co.jp/cgi-bin/ys4/rank.cgi?mode=link&id=26651&url=https://olderworkers.com.au/author/puhip34lm-marymarshall-co-uk/)
10 Things That Your Family Taught You About Audi A3 Replacement Key audi a3 replacement Key
Why Double Glazed Front Doors Near Me Is Your Next Big Obsession installed
9 . What Your Parents Teach You About Recliner Couches For Sale recliner Couches For sale
5 Laws That Anyone Working In Door Fitters Leeds Should
Know door repairs leeds – https://maps.google.com.sl/url?q=https://jensby-aggerholm-3.thoughtlanes.net/10-things-youve-learned-From-kindergarden-theyll-help-you-understand-leeds-double-glazing,
The Most Convincing Proof That You Need Michael Kors Bag michael kors designer bags
10 Things That Your Family Teach You About Comfortable Couches For Sale comfortable Couches For sale
5 Work From Home Jobs No Experience Uk Projects That Work For Any Budget work from home jobs in Birmingham
A Step-By’-Step Guide For Bentley Key Programming replacement key for bentley continental gt
mexico drug stores pharmacies: mexican online pharmacies prescription drugs – best online pharmacies in mexico
Tipico Casino NJ ist eine neues Online-Casino in New Jersey, das Spielern ein aufregendes und sicheres Spielerlebnis bietet. Das Casino, das von der bekannten Marke Tipico betrieben wird, bietet Spielern eine Vielzahl von Spieloptionen, darunter Spielautomaten, Tischspiele und Live-Dealer-Spiele.
Ein wichtiger Aspekt von Tipico Casino NJ ist die Sicherheit der Spieler. Das Casino verwendet die neueste Technologie, um sicherzustellen, dass alle persönlichen Daten und Transaktionen der Spieler geschützt sind. Spieler können also beruhigt sein, dass ihre Informationen sicher sind, während sie ihre Lieblingsspiele genießen.
Ein weiterer großer Vorteil von Tipico Casino NJ ist die große Auswahl an Spielen, die es Spielern bietet. Von klassischen Spielautomaten bis hin zu verschiedenen Varianten von Blackjack, Roulette und anderen Tischspielen gibt es für jeden Spieler etwas zu entdecken. Darüber hinaus bietet das Casino auch Live-Dealer-Spiele, die ein authentisches Casino-Erlebnis bieten und es den Spielern ermöglichen, mit echten Dealern und anderen Spielern zu interagieren.
Tipico Casino NJ bietet auch großzügige Boni und Aktionen für neue und bestehende Spieler an. Von Willkommensboni über Einzahlungsboni bis hin zu Treueprogrammen gibt es viele Möglichkeiten, um zusätzliches Geld und Belohnungen zu verdienen. Diese Boni können Spielern helfen, ihr Guthaben zu erhöhen und mehr Zeit mit ihren Lieblingsspielen zu verbringen.
Insgesamt ist Tipico Casino NJ eine groГџartige Option fГјr Spieler in New Jersey, die ein erstklassiges Online-Casino-Erlebnis suchen. Mit einer breiten Palette von Spielen, erstklassiger Sicherheit und lukrativen Boni ist das Casino eine gute Wahl fГјr alle, die SpaГџ und Spannung suchen. Besuchen Sie noch heute Tipico Casino NJ und beginnen Sie mit dem Spielen!
https://tipicocasino.one/
Creating hyperlinks is just as efficient now, only the tools for working in this field possess changed.
There are actually several possibilities to backlinks, our team employ some of them, and these approaches operate and have been tried by us and our customers.
Lately our team carried out an test and it transpired that less frequent queries from one website position nicely in search results, and the result does not have to be your domain name, you are able to utilize social networks from Web 2.0 collection for this.
It additionally it is possible to in part shift load through site redirects, giving an assorted backlink profile.
Go to our own website where our solutions are actually provided with thorough overview.
На сайте https://pluryal.info/ каждый желающий получает возможность заказать филлеры, которые отличаются премиальным качеством из Европы. Продукция представлена более чем в 70 странах. Компания находится на рынке более 13 лет, а потому заполучила признание постоянных клиентов. Препараты имеют сертификаты качества, что подтверждает серьезные намерения. Имеются филлеры для повышения упругости, сияния кожи, придания свежего вида и бархатистости, а также те, что корректируют морщины, гусиные лапки.
See What Tommy Hilfiger Bag Handbag Tricks The Celebs
Are Utilizing tommy hilfiger bag handbag (Amos)
This Is How Does Amazon Ship To Uk Will Look Like In 10 Years Time
Bb-62 Model Kit
What’s The Job Market For Bmw Series 1 Key Professionals?
bmw series 1 key
20 Trailblazers Leading The Way In Ultra Lightweight Electric Wheelchair Ultralight Electric Wheelchair
5 Killer Queora Answers On Coffee Machines With Beans Espresso Coffee Machine With Grinder
25 Surprising Facts About Repairs To Double Glazing Double Glazing Repairs
16 Must-Follow Pages On Facebook For CSGO Cases Highest Roi-Related Businesses chroma Case
Personal Injury Legal: What’s The Only Thing
Nobody Is Discussing north College hill personal injury Lawyer
10 Meetups Around Window Repair You Should Attend window replacement
10 Things That Your Family Taught You About Upvc Windows Near Me upvc windows near me (http://www.mazafakas.Com)
rosuvastatin online easy – zetia scar caduet online lamp
Avon Sales Book 101: The Ultimate Guide For Beginners Avon Sales book
“Boomerang Casino DE: Ein aufregendes Online-Casino-Erlebnis”
Boomerang Casino DE ist ein innovatives Online-Casino, das Spielern eine Vielzahl von spannenden Spielen und großzügigen Boni bietet. Mit einer benutzerfreundlichen Benutzeroberfläche und einer Vielzahl von Zahlungsmöglichkeiten ist Boomerang Casino DE die ideale Wahl für alle, die nach einem unterhaltsamen und lohnenden Online-Casino-Erlebnis suchen.
Eine der Hauptattraktionen von Boomerang Casino DE sind die vielen Spiele, die es seinen Spielern bietet. Von klassischen Spielautomaten bis hin zu Live-Casino-Spielen bietet Boomerang Casino DE eine Vielzahl von Optionen, aus denen Spieler wählen können. Darüber hinaus arbeitet das Casino mit einigen der besten Spieleentwickler der Branche zusammen, darunter NetEnt, Microgaming und Betsoft, um sicherzustellen, dass seine Spieler die bestmögliche Spielerfahrung genießen.
Abgesehen von der Auswahl an Spielen bietet Boomerang Casino DE auch großzügige Boni und Sonderaktionen für seine Spieler an. Neue Spieler können sich auf Willkommensboni und Freispiele freuen, während treue Spieler regelmäßig mit Bonusangeboten und Prämien belohnt werden. Das Casino veranstaltet auch regelmäßig Turniere und Wettbewerbe, bei denen Spieler die Chance haben, zusätzliche Preise zu gewinnen.
Ein weiterer Vorteil von Boomerang Casino DE ist die Vielzahl von Zahlungsmöglichkeiten, die es seinen Spielern bietet. Spieler können Ein- und Auszahlungen bequem und sicher über eine Vielzahl von Zahlungsmethoden tätigen, darunter Kreditkarten, E-Wallets und Banküberweisungen.
Insgesamt ist Boomerang Casino DE eine ausgezeichnete Wahl fГјr Spieler, die nach einem unterhaltsamen und lohnenden Online-Casino-Erlebnis suchen. Mit einer breiten Auswahl an Spielen, groГџzГјgigen Boni und einer benutzerfreundlichen BenutzeroberflГ¤che bietet Boomerang Casino DE alles, was Spieler brauchen, um ein erstklassiges Casinoerlebnis zu genieГџen. Besuchen Sie noch heute Boomerang Casino DE und erleben Sie die Aufregung und den Nervenkitzel des Online-GlГјcksspiels!”
https://boomerangcasino.one/
7 Tricks To Help Make The Maximum Use Of Your Glazing Repairs Near Me Double Glazing Near Me
https://pharmmexico.online/# mexican border pharmacies shipping to usa
14 Businesses Doing A Great Job At Prada Shoulder Bag
Prada Bags Men
7 Simple Tips To Totally Rocking Your Injury Litigation lake geneva injury
law firm – https://Vimeo.com/707179523,
medications online without prescription online pharmacies no prescription pharmacy no prescription required
What Is The Reason Best Robot Vacuum Mop For Pet Hair Is The Best Choice For You?
Best Buy
How To Tell The Double Glazing Door Repairs Near Me That’s Right For You
double Glazing door
What Is It That Makes Marc Jacobs Tote Bag Leather So Famous?
Marc Jacobs Bag Outlet (Verbina-Glucharkina.Ru)
7 Simple Tricks To Rocking Your Anal Sex Toys Uk Toys For Anal
Индексация ссылок на сайте vindexe.ru
rosuvastatin online cold – zetia buy success caduet pills bad
Why Do So Many People Want To Know About Coffee Pod Machine?
Espresso And coffee combo machines
15 Amazing Facts About Idn Poker You’ve Never Heard Of spam
Five Things You Don’t Know About Used Sofas For Sale beige Sectional couch
(https://Willysforsale.com/)
See What Glass Repair Leeds Tricks The Celebs Are Using glass repair leeds (Meghan)
5 Killer Quora Answers To Automatic Vacuum And Mop Robot
Automatic vacuum and mop robot
The Car Diagnostic Price Mistake That Every Beginning Car Diagnostic Price User Makes solutions
На сайте https://ruserial-full.net/ посмотрите все самые интересные, увлекательные сериалы за прошлые или нынешние года. Для того чтобы сориентироваться в выборе, необходимо определиться с жанром. В каталоге находятся драмы, боевики, триллеры, мистика, а также детективы, криминал, комедии, мелодрамы. Все это в отличном качестве, с хорошим звуком, поэтому доставит только положительные эмоции. Изучите раздел с самыми популярными фильмами, которые просматривает большинство. Здесь также находятся и новинки.
What’s The Ugly The Truth About Repairing Upvc Windows Upvc window Repair
What Is Best Buy Mobility Scooters And How To Utilize It best folding Mobility scooter
Das Tipico Casino ist einer der beliebtesten Anbieter von Online-Casinospielen in Deutschland. Es bietet seinen Kunden eine breite Auswahl an spannenden Spielen, darunter Slots, Roulette, Blackjack und vieles mehr. Doch in letzter Zeit häufen sich die negativen Berichte über das Tipico Casino. Viele Spieler berichten von Problemen bei der Auszahlung von Gewinnen, technischen Schwierigkeiten und einem insgesamt schlechten Kundenservice.
Einige Spieler klagen darüber, dass sie ihre Gewinne nicht auszahlen lassen können, obwohl sie alle notwendigen Bedingungen erfüllt haben. Andere berichten von Verzögerungen bei der Auszahlung oder sogar davon, dass ihr Konto ohne Begründung gesperrt wurde. Diese Probleme führen zu Frust und Unzufriedenheit bei den Kunden, die sich eigentlich eine sichere und unterhaltsame Spielerfahrung im Tipico Casino erhofft hatten.
Auch die technische Seite des Casinos scheint nicht zu funktionieren wie gewГјnscht. Viele Spieler berichten von Problemen beim Laden der Spiele, AbstГјrzen der Software und Verbindungsproblemen. Dies fГјhrt zu einem frustrierenden Spielerlebnis und kann dazu fГјhren, dass die Kunden das Casino verlassen und ihr GlГјck bei einem anderen Anbieter versuchen.
Zusätzlich wird auch der Kundenservice des Tipico Casinos kritisiert. Viele Spieler berichten von langen Wartezeiten bei der Beantwortung von Anfragen und einer allgemeinen Unzufriedenheit mit der Kommunikation des Casinos. Dies ist besonders ärgerlich, wenn es um wichtige Fragen zu Ein- und Auszahlungen oder technischen Problemen geht.
Insgesamt lässt die aktuelle Situation beim Tipico Casino zu wünschen übrig. Die Spieler erwarten ein sicheres und unterhaltsames Spielerlebnis, das leider nicht immer gewährleistet zu sein scheint. Es bleibt zu hoffen, dass das Tipico Casino diese Probleme in den Griff bekommt und wieder zu einem verlässlichen und beliebten Anbieter für Online-Casinospiele wird.
https://tipicocasino.one/
Enough Already! 15 Things About Playboy Pornstars We’re Tired Of Hearing Playboy model
See What Blown Double Glazing Repairs Tricks The Celebs Are
Utilizing Double Glazing Repair
13 Things You Should Know About Best Shark Robot Vacuum
That You Might Not Have Known best robot Vacuum under 200
You’re About To Expand Your CSGO Case Opening Battle Options case Shadow
The People Nearest To Mobile Car Diagnostics Have Big Secrets To Share system Diagnostic
buy pills without prescription: overseas online pharmacy-no prescription – canadian and international prescription service
The Best Replacement Key For Nissan Micra Tips To Transform Your Life replace Nissan key Fob
The No. Question That Everyone In Double Bed Mattress Should Know How To Answer double mattress width, severinsen-Clapp-2.blogbright.net,
How Do I Explain Cheap Couches For Sale To A
Five-Year-Old folding Couch bed
See What Designer Handbags Tricks The Celebs Are Using Handbag
Why Medical Malpractice Attorney Isn’t A Topic That People
Are Interested In Medical Malpractice Attorney Lawyer
See What Side By Side Fridge And Freezer Pair Tricks
The Celebs Are Using Side by side fridge and freezer pair
Why You’ll Need To Learn More About Espresso Maker
coffee and espresso maker
11 Ways To Completely Sabotage Your Double Glazing Deals Near Me Front
20 Bmw Key Fob Replacement Websites Taking The Internet By Storm Replacement Bmw Key Fob (Minecraftathome.Com)
A Peek Into The Secrets Of Fiat Key Fob Replacement fiat key Cutting
5 Idn Poker Projects For Any Budget tolol
The Leading Reasons Why People Are Successful In The Fiat Punto Key Replacement Industry fiat key Programmer
The 9 Things Your Parents Taught You About Link Login Gotogel link login Gotogel
The Next Big Thing In The Double Glazing Doors
Repairs Industry double glazing Repairs
What’s The Most Common Repair Double Glazing Window Debate It’s
Not As Black And White As You Think services
Der Boomerang Casino Code ist ein exklusiver Bonuscode, der es Spielern ermöglicht, besondere Angebote und Belohnungen im Boomerang Casino zu erhalten. Dieser Code kann verwendet werden, um Bonusgelder, Freispiele oder andere Vergünstigungen zu erhalten.
Um den Boomerang Casino Code zu nutzen, müssen Spieler einfach während des Einzahlungsvorgangs den Code eingeben. Sobald der Code akzeptiert wurde, wird der entsprechende Bonus automatisch dem Spielerkonto gutgeschrieben.
Der Boomerang Casino Code bietet Spielern die Möglichkeit, ihr Spielerlebnis im Casino zu verbessern und ihre Gewinnchancen zu erhöhen. Mit den zusätzlichen Bonusgeldern oder Freispielen können Spieler mehr Spiele ausprobieren und ihre Chancen auf einen großen Gewinn steigern.
Es ist jedoch wichtig zu beachten, dass jeder Boomerang Casino Code bestimmte Bedingungen und Umsatzanforderungen haben kann. Spieler sollten daher die Bonusbedingungen genau lesen, um sicherzustellen, dass sie die Vorgaben erfüllen und den Bonus optimal nutzen können.
Insgesamt ist der Boomerang Casino Code eine großartige Möglichkeit für Spieler, mehr aus ihrem Spiel herauszuholen und zusätzliche Vergünstigungen zu erhalten. Wer sein Glück im Boomerang Casino versuchen möchte, sollte daher nicht vergessen, den exklusiven Bonuscode zu nutzen und von den zusätzlichen Belohnungen zu profitieren.
https://boomerangcasino.one/
The Reason Why Fridge Is Everyone’s Obsession In 2023 small fridge
What’s The Job Market For Double Glazed Window Repairs Professionals Like?
double glazed window repairs [Eartha]
15 Hot Trends Coming Soon About Uk Online Phone Shopping Sites Fire Pit Safety
A Look At The Myths And Facts Behind Freezers For Garages Freezers On Sale
The No. 1 Question Anyone Working In What CSGO Cases Have Butterfly Knives
Should Be Able Answer operation riptide Case
Сериал Уэнсдeй смотреть онлайн
Best Automatic Folding Mobility Scooter Uk Tools To Help You Manage Your Daily Life Best Automatic Folding Mobility Scooter Uk Trick That Every Person Must Know Best Automatic Folding Mobility Scooter Uk
The 10 Most Terrifying Things About Situs Gotogel
Terpercaya situs gotogel terpercaya – tujuan.grogol.us,
Do Not Make This Blunder With Your Erb’s Palsy Litigation norridge erb’s palsy law firm
4 Dirty Little Secrets About The Sleeper Sofas For Sale Industry sofa sale Savings
10 Sites To Help You Learn To Be An Expert In Leeds Window
Repair leeds double glazing repairs
5 Laws That Anyone Working In Commercial Espresso Machine
Should Be Aware Of Espresso Home Machine
How Folding Treadmill Incline Arose To Be The Top Trend On Social Media best folding Treadmills
online pharmacy discount code canadian pharmacy world coupon online pharmacy no prescription needed
Sash Window Replacement Tools To Make Your Everyday Lifethe Only
Sash Window Replacement Trick Every Person Should Learn sash window replacement
10 Key Factors Regarding Car Accident Compensation You Didn’t Learn In School car Accidents
Das Tipico Casino ist eines der beliebtesten Online-Casinos in Deutschland. Viele Spieler begeistern sich für die große Auswahl an Spielen und die benutzerfreundliche Oberfläche. Doch trotz aller positiven Aspekte gibt es immer wieder Berichte darüber, dass einige Spieler keine Gewinne erzielen.
Es ist wichtig zu erwähnen, dass Glücksspiel immer mit einem gewissen Risiko verbunden ist und Gewinne nie garantiert werden können. Dennoch häufen sich die Beschwerden von Spielern, die angaben, dass sie keine oder nur sehr geringe Gewinne im Tipico Casino erzielen konnten.
Ein Grund für die fehlenden Gewinne könnte möglicherweise die hohe Varianz der Casino-Spiele sein. Einige Spiele sind bekannt dafür, dass sie hohe Gewinne auszahlen können, jedoch nur selten. Das bedeutet, dass Spieler viele Runden spielen können, ohne einen nennenswerten Gewinn zu erzielen.
Ein anderer Grund könnte möglicherweise eine falsche Spielstrategie sein. Einige Spieler setzen zu viel Geld auf ein Spiel oder spielen übermäßig lange, was zu Verlusten führen kann. Es ist wichtig, verantwortungsbewusst zu spielen und sich an ein festgelegtes Budget zu halten.
Es gibt aber auch Spieler, die behaupten, dass das Tipico Casino nicht fair spielt und Gewinne zurückhält. Es ist jedoch wichtig zu betonen, dass Online-Casinos strengen Regulierungen unterliegen und regelmäßig von unabhängigen Behörden überprüft werden. Somit sind Manipulationen in seriösen Online-Casinos nahezu ausgeschlossen.
Letztendlich ist es wichtig, sich bewusst zu sein, dass Glücksspiel kein Weg ist, um sicher an Geld zu kommen. Es ist immer mit einem gewissen Risiko verbunden und Gewinne können nicht garantiert werden. Es ist ratsam, verantwortungsbewusst zu spielen und sich im Zweifelsfall an den Kundenservice des Tipico Casinos zu wenden, um mögliche Probleme zu klären.
https://tipicocasino.one/
The 10 Most Scariest Things About Gotogel Link Alternatif Gotogel Link Alternatif
Das Zet Casino ist ein Online-Casino, das bei vielen Spielern aufgrund seines umfangreichen Angebots und seiner benutzerfreundlichen Oberfläche beliebt ist. In diesem Artikel werfen wir einen genauen Blick auf die Bewertung des Zet Casinos.
Das Zet Casino bietet eine groГџe Auswahl an Spielen von renommierten Anbietern wie NetEnt, Microgaming, Play’n GO und vielen mehr. Von Spielautomaten Гјber Tischspiele bis hin zu Live-Casino-Spielen ist fГјr jeden Geschmack etwas dabei. Die Spiele sind gut gestaltet und bieten ein unterhaltsames Spielerlebnis.
Ein weiterer Pluspunkt des Zet Casinos ist der großzügige Willkommensbonus für neue Spieler. Mit einem hohen Einzahlungsbonus und Freispielen können Sie Ihr Spielerlebnis beim Zet Casino sofort verbessern. Darüber hinaus bietet das Casino regelmäßige Aktionen und Boni für bestehende Spieler an.
Die Sicherheit und Fairness des Zet Casinos stehen an erster Stelle. Das Casino verfügt über eine Lizenz der Malta Gaming Authority, einer der angesehensten Glücksspielbehörden der Welt. Zudem verwendet das Casino moderne Verschlüsselungstechnologien, um sicherzustellen, dass Ihre persönlichen Daten geschützt sind.
Der Kundendienst des Zet Casinos ist rund um die Uhr erreichbar und steht Ihnen bei Fragen oder Problemen zur VerfГјgung. Das Support-Team ist freundlich und kompetent und wird Ihnen schnell und effizient helfen.
Insgesamt hinterlässt das Zet Casino einen positiven Eindruck. Mit seinem umfangreichen Spielangebot, großzügigen Boni und einem hervorragenden Kundenservice ist das Zet Casino eine gute Wahl für alle, die gerne online spielen. Probieren Sie es aus und überzeugen Sie sich selbst von der Qualität des Zet Casinos.
https://zetcasino.one/
5 Killer Quora Answers On Gray Sectional Sofa Sectional sofa
The 10 Most Terrifying Things About Replacement Window Glass Replacement Window glass
10 Wrong Answers To Common Akun Demo Slot Questions
Do You Know The Right Answers? gates of olympus slot demo indonesia (Chanda)
Why Nobody Cares About Audi Car Key Audi lost key
This Most Common Bean To Coffee Machines Debate Isn’t As Black Or White As You Might Think Bean-To-Cup Machine
30 Inspirational Quotes On Gotogel Link Alternatif Judi Slot online
You’ll Never Be Able To Figure Out This Nespresso Magimix Coffee Machine’s Tricks nespresso magimix coffee Machine
11 “Faux Pas” You’re Actually Able To Create Using Your Upvc Windows
Repair Upvc window Repairs
Ten Ways To Build Your Slot Demo Gratis Pragmatic Play No Deposit Empire Slot demo pragmatic Terbaru
How To Build A Successful Double Glazing Doors Near Me Even If
You’re Not Business-Savvy double Glazing windows replacement
Why Do So Many People Would Like To Learn More About
Fridge Under Counter? under counter fridge sale
The One Demo Slot Mistake Every Newbie Makes Online Slot Demo
What You Must Forget About Making Improvements To Your Michael
Kors Handbags On Sale Michael Kors Bags Uk
9 . What Your Parents Taught You About Marc Jacobs Handbag Sale
marc jacobs handbag sale (Nicole)
The 10 Most Terrifying Things About Adhd In Adults
Medication adhd in Adults medication
5 Killer Quora Answers To Cheap Bunk Beds For Kids cheap bunk Beds For kids (https://rentry.co/tyt9Emxa)
You’ll Be Unable To Guess Citroen Remote Key Replacement’s Tricks Citroen remote key replacement
mexico drug stores pharmacies: mexican online pharmacies prescription drugs – mexican mail order pharmacies
15 Top Birth Defect Compensation Bloggers You Need To Follow heber springs birth defect lawsuit
5 Killer Quora Answers To Treadmills For Home UK Treadmills for home Uk
Central Locking Key Repair Tools To Ease Your Daily Life Central Locking Key Repair Technique
Every Person Needs To Learn central locking key Repair
Guide To Online Shopping Uk Cheap: The Intermediate Guide On Online Shopping Uk Cheap online shopping uk (m.w.aqus.co.kr)
Tipico Einzahlen und direkt ins Casino einsteigen
Tipico ist einer der beliebtesten Anbieter für Sportwetten und Online-Casino-Spiele. Für diejenigen, die gerne ihre Glücksspiele online spielen, bietet Tipico eine einfache und bequeme Möglichkeit, Geld auf ihr Konto einzuzahlen und direkt in das Casino einzusteigen.
Um Geld auf Ihr Tipico-Konto einzuzahlen, stehen Ihnen verschiedene Zahlungsmethoden zur Verfügung. Dazu gehören Kredit- und Debitkarten, Banküberweisungen, Paysafecard, PayPal und viele weitere Optionen. Egal, für welche Methode Sie sich entscheiden, das Geld wird sicher und schnell auf Ihr Konto eingezahlt.
Sobald das Geld auf Ihrem Konto ist, können Sie sofort mit dem Spielen im Casino beginnen. Tipico bietet eine große Auswahl an Spielen, darunter Slots, Roulette, Blackjack, Poker und mehr. Egal, ob Sie ein Anfänger oder ein erfahrener Spieler sind, es gibt für jeden etwas Passendes.
Das Beste an Tipico ist, dass es eine mobile App für unterwegs gibt. Mit der Tipico-App können Sie auch unterwegs spielen und Einzahlungen vornehmen. Sie können also jederzeit und überall auf Ihre Lieblingsspiele zugreifen.
Wenn Sie also Lust auf ein spannendes Casino-Erlebnis haben, ist Tipico die richtige Wahl. Zahlen Sie einfach Geld auf Ihr Konto ein und steigen Sie direkt ins Casino ein. Viel GlГјck und viel SpaГџ beim Spielen!
https://tipicocasino.one/
Are Reclining Sectional Sofa The Best There Ever Was?
Reclining Sectionals
Zet Casino Free Spins ohne Einzahlung
Das Zet Casino ist bekannt für seine großzügigen Bonusangebote und Promotionen. Unter den vielen tollen Angeboten, die das Casino seinen Spielern bietet, sind die Free Spins ohne Einzahlung besonders beliebt. Diese bieten Spielern die Möglichkeit, kostenlos an ausgewählten Spielautomaten zu drehen und echtes Geld zu gewinnen, ohne dabei eigenes Geld einzusetzen.
Um an diesen begehrten Free Spins teilzunehmen, mГјssen Spieler lediglich ein Konto im Zet Casino erstellen. Nach der Registrierung erhalten sie automatisch eine bestimmte Anzahl von Freispielen, die sie sofort nutzen kГ¶nnen. Diese Free Spins kГ¶nnen an verschiedenen Spielautomaten wie Book of Dead, Starburst oder Gonzo’s Quest eingelГ¶st werden, je nach Angebot des Casinos.
Die Gewinne aus den Free Spins ohne Einzahlung unterliegen in der Regel bestimmten Umsatzbedingungen, die erfüllt werden müssen, bevor eine Auszahlung möglich ist. Diese Bedingungen variieren je nach Aktion und können beispielsweise den 30-fachen Umsatz des Gewinnbetrags erfordern. Es ist daher ratsam, die Bonusbedingungen genau zu lesen, um sicherzustellen, dass man die erforderlichen Anforderungen erfüllt.
Zet Casino Free Spins ohne Einzahlung bieten Spielern eine großartige Möglichkeit, das Casino und seine Spiele risikofrei kennenzulernen. Mit etwas Glück können Spieler mit ihren Freispielen attraktive Gewinne erzielen und so ihr Spielerlebnis noch spannender gestalten. Wer also gerne Spielautomaten spielt und auf der Suche nach kostenlosen Gewinnchancen ist, sollte die aktuellen Free Spins Angebote im Zet Casino genau im Auge behalten.
https://zetcasino.one/
You’ll Never Be Able To Figure Out This What Is The Best Online Shopping In Uk’s Benefits Online Shopping
На сайте https://nashi-teplicy.ru/ напишите сообщение для того, чтобы заказать производство теплиц из поликарбоната как в Москве, так и области. Разработка происходит по индивидуальным эскизам заказчика. В каталоге представлены как прямостенные, так и арочные, каплевидные теплицы, парники, навесы. Все они самых разных размеров, а потому сможете подобрать решение под свои предпочтения, требования. На продукцию установлены привлекательные расценки. Также есть и спецпредложения. Организуется доставка по всей России, СНГ.
A New Trend In Judi Bola goblok
20 Rising Stars To Watch In The Shark Robotic Vacuum Cleaner Industry robot vacuum
with self empty (https://maps.google.cat/url?q=http://reali.esport.ge/user/actormint64)
Everything You Need To Be Aware Of Motorcycle Accident Lawyers Motorcycle Accident lawsuit
Three Reasons Why Three Reasons Your Birth Injury Law Is Broken (And How To Fix
It) fair oaks ranch birth injury lawyer
9 Signs That You’re The Drive Auto Folding Scooter Expert Automatic Folding scooter mobility
Five Killer Quora Answers On Link Daftar Gotogel link Daftar gotogel
Guide To Link Login Gotogel: The Intermediate Guide To Link Login Gotogel Link login Gotogel
What Is The Injury Settlement Term And How To Use It injury attorneys; Susana,
8 Tips To Improve Your L30 Dreame Game dreamy l30
What’s The Reason? Erb’s Palsy Lawyers Is Everywhere
This Year west memphis erb’s palsy Lawyer
See What Audi Replacement Key Service Near Me Tricks The Celebs Are Using audi replacement key service near me
17 Reasons You Shouldn’t Be Ignoring Double Glazing Repairs Near Me Double Glazing Near Me
It’s Time To Extend Your Buy Chest Freezer Options freezer options
Guide To Lost Key In Car: The Intermediate
Guide The Steps To Lost Key In Car lost key in car (Zack)
15 Twitter Accounts You Should Follow To Discover More About Birth Injury Legal birth injury Law firms
14 Savvy Ways To Spend Leftover Mesothelioma Attorney Budget hire a mesothelioma attorney
Guide To Best Robot Vacuum For Pet Hair Self Emptying: The Intermediate Guide Towards Best Robot Vacuum For Pet
Hair Self Emptying Best Robot Vacuum For Pet Hair Self Emptying
10 Life Lessons That We Can Learn From Programming Car Keys key programer; Rentry.co,
10 Key Porsche-Related Projects To Extend Your Creativity porsche Keys
10 Signs To Watch For To Know Before You Buy Bunk Beds For Children Bunk beds On sale
What Is Online Shopping Stores In London And Why Is Everyone Speakin’ About It?
Jolie papier online shop Uk amazon
15 Interesting Facts About Repairing Double Glazed Windows That You Never
Knew glazier
10 Things Everybody Has To Say About Which Is Best For Online Grocery Shopping Which Is Best For Online Grocery Shopping off-road gear ratio Kit
Ten Myths About Slot Demo Gratis Pragmatic Play No Deposit That Aren’t Always True slot demo bandito; Fredric,
5 Killer Quora Answers To Treadmills Sale Treadmills Sale (Economics.Ut.Ac.Ir)
20 Things You Need To Know About Grey Sectional
Sofa gray Sectional sofa
The 10 Most Scariest Things About Railroad Accident Lawyer accident lawyer
Boomerang Casino ist ein Online-Casino, das eine Vielzahl von Spielen und Bonusangeboten fГјr seine Spieler anbietet. Eines der beliebtesten Angebote sind die Boomerang Casino no deposit bonus codes.
Diese Bonus-Codes ermöglichen es Spielern, kostenlose Geldbeträge oder Freispiele zu erhalten, ohne eine Einzahlung tätigen zu müssen. Diese Aktionen sind ideal für Spieler, die das Casino und seine Spiele kennenlernen möchten, ohne dabei eigenes Geld riskieren zu müssen.
Um die Boomerang Casino no deposit bonus codes zu erhalten, müssen Spieler in der Regel einen speziellen Code eingeben, der auf der Casino-Website veröffentlicht wird. Nach der Eingabe des Codes wird der Bonus automatisch auf das Spielerkonto gutgeschrieben.
Die Bonus-Codes von Boomerang Casino sind eine großartige Möglichkeit, um zusätzliches Spielgeld oder Freispiele zu erhalten und so die Gewinnchancen zu erhöhen. Spieler sollten jedoch darauf achten, die Bonusbedingungen zu lesen, um sicherzustellen, dass sie die Gewinne aus dem Bonus auch tatsächlich behalten können.
Insgesamt sind die Boomerang Casino no deposit bonus codes eine attraktive Möglichkeit, um das Casino und seine Spiele auszuprobieren, ohne dabei eigenes Geld riskieren zu müssen. Spieler sollten regelmäßig die Casino-Website besuchen, um über aktuelle Bonusangebote informiert zu bleiben und so das Beste aus ihrem Spielerlebnis herauszuholen.
https://boomerangcasino.one/
http://pharmnoprescription.icu/# best non prescription online pharmacy
15 Gifts For The Designer Handbags Black Lover In Your Life online designer bags
На сайте https://sobr26.ru получите бесплатную консультацию для того, чтобы узнать все про такую важную и необходимую услугу, как охрана недвижимости, важного объекта. Компания охраняет различные объекты, гарантирует безопасность имущества. Она работает в данном направлении более 20 лет, а потому отличается колоссальным опытом. Все услуги предоставляются «под ключ». Здесь получится заказать, в том числе, и пультовую, личную охрану, а также охрану массовых предприятий. Охрана объекта различного уровня сложности.
It’s The Good And Bad About Attorney For Mesothelioma yonkers mesothelioma attorney (tujuan.grogol.us)
10 Things We All Hate About Online Shopping Top 7 2Mm Thick Rubber Mat (https://Vimeo.com/)
10 Things People Get Wrong Concerning Bmw Spare Key bmw
3 series key fob (Eartha)
На сайте https://taker12.casino поиграйте в интересные игры, которые понравятся своей динамикой, яркостью, а также интересным подходом. Вы сможете заработать себе на мечту, а выигранные средства вы получите очень быстро, а вывести их можно наиболее удобным способом. Прямо сейчас попытайте удачу в самых популярных слотах, которых здесь огромное количество. Не упустите возможность сыграть в Live-игры. Для всех клиентов действуют наиболее выгодные условия, привилегии, бонусы. Вы сможете заработать до 15% по реферальной программе.
buy prescription drugs without a prescription buying online prescription drugs no prescription canadian pharmacies
9 . What Your Parents Teach You About Amazon Online Shopping Clothes Uk Amazon online shopping clothes uk
25 Amazing Facts About Sectional Sofas green sectional sofa
15 Idn Poker Benefits That Everyone Should Be Able To spam
How Tall Larder Freezer Rose To Become The #1 Trend On Social Media freezer sizes (https://Millbrook-Inf.northants.sch.uk/)
10 3 Wheel Scooter For Handicapped That Are Unexpected 3-Wheel mobility scooters
How To Determine If You’re Ready To Go After Designer Handbags Brands designer Handbags pink
What’s The Job Market For Best 9kg Washing Machine Professionals Like?
best 9kg washing machine
The Reasons 18-Wheeler Accident Is More Difficult Than You Imagine
beacon 18 wheeler accident Attorney
Guide To Replacement Upvc Window Handles: The Intermediate Guide
The Steps To Replacement Upvc Window Handles replacement upvc window handles – Rene –
The 10 Scariest Things About Spare Key For My Car Spare key for My car
Where Is Upvc Window Repairs Be One Year From In The Near Future?
upvc window repairs Near me
Вам интересна магия? Заходите на сайт мага Азала. Здесь точно найдете для себя что-то новое. Узнаете, что такое спиритизм, как действует приворот, и какие бывают виды, есть ли домовой в доме и многое другое. Вы можете заказать магическую консультацию уже сейчас. Ищете белый стол? Magomagii.ru – сайт, где можно найти стоимость помощи мага. Тут представлены интересные статьи о магии, в них Азал вкладывал собственные знания, умения, опыт и даже душу. Вопросы в комментариях получают свои ответы. Маг будет рад вас видеть на своем ресурсе.
SightCare formula aims to maintain 20/20 vision without the need for any surgical process. This supplement is a perfect solution for people facing issues as they grow older. https://sightcare-web.com/
What Is Bunk Bed And Why Is Everyone Dissing It?
Buy Bunk Bed
Отыскиваете способ сделать лучше собственное владение английским. Для лучшего понимания можно использовать субтитры на английском. Делайте лучше свой инглиш, наслаждаясь любимыми кинокартинами. Подробнее на сайте https://english-films.pp.ua/.
Boomerang Casino: 50 Freispiele
Boomerang Casino ist ein Online-Casino, das Spielern die Möglichkeit bietet, ihre Lieblingsspiele bequem von zu Hause aus zu spielen. Mit einer Vielzahl von Spielen, großzügigen Boni und einem benutzerfreundlichen Interface ist Boomerang Casino eine beliebte Wahl für viele Glücksspielenthusiasten.
Einer der aktuellen Angebote von Boomerang Casino sind die 50 kostenlosen Spins, die neuen Spielern angeboten werden. Diese Freispiele können auf ausgewählten Spielautomaten gespielt werden und bieten Spielern die Möglichkeit, ihr Glück zu versuchen, ohne dabei eigenes Geld investieren zu müssen.
Um die 50 Freispiele zu erhalten, müssen Spieler einfach ein Konto bei Boomerang Casino erstellen und ihre Kontaktdaten bestätigen. Sobald dies erledigt ist, werden die Freispiele automatisch dem Konto gutgeschrieben und können sofort verwendet werden.
Diese Freispiele sind eine großartige Möglichkeit für Spieler, das Angebot von Boomerang Casino kennenzulernen und ihre Lieblingsspiele auszuprobieren. Mit etwas Glück können Spieler sogar einige Gewinne erzielen, ohne dabei eigenes Geld riskieren zu müssen.
Also, wenn Sie auf der Suche nach einem neuen Online-Casino sind und gerne Spielautomaten spielen, dann sollten Sie sich die 50 Freispiele von Boomerang Casino nicht entgehen lassen. Registrieren Sie sich noch heute und genieГџen Sie ein spannendes Spielerlebnis mit einer Vielzahl von Spielen und groГџzГјgigen Boni. Viel SpaГџ und viel GlГјck!
https://boomerangcasino.one/
15 Strange Hobbies That Will Make You More Successful At Replace Nissan Key Fob nissan qashqai key replacement; refsgaard-Winther.Blogbright.net,
5 Laws Anyone Working In Affordable Couches For Sale Should Know fold up couch
Zet Casino sperren: Schutz vor problematischem Spielverhalten
In den letzten Jahren ist das Thema Glücksspiel verstärkt in den Fokus der Öffentlichkeit gerückt. Immer mehr Menschen zeigen ein problematisches Spielverhalten und geraten dadurch in finanzielle und persönliche Schwierigkeiten. Um diesem Trend entgegenzuwirken, gibt es verschiedene Maßnahmen, die Spielerinnen und Spieler schützen sollen.
Eine dieser Maßnahmen ist das Sperren von Online-Casinos wie dem Zet Casino. Durch das Setzen von Limits oder das vollständige Sperren des Kontos können Spielerinnen und Spieler sich selbst vor übermäßigem Spielen schützen. Zet Casino bietet seinen Kundinnen und Kunden die Möglichkeit, sich selbst zu sperren, um so kontrolliertes Spielverhalten zu fördern.
Die Selbstsperre im Zet Casino bietet einige Vorteile: Zum einen können Spielerinnen und Spieler so verhindern, dass sie mehr Geld ausgeben, als sie eigentlich geplant hatten. Zum anderen können sie sich vor unkontrolliertem Spielverhalten schützen und somit langfristige finanzielle Probleme vermeiden. Die Selbstsperre im Zet Casino hilft, die Kontrolle über das eigene Spielverhalten zu behalten und verantwortungsvoll mit Glücksspielen umzugehen.
Wer also merkt, dass er nicht mehr spaßeshalber, sondern aus Zwang spielt, sollte die Möglichkeit nutzen, sich im Zet Casino zu sperren. Denn nur so kann langfristig problematisches Spielverhalten vermieden werden. Es ist wichtig, rechtzeitig die Notbremse zu ziehen und sich selbst zu schützen. Die Selbstsperre im Zet Casino ist hierfür eine effektive Maßnahme, die Spielerinnen und Spieler unterstützt, ein gesundes Spielverhalten zu entwickeln.
https://zetcasino.one/
15 Amazing Facts About Male.Masturbator That You Didn’t Know About
Top Male Masturbators
Are Car Accident Lawyers As Important As Everyone Says? paramount car accident lawsuit (https://vimeo.com/707218350)
5 Killer Quora Answers To Upvc Windows And Doors repair upvc Window
20 Top Tweets Of All Time 4 Wheel Electric Scooter 4
Wheeled Scooters (Historydb.Date)
3 Reasons Commonly Cited For Why Your Fiat Panda Key Fob
Replacement Isn’t Performing (And How To Fix It) reprogram Fiat 500 key fob
A Look Inside The Secrets Of Jobs Working Remotely work from Home Jobs leeds
Достойное место в отрасли занимает Московская коллегия адвокатов по уголовным делам. Костяк команды составляют опытные адвокаты, выполняющие свою работу грамотно. На счету специалистов много побед, для вашего спасения они делают все возможное. Необходим адвокат по мошенничеству? Уголовный-адвокат-юрист.рф – сайт, где имеется номер нашего телефона и актуальная стоимость услуг. Позвоните нам прямо сейчас и получите бесплатную консультацию. Выполните первый шаг к решению проблемы!
See What Robotic Vacuum Cleaner Self Emptying Tricks The Celebs Are Using robotic vacuum cleaner self Emptying
11 “Faux Pas” That Actually Are Okay To Make With Your How Many Cases Can You Get In CSGO Case Falchion
10 Graphics Inspirational About Best Accident Attorney Near Me pedestrian
buy neurontin online no prescription: neurontin 300mg tablet cost – neurontin prescription coupon
Your Family Will Thank You For Getting This Avon Uk Perfume avon Uk perfume
Learn More About Semi Truck Lawyer While You Work
From The Comfort Of Your Home Sheffield semi truck accident
law firm [https://vimeo.Com/709837593]
10 Fundamentals About Bentley Valet Key You Didn’t Learn In School bentley
car key (Magnolia)
What’s Next In Walking Desk Treadmill Treadmills Desk
The 12 Most Unpleasant Types Of Which Is The Best Online Supermarket Tweets You Follow Cosmo Wallet Slim Case Xr
Five Killer Quora Answers On Designer Handbags For Cheap designer handbags for cheap
10 Birth Defect Case-Related Projects To Stretch Your Creativity Duluth Birth Defect Attorney
3 Common Reasons Why Your Amazon Online Shopping Clothes Uk Isn’t
Performing (And How To Fix It) Infuser Teapot For Tea
Boomerang Casino Kokemuksia
Boomerang Casino ist ein neues Online-Casino, das sich durch sein einzigartiges Design und seine Vielfalt an Spielen auszeichnet. Das Casino wurde im Jahr 2020 gegrГјndet und hat seitdem zahlreiche Spieler aus der ganzen Welt angezogen. In diesem Artikel werden wir die Erfahrungen mit Boomerang Casino genauer betrachten.
Eines der auffГ¤lligsten Merkmale von Boomerang Casino ist sein ansprechendes Design. Die Webseite ist Гјbersichtlich gestaltet und leicht zu navigieren, was das Spielerlebnis insgesamt angenehmer macht. DarГјber hinaus verfГјgt das Casino Гјber eine Vielzahl von Spielen, darunter Spielautomaten, Tischspiele, Live-Casino-Spiele und mehr. Die Spiele stammen von renommierten Anbietern wie NetEnt, Microgaming, Play’n GO und vielen anderen, was fГјr eine hohe QualitГ¤t und Vielfalt sorgt.
Ein weiterer Pluspunkt von Boomerang Casino sind die großzügigen Boni und Promotionen, die regelmäßig angeboten werden. Neue Spieler können einen Willkommensbonus bei ihrer ersten Einzahlung erhalten, und es gibt auch ständig wechselnde Aktionen, wie beispielsweise Freispiele oder Cashback-Angebote. Diese Boni können dazu beitragen, das Spielvergnügen zu erhöhen und die Gewinnchancen zu verbessern.
Die Zahlungsmöglichkeiten bei Boomerang Casino sind vielfältig und sicher. Spieler können zwischen verschiedenen Zahlungsmethoden wie Kreditkarten, E-Wallets, Banküberweisungen und sogar Kryptowährungen wählen. Die Auszahlungen werden schnell bearbeitet, was für eine reibungslose und unkomplizierte Spielerfahrung sorgt.
Alles in allem sind die Erfahrungen mit Boomerang Casino durchweg positiv. Das Casino überzeugt durch sein attraktives Design, die Vielfalt an Spielen und die großzügigen Boni und Promotionen. Spieler können hier sicher und unterhaltsam spielen und haben die Chance auf attraktive Gewinne. Wir empfehlen Boomerang Casino daher allen, die nach einer erstklassigen Online-Glücksspielplattform suchen.
https://boomerangcasino.one/
The Most Important Reasons That People Succeed In The Mazda Key Fob Industry mazda Key fobs
Online Casino Zet: Ein aufregendes Spielerlebnis
Das Online Casino Zet ist ein beliebtes Ziel fГјr Spieler, die auf der Suche nach einem spannenden und unterhaltsamen GlГјcksspiel-Erlebnis sind. Mit einer breiten Auswahl an Spielen, groГџzГјgigen Promotionen und einem benutzerfreundlichen Interface bietet das Casino alles, was das Spielerherz begehrt.
Eine der größten Attraktionen des Online Casino Zet sind die vielen verschiedenen Spiele, die hier angeboten werden. Von klassischen Tischspielen wie Roulette und Blackjack bis hin zu aufregenden Spielautomaten und Live-Dealer-Spielen – hier findet jeder Spieler sein Lieblingsspiel. Die Spiele stammen von renommierten Entwicklern wie NetEnt, Microgaming und Play’n GO und garantieren so ein HГ¶chstmaГџ an QualitГ¤t und Fairness.
Neben der groГџen Auswahl an Spielen bietet das Online Casino Zet auch regelmäßige Promotionen und Boni fГјr seine Spieler. Von Willkommensboni fГјr neue Spieler bis hin zu wГ¶chentlichen Reload-Boni und Freispielen – hier gibt es immer etwas zu gewinnen. DarГјber hinaus belohnt das Casino treue Spieler mit einem exklusiven VIP-Programm, das zusГ¤tzliche Vorteile und Belohnungen bietet.
Das Online Casino Zet legt großen Wert auf die Sicherheit und Fairness seiner Spiele. Alle Spiele werden regelmäßig von unabhängigen Prüfungsbehörden überwacht, um sicherzustellen, dass sie fair und zufällig sind. Darüber hinaus verwendet das Casino branchenübliche Verschlüsselungstechnologien, um die persönlichen und finanziellen Daten seiner Spieler zu schützen.
Insgesamt bietet das Online Casino Zet ein erstklassiges Spielerlebnis fГјr alle, die auf der Suche nach einem unterhaltsamen und sicheren GlГјcksspiel-Erlebnis sind. Mit einer breiten Auswahl an Spielen, groГџzГјgigen Promotionen und erstklassigem Kundenservice ist das Casino definitiv einen Besuch wert. Probieren Sie es noch heute aus und erleben Sie die Aufregung des Online Casino Zet!
https://zetcasino.one/
How To Survive Your Boss On Railroad Injuries Attorneys Kuna Railroad Injuries Lawyer
The Advanced Guide To Auto Lock Smith auto lock smiths
15 Of The Best Pinterest Boards Of All Time About Certified
Online Jobs Work From Home weekend Work From Home jobs
The 10 Scariest Things About Designer Handbags Black Designer handbags Black
Интересуетесь улучшить свои английский? Погрузитесь в увлекательный мир английского языка через кинокартины и сериалы на английском и британском языках. Насладитесь процессом изучения, погружаясь в увлекательные сюжеты и диалоги на языке оригинала. Фильмы и сериалы на английском не только помогут вам расширить словарный запас, но и сделают лучше понимание английской языка на слух. Используйте просмотры сериалов на английском в качестве увлекательного метода освоения. Подробнее здесь https://serialy-na-angliiskom.pp.ua.
9 Things Your Parents Teach You About Cheap Treadmill Desk cheap
treadmill desk (Bernie)
You’ll Never Guess This Upvc Window Repair’s Tricks upvc window repair
The 10 Most Scariest Things About Best Double Ended Dildos Best double ended dildos
7 Easy Tips For Totally Making A Statement With Your Leather Sofas For Sale dark green couch
The Most Underrated Companies To Follow In The Bunk Bed For Adults Industry bunk beds for sale
You’ll Be Unable To Guess Outdoor Sectional Sofa’s Tricks outdoor sectional sofa
(https://pihl-Kahn.Blogbright.net)
You Are Responsible For The Double Glazed Windows Near Me Budget?
12 Best Ways To Spend Your Money replacement double glazed window
amoxicillin 500mg capsules antibiotic generic amoxicillin online order amoxicillin 500mg
15 Things You’re Not Sure Of About Cerebral Palsy Settlement Vimeo.com
4 Dirty Little Secrets About Slot Demo Gratis Pragmatic Play No Deposit And The Slot
Demo Gratis Pragmatic Play No Deposit Industry
Akun Demo olympus (doodleordie.com)
10 Quick Tips For Upvc Window Repair Upvc Repair
10 Things You Learned In Kindergarden That Will Help You With
Work Home From Jobs Work From home Employment
Das Tipico Casino bietet seinen Kunden die Möglichkeit, ihre Gewinne zu verdoppeln – ein Feature, das viele Spieler fasziniert. Doch wie funktioniert das Verdoppeln im Tipico Casino eigentlich?
Beim Verdoppeln handelt es sich um eine einfache Strategie, um die Gewinne beim Spielen im Casino zu steigern. Dabei setzt der Spieler seinen Gewinn auf eine zusätzliche Wette und versucht, diese zu verdoppeln. Beim Tipico Casino erfolgt dies in der Regel über ein spezielles Feature oder eine Funktion, die es dem Spieler ermöglicht, seinen Gewinn zu verdoppeln.
Um im Tipico Casino erfolgreich zu verdoppeln, ist es wichtig, die richtige Strategie zu wählen. Der Spieler muss sich gut überlegen, wann und wie er sein Geld einsetzt, um die Chancen auf einen Gewinn zu maximieren. Zudem ist es wichtig, die Regeln und Bedingungen des Verdoppelns im Tipico Casino zu kennen, um keine Fehler zu machen.
Es ist zu beachten, dass das Verdoppeln im Tipico Casino auch mit Risiken verbunden ist. Es kann dazu führen, dass der Spieler seinen Gewinn komplett verliert, wenn die zusätzliche Wette nicht erfolgreich ist. Daher ist es wichtig, verantwortungsvoll zu spielen und nur Geld einzusetzen, das man sich leisten kann zu verlieren.
Insgesamt bietet das Verdoppeln im Tipico Casino eine spannende Möglichkeit, die Gewinne beim Spielen zu erhöhen. Mit der richtigen Strategie und etwas Glück können Spieler ihren Einsatz verdoppeln und so noch mehr Spaß am Spiel haben. Wer die Regeln und Bedingungen beachtet und verantwortungsvoll spielt, kann das Verdoppeln im Tipico Casino erfolgreich nutzen.
https://tipicocasino.one/
11 Ways To Completely Revamp Your Self Emptying Robot Vacuum top 10
What’s The Current Job Market For Best Sextoy Men Professionals?
best sextoy men – Darell,
На сайте https://www.youtube.com/@mozspb вы сможете ознакомиться с информацией, а также видеоматериалами от популярного геймера Алексея, который проживает в Санкт-Петербурге. Ему 41 год и он особенно любит играть в шутеры. А после знакомства с Михаилом Алексей плотно подсел на такую игру, как PUBG. А в феврале 2024 его уговорили на то, чтобы он начал стримить. Алексей будет рад всем, кто хочет присоединиться и погрузиться в мир игр. Всего на канале более тысячи подписчиков, размещено 29 видео. Канал был зарегистрирован 16 ноября 2019 года.
Wenn Sie Ihr Zet Casino Konto löschen möchten, gibt es einige Schritte, die Sie befolgen müssen. Zunächst einmal sollten Sie sich darüber im Klaren sein, dass das Löschen Ihres Kontos endgültig ist und nicht rückgängig gemacht werden kann. Es ist also wichtig, sicherzustellen, dass Sie diese Entscheidung wirklich treffen möchten.
Um Ihr Zet Casino Konto zu löschen, müssen Sie sich zunächst bei Ihrem Konto anmelden. Klicken Sie dann auf Ihr Profil und gehen Sie zu den Kontoeinstellungen. Dort sollte es eine Option geben, mit der Sie Ihr Konto löschen können. Folgen Sie den Anweisungen und bestätigen Sie Ihre Entscheidung.
Es ist auch wichtig zu beachten, dass Sie möglicherweise noch ausstehende Guthaben auf Ihrem Konto haben. Bevor Sie Ihr Konto löschen, sollten Sie sicherstellen, dass Sie Ihr Guthaben ausgezahlt haben oder anderweitig verwendet haben.
Das Löschen Ihres Zet Casino Kontos kann verschiedene Gründe haben, sei es aufgrund von Spielsucht, persönlichen Gründen oder aus einem anderen Grund. Wenn Sie sich jedoch entscheiden, Ihr Konto zu löschen, ist es wichtig, dies auf sichere Weise zu tun und sicherzustellen, dass alle erforderlichen Schritte befolgt werden.
Wenn Sie weitere Fragen zum Löschen Ihres Zet Casino Kontos haben, können Sie sich jederzeit an den Kundendienst des Casinos wenden, um Unterstützung zu erhalten. Es ist wichtig, dass Sie sich wohl fühlen und nicht zögern, Hilfe in Anspruch zu nehmen, wenn Sie sie benötigen.
https://zetcasino.one/
http://zithromaxa.store/# zithromax 600 mg tablets
Who’s The World’s Top Expert On Best Dildo To Squirt?
squirting dildo (Peatix.Com)
The 10 Scariest Things About Double Glazing Window Repairs
Double glazing
Glazing Repairs Near Me: The History Of Glazing Repairs Near Me In 10 Milestones double glazing repairs Near me
neurontin 100mg tablets: neurontin canada – neurontin medication
Everything You Need To Know About Dreame L30 Ultra Review Vacuum Mops
Small Bunk Bed For Kids Tips To Relax Your Daily Life Small
Bunk Bed For Kids Trick That Everyone Should Know
small bunk bed for kids (Bailey)
You’ll Never Guess This Best Robot Vacuum Self Emptying’s Tricks Best Robot Vacuum Self Emptying; http://Demo2-Ecomm.In.Ua/User/Thrillhelmet46,
You’ll Never Guess This Birth Injury Attorney Fort Collins’s Benefits birth injury attorney fort collins
Double Glazing Installers Near Me Tips From The Top
In The Business Double Glazing Windows Handles
How Much Do Double Glazing Offers Near Me Experts Make? Double Glzing
See What Audi Key Tricks The Celebs Are Utilizing audi Key
Unexpected Business Strategies For Business That Aided Door Unlock Service Achieve Success
cost
The 9 Things Your Parents Taught You About
Motorcycle Accident Lawsuit motorcycle Accident lawsuit
prednisone 20mg buy online: buy prednisone from india – drug prices prednisone
The 9 Things Your Parents Teach You About Link Login Gotogel link login gotogel
20 Questions You Should ASK ABOUT Double Glazing Repair Near Me Before You Decide To Purchase It wooden double glazed windows
Boomerang Casino: Das aufstrebende GlГјcksspielziel Griechenlands
Griechenland ist längst nicht mehr nur für seine antiken Sehenswürdigkeiten und traumhaften Strände bekannt, sondern auch für seine boomende Glücksspielindustrie. Ein herausragendes Beispiel dafür ist das Boomerang Casino, das sich als eines der beliebtesten Casinos des Landes etabliert hat.
Das Boomerang Casino bietet seinen Besuchern eine Vielzahl von Spielen, darunter Slots, Tischspiele und Live-Casino-Spiele. Die atemberaubende Auswahl an Spielen und die hochmoderne Software sorgen dafür, dass Spieler aller Erfahrungsstufen hier auf ihre Kosten kommen. Darüber hinaus bietet das Casino regelmäßig spannende Aktionen und Boni, um seinen Kunden ein unvergessliches Spielerlebnis zu garantieren.
Ein weiterer Grund für den Erfolg des Boomerang Casinos ist die erstklassige Gästebetreuung. Das freundliche und professionelle Personal steht den Besuchern rund um die Uhr zur Verfügung und sorgt dafür, dass ihr Aufenthalt so angenehm wie möglich verläuft. Zudem bietet das Casino eine Vielzahl von Zahlungsoptionen, schnelle Auszahlungen und eine garantierte Sicherheit der persönlichen Daten.
Neben dem erstklassigen Service und der umfangreichen Spielauswahl zeichnet sich das Boomerang Casino auch durch seine atemberaubende Atmosphäre aus. Mit elegantem Design, modernster Technologie und einer warmen und einladenden Atmosphäre ist das Casino der perfekte Ort, um sich zu entspannen und Spaß zu haben.
Insgesamt ist das Boomerang Casino in Griechenland zu Recht zu einem der Top-Glücksspielziele des Landes geworden. Mit seinem erstklassigen Service, seiner umfangreichen Spielauswahl und seiner einzigartigen Atmosphäre bietet das Casino ein unvergessliches Erlebnis für jeden Besucher. Wer also auf der Suche nach einem aufregenden und unterhaltsamen Glücksspielerlebnis ist, sollte das Boomerang Casino auf jeden Fall einen Besuch abstatten.
https://boomerangcasino.one/
20 Fun Informational Facts About Sofas Sale Recliner sofas For sale
The Best Double Glazing Repairs Near Me Is Gurus. Three Things Double Glazing Replacement
Guide To Robot Vacuum And Mop With Self Emptying:
The Intermediate Guide For Robot Vacuum And Mop With Self Emptying
robot vacuum and mop with self empty
The 10 Most Scariest Things About Uk Online Shopping Sites For Electronics
uk online shopping sites for electronics – Hildred –
Ten Double Bunk Beds That Really Improve Your Life
Double Bunk Beds
cialis patient assistance
Quiz: How Much Do You Know About Car Accident Lawyers? car accident law firm
Repair Misted Double Glazing Near Me Tips That Will Change Your Life replacement
15 Twitter Accounts That Are The Best To Learn About Mesothelioma Compensation mesothelioma lawyer
10 Sites To Help You Develop Your Knowledge About Uk Online
Shopping Sites For Electronics Large Pet Towel 28X50
10 Things That Your Family Taught You About Robot Vacuum Best robot vacuum for pet hair
Nine Things That Your Parent Taught You About
Handbag Tommy Hilfiger handbag Tommy Hilfiger
12 Companies That Are Leading The Way In Cars Locksmith Near Me nearby
Five Dreame L30 Review Projects To Use For Any Budget dreame l30 ultra
10 Quick Tips For Tommy Hilfiger Xbody Bag tommy hilfiger bag duffle
20 Resources That’ll Make You Better At How Do You Unlock A Car Without
A Key how to unlock Your car
The Reasons Irobot Vacuum Is More Dangerous Than You Believed robot vacuums
Ten Bunk Bed For Children Myths You Should Not Share On Twitter Bed bunks for sale
What’s The Job Market For Online Shopping Uk For Clothes Professionals Like?
Online Shopping Uk For Clothes
amoxicillin 500mg price canada: generic amoxil 500 mg – amoxicillin 30 capsules price
Why People Don’t Care About Michael Kors Handbags On Sale Michael Handbag Kors
Die Temperaturen steigen und auch die Casino-Slots bei Tipico sind heiГџer als je zuvor! Mit einer Vielzahl von Spielen und Jackpots, die darauf warten, geknackt zu werden, ist Tipico der perfekte Ort fГјr alle Casino-Liebhaber.
Egal, ob Sie ein Fan von klassischen Spielautomaten oder modernen Video-Slots sind, Tipico hat fГјr jeden Geschmack das Richtige. Mit aufregenden Themen, hochwertiger Grafik und spannenden Bonusfunktionen werden Sie garantiert stundenlangen SpaГџ haben.
Ein besonderes Highlight sind die progressiven Jackpots, bei denen die Gewinnsumme kontinuierlich steigt, bis ein glücklicher Spieler den Hauptpreis knackt. Diese Slots bieten die Chance auf lebensverändernde Gewinne und sorgen für eine extra Portion Spannung.
Aber nicht nur die Slots sind heiГџ bei Tipico – auch die Promotionen und Aktionen lassen das Spielerherz hГ¶herschlagen. Von Freispielen Гјber Einzahlungsboni bis hin zu Gewinnspielen gibt es immer wieder neue MГ¶glichkeiten, um Ihre Gewinnchancen zu maximieren.
Also worauf warten Sie noch? Tauchen Sie ein in die aufregende Welt der Casino-Slots bei Tipico und lassen Sie sich von der Hitze der Gewinne verfГјhren! Viel GlГјck und viel SpaГџ beim Spielen!
https://tipicocasino.one/
Why Auto Accident Case Is Your Next Big Obsession auto accident lawyers
Why Nobody Cares About Upvc Windows Repair window Replacement near me
https://microbladingeyebrowsalon.com/
10 Unexpected Desk Treadmill Foldable Tips desk treadmills – http://alt1.toolbarqueries.google.com.jm/,
Zet Casino Geld zurГјckfordern: Eine Anleitung fГјr Spieler
In der Welt der Online-Casinos ist es nicht ungewöhnlich, dass Spieler auf Probleme stoßen. Eine häufige Herausforderung, mit der Spieler konfrontiert sind, ist die Möglichkeit, Geld zurückfordern zu müssen. Dies kann verschiedene Gründe haben, wie z.B. eine fehlerhafte Abbuchung, ein technisches Problem oder sogar Betrug.
Wenn Sie sich in einer Situation befinden, in der Sie Geld von Zet Casino zurГјckfordern mГјssen, ist es wichtig, dass Sie die richtigen Schritte befolgen, um Ihr Geld zurГјckzuerhalten. Hier sind einige wichtige Schritte, die Sie befolgen sollten:
1. Überprüfen Sie Ihre Transaktionen: Bevor Sie Geld zurückfordern, sollten Sie sicherstellen, dass es tatsächlich ein Problem gibt. Überprüfen Sie Ihre Transaktionen und vergewissern Sie sich, dass die Abbuchung nicht korrekt war.
2. Kontaktieren Sie den Kundensupport: Wenn Sie feststellen, dass es ein Problem gibt, sollten Sie sich umgehend an den Kundensupport von Zet Casino wenden. Informieren Sie sie Гјber das Problem und geben Sie alle relevanten Informationen an, wie z.B. Ihre Kontodaten und Transaktionsdetails.
3. Behalten Sie alle relevanten Dokumente bei: Es ist wichtig, alle relevanten Dokumente aufzubewahren, wie z.B. E-Mails, Screenshots und andere Beweise für das Problem. Diese können Ihnen dabei helfen, Ihr Geld zurückzufordern.
4. Fordern Sie Ihr Geld zurГјck: Sobald Sie alle Informationen gesammelt haben, sollten Sie Ihr Geld zurГјckfordern. Fordern Sie dies schriftlich an und geben Sie alle relevanten Informationen an.
5. Behalten Sie die Kommunikation im Auge: Es kann einige Zeit dauern, bis Ihr Geld zurückgezahlt wird. Behalten Sie die Kommunikation mit dem Kundensupport im Auge und lassen Sie sich regelmäßig über den Stand der Dinge informieren.
Insgesamt ist es wichtig, geduldig zu sein und alle erforderlichen Schritte zu befolgen, um Ihr Geld von Zet Casino zurГјckzufordern. Wenn Sie die oben genannten Schritte befolgen, sollten Sie in der Lage sein, Ihr Geld erfolgreich zurГјckzuerhalten.
https://zetcasino.one/
So , You’ve Bought Replacement Windows Leeds …
Now What? Window doctor leeds
purchase amoxicillin online amoxicillin buy no prescription amoxicillin 500 mg without a prescription
Five Killer Quora Answers On Treadmills Sale Treadmills sale
5 Reasons To Be An Online Double Glazing Windows Near Me Buyer And 5 Reasons Not To Double Glazing misting
Guide To Cars Locksmith Near Me: The Intermediate Guide For Cars Locksmith Near Me cars locksmith near me
What Is Diagnostic Check Near Me And Why Is Everyone
Speakin’ About It? vauxhall Diagnostic near Me
Watch This: How CS GO Weapon Case Is Taking
Over And What To Do About It Esports 2013 case
7 Simple Tips To Totally Rocking Your 12kg Washing Machine Sale 12Kg Washing Machines
Why Erb’s Palsy Settlement Is Your Next Big Obsession algona erb’s Palsy lawyer
10 Unexpected Best SEO Software Tips seo Audit
10 Things We Were Hate About Upvc Doors Leeds New Glazing leeds
5 Laws Anybody Working In CSGO New Case Should Be Aware Of Operation bravo Case
Male Masterbator Tips To Relax Your Daily Life Male Masterbator Trick That Every
Person Must Know male masterbator
15 Funny People Working In Sectional Sofa In Sectional
Sofa Sectional Sofas (https://Peatix.Com/)
Guide To 12kg Washing Machine Sale: The Intermediate Guide Towards 12kg Washing Machine Sale 12kg washing Machine sale
Guide To Self-Empty Robot Vacuum: The Intermediate Guide The
Steps To Self-Empty Robot Vacuum self-empty robot vacuum
11 Creative Methods To Write About Compact Treadmill With Incline best compact treadmill with incline
20 Trailblazers Leading The Way In Accident Case lafayette Accident attorney
What You Should Be Focusing On Improving Gotogel Link Alternatif
Judi Live
The 9 Things Your Parents Teach You About Ranking SEO Software Ranking seo Software
3 Ways That The Window Repair Near Can Affect Your Life
upvc window repair near Me
Tipico Casino Bonus freispielen: So geht’s!
Der Tipico Casino Bonus ist ein attraktives Angebot für alle Spieler, die gerne im Online Casino spielen. Doch um den Bonus freizuspielen, müssen bestimmte Bedingungen erfüllt werden. In diesem Artikel erklären wir, wie das genau funktioniert.
Zunächst einmal muss man sich als neuer Spieler bei Tipico registrieren und eine Einzahlung tätigen, um den Casino Bonus zu erhalten. Je nach Angebot kann es sich um einen Einzahlungsbonus, Freispiele oder andere Boni handeln. Sobald der Bonus gutgeschrieben wurde, gilt es, ihn freizuspielen.
Um den Tipico Casino Bonus freizuspielen, muss man den Bonusbetrag eine bestimmte Anzahl von Malen umsetzen. Diese Umsatzbedingungen variieren je nach Angebot und mГјssen innerhalb eines bestimmten Zeitraums erfГјllt werden. Es ist wichtig, die genauen Bedingungen im Auge zu behalten, um den Bonus erfolgreich freizuspielen.
Es gibt verschiedene Spiele im Tipico Casino, die zum Freispielen des Bonus beitragen. Slots tragen in der Regel zu 100% zur Erfüllung der Umsatzbedingungen bei, während Tischspiele wie Roulette und Blackjack oft nur zu einem gewissen Prozentsatz gewertet werden. Es ist wichtig, sich vorab über die Spiele zu informieren, die zum Freispielen des Bonus beitragen.
Zusammenfassend lässt sich sagen, dass der Tipico Casino Bonus ein attraktives Angebot für Spieler darstellt, die gerne im Online Casino spielen. Um den Bonus erfolgreich freizuspielen, ist es wichtig, die Umsatzbedingungen und Spiele genau zu kennen und zu beachten. Mit etwas Glück und Geschick kann man den Bonus in einen ordentlichen Gewinn umwandeln und sich über zusätzliches Spielgeld freuen.
https://tipicocasino.one/
Boomerang Casino Freispiele: Ein Muss fГјr alle GlГјcksspielenthusiasten
Boomerang Casino ist ein aufstrebendes Online-Casino, das sich durch sein großzügiges Bonussystem auszeichnet. Eine der beliebtesten Aktionen bei Boomerang Casino sind die Free Spins, die den Spielern die Möglichkeit bieten, ihre Lieblingsspiele kostenlos zu genießen.
Die Boomerang Casino Freispiele sind eine attraktive Möglichkeit, um neue Spiele auszuprobieren oder einfach nur zusätzliche Gewinnchancen zu erhalten. Wenn Sie sich für ein Konto bei Boomerang Casino registrieren, werden Sie mit einer Vielzahl von Freispielen belohnt, die Sie direkt in Ihren Lieblingsspielen einsetzen können.
Die Free Spins bei Boomerang Casino sind an keine Umsatzbedingungen geknüpft, was bedeutet, dass alle Gewinne, die Sie mit den Freispielen erzielen, sofort auszahlbar sind. Dies macht die Boomerang Casino Freispiele besonders attraktiv für Spieler, die gerne ohne Einschränkungen spielen möchten.
Darüber hinaus bietet Boomerang Casino regelmäßig Sonderaktionen an, bei denen Sie zusätzliche Freispiele erhalten können. Dies kann beispielsweise durch Einzahlungsboni oder durch die Teilnahme an speziellen Turnieren geschehen. Die Freispiele bei Boomerang Casino sind also nicht nur eine einmalige Belohnung, sondern können Ihnen regelmäßig zusätzliche Gewinnchancen bieten.
Insgesamt sind die Boomerang Casino Freispiele eine attraktive und großzügige Aktion, die es Spielern ermöglicht, ihre Lieblingsspiele ohne Risiko zu genießen und dabei zusätzliche Gewinne zu erzielen. Wenn Sie also auf der Suche nach einem Online-Casino mit lukrativen Bonusangeboten sind, sollten Sie unbedingt Boomerang Casino ausprobieren.
https://boomerangcasino.one/
15 Gifts For The 10kg Washing Machine For Sale Lover In Your Life 10Kg Capacity Washing Machine
15 Reasons You Shouldn’t Overlook Tumble Dryer With Heat Pump Heat Pump Tumble
https://gabapentinneurontin.pro/# neurontin cost generic
Are You Responsible For An Double Over Double Bunk Beds For Adults Budget?
10 Unfortunate Ways To Spend Your Money double Bunk With storage
10 Failing Answers To Common Freestanding Fridge Questions: Do You Know The Right
Ones? fridge freestanding (Claribel)
The Next Big Trend In The Lawyer Auto Industry Auto Accident Attorney Las Vegas
Some Of The Most Common Mistakes People Make With Railroad Injuries Law railroad shoulder injury settlements
How Much Can Tommy Hilfiger Cross Bag Experts Earn? Tommy Hilfiger Cross Body Bag
What’s The Job Market For Robots That Vacuum And Mop Professionals?
Robots That Vacuum And Mop
Immer mehr Online-Casinos bieten ihren Spielern die Möglichkeit, mit PayPal Ein- und Auszahlungen vorzunehmen. Zet Casino ist eines dieser Casinos, das diese beliebte Zahlungsmethode akzeptiert.
PayPal ist eine der führenden Online-Zahlungsmethoden weltweit und zeichnet sich durch die einfache Handhabung und hohe Sicherheitsstandards aus. Spieler können ihre Transaktionen schnell und unkompliziert über ihr PayPal-Konto tätigen, ohne sensible Bankdaten direkt beim Casino angeben zu müssen.
Zet Casino bietet seinen Spielern eine breite Palette an Spielen, von Slots über Tischspiele bis hin zu Live-Casino-Spielen. Mit PayPal als Zahlungsmethode können Spieler bequem und sicher Geld auf ihr Konto einzahlen, um sofort mit dem Spielen zu beginnen.
Darüber hinaus bietet Zet Casino seinen Spielern regelmäßige Aktionen und Boni an, die das Spielerlebnis noch spannender machen. Mit PayPal als Zahlungsmethode können Spieler von schnellen Ein- und Auszahlungen profitieren und sich ganz auf ihr Spiel konzentrieren.
Insgesamt bietet Zet Casino eine erstklassige Spielerfahrung für alle, die gerne online spielen. Mit PayPal als Zahlungsmethode können Spieler sich auf eine sichere und zuverlässige Abwicklung ihrer Transaktionen verlassen und sich voll und ganz auf ihr Spiel konzentrieren.
https://zetcasino.one/
How To Tell If You’re In The Right Place For Lightweight Wheelchair Electric convertible dual wheel Powerstroll for manual wheelchairs (http://www.Mymobilityscooters.uk)
Responsible For The Upvc Window Repairs Budget? 12 Best Ways To Spend Your Money window repairs Near me
На сайте https://premiumface.ru/ почитайте информацию об уникальной и инновационной процедуре многоуровневой комплексной подтяжке лица. Для того чтобы получить необходимый результат, идеальное лицо, используются исключительно высокотехнологичные Европейские препараты премиального уровня. Они созданы на базе гиалуроновой кислоты, различных полезных добавок, которые восстанавливают кожу, придают ей упругость, эластичность, роскошный внешний вид. Такая процедура обязательно вам подойдет, если желаете выглядеть ухоженно, но без одутловатого лица, стремитесь сохранить естественную красоту.
Double Glazed Window Repair Tools To Help You Manage Your Daily Lifethe
One Double Glazed Window Repair Trick That Every Person Should
Be Able To upvc repairs near me; Kara,
Veleco Uk Tools To Ease Your Daily Lifethe One Veleco Uk Trick
That Every Person Must Learn Veleco uk
Where Will Cheap Treadmill Desk Be 1 Year From What Is Happening Now?
hometreadmills
12 Companies Leading The Way In Key Smith For Cars locksmith Car key Maker (http://promarket.in.ua/user/soupbean7)
5 Killer Quora Questions On Porsche Key Fobs remote
Ask Me Anything: 10 Responses To Your Questions About Fiat 500 Key Replacement fiat 500x key Fob replacement
What You Need To Do With This Avon Become A Rep become an Avon sales rep
Do Not Forget Online Shopping Sites In United Kingdom:
10 Reasons Why You Don’t Have It Scrubs V-Neck Shirt Blue Fog
20 Reasons Why Double Glazing Repair Leeds Will Never Be Forgotten window repairs leeds;
Jerrell,
It’s The Which CS GO Case Is Best To Open Case Study You’ll
Never Forget shadow case (techmedia-think.hatenablog.com)
The Most Negative Advice We’ve Ever Heard About Mesothelioma Attorney Maine Idaho Mesothelioma Attorney
10 Graphics Inspirational About Double Glazing Repairs Near Me double glazing
near me (Ira)
See What Replacement Window Seals Tricks The Celebs Are Making Use Of
replacement Window seals
A Step-By-Step Guide To Railroad Injuries Lawyer From Start To Finish
railroad injury help
“The Best CSGO Case Sites Awards: The Most, Worst, And Strangest Things We’ve Ever Seen counter strike
Global offensive
buy cheap prednisone: prednisone oral – buy prednisone without prescription paypal
How Can A Weekly Audi A5 Replacement Key Project Can Change Your Life programming audi key (http://Yerliakor.com/user/tightssteven0/)
The Little-Known Benefits Of Electric Wheelchair Benefits Modern Electric Wheelchair
Erfahrungen Boomerang Casino: Unser Fazit nach ausgiebigen Tests
Das Boomerang Casino ist ein relativ neues Online-Casino, das erst im Jahr 2020 gegrГјndet wurde. Da wir immer auf der Suche nach neuen und interessanten GlГјcksspielanbietern sind, haben wir uns dazu entschlossen, das Boomerang Casino genauer unter die Lupe zu nehmen und unsere Erfahrungen mit Ihnen zu teilen.
Zunächst einmal fällt die ansprechende und benutzerfreundliche Webseite des Boomerang Casinos ins Auge. Die Navigation ist einfach und übersichtlich gestaltet, sodass wir uns schnell zurechtgefunden haben. Auch das Design und die Grafiken sind modern und ansprechend, was für ein angenehmes Spielerlebnis sorgt.
Was die Spielauswahl betrifft, konnten wir im Boomerang Casino eine breite Palette an Slots, Tischspielen, Live-Casino-Spielen und Jackpot-Slots entdecken. Dabei arbeitet das Casino mit renommierten Spieleentwicklern wie NetEnt, Microgaming und Play’n GO zusammen, was fГјr eine hohe QualitГ¤t und Vielfalt der Spiele sorgt.
Besonders beeindruckt hat uns die große Auswahl an Bonusangeboten im Boomerang Casino. Neben einem großzügigen Willkommensbonus für Neukunden gibt es regelmäßige Aktionen, Freispiele und Turniere, bei denen man attraktive Preise gewinnen kann. Auch das Treueprogramm belohnt loyalen Spieler mit exklusiven Boni und Prämien.
Ein weiterer Pluspunkt des Boomerang Casinos ist der Kundenservice. Das Supportteam steht rund um die Uhr per Live-Chat und E-Mail zur Verfügung und hat uns bei unseren Anfragen stets schnell und kompetent geholfen. Auch die Zahlungsmöglichkeiten sind vielfältig und sicher, was für ein reibungsloses Ein- und Auszahlen sorgt.
Insgesamt können wir das Boomerang Casino nach unseren ausgiebigen Tests uneingeschränkt empfehlen. Das Casino überzeugt durch ein breites Spielangebot, attraktive Bonusangebote, einen kompetenten Kundenservice und eine benutzerfreundliche Webseite. Wir hatten viel Spaß beim Spielen im Boomerang Casino und werden sicherlich wiederkommen.
https://boomerangcasino.one/
Avon In The UK: 10 Things I Wish I’d Known In The Past avon in The uk
You’ll Never Guess This Self Emptying Robot Vacuum Mop’s
Tricks Self Emptying Robot vacuum mop
How Motorcycle Accident Claim Propelled To The Top Trend In Social
Media motorcycle accident lawsuit
Five Idn Poker Projects For Any Budget spam
10 Beautiful Images Of Cheap Sofas For Sale real leather couch
One Personal Injury Litigation Success Story You’ll Never Imagine Bloomingdale Personal injury Lawsuit
Watch Out: How Rooms To Go Sofa Sale Is Taking Over And What Can We Do About It Outdoor sofa sale
One Local SEO Experts Success Story You’ll Never Imagine optimisation
The Ultimate Glossary Of Terms About Door Repair Near Me Window Replacement Near Me
(http://Spectr-Sb116.Ru/)
The Reason Nissan Qashqai Key Replacement Is
Fast Becoming The Hottest Fashion Of 2023 nissan juke spare
key (Melinda)
10 Things You Learned In Kindergarden They’ll Help You
Understand Shark Robotic Vacuum Cleaner Cheap robot vacuum cleaner
10 Facebook Pages That Are The Best Of All-Time About Door Fitters Leeds window Hinge repair leeds
Zet Casino ist eine der beliebtesten Online-GlГјcksspielseiten unter Spielern aus verschiedenen LГ¤ndern. Die Spieler haben die MГ¶glichkeit, ihre eigenen Erfahrungen mit dem Casino zu teilen, indem sie ihre Meinungen und Bewertungen auf verschiedenen Plattformen verГ¶ffentlichen. Diese sogenannten “zet casino vГ©lemГ©nyek” geben anderen Spielern wichtige Informationen darГјber, was sie von dem Casino erwarten kГ¶nnen.
Die meisten Bewertungen von Zet Casino sind positiv und loben die Vielfalt der angebotenen Spiele, die Benutzerfreundlichkeit der Website und den effizienten Kundenservice. Viele Spieler schätzen auch die verschiedenen Bonusangebote und Aktionen, die regelmäßig angeboten werden. Ein weiterer Pluspunkt ist die schnelle Auszahlung von Gewinnen, was bei vielen Spielern sehr positiv bewertet wird.
Natürlich gibt es auch vereinzelt negative Bewertungen über Zet Casino. Einige Spieler bemängeln zum Beispiel die Bedingungen für Bonusangebote oder die Geschwindigkeit der Auszahlungen. Es ist jedoch wichtig zu beachten, dass es bei jeder Online-Glücksspielseite immer einige negative Bewertungen geben wird, da die Erfahrungen der Spieler variieren können.
Insgesamt scheint Zet Casino eine vertrauenswГјrdige und beliebte GlГјcksspielseite zu sein, die eine groГџe Auswahl an Spielen und attraktive Bonusangebote bietet. Die “zet casino vГ©lemГ©nyek” der Spieler sind ein guter Anhaltspunkt fГјr potenzielle Neukunden, die sich Гјber das Casino informieren mГ¶chten. Es ist jedoch ratsam, die verschiedenen Meinungen zu lesen und sich ein eigenes Bild zu machen, bevor man sich bei Zet Casino anmeldet.
https://zetcasino.one/
A Productive Rant Concerning Accident Lawsuit southern Pines Accident lawsuit
Nine Things That Your Parent Teach You About Best Smart
Vacuum For Pet Hair Best smart vacuum for Pet hair
20 Myths About Birth Defect Compensation: Dispelled Vimeo
Watch Out: How Online Shopping Sites In United Kingdom Is Taking Over And What
We Can Do About It Daylight White Led Light (Terry)
Guide To Mini Key: The Intermediate Guide On Mini Key mini
5 Killer Quora Answers On Online Clothes Shopping Sites Uk online clothes shopping Sites uk
How Much Can Planet Spa Body Scrub Experts Make? planet spa Oil
На ресурсе smotret.net можно отыскать большую коллекцию лучших сериалов. Вам будет предложено поразительное количество разных жанров. Вас ждет много захватывающих историй и эмоций. Ищете сериалы в hd качестве онлайн? Smotret.net – сайт, где вы найдете для себя что-то интересное. Вы можете воспользоваться удобным поиском. Получайте удовольствие от просмотра сериалов в отменном качестве. Уверены, что наш портал вам понравится, и вы захотите вернуться к нам вновь. Нравится смотреть сериалы? Тогда предлагаем вам прямо сейчас познакомиться с уникальным ресурсом Smotret.net!
15 Strange Hobbies That Will Make You Better At Car Opening opening car
30 Inspirational Quotes On Upvc Windows Repair window repairs
Where Can You Get The Most Reliable Ai Sentence
Rewriter Information? ai word rewriter
The No. One Question That Everyone Working In Truck Accidents Lawyer Should Know How To Answer Big Truck Accident Legal Assistance
buy amoxicillin 250mg: amoxicillin 500 coupon – generic amoxil 500 mg
The 10 Scariest Things About Round Sectional Sofa Round Sectional Sofa
What Washing Machine Sale 12kg Experts Want You To Know combo
What’s The Job Market For Sofas Sectionals Professionals
Like? sofas sectionals – https://wayranks.com/author/startray65-136101/,
Boomerang Casino Erfahrungen: Alles Гјber Auszahlungen
Boomerang Casino ist ein Online-Casino, das Spielern eine Vielzahl von Spielen und großzügigen Boni bietet. In diesem Artikel werden wir uns genauer mit den Erfahrungen der Spieler in Bezug auf Auszahlungen beschäftigen.
Die meisten Spieler, die Erfahrungen mit Boomerang Casino gemacht haben, berichten von schnellen und zuverlässigen Auszahlungen. Die Auszahlungszeiten variieren je nach Auszahlungsmethode, aber in der Regel werden Auszahlungen innerhalb von 24 Stunden bearbeitet. Spieler können zwischen verschiedenen Zahlungsmethoden wie Kreditkarten, E-Wallets und Banküberweisungen wählen.
Ein weiterer positiver Aspekt von Boomerang Casino ist die Tatsache, dass Auszahlungen in der Regel gebührenfrei sind. Dies bedeutet, dass Spieler ihr gesamtes Guthaben ohne Abzüge erhalten können.
Einige Spieler haben jedoch berichtet, dass sie gelegentlich Verzögerungen bei ihren Auszahlungen erlebt haben. In den meisten Fällen handelt es sich dabei um Probleme mit der Verifizierung der Identität oder der Erfüllung der Bonusbedingungen. Spieler sollten daher sicherstellen, dass sie alle erforderlichen Dokumente einreichen und die Bonusbedingungen vollständig erfüllen, um Verzögerungen bei ihren Auszahlungen zu vermeiden.
Insgesamt sind die Erfahrungen der Spieler mit Boomerang Casino in Bezug auf Auszahlungen größtenteils positiv. Schnelle und zuverlässige Auszahlungen sowie gebührenfreie Transaktionen sorgen dafür, dass Spieler ihre Gewinne schnell und einfach erhalten können. Es ist jedoch wichtig, die Bonusbedingungen zu beachten und alle erforderlichen Dokumente einzureichen, um Verzögerungen zu vermeiden.
https://boomerangcasino.one/
15 Gifts For The Railroad Injuries Legal Lover In Your Life Railroad
Accident Lawyer Edinburgh (Minecraftcommand.Science)
Buzzwords De-Buzzed: 10 Other Ways To Deliver Railroad Injuries Legal railroad injury fela lawyer (https://peatix.Com/user/22023965)
You’ll Be Unable To Guess Are Heat Pump Tumble
Dryers Any Good’s Benefits are heat pump tumble dryers any good (Landon)
The Best Advice You Could Ever Receive On Leeds Window Repair glazing leeds
Why Adding A Freezer For Outbuilding To Your Life Can Make All The Difference Top Freezer Brands
15 Top Pinterest Boards Of All Time About Asbestos Asbestos Attorney
Хотите купить на dvd увлекательные сериалы? Serialexpress вам поможет в этом. Здесь вы найдете диски, которых в других магазинах нет. Качество записи сериалов отличное, уверены, что вы останетесь довольны приобретением. Товары доступны по разумной цене, они целые и хорошо упакованы. Ищете чисто английские убийства купить? Serialexpress.ru – сайт, где имеется каталог. Здесь вы также можете ознакомиться с условиями оплаты. У нас действует накопительные скидки. Качество доставки вас порадует. Все вопросы можно задать менеджерам по электронной почте.
Nine Things That Your Parent Teach You About Upvc Window Repairs Near Me upvc window repairs near me, Telegra.ph,
5 Killer Quora Answers To Replacement Double Glazing Units Near Me replacement double glazing units near me
10 Life Lessons That We Can Learn From Semi Truck Lawyer Semi truck accident lawyers
9 Things Your Parents Taught You About Online Shopping vimeo
20 Blown Double Glazing Repair Websites Taking The Internet By Storm window repairs
A Vibrant Rant About Double Glazing Condensation Repair
Kit Window doctor
можно ли разорвать контракт сво
С началом СВО уже спустя полгода была объявлена первая волна мобилизации. При этом прошлая, в последний раз в России была аж в 1941 году, с началом Великой Отечественной Войны. Конечно же, желающих отправиться на фронт было не много, а потому люди стали искать способы не попасть на СВО, для чего стали покупать справки о болезнях, с которыми можно получить категорию Д. И все это стало возможным с даркнет сайтами, где можно найти практически все что угодно. Именно об этой отрасли темного интернета подробней и поговорим в этой статье.
You’ll Never Guess This Window Seal Replacement’s Benefits Window Seal Replacement
5 Killer Quora Answers On Fridge Freezer fridge freezer (maps.google.cg)
doxycycline hyclate 100 mg cap: buy doxycycline cheap – doxycycline
15 Gifts For The Truck Attorneys Near Me Lover In Your Life Warren Truck Accident Law Firm
Casinos en ligne sind heutzutage sehr beliebt und bieten eine Vielzahl von Spielen fГјr Spieler aus der ganzen Welt. Eine der aufregendsten Optionen fГјr deutsche Spieler ist das Casino en ligne Boomerang. Mit einer breiten Auswahl an Spielen und groГџartigen Bonusangeboten ist dieses Casino eine Top-Wahl fГјr alle, die eine unterhaltsame und spannende Online-GlГјcksspiel-Erfahrung suchen.
Das Casino en ligne Boomerang bietet eine Vielzahl von beliebten Spielen, darunter Spielautomaten, Tischspiele wie Blackjack und Roulette, sowie Live-Casino-Spiele mit echten Dealern. Die Grafiken und Animationen sind hochwertig und sorgen fГјr ein realistisches Spielerlebnis. Die Spiele werden von fГјhrenden Softwareentwicklern wie NetEnt, Microgaming und Play’n GO bereitgestellt, was fГјr faire und unterhaltsame Spielrunden sorgt.
Ein weiterer großer Vorteil des Casino en ligne Boomerang sind die großzügigen Bonusangebote für neue Spieler. Mit einem Willkommensbonus, der Freispiele und Bonusgeld umfasst, können Spieler ihr Startkapital deutlich erhöhen und mehr Zeit mit dem Spielen ihrer Lieblingsspiele verbringen. Darüber hinaus bietet das Casino regelmäßige Promotionen und Aktionen, um loyalen Spielern zusätzliche Belohnungen zu bieten.
Das Casino en ligne Boomerang verfügt über eine benutzerfreundliche Website, die es einfach macht, Spiele zu finden und zu spielen. Spieler können Zahlungen sicher und bequem über gängige Zahlungsmethoden wie Kreditkarten, E-Wallets und Banküberweisungen vornehmen. Der Kundenservice ist rund um die Uhr verfügbar und hilft bei Fragen oder Problemen schnell und professionell weiter.
Insgesamt ist das Casino en ligne Boomerang eine erstklassige Option fГјr deutsche Spieler, die ein aufregendes Online-Casino-Erlebnis suchen. Mit einer breiten Auswahl an Spielen, groГџzГјgigen Bonusangeboten und einer benutzerfreundlichen Website ist dieses Casino definitiv einen Besuch wert.
https://boomerangcasino.one/
На сайте https://antonenko-media.com оставьте заявку для того, чтобы заказать видеосъемку не только в городе, но и по области. Перед вами весь перечень услуг как по фотосъемке, так и видеосъемке. Компетентные, проверенные сотрудники без труда и на профессиональном уровне организуют онлайн-трансляцию любого мероприятия. И самое главное, что все пройдет именно так, как и нужно. Работы выполняются только на инновационном, высокотехнологичном оборудовании. Работать со специалистами компании всегда приятно, непринужденно.
5 Clarifications On Window Repair Near Upvc window repair Near me
5 Killer Quora Answers On Double Glazing Repairs Leeds
double glazing repairs leeds (hikvisiondb.webcam)
10 Things Everyone Makes Up About The Word “Online Charity Shop Uk Clothes.” Realistic Wild
Dog Plush (https://vimeo.com/931044844)
11 Ways To Completely Sabotage Your Double Glazed Windows Leeds upvc door repair meanwood
Upvc Windows Near Me Tools To Ease Your Everyday Lifethe Only
Upvc Windows Near Me Trick That Everyone Should Learn upvc windows near me
stone Park Asbestos Lawsuit cases can be complicated because they
are a mix of jurisdictions. Law firms with experience in processing asbestos
claims at the state and national levels are aware of the specific laws that apply.
The Most Hilarious Complaints We’ve Received About Upvc Window Repairs upvc Window repairs Near me
Das Zet Casino ist eine beliebte Online-Spielplattform, die eine Vielzahl von Spielen und großzügigen Boni für Spieler anbietet. Ein wichtiger Aspekt für Spieler ist die Auszahlungsdauer, also die Zeit, die es benötigt, bis Gewinne auf das Konto des Spielers überwiesen werden.
Die gute Nachricht ist, dass das Zet Casino eine schnelle Auszahlungsdauer hat. In der Regel können Spieler ihre Gewinne innerhalb von 24 Stunden erhalten, nachdem sie eine Auszahlungsanforderung gestellt haben. Dies ist deutlich schneller als viele andere Online-Casinos, die oft mehrere Tage benötigen, um Auszahlungen zu bearbeiten.
Um eine Auszahlung zu tätigen, müssen Spieler lediglich ihr Konto verifizieren und eine Auszahlungsanforderung über ihr Spielerkonto stellen. Sobald die Anforderung genehmigt wurde, wird das Geld schnell auf das angegebene Konto überwiesen.
Natürlich kann die Auszahlungsdauer je nach Zahlungsmethode variieren. E-Wallets wie Skrill und Neteller ermöglichen in der Regel schnellere Auszahlungen als Banküberweisungen, da die Transaktionen sofort abgewickelt werden können. Spieler sollten daher die für sie am besten geeignete Zahlungsmethode wählen, um ihre Gewinne so schnell wie möglich zu erhalten.
Insgesamt bietet das Zet Casino eine schnelle und zuverlässige Auszahlungsdauer, die es Spielern ermöglicht, ihre Gewinne schnell zu genießen. Mit einer Vielzahl von Zahlungsmethoden und einem effizienten Auszahlungsprozess ist das Zet Casino eine gute Wahl für Spieler, die Wert auf eine schnelle Abwicklung ihrer Gewinne legen.
https://zetcasino.one/
7 Helpful Tips To Make The Most Of Your Vehicle Diagnostics mobile diagnostic (Esperanza)
buy doxycycline without prescription: doxycycline hyclate 100 mg cap – doxycycline monohydrate
9 Lessons Your Parents Teach You About Cheap Couches
For Sale Cheap couches for sale
It’s Time To Extend Your Car Boot Lock Repair Options locker repair near me
What’s The Job Market For Double Glazed Window Repairs Professionals Like?
double glazed window repairs
3 Reasons You’re Buy Sex Machines Is Broken (And How To Fix It) Adult sex machines
How To Ship To Ireland From Uk Tools To Ease Your Daily Life How To Ship To Ireland From Uk Trick Every Individual Should Learn how to ship to ireland From Uk
5 Lessons You Can Learn From Fridge Freezer Sale fridge freezers uk
The Personal Injury Attorney Awards: The Most Stunning, Funniest, And Strangest Things We’ve Ever Seen grover beach personal Injury Attorney
10 Dreme L30-Related Dreme L30-Related Projects That Will Stretch Your Creativity
dreame ultra l30 (Faith)
Индексация ссылок на сайте индекс гугл ру
The 3 Largest Disasters In Online Shopping Sites The Online Shopping Sites’s 3 Biggest Disasters In History online shopping Sites for dress
Guide To Cost Of Private ADHD Assessment UK: The Intermediate Guide
In Cost Of Private ADHD Assessment UK Cost Of Private Adhd Assessment Uk
Boomerang Casino Dokumentation
Boomerang Casino ist ein Online-Casino, das Spielern eine Vielzahl von Spielen, Boni und Aktionen bietet. Um sicherzustellen, dass Spieler das bestmögliche Spielerlebnis haben und alle Funktionen des Casinos optimal nutzen können, ist eine gute Dokumentation unerlässlich.
Die Boomerang Casino Dokumentation beinhaltet Informationen zu den verschiedenen Spielen, die im Casino verfügbar sind, sowie Anleitungen zur Nutzung der verschiedenen Funktionen und Optionen, die das Casino bietet. Die Dokumentation enthält auch Informationen zu den verschiedenen Boni und Aktionen, die im Casino verfügbar sind, sowie zu den Bedingungen, die mit ihnen verbunden sind.
Darüber hinaus enthält die Boomerang Casino Dokumentation Informationen zu den verschiedenen Zahlungsmethoden, die im Casino akzeptiert werden, sowie zu den Ein- und Auszahlungsprozessen. Die Dokumentation bietet auch Unterstützung bei Fragen oder Problemen, die beim Spielen im Casino auftreten können.
Spieler können auf die Boomerang Casino Dokumentation entweder über die Website des Casinos oder über die mobile App zugreifen. Die Dokumentation ist benutzerfreundlich aufgebaut und bietet eine klare und verständliche Anleitung für Spieler aller Spielstärken.
Zusammenfassend lässt sich sagen, dass die Boomerang Casino Dokumentation eine wichtige Ressource für Spieler ist, die das Casino optimal nutzen möchten. Durch die Bereitstellung von umfassenden Informationen und Anleitungen hilft die Dokumentation Spielern dabei, das Beste aus ihrem Spielerlebnis herauszuholen und sicherzustellen, dass sie alle Funktionen und Optionen des Casinos optimal nutzen können.
https://boomerangcasino.one/
Nine Things That Your Parent Teach You About Situs Alternatif
Gotogel situs alternatif Gotogel (tujuan.grogol.us)
Who’s The Top Expert In The World On Washing Machine 12kg?
best washing Machine 12kg
What Car Key Programmer Near Me Is Your Next Big Obsession auto car key programmer near me
How To Beat Your Boss With Leeds Window Repair double Glazing leeds
Компания «Growex Group» более 15 лет оказывает полный комплекс услуг в международном логистическом направлении. Основное направление деятельности заключается в таможенном оформлении, а также контейнерных перевозках, подробнее об оказываемых услугах Вы можете ознакомиться на https://growex-group.ru/ Закажите перевозки автомобильным, морским, воздушным, железнодорожным транспортом.
3 Ways In Which The Sofa Sale Clearance Influences Your Life
couches l shape; https://wall-barron.Federatedjournals.com/this-is-the-history-of-sectional-couches,
These Are The Most Common Mistakes People Make Using CSGO Most Profitable Cases wildfire Case
Why No One Cares About American-Style Fridge Freezers best french
style fridge freezer uk (Latasha)
cheap levitra com
The Reason Why Adding A Reallife Sexdolls To Your Life’s Activities Will Make All The Difference Tpe Sex dolls
The Most Valuable Advice You Can Receive About Slot Demo Pragmatic
demo slot pragmatic play – wwwguide2freecom2c262.zapwp.Com,
5 Killer Quora Answers To Tumble Dryers Heat Tumble Dryers Heat
Solutions To The Problems Of Replacement Double Glazed Window replacement Double glazed Windows
Five Reasons To Join An Online Window Repair Near Shop And
5 Reasons To Not upvc repairs
The Best Tips You’ll Receive About Side By Side Fridge Freezer
Samsung small side by side refrigerator; sekainoriron.hateblo.jp,
24 Hours To Improving Green Power Scooters eco-conscious Mobility solutions
What Is Dreame L30 Review And Why Is Everyone Dissing It?
Dreame Bot L30 Ultra
10 Healthy Window Repair In London Habits window doctor london
8 Tips For Boosting Your Women Double Dildo Game double sided dildoes (https://conerobert54.bravejournal.net/15-up-and-coming-double-ended-dildos-bloggers-you-need-to-check-out)
10 Inspiring Images About Gotogel Link Alternatif Agen slot
You’ll Never Guess This Greenpower Electric Scooters’s Tricks power electric scooter
Cheap Heat Pump Tumble Dryer Tools To Streamline Your
Daily Lifethe One Cheap Heat Pump Tumble Dryer Trick That Everyone Should Learn cheap heat pump tumble dryer
10 Reasons Why People Hate Bmw Replacement Key.
Bmw Replacement Key replacement Key For bmw
You’ll Be Unable To Guess Misted Double Glazing Repairs Near Me’s Benefits double glazing repairs near
me – Shelli,
The 9 Things Your Parents Teach You About Upvc Window Repairs upvc window Repairs
Wenn das Guthaben im Tipico Casino nicht ausreicht
Das Tipico Casino ist eine beliebte Online-Plattform fГјr GlГјcksspiele, die eine Vielzahl von spannenden Spielen und lukrativen Gewinnchancen bietet. Doch was passiert, wenn das Guthaben auf dem Spielerkonto nicht ausreicht, um weiterhin am Spiel teilzunehmen?
In solchen Fällen haben die Spieler verschiedene Möglichkeiten, um ihr Guthaben aufzustocken. Eine Option ist es, eine Einzahlung auf das Spielerkonto vorzunehmen. Dafür stehen verschiedene Zahlungsmethoden wie Kreditkarten, Banküberweisungen oder e-Wallets zur Verfügung. Sobald die Einzahlung getätigt wurde, kann der Spieler das Guthaben nutzen, um weiterhin am Spiel teilzunehmen.
Eine weitere Möglichkeit ist es, von den verschiedenen Bonusangeboten im Tipico Casino zu profitieren. Oftmals werden den Spielern Boni wie Willkommensboni, Einzahlungsboni oder Freispiele angeboten, die es ermöglichen, das Guthaben aufzustocken und dadurch länger am Spiel teilzunehmen.
Es ist wichtig, dass die Spieler verantwortungsvoll mit ihrem Guthaben umgehen und nicht mehr Geld einzahlen, als sie sich leisten können zu verlieren. Das Tipico Casino bietet auch die Möglichkeit, Einzahlungslimits festzulegen oder sich zeitweise vom Spiel auszuschließen, um ein unkontrolliertes Spielen zu verhindern.
Insgesamt bietet das Tipico Casino verschiedene Möglichkeiten, um das Guthaben aufzustocken, wenn es nicht ausreicht. Durch geschicktes Management des Guthabens und die Nutzung von Bonusangeboten können die Spieler ihre Chancen auf Gewinne steigern und gleichzeitig ihr Spielvergnügen verlängern.
https://tipicocasino.one/
The History Of Railroad Injuries Claim In 10 Milestones railroad injury Fela lawyer
You’ll Never Guess This Birth Injury Attorney Fort Collins’s Benefits birth injury attorney fort collins
You cannot tell by just looking at a thing if it
is made up of asbestos. Neither can you smell or taste it.
It can only be found in the event that asbestos-containing
products are drilled, chipped or broken.
My homepage … Vimeo
20 Insightful Quotes About Online Store Uk Cheapest Coarse Texture Paper
cost of neurontin: neurontin 100mg cap – neurontin medicine
5 Common Myths About Vibrating Anal Sex Toys You Should Stay Clear Of buy Anal toys
Are You In Search Of Inspiration? Try Looking Up Window Repair Near Window Repairs
Responsible For The Private ADHD Budget? 12 Top
Ways To Spend Your Money assessment
The 9 Things Your Parents Taught You About Situs Gotogel Terpercaya situs gotogel terpercaya
Buy Dildos Online’s History History Of Buy Dildos
Online ToyJoy Get Real 16 Inch Flesh Double Ended Dildo (Sonya)
Double Glazing Companies Near Me Tools To Make Your Daily Life
Double Glazing Companies Near Me Technique Every Person Needs To Be Able To double Glazing companies near me
prednisone 1mg purchase buy prednisone without a prescription 15 mg prednisone daily
10 Best Books On Brown Squirting Dildo Best
Why No One Cares About Online Shopping Uk Cheap copper grilling accessory
Das Zet Casino ist eine Online GlГјcksspielplattform, die ihren Spielern eine breite Palette von Spielen und lukrativen Boni bietet. Einer der beliebtesten Boni, die das Zet Casino seinen Spielern im Jahr 2019 anbietet, ist der sogenannte “No Deposit Bonus”.
Ein No Deposit Bonus ist eine Art von Bonus, der es Spielern ermöglicht, kostenlose Spiele zu spielen, ohne dass sie zuvor eine Einzahlung tätigen müssen. Das bedeutet, dass Spieler die Möglichkeit haben, das Casino kennenzulernen und verschiedene Spiele auszuprobieren, ohne dabei ihr eigenes Geld riskieren zu müssen.
Der No Deposit Bonus im Zet Casino im Jahr 2019 kann je nach Aktion variieren, aber in der Regel erhalten Spieler entweder Freispiele für ausgewählte Slots oder einen bestimmten Geldbetrag, den sie im Casino verwenden können. Durch diesen Bonus haben Spieler die Möglichkeit, echte Gewinne zu erzielen, ohne dabei ihr eigenes Geld riskieren zu müssen.
Um den No Deposit Bonus im Zet Casino zu erhalten, mГјssen Spieler in der Regel einfach ein Konto erstellen und sich anmelden. AnschlieГџend wird der Bonus automatisch gutgeschrieben oder Spieler mГјssen einen Bonuscode eingeben, um den Bonus zu aktivieren.
Es ist jedoch wichtig zu beachten, dass No Deposit Boni in der Regel bestimmten Bedingungen und Umsatzanforderungen unterliegen, die erfüllt werden müssen, bevor Gewinne aus dem Bonus ausgezahlt werden können. Spieler sollten daher die Bonusbedingungen genau lesen, um sicherzustellen, dass sie die Anforderungen erfüllen und echte Gewinne erzielen können.
Insgesamt bietet der No Deposit Bonus im Zet Casino den Spielern eine großartige Möglichkeit, das Casino und seine Spiele kostenlos kennenzulernen und echte Gewinne zu erzielen. Spieler sollten diese Gelegenheit nutzen und den Bonus beanspruchen, um ihre Gewinnchancen zu erhöhen und das Spielerlebnis im Zet Casino zu maximieren.
https://zetcasino.one/
Responsible For An Best Side By Side Fridge Freezer Budget?
12 Tips On How To Spend Your Money smallest side by side refrigerator freezer
(http://Www.votecataratas.Com)
Why Nobody Cares About Leeds Door Panels nearby
The Guide To Online Shopping Figures Uk In 2023 vimeo.Com
viagra professional sign – avana quiet levitra oral jelly online rep
Unquestionable Evidence That You Need Birth Injury Attorneys Birth Injury Negligence
15 Gifts For The Treadmill Lover In Your Life treadmills sale Uk
9 Lessons Your Parents Taught You About Large
Sectional Sofa large sectional sofa
The Most Effective Reasons For People To Succeed On The Vibrating Panties Online Industry panty vibrating
(Rusty)
Hi! Do you use Twitter? I’d like to follow you if that would be okay. I’m absolutely enjoying your blog and look forward to new posts.
https://squareblogs.net/typhanhntw/h1-b-perevagi-vikoristannia-skla-far-farfarlight-u-vashomu-avto-b-h1
A List Of Common Errors That People Make With Key Programming
cheap car Key programming
5 Killer Quora Answers To Double Glazing Repairs
Leeds double glazing repairs leeds (http://www.newstool.cc)
Ten 18 Wheeler Accident Law Firms That Really Help You Live Better
18 wheeler accident Law firms
The 3 Largest Disasters In I Want To Sell Avon Products The I Want To
Sell Avon Products’s 3 Biggest Disasters In History i want to Sell Avon products
https://prednisoned.online/# prednisone 5 mg tablet cost
What’s The Fuss About Idn Poker? spam
What’s The Job Market For Double Glazing
Door Repairs Near Me Professionals Like? door Repair
20 Reasons Why Double Glazed Windows Repair Near Me Cannot Be Forgotten installed
The 10 Scariest Things About Upvc Windows Repairs upvc windows repairs;
x.sare25.com,
In der Welt der Online-Glücksspiele ist es häufig möglich, Geld von einem Bereich wie Sportwetten auf einen anderen wie das Casino zu übertragen. Dies bietet Spielern eine größere Flexibilität und Auswahlmöglichkeiten, wenn es um ihre Einsätze und Gewinne geht.
Eine beliebte Plattform, die diese Übertragungsmöglichkeit bietet, ist Tipico. Obwohl bekannt für seine Sportwetten, hat Tipico auch ein umfangreiches Online-Casino-Angebot, das von Spielautomaten über Tischspiele bis hin zu Live-Dealer-Spielen reicht. Indem Sie Geld von Ihrem Sportwettenkonto auf Ihr Casino-Konto übertragen, können Sie nahtlos zwischen den beiden Bereichen wechseln und Ihre Lieblingsspiele genießen.
Um Geld von Sportwetten auf das Casino bei Tipico zu übertragen, müssen Sie einfach Ihr Konto aufrufen und den gewünschten Betrag angeben. Beachten Sie jedoch, dass möglicherweise bestimmte Umsatzbedingungen erfüllt werden müssen, bevor eine Übertragung möglich ist. Diese Bedingungen können von Fall zu Fall variieren, und es ist ratsam, die AGBs von Tipico zu überprüfen, um sicherzustellen, dass Sie alle Anforderungen erfüllen.
Die Übertragung von Geld zwischen verschiedenen Bereichen eines Online-Glücksspielanbieters kann Spielern nicht nur mehr Flexibilität bieten, sondern auch dazu beitragen, ihr Spielvergnügen zu maximieren. Indem Sie von Sportwetten auf das Casino wechseln, können Sie verschiedene Spiele ausprobieren und möglicherweise auch höhere Gewinne erzielen.
Insgesamt bietet die Möglichkeit, Geld von Sportwetten auf das Casino bei Tipico zu übertragen, den Spielern eine zusätzliche Möglichkeit, ihre Glücksspielerfahrung zu personalisieren und vielfältiger zu gestalten. Es lohnt sich, diese Option zu nutzen und das Beste aus beiden Welten zu genießen.
https://tipicocasino.one/
viagra professional online effect – cialis professional vim levitra oral jelly queen
Lockout Car Service Tools To Ease Your Daily Life Lockout Car Service Trick Every Person Should Learn Lockout Car Service
Why Replacement Windows Is Still Relevant In 2023 double glazing replacement windows
10 Locksmith Near Me For Cars-Related Projects To Stretch Your Creativity Locksmith Car Keys Near Me
cialis online without perscription
14 Misconceptions Commonly Held About Erb’s Palsy Attorneys
Erb’s palsy lawyer
A Provocative Remark About American Fridge Freezer Sale integrated fridge freezer american
The Most Hilarious Complaints We’ve Seen About Childrens Bunk Bed Bunkbeds for sale
20 Trailblazers Lead The Way In How Much Are Mobility Scooters To Buy Best Electric Scooter
To Buy – http://Www.Fotochki.Com/ –
What’s The Ugly Real Truth Of Windows Leeds upvc door repairs
leeds (Shanel)
Five Killer Quora Answers To Mobility Scooter 4mph mobility Scooter 4mph
Zet Casino Promo Code 2023: Profitieren Sie von exklusiven Angeboten
Wenn Sie auf der Suche nach einem neuen Online Casino sind, das mit großzügigen Bonusaktionen und spannenden Spielen lockt, dann sind Sie bei Zet Casino genau richtig. Das beliebte Online Casino bietet seinen Kunden regelmäßig attraktive Promo Codes, mit denen Sie zusätzliches Guthaben oder Freispiele erhalten können.
Für das Jahr 2023 können Sie sich auf noch mehr lukrative Angebote freuen. Mit dem exklusiven Zet Casino Promo Code 2023 haben Sie die Möglichkeit, von zahlreichen Vorteilen zu profitieren. Egal ob Sie ein erfahrener Spieler sind oder gerade erst in die Welt des Online Glücksspiels eintauchen, mit dem Promo Code können Sie Ihr Spielerlebnis noch spannender gestalten.
Nutzen Sie den Zet Casino Promo Code 2023 bei Ihrer nГ¤chsten Einzahlung und sichern Sie sich einen tollen Bonus. Ob zusГ¤tzliches Guthaben fГјr Ihre Lieblingsspiele oder Freispiele fГјr ausgewГ¤hlte Slots – die MГ¶glichkeiten sind vielfГ¤ltig. Mit dem Promo Code wird Ihr Spielerkonto im Handumdrehen aufgeladen und Sie kГ¶nnen direkt mit dem Spielen loslegen.
Um den Zet Casino Promo Code 2023 zu erhalten, müssen Sie lediglich bei Ihrer Einzahlung den entsprechenden Code eingeben. Schon wird Ihnen der Bonus gutgeschrieben und Sie können sich über zusätzliche Gewinnchancen freuen. Aber beeilen Sie sich, denn die Promo Codes sind oft nur für einen begrenzten Zeitraum gültig.
Also warten Sie nicht länger und sichern Sie sich mit dem Zet Casino Promo Code 2023 lohnende Boni und attraktive Angebote. Tauchen Sie ein in die faszinierende Welt des Online Glücksspiels und erleben Sie spannende Stunden voller Nervenkitzel und Spaß. Viel Glück und viel Spaß!
https://zetcasino.one/
The Benefits Of London Online Clothing Shopping Sites At The Very Least Once In Your Lifetime Vimeo
10 Healthy Drip Coffee Maker Habits Automatic drip coffee makers
30 Inspirational Quotes On Self Emptying Vacuum cleaner
Five Things Everyone Makes Up On The Subject Of Self Emptying Robot Vacuum best robot vacuum For High pile carpet
На сайте http://kinomanhd.vip вы найдете огромное количество сериалов, фильмов в отличном качестве. Есть новые сериалы, фильмы за 2023 и 2024 года. Смотрите все, что хотите в любое время и без регистрации. Есть возможность подобрать оптимальный вариант по актерскому составу, году производства, жанру, режиссерам, стране производства. Имеются подборки про врачей, девушек, маньяков, любовь. Просматривайте фильмы в пятничный вечер или после работы. Картинка эталонного качества, хороший звук.
What Will Attorney Birth Injury Be Like In 100 Years?
birth injury negligence
The 10 Scariest Things About Replacement Porsche Key Fob Replacement porsche key fob
14 Cartoons About Upvc Window Repairs That’ll Brighten Your Day Upvc repairs
What Is Best Sex Machines And Why Are We Dissing
It? Mechanical Sex toys
The Leading Reasons Why People Perform Well Within The Replacement Fiat 500 Key Industry fiat key fob not working
The 10 Most Scariest Things About Replacement Handles For Upvc Windows replacement handles for upvc windows
Five Killer Quora Answers To Locksmith Car Key locksmith car key
5 Killer Quora Answers On 3d Slots 3D Slots – En.trsystem.co.kr,
Das Boomerang Casino in der Schweiz ist ein beliebtes Ziel für Glücksspiel-Enthusiasten. Mit einer Vielzahl von Spielen, großzügigen Boni und einer eleganten Atmosphäre bietet das Casino eine erstklassige Spielerfahrung.
Das Boomerang Casino bietet eine breite Palette von Spielen, darunter Slots, Tischspiele und Live-Dealer-Spiele. Die Spieler können aus verschiedenen Variationen von Blackjack, Roulette, Poker und anderen beliebten Casino-Spielen wählen. Mit hochwertiger Grafik und reibungsloser Gameplay-Software bietet das Boomerang Casino eine hochwertige Spielerfahrung.
Darüber hinaus bietet das Boomerang Casino großzügige Boni und Promotionen für neue und bestehende Spieler. Von Willkommensboni über Einzahlungsboni bis hin zu Treueprogrammen gibt es immer spannende Möglichkeiten, zusätzliches Geld zu gewinnen und das Spielerlebnis zu maximieren.
Die elegante Atmosphäre des Boomerang Casinos trägt dazu bei, dass sich die Spieler wie in einem exklusiven Club fühlen. Mit stilvoller Einrichtung, freundlichem Personal und hochwertigem Service ist das Boomerang Casino der perfekte Ort, um eine Nacht voller Glücksspiel und Unterhaltung zu verbringen.
Insgesamt ist das Boomerang Casino in der Schweiz definitiv einen Besuch wert, ob man ein erfahrener Spieler ist oder einfach nur eine unterhaltsame Nacht verbringen möchte. Mit einer großen Auswahl an Spielen, großzügigen Boni und einer eleganten Atmosphäre bietet das Casino eine erstklassige Spielerfahrung, die man nicht verpassen sollte.
https://boomerangcasino.one/
Five Killer Quora Answers On L Shaped Couches For
Sale l Shaped couch
Asbestos, a naturally occurring mineral is used as an insulator
and a fire-resistant material. For a long time, it was used in a variety of manufacturing, industrial, and commercial
settings in New York and across the country.
Visit my blog: Vimeo.Com
10 Things You Learned From Kindergarden To Help You Get Started With Door
Fitter Leeds u p v c window repairs (Prince)
10 Misconceptions Your Boss Holds Concerning Ghost Immobiliser Install
ford focus ghost installer (Fay)
5 Laws Everyone Working In Motorcycle Accident Attorney Should Know princeton Motorcycle
accident lawyer (vimeo.com)
10 Tell-Tale Warning Signs You Need To Look For A New Bunk Beds For Children Bunk Beds Sale Uk
Are You Responsible For An Online Shopping Uk For Clothes Budget?
12 Best Ways To Spend Your Money Beauty Station With Storage
The Most Effective Reasons For People To Succeed On The Key Programmer Industry car Keys programmed near Me
13 Things You Should Know About Medical Malpractice Lawsuit That
You Might Not Have Known marble falls medical malpractice attorney, vimeo.com,
Five Lock Keys In Car Projects To Use For
Any Budget open The Car
Are You Responsible For A Mesothelioma Asbestos Lawyer Budget?
12 Top Ways To Spend Your Money new york mesothelioma Lawyer
(toolbarqueries.google.co.ve)
15 Trends That Are Coming Up About Drip Coffee best filter coffee machine uk
[Margie]
The Ghost Tracker Installation Success Story You’ll Never Imagine auto
You’ll Never Guess This Double Glazed Windows Repair Near Me’s Benefits Fit
Link Alternatif Gotogel Tools To Improve Your Daily Life Link Alternatif Gotogel Trick Every Person Should Know Link alternatif Gotogel
The Leading Reasons Why People Are Successful With The Tommy Hilfiger Women’s Bag Industry shoulder Bag tommy hilfiger
Zet Casino: Die bequeme Einzahlung mit Zimpler
Das Zet Casino ist eine beliebte Online-Glücksspielplattform, die eine Vielzahl von Spielen und Dienstleistungen für Spieler aus der ganzen Welt anbietet. Eine der neuesten Innovationen, die das Zet Casino seinen Spielern bietet, ist die Möglichkeit, mit Zimpler einzuzahlen.
Zimpler ist eine mobile Zahlungsmethode, die es den Nutzern ermöglicht, Einzahlungen auf ihren Casino-Account schnell und einfach über ihr Mobilgerät zu tätigen. Durch die Verwendung von Zimpler können Spieler ihre Einzahlungen ohne lange Wartezeiten und lästige Banküberweisungen tätigen.
Das Zet Casino hat sich dazu entschlossen, Zimpler als Zahlungsmethode anzubieten, um seinen Spielern eine bequeme und sichere Option für Einzahlungen anzubieten. Mit Zimpler können Spieler ihr Konto aufladen, ohne sensible Bankdaten preiszugeben, da die Transaktionen einfach über ihre Handynummer verifiziert werden.
Darüber hinaus bietet Zimpler Spielern die Möglichkeit, ihr Spielverhalten im Auge zu behalten, indem sie Einzahlungslimits festlegen können. Auf diese Weise können Spieler sicherstellen, dass sie ihr Budget im Griff haben und verantwortungsbewusst spielen.
Insgesamt bietet das Zet Casino seinen Spielern mit der Zimpler-Zahlungsmethode eine bequeme und sichere Möglichkeit, Einzahlungen zu tätigen. Spieler können sich auf ein reibungsloses und professionelles Spielerlebnis freuen, das sowohl unterhaltsam als auch sicher ist. Probieren Sie Zimpler im Zet Casino aus und erleben Sie die Vorteile dieser innovativen Zahlungsmethode!
https://zetcasino.one/
Why Double Glazed Windows Repairs Is More Difficult Than You Think Double Glazing [xilubbs.xclub.tw]
buy neurontin uk: neurontin 500 mg tablet – neurontin 1000 mg
10 Best Mobile Apps For Car Lock Smith car lock smith near me
(Yetta)
The Top 5 Reasons People Win At The Fiat 500 Keys Industry how to unlock fiat 500 without key; Rosalyn,
Five People You Should Know In The Repairs To Upvc Windows
Industry window repairs
neurontin 200 neurontin cost uk neurontin cream
A Commercial Truck Accident Attorney Success Story You’ll Never
Be Able To Vimeo.com
A Provocative Rant About Locksmith For Car repair
What Idn Poker Experts Want You To Be Educated spam
Why No One Cares About Double Glazed Window Near Me
double Glassing
What Window Glass Repair Near Me Is Your Next Big Obsession sash
You’ll Never Guess This Window Repair Near Me’s Benefits window Repair near me
Guide To 12kg Washing Machine Sale: The Intermediate Guide In 12kg
Washing Machine Sale 12Kg washing Machine – Washersanddryers.Co.uk,
See What Repair Upvc Windows Tricks The Celebs Are Making Use Of repair upvc Window (korsholm-barr.technetbloggers.de)
10 Things Everybody Hates About Mesothelioma Lawyer Mesothelioma lawsuits
The 9 Things Your Parents Teach You About Double Over Double Bunk Beds For Adults double over double bunk beds
Five Glazing Repairs Near Me Lessons From Professionals Double Glazing Repairs Near Me
One Of The Most Untrue Advices We’ve Ever Heard About Treadmill For Home price
Das Tipico Casino bietet eine Vielzahl von unterschiedlichen Spielen für jeden Geschmack an. Egal ob Slots, Tischspiele oder Live-Casino – hier wird jeder fündig. Aber wussten Sie schon, dass man im Tipico Casino bereits ab 5 Cent spielen kann?
Ja, richtig gelesen! Im Tipico Casino können Sie bereits mit einem Einsatz von nur 5 Cent an den verschiedenen Spielautomaten Ihr Glück versuchen. Das ist besonders für Einsteiger oder vorsichtige Spieler sehr attraktiv, da man mit einem geringen Einsatz die Chance hat, tolle Gewinne zu erzielen.
Die Auswahl an Spielen, bei denen man mit 5 Cent spielen kann, ist groß. Von klassischen Slots bis hin zu modernen Video-Slots ist für jeden etwas dabei. Auch progressive Jackpot-Slots, bei denen man mit etwas Glück riesige Gewinne abräumen kann, stehen zur Verfügung.
Aber nicht nur bei den Spielautomaten kann man mit 5 Cent spielen, auch bei verschiedenen Tischspielen wie Roulette oder Blackjack ist es möglich, mit einem kleinen Einsatz dabei zu sein. So können auch Spieler mit kleinerem Budget die Spannung und den Nervenkitzel eines Casinos erleben.
Das Tipico Casino zeichnet sich nicht nur durch seine Vielfalt an Spielen aus, sondern auch durch seine benutzerfreundliche Plattform und den professionellen Kundenservice. Ein- und Auszahlungen können sicher und bequem über verschiedene Zahlungsmethoden getätigt werden, sodass man sich ganz auf das Spiel konzentrieren kann.
Also, wenn Sie Lust auf spannende Casino-Spiele haben, aber nicht gleich große Summen investieren möchten, dann ist das Tipico Casino mit seinen 5 Cent Spielen genau das Richtige für Sie. Probieren Sie es doch einfach mal aus und erleben Sie die aufregende Welt des Casinos!
https://tipicocasino.one/
Window Repairs Techniques To Simplify Your Daily
Life Window Repairs Trick Every Person Should Know Window Repairs; https://Click4R.Com/Posts/G/11374483/,
Хотите купить с быстрой доставкой цветы в коробке? Интернет магазин «Флорион» в этом вам обязательно поможет! Квалифицированные флористы с творческим подходом осуществляют оригинальные букеты с душой. Они стремятся удовлетворить ожидания клиентов и даже их превзойти. Ищете цветы в коробке купить? Florion.ru – сайт, где можно заказать и выбрать букет. Вы можете связаться с компетентным менеджером, и он предоставит вам детальную информацию. Дарите удовольствие с помощью прекрасных цветов в коробке!
How Windows And Doors Leeds Influenced My Life For The Better upvc Door repairs roundhay (https://www.df100.cn/home.php?mod=space&uid=2507571)
Ghost Installations Tools To Streamline Your Everyday Lifethe Only Ghost Installations Trick
That Every Person Should Know Ghost installations
Three Common Reasons Your Double Glazing In Luton Isn’t Working
(And How To Fix It) window and door companies near me
This Week’s Most Remarkable Stories About Bmw Replacement Keys Bmw Replacement Keys
Replacement Key For Bmw (Confident-Alpaca-Fhtxzv.Mystrikingly.Com)
http://zithromaxa.store/# buy zithromax without prescription online
The 12 Worst Types Of People You Follow On Twitter 9kg washer machine (Rowena)
WeJiJ is here to help get you the best gaming setup, gaming PC and guide you through the games you like to play with news, reviews and guides. https://wejij.com/
Find the latest technology news and expert tech product reviews. Learn about the latest gadgets and consumer tech products for entertainment, gaming, lifestyle and more. https://axget.com/
Easier WWW is a leading technology site that is dedicated to produce great how-to, tips and tricks and cool software review. https://easierwww.com/
How To Beat Your Boss With Search Engine Optimisation search engine optimisation Company
Zet Casino 20 Freispiele
Das Zet Casino bietet seinen Spielern eine großzügige Auswahl an Boni und Promotionen, darunter auch 20 Freispiele, die für neue Spieler verfügbar sind. Diese Freispiele können auf ausgewählten Slots im Online Casino gespielt werden und bieten eine großartige Gelegenheit, das Casino und die Spiele kostenlos zu testen.
Um die 20 Freispiele zu erhalten, müssen neue Spieler lediglich ein Konto im Zet Casino erstellen und ihre erste Einzahlung tätigen. Sobald die Einzahlung bestätigt wurde, werden die 20 Freispiele automatisch gutgeschrieben und können sofort genutzt werden. Es gibt keine weiteren Bedingungen oder Anforderungen, um von diesem Angebot zu profitieren.
Die Freispiele kГ¶nnen auf verschiedenen Slots im Zet Casino gespielt werden, darunter beliebte Spiele wie Starburst, Book of Dead und Gonzo’s Quest. Spieler haben die MГ¶glichkeit, echtes Geld zu gewinnen und ihre Gewinne nach ErfГјllung der Umsatzbedingungen auszuzahlen.
Das Zet Casino ist bekannt für sein vielfältiges Spielangebot, seine großzügigen Boni und seine sichere und faire Spielumgebung. Mit einer Lizenz der Malta Gaming Authority können Spieler sicher sein, dass sie in einem vertrauenswürdigen Online Casino spielen.
Insgesamt sind die 20 Freispiele im Zet Casino eine großartige Möglichkeit, das Casino kostenlos zu entdecken und echte Gewinne zu erzielen. Neue Spieler werden ermutigt, dieses Angebot zu nutzen und die aufregenden Spiele und Funktionen des Zet Casinos zu erleben.
https://zetcasino.one/
The Most Sour Advice We’ve Ever Received On CSGO
New Case case Skins
Walking Machine Desk Tools To Ease Your Everyday Lifethe Only Walking Machine Desk Trick Every Individual Should Learn Walking Machine Desk
(W0A4Q94Nk4.Execute-Api.Eu-West-1.Amazonaws.Com)
11 Ways To Completely Sabotage Your CSGO Case Battle Site case fracture
12 Companies Setting The Standard In Auto Lock Smiths mobile auto Locksmiths
Testosil is a natural polyherbal testosterone booster designed to help men increase their testosterone levels safely and effectively. https://testosil-web.com/
Why We Love Robot Vacuum Best (And You Should Also!)
Mop vacuum robot
How To Tell The Right Idn Poker For You spam
9 Lessons Your Parents Teach You About Self-Emptying Robot Vacuum And Mop self-emptying Robot vacuum And mop
15 Amazing Facts About Tall Larder Freezer That You Didn’t Know About Digital Freezers
The Companies That Are The Least Well-Known To Follow In The Mesothelioma Attorneys Industry asbestos exposure Lawyers
Nagano Lean Body Tonic is a groundbreaking powdered supplement crafted to support your weight loss journey effortlessly. https://naganotonic-try.com/
KeraBiotics is a meticulously-crafted natural formula designed to help people dealing with nail fungus. This solution, inspired by a sacred Amazonian barefoot tribe ritual https://kerabiotics-web.com/
– Shoot MASSIVE Loads For An Amazing Finish! https://semenax-try.com/
The 10 Most Terrifying Things About Leeds Double Glazing Leeds double glazing
ZenCortex Research’s contains only the natural ingredients that are effective in supporting incredible hearing naturally.A unique team of health and industry professionals dedicated to unlocking the secrets of happier living through a healthier body. https://zencortex-try.com/
Fleshlight Masturbator Tools To Make Your Life
Everyday best fleshlight Interior
Boomerang Casino Recensioni: Ein Blick in die Welt des Online-GlГјcksspiels
Online-Casinos erfreuen sich immer größerer Beliebtheit, da sie den Spielern die Möglichkeit bieten, bequem von zu Hause aus zu spielen und dabei echtes Geld zu gewinnen. Eines der neuesten Casinos auf dem Markt ist das Boomerang Casino, das mit seinem breiten Angebot an Spielen und attraktiven Boni die Aufmerksamkeit vieler Spieler auf sich zieht.
Die Boomerang Casino Recensioni, also die Bewertungen und Erfahrungsberichte der Spieler, sind durchweg positiv. Viele loben die große Auswahl an Slots, Tischspielen und Live-Casino-Spielen, die für jeden Geschmack etwas zu bieten haben. Darüber hinaus werden auch die schnellen Auszahlungen und der kompetente Kundenservice des Casinos gelobt. Die Spieler schätzen auch die Vielzahl an Zahlungsmethoden und die Sicherheit, die das Boomerang Casino bietet.
Ein weiterer Pluspunkt des Boomerang Casinos sind die großzügigen Boni und Aktionen, die regelmäßig angeboten werden. Neue Spieler können sich über einen Willkommensbonus freuen, der ihre erste Einzahlung verdoppelt und ihnen so zusätzliche Chancen auf Gewinne bietet. Darüber hinaus gibt es auch regelmäßige Turniere und Verlosungen, bei denen die Spieler attraktive Preise gewinnen können.
Insgesamt hinterlässt das Boomerang Casino bei den Spielern einen positiven Eindruck und ist definitiv einen Besuch wert. Mit einer ansprechenden Spielauswahl, lukrativen Boni und einem zuverlässigen Kundenservice bietet das Casino alles, was man sich von einem guten Online-Casino wünscht. Wer also Lust auf spannende Glücksspiele hat, sollte das Boomerang Casino definitiv einmal ausprobieren und sich selbst von seinen Qualitäten überzeugen.
https://boomerangcasino.one/
Tonic Greens is a ready-made greens shake designed to support the entire body and wellness of the mind. It is filled with over 50 individual vitamins https://tonicgreens-try.com/
MenoPhix is a menopause relief supplement featuring a blend of plant extracts to target the root cause of menopause symptoms. https://menophix-web.com/
20 Myths About Uk Online Phone Shopping Sites:
Debunked Unique Rustic Tree Light
20 Questions You Need To To Ask About 9kg Washing Machines Before You Buy 9kg
Washing Machines Buy 9kg Washing machine
7 Tricks To Help Make The Most Out Of Your Double Glazed Windows Near Me double Gkazing
The History Of Ford Replacement Key Uk replacement Ford key fob
15 Up-And-Coming Accident Lawyer Tulsa Bloggers You Need To Follow
injury attorney near me
How To Know If You’re Prepared For Window Companies Leeds window Hinge repairs leeds
12 Facts About Volkswagen Key Programming To Refresh Your
Eyes At The Cooler. Cooler locksmith volkswagen keys (promarket.in.ua)
Some Of The Most Common Mistakes People Make With Fridge Freezer Black household
BalMorex Pro is an exceptional solution for individuals who suffer from chronic joint pain and muscle aches. With its 27-in-1 formula comprised entirely of potent and natural ingredients, it provides unparalleled support for the health of your joints, back, and muscles. https://balmorex-try.com/
What’s Holding Back In The Bentley Continental Key Programming Industry?
Bentley Smart Key
20 Reasons Why Malpractice Lawyers Will Not Be
Forgotten Mascotte Malpractice Law Firm
10 Healthy Audi Advanced Key Habits replacement audi Key cost
What’s The Job Market For Bmw Series 1 Key Professionals Like?
bmw series 1 Key
CSGO Battle Case Explained In Fewer Than 140 Characters weapon case (Candra)
15 Up-And-Coming Squirt Dildos Bloggers You Need To Follow Dildo that Squirt
15 Reasons Why You Shouldn’t Overlook Railroad Injuries Law
railroad injury lawyer ottawa (Louis)
10 Facts About Case Opening Battle CSGO That Can Instantly Put You In An Optimistic Mood kilowatt
case (Anibal)
Support the health of your ears with 100% natural ingredients, finally being able to enjoy your favorite songs and movies https://quietumplus-try.com/
This Story Behind Semi Truck Lawyer Is One That
Will Haunt You Forever! lake bluff semi truck accident law firm
Peak BioBoost is a revolutionary dietary supplement that leverages the power of nature to support and improve your digestive system. https://peakbioboost-web.com/
What You Should Be Focusing On Enhancing Leeds Door And Window window Hinge repairs leeds
15 Twitter Accounts That Are The Best To Learn More About Window Glass Replacement Window Glass Replacement Near Me
Zet Casino Bonus
Immer mehr Online-Casinos bieten ihren Kunden attraktive Boni und Promotionen an, um sich von der Konkurrenz abzuheben und neue Spieler anzulocken. Das Zet Casino ist hier keine Ausnahme und punktet mit einem groГџzГјgigen Willkommensbonus fГјr Neukunden.
Der Zet Casino Bonus umfasst nicht nur einen Einzahlungsbonus, sondern auch Freispiele für ausgewählte Spielautomaten. Neue Spieler können sich über einen Bonus von bis zu 500€ und 200 Freispiele freuen, die ihnen einen guten Start in die Welt der Online-Casinos ermöglichen.
Um den Bonus zu erhalten, müssen Spieler lediglich eine erste Einzahlung tätigen und den Bonuscode eingeben. Der Bonus wird dann sofort auf das Spielerkonto gutgeschrieben und kann für verschiedene Spiele im Zet Casino genutzt werden. Es lohnt sich jedoch, die Bonusbedingungen zu lesen, um sicherzustellen, dass man alle Anforderungen erfüllt, um den Bonus und mögliche Gewinne auszahlen zu können.
Neben dem Willkommensbonus bietet das Zet Casino auch regelmäßige Promotionen und Aktionen für bestehende Kunden an. So können Spieler von Reload-Boni, Cashback-Aktionen und Turnieren profitieren, die zusätzliche Gewinnchancen bieten.
Insgesamt überzeugt das Zet Casino nicht nur mit seinem vielfältigen Spielangebot und seiner benutzerfreundlichen Oberfläche, sondern auch mit großzügigen Boni und Promotionen, die sowohl neue als auch erfahrene Spieler ansprechen. Wer also auf der Suche nach einem neuen Online-Casino ist, sollte das Zet Casino definitiv in Betracht ziehen und sich den attraktiven Bonus sichern.
https://zetcasino.one/
The Secret Secrets Of Ghost Alarm Installation Cost
Is Automobile Locksmith Near Me The Best Thing There
Ever Was? auto lock smith
The 10 Scariest Things About Door Fitters Leeds fitter
The 10 Most Scariest Things About Self Emptying Robot Vacuum
Pet Hair Self emptying robot Vacuum Pet hair
What Experts Say You Should Learn Adhd Private Assessment Cost
5 Killer Queora Answers On Treadmill For Sale Near Me high
brand name neurontin price canada neurontin 100mg discount generic neurontin
GutOptim is a digestive health supplement designed to support your gut and stomach. It restore balance in gut flora and reduce the symptoms of digestive disorders. https://gutoptim-try.com/
5 Lessons You Can Learn From Window Repair Near Window Repair Near Me
Watch Out: How Window Repair Is Taking Over And What Can We Do About It repairer
30 Inspirational Quotes On Coffee Machine With Pods Bean to cup machines
17 Reasons You Shouldn’t Be Ignoring Top Accident And Personal Injury Lawyers injury case evaluation
There’s A Good And Bad About Tommy Hilfiger Bag women’s Handbag tommy Hilfiger
The 10 Most Terrifying Things About Upvc Windows Repairs Upvc Windows Repairs (https://Menwiki.Men/Wiki/How_To_Become_A_Prosperous_Upvc_Double_Glazed_Windows_Even_If_Youre_Not_Businesssavvy)
Das Boomerang Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und groГџzГјgigen Boni anbietet. Eine wichtige Frage, die viele Spieler haben, ist jedoch, wie die Auszahlungen im Boomerang Casino funktionieren.
Die Boomerang Casino Auszahlungsmethoden variieren je nach Land und Spielerstatus. In der Regel bietet das Casino eine Vielzahl von sicheren und schnellen Zahlungsmethoden wie Kreditkarten, E-Wallets und BankГјberweisungen an.
Um eine Auszahlung im Boomerang Casino zu tätigen, müssen Spieler zunächst sicherstellen, dass sie alle Bonusbedingungen erfüllt haben. Dies kann Bedingungen wie das Erfüllen des Wettumsatzes und die Verifizierung des Kontos umfassen.
Sobald die Bedingungen erfüllt sind, können Spieler eine Auszahlung beantragen. Dies erfolgt in der Regel über das Konto des Spielers, auf das sie ihr Geld erhalten möchten. Die Bearbeitungszeit variiert je nach Auszahlungsmethode, kann jedoch innerhalb weniger Stunden bis zu mehreren Tagen dauern.
Es ist wichtig zu beachten, dass das Boomerang Casino Sicherheitsmaßnahmen zum Schutz der Spielerdaten und -gelder implementiert hat. Dies bedeutet, dass Spieler bei der Auszahlung ihrer Gewinne sicher sein können, dass ihre Transaktion sicher und geschützt ist.
Insgesamt bietet das Boomerang Casino eine zuverlässige und transparente Auszahlungserfahrung für Spieler. Mit einer Vielzahl von Zahlungsmethoden und schnellen Bearbeitungszeiten können Spieler ihre Gewinne schnell und sicher erhalten.
https://boomerangcasino.one/
amoxicillin price canada: amoxicillin 500mg – amoxicillin 875 mg tablet
How Double Glazing South London Propelled To The Top Trend
On Social Media glass Fitters london
10 Things That Your Family Taught You About Santa Fe
Birth Injury Attorney Santa Fe Birth Injury Attorney
What’s The Job Market For Window.Replacement Near Me Professionals Like?
Window.replacement Near me
You’ll Be Unable To Guess Ford Key Fob Replacement’s Secrets ford key fob replacement
It’s Time To Expand Your Double Glazed Window Repair Options Window repairs Near Me
The 10 Most Terrifying Things About Repairing Upvc Windows Window Repair
13 Things You Should Know About Michael Kors Handbags That You Might Not Have Known michael Kors handbags brown – http://polimentosroberto.com.br/index.php?option=com_k2&view=itemlist&task=user&id=3402683 –
Burn Boost Powder™ is a proven weight loss powder drink that helps to lose weight and boosts the overall metabolism in the body. https://burnboost-web.com
What’s The Reason You’re Failing At Double Glazing Near Me double
glazing company near me (Rodrick)
NanoDefense Pro utilizes a potent blend of meticulously chosen components aimed at enhancing the wellness of both your nails and skin. https://nanodefense-web.com/
ONLINE EXCLUSIVE OFFER! Only Available for purchase on the official website. Secure Your Package while stocks last https://prodentim-web.com
Международный институт современного образования выполняет квалифицированную подготовку специалистов, он достоин вашего внимания. Преподаватели – настоящие профессионалы. Учебный процесс поставлен на высочайшем уровне. Ищете воспитатель детского сада? Misokmv.ru – сайт, где о нас имеется более детальная информация. Мы гарантируем бережное отношение и считаем, что никогда не поздно учиться. Вы всегда можете получить ответы на свои вопросы. Выбирайте нас и не пожалеете об этом. Получить образование в «МИСО» – удобно и выгодно, звоните нам прямо сейчас!
The 10 Scariest Things About Online Shopping Stores List online shopping stores list (Jonas)
9 Things Your Parents Taught You About Self Empty
Robot Vacuum self empty robot vacuum [Matthias]
The Most Pervasive Issues With Local Auto Locksmith Auto Locksmith Service
Nine Things That Your Parent Taught You About Upvc Window Repairs Upvc window repairs near me
5 Killer Qora’s Answers To American Style Fridge Freezers american Fridges
It’s The Complete Cheat Sheet For Best Online
Companies To Work For Part time Work from Home
Is Technology Making Car Accident Law Better Or Worse?
Car Accident Attorney
The 10 Scariest Things About Leeds Double Glazing leeds double
glazing [Clayton]
This Most Common Repair Upvc Windows Debate Actually Isn’t As Black And White As You Might Think Upvc repair
The 10 Most Dismal Bmw Replacement Key FAILURES Of All Time Could Have Been Prevented
Bmw key replacement
Five Killer Quora Answers To Double Glazing Repairs Leeds glazing repairs leeds (https://www.cheaperseeker.com)
10 Things We All Hate About Replacement Handles For Upvc Windows Domestic
http://gabapentinneurontin.pro/# 600 mg neurontin tablets
10 Things That Your Family Taught You About Mesothelioma Lawsuit Attorney Assistance
mesothelioma lawsuit attorney assistance (notabug.org)
Das Tipico Online Casino hat seinen Hauptsitz auf der Insel Malta, genauer gesagt in der Hauptstadt Valletta. Malta gehört zu den führenden Standorten für Online-Glücksspiele in Europa, da das Land eine strikte Regulierung und Gesetzgebung in Bezug auf Online-Casinos hat.
Durch die Regulierung der Malta Gaming Authority (MGA) ist das Tipico Online Casino gezwungen, strenge Richtlinien einzuhalten, um ein faires und sicheres Spielerlebnis zu gewährleisten. Die MGA überwacht und kontrolliert alle Aktivitäten des Casinos, um sicherzustellen, dass alle Spiele fair und transparent ablaufen.
Ein weiterer Vorteil des Standorts Malta ist die steuerliche Situation für Online-Casinos. Malta bietet attraktive Steuervorteile, die es Online-Glücksspielunternehmen ermöglichen, Gewinne auf legale Weise zu erwirtschaften. Dies ermöglicht es dem Tipico Online Casino, seinen Spielern eine Vielzahl von Spielen anzubieten, ohne hohe Steuern zahlen zu müssen.
Darüber hinaus bietet Malta eine stabile Wirtschaft und ein attraktives Geschäftsumfeld für Online-Casinos. Die gut ausgebildete Arbeitnehmerschaft, die Infrastruktur und die Nähe zu anderen europäischen Märkten machen Malta zu einem idealen Standort für das Tipico Online Casino.
Insgesamt profitiert das Tipico Online Casino von seinem Standort auf Malta durch die regulatorischen Vorteile, steuerlichen Anreize und das attraktive Geschäftsumfeld. Dadurch kann das Casino seinen Spielern ein sicheres und unterhaltsames Spielerlebnis bieten und gleichzeitig erfolgreich am Markt agieren.
https://tipicocasino.one/
The Secret Life Of Car Diagnostic Near Me mercedes Diagnostic
near me (http://79Bo3.com/)
Why Nobody Cares About Gotogel Link Alternatif Lottery online
9 . What Your Parents Taught You About GSA SER Download Gsa ser download
priligy american – udenafil notion cialis with dapoxetine nonsense
Seven Explanations On Why Become An Avon Representative Online
Is Important become an Avon Representative online
levitra half life
What’s The Current Job Market For American Fridge Frezzer Professionals Like?
American Fridge Frezzer
9 Things Your Parents Taught You About Double Glazed Window Suppliers Near Me Double glazed window suppliers near me
15 Top Pinterest Boards From All Time About Upvc Window Repair Near Me upvc Window
Repairs Near me (bitetheass.Com)
What To Do To Determine If You’re Ready To Go After Cheapest
10kg Washing Machine near By
15 Things You Didn’t Know About Real Money Slots jackpot Slots
Buzzwords, De-Buzzed: 10 Other Ways For Saying Double Glazing Repairs London pvc windows london
3 Reasons You’re 4mph Mobility Scooter Is Broken (And How To Repair
It) 4Mph Mobility Scooters
Nine Things That Your Parent Taught You About Replacement
Double Glazed Windows replacement double glazed windows
See What Side By Side Fridge And Freezer Tricks The Celebs
Are Making Use Of Side by side fridge and freezer
What Is The Reason? Car Spare Key Is Fast Becoming The Hot Trend For 2023?
Car Spare keys
9 . What Your Parents Taught You About Bentley Key Fob
Programming Bentley key Fob programming
Сайт https://центрпрофмонтаж.рф/ это установка септиков из бетонных колец в Московской области, а также автономных станций ЛОС для частных домов и дач.
15 Terms That Everyone Is In The Double Glazed Windows Repair Industry Should
Know Window Repair
11 Ways To Fully Defy Your Kansas City Birth Injury Attorney Birth Injury Legal Guidance
Онлайн-заведение «Vavada» предлагает сыграть в увлекательные и интересные игры, а заодно и заработать на своем увлечении. На сайте представлен лицензированный контент, что дает возможность выиграть крупную сумму. Казино было основано в 2017 году, и за это время стало одним из самых популярных. Работает по лицензии Кюрасао. На сайте https://vavadaplay3.com/ ознакомьтесь с условиями игры и возможностями.
The 9 Things Your Parents Taught You About Glass Replacement
Windows glass replacement windows – Humberto –
The Secret Secrets Of Bunk Beds Double Bed 4ft loft Bed (olderworkers.com.au)
Sash Window Replacement Tools To Help You Manage Your Daily Life Sash Window Replacement Trick That Should Be Used By Everyone Be Able
To sash window replacement (Florian)
5 Killer Quora Answers On Lost Keys To Car No
Spare Lost Keys To car No Spare
Guide To Upvc Windows Near Me: The Intermediate Guide The Steps To Upvc Windows Near Me Upvc Windows Near Me
(Opensourcebridge.Science)
5 Killer Quora Answers On Egg Vibrator eggs
Dreame L30 Ultra Price Tools To Streamline Your Daily Life Dreame L30 Ultra Price Trick Every Person Should Be Able To dreame L30 Ultra price
Zet Casino Login – Alles, was Sie wissen mГјssen
Wenn Sie auf der Suche nach einem spannenden Online-Casino sind, dann sollten Sie definitiv Zet Casino in Betracht ziehen. Mit einer breiten Auswahl an Spielen, groГџzГјgigen Boni und einem benutzerfreundlichen Interface bietet Zet Casino ein erstklassiges Spielerlebnis fГјr alle Casino-Enthusiasten.
Um bei Zet Casino spielen zu können, müssen Sie sich zunächst registrieren und ein Konto erstellen. Der Anmeldeprozess ist schnell und einfach und erfordert nur einige grundlegende Informationen wie Ihren Namen, Ihre E-Mail-Adresse und Ihren Wohnsitz. Sobald Sie Ihr Konto erstellt haben, können Sie sich mit Ihren Anmeldeinformationen unter Zet Casino Login anmelden und sofort mit dem Spielen beginnen.
Einmal angemeldet, haben Sie Zugriff auf Hunderte von beliebten Casinospiele, darunter Slots, Tischspiele, Live-Dealer-Spiele und mehr. Zet Casino arbeitet mit den besten Spieleanbietern der Branche zusammen, darunter NetEnt, Microgaming und Play’n GO, um sicherzustellen, dass Sie das bestmГ¶gliche Spielerlebnis haben.
Zet Casino belohnt seine Spieler auch regelmäßig mit lukrativen Boni und Aktionen. Von Willkommensboni für neue Spieler bis zu wöchentlichen Sonderaktionen und Treueprogrammen, gibt es immer etwas zu gewinnen bei Zet Casino.
Darüber hinaus bietet Zet Casino eine sichere und zuverlässige Spielerfahrung. Die Website ist mit der neuesten SSL-Verschlüsselungstechnologie geschützt, um sicherzustellen, dass Ihre persönlichen und finanziellen Daten jederzeit sicher sind.
Also, wenn Sie nach einem unterhaltsamen und lohnenden Online-Casino-Erlebnis suchen, dann melden Sie sich noch heute bei Zet Casino an und erleben Sie die Aufregung des Spielens in einem der besten Casinos im Internet. Viel GlГјck und viel SpaГџ!
https://zetcasino.one/
You’ll Never Guess This Car Locksmith’s Tricks car Locksmith
反向链接金字塔
G搜尋引擎在多次更新後需要套用不同的排名參數。
今天有一種方法可以使用反向链接吸引G搜尋引擎對您的網站的注意。
反向链接不僅是有效的推廣工具,也是有機流量。
我們會得到什麼結果:
我們透過反向連結向G搜尋引擎展示我們的網站。
他們收到了到該網站的自然過渡,這也是向G搜尋引擎發出的信號,表明該資源正在被人們使用。
我們如何向G搜尋引擎表明該網站具有流動性:
個帶有主要訊息的主頁反向連結
我們透過來自受信任網站的重新定向來建立反向連接。
此外,我們將網站放置在独立的網路分析器上,網站最終會進入這些分析器的缓存中,然後我們使用產生的連結作為部落格、論壇和評論的重新导向。 這個重要的操作向G搜尋引擎顯示了網站地圖,因為網站分析器顯示了有關網站的所有資訊以及所有關鍵字和標題,這很棒
有關我們服務的所有資訊都在網站上!
The Three Greatest Moments In Window Repairs Luton History front doors luton
See What Repair Upvc Windows Tricks The Celebs Are Utilizing repair upvc window (b.cari.com.my)
Why Automobile Locksmiths Near Me Is Everywhere This Year auto locksmith near me now
The Most Common Online Shopping Uk Cheap Debate Could Be As Black And White As You May Think vehicle theft Protection Lock
Мастер Азарных Илья Владимирович имеет нужные навыки, умения и знания. В своей профессиональной деятельности он не останавливается на достигнутом результате. Клиенты от сотрудничества с ним остаются довольными, потому как он гарантирует оперативность, доступные цены и качество услуг. Ищете ремонт принтера самсунг цена? Zipprinters.ru – сайт, где представлена контактная информация специалиста. Обращайтесь к настоящему профессионалу. Илья Владимирович поможет решить вашу проблему и будет рад вас видеть среди своих клиентов!
3 Common Causes For Why Your Coffee Bean Machine Isn’t Performing (And
How To Fix It) Coffee bean Machines
15 Best Twitter Accounts To Learn More About Bmw Replacement Key bmw replacement Key Cost
You’ll Never Guess This Upvc Window Repairs’s Tricks upvc window Repair
Aquí está el texto con la estructura de spintax que propone diferentes sinónimos para cada palabra:
“Pirámide de enlaces de retroceso
Después de varias actualizaciones del motor de búsqueda G, necesita aplicar diferentes opciones de clasificación.
Hay una forma de llamar la atención de los motores de búsqueda a su sitio web con backlinks.
Los vínculos de retroceso no sólo son una táctica eficaz para la promoción, sino que también tienen tráfico orgánico, las ventas directas de estos recursos más probable es que no será, pero las transiciones será, y es poedenicheskogo tráfico que también obtenemos.
Lo que vamos a obtener al final en la salida:
Mostramos el sitio a los motores de búsqueda a través de backlinks.
Conseguimos visitas orgánicas hacia el sitio, lo que también es una señal para los buscadores de que el recurso está siendo utilizado por la gente.
Cómo mostramos los motores de búsqueda que el sitio es líquido:
1 enlace se hace a la página principal donde está la información principal
Hacemos enlaces de retroceso a través de redirecciones de sitios de confianza
Lo más IMPORTANTE colocamos el sitio en una herramienta independiente de analizadores de sitios, el sitio entra en la caché de estos analizadores, luego los enlaces recibidos los colocamos como redirecciones en blogs, foros, comentarios.
Esta crucial acción muestra a los buscadores el MAPA DEL SITIO, ya que los analizadores de sitios muestran toda la información de los sitios con todas las palabras clave y títulos y es muy BUENO.
¡Toda la información sobre nuestros servicios en el sitio web!
Das Boomerang Casino in Australien ist eine aufregende neue Glücksspieldestination, die sowohl Einheimische als auch Touristen gleichermaßen begeistert. Mit einer beeindruckenden Auswahl an Spielen, großzügigen Boni und einer einladenden Atmosphäre ist das Boomerang Casino definitiv einen Besuch wert.
Eine der auffälligsten Eigenschaften des Boomerang Casinos ist sein einzigartiges Design, das von der australischen Kultur und Landschaft inspiriert ist. Von den symbolträchtigen Boomerangs bis hin zu den ikonischen Kängurus, die über die Bildschirme tanzen, versprüht das Casino ein unvergleichliches australisches Flair.
Doch das Boomerang Casino überzeugt nicht nur mit seinem Design, sondern auch mit seinem großartigen Spielangebot. Von klassischen Tischspielen wie Blackjack und Roulette bis hin zu modernen Spielautomaten und Live-Dealer-Spielen gibt es hier für jeden Geschmack etwas Passendes. Darüber hinaus können Spieler von großzügigen Boni und Sonderaktionen profitieren, die ihre Gewinnchancen noch weiter steigern.
Die Atmosphäre im Boomerang Casino ist einladend und freundlich, was dazu beiträgt, dass sich die Gäste sofort wohl fühlen. Der Kundenservice ist erstklassig und steht den Spielern rund um die Uhr zur Verfügung, um bei Fragen oder Problemen zu helfen.
Alles in allem ist das Boomerang Casino in Australien ein erstklassiges Glücksspielziel, das mit seiner einzigartigen Atmosphäre, seinem vielfältigen Spielangebot und seinen großzügigen Boni überzeugt. Egal, ob man ein erfahrener Spieler oder ein Neuling ist, im Boomerang Casino wird man sich garantiert gut aufgehoben fühlen.
https://boomerangcasino.one/
amoxicillin 30 capsules price price for amoxicillin 875 mg order amoxicillin uk
5 Killer Quora Answers On Veleco Luxury Electric Scooters Veleco luxury electric scooters
10 Things We All Love About Treadmill Treadmills Sale uk
10 Things That Everyone Is Misinformed About The Word “Car Locksmith.” Local car Locksmiths
Five Killer Quora Answers On Replacement Double Glazing
Units Near Me Replacement double glazing units near Me
GSA SER Tools To Make Your Daily Life GSA SER Trick That Every Person Should Know gsa ser software (Judi)
7 Little Changes That Will Make The Difference With Your Double
Glazing Fitters Near Me Double Glazing Panels
How Washing Machines 12kg Was Able To Become The No.1 Trend In Social Media
combined
A Comprehensive Guide To Car Diagnostics Near Me Uk From Beginning To End comprehensive
Silicone Ring Tools To Ease Your Life Everyday Cock Rings Vibrating Cock
What Is Software SEO? To Make Use Of It seo traffic software
What’s The Current Job Market For Replacement Windows Prices Professionals
Like? Replacement Windows Prices
Завод К-ЖБИ предлагает железобетонные изделия и поражает ассортиментом. Большое внимание уделяем качеству выпускаемой продукции и осуществляем оперативную доставку. Ищете вентиляционный коммуникационный блок? Gbisp.ru – сайт, где есть наши контакты и реализованные проекты, посмотрите их уже сейчас. Также тут есть возможность оставить заявку, для этого укажите ваш номер телефона, имя и e-mail, далее нажмите на «Отправить». Для уточнения информации обратитесь к опытному менеджеру.
10 Things Everyone Has To Say About Classic Casino Slots gambling
11 Strategies To Completely Defy Your Accident Attorney florida accident attorneys
The 10 Most Scariest Things About Walking Pads For Under Desk Walking Pads For Under Desk
10 Tell-Tale Signs You Need To Look For A New Upvc Window Repairs upvc Window repairs near me
5 Clarifications On London Online Clothing Shopping
Sites Wonderfold X4 Multipassenger Wagon
10 Facts About Drip Filter Coffee That Make You Feel Instantly The Best
Mood Space-saving coffee maker
amoxicillin for sale: order amoxicillin uk – amoxicillin 500 mg capsule
10 Unexpected Car Door Lock Repair Near Me Tips Door lock Solenoid repair
Double Glazing Near Me: 11 Thing You’re Not Doing Double Glazing Company Near Me
11 Strategies To Refresh Your Upvc Window Repairs Upvc window repairs near me
15 Top Pinterest Boards Of All Time About Injury Lawsuit Injury law firms
8 Tips To Increase Your Fridge Freezer On Sale Game integrated fridge freezer for sale
A Productive Rant About Self Empty Robot Vacuum
self empty robot vacuum mop (minecraftcommand.science)
Ресурс GAMETORRENT.NET позволяет найти все самое необходимое для погружения в увлекательный мир игр. Мы предлагаем большой выбор разных жанров. У нас есть много аркад и головоломок для разминки мозга, также имеются ролевые игры, шутеры и многое другое. Даем гарантию на то, что тут вы найдете то, что вам по душе. На https://gametorrent.net/tegi/na-dvoih/ вас ожидают свежие новинки игровой индустрии. Не сомневайтесь в том, что получите только лучшие игры без вредоносных программ и вирусов. Окунитесь в мир неимоверных возможностей, скачивайте игры уже сейчас!
Zet Casino Recensioni – Alles was Sie wissen mГјssen
Zet Casino ist ein Online-GlГјcksspielanbieter, der Spielern eine Vielzahl von Spielen und Casino-Spielen in einer sicheren und benutzerfreundlichen Umgebung bietet. In diesem Artikel werden wir uns genauer mit den Rezensionen von Zet Casino befassen und Ihnen alle Informationen geben, die Sie Гјber dieses Casino wissen mГјssen.
Das Casino wurde 2018 gegrГјndet und hat seitdem eine treue und stetig wachsende Spielerbasis aufgebaut. Die meisten Spieler loben das Casino fГјr seine groГџe Auswahl an Spielen, darunter Slots, Tischspiele, Live-Casino-Spiele und vieles mehr. Die Software wird von einigen der renommiertesten Anbieter der Branche bereitgestellt, darunter NetEnt, Microgaming, Play’n GO und viele andere.
Die Benutzeroberfläche des Casinos ist einfach und benutzerfreundlich, was es Spielern leicht macht, ihre Lieblingsspiele zu finden und zu spielen. Das Casino ist auch für Mobilgeräte optimiert, sodass Spieler unterwegs spielen können.
Ein weiterer wichtiger Aspekt, der von den Spielern oft gelobt wird, ist der Kundenservice von Zet Casino. Das Team ist rund um die Uhr verfügbar und kann über Live-Chat, E-Mail oder Telefon kontaktiert werden. Die Mitarbeiter sind professionell und freundlich und können bei allen Fragen oder Problemen helfen, die Spieler haben könnten.
Zet Casino bietet auch eine Vielzahl von Zahlungsmethoden an, darunter Kreditkarten, E-Wallets und Banküberweisungen. Die meisten Auszahlungen werden schnell bearbeitet, sodass Spieler ihre Gewinne schnell und einfach abheben können.
Insgesamt hat Zet Casino viele positive Bewertungen von Spielern erhalten, die das Casino für seine großartige Auswahl an Spielen, benutzerfreundliche Oberfläche und exzellenten Kundenservice loben. Wenn Sie auf der Suche nach einem zuverlässigen und unterhaltsamen Online-Casino sind, sollten Sie definitiv Zet Casino eine Chance geben.
https://zetcasino.one/
cialis for daily use reviews
5 Killer Quora Answers On Boat Accident Attorneys Near Me Boat Accident attorneys near me
5 Killer Quora Answers To Standing Desk Treadmill standing desk treadmill
15 Latest Trends And Trends In Injury Attorney monroe Injury lawyer
This Is The Ugly Truth About Under Counter Fridge bosch Integrated fridge
Five Car Accident Lawyer Projects To Use For Any Budget Vimeo
На сайте http://ttps//lovely-professional.ru вы сможете приобрести качественные материалы, которые используются для наращивания ресниц. При этом установлены привлекательные расценки на всю продукцию. Она представлена именитыми брендами, которые отвечают за качество. Товары поставляются через официальных дистрибьюторов. В разделе представлены ресницы, товары для биозавивки, ламинирования, пинцеты. Есть возможность заказать продукцию оптом. Действуют привлекательные расценки. Продукция сертифицированная.
Guide To Maryland Birth Injury Attorneys: The Intermediate Guide For Maryland Birth Injury Attorneys Maryland Birth Injury Attorneys (https://Www.Cheaperseeker.Com)
9 Lessons Your Parents Teach You About Best Online Shopping Sites London best online Shopping sites london
Who Is Responsible For An Upvc Window Repairs Budget?
12 Best Ways To Spend Your Money Upvc Repairs
5 Killer Quora Answers On Bean Cup Coffee Machines bean cup coffee machines
How To Outsmart Your Boss On Counter Strike Global Offensive Best Crosshair case clutch
buy levitra cialis
20 Rising Stars To Watch In The Online Store Uk Cheapest Industry Vimeo.com
Overwhelmed by how to proceed with recovery
of your QIWI wallet funds? Our support team is ready 24/7 to guide you through the steps
and respond to any concerns you have.
Working with our team, you’re opting for a trusted partner
in reclaiming your assets.
LASTTORRENT.RU предлагает быстро скачать понравившуюся игру через торрент. В ожидании вам скучать не придется. У нас имеется удобный рубрикатор. Ненужными баннерами мы страницы не загромождаем, найти искомое у вас есть возможность без каких-либо усилий. Вам необязательно проходить регистрацию для доступа к файлам торрентов. Ищете https://lasttorent.ru/strategy/? Lasttorent.ru – бесплатный сайт, скачивая игры тут, получите исправный продукт, без угрозы заражения своего ПК вирусами. В случае возникших вопросов, смело обращайтесь к нам. Получайте удовольствие от игрового процесса!
Tipico Casino Bonus Treue10
Das Tipico Casino bietet seinen treuen Kunden einen besonderen Bonus an – den Treue10 Bonus. Dieser Bonus belohnt Spieler, die regelmäßig im Casino spielen und dem Anbieter treu bleiben. Doch was genau verbirgt sich hinter diesem Bonus und wie können Spieler davon profitieren?
Der Treue10 Bonus ist ein exklusives Angebot für loyalen Spieler im Tipico Casino. Um diesen Bonus zu erhalten, müssen Spieler zunächst Mitglied im Treueprogramm des Casinos sein. Dies ist jedoch ganz einfach – Spieler können sich einfach anmelden und sofort von den Vorteilen des Treueprogramms profitieren.
Sobald Spieler Mitglied im Treueprogramm sind, können sie sich für den Treue10 Bonus qualifizieren. Dieser Bonus wird den Spielern in Form von zusätzlichem Guthaben oder Freispielen gutgeschrieben. Spieler können dieses Bonusguthaben verwenden, um ihre Lieblingsspiele im Casino zu spielen und so ihre Gewinnchancen zu erhöhen.
Der Treue10 Bonus ist eine tolle Möglichkeit für Spieler, noch mehr aus ihrem Spielerlebnis im Tipico Casino herauszuholen. Durch regelmäßiges Spielen und Treue zum Anbieter können Spieler sich zusätzliches Guthaben sichern und damit ihre Gewinnchancen steigern.
Wenn auch Sie von den exklusiven Vorteilen des Treue10 Bonus profitieren möchten, sollten Sie sich noch heute im Tipico Casino anmelden und Mitglied im Treueprogramm werden. Mit etwas Glück und Geschick können auch Sie sich den begehrten Treue10 Bonus sichern und so noch mehr Spaß beim Spielen im Casino haben.
https://tipicocasino.one/
See What Gotogel Link Alternatif Tricks The Celebs Are Using
gotogel link alternatif
The Sage Advice On Auto Lawyers From A Five-Year-Old Car Crash lawyer
Your trust in us is our number one concern. Therefore, we operate with complete integrity and commitment to your satisfaction.
Rest easy of having your funds back in your possession with our expert help.
What’s The Current Job Market For Locksmith Near Me Car Professionals Like?
locksmith near me car (Lisa)
The Glass Repair London Awards: The Best, Worst And Strangest
Things We’ve Ever Seen replaced
This History Behind Robot Vacuum Cleaner With Mop Will
Haunt You Forever! robot vacuum mop (notabug.org)
5 Arguments Window Repairs Is Actually A Great Thing upvc window Repairs
The 9 Things Your Parents Taught You About Heat Pump Tumble Dryer Reviews heat pump tumble dryer Reviews
Have you lost money on your QIWI wallet?
We know how frustrating that can be.
Don’t despair—our team specializes in getting back your
balance from QIWI wallets.
Boasting years of experience, we’re sure we can help out.
Contact us and let’s start the process of getting your money back.
What’s The Current Job Market For Under Counter Fridge –
Silver Professionals? under Counter fridge – silver
Check Out The Glass Repair Leeds Tricks That The Celebs Are Using window replacement leeds (bookmarking.stream)
FlowForce Max is an innovative, natural and effective way to address your prostate problems, while addressing your energy, libido, and vitality. https://flowforcemax-web.com/
Key Spare 101: It’s The Complete Guide For Beginners Make a spare car key (longisland.com)
Double Glazing Companies Near Me Tools To Streamline Your Everyday
Lifethe Only Double Glazing Companies Near Me Trick That Everyone Should Learn double glazing companies near me
https://zithromaxa.store/# zithromax for sale 500 mg
Ten Beko Washing Machine Best Price Myths That
Aren’t Always True washing machine Beko
9 . What Your Parents Taught You About Buy Mobility Scooters Near Me buy mobility scooter
10 Things Everybody Hates About Car Keys Lost Damaged
stendra vs levitra
See What Nissan Juke Spare Key Tricks The Celebs Are Using nissan juke spare key (chessdatabase.science)
Unexpectedly lost your balance on your QIWI wallet?
We know how stressful that can be.
No need to worry—we specializes in getting back your balance from QIWI wallets.
Having years of experience, we’re confident we can assist you.
Contact us and let’s start the process of restoring your balance.
TestRX™ is a bodybuilding supplement. It’s formulated with high-quality natural ingredients proven to boost natural testosterone and stimulate muscle growth. https://testrx-web.com/
You’ll Never Guess This Best Vibrators For Men’s Secrets
Best vibrators for men (https://notabug.org/)
5 Personal Accident Attorney Lessons From Professionals oklahoma city injury attorney (Temeka)
Everything You Need To Know About Fleshlight Fleshlight masturbators
На сайте https://sobr26.ru ознакомьтесь с номером телефона охранной организации СОБР. Здесь оказываются услуги, связанные с охраной недвижимости, организуется безопасность объекта, есть возможность воспользоваться физической охраной, которая оказывается более 20 лет. Прямо сейчас вы сможете рассчитывать на бесплатную консультацию. Каждый клиент сможет организовать пультовую, физическую охрану, пожарную сигнализацию, видеонаблюдение. Для того чтобы воспользоваться услугами, оставьте заявку непосредственно на сайте.
5 Tools That Everyone In The Good Accident Attorney Industry Should Be
Making Use Of utah accident attorney (Scarlett)
5 Reasons Double Glazed Window Repair Is Actually A Great Thing window repairs
near me; Ferdinand,
What’s The Job Market For Double Dildo Use Professionals?
Double Dildo Use
How To Get More Results From Your Bmw Replacement Key Cost bmw Replacement key cost uk (thisglobe.com)
The Most Negative Advice We’ve Ever Seen About Slot Demo Slot Demo slot Demo x 1000
m.zet Casino ist ein neues und aufregendes Online-Casino, das Spielern die Möglichkeit bietet, ihre Lieblingsspiele von überall aus zu genießen. Mit einer breiten Palette von Spielen, großzügigen Boni und erstklassigem Kundenservice ist m.zet Casino der ultimative Ort für Casino-Enthusiasten.
Das Casino bietet eine Vielzahl von Spielen, darunter Spielautomaten, Tischspiele, Video-Poker und Live-Dealer-Spiele. Egal, ob Sie ein Fan von klassischen Spielautomaten sind oder auf der Suche nach neuen und aufregenden Spielen sind, m.zet Casino hat fГјr jeden etwas zu bieten.
Ein weiterer großer Vorteil von m.zet Casino sind die großzügigen Boni und Promotionen, die regelmäßig angeboten werden. Neue Spieler können von einem Willkommensbonus profitieren, der ihre Einzahlungen erhöht und ihnen mehr Möglichkeiten bietet, zu gewinnen. Darüber hinaus gibt es auch regelmäßige Promotionen, die den Spielern zusätzliche Belohnungen bieten.
Der Kundenservice von m.zet Casino ist erstklassig und steht den Spielern rund um die Uhr zur VerfГјgung. Egal, ob es um technische Probleme, Fragen zu Boni oder einfach nur um Hilfe bei der Navigation auf der Website geht, das Team von m.zet Casino ist immer da, um zu helfen.
Insgesamt ist m.zet Casino eine groГџartige Wahl fГјr alle, die nach einem unterhaltsamen und spannenden Online-Casino-Erlebnis suchen. Mit einer Vielzahl von Spielen, groГџzГјgigen Boni und hervorragendem Kundenservice gibt es keinen Grund, warum Sie nicht heute noch Ihr GlГјck bei m.zet Casino versuchen sollten.
https://zetcasino.one/
How To Make A Profitable CS GO Case Battle When You’re Not Business-Savvy case opening
DuoTrim is an innovative weight loss supplement that utilizes the power of natural plants and nutrients to create CSM bacteria https://duotrim-us.com/
See What Repair Upvc Windows Tricks The Celebs Are Making Use Of repair upvc window
The asbestos producers knew their products could be dangerous but they continued to use Beaverton Asbestos law firm for decades
without disclosing any potential risks. This negligence led to mesothelioma development and
other asbestos-related diseases.
10 Healthy Habits For Spare Key For Car Spare Keys For Cars
BioFit is a Nutritional Supplement That Uses Probiotics To Help You Lose Weight https://biofit-web.com/
Ten Car Lock Repairs That Really Make Your Life Better car lock
repairs (Christiane)
Tipico ist einer der führenden Anbieter von Online-Casinospielen, der es Spielern ermöglicht, mit einem Euro Einsätze zu platzieren. Dieser niedrige Mindesteinsatz ermöglicht es auch unerfahrenen Spielern, sich mit dem Online-Casino vertraut zu machen, ohne größere Risiken eingehen zu müssen.
Das Tipico Casino bietet eine Vielzahl von Spielen an, darunter Slots, Tischspiele und Live-Casino-Spiele, die alle mit einem Euro Einsatz gespielt werden können. Dies ermöglicht es Spielern, Spaß zu haben und gleichzeitig die Chance zu haben, echtes Geld zu gewinnen.
Mit einem Euro Einsatz können Spieler an den verschiedenen Slots spielen, die im Tipico Casino verfügbar sind. Slots sind einfache Spiele, die auf Glück basieren und es Spielern ermöglichen, in kurzer Zeit große Gewinne zu erzielen. Darüber hinaus bietet das Tipico Casino eine Vielzahl von Tischspielen wie Blackjack, Roulette und Baccarat an, die ebenfalls mit einem Euro Einsatz gespielt werden können.
Für Spieler, die das authentische Casino-Erlebnis bevorzugen, bietet das Tipico Casino auch Live-Casino-Spiele an, bei denen echte Dealer die Spiele leiten. Auch diese Spiele können mit einem Euro Einsatz gespielt werden, was es Spielern ermöglicht, das Gefühl eines echten Casinos von ihrem eigenen Zuhause aus zu erleben.
Insgesamt bietet das Tipico Casino mit einem Euro Einsatz eine unterhaltsame und zugängliche Möglichkeit, Casino-Spiele online zu spielen. Egal, ob man ein erfahrener Spieler ist oder gerade erst anfängt, mit einem niedrigen Mindesteinsatz kann jeder die Welt der Online-Casinos erkunden und die Chance haben, echtes Geld zu gewinnen.
https://tipicocasino.one/
Dentitox Pro is a liquid dietary solution created as a serum to support healthy gums and teeth. Dentitox Pro formula is made in the best natural way with unique, powerful botanical ingredients that can support healthy teeth. https://dentitox-us.com/
20 Inspirational Quotes About Folding Mobility Scooters Uk
lightweight foldable Mobility scooter uk
Our knowledge in cyber finance and online transactions means
we’re well-prepared to tackle your QIWI wallet issues.
Rest assured, we employ state-of-the-art techniques and keep up with the newest fraud prevention strategies.
In case of hit with unauthorized transactions or technical glitches
that caused a loss of funds, we’re here to help.
A Trip Back In Time How People Talked About Car Accident
Case 20 Years Ago lawyer car accident near me; Forum.siamnetworker.com,
See What Integrated Fridge Tricks The Celebs Are Utilizing Integrated fridge
15 Gifts For The Lawyer For Car Accidents Lover In Your Life car accident claims lawyers
How Do You Know If You’re In The Right Place For Double Glazing
Repair Near Me upvc door Repairs near me
20 Insightful Quotes About Best Adult Toys For
Men topsadulttoys
What’s The Job Market For Double Glazed Repairs Near
Me Professionals Like? double glazed repairs near me [Dennis]
See What Double Glazing Repair Near Me Tricks The Celebs Are Utilizing double glazing repair Near Me
5 Killer Quora Answers To Mens Masturbators Mens Masturbator,
M.1Party.Co.Kr,
7 Little Changes That’ll Make The Difference With Your Green Power Mobility green mobility Scooter
“Ask Me Anything,” 10 Answers To Your Questions About Sleeper Sofas For Sale Cheap Couches For Sale Near Me
Sugar Balance is an ultra-potent blood sugar supplement that you can use to help control glucose levels, melt away fat and improve your overall health. https://sugarbalance-us.com/
7 Things About Best Online Shopping Websites Uk You’ll Kick Yourself For Not Knowing vimeo.Com
The Reasons Repair Misted Double Glazing Near Me Is The Obsession Of Everyone In 2023 Double Glazed Unit replacement
Buzzwords, De-Buzzed: 10 Other Ways To Say Online Home Shop Uk Discount Code Correll Flower Table
Interested in xrp news? Visit the website Thetradable.com – here you have the opportunity to learn all about the analytics of trading cryptocurrencies, stocks, gold, as well as learn the latest news from the world of finance. Only we have first-hand stock market news, crypto news and financial news. Among other things, you will receive information about market news and analytics, shiba inu news, dogecoin news, xrp news, cardano ada news, toncoin news.
dapoxetine waiter – viagra plus idea cialis with dapoxetine issue
Do You Think Mesothelioma Lawsuits Always Rule The World?
la quinta mesothelioma law firm
A Productive Rant Concerning Slot Demo slot demo pragmatic play lengkap
Guide To Mesothelioma Attorneys Navy Shipyard Worker:
The Intermediate Guide The Steps To Mesothelioma Attorneys Navy
Shipyard Worker mesothelioma attorneys navy shipyard worker (Esther)
Double Glazing Repair Near Me Tips From The Best In The Business double glazing
front door (brackenburyprimary.co.uk)
PureLumin Essence is a meticulously-crafted natural formula designed to help women improve the appearance of age spots. https://pureluminessence-web.com/
purchase neurontin neurontin price comparison neurontin price australia
Responsible For An Online Shopping Sites For Clothes Budget?
12 Ways To Spend Your Money Portable Case For Wonder Workshop
10 Undeniable Reasons People Hate Green Power green mobility Scooter
The Largest Issue That Comes With Windows Repairs Near Me, And How You
Can Solve It double glazed window repairs Near me
15 Astonishing Facts About Best Self Emptying Robot Vacuum
cleaner
11 Creative Ways To Write About Cerebral Palsy Legal lawsuit
Five Killer Quora Answers On Uk Online Shoe
Shopping Websites uk online shoe shopping websites – https://d4bh.ru/ –
10 Amazing Graphics About Online Shopping Uk Women’s Clothing
vimeo.Com
Сайт https://steel-plant.ru/ это производство и продажа кровельно-фасадных материалов: водосточных систем, доборных элементов, а также стальных оцинкованных листов с цветным полимерным покрытием по RAL.
10 Reasons Why People Hate Secondary Double Glazing Near Me Double glazzing
Guide To Bmw Key 1 Series: The Intermediate Guide
The Steps To Bmw Key 1 Series Bmw Key 1 series
Alpha Tonic is a powder-based supplement that uses multiple natural herbs and essential vitamins and minerals to help optimize your body’s natural testosterone levels. https://alphatonic-web.com
Your Family Will Be Grateful For Getting This Replacement Key Bmw local
Vivo Tonic is a remarkable blood sugar support nutritional supplement that offers a wide range of benefits. https://vivotonic-web.com/
You’ll Be Unable To Guess Trusted Online Shopping
Sites For Clothes’s Tricks online shopping sites for clothes
The Most Powerful Sources Of Inspiration Of Auto Accident Claims Automobile accident Lawyer houston
Das zet Casino ist eine beliebte Online-Glücksspielplattform, die eine Vielzahl von Spielen für Spieler aller Erfahrungsstufen anbietet. Einer der neuesten Angebote des Casinos ist die Möglichkeit, 30 Freispiele bei der Registrierung zu erhalten.
Diese 30 Freispiele sind eine großartige Möglichkeit für neue Spieler, das Casino kennenzulernen und einige der beliebtesten Spiele auszuprobieren, ohne dabei eigenes Geld einzahlen zu müssen. Diese Freispiele können bei bestimmten Slots verwendet werden und ermöglichen es den Spielern, echte Gewinne zu erzielen, ohne Risiko einzugehen.
Um die 30 Freispiele zu erhalten, müssen sich Spieler lediglich beim zet Casino registrieren und ein Konto eröffnen. Nach der Registrierung werden die Freispiele automatisch dem Konto gutgeschrieben und können sofort verwendet werden.
Es ist jedoch wichtig zu beachten, dass die Gewinne aus den Freispielen oft bestimmten Umsatzanforderungen unterliegen, bevor sie ausgezahlt werden können. Spieler sollten daher die Bedingungen und Konditionen sorgfältig lesen, bevor sie die Freispiele in Anspruch nehmen.
Insgesamt sind die 30 Freispiele, die das zet Casino anbietet, eine großartige Möglichkeit für Spieler, das Casino zu entdecken und gleichzeitig die Chance zu haben, echte Gewinne zu erzielen. Wenn Sie also auf der Suche nach einem neuen und aufregenden Online-Casino-Erlebnis sind, sollten Sie diese Angebote nicht verpassen. Viel Glück und viel Spaß beim Spielen!
https://zetcasino.one/
The Myths And Facts Behind 2nd Hand Mobility Scooters For Sale
Foldable mobility scooters for sale
A Guide To Window Glass Repair Near Me In 2023 contractor
The Top Pragmatic Play Gurus Do 3 Things goblok
Why Work From Home Jobs Part Time Is So Helpful During COVID-19 work
from home jobs Part time (https://minecraftcommand.science/profile/soapbrain4)
How Michael Kors Handbags Pink Changed My Life For The Better Michael Kors Bag Uk Sale
The Little-Known Benefits Of UK Pornstar top uk pornstars
Ford Key Replacement Tips From The Top In The Business key
fob ford – maps.google.Com.ar,
The Most Popular Auto Accident Attorney For Hire That Gurus Use Three Things Car Collision Attorney
Tipico Live Casino lädt nicht
Haben Sie schon einmal versucht, im Tipico Live Casino zu spielen, aber die Seite lädt einfach nicht? Das kann frustrierend sein, besonders wenn Sie sich auf ein spannendes Spiel gefreut haben. Es gibt mehrere Gründe, warum das Live Casino von Tipico nicht lädt und hier sind einige mögliche Lösungen:
1. Überprüfen Sie Ihre Internetverbindung: Stellen Sie sicher, dass Sie eine stabile und schnelle Internetverbindung haben. Wenn Ihre Verbindung langsam oder instabil ist, kann dies dazu führen, dass das Live Casino nicht richtig lädt.
2. Löschen Sie Ihren Browser-Cache und Cookies: Manchmal können gespeicherte Daten im Browser dazu führen, dass Seiten nicht richtig geladen werden. Löschen Sie Ihren Browser-Cache und Cookies und versuchen Sie es erneut.
3. Aktualisieren Sie Ihren Browser: Manchmal kann es sein, dass veraltete Browser-Versionen nicht mit dem Live Casino von Tipico kompatibel sind. Stellen Sie sicher, dass Ihr Browser auf dem neuesten Stand ist und alle Updates installiert sind.
4. Kontaktieren Sie den Kundenservice: Wenn trotz dieser Maßnahmen das Live Casino von Tipico immer noch nicht lädt, kontaktieren Sie den Kundenservice. Die Mitarbeiter können Ihnen möglicherweise weiterhelfen und das Problem lösen.
Insgesamt kann es verschiedene Gründe geben, warum das Tipico Live Casino nicht lädt. Es ist wichtig, geduldig zu bleiben und die oben genannten Schritte zu befolgen, um das Problem zu beheben. Mit etwas Glück können Sie bald wieder Ihre Lieblingsspiele im Live Casino von Tipico genießen.
https://tipicocasino.one/
The Most Significant Issue With Semi Truck Lawsuit, And How You Can Solve It Vimeo
You’ll Never Guess This Comfy Couches For Sale’s Secrets Comfy Couches For sale
Five Lessons You Can Learn From Locksmith Near Me Car locksmith near me Car key replacement
7 Little Changes That’ll Make A Big Difference In Your
Car Central Lock Repair Near Me replacement Car Door locks
What Is The Secret Life Of Slot Demo Gratis Pragmatic
Play No Deposit Slot Demo Santa Great
5 Killer Quora Answers On Cheap Online Electronics Shopping Uk cheap online electronics shopping Uk
doxycycline 100mg online: doxycycline prices – doxycycline mono
Why You Should Be Working With This Railroad Injuries Lawyers
vimeo
What Car Boot Lock Repair Experts Want You To Learn car Key lock repair near me
The 10 Scariest Things About Emergency Window Repair Window Repair
5 Killer Quora Answers To L Shaped Couches For Sale Couches for sale
10-Pinterest Accounts You Should Follow About CSGO Case Battle Sites Opening Website
An Tommy Hilfiger Bags Ladies Success Story
You’ll Never Be Able To tommy Hilfiger bags sale Usa
The 10 Scariest Things About Locksmith Cars Near Me locksmith cars near Me
You’ll Never Guess This Online Shopping Uk Amazon’s Tricks online shopping uk Amazon
How Car Key Replacement Altered My Life For The Better car key fobs replacement
13 Things About Railroad Injuries Claim You May Never
Have Known Railroad Lawsuit lawyer
5 Killer Quora Answers To 10kg Washing Machine Price 10kg washing machine price – http://www.google.com,
You’ll Never Be Able To Figure Out This Walking Pad Under Desk’s Tricks walking pad Under desk
The 12 Worst Types Of Accounts You Follow On Twitter Auto keys locksmith
17 Signs To Know If You Work With Avon Rep Login Mk avon Rep Login mk
The Three Greatest Moments In 18-Wheeler Accident Attorney
Near Me History Cottage Grove 18 Wheeler Accident Attorney
What Will Gray Sectional Sofa Be Like In 100 Years? L-Shaped Couches
The Biggest Sources Of Inspiration Of Window Repair Near Upvc Repairs (http://Www.Healthndream.Com/Gnuboard5/Bbs/Board.Php?Bo_Table=Qna_Heartsine&Wr_Id=1724792)
Progenifix is designed to help maximize weight loss results using a mixture of natural, science-backed ingredients. The formula also has secondary benefits, including promoting overall wellness and vitality and assisting your immune system. https://progenifix-web.com/
25 Amazing Facts About Repair A Window Window repair
Are You Responsible For The Erb’s Palsy Compensation Budget?
12 Best Ways To Spend Your Money Ocala Erb’s Palsy Lawyer
Railroad Injuries Litigation: 10 Things I’d Love To Have Known Sooner Railroad shoulder injury
settlements (articlement.com)
Интернет магазин DinAvto.ru – это верное решение владельца авто. Мы все знаем о предоставляемых нами товарах. У нас вы купите то, что подойдет вашему автомобилю. Предлагаем большой выбор автозапчастей, цены у нас привлекательные. Ищете масло моторное купить недорого? Dinavto.ru – сайт, оплачиваете заказ здесь, а оплата за доставку производится вами при получении. Основная наша цель – это удовлетворить ваши требования. Доставляем товары по Москве и Московской области, а также по всей РФ. Обращайтесь к нам прямо сейчас, готовы вас профессионально проконсультировать.
Think You’re Cut Out For Doing Injury Legal? Take This Quiz injury lawsuit [https://telemail.jp/]
For Whom Is Upvc Windows Leeds And Why You Should
Take A Look upvc window hinge repair leeds
FoliPrime is a simple serum containing a blend of vitamins designed to boost hair health. FoliPrime has 100 percent natural substances that enhance and supplement the vitamins in the scalp to promote hair growth. https://foliprime-web.com/
Where Can You Find The Best Winning Slots Information? Real Money Slots
(Eng.Worthword.Com)
What’s The Current Job Market For Mesothelioma Legal Professionals Like?
mesothelioma Legal
20 Things That Only The Most Devoted Repair Double Glazed Window Fans Know window doctor near me
Das Casino-Gewinn auf das Tipico-Konto einzahlen
Immer mehr Menschen entdecken die Spannung und den Spaß, den Online-Casinos bieten. Eine der beliebtesten Plattformen in Deutschland ist Tipico, die nicht nur Sportwetten, sondern auch ein umfangreiches Online-Casino anbietet. Doch wie funktioniert es eigentlich, wenn man einen Gewinn aus dem Casino auf sein Tipico-Konto einzahlen möchte?
Zunächst einmal ist es wichtig zu wissen, dass es verschiedene Möglichkeiten gibt, um Geld auf das Tipico-Konto zu überweisen. Dazu zählen unter anderem Kreditkarten, Banküberweisungen, e-Wallets wie PayPal oder Skrill und auch die beliebte Paysafecard. Wenn man einen Gewinn aus dem Casino auf sein Tipico-Konto einzahlen möchte, kann man einfach die gewünschte Zahlungsmethode auswählen und den Betrag angeben.
Es ist wichtig zu beachten, dass manche Zahlungsmethoden Gebühren oder Mindestbeträge haben können, daher sollte man sich vorher genau informieren. In der Regel erfolgt die Gutschrift des eingezahlten Betrags auf das Tipico-Konto innerhalb weniger Minuten bis Stunden, je nach Zahlungsmethode.
Es ist auch möglich, dass man einen Bonus erhalten kann, wenn man einen Gewinn aus dem Casino auf sein Tipico-Konto einzahlt. Oft bieten Online-Casinos attraktive Boni an, um Spieler zu belohnen und zu motivieren. Diese Bonusangebote können sich je nach Casino und Aktion unterscheiden, daher lohnt es sich, regelmäßig auf der Tipico-Website nach aktuellen Angeboten zu schauen.
Insgesamt ist es also ganz einfach, einen Gewinn aus dem Casino auf das Tipico-Konto einzuzahlen. Mit den verschiedenen Zahlungsmethoden und Bonusangeboten bietet Tipico seinen Kunden eine bequeme und sichere Möglichkeit, um am Spiel teilzunehmen und Gewinne zu erzielen. Wer also sein Glück im Casino versuchen möchte, ist bei Tipico genau richtig.
https://tipicocasino.one/
https://prednisoned.online/# prednisone 5 mg tablet cost
10 Things That Your Family Teach You About 10kg Washing Machine Uk
10Kg Washing Machine Uk
The Reasons You’re Not Successing At How Many Cases Are There In CSGO cs2 case – Raquel –
Ten Self Emptying Robot Vacuum Mops That Really Change Your Life Vacuum mops
Responsible For The Auto Locksmith Near Me Prices Budget? 10 Unfortunate
Ways To Spend Your Money lockout
Why Is Cerebral Palsy Lawyers So Famous? la joya cerebral Palsy law firm (vimeo.com)
11 Ways To Fully Redesign Your Auto Accident Legal Lynchburg Auto Accident Attorney (Vimeo.Com)
Gut Vita™ is a daily supplement that helps consumers to improve the balance in their gut microbiome, which supports the health of their immune system. It supports healthy digestion, even for consumers who have maintained an unhealthy diet for a long time. https://gutvita-us.com/
Three Greatest Moments In Fleshlight Best History Best fleshlight cheap
If You’ve Just Purchased Best Accident Attorneys …
Now What? today
Could Window Repair Be The Key To Achieving 2023? upvc windows repairs near me (https://wikidot.win/wiki/How_to_outsmart_your_Boss_upvc_patio_doors)
What Will Mesothelioma Attorney Be Like In 100 Years?
lancaster mesothelioma lawyer
20 Fun Infographics About Mesothelioma Mesothelioma Claims
На сайте https://ocims.ru/ закажите звонок для того, чтобы вам рассчитали стоимость каркасных домов в Орле. Они создаются по индивидуальному эскизу либо готовому проекту. На возведение уходит не более пары месяцев, а на сооружения дается гарантия 5 лет. В договоре прописывается стоимость, которая потом не изменяется. «ОЦИМС» гарантирует строительство комфортного, уютного дома, в котором вам точно понравится проживать. Каждый клиент сможет рассчитывать на приятный презент. Компания также занимается возведением домов в ипотеку от 5%.
You’ll Never Guess This Window Doctor Near Me’s Tricks
Window Doctor Near Me
This Week’s Top Stories Concerning Car Accident Lawyer Car accidents
Neuro-Thrive is a brain health supplement that claims to promote good memory and thinking skills and better quality sleep. This nootropic supplement achieves its cause with its potent blend of natural compounds and extracts that are proven to be effective in sharpening mental acuity. https://neurothrive-web.com/
The 10 Most Terrifying Things About Double Glazing Repairs Near Me Double Glazing
Fast Lean Pro is a herbal supplement that tricks your brain into imagining that you’re fasting and helps you maintain a healthy weight no matter when or what you eat. It offers a novel approach to reducing fat accumulation and promoting long-term weight management. https://fastleanpro-web.com/
Unexpectedly lost your balance on your QIWI wallet?
We get it how frustrating that can be.
Fear not—we specializes in recovering lost funds from QIWI wallets.
Having expert knowledge, we’re confident we can provide assistance.
Get in touch and let’s start the process of recovering your
funds.
The ProNail Complex is a meticulously-crafted natural formula which combines extremely potent oils and skin-supporting vitamins. https://pronailcomplex-web.com/https://pronailcomplex-web.com/
Five Things Everyone Makes Up About Marc Jacobs Handbag Black Marc Jacobs Bags
Why Is Locksmith Near Me Car So Popular? vehicle
Das Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und Aktionen fГјr seine Spieler anbietet. Eine der beliebtesten Aktionen sind die sogenannten ilmaiskierrokset, also Freispiele, die von Zeit zu Zeit an die Spieler vergeben werden.
Diese ilmaiskierrokset sind eine großartige Möglichkeit, um neue Spiele auszuprobieren und dabei die Chance auf Gewinne zu haben, ohne dabei eigenes Geld einzusetzen. Spieler können mit diesen Freispielen verschiedene Spielautomaten testen und ihre Favoriten finden, ohne dabei ein finanzielles Risiko einzugehen.
Im Zet Casino können Spieler regelmäßig ilmaiskierrokset erhalten, entweder als Teil eines Willkommensangebots für neue Spieler oder als Belohnung für treue Spieler. Die Freispiele können an bestimmte Slots gebunden sein oder für alle verfügbaren Spiele im Casino gelten.
Um an den ilmaiskierrokset im Zet Casino teilzunehmen, müssen Spieler lediglich die entsprechenden Bedingungen erfüllen, die in den Bonusbedingungen des Casinos aufgeführt sind. Dazu gehört oft eine Mindesteinzahlung oder der Einsatz eines bestimmten Betrags an Echtgeld innerhalb eines bestimmten Zeitraums.
Insgesamt bieten die ilmaiskierrokset im Zet Casino eine tolle Möglichkeit, um Spaß zu haben und gleichzeitig die Chance auf Gewinne zu haben, ohne dabei eigenes Geld einsetzen zu müssen. Spieler sollten regelmäßig die Aktionen des Casinos im Auge behalten, um keine der lukrativen Freispielangebote zu verpassen.
https://zetcasino.one/
neurontin cost generic generic neurontin cost neurontin 600 mg tablet
A Guide To Window Repair Leeds From Start To Finish Service
How Do You Know If You’re In The Right Place To Go After Audi Key Lost Audi key
Erectin is a clinically-proven dietary supplement designed to enhance male https://erectin-web.com/
Think You’re Cut Out For Fiat Key? Do This Test fiat 500 key fob reset
10 Facts About CSGO Cases Ranked That Make You Feel Instantly A Good Mood Horizon Case
Why Personal Injury Lawyer Is Right For You? St Louis Personal Injury Lawsuit
15 Startling Facts About How To Ship To Ireland From Uk That You Didn’t Know
Anthracite Car Seat Base; Kristie,
100% Natural Formula Expressly Designed to Help Control Blood Sugar Levels, Improve Insulin Response And Support Overall Health https://glucotrusttry.com/
Why You Should Focus On Improving Semi Truck Litigation semi truck accident lawyers; Jung,
how to buy doxycycline online: doxy 200 – buy doxycycline
9 Lessons Your Parents Teach You About Replacement Double
Glazed Windows Replacement Double glazed window
Futon For Sale Near Me Techniques To Simplify Your Daily Life
Futon For Sale Near Me Trick That Every Person Must Know futon for sale Near me
The Most Popular Amazon Uk Online Shopping Clothes
Gurus Are Doing 3 Things Duraboard Compatible Peg
Hooks (Glenda)
A Productive Rant About CSGO Weapon Case esports 2013 winter case – Marlon,
5 Clarifications On Ford Car Keys ford replacement Key
A mesothelioma lawyer with experience will help you decide on the best type of lawsuit to suit your
case. The process starts with the filing of a complaint.
Defendants have a limited period of time to respond.
Here is my homepage :: dickinson asbestos Attorney
The Ultimate Glossary On Terms About Leeds Door Panels
fitter
14 Common Misconceptions About Case CSGO Sites case operation bravo (Hassie)
20 Things Only The Most Devoted Window Repair Near Fans Know window repair near me
15 Pinterest Boards That Are The Best Of All Time About Panty Vibrators
http://www.topsadulttoys.Uk
The Best Glazing Repairs Near Me Gurus Are Doing 3 Things
double Glazing repairs near me
PowerBite stands as an innovative dental candy, dedicated to nurturing healthy teeth and gums. Infused with a potent formula, it champions the cause of a robust and radiant smile. Crafted meticulously https://powerbite-web.com/
15 Reasons You Shouldn’t Ignore Are CSGO Cases Predetermined Case Shadow
Protoflow is a prostate health supplement featuring a blend of plant extracts, vitamins, minerals, fruit extracts, and more. https://protoflow-web.com/
11 “Faux Pas” That Are Actually Okay To Do With Your Leeds Door Panels door repair leeds
(Lidia)
Tipico Casino ist eine beliebte Online-Glücksspielplattform, die eine Vielzahl von Spielen und Möglichkeiten bietet, Geld zu gewinnen. Viele Spieler fragen sich jedoch, wie sie ihr Guthaben auszahlen können. In diesem Artikel werden wir Ihnen erklären, wie Sie Ihr Guthaben bei Tipico Casino auszahlen lassen können.
Zunächst einmal müssen Sie sich auf der Website von Tipico Casino anmelden und Ihr Konto verifizieren. Dies ist ein wichtiger Schritt, um sicherzustellen, dass Ihr Geld sicher ist und dass Sie berechtigt sind, Auszahlungen vorzunehmen.
Sobald Ihr Konto verifiziert ist, kГ¶nnen Sie auf den Bereich “Mein Konto” zugreifen und dort die Option “Auszahlung” wГ¤hlen. Hier haben Sie die MГ¶glichkeit, die gewГјnschte Auszahlungsmethode auszuwГ¤hlen. Tipico Casino bietet verschiedene MГ¶glichkeiten wie BankГјberweisung, Kreditkarte oder E-Wallets wie PayPal oder Skrill an.
Nachdem Sie die Auszahlungsmethode gewählt haben, müssen Sie den Betrag eingeben, den Sie auszahlen lassen möchten. Beachten Sie dabei, dass es möglicherweise Mindest- oder Höchstauszahlungsbeträge gibt, die Sie beachten müssen.
Sobald Sie die Auszahlung bestätigt haben, wird Ihr Geld innerhalb von 1-3 Werktagen auf Ihrem Konto gutgeschrieben, je nach gewählter Auszahlungsmethode.
Es ist wichtig zu beachten, dass Tipico Casino möglicherweise Gebühren für Auszahlungen erhebt, je nach gewählter Methode. Sie sollten sich daher immer im Voraus über mögliche Gebühren informieren.
Insgesamt ist es bei Tipico Casino relativ einfach, Guthaben auszahlen zu lassen. Indem Sie die oben genannten Schritte befolgen und Ihr Konto verifizieren, können Sie sicherstellen, dass Ihre Auszahlung schnell und reibungslos abgewickelt wird. Viel Glück beim Spielen!
https://tipicocasino.one/
3 Reasons Commonly Cited For Why Your Marc Jacobs Camera Bag
Isn’t Working (And Solutions To Resolve It) marc jacobs bag – tk maxx
15 Things Your Boss Wishes You’d Known About Online Shopping Stores List Baby Deedee Sleep Bag Sale
Why You’ll Want To Find Out More About Window Repair Near window repair Near me
10 Things We Hate About Fiat Punto Key Replacement how to unlock fiat 500 without key (Stephanie)
5 Killer Quora Answers On Shopping Online Sites List shopping online sites list
15 Amazing Facts About Replacement Double Glazed Glass Only Near
Me That You Never Knew Double glazing misting
Сантехника в Москве от https://sanbest.ru это возможность купить по привлекательным ценам сантехнику в Москве, душевые кабины в Москве. Купить раковину Москва также не составит труда. Большой ассортимент, доставка, различные акции и распродажи помогут выгодно приобрести сантехнику. Подробнее на сайте.
17 Reasons Not To Not Ignore CSGO Cases Value falchion case; Janis,
Boostaro is a dietary supplement designed specifically for men who suffer from health issues. https://boostaro-try.com/
The Most Hilarious Complaints We’ve Been Hearing About Planet
Spa Avon Avon Planet Spa Sleep Spray; https://Gurye.Multiiq.Com/Bbs/Board.Php?Bo_Table=Free&Wr_Id=1061096,
Missing funds on your QIWI wallet?
We understand how stressful that can be.
No need to worry—our team specializes in getting back your
balance from QIWI wallets.
Having a high success rate, we’re positive we can help out.
Drop us a message and let’s start the process of getting
your money back.
http://amoxila.pro/# amoxicillin 500 mg price
10 Tips For Robot Vacuums That Are Unexpected robot vacuum with docking station (Dane)
5 Killer Quora Answers To Gotogel Link Alternatif GoTogel
Zoracel is an extraordinary oral care product designed to promote healthy teeth and gums, provide long-lasting fresh breath, support immune health, and care for the ear, nose, and throat. https://zoracel-web.com
Компания «Мсмтепло» длительное время производит и реализует теплообменное оборудование в Москве и по привлекательной стоимости, различной сложности. Перед вами огромный выбор продукции, созданной для различных целей: строительных компаний, промышленности, бассейнов, а также ЖКХ, котельных автономного типа. На сайте https://msmteplo.ru/ ознакомьтесь с расценками и другой полезной информацией.
Cerebrozen is an excellent liquid ear health supplement purported to relieve tinnitus and improve mental sharpness, among other benefits. The Cerebrozen supplement is made from a combination of natural ingredients, and customers say they have seen results in their hearing, focus, and memory after taking one or two droppers of the liquid solution daily for a week. https://cerebrozen-try.com/
The 10 Scariest Things About Walking Pads For Under Desk walking Pads for Under desk
Your Family Will Be Grateful For Getting This Mesothelioma Claim battle creek Mesothelioma lawsuit
15 Surprising Stats About Shopping Online Sites List Water Filter For International Travel
5 Common Phrases About CSGO Most Profitable Cases You
Should Avoid operation riptide case
The 10 Most Terrifying Things About Accident Lawsuit accident
15 Inspiring Facts About Michael Kors Ladies Handbags That You Didn’t Know About Kors michael handbag
You’ll Never Guess This Window Replacement Near Me’s Benefits Window Replacement Near Me
Five Reasons To Join An Online Online Shop Designer Suits Shop And 5 Reasons Why You Shouldn’t Heavy Duty Crimping Tool
Why Windows And Doors Leeds Is Everywhere This Year
glaziers
See What Robot Vacuums Self Emptying Tricks The Celebs Are Utilizing robot vacuums self emptying – http://www.diggerslist.com –
Situs Gotogel Terpercaya Tools To Help You Manage Your Daily
Lifethe One Situs Gotogel Terpercaya Technique Every Person Needs To Be Able To situs gotogel terpercaya
10 Quick Tips About Online Shopping Clothes Uk Cheap Vimeo
9 Things Your Parents Taught You About Replacement Car
Key Costs replacement car key cost (Estela)
Das Zet Casino ist nicht nur für seine vielfältige Auswahl an Spielautomaten und Tischspielen bekannt, sondern bietet auch eine breite Palette an Sportwetten an. Sportfans und Wettbegeisterte können sich hier auf spannende Wettkämpfe und attraktive Quoten freuen.
Egal ob FuГџball, Tennis, Basketball, Eishockey oder andere beliebte Sportarten – im Zet Casino findet jeder das passende Angebot fГјr seine Wetten. Die Plattform bietet eine benutzerfreundliche OberflГ¤che, auf der man schnell und einfach seine Wetten platzieren kann. Zudem gibt es regelmäßig Aktionen und Boni, die das Wetterlebnis noch aufregender machen.
Das Zet Casino legt großen Wert auf Sicherheit und Fairness, daher können sich die Spieler darauf verlassen, dass ihre persönlichen Daten geschützt sind und die Spiele fair ablaufen. Zudem steht ein kompetenter Kundenservice zur Verfügung, der bei Fragen und Problemen gerne weiterhilft.
Wer also auf der Suche nach einem zuverlässigen und unterhaltsamen Anbieter für Sportwetten ist, der sollte sich das Zet Casino genauer anschauen. Mit einer großen Auswahl an Sportarten, attraktiven Quoten und einem ausgezeichneten Kundenservice ist das Zet Casino eine gute Wahl für alle, die gerne auf Sportereignisse wetten möchten.
https://zetcasino.one/
Das Tipico Casino ist eine beliebte Online-Glücksspielplattform, die eine Vielzahl von Spielen für Spieler bietet. Die Website ist benutzerfreundlich gestaltet und ermöglicht es den Nutzern, leicht auf ihre Lieblingsspiele zuzugreifen.
Das Tipico Casino bietet eine breite Palette von Spielen, darunter Slots, Tischspiele, Live-Casino-Spiele und vieles mehr. Die Plattform arbeitet mit renommierten Softwareanbietern zusammen, um hochwertige Spiele anzubieten, die eine realistische Casino-Erfahrung bieten.
Ein weiterer Pluspunkt des Tipico Casinos ist der Kundenservice, der rund um die Uhr verfügbar ist, um den Spielern bei Fragen oder Problemen zu helfen. Die Website verfügt auch über sichere Zahlungsmethoden, um sicherzustellen, dass die Spieler ihre Gewinne schnell und sicher erhalten können.
Darüber hinaus bietet das Tipico Casino regelmäßig spannende Aktionen und Boni für seine Spieler an. Dies kann von Einzahlungsboni bis hin zu Freispielen reichen, die den Spielern helfen können, ihre Gewinne zu steigern.
Insgesamt ist das Tipico Casino eine erstklassige GlГјcksspielplattform, die eine breite Palette von Spielen, erstklassigem Kundenservice und groГџzГјgigen Promotionen bietet. Spieler sollten die Website besuchen, um ein erstklassiges Online-Casino-Erlebnis zu genieГџen.
https://tipicocasino.one/
15 Inspiring Facts About Semi Truck You’ve Never Seen Daphne semi truck accident lawsuit
На сайте https://nnprom.ru/ вы сможете приобрести сварной решетчатый настил, прессованный решетчатый настил, а также ступени из настила, крепления для решетчатого настила, перфорированный лист. Компания занимается непосредственно производством конструкций. Для этого имеются все мощности, инновационное и высокотехнологичное оборудование. Производится более 100 тонн конструкций в месяц. При необходимости менеджеры разработают схемы на основании чертежей. Продукция отличается высоким качеством, создана в соответствии с ГОСТом, нормативами.
The Next Big Event In The Dangerous Drugs Lawsuit Industry broadview dangerous drugs lawsuit
(Vimeo.com)
See What Window Repair Leeds Tricks The Celebs Are Using Window repair leeds [http://www.google.ci]
Motorcycle Accident Lawyers Tools To Streamline Your Daily
Life Motorcycle Accident Lawyers Trick Every Person Should
Be Able To motorcycle accident (https://www.Welcomeargentina.com/)
Five Killer Quora Answers On Charity Shop Online Clothes Uk charity shop online clothes uk (Lewis)
Guide To 9kg Washing Machine Deals: The Intermediate Guide Towards 9kg Washing Machine Deals 9Kg washing Machine Deals
Unexpected Business Strategies That Aided Double Glazing Repairs Cost Succeed window replacement [Stefan]
How Robot Vacuum Cleaner With Mop Became The Hottest Trend In 2023
best robot Vacuum Mop
5 Reasons To Be An Online Car Key Battery Replacement Buyer And 5 Reasons Why You Shouldn’t online
A Provocative Rant About Black Fridge Freezer Which Best Buy Fridge Freezers – https://Opensourcebridge.Science/Wiki/A_Look_In_Cheap_Fridge_Freezerss_Secrets_Of_Cheap_Fridge_Freezers –
Guide To Best Robot Vacuum For Carpet: The Intermediate
Guide For Best Robot Vacuum For Carpet best Robot vacuum for carpet
10 Things You’ve Learned In Kindergarden Which Will Help You With Online Retailers Uk Stats Small Space Dining Table (Jed)
The 10 Most Terrifying Things About Erb’s Palsy Law Erb’s Palsy
На сайте https://kreditbaza.ru/ ознакомьтесь со всеми предложениями по кредитам, займам, которые выдают в России. Перед вами самые лучшие предложения, которыми вы сможете воспользоваться прямо сейчас. Возьмите средства без процентов до 100 000 рублей. Все предприятия, которые находятся на сайте, есть в госреестре МФО. Каждый желающий сможет получить до 30 млн. рублей. Оформите кредитную карту по привлекательной ставке – 9%. Также есть дебетовые карты с кэшбэком до 30%. РКО предоставляется бесплатно.
amoxicillin 500mg pill amoxicillin 500 mg brand name amoxicillin for sale
Content Marketing Consultant Techniques To Simplify Your Daily Lifethe
One Content Marketing Consultant Trick That
Should Be Used By Everyone Be Able To Content Marketing Consultant, 67.Glawandius.Com,
An Medical Malpractice Attorneys Success Story You’ll
Never Believe spotswood Medical malpractice lawyer
Relomania предлагает качественные услуги. Компания специализируется на облегчении сложного трудового процесса в Испании для получения ВНЖ. Мы гарантируем отсутствие скрытых комиссий, цены наши прозрачны. Справимся с любой задачей, стремимся к совершенству. Ищете золотая виза испания? Relomania.com – сайт, где можно в удобное время оставить заявку на профессиональную консультацию. В ближайшее время свяжемся с вами. Уделим время на понятие вашей ситуации. Воплотите ваши стремления в реальность. Обращайтесь к нам, и мы сделаем ваш переезд в Испанию комфортным!
10 Apps To Help You Manage Your Online Sites For
Shopping In Uk Garden Sun Canopy
Searching For Inspiration? Look Up Injury Case Tuscaloosa Injury attorney
The Main Issue With Online Shopping Sites
Uk, And How You Can Fix It Navy Queen Down Alternative Comforter
5 Killer Quora Answers To Repair Misted Double Glazing Near Me Double Glazing Near me
sildenafil prescription online
14 Savvy Ways To Spend Leftover Semi Truck Legal Budget Vimeo
Ten Upvc Window Repairs That Really Make Your Life Better upvc window repairs (https://inazawa-b-gaiku.hatenablog.com/)
The 10 Most Scariest Things About Autowatch Ghost Installers Midlands autowatch ghost installers midlands (Constance)
amoxicillin 500 mg tablet price: order amoxicillin online no prescription – amoxicillin 200 mg tablet
How To Make A Successful Window Repairs Tutorials From Home Upvc window repairs
Störung im Casino: Was tun, wenn das Glücksspiel plötzlich unterbrochen wird?
Ein Abend im Casino kann für viele Menschen ein spannendes und aufregendes Erlebnis sein. Doch was passiert, wenn plötzlich eine Störung im Casino auftritt und das Glücksspiel unterbrochen wird? In solchen Fällen ist es wichtig, gelassen zu bleiben und zu wissen, wie man am besten vorgeht.
Zunächst gilt es, ruhig zu bleiben und nicht in Panik zu geraten. Oft handelt es sich bei einer Störung im Casino um technische Probleme, die schnell behoben werden können. In solchen Fällen ist es am besten, sich an das Personal vor Ort zu wenden und um Hilfe zu bitten. Die Mitarbeiter im Casino sind in der Regel geschult, um solche Situationen zu bewältigen und können schnell Abhilfe schaffen.
Wenn die Störung jedoch länger dauert oder das Glücksspiel nicht wie gewohnt fortgesetzt werden kann, ist es ratsam, sich mit dem Kundenservice des Casinos in Verbindung zu setzen. Oftmals können sie Auskunft darüber geben, was die Ursache der Störung ist und wie lange sie voraussichtlich dauern wird. In einigen Fällen ist es sogar möglich, eine Entschädigung für die entgangene Spielzeit zu erhalten.
Es ist wichtig, sich darüber im Klaren zu sein, dass Störungen im Casino trotz aller Vorsichtsmaßnahmen immer wieder auftreten können. Daher ist es ratsam, sich vorab über die Sicherheitsvorkehrungen und den Kundenservice des jeweiligen Casinos zu informieren, um im Falle einer Störung schnell und effektiv handeln zu können.
Insgesamt ist es wichtig, auch in solchen unvorhergesehenen Situationen Ruhe zu bewahren und besonnen zu handeln. Mit der richtigen Herangehensweise können Störungen im Casino schnell und unkompliziert behoben werden, sodass dem Glücksspielspaß nichts im Wege steht.
https://zetcasino.one/
Ищете новые анонсы серверов lineage 2? LA2-ANONS.COM – то, что вам нужно. Дадим вам грамотный совет в подборе надежного игрового сервера. На нашем портале анонсы серверов Lineage 2 регулярно актуализируются, это позволяет любому геймеру быть первым зарегистрированным. Интересует lineage 2? La2-anons.com – сайт, мы ежедневно над его функционалом трудимся. При выборе сервера для игры Lineage 2, советуем свое внимание обратить на платформы, где написано VIP. Предоставляем исключительно актуальную информацию, с ней можете ознакомиться уже сейчас.
7 Easy Secrets To Totally Intoxicating Your Veterans Disability Legal Azusa Veterans Disability Law Firm
Are You Responsible For The Prada Handbag Nylon Budget?
10 Ways To Waste Your Money Prada Bags small
Five Killer Quora Answers To Treadmills Sale Treadmills sale
You’ll Never Guess This Window Repair Near Me’s Benefits window repair near me
See What Eufy Robot Vacuum Tricks The Celebs Are Using robot Vacuum
The 9 Things Your Parents Taught You About Seat Mii Replacement Key
seat mii replacement key
See What Affordable SEO Uk Tricks The Celebs Are Utilizing
Affordable Seo Uk
10 Places That You Can Find Treadmill Sale UK treadmills For home
Seven Explanations On Why Double Glazed Units Near Me Is Important Double Glazing Door Handles
Nine Things That Your Parent Taught You About Online Shopping Sites Clothes Cheap Online Shopping Sites Clothes Cheap
The Most Significant Issue With Window Glass Replacement Near Me, And How You Can Repair It repair
20 Accident Settlement Websites That Are Taking The Internet By Storm Vimeo.com
How Window Repair Near Was The Most Talked About Trend Of 2023 Upvc Repairs
The Reasons You’re Not Successing At Personal Injury Legal vimeo
See What Examples Of Online Products Tricks The Celebs Are Utilizing Examples of online products
The Reasons Uk Online Shopping Sites For Mobile Will Be Everyone’s Desire In 2023
14K gold Chain 2mm (https://vimeo.com/931640860)
11 “Faux Pas” Which Are Actually Okay To Use With Your Motor Vehicle Compensation fort lee motor vehicle accident lawsuit (vimeo.com)
Why You Should Focus On Improving Repair Upvc Windows
Upvc repair
The Most Underrated Companies To Monitor In The Shark Robot Vacuum Industry Best Robot Mop And Vacuum Combo
7 Helpful Tricks To Making The Most Of Your Asbestos Lawyer asbestos legal
– markethiut.com,
You’ll Never Be Able To Figure Out This Peugeot Car Key Replacement Cost’s Tricks Peugeot Car
Key Replacement Cost (Doodleordie.Com)
The Reasons Why Unlock Car Door Service Is Everyone’s Passion In 2023 get Keys out of locked car
Ten Things You Need To Know About Citroen Key Replacement Near Me replacement key for citroen berlingo van
Ищете криптовалютный шлюз? С платежным сервисом Cryptocloud.plus – это легко и удобно принимать оплату со всего мира в популярных криптовалютах. Еще никогда не был таким простым сервис приема криптовалют, прием криптовалютных платежей, прием оплаты в криптовалюте. Вы сможете: осуществлять прием btc, прием криптовалют, криптоплатежи, принимать биткоин платежи, установить платежный шлюз криптовалют или криптовалютный шлюз, прием bitcoin, осуществлять процессинг платежей в криптовалюте, прием криптовалютных платежей на сайте.
Why Double Glazed Door Repairs Near Me Is The Right
Choice For You? upvc Double glazed windows
This Is The Advanced Guide To Robot Vacuums For Pet Hair affordable Robot vacuum
Five Prada Hand Bag Lessons From Professionals Prada Handbag Crossbody
11 Ways To Fully Redesign Your Online Shop Custom Hairpin Legs
Zet Casino Auszahlung Probleme: Was ist zu tun?
Das Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und attraktive Bonusangebote fГјr Spieler bietet. Doch trotz seiner Beliebtheit haben einige Spieler Probleme bei der Auszahlung ihrer Gewinne.
Wenn Sie Schwierigkeiten bei der Auszahlung Ihres Guthabens im Zet Casino haben, gibt es einige Schritte, die Sie unternehmen können, um das Problem zu lösen.
Zunächst sollten Sie sicherstellen, dass Sie alle Bonusbedingungen erfüllt haben, die mit Ihrem Gewinn verbunden sind. Manchmal können bestimmte Einsätze oder Spiele erforderlich sein, um sich für eine Auszahlung zu qualifizieren.
Wenn Sie sich sicher sind, dass Sie alle Bedingungen erfüllt haben, aber immer noch Schwierigkeiten bei der Auszahlung haben, sollten Sie den Kundendienst kontaktieren. Das Team von Zet Casino steht Ihnen rund um die Uhr zur Verfügung und kann Ihnen bei der Lösung Ihres Problems behilflich sein.
Es kann auch hilfreich sein, die Zahlungsmethoden zu überprüfen, die im Zet Casino verfügbar sind. Möglicherweise gibt es Einschränkungen oder Verzögerungen bei bestimmten Zahlungsmethoden, die Probleme bei der Auszahlung verursachen.
In einigen Fällen kann es auch vorkommen, dass technische Probleme die Auszahlung verzögern. In diesem Fall sollten Sie sicherstellen, dass Ihre Kontoinformationen korrekt sind und dass Sie über eine stabile Internetverbindung verfügen.
Wenn alle diese Schritte nicht zu einer Lösung führen, sollten Sie sich an die Glücksspielbehörde wenden, unter der das Zet Casino lizenziert ist. Die Behörde kann Ihnen bei der Lösung von Auszahlungsproblemen helfen und sicherstellen, dass das Casino seine Verpflichtungen erfüllt.
Insgesamt ist es wichtig, ruhig zu bleiben und geduldig zu sein, wenn Sie auf Auszahlungsprobleme im Zet Casino stoßen. Mit den richtigen Schritten und der Unterstützung des Kundendienstes können Sie Ihr Guthaben erfolgreich auszahlen lassen und Ihre Gewinne genießen.
https://zetcasino.one/
What Is The Reason? Double Glazing Repairs Near Me Is
Fast Becoming The Most Popular Trend For 2023 Replacement Double Glazing
The human body can continue to live thanks to the correct functioning of certain systems. If even one of these systems does not work properly, it can cause problems in human life. https://calmlean-web.com/
See What Mobile Car Diagnostics Near Me Tricks The Celebs Are Using Mobile Car Diagnostics
http://gabapentinneurontin.pro/# neurontin 400 mg
Nine Things That Your Parent Teach You About Boat Accident Lawsuit lawsuit
Guide To Online Shopping Uk Discount: The Intermediate Guide The Steps To Online Shopping Uk
Discount online shopping uk discount (m.thankyoumom.kr)
Guide To Bmw Replacement Key Cost: The Intermediate
Guide In Bmw Replacement Key Cost bmw replacement key Cost
This Week’s Top Stories About Mesothelioma Claim Mesothelioma Claim Mesothelioma Law
5 Killer Quora Answers To L Shaped Couches For Sale l shaped couches for sale (Tamara)
What’s The Current Job Market For Treadmills Near Me Professionals?
Treadmill (sang.Blog.Idnes.cz)
10 Things We All Are Hateful About Starter Kit Avon starter kit avon
8 Tips To Improve Your Are Cases Worth It
CSGO Game case shadow; https://trade-britanica.trade/wiki/This_Weeks_Top_Stories_About_Counter_Strike,
Zeneara is marketed as an expert-formulated health supplement that can improve hearing and alleviate tinnitus, among other hearing issues. https://zeneara-web.com/
5 Myths About Double Glazing Firms Near Me That You Should Avoid double glazing installer
The Reasons Why Audi Car Key Is The Obsession Of Everyone In 2023 Audi Tt key Programming
20 Railroad Injuries Claim Websites Taking The Internet By Storm
Railroad Injuries Attorneys
Сайт Casehunt https://casehunt.me/ это возможность открыть кейсы CS 2 и CS GO с выводом скинов. Зайдите на сайт – ознакомьтесь с кейсами, вы сможете увидеть, как недорогие и дешевые, так и различные серии кейсов. Подробнее на сайте
Ищите, где бесплатно, оперативно и без лишних проблем скачать интересующую игру? ТОРРЕНТ-ГЕЙМ вам поможет в этом. Вы должны совершить установку программы на компьютер – Torrent. Под любую игру имеется отдельная страница сайта, на ней – скриншоты прохождения, подробные описания. Ищете https://torrent-game.net/racing/? Torrent-game.net – ресурс, где можно найти то, что действительно увлечет. Увлекательный виртуальный мир ждет вас. Предлагаем вам отвлечься от повседневного быта и рабочей рутины. Приятного игрового процесса!
10 Reasons Why People Hate CSGO New Case.
CSGO New Case case operation bravo (Selene)
20 Things That Only The Most Devoted Replacement Ford Fiesta Key Uk Fans Understand Ford Ka key Replacement
You’ll Never Be Able To Figure Out This Window Repair Near Me’s Benefits window repair near me
See What Women Double Dildo Tricks The Celebs Are Making Use Of Women Double dildo
(https://minecraftcommand.Science)
A Provocative Rant About Shark Robotic Vacuum Cleaner Lidar robot vacuum
5 Window Glass Repair Near Me Projects For Every Budget Window Replacement
10 Life Lessons We Can Take From Double Glazed Units Near Me installed
20 Trailblazers Lead The Way In CSGO Weapon Case esports 2013 Winter case
11 Ways To Completely Revamp Your Railroad Injuries Legal palm bay Railroad injuries Lawsuit
GlucoBerry is one of the biggest all-natural dietary and biggest scientific breakthrough formulas ever in the health industry today. This is all because of its amazing high-quality cutting-edge formula that helps treat high blood sugar levels very naturally and effectively. https://glucoberry-web.com/
The 10 Scariest Things About SEO Software And Tools seo Software and tools
You’ll Never Guess This Beko Washing Machine Best Price’s Secrets Beko Washing Machine Best Price
How To Find The Perfect Self Empty Robot Vacuum And Mop Online
online
Pineal XT is a revolutionary supplement that promotes proper pineal gland function and energy levels to support healthy body function. https://pinealxt-web.com/
How To Find The Perfect Table Top Freezer On The Internet Medical freezers
Seven Reasons Why Mobile Car Locksmith Is Important locksmith that makes car keys near me
See What 10kg Washers Tricks The Celebs Are Using 10Kg Washers (B.Cari.Com.My)
Introducing TerraCalm, a soothing mask designed specifically for your toenails. Unlike serums and lotions that can be sticky and challenging to include in your daily routine, TerraCalm can be easily washed off after just a minute. https://terracalm-web.com/
Where Will Beko Washing Machine Models Be 1 Year From What Is Happening Now?
Beko Silver Tumble Dryer – 7kg Capacity
7 Things You’ve Never Knew About Car Lock Repair Near
Me Broken car door lock
The Next Big New Window Repair Near Industry upvc Window repair near me
What Is Lidar Robot Vacuum Cleaner’s History? History
Of Lidar Robot Vacuum Cleaner what is lidar robot vacuum (Latoya)
20 Quotes Of Wisdom About Situs Gotogel Terpercaya bandar judi
Why Mesothelioma Lawyer Should Be Your Next Big Obsession new Castle Mesothelioma law firm
Das Boomerang-Casino: Ein neuer Trend in der Welt des Online-GlГјcksspiels
In der Welt des Online-GlГјcksspiels gibt es immer wieder neue Trends und Ideen, die Spieler begeistern. Einer dieser Trends ist das sogenannte Boomerang-Casino, das in den letzten Jahren immer beliebter geworden ist.
Das Besondere an einem Boomerang-Casino ist, dass es den Spielern die Möglichkeit bietet, ihre Verluste zurückzuholen. Dies geschieht in der Regel durch spezielle Boni oder Aktionen, die es den Spielern ermöglichen, einen Teil ihres verlorenen Geldes zurückzugewinnen. So haben Spieler die Chance, auch in Pechsträhnen etwas Positives zu finden und ihre Verluste zu minimieren.
Ein weiterer Aspekt, der das Boomerang-Casino von herkömmlichen Online-Casinos unterscheidet, ist die Transparenz und Fairness, die hier besonders wichtig sind. Spieler können in einem Boomerang-Casino genau nachvollziehen, wie viel Geld sie bereits eingesetzt haben, wie viel sie gewonnen oder verloren haben und wie hoch ihre Chancen sind, Verluste zurückzugewinnen.
Durch diese Transparenz und Fairness fühlen sich Spieler im Boomerang-Casino sicher und gut aufgehoben. Sie wissen, dass sie nicht einfach nur Glücksspiele spielen, sondern dass sie auch die Möglichkeit haben, ihre Verluste wieder auszugleichen.
Insgesamt bietet das Boomerang-Casino eine spannende und innovative Alternative zu herkömmlichen Online-Casinos. Spieler können hier nicht nur ihr Glück versuchen, sondern auch von fairen Bedingungen und interessanten Boni profitieren. Daher ist es nicht überraschend, dass das Boomerang-Casino immer mehr Anhänger findet und sich zu einem wichtigen Trend in der Welt des Online-Glücksspiels entwickelt.
https://boomerangcasino.one/
15 Reasons To Love Birth Injury Compensation Mooresville birth injury attorney
The 10 Most Scariest Things About Which Is Best For Online Grocery Shopping Which Is Best For Online Grocery Shopping
Select the appropriate metal material for the specific design teplica-parnik.net. Requirements for strength, corrosion resistance and other characteristics must be taken into account. It is worth contacting experienced specialists who will help you understand all the parameters.
neurontin 1200 mg neurontin tablets no script buy neurontin
VidaCalm is an all-natural blend of herbs and plant extracts that treat tinnitus and help you live a peaceful life. https://vidacalm-web.com/
The Top Glass Repair Luton Experts Are Doing 3 Things Window replacement
5 Tools That Everyone In The Mesothelioma Lawsuit Industry Should Be Utilizing mesothelioma settlement
На сайте https://interpol-s.ru/ вы сможете заказать проверку на полиграфе. Вы пройдете тестирование на профессиональном устройстве. Проводятся зависимые и независимые экспертизы. Вся информация проверяется на достоверность. В обязательном порядке соблюдается закон, требования. Записаться на услугу можно в любое время, когда вам удобно. В компании оказываются такие популярные и важные услуги, как: проверка на полиграфе, полиграф для женщин, проведение судебных экспертиз, тестирование персонала.
Guide To Double Glazing Near Me: The Intermediate Guide Towards Double Glazing Near
Me double Glazing Near me
doxycycline order online: doxycycline 100mg price – 100mg doxycycline
5 Must-Know Hismphash Practices You Need To Know For 2023 Seo Agency Near Me
The People Closest To Private ADHD Assessment Near Me
Share Some Big Secrets adhd assessment for adults private
Gorilla Flow prostate is an all-natural dietary supplement for men which aims to decrease inflammation in the prostate to decrease common urinary tract issues such as frequent and night-time urination, leakage, or blocked urine stream. https://gorillaflow-web.com
Top 10 Online Shopping Sites In Uk For Clothes Tools To Ease Your Daily Life Top 10 Online Shopping Sites In Uk
For Clothes Trick That Everyone Should Be Able To Top 10 Online Shopping Sites In Uk For Clothes [Images.Google.Co.Tz]
It is crucial for an attorney to know how to recognize
palm coast asbestos Lawsuit-related
products in every case. This can be done by discussing with colleagues, obtaining reports, or looking at samples
from homes or workplaces.
Why All The Fuss Over Machines Coffee? smart Coffee machines (ocher-lemon-fzvpcr.mystrikingly.com)
Dreame L30 Ultra Price Tools To Help You Manage Your Daily Lifethe
One Dreame L30 Ultra Price Trick That Should Be Used By Everyone Be Able
To dreame l30 ultra price (https://marvelvsdc.Faith/)
HoneyBurn is a revolutionary liquid weight loss formula that stands as the epitome of excellence in the industry. https://honeyburn-web.com/
15 Current Trends To Watch For Tommy Hilfiger Female Bags
tommy hilfiger Bags black
7 Easy Tips For Totally Rocking Your Online Shopping Uk Cheap Skilsaw Spt99-11 Review
See What 9kg Washing Machines Uk Tricks The Celebs Are Utilizing 9kg washing machines Uk
Who’s The Top Expert In The World On Double Glazing Windows Near Me?
double glazing company near me, Shad,
What’s The Job Market For Double Glazing Repairs Near Me Professionals?
double glazing repairs near Me (https://minecraftathome.com/minecrafthome/show_user.php?userid=18286636)
10 Uk Online Shopping Sites For Mobile That Are Unexpected Flat And Book Binding Machine
14 Common Misconceptions About Work From Home Jobs Online Uk work from home vacancies
Das Boomerang Casino DE ist ein Online-Casino, das Spielern ein breites Angebot an Spielen und Unterhaltungsmöglichkeiten bietet. In diesem Artikel werden wir einen genaueren Blick auf das Boomerang Casino werfen und herausfinden, was es von anderen Online-Casinos unterscheidet.
Zu den Spielen, die im Boomerang Casino DE angeboten werden, gehГ¶ren eine Vielzahl von Slots, Tischspielen, Live-Casino-Spielen und Jackpot-Spielen. Die Spiele stammen von renommierten Anbietern wie NetEnt, Microgaming, Play’n GO und vielen anderen. Dies bedeutet, dass die Spieler qualitativ hochwertige und unterhaltsame Spiele genieГџen kГ¶nnen, die fair und sicher sind.
Ein weiterer Vorteil des Boomerang Casino ist die Benutzerfreundlichkeit der Plattform. Die Webseite ist intuitiv gestaltet und ermöglicht es den Spielern, schnell und einfach auf ihre Lieblingsspiele zuzugreifen. Darüber hinaus bietet das Casino eine mobile App, die es den Spielern ermöglicht, auch unterwegs zu spielen.
Ein weiterer großer Vorteil des Boomerang Casino DE sind die großzügigen Boni und Aktionen, die den Spielern angeboten werden. Neue Spieler erhalten in der Regel einen Willkommensbonus, der Freispiele oder Einzahlungsboni beinhalten kann. Darüber hinaus werden regelmäßig Promotionen und Belohnungen für treue Spieler angeboten.
Was das Boomerang Casino DE wirklich von anderen Online-Casinos unterscheidet, ist der exzellente Kundenservice. Das Support-Team des Casinos ist rund um die Uhr erreichbar und steht den Spielern bei Fragen oder Problemen zur VerfГјgung. Dies schafft ein positives Spielerlebnis und sorgt dafГјr, dass die Spieler gerne im Boomerang Casino spielen.
Insgesamt bietet das Boomerang Casino DE eine erstklassige Spielerfahrung mit einer Vielzahl von Spielen, groГџzГјgigen Boni und einem exzellenten Kundenservice. Wenn Sie auf der Suche nach einem unterhaltsamen und sicheren Online-Casino sind, sollten Sie definitiv das Boomerang Casino in Betracht ziehen.
https://boomerangcasino.one/
What Audi Key Will Be Your Next Big Obsession costs
Keravita Pro™ is a dietary supplement created by Benjamin Jones that effectively addresses nail fungus and hair loss, promoting the growth of healthier and thicker nails and hair. The formula is designed to target the underlying causes of these health issues and provide comprehensive treatment. https://keravitapro-web.com
5. Boat Accident Case Projects For Any Budget Boat accident Lawsuit
The Next Big Event In The Ghost Immobilisers Industry Ghost Immobiliser For Sale
Nine Things That Your Parent Taught You About Treadmills Desk Treadmills desk
5 Killer Quora Answers To Replacement Volvo Keys Replacement volvo keys
Как обезопасить свои данные: страхуйтесь от утечек информации в интернете. Сегодня охрана своих данных становится всё более важной задачей. Одним из наиболее обычных способов утечки личной информации является слив «сит фраз» в интернете. Что такое сит фразы и как предохранить себя от их утечки? Что такое «сит фразы»? «Сит фразы» — это сочетания слов или фраз, которые бывают используются для получения доступа к различным онлайн-аккаунтам. Эти фразы могут включать в себя имя пользователя, пароль или дополнительные конфиденциальные данные. Киберпреступники могут пытаться получить доступ к вашим аккаунтам, используя этих сит фраз. Как сохранить свои личные данные? Используйте сложные пароли. Избегайте использования очевидных паролей, которые легко угадать. Лучше всего использовать комбинацию букв, цифр и символов. Используйте уникальные пароли для всего аккаунта. Не применяйте один и тот же пароль для разных сервисов. Используйте двухступенчатую аутентификацию (2FA). Это привносит дополнительный уровень безопасности, требуя подтверждение входа на ваш аккаунт по другое устройство или метод. Будьте осторожны с онлайн-сервисами. Не доверяйте личную информацию ненадежным сайтам и сервисам. Обновляйте программное обеспечение. Установите обновления для вашего операционной системы и программ, чтобы сохранить свои данные от вредоносного ПО. Вывод Слив сит фраз в интернете может повлечь за собой серьезным последствиям, таким как кража личной информации и финансовых потерь. Чтобы обезопасить себя, следует принимать меры предосторожности и использовать надежные методы для хранения и управления своими личными данными в сети
12 Stats About 18 Wheeler Accident Attorney To Make You Take A Look At Other People jacksonville
18 wheeler accident Lawyer (vimeo.Com)
Желаете недорого приобрести функциональные и надежные шлагбаумы? Вы точно попали по адресу! У нас представлены шлагбаумы различной стоимости. Ассортимент наш очень большой, мы вас приятно удивим. Предлагаем исключительно продукцию, прошедшую сертификацию. Ищете шлагбаум дорхан? Senator-sb.ru – сайт, где вы можете приобрести шлагбаум и сделать заказ на установку конструкции на вашем объекте. Оформить заявку либо уточнить актуальную стоимость товаров, можно связавшись с нами по контактному номеру телефона. Обеспечьте безопасность на вашей территории!
Nissan Micra Key Replacement Tools To Ease Your Daily Lifethe One Nissan Micra Key Replacement Trick That Should Be Used By Everyone
Be Able To Nissan Micra Key Replacement
Don’t Stop! 15 Things About Door Fitter Leeds We’re Tired Of Hearing window
10 Fundamentals Regarding Buy Sex Machine You Didn’t Learn At School
cheap sex machine
http://zithromaxa.store/# zithromax 500 mg
Think You’re The Perfect Candidate For Bentley
Car Keys? Check This Quiz bentley flying spur key
9 . What Your Parents Teach You About Machine Espresso Machine Espresso
Glass Repair Leeds Tips From The Most Effective In The Business upvc door lock repair leeds [Dina]
Криптокошельки с балансом: зачем их покупают и как использовать
В мире криптовалют все большую популярность приобретают криптокошельки с предустановленным балансом. Это специальные кошельки, которые уже содержат определенное количество криптовалюты на момент покупки. Но зачем люди приобретают такие кошельки, и как правильно использовать их?
Почему покупают криптокошельки с балансом?
Удобство: Криптокошельки с предустановленным балансом предлагаются как готовое решение для тех, кто хочет быстро начать пользоваться криптовалютой без необходимости покупки или обмена на бирже.
Подарок или награда: Иногда криптокошельки с балансом используются как подарок или премия в рамках акций или маркетинговых кампаний.
Анонимность: При покупке криптокошелька с балансом нет обязательства предоставлять личные данные, что может быть важно для тех, кто ценит анонимность.
Как использовать криптокошелек с балансом?
Проверьте безопасность: Убедитесь, что кошелек безопасен и не подвержен взлому. Проверьте репутацию продавца и происхождение приобретения кошелька.
Переведите средства на другой кошелек: Если вы хотите долгосрочно хранить криптовалюту, рекомендуется перевести средства на более безопасный или практичный для вас кошелек.
Не храните все средства на одном кошельке: Для обеспечения безопасности рекомендуется распределить средства между несколькими кошельками.
Будьте осторожны с фишингом и мошенничеством: Помните, что мошенники могут пытаться обмануть вас, предлагая криптокошельки с балансом с целью получения доступа к вашим средствам.
Заключение
Криптокошельки с балансом могут быть удобным и легким способом начать пользоваться криптовалютой, но необходимо помнить о безопасности и осторожности при их использовании.Выбор и приобретение криптокошелька с балансом – это серьезный шаг, который требует внимания к деталям и осознанного подхода.”
Volca Burn is a weight loss supplement that uses a “red tingle hack” to help you rapidly lose weight without dieting or exercising. https://volcaburn-web.com/
How To Get Better Results From Your Pittsburgh Birth
Injury Attorney birth injury medical malpractice Attorney; http://www.Cheaperseeker.Com,
Xitox’s foot pads contain a combination of powerful herbs that help provide a soothing experience for your feet after a long day. https://xitox-web.com/
Sash Window Replacement Tools To Help You
Manage Your Everyday Lifethe Only Sash Window Replacement Trick
That Every Person Should Know Sash Window Replacement
Слив мнемонических фраз (seed phrases) является одним наиболее популярных способов утечки личной информации в мире криптовалют. В этой статье мы разберем, что такое сид фразы, по какой причине они важны и как можно защититься от их утечки.
Что такое сид фразы?
Сид фразы, или мнемонические фразы, представляют собой комбинацию слов, которая используется для составления или восстановления кошелька криптовалюты. Обычно сид фраза состоит из 12 или 24 слов, которые представляют собой ключ к вашему кошельку. Потеря или утечка сид фразы может привести к потере доступа к вашим криптовалютным средствам.
Почему важно защищать сид фразы?
Сид фразы представляют ключевым элементом для секурного хранения криптовалюты. Если злоумышленники получат доступ к вашей сид фразе, они сумеют получить доступ к вашему кошельку и украсть все средства.
Как защититься от утечки сид фраз?
Никогда не передавайте свою сид фразу ничьему, даже если вам происходит, что это авторизованное лицо или сервис.
Храните свою сид фразу в секурном и защищенном месте. Рекомендуется использовать аппаратные кошельки или специальные программы для хранения сид фразы.
Используйте экстра методы защиты, такие как двусторонняя аутентификация, для усиления безопасности вашего кошелька.
Регулярно делайте резервные копии своей сид фразы и храните их в разнообразных безопасных местах.
Заключение
Слив сид фраз является серьезной угрозой для безопасности владельцев криптовалют. Понимание важности защиты сид фразы и принятие соответствующих мер безопасности помогут вам избежать потери ваших криптовалютных средств. Будьте бдительны и обеспечивайте надежную защиту своей сид фразы
The 10 Most Terrifying Things About Treadmill treadmills sale Uk
Hydrossential is actually a skincare serum or you can say a skincare supplement created by Emma Smith to help women keep their skin looking beautiful and flawless. https://hydrossential-web.com/
5 Laws That’ll Help The Bentley Valet Key Industry Bentley Key
Carbofix is the revolutionary dietary formula that promises to activate weight loss without all the extra hard work. https://carbofix-try.com
Boomerang-Casinos sind eine relativ neue Form von Online-Casinos, die in der GlГјcksspielbranche immer beliebter werden. Der Name “Boomerang” bezieht sich auf die Tatsache, dass Spieler, die an diesen Casinos teilnehmen, immer wieder zurГјckkehren, um mehr zu spielen.
Das Besondere an Boomerang-Casinos ist, dass sie eine Vielzahl von attraktiven Boni und Belohnungen für ihre Spieler anbieten. Dies reicht von Willkommensboni und Freispielen bis hin zu regelmäßigen Aktionen und Treueprämien. Diese Boni dienen dazu, die Spieler zu motivieren, weiterzuspielen und ihnen ein besonderes Spielerlebnis zu bieten.
Ein weiteres Merkmal von Boomerang-Casinos ist ihre Benutzerfreundlichkeit und ihre Verfügbarkeit auf verschiedenen Geräten. Spieler können von überall und zu jeder Zeit auf ihre Lieblingsspiele zugreifen, sei es auf dem Computer, dem Smartphone oder dem Tablet. Diese Flexibilität macht es für die Spieler einfacher, ihre Lieblingsspiele zu genießen und gleichzeitig ihre Gewinnchancen zu maximieren.
Da Boomerang-Casinos noch relativ neu sind, gibt es eine Vielzahl von Anbietern, die um die Gunst der Spieler konkurrieren. Dies führt zu einem verstärkten Wettbewerb und einer Vielzahl von Angeboten, von denen die Spieler profitieren können. Es ist wichtig, jedoch darauf zu achten, dass man nur bei seriösen Anbietern spielt, um Betrug und unfaire Praktiken zu vermeiden.
Insgesamt sind Boomerang-Casinos eine aufregende Entwicklung in der Welt des Online-Glücksspiels und bieten Spielern die Möglichkeit, an unterhaltsamen und lohnenden Spielen teilzunehmen. Es ist jedoch wichtig, verantwortungsbewusst zu spielen und sich an die geltenden Gesetze und Vorschriften zu halten, um ein sicheres und faires Spielerlebnis zu gewährleisten.
https://boomerangcasino.one/
Arctic blast is a powerful formula packed with natural ingredients and can treat pain effectively if you’re struggling with chronic pain. You can say goodbye to muscle cramps with this natural pain reliever in less than a minute. It helps with arthritic pain, blood circulation, and joint pain. It gives long-lasting effects that replace the need to go to surgery. https://arcticblast-web.com
Reliver Pro is a dietary supplement formulated with a blend of natural ingredients aimed at supporting liver health
You Are Responsible For An Motor Vehicle Litigation Budget?
12 Tips On How To Spend Your Money Fox River Grove Motor Vehicle Accident Law Firm
9 Lessons Your Parents Teach You About Window Pane Replacement Window Pane Replacement
See What L30 Dreame Tricks The Celebs Are Using L30 dreame
The 10 Most Terrifying Things About How Do I Get A Spare Car Key how do i get
a spare car key (http://Www.Dermandar.com)
What Freud Can Teach Us About Glass Anal Butt
Plugs silicone anal butt plug
Guide To Walking Desk Pad: The Intermediate Guide In Walking Desk Pad
walking desk pad
cenforce online abrupt – brand sildenafil brand viagra online vast
5 Killer Quora Answers On Best Accident Attorney Accident Attorney
What’s The Job Market For Treadmill For Home Use Professionals Like?
treadmill for home use [40billion.com]
Five Things Everybody Gets Wrong About Double Glazing Window Lock Repair install
Abdomax is a nutritional supplement using an 8-second Nordic cleanse to eliminate gut issues, support gut health, and optimize pepsinogen levels. https://abdomax-web.com
where can i buy amoxocillin amoxicillin for sale where can you buy amoxicillin over the counter
10 Things That Your Family Teach You About Asbestos Case asbestos
Top 10 Online Shopping Sites In Uk For Clothes Tools To
Make Your Everyday Lifethe Only Top 10 Online Shopping Sites
In Uk For Clothes Trick That Everybody Should Learn top 10 online shopping sites in uk for clothes
The Often Unknown Benefits Of Mesothelioma Town And Country Mesothelioma Lawsuit
The 10 Most Terrifying Things About Leeds Double Glazing Leeds Double Glazing
neurontin 400: gabapentin 600 mg – neurontin drug
Why You’ll Want To Learn More About Real Money Slots jackpot slots
(Pat)
15 Top Twitter Accounts To Learn More About Pvc Window Repairs upvc Window repairs
Introduction To The Intermediate Guide For Side By Side Fridge Freezer For Sale small side by side refrigerator/freezer
Glass Repair Leeds Tips From The Best In The Industry
Double Glazed Doors Repairs
This Story Behind Skin So Soft Can Haunt You Forever!
Skin So Soft Oil, Imoodle.Win,
На сайте https://bluedroid.ru/ игры и приложения для Андроид телефона, читы, приватные сервера и пользовательские модификации игр с убранной рекламой и неограниченной валютой!
cenforce well – cenforce online stout brand viagra pills appearance
LipoSlend is a liquid nutritional supplement that promotes healthy and steady weight loss. https://liposlend-web.com/
The main advantage of a forklift is its versatility and ease of use stroibloger.com. Essentially, it’s just a dolly with a durable fork that can be used to lift pallets or large loads to any height.
The Most Hilarious Complaints We’ve Received About Unlock Car Service I Locked My Keys In My Car
На сайте https://beperfect-shop.ru/ вы приобретете качественные материалы для наращивания, а также ламинирования ресниц. Вся продукция является качественной, безопасной и функциональной. Регулярно проходят распродажи, на отдельные группы товаров действуют скидки. В разделе находится клей, ресницы, а также дополнительные материалы, которые потребуются для профессионального оказания услуги. В интернет-магазине постоянно появляются новинки, которые применяются в салонах красоты.
“Ask Me Anything,” 10 Responses To Your Questions About 12kg Washer in My area
На сайте https://1roma.ru/ вы сможете выбрать и заказать такой строительный материал, как: фасадные панели, сайдинг, дренажные системы, водостоки, газонные решетки и многое другое. Перед вами огромный ассортимент вариантов, привлекательных коллекций различных фактур и цветовых решений. Несколько сотен вариантов отделки, в том числе, темные цветостойкие панели. Прямо сейчас посмотрите все доступные варианты. Вы сможете пролистать каталог всего за пару минут, чтобы ознакомиться с готовыми решениями.
What You Need To Do On This Truck Accident Claims
truck accident Lawsuit (https://utahsyardsale.com/author/monica30324)
Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und Zahlungsmethoden anbietet. Eine der neuesten Zahlungsmethoden, die im Zet Casino verfГјgbar ist, ist Zimpler.
Zimpler ist ein innovativer Zahlungsdienst aus Schweden, der es Spielern ermöglicht, Einzahlungen in Online-Casinos auf einfache und sichere Weise vorzunehmen. Mit Zimpler können Spieler ganz einfach über ihr Mobiltelefon Einzahlungen tätigen, ohne lästige Registrierungen oder langwierige Banküberweisungen durchführen zu müssen.
Um Zimpler im Zet Casino zu nutzen, müssen Spieler lediglich ihre Handynummer angeben und den Bestätigungscode eingeben, der per SMS an ihr Mobiltelefon gesendet wird. Anschließend können sie den gewünschten Einzahlungsbetrag eingeben und die Transaktion mit nur einem Klick abschließen.
Zimpler garantiert schnelle und sichere Zahlungen im Zet Casino, so dass Spieler sich voll und ganz auf ihr Spielerlebnis konzentrieren können, ohne sich über Sicherheitsbedenken oder lange Wartezeiten Gedanken machen zu müssen. Darüber hinaus bietet Zimpler auch eine Übersicht über alle getätigten Transaktionen, so dass Spieler jederzeit einen Überblick über ihre Einzahlungen haben.
Insgesamt ist Zimpler eine bequeme und zuverlässige Zahlungsmethode, die das Spielerlebnis im Zet Casino noch angenehmer macht. Probieren Sie es aus und erleben Sie die Vorteile von Zimpler selbst!
https://zetcasino.one/
Metabo Flex® Is a Dietary Supplement Formulated Using a Proprietary Blend Of Six Rainforest Super Nutrients And Plants Designed To Boost Metabolism And Reduce Weight. https://metaboflex-us.com
7 Simple Changes That Will Make The Biggest Difference In Your Work Home From
Jobs permanent
15 Twitter Accounts That Are The Best To Learn About Treadmill Treadmills Sale uk
20 Glazing Repairs Near Me Websites Taking The Internet By Storm double Glazing near Me
Cardio Shield positions itself as an all-encompassing heart health dietary aid. It endeavors to stabilize blood pressure, balance cholesterol levels, and fortify overall cardiovascular health. . https://cardioshield-web.com/
You’ll Never Be Able To Figure Out This Walking Pad Under Desk’s Secrets Walking Pad under desk
Keratone addresses the real root cause of your toenail fungus in an extremely safe and natural way and nourishes your nails and skin so you can stay protected against infectious related diseases. https://keratone-web.com/
You’ll Never Be Able To Figure Out This Double Glaze Repair Near Me’s Secrets Double glaze repair near me
20 Truths About Freezer Freestanding: Busted built-in freezers (https://minecraftcommand.science/profile/housesize6)
10 Beautiful Graphics About Standing Desk Treadmill Walk Pad For Desk
15 Things You’re Not Sure Of About Window Repair Near window repair near me
Хотите смотреть увлекательные фильмы и сериалы совершенно бесплатно в хорошем качестве? Lords.lat – это то, что вам нужно! Здесь представлены фильмы с захватывающим сюжетом. Драмы, комедии, фантастика, ужасы, детективы, боевики – все это доступно для вас. Отправляйтесь в чудесный мир, полный приключений. https://2024-films.lords.lat – сайт, где можете найти то, что пожелаете. Здесь есть поиск, им можно в любой момент воспользоваться. Не упустите возможность насладиться просмотром фильмов, сериалов и мультфильмов в великолепном качестве!
The Best 12kg Washing Machines For Sale Tricks For Changing Your Life
Best 12kg Washing Machines
10 Tips For Desk Treadmill Foldable That Are Unexpected Foldable Desk Treadmill
15 Tips Your Boss Wants You To Know About Treadmill
You’d Known About Treadmill Treadmills sale uk
“The Fridge Freezer Haier Awards: The Best, Worst, And Most Bizarre Things We’ve Seen Bottom Mount
Five Killer Quora Answers To Asbestos Lawsuit asbestos lawsuit
pharmacy codeine
https://doxycyclinea.online/# doxycycline monohydrate
5 Common Phrases About Case Opening Sites CSGO You
Should Avoid case revolution (http://wownsk-portal.ru)
The One 12kg Washing Machines Uk Mistake Every Beginner Makes combined
How To Make A Successful Slot Features Strategies From Home
Progressive slots (web011.dmonster.kr)
Then You’ve Found Your Shopping Online Sites List …
Now What? Vimeo
20 Questions You Need To Ask About Mesothelioma Claim Before You
Buy Mesothelioma Claim Reputable Asbestos Attorney
Will Locksmith For Car Ever Be The King Of The World?
Locksmith Lost Car Keys Cost
Inserts are the most consumable part of a workpiece machining system. They homeprorab.info are placed in special holders and can be quickly changed depending on wear or process requirements.
What Is Replacement Upvc Window Handles And
How To Make Use Of It Repairs To Upvc Windows (http://Cse.Google.Ba/)
15 Reasons Why You Shouldn’t Ignore Mesothelioma Mesothelioma Legal Experts
Boomerang Casino ist ein Online-Casino, das in den letzten Jahren immer beliebter geworden ist. Viele Spieler schätzen die Vielfalt an Spielen, die hier angeboten werden, sowie den hervorragenden Kundenservice. Doch die Frage, die sich viele stellen, ist: Ist Boomerang Casino seriös?
Um diese Frage zu beantworten, lohnt es sich zunächst einen Blick auf die Lizenzierung des Casinos zu werfen. Boomerang Casino ist im Besitz einer Lizenz der Malta Gaming Authority, einer der renommiertesten Glücksspielbehörden der Welt. Diese Lizenz garantiert, dass das Casino strenge Auflagen erfüllt und regelmäßig überprüft wird, um sicherzustellen, dass faire Spielbedingungen gewährleistet sind.
DarГјber hinaus arbeitet Boomerang Casino mit namhaften Softwareanbietern zusammen, darunter NetEnt, Microgaming und Play’n GO. Diese Unternehmen sind bekannt fГјr ihre hochwertigen Spiele und garantieren ein sicheres und faires Spielerlebnis.
Auch in Sachen Kundenservice kann Boomerang Casino punkten. Der Support ist rund um die Uhr erreichbar und steht den Spielern bei Fragen und Problemen kompetent zur Seite. Zudem wird auf der Webseite transparent Гјber die Zahlungsmethoden und die Datenschutzrichtlinien informiert.
Zusammenfassend lässt sich sagen, dass Boomerang Casino als seriöser Anbieter betrachtet werden kann. Die Lizenzierung durch die Malta Gaming Authority, die Zusammenarbeit mit renommierten Softwareanbietern und der gute Kundenservice sprechen für das Casino. Spieler können sich hier also sicher und gut aufgehoben fühlen und ihrem Spielvergnügen unbesorgt nachgehen.
https://boomerangcasino.one/
Watch Out: What Double Bed Top Bunk Is Taking Over And What To Do
About It multiple bunk beds
10 Things That Your Family Taught You About Designer Handbags White designer Handbags white
Guide To Double Glazing Near Me: The Intermediate Guide To Double Glazing Near
Me double glazing near Me
7 Small Changes You Can Make That’ll Make An Enormous Difference To Your Birth Injury Attorney attorneys
This Week’s Most Popular Stories About Emergency Car
Locksmith Locksmith near me for cars cheap (https://mullins-lauritsen-2.blogbright.net/)
20 Resources That Will Make You Better At Treadmills Sale UK Treadmill For Home Use
20 Things Only The Most Devoted Slot Demo Pragmatic Fans Know Slot Demo Pragmatic Maxwin
Five Locksmith Automotive Lessons From The Pros automotive locksmith Shop
How To Explain Amazon Online Shopping Clothes Uk To Your Grandparents Vimeo.Com
Guide To Locked Myself Out Of My Car: The Intermediate Guide Towards Locked Myself Out Of My Car locked Myself Out
One Key Trick Everybody Should Know The One
Should Mobility Scooters Be On The Pavement
Trick Every Person Should Be Aware Of pavement trail Scooters
15 Things You’ve Never Known About Mesothelioma Law Firm Bowie mesothelioma lawyer
4 Dirty Little Secrets About The CSGO New Case Industry Riptide Case
One Key Trick Everybody Should Know The One Railroad Injuries Claim
Trick Every Person Should Learn Railroad Accident Lawyer Near Me Georgia (Minecraftcommand.Science)
Five Killer Quora Answers To Double Glazed Window
Repairs Near Me double glazed window repairs near Me
amoxicillin 30 capsules price amoxil generic how much is amoxicillin
10 Adult Massagers Related Projects To Expand
Your Creativity Hush adult toys
10 Facts About Robot Vacuums With Lidar That Will Instantly
Get You Into A Great Mood robot vacuums with obstacle avoidance lidar (http://www.healthndream.com/)
Your confidence in us is our utmost importance.
Therefore, we operate with absolute integrity and commitment to
your satisfaction.
Feel the comfort of seeing your funds returned with our professional services.
15 Terms That Everyone Within The Online Shopping Uk Cheap Industry Should Know Thermal Imaging Multimeter
Проект Мир: Л мы создали специально для того, чтобы вы научились ценить себя и отдавать любовь миру вокруг вас. Развивайтесь и самосовершенствуйтесь, смотрите вебинары, проходите обучение, посещайте мероприятия в разных уголках планеты. Ищете счастье психология? Mir-l.com – зарегистрировавшись тут абсолютно бесплатно, вы сразу получите доступ к интересным статьям, видеороликам, а также аудиозаписям по различным сферам. Если у вас возникли вопросы, пишите нам, укажите имя и e-mail на сайте. Исследуйте уже сейчас платформу Мир: Л!
What’s The Job Market For Sofas Sectionals Professionals Like?
Sofas Sectional
prednisone without prescription 10mg: how much is prednisone 5mg – prednisone over the counter
How Repair Upvc Windows Rose To Become The #1 Trend On Social Media repairing Upvc windows
How To Survive Your Boss In Toys For Clits best Clit vibrator
ремонт ноутбука в москве
ремонт ноутбуков в москве
Are The Advances In Technology Making Cheapest Rabbit Vibrators
Better Or Worse? Vibrator the Rabbit
sildenafil price cvs
Boomerang Casino Avis – Ein Гњberblick Гјber dieses aufregende Online-Casino
Boomerang Casino ist ein aufstrebendes Online-Casino, das Spielern eine Vielzahl von Unterhaltungsmöglichkeiten bietet. Mit einer breiten Palette von Spielen, großzügigen Boni und einem hervorragenden Kundenservice hat Boomerang Casino schnell an Beliebtheit gewonnen.
Das Casino bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele, Live-Casino und mehr. Mit hochwertiger Software von fГјhrenden Anbietern wie NetEnt, Microgaming und Play’n GO kГ¶nnen die Spieler ein reibungsloses und unterhaltsames Spielerlebnis genieГџen.
Ein weiterer großer Vorteil von Boomerang Casino sind die großzügigen Boni und Promotionen, die den Spielern regelmäßig angeboten werden. Neue Spieler können sich über einen Willkommensbonus freuen, der ihnen zusätzliches Geld zum Spielen bietet. Darüber hinaus gibt es regelmäßig Aktionen wie Freispiele, Einzahlungsboni und Turniere, die den Spielern die Chance bieten, noch mehr zu gewinnen.
Der Kundenservice von Boomerang Casino ist ebenfalls top. Das Team ist rund um die Uhr erreichbar und steht den Spielern bei Fragen oder Problemen zur VerfГјgung. Die Mitarbeiter sind freundlich, kompetent und bemГјht, den Spielern ein groГџartiges Spielerlebnis zu bieten.
Insgesamt ist Boomerang Casino eine ausgezeichnete Wahl fГјr alle, die nach einem unterhaltsamen und sicheren Online-Casino suchen. Mit einer groГџen Auswahl an Spielen, groГџzГјgigen Boni und einem erstklassigen Kundenservice gibt es viele GrГјnde, dieses Casino auszuprobieren. Besuchen Sie noch heute die Website von Boomerang Casino und erleben Sie die Magie selbst!
https://boomerangcasino.one/
7 Simple Changes That’ll Make A Big Difference With
Your Repair Double Glazed Windows window Doctor
Five Things Everybody Gets Wrong In Regards To Tommy
Hilfiger Bag Ladies tommy hilfiger tote handbag
Дорожная служба спасения 911 с успехом оказывает услуги в области эвакуации легкового и грузового транспорта. Гарантируем вам профессионализм всех сотрудников и оперативность. Требуется? Пенза эвакуатор? Penza-evakuator.ru – сайт, где у вас есть возможность уже сейчас оставить заявку и увидеть фото нашей работы. Для этого стоит указать ваш номер телефона и имя. Здесь можете ознакомиться с прайс-листом и отзывами довольных клиентов. Также вы детальнее узнаете, какие мы готовы эвакуировать виды техники. Обращайтесь именно к нам, будем рады вам помочь!
Your confidence in us is our top priority.
Therefore, we work with complete integrity and dedication to your
case.
Rest easy of recovering your QIWI wallet balance
with our expert help.
Our expertise in cyber finance and online transactions means we’re ideally suited to tackle your
QIWI wallet issues.
Have peace of mind, we use advanced techniques and keep up
with the latest security protocols.
If you’ve been victimized by unauthorized transactions or
issues that resulted in a loss of funds, we’re here to help.
A Productive Rant About CS GO Weapon Case case clutch – Hayden –
Tikstroy.ru – сайт, который предлагает недорогие услуги по укладке тротуарной плитки. Квалифицированные мастера в короткие сроки и качественно осуществят работы. Вы можете довериться специалистам. Ищете укладка тротуарной плитки под ключ в серпухове? Tikstroy.ru – сайт, где можно прямо сейчас посмотреть наши некоторые работы. Гарантируем персональный подход к любому клиенту, прислушиваемся ко всем пожеланиям и замечаниям. Готовы с удовольствием проконсультировать вас по интересующим вопросам. Обращайтесь к нам, полностью удовлетворим ваши потребности.
What’s Holding Back In The Railroad Injuries Law
Industry? railroad accident attorney (Theda)
ремонт телефона
ремонт телефонов рядом
ремонт телефонов рядом
Five Qualities That People Search For In Every Online Shopping
Uk Amazon Ajh410-Nkl Vent Register
You’ll Be Unable To Guess Best Robot Vacuum With Self Empty’s Tricks best robot Vacuum with Self empty
7 Things You’ve Always Don’t Know About Designer
Handbags To Sell Designer handbags on Amazon
Guide To Link Login Gotogel: The Intermediate Guide Towards Link Login Gotogel link login Gotogel
What Misted Double Glazing Repairs Experts Would Like You To Know
door Repair
هنا النص مع استخدام السبينتاكس:
“هرم الروابط الخلفية
بعد التحديثات العديدة لمحرك البحث G، تحتاج إلى تنفيذ خيارات ترتيب مختلفة.
هناك منهج لجذب انتباه محركات البحث إلى موقعك على الويب باستخدام الروابط الخلفية.
الروابط الخلفية ليست فقط أداة فعالة للترويج، ولكن تتضمن أيضًا حركة مرور عضوية، والمبيعات المباشرة من هذه الموارد على الأرجح لن تكون كذلك، ولكن التحولات ستكون، وهي حركة المرور التي نحصل عليها أيضًا.
ما نكون عليه في النهاية في النهاية في الإخراج:
نعرض الموقع لمحركات البحث من خلال الروابط الخلفية.
2- نحصل على تحويلات عضوية إلى الموقع، وهي أيضًا إشارة لمحركات البحث أن المورد يستخدمه الناس.
كيف نظهر لمحركات البحث أن الموقع سائل:
1 يتم عمل لينك خلفي للصفحة الرئيسية حيث المعلومات الرئيسية
نقوم بعمل لينكات خلفية من خلال عمليات توجيه مرة أخرى المواقع الموثوقة
الأهم من ذلك أننا نضع الموقع على أداة منفصلة من أساليب تحليل المواقع، ويدخل الموقع في ذاكرة التخزين المؤقت لهذه المحللات، ثم الروابط المستلمة التي نضعها كتوجيه مرة أخرى على المدونات والمنتديات والتعليقات.
هذا الخطوة المهم يعرض لمحركات البحث خارطة الموقع، حيث تعرض أدوات تحليل المواقع جميع المعلومات عن المواقع مع جميع الكلمات الرئيسية والعناوين وهو عمل جيد جداً
جميع المعلومات عن خدماتنا على الموقع!
Personal Injury Legal: What’s The Only Thing
Nobody Has Discussed st petersburg personal injury attorney
20 Things Only The Most Devoted What Is The Best Online Shopping In Uk Fans Are Aware Of
Fender Liner Set Of 2 (Silas)
See What Bmw Car Key Cover Tricks The Celebs Are
Using bmw car key cover (https://www.longisland.com)
10 Things You Learned In Kindergarden That Will Help You Get Hiring Car Accident Lawyers car crash attorney in houston – Alfred,
15 Fun And Wacky Hobbies That’ll Make You More Successful At Cheap Online Electronics Shopping Uk Steam Smart Gruuv Racquetball Racquet
Специализированный магазин, предлагающий широкий выбор раковина для кухни квадратная для вашего интерьера.
A Good Rant About Unlock Car Service Car Lock Out Service (Telegra.Ph)
Reclaiming what’s yours shouldn’t be a hassle. That’s why our
methodology is straightforward and transparent.
Just provide us with some basic information, and we’ll handle everything else.
Don’t let a simple mistake prevent you from your hard-earned money.
We’re committed to help you recover every cent.
You’ll Be Unable To Guess Lost Car Key No Spare’s Tricks Lost Car Key No Spare
На сайте https://stimul57.ru/ сделайте заказ для того, чтобы приобрести дорожные знаки напрямую от производителя. К важным преимуществам компании относят то, что у нее собственное производство, практичные крепления, а на всю продукцию предоставляются гарантии 7 лет. В работе применяются материалы высокого качества, сертифицированные. Организуется доставка по всей России. Все товары полностью отвечают техническому регламенту, требованиям. На всех этапах производства проходят контроль качества.
It is difficult to tell by looking at a thing if it’s made of chanute asbestos attorney.
Neither can you smell or taste it. It is only found in the event that asbestos-containing products are drilled,
chipped or broken.
Our skillset in e-wallets and online transactions means we’re well-prepared
to tackle your QIWI wallet issues.
Be assured, we employ state-of-the-art techniques and stay updated with the latest recovery methods.
For those who’ve been victimized by unauthorized transactions or
errors that resulted in a loss of funds, you’ve got an ally
in us.
Washer Machine 10kg Tips To Relax Your Daily Lifethe One Washer Machine 10kg Trick That Every Person Should Know Washer Machine 10Kg
How Glass Repair Leeds Became The Top Trend In Social
Media upvc door repairs roundhay
The 10 Scariest Things About Sofa Sale Sofa Sale
QIWI wallet balance not adding up?
Let us take the lead in recovering what isrightfully yours.
Get in touch now and take the first step towards getting your money back.
Мы рекомендуем посетить веб-сайт ссылка.
Why You’re Failing At Coffee Pods Machine Coffee Brewing Machines
The Underrated Companies To Keep An Eye On In The Leather Couches For Sale Industry living room couch
10 Life Lessons We Can Learn From Veterans Disability Case veterans Disability attorney
На сайте https://www.prokinvest.ru/ вы сможете купить квартиру в СПб от застройщика ГК ПРОК, готовые квартиры в новостройках и в строящихся домах. Зайдите на сайт, ознакомьтесь с вариантами, условиями покупки, акциями застройщика и выберите для себя идеальный вариант.
How London Online Mobile Shopping Sites Is A Secret Life Secret Life
Of London Online Mobile Shopping Sites Led Matrix Module 64X32 Pixels
10 Rng Slots Tricks Experts Recommend Slot Bonuses
The Most Successful Real Doll Gurus Can Do 3
Things Sex doll tpe
Five Killer Quora Answers To Locksmith Car Key locksmith car key (https://nerdgaming.science/)
First of all, it should be clearly understood that these are uquest.net completely different concepts in geography. For example, when considering absolute height, it is precisely this that acts as the most important indicator, which is measured in meters, thereby determining the height of geographical objects above sea level.
10 Healthy Habits For Railroad Injuries Lawyer railroad accident Lawyer
near Me vancouver [Qooh.me]
What Is It That Makes Espresso Machine So Popular?
dual boiler
Why You Should Focus On Enhancing Mesothelioma Attorneys mesothelioma Compensation
The Most Effective Online Shopping Sites List For Clothes
Tips To Make A Difference In Your Life Cross Ferrari Brushed Black Pen
The Ultimate Glossary On Terms About ADHD Diagnosis Private UK Adhd assessment for adults private
Tipico ist eines der beliebtesten Online-Casinos in Deutschland. Spieler können eine Vielzahl von Casino-Spielen genießen und tolle Gewinne erzielen. Es kann jedoch vorkommen, dass es zu Problemen beim Spielen kommt oder Spieler unzufrieden sind mit ihrem Erlebnis im Online-Casino. In solchen Fällen bietet Tipico eine Geld-zurück-Garantie an, um die Zufriedenheit der Spieler sicherzustellen.
Die Geld-zurück-Garantie bei Tipico ist eine großartige Möglichkeit für Spieler, ihr Geld zurückzuerhalten, wenn sie unzufrieden sind mit dem Service oder den Spielen im Casino. Spieler können einen Antrag auf Rückerstattung stellen und erhalten ihr Geld innerhalb weniger Tage auf ihr Konto zurück.
Um eine Rückerstattung zu beantragen, müssen Spieler einfach den Kundenservice von Tipico kontaktieren und ihr Anliegen erklären. Der Kundenservice wird dann den Fall überprüfen und entscheiden, ob eine Rückerstattung möglich ist. In den meisten Fällen sind die Mitarbeiter von Tipico sehr kulant und bemüht, die Zufriedenheit der Spieler sicherzustellen.
Die Geld-zurück-Garantie von Tipico ist ein großer Vorteil für Spieler, die sich nicht sicher sind, ob sie im Casino spielen möchten. Mit dieser Garantie können sie beruhigt spielen und wissen, dass sie im Falle von Problemen ihr Geld zurückerhalten können.
Insgesamt ist die Geld-zurück-Garantie von Tipico eine großartige Möglichkeit für Spieler, sich vor Verlusten zu schützen und sicherzustellen, dass ihr Spielerlebnis im Online-Casino angenehm und fair ist. Wir empfehlen allen Spielern, diese Garantie in Anspruch zu nehmen, um ihr Spielerlebnis bei Tipico zu optimieren.
https://tipicocasino.one/
The Often Unknown Benefits Of American Fridge Freezer Uk american fridge freezers
– http://www.mishizhuti.Com –
Five Killer Quora Answers On Replacement Double Glazing Units Near Me replacement double Glazing units near me
Looking Into The Future What’s The Locksmith Car Industry Look Like In 10 Years?
cheapest locksmith for cars near Me
10 Tips For Getting The Most Value From Personal Injury Claim firms
As for relative height, it is usually measured in meters plitki.com. Moreover, it is worth noting that it is precisely this that will show the difference between the absolute height of geographical objects, as well as the height of the terrain. If the mountain has an absolute height of 2000 meters, but the surrounding area is located at an altitude of 1000 meters, then as for the comparative height of the mountain, it will be 1000 meters.
12 Companies Leading The Way In Truck Accident Attorney Near Me spotswood Truck accident Law firm [vimeo.Com]
14 Businesses Doing An Amazing Job At Slot Strategies Progressive slots
The For Outbuildings Tricks To Transform Your Life Best Freezers
http://prednisoned.online/# prednisone 30 mg daily
Your trust in us is our utmost importance. Therefore, we work with complete integrity and
dedication to your case.
Rest easy of seeing your funds returned with our expert assistance.
The Most Popular Avon Online Work That Gurus Use 3 Things stay at home mom jobs
The Evolution Of Window Repair Window repairs
Guide To Online Shopping Sites In United Kingdom: The Intermediate Guide Towards Online Shopping Sites In United Kingdom online shopping sites in united kingdom
7 Things About Car Locksmith You’ll Kick Yourself For Not
Knowing nearest locksmith for cars (yogicentral.science)
The Secret Life Of Double Bunk Beds With Storage Double Bed top bunk
What Is What CSGO Cases Have Butterfly Knives? Heck What
Is What CSGO Cases Have Butterfly Knives? Spectrum Case
Your faith in us is our top priority. That’s why we conduct our services with complete transparency and
commitment to your satisfaction.
Feel the comfort of seeing your funds returned with our specialized help.
The One Ford Car Key Replacement Trick Every Person Should Know replace ford key
Safety standards must be followed when working everbestnews.com with metal. Use protective equipment, use tools and equipment according to the rules so as not to encounter difficulties.
5 Killer Quora Answers To Starlight Princess 1000 Demo Slot starlight princess 1000 demo slot, Tamie,
What’s The Reason Nobody Is Interested In Find Accident Attorney
rear end accident attorney (Mallory)
Buy Nespresso Machine Tips That Will Change Your Life Nespresso Creatista Plus Coffee Machine
Five Reasons To Join An Online Compensation Mesothelioma Buyer And
5 Reasons You Shouldn’t mesothelioma compensation Self-employed
What’s The Job Market For Washington Birth Injury Attorney Professionals
Like? washington birth injury attorney
20 Myths About Best American Style Fridge Freezer: Busted American non plumbed Fridge Freezer
See What Kids Bunk Bed With Stairs Tricks The Celebs Are Using kids bunk bed with stairs; Stephany,
See What 9kg Washing Machines Uk Tricks The Celebs Are Using 9kg washing machines uk
How Much Can Double Glazed Window Leeds Experts
Make? Upvc Window Hinge Repairs Leeds (Shorl.Com)
15 Asbestos Settlement Benefits Everybody Should Be Able To asbestos Litigation
How To Survive Your Boss On Locksmiths Near Me For Car car
lock smith near me, Shelia,
Five Killer Quora Answers On Lost Keys Car lost Keys car
Customers receive products not only from the IT sector. They must provide krepezh.net high-quality services at every stage of interaction with cloud solutions.
What Is It That Makes Automatic Locksmith So Famous?
auto Locksmiths
The Secret Secrets Of Zanussi Under Counter Side By Side Fridge Freezer
what is the Best side by Side fridge to buy (peatix.com)
What’s The Current Job Market For Bentley Keys For Sale
Professionals? Bentley Keys For Sale
Confused about how to proceed with recovery of your QIWI wallet
funds? Our support team is on standby to help to guide you through the process
and answer any concerns you may encounter.
Choosing our company, you’re choosing a reliable ally in getting your money back.
10 Life Lessons We Can Learn From Robot Vacuum That Mops robot vacuum
and mop self empty; Quentin,
Are Double Glaze Repair Near Me The Best There Ever Was?
glazier
The Underrated Companies To In The Repairing Double Glazing Industry
Double Glazing Repairs
Boomerang Casino Avis
Das Boomerang Casino ist eine beliebte Online-GlГјcksspielseite, die fГјr ihr breites Angebot an Spielen und groГџzГјgigen Boni bekannt ist. In diesem Artikel werfen wir einen genaueren Blick darauf, was das Boomerang Casino zu bieten hat und welche Erfahrungen Spieler damit gemacht haben.
Das Boomerang Casino bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele, Live-Casino-Spiele und Jackpot-Slots. Die Spiele stammen von renommierten Softwareanbietern wie NetEnt, Microgaming, Play’n GO und vielen mehr. Dies garantiert eine hohe QualitГ¤t und Vielfalt der Spiele, die den Spielern zur VerfГјgung stehen.
Darüber hinaus bietet das Boomerang Casino großzügige Boni und Promotionen für seine Spieler an. Neue Spieler können sich über einen Willkommensbonus freuen, der zusätzliches Guthaben und Freispiele beinhaltet. Es gibt auch regelmäßige Aktionen und Turniere, bei denen die Spieler fantastische Preise gewinnen können.
Die Benutzerfreundlichkeit der Website und die Sicherheit der Spieler stehen im Boomerang Casino an erster Stelle. Die Website ist leicht zu navigieren und bietet eine Vielzahl von Zahlungsmöglichkeiten, um Ein- und Auszahlungen einfach und sicher zu machen. Darüber hinaus ist das Casino lizenziert und reguliert, was bedeutet, dass es strengen Vorschriften und Standards entsprechen muss, um fair und verantwortungsbewusst zu agieren.
Nach unserer Recherche und den Erfahrungen einiger Spieler scheint das Boomerang Casino eine gute Wahl fГјr alle GlГјcksspiel-Enthusiasten zu sein. Die groГџe Auswahl an Spielen, groГџzГјgigen Boni und die Sicherheit, die das Casino bietet, machen es zu einer attraktiven Option fГјr Spieler auf der Suche nach einem unterhaltsamen und sicheren Online-Casino-Erlebnis.
https://boomerangcasino.one/
20 Things You Should Be Asking About Door Fitter Leeds Before Purchasing It upvc door repair
meanwood [Margarito]
A person can set up the system on his own or sveto-copy.com contact an organization to use the feature, focusing on his product.
What Will CSGO Gambling Sites Be Like In 100 Years? cases (Securityholes.science)
How To Build Successful Self Empty Robot Vacuum And Mop Strategies From Home self-emptying Robot vacuum and mop
Five Killer Quora Answers To Tumble Dryers Heat Pump Vs Condenser sale
The 9 Things Your Parents Teach You About Window Doctor Near Me window doctor near me (smart-ant-hvwbvg.mystrikingly.com)
brand cialis scramble – forzest king penisole file
doxycycline 100mg: order doxycycline – doxycycline 100 mg
Who’s The Top Expert In The World On Best Robot Vacuum Self Emptying?
Vacuum And Mop
neurontin cost in singapore medicine neurontin buying neurontin online
9 Things Your Parents Teach You About Upvc Window Repairs upvc window repairs
Хотите посмотреть интересный фильм? Наш сайт то, что вам нужно. Мы собрали лучшую коллекцию фильмов всех жанров. У нас вы всегда найдете то, что вас интересует. Ищете https://vkinogo.net/multfilmy/? Vkinogo.net – популярный сайт, который вам понравится хорошим плеером, большим количеством фильмов и интерфейсом. Здесь постоянно добавляются новинки с замечательным переводом. Сайт без зависаний транслирует фильмы. Гарантируем отличный звук и качество. Смотрите смешные мультики и захватывающие фильмы на нашем портале всей семьей.
10 Beautiful Images Of Blown Double Glazing Repairs Near Me double glazed door handle
The No. Question That Everyone In 18 Wheeler Wreck Lawyers Must Know How To Answer
Berea 18 Wheeler Accident Lawyer
Quiz: How Much Do You Know About Window Repair Near? upvc window Repair Near Me
Washing Machines Beko Techniques To Simplify Your Daily Life Washing Machines
Beko Trick Every Person Should Be Able To washing machines beko (http://m.Vn.envylook.com/member/login.html?noMemberOrder=&returnUrl=http://valetinowiki.racing/wiki/11_Ways_To_Completely_Redesign_Your_Beko_Washing_Machine_New)
What’s The Current Job Market For Floor Vacuum Robot Professionals?
Floor Vacuum Robot (http://Www.Mazafakas.Com)
See What L30 Dreame Tricks The Celebs Are Utilizing L30 dreame
5 Killer Quora Answers To Walking Machine Under Desk walking machine under desk (Melody)
Five Things Everybody Gets Wrong In Regards To Shopping Online Uk Clothes 16Gb Ram Kit (https://Vimeo.Com/931521860)
The Reasons To Focus On Making Improvements Accident Attorney Lawyer accident attorney new jersey
(https://d.yoooa.com/accidentattorneyboca271292)
7 Tips To Make The Most Of Your Birth Defect Claim moorhead Birth Defect lawsuit – https://vimeo.com/707197926,
Why We Are In Love With Michael Kors Handbags
Black (And You Should Also!) michael Kors black handbag
Ищете захватывающие фильмы с интересным сюжетом? Наш сайт вам в этом поможет. Он предоставляет большой ассортимент фильмов разных жанров. Предлагаем вам уже сейчас окунуться в мир необыкновенных приключений. Ищете новые фильмы 2024 смотреть онлайн бесплатно? Skinogo.net – сайт, который порадует вас не только разнообразием фильмов, но и удобным интерфейсом, простотой применения, отличным плеером. Здесь вы сможете отыскать новинки с хорошим переводом и смотреть фильмы без зависаний. Мы гарантируем замечательное качество звука и изображения. Лучшее кино ждет именно вас!
The 10 Most Terrifying Things About Tread
Mills tread mills – forum.crimea-portal.info –
Could Treadmill Sale UK Be The Key To 2023’s Resolving? treadmill at home, Raymundo,
These Are The Most Common Mistakes People Make With Freezers Uk Residential Freezers
5 Killer Quora Answers To Situs Alternatif Gotogel Situs alternatif gotogel
Your trust in us is our top priority. That’s why we conduct our services with full integrity and
focus on results.
Experience the relief of seeing your funds returned with our expert assistance.
11 Ways To Completely Redesign Your Mesothelioma
Compensation Mesothelioma Law
You’ll Never Be Able To Figure Out This Double Glazing Repair Leeds’s
Secrets double Glazed window repairs
14 Businesses Doing A Great Job At Upvc Window Repairs window repairs near me
What’s The Job Market For Key Replacement Bmw Professionals?
key replacement bmw
What Is Online Shopping Uk Electronics And Why Is Everyone Speakin’ About
It? luxury bmw wristwatch bmw8000
The Reasons Car Accident Lawyer Is Harder Than You Imagine Austin Car Accident
Attorney (Adamrykala.Blog.Idnes.Cz)
Zet Casino: Ein seriöses Online-Casino
Das Glücksspiel im Internet gewinnt immer mehr an Beliebtheit, jedoch ist es wichtig, sich in einem sicheren und seriösen Online-Casino zu registrieren. Ein solches Casino ist Zet Casino, das eine Lizenz der Curacao eGaming besitzt und somit den strengen Richtlinien für Glücksspielanbieter entspricht.
Zet Casino bietet eine breite Auswahl an Spielen von renommierten Softwareanbietern wie NetEnt, Microgaming und Betsoft. Von Spielautomaten über Tischspiele bis hin zu Live-Casino-Spielen ist für jeden Geschmack etwas dabei. Die Spiele sind fair und werden regelmäßig auf ihre Zufälligkeit überprüft, um ein faires Spielerlebnis zu gewährleisten.
Ein weiterer Pluspunkt von Zet Casino ist der professionelle Kundenservice, der rund um die Uhr erreichbar ist. Egal, ob es um technische Probleme, Boni oder Auszahlungen geht, das Support-Team steht den Spielern kompetent und freundlich zur Seite.
Auch in Sachen Sicherheit und Datenschutz kann Zet Casino überzeugen. Die Webseite ist SSL-verschlüsselt, sodass persönliche Daten geschützt sind. Zudem bietet das Casino verschiedene sichere Zahlungsmethoden an, damit Ein- und Auszahlungen schnell und unkompliziert durchgeführt werden können.
Insgesamt kann man sagen, dass Zet Casino ein seriöser Anbieter ist, der den Spielern ein sicheres und unterhaltsames Spielerlebnis bietet. Wer auf der Suche nach einem zuverlässigen Online-Casino ist, sollte Zet Casino definitiv in Betracht ziehen.
https://zetcasino.one/
Рады вас приветствовать на BDA Logistic! Мы предлагаем комплексное решение для продавцов на маркетплэйсах и специализируемся на доставке товаров из Китая в РФ. Работаем с физическими и юридическими лицами. https://bdalogistic.ru – здесь вы сможете узнать, можно ли застраховать груз, как проверяется качество товара и как выполняется оплата. Также у вас есть возможность тут получить индивидуальное предложение и оставить заявку. Для этого в специальную форму на сайте необходимо ввести ваше имя и контактный номер телефона, после чего нажать на кнопку «Отправить».
What’s The Current Job Market For Double Glazing Repair Kit Professionals?
double Glazing repair
15 Pinterest Boards That Are The Best Of All Time About Railroad Injuries Lawyer yazoo city railroad injuries law firm
The Ultimate Cheat Sheet On Car Accident Compensation Claims car
injury lawyers near me, Candelaria,
Guide To Ghost 2 Immobiliser Fitting Near Me: The Intermediate Guide To Ghost
2 Immobiliser Fitting Near Me ghost 2 immobiliser fitting near
me [Clarice]
Undisputed Proof You Need Window Replacement replaced
Five American Fridge Freezer Uk Projects For Any Budget premium-quality Fridge freezer
See What Couch Sets For Sale Tricks The Celebs
Are Making Use Of Couch Set
Double Glazing Repairs Near Me Tools To Ease Your
Daily Lifethe One Double Glazing Repairs
Near Me Trick Every Individual Should Be Able To double glazing repairs near me
This Week’s Top Stories Concerning Skoda Key Programming skoda smart key (Leroy)
See What Designer Handbags Brands Tricks The Celebs Are Using designer handbags brands [Nichol]
Where To Research Designer Handbags On Sale Online designer handbags and purses
15 Undeniable Reasons To Love Property Accident Lawyers
injury lawyer chicago [https://frank-Ernstsen.technetbloggers.de]
Upvc Door Repairs Tips That Will Change Your Life upvc windows repairs near me
На сайте https://aprazer.com.ru почитайте информацию о популярной компании Aprazer, которая производит качественные и инновационные препараты. Они предназначены для потребителей различного сегмента, продаются по привлекательным расценкам. Производитель является сертифицированным, популярным. Все препараты вернут бесценное здоровье, подарят отличное самочувствие. Поставки организуются в различные города России. Качество препаратов проверяется на каждом этапе производства. Установлены доступные расценки.
15 Gifts For The Replacement Lost Car Keys Lover In Your Life lost car keys replacement cost uk (notabug.org)
ProstaBiome is a carefully crafted dietary supplement aimed at promoting prostate health. Bid farewell to restless nights and discomfort with ProstaBiome precise strategy for addressing prostate concerns. https://prostabiome-web.com/
10 Apps That Can Help You Control Your Best Slot Machines Multi-Line Slots
PotentStream is designed to address prostate health by targeting the toxic, hard water minerals that can create a dangerous buildup inside your urinary system It’s the only dropper that contains nine powerful natural ingredients that work in perfect synergy to keep your prostate healthy and mineral-free well into old age. https://potentstream-web.com/
10 Top Mobile Apps For Ghost Immobiliser Review Ghost immobiliser Installers near Me
Cacao Bliss is a powder form of unique raw cacao that can be used similarly to chocolate in powder form but comes with added benefits. It is designed to provide a rich and satisfying experience while delivering numerous health benefits. https://cacaobliss-web.com/
10 Unexpected Tommy Hilfiger Purse Bag Tips Tommy Hilfiger Bags Men
5 Killer Quora Answers On Treadmills UK Reviews treadmills uk reviews (genomicdata.hacettepe.edu.tr)
Вы находитесь в поисках достойного SEO специалиста? Алексей – настоящий профессионал, который успешно занимается продвижением сайтов. Он постоянно на связи и открыт к общению. Специалист гарантирует высокие результаты, бонусы для постоянных заказчиков и доступные цены. Требуется частный seo специалист? SEOalex.ru – сайт, где можете подробнее ознакомиться с проектами по SEO. Также здесь есть прекрасная возможность оставить заявку. Обращайтесь к Алексею, он знает свое дело на 100% и ответит с радостью на все ваши вопросы.
Five Killer Quora Answers On Birth Injury Attorney Washington County Birth Injury Attorney Washington county
Why People Don’t Care About Upvc Windows Repair Repair Upvc Window
20 Up-And-Comers To Watch In The Small Double Mattresses Industry double bed mattress included
Ten Things You Need To Know About Online Shopping Uk Groceries heavy duty garment
Rack with wheels (https://Vimeo.com/931287411)
Confused about how to start the recovery of your QIWI wallet funds?
Our customer support are available 24/7 to guide you through the steps
and respond to any queries you may encounter.
Choosing our company, you’re choosing a dependable helper
in reclaiming your assets.
http://zithromaxa.store/# zithromax pill
You Will Meet Your Fellow Case Key CSGO Enthusiasts. Steve Jobs Of The Case Key CSGO Industry operation Bravo case
The Top Reasons Why People Succeed In The Bean Cup Coffee Machine Industry Bean Cup Coffee Machines
The Top Michael Kors Bag On Sale Gurus Can Do 3 Things Michael Kors Bags On Sale
Жіночий блог MeatPortal пропонує корисну інформацію: рецепти, поради і лайфхаки. Цікавтеся на сайті https://meatportal.com.ua/ актуальним темами для жінок у зручному форматі.
This Week’s Best Stories Concerning Double Glazed Doors Near Me replacement units for Double glazing
10 Misconceptions Your Boss Shares Regarding Sectional Sofa Sale
couches For sale under $500
Asbestos Settlement Tools To Help You Manage Your Daily Life Asbestos Settlement Trick That Every
Person Must Learn asbestos settlement (Odell)
The People Nearest To Private Consultant Psychiatrist Tell You
Some Big Secrets private psychiatrist Leeds
See What Ford Car Key Replacement Tricks The Celebs Are Using ford car key Replacement
Das Boomerang Casino wurde von AskGamblers als eines der besten Online-Casinos ausgezeichnet. Mit einer groГџen Auswahl an Spielen, groГџzГјgigen Boni und professionellem Kundenservice hat sich das Casino einen erstklassigen Ruf erarbeitet.
Das Boomerang Casino bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele, Live-Casino-Spiele und mehr. Spieler kГ¶nnen aus einer Vielzahl von Titeln von fГјhrenden Softwareanbietern wГ¤hlen, darunter NetEnt, Microgaming, Play’n GO und viele andere.
Das Casino belohnt seine Spieler mit großzügigen Boni und Aktionen, darunter Willkommensboni, Einzahlungsboni, Freispiele und mehr. Spieler können auch an aufregenden Turnieren und Wettbewerben teilnehmen, um zusätzliche Preise zu gewinnen.
Der Kundenservice im Boomerang Casino ist rund um die Uhr verfГјgbar und bietet professionelle und schnelle UnterstГјtzung bei allen Fragen und Anliegen der Spieler. Das Casino legt groГџen Wert auf Kundenzufriedenheit und arbeitet hart daran, ein sicheres und faires Spielumfeld zu schaffen.
Mit seinem breiten Spielangebot, großzügigen Boni und erstklassigem Kundenservice ist das Boomerang Casino definitiv einen Besuch wert. Spieler können sich darauf verlassen, dass sie ein unterhaltsames und lohnendes Erlebnis haben werden, wenn sie sich für dieses erstklassige Online-Casino entscheiden.
https://boomerangcasino.one/
How Mobile Car Diagnostics Has Become The Most Sought-After Trend Of 2022 Diagnostic Test
3 Ways The Leeds Windows Influences Your Life double Glazing Door repairs
The Most Hilarious Complaints We’ve Heard About Best Shark Robot Vacuum Robot Vacuum For Stairs
A Brief History Of Folding Mobility Scooters
For Sale In 10 Milestones Best Folding Mobility Scooter Uk
Стремитесь улучшить свои английский? Окунитесь в увлекательный мир английского языка через кинофильмы и сериалы на английском. Насладитесь процессом изучения, погружаясь в захватывающие сюжеты и диалоги на языке оригинала. Подробнее тут https://serialy-na-angliiskom.pp.ua. Фильмы и сериалы на английском не только помогут вам расширить словарный запас, но и улучшат понимание английской языка на слух. Используйте просмотры сериалов на английском в качестве интересного метода освоения.
Are You Getting The Most From Your Michael Kors Pink Handbag?
michael kors Pink handbags
Desk Treadmill Foldable Tools To Streamline Your Daily Lifethe One Desk Treadmill Foldable
Trick That Should Be Used By Everyone Be Able To Desk Treadmill Foldable, Baskino.Cc,
Guide To Treadmill For Home: The Intermediate Guide To Treadmill For Home
treadmill for home (http://www.ecwusers.Com/?URL=spectr-sb116.ru/user/starquartz3/)
What Is The Reason? Birth Defect Lawyer Is Fast Increasing To Be The Hottest
Trend Of 2023? lawsuit
You’ll Never Guess This Mobile Automobile Locksmith Near
Me’s Tricks mobile automobile locksmith near Me
15 Inspiring Facts About Espresso Makers That You’d Never Been Educated About best Espresso maker
20 Resources That Will Make You Better At Largest Personal Injury Law
Firms In Us denver Personal injury lawyer (https://te.legra.ph/15-Startling-Facts-About-Personal-Injury-Lawyer-Assault-Youve-Never-Seen-09-03)
What Is The Reason Why Car Keys Replacement Cost Are So Helpful
When COVID-19 Is In Session duplicate car Keys
Guide To Upvc Windows Near Me: The Intermediate
Guide Towards Upvc Windows Near Me Upvc Windows Near Me
The People Who Are Closest To Home Espresso Machine Share Some Big Secrets Best Budget Espresso Machine
14 Companies Doing An Excellent Job At Accident Lawsuits Accident attorneys – http://cgi.members.interq.or.jp –
Why All The Fuss? Best Online Shopping Sites For Clothes?
Compact Folding Housekeeping Cart
Upvc Windows Near Me: 11 Things You’re Leaving Out upvc
windows repair near me (Carmela)
Responsible For The Online Shopping Websites For Clothes Budget?
10 Very Bad Ways To Invest Your Money Insulated Shaving Cream Bowl
娛樂城評價
Player線上娛樂城遊戲指南與評測
台灣最佳線上娛樂城遊戲的終極指南!我們提供專業評測,分析熱門老虎機、百家樂、棋牌及其他賭博遊戲。從遊戲規則、策略到選擇最佳娛樂城,我們全方位覆蓋,協助您更安全的遊玩。
Player如何評測:公正與專業的評分標準
在【Player娛樂城遊戲評測網】我們致力於為玩家提供最公正、最專業的娛樂城評測。我們的評測過程涵蓋多個關鍵領域,旨在確保玩家獲得可靠且全面的信息。以下是我們評測娛樂城的主要步驟:
娛樂城是什麼?
娛樂城是什麼?娛樂城是台灣對於線上賭場的特別稱呼,線上賭場分為幾種:現金版、信用版、手機娛樂城(娛樂城APP),一般來說,台灣人在稱娛樂城時,是指現金版線上賭場。
線上賭場在別的國家也有別的名稱,美國 – Casino, Gambling、中國 – 线上赌场,娱乐城、日本 – オンラインカジノ、越南 – Nhà cái。
娛樂城會被抓嗎?
在台灣,根據刑法第266條,不論是實體或線上賭博,參與賭博的行為可處最高5萬元罰金。而根據刑法第268條,為賭博提供場所並意圖營利的行為,可能面臨3年以下有期徒刑及最高9萬元罰金。一般賭客若被抓到,通常被視為輕微罪行,原則上不會被判處監禁。
信用版娛樂城是什麼?
信用版娛樂城是一種線上賭博平台,其中的賭博活動不是直接以現金進行交易,而是基於信用系統。在這種模式下,玩家在進行賭博時使用虛擬的信用點數或籌碼,這些點數或籌碼代表了一定的貨幣價值,但實際的金錢交易會在賭博活動結束後進行結算。
現金版娛樂城是什麼?
現金版娛樂城是一種線上博弈平台,其中玩家使用實際的金錢進行賭博活動。玩家需要先存入真實貨幣,這些資金轉化為平台上的遊戲籌碼或信用,用於參與各種賭場遊戲。當玩家贏得賭局時,他們可以將這些籌碼或信用兌換回現金。
娛樂城體驗金是什麼?
娛樂城體驗金是娛樂場所為新客戶提供的一種免費遊玩資金,允許玩家在不需要自己投入任何資金的情況下,可以進行各類遊戲的娛樂城試玩。這種體驗金的數額一般介於100元到1,000元之間,且對於如何使用這些體驗金以達到提款條件,各家娛樂城設有不同的規則。
A ticket is an application of requests balforum.net that is registered by support services. The ticket system is an advanced tool that automates the operation of various services. Solutions relevant for registration, as well as processing customer requests.
12 Facts About Malpractice Lawsuit That Will Make
You Look Smart Around The Cooler. Cooler mount dora malpractice Attorney
Why Is It Worth Hiring A Personal Injury Attorney Will Be Your Next Big Obsession Personal Injury
Lawyer Bronx; http://Www.4Rf.Com,
This Is The Good And Bad About Online Shopping Sites List For Clothes Jolie papier online shop uk Amazon
Economics of personal time. While the employees are cleaning poiskmonet.com, the customer can fully relax or assign additional work.
Say “Yes” To These 5 Accident Settlement Tips Vimeo.com
amoxicillin 500 mg capsule buy amoxicillin 500mg canada 875 mg amoxicillin cost
You’ll Never Guess This Treadmills For Home UK’s Tricks Treadmills for home
Why You Should Forget About Making Improvements To Your Nespresso Compatible Machine white nespresso coffee machine
A Peek Inside London Online Clothing Shopping Sites’s Secrets
Of London Online Clothing Shopping Sites Smart Bathroom Scale Fitbit
Washing Machine 9kg Capacity Tips To Relax Your Everyday Lifethe
Only Washing Machine 9kg Capacity Trick That Every Person Should Learn washing machine 9kg, Selina,
This Is The One Erb’s Palsy Lawyer Trick Every Person Should Learn Vimeo.com
A Step-By-Step Guide To Selecting Your Window Companies Leeds french door repair Leeds
tadacip online pharmacy
How To Design And Create Successful Window Repairs Tutorials
From Home Upvc Repairs
The Most Underrated Companies To Follow In The Repairing Upvc Windows
Industry upvc window repair
You’re About To Expand Your Top Table Freezer Options Freezer Options
12 Companies Are Leading The Way In Personal Injury Claim oak grove personal Injury law firm
Need Inspiration? Check Out Mobile Car Diagnostics Near
Me Uk bmw Diagnostics software
sildenafil how long to work
What Is It That Makes Mobile Auto Diagnostic Services Near
Me So Famous? solutions
Der Boom im Online Casino Gaming ist nicht aufzuhalten und immer mehr Spieler werden von der groГџen Auswahl an Spielen und den hohen Gewinnchancen angezogen. Besonders beliebt ist das Boomerang Casino, das mit seinem breiten Angebot an Spielen und attraktiven Bonusaktionen Гјberzeugt.
Das Boomerang Casino bietet eine Vielzahl von verschiedenen Spielen, darunter Slots, Tischspiele wie Roulette und Blackjack sowie Live Casino Spiele. Besonders hervorzuheben ist das Spiel “Miglior Gioco”, das als das beste Spiel im Casino gilt.
“Miglior Gioco” ist ein spannendes und unterhaltsames Spiel, das auf GlГјck und Strategie basiert. Die Spieler kГ¶nnen zwischen verschiedenen EinsГ¤tzen wГ¤hlen und haben die MГ¶glichkeit, hohe Gewinne zu erzielen. Das Spiel zeichnet sich durch eine einfache Bedienung und ansprechende Grafik aus, was es zu einem wahren Highlight im Boomerang Casino macht.
Neben dem Spiel “Miglior Gioco” bietet das Boomerang Casino auch eine Vielzahl von weiteren Spielen, die fГјr Abwechslung und Unterhaltung sorgen. Dank der benutzerfreundlichen Plattform kГ¶nnen die Spieler problemlos durch das Casino navigieren und ihre Lieblingsspiele finden.
Darüber hinaus lockt das Boomerang Casino mit großzügigen Bonusaktionen und Promotionen, die den Spielern zusätzliche Gewinnchancen bieten. Mit regelmäßigen Turnieren und Gewinnspielen haben die Spieler die Möglichkeit, attraktive Preise zu gewinnen und ihr Spielerlebnis noch spannender zu gestalten.
Insgesamt Гјberzeugt das Boomerang Casino mit einem umfangreichen Spielangebot, ansprechendem Design und lukrativen Bonusaktionen. Wer auf der Suche nach dem besten Spiel im Casino ist, sollte unbedingt “Miglior Gioco” im Boomerang Casino ausprobieren. Vielleicht wartet dort ja der nГ¤chste groГџe Gewinn!
https://boomerangcasino.one/
даркнет сливы тг
Даркнет и сливы в Телеграме
Даркнет – это компонент интернета, которая не индексируется стандартными поисковыми системами и требует особых программных средств для доступа. В даркнете существует обилие скрытых сайтов, где можно найти различные товары и услуги, в том числе и нелегальные.
Одним из популярных способов распространения информации в даркнете является использование мессенджера Телеграм. Телеграм предоставляет возможность создания закрытых каналов и чатов, где пользователи могут обмениваться информацией, в том числе и нелегальной.
Сливы информации в Телеграме – это способ распространения конфиденциальной информации, такой как украденные данные, базы данных, персональные сведения и другие материалы. Эти сливы могут включать в себя информацию о кредитных картах, паролях, персональных сообщениях и даже фотографиях.
Сливы в Телеграме могут быть опасными, так как они могут привести к утечке конфиденциальной информации и нанести ущерб репутации и финансовым интересам людей. Поэтому важно быть бдительным при обмене информацией в интернете и не доверять сомнительным источникам.
Вот кошельки с балансом у бота
What’s Holding Back The Double Glazed Near Me Industry?
double glazed window suppliers near Me (lovewiki.faith)
order zithromax over the counter: zithromax 500 mg for sale – zithromax tablets for sale
These Are The Most Common Mistakes People Make With Autowatch Ghost 2 Installers Near Me autowatch ghost installer
5 Killer Quora Answers To Treadmill Home Treadmill
10 Locations Where You Can Find Window Repair Near Upvc Window Repairs
сид фразы кошельков
Сид-фразы, или памятные фразы, представляют собой сумму слов, которая используется для составления или восстановления кошелька криптовалюты. Эти фразы обеспечивают возможность к вашим криптовалютным средствам, поэтому их секурное хранение и использование весьма важны для защиты вашего криптоимущества от утери и кражи.
Что такое сид-фразы кошельков криптовалют?
Сид-фразы являются набор случайными средствами сгенерированных слов, обычно от 12 до 24, которые предназначены для создания уникального ключа шифрования кошелька. Этот ключ используется для восстановления возможности доступа к вашему кошельку в случае его повреждения или утери. Сид-фразы обладают высокой защиты и шифруются, что делает их защищенными для хранения и передачи.
Зачем нужны сид-фразы?
Сид-фразы необходимы для обеспечения безопасности и доступности вашего криптоимущества. Они позволяют восстановить вход к кошельку в случае утери или повреждения физического устройства, на котором он хранится. Благодаря сид-фразам вы можете легко создавать резервные копии своего кошелька и хранить их в безопасном месте.
Как обеспечить безопасность сид-фраз кошельков?
Никогда не раскрывайте сид-фразой ни с кем. Сид-фраза является вашим ключом к кошельку, и ее раскрытие может влечь за собой утере вашего криптоимущества.
Храните сид-фразу в защищенном месте. Используйте физически безопасные места, такие как банковские ячейки или специализированные аппаратные кошельки, для хранения вашей сид-фразы.
Создавайте резервные копии сид-фразы. Регулярно создавайте резервные копии вашей сид-фразы и храните их в разных безопасных местах, чтобы обеспечить вход к вашему кошельку в случае утери или повреждения.
Используйте дополнительные меры безопасности. Включите другие методы защиты и двухфакторную аутентификацию для своего кошелька криптовалюты, чтобы обеспечить дополнительный уровень безопасности.
Заключение
Сид-фразы кошельков криптовалют являются ключевым элементом надежного хранения криптоимущества. Следуйте рекомендациям по безопасности, чтобы защитить свою сид-фразу и обеспечить безопасность своих криптовалютных средств.
The 10 Scariest Things About Mesothelioma Compensation Payouts
mesothelioma compensation payouts (olympia.fmbb.ru)
What’s The Job Market For Double Glazed Window Repairs Professionals Like?
Double glazed window Repairs
13 Things You Should Know About Mop Robot Vacuum That You Might Not Have Known rated
online viagra pharmacy reviews
This Week’s Top Stories About Double Glazing Shops Near
Me Double Glazing Shops Near Me replace
10 Inspiring Images About Uk Butt Plugs vibrating butt plugs (Emil)
20 Quotes That Will Help You Understand List Of Online Shopping Sites
Uk Athletic Shoes Men’s New Balance
To speed up the search according to the parameters required by the user politeconomics.org, the site page has a filter system that allows you to select tours based on the following indicators.
10 Things You Learned In Kindergarden That Will Help You With Door Fitter Leeds Composite Door Repairs Leeds
10 Times You’ll Have To Be Educated About Upvc Windows Repair
Upvc windows Repair near me (hikvisiondb.webcam)
brand cialis desire – forzest thief penisole complete
10 Inspiring Images About Mesothelioma Law Firm athens mesothelioma Law firm
Why Adding A Treadmills Under Desk To Your Life’s Activities
Will Make All The Impact treadmill under desk –
https://martinsen-dehn-2.mdwrite.net/,
What You Need To Do On This Sofa Sale Clearance Sofa Sleeper Couch
10 Healthy Sex Machines Price UK Habits fucking machine for Sale
The Ultimate Glossary Of Terms About CSGO Battle Case Cs20 Case
What Is Work From Home Jobs Online And Why Is Everyone Talking About It?
Advice
Guide To Fiat Keys: The Intermediate Guide For Fiat Keys
fiat 500X key fob
Selecting and comparing offers is quick and easy mmo5.info. The site allows you to set the issue according to an economical, optimal or luxury vacation option. For families, couples, or companies, you can choose your own tour options, where you can accurately calculate all the parameters and determine the cost of travel for everyone or for one person.
You’ll Be Unable To Guess London Online Clothing Shopping Sites’s Tricks london online clothing shopping sites – utahsyardsale.com,
The 10 Scariest Things About Double Glazing Repairs Near Me Double glazing Repairs near me
The People Nearest To Heatpump Dryer Share Some Big Secrets near
10 Apps That Can Help You Control Your Window Repairs Leeds
Upvc window hinge repair Leeds
Everything You Need To Know About Best Vibrator For Clit clitoral massagers (forum.Prolifeclinics.ro)
The 3 Greatest Moments In Car Unlock Service History
how to get keys out of locked car (https://lentz-thrane-3.thoughtlanes.net/10-quick-tips-for-locked-keys-in-car-how-to-open)
15 Lessons Your Boss Wishes You Knew About Double Glazing Repairs Near Me services
Is Your Company Responsible For The Heat Pump Tumble Dryer Reviews Budget?
12 Top Notch Ways To Spend Your Money heat pump technology
The 10 Most Terrifying Things About Birth Injury Attorneys birth injury attorneys – Jamey –
The Most Underrated Companies To Keep An Eye On In The Mesothelioma
Lawyer Industry north wildwood mesothelioma lawyer
Five Killer Quora Answers To Cheap Washing Machine 9kg cheap washing machine 9kg (https://Levelnickel0.bravejournal.net/quiz-how-much-do-you-know-about-washing-machine-9kg)
Five Killer Quora Answers On Secondary Double Glazing Near Me Double Glazing Near Me
How To Choose The Right Private Psychiatrist On The Internet private psychiatrist glasgow uk
Situs Gotogel Terpercaya Tools To Ease Your Daily
Life Situs Gotogel Terpercaya Trick That Everyone Should Know situs
gotogel terpercaya; Pearl,
The 10 Most Scariest Things About Which Beko Washing Machine
which beko washing machine
See What Appliances Online Beko Washing Machine Tricks The Celebs Are Utilizing appliances online Beko Washing machine
15 Gifts For The Leeds Window Repair Lover In Your Life repair double Glazing; thisglobe.com,
5 Killer Quora Answers To Replacement Double Glazing Units Near Me Replacement double glazing units near me
10 Facts About Bmw Key That Will Instantly Put You In Good Mood bmw keys
The Top Reasons Why People Succeed Within The Designer Bags Industry Designer Handbags On Sale Cheap
Bei Tipico mit PayPal einzahlen fГјr Casino und umbuchen
Tipico ist einer der beliebtesten Online-Glücksspielanbieter in Deutschland. Neben Sportwetten bietet Tipico auch eine Vielzahl von Casino-Spielen an, die die Spieler stundenlang unterhalten können. Um die Zahlungsvorgänge für die Spieler so einfach wie möglich zu gestalten, bietet Tipico die Möglichkeit, mit PayPal einzuzahlen und Geld umzubuchen.
PayPal ist eine der bekanntesten und sichersten Online-Zahlungsmethoden, die von Millionen von Menschen weltweit genutzt wird. Mit PayPal können die Spieler schnell und einfach Geld auf ihr Tipico-Konto einzahlen, um sofort mit dem Spielen im Casino zu beginnen. Das Einzahlen mit PayPal ist einfach und unkompliziert. Dazu muss der Spieler einfach die Zahlungsmethode auswählen, den gewünschten Betrag eingeben und die Transaktion abschließen. Das Geld wird sofort auf das Spielerkonto gutgeschrieben und kann für Casino-Spiele genutzt werden.
Aber nicht nur das Einzahlen, sondern auch das Umbuchen von Geld auf dem Tipico-Konto ist mit PayPal möglich. Wenn ein Spieler Gewinne erzielt hat und das Geld auf seinem Tipico-Konto umbuchen möchte, kann er dies ganz einfach mit PayPal tun. Dazu muss der Spieler einfach den gewünschten Betrag auswählen und die Umstellung bestätigen. Das Geld wird sofort auf das PayPal-Konto des Spielers überwiesen und kann von dort aus für andere Einkäufe oder Transaktionen genutzt werden.
Mit PayPal bei Tipico einzuzahlen und Geld umzubuchen ist also eine bequeme und sichere Möglichkeit, um das Spielerlebnis im Casino zu genießen. Spieler können sich auf schnelle und unkomplizierte Transaktionen verlassen und ihre Gewinne einfach verwalten. Wer also gerne im Tipico Casino spielt, sollte unbedingt die Möglichkeit nutzen, mit PayPal einzuzahlen und Geld umzubuchen.
https://tipicocasino.one/
10 Things Competitors Teach You About Mesothelioma Attorney urbana mesothelioma attorney
naoni.info
15 Weird Hobbies That’ll Make You Smarter At Robot Vacuums
For Pet Hair Smart
What’s The Reason Everyone Is Talking About Fiat 500 Key Replacement Cost Right Now
fiat replacement car keys (Stacey)
audio-kravec.com
You’ll Be Unable To Guess Double Glazed Units Near Me’s Secrets Double Glazed Units Near Me
Filtered Coffee Makers Tools To Streamline Your Life Everyday machine
drip (wayranks.com)
7 Secrets About Mobile Car Locksmith That Nobody Will Share With You
auto Car Locksmith
Ten Common Misconceptions About Replacement Window Handle That
Aren’t Always True upvc Replacement window handles
Unexpected Business Strategies Helped Double Glazed Units Near Me To Succeed replacement double glazed units near me
[marublog129.hateblo.Jp]
What To Say About Fridge Freezer Samsung To Your Mom Best integrated fridge Freezer 50/50 split frost free
What’s The Current Job Market For Coffee Machines Bean To Cup Professionals Like?
Coffee machines bean to cup
10 Apps To Help Manage Your Deep Sectional Sofa sectional With sleeper
Why Best Online Shopping Uk Clothes Is Harder Than You Imagine khaki Futon mattress
See What Replacement Sash Windows Tricks
The Celebs Are Using Replacement sash windows; http://fpcom.co.kr/bbs/board.php?bo_table=free&wr_id=4745,
You’ll Never Be Able To Figure Out This Online Shopping Uk Amazon’s
Benefits Vimeo.Com
15 Gifts For The Boat Accident Attorneys For Hire Lover In Your Life boat accident
attorneys panama city [https://gammelgaard-Burgess.technetbloggers.de]
You’ll Never Guess This Small Under The Desk Treadmill’s Tricks small under the desk treadmill
Five Killer Quora Answers To Double Glazing Repairs Luton double glazing repairs luton
7 Small Changes That Will Make A Huge Difference In Your Uk
Women’s Online Shopping Websites Tungsten Steel Burrs (vimeo.com)
Examples Of Online Products Tools To Enhance Your
Life Everyday Antique Drawer Handles
5 Cliches About Birth Defect Legal You Should Stay Clear Of doylestown birth defect Attorney
Motorcycle Accident Lawsuit Tips From The Most Effective In The Industry Motorcycle accidents
What’s The Current Job Market For Double Glazing Door Repairs Near Me Professionals?
Door repair
20 Things You Should Know About CS GO Cases Opening Revolver Case
Why You Should Concentrate On Improving Seo Website Optimization local Search optimisation
The Leading Reasons Why People Are Successful On The Motor
Vehicle Compensation Industry motor Vehicle Accidents
The 9 Things Your Parents Teach You About
Cheap Treadmill Desk cheap treadmill desk (Pearline)
What’s The Current Job Market For Floor Vacuum Robot Professionals Like?
floor vacuum robot (Arleen)
Where Will Mesothelioma Lawsuits Be One Year From
This Year? ellettsville mesothelioma lawyer (https://vimeo.com)
30 Inspirational Quotes About Robotic Shark Vacuum Cheap Robot Vacuum
10 Undeniable Reasons People Hate Car Locksmiths Near Me Carkey Locksmith
10 Unexpected Adhd Medication Tips Adhd adults medication
Are You Responsible For An Online Shopping Sites Budget? 12
Ways To Spend Your Money online shopping Sites for dress
15 Of The Best Documentaries On Bentley Key Fob Replacement bentley Continental key programming
7 Helpful Tips To Make The Most Out Of Your Window Repairs upvc Repair
Why Case Battle CS GO Is A Must At The Very Least
Once In Your Lifetime Counter Strike
Key For Bmw Tips To Relax Your Daily Lifethe
One Key For Bmw Trick That Should Be Used By Everyone Be Able To Key For Bmw
7 Things About Fair Trade Coffee Beans 1kg You’ll
Kick Yourself For Not Knowing ground
10 Things Everyone Hates About Audi A3 Keys Replacement Audi A3 Key
Хотите погрузиться в мир музыки и почувствовать себя истинной звездой? Предлагаем вам приобрести у нас профессиональное караоке. В своем оборудовании мы уверены. Стараемся наших покупателей радовать достойными ценами. Умеем вовремя определить ваши потребности и желания. Ищете магазин караоке? AudioLiga.ru – сайт, где у вас есть возможность узнать, почему нас выбирают. Наша главная цель – длительные дружеские отношения с клиентами и их рекомендации. Готовы ваш заказ оперативно доставить. Обращайтесь к нам, и вы получите информационную от нас поддержку.
https://doxycyclinea.online/# doxycycline 100mg price
20 Trailblazers Setting The Standard In CSGO Cases New clutch Case
10 Things People Get Wrong About The Word “Cerebral Palsy Claim” cerebral palsy lawyer (http://keystone-jacks.com)
A Rewind A Trip Back In Time: What People Talked About Central Locking Repairs
Near Me 20 Years Ago central locking repair near me
Zet Casino Freispiele ohne Einzahlung
Das Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen für die Spieler anbietet. Eine großartige Möglichkeit, das Casino kennenzulernen und gleichzeitig die Chance auf hohe Gewinne zu haben, sind die Freispiele ohne Einzahlung.
Was sind Freispiele ohne Einzahlung? Bei Freispielen ohne Einzahlung erhalten die Spieler die Möglichkeit, an ausgewählten Spielautomaten kostenlos zu spielen, ohne eigenes Geld einzahlen zu müssen. Die Gewinne, die mit diesen Freispielen erzielt werden, können in der Regel behalten werden, jedoch unterliegen sie meist bestimmten Umsatzbedingungen.
Das Zet Casino bietet sowohl neuen als auch bestehenden Spielern regelmäßig Freispiele ohne Einzahlung an. Diese können zum Beispiel als Belohnung für eine Einzahlung, bei der Anmeldung oder als Teil eines speziellen Angebots vergeben werden. Die Spieler haben die Möglichkeit, ihre Lieblingsspiele zu spielen und dabei echtes Geld zu gewinnen, ohne dabei ihr eigenes Geld riskieren zu müssen.
Um von den Freispielen ohne Einzahlung im Zet Casino zu profitieren, müssen die Spieler lediglich ein Konto erstellen und gegebenenfalls einen Bonuscode eingeben, der die Freispiele freischaltet. Anschließend können die Spieler die Freispiele nutzen und hoffentlich gute Gewinne erzielen.
Es ist jedoch wichtig zu beachten, dass die Gewinne aus den Freispielen in der Regel bestimmten Umsatzbedingungen unterliegen, bevor sie ausgezahlt werden können. Diese Bedingungen variieren je nach Angebot und sollten vor der Nutzung der Freispiele sorgfältig gelesen werden.
Freispiele ohne Einzahlung im Zet Casino bieten eine großartige Möglichkeit, das Online-Casino kennenzulernen und gleichzeitig die Chance auf hohe Gewinne zu haben. Spieler sollten regelmäßig die Promotionsseite des Casinos besuchen, um über aktuelle Angebote informiert zu sein und keine Freispielangebote zu verpassen.
https://zetcasino.one/
See What Double Glazing Units Near Me Tricks The Celebs Are Using double glazing units near me (http://fpcom.co.kr/bbs/Board.php?bo_table=free&wr_id=1210717)
biznesnewss.com
15 Pinterest Boards That Are The Best Of All Time About Window Glass
Replacement glaziers
auto-kar.net
Why We Our Love For Double Size Bunk Bed (And You Should Also!) double Bed with Bunk – https://www.longisland.com/,
Five Things You’re Not Sure About About Window Repair Near upvc Window repair near me
How You Can Use A Weekly Vehicle Diagnostics Project Can Change Your Life Diagnostics Mobile
Зайдите на сайт https://tyumen.dental/ в Тюмени, где вы сможете найти широкий спектр стоматологических услуг. Профессиональные специалисты, новейшее оборудование, доступные цены, удобное расположение. Вылечить кариес, исправить прикус, провести имплантацию или протезирование зубов, вылечить десны – все эти услуги оказывает наша клиника.
What NOT To Do When It Comes To The Double Glazing
Fitters Near Me Industry double Glazing Fitters
Nine Things That Your Parent Teach You About L30 Ultra Dreame l30 ultra dreame
Хотите смотреть фильмы онлайн в отличном качестве? Приглашаем вас на портал Киного! Здесь найдете множество интересных фильмов, которые помогут вам быстро поднять настроение после тяжелого дня. С помощью их вы забудете о насущных проблемах. Ищете комедии смотреть онлайн бесплатно? Kinogo-fil.net – сайт, который создан для любителей кино любых жанров. Интерфейс ресурса – удобный, имеется функция поиска. Больше не надо идти в кинотеатр и тратить деньги на покупку билетов. Вы можете абсолютно бесплатно смотреть у нас онлайн фильмы. Новинки кино ждут вас!
See What Best Buy Mobility Scooters Tricks The Celebs Are
Using Best buy mobility scooters
15 Fun And Wacky Hobbies That’ll Make You More Effective At Shopping Online Uk Clothes
Water Resistant Suv Cover
17 Reasons Not To Avoid Male Masturbators toys
10 Things People Get Wrong Concerning Car Lawyer Near Me Best Car Crash Attorney – https://Telegra.Ph/The-Most-Hilarious-Complaints-Weve-Seen-About-Car-Accident-Lawyer-Near-Me-05-04 –
Some Wisdom On Window Service London From A Five-Year-Old glazed
10 Things That Everyone Is Misinformed About Glazing Repairs Near
Me double glazing Repairs near Me
Why Is Window Repair Leeds So Effective In COVID-19?
upvc window handle repair leeds
15 Things You Don’t Know About Car Accident Compensation Claim car wreck lawyers near me;
Ines,
10 Facts About Mop Robot Vacuum That Make You Feel Instantly A Good Mood robot Vacuums
9 Things Your Parents Taught You About L30 Ultra Dreame L30 ultra dreame
Ten Apps To Help Control Your Upvc Sash Windows upvc windows repair near Me
How To Outsmart Your Boss On Mobility Scooter Batteries Near Me Buy Mobility Scooter Near Me
10 Facts About CSGO Battle Case That Will Instantly Set You In A Positive Mood winter
offensive weapon case (Dwayne)
See What Renault Trafic Key Replacement Tricks The Celebs
Are Utilizing renault Trafic key replacement (pediascape.science)
How To Recognize The Online Shopping Uk Electronics To Be Right For You Adidas Nmd_R2 Sneakers
What Experts In The Field Want You To Learn treadmill
at home (http://www.google.com/url?q=https://openinput80.bravejournal.net/15-reasons-you-shouldnt-overlook-treadmill-home-gym)
Five Killer Quora Answers On Patio Door Installers In London Patio door installers in London
buy doxycycline cheap doxycycline vibramycin doxycycline 100mg price
The Infrequently Known Benefits To Glass Repair Leeds upvc Window repair
You’ll Never Guess This Small Sectional Sofa’s Tricks Small Sectional Sofa
The Best Advice You Could Ever Receive About Rooms To Go Sofa Sale big Lots furniture sale couches
(http://vesti46.ru/)
What’s The Current Job Market For Online Shopping Uk Groceries Professionals?
online shopping uk groceries
Buying Online From Uk To Ireland Strategies That Will Change Your Life 15 Inch Safety Boots Black
How Much Do Small American Fridge Freezer Experts Make?
Cutting-edge fridge Freezer
5 Killer Quora Answers On Double Glazed Window Repairs
Near Me double Glazed window repairs near me
Responsible For A Double Glazing Repair Near Me Budget?
10 Ways To Waste Your Money double glazed windows cost (Shayne)
It’s Time To Upgrade Your Titrating Medication Options options
10 Misconceptions Your Boss Holds Concerning Starlight Princess 1000 Demo Slot Demo pragmatic starlight princess
See What Modern Sectional Sofa Tricks The
Celebs Are Utilizing Modern sectional sofa
Guide To Dangerous Drugs Lawyers: The Intermediate Guide To Dangerous Drugs Lawyers Dangerous Drugs Lawyers
9 . What Your Parents Taught You About Window Fixer London Window Fixer London
africanownews.com
The Little Known Benefits Of Injury Lawyer Shiloh Injury
Lawsuit (Vimeo.Com)
219news.com
10 Things That Your Family Teach You About Spare Keys Cut Spare keys
Why We Why We Mesothelioma Law Firm (And You Should,
Too!) Mesothelioma Compensation
Ten Things You Learned At Preschool That Can Help You In Auto Door Lock
Repair Near Me car door lock unlock
Where Are You Going To Find Double Glazing Supplies Near Me One
Year From In The Near Future? Replacement glass for double Glazing
15 Terms Everybody Within The Birth Defect Compensation Industry Should Know oakdale Birth Defect lawyer
20 Trailblazers Leading The Way In Titration For ADHD Local To Me
The Next Big Trend In The Mini Car Key Industry replacement Key for mini cooper
What’s The Current Job Market For Ghost Installations Professionals?
Ghost installation
This Is The Birth Defect Litigation Case Study You’ll Never Forget buffalo grove birth defect lawsuit
Das Tipico Casino ist eine beliebte Wahl unter den Online-Casino-Spielern, und dies aus gutem Grund. Das Casino ist Teil der bekannten Tipico-Gruppe, die bereits seit vielen Jahren fГјr ihre professionellen Dienstleistungen im Bereich Sportwetten bekannt ist. Nun haben sie ihr Angebot um ein hochwertiges Online-Casino erweitert, das Spieler aus der ganzen Welt begeistert.
Eine der Hauptattraktionen des Tipico Casinos sind die vielfГ¤ltigen und spannenden Spiele, die es zu bieten hat. Von klassischen Spielautomaten Гјber Roulette und Blackjack bis hin zu modernen Video-Slots – hier ist fГјr jeden Geschmack etwas dabei. Die Spiele stammen von renommierten Herstellern wie NetEnt, Microgaming und Play’n GO, was fГјr hohe QualitГ¤t und ein erstklassiges Spielerlebnis bГјrgt.
Auch in Sachen Sicherheit und Seriosität kann das Tipico Casino überzeugen. Das Casino verfügt über eine Lizenz der Malta Gaming Authority, einer der angesehensten Glücksspielbehörden der Welt. Dadurch wird sichergestellt, dass alle Spiele fair ablaufen und die persönlichen Daten der Spieler geschützt sind. Zudem arbeitet das Casino mit zuverlässigen Zahlungsdienstleistern zusammen, um sichere Transaktionen zu gewährleisten.
Ein weiterer Pluspunkt des Tipico Casinos ist der exzellente Kundenservice. Die Mitarbeiter stehen rund um die Uhr zur VerfГјgung, um den Spielern bei Fragen oder Problemen freundlich und kompetent weiterzuhelfen. Zudem bietet das Casino attraktive Bonusangebote fГјr neue und bestehende Spieler, um das Spielerlebnis noch spannender zu gestalten.
Alles in allem ist das Tipico Casino eine klare Empfehlung für alle, die auf der Suche nach einem seriösen und unterhaltsamen Online-Casino sind. Mit einer tollen Spielauswahl, einem hervorragenden Kundenservice und attraktiven Bonusangeboten überzeugt das Casino auf ganzer Linie. Wer also Lust auf erstklassige Casino-Unterhaltung hat, sollte das Tipico Casino definitiv einmal ausprobieren. Viel Spaß beim Spielen!
https://tipicocasino.one/
An experienced asbestos lawyer can help families of victims to receive compensation. There
are limitations on time which are referred to as statutes of limitations within which asbestos Claim victims can claim compensation.
Das Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von spannenden Spielen und aufregenden Aktionen für seine Spieler bietet. Eines der Highlights des Zet Casinos ist der No Deposit Bonus Code, der den Spielern die Möglichkeit bietet, ohne Einzahlung zu spielen und trotzdem echtes Geld zu gewinnen.
Der No Deposit Bonus Code für das Jahr 2021 bietet den Spielern eine großzügige Bonussumme, die sie nutzen können, um verschiedene Spiele im Casino auszuprobieren und ihr Glück zu testen. Dieser Bonus Code ist eine großartige Möglichkeit für neue Spieler, das Zet Casino kennenzulernen, ohne dabei ihr eigenes Geld riskieren zu müssen.
Um den No Deposit Bonus Code zu erhalten, müssen die Spieler lediglich ein Konto beim Zet Casino erstellen und den entsprechenden Bonus Code eingeben. Nachdem der Code eingegeben wurde, wird der Bonus automatisch gutgeschrieben und die Spieler können sofort mit dem Spielen beginnen.
Es ist wichtig zu beachten, dass der No Deposit Bonus Code bestimmten Umsatzbedingungen unterliegt, die erfüllt werden müssen, bevor die Gewinne aus dem Bonus ausgezahlt werden können. Die genauen Bedingungen können auf der Website des Zet Casinos eingesehen werden.
Insgesamt ist der No Deposit Bonus Code 2021 eine großartige Möglichkeit für Spieler, das Zet Casino kennenzulernen und ihre Lieblingsspiele zu genießen, ohne dabei ihr eigenes Geld zu riskieren. Wir empfehlen daher allen Casino-Liebhabern, sich diesen Bonus nicht entgehen zu lassen und das Zet Casino noch heute auszuprobieren. Viel Glück und viel Spaß beim Spielen!
https://zetcasino.one/
The Three Greatest Moments In Double Glazed Window Replacement Near
Me History double glazing Windows replacement
What’s The Job Market For Asbestos Attorney Professionals?
Asbestos Attorney
See What Railroad Injuries Claim Tricks The Celebs Are Utilizing Railroad Injuries
10 Best Mobile Apps For CSGO Cases To Invest In case falchion (Rosalind)
9 . What Your Parents Taught You About Upvc Windows Near Me upvc windows near Me
Ghost Alarm Installation Near Me Tools To Make Your Daily Life
Ghost Alarm Installation Near Me Trick Every Person Should Learn Near me
10 Things Everyone Makes Up Concerning Cost To Replace Windows Uk
fitters
Why Do So Many People Are Attracted To Private
Psychiatrists Near Me? Psychiatrist Private London
buy cheap zithromax online: azithromycin zithromax – zithromax antibiotic
10 Things We All Are Hateful About Mesothelioma Law Falcon Heights Mesothelioma Law Firm
What Experts From The Field Of Best Robot Vacuum Self Empty Want You To Know?
Best self emptying robot vacuum for pet Hair
8 Tips To Increase Your Examples Of Online Products Game Vimeo
The Three Greatest Moments In Self-Emptying Robot Vacuums History local
10 Wrong Answers To Common Online Shopping
Sites Questions: Do You Know The Correct Answers? Individual Loaf Pans
Five Killer Quora Answers On Standing Desk Treadmill Standing desk treadmill
9 . What Your Parents Taught You About Window Fixer London window fixer London
10 Ways To Create Your Personal Injury Lawyer Empire Vimeo
The 10 Most Terrifying Things About American Fridge Freezer Sale american fridge Freezer sale
Our knowledge in digital wallets and online transactions means we’re well-prepared to
tackle your QIWI wallet issues.
Rest assured, we utilize advanced techniques and keep up with
the latest recovery methods.
For those who’ve been hit with unauthorized transactions or issues that resulted in a loss
of funds, you’ve got an ally in us.
The 10 Most Scariest Things About Citroen Berlingo Van Key Replacement citroen key (Championsleage.Review)
Fiat Punto Key Replacement Explained In Fewer Than 140 Characters fiat 500 flip key repair
Upvc Windows Near Me Tools To Ease Your Daily Lifethe One Upvc Windows Near Me Technique Every Person Needs To
Learn upvc windows near me (Silas)
Are You Responsible For The 10kg Washing Machine Uk Budget?
12 Ways To Spend Your Money 10Kg washing machines uk
15 Reasons To Love Online Shopping Uk Cheap Industrial Grinding Plate – Evelyne –
What’s The Current Job Market For Link Daftar Gotogel Professionals?
link Daftar Gotogel, http://Www.valleyforge.org,
The 9 Things Your Parents Teach You About Auto
Accident Lawsuit Auto Accident lawsuit
11 “Faux Pas” Which Are Actually Okay To Use With Your Slot Reviews
Casino slot machines, Onlinenursing.duq.edu,
The Most Hilarious Complaints We’ve Heard About Upvc Window Repairs Window Repairs Near Me
14 Questions You Might Be Afraid To Ask About
Kimbo Extra Cream Espresso Beans 1kg specialty
12 Facts About Fleshlight That Will Get You Thinking About
The Water Cooler best feeling fleshlight sleeve (Alysa)
Lasixiv provides news and analysis for IT executives. We cover big data, IT strategy, cloud computing, security, mobile technology, infrastructure, software and more. https://lasixiv.com
10 Unquestionable Reasons People Hate Cheapest Rabbit Vibrators best rabbit Dildo
The 3 Most Significant Disasters In Best American Style Fridge Freezer The Best American Style Fridge Freezer’s
3 Biggest Disasters In History best american-style Fridge freezer
Птицеводство – интернет-магазин, который предлагает качественное инкубационное яйцо кур-бройлеров, уток и гусей, индейки от ведущих фабрик России и Европы. Для нас очень важна репутация среди постоянных покупателей. Готовы предоставить для вас все самое лучшее. https://incubatoreggs.ru – сайт, где есть возможность найти удобный поиск и каталог товаров. Также у вас есть возможность ознакомиться с отзывами о магазине и условиями доставки. Работаем мы с 9 до 20.00. Обращайтесь к нам уже сейчас. Разумные цены на инкубационное яйцо вас точно порадуют!
See What Replacement Sash Windows Tricks The Celebs Are Making Use Of Replacement Sash Windows
Хотите посмотреть онлайн аниме? Вам поможет в этом ANIME777. Изучите удивительный и захватывающий мир японской анимации. Ежедневно к нам присоединяются множество новых пользователей. Ищете сейлормун все сезоны скачать торрент? Anime777.ru – сайт, где вы найдете все, что вам необходимо. Можно в любое удобное время почитать комиксы манга. Вам предоставляется отличная возможность скачать аниме по прямой ссылке и через торрент совершено бесплатно. В прямом эфире можно увидеть трансляции игр и аниме. Посоветуйте наш проект ANIME777 своим знакомым и друзьям!
Worried about your QIWI wallet transactions?
Let us handle the stress in retrieving what isrightfully yours.
Contact us today and start the recovery journey.
14 Businesses Doing A Superb Job At Best Car Accident Lawyer Near Me Car Wreck Attorney
Tipico Casino Trick
Das Tipico Casino bietet eine Vielzahl von Spielen und Möglichkeiten, um Geld zu gewinnen. Doch gibt es auch Tricks, um seine Chancen auf einen Gewinn zu erhöhen? In diesem Artikel werden einige Tipps und Tricks vorgestellt, um beim Tipico Casino erfolgreich zu sein.
1. Nutzen Sie die Willkommensboni: Das Tipico Casino bietet neuen Spielern großzügige Willkommensboni an. Nutzen Sie diese Boni, um Ihr Spielkapital zu erhöhen und Ihre Chancen auf einen Gewinn zu maximieren.
2. Setzen Sie sich ein Budget: Bevor Sie mit dem Spielen beginnen, legen Sie sich ein Budget fest und halten Sie sich daran. So vermeiden Sie, mehr Geld zu verlieren als Sie sich leisten können.
3. Spielen Sie nur bei seriösen Anbietern: Achten Sie darauf, dass das Tipico Casino eine gültige Glücksspiellizenz besitzt und seine Spiele regelmäßig von unabhängigen Prüfinstituten überprüft werden. Nur so können Sie sicher sein, dass die Spiele fair und transparent sind.
4. Setzen Sie auf Spiele mit niedrigem Hausvorteil: Manche Spiele im Tipico Casino haben einen geringeren Hausvorteil als andere. Setzen Sie auf Spiele wie Blackjack oder Video Poker, um Ihre Gewinnchancen zu maximieren.
5. Nutzen Sie Strategien: Viele Spiele im Tipico Casino erfordern eine gewisse Strategie, um erfolgreich zu sein. Informieren Sie sich Гјber die besten Strategien fГјr Ihr Lieblingsspiel und setzen Sie diese gezielt ein.
Insgesamt gibt es also einige Tricks und Tipps, um beim Tipico Casino erfolgreich zu sein. Doch vergessen Sie nicht, dass Glücksspiel immer mit einem gewissen Risiko verbunden ist. Spielen Sie verantwortungsbewusst und setzen Sie niemals mehr Geld ein, als Sie sich leisten können zu verlieren. Viel Spaß und viel Erfolg im Tipico Casino!
https://tipicocasino.one/
Zet Casino Störung
Das beliebte Online-Casino Zet Casino hat in letzter Zeit mit einigen technischen Störungen zu kämpfen. Viele Spieler berichten von Verbindungsproblemen, langen Ladezeiten und sogar Abstürzen während des Spielens. Diese Störungen führen nicht nur zu Frustration bei den Spielern, sondern können auch dazu führen, dass diese ihr Vertrauen in das Casino verlieren und sich nach einer anderen Plattform umsehen.
Die Ursachen für diese Störungen sind bisher nicht bekannt. Es wird jedoch vermutet, dass sie auf technische Probleme mit den Servern oder der Software des Casinos zurückzuführen sind. Die Betreiber des Casinos arbeiten bereits daran, diese Probleme so schnell wie möglich zu beheben und die bestmögliche Spielerfahrung zu gewährleisten.
In der Zwischenzeit empfehlen wir den Spielern, geduldig zu sein und die offiziellen Social-Media-Kanäle des Casinos im Auge zu behalten, um über den aktuellen Stand der Störungen informiert zu bleiben. Es ist auch ratsam, regelmäßig die Webseite des Casinos zu besuchen, um Updates zu erhalten und mögliche Entschädigungen oder Sonderaktionen in Anspruch zu nehmen.
Trotz der aktuellen Probleme bleibt Zet Casino eine der beliebtesten Online-Glücksspielplattformen und bietet eine Vielzahl von Spielen und Bonusangeboten für seine Spieler. Wir hoffen, dass die Störungen bald behoben werden und die Spieler wieder ein reibungsloses Spielerlebnis genießen können.
https://zetcasino.one/
You’ll Never Guess This Double Glazed Replacement
Windows’s Tricks Double Glazed Replacement Windows
What’s The Current Job Market For Double Glazed Window Repairs Professionals?
Window Repair
Five CSGO Case Opening Battle Projects For Any Budget open Cs2 cases
Kantorbola adalah situs slot gacor terbaik di indonesia , kunjungi situs RTP kantor bola untuk mendapatkan informasi akurat slot dengan rtp diatas 95% . Kunjungi juga link alternatif kami di kantorbola77 dan kantorbola99 .
See What Examples Of Online Products Tricks The Celebs Are Using examples Of Online products
What’s The Job Market For Double Glazing Near Me Professionals
Like? Double Glazing Near Me
Unexpectedly lost your balance on your QIWI wallet?
We get it how stressful that can be.
No need to worry—we specializes in recovering your balance from QIWI wallets.
Boasting a high success rate, we’re positive we can assist you.
Drop us a message and let’s begin of restoring your
balance.
The 10 Most Scariest Things About Medical Malpractice Compensation medical malpractice lawsuit (http://line04.co.kr/white/board/goto.php?url=aHR0cHM6Ly9zbGltZXgzNjUuY29tL3dlaXJ0b25tZWRpY2FsbWFscHJhY3RpY2VsYXdzdWl0NjcwMjU5&encoded=1)
14 Questions You’re Afraid To Ask About Dreametech L30 Dreamy L30
Audi Car Keys Replacement Isn’t As Difficult As
You Think Replace audi Key
A Productive Rant Concerning Online Shop Online Shopping (http://Traff.Space)
You’ll Never Guess This Are Heat Pump Tumble Dryers Any
Good’s Secrets heat pump tumble dryer
Double Glazing Company Near Me: What Nobody Has Discussed Double glaze Units
The Expert Guide To Slot Variance Top Mobile Slots (Leewhan.Com)
The Ultimate Glossary For Terms Related To Tommy Hilfiger
And Bags sale bags tommy hilfiger
ремонт сотовых телефонов рядом
ремонт телефонов
срочный ремонт телефонов
10 Untrue Answers To Common Nespresso Compatible Machine Questions
Do You Know The Correct Answers? Krups Nespresso Coffee Machines
отремонтировать телефон
ремонт телефонов
9 Lessons Your Parents Taught You About Glass Replacement Windows glass replacement windows
The Most Successful Repairing Double Glazed Windows Gurus Do Three Things Double Glazing
How Assessing Mental Health Has Transformed My Life
The Better Mental Health online assessment uk
Are You Responsible For An Leeds Door And Window Budget?
12 Top Notch Ways To Spend Your Money repairs to double glazed Windows
17 Reasons Why You Shouldn’t Ignore Truck Accident Attorneys Truck Accidents
Guide To Glass Window Replacement: The Intermediate Guide To Glass Window Replacement glass window replacement (mariskamast.net)
10 Motor Vehicle Lawyers Hacks All Experts Recommend motor vehicle Accident attorneys
How Much Can Car Accidents Lawyer Near Me Experts Make? car Accidents attorneys near me
24-Hours To Improve CSGO Cases Explained chroma 2 case (Mandy)
The 10 Most Scariest Things About Pvc Window Repairs Window repairs
Get To Know The Steve Jobs Of The Glazing Repair Industry window doctor
The 10 Most Terrifying Things About Blown Double Glazing Repairs Near Me double Glazing repairs near me
What Is It That Makes Online Shopping Uk Sites
So Famous? Chevy Truck Bed Protection Covers (Kandice)
This Story Behind Cerebral Palsy Case Will Haunt You For
The Rest Of Your Life! Linwood cerebral palsy Attorney
Tipico Casino stellt für viele Glücksspielbegeisterte eine beliebte Anlaufstelle dar, um spannende Stunden voller Nervenkitzel und Spaß zu verbringen. Doch was ist los, wenn Tipico Casino plötzlich nicht mehr erreichbar ist? Warum geht Tipico Casino heute nicht?
Es gibt verschiedene Gründe, warum Tipico Casino heute nicht erreichbar sein könnte. Einer der häufigsten Gründe ist eine technische Störung aufseiten des Anbieters. In solchen Fällen arbeitet das Team von Tipico Casino mit Hochdruck daran, das Problem zu beheben und die Plattform so schnell wie möglich wieder online zu bringen.
Ein weiterer möglicher Grund für die Nichterreichbarkeit von Tipico Casino könnte sein, dass Wartungsarbeiten durchgeführt werden. In diesem Fall wird die Plattform vorübergehend offline genommen, um Verbesserungen und Updates vorzunehmen. Diese Maßnahmen dienen dazu, die Sicherheit und Stabilität des Casinos zu gewährleisten und das Spielerlebnis für die Nutzer zu optimieren.
Es kann auch vorkommen, dass Tipico Casino aufgrund von behördlichen Auflagen oder technischen Problemen anderer Dienstleister vorübergehend nicht erreichbar ist. In solchen Fällen ist es wichtig, Geduld zu haben und darauf zu vertrauen, dass das Unternehmen schnellstmöglich eine Lösung für das Problem findet.
Wenn Tipico Casino heute nicht erreichbar ist, können Spieler alternativ auf andere Online-Casinos ausweichen, um ihrem Glücksspiel nachzugehen. Es gibt viele seriöse Anbieter auf dem Markt, die ein breites Angebot an spannenden Spielen und attraktiven Boni bereithalten.
Insgesamt ist es wichtig zu verstehen, dass Ausfälle und Störungen im Online-Glücksspielbereich leider nicht ausgeschlossen sind. Trotzdem können Spieler darauf vertrauen, dass Unternehmen wie Tipico Casino alles daran setzen, um ihre Plattformen so zuverlässig und sicher wie möglich zu gestalten.
https://tipicocasino.one/
How Malpractice Claim Propelled To The Top Trend On Social Media Vimeo.Com
Five Things You Didn’t Know About Convertible Sectional Sofa
sectional sofa Sale
12 Facts About 9kg Washer To Refresh Your Eyes At The Cooler Water Cooler 9kg washers
Ist das Zet Casino sicher?
Das Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und attraktiven Bonusangeboten fГјr Spieler anbietet. Doch ist das Zet Casino auch sicher und vertrauenswГјrdig?
Um diese Frage zu beantworten, lohnt es sich, einen Blick auf die Lizenzierung und Regulierung des Casinos zu werfen. Das Zet Casino ist im Besitz einer Lizenz der Malta Gaming Authority, einer der angesehensten Glücksspielbehörden in der Branche. Dies bedeutet, dass das Casino strengen Vorschriften und Regularien folgen muss, um sicherzustellen, dass die Spieler geschützt sind und faire Spielbedingungen gewährleistet sind.
Darüber hinaus verwendet das Zet Casino eine SSL-Verschlüsselungstechnologie, um die persönlichen und finanziellen Daten der Spieler zu schützen. Diese Technologie sorgt dafür, dass alle Daten sicher und geschützt übertragen werden und nicht von Dritten abgefangen oder ausgelesen werden können.
Das Zet Casino arbeitet auch mit renommierten Spieleentwicklern zusammen, deren Spiele regelmäßig auf Fairness und Zufälligkeit überprüft werden. Dies garantiert den Spielern, dass sie eine faire Chance haben, zu gewinnen, und dass die Spiele nicht manipuliert sind.
Zusammenfassend lässt sich sagen, dass das Zet Casino als sicher und vertrauenswürdig eingestuft werden kann. Die Lizenzierung der Malta Gaming Authority, die Verwendung von SSL-Verschlüsselung und die Zusammenarbeit mit seriösen Spieleentwicklern sind starke Indikatoren für die Sicherheit des Casinos. Spieler können also beruhigt sein, wenn sie im Zet Casino spielen.
https://zetcasino.one/
9 . What Your Parents Teach You About Mop Robot
Vacuum mop robot vacuum (Emerson)
3 Ways The Car Diagnostics Near Me Will Influence Your Life engine diagnostic near me
Five Best Vibrating Panties Projects For Any Budget Panties vibrating
How Buy A Mobility Scooter Near Me Rose To Become The #1 Trend In Social Media places That buy mobility scooters near Me
15 Window Replacement Bloggers You Should Follow replacement windows
http://prednisoned.online/# prednisone generic cost
This History Behind Window Repair Near Will Haunt You For The Rest Of
Your Life! upvc window repair Near me
7 Things About Key Programmer You’ll Kick Yourself For Not Knowing auto
Хотите через торрент и совершенно бесплатно скачать игры на ПК? Вам поможет ТОРРЕНТ-ГЕЙМ. Необходимо скачать торрент. На любую игру имеется на ресурсе отдельная страница, на ней есть детальные описания и скриншоты прохождения. Ищете игры на двоих? Gametorrento.net – сайт, где есть возможность выбрать необходимый для вас продукт. Выбор невероятно огромен, обязательно найдете то, что вас заинтересует. Вас ожидает увлекательный виртуальный мир. Предлагаем вам расслабиться и хорошо провести свое время. Приятного вам игрового процесса!
Say “Yes” To These 5 Top 10 Online Shopping Sites In Uk For Clothes Tips Professional Juice Extractor
4-Wheeled Scooter 10 Things I Wish I’d Known Earlier Scooters 4 Wheels
What’s The Current Job Market For Bmw Series 1 Key Professionals Like?
bmw series 1 key
5 Laws Anybody Working In Pvc Window Repairs Should Know upvc repair (Aundrea)
10 Birth Injury Lawsuit Tips All Experts Recommend Vimeo.com
An In-Depth Look Back The Conversations People Had About 18-Wheeler Lawyer 20
Years Ago Stillwater 18 Wheeler Accident Lawsuit (Vimeo.Com)
zithromax for sale usa buy azithromycin zithromax zithromax online usa
What Will Replacement Windows Leeds Be Like In 100 Years?
Upvc Door Repairs Meanwood
Why Adding Amazon Uk Online Shopping Clothes To Your Life Will Make All The Different
Tan Masking Tape 60 Yards (https://vimeo.com/932330639)
This Is The Advanced Guide To Best Side By Side Fridge Freezer
narrow side By side refrigerator
What’s The Job Market For Double Glazed Window Repairs Professionals Like?
Double Glazed Window Repairs
Are You Responsible For A Double Glazed Repairs Near
Me Budget? 10 Terrible Ways To Spend Your Money repairing double glazing
How To Solve Issues Related To Heat Pump Tumble Dryers Are Heat Pump Tumble Dryers Any Good
20 Trailblazers Lead The Way In CSGO New Case prisma 2 case
Ten Things You Should Never Share On Twitter best bunk beds for kids (adroit-marigold-fdjgf0.mystrikingly.com)
What Door Repairs Near Me Experts Would Like You To Learn upvc door repairs near me
Mesothelioma Lawyer: The Ugly Facts About Mesothelioma Lawyer lakeway mesothelioma lawyer
How To Become A Prosperous Best 18 Wheeler Accident Lawyer When You’re Not Business-Savvy Bell 18 Wheeler Accident Attorney
10 Glass Repair Leeds Tricks All Experts Recommend upvc Window repair
pronovosti.org
365newss.net
Guide To Double Glazed Window Near Me: The Intermediate
Guide In Double Glazed Window Near Me double glazed window near me (Latosha)
10 Things Everybody Has To Say About Fridges For Sale cheap fridges for sale (Howard)
15 Reasons To Not Ignore Best 18 Wheeler Accident Attorneys fort worth 18 Wheeler accident lawsuit
10 Wrong Answers For Common Cerebral Palsy Attorney Questions: Do You Know The Right Answers?
cerebral palsy attorneys – Charissa –
10 Things People Hate About Online Shopping Sites For Clothes famous online shopping sites for clothes
It’s Time To Upgrade Your Become Avon Representative Options how to become an avon rep –
Lesli –
Five Best Robot Vacuum Lessons From The Pros best Robot vacuum Mop Combo
How To Identify The Right Upvc Windows And Doors Near Me For
You Upvc Windows Repairs Near Me
Three Reasons To Identify Why Your L30 Ultra Dreame Isn’t Working (And Solutions To
Resolve It) dreame l30 Ultra
Ten Things You’ve Learned In Kindergarden They’ll Help You Understand
Upvc Window Repairs Upvc repair
Nine Things That Your Parent Taught You About Double Glazed
Windows Near Me double glazed windows near me (http://leewhan.com/bbs/board.php?bo_table=free&wr_id=3374255)
How To Create An Awesome Instagram Video About Self Emptying Robot Vacuum mopping robot vacuum cleaner
Желаете смотреть фильмы и сериалы онлайн в отменном качестве? Портал kinogoby.zone в этом вам поможет. Здесь постоянно есть свежие новинки. Фильмы достойные, смотреть их можно абсолютно бесплатно, не выходя из дома. Поиск позволяет найти то, что вы желаете. Ищете https://kinogoby.zone/genre/melodrama/? Kinogoby.zone – сайт, который выделяется среди остальных. Портал предоставляет доступ к множеству разнообразных фильмов. Создатели ресурса сделали удобный интерфейс для зрителей. Выбирайте прямо сейчас кино и наслаждайтесь. Смотрите с удовольствием!
Double Glazing Companies Near Me Techniques To Simplify Your Daily Life Double Glazing Companies Near Me Technique Every
Person Needs To Know Double Glazing Companies Near Me
20 Things You Need To Be Educated About Rooms To Go Sofa Sale
couch loveseat set (Conrad)
10 Life Lessons We Can Learn From Railroad Injuries Settlement railroad Always wins lawsuit
A Time-Travelling Journey A Trip Back In Time: What People Talked About Asbestos Lawsuit 20
Years Ago asbestos attorney
The Most Hilarious Complaints We’ve Been Hearing About Upvc Window
Repairs Window Repairs Near Me
What’s The Job Market For Birth Injury Attorney Boulder Professionals?
Birth Injury Attorney Boulder
Are CSGO Case Opening Battle Just As Important
As Everyone Says? skins
The Worst Advice We’ve Ever Been Given About
Robot Vacuum And Mop Bagless Robot Vacuum
The 10 Most Infuriating Bunk Bed Price-Related FAILS Of All
Time Could Have Been Prevented bunk beds for kids sale, telegra.ph,
The Companies That Are The Least Well-Known To
Follow In The Mesothelioma Legal Industry Mesothelioma Case
What’s The Current Job Market For Robot Self Emptying Vacuum
Professionals Like? self emptying vacuum (http://vn.easypanme.com/board/bbs/board.Php?bo_table=master&wr_id=1521449)
The Companies That Are The Least Well-Known To In The Double
Glazing Suppliers Near Me Industry Double glazinf
Das Meinsino Casino Tipico ist eine beliebte Online-Spielothek, die Spielern eine Vielzahl von Unterhaltungsoptionen bietet. Mit einer breiten Palette von Spielen, großzügigen Boni und einer benutzerfreundlichen Benutzeroberfläche hat das Meinsino Casino Tipico viel zu bieten.
Eines der herausragenden Merkmale des Meinsino Casino Tipico ist die Vielfalt der Spiele, die es seinen Kunden anbietet. Von klassischen Tischspielen wie Blackjack und Roulette bis hin zu aufregenden Spielautomaten und Live-Casino-Spielen – es gibt fГјr jeden etwas dabei. Die Spiele sind von fГјhrenden Softwareentwicklern wie NetEnt, Microgaming und Evolution Gaming bereitgestellt, was fГјr QualitГ¤t und Fairness steht.
Ein weiterer großer Anreiz für Spieler, das Meinsino Casino Tipico zu besuchen, sind die großzügigen Boni und Promotionen, die regelmäßig angeboten werden. Neue Spieler können einen Willkommensbonus erhalten, während Stammkunden von wöchentlichen Aktionen und Belohnungen profitieren können. Diese Boni sind eine großartige Möglichkeit, das Spielerlebnis zu verbessern und die Chancen auf Gewinne zu erhöhen.
Die Benutzeroberfläche des Meinsino Casino Tipico ist einfach zu bedienen und bietet eine nahtlose Spielerfahrung. Die Website ist gut strukturiert und intuitiv gestaltet, was es selbst Neulingen leicht macht, sich zurechtzufinden. Zudem ist das Casino mobiloptimiert, so dass Spieler auch unterwegs ihre Lieblingsspiele genießen können.
Insgesamt hat das Meinsino Casino Tipico viel zu bieten und ist definitiv einen Besuch wert. Mit einer Vielzahl von Spielen, großzügigen Boni und einer benutzerfreundlichen Benutzeroberfläche ist dieses Online-Casino eine gute Wahl für Spieler, die nach einer unterhaltsamen und lohnenden Spielerfahrung suchen.
https://tipicocasino.one/
10 Facts About Online Shop That Can Instantly Put You In An Upbeat
Mood Air Line Conditioning Equipment
“A Guide To Washing Machine 10kg In 2023 Washing machines 10Kg
Интернет-магазин, где можно найти черная раковина над стиральной машиной для любого интерьера и бюджета.
Zet Casino ist ein aufstrebendes Online-Casino, das Spielern eine breite Auswahl an Spielen und attraktiven Boni bietet. Das Casino verfГјgt auch Гјber ein Partnerprogramm, das als Zet Casino Affiliates bekannt ist.
Das Zet Casino Affiliates-Programm bietet Website-Betreibern die Möglichkeit, mit dem Casino zusammenzuarbeiten und Provisionen für die Vermittlung von Spielern zu verdienen. Als Affiliate von Zet Casino erhalten Sie Zugang zu einer Vielzahl von Marketingmaterialien und Tools, um die Promotion des Casinos zu unterstützen. Dies beinhaltet personalisierte Tracking-Links, Bannerwerbung und andere Werbemittel.
Das Partnerprogramm von Zet Casino bietet attraktive Provisionssätze und flexible Zahlungsmethoden, um sicherzustellen, dass Affiliates angemessen für ihre Bemühungen belohnt werden. Darüber hinaus bietet das Programm eine detaillierte Berichterstattung und Analysetools, um Affiliates dabei zu unterstützen, ihre Kampagnen zu optimieren und ihren Erfolg zu steigern.
Wenn Sie eine Website im Bereich Glücksspiel betreiben und daran interessiert sind, mit einem seriösen und profitablen Casino zusammenzuarbeiten, dann könnte das Zet Casino Affiliates-Programm genau das Richtige für Sie sein. Melden Sie sich noch heute an und profitieren Sie von den zahlreichen Vorteilen, die das Partnerprogramm zu bieten hat.
Insgesamt ist das Zet Casino Affiliates-Programm eine fantastische Möglichkeit, um mit dem boomenden Online-Glücksspielmarkt Geld zu verdienen. Mit einer Vielzahl von Spielen, großzügigen Boni und einem engagierten Affiliate-Team, kann man sicher sein, dass man mit Zet Casino eine erfolgreiche Partnerschaft eingehen wird.
https://zetcasino.one/
14 Misconceptions Commonly Held About Locksmith Car Key locksmith car key maker near me
7 Small Changes You Can Make That’ll Make An Enormous Difference To Your Male Masturbator Mens masterbator (bulangiul.net)
7 Helpful Tricks To Making The Most Of Your Glazing Repairs Near Me
double glazing near me, telegra.Ph,
9 Lessons Your Parents Teach You About Replace Upvc Window Handle replace Upvc Window Handle
The 10 Most Scariest Things About A+++ Tumble Dryer Heat Pump A+++ Tumble Dryer Heat Pump
10 Healthy Glass Repair Luton Habits Window replacement
See What Repair Upvc Windows Tricks The Celebs Are Using Repair Upvc Windows
The 10 Most Terrifying Things About Coffee Machine
Coffee Beans coffee machine coffee beans
20 Trailblazers Lead The Way In Designer Bags designer handbags cheap
10 Healthy Part Time Work From Home Jobs Habits Work from home Employment
Window Repairs Tools To Improve Your Daily Lifethe One Window Repairs
Trick That Everybody Should Know window repair
Where Will 10kg Washing Machine Be 1 Year From In The Near Future?
best Price 10kg washing machine
The 12 Worst Types Slot Software Users You Follow On Twitter video poker slots –
k-vsa.org,
Refridgerator Techniques To Simplify Your Daily Life
Refridgerator Trick That Every Person Must Be Able To fridge
You Can Explain Buy Used Mobility Scooter To Your Mom Best Buy Electric Scooters For Sale (https://Telegra.Ph/What-Is-The-Best-4-Wheel-Mobility-Scooter-Tips-That-Can-Change-Your-Life-04-21)
The 10 Most Scariest Things About Buy Beko Washing Machine Beko Washing Machine
How Auto Accident Attorneys Near Me Influenced My Life
For The Better automobile Accident lawyers (https://offers.sidex.ru/)
20 Myths About Panty Vibrators Sex Toy: Dispelled best women vibrators (latexcandle94.werite.net)
The Reasons All CSGO Skins Has Become The Obsession Of Everyone In 2023 gamma 2 case (Adriene)
Why All The Fuss? Designer Handbags To Sell? Designer handbags manchester
See What Double Glazing Units Near Me Tricks The Celebs Are
Using double Glazing Units near me – gwwa.yodev.net –
See What 1kg Coffee Beans Price Tricks The Celebs Are Using 1Kg Coffee Beans Price
A Provocative Rant About Mental Health UK private mental health assessment cost uk
You’ll Never Guess This Link Alternatif Gotogel’s Tricks Link alternatif gotogel
Why The Biggest “Myths” About Car Locks Smith Could Be A Lie Keys
Auto Accident Law: What’s The Only Thing Nobody Is Talking About reynoldsburg auto accident
attorney (Vimeo.com)
A Step-By-Step Guide For Choosing Your Door Repairs Near Me upvc door repairs near
me (peatix.com)
What Is Injury Lawyer And Why Is Everyone Speakin’ About It?
Angleton Injury Lawsuit
How To Outsmart Your Boss Car Key Cover Fiat 500 Fiat key Programmer
You’ll Never Be Able To Figure Out This Espresso Coffee Maker’s Tricks espresso coffee maker
10 Things You’ll Need To Be Educated About Used Mobility Scooters Near Me Electric mobility scooters for sale near me
Tipico Casino Chips Blockiert: Was ist zu tun?
Wenn Sie ein Spieler im Tipico Casino sind und plötzlich feststellen, dass Ihre Casino Chips blockiert sind, kann das sehr frustrierend sein. Doch keine Sorge, es gibt einige Schritte, die Sie unternehmen können, um das Problem zu lösen.
Zunächst einmal sollten Sie überprüfen, ob Sie möglicherweise die Bonusbedingungen des Casinos nicht erfüllt haben. Oftmals werden Casino Chips blockiert, wenn Sie versuchen, Gewinne aus einem Bonus ohne Einzahlung abzuheben, ohne die entsprechenden Umsatzanforderungen erfüllt zu haben.
In diesem Fall empfehlen wir Ihnen, Kontakt mit dem Kundensupport von Tipico aufzunehmen. Die Mitarbeiter können Ihnen weiterhelfen und das Problem genauer überprüfen. Möglicherweise müssen Sie zusätzliche Dokumente zur Verifizierung einreichen, um die Blockierung aufzuheben.
Es ist auch möglich, dass Ihre Casino Chips aus Sicherheitsgründen blockiert wurden. Dies kann beispielsweise der Fall sein, wenn ungewöhnliche Aktivitäten auf Ihrem Konto festgestellt werden. In einem solchen Fall ist es wichtig, sich mit dem Kundensupport in Verbindung zu setzen und alle erforderlichen Schritte zur Verifizierung durchzuführen.
Zusammenfassend lässt sich sagen, dass eine Blockierung von Casino Chips im Tipico Casino ärgerlich sein kann, aber in den meisten Fällen gibt es eine Lösung. Nehmen Sie Kontakt mit dem Kundensupport auf, um das Problem zu klären und Ihre Chips freizuschalten.
https://tipicocasino.one/
What Is Washing Machine 9kg Uk? History Of Washing Machine 9kg Uk Best
9kg washing machines [84.Glawandius.com]
Our skillset in cyber finance and electronic payments means we’re well-prepared
to tackle your QIWI wallet issues.
Be assured, we utilize advanced techniques and keep up with the latest fraud prevention strategies.
If you’ve been affected by unauthorized transactions or technical glitches that caused a loss of funds, we’re here to help.
10 Life Lessons We Can Learn From Amazon Online
Grocery Shopping Uk Kayak Accessory Replacement
QIWI wallet balance not adding up?
Let us handle the stress in retrieving what isrightfully yours.
Contact us today and begin reclaiming your funds.
Why Adult Sexdoll Is Your Next Big Obsession? Sex Dolls Review
Bei Zet Casino handelt es sich um einen beliebten Online-Glücksspielanbieter, der seinen Spielern eine Vielzahl von spannenden Spielen und lukrativen Bonusangeboten bietet. Einer dieser Boni ist der Zet Casino Bonus Code ohne Einzahlung, der den Spielern die Möglichkeit gibt, kostenloses Bonusguthaben zu erhalten, ohne dafür eine Einzahlung tätigen zu müssen.
Um diesen Bonus zu erhalten, müssen Spieler lediglich den entsprechenden Bonus Code bei der Registrierung ihres Kontos eingeben. Anschließend wird das Bonusguthaben automatisch auf ihr Konto gutgeschrieben und sie können damit die verschiedenen Spiele im Casino ausprobieren, ohne eigenes Geld einzahlen zu müssen.
Der Zet Casino Bonus Code ohne Einzahlung ist eine großartige Möglichkeit für Spieler, das Casino und seine Spiele risikofrei kennenzulernen und dabei echte Gewinne zu erzielen. Allerdings sollten Spieler beachten, dass diese Art von Bonus oft mit bestimmten Umsatzbedingungen verbunden ist, die sie erfüllen müssen, bevor sie sich ihre Gewinne auszahlen lassen können.
Insgesamt ist der Zet Casino Bonus Code ohne Einzahlung eine attraktive Option für Spieler, die nach einem risikofreien Einstieg in die Welt des Online-Glücksspiels suchen. Mit diesem Bonus können Spieler die verschiedenen Spiele im Casino ausprobieren, ohne dabei ihr eigenes Geld aufs Spiel zu setzen. Wer sein Glück versuchen möchte, sollte diesen Bonus auf jeden Fall in Anspruch nehmen und die spannenden Spiele im Zet Casino entdecken.
https://zetcasino.one/
It’s The Ugly Truth About Window Repair Near Me
upvc windows repair near me (tujuan.grogol.us)
15 Bizarre Hobbies That’ll Make You More Successful At Slot Starlight Princess Akun demo Slot starlight princess
Магазин с широким выбором накладные раковины cersanit для вашей ванной комнаты.
What You Can Do To Get More From Your Upvc Repairs
Near Me upvc windows repair near me (alt1.toolbarqueries.google.rs)
The No. 1 Question Anyone Working In Birth Defect Litigation Should Be Able Answer birth defect law firm
You’ll Never Guess This Window Replacement Companies’s Tricks window Replacement Companies
Double Glazed Window Repair Tips That Will Change Your Life window Repairs Near me
Guide To Bmw Replacement Key Cost: The Intermediate Guide To Bmw Replacement Key Cost bmw replacement key cost
ремонт телефонов рядом
Glass Window Repair Isn’t As Difficult As You Think nearby
The Ultimate Guide To Replace Window Handle Replacement Window handle
A Good Rant About Freestanding Freezer Modern Freezers
24-Hours To Improve Vehicle Door Lock Repair Car Central Locking Repair Near Me
Guide To Upvc Windows Repair: The Intermediate Guide Towards Upvc Windows Repair pvc
Wedstraunt has the latest news in the restaurant industry, covering topics like consumer trends, technology, marketing and branding, operations, mergers https://wedstraunt.com
The Most Worst Nightmare About Auto Accident Law Firm Come To Life Michigan auto accident lawyers (http://www.whoohoo.co.uk)
The 10 Most Scariest Things About Mesothelioma Victims Compensation mesothelioma
victims compensation, Skye,
Online Clothing Sites Uk: The History Of Online Clothing Sites Uk In 10
Milestones Cycling Cleaning Tools
ремонт телефонов в москве
What’s The Job Market For Upvc Repairs Near Me
Professionals Like? Upvc Repairs Near Me
7 Simple Tips To Totally Rocking Your Double Glazing Repairs Near Me Double Glazing near me
It Is Also A Guide To Truck Accident Lawsuit In 2022 lewisville truck accident lawyer (https://vimeo.com/707183236)
Unsure of how to proceed with recovery of your QIWI wallet
funds? Our support team are ready around the clock to
guide you through the process and answer any concerns
you have.
Working with our team, you’re opting for a dependable partner in getting your money
back.
Upvc Repairs Near Me Tools To Improve Your Daily Lifethe One Upvc
Repairs Near Me Trick Every Person Should Learn upvc repairs
near me (https://clients1.google.fi/url?q=https://lausen-hede-2.Federatedjournals.com/the-most-successful-double-glazed-front-doors-near-me-gurus-are-doing-three-things-1707299343/)
10 Methods To Build Your Diagnostic Check Near Me Empire diagnostic car (http://go.informpartner.com/return/wap/?ret=https://wownsk-portal.ru/user/squashbrass24/&puid=2280963900011_3669&operation_status=noauth&transactid=2280963900011_3669)
You’ll Never Be Able To Figure Out This Replacement
Ford Fiesta Key Uk’s Benefits ford transit keys
What Makes The Motorcycle Accident Claim So Effective?
During COVID-19 clayton motorcycle accident lawyer
10 Car Key Immobiliser Repair Hacks All Experts Recommend keys
http://mexicanpharmacy1st.com/# п»їbest mexican online pharmacies
10 Healthy Habits For A Healthy Creampie Compilation
Boomerang Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und spannenden Bonusangeboten bietet. Viele Spieler interessieren sich aber auch fГјr die Erfahrungen mit Auszahlungen im Boomerang Casino.
Die meisten Spieler berichten, dass die Auszahlungen im Boomerang Casino schnell und unkompliziert abgewickelt werden. Das Casino bietet eine Vielzahl von Zahlungsmethoden an, darunter Kreditkarten, E-Wallets und BankГјberweisungen. Die meisten Auszahlungen werden innerhalb von 24 Stunden bearbeitet, und die Spieler erhalten ihr Geld in der Regel innerhalb weniger Tage.
Einige Spieler haben jedoch berichtet, dass es gelegentlich zu Verzögerungen bei Auszahlungen kommen kann. Diese Verzögerungen sind in der Regel auf Sicherheitsüberprüfungen zurückzuführen, die das Boomerang Casino durchführt, um sicherzustellen, dass alle Auszahlungen korrekt und sicher abgewickelt werden.
Insgesamt sind die Erfahrungen mit Auszahlungen im Boomerang Casino größtenteils positiv. Die meisten Spieler erhalten ihr Geld schnell und zuverlässig, und das Casino ist bekannt für seinen hervorragenden Kundenservice und seine Transparenz bei Auszahlungen. Wer also auf der Suche nach einem seriösen Online-Casino ist, sollte Boomerang Casino definitiv in Betracht ziehen.
https://boomerangcasino.one/
The 10 Most Scariest Things About Accident Cedar Hill Accident Lawsuit
14 Businesses Doing An Amazing Job At Adhd In Women Symptoms adhd In adult women symptoms
15 Gifts For The Double Glazing Firms Near Me Lover In Your Life Repair Double Glazed Windows
The 9 Things Your Parents Teach You About Veleco Mobility Scooter Uk veleco mobility scooter uk
8 Tips To Boost Your Automobile Locksmith Game auto locksmiths near My location (cmenews.cn)
Asbestos is a naturally occurring mineral that was once used extensively
in construction projects and manufacturing industries.
Those who were exposed to haltom City asbestos attorney often developed serious and life-threatening diseases.
Bei Zet Casino gibt es immer wieder spannende Aktionen und Angebote fГјr die Spieler. Einer der beliebtesten ist der sogenannte “zet casino promГіciГіs kГіdod”, der es den Spielern ermГ¶glicht, sich zusГ¤tzliche Boni und VergГјnstigungen zu sichern.
Um den “zet casino promГіciГіs kГіdod” zu nutzen, mГјssen die Spieler einfach den entsprechenden Code eingeben, wenn sie eine Einzahlung tГ¤tigen. Dadurch erhalten sie zum Beispiel zusГ¤tzliches Bonusguthaben, Freispiele oder andere attraktive Extras. Diese Aktionen kГ¶nnen regelmäßig wechseln, daher lohnt es sich, immer mal wieder auf der Website von Zet Casino vorbeizuschauen, um keine der aktuellen Angebote zu verpassen.
Der “zet casino promГіciГіs kГіdod” ist eine tolle MГ¶glichkeit, um das Spielerlebnis bei Zet Casino noch spannender und abwechslungsreicher zu gestalten. Wer gerne mit zusГ¤tzlichen Boni und VergГјnstigungen spielt, sollte sich diese Aktionen auf keinen Fall entgehen lassen. Also nicht vergessen, den “zet casino promГіciГіs kГіdod” bei der nГ¤chsten Einzahlung einzugeben und von den attraktiven Extras zu profitieren!
https://zetcasino.one/
See What Treadmill Home Gym Tricks The Celebs Are Making Use Of treadmill Home
A Trip Back In Time What People Said About Online Store Uk Cheapest 20 Years Ago Vimeo.Com
Your trust in us is our top priority. That’s why we
work with full transparency and focus on results.
Experience the relief of having your funds back in your possession with our expert services.
20 Tools That Will Make You More Efficient At Attorneys For
Mesothelioma florida mesothelioma attorney
5 Clarifications On Private Mental Health Assessment how to get a private mental health assessment
11 “Faux Pas” That Are Actually Acceptable To Make With Your Slimline Side By
Side Fridge Freezer freezer storage
9 Lessons Your Parents Teach You About Fridge Freezers
Side By Side Fridge Freezers Side By Side
Guide To Self-Emptying Robot Vacuums: The Intermediate Guide
Towards Self-Emptying Robot Vacuums self-emptying robot vacuums
Retrieving what’s yours shouldn’t be a hassle.
That’s why our process is user-friendly and transparent.
You just need to supply some basic information, and we’ll handle the rest.
Don’t let technical problems keep you from your hard-earned money.
Our goal is to assist you in reclaiming every penny.
What The 10 Most Stupid Best Slot Machines Fails Of All Time Could Have Been Prevented Multi-Line Slots
The Most Pervasive Problems With Fold Away Treadmill hometreadmills.Uk
Guide To Lost Car Key Replacement Cost: The Intermediate Guide Towards Lost Car
Key Replacement Cost lost car key Replacement Cost
You’ll Never Guess This Dreametech L30’s Secrets dreametech l30
The Most Hilarious Complaints We’ve Seen About Hyundai Replacement
Key Cost hyundai key Fob replacement Cost uk
You’ll Never Guess This Cost Of Car Key Replacement’s Benefits cost of car Key replacement
How To Determine If You’re All Set For Prada Bag Crossbody prada Cross Bag
The 10 Most Terrifying Things About Replacement Car Keys Nissan replacement car keys nissan, pugh-david-4.federatedjournals.com,
The Three Greatest Moments In Online Shopping Uk Cheap History Gorillapod Ballhead
8 Tips To Improve Your Boating Accident Attorneys Near
Me Game louisville boat accident attorneys (Image.google.ci)
Five Killer Quora Answers On Situs Alternatif Gotogel Situs alternatif Gotogel [amidagroup.ir]
9 Things Your Parents Taught You About Heat Pump Tumble Dryer Reviews Heat pump tumble dryer
10 Misconceptions Your Boss Holds Regarding Windows Replacement
Double glazed windows replacement (Frickler.net)
The Double Glazed Units Near Me Mistake That Every Newbie Makes replacement Double glazed Units Near me
15 Gifts For The Online Shop Lover In Your Life Vimeo
5 Killer Quora Answers On Uk Online Grocery Shopping Sites uk Online grocery shopping Sites
15 Reasons To Not Overlook Robot Vacuum Mop Robot Vacuum And Mop Self Empty
5 Clarifications On CSGO Skin Gambling Sites case spectrum (Kristen)
15 Startling Facts About 18-Wheeler Accident Attorneys That You Didn’t Know
el cerrito 18 wheeler accident lawyer
Slot Demo Explained In Less Than 140 Characters slot demo Pragmatic rupiah
The 10 Most Scariest Things About Online Store Uk Cheapest online store uk cheapest
You’ll Never Guess This Double Glazing Repair Leeds’s
Tricks double glazing repair leeds
Why Best Rated Robot Vacuum Is Harder Than You Think Self Cleaning Robot Vacuum
See What Window Replacement London Tricks The Celebs Are Making Use
Of Window replacement london (Elearnportal.science)
9 Things Your Parents Taught You About Bmw Replacement Car Keys bmw Replacement car keys
How Motor Vehicle Case Is A Secret Life Secret Life Of Motor Vehicle Case lawsuit
5 Killer Quora Answers On Double Glazed Window Repairs Near Me double glazed window repairs Near me
20 Insightful Quotes On Lost Car Key how to replace car keys when lost
What’s The Job Market For Double Glazed Window Repairs Professionals?
double glazed window repairs (Emilia)
See What Replacement Key Bmw Tricks The Celebs Are Making
Use Of Key Bmw
The Most Convincing Proof That You Need Best Accident Attorney
injury Lawsuit advice
7 Helpful Tips To Make The Most Of Your Auto Accident houston automobile accident attorneys
Indisputable Proof Of The Need For Double Glazed Window Repairs Near Me Double Glazed Windows
16 Must-Follow Instagram Pages For Double Glazing
In Leeds-Related Businesses window replacement Leeds – http://Www.google.st,
7 Little Changes That’ll Make An Enormous Difference To Your How To Get CS GO
Cases Case operation bravo (http://lineyka.org/user/archerchin1)
15 Shocking Facts About Local Personal Injury Lawyer Denver Personal Injury Lawyers
The Reasons To Work With This Togel Singapore
tolol
Das Tipico Online Casino hat sich als beliebte Spielplattform unter GlГјcksspiel-Fans etabliert. Doch wie schneidet das Casino in Bezug auf Auswahl an Spielen, Benutzerfreundlichkeit, Kundenservice und Bonusangebote ab? In dieser Bewertung werfen wir einen genauen Blick auf das Tipico Online Casino.
Das Tipico Online Casino bietet eine breite Palette an Spielen, darunter klassische Tischspiele wie Blackjack und Roulette, spannende Spielautomaten und vieles mehr. Die Spiele stammen von renommierten Software-Anbietern wie NetEnt, Microgaming und Play’n GO, was fГјr eine hohe QualitГ¤t und ein ansprechendes Spielerlebnis sorgt.
Die Benutzeroberfläche des Casinos ist einfach zu navigieren und ansprechend gestaltet. Spieler können problemlos zwischen den verschiedenen Spielen und Funktionen wechseln und finden schnell, wonach sie suchen. Darüber hinaus ist das Casino sowohl für Desktop- als auch für mobile Geräte optimiert, was es Spielern ermöglicht, ihre Lieblingsspiele auch unterwegs zu genießen.
Der Kundenservice von Tipico ist rund um die Uhr erreichbar und bietet schnelle und kompetente UnterstГјtzung bei Fragen oder Problemen. Die Mitarbeiter sind freundlich und hilfsbereit und stehen den Spielern per Live-Chat, E-Mail oder Telefon zur VerfГјgung.
Bonuas und Promotions sind ein wichtiger Faktor für viele Spieler bei der Auswahl eines Online-Casinos. Tipico bietet seinen Kunden regelmäßig attraktive Bonusangebote, darunter Willkommensboni, Freispiele und Cashback-Aktionen. Diese Boni helfen den Spielern, ihr Guthaben zu maximieren und die Gewinnchancen zu verbessern.
Insgesamt ist das Tipico Online Casino eine empfehlenswerte Spielplattform für alle, die nach einer Vielzahl von hochwertigen Spielen, einer benutzerfreundlichen Benutzeroberfläche, exzellentem Kundenservice und großzügigen Bonusangeboten suchen. Worauf also noch warten? Melden Sie sich noch heute an und erleben Sie die Faszination des Tipico Online Casinos selbst!
https://tipicocasino.one/
The Reason You Shouldn’t Think About Improving Your Windows Leeds Double Glazing Door Repairs
Lightweight Travel Electric Wheelchair Tools To Ease Your Everyday
Lifethe Only Lightweight Travel Electric Wheelchair Technique Every Person Needs To Learn lightweight travel electric wheelchair (Keeley)
The 10 Scariest Things About Private ADHD Assessment Liverpool Cost Private adhd Assessment
4 Dirty Little Secrets About The Automatic Folding Lightweight Mobility Scooter Industry
auto fold mobility scooter [lawsocietytribunal.ca]
What’s The Job Market For Double Glazing Door Repairs Near Me Professionals Like?
Door Repair (click4R.Com)
Zet Casino ist eine beliebte Online-Glücksspielplattform, die ihren Nutzern eine Vielzahl von spannenden Spielen und großzügigen Werbeaktionen bietet. Einer der besten Wege, um das Spielerlebnis noch aufregender zu gestalten, ist die Verwendung eines Zet Casino Promo-Codes. Mit einem Promo-Code können die Spieler tolle Boni und Vergünstigungen erhalten, die ihre Gewinnchancen erhöhen und ihr Casino-Erlebnis verbessern.
Um einen Zet Casino Promo-Code zu erhalten, müssen die Spieler häufig bestimmte Bedingungen erfüllen, wie zum Beispiel eine Mindesteinzahlung tätigen oder an bestimmten Spielen teilnehmen. Sobald der Promo-Code eingelöst wurde, werden die Boni oder Vergünstigungen automatisch dem Spielerkonto gutgeschrieben und können sofort verwendet werden.
Die Verwendung eines Promo-Codes im Zet Casino ist eine großartige Möglichkeit, um das Beste aus Ihrem Spielerlebnis herauszuholen und mehr Spaß beim Spielen zu haben. Die Bonusse und Vergünstigungen, die Sie mit einem Promo-Code erhalten können, können Ihre Gewinnchancen deutlich verbessern und Ihnen helfen, mehr aus Ihrem Glücksspiel-Erlebnis herauszuholen.
Wenn Sie also gerne im Zet Casino spielen und auf der Suche nach einer Möglichkeit sind, Ihr Spielerlebnis aufzupeppen, dann sollten Sie unbedingt nach einem Zet Casino Promo-Code suchen. Nutzen Sie die großzügigen Angebote und verbessern Sie Ihre Gewinnchancen noch heute!
https://zetcasino.one/
See What Kids Beds Bunk Beds Tricks The Celebs Are Making Use Of kids Beds Bunk
The 10 Most Scariest Things About Buy Beko Washing Machine Buy Beko Washing Machine (http://Uhrtest.Rehbein.Net/)
mexico drug stores pharmacies: best online pharmacies in mexico – mexican drugstore online
Five Essential Qualities Customers Are Searching For In Every Ford
Key Replacement Near Me Service
A Proficient Rant About Upvc Windows And Doors Upvc windows repairs
mexican drugstore online mexico pharmacies prescription drugs medicine in mexico pharmacies
10 Failing Answers To Common Walking Treadmill Under
Desk Questions: Do You Know The Correct Answers? best walking Treadmill under desk
Conventionally, forklifts can be divided domstroi.info into manual and self-propelled. The manual version must be moved by the operator, which may require some effort if the weight of the load exceeds a thousand kilograms. The advantage of this type is its low cost and complete lack of maintenance. However, such a loader will not lift the load to too great a height.
9 . What Your Parents Taught You About Double Glazing Window Repairs Near Me Window Repair
ukrtvoru.info
You’ll Never Be Able To Figure Out This Shopping Online Uk To Ireland’s Tricks
Shopping online uk To ireland
Your trust in us is our top priority. That’s why we conduct our services with full honesty and commitment to your
satisfaction.
Rest easy of having your funds back in your possession with
our professional assistance.
Qcmpt provides in-depth journalism and insight into the news and trends impacting the customer experience space. https://qcmpt.com/
5 Killer Quora Answers On Upvc Windows And Doors Upvc Window Repairs
(https://Www.Diggerslist.Com/66272B5283E35/About)
15 Great Documentaries About Window Companies Leeds double glazed doors repairs
The 10 Scariest Things About Cerebral Palsy Attorneys Cerebral palsy Attorneys
Желаете смотреть новые фильмы и сериалы онлайн в наилучшем качестве? Обратите внимание на портал Kinogo. Этот сервис позволяет смотреть фильмы абсолютно бесплатно. Ищете мелодрамы смотреть онлайн бесплатно? Kinogo-la.net – сайт, который считается безопасным. Сервис имеет простой интерфейс, который делает его применение легким и удобным. Здесь вы сможете быстро отыскать интересующий вас фильм. Содержимое ресурса всегда актуально. Поудобнее устраивайтесь и наслаждайтесь просмотром любимых фильмов!
Why Auto Locksmith Is Fast Increasing To Be The Hot Trend For 2023?
automatic locksmith
Confused about how to go about the recovery of your QIWI
wallet funds? Our support team are available around the clock
to guide you through the procedure and respond to any queries you
might have.
Choosing our company, you’re choosing a trusted helper in getting your money back.
Nine Things That Your Parent Taught You About Best Online Clothing Sites
Uk best online clothing sites Uk [p3terx.com]
10 Quick Tips For Cerebral Palsy Lawyers Selma cerebral Palsy lawsuit
Why We Our Love For Seat Leon Replacement Key (And
You Should, Too!) Seat Leon Key Programming – https://Qooh.Me/ –
The Most Significant Issue With American Freezer Fridge, And How You Can Repair
It american fridge freezer (Markus)
Ten Startups That Will Revolutionize The Rooms To Go Sofa Sale Industry For The Better red leather couch
10 Apps To Help Manage Your Replacement Bmw Key replacement Bmw key Cost
Why You Should Concentrate On Enhancing Car Key Replacements Replacement Car key fob
15 Weird Hobbies That Will Make You More Effective At Online Home Shop
Uk Discount Code Decorative area rugs
15 Terms Everybody Within The Marc Jacobs Bags Industry Should Know
marc jacobs handbag
The Next Big Event In The Real Money Slots Industry slot sites [dott-Comm.Com]
11 Strategies To Completely Block Your Boat Accident Legal
boat accident lawyer
The 10 Scariest Things About Classic Casino Slots classic casino slots – Katharina,
The Reasons To Focus On Enhancing Bags Prada Prada Bag For Woman
10 Fiat Replacement Key-Related Projects That Stretch Your Creativity Fiat Replacement Key
Fob (Rentry.Co)
10 Asbestos Claim Tricks All Experts Recommend asbestos compensation
Tipico ist ein beliebter Anbieter von Sportwetten und Online-Casinospielen, der es den Spielern ermöglicht, ihr Glück bei verschiedenen Spielen zu versuchen. Viele Menschen fragen sich, ob es möglich ist, Geld von Tipico Sportwetten auf das Casino zu übertragen.
Die Antwort lautet ja, es ist möglich, Geld von Tipico Sportwetten auf das Casino zu überweisen. Dies kann auf verschiedene Weisen geschehen, zum Beispiel durch die Verwendung einer gemeinsamen Geldbörse oder durch manuelles Übertragen des Geldes von einem Konto zum anderen.
Es ist wichtig zu beachten, dass es möglicherweise einige Regeln und Einschränkungen gibt, wenn es darum geht, Geld von Sportwetten auf das Casino zu übertragen. Beispielsweise können manche Boni nur für bestimmte Spiele oder Sportwetten verwendet werden und können nicht auf das Casino übertragen werden.
Wenn Sie Geld von Tipico Sportwetten auf das Casino übertragen möchten, sollten Sie sich daher am besten vorher über die genauen Regeln und Bedingungen informieren. Auf der Website von Tipico finden Sie alle notwendigen Informationen dazu.
Alles in allem ist es also durchaus möglich, Geld von Tipico Sportwetten auf das Casino zu überweisen. Mit einem verantwortungsvollen Umgang und der Einhaltung der Regeln können Sie Ihr Glück bei verschiedenen Spielen versuchen und hoffentlich hohe Gewinne erzielen. Viel Spaß und Erfolg beim Spielen!
https://tipicocasino.one/
15 Things You Don’t Know About Greenpower Mobility Scooters clean Energy Scooters
8 Tips To Increase Your Car Spare Key Game Car spare keys
(sciencewiki.science)
https://mexicanpharmacy1st.com/# mexican border pharmacies shipping to usa
The 10 Most Terrifying Things About Erb’s Palsy Legal erb’s
ecobusinessdesign.com
The Little-Known Benefits Classic Slots Modern Slots
15 Bizarre Hobbies That’ll Make You More Effective At Nespresso Coffee
Machine With Milk Frother pink nespresso machine
women-art.net
Das Online-Casino-Zetz Casino hat in den letzten Wochen fГјr Aufsehen gesorgt, jedoch nicht auf die positive Art und Weise. Viele Spieler berichten davon, dass das Casino ihre Gewinne nicht auszahlt, obwohl sie die erforderlichen Umsatzbedingungen erfГјllt haben.
Dies hat zu einer Welle der Kritik und Unzufriedenheit unter den Spielern geführt. Viele fühlen sich betrogen und fühlen sich um ihr hart verdientes Geld betrogen. Es ist besonders frustrierend, da das Zet Casino zunächst einen guten Ruf hatte und viele Spieler angezogen hat.
Die GrГјnde fГјr die Nicht-Auszahlung der Gewinne sind unklar. Einige Spieler spekulieren, dass es sich um eine gezielte Taktik des Casinos handelt, um Kosten zu sparen und Gewinne einzubehalten. Andere vermuten, dass es sich um technische Probleme handelt, die schnell behoben werden sollten.
In jedem Fall ist es wichtig, dass Spieler, die Probleme mit der Auszahlung ihrer Gewinne im Zet Casino haben, sich an den Kundenservice wenden und ihr Anliegen klar und deutlich kommunizieren. Es ist auch ratsam, alle notwendigen Informationen und Dokumente bereitzustellen, um den Prozess zu beschleunigen.
Es ist enttäuschend zu sehen, dass ein Casino, das zuvor einen guten Ruf hatte, in solche Schwierigkeiten geraten ist. Hoffentlich wird das Zet Casino seine Probleme in den Griff bekommen und seinen Spielern wieder ein vertrauenswürdiges und zuverlässiges Spielerlebnis bieten können. Bis dahin ist es ratsam, vorsichtig zu sein und sich gut zu informieren, bevor man im Zet Casino spielt.
https://zetcasino.one/
Double Loft Bed With Stairs Tools To Ease Your Daily Lifethe One Double Loft Bed With Stairs Trick That
Every Person Must Know loft bed with Stairs
A Look At The Myths And Facts Behind Double Glazing Units
Near Me double Glazed Door handles
5 Killer Queora Answers On Upvc Window Repairs Upvc Window Repairs Near Me
10 Things Everybody Hates About Good Online Shopping Sites Uk Airbrush Foundation Kit
7 Simple Changes That Will Make A Big Difference In Your Best Mens Sex Toy mens sex toys,
Bernd,
15 Gifts For The Seat Key Cover Lover In Your Life key Seat
3 Ways In Which The Dangerous Drugs Law Firms
Will Influence Your Life Kerman dangerous drugs Attorney
A Intermediate Guide The Steps To Medical Malpractice Attorney medical Malpractice Lawyer
The Most Convincing Proof That You Need Certified Slots
slots Online
9 Lessons Your Parents Teach You About Replacement Double Glazing Windows replacement double glazing windows
Handbags Prada Tools To Make Your Daily Life Handbags Prada Trick That
Should Be Used By Everyone Be Able To Handbags prada
The Little-Known Benefits Of Window Repairs Upvc window repairs
Where To Research Akun Demo Slot Online Akun demo slot online
Amazon Uk Online Shopping Clothes 101 A Complete Guide For Beginners Performance Hiking Socks
5 Laws That’ll Help The Best Clitoral Vibe Uk Industry Adult Toys For Woman
See What Cost To Replace Windows Uk Tricks The Celebs
Are Using Cost To Replace Windows Uk
15 Reasons Not To Be Ignoring Fridge Freezer Best American Fridge Freezer Uk
What’s The Job Market For Window Repairs Luton Professionals?
window repairs Luton
Ghost Installations Tools To Ease Your Everyday Lifethe Only Ghost Installations Trick That Every Person Must Know ghost installations, Bernice,
20 Trailblazers Lead The Way In Repairing Upvc Windows upvc window repair
The 10 Most Terrifying Things About Slot Animations
Slot Animations
A Brief History Of Mesothelioma Law Firm In 10 Milestones bay st louis mesothelioma attorney (Charity)
7 Simple Tricks To Totally Doing The Which Is Best For Online Grocery Shopping shopping online uk Websites
The Top Double Glazing Glass Replacement Near Me
Is Gurus. Three Things glazier
Five Essential Qualities Customers Are Searching For In Every Mobile Automobile
Locksmith Automotive locksmiths in my area
20 Fun Facts About Replacement Windows Leeds french
door repair leeds (Boyle-prince-2.mdwrite.Net)
Shop Online Uk Women’s Fashion: A Simple Definition Aps 4″ Running Board Ram (Booker)
It’s The Evolution Of Dangerous Drugs Law Firm dangerous drugs lawyers
10 Situations When You’ll Need To Be Educated About Integrated Fridge Frezer Integrated Full Height Fridge
Unquestionable Evidence That You Need Mesothelioma Attorneys clinton Mesothelioma Lawsuit
How The 10 Most Disastrous Window Doctor Near Me Fails Of All Time Could’ve Been Prevented In My Area
Why Sectional Sleeper Sofa Might Be Your Next Big Obsession Small sectional sleeper sofa (m.cosplayfu.es)
The 9 Things Your Parents Taught You About Double Glazed Window Suppliers
Near Me double glazed window Suppliers near me (https://luxuriousrentz.com/the-10-scariest-things-About-double-glazing-companies-near-me)
10 Quick Tips On Upvc Window Repairs window Repairs Near me
The 9 Things Your Parents Taught You About Examples Of Online Shopping examples of online shopping (oi2bj1bgty1t8ty.com)
Medical Malpractice Lawyers Tips To Relax Your Daily Lifethe One Medical Malpractice Lawyers
Technique Every Person Needs To Know medical malpractice
lawyer (https://images.google.com.ec/url?q=https://motorcycletraining.us/wp-content/themes/atmosphere-pro/dmm_custom/Go.php?provider=aHR0cHM6Ly92aW1lby5jb20vNzA5NDM2NTUz)
The 10 Most Terrifying Things About Fridge Freezer Black Fridge freezer black
Think You’re Ready To Start Doing Couches For Sale Near Me?
Answer This Question Couches for sale Under $500
7 Simple Secrets To Completely You Into Accident Claim Chestnut ridge accident lawyer – vimeo.com –
15 Of The Best Twitter Accounts To Find Out More About Cheapest Online Grocery Shopping Uk cheap online grocery shopping uk
Boomerang Casino ist ein beliebtes Online-Casino, das Spielern eine Vielzahl von hochwertigen Spielen und lukrativen Boni bietet. Um auf der Plattform spielen zu können, müssen Benutzer jedoch eine Verifizierungsprozedur durchlaufen, um ihre Identität zu bestätigen.
Die Boomerang Casino Verifizierung ist ein wichtiger Schritt, um die Sicherheit und Seriosität des Casinos zu gewährleisten und Betrug zu verhindern. Spieler müssen Dokumente wie einen Personalausweis, Reisepass oder Führerschein vorlegen, um ihre Identität und Wohnadresse zu bestätigen.
Die Verifizierung kann in der Regel einfach und schnell durchgeführt werden, indem die erforderlichen Dokumente hochgeladen werden. Sobald die Überprüfung abgeschlossen ist, können Spieler ihre Lieblingsspiele genießen und sich ihre Gewinne auszahlen lassen.
Es ist wichtig, die Verifizierung so schnell wie möglich durchzuführen, um keine Verzögerungen bei Auszahlungen zu erleben. Boomerang Casino legt großen Wert auf Sicherheit und Fairness, daher sollten Spieler die Verifizierung als normalen Prozess betrachten, um ihr Spielerlebnis zu verbessern.
Insgesamt ist die Boomerang Casino Verifizierung ein notwendiger Schritt, um die Sicherheit der Spieler zu gewährleisten und ein positives Spielerlebnis zu bieten. Indem Spieler ihre Identität bestätigen, können sie sich ganz auf das Spielen konzentrieren und die aufregende Welt des Online-Glücksspiels genießen.
https://boomerangcasino.one/
It’s The Good And Bad About Double Mattress Memory Foam Soft Double mattress
Why You Should Concentrate On Enhancing Audi Key Replacement
Audi a3 key fob replacement
10 Healthy Slot Demo Gratis Pragmatic Play No Deposit
Habits Slot Pragmatic Play Demo
Online Home Based Work Tools To Enhance Your Life Everyday
Work from home Jobs liverpool
The Most Common Online Shopping Uk Cheap Debate Could Be
As Black And White As You Think On-The-Go Citrus Water
Enhancer (Aundrea)
For Whom Is Portable Wheelchair Electric And Why You Should Consider Portable Wheelchair Electric portable electric wheelchair
mexico pharmacy: mexican rx online – buying prescription drugs in mexico
Zet Bet Casino ist eine beliebte Online-GlГјcksspielplattform, die Spielern aus der ganzen Welt eine Vielzahl von Casino-Spielen und Sportwetten anbietet. Das Casino zeichnet sich durch sein umfangreiches Spielangebot, groГџzГјgige Boni und Promotionen sowie ein benutzerfreundliches Design aus.
Eines der Highlights von Zet Bet Casino ist die Auswahl an Spielautomaten, einschlieГџlich beliebter Titel von fГјhrenden Entwicklern wie NetEnt, Microgaming und Play’n GO. Spieler kГ¶nnen aus Hunderten von Slots wГ¤hlen, darunter klassische Fruchtmaschinen, Video-Slots mit aufregenden Bonusrunden und progressiven Jackpot-Spielen, die lebensverГ¤ndernde Gewinne bieten kГ¶nnen.
Neben Spielautomaten bietet Zet Bet Casino auch eine breite Palette von Tischspielen wie Blackjack, Roulette, Baccarat und Poker an. Diese Spiele sind in verschiedenen Varianten verfГјgbar, um den BedГјrfnissen und Vorlieben aller Spieler gerecht zu werden.
Für diejenigen, die Sportwetten bevorzugen, bietet Zet Bet auch eine umfangreiche Auswahl an Wettoptionen für eine Vielzahl von Sportarten und Veranstaltungen. Von Fußball über Tennis bis hin zu eSports können Spieler auf ihre Lieblingsteams und -spieler wetten und ihre Gewinnchancen maximieren.
Zet Bet Casino belohnt neue Spieler mit großzügigen Willkommensboni und bietet auch regelmäßige Werbeaktionen und Belohnungen an bestehende Spieler. Darüber hinaus bietet das Casino ein Treueprogramm, das es Spielern ermöglicht, Punkte zu sammeln und gegen Bonusguthaben, Freispiele und andere attraktive Preise einzutauschen.
Mit einer sicheren und transparenten Spielumgebung, erstklassigem Kundenservice und schnellen Auszahlungen ist Zet Bet Casino eine ausgezeichnete Wahl fГјr Spieler, die nach einer unterhaltsamen und lohnenden Spielerfahrung suchen. Besuchen Sie noch heute das Zet Bet Casino und entdecken Sie die aufregende Welt des Online-GlГјcksspiels!
https://zetcasino.one/
7 Small Changes You Can Make That’ll Make A Big Difference In Your Vibrating Anal Sex Toy anal Toys Shop
15 Of The Top Designer Handbags Brown Bloggers You Need To Follow designer handbags amazon
Ten Upvc Window Repairs That Really Make
Your Life Better upvc window repairs – tntech.kr –
15 Lessons Your Boss Would Like You To Know You Knew About Car Ignition Lock Repair car remote Lock repair near me
mexico drug stores pharmacies mexican mail order pharmacies buying prescription drugs in mexico online
20 Things Only The Most Devoted Shopping Online Fans Understand Vimeo
20 Questions You Must Always Have To Ask About Best SEO Company UK Before You Purchase Best SEO Company
UK Seo Consultant Companies
The 10 Most Terrifying Things About Car Locksmiths Near Me Auto Car Locksmith
10 Misted Double Glazing Repairs Related Projects That Can Stretch Your Creativity Door repair
Five Things You’ve Never Learned About Online Shopping Sites Top 7 Rolling Head Pry Bars (https://Vimeo.Com/932337583)
10 Unexpected Adult Toys For Women Tips adult anal toys
The Ultimate Glossary For Terms Related To Government Mesothelioma Compensation mesothelioma compensation rights
Desk Treadmill Foldable Tools To Streamline Your Daily Lifethe One Desk Treadmill Foldable Trick That
Every Person Should Be Able To Desk Treadmill Foldable
“The Malpractice Attorney Awards: The Most Stunning, Funniest, And Most Bizarre Things We’ve Seen malpractice Lawsuits
What’s The Job Market For Double Glazed Repairs Near Me Professionals Like?
double Glazed repairs near Me
5 Killer Quora Answers On Gotogel Link Alternatif gotogel Link alternatif
10 Easy Steps To Start Your Own Window Repair Near Business upvc window repairs
The 10 Most Terrifying Things About London Window Repairs london window repairs
How To Create An Awesome Instagram Video About
Steel Anal Butt Plug Anal Plug
5 Reasons Dangerous Drugs Is Actually A Great Thing Vimeo.com
15 Best American-Style Fridge Freezers Bloggers You Must Follow best american-style
fridge Freezer – joase.org,
10 Places Where You Can Find Treadmill For Sale Treadmill for sale near me
5 Laws Anyone Working In Upvc Repairs Near Me Should
Know Installers
16 Must-Follow Facebook Pages For Shop Anal Sex Toy Marketers Best Anal Toys For Men
15 Things You Didn’t Know About Shopping Online Uk To Ireland cheap online Clothing stores with free shipping worldwide
The 3 Most Significant Disasters In Fiat 500 Key Replacement The
Fiat 500 Key Replacement’s 3 Biggest Disasters In History fiat punto key Fob
The Top Companies Not To Be Monitor In The How To Buy Clothes Online From Uk Industry Vimeo.Com
You’ll Never Guess This Online Clothes Shopping Websites Uk’s Benefits online clothes
shopping websites uk (Theron)
Guide To Replacement Upvc Window Handles: The Intermediate Guide On Replacement Upvc Window Handles replacement
upvc window handles (Derick)
What Experts In The Field Would Like You To Learn seat key replacement – Angeles,
Guide To Double Glazed Window Near Me: The Intermediate Guide The Steps To Double
Glazed Window Near Me double glazed window near me
Why People Don’t Care About Best Slot Machines multi-line slots (https://luxuriousrentz.com/10-healthy-habits-for-play-Casino-slots-2/)
Guide To Best Men Sex Toys: The Intermediate Guide On Best Men Sex Toys
Men Sex toy
The Ugly Truth About Online Shopping Websites For Clothes
Vimeo.Com
An Intermediate Guide For Which CS GO Case Is Best To
Open prisma 2 case, rn.rnsh.net,
20 Great Tweets From All Time Meso Lawyer asbestos Cancer Attorney
How Much Can Auto Locksmith Experts Make? local auto locksmiths
One Semi Truck Attorney Success Story You’ll Never Be
Able To semi truck accident law firms
15 Best Twitter Accounts To Learn About Programmable Car Keys reprogramming car key
The Three Greatest Moments In Treadmill Desk History treadmill desk attachment (https://www.ballpark-sanjo.com)
9 Lessons Your Parents Taught You About Washing Machine 12kg Price washing machine 12kg
price – ai-db.science,
What A Weekly Sexy Sexdoll Project Can Change Your Life Sex doll for Sale
8 Tips To Enhance Your Asbestos Lawyer Game asbestos compensation (Alberto)
10 Things Everybody Gets Wrong About Car Locksmith Near Me Car key locksmith
https://mexicanpharmacy1st.shop/# mexican drugstore online
How Adding A Squirting Dildo For Sale To Your Life’s
Activities Will Make All The Difference squirting dildo buy (Savannah)
Boomerang Casino Bonus ohne Einzahlung
In der Welt der Online-Casinos gibt es eine Vielzahl von Boni und Werbeaktionen, die Spieler dazu ermutigen sollen, sich anzumelden und zu spielen. Einer der beliebtesten Boni ist der Bonus ohne Einzahlung, bei dem Spieler kostenlose Gelder erhalten, ohne etwas einzahlen zu müssen. Das Boomerang Casino bietet auch einen solchen Bonus an, der Spielern die Möglichkeit gibt, das Casino zu erkunden und echtes Geld zu gewinnen, ohne ihr eigenes Geld auszugeben.
Der Boomerang Casino Bonus ohne Einzahlung kann in Form von Freispielen, Bonusgeld oder anderen Vergünstigungen angeboten werden. Um diesen Bonus zu erhalten, müssen Spieler sich lediglich auf der Website des Casinos registrieren und müssen oft einen Bonuscode eingeben, um den Bonus zu aktivieren. Sobald der Bonus aktiviert ist, können die Spieler frei spielen und echtes Geld gewinnen, ohne dass sie zuerst eine Einzahlung tätigen müssen.
Dieser Bonus ohne Einzahlung kann eine großartige Möglichkeit für neue Spieler sein, ein Online-Casino auszuprobieren, ohne dabei ein finanzielles Risiko eingehen zu müssen. Es ermöglicht Spielern, die Spiele und die Software des Casinos kennenzulernen, bevor sie entscheiden, ob sie eine Einzahlung tätigen wollen. Durch den Boomerang Casino Bonus ohne Einzahlung können Spieler auch echtes Geld gewinnen, ohne dabei eigenes Geld riskieren zu müssen.
Es ist jedoch wichtig zu beachten, dass bei solchen Boni oft bestimmte Bedingungen und Umsatzanforderungen gelten. Spieler sollten sich daher immer die Bonusbedingungen genau durchlesen, bevor sie sich für einen Bonus ohne Einzahlung entscheiden. Dies kann helfen, Missverständnisse und Enttäuschungen zu vermeiden und sicherzustellen, dass Spieler das Beste aus ihrem Bonus herausholen können.
Insgesamt ist der Boomerang Casino Bonus ohne Einzahlung eine großartige Möglichkeit für Spieler, ein neues Online-Casino auszuprobieren und echtes Geld zu gewinnen, ohne dabei eigenes Geld riskieren zu müssen. Spieler sollten sich jedoch bewusst sein, dass es bestimmte Bedingungen gibt, die sie einhalten müssen, um den Bonus nutzen zu können. Wenn Spieler diese Bedingungen erfüllen, können sie jedoch viel Spaß haben und möglicherweise auch ordentliche Gewinne erzielen.
https://boomerangcasino.one/
Why Tommy Hilfiger Purse Bag Is Your Next Big Obsession Tommy hilfiger bags laptop
Don’t Buy Into These “Trends” About Mesothelioma Lawsuits Mesothelioma Settlement
Why No One Cares About Repairing Upvc Windows service
Double Glazing Window Repair Tools To Ease Your Daily Lifethe One Double Glazing Window Repair Trick That Everybody
Should Be Able To window
Why Avon Glimmer Is The Next Big Obsession avon glimmersticks lip liner – Berry –
Ford Fiesta Replacement Key Cost Uk’s History Of Ford Fiesta Replacement Key Cost Uk In 10 Milestones repairer
Who Is Responsible For A Reallife Sexdoll Budget?
12 Top Notch Ways To Spend Your Money cheap sex Dolls – http://www.italianculture.Net,
15 Things To Give That Seo Search Engine Optimisation Lover In Your Life Search Engine Optimisation Company
The 9 Things Your Parents Teach You About Replace Window Handles replace window handle (Osvaldo)
Searching For Inspiration? Look Up Bentley Key bentley key replacement
What’s The Current Job Market For Cheapest Folding Mobility
Scooter Professionals Like? Cheapest Folding Mobility Scooter
20 Reasons Why What Is The Best Online Shopping In Uk Will Never Be Forgotten vimeo.com
Why Is Everyone Talking About SEO Services Right Now seo services London
10 Meetups About Uk Online Shopping Sites Like Amazon You
Should Attend build your own guitar cabinet (vimeo.com)
Situs Gotogel Terpercaya Tools To Help You Manage Your Daily Lifethe One Situs Gotogel Terpercaya Trick Every Individual Should Know Situs Gotogel terpercaya
Online Shopping Sites List For Clothes Techniques To Simplify Your Daily
Lifethe One Online Shopping Sites List For Clothes Trick
That Everybody Should Learn Vimeo
Guide To Mesothelioma Lawsuit: The Intermediate Guide In Mesothelioma Lawsuit mesothelioma
See What Best Online Shopping Uk Clothes Tricks The
Celebs Are Utilizing best online shopping uk clothes (https://kanose.hateblo.jp/iframe/hatena_bookmark_comment?canonical_uri=https://www.google.bf/url?q=https://vimeo.com/932306145)
10 Myths Your Boss Is Spreading Regarding Private Assessments For
ADHD adhd private assessment
aparthome.org
10 Reasons That People Are Hateful To Upvc Window Repairs Upvc Window Repairs
window repairs Near me (http://daywell.kr/bbs/board.php?bo_table=free&wr_Id=471315)
besttoday.org
24 Hours To Improve Prada Handbag For Man prada bag Saffiano
7 Simple Tricks To Totally Enjoying Your Avon Brochure online brochure
The Advanced Guide To Double Glazed Window Repair double glazing repair
(http://gwwa.yodev.Net/)
15 Up-And-Coming Mental Health Bloggers You Need To Follow How To Get A Mental Health Assessment
This Story Behind Truck Accident Lawyers Will Haunt You
For The Rest Of Your Life! trucking Accident lawsuit Representation
15 Best Twitter Accounts To Find Out More About
Double Glazing Companies Near Me double glazed Window handle
The Most Hilarious Complaints We’ve Been Hearing About Designer Handbags In Sale Designer Bags
15 Facts Your Boss Wishes You’d Known About Emergency Window Repair Window
repairs (milkyway.Cs.rpi.Edu)
15 Pinterest Boards That Are The Best Of All Time About Replacement
Handles For Upvc Windows commercial
What’s The Current Job Market For Double Glazing Door Repairs Professionals
Like? Door repair
10 Things We Hate About Rep Kit avon kit
Unexpected Business Strategies Helped Double Glazed Units Near Me To Succeed replacement double glazed units near me
A Look At The Myths And Facts Behind Double Glazing Glass Replacement Near Me Fit
Why We Do We Love Cerebral Palsy Litigation (And You Should
Too!) Vimeo
10 Tell-Tale Warning Signs You Need To Know Before You Buy Car
Locksmiths Near Me replacement
Who Is 18 Wheeler Accident Law Firm And Why You Should Be Concerned pleasanton 18 wheeler accident Law firm
Why Is This Free Stand Freezer So Beneficial? During COVID-19 http://www.frydge.uk
What’s The Job Market For Window Repair Near Me
Professionals Like? window repair Near Me
Tipico Guthaben in Casino Chips
Immer mehr Menschen entscheiden sich dafür, ihr Tipico Guthaben in Casino Chips umzuwandeln, um in den zahlreichen Online Casinos spielen zu können. Doch was bedeutet es, sein Guthaben in Chips umzuwandeln und wie funktioniert dieser Prozess?
Wenn man sein Tipico Guthaben in Casino Chips umwandelt, tauscht man sein virtuelles Guthaben in Spielchips um, die in den Online Casinos als Währung gelten. Man kann diese Chips dann nutzen, um an verschiedenen Spielen wie Slots, Roulette oder Blackjack teilzunehmen. Es ermöglicht den Spielern, das Guthaben besser zu verwalten und sich auf das eigentliche Spiel zu konzentrieren, ohne sich ständig um den aktuellen Kontostand kümmern zu müssen.
Der Prozess, sein Guthaben in Chips umzuwandeln, ist in der Regel sehr einfach. Man muss lediglich die Option “Chips kaufen” im Online Casino auswГ¤hlen und den gewГјnschten Betrag eingeben. AnschlieГџend wird das Guthaben automatisch in Chips umgewandelt und man kann sofort mit dem Spielen beginnen.
Viele Spieler bevorzugen es, ihr Guthaben in Casino Chips umzuwandeln, da es ihnen ein besseres Spielerlebnis bietet. Man kann sich voll und ganz auf das Spiel konzentrieren, ohne von externen Faktoren abgelenkt zu werden. Zudem ermöglicht es eine bessere Kontrolle über das eigene Spielverhalten, da man genau sieht, wie viel man bereits eingesetzt hat und wie viel Guthaben noch verfügbar ist.
Insgesamt ist die Umwandlung von Tipico Guthaben in Casino Chips eine sinnvolle Option für alle, die gerne in Online Casinos spielen. Es bietet eine bessere Kontrolle über das eigene Spielverhalten und ermöglicht ein angenehmeres Spielerlebnis. Wer also sein Glück in Online Casinos versuchen möchte, sollte die Möglichkeit der Umwandlung seines Guthabens in Chips in Betracht ziehen.
https://tipicocasino.one/
See What Cost To Replace Windows Uk Tricks The Celebs
Are Utilizing Cost to replace windows uk
10 Things You Learned In Kindergarden That Will Aid You In Obtaining Sex Machines Online sex thrust machine (https://www.quendu.com/)
20 Things You Must Know About Window Repairman window Repairs
Ten Phoenix Mesothelioma Lawyers That Really Improve
Your Life mesothelioma lawyers
п»їbest mexican online pharmacies pharmacies in mexico that ship to usa reputable mexican pharmacies online
What NOT To Do In The Realistic Sexdolls Industry Petite sex doll (andrejruscak.blog.idnes.cz)
Zet Casino Deutschland – Top Online Spielothek
Das Zet Casino ist eine beliebte Online Spielothek, die auch in Deutschland immer mehr Spieler anzieht. Die Website bietet eine groГџe Auswahl an Spielen, darunter Spielautomaten, Tischspiele, Live-Casino Spiele und mehr. Die Plattform ist benutzerfreundlich und bietet eine sichere und faire Spielumgebung fГјr alle Spieler.
Das Zet Casino Deutschland bietet auch eine Vielzahl von Zahlungsmethoden für deutsche Spieler, darunter Kreditkarten, E-Wallets und Banküberweisungen. Die Auszahlungen sind schnell und unkompliziert, was die Spieler sicherlich zu schätzen wissen.
Ein weiterer groГџer Vorteil des Zet Casinos ist der Kundenservice. Das Support-Team ist rund um die Uhr erreichbar und hilft bei allen Fragen und Anliegen. Die Mitarbeiter sind freundlich, professionell und sehr kompetent.
Zet Casino Deutschland bietet auch großzügige Boni und Promotionen für neue und bestehende Spieler. Diese können Freispiele, Einzahlungsboni und Cashback-Angebote umfassen. Es lohnt sich also, regelmäßig nach den neuesten Aktionen Ausschau zu halten.
Insgesamt ist das Zet Casino eine ausgezeichnete Wahl fГјr deutsche Spieler, die nach einer unterhaltsamen und sicheren Online-Spielothek suchen. Mit einer groГџen Auswahl an Spielen, einer benutzerfreundlichen Website und einem erstklassigen Kundenservice ist das Zet Casino Deutschland definitiv einen Besuch wert.
https://zetcasino.one/
stroihome.net
На сайте http://magomagii.ru вы сможете получить всю необходимую информацию об обрядах, узнать про магические заклинания, увлекательные обряды, а также эзотерику. При этом вы сможете ознакомиться с полезными и любопытными материалами, а также пообщаться с единомышленниками, оценить посты и высказать свое мнение. Кроме того, можно будет попробовать провести обряды самостоятельно, чтобы получить необходимый результат. Ознакомьтесь со всеми рубриками сайта. Среди них: магия и отношения, магический словарь, магический календарь, заметки, магическая кулинария.
10 Things That Your Family Teach You About Situs
Alternatif Gotogel situs Alternatif gotogel
pharmacies in mexico that ship to usa: best mexican online pharmacies – mexico pharmacy
domfenshuy.net
11 Ways To Fully Defy Your Designer Handbags For
Ladies Designer Handbags Chanel
10 Facts About Central Locking Repair Cost That
Will Instantly Put You In An Upbeat Mood fix car door lock,
Johnnie,
You’ll Never Guess This Ford Key Cutting’s Tricks ford Key Cutting
The 10 Most Scariest Things About Sofas For
Sale Near Me sofas for Sale near me
Window Repairs Tips That Will Change Your Life upvc repair (Manuela)
Why Do So Many People Want To Know About Fridge Freezers For Sale?
Side-By-Side Fridge Freezer
How To Explain Upvc Windows Repair To Your Mom window repair
5 Door Fitters Luton Myths You Should Stay Clear
Of window and door companies near me
What Are The Myths And Facts Behind Lightweight Mobility Scooters For Sale go go mobility scooters for sale [Julieta]
Double Glazing Units Near Me Tools To Facilitate Your
Everyday Life repair
Компания «Дока строй» успешно занимается ремонтом квартир с 2007 года. Здесь работают истинные специалисты с профильным образованием. Сотрудники учитывают все нюансы и прекрасно знают свою сферу. Предлагаем только высококачественные услуги и гарантируем доступную стоимость. Ищете ремонт Волгоград квартиры под ключ цена? Doka-stroi.ru – сайт, где у вас есть возможность уже сейчас посмотреть отзывы довольных клиентов и наши выполненные проекты. Обращайтесь именно к нам, мы всегда идем до конца. Уверены, что будете советовать нас своим знакомым.
brand cialis sip – forzest department penisole distract
Why All The Fuss? Double Glazed Front Doors Near Me?
double glaing – Denisha –
15 Reasons To Not Overlook Lightweight Folding Wheelchairs caregiver-friendly
15 Gifts For The Double Glazing Near Me Lover In Your Life double glazing glass replacement Cost
Проект Мир: Л мы создали специально для того, чтобы вы научились ценить себя и отдавать любовь миру вокруг вас. Развивайтесь и самосовершенствуйтесь, смотрите вебинары, проходите обучение, посещайте мероприятия в разных уголках планеты. Ищете арт терапия методы? Mir-l.com – зарегистрировавшись тут абсолютно бесплатно, вы сразу получите доступ к интересным статьям, видеороликам, а также аудиозаписям по различным сферам. Если у вас остались какие-либо вопросы, напишите нам, укажите на нашем сайте ваше имя и e-mail. Исследуйте уже сейчас платформу Мир: Л!
Upvc Windows Repairs: What’s The Only Thing Nobody Is Talking About repairing upvc windows
9 Things Your Parents Taught You About Replacement Double Glazing Windows
Replacement Double Glazing Windows
How Do You Know If You’re In The Right Position To
Go After Truck Lawyer Near Me aberdeen truck accident Law firm
A Step-By-Step Guide For Choosing The Right Treehouse Canopy
tree house cabin bed, Bernard,
The 9 Things Your Parents Teach You About Upvc
Window Repairs Near Me Upvc Window Repairs Near Me
11 Ways To Completely Sabotage Your Slot Strategies
legitimate slots
You’ll Be Unable To Guess Window Repair Near Me’s Tricks Window Repair near me
15 Pinterest Boards That Are The Best Of All Time About Mid
Sleeper Treehouse Bed embrace twin loft bed – https://Pediascape.science/wiki/Five_Killer_Quora_Answers_To_Treehouse_Bunk_Bed_With_Slide –
The Most Pervasive Problems With Upvc Windows Repair
upvc window repairs near me
В мире женщин – онлайн журнал, который предлагает занимательную и актуальную информацию. Здесь имеются такие рубрики: мода, красота, здоровье, отношения, звезды, стиль, психология, юмор, гороскопы. Вы узнаете, как выглядит самый дорогой свадебный торт в мире, почему советские джинсы так и не стали модными, стоит ли ходить в тренажерный зал во время пандемии. https://vmirezhenshchin.ru – сайт, который сделан так, чтобы вам было комфортно им пользоваться. Мы размещаем качественные фотографии. У нас вы сможете найти много интересной информации.
Boomerang Casino Bewertung
Boomerang Casino ist ein aufregendes Online-Casino, das Spielern eine Vielzahl von Spielen und groГџzГјgigen Bonusangeboten bietet. In dieser Bewertung werden wir einen genaueren Blick auf alle wichtigen Aspekte dieses Casinos werfen.
Das erste, was auffГ¤llt, wenn man Boomerang Casino betritt, ist das benutzerfreundliche Design der Website. Die Navigation ist einfach und intuitiv, so dass Spieler leicht finden kГ¶nnen, wonach sie suchen. Das Casino bietet eine beeindruckende Auswahl an Spielen, darunter Slots, Tischspiele, Live-Casino-Spiele und mehr. Die Spiele stammen von renommierten Anbietern wie NetEnt, Microgaming, Play’n GO und vielen anderen.
Ein weiterer großer Vorteil von Boomerang Casino sind die großzügigen Bonusangebote. Neue Spieler erhalten einen lukrativen Willkommensbonus, der ihnen zusätzliches Geld und Freispiele für ausgewählte Spiele bietet. Darüber hinaus gibt es regelmäßige Promotionen und Sonderangebote für bestehende Spieler. Dies sorgt für zusätzliche Spannung und Unterhaltung beim Spielen im Casino.
Die Sicherheit der Spieler hat oberste Priorität bei Boomerang Casino. Das Casino verwendet eine hochmoderne SSL-Verschlüsselungstechnologie, um sicherzustellen, dass alle persönlichen Daten der Spieler geschützt sind. Darüber hinaus ist das Casino vollständig lizenziert und reguliert, was bedeutet, dass es strengen Standards und Vorschriften entspricht.
Der Kundensupport bei Boomerang Casino ist professionell und freundlich. Spieler können das Support-Team per Live-Chat, E-Mail oder Telefon erreichen und ihre Fragen und Anliegen schnell klären lassen. Dies ist besonders wichtig, um sicherzustellen, dass Spieler ein reibungsloses und unterhaltsames Spielerlebnis haben.
Insgesamt ist Boomerang Casino ein hervorragendes Online-Casino, das Spielern eine groГџartige Auswahl an Spielen, groГџzГјgige Bonusangebote und erstklassigen Kundensupport bietet. Wenn Sie auf der Suche nach einem unterhaltsamen und sicheren Ort zum Spielen sind, sollten Sie definitiv Boomerang Casino eine Chance geben.
https://boomerangcasino.one/
A Peek In Double Glazing Repair Leeds’s Secrets Of Double Glazing
Repair Leeds repaired
Speak “Yes” To These 5 Railroad Injuries Case Tips Independence Railroad Injuries lawyer
Вам необходима квалифицированная помощь автоюриста в Самаре? Анатолий Владимирович Мотин готов вам помочь. Адвокат по ДТП если берется за ведение дела, то доводит его до самого конца. Он не обещает то, чего выполнить не сможет. Специалист выезжает на ведение процессов по всей Самарской области. Ищете автоюристы адрес? Advokat-samara.ru – сайт, где вы увидите цены, можете уже сейчас с ними ознакомиться. Здесь также представлены советы адвоката по транспортным происшествиям. Вы узнаете, как при ДТП вести себя пассажиру и пешеходу.
12 Kilo Washing Machine Tools To Improve Your Daily Lifethe One
12 Kilo Washing Machine Trick That Every Person Must Learn 12 kilo washing machine (Phillipp)
Why Everyone Is Talking About Nespresso Commercial Machine Right Now Travel nespresso machine
10 Things Everyone Hates About Semi Truck Law Semi trucking
The Little Known Benefits Of Demo Princess princess slot demo (Sang)
You’ll Never Guess This Upvc Window Repairs Near Me’s Tricks upvc Window repairs near Me
5 Killer Quora Answers On Buy 12kg Washing Machine buy 12kg Washing Machine
5 Laws That Will Help To Improve The Cars Locksmith Near Me Industry Near by
The Reasons Double Glazing Door Repairs Near Me Is More Risky Than You
Think Secondary Double Glazing Near Me
What NOT To Do Within The Birth Injury Attorney
Iowa Industry birth injury legal advice
Ten Startups That Will Revolutionize The Auto Law Firm Industry For The Better Car Accident Injury Attorney
This Is What Window Repair Near Will Look In 10 Years Window Repair near me
Zet Casino – Kasinoomtaler
Zet Casino ist ein Online-Kasino, das sich in den letzten Jahren zu einer beliebten Anlaufstelle für Glücksspiel-Fans entwickelt hat. Das Kasino bietet eine Vielzahl von Spielen, großzügige Boni und eine benutzerfreundliche Oberfläche, die es Spielern ermöglicht, ein erstklassiges Spielerlebnis zu genießen.
Die Auswahl an Spielen bei Zet Casino ist beeindruckend. Von klassischen Tischspielen wie Blackjack und Roulette bis hin zu modernen Video-Slots und Live-Casino-Spielen – hier ist fГјr jeden Geschmack etwas dabei. Die Spiele werden von renommierten Software-Anbietern wie NetEnt, Microgaming und Play’n GO bereitgestellt, was fГјr Fairness und hohe QualitГ¤t garantiert.
Ein weiterer großer Pluspunkt des Kasinos sind die großzügigen Boni und Aktionen, die regelmäßig angeboten werden. Neue Spieler können sich über einen großzigen Willkommensbonus freuen, der ihre erste Einzahlung verdoppelt und ihnen zusätzliche Freispiele für ausgewählte Spiele bietet. Darüber hinaus gibt es regelmäßig Turniere und Verlosungen, bei denen Spieler attraktive Preise gewinnen können.
Die Benutzeroberfläche von Zet Casino ist intuitiv und benutzerfreundlich gestaltet, was es auch unerfahrenen Spielern leicht macht, sich zurechtzufinden. Das Kasino ist vollständig mobiloptimiert, so dass Spieler auch von unterwegs aus auf ihre Lieblingsspiele zugreifen können.
Insgesamt bietet Zet Casino ein erstklassiges Spielerlebnis, das sowohl für Anfänger als auch für erfahrene Spieler geeignet ist. Mit einer riesigen Auswahl an Spielen, großzügigen Boni und einer benutzerfreundlichen Oberfläche ist dieses Kasino definitiv einen Besuch wert.
https://zetcasino.one/
10 Replacement Upvc Window Handles-Related Projects That Stretch
Your Creativity upvc window Repair near me
Link Login Gotogel Tools To Ease Your Everyday Lifethe Only Link
Login Gotogel Trick That Every Person Must Be Able To Link Login Gotogel
10 Things That Your Family Taught You About Window Doctor Near Me Window Doctor Near Me
It’s The Treadmill With Incline Case Study You’ll Never
Forget range of treadmills
A Cheat Sheet For The Ultimate On Side By Side Fridge Freezers Uk Freezer And fridge Unit
The Three Greatest Moments In CSGO Battle Case History prisma case (images.google.com.gt)
Susibu provides in-depth journalism and insight into the news and trends impacting the hotel https://susibu.com/
Sisanit provides in-depth journalism and insight into the news and trends impacting corporate counsel. https://sisanit.com/
Where Can You Find The Most Effective Replacement Window Handle Information? upvc Replacement window handles
Why Semi Truck Claim Is Fast Becoming The
Most Popular Trend For 2023? Winterset Semi Truck Accident Law Firm
https://mexicanpharmacy1st.com/# mexican pharmacy
Guide To Windows Replacement: The Intermediate Guide In Windows Replacement Windows replacement
Guide To Best Sex Toys For Him: The Intermediate Guide On Best Sex Toys For Him Best sex toys for Him
20 Myths About Semi Truck Legal: Busted Vimeo.Com
На сайте http://magomagii.ru изучите интересную, увлекательную и содержательную информацию, которая связана с магией, эзотерикой. Вы научитесь правильно проводить обряды, пользоваться магией и будете радоваться полученным результатам. Маг размещает авторские статьи собственного сочинения. Он вкладывает в них свои умения, знания, душу. И точно знает, что данной темой заинтересуются. Здесь каждый сможет отыскать для себя что-то стоящее и интересное. На сайте можно и просто общаться, делиться впечатлениями.
How To Make A Successful Magimix Nespresso Coffee Machine Instructions For Homeschoolers From
Home magimix nespresso machine
9 . What Your Parents Teach You About Couches Sale Couches sale
The 10 Scariest Things About List Of Online Shopping Sites Uk list of Online shopping sites uk
GSA SER Review Tips To Relax Your Daily Lifethe One GSA SER Review Technique
Every Person Needs To Learn Gsa Ser Review
Treadmills Near Me Tools To Help You Manage Your Daily Lifethe One Treadmills Near Me Trick Every
Person Should Be Able To Treadmills Near Me
The Under-Appreciated Benefits Of CS GO Case New prisma case (Asa)
15 Top Documentaries About Replacement Upvc Window
Handles repairing upvc windows (masekaihatsu.Com)
Is Technology Making Double Glazing Window Repairs Near Me Better Or Worse?
Double Glazing Deals Near Me (Blanarova.Blog.Idnes.Cz)
14 Questions You Might Be Insecure To Ask About Designer Bags designer handbags Chanel
10 Unexpected Marc Jacobs Bags For Sale Tips marc jacobs bag Outlet
The Reasons Kit Avon 2023 Is Tougher Than You Think kit Avon (sc.sie.gov.hk)
What Freud Can Teach Us About Personal Injury Law Montebello Personal Injury Lawsuit
5 Killer Quora Answers On Replacement Double Glazing Units
Near Me double Glazing units Near me (http://www.Moaprint.com)
Guide To Link Alternatif Gotogel: The Intermediate Guide Towards Link
Alternatif Gotogel Link Alternatif Gotogel
Filter Coffee: The Ugly Real Truth Of Filter Coffee filter coffee makers;
Israel,
Best Anal Toys: Myths And Facts Behind Best Anal
Toys Anal Toys Best
Where Do You Think Window Fixer London Be 1 Year From What
Is Happening Now? Repairing
3 Reasons Your Double Glazed Window Repairs Near Me
Is Broken (And How To Fix It) Double Glazed Window Repairs
Why CSGO New Cases Can Be More Risky Than You Think
recoil case (Maik)
You’ll Never Guess This 9kg Washing Machine For Sale’s Benefits 9Kg Washing Machine For Sale
Solutions To The Problems Of Upvc Window Repairs window repairs near
Me (https://dun-lion-Fkq3g5.mystrikingly.com)
cialis soft tabs online strike – cialis oral jelly snatch viagra oral jelly online result
Das Boomerang Casino hat das Jahr 2021 mit einer aufregenden Neuigkeit für seine Spieler eingeläutet: Neue und spannende No Deposit Bonus Codes. Diese Codes ermöglichen es den Spielern, kostenlos zu spielen und echtes Geld zu gewinnen, ohne dabei eigenes Geld einzusetzen.
Ein No Deposit Bonus Code ist eine Art Belohnung, die vom Casino an seine Spieler vergeben wird, ohne dass eine Einzahlung erforderlich ist. Diese Codes können auf verschiedenen Plattformen wie Websites, E-Mails oder sozialen Medien gefunden werden und müssen dann einfach nur im entsprechenden Feld auf der Casino-Website eingegeben werden, um den Bonus zu erhalten.
Die No Deposit Bonus Codes für das Boomerang Casino im Jahr 2021 bieten den Spielern die Möglichkeit, neue Spiele auszuprobieren und ihre Lieblingsspiele zu spielen, ohne dabei Risiken einzugehen. Zusätzlich gibt es die Chance, echtes Geld zu gewinnen und sich diesen Gewinn auch auszahlen zu lassen.
Um über die aktuellen No Deposit Bonus Codes informiert zu bleiben, empfiehlt es sich, die offizielle Website des Boomerang Casinos regelmäßig zu besuchen oder den Newsletter zu abonnieren. Dort werden regelmäßig neue Aktionen und Codes bekannt gegeben, die die Spieler nutzen können, um ihr Spielerlebnis noch spannender zu gestalten.
Insgesamt bieten die No Deposit Bonus Codes für das Jahr 2021 im Boomerang Casino eine tolle Möglichkeit, kostenlos zu spielen und dabei echtes Geld zu gewinnen. Es lohnt sich also, die Augen offen zu halten und die Codes zu nutzen, um das Beste aus dem eigenen Spielerlebnis herauszuholen.
https://boomerangcasino.one/
Your Worst Nightmare About Online Shopping Uk For
Clothes Come To Life Vimeo
You’ll Never Guess This Double Glazed Units Near Me’s Tricks double glazed units Near me
What Is The Reason Dildo Sex Toy Is The Best Choice
For You? Topsadulttoys.uk
3 Ways The Realsex Doll Will Influence Your Life sex doll review
Five Killer Quora Answers On Treadmill Used For Sale
treadmill used for Sale
10 Unexpected All CSGO Skins Tips Gamma 2 Case
How To Solve Issues Related To Upvc Window Repairs upvc window repairs near me
You’ll Be Unable To Guess Double Glazing Repair Leeds’s Tricks double glazing repair, https://www.google.pn,
In der Welt der Online Casinos gibt es eine Vielzahl von Möglichkeiten, um Spieler anzulocken und zu belohnen. Eine beliebte Methode, um neue Kunden zu gewinnen und bestehende Spieler zu binden, sind Promo-Codes. Diese speziellen Codes ermöglichen es den Spielern, verschiedene Boni und Vergünstigungen zu erhalten, wenn sie sie bei der Registrierung oder Einzahlung verwenden.
Ein Casino, das dieses Jahr mit einem besonders lukrativen Promo-Code aufwartet, ist das Zet Casino. Der Zet Casino Promo-Code 2020 verspricht groГџzГјgige Boni und spannende Aktionen, die sowohl Neulinge als auch erfahrene Spieler begeistern werden.
Wenn Sie sich entscheiden, den Zet Casino Promo-Code 2020 zu nutzen, können Sie von verschiedenen Boni profitieren. Dazu gehören beispielsweise Einzahlungsboni, Freispiele, Cashback-Angebote und vieles mehr. Diese Boni können Ihnen helfen, Ihr Spielkapital zu erhöhen und Ihre Gewinnchancen zu maximieren.
Um den Zet Casino Promo-Code 2020 zu nutzen, müssen Sie lediglich während der Registrierung oder Einzahlung den entsprechenden Code eingeben. Sobald Sie dies getan haben, werden die Boni automatisch Ihrem Konto gutgeschrieben und Sie können sofort mit dem Spielen beginnen.
Es ist jedoch wichtig zu beachten, dass jeder Promo-Code seine eigenen Bedingungen und Konditionen hat. Bevor Sie also einen Promo-Code verwenden, sollten Sie sich unbedingt über diese informieren, um sicherzustellen, dass Sie die Boni optimal nutzen können.
Insgesamt bietet der Zet Casino Promo-Code 2020 Spielern die Möglichkeit, ihr Casinoerlebnis aufregender und lohnenswerter zu gestalten. Wenn Sie also auf der Suche nach einem neuen Online-Casino sind, sollten Sie sich auf jeden Fall die Aktionen von Zet Casino genauer ansehen und den Promo-Code 2020 nutzen. Viel Spaß und viel Glück beim Spielen!
https://zetcasino.one/
The 10 Scariest Things About Upvc Windows Repairs upvc windows repairs
What Is The Heck What Is Princess Slot Demo? Slot Demo Pragmatic Starlight Princess
1000 (https://Ordays.Co.Kr/Member/Login.Html?Nomemberorder=&Returnurl=Http://Qooh.Me/Cloudhour0)
You’ll Never Guess This Are Heat Pump Tumble Dryers Any Good’s Tricks Are heat pump tumble Dryers any good
Quiz: How Much Do You Know About Slot Demo Pragmatic?
gates of olympus slot demo
Is Technology Making Double Glazing Window Repairs Near Me Better
Or Worse? double glazing window Repairs
10 Things That Your Family Teach You About ADHD Diagnosis UK Adults
Adhd Diagnosis Uk Adults
Guide To Double Glazed Window Near Me: The Intermediate Guide On Double Glazed Window
Near Me double glazed Window near me
Many Of The Common Errors People Do With Male Masturbation Toys best Male auto masturbator (infocallp.edu.bo)
Be On The Lookout For: How Semi Truck Litigation Is Taking Over And What You Can Do About It semi truck accident lawyers
Motorcycle Accident Compensation: A Simple Definition Sandy motorcycle Accident lawyer
Why You Should Concentrate On Enhancing Mesothelioma Law Springfield Mesothelioma Lawyer
20 Trailblazers Leading The Way In Private ADHD assessment
Similar parts are created from hard alloys etalonsadforum.com such as tungsten carbide, titanium or tantalum with the addition of cobalt. After melting, such parts are pressed under high pressure to obtain the desired parameters.
cialis soft tabs online climb – valif pills people viagra oral jelly splendid
Ищите профессионала в области химчистки и ухода за мягкой мебелью? Cleaning 34 предоставляет высококачественные услуги. Используем безопасные моющие средства и даем гарантию на реальное удаление сложных загрязнений. Ищете чистка дивана? Fresh-Cleaning.ru – сайт, где указаны цены. Пенсионерам и молодым семьям предусмотрены скидки. Приезжаем к вам, чтобы произвести все нужные работы без лишних хлопот. Делаем все возможное для вашего комфорта. Оцените достоинства сотрудничества с нами. Мы сделаем ваш дом идеально чистым!
Do You Think You’re Suited For Doing Upvc Windows Near Me?
Check This Quiz Upvc Window Repairs
1newss.com
The No. One Question That Everyone In Window.Replacement Near Me Must Know How To Answer repairs
reputable mexican pharmacies online: mexican pharmacy – mexican rx online
Responsible For The Upvc Window Repairs Budget? 12 Top Ways To Spend Your
Money upvc Window repairs near me
The Next Big Event In The Online Shopping Uk Industry bessey 5-1xxx Review
The Most Popular Car Spare Key The Gurus Are Using 3
Things spare Keys near Me
5 Killer Quora Answers To Double Glazed Near Me Double glazed Near me
15 Inspiring Facts About Assessment In Mental Health
That You’d Never Been Educated About mental Health assessments
mexico drug stores pharmacies mexican mail order pharmacies reputable mexican pharmacies online
5 Killer Quora Answers On Double Glazed Window Repairs Near Me double glazed window repairs Near me
20 Myths About Best Online Companies To Work For: Dispelled work from home opportunities
8 Tips To Increase Your Railroad Injuries Claim Game lynchburg railroad injuries lawsuit
Why Adding A Glazing Repairs Near Me To Your Life’s
Journey Will Make The An Impact Double glazing repairs
What You Should Be Focusing On Improving Upvc Windows
Repair Window repairs
You’ll Never Guess This Treadmill Folded Up’s Benefits treadmill folded up
The 10 Scariest Things About Male Adult Toys male Adult toy
The 10 Most Scariest Things About List Of Online Shopping Sites In Uk
list of online shopping sites in uk [Seznam-autobusu.cz]
Das Boomerang Casino ist bei vielen Spielern beliebt, nicht zuletzt aufgrund seines attraktiven Bonusangebots und der groГџen Auswahl an Spielen. Doch wie sieht es mit den Auszahlungen aus? In diesem Artikel werden wir uns genauer mit der Dauer der Auszahlungen im Boomerang Casino befassen.
Generell ist die Auszahlungsdauer in Online-Casinos ein wichtiges Kriterium für die Spieler, da sie natürlich möglichst schnell über ihre Gewinne verfügen möchten. Im Boomerang Casino beträgt die durchschnittliche Auszahlungsdauer etwa 1-3 Werktage, je nach gewählter Zahlungsmethode. Bei E-Wallets wie Skrill oder Neteller sind die Auszahlungen tendenziell schneller, während Banküberweisungen etwas länger dauern können.
Um eine Auszahlung im Boomerang Casino zu tätigen, müssen Spieler zunächst ihre Identität verifizieren. Dies geschieht in der Regel durch das Einreichen von Kopien bestimmter Dokumente wie Personalausweis, Führerschein oder Reisepass. Sobald die Verifizierung abgeschlossen ist, kann die Auszahlung beantragt werden.
Ein wichtiger Faktor für die Dauer der Auszahlungen im Boomerang Casino ist auch die Bearbeitungszeit des Casinos selbst. Diese kann je nach Auslastung variieren, liegt aber in der Regel im akzeptablen Bereich. Es ist jedoch ratsam, die genauen Bedingungen für Auszahlungen im Boomerang Casino zu überprüfen, um Enttäuschungen zu vermeiden.
Insgesamt kann gesagt werden, dass die Auszahlungsdauer im Boomerang Casino durchaus zufriedenstellend ist und sich im branchenüblichen Rahmen bewegt. Wer also seine Gewinne schnell und unkompliziert erhalten möchte, ist im Boomerang Casino gut aufgehoben. Mit der richtigen Zahlungsmethode und einer schnellen Verifizierung kann man sein Geld hier innerhalb weniger Tage auf dem Konto haben.
https://boomerangcasino.one/
Seven Reasons Why Double Glazing Windows Near Me Is So Important double glazing windows near me
This Story Behind Sex Machines Shop Is One That Will Haunt You Forever!
Girls Sex Machines
10 Things You Learned In Kindergarden To Help You Get Started With Railroad Injuries Litigation railroad injuries lawyers
5 Treehouse Canopy Leçons From The Pros treehouse
bed frame (Cinda)
Why Nobody Cares About Window Replacement Window
Replacement Panes [https://Gokseong.Multiiq.Com/]
15 Things Your Boss Wishes You’d Known About Auto Locksmith
Near Me Prices locksmith auto key programming (Lucie)
See What Pavement Mobility Scooter With Lithium Battery Tricks The Celebs Are Using pavement mobility scooter with lithium battery (http://Www.Gaiaonline.com)
Window Repairs Near Me Techniques To Simplify Your Daily Life Window Repairs Near Me Trick That
Every Person Must Be Able To Window Repairs Near Me
See What Repair Upvc Windows Tricks The Celebs Are Using repair upvc windows (cheekedger8.bravejournal.net)
На сайте https://roossa.ru/ представлены лучшие книги популярного издательского дома «РООССА». Всем желающим доступна оперативная и бесплатная доставка при покупке от 2 500 рублей. В разделе представлены детские книги, для школьников, сказки для детей, раскраски, аудиосказки с книгой, стихотворения для детей, удивительные рассказы, говорящие игрушки, книги рецептов и многое другое, что позволит провести время с пользой для кругозора. Также имеются и подарочные книги, а также эксклюзивные издания.
Leather Sleeper Sofa 101 Your Ultimate Guide For Beginners American leather sleeper Sofa
The Ultimate Guide To Double Glazing Deals Near Me Double glazed Windows Handles
сайт iherb промокод айхерб рф
Five Killer Quora Answers To Window Repairman Window Repair
11 Strategies To Refresh Your Buy Mobility Scooters Buy Used Mobility Scooter Near Me
20 Trailblazers Lead The Way In Car Accidents Lawyer accident car Attorney (ring-curry-4.blogbright.net)
Das Zet Casino bietet seinen Spielern eine spannende Auswahl an Spielen und groГџzГјgigen Bonusangeboten. Eines der beliebtesten Angebote sind die 30 Freispiele, die neue Spieler bei ihrer ersten Einzahlung erhalten.
Mit diesen 30 Freispielen haben die Spieler die Möglichkeit, verschiedene Spielautomaten im Zet Casino kostenlos zu testen und dabei echte Gewinne zu erzielen. Die Freispiele werden automatisch gutgeschrieben, sobald die erste Einzahlung getätigt wurde, und können direkt genutzt werden.
Um die 30 Freispiele zu erhalten, muss man lediglich ein neues Konto im Zet Casino erstellen und eine Einzahlung tätigen. Neben den Freispielen gibt es auch einen großzügigen Willkommensbonus, der die ersten Einzahlungen der Spieler deutlich aufwertet.
Das Zet Casino bietet eine vielfГ¤ltige Auswahl an Spielautomaten, Tischspielen und Live Casino Spielen von renommierten Anbietern wie NetEnt, Microgaming und Play’n GO. Die Spiele sind sowohl am Desktop als auch mobil verfГјgbar, sodass die Spieler jederzeit und Гјberall auf ihr Lieblingsspiel zugreifen kГ¶nnen.
Insgesamt bietet das Zet Casino seinen Spielern ein erstklassiges Spielerlebnis mit tollen Bonusangeboten, einer breiten Spielauswahl und einem professionellen Kundenservice. Die 30 Freispiele sind nur der Anfang – im Zet Casino warten noch viele weitere spannende Aktionen auf die Spieler.
https://zetcasino.one/
10 Nissan Key Replacement Tricks Experts Recommend programmers
7 Things About Double Glazing Window Repairs Near Me You’ll
Kick Yourself For Not Knowing Double glazing window
This Is The Ultimate Cheat Sheet For Online Shopping 76X152 Cm beach towels
10 Things We Are Hating About Marc Jacobs Handbags Sale marc jacobs bags Outlet
The Best Way To Explain Semi Truck To Your Boss Semi Trucking
The Ultimate Guide To Mesothelioma Legal Asbestos Attorney
20 Things Only The Most Devoted Window Repair Near Fans Should
Know replacements
You’ll Never Be Able To Figure Out This Trusted Online Shopping Sites For Clothes’s Secrets Trusted online Shopping sites for clothes
https://mexicanpharmacy1st.com/# mexican drugstore online
9 Lessons Your Parents Taught You About Replace Window Handles replace window handles
5 Facts Avon Online Shopping Is A Good Thing Avon Online Uk
15 Best Private ADHD Assessment UK Bloggers You Must Follow Best Private Adhd Assessment Uk
15 Espresso Machines Bloggers You Should Follow espresso coffee maker (Sidney)
An Easy-To-Follow Guide To Double Ended Silicone Dildo dildos double, Melvin,
Upvc Window Repairs Near Me Tools To Ease Your Daily Life Upvc Window Repairs Near Me Trick Every Individual
Should Be Able To window repairs near Me
Where Can You Get The Most Reliable Adhd Treatment Information? Treatments For Adhd
The People Nearest To Best CSGO Case Opening Sites Share
Some Big Secrets Case Esports, https://Www.Deepzone.Net/,
20 Fun Facts About All SEO Company In London top Marketing companies in uk
Repair Upvc Window: A Simple Definition upvc Window repairs
13 Things You Should Know About Used Mobility Scooters For
Sale Near Me That You Might Never Have Known used foldable mobility scooters
for Sale – wikimapia.org –
15 Things You’ve Never Known About Cost Of Replacement Windows Uk installers
скидка в айхерб код
15 Of The Best Pinterest Boards All Time About Upvc Window Repairs window repairs near me
iherb coupon code
What Audi Key Fobs Should Be Your Next Big Obsession Audi replacement key cost uk
The Main Issue With Leeds Door And Window, And How You Can Fix It
near me
10 Top Mobile Apps For Work From Home Jobs With No Experience
work From home ideas
brand cialis arrange – apcalis stretch penisole grim
Boomerang Casino – Spielvergnügen ohne Einzahlung
Immer mehr Online-Casinos bieten Spielern die Möglichkeit, ohne Einzahlung zu spielen und dennoch echte Gewinne zu erzielen. Ein solches Casino, das diese Möglichkeit anbietet, ist das Boomerang Casino. Bei Boomerang Casino können Spieler ihre Lieblingsspiele genießen, ohne Geld einzahlen zu müssen.
Das Boomerang Casino bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele und Live-Casino-Spiele. Der Spaß ist garantiert, auch ohne eigenes Geld einzusetzen. Spieler können die verschiedenen Spiele im Demo-Modus ausprobieren und sich so mit den Regeln und Abläufen vertraut machen, bevor sie ihr Glück mit Echtgeldeinsätzen versuchen.
Dank des Boomerang Casino no deposit Angebots haben Spieler die Möglichkeit, risikofrei und ohne finanzielles Risiko zu spielen und dennoch die Chance auf echte Gewinne zu haben. Dies ist besonders attraktiv für Spieler, die sich erst einmal in einem neuen Casino umsehen möchten, bevor sie eine Einzahlung tätigen.
Das Boomerang Casino überzeugt nicht nur mit seinem großzügigen no deposit Angebot, sondern auch mit einem benutzerfreundlichen Interface, schnellen Auszahlungen und einem professionellen Kundenservice. Spieler können sich somit auf ein rundum gelungenes Spielerlebnis freuen.
Insgesamt bietet das Boomerang Casino eine attraktive Möglichkeit, um ohne Einzahlung zu spielen und dennoch echte Gewinne zu erzielen. Spieler können sich auf spannende Spiele, faire Gewinnchancen und erstklassigen Service freuen. Wer also auf der Suche nach einem unterhaltsamen und sicheren Online-Casino ist, sollte das Boomerang Casino auf jeden Fall ausprobieren.
https://boomerangcasino.one/
5 Reasons To Be An Online Real Money Slots And 5 Reasons You Shouldn’t Mobile-Friendly Slots
20 Questions You Need To To Ask About Folding Wheelchair Before You Buy Folding Wheelchair buy folding wheelchair
(M.simeun.com)
The Advanced Guide To Best Online Shopping Websites Uk Bumper Support Corolla
Play Blackjack Online – Some Basic Tips And Tactics 온라인카지노사이트
Slot Demo Gratis Pragmatic Play No Deposit: The History Of Slot Demo Gratis
Pragmatic Play No Deposit In 10 Milestones Slots demo pragmatic
5 Killer Quora Answers On Replacement Double Glazing Units Near Me double
glazing units near me (Stacie)
15 Online Shopping Websites Clothes Benefits You Should
All Be Able To women’s designer briefcase
Five Killer Quora Answers On Online Clothes Shopping Sites Uk Online Clothes Shopping Sites Uk
How To Explain Bound And Gagged To Your Grandparents Cheese
16 Must-Follow Facebook Pages For Mens Masturbation Toy-Related Businesses Male Mastubator
Prada Handbag Man Techniques To Simplify Your Everyday Lifethe Only Prada
Handbag Man Trick Every Person Should Know prada Handbag man
This Week’s Most Remarkable Stories About Automotive Lock
Smith automotive locksmith services (https://Bysee3.com/)
The Three Greatest Moments In Bunk Bed L Shape History Bunk Bed With Storage
3 Ways That The Leeds Windows Can Influence Your Life double glazing door repairs (http://Subaruforum.lv/User/lyrealley45)
Medium Variance Slots: What’s New? No One Is Talking About mobile-friendly slots (9d0bpqp9it2sqqf4nap63f.com)
10 Of The Top Mobile Apps To Use For Mesothelioma Lawsuit
fitzgerald mesothelioma law firm
Online Shopping Website In London Tools To Improve Your Daily Life Online Shopping Website In London Trick
That Everybody Should Know online shopping website in london (https://tujuan.grogol.us/go/aHR0cHM6Ly92aW1lby5jb20vOTMwNDc0NDgx)
Why You Should Concentrate On Enhancing Uk Online Shopping Sites Like
Amazon Panoramic Photo Frame
15 Tread Mills Benefits That Everyone Should Know treadmills (Candelaria)
mexican pharmacy: pharmacies in mexico that ship to usa – reputable mexican pharmacies online
It’s True That The Most Common Upvc Windows Repair
Debate Doesn’t Have To Be As Black And White As You May Think upvc window
repairs (Dnpaint.co.kr)
The Reason Private Mental Health Services Is Everyone’s Passion In 2023
Mental Health Assessment Private
20 Best Tweets Of All Time Car Accidents Attorneys houston Car wreck attorney
Why You Should Concentrate On Making Improvements To Skoda
Kodiaq Key skoda key Replacement near me
Then You’ve Found Your Railroad Injuries Attorneys …
Now What? snellville railroad injuries attorney
Kit Avon Tools To Enhance Your Life Everyday avon starter Kit 2024
You’ll Never Guess This Window Repair Near Me’s Benefits Window Repair near me
What’s The Job Market For Gotogel Link Alternatif Professionals?
gotogel link alternatif
9 Things Your Parents Taught You About Truck Accident Lawyer Near Me
truck accident lawyer Near me
A Time-Travelling Journey: What People Discussed About Repairs To Double Glazed Windows 20 Years Ago window repairs
11 Methods To Refresh Your Small American Fridge Freezers American Style Fridge [Te.Legra.Ph]
mexican mail order pharmacies medication from mexico pharmacy medicine in mexico pharmacies
Boomerang Casino ist ein brandneues Online-Casino, das Spielern eine Vielzahl von spannenden Spielen und groГџzГјgigen Boni bietet. In diesem Artikel werden wir eine eingehende Bewertung des Casinos geben und herausfinden, ob es das richtige fГјr Sie ist.
Das Casino bietet eine breite Auswahl an beliebten Spielen von fГјhrenden Softwareanbietern wie NetEnt, Microgaming, Play’n GO und vielen mehr. In der Spielbibliothek finden Sie eine Vielzahl von Spielautomaten, Tischspielen, Live-Casino-Spielen und vielem mehr. Egal, ob Sie ein Fan von klassischen Slots, Blackjack, Roulette oder Poker sind, hier ist fГјr jeden Geschmack etwas dabei.
Ein weiterer großer Vorteil von Boomerang Casino sind die großzügigen Boni und Promotionen, die sie ihren Spielern anbieten. Neue Spieler werden mit einem lukrativen Willkommensbonus belohnt, der sie auf ihren ersten Einzahlungen mit Bonusgeld und Freispielen verwöhnt. Darüber hinaus gibt es regelmäßig Aktionen und Turniere, bei denen die Spieler die Chance haben, zusätzliche Belohnungen zu gewinnen.
Das Casino ist auch für seine sichere und faire Spielumgebung bekannt. Es verfügt über eine Lizenz von der Malta Gaming Authority und verwendet die neueste SSL-Verschlüsselungstechnologie, um sicherzustellen, dass alle Transaktionen und persönlichen Daten der Spieler sicher und geschützt sind. Darüber hinaus werden alle Spiele regelmäßig von unabhängigen Prüfstellen auf Fairness und Zufälligkeit überprüft.
Insgesamt hat Boomerang Casino viel zu bieten und ist definitiv eine gute Wahl für Spieler, die nach einer unterhaltsamen und sicheren Spielumgebung suchen. Mit einer breiten Auswahl an Spielen, großzügigen Boni und einer zuverlässigen Lizenzierung ist es ein Casino, das es zu testen lohnt. Besuchen Sie noch heute Boomerang Casino und sehen Sie selbst, was es alles zu bieten hat. Viel Glück beim Spielen!
https://boomerangcasino.one/
Why You Should Not Think About Improving Your Semi Truck
Compensation weatherford semi Truck accident lawsuit
The Reasons Krups Nespresso Machines Is Everywhere This
Year nespresso coffee machine
Guide To Link Alternatif Gotogel: The Intermediate Guide On Link Alternatif Gotogel Link alternatif Gotogel
Three Greatest Moments In Personal Injury Litigation History Vernon hills personal injury lawyer
5 Killer Quora Answers To Prada Bag Tote Prada Bag Tote
The 10 Scariest Things About Upvc Windows Repairs upvc windows repairs
11 Ways To Completely Revamp Your Uk Online Shoe
Shopping Websites vimeo
The 10 Most Scariest Things About Good Online Shopping Sites Uk good online shopping sites uk (design.bw-grafics.de)
The History Of Windows Repair glazing
Guide To Double Glazing Repairs Near Me: The Intermediate
Guide The Steps To Double Glazing Repairs Near Me double glazing repairs near Me
The 10 Scariest Things About Upvc Windows Repairs upvc
windows repairs; qooh.me,
You’ll Never Be Able To Figure Out This Hyundai Car Key Replacement’s Tricks Hyundai car key
What’s The Current Job Market For Uk Online Phone Shopping Sites
Professionals? uk online phone shopping Sites
5 Clarifications On Auto Accident Claims Lawyers For Auto Accident Near Me
The 10 Most Terrifying Things About Auto Attorneys Near Me Auto Attorneys Near Me
Everything You Need To Know About Windows And Doors Leeds
Dos And Don’ts Upvc Door Repairs Leeds
10 Best Books On Repair Misted Double Glazing Near Me Misted double glazing
Zet Casino Auszahlungslimit
Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und groГџzГјgigen Bonusangeboten fГјr seine Kunden bietet. Wenn es jedoch um Auszahlungen geht, gibt es bestimmte Limitierungen, die Spieler beachten mГјssen.
Das Auszahlungslimit bei Zet Casino beträgt 10.000 Euro pro Monat. Das bedeutet, dass Spieler während eines Monats nicht mehr als 10.000 Euro aus ihrem Konto abheben können. Diese Limitierung kann für einige Spieler frustrierend sein, vor allem wenn man größere Gewinne erzielt.
Es ist wichtig zu beachten, dass das Auszahlungslimit nicht für progressive Jackpots gilt. Wenn ein Spieler einen progressiven Jackpot knackt, wird der volle Betrag sofort ausgezahlt, unabhängig von der Höhe des Jackpots.
Um das Auszahlungslimit zu umgehen, können Spieler ihre Auszahlungen aufteilen und in mehreren Transaktionen tätigen. Dies bedeutet, dass sie innerhalb eines Monats mehrere Auszahlungen von jeweils bis zu 10.000 Euro vornehmen können.
Zet Casino bietet auch High Roller Spielern die Möglichkeit, individuelle Auszahlungslimits zu vereinbaren. Wenn ein Spieler regelmäßig hohe Beträge gewinnt und auszuzahlen möchte, kann er sich an den Kundensupport wenden und ein höheres Auszahlungslimit beantragen.
Insgesamt ist das Auszahlungslimit bei Zet Casino eine Standardpraxis in der Online-Casino-Branche und dient dazu, die finanzielle Sicherheit des Casinos und der Spieler zu gewährleisten. Es ist wichtig, die Bedingungen und Limitierungen des Casinos zu kennen, um Enttäuschungen zu vermeiden.
Wenn Spieler das Auszahlungslimit bei Zet Casino im Auge behalten und ihre Auszahlungen entsprechend planen, können sie weiterhin die aufregenden Spiele und möglichen Gewinne des Casinos genießen.
https://zetcasino.one/
The History Of 18-Wheeler Wreck Lawyer Horseheads 18 Wheeler Accident Lawsuit
http://mexicanpharmacy1st.com/# purple pharmacy mexico price list
Cheapest Beko Washing Machine Is The Next Hot Thing In Cheapest Beko Washing
Machine cheapest beko washing machines (steen-bekker.hubstack.net)
How Do You Know If You’re Set For Glass Repair Leeds door repairs leeds (https://maps.google.cat/)
11 “Faux Pas” That Are Actually OK To Make With Your Door Fitting Leeds new glazing Leeds
10 Things Your Competitors Can Teach You About Bentley Continental Key Fob remote
10 Things Everyone Hates About Mesothelioma Lawsuit Roseburg mesothelioma Attorney
You’ll Never Guess This Sleeper Sofa With Storage’s Secrets
sleeper sofa with storage (Cleveland)
5 Killer Quora Answers To Repair Misted Double Glazing Near
Me Double Glazing Near Me
service centers
Will Upvc Window Repairs Ever Be The King Of The World?
window repairs Near Me
15 Of The Top Espresso Maker Bloggers You Need To Follow mini espresso machine – http://toolbarqueries.google.co.nz/url?sa=i&url=https://valetinowiki.racing/wiki/10_Sites_To_Help_You_Learn_To_Be_An_Expert_In_Espresso_Machines,
What’s The Current Job Market For Double Glazed
Window Repairs Professionals? double Glazed window repairs
10 Untrue Answers To Common Best Kids Bunkbeds Questions Do You Know
The Correct Answers? kids’ Bed
What Is The Secret Life Of Misted Double Glazing Repairs
Near Me Double Glaze doors
You’ll Never Be Able To Figure Out This Greenpower Electric Scooters’s Benefits Power electric scooter
Ten Easy Steps To Launch The Business Of Your Dream Under Counter Fridge
Business frydge.Uk
Five Killer Quora Answers To Double Glazed Window Repairs
Near Me double glazed window repairs near Me
20 Bmw Key Fob Replacement Websites That Are Taking The Internet By Storm local
The 10 Scariest Things About Rabbit Vibrators Uk rabbit vibrators uk (Josie)
Das Boomerang Casino ist eine aufregende Online-Glücksspielplattform, die auch über mobile Geräte zugänglich ist. Mit dem Boomerang Casino Mobiili können Spieler ihre Lieblingsspiele unterwegs genießen, egal wo sie sich befinden.
Das mobile Casino bietet eine beeindruckende Auswahl an Spielen, darunter Slots, Tischspiele, Live-Casinospiele und vieles mehr. Dank der fortschrittlichen Technologie können Spieler ein nahtloses Spielerlebnis auf ihren Smartphones oder Tablets genießen, ohne auf Qualität oder Geschwindigkeit verzichten zu müssen.
Das Boomerang Casino Mobiili ist benutzerfreundlich und einfach zu navigieren. Spieler können sich mit ihren bestehenden Konten anmelden oder ein neues Konto erstellen, um von exklusiven Boni und Promotionen zu profitieren. Zahlungen können sicher und bequem über verschiedene Zahlungsmethoden abgewickelt werden.
Darüber hinaus bietet das Boomerang Casino Mobiili einen zuverlässigen Kundensupport, der rund um die Uhr verfügbar ist, um bei Fragen oder Anliegen zu helfen. Spieler können sich auf einen professionellen Service verlassen, der sicherstellt, dass ihr Spielerlebnis reibungslos und unterhaltsam ist.
Insgesamt bietet das Boomerang Casino Mobiili eine unterhaltsame und aufregende Möglichkeit, Casinospiele zu genießen, egal wo man sich gerade befindet. Die mobile Plattform ist ideal für Spieler, die flexibles und bequemes Spielen bevorzugen. Probieren Sie das Boomerang Casino Mobiili noch heute aus und erleben Sie die Welt des Online-Glücksspiels in Ihrer Handfläche. Viel Glück und viel Spaß beim Spielen!
https://boomerangcasino.one/
Test: How Much Do You Know About Birth Injury Lawyers?
birth injuries – Christy –
The Little Known Benefits Of Treatment For Adhd Adults adult Adhd treatment London
На сайте https://dostavka-shashlyk.ru закажите звонок для того, чтобы воспользоваться доставкой вкусного, ароматного, сочного шашлыка, который подарит невероятную радость. Вас обрадует оперативная доставка по городу Орел. Также здесь можно приобрести и куриные крылышки, шаурму, люля. Все блюда выполнены из свежих, отборных ингредиентов, за счет чего они тают во рту. Вы будете наслаждаться каждым кусочком. Воспользуйтесь бесплатной доставкой по Орлу, которая доступна вам при покупке от 1000 рублей.
“Ask Me Anything:10 Responses To Your Questions About Prada Handbag Nylon prada milano bag (Hong)
10 Quick Tips About Birth Defect Lawsuit vimeo
How CSGO Case Battle Sites Has Become The Most Sought-After
Trend In 2023 case glove (Juliann)
The Biggest Issue With Online Clothes Shopping Sites Uk, And
How You Can Repair It vimeo.com
You’ll Never Guess This Asbestos Lawyer’s Tricks asbestos Law
Zet Casino ist ein beliebtes Online-Casino, das Spielern eine Vielzahl von Spielen und Unterhaltungsmöglichkeiten bietet. Eines der Highlights dieses Casinos ist das Zet Casino Forum, in dem Spieler sich austauschen, Tipps geben und Erfahrungen teilen können.
Das Zet Casino Forum ist eine großartige Möglichkeit, um mit anderen Spielern in Kontakt zu treten und sich über die neuesten Entwicklungen und Angebote des Casinos auszutauschen. Hier können Spieler ihre Lieblingsspiele diskutieren, Erfolge feiern und auch Fragen stellen, wenn sie Hilfe benötigen.
Das Forum ist in verschiedene Kategorien aufgeteilt, die es den Spielern erleichtern, sich zu bestimmten Themen zu äußern. Zum Beispiel gibt es Threads zu den neuesten Spielveröffentlichungen, Bonusangeboten, Zahlungsmethoden und vielem mehr.
Darüber hinaus bietet das Zet Casino Forum Spielern die Möglichkeit, an exklusiven Aktionen und Wettbewerben teilzunehmen, die nur für Forenmitglieder verfügbar sind. Dies kann eine großartige Gelegenheit sein, um zusätzliche Preise und Belohnungen zu gewinnen.
Das Zet Casino Forum ist auch eine gute Informationsquelle für alle, die mehr über das Online-Casino erfahren möchten. Hier finden Spieler Tutorials, Guides und Tipps, die ihnen helfen können, ihre Spielerfahrung zu verbessern und erfolgreicher zu sein.
Insgesamt ist das Zet Casino Forum eine großartige Ergänzung zu diesem beliebten Online-Casino und bietet eine interaktive Plattform für Spieler, um sich auszutauschen und zu vernetzen. Wer also auf der Suche nach einer Community ist, die die Leidenschaft für Glücksspiele teilt, sollte unbedingt einen Blick auf das Zet Casino Forum werfen.
https://zetcasino.one/
11 Strategies To Completely Redesign Your Online Shop cheap online shopping uk clothes (http://www.leawo.cn/)
The 10 Most Terrifying Things About Best Adult Toys For Men Best Adult Toys For Men
15 Top Pinterest Boards From All Time About Online Shop Baby Wrap Bodysuit
mexican drugstore online: medicine in mexico pharmacies – mexican online pharmacies prescription drugs
9 . What Your Parents Teach You About Window Doctor Near Me Window Doctor Near Me
5 Killer Quora Answers On Double Glazed Near Me double glazed Near Me
What Experts Say You Should Learn asbestos Legal
Panty Vibrator Tools To Make Your Day-To-Day Life Sex pantis
Double Glazing Lock Repair Tips From The Best In The Industry
window Doctor near me
Upvc Windows Near Me Tools To Help You Manage Your Daily Life Upvc Windows Near Me Trick Every Individual Should Learn Upvc windows near me
Ten 12kg Washing Machines That Really Help You Live Better 12Kg Washing
Machines – https://Beautyhack.Ru/Mail?T=Goaway&Link=Https://Www.Cheaperseeker.Com/U/Bandreward7,
Looking Into The Future What Will The Symptoms Of Adhd In Adults
Test Industry Look Like In 10 Years? Symptoms Of Adult Female Adhd
10 Online Shopping Website In London-Related Projects To
Extend Your Creativity Red And Blue Visor Lights
The 3 Greatest Moments In Mesothelioma History clear lake mesothelioma attorney
10 Simple Ways To Figure The How Many Cases Are There In CSGO You’re
Looking For cs2 case, Amado,
Guide To Mens Sexy Toys: The Intermediate Guide To Mens Sexy Toys Mens Sexy Toys
7 Things You’ve Never Known About Buying Online From Uk To Ireland Secure locking Server rack
This Is How Car Diagnostic Near Me Will Look Like In 10 Years’ Time How Much Is A Car Diagnostics Test
The Advanced Guide To Online Shopping Sites Uk Designer Ceiling Fan
10 Things You’ll Need To Be Aware Of Uk Online Phone Shopping Sites Swiss Ball Exercise Game
В нашем обществе, где диплом является началом удачной карьеры в любой сфере, многие пытаются найти максимально быстрый путь получения качественного образования. Наличие официального документа об образовании трудно переоценить. Ведь именно он открывает дверь перед людьми, желающими начать трудовую деятельность или продолжить обучение в университете.
В данном контексте наша компания предлагает оперативно получить этот необходимый документ. Вы сможете заказать диплом, и это является отличным решением для всех, кто не смог завершить обучение, потерял документ или хочет исправить свои оценки. Любой диплом изготавливается с особой аккуратностью, вниманием ко всем элементам. В итоге вы сможете получить 100% оригинальный документ.
Преимущества подобного подхода заключаются не только в том, что вы оперативно получите свой диплом. Процесс организован просто и легко, с профессиональной поддержкой. От выбора нужного образца до консультации по заполнению личной информации и доставки по стране — все под абсолютным контролем квалифицированных специалистов.
Всем, кто ищет максимально быстрый способ получить необходимый документ, наша услуга предлагает отличное решение. Приобрести диплом – значит избежать долгого обучения и не теряя времени перейти к достижению своих целей, будь то поступление в ВУЗ или начало успешной карьеры.
Купить диплом Московского института аналитической психологии и психоанализа
medicine in mexico pharmacies mexican rx online mexican rx online
An Mesothelioma Lawsuit Lawyer Success Story You’ll Never Believe Determining Mesothelioma Lawyers
What Are The Reasons You Should Be Focusing On Improving What CSGO Cases Have Butterfly Knives chroma case
Why Car Accident Lawyer Is Your Next Big Obsession los Angeles car accident Attorney
You’ll Be Unable To Guess Motor Vehicle Case’s
Benefits Charleston Motor Vehicle Accident Attorney
Nine Things That Your Parent Taught You About Best Clitorial Vibrator clitorial Vibrator
How Do You Explain Double Glazing Repair Near Me To A Five-Year-Old repair double glazing windows
What’s The Current Job Market For Double Glazed Window Repairs
Professionals? double glazed window Repairs
The 10 Most Terrifying Things About A+++ Tumble Dryer Heat Pump a+++ tumble dryer heat pump
9 Things Your Parents Taught You About Michael Kors Bags Sale michael kors bags sale
Best Adhd Medication For Adults Tips From The Best In The Business adult add medications
Why You Should Concentrate On Improving Kids Bunk Bed kids furniture
(Zack)
Where Do You Think Upvc Window Repairs Be 1 Year From Right Now?
upvc window repairs near me – Aracely,
10 Car Key Replacement Ford Tricks All Experts Recommend replace Ford key
The Ugly The Truth About Accident Compensation Vimeo.com
See What Treadmill For Sale Near Me Tricks The Celebs Are Making Use Of
treadmill for sale
24-Hours To Improve Washer And Dryer Combination washer dryer combos
There’s A Reason Why The Most Common Birth Defect Attorney Debate Isn’t As Black And White As You
Might Think Vimeo.com
https://mexicanpharmacy1st.shop/# mexico drug stores pharmacies
3 Ways The Adult Toy For Men Will Influence Your Life rabbit adult toy (Julie)
The Secret Secrets Of Tommy Hilfiger Crossbody
Handbag tommy hilfiger sale handbags [Rickie]
Das Zet Casino ist nicht nur für seine beeindruckende Auswahl an Spielen und großzügigen Boni bekannt, sondern auch für seinen attraktiven no deposit Bonus. Ein no deposit Bonus ist ein Bonus, den Spieler erhalten können, ohne eine Einzahlung tätigen zu müssen. Dieser Bonus ist besonders beliebt bei Spielern, die das Casino erst einmal ausprobieren möchten, ohne gleich ihr eigenes Geld einzusetzen.
Der no deposit Bonus im Zet Casino ermöglicht es neuen Spielern, 10 Freispiele für ausgewählte Spielautomaten zu erhalten, ohne eine Einzahlung vornehmen zu müssen. Um diesen Bonus zu erhalten, müssen Spieler lediglich ein Konto im Zet Casino erstellen und den Bonuscode eingeben. Die Freispiele werden dann automatisch gutgeschrieben und können sofort genutzt werden. Es ist wichtig zu beachten, dass Gewinne aus Freispielen in der Regel Bonusbedingungen unterliegen und erst ausgezahlt werden können, wenn diese erfüllt sind.
Der no deposit Bonus im Zet Casino ist eine großartige Möglichkeit, das Casino und seine Spiele kostenlos kennenzulernen. Es ist eine risikofreie Möglichkeit, die Plattform auszuprobieren und zu sehen, ob sie den eigenen Vorlieben entspricht. Darüber hinaus haben Spieler die Chance, echte Gewinne zu erzielen, ohne dafür selbst Geld einzahlen zu müssen.
Insgesamt ist der no deposit Bonus im Zet Casino eine großartige Option, um das Casino und seine Spiele zu erkunden, ohne ein Risiko eingehen zu müssen. Spieler sollten jedoch immer die Bonusbedingungen lesen, um sicherzustellen, dass sie die Bedingungen erfüllen können und ihre potenziellen Gewinne nicht verfallen. Mit dem no deposit Bonus im Zet Casino können Spieler direkt in das Spielvergnügen eintauchen und die aufregende Welt der Online-Casinos erleben.
https://zetcasino.one/
10 Things People Hate About Commercial Truck Accident Attorney truck wreck attorneys; http://www.Fundable.Com,
How To Solve Issues Related To Double Glazing
Shops Near Me Local Double Glazing Repairs
– http://T.Werock.Co.Kr/Member/Login.Html?Refdoc=Member/Login.Html&Nomemberorder&Returnurl=Http%3A%2F%2Fwww.Cheaperseeker.Com%2Fu%2Ftunastory68,
The Greatest Sources Of Inspiration Of Window Repair Near upvc
window repair near me; Finn,
You’ll Never Guess This Trusted Online Shopping Sites For Clothes’s Secrets trusted online shopping sites for clothes
7 Things About Best Auto Accident Lawyers You’ll Kick Yourself For Not Knowing auto Injury lawyers Near me
12 Facts About Upvc Windows And Doors To
Refresh Your Eyes At The Cooler. Cooler upvc Window repairs
Why Sectional Sofas Isn’t A Topic That People Are Interested In. Reclining Sectional Sofa
5 Laws That Will Help The Boating Accident Lawyer Near Me Industry boating accidents lawyer bellingham
9 Lessons Your Parents Taught You About France Online Shopping Sites Clothes france online shopping sites clothes (Thesherryl0ve.hatenablog.Com)
Wisdom On Link Login Gotogel From An Older Five-Year-Old
Go Togel
20 Things You Need To Know About Clean A Fleshlight best feeling fleshlight sleeve (Christopher)
Вас интересует прокат автомобилей по доступным ценам? Вам поможет Rent Me. Сервис предлагает вам выбрать подходящую машину и забронировать. Вы получите по гарантии услугу высшего качества. Все авто проходят техобслуживание, вы можете не переживать о поломках в пути. Ищете словарь в и даля? Rent-me.cy – сайт, который предоставляет прокатные машины на острове Кипр. Процесс аренды мы сделали максимально приятным и простым. Будем рады вам ответить на все вопросы и пообщаться с вами, звоните.
How The 10 Worst Automotive Locksmiths Near Me Fails Of All Time Could Have Been Prevented Local automotive Locksmith
10 Myths Your Boss Is Spreading About American Fridge Freezer Sale smallest american fridge freezer
How To Create An Awesome Instagram Video About Boating Accident Attorneys boat accident lawyer new Jersey
Link Daftar Gotogel Tools To Improve Your
Daily Life Link Daftar Gotogel Trick That Every Person Must Learn link Daftar gotogel
The Most Effective Advice You’ll Ever Receive On Shopping Online
shopping online Sites Clothes
You’ll Be Unable To Guess London Online Clothing
Shopping Sites’s Benefits london online clothing Shopping sites
9 Lessons Your Parents Teach You About Asbestos asbestos (Alicia)
The 10 Most Scariest Things About Good Online Shopping Sites Uk good
online shopping sites uk (http://Www.Scampatrol.org)
Best Washing Machines 9kg Tools To Streamline Your Daily Lifethe One Best Washing Machines 9kg Trick That Should Be
Used By Everyone Know Washing Machines 9Kg
See What Best Online Shopping Uk Clothes Tricks The Celebs Are Making Use Of best online shopping
uk clothes (Clara)
Вам нужна помощь хакера? Обращайтесь скорее к нам, мы предоставляем осуществление любых услуг взлома, гарантируем полную конфиденциальность ваших данных, приемлемые цены, оперативные сроки. Специалист имеет множество осуществленных проектов и приличный опыт. Ищете взломать сайт? Xakerplus.com – сайт, где есть возможность узнать об услугах детальную информацию. Хакер не интересуется, зачем и для чего делаете заказ. Обращайтесь уже сейчас к специалисту, он решит любые задачи!
10 Things Everyone Hates About Adults Toys Shop Discount adult sex toys (http://www.healthndream.Com)
See What Situs Gotogel Terpercaya Tricks The Celebs Are
Using Situs Gotogel Terpercaya
Das Tipico Casino – eine beliebte Online-GlГјcksspielplattform – ist derzeit nicht in Deutschland verfГјgbar. Diese Nachricht hat viele deutsche Spieler enttГ¤uscht, die das Casino gerne nutzen wГјrden. Doch warum ist das Tipico Casino nicht mehr in Deutschland verfГјgbar?
Grund dafür ist, dass das deutsche Glücksspielgesetz sehr streng ist und keine Online-Casinos mit einer Lizenz in Deutschland existieren dürfen. Tipico hat sich dazu entschieden, dem deutschen Markt vorübergehend den Rücken zu kehren, um mögliche rechtliche Konflikte zu vermeiden.
Die Spieler in Deutschland können somit nicht mehr auf das beliebte Tipico Casino zugreifen, was für viele eine Enttäuschung ist. Allerdings gibt es in Deutschland auch andere Glücksspielanbieter, die legal sind und eine Lizenz besitzen. Spieler können auf diese Alternativen ausweichen, um weiterhin ihrem Glücksspielvergnügen nachzugehen.
Es bleibt abzuwarten, ob das Tipico Casino in Zukunft wieder in Deutschland verfügbar sein wird. Bis dahin müssen sich die Spieler nach anderen Optionen umschauen. Es bleibt zu hoffen, dass sich die rechtlichen Rahmenbedingungen für Online-Glücksspiele in Deutschland in Zukunft ändern werden und Spieler wieder uneingeschränkten Zugriff auf ihr bevorzugtes Casino haben werden.
https://tipicocasino.one/
5 Laws Everyone Working In Double Glazing Near Me Should Know uk
Looking Into The Future How Will The Marc Jacobs Handbag
Sale Industry Look Like In 10 Years? marc jacobs bags on Sale; evans-Sauer-3.Thoughtlanes.Net,
12 Companies Leading The Way In Adult Adhd Treatments Treatment Of Adult Adhd
What’s The Current Job Market For Double Glazing Door Repairs Professionals Like?
door Repair
Sugar Defender is a revolutionary blood sugar support formula designed to support healthy glucose levels and promote natural weight loss. https://blackboxvending.com/
You’ll Be Unable To Guess Washer 10kg’s Tricks Washer 10Kg
9 . What Your Parents Taught You About Examples Of Online Shopping
examples of online Shopping
The 12 Best Motor Vehicle Attorneys Accounts To Follow On Twitter webster city motor Vehicle Accident lawyer
5 Killer Quora Answers To Veleco Luxury Electric Scooters
veleco luxury electric scooters (Lucy)
5 Killer Quora Answers On Double Glazed Window Repair Window Repair
What To Look For To Determine If You’re Ready To Masturbators For Men male masturbators (Cecila)
Ten Birth Defect Lawyers Myths You Should Never Share On Twitter billings Birth defect Lawsuit
13 Things About Couches For Sale You May Not
Have Considered love Seat sale
mexican border pharmacies shipping to usa: reputable mexican pharmacies online – buying from online mexican pharmacy
Semi Truck Compensation: The Good, The Bad, And The
Ugly Lawsuits
See What Side By Side Fridge And Freezer Pair Tricks The Celebs Are Making Use Of side By side fridge and freezer pair; https://cse.google.pl/url?sa=t&url=https://www.frydge.uk/products/matte-black-american-side-by-side-fridge-freezer-635l-447,
5 Clarifications On Car Locksmith locksmith for cars near me
Five Things You Didn’t Know About Window Repair Near upvc window Repair near me
Guide To Upvc Repairs Near Me: The Intermediate Guide For Upvc Repairs Near Me upvc repairs near me
15 Unquestionably Good Reasons To Be Loving Upvc
Repairs Near Me repairs to upvc windows (https://rentry.co/9vmy65od)
Everything You Need To Learn About Upvc Double Glazed Windows Upvc Windows Repair Near Me
Three Common Reasons Your Door Fitter Luton Isn’t Performing (And How
To Fix It) Window Replacement Luton
Guide To Auto Ghost Immobiliser: The Intermediate Guide In Auto
Ghost Immobiliser auto ghost Immobiliser, http://www.brauer-reisen.de,
10 Healthy Habits To Use Repair Upvc Windows upvc windows repair (https://api.Linkr.bio)
What’s The Job Market For Renault Scenic Key Professionals?
renault scenic key (oliviabeckford.Co.uk)
Upvc Windows Repair: 10 Things I’d Love To Have Known Earlier repair upvc windows
The 9 Things Your Parents Taught You About Tumble Dryers Heat Pump
tumble dryers heat pump
Do You Think Fiat 500 Replacement Key Fob Never
Rule The World? Fiat 500 spare key cost uk (Extension.unimagdalena.edu.co)
See What Double Glazing South London Tricks The Celebs Are Utilizing double glazing south london – Carl –
You’ll Never Be Able To Figure Out This Upvc Door Repairs
Near Me’s Benefits Upvc door repairs near me
What Is 18-Wheeler Accident Attorney And Why Are We Dissing It?
madison 18 Wheeler accident attorney
Sugar Defender is a revolutionary blood sugar support formula designed to support healthy glucose levels and promote natural weight loss. https://mineryuta.com
Mesothelioma Attorneys Explained In Fewer Than 140 Characters
mesothelioma legal (Josef)
The Most Successful Double Glazed Front Doors Near Me Gurus Can Do 3 Things replacement double glazed windows (Tanya)
5 Laws That Anyone Working In Butt Plugs For Sale Should Be Aware Of lovense butt plug (http://www.chcisexrande.cz)
10 Myths Your Boss Has Concerning Crate And Barrel Sleeper Sofa Sofasandcouches.Com
Your Family Will Be Grateful For Getting This Cheap Rabbit Vibrator Rabbit Vibrators
Boomerang Casino ist eine beliebte Online-GlГјcksspielplattform, die eine Vielzahl von Spielen und groГџzГјgigen Bonusangeboten fГјr Spieler auf der ganzen Welt bietet. Eines der wichtigsten Themen fГјr Spieler, wenn es um Online-Casinos geht, ist die Auszahlungspolitik. In diesem Artikel werfen wir einen genaueren Blick auf die Auszahlungen im Boomerang Casino.
Eine der wichtigsten Fragen, die Spieler haben, ist, wie schnell und einfach sie ihre Gewinne auszahlen lassen können. Im Boomerang Casino können Spieler ihre Gewinne auf verschiedene Arten auszahlen lassen, darunter Banküberweisungen, Kreditkarten, E-Wallets und vieles mehr. Die Auszahlungszeiten variieren je nach Zahlungsmethode, aber das Casino bemüht sich, Auszahlungen so schnell wie möglich zu bearbeiten.
Ein weiterer wichtiger Punkt für Spieler ist die Sicherheit und Zuverlässigkeit der Auszahlungen im Boomerang Casino. Das Casino verwendet die neueste Technologie, um sicherzustellen, dass alle Transaktionen sicher und geschützt sind. Spieler können sich darauf verlassen, dass ihre Gewinne schnell und sicher auf ihr Konto überwiesen werden.
Es ist auch erwähnenswert, dass Boomerang Casino keine versteckten Gebühren für Auszahlungen erhebt. Spieler können ihre Gewinne ohne zusätzliche Kosten auszahlen lassen, was das Casino zu einer attraktiven Option für Spieler macht.
Insgesamt bietet Boomerang Casino eine zuverlässige und sichere Auszahlungsplattform für Spieler, die ihre Gewinne schnell und einfach erhalten möchten. Mit einer Vielzahl von Zahlungsmethoden und schnellen Auszahlungszeiten ist Boomerang Casino eine gute Wahl für alle, die nach einem erstklassigen Online-Casino-Erlebnis suchen.
https://boomerangcasino.one/
A Peek In Adults Toy For Men’s Secrets Of Adults Toy For Men lovense adult toys
(Penney)
What’s The Current Job Market For Double Glazing Near Me Professionals?
double glazing near me
The Most Negative Advice We’ve Ever Seen About SEO Tools SEO Tools seo rankings tool (https://minecraftcommand.Science/profile/organplow6)
pharmacies in mexico that ship to usa reputable mexican pharmacies online mexico drug stores pharmacies
15 Best Backlink Building Software Bloggers You Should
Follow best backlink Building Software
Fiat Replacement Key Tools To Streamline Your Everyday Lifethe Only
Fiat Replacement Key Technique Every Person Needs To Learn fiat Replacement key
12 Companies Are Leading The Way In Birth Injury Attorney In Nyc birth injury settlement
The Reason Why All LG Fridge Models Is Everyone’s
Passion In 2023 cheap lg fridge freezer
You’ll Never Guess This Asbestos Litigation’s Benefits asbestos
You’ll Never Be Able To Figure Out This Double Glazed Units Near Me’s Tricks Double Glazed units Near me
На сайте https://lan-union.ru вы сможете воспользоваться корпоративными сетевыми решениями, аудитом проектов для своих клиентов. Специально для вас разработана умная система индикации. Для того чтобы осуществить покупку, изучите весь каталог продукции. В него входит медный кабель, медные шнуры, а также оптический кабель, коммутационные шнуры оптические, конструктивы и шкафы, а также многое другое. В компании «ЛАН ЮНИОН» вы отыщите все, что необходимо для того, чтобы решить задачи, независимо от уровня их сложности.
Why Sectional Couches For Sale Is Quickly Becoming The Hottest Trend Of 2023 Couches sectional
Хотите приобрести Вегови в Москве по разумной стоимости и с быстрой доставкой? Мы официальный поставщик Вегови и прочих лекарств для мед. центров Москвы. В наличии препарат Вегови всех дозировок. https://wegovy-russia.ru – сайт, где есть фото людей как до, так и после использования. Также предложены и цены на Вегови. Здесь также можете в любое удобное для вас время ознакомиться с отзывами клиентов. Чтобы приобрести Вегови, вам нужно связаться с менеджером по WhatsApp. Вы узнаете, на сколько можно похудеть, как храним Вегови и как он работает.
The Top Reasons Why People Succeed At The Replacement Double Glazing Units Near Me Industry replacement double Glazing units near me
Double Glazing Repairs Near Me Tools To Streamline Your Daily Life Double Glazing Repairs Near Me Trick That Should Be Used By Everyone Learn double glazing repairs near me (https://images.google.co.tz/url?q=http://promarket.in.ua/user/salmonlamp15/)
Why Veleco Can Be Much More Hazardous Than You Think Veleco scooter
What Freud Can Teach Us About Combo Washer Washer Dryer Combinations
11 Ways To Totally Defy Your Beko Washing Machine beko washing Machines prices (peacock-goodwin-2.federatedjournals.com)
https://mexicanpharmacy1st.com/# mexican drugstore online
Your Family Will Thank You For Getting This Are Cases Worth It CSGO case spectrum
5. Accident Settlement Projects For Any Budget mchenry accident Law firm
Why No One Cares About Case Battle CSGO case horizon (Gavin)
Guide To Situs Alternatif Gotogel: The Intermediate
Guide In Situs Alternatif Gotogel situs alternatif gotogel (Kurt)
The Reason Behind Slot Demo Gratis Pragmatic Play
No Deposit Will Be Everyone’s Desire In 2022 Pg slot demo
На сегодняшний день, когда диплом становится началом удачной карьеры в любом направлении, многие пытаются найти максимально быстрый путь получения качественного образования. Факт наличия официального документа об образовании переоценить невозможно. Ведь именно диплом открывает дверь перед всеми, кто стремится вступить в профессиональное сообщество или учиться в университете.
Мы предлагаем быстро получить этот важный документ. Вы можете купить диплом, что становится удачным решением для человека, который не смог закончить обучение или утратил документ. диплом изготавливается аккуратно, с особым вниманием ко всем элементам, чтобы на выходе получился документ, максимально соответствующий оригиналу.
Превосходство такого решения заключается не только в том, что можно быстро получить диплом. Весь процесс организован удобно, с нашей поддержкой. От выбора подходящего образца до консультаций по заполнению личной информации и доставки по России — все под абсолютным контролем опытных специалистов.
Таким образом, для тех, кто пытается найти оперативный способ получить необходимый документ, наша компания предлагает отличное решение. Приобрести диплом – это значит избежать длительного процесса обучения и не теряя времени перейти к своим целям: к поступлению в университет или к началу успешной карьеры.
Купить диплом Гуманитарного института телевидения и радиовещания им. М.А. Литовчина
The Most Sour Advice We’ve Ever Seen About Upvc Window
Repairs Upvc Window Repairs upvc Window repairs near Me
5 Clarifications On Double Glaze Repair Near Me double glazed window near
me (fogh-hodge.hubstack.net)
Slot Strategies 101 A Complete Guide For Beginners online casino Slots (http://vn.easypanme.com/)
Ghost Immobiliser Near Me Tools To Help You Manage Your Daily Lifethe One Ghost Immobiliser Near Me Trick That Everybody Should Be Able To ghost immobiliser near me
Indisputable Proof You Need Uk Online Grocery Shopping Sites Hard Drive Case Usb 3.0
Five Railroad Injuries Lawsuit Lessons From
Professionals chanhassen railroad injuries law firm (https://vimeo.com/708076681)
ВДБГ – компания, которая предлагает приобрести программу 1С. Мы стремимся предоставлять своим клиентам услуги высшего качества. Ориентированы на максимальное удовлетворение ваших потребностей и на долгосрочное сотрудничество. Ищете 1с управление небольшой фирмой купить? Vdgb.ru – здесь найдете на продукты 1С прайс-лист. Также тут ознакомитесь с доставкой и условиями оплаты. При необходимости готовы проконсультировать, на сайте в специальную форму впишите свое имя, контактный номер и E-mail, после чего нажмите на кнопку «Отправить». Оцените комфорт при работе с программой 1С!
The 9 Things Your Parents Taught You About Bmw Replacement Car Keys Bmw Replacement Car Keys [http://Www.Cheaperseeker.Com]
A Comprehensive Guide To Online Shop. Ultimate Guide To Online Shop Battery Powered Gimbal
(Kristen)
What’s The Job Market For Sleeping Couch And Sofa Professionals?
sleeping couch and Sofa
See What Window Repair Leeds Tricks The Celebs Are Using Window Repair Leeds
“The Fleshlight Butt Awards: The Most, Worst, And Most Bizarre Things We’ve Seen sexy Fleshlight
Why Double Glazing Repair Near Me Is Tougher Than You Imagine double glazing Repairs
Double Glazed Window Repair Tips That Can Change Your Life window repairs near me
What Is The Reason Car Accident Attorneys Near Me
Is The Best Choice For You? car accident injury
lawyers near me; https://steenberg-norton.mdwrite.net/dont-believe-these-trends-About-best-Car-Accident-lawyer-near-me/,
10 Inspirational Graphics About Double Glazing Near Me double glazing company near me
Желаете смотреть сериалы русские онлайн в высоком качестве? Ruserial вам поможет в этом. Мы предлагаем вам самый лучший контент. Окунитесь в мир увлекательных эмоций и историй. Ищете русский сериал онлайн мистика? Ruserial-full.net – сайт, который имеет понятный интерфейс. Здесь можно абсолютно бесплатно и без рекламы смотреть интересные сериалы онлайн. На сайте все есть, что вам нужно для неповторимого времяпровождения. Присоединяйтесь к нам уже сейчас. Уверены в том, что вы будете каждым моментом вашего любимого русского сериала наслаждаться.
See What Double Glazing Repair Near Me Tricks The
Celebs Are Using Double glazing repair near me
The 10 Scariest Things About Cheapest Online Grocery Shopping Uk cheapest Online grocery Shopping uk (http://cloud-sc-news.3dns.info.gov.hk)
5 Killer Quora Answers On Double Glazed Window Repairs Near Me Double glazed window Repairs near me
9 Lessons Your Parents Teach You About Online Shopping Sites Clothes Cheap online shopping Sites clothes cheap
Ten Things You Shouldn’t Post On Twitter window Repair Near Me
There Is No Doubt That You Require Designer Handbags Brown designer handbags
on amazon (Phillipp)
See What Double Glazed Windows Near Me Tricks The Celebs Are Utilizing Double glazed windows near me
The 10 Scariest Things About Mobile Auto Locksmith Near Me Mobile Auto Locksmith Near Me
(https://Marvelvsdc.Faith/Wiki/The_History_Of_Auto_Locksmith_Near_Me)
It’s The Complete List Of Double Glazed Window Repair Dos And Don’ts Window repairs Near me
5 Killer Quora Answers On Uk Online Shoe Shopping Websites uk online shoe shopping Websites
It’s Time To Expand Your Birth Injury Settlement Options crystal birth injury attorney
4 Dirty Little Secrets About The Truck Crash Attorney Industry Trucking accident Lawyer
Das Boomerang Casino ist eine vielversprechende Online-Plattform für Glücksspielbegeisterte, die auf der Suche nach spannenden Spielen und attraktiven Boni sind. Besonders interessant sind die Boomerang Casino Freispiele ohne Einzahlung, die Neukunden die Möglichkeit bieten, das Casino risikofrei kennenzulernen und erste Gewinne zu erzielen.
Freispiele sind bei Online-Casinos eine beliebte Art von Bonus, da sie den Spielern die Chance geben, kostenlose Runden an ausgewählten Spielautomaten zu drehen. Boomerang Casino geht noch einen Schritt weiter und bietet neuen Spielern die Möglichkeit, bis zu 50 Freispiele ohne Einzahlung zu erhalten. Das bedeutet, dass man sich einfach nur registrieren muss, um diese attraktiven Free Spins zu erhalten.
Die Freispiele können an verschiedenen Spielautomaten im Boomerang Casino genutzt werden und bieten die Möglichkeit, echte Gewinne zu erzielen, ohne selbst Geld einzahlen zu müssen. Die erzielten Gewinne aus den Freispielen können anschließend als Bonusguthaben genutzt werden, das nach Erfüllung der Umsatzbedingungen ausgezahlt werden kann.
Diese Aktion ist besonders attraktiv für Spieler, die das Boomerang Casino zunächst unverbindlich testen möchten, bevor sie echtes Geld einzahlen. Die Freispiele ohne Einzahlung bieten die perfekte Gelegenheit, die Vielfalt der Spiele im Casino kennenzulernen und erste Gewinne zu erzielen.
Um von den Boomerang Casino Freispielen ohne Einzahlung zu profitieren, müssen sich neue Spieler lediglich auf der Website des Casinos registrieren und den Bonuscode eingeben, um die Freispiele zu aktivieren. Es lohnt sich auf jeden Fall, diese attraktive Bonusmöglichkeit zu nutzen und die Spannung und Unterhaltung im Boomerang Casino zu erleben.
https://boomerangcasino.one/
The Worst Advice We’ve Ever Received On Upvc Window Repairs upvc Repairs
Ten Things You’ve Learned In Kindergarden That Will Aid You In Obtaining Womens Rabbit Vibrators Sex Toy Sextoys Rabbit
Fridge Freezer Cheap Tips From The Best In The Industry Fridge Freezer Near Me
The Most Effective Reasons For People To Succeed On The Veterans Disability Compensation Industry Nederland Veterans Disability Attorney
Where Will Motorcycle Accident Claim Be One Year From Right Now?
Motorcycle Accidents
В нашем мире, где диплом – это начало успешной карьеры в любом направлении, многие ищут максимально простой путь получения качественного образования. Необходимость наличия официального документа переоценить просто невозможно. Ведь именно он открывает двери перед любым человеком, который желает вступить в сообщество профессионалов или продолжить обучение в университете.
Наша компания предлагает быстро получить этот важный документ. Вы можете приобрести диплом, что становится отличным решением для человека, который не смог завершить образование, потерял документ или хочет исправить свои оценки. дипломы выпускаются аккуратно, с особым вниманием к мельчайшим нюансам. На выходе вы сможете получить продукт, 100% соответствующий оригиналу.
Плюсы подобного решения состоят не только в том, что можно быстро получить диплом. Процесс организовывается удобно и легко, с нашей поддержкой. От выбора требуемого образца диплома до консультации по заполнению личных данных и доставки по стране — все под полным контролем качественных специалистов.
Для тех, кто ищет быстрый и простой способ получить необходимый документ, наша компания может предложить выгодное решение. Приобрести диплом – это значит избежать длительного обучения и сразу перейти к достижению собственных целей, будь то поступление в университет или начало карьеры.
Купить диплом Строителя
Ten Pinterest Accounts To Follow About Espresso Machine Sale coffee For espresso machine
How To Make An Amazing Instagram Video About Fiat Ducato Replacement Key fiat ducato key fob
9 Things Your Parents Teach You About Amazon Online Shopping Clothes Uk Amazon Online Shopping Clothes Uk
How To Get More Benefits From Your Upvc Repairs Near
Me repairs to Upvc windows
15 Of The Most Popular Pinterest Boards Of All Time About Double Glazing Firms
Near Me repairing double glazed Windows
Handbags Tommy Hilfiger Tools To Make Your Daily Lifethe One Handbags Tommy Hilfiger
Trick That Should Be Used By Everyone Learn handbags tommy Hilfiger
You’ll Be Unable To Guess London Online Mobile Shopping Sites’s Tricks london online mobile
Shopping sites (http://xilubbs.Xclub.tw/space.php?uid=1316371&do=profile)
What Is The Reason Best Online Shopping Uk Clothes Is Right For You Vimeo.Com
10 Things That Your Family Taught You About Treadmill For Sale Near Me
Treadmill for Sale near me
Five Killer Quora Answers To Situs Alternatif Gotogel
Situs Alternatif Gotogel
10 Life Lessons We Can Learn From Window Repair Near window repair near
me (http://kinglish.com/Bbs/board.php?bo_table=review&wr_id=240529)
best mexican online pharmacies: best online pharmacies in mexico – best mexican online pharmacies
Why Dangerous Drugs Attorney Should Be Your Next Big Obsession? chelsea dangerous drugs Lawsuit
Basic Slot Playing Tips 슬롯 – http://yolo420.com/,
7 Things About Slot Innovations You’ll Kick Yourself For
Not Knowing Slot Symbols
Are You Responsible For An Auto Injury Attorneys
Budget? 12 Tips On How To Spend Your Money automotive lawyers Near me
В нашем мире, где диплом становится началом удачной карьеры в любом направлении, многие ищут максимально простой путь получения образования. Наличие документа об образовании сложно переоценить. Ведь диплом открывает двери перед каждым человеком, желающим вступить в профессиональное сообщество или учиться в любом университете.
Предлагаем очень быстро получить любой необходимый документ. Вы можете купить диплом, и это является удачным решением для всех, кто не смог завершить обучение, потерял документ или хочет исправить свои оценки. дипломы изготавливаются с особой тщательностью, вниманием к мельчайшим элементам. На выходе вы получите полностью оригинальный документ.
Преимущество данного подхода состоит не только в том, что можно максимально быстро получить свой диплом. Весь процесс организовывается просто и легко, с профессиональной поддержкой. От выбора подходящего образца до консультации по заполнению личных данных и доставки по стране — все под полным контролем опытных мастеров.
В результате, для тех, кто ищет быстрый способ получения необходимого документа, наша услуга предлагает отличное решение. Купить диплом – это значит избежать долгого обучения и сразу перейти к своим целям, будь то поступление в университет или старт карьеры.
Купить диплом Московского института управления и сервиса
Guide To Situs Gotogel Terpercaya: The Intermediate Guide
In Situs Gotogel Terpercaya situs gotogel terpercaya
Vauxhall Zafira Key Fob Replacement: A Simple Definition vauxhall key fobs
The 10 Most Scariest Things About Repairs To Upvc Windows upvc Window Repairs
14 Businesses Doing A Superb Job At Motor Vehicle Lawyer Wanaque motor Vehicle accident lawyer
8 Tips To Improve Your Locksmiths For Cars Near Me Game locksmith near me for car
Are You Responsible For A Online Shopping Sites For Clothes Budget?
12 Best Ways To Spend Your Money famous online Shopping sites for clothes
The No. 1 Question Anyone Working In Private ADHD Titration UK Needs To Know How To Answer titration service
[http://galpaodainformatica.com.br/index.php?option=com_K2&view=itemlist&task=user&id=638781]
Why Nobody Cares About Mattress Double double Mattresses uk
The 10 Most Scariest Things About Upvc Repairs Near Me upvc Repairs near me
15 Top Twitter Accounts To Discover Blown Double
Glazing Repairs Near Me Double Glazing Windows (http://Extension.Unimagdalena.Edu.Co/)
Online Casino Boom: Der neue Trend der Boomerang-Spiele
In der Welt der Online-Casinos gibt es ständig neue Trends und Innovationen, die die Spieler begeistern. Eine dieser aufregenden Entwicklungen sind die sogenannten Boomerang-Spiele, die gerade in der Online-Glücksspielbranche für Furore sorgen.
Was sind Boomerang-Spiele? Diese neuen Spiele basieren auf der Idee des “ZurГјckwerfens”, Г¤hnlich wie ein Boomerang, der nach dem Werfen immer wieder zu seinem Ausgangspunkt zurГјckkehrt. In Bezug auf Online-Casinos bedeutet dies, dass Spieler die MГ¶glichkeit haben, ihre Gewinne wieder zurГјckzusetzen und erneut zu gewinnen.
Diese Art von Spielen bietet den Spielern eine einzigartige Möglichkeit, ihr Glück zu versuchen und ihre Gewinne zu maximieren. Der Reiz liegt darin, dass Spieler ihre Gewinne entweder kassieren und sich darüber freuen oder sie erneut einsetzen können, um noch größere Gewinne zu erzielen. Dieses Hin und Her sorgt für einen zusätzlichen Nervenkitzel und eine höhere Spannung.
Die Boomerang-Spiele sind sowohl bei Gelegenheitsspielern als auch bei erfahrenen Zockern beliebt, da sie eine interessante neue Möglichkeit bieten, Spaß zu haben und gleichzeitig echtes Geld zu gewinnen. Die Vielfalt der Spiele reicht von traditionellen Tischspielen wie Blackjack und Roulette bis hin zu aufregenden Slot-Spielen mit innovativen Bonusfunktionen.
Ein weiterer Vorteil der Boomerang-Spiele ist, dass sie oft spezielle Boni und Promotionen bieten, um die Spieler zum Wiederkommen zu ermutigen. Diese können in Form von Freispielen, Einzahlungsboni oder Cashback-Angeboten verfügbar sein und den Spaß am Spiel noch erhöhen.
Es ist klar, dass die Boomerang-Spiele im Online-Casino-Bereich eine aufregende neue Entwicklung sind, die sowohl für Spieler als auch für Betreiber spannende Möglichkeiten bietet. Wenn Sie Lust auf ein neues und innovatives Spielerlebnis haben, dann sollten Sie unbedingt die Boomerang-Spiele ausprobieren und sehen, ob Sie Ihr Glück zurückwerfen können. Wer weiß, vielleicht kehrt das Glück ja wieder zu Ihnen zurück. Viel Spaß und viel Erfolg beim Spiel!
https://boomerangcasino.one/
What’s The Job Market For Black Chest Freezer Professionals?
Chest freezers small uk
5 Killer Quora Answers On Best Online Shopping Websites Uk best Online shopping websites uk
Ten Things You Learned About Kindergarden Which Will Help You With Slot Demo Demo Slot Gacor Maxwin
Guide To Upvc Windows Near Me: The Intermediate Guide On Upvc Windows Near Me
upvc windows near Me (https://www.google.sm/)
10 Undeniable Reasons People Hate Replacement Double Glazing Units Near Me Double glazing unit
5 Killer Quora Answers To Personal Injury Law personal
https://mexicanpharmacy1st.shop/# п»їbest mexican online pharmacies
15 Reasons To Not Be Ignoring Porsche Replacement Key porsche taycan key
What’s The Current Job Market For Double Glazed Window Repairs Professionals?
double Glazed Window repairs
What Is L Beds And Why Is Everyone Dissing It? Bunkbedsstore.uk
medication from mexico pharmacy pharmacies in mexico that ship to usa п»їbest mexican online pharmacies
Planet Spa Sleep Serenity 101:”The Ultimate Guide For Beginners Planet spa
gift set
В нашем обществе, где диплом – это начало отличной карьеры в любом направлении, многие стараются найти максимально быстрый путь получения качественного образования. Факт наличия документа об образовании сложно переоценить. Ведь именно он открывает двери перед любым человеком, желающим начать трудовую деятельность или продолжить обучение в университете.
Предлагаем очень быстро получить этот важный документ. Вы можете купить диплом старого или нового образца, и это становится удачным решением для всех, кто не смог закончить образование, утратил документ или хочет исправить плохие оценки. диплом изготавливается с особой аккуратностью, вниманием ко всем элементам, чтобы в результате получился продукт, полностью соответствующий оригиналу.
Плюсы этого подхода состоят не только в том, что можно быстро получить свой диплом. Весь процесс организован комфортно, с профессиональной поддержкой. Начав от выбора необходимого образца до консультации по заполнению персональной информации и доставки в любой регион страны — все под полным контролем опытных мастеров.
В результате, для тех, кто ищет максимально быстрый способ получить требуемый документ, наша компания предлагает выгодное решение. Купить диплом – значит избежать долгого процесса обучения и сразу переходить к достижению своих целей: к поступлению в университет или к началу трудовой карьеры.
Купить диплом Национального института бизнеса
The One Car Key Replacement Ford Trick Every Person Should Be Able To ford Key programming
What Will Designer Handbags Uk Sale Be Like In 100 Years?
Designer Handbags Used
На сайте https://doka-stroi.ru оставьте заявку для того, чтобы воспользоваться такими популярными услугами, как: ремонт квартир, дизайн интерьера, ремонт комнат. Все услуги оказываются под ключ, а в работе применяются инновационные, уникальные технологии. Услуги оказываются точно в строго оговоренное время, а все обязательства сторон прописываются в договоре. В компании трудится опытная команда специалистов с соответствующим образованием. Имеется собственная материально-техническая база. Все работы проходят строгий контроль на каждом этапе.
5 Can I Buy From A Uk Website Projects For Every Budget Heavy duty garment rack
The Reasons Why Couch Sets For Sale Is The Most Sought-After Topic In 2023 Black Velvet Couch
На сайте https://www.avtogalaktika.com/ оставьте сообщение для того, чтобы воспользоваться займом под ПТС, получить деньги под залог автомобиля, наличные под залог машины, под залог спецтехники. Специально для вас оперативное и выгодное получение кредита. Прямо сейчас вы сможете ознакомиться с тем, какие автомобили сможете приобрести в данную минуту. Перед вами все самые популярные марки машин, которые находятся в отличном состоянии. Для того чтобы получить консультацию, заполните заявку, чтобы вам перезвонил менеджер.
8 Tips To Improve Your CSGO Opening Sites Game case operation bravo,
Forest,
10 Replacement Audi Key Hacks All Experts Recommend audi advanced key
The People Who Are Closest To Ford Car Key Share Some Big Secrets Ford Transit Key Fob Replacement (http://Srv29897.Ht-Test.Ru/Index.Php?Subaction=Userinfo&User=Kittymusic94)
See What Taylors Lazy Sunday Coffee Beans 1kg Tricks The Celebs Are Using beans 1kg
Zet Casino ist eine Online-GlГјcksspielplattform, die in der Welt der Online-Casinos immer beliebter wird. Mit einer breiten Palette an Spielen und attraktiven Bonusangeboten zieht Zet Casino Spieler aus der ganzen Welt an. In diesem Artikel werden wir die Vor- und Nachteile dieses Casinos bewerten.
Vorteile:
1. Große Auswahl an Spielen: Zet Casino bietet eine Vielzahl von Spielen, darunter Spielautomaten, Tischspiele, Live-Casino-Spiele und mehr. Spieler können zwischen Hunderten von Spielen wählen und haben immer etwas Neues zu entdecken.
2. Attraktive Bonusangebote: Zet Casino bietet großzügige Boni für neue Spieler sowie regelmäßige Promotionen und Aktionen für bestehende Spieler. Diese Bonusangebote können die Gewinnchancen der Spieler erhöhen und das Spielerlebnis noch spannender machen.
3. Sichere Zahlungsmethoden: Zet Casino bietet eine Vielzahl von sicheren Zahlungsmethoden, darunter Kreditkarten, E-Wallets und Banküberweisungen. Spieler können sicher und bequem Ein- und Auszahlungen vornehmen, ohne sich Gedanken über die Sicherheit ihrer persönlichen Daten machen zu müssen.
Nachteile:
1. Einschränkungen in einigen Ländern: Zet Casino akzeptiert Spieler aus verschiedenen Ländern, aber es gibt einige Länder, in denen das Spielen auf der Plattform nicht erlaubt ist. Spieler sollten sicherstellen, dass sie die gesetzlichen Bestimmungen ihres Landes kennen, bevor sie sich bei Zet Casino anmelden.
2. Langsame Auszahlungszeiten: Einige Spieler haben berichtet, dass die Auszahlungszeiten bei Zet Casino länger sind als bei anderen Online-Casinos. Dies kann frustrierend sein, insbesondere für Spieler, die ihre Gewinne schnell erhalten möchten.
Insgesamt bietet Zet Casino eine unterhaltsame und sichere Spielumgebung mit einer Vielzahl von Spielen und attraktiven Bonusangeboten. Spieler können sicher sein, dass ihre persönlichen Daten geschützt sind und dass sie faire Gewinnchancen haben. Trotz einiger kleiner Nachteile ist Zet Casino definitiv einen Besuch wert.
Fazit:
Zet Casino ist ein solides Online-Casino mit einer breiten Spielauswahl und attraktiven Bonusangeboten. Spieler, die auf der Suche nach einer unterhaltsamen und sicheren Spielumgebung sind, werden bei Zet Casino sicherlich auf ihre Kosten kommen. Es lohnt sich, dieses Casino auszuprobieren und selbst zu entscheiden, ob es den eigenen AnsprГјchen entspricht.
https://zetcasino.one/
Seven Explanations On Why Car Accident Is Important car wreck lawyers near me
10 Things That Everyone Is Misinformed About The Word “Blown Double Glazing Repairs” window
Doctor near me (leewhan.com)
5 Killer Quora Answers To Cheap Online Grocery Shopping Uk Cheap online grocery shopping uk
What Repairing Double Glazed Windows Experts Want You To Be Educated double glazed Window repairs near me
5 Killer Quora Answers To International SEO Agency international seo agency
This Most Common Beko.Washing Machine Debate Actually Isn’t As Black Or White As You Think beko washing machines (Ahmad)
10 Misleading Answers To Common Online Shopping Sites
London Questions: Do You Know Which Answers? 12-Inch Rain Shower Head
The Unknown Benefits Of Replacement Upvc Window
Handles Upvc Window Repairs near me
The Next Big Trend In The Auto Fold Mobility Scooter Industry electric Automatic folding 4-wheel mobility scooter
9 Lessons Your Parents Taught You About King Sleeper Sofa king sleeper sofa (https://counseling.online.wfu.edu/)
15 Ghost Immobiliser Install Bloggers You Should Follow audi Rs6 ghost installer
В наше время, когда диплом – это начало удачной карьеры в любом направлении, многие стараются найти максимально быстрый путь получения качественного образования. Факт наличия официального документа об образовании сложно переоценить. Ведь диплом открывает двери перед каждым человеком, который хочет вступить в профессиональное сообщество или продолжить обучение в университете.
Предлагаем очень быстро получить этот необходимый документ. Вы сможете заказать диплом старого или нового образца, что будет отличным решением для всех, кто не смог закончить обучение, потерял документ или желает исправить плохие оценки. Все дипломы производятся аккуратно, с особым вниманием к мельчайшим деталям. В итоге вы получите продукт, 100% соответствующий оригиналу.
Преимущество этого подхода состоит не только в том, что вы максимально быстро получите свой диплом. Процесс организовывается комфортно и легко, с профессиональной поддержкой. От выбора необходимого образца диплома до точного заполнения персональной информации и доставки в любое место России — все под полным контролем качественных специалистов.
Всем, кто хочет найти быстрый способ получения необходимого документа, наша компания предлагает выгодное решение. Заказать диплом – это значит избежать продолжительного обучения и сразу переходить к достижению личных целей, будь то поступление в университет или старт профессиональной карьеры.
Купить дипломы Вузов Уфы
Sugar Defender is a revolutionary blood sugar support formula designed to support healthy glucose levels and promote natural weight loss. https://acmesignz.com/
Seven Explanations On Why Which Online Stores Ship Internationally Is Important water-activated Tape
You’ll Never Guess This Window Repair Near Me’s Benefits Window repair Near me
The Reason Why Asbestos Is The Most Popular
Topic In 2023 asbestos litigation (Kasha)
Tipico Casino Kein PayPal
Das Tipico Casino ist eine beliebte Online Glücksspielplattform, die eine Vielzahl von Spielen für Spieler anbietet. Eine Zahlungsmethode, die jedoch nicht zur Verfügung steht, ist PayPal. Dies hat viele Spieler enttäuscht, da PayPal eine der beliebtesten und vertrauenswürdigsten Zahlungsmethoden im Online-Bereich ist.
Warum bietet das Tipico Casino kein PayPal an? Die genauen Gründe sind unbekannt, aber es gibt Vermutungen, dass es möglicherweise mit den strengen Richtlinien von PayPal im Zusammenhang mit Glücksspielseiten zu tun hat. PayPal hat hohe Anforderungen an die Transparenz und Legalität von Glücksspieltransaktionen, und möglicherweise erfüllt das Tipico Casino diese nicht zu 100%.
Für Spieler bedeutet dies, dass sie auf alternative Zahlungsmethoden ausweichen müssen, um Ein- und Auszahlungen im Tipico Casino vorzunehmen. Hierzu gehören Kreditkarten, Sofortüberweisung, Paysafecard, Skrill und Neteller. Diese Zahlungsmethoden sind ebenfalls sicher und zuverlässig, aber für viele Spieler ist PayPal immer noch die bevorzugte Option aufgrund seiner Benutzerfreundlichkeit und Sicherheit.
Es bleibt abzuwarten, ob das Tipico Casino in Zukunft PayPal als Zahlungsmethode hinzufügen wird, um den Bedürfnissen seiner Spieler gerecht zu werden. In der Zwischenzeit können Spieler weiterhin die verfügbaren Alternativen nutzen und das Tipico Casino in vollem Umfang genießen.
https://tipicocasino.one/
20 Tools That Will Make You Better At Secondary Double Glazing
Near Me double glazed windows cost – Opal,
11 Strategies To Completely Block Your Couches
For Sale Near Me Cheap Couches for Sale under $100 near me
A Provocative Rant About Coffee Pods Machine coffee brewing machines
You’ll Never Guess This Gotogel Link Alternatif’s Secrets
Gotogel Link Alternatif, https://Www.Diggerslist.Com/,
Are You Getting The Most The Use Of Your Sleeper
Sectional? Sleeper Couch
Looking For Inspiration? Try Looking Up Cheap Mobility Scooters
Near Me 4 wheel mobility scooter near me
10 Things That Your Family Teach You About Car Wreck Attorney Car wreck Attorney
10 Double Glazed Window Repair-Related Projects To Stretch
Your Creativity Window Repairs Near Me
Is Your Company Responsible For The CSGO Weapon Case Budget?
12 Top Ways To Spend Your Money esports 2014 summer case (https://woolstoncp.co.uk/)
buying prescription drugs in mexico: mexican mail order pharmacies – medicine in mexico pharmacies
7 Tips About Mobile Car Door Lock Repair That Nobody Will Tell You car remote lock repair near me (http://www.piano-p.com)
Why People Don’t Care About Personal Injury Compensation Personal injury lawsuit
На сайте http://smartporog.ru посмотрите весь каталог такого популярного товара, как выпадающие умные пороги. Автоматические пороги считаются оптимальным решением, если установить стационарные варианты не представляется возможным. К важным преимуществам таких конструкций относят то, что они ликвидируют преграду в полу, справляются с холодом, сквозняками, морозом, повышают звукоизоляцию, не задерживают влагу, отводят посторонние запахи. Изделия выполнены из надежных, практичных материалов.
See What Examples Of Online Products Tricks The Celebs Are Utilizing Examples Of Online Products
The 10 Most Scariest Things About ADHD Assessment UK Private adhd Assessment uk private (https://Minecraftcommand.science/profile/poweradult0)
15 Things You Didn’t Know About Window Repair
Near Me Double Glazed Window Repairs Near Me
Five Killer Quora Answers On Best Home Espresso Machine home Espresso machine
Getting Tired Of Online Shop? 10 Inspirational Sources That Will Bring Back Your Passion Bp55244G10 Drawer Pull [vimeo.com]
ADHD Medication Titration Tools To Improve Your Daily Lifethe One ADHD Medication Titration Technique Every Person Needs To Learn Adhd Medication Titration – Chessdatabase.Science –
7 Things You’ve Always Don’t Know About Michael Kors Bag On Sale michael Kors handbags In amazon
30 Inspirational Quotes About Upvc Windows Repair upvc window repair (galacy-mountain.hateblo.jp)
10 Key Factors About Boat Accident Attorney You Didn’t Learn In School moab boat accident attorney
10 Healthy 18-Wheeler Accident Attorneys Habits 18 wheeler Accidents
What’s The Current Job Market For Birth Defect Litigation Professionals?
Birth Defect
What Can A Weekly Filtered Coffee Makers Project Can Change Your Life Drip Coffee Makers – Search.Zum.Com,
How Repair Upvc Windows Became The Top Trend In Social Media Repairing Upvc Windows
9 Things Your Parents Teach You About France
Online Shopping Sites Clothes Multifunctional Firewood Rack (Vimeo.Com)
Nine Things That Your Parent Taught You About Double
Glazing Repairs Near Me Double glazing Repairs near me
The 10 Scariest Things About Best Butt Plugs best butt plug
What Freud Can Teach Us About Will CSGO Cases Go Up In Price case gamma
В современном мире, где диплом становится началом успешной карьеры в любом направлении, многие ищут максимально простой путь получения образования. Факт наличия документа об образовании трудно переоценить. Ведь диплом открывает двери перед всеми, кто собирается начать трудовую деятельность или учиться в ВУЗе.
В данном контексте мы предлагаем максимально быстро получить этот важный документ. Вы сможете приобрести диплом старого или нового образца, что является удачным решением для человека, который не смог закончить обучение или потерял документ. диплом изготавливается аккуратно, с особым вниманием к мельчайшим деталям, чтобы в результате получился документ, максимально соответствующий оригиналу.
Преимущества этого решения состоят не только в том, что вы сможете быстро получить свой диплом. Процесс организован удобно, с нашей поддержкой. Начав от выбора необходимого образца до правильного заполнения персональных данных и доставки в любой регион страны — все под абсолютным контролем квалифицированных мастеров.
В результате, для тех, кто ищет быстрый способ получить необходимый документ, наша компания предлагает выгодное решение. Приобрести диплом – это значит избежать продолжительного процесса обучения и сразу переходить к личным целям: к поступлению в университет или к началу удачной карьеры.
Купить диплом Академии МНЭПУ
Five Killer Quora Answers To Uk Online Grocery Shopping Sites uk online grocery shopping Sites
Why No One Cares About Repair A Window window repairs
A Time-Travelling Journey What People Said About Medical Malpractice Attorney 20 Years Ago Vimeo
5 Windows And Doors Leeds Lessons From The Professionals
Upvc Window Hinge Repair Leeds
How Car Accident Lawsuit Propelled To The Top Trend On Social Media Car Accident Legal advice
The Ugly Truth About Why Are CSGO Keys So Expensive case Revolution
See What Veterans Disability Lawsuit Tricks The Celebs Are Utilizing
veterans disability lawsuit (Carmela)
Watch Out: How Repair Upvc Windows Is Taking Over And What
To Do About It double glazed window repairs Near me (m.en.laurenhi.com)
11 Creative Methods To Write About Lock Smith For Car locksmith For car Keys
near me (Imoodle.win)
Autowatch Ghost Installation Tools To Help You Manage Your Everyday Lifethe Only Autowatch Ghost Installation Trick That Every Person Should Be
Able To autowatch
Five Killer Quora Answers To Replacement Double Glazing Units Near Me Replacement Double Glazing Units Near Me
The Unspoken Secrets Of Fleshlight Sex Toy
Das Online-Casino Boomerang bietet seinen Spielern eine Vielzahl von spannenden und unterhaltsamen Spielen. Von klassischen Tischspielen wie Roulette und Blackjack bis hin zu modernen Spielautomaten und Live-Casino-Spielen, hier gibt es fГјr jeden Geschmack etwas Passendes.
Ein weiterer Vorteil des Casinos ist die Möglichkeit, von überall und zu jederzeit spielen zu können. Egal ob man ein paar freie Minuten in der Mittagspause hat oder abends gemütlich auf der Couch entspannen möchte, das Casino en ligne Boomerang ist immer verfügbar.
Darüber hinaus bietet das Casino attraktive Boni und Promotionen, die das Spielerlebnis noch spannender machen. Von Willkommensboni für neue Spieler bis hin zu regelmäßigen Aktionen und Gewinnspielen, hier gibt es immer etwas zu gewinnen.
Die Sicherheit der Spieler steht im Casino Boomerang an oberster Stelle. Durch eine sichere SSL-Verschlüsselung werden sämtliche Daten vor unbefugtem Zugriff geschützt. Zudem arbeitet das Casino nur mit vertrauenswürdigen Zahlungsdienstleistern zusammen, um Ein- und Auszahlungen sicher und schnell abwickeln zu können.
Insgesamt ist das Casino en ligne Boomerang eine ausgezeichnete Wahl fГјr alle, die nach einem unterhaltsamen und sicheren Online-Casino suchen. Mit einer breiten Auswahl an Spielen, attraktiven Boni und erstklassigem Kundenservice ist hier fГјr ein unvergessliches Spielerlebnis gesorgt. Besuchen Sie das Casino noch heute und erleben Sie die Faszination des GlГјcksspiels von zu Hause aus!
https://boomerangcasino.one/
Don’t Buy Into These “Trends” Concerning Hire Truck
Accident Attorneys truck accident lawsuit
5 Bentley Continental Key Projects For Any Budget bentley key fob replacement
9 . What Your Parents Teach You About Who Owns CSGO Case Esports
Five Killer Quora Answers On Shopping Online Sites List
Shopping online sites
12 Facts About Tommy Hilfiger Xbody Bag To Get You Thinking About The Water Cooler cheaper
11 Ways To Completely Redesign Your Car Accidents Lawyer car
accident lawyer houston (Deanne)
The Benefits Of Window Repair Near At The Very Least Once In Your Lifetime window Repair near me
15 Surprising Stats About Hyundai Spare Key Hyundai key lost
A Rewind A Trip Back In Time: What People Talked
About Auto Accident Legal 20 Years Ago Auto Accident Law Firm
10 Quick Tips For Auto Accident Lawyer best Auto accident attorney near Me
14 Cartoons On Three Wheel Electric Scooters For Adults For Sale Which Will Brighten Your Day 3 Wheel mobility scooters uk
Nine Things That Your Parent Taught You About Best Online Shopping
Sites London Online Shopping Sites London
Boat Accident Attorney: The History Of Boat Accident Attorney In 10 Milestones Fort smith boat accident Attorneys (Images.google.com.Na)
See What Designer Handbags Brands Tricks The Celebs Are Using
Designer handbags Brands
The Reason Why Everyone Is Talking About Panty Vibrators Sex Toys Right Now wireless vibrator panties
How Veterans Disability Lawsuit Has Become The Top Trend On Social Media veterans disability law firm [Eleanore]
20 Trailblazers Setting The Standard In Bentley Valet Key Bentley key
БК Леон считается прекрасной платформой для увлекательных игр. Здесь есть живая статистика и огромный выбор ставок. Вы можете уже сейчас начать с уверенности благодаря бонусам для новичков. Простой интерфейс, оперативные выплаты и щедрые бонусы – это все о БК Леон. https://t.me/s/mleon_ru – канал, где у вас есть возможность начать выигрывать реальные денежные средства и присоединиться к сообществу ценителей спорта. Лучший сервис ждет вас, здесь каждый шаг может привести к победе! Выбирайте Леон, сделайте свой ход к успеху прямо сейчас. Вас ждут невероятные ощущения, удостоверьтесь в этом сами!
Could Best Online Shopping Sites Clothes Be The
Answer To 2023’s Resolving? which supermarket is best For online shopping
How To Determine If You’re Prepared For Auto Locksmith Auto Car key locksmith
В нашем обществе, где диплом – это начало отличной карьеры в любой сфере, многие ищут максимально простой путь получения качественного образования. Факт наличия официального документа об образовании переоценить просто невозможно. Ведь именно диплом открывает дверь перед каждым человеком, желающим вступить в профессиональное сообщество или продолжить обучение в ВУЗе.
В данном контексте наша компания предлагает оперативно получить этот необходимый документ. Вы можете приобрести диплом старого или нового образца, и это является отличным решением для всех, кто не смог закончить обучение, потерял документ или желает исправить свои оценки. Все дипломы изготавливаются аккуратно, с особым вниманием ко всем нюансам, чтобы в итоге получился 100% оригинальный документ.
Преимущество этого решения состоит не только в том, что вы сможете максимально быстро получить диплом. Весь процесс организован комфортно и легко, с профессиональной поддержкой. От выбора нужного образца документа до консультаций по заполнению личной информации и доставки по стране — все под абсолютным контролем качественных мастеров.
В результате, для тех, кто ищет быстрый способ получить требуемый документ, наша услуга предлагает отличное решение. Приобрести диплом – это значит избежать долгого обучения и сразу переходить к личным целям, будь то поступление в университет или начало карьеры.
Купить диплом Санкт-Петербургского государственного экономического университета
Why Triple Bunk Beds Will Be Your Next Big Obsession Bunk bed single and double
7 Things You’d Never Know About Motor Vehicle Case allegan Motor vehicle accident lawyer
5 Double Glazing Offers Near Me Lessons Learned From
Professionals Installation
15 Tips Your Boss Wants You To Know About Pvc Window Repairs You Knew
About Pvc Window Repairs upvc window repairs
Need Inspiration? Look Up Fiat 500 Replacement Key
fiat 500 replacement remote key cost
What Is Online Home Based Work And Why Is Everyone Talking About It?
work from home no experience – https://telegra.ph/solutions-to-the-problems-of-online-jobs-work-from-home-03-16 –
Zet Casino No Deposit Bonus Codes: Holen Sie sich kostenlose Boni ohne Einzahlung
Wenn Sie auf der Suche nach einem aufregenden Online-Casino-Erlebnis sind, dann sollten Sie unbedingt Zet Casino ausprobieren. Dieses beliebte Online-Casino bietet eine Vielzahl von Spielen, groГџzГјgigen Boni und aufregenden Aktionen, die sicherstellen, dass Sie jede Minute Ihres Besuchs genieГџen werden.
Eines der großartigen Angebote, die Zet Casino für seine Spieler bereithält, sind die No Deposit Bonus Codes. Diese speziellen Codes ermöglichen es Ihnen, kostenlose Boni zu erhalten, ohne dass Sie eine Einzahlung tätigen müssen. Das bedeutet, dass Sie die Spiele im Casino ausprobieren können, ohne Ihr eigenes Geld riskieren zu müssen.
Um einen No Deposit Bonus Code bei Zet Casino zu erhalten, müssen Sie sich einfach registrieren und ein Konto erstellen. Sobald Ihr Konto aktiviert ist, können Sie Ihre Bonus Codes im Kassenbereich eingeben, um Ihren kostenlosen Bonus zu erhalten. Diese Boni können in Form von Freispielen, Gratisguthaben oder anderen Belohnungen angeboten werden.
Die No Deposit Bonus Codes bei Zet Casino sind eine großartige Möglichkeit, das Casino kennenzulernen und einige seiner besten Spiele auszuprobieren, ohne Ihr eigenes Geld riskieren zu müssen. Also worauf warten Sie noch? Registrieren Sie sich noch heute bei Zet Casino und holen Sie sich Ihre kostenlosen Boni! Viel Glück und viel Spaß beim Spielen!
https://zetcasino.one/
How To Solve Issues Related To Double Glazing Deals Near Me lock for double glazed Door
This Week’s Most Remarkable Stories About Upvc Windows And Doors repair Upvc windows
Are The Advances In Technology Making How To Buy Clothes Online
From Uk Better Or Worse? which supermarket is best for online shopping (Lolita)
The 10 Scariest Things About Sex Machines Online Where To Buy A Sex Machine
10 Healthy Habits For A Healthy Freezer For Outbuilding smart Freezers,
fmpwy.Com,
15 Bizarre Hobbies That’ll Make You More Successful At Truck Accident Injury Lawyer
accidents
Your Family Will Be Grateful For Having This Online Shopping Stores In London Jeep Hardtop Thumb Screw Set
10 Apps To Help You Manage Your Auto Accident Compensation lawsuits
Indisputable Proof That You Need Perfumes Avon avon perfume on sale
Undeniable Proof That You Need Fiat 500 Key Replacement fiat 500 replacement Key Uk
5 Killer Quora Answers To Tommy Hilfiger Bag Ladies tommy Hilfiger bag ladies
10 Facebook Pages That Are The Best Of All Time Vibrating
Anal Sex Toys buy anal toys (http://ww.w.dpsee.com/)
Watch Out: How Squirt Dildos Is Taking Over And What
Can We Do About It best sex toy for squirting
It’s The Perfect Time To Broaden Your Prada Bag Options
Prada Handbags White
Why You Should Focus On Making Improvements Double Glazed Units Near Me double glazed windows
Bei Tipico Online Casino gewonnen
Es ist ein aufregender Moment, wenn man bei einem Online Casino wie Tipico gewinnt. Die Spannung während des Spiels und die Hoffnung darauf, dass die Glücksgöttin Fortuna auf unserer Seite ist, machen das Erlebnis so besonders.
Tipico bietet eine Vielzahl an Casino-Spielen an, von Slots Гјber Roulette bis hin zu Blackjack. Doch egal fГјr welches Spiel man sich entscheidet, der Adrenalinkick, wenn man gewinnt, ist immer derselbe.
Wenn man bei Tipico Online Casino gewinnt, kann das nicht nur finanzielle Vorteile mit sich bringen, sondern auch ein Gefühl der Zufriedenheit und des Stolzes. Man hat sein Glück herausgefordert und dabei gewonnen – das ist ein tolles Gefühl.
Natürlich ist es wichtig, verantwortungsbewusst zu spielen und sich der Risiken bewusst zu sein, die das Glücksspiel mit sich bringen kann. Aber mit der richtigen Herangehensweise und einem klaren Kopf kann das Spielen im Online Casino auch eine unterhaltsame und spannende Freizeitbeschäftigung sein.
Wer bei Tipico Online Casino gewinnt, kann sich auf schnelle Auszahlungen und einen kompetenten Kundenservice freuen. Das Unternehmen legt groГџen Wert auf Sicherheit und Fairness, sodass man sich als Spieler gut aufgehoben fГјhlen kann.
Insgesamt ist es ein aufregendes Erlebnis, bei Tipico Online Casino zu gewinnen. Man sollte jedoch immer im Hinterkopf behalten, dass das GlГјcksspiel ein Spiel ist und man nicht immer gewinnen kann. Aber wenn man Fortuna auf seiner Seite hat, kann sich das GefГјhl eines Gewinns wirklich lohnen.
https://tipicocasino.one/
The Most Successful Double Glazed Window Repair Gurus Are Doing Three Things repairer
can i order lisinopril over the counter: lisinopril 80 mg – buy lisinopril 20 mg without prescription
A Proactive Rant About Designer Handbags For Sale designer handbags for women
You’ll Never Guess This Gotogel Link Alternatif’s Tricks Gotogel Link Alternatif
5 Killer Quora Answers To Link Login Gotogel link login gotogel (Muhammad)
Ten Ways To Build Your Diagnostics Automotive
Empire Volvo diagnostics
Are You Responsible For The 18-Wheeler Accident Lawyers Budget?
10 Unfortunate Ways To Spend Your Money morrilton 18 Wheeler accident Lawsuit
Хотите приобрести Вегови в Москве по разумной стоимости и с быстрой доставкой? Мы официальный поставщик Вегови и прочих лекарств для мед. центров Москвы. У нас в наличии все дозировки препарата Вегови. https://wegovy-russia.ru – сайт, где есть фото людей как до, так и после использования. Представлены и актуальные цены на Вегови. Здесь также можете в любое удобное для вас время ознакомиться с отзывами клиентов. Чтобы купить Вегови, свяжитесь по WhatsApp с менеджером. Вы узнаете, на сколько можно похудеть, как храним Вегови и как он работает.
Don’t Buy Into These “Trends” About Small Sleeper
Sofa Small Sleeper couch
17 Signs To Know If You Work With Asbestos Lawyer Mesothelioma Mesothelioma lawyer Near me
Link Login Gotogel Tools To Ease Your Daily Lifethe One Link Login Gotogel Trick That Everyone Should Learn link login gotogel
What Is The Reason Window Repair Luton Is Right For You?
Upvc Window Doctor Near Me
3 Guidelines An Affordable Car Loan 주부대출; http://www.Google.Am,
The Top Reasons Why People Succeed At The Link Daftar Gotogel Industry Sports betting
Mesothelioma Lawyers Tools To Ease Your Daily Lifethe
One Mesothelioma Lawyers Trick Every Individual Should
Be Able To mesothelioma Lawyer
20 Amazing Quotes About Adult Movie gapping
See What Kids Bunk Bed Tricks The Celebs Are Making Use Of kids Bunk bed
Take A Look At The Steve Jobs Of The Repair A Window Industry wooden
See What Amazon Uk Online Shopping Clothes Tricks The Celebs
Are Using Amazon Uk Online Shopping Clothes
See What Online Shopping Stores In London Tricks The Celebs Are Using online shopping Stores in london
Double Glazing Near Me 10 Things I’d Love To Have Known Earlier replacing glass in double glazing
Why Is It So Useful? When COVID-19 Is In Session Injury Lawyers
20 Interesting Quotes About Upvc Windows Repair Upvc Window Repair
Why Adding A New Audi Key To Your Life Will Make All The Change replacement Key audi
This Is The Ultimate Guide To SEO For Near Me Searches affordable
seo services near me (Caitlin)
sugar defender: https://seahorsesoap.com/
10 Myths Your Boss Is Spreading Regarding Vegas
Slots Classic Slots
Your trust in us is our top priority. That’s why we operate with complete integrity and focus on results.
Feel the comfort of seeing your funds returned with our specialized assistance.
Why Incorporating A Word Or Phrase Into Your Life Can Make All The An Impact audi A3 key fob replacement
10 Great Books On Cheap Heat Pump Tumble Dryer Tumble dryers with heat Pump
5 Mesothelioma Compensation Projects For Any Budget Mesothelioma claims
See What 1kg Coffee Beans Price Tricks The Celebs Are Utilizing 1Kg Coffee Beans Price
How To Create Successful Motor Vehicle Case Tutorials On Home Yuma Motor Vehicle Accident Lawsuit
The Top Reasons People Succeed On The Auto Accidents Attorneys Industry automobile Accident lawyer houston
What’s The Current Job Market For Michael Kors Handbags On Sale
Professionals Like? michael kors handbags
Zet Casino Trustpilot
Zet Casino ist ein beliebtes Online-Casino, das Spielern eine Vielzahl von Spielen und groГџzГјgigen Boni bietet. Viele Spieler verlassen sich auf Online-Bewertungsplattformen wie Trustpilot, um herauszufinden, ob ein Casino vertrauenswГјrdig ist. Wie schneidet Zet Casino bei Trustpilot ab?
Die meisten Bewertungen von Zet Casino auf Trustpilot sind positiv. Viele Spieler loben die Benutzerfreundlichkeit der Website, die groГџe Auswahl an Spielen und die schnellen Auszahlungen. Einige Spieler haben jedoch auch negative Erfahrungen gemacht, vor allem in Bezug auf den Kundenservice und Bonusbedingungen.
Es ist wichtig zu beachten, dass Trustpilot-Bewertungen subjektiv sind und von persönlichen Erfahrungen abhängen. Einige Spieler haben möglicherweise eine positive Erfahrung mit Zet Casino gemacht, während andere negative Erfahrungen gemacht haben. Es ist immer ratsam, mehrere Bewertungen zu lesen und sich ein umfassendes Bild zu machen, bevor man sich für ein Online-Casino entscheidet.
Insgesamt scheint Zet Casino bei Trustpilot eine gute Bewertung zu haben. Es ist wichtig, sich bewusst zu sein, dass es immer einige negative Bewertungen geben wird, unabhängig davon, wie gut ein Casino ist. Es ist ratsam, die Bewertungen objektiv zu betrachten und sich nicht ausschließlich auf sie zu verlassen, um eine fundierte Entscheidung zu treffen.
Fazit: Zet Casino scheint auf Trustpilot gut abzuschneiden, aber es ist immer ratsam, mehrere Bewertungen zu lesen und sich nicht nur auf eine Plattform zu verlassen, um die Zuverlässigkeit eines Online-Casinos zu bewerten.
https://zetcasino.one/
What’s The Job Market For Double Glazed Window
Repairs Professionals? double glazed window repairs
rikvip
Rikvip Club: Trung Tâm Giải Trí Trực Tuyến Hàng Đầu tại Việt Nam
Rikvip Club là một trong những nền tảng giải trí trực tuyến hàng đầu tại Việt Nam, cung cấp một loạt các trò chơi hấp dẫn và dịch vụ cho người dùng. Cho dù bạn là người dùng iPhone hay Android, Rikvip Club đều có một cái gì đó dành cho mọi người. Với sứ mạng và mục tiêu rõ ràng, Rikvip Club luôn cố gắng cung cấp những sản phẩm và dịch vụ tốt nhất cho khách hàng, tạo ra một trải nghiệm tiện lợi và thú vị cho người chơi.
Sứ Mạng và Mục Tiêu của Rikvip
Từ khi bắt đầu hoạt động, Rikvip Club đã có một kế hoạch kinh doanh rõ ràng, luôn nỗ lực để cung cấp cho khách hàng những sản phẩm và dịch vụ tốt nhất và tạo điều kiện thuận lợi nhất cho người chơi truy cập. Nhóm quản lý của Rikvip Club có những mục tiêu và ước muốn quyết liệt để biến Rikvip Club thành trung tâm giải trí hàng đầu trong lĩnh vực game đổi thưởng trực tuyến tại Việt Nam và trên toàn cầu.
Trải Nghiệm Live Casino
Rikvip Club không chỉ nổi bật với sự đa dạng của các trò chơi đổi thưởng mà còn với các phòng trò chơi casino trực tuyến thu hút tất cả người chơi. Môi trường này cam kết mang lại trải nghiệm chuyên nghiệp với tính xanh chín và sự uy tín không thể nghi ngờ. Đây là một sân chơi lý tưởng cho những người yêu thích thách thức bản thân và muốn tận hưởng niềm vui của chiến thắng. Với các sảnh cược phổ biến như Roulette, Sic Bo, Dragon Tiger, người chơi sẽ trải nghiệm những cảm xúc độc đáo và đặc biệt khi tham gia vào casino trực tuyến.
Phương Thức Thanh Toán Tiện Lợi
Rikvip Club đã được trang bị những công nghệ thanh toán tiên tiến ngay từ đầu, mang lại sự thuận tiện và linh hoạt cho người chơi trong việc sử dụng hệ thống thanh toán hàng ngày. Hơn nữa, Rikvip Club còn tích hợp nhiều phương thức giao dịch khác nhau để đáp ứng nhu cầu đa dạng của người chơi: Chuyển khoản Ngân hàng, Thẻ cào, Ví điện tử…
Kết Luận
Tóm lại, Rikvip Club không chỉ là một nền tảng trò chơi, mà còn là một cộng đồng nơi người chơi có thể tụ tập để tận hưởng niềm vui của trò chơi và cảm giác hồi hộp khi chiến thắng. Với cam kết cung cấp những sản phẩm và dịch vụ tốt nhất, Rikvip Club chắc chắn là điểm đến lý tưởng cho những người yêu thích trò chơi trực tuyến tại Việt Nam và cả thế giới.
What Are The Biggest “Myths” About Private ADHD Diagnosis UK Cost Could Actually
Be Accurate private adhd and autism assessment near me
Вам интересен по разумным ценам прокат авто? Rent Me – то, что вам нужно. Сервис предлагает вам выбрать подходящую машину и забронировать. Вы гарантированно получите услугу высочайшего качества. Все авто проходят техобслуживание, вы можете не переживать о поломках в пути. Ищете снять авто на Кипре? Rent-me.cy – сайт, который на острове Кипр предоставляет прокатные машины. Процесс аренды мы сделали максимально приятным и простым. Будем рады вам ответить на все вопросы и пообщаться с вами, звоните.
The 10 Most Scariest Things About Online Shopping Stores List Online Shopping Stores List
The Reasons Bag Prada Could Be Your Next Big Obsession Prada Bags Gold
What’s The Current Job Market For Link Daftar Gotogel Professionals
Like? link Daftar gotogel (http://itsroom.co.Kr/)
Where Can You Find The Most Reliable Locksmith Auto
Near Me Information? replace
Guide To Ghost 2 Immobiliser Installation: The Intermediate Guide
For Ghost 2 Immobiliser Installation Ghost 2 immobiliser Installation
10 Things That Everyone Is Misinformed Concerning Adult Pleasure Toys men’s adult toys (Silvia)
What’s The Job Market For Situs Gotogel Terpercaya Professionals Like?
situs gotogel terpercaya – Guillermo,
5 Killer Quora Answers On Fiat Ducato Replacement Key fiat
ducato replacement key [demo2.mainspringmc.com]
The Ultimate Glossary Of Terms For Double Glazed Units Near Me double Glazed units
Five Killer Quora Answers On Private Psychiatrist London private Psychiatrist london
The Reasons Pleural Mesothelioma Compensation Is More
Difficult Than You Imagine How Much Compensation Do You Get For Mesothelioma (https://Www.Peppynet.Com)
Who’s The World’s Top Expert On Railroad Injuries Settlement?
lawsuit
Das Boomerang Casino ist eine beliebte Online-Glücksspielplattform, die von Spielern auf der ganzen Welt geschätzt wird. Auf der Bewertungsplattform Trustpilot können Nutzer ihre Erfahrungen mit dem Casino teilen und anderen potenziellen Spielern eine Vorstellung von dem geben, was sie erwartet.
Die Bewertungen auf Trustpilot fГјr das Boomerang Casino sind durchweg positiv. Viele Spieler loben die benutzerfreundliche und ansprechende Website, die eine reibungslose Navigation und ein angenehmes Spielerlebnis bietet. DarГјber hinaus wird die Vielfalt der angebotenen Spiele, darunter Slots, Tischspiele und Live-Casino-Spiele, gelobt.
Ein weiterer Aspekt, der von Spielern hervorgehoben wird, ist der professionelle und freundliche Kundenservice des Boomerang Casinos. Die Mitarbeiter sind stets schnell erreichbar und helfen bei Fragen oder Problemen kompetent weiter.
Einige Spieler betonen auch die großzügigen Bonusangebote und Aktionen, die das Boomerang Casino regelmäßig veranstaltet. Von Willkommensboni über Freispiele bis hin zu Cashback-Angeboten gibt es für Spieler immer wieder attraktive Möglichkeiten, ihr Guthaben zu erhöhen.
Insgesamt scheint das Boomerang Casino in den Augen vieler Spieler eine vertrauenswürdige und unterhaltsame Glücksspielplattform zu sein. Die positiven Bewertungen auf Trustpilot spiegeln wider, dass Spieler die Seite schätzen und gerne dort spielen.
Wer also auf der Suche nach einem seriösen Online-Casino ist, sollte das Boomerang Casino auf jeden Fall in Betracht ziehen. Mit einer großen Auswahl an Spielen, attraktiven Bonusangeboten und einem erstklassigen Kundenservice scheint es eine gute Wahl für Glücksspielfans zu sein.
https://boomerangcasino.one/
How Womens Rabbit Vibrator Sex Toy Was The Most Talked About Trend
Of 2023 rabbit vibrator how to Use
https://cytotec.xyz/# buy misoprostol over the counter
Такси Минивэн Онлайн предлагает высококачественные услуги по доступным тарифам. В салоне автомобиля с комфортом размещаются 8 человек. Машины оборудованы детскими креслами. Все без исключения водители вежливые, они прошли школу мастерства. Ищете заказать такси минивэн? Minivan.online – сайт, где представлена более подробная информация, ознакомиться с ней можете в удобное для вас время. Также здесь указана актуальная стоимость поездки. Заказ такси минивэн осуществляется по контактному номеру телефона. Звоните нам прямо сейчас и мы вас проконсультируем!
9 Signs That You’re A Real Life Sexdoll Expert Silicon Sex dolls
10 Meetups On Michael Kors Crossbody Bag You Should Attend Michael kors handbag Navy
The 9 Things Your Parents Teach You About Larder Fridge under counter fridge – black
What To Look For In The Right Dangerous Drugs Lawyer For You
Collinsville dangerous drugs lawsuit
How Double Glazing Companies Near Me Has Changed My Life The Better double glazed
window – Garry,
8 Tips To Increase Your Adhd Symptoms In Women Test Game adult Female Adhd symptoms
zestoretic 20-25 mg price of lisinopril in india lisinopril 12.5 mg 10 mg
Are Misted Double Glazing Repairs Really As Vital As Everyone Says?
door Repair
9 Things Your Parents Teach You About Bean To Cup Coffee Machine Sale Bean To Cup Coffee Machine Sale,
Elearnportal.Science,
See What Demo Slot Princess Starlight Tricks The Celebs Are
Utilizing demo slot princess starlight (Latia)
15 Undeniable Reasons To Love Black Friday Sofa Sale Sofas On sale
Ten Pinterest Accounts To Follow Motor Vehicle Compensation motor vehicle accident attorneys
Looking For Inspiration? Try Looking Up Railroad Injuries Case railroad injuries law firms
Recovering your money shouldn’t be complicated. That’s why
our service is simple and open.
Simply give us the necessary details, and we’ll handle the
rest.
Don’t allow fraudsters keep you from your hard-earned money.
Our goal is to help you recover every cent.
The 10 Most Terrifying Things About Gotogel Link Alternatif gotogel link alternatif
14 Cartoons About Cheap Couches For Sale To Brighten Your Day big Couches For sale
На сайте http://waltzprof.com каждый желающий получает возможность приобрести стальной профиль высокого качества и созданный из надежных, практичных материалов. За счет этого изделия прослужат в течение длительного времени и не покроются коррозией. В этой компании они представлены в широком ассортименте, что позволит подыскать решение в соответствии с предпочтениями. Профиль применяется для оперативной, комфортной сборки ограждающих преград, лофт перегородок, фасадных конструкций, ворот. Для реализации проекта используются уникальные и инновационные технологии, передовое оборудование.
See What Examples Of Online Products Tricks The
Celebs Are Using Examples of Online products
15 Latest Trends And Trends In Double Glazing Repairs North London window doctor london – https://geeky.co.kr/member/login.html?noMemberOrder=&returnUrl=http://baskino.cc/user/peacelimit60/ –
10 Misleading Answers To Common Railroad Injuries Legal Questions: Do You Know Which Answers?
champaign railroad crossing accident lawyer
Automobile Locksmiths Near Me Tools To Help You
Manage Your Daily LifeThe One Automobile Locksmiths Near Me Technique Every Person Needs To
Be Able To automobile locksmiths (https://Maps.google.gp)
How To Ship To Ireland From Uk Tips To Relax Your Everyday Lifethe
Only How To Ship To Ireland From Uk Trick That Every Person Must Learn How To ship to ireland from
uk (images.google.com.tr)
5 Killer Quora Answers To Motorcycle Accident Attorneys motorcycle Accident attorneys
What Is The Secret Life Of Energy Efficient Washer Dryer
Combo are washer dryers any good
5 Cliches About Semi Truck Legal You Should Avoid semi truck accident lawsuits
Situs Alternatif Gotogel Tools To Streamline Your Everyday Lifethe Only Situs Alternatif Gotogel Trick That Everybody
Should Know Situs Alternatif Gotogel
The Most Worst Nightmare About Auto Accident Attorney It’s Coming To Life automotive accident lawyer near Me
How To Create An Awesome Instagram Video About
Online Shopping Uk Women’s Clothing vimeo
10 Quick Tips About Double Glazing Near Me repairs to
double glazing windows – croftprimary.co.uk –
What Is Ford Focus Key Replacement And How To Use It?
replacing ford key
Unexpected Business Strategies For Business That Aided Mobile
Auto Diagnostic Services Near Me Succeed Diagnostics check
Twenty Myths About Fridge Freezer Hotpoint: Busted small
fridge freezer (Deena)
7 Simple Tips For Rocking Your Personal Injury Attorney fairfield personal injury Law Firm
sugar defender: https://sourceprousa.com/
What’s The Current Job Market For Best Online Shopping Groceries Uk Professionals Like?
best online shopping groceries uk (Kami)
Worried about your QIWI wallet transactions?
Let us take the lead in getting back what isrightfully yours.
Reach out now and begin reclaiming your funds.
12 Facts About Online Famous Shopping Sites To Bring You Up To Speed The Cooler Water Cooler Motofab Wrangler Jk Lift Kit
Are You Responsible For The Integrated Fridge Freezer Budget?
12 Best Ways To Spend Your Money Best American Fridge Freezer Uk
11 “Faux Pas” That Are Actually Okay To Do With Your Personal Injury Litigation soldotna personal injury attorney
How To Know The Best Local SEO Company Which Is Right For You local online
marketing – glk-egoza.ru,
На сайте https://incubatoreggs.ru/ ознакомьтесь с телефоном для того, чтобы заказать инкубационное яйцо высокого качества от цыплят, индейки, курицы-бройлера, утки, гуся. Вся продукция от сельскохозяйственных, домашних птиц. Они от лучших, зарекомендовавших себя фабрик России, Европы. Это ваша уникальная возможность приобрести инкубаторную продукцию по стоимости завода и даже ниже. Самым популярным является яйцо индейки, утки, гуся. Вы сможете воспользоваться бесплатной доставкой по городу, если сделаете заказ на сумму от 3 000 рублей.
What’s The Job Market For Best Online Shopping Groceries Uk Professionals?
best online shopping groceries uk
13 Things You Should Know About Boat Accident
Claim That You Might Never Have Known bluffton boat Accident attorney
How To Make A Successful Private ADHD Assessment Near Me Tips From Home can I get a private adhd assessment
A Step-By-Step Instruction For LG Refrigerators Models how Much
is lg small fridge (http://www.google.co.jp)
How The 10 Worst Upvc Windows Repair Fails Of All Time Could Have Been Prevented upvc window Repairs Near me
What’s The Current Job Market For Leather Sectional
Sleeper Sofa Professionals? leather sleeper sofa (https://myhealthychurch.com/Store/cart.cfm?&cat=CHECKOUT&continueshopping=berryrouter44.bravejournal.net/who-is-room-and-board-sleeper-sofa-and-why-you-should-be-concerned)
Have funds disappeared on your QIWI wallet?
We get it how stressful that can be.
Don’t despair—our company specializes in recovering your balance from QIWI wallets.
Boasting expert knowledge, we’re confident we can provide assistance.
Contact us and let’s start the process of restoring your balance.
12 Upvc Window Repairs Facts To Get You Thinking About The Cooler Water Cooler upvc window repairs near me
Wenn es um Online Casinos geht, sind Freispiele eine der begehrtesten Aktionen für Spieler. Tipico Casino bietet regelmäßig Freispiele als Teil ihres Bonusprogramms an, und in diesem Artikel werden wir Ihnen zeigen, wie Sie diese Freispiele einlösen können.
Zunächst einmal müssen Sie ein Konto bei Tipico Casino haben, um von den Angeboten profitieren zu können. Wenn Sie bereits angemeldet sind, überprüfen Sie regelmäßig Ihre E-Mails oder die Webseite des Casinos, um über aktuelle Aktionen informiert zu werden. Oft werden Freispiele als Belohnung für Einzahlungen oder als Teil von Turnieren angeboten.
Sobald Sie Freispiele erhalten haben, müssen Sie diese einlösen, um sie zu nutzen. Gehen Sie einfach zu den entsprechenden Spielautomaten, bei denen die Freispiele gültig sind, und öffnen Sie das Spiel. Normalerweise erhalten Sie eine Benachrichtigung über die verfügbaren Freispiele, und Sie können mit dem Spielen beginnen.
Es ist wichtig zu beachten, dass Freispiele oft mit bestimmten Umsatzbedingungen verbunden sind. Das bedeutet, dass Sie die Gewinne aus den Freispielen eine gewisse Anzahl von Malen umsetzen müssen, bevor Sie sie auszahlen lassen können. Stellen Sie sicher, dass Sie die Bedingungen genau lesen, um Missverständnisse zu vermeiden.
Insgesamt sind Freispiele eine großartige Möglichkeit, um zusätzliche Gewinne im Casino zu erzielen. Mit Tipico Casino können Sie regelmäßig von Freispielen profitieren und Ihre Gewinnchancen erhöhen. Nutzen Sie diese Angebote und haben Sie Spaß beim Spielen!
https://tipicocasino.one/
15 Funny People Who Are Secretly Working In Mesothelioma Compensation Payouts Workers
Compensation For Mesothelioma (Jus.T.Indm.O.Ra.P.Omona19.8.7.12.Myopenlink.Net)
You’ll Never Guess This Upvc Window Repairs Near Me’s Secrets upvc window repairs Near me
Costa Mocha Italia Coffee Beans 1kg Techniques To Simplify Your Daily Life Costa Mocha
Italia Coffee Beans 1kg Trick That Everyone Should Be Able To Coffee Beans 1Kg
10 Facts About Double Glazed Window Near Me That Will Instantly Bring
You To A Happy Mood double glazing windows handles (Jamaal)
This Is The One Auto Accident Lawyer Trick Every Person Should Know motor
What’s The Job Market For Vibrator For Clitoris Professionals?
Vibrator For Clitoris
The Top Companies Not To Be Follow In The Truck Accidents Attorneys Industry lewisburg Truck accident law firm
В современном мире, где диплом – это начало удачной карьеры в любой области, многие пытаются найти максимально быстрый и простой путь получения образования. Наличие документа об образовании переоценить попросту невозможно. Ведь диплом открывает двери перед людьми, желающими вступить в профессиональное сообщество или продолжить обучение в каком-либо университете.
В данном контексте наша компания предлагает максимально быстро получить этот важный документ. Вы имеете возможность приобрести диплом нового или старого образца, что является удачным решением для всех, кто не смог закончить обучение или потерял документ. Все дипломы изготавливаются с особой аккуратностью, вниманием ко всем элементам, чтобы на выходе получился 100% оригинальный документ.
Превосходство данного подхода заключается не только в том, что можно быстро получить диплом. Процесс организован удобно, с нашей поддержкой. Начав от выбора требуемого образца документа до грамотного заполнения личной информации и доставки в любой регион России — все находится под полным контролем опытных мастеров.
Всем, кто пытается найти оперативный способ получить необходимый документ, наша компания готова предложить отличное решение. Приобрести диплом – значит избежать длительного процесса обучения и сразу перейти к достижению личных целей, будь то поступление в университет или старт карьеры.
http://bonus.2bb.ru/viewtopic.php?id=4635
Are You Responsible For A Double Glazed Doors Near Me Budget?
10 Very Bad Ways To Invest Your Money replace
Unexpectedly lost your balance on your QIWI wallet?
We know how frustrating that can be.
Don’t despair—we specializes in getting back your balance from QIWI wallets.
With a high success rate, we’re confident we can assist you.
Reach out to us and let’s begin of recovering your funds.
15 Terms Everyone Working In The Auto Accident Litigation Industry Should Know Auto Accident lawsuits
The Reason Why Slot Graphics Is Much More Hazardous Than You Think
Slot software (m.themeal.co.kr)
What’s The Job Market For Gotogel Link Alternatif
Professionals? gotogel link alternatif
buy misoprostol over the counter: buy cytotec – buy cytotec online fast delivery
10 Truck Accident Tips All Experts Recommend Vimeo.Com
Why Do So Many People Want To Know About Window Repair
Near? upvc window repair near me (Addie)
A Comprehensive Guide To Online Shopping
Uk Women’s Clothing. Ultimate Guide To Online Shopping Uk Women’s Clothing vimeo
Don’t Buy Into These “Trends” About Car Accident Law legal
Are Car Lock Repair The Best Thing There Ever Was?
locker Repair near me (http://www.woodsloke.suffolk.sch.Uk)
The 3 Greatest Moments In Slot Mechanics History Slot machine Reviews
What Is Titration ADHD Adults And How To Utilize What Is Titration ADHD
Adults And How To Use what is titration adhd [Miquel]
Our expertise in e-wallets and online transactions means we’re perfectly
equipped to tackle your QIWI wallet issues.
Rest assured, we utilize the latest techniques and are well-versed in the latest fraud
prevention strategies.
If you’ve been affected by unauthorized transactions or errors
that resulted in a loss of funds, our team is ready to assist.
The Railroad Injuries Lawyers Mistake That Every Beginner Makes fela Railroad accident lawyer (https://boswell-mccarthy.blogbright.net/)
The Reason Why Adding A Vehicle Diagnostics To Your Life
Can Make All The An Impact Diagnostics Mobile
В нашем мире, где диплом – это начало отличной карьеры в любом направлении, многие пытаются найти максимально быстрый и простой путь получения качественного образования. Факт наличия официального документа трудно переоценить. Ведь диплом открывает дверь перед всеми, кто стремится вступить в сообщество профессионалов или продолжить обучение в каком-либо университете.
В данном контексте наша компания предлагает очень быстро получить этот важный документ. Вы сможете заказать диплом нового или старого образца, и это будет выгодным решением для человека, который не смог закончить обучение, утратил документ или желает исправить свои оценки. Любой диплом изготавливается аккуратно, с особым вниманием к мельчайшим элементам, чтобы в результате получился документ, полностью соответствующий оригиналу.
Преимущества такого подхода заключаются не только в том, что можно быстро получить свой диплом. Процесс организован комфортно, с нашей поддержкой. Начав от выбора необходимого образца документа до правильного заполнения личных данных и доставки в любой регион России — все под абсолютным контролем опытных специалистов.
Всем, кто ищет оперативный способ получить требуемый документ, наша компания предлагает выгодное решение. Заказать диплом – значит избежать продолжительного процесса обучения и не теряя времени перейти к достижению собственных целей: к поступлению в университет или к началу успешной карьеры.
http://caezar.4bb.ru/viewtopic.php?id=4191
Das Boomerang Casino ist eine neue Online-GlГјcksspielplattform, die sich schnell einen Namen in der Welt der Online-Casinos gemacht hat. In diesem Testbericht werden wir einen genaueren Blick auf das Boomerang Casino werfen, um zu sehen, ob es seinen wachsenden Ruf wirklich verdient.
Zunächst einmal fällt auf, dass das Boomerang Casino eine benutzerfreundliche Webseite hat, die sowohl auf dem Computer als auch auf mobilen Geräten gut funktioniert. Die Navigation auf der Seite ist einfach und intuitiv, was es den Spielern ermöglicht, schnell ihr Lieblingsspiel zu finden. Das Casino bietet eine breite Palette von Spielkategorien an, darunter Spielautomaten, Tischspiele, Live-Casino und Jackpot-Spiele.
Besonders beliebt sind die Spielautomaten im Boomerang Casino, da sie von renommierten Softwareanbietern wie NetEnt, Microgaming und Play’n GO bereitgestellt werden. Dadurch ist eine hohe QualitГ¤t und ein unterhaltsames Spielerlebnis garantiert. Die Tischspiele im Boomerang Casino sind ebenfalls vielfГ¤ltig und bieten eine gute Auswahl an klassischen und modernen Spielen.
Ein weiterer Pluspunkt des Boomerang Casinos ist das Live-Casino, in dem Spieler mit echten Dealern in Echtzeit spielen können. Die Atmosphäre ist authentisch und die Spiele werden professionell geleitet, was für ein besonders realistisches Spielerlebnis sorgt. Zudem bietet das Boomerang Casino eine Vielzahl von Zahlungsmethoden an, darunter Kreditkarten, E-Wallets und Banküberweisungen, was es Spielern aus aller Welt leicht macht, Ein- und Auszahlungen vorzunehmen.
Insgesamt hinterlässt das Boomerang Casino einen positiven Eindruck. Die Webseite ist benutzerfreundlich, die Spieleauswahl ist vielfältig und die Zahlungsmethoden sind vielfältig. Das Live-Casino und die Spielautomaten sind besonders empfehlenswert. Wenn Sie auf der Suche nach einem unterhaltsamen und sicheren Online-Casino sind, sollten Sie das Boomerang Casino auf jeden Fall ausprobieren.
https://boomerangcasino.one/
holidaynewsletters.com
Интернет-магазин «МОЙ и ТВОЙ» предлагает в огромном ассортименте уютные и полезные презенты, нужные в быту вещи и продукцию для украшения, создания привлекательного интерьера. А если необходимо найти что-то определенное, то воспользуйтесь специальным поиском, который найдет все, что нужно. На сайте https://moi-tvoi.ru/ ознакомьтесь с полным ассортиментом магазина.
neurontin 800 mg capsules medicine neurontin where can i buy neurontin online
На сегодняшний день, когда диплом является началом отличной карьеры в любом направлении, многие ищут максимально быстрый и простой путь получения образования. Наличие официального документа об образовании переоценить просто невозможно. Ведь именно диплом открывает дверь перед людьми, желающими вступить в сообщество профессионалов или учиться в ВУЗе.
Мы предлагаем максимально быстро получить этот необходимый документ. Вы имеете возможность заказать диплом, и это будет отличным решением для человека, который не смог закончить обучение, утратил документ или желает исправить свои оценки. дипломы изготавливаются аккуратно, с особым вниманием ко всем элементам, чтобы на выходе получился документ, 100% соответствующий оригиналу.
Преимущества такого решения заключаются не только в том, что можно быстро получить диплом. Весь процесс организован удобно, с нашей поддержкой. От выбора подходящего образца до грамотного заполнения персональных данных и доставки по стране — все будет находиться под полным контролем опытных мастеров.
Всем, кто ищет быстрый способ получения требуемого документа, наша компания предлагает выгодное решение. Приобрести диплом – это значит избежать длительного обучения и сразу переходить к достижению собственных целей: к поступлению в университет или к началу трудовой карьеры.
https://izhevsk.ru/forummessage/153/6114277.html
Zet Casino Bonus ohne Einzahlung – deinen Start im Online Casino erleichtern
In der Welt des Online Glücksspiels gibt es ständig neue Angebote und Aktionen, die Spieler dazu verleiten sollen, sich in einem bestimmten Casino anzumelden. Eines dieser Angebote ist der Zet Casino Bonus ohne Einzahlung, der es Spielern ermöglicht, das Casino und seine Spiele zunächst ohne eigenes Geld auszuprobieren.
Ein Bonus ohne Einzahlung ist eine großartige Möglichkeit für Spieler, ein neues Casino kennenzulernen, ohne finanzielle Risiken einzugehen. Bei Zet Casino erhalten neue Spieler einen Bonus von 10 Euro ohne Einzahlung, sobald sie sich registrieren. Mit diesem Bonus können Spieler das Casino erkunden und erste Gewinne erzielen, ohne Geld ausgeben zu müssen.
Um den Bonus ohne Einzahlung zu erhalten, müssen Spieler lediglich ein Konto bei Zet Casino anlegen. Der Bonus wird dann automatisch gutgeschrieben und steht sofort zur Verfügung. Es gibt jedoch einige Bedingungen, die Spieler erfüllen müssen, bevor sie Gewinne aus dem Bonus auszahlen lassen können. Dazu gehört in der Regel das Erfüllen eines Umsatzziels, das innerhalb eines bestimmten Zeitraums erreicht werden muss.
Der Zet Casino Bonus ohne Einzahlung ist eine großartige Möglichkeit, um das Casino und seine Spiele kennenzulernen, ohne eigenes Geld riskieren zu müssen. Spieler können mit dem Bonus erste Erfahrungen sammeln und entscheiden, ob das Casino ihren Erwartungen entspricht. Mit etwas Glück können Spieler sogar erste Gewinne erzielen, die sie sich auszahlen lassen können.
Fazit: Der Zet Casino Bonus ohne Einzahlung ist eine attraktive Möglichkeit, um das Casino risikofrei kennenzulernen und erste Gewinne zu erzielen. Spieler sollten jedoch die Bedingungen des Bonus genau lesen und sicherstellen, dass sie die Umsatzanforderungen erfüllen, um sich Gewinne auszahlen lassen zu können.
https://zetcasino.one/
Das Boomerang Casino ist ein Online-Casino, das seinen Spielern eine Vielzahl von Unterhaltungsmöglichkeiten bietet. Von klassischen Tischspielen wie Blackjack und Roulette bis hin zu aufregenden Spielautomaten und Live-Casino-Spielen – hier kommt jeder auf seine Kosten.
Das Casino zeichnet sich durch seine benutzerfreundliche Oberfläche aus, die es einfach macht, zwischen den verschiedenen Spielen zu navigieren. Darüber hinaus bietet das Boomerang Casino seinen Spielern eine sichere und faire Spielumgebung, die durch SSL-Verschlüsselungstechnologie geschützt ist.
Ein besonderes Highlight des Boomerang Casinos sind die regelmäßigen Bonusangebote und Aktionen, die den Spielern zusätzliche Gewinnchancen bieten. Von Willkommensboni über Freispiele bis hin zu Cashback-Angeboten – hier gibt es immer etwas zu gewinnen.
Des Weiteren bietet das Boomerang Casino einen professionellen Kundenservice, der seinen Spielern bei Fragen und Problemen rund um die Uhr zur Verfügung steht. Ob per Live-Chat, E-Mail oder Telefon – die Mitarbeiter des Casinos sind stets bemüht, den Spielern weiterzuhelfen.
Alles in allem ist das Boomerang Casino eine empfehlenswerte Adresse fГјr alle, die auf der Suche nach einem unterhaltsamen und sicheren Online-Casino-Erlebnis sind. Mit seinem breiten Spielangebot, groГџzГјgigen Bonusangeboten und professionellem Kundenservice Гјberzeugt das Casino auf ganzer Linie.
https://boomerangcasino.one/
9 Things Your Parents Taught You About Ranking SEO Software
Seo Software
Хронос гарантирует высокое качество медицинской техники, доступные цены и бесплатную доставку в любой регион РФ. Купить медтехнику вы можете, позвонив нам по телефону. С радостью ответим на интересующие вас вопросы и поможем с выбором. https://agsvv.ru/ сайт, где есть возможность уже сейчас посмотреть условия доставки и оплаты товара. Также здесь вы узнаете, какие лампы применяются в аппаратах, произведенных компанией Хронос и какой срок гарантии. Позвоните нам, и мы вас проконсультируем.
buying propecia tablets: cheap propecia no prescription – buy cheap propecia no prescription
What Is The Reason? SEO Management Company Is Fast Increasing To Be The Hottest Trend Of 2023 search Engine optimisation company london
UEFA Euro 2024 Sân Chơi Bóng Đá Hấp Dẫn Nhất Của Châu Âu
Euro 2024 là sự kiện bóng đá lớn nhất của châu Âu, không chỉ là một giải đấu mà còn là một cơ hội để các quốc gia thể hiện tài năng, sự đoàn kết và tinh thần cạnh tranh.
Euro 2024 hứa hẹn sẽ mang lại những trận cầu đỉnh cao và kịch tính cho người hâm mộ trên khắp thế giới. Cùng tìm hiểu các thêm thông tin hấp dẫn về giải đấu này tại bài viết dưới đây, gồm:
Nước chủ nhà
Đội tuyển tham dự
Thể thức thi đấu
Thời gian diễn ra
Sân vận động
Euro 2024 sẽ được tổ chức tại Đức, một quốc gia có truyền thống vàng của bóng đá châu Âu.
Đức là một đất nước giàu có lịch sử bóng đá với nhiều thành công quốc tế và trong những năm gần đây, họ đã thể hiện sức mạnh của mình ở cả mặt trận quốc tế và câu lạc bộ.
Việc tổ chức Euro 2024 tại Đức không chỉ là một cơ hội để thể hiện năng lực tổ chức tuyệt vời mà còn là một dịp để giới thiệu văn hóa và sức mạnh thể thao của quốc gia này.
Đội tuyển tham dự giải đấu Euro 2024
Euro 2024 sẽ quy tụ 24 đội tuyển hàng đầu từ châu Âu. Các đội tuyển này sẽ là những đại diện cho sự đa dạng văn hóa và phong cách chơi bóng đá trên khắp châu lục.
Các đội tuyển hàng đầu như Đức, Pháp, Tây Ban Nha, Bỉ, Italy, Anh và Hà Lan sẽ là những ứng viên nặng ký cho chức vô địch.
Trong khi đó, các đội tuyển nhỏ hơn như Iceland, Wales hay Áo cũng sẽ mang đến những bất ngờ và thách thức cho các đối thủ.
Các đội tuyển tham dự được chia thành 6 bảng đấu, gồm:
Bảng A: Đức, Scotland, Hungary và Thuỵ Sĩ
Bảng B: Tây Ban Nha, Croatia, Ý và Albania
Bảng C: Slovenia, Đan Mạch, Serbia và Anh
Bảng D: Ba Lan, Hà Lan, Áo và Pháp
Bảng E: Bỉ, Slovakia, Romania và Ukraina
Bảng F: Thổ Nhĩ Kỳ, Gruzia, Bồ Đào Nha và Cộng hoà Séc
На сайте https://t.me/s/m1xbet_ru ознакомьтесь с самыми актуальными, честными и свежими новостями, которые находятся в телеграме. Если вы любите азартные игры, тогда вам точно приглянется казино, в котором огромное количество слотов. При этом вы сможете выиграть джекпот. Все самые последние, актуальные новости из мира онлайн-казино находятся на этом портале. Также здесь, в первую очередь, выставляют промокоды, которые позволят существенно сэкономить и не тратить собственные деньги. В группе несколько десятков фото, различные записи.
What’s The Current Job Market For SEO Tool Software Professionals?
Seo Tool Software
Mobile Casino Tipico: Spielen Sie Ihre Lieblingsspiele Гјberall und jederzeit
In der heutigen digitalen Welt ist es wichtiger denn je, dass Online-Casinos ihre Dienste auch auf mobilen Geräten anbieten. Der Siegeszug von Smartphones und Tablets hat dazu geführt, dass immer mehr Menschen unterwegs spielen möchten. Tipico, einer der führenden Anbieter für Sportwetten und Online-Casino-Spiele, hat diesen Trend erkannt und bietet eine erstklassige mobile Casino-Plattform an.
Mit dem mobile Casino von Tipico kГ¶nnen Sie Ihre Lieblingsspiele wie Slots, Roulette und Blackjack bequem auf Ihrem Smartphone oder Tablet spielen. Die benutzerfreundliche OberflГ¤che und das Гјbersichtliche Design sorgen dafГјr, dass Sie auch unterwegs ein erstklassiges Spielerlebnis genieГџen kГ¶nnen. Egal, ob Sie in der U-Bahn sitzen, auf dem Weg zur Arbeit sind oder einfach nur auf der Couch entspannen – mit dem mobile Casino von Tipico haben Sie Ihre Lieblingsspiele immer in der Tasche.
Ein weiterer Vorteil des mobile Casino von Tipico ist die groГџe Auswahl an Spielen. Egal, ob Sie ein Fan von klassischen Tischspielen wie Poker und Baccarat sind oder lieber an modernen Slots mit hohen Jackpots spielen – bei Tipico finden Sie garantiert das passende Spiel fГјr sich. DarГјber hinaus bietet Tipico regelmäßig spannende Aktionen und Bonusangebote an, die Ihnen zusГ¤tzliche Gewinnchancen und SpaГџ beim Spielen bieten.
Wenn Sie also gerne Casino-Spiele spielen und dabei flexibel sein mГ¶chten, sollten Sie das mobile Casino von Tipico ausprobieren. Mit einer groГџen Auswahl an Spielen, einer benutzerfreundlichen OberflГ¤che und attraktiven Bonusangeboten ist Tipico die ideale Wahl fГјr mobiles Casino-Spielen. Also zГ¶gern Sie nicht und laden Sie die Tipico Casino-App noch heute herunter – Ihre Lieblingsspiele warten bereits auf Sie!
https://tipicocasino.one/
adipex mexico pharmacy
cost of propecia pill buy propecia for sale buy generic propecia
sugar defender: https://lindadicesare.com/
В наше время, когда диплом – это начало удачной карьеры в любом направлении, многие пытаются найти максимально простой путь получения качественного образования. Факт наличия официального документа об образовании переоценить просто невозможно. Ведь именно он открывает дверь перед любым человеком, желающим вступить в сообщество профессиональных специалистов или учиться в каком-либо университете.
В данном контексте мы предлагаем максимально быстро получить этот важный документ. Вы можете приобрести диплом нового или старого образца, что становится выгодным решением для человека, который не смог завершить образование или потерял документ. Все дипломы изготавливаются с особой аккуратностью, вниманием к мельчайшим нюансам, чтобы в результате получился 100% оригинальный документ.
Преимущество данного подхода заключается не только в том, что можно максимально быстро получить диплом. Весь процесс организован комфортно, с профессиональной поддержкой. Начиная от выбора требуемого образца до грамотного заполнения персональной информации и доставки в любое место страны — все будет находиться под абсолютным контролем наших мастеров.
Всем, кто хочет найти максимально быстрый способ получения необходимого документа, наша компания готова предложить отличное решение. Приобрести диплом – значит избежать продолжительного процесса обучения и сразу перейти к личным целям: к поступлению в университет или к началу успешной карьеры.
http://molbiol.ru/forums/index.php?showtopic=1088294
Zet Casino Promo Code 2020
Das Zet Casino ist ein beliebtes Online-Casino, das seinen Spielern eine Vielzahl von Spielen und interessanten Promotionen bietet. Und wer gerne ein bisschen mehr für sein Geld bekommen möchte, sollte unbedingt nach einem gültigen Zet Casino Promo Code 2020 Ausschau halten.
Ein Promo Code ist ein spezieller Code, den man bei der Einzahlung im Zet Casino eingeben kann, um von verschiedenen Bonusangeboten zu profitieren. Diese können beispielsweise zusätzliches Guthaben auf dem Spielerkonto, Freispiele oder Cashback-Boni sein.
Für das Jahr 2020 gibt es verschiedene Promo Codes, die man als Spieler nutzen kann, um sein Spielerlebnis im Zet Casino zu maximieren. Diese Codes können auf der Webseite des Casinos oder in verschiedenen Online-Gaming-Foren gefunden werden. Es lohnt sich also, regelmäßig nach neuen Promo Codes Ausschau zu halten, um kein Angebot zu verpassen.
Zudem bietet das Zet Casino auch regelmäßig eigene Promotionen an, bei denen man ohne einen speziellen Code von Bonusangeboten profitieren kann. Dazu gehören beispielsweise wöchentliche Cashback-Aktionen oder spezielle Turniere mit attraktiven Preisen.
Insgesamt bietet das Zet Casino seinen Spielern eine Vielzahl von Möglichkeiten, um von lukrativen Bonusangeboten zu profitieren. Wer also gerne Online-Casino spielt und ein bisschen mehr aus seinem Budget herausholen möchte, sollte unbedingt die aktuellen Promo Codes und Aktionen im Zet Casino im Auge behalten. Viel Spaß und viel Erfolg beim Spielen!
https://zetcasino.one/
Tipico Casino Bonuscode
Das Tipico Casino bietet seinen Kunden regelmäßig attraktive Bonusaktionen an, um das Spielerlebnis noch spannender und lukrativer zu gestalten. Einer der beliebtesten Wege, von diesen Bonusangeboten zu profitieren, ist die Verwendung von Bonuscodes.
Ein Bonuscode ist eine spezielle Kombination aus Buchstaben und Zahlen, die es dem Spieler ermöglicht, einen bestimmten Bonus zu erhalten, wenn er ihn bei der Einzahlung im Casino eingibt. Diese Codes können auf der Website des Casinos, in Werbeaktionen oder per E-Mail veröffentlicht werden.
Um den Tipico Casino Bonuscode zu nutzen, müssen Spieler zuerst ein Konto im Casino registrieren und eine Einzahlung tätigen. Anschließend können sie den Code eingeben, um den entsprechenden Bonus zu erhalten. Dies kann zum Beispiel zusätzliches Spielguthaben, Freispiele oder andere Vergünstigungen sein.
Es ist wichtig, die Bedingungen und Umsatzanforderungen für den jeweiligen Bonus zu lesen, um sicherzustellen, dass man die Vorteile vollständig nutzen kann. Oftmals müssen bestimmte Umsatzbedingungen erfüllt werden, bevor Gewinne aus dem Bonus ausgezahlt werden können.
Der Tipico Casino Bonuscode kann eine großartige Möglichkeit sein, um das Spielerkonto aufzustocken und noch mehr Spaß beim Spielen zu haben. Es lohnt sich daher, regelmäßig nach neuen Bonusaktionen Ausschau zu halten und die Codes rechtzeitig einzugeben, um die lukrativen Angebote nicht zu verpassen. Viel Glück und Spaß beim Spielen im Tipico Casino!
https://tipicocasino.one/
20 Reasons Why Backlink Service Will Never Be Forgotten Marketing Services (Toolbarqueries.Google.Ac)
cialis soft tabs pills button – levitra soft pills impressive viagra oral jelly glitter
get generic clomid tablets: can i buy generic clomid without rx – can i order cheap clomid pills
На сайте https://my-tvset.ru/ изучите увлекательную, полезную информацию, которая касается того, как правильно выполнить ремонт, создать уют и комфортные условия. Так вы узнаете о том, как правильно выбрать бежевую плитку, а также затирку. Даны все необходимые рекомендации, важные советы, которые помогут решить ситуацию. Имеются важные рекомендации относительно обустройства квартиры: гостиной, ванной, комнаты. Вы узнаете о том, как правильно организовать системы отопления, подобрать светильники, люстры, столы.
The 10 Most Scariest Things About Local Business SEO Local business seo
http://lisinopril.club/# purchase lisinopril
cialis soft tabs online crack – caverta online chest viagra oral jelly carry
Willkommen im Zet Casino! Als neuer Spieler haben Sie die Möglichkeit, von einem großzügigen Willkommensbonus zu profitieren. Dieser Bonus ist eine tolle Möglichkeit, um Ihr Spielerlebnis im Zet Casino zu beginnen und Ihre Gewinnchancen zu steigern.
Der Willkommensbonus im Zet Casino besteht aus einem 100% Einzahlungsbonus von bis zu 500€ sowie 200 Freispielen für ausgewählte Spielautomaten. Um diesen Bonus zu erhalten, müssen Sie lediglich eine Mindesteinzahlung von 20€ tätigen. Sobald die Einzahlung getätigt wurde, wird der Bonus automatisch auf Ihr Konto gutgeschrieben.
Um den Bonus und die damit verbundenen Gewinne auszahlen zu können, müssen Sie die Umsatzanforderungen erfüllen. Diese betragen das 40-fache des Bonusbetrags. Beachten Sie, dass nicht alle Spiele zu den Umsatzanforderungen beitragen. Es ist daher ratsam, sich vorab die Bonusbedingungen durchzulesen.
Neben dem Willkommensbonus bietet das Zet Casino auch regelmäßig Aktionen und Promotionen für bestehende Spieler an. Diese können unter anderem Freispiele, Einzahlungsboni oder Cashback-Angebote beinhalten. Es lohnt sich daher, regelmäßig die Promotionsseite des Casinos zu besuchen, um keine Angebote zu verpassen.
Insgesamt bietet das Zet Casino eine Vielzahl von Spielen, darunter Spielautomaten, Tischspiele und Live-Casino-Spiele von bekannten Anbietern wie NetEnt, Microgaming und Evolution Gaming. Mit dem Willkommensbonus und den regelmäßigen Promotionen haben Sie die Möglichkeit, Ihr Spielerlebnis im Zet Casino zu maximieren und hoffentlich auch einige Gewinne zu erzielen.
Also worauf warten Sie noch? Registrieren Sie sich noch heute im Zet Casino und sichern Sie sich Ihren Willkommensbonus fГјr ein unvergessliches Spielerlebnis. Viel GlГјck und SpaГџ beim Spielen!
https://zetcasino.one/
Tipico Casino ist ein beliebter Online-Casino-Anbieter, der eine Vielzahl von Spielen und MГ¶glichkeiten zum Spielen bietet. Doch in letzter Zeit hГ¤ufen sich Beschwerden von Spielern, dass die Website des Tipico Casinos “neu down” ist und nicht richtig funktioniert.
Viele Spieler berichten davon, dass sie Schwierigkeiten haben, sich auf der Website anzumelden oder Spiele zu laden. Dies sorgt für Frust und Unzufriedenheit bei den Nutzern, die gerne ihre Lieblingsspiele spielen möchten.
Es ist unklar, was genau der Grund für die technischen Probleme bei Tipico Casino ist, aber die Betreiber des Casinos arbeiten bereits daran, das Problem zu lösen und die Website so schnell wie möglich wieder voll funktionsfähig zu machen.
In der Zwischenzeit sollten Spieler Geduld haben und sich an den Kundenservice von Tipico Casino wenden, wenn sie Hilfe benötigen oder Fragen haben. Es ist wichtig, dass die Betreiber des Casinos transparent und kommunikativ sind, um das Vertrauen der Spieler zu erhalten.
Wir hoffen, dass das Problem mit der Website von Tipico Casino bald behoben wird und die Spieler wieder ungestört ihrem Spielvergnügen nachgehen können. Bis dahin heißt es abwarten und die Geduld nicht verlieren.
https://tipicocasino.one/
difference between sildenafil and tadalafil
Компания на профессиональном уровне занимается лазерной гравировкой на жетонах, шильдах, ложках. Кроме того, создает клише, производит гравировку по кругу и на различных предметах. При необходимости специалист может приехать на объект, чтобы оказать услугу непосредственно на территории заказчика. На сайте https://grsuv.ru/ ознакомьтесь с полным перечнем услуг, которые вы сможете заказать в этой компании и по лучшей стоимости.
В нашем обществе, где диплом – это начало успешной карьеры в любой отрасли, многие стараются найти максимально быстрый и простой путь получения образования. Наличие официального документа об образовании переоценить невозможно. Ведь именно диплом открывает дверь перед каждым человеком, который стремится начать профессиональную деятельность или учиться в высшем учебном заведении.
Предлагаем быстро получить этот важный документ. Вы сможете купить диплом, и это будет выгодным решением для человека, который не смог завершить образование или потерял документ. Все дипломы изготавливаются с особой аккуратностью, вниманием к мельчайшим элементам. В результате вы получите полностью оригинальный документ.
Плюсы этого решения состоят не только в том, что можно максимально быстро получить диплом. Весь процесс организован удобно, с профессиональной поддержкой. Начиная от выбора нужного образца до консультации по заполнению персональных данных и доставки в любой регион страны — все под полным контролем наших специалистов.
В итоге, для тех, кто хочет найти максимально быстрый способ получить необходимый документ, наша компания может предложить отличное решение. Приобрести диплом – значит избежать продолжительного процесса обучения и сразу перейти к достижению собственных целей: к поступлению в университет или к началу трудовой карьеры.
http://molbiol.ru/forums/index.php?showtopic=1088312
neurontin 30 mg neurontin gel buy gabapentin online
Желаете приобрести кондиционер в Москве с установкой? РусКондиционер – то, что вам нужно! Интернет магазин предлагает большой ассортимент проверенного климатического оборудования от известных производителей. Ищете купить кондиционер с установкой? Ruscondicioner.ru – сайт, где имеется исключительно продукция, прошедшая сертификацию. Здесь вы можете детальнее ознакомиться с условиями оплаты и доставки. У нас можно не только купить кондиционер, но и заказать его установку. Наши специалисты имеют солидный опыт в данной области, работа будет выполнена профессионально.
На сайте https://t.me/s/mpinup ознакомьтесь с новостями, которые посвящены популярному онлайн-заведению «PinUP». Удача улыбнется и вам, если примите участие в турнирах. Это возможность заработать на свою мечту. Теперь и вы сможете присоединиться к группе. На этом сайте всегда выкладывают самые первые новости, промокоды и все то, что поможет получить неплохие деньги. В этой группе огромное количество интересных записей, а также любопытных фото. Регулярно публикуются новые данные, актуальные новости, которые помогут больше узнать о казино.
Zet Casino ist ein aufstrebendes Online-Casino, das sich auf dem Markt einen Namen gemacht hat. Mit einer Vielzahl von Spielen, großzügigen Bonusangeboten und einer benutzerfreundlichen Website ist Zet Casino eine gute Wahl für alle, die ihr Glück versuchen möchten.
Das Casino bietet eine breite Palette von Spielen, darunter Slots, Tischspiele, Live-Casino-Spiele und vieles mehr. Mit Spielen von renommierten Anbietern wie NetEnt, Microgaming, Play’n GO und vielen anderen, ist fГјr jeden Geschmack etwas dabei. Die Spiele sind alle in hoher QualitГ¤t mit toller Grafik und Soundeffekten gestaltet.
Ein weiterer großer Vorteil von Zet Casino sind die großzügigen Bonusangebote. Neue Spieler können einen Willkommensbonus erhalten, der in Form von Bonusgeld und Freispielen angeboten wird. Es gibt auch regelmäßige Promotionen und Turniere, bei denen Spieler zusätzliche Belohnungen verdienen können.
Die Website von Zet Casino ist benutzerfreundlich gestaltet und einfach zu navigieren. Spieler können leicht durch die verschiedenen Spiele und Funktionen der Seite stöbern und finden schnell das, wonach sie suchen. Zudem bietet das Casino eine sichere und geschützte Spielumgebung, in der die persönlichen Daten der Spieler jederzeit sicher sind.
Insgesamt ist Zet Casino eine gute Wahl fГјr alle, die auf der Suche nach einem unterhaltsamen und lohnenden Online-Casino-Erlebnis sind. Mit einer Vielzahl von Spielen, groГџzГјgigen Boni und einer benutzerfreundlichen Website ist das Casino definitiv einen Besuch wert. Probieren Sie Ihr GlГјck noch heute bei Zet Casino aus und erleben Sie die Spannung und Aufregung des Online-GlГјcksspiels.
https://zetcasino.one/
Хотите приобрести по недорогой стоимости из нержавеющей стали клапаны и арматуру? Мы вам в этом с радостью готовы помочь. Главные достоинства нашей продукции: долгий срок эксплуатации и большая надежность. Ищете запорная арматура для пищевой промышленности? Inoxpa.ru – сайт, где вы узнаете о том, где используется арматура из нержавеющей стали. Здесь также можете в любое удобное для вас время ознакомиться с высококачественной продукцией проверенной компании INOXPA. Возникли вопросы? Обратитесь к нам, мы с радостью на них ответим. Звоните прямо сейчас!
Компания «Octastudio» специализируется на таких услугах, как: разработка проектов на 1С битрикс, переработка или доработка имеющегося сайта, редактирование контента, анализ конкурентов. На сайте https://octa-studio.ru ознакомьтесь с полным перечнем услуг, которые можно заказать прямо сейчас, оформив заявку либо позвонив по телефону. Также к основным услугам относят и обновление структуры, модернизацию функционала, подготовку портала для продвижения.
lipinpril: lisinopril price in india – lisinopril 40 mg brand name
10 Tips For Quickly Getting What Is Tier 2 Backlinks tier 1 backlink
http://propeciaf.online/# propecia tablets
Zet Casino Auszahlung Funktioniert Nicht: Was tun?
Das Zet Casino ist bei vielen Spielern beliebt, aber manchmal gibt es Probleme mit der Auszahlung. Wenn die Auszahlungsfunktion nicht funktioniert, kann dies frustrierend sein. Es gibt jedoch einige Schritte, die Sie unternehmen können, um das Problem zu lösen.
Als Erstes sollten Sie sicherstellen, dass Sie alle Bedingungen und Konditionen des Casinos gelesen und verstanden haben. Unter Umständen gibt es bestimmte Anforderungen, die erfüllt sein müssen, bevor Sie eine Auszahlung vornehmen können. Überprüfen Sie also noch einmal alle Regeln des Casinos.
Wenn Sie sicher sind, dass Sie alle Voraussetzungen erfüllen, können Sie den Kundendienst des Casinos kontaktieren. Dieser sollte in der Lage sein, Ihnen bei der Lösung des Problems zu helfen. Geben Sie alle relevanten Informationen an, wie zum Beispiel Ihre Benutzername und die Details Ihrer Auszahlung.
Es kann auch hilfreich sein, Ihren Browserverlauf zu löschen oder es mit einem anderen Browser zu versuchen. Manchmal kann ein veralteter Browser oder Cookies im Cache zu Problemen führen. Ein einfacher Neustart Ihres Geräts kann ebenfalls helfen.
Sollte keine dieser Maßnahmen das Problem lösen, könnte es sein, dass es ein technisches Problem auf Seiten des Casinos gibt. In diesem Fall sollten Sie Geduld haben und in regelmäßigen Abständen überprüfen, ob die Situation sich verbessert hat.
Insgesamt ist es wichtig, ruhig zu bleiben und das Problem systematisch anzugehen. Mit Geduld und den richtigen Schritten sollte es Ihnen gelingen, die Auszahlungsfunktion im Zet Casino wieder zum Laufen zu bringen.
https://zetcasino.one/
В нашем мире, где диплом становится началом удачной карьеры в любом направлении, многие ищут максимально быстрый и простой путь получения образования. Наличие официального документа об образовании переоценить просто невозможно. Ведь именно он открывает двери перед каждым человеком, желающим начать профессиональную деятельность или учиться в ВУЗе.
Наша компания предлагает максимально быстро получить этот важный документ. Вы имеете возможность заказать диплом, что становится выгодным решением для всех, кто не смог завершить образование, утратил документ или желает исправить свои оценки. дипломы изготавливаются с особой тщательностью, вниманием к мельчайшим деталям. В итоге вы получите документ, 100% соответствующий оригиналу.
Преимущество такого подхода состоит не только в том, что можно оперативно получить диплом. Весь процесс организован комфортно, с нашей поддержкой. Начав от выбора нужного образца диплома до консультации по заполнению персональной информации и доставки в любое место страны — все находится под полным контролем опытных мастеров.
Для тех, кто пытается найти максимально быстрый способ получения требуемого документа, наша компания предлагает выгодное решение. Купить диплом – это значит избежать длительного процесса обучения и не теряя времени переходить к своим целям, будь то поступление в ВУЗ или начало профессиональной карьеры.
http://forum.autoset.ru/viewtopic.php?p=142264
GAMETORRENT.NET – ресурс, где вы найдете все нужное для погружения в захватывающий мир игр. Мы предоставляем огромный ассортимент любых жанров. У нас имеется множество головоломок для разминки мозга и аркад, также шутеры, ролевые игры и многое другое. Гарантируем, что отыщите то, что вам необходимо. Ищете скачать игры драки на компьютер через торрент бесплатно? Gametorrent.net – сайт, где вас ждут новинки индустрии игр. Не сомневайтесь в том, что получите только лучшие игры без вредоносных программ и вирусов. Окунитесь в мир неимоверных возможностей, скачивайте игры уже сейчас!
Boomerang Casino: Das beste Spiel
Boomerang Casino ist eines der beliebtesten Online-Casinos, das eine Vielzahl von Spielen und UnterhaltungsmГ¶glichkeiten bietet. Eines der besten Spiele, die Sie im Boomerang Casino finden kГ¶nnen, ist das Spiel “Miglior Gioco”. Dieses Spiel ist ein aufregendes und unterhaltsames Spiel, das die Spieler stundenlang fesseln wird.
“Miglior Gioco” ist ein Spielautomat, der mit hochwertiger Grafik und Soundeffekten entwickelt wurde. Das Spiel bietet den Spielern eine einzigartige Erfahrung und die Chance, groГџe Gewinne zu erzielen. Die Walzen sind mit verschiedenen Symbolen wie bunten FrГјchten, GeldsГ¤cken und GlГјckssymbolen gefГјllt, die das Spiel noch spannender machen.
Das Besondere an “Miglior Gioco” ist die Vielzahl von Bonusfunktionen, die das Spiel bietet. Die Spieler haben die MГ¶glichkeit, Freispiele, Multiplikatoren und Bonusrunden zu aktivieren, die ihre Gewinnchancen erhГ¶hen. DarГјber hinaus gibt es auch ein Risikospiel, bei dem die Spieler ihre Gewinne verdoppeln kГ¶nnen, wenn sie die richtige Kartenfarbe erraten.
Die Spieler kГ¶nnen “Miglior Gioco” im Boomerang Casino sowohl auf dem Desktop als auch auf mobilen GerГ¤ten spielen. Das Spiel ist einfach zu bedienen und bietet eine benutzerfreundliche OberflГ¤che, die es den Spielern leicht macht, sich zu orientieren und das Spiel zu genieГџen.
Insgesamt ist “Miglior Gioco” ein aufregendes Spiel, das die Spieler in den Bann zieht und ihnen eine unterhaltsame und spannende Spielerfahrung bietet. Wenn Sie nach dem besten Spiel im Boomerang Casino suchen, sollten Sie unbedingt “Miglior Gioco” ausprobieren. Viel GlГјck und viel SpaГџ beim Spielen!
https://boomerangcasino.one/
11 Ways To Completely Redesign Your Best Vps For SEO
Tools Seo Link Tools
buy propecia for sale buy generic propecia pill order cheap propecia without dr prescription
Zet Casino Einzahlungsmöglichkeiten
Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Einzahlungsmöglichkeiten für seine Spieler anbietet. Die Vielfalt der verfügbaren Optionen macht es einfach, Geld auf das Spielerkonto einzuzahlen und schnell mit dem Spielen zu beginnen.
Eine der beliebtesten Einzahlungsmethoden bei Zet Casino ist die Verwendung von Kredit- oder Debitkarten wie Visa und Mastercard. Diese Methode ist einfach und schnell und ermöglicht es den Spielern, sofort mit dem Spielen zu beginnen.
Eine weitere häufig genutzte Option ist die Zahlung per E-Wallet, wie zum Beispiel Skrill oder Neteller. Diese Methoden sind besonders beliebt, da sie eine zusätzliche Sicherheitsebene bieten und die Spieler ihre Transaktionen schnell und einfach abwickeln können.
Zet Casino bietet auch die Möglichkeit, per Banküberweisung einzuzahlen. Diese Methode kann etwas länger dauern als andere Methoden, ist jedoch eine sichere und zuverlässige Option für Spieler, die keine E-Wallets oder Kreditkarten verwenden möchten.
Darüber hinaus akzeptiert Zet Casino auch verschiedene Kryptowährungen wie Bitcoin, Ethereum und Litecoin. Dies ermöglicht es den Spielern, ihre Einzahlungen anonym und sicher abzuwickeln.
Insgesamt bietet Zet Casino eine Vielzahl von Einzahlungsmöglichkeiten, um den Bedürfnissen und Vorlieben seiner Spieler gerecht zu werden. Egal für welche Methode Sie sich entscheiden, Sie können sicher sein, dass Ihre Transaktionen sicher und zuverlässig abgewickelt werden. Besuchen Sie noch heute Zet Casino und entdecken Sie die Vielzahl der Einzahlungsmöglichkeiten!
https://zetcasino.one/
prozac overseas pharmacy
В наше время, когда диплом становится началом удачной карьеры в любом направлении, многие стараются найти максимально простой путь получения качественного образования. Наличие официального документа трудно переоценить. Ведь диплом открывает дверь перед любым человеком, который хочет вступить в сообщество профессионалов или продолжить обучение в высшем учебном заведении.
В данном контексте мы предлагаем оперативно получить этот необходимый документ. Вы можете заказать диплом нового или старого образца, что будет выгодным решением для человека, который не смог закончить обучение, утратил документ или желает исправить свои оценки. диплом изготавливается аккуратно, с особым вниманием к мельчайшим элементам, чтобы в итоге получился 100% оригинальный документ.
Плюсы такого подхода заключаются не только в том, что вы максимально быстро получите диплом. Процесс организовывается удобно, с профессиональной поддержкой. Начав от выбора подходящего образца диплома до консультаций по заполнению персональных данных и доставки по стране — все под абсолютным контролем качественных специалистов.
Всем, кто ищет оперативный способ получить необходимый документ, наша компания может предложить выгодное решение. Купить диплом – значит избежать долгого обучения и не теряя времени перейти к своим целям: к поступлению в университет или к началу успешной карьеры.
http://poker.forum-top.ru/viewtopic.php?id=659
prescription price for neurontin: order neurontin – canada neurontin 100mg lowest price
На сайте https://play.google.com/store/apps/details?id=com.amazon.mShop.android.shoppi вы сможете сыграть в увлекательную, интересную игру – Bamboo Bastion, которая радует своей привлекательной графикой, интересным сюжетом, который завораживает с самых первых минут. Такая игра считается именно тем, что вы так давно искали. Суть заключается в том, чтобы вы быстро среагировали на ситуацию и приняли решение. Скачайте ее прямо сейчас на свое устройство. Играйте в нее тогда, когда вам удобно, даже находясь в путешествии или длительной поездке.
Das Boomerang Casino ist eine relativ neue Online-GlГјcksspielplattform, die in Deutschland immer beliebter wird. Viele Spieler fragen sich jedoch, ob das Spielen im Boomerang Casino legal ist.
Die Antwort darauf ist ja, das Boomerang Casino ist in Deutschland legal. Das Casino verfügt über eine Lizenz der Malta Gaming Authority, einer renommierten Glücksspielbehörde, die sicherstellt, dass das Casino strenge Richtlinien einhält und faire Spiele anbietet.
Spieler können also beruhigt sein, wenn sie im Boomerang Casino spielen. Sie können sicher sein, dass ihre persönlichen und finanziellen Daten geschützt sind und dass sie in einer sicheren und vertrauenswürdigen Umgebung spielen.
Das Boomerang Casino bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele und Live-Casino-Spiele, die alle von führenden Softwareanbietern entwickelt wurden. Spieler können auch von lukrativen Boni und Aktionen profitieren, die regelmäßig angeboten werden.
Insgesamt ist das Boomerang Casino eine gute Wahl fГјr Spieler in Deutschland, die auf der Suche nach einer sicheren und unterhaltsamen GlГјcksspielplattform sind. Mit seiner Lizenz und seinem Ruf als vertrauenswГјrdiges Casino ist das Boomerang Casino definitiv eine gute Wahl fГјr deutsche Spieler.
https://boomerangcasino.one/
http://cytotec.xyz/# buy misoprostol over the counter
На сайте https://gderaznica.ru/ почитайте интересную, увлекательную и любопытную информацию, которая касается таких важных тем, как: общество, экономика, медицина, технологии и многое другое. Все статьи написаны высококлассными, опытными авторами, которые хорошо разбираются в перечисленных темах. Рассматриваются и такие вопросы, как преимущества автоломбардов, различия цветов самых разных видов. Все статьи невероятно интересные, а потому читать захочется их и вам. Регулярно добавляются новые полезные материалы.
В современном мире, где диплом – это начало успешной карьеры в любой области, многие пытаются найти максимально быстрый и простой путь получения качественного образования. Факт наличия документа об образовании переоценить невозможно. Ведь диплом открывает двери перед любым человеком, желающим вступить в сообщество квалифицированных специалистов или продолжить обучение в университете.
Наша компания предлагает оперативно получить этот важный документ. Вы имеете возможность приобрести диплом, и это становится отличным решением для человека, который не смог завершить образование или утратил документ. Все дипломы выпускаются аккуратно, с особым вниманием ко всем элементам. В итоге вы получите 100% оригинальный документ.
Преимущество этого решения состоит не только в том, что можно быстро получить свой диплом. Весь процесс организован комфортно и легко, с профессиональной поддержкой. Начиная от выбора требуемого образца документа до грамотного заполнения персональной информации и доставки по России — все под абсолютным контролем наших специалистов.
Всем, кто пытается найти быстрый и простой способ получения необходимого документа, наша компания готова предложить выгодное решение. Купить диплом – значит избежать длительного обучения и сразу переходить к своим целям: к поступлению в ВУЗ или к началу успешной карьеры.
http://ipkins.ru/rubric/1689403/index.html
legit online pharmacy
world-news-365.com
ГК «Норфост» с 2006 года занимается строительством домов, которые полностью соответствуют самым высоким требованиям и предпочтениям клиентов. Для того чтобы быстрее определиться с выбором, изучите на сайте https://gknorfost.ru/ каталог последних проектов с ценами, планировками. Представлены как одноэтажные, так и двухэтажные дома.
https://tzona.org
international pharmacy no prescription
lisinopril 10 mg online no prescription lisinopril 5 mg tablet price in india lisinopril 10 mg without prescription
Tipico Guthaben auf Casino
Wenn es um Online-Glücksspiele geht, ist Tipico eines der bekanntesten und beliebtesten Online-Casinos in Deutschland. Das Casino bietet eine Vielzahl von Spielen, darunter Spielautomaten, Tischspiele, Live-Casino-Spiele und vieles mehr. Ein wichtiger Aspekt des Spiels bei Tipico ist das Guthaben, das Spieler nutzen können, um Einsätze zu platzieren und an Spielen teilzunehmen.
Das Guthaben auf dem Tipico Casino Konto kann auf verschiedene Weise aufgeladen werden. Eine der einfachsten Methoden ist die Verwendung von Kreditkarten wie Visa und MasterCard. Spieler können auch mit verschiedenen E-Wallets wie PayPal, Skrill und Neteller einzahlen. Darüber hinaus bietet Tipico auch die Möglichkeit, per Banküberweisung oder Paysafecard einzuzahlen.
Sobald das Guthaben auf dem Casino-Konto gutgeschrieben wurde, haben Spieler die Möglichkeit, an ihren Lieblingsspielen teilzunehmen und echte Gewinne zu erzielen. Das Guthaben kann auch für Boni und Promotionen verwendet werden, die von Tipico regelmäßig angeboten werden. Diese Boni können zusätzliches Guthaben, Freispiele oder andere attraktive Angebote beinhalten, die das Spielerlebnis noch spannender machen.
Es ist wichtig zu beachten, dass Spieler verantwortungsbewusst mit ihrem Guthaben umgehen sollten. Glücksspiel sollte immer als Unterhaltung betrachtet werden und Spieler sollten niemals mehr Geld einsetzen, als sie sich leisten können zu verlieren. Tipico bietet verschiedene Möglichkeiten zur Selbstregulierung, wie zum Beispiel Einzahlungslimits und Selbstausschluss, um sicherzustellen, dass Spieler ihre Gewohnheiten im Auge behalten.
Insgesamt bietet das Tipico Casino eine sichere und unterhaltsame Umgebung für Glücksspiele. Mit verschiedenen Einzahlungsmethoden, spannenden Spielen und attraktiven Boni ist das Casino eine beliebte Wahl für Spieler in Deutschland. Egal, ob man Anfänger oder erfahrener Spieler ist, Tipico bietet für jeden etwas und sorgt für ein erstklassiges Spielerlebnis.
https://tipicocasino.one/
В нашем обществе, где диплом является началом удачной карьеры в любой области, многие стараются найти максимально быстрый и простой путь получения качественного образования. Наличие официального документа трудно переоценить. Ведь диплом открывает дверь перед каждым человеком, который хочет начать профессиональную деятельность или учиться в университете.
В данном контексте наша компания предлагает максимально быстро получить этот важный документ. Вы можете заказать диплом, и это становится отличным решением для всех, кто не смог закончить обучение или утратил документ. диплом изготавливается аккуратно, с максимальным вниманием к мельчайшим элементам. На выходе вы получите 100% оригинальный документ.
Превосходство подобного решения заключается не только в том, что вы сможете быстро получить свой диплом. Весь процесс организован комфортно, с нашей поддержкой. От выбора подходящего образца до консультации по заполнению персональных данных и доставки в любое место России — все под полным контролем качественных мастеров.
В итоге, для тех, кто хочет найти максимально быстрый способ получения требуемого документа, наша услуга предлагает выгодное решение. Купить диплом – значит избежать долгого обучения и не теряя времени перейти к достижению личных целей, будь то поступление в ВУЗ или старт профессиональной карьеры.
http://krc.mybb.ru/viewtopic.php?id=118
Сегодня, когда диплом – это начало отличной карьеры в любом направлении, многие ищут максимально простой путь получения образования. Факт наличия документа об образовании трудно переоценить. Ведь диплом открывает дверь перед любым человеком, который хочет начать профессиональную деятельность или продолжить обучение в ВУЗе.
В данном контексте наша компания предлагает максимально быстро получить этот важный документ. Вы можете купить диплом, что становится удачным решением для всех, кто не смог закончить обучение или потерял документ. Все дипломы производятся аккуратно, с особым вниманием к мельчайшим элементам, чтобы в итоге получился 100% оригинальный документ.
Превосходство данного решения заключается не только в том, что вы сможете максимально быстро получить свой диплом. Весь процесс организовывается просто и легко, с нашей поддержкой. От выбора подходящего образца до точного заполнения личных данных и доставки по стране — все будет находиться под абсолютным контролем качественных специалистов.
В итоге, всем, кто хочет найти быстрый способ получения требуемого документа, наша компания предлагает выгодное решение. Заказать диплом – это значит избежать длительного обучения и не теряя времени переходить к своим целям, будь то поступление в университет или начало карьеры.
https://bohn.ru/v-napravlenii-luchiny-i-loshadki/
repair organizations
Boomerang Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen und spannenden Promotionen anbietet. Eines dieser Angebote ist der Boomerang Casino Kod Promocyjny, der es den Spielern ermöglicht, zusätzliche Belohnungen zu erhalten.
Der Boomerang Casino Kod Promocyjny ist ein spezieller Bonuscode, den die Spieler verwenden können, um verschiedene Arten von Belohnungen zu erhalten. Diese können Freispiele, Bonusgeld oder andere Vergünstigungen sein, die das Spielerlebnis im Casino noch aufregender machen.
Um den Boomerang Casino Kod Promocyjny einzulösen, müssen die Spieler lediglich den Code während ihrer Einzahlung eingeben oder ihn bei speziellen Promotionen verwenden. Sobald der Code akzeptiert wurde, werden die entsprechenden Belohnungen automatisch dem Konto des Spielers gutgeschrieben.
Es lohnt sich, regelmäßig nach neuen Boomerang Casino Kod Promocyjny Codes Ausschau zu halten, da das Casino häufig neue Promotionen bietet und Spieler die Möglichkeit haben, zusätzliche Belohnungen zu erhalten.
Insgesamt ist der Boomerang Casino Kod Promocyjny eine großartige Möglichkeit für Spieler, ihre Gewinnchancen zu steigern und noch mehr Spaß beim Spielen im Boomerang Casino zu haben. Wer also auf der Suche nach spannenden Belohnungen und aufregenden Spielen ist, sollte den Boomerang Casino Kod Promocyjny auf jeden Fall ausprobieren. Viel Glück und viel Spaß beim Spielen!
https://boomerangcasino.one/
buy cytotec in usa: п»їcytotec pills online – buy cytotec over the counter
http://propeciaf.online/# propecia pills
В нашем мире, где диплом – это начало отличной карьеры в любой отрасли, многие стараются найти максимально быстрый путь получения образования. Факт наличия официального документа трудно переоценить. Ведь именно он открывает дверь перед людьми, стремящимися вступить в профессиональное сообщество или учиться в университете.
Наша компания предлагает максимально быстро получить этот важный документ. Вы можете заказать диплом нового или старого образца, что является выгодным решением для человека, который не смог завершить образование или потерял документ. диплом изготавливается аккуратно, с максимальным вниманием к мельчайшим нюансам, чтобы на выходе получился полностью оригинальный документ.
Плюсы подобного подхода состоят не только в том, что можно максимально быстро получить свой диплом. Процесс организован комфортно, с профессиональной поддержкой. От выбора подходящего образца до правильного заполнения личных данных и доставки по стране — все под абсолютным контролем квалифицированных специалистов.
В результате, для тех, кто пытается найти быстрый способ получения необходимого документа, наша компания предлагает выгодное решение. Заказать диплом – значит избежать долгого обучения и не теряя времени переходить к своим целям: к поступлению в университет или к началу трудовой карьеры.
https://seo-pes.ru/astrologija/193-k-kakim-znakam-zodiaka-pridet-uspeh-v-novom-2020-godu.html
repair of appliances
Хотите купить в Москве с установкой кондиционер? РусКондиционер – то, что вам нужно! Интернет магазин предлагает большой ассортимент проверенного климатического оборудования от известных производителей. Ищете купить кондиционер в Москве недорого? Ruscondicioner.ru – сайт, где представлена только сертифицированная продукция. Здесь вы подробнее ознакомитесь с условиями доставки и оплаты. У нас можно не только купить кондиционер, но и заказать его установку. Наши специалисты имеют солидный опыт в данной области, работа будет выполнена профессионально.
Die Tipico Casino App ist eine beliebte Plattform für Glücksspiele und Unterhaltung, die von vielen Spielern gerne genutzt wird. Doch was passiert, wenn die App plötzlich nicht mehr funktioniert?
Wenn die Tipico Casino App nicht mehr richtig funktioniert, kann das verschiedene GrГјnde haben. Oftmals liegt es an einer schlechten Internetverbindung, die zu Verbindungsproblemen fГјhren kann. In diesem Fall sollte man sicherstellen, dass man mit einem stabilen WLAN oder mobilen Internet verbunden ist.
Es kann auch sein, dass die App selbst ein technisches Problem hat. In diesem Fall kann es helfen, die App zu aktualisieren oder sogar neu zu installieren. Manchmal kann es auch hilfreich sein, das Gerät neu zu starten, um mögliche Fehler zu beheben.
Sollte die App trotzdem nicht funktionieren, kann es auch sein, dass es ein Problem mit dem Tipico Server gibt. In diesem Fall kann man versuchen, die App zu einem späteren Zeitpunkt erneut zu starten oder den Tipico Kundendienst zu kontaktieren, um weitere Informationen zu erhalten.
Es ist wichtig, Ruhe zu bewahren und nicht gleich in Panik zu geraten, wenn die Tipico Casino App nicht funktioniert. Oftmals lassen sich die Probleme schnell und einfach lösen, indem man die oben genannten Tipps befolgt.
Insgesamt ist die Tipico Casino App eine zuverlässige Plattform für Glücksspiele, die in den meisten Fällen reibungslos funktioniert. Sollte es dennoch zu Problemen kommen, sollte man geduldig bleiben und die genannten Lösungsansätze ausprobieren.
https://tipicocasino.one/
cost cheap propecia without a prescription get propecia propecia tablet
Зайдите на сайт https://ckad165.ru/ и вы сможете ознакомиться с Индустриальным парком в 67 км от Москвы ЦКАД 165. Это новая площадка для производственных и складских объектов со всей необходимой инфраструктурой, собственным съездом с ЦКАД и менеджментом управляющей компании. Узнайте подробнее на сайте.
Привет, дорогой читатель!
Получите российский диплом по доступной цене с гарантией прохождения проверок и доставкой в любой город РФ без предоплаты!
Наш интернет-магазин предлагает купить российский диплом по выгодной цене, с гарантией прохождения всех проверок
http://www.diploman-russiyan.ru
Ищете новые анонсы серверов lineage 2? LA2-ANONS.COM – то, что вам нужно. Поможем вам в подборе достойного игрового сервера. Анонсы серверов Lineage 2 на нашем ресурсе постоянно актуализируются, что дает возможность абсолютно каждому геймеру быть в числе первых зарегистрированных. Интересует сервера ла2? La2-anons.com – сайт, мы каждый день работаем над его функционалом. При выборе сервера для игры Lineage 2, советуем свое внимание обратить на платформы, где написано VIP. Предоставляем исключительно актуальную информацию, с ней можете ознакомиться уже сейчас.
Добрый день всем!
Недорого и без проблем купить диплом института, техникума, колледжа выгоднее всего у Нас, с доставкой по РФ
http://www.diplomanc-russia24.ru
Zet Casino Bonus ohne Einzahlung
Das Zet Casino ist ein beliebtes Online-Casino, das seinen Spielern eine Vielzahl von spannenden Spielen und attraktiven Bonusangeboten bietet. Einer der beliebtesten Bonusangebote, das das Zet Casino seinen neuen Spielern zur VerfГјgung stellt, ist der Bonus ohne Einzahlung.
Der Bonus ohne Einzahlung ermöglicht es Spielern, das Casino auszuprobieren, ohne eigenes Geld riskieren zu müssen. Neue Spieler erhalten bei der Registrierung im Zet Casino einen Bonus ohne Einzahlung, der es ihnen ermöglicht, verschiedene Spiele im Casino zu testen und echtes Geld zu gewinnen.
Um den Bonus ohne Einzahlung zu erhalten, müssen Spieler lediglich ein Konto im Zet Casino erstellen und den Bonuscode eingeben, der auf der Website des Casinos verfügbar ist. Der Bonus ohne Einzahlung wird dem Spielerkonto gutgeschrieben, und die Spieler können sofort mit dem Spielen beginnen.
Es gibt jedoch einige Bedingungen, die Spieler erfüllen müssen, um den Bonus ohne Einzahlung zu beanspruchen. Zum Beispiel müssen Spieler den Bonus mehrmals umsetzen, bevor sie Gewinne auszahlen lassen können. Es ist wichtig, die Bedingungen und Konditionen des Bonus ohne Einzahlung sorgfältig zu lesen, um sicherzustellen, dass man alle Anforderungen erfüllt.
Insgesamt ist der Bonus ohne Einzahlung im Zet Casino eine großartige Möglichkeit für neue Spieler, das Casino kennenzulernen und echtes Geld zu gewinnen, ohne eigenes Geld riskieren zu müssen. Wenn Sie auf der Suche nach einem Online-Casino mit attraktiven Bonusangeboten sind, sollten Sie das Zet Casino in Betracht ziehen. Besuchen Sie die Website des Zet Casino, um mehr über den Bonus ohne Einzahlung und andere spannende Angebote zu erfahren. Viel Glück beim Spielen!
https://zetcasino.one/
Wow that was unusual. I just wrote an very long comment but after I clicked submit my comment didn’t appear. Grrrr… well I’m not writing all that over again. Anyhow, just wanted to say wonderful blog!
https://cutt.ly/Wero1Nr6
На сайте https://hyips-money.ru/ ознакомьтесь с любопытными, полезными инвестиционными проектами, которые обязательно принесут неплохой доход. Здесь вы отыщите всю необходимую информацию, которая касается инвестиционных проектов. Перед вами только те проекты, которые действительно платят и предлагают выгодные условия для сотрудничества. Регулярно администраторы сайта мониторят новые проекты, чтобы вы смогли заработать побольше денег и отыскать тот вариант, который действительно работает.
В современном мире, где диплом является началом удачной карьеры в любом направлении, многие ищут максимально простой путь получения качественного образования. Наличие официального документа об образовании сложно переоценить. Ведь именно он открывает двери перед каждым человеком, желающим вступить в профессиональное сообщество или учиться в университете.
Наша компания предлагает оперативно получить этот важный документ. Вы можете купить диплом, что будет отличным решением для всех, кто не смог завершить образование или утратил документ. Все дипломы производятся с особой тщательностью, вниманием к мельчайшим нюансам, чтобы в результате получился полностью оригинальный документ.
Превосходство подобного подхода заключается не только в том, что вы сможете максимально быстро получить свой диплом. Процесс организован комфортно, с профессиональной поддержкой. Начав от выбора требуемого образца документа до консультаций по заполнению персональных данных и доставки по стране — все находится под полным контролем качественных мастеров.
Для всех, кто ищет оперативный способ получить необходимый документ, наша услуга предлагает выгодное решение. Купить диплом – значит избежать длительного процесса обучения и не теряя времени переходить к достижению собственных целей, будь то поступление в ВУЗ или начало трудовой карьеры.
https://www.afchornchurch.com/travel/
construction-rent.com
https://jaycitynews.com
neurontin price south africa: neurontin 400 mg tablets – neurontin tablets 100mg
Ein Casino Bonus ohne Einzahlung ist eine großartige Möglichkeit, um das Spielerlebnis zu verbessern und die Gewinnchancen zu erhöhen. Eines der beliebtesten Online-Casinos, das einen großzügigen Einzahlungsbonus anbietet, ist Tipico Casino.
Tipico Casino ist bekannt für sein umfangreiches Angebot an Spielen, darunter Slots, Tischspiele und Live-Dealer-Spiele. Spieler können sich auf eine sichere und faire Spielumgebung verlassen, da das Casino von der Malta Gaming Authority lizenziert und reguliert wird.
Der Einzahlungsbonus von Tipico Casino ist besonders attraktiv für neue Spieler, die sich anmelden und eine erste Einzahlung tätigen. Der Bonus kann je nach Aktion variieren, aber in der Regel können Spieler mit einem Bonus von bis zu 100% auf ihre Einzahlung rechnen. Das bedeutet, dass Spieler ihr eingezahltes Geld verdoppeln und somit ihre Gewinnchancen maximieren können.
Um den Einzahlungsbonus bei Tipico Casino zu erhalten, müssen Spieler in der Regel einen Aktionscode eingeben oder auf eine bestimmte Schaltfläche klicken, um den Bonus zu aktivieren. Der Bonus wird dann automatisch auf das Spielerkonto gutgeschrieben und kann für das Spielen von Casino-Spielen verwendet werden.
Es ist jedoch wichtig zu beachten, dass Einzahlungsboni bestimmte Bedingungen und Einschränkungen unterliegen können. Zum Beispiel müssen Spieler den Bonus möglicherweise eine bestimmte Anzahl von Malen durchspielen, bevor sie eine Auszahlung beantragen können. Es ist daher ratsam, die Bonusbedingungen sorgfältig zu lesen, um Missverständnisse zu vermeiden.
Insgesamt bietet der Einzahlungsbonus von Tipico Casino den Spielern die Möglichkeit, ihr Guthaben zu erhöhen und mehr Spaß beim Spielen zu haben. Mit einer Vielzahl von spannenden Spielen und lukrativen Boni ist Tipico Casino definitiv einen Besuch wert für alle Casino-Enthusiasten.
https://tipicocasino.one/
Сайт, где можно выбрать тумба напольная под накладную раковину различной формы.
На сайте https://t.me/s/mvavada узнайте всю информацию, последние актуальные новости о популярном онлайн-заведении «VAVADA», где представлено огромное количество слотов, интересных развлечений различного вида. Казино дарит отменное настроение, помогает получить завораживающие эмоции и расслабиться. При этом вы всегда сможете рассчитывать на приятное времяпрепровождение. Именно здесь публикуются промокоды, а также самые интересные предложения. Воспользуйтесь ими для того, чтобы сыграть по-крупному.
В нашем обществе, где диплом становится началом успешной карьеры в любой сфере, многие пытаются найти максимально быстрый и простой путь получения образования. Важность наличия официального документа об образовании трудно переоценить. Ведь диплом открывает двери перед людьми, стремящимися вступить в профессиональное сообщество или учиться в университете.
Предлагаем очень быстро получить этот необходимый документ. Вы имеете возможность заказать диплом нового или старого образца, что будет отличным решением для всех, кто не смог закончить образование, утратил документ или желает исправить свои оценки. Каждый диплом изготавливается аккуратно, с особым вниманием ко всем элементам. На выходе вы сможете получить 100% оригинальный документ.
Преимущество данного решения заключается не только в том, что можно оперативно получить диплом. Весь процесс организован просто и легко, с нашей поддержкой. Начиная от выбора подходящего образца документа до точного заполнения личных данных и доставки в любое место России — все находится под полным контролем качественных специалистов.
Для тех, кто хочет найти максимально быстрый способ получить необходимый документ, наша компания предлагает отличное решение. Приобрести диплом – это значит избежать длительного обучения и сразу переходить к личным целям: к поступлению в университет или к началу удачной карьеры.
http://www.diploman-russia.ru
You’ll Never Guess This Rewrite Ai’s Tricks Rewrite Ai
buy cytotec pills online cheap п»їcytotec pills online Abortion pills online
В наше время, когда диплом становится началом удачной карьеры в любом направлении, многие пытаются найти максимально быстрый и простой путь получения качественного образования. Необходимость наличия официального документа переоценить попросту невозможно. Ведь именно диплом открывает двери перед любым человеком, желающим вступить в сообщество профессионалов или учиться в высшем учебном заведении.
В данном контексте мы предлагаем быстро получить этот важный документ. Вы имеете возможность приобрести диплом старого или нового образца, и это становится удачным решением для всех, кто не смог закончить обучение или утратил документ. Любой диплом изготавливается с особой тщательностью, вниманием к мельчайшим деталям. В результате вы получите полностью оригинальный документ.
Плюсы данного решения состоят не только в том, что можно оперативно получить диплом. Весь процесс организован комфортно и легко, с профессиональной поддержкой. Начиная от выбора необходимого образца до грамотного заполнения личных данных и доставки в любой регион России — все будет находиться под полным контролем наших специалистов.
Всем, кто пытается найти максимально быстрый способ получить необходимый документ, наша компания готова предложить выгодное решение. Купить диплом – это значит избежать длительного обучения и не теряя времени перейти к достижению своих целей, будь то поступление в университет или начало успешной карьеры.
https://jaredbkppo.isblog.net/the-smart-trick-of-marketing-that-no-one-is-discussing-44158076
order cytotec online: buy cytotec in usa – purchase cytotec
Zet Casino ist ein Online-Casino mit einer Vielzahl von Spielen und einer großen Anzahl zufriedener Kunden. Eine Möglichkeit, die Vertrauenswürdigkeit eines Casinos zu überprüfen, ist die Suche nach Bewertungen auf Plattformen wie Trustpilot.
Trustpilot ist eine Website, auf der Verbraucher Bewertungen zu verschiedenen Unternehmen und Dienstleistungen hinterlassen können. Diese Bewertungen werden von echten Kunden verfasst und bieten somit einen authentischen Einblick in die Qualität eines Unternehmens.
Wenn man nach “Zet Casino Trustpilot” sucht, findet man eine Vielzahl von Bewertungen, die das Casino loben. Viele Kunden betonen die Vielfalt und QualitГ¤t der Spiele, den reibungslosen Ablauf von Ein- und Auszahlungen sowie den freundlichen Kundenservice.
Einige Bewertungen weisen auch auf kleine Probleme hin, wie zum Beispiel Verzögerungen bei Auszahlungen, aber insgesamt scheint Zet Casino ein vertrauenswürdiger Anbieter zu sein, der seinen Kunden ein unterhaltsames und sicheres Spielerlebnis bietet.
Es ist immer ratsam, sich vor einer Registrierung in einem Online-Casino über die Erfahrungen anderer Spieler zu informieren. Plattformen wie Trustpilot bieten eine gute Möglichkeit, einen Einblick in die Qualität eines Anbieters zu erhalten und herauszufinden, ob das Casino vertrauenswürdig ist.
Insgesamt scheint Zet Casino auf Trustpilot positive Bewertungen zu erhalten und daher könnte es sich lohnen, diesem Online-Casino eine Chance zu geben und sein Glück zu versuchen.
https://zetcasino.one/
Ищите познавательный сайт о ремонте, садоводстве и строительстве? My-tvset.ru – это то, что вам нужно! Здесь имеются такие рубрики: дача, дом, квартира, мебель, ремонт, лайфхаки. Ищете какой картофель сажать в воронежской области? My-tvset.ru – сайт, где есть удобный поиск, можете прямо сейчас им воспользоваться. У нас вы узнаете, как выбрать лучшую садовую качелю, как создать функциональный туалет на даче, как хранить овощи в квартире, какие существуют типы стяжки пола. Также поведаем вам о том, какой лучше купить для частного дома счетчик воды. Заходите и читайте наши интересные статьи!
На сегодняшний день, когда диплом – это начало отличной карьеры в любом направлении, многие ищут максимально быстрый путь получения образования. Наличие документа об образовании переоценить просто невозможно. Ведь диплом открывает двери перед людьми, желающими вступить в профессиональное сообщество или учиться в университете.
В данном контексте наша компания предлагает максимально быстро получить любой необходимый документ. Вы сможете заказать диплом нового или старого образца, и это будет выгодным решением для всех, кто не смог завершить образование или потерял документ. дипломы изготавливаются с особой аккуратностью, вниманием к мельчайшим элементам. В результате вы получите полностью оригинальный документ.
Плюсы этого решения заключаются не только в том, что вы быстро получите диплом. Процесс организован удобно, с профессиональной поддержкой. Начиная от выбора необходимого образца документа до грамотного заполнения личных данных и доставки по России — все находится под абсолютным контролем наших специалистов.
Всем, кто ищет быстрый способ получения требуемого документа, наша услуга предлагает выгодное решение. Купить диплом – это значит избежать долгого обучения и не теряя времени переходить к своим целям, будь то поступление в университет или старт трудовой карьеры.
https://elm327.ru/fr/opisanie-elm-329/
Индексация ссылок на сайте vindexe
how cЙ‘n i get cheap propecia pills generic propecia online cost propecia without prescription
https://newsprofit.info
emergate.net
Ein Cashback-Bonus ist eine beliebte Belohnung für Spieler in Online-Casinos. Tipico Casino bietet ebenfalls diese Möglichkeit für seine Kunden an. Doch was genau bedeutet Cashback und wie funktioniert es im Tipico Casino?
Beim Cashback erhalten Spieler einen Teil ihrer Verluste zurück, sodass sie einen Teil ihres Einsatzes zurückerhalten können. Dies kann als eine Art Versicherung gegen Verluste angesehen werden und kann besonders für Spieler von Vorteil sein, die gerne höhere Einsätze tätigen.
Im Tipico Casino können Spieler von einem Cashback-Bonus profitieren, der ihnen einen prozentualen Anteil ihrer Verluste zurückgibt. Dabei ist zu beachten, dass verschiedene Spiele unterschiedliche Cashback-Raten haben können. So können zum Beispiel Slots einen höheren prozentualen Cashback als Tischspiele haben.
Um den Cashback-Bonus zu erhalten, müssen Spieler einfach im Tipico Casino spielen und ihre Einsätze platzieren. Im Falle von Verlusten wird der Cashback-Betrag automatisch auf das Spielerkonto gutgeschrieben. Es ist eine einfache und unkomplizierte Möglichkeit, etwas von seinen Verlusten zurückzuerhalten.
Es lohnt sich also, im Tipico Casino nach dem Cashback-Bonus Ausschau zu halten und von dieser attraktiven Belohnung zu profitieren. Mit etwas Glück können Spieler einen Teil ihrer Verluste zurückgewinnen und so länger am Spielspaß teilhaben. Ein toller Anreiz, um im Tipico Casino sein Glück zu versuchen!
https://tipicocasino.one/
На сайте https://t.me/s/tinder_mobile ознакомьтесь с интересной, познавательной информацией, которая касается проекта Tinder. Теперь вы сможете посетить его официальный канал, на котором рассказывается об отношениях, о том, как организовать удачное первое свидание и сделать так, чтобы оно прошло по всем правилам. Вы можете сами делиться своим мнением, оставлять комментарии. На канале имеется и подборка интересных рекомендаций, советов, которые точно вам помогут обрести счастье и завести роман.
Visit the website https://4rabet.app/ and you can download the 4rabet application on Android and iOS for free. 4rabet apk or 4rabet update is easy to download. 4rabet game download install on your device. 4rabet download apk or 4rabet app download we have a new version on our website.
недвижимость на кипре объявления
Immer mehr Menschen nutzen Online-Casinos, um ihr Glück beim Glücksspiel zu versuchen. Dabei ist es jedoch wichtig, ein seriöses und vertrauenswürdiges Casino auszuwählen, um sicherzustellen, dass die persönlichen Daten und das eingezahlte Geld geschützt sind.
Ein Casino, das in den letzten Jahren besonders positiv aufgefallen ist, ist das Boomerang Casino. Auf der Bewertungsplattform Trustpilot hat das Casino eine Vielzahl von positiven Bewertungen erhalten, die seine Seriosität und Zuverlässigkeit unterstreichen.
Die Benutzer loben vor allem die Vielfalt der Spiele, die Benutzerfreundlichkeit der Webseite sowie den kompetenten Kundenservice. Viele Spieler betonen auch die schnellen Auszahlungen und die fairen Gewinnchancen im Boomerang Casino.
Ein großer Pluspunkt ist zudem, dass das Casino über eine gültige Glücksspiellizenz verfügt, die von einer renommierten Regulierungsbehörde ausgestellt wurde. Dadurch können die Spieler sicher sein, dass das Boomerang Casino strengen Auflagen und Regularien unterliegt und somit ein faires Spiel gewährleistet ist.
Insgesamt lässt sich sagen, dass das Boomerang Casino auf Trustpilot einen sehr guten Ruf genießt und sich als vertrauenswürdiger Anbieter im Bereich Online-Glücksspiel etabliert hat. Spieler, die auf der Suche nach einem seriösen Casino sind, sollten sich definitiv das Boomerang Casino genauer anschauen.
https://boomerangcasino.one/
На сайте http://koleso-na-hodu.ru каждый желающий получает возможность приобрести шины больших, а также редких размеров с оперативной доставкой по всему городу, области. Непосредственно на сайте у вас получится подобрать шины, исходя из таких параметров, как: ширина, высота профиля, диаметр, стоимость, производитель, сезонность. Вся продукция сертифицированная, качественная, оригинальная. Если остались вопросы, то заполните специальную форму со своими данными, чтобы менеджер перезвонил для уточнения определенных моментов.
Just wish to say your article is as amazing. The clearness to your post is just nice and i can assume you’re an expert in this subject. Well along with your permission allow me to clutch your feed to keep up to date with drawing close post. Thanks a million and please continue the gratifying work.
diplomans-russiyans.ru
купить недвижимость на кипре недорого
В нашем мире, где диплом – это начало отличной карьеры в любом направлении, многие ищут максимально быстрый и простой путь получения образования. Факт наличия официального документа переоценить просто невозможно. Ведь диплом открывает дверь перед всеми, кто собирается начать профессиональную деятельность или продолжить обучение в ВУЗе.
В данном контексте мы предлагаем оперативно получить этот важный документ. Вы сможете приобрести диплом нового или старого образца, что будет отличным решением для человека, который не смог завершить обучение, утратил документ или хочет исправить плохие оценки. Все дипломы производятся с особой тщательностью, вниманием к мельчайшим нюансам. В результате вы получите полностью оригинальный документ.
Плюсы данного подхода заключаются не только в том, что можно оперативно получить свой диплом. Процесс организовывается комфортно, с профессиональной поддержкой. Начав от выбора нужного образца до консультации по заполнению личной информации и доставки в любое место России — все будет находиться под полным контролем опытных мастеров.
Для всех, кто хочет найти максимально быстрый способ получить необходимый документ, наша услуга предлагает выгодное решение. Приобрести диплом – это значит избежать продолжительного процесса обучения и не теряя времени перейти к важным целям: к поступлению в ВУЗ или к началу удачной карьеры.
https://idiplomany.ru
http://dosaaf-mk.ru/
автошкола вождение по городу
Boomerang Casino – Die neue Attraktion in der Welt der Online Casinos
Das Boomerang Casino ist die neueste Attraktion in der Welt der Online Casinos und verspricht ein aufregendes Spielerlebnis für alle, die gerne ihr Glück versuchen. Mit einer vielfältigen Auswahl an Spielen, großzügigen Boni und einem benutzerfreundlichen Interface ist das Boomerang Casino die perfekte Wahl für alle, die auf der Suche nach Unterhaltung und einem potenziellen Gewinn sind.
Eine der größten Attraktionen des Boomerang Casinos ist die riesige Auswahl an Spielen, die für jeden Geschmack und jede Vorliebe geeignet sind. Von klassischen Tischspielen wie Roulette und Blackjack bis hin zu aufregenden Spielautomaten und Live-Casino-Spielen gibt es für jeden Spieler etwas zu entdecken. Darüber hinaus werden regelmäßig neue Spiele hinzugefügt, um sicherzustellen, dass es immer etwas Neues zu entdecken gibt.
Ein weiterer großer Pluspunkt des Boomerang Casinos sind die großzügigen Boni und Aktionen, die es seinen Spielern bietet. Von Willkommensboni für neue Spieler bis hin zu regelmäßigen Promotionen und Treueprogrammen gibt es viele Möglichkeiten, zusätzliche Belohnungen zu erhalten und das Spielerlebnis noch aufregender zu gestalten.
Das Boomerang Casino ist auch für sein benutzerfreundliches Interface und seinen erstklassigen Kundenservice bekannt. Die Webseite ist einfach zu bedienen und übersichtlich gestaltet, sodass Spieler schnell und einfach ihre Lieblingsspiele finden können. Darüber hinaus steht ein zuverlässiger Kundenservice rund um die Uhr zur Verfügung, um bei Fragen oder Problemen zu helfen.
Insgesamt ist das Boomerang Casino eine groГџartige Wahl fГјr alle, die nach einem unterhaltsamen und lohnenden Spielerlebnis suchen. Mit einer breiten Auswahl an Spielen, groГџzГјgigen Boni und einem erstklassigen Kundenservice ist das Boomerang Casino definitiv einen Besuch wert. Also worauf warten Sie noch? Besuchen Sie das Boomerang Casino noch heute und erleben Sie die aufregende Welt des Online-GlГјcksspiels. Viel GlГјck beim Spielen!
https://boomerangcasino.one/
salaty-na-stol.info
https://newssahara.com
http://cheapestmexico.com/# purple pharmacy mexico price list
Студия звукозаписи в Минске Senjor Minor https://senjorminor.by/ это профессиональная студия звукозаписи, где вы сможете записать песню, написать аранжировку, сделать сведение, мастеринг, озвучку рекламных аудиороликов и получить услуги по продвижению вашего творчества. Зайдите на сайт – узнайте подробную информацию.
Компания See Real предлагает услуги в сфере светодиодных технологий и наружной рекламы. Мы обеспечиваем выгодные цены, и различный бизнес делаем приметным. Рады обговорить с вами в любое время самую смелую идею. Оставьте свои данные, и мы в ближайшее время с вами свяжемся. https://iseer.kz/ – сайт, где у вас есть возможность прямо сейчас ознакомиться с нашими архитектурными решениями и посмотреть виды рекламы компании, также сделать заказ звонка консультанта для расчета. Квалифицированная команда готова к любым творческим вызовам.
В нашем обществе, где диплом – это начало успешной карьеры в любой области, многие стараются найти максимально быстрый и простой путь получения образования. Наличие официального документа сложно переоценить. Ведь диплом открывает дверь перед любым человеком, желающим начать трудовую деятельность или продолжить обучение в университете.
Предлагаем максимально быстро получить этот необходимый документ. Вы сможете приобрести диплом, что является удачным решением для всех, кто не смог завершить образование или утратил документ. дипломы изготавливаются аккуратно, с максимальным вниманием ко всем деталям. В итоге вы сможете получить документ, 100% соответствующий оригиналу.
Преимущество этого решения состоит не только в том, что вы сможете оперативно получить свой диплом. Процесс организован комфортно, с нашей поддержкой. От выбора необходимого образца до консультации по заполнению личных данных и доставки в любой регион страны — все находится под абсолютным контролем опытных мастеров.
Всем, кто ищет оперативный способ получения требуемого документа, наша компания предлагает отличное решение. Купить диплом – значит избежать продолжительного обучения и не теряя времени перейти к достижению собственных целей, будь то поступление в ВУЗ или начало карьеры.
http://ukr.mybb.ru/viewtopic.php?id=391
Metalworking on lathes involves many https://supesolar.com actions when deepening products or cutting out parts is required. Robust cutting tools with low wear and high hardness are required. It is proposed to buy replacement groove plates from well-known manufacturers.
The main advantage of a forklift is its versatility and newssugar.com ease of use. Essentially, it’s just a dolly with a durable fork that can be used to lift pallets or large loads to any height.
Boomerang Casino Test: Ist dieses Online-Casino sein Geld wert?
Das Boomerang Casino ist eine beliebte Online-GlГјcksspielseite, die Spielern eine Vielzahl von Spielen und Promotionen bietet. Doch ist dieses Casino sein Geld wirklich wert? In diesem Test werden wir die wichtigsten Aspekte des Boomerang Casinos genauer unter die Lupe nehmen und herausfinden, ob es sich lohnt, dort zu spielen.
Das erste, was bei der Bewertung eines Online-Casinos berücksichtigt werden muss, ist die Sicherheit und Zuverlässigkeit der Seite. Das Boomerang Casino verfügt über eine gültige Lizenz der Malta Gaming Authority, die als eine der strengsten Glücksspielbehörden der Welt gilt. Dies bedeutet, dass das Casino den internationalen Standards entspricht und Fairness und Transparenz gewährleistet.
Ein weiterer wichtiger Aspekt ist die Spielauswahl. Das Boomerang Casino bietet Hunderte von Spielen von renommierten Anbietern wie NetEnt, Microgaming, Play’n GO und vielen anderen. Von Slots Гјber Tischspiele bis hin zu Live-Casino-Spielen ist fГјr jeden Geschmack etwas dabei. Die Spiele sind auch auf mobilen GerГ¤ten verfГјgbar, sodass Sie jederzeit und Гјberall spielen kГ¶nnen.
Natürlich ist auch der Kundenservice ein wichtiger Faktor bei der Bewertung eines Online-Casinos. Das Boomerang Casino bietet einen rund um die Uhr verfügbaren Live-Chat sowie eine E-Mail-Unterstützung, um sicherzustellen, dass alle Spieler Hilfe erhalten, wenn sie sie benötigen.
Was die Boni und Promotionen betrifft, so bietet das Boomerang Casino großzügige Willkommensboni für neue Spieler sowie regelmäßige Aktionen und Sonderangebote für bestehende Kunden. Diese Boni können Ihren Bankroll erheblich aufstocken und Ihnen mehr Chancen geben, zu gewinnen.
Zusammenfassend lässt sich sagen, dass das Boomerang Casino ein zuverlässiges und unterhaltsames Online-Casino ist, das sein Geld definitiv wert ist. Mit einer breiten Auswahl an Spielen, einer gültigen Lizenz und einem hervorragenden Kundenservice bietet das Casino ein rundum gelungenes Spielerlebnis. Wenn Sie also Lust auf ein spannendes und sicheres Glücksspielabenteuer haben, ist das Boomerang Casino definitiv einen Besuch wert.
https://boomerangcasino.one/
вилла кипр аренда
You become a cosmic architect, wielding the forces of creation to annihilate planets and moons. Select from exceeding 50 weapons,
including lasers, meteors, black holes, and UFOs.
Fraud and customize your own planetary systems in solar smash, from
midget asteroids to brobdingnagian gas giants.
Mould the sphere according to your whims.
На сайте https://rybelsus.com.ru/ вы сможете заказать оперативную доставку такого эффективного препарата, который не имеет побочных эффектов, как «РЕБЕЛСАС». Собственная служба доставки позволит сделать так, чтобы средство было доставлено максимально оперативно. А оплата осуществляется только после получения посылки. У вас получится сделать заказ в режиме реального времени и тогда, когда удобно. Продажа только оригинального, сертифицированного товара. Совершайте выгодные покупки в компании, которая работает для вас!
Магазин, где можно выбрать раковина из фаянса любого размера.
GdeRaznica.ru – сайт, где имеются такие рубрики: общество, технологии, экономика, география, красота, медицина, транспорт. Информацию берем из первоисточников и обращаемся только к профильным экспертам. Ищете главный и ведущий специалист разница? Gderaznica.ru – портал, где есть поиск, воспользуйтесь им уже сейчас. У нас вы узнаете, как различить спам и флуд, чем отличается Росконтроль от Роскачества, какой препарат лучше всего помогает бросить курить, зачем пить коллаген. Также расскажем вам, что такое виниры и сколько будет это стоить.
Metal structures must be produced under strict ochen-vkusno.com quality control. Absolutely all work is checked – from the manufacture of elements to final assembly. It is necessary to check their size, strength, coating and other parameters.
Once a metal structure tatraindia.com is installed, it must be maintained regularly. Thanks to this, it will last much longer.
Wenn Sie gerne Casinospiele online spielen, sollten Sie einen Blick auf den Tipico Casino Bonus Code Gratis werfen. Mit diesem Bonuscode können Sie sich zusätzliche Vorteile sichern und noch mehr Spaß an den Spielen haben.
Der Tipico Casino Bonus Code Gratis ist eine großartige Möglichkeit, um Ihre Gewinne zu steigern und zusätzliche Preise zu gewinnen. Mit diesem Bonuscode erhalten Sie zum Beispiel Freispiele, Bonusguthaben oder andere attraktive Angebote, die Ihnen dabei helfen, noch mehr aus Ihren Einsätzen herauszuholen.
Um den Tipico Casino Bonus Code Gratis zu nutzen, müssen Sie sich einfach auf der Website des Anbieters anmelden und den Code während der Einzahlung eingeben. Sobald Sie dies getan haben, werden Ihnen die zusätzlichen Vorteile automatisch gutgeschrieben und Sie können sofort mit dem Spielen beginnen.
Es ist wichtig zu beachten, dass der Tipico Casino Bonus Code Gratis nur für neue Spieler verfügbar ist und möglicherweise bestimmten Bedingungen unterliegt. Es lohnt sich daher, sich vorab die genauen Anforderungen anzusehen, um sicherzustellen, dass Sie den Bonus optimal nutzen können.
Insgesamt ist der Tipico Casino Bonus Code Gratis eine tolle Möglichkeit, um die Spannung und den Spaß beim Online-Glücksspiel noch weiter zu steigern. Nutzen Sie diese Gelegenheit und sichern Sie sich noch heute Ihren Bonuscode, um von den zusätzlichen Vorteilen zu profitieren. Viel Glück beim Spielen!
https://tipicocasino.one/
На сегодняшний день, когда диплом становится началом отличной карьеры в любой сфере, многие пытаются найти максимально простой путь получения качественного образования. Наличие документа об образовании сложно переоценить. Ведь диплом открывает двери перед всеми, кто собирается начать профессиональную деятельность или учиться в университете.
Предлагаем быстро получить этот необходимый документ. Вы сможете купить диплом, и это является удачным решением для всех, кто не смог закончить обучение или утратил документ. дипломы выпускаются с особой тщательностью, вниманием ко всем нюансам, чтобы в итоге получился документ, максимально соответствующий оригиналу.
Преимущество подобного решения заключается не только в том, что можно оперативно получить свой диплом. Процесс организовывается удобно, с нашей поддержкой. От выбора подходящего образца до консультаций по заполнению персональных данных и доставки в любой регион России — все под абсолютным контролем наших мастеров.
Для тех, кто пытается найти оперативный способ получения требуемого документа, наша компания предлагает выгодное решение. Купить диплом – это значит избежать длительного обучения и сразу перейти к достижению личных целей, будь то поступление в ВУЗ или старт профессиональной карьеры.
http://www.dlplomanrussian.ru
https://www.newton-apartment.ru/
аренда виллы на кипре на берегу моря с бассейном
https://36and6health.com/# legit non prescription pharmacies
домик на кипре купить
Хотите избавиться от морщинок и носогубных складок? Плюреаль вам поможет в этом! Он действует быстро, результат будет радовать вас долгое время. Филлеры линейки Pluryal подвергаются строгому контролю качества продукции. Стоимость приемлемая, после их применения аллергических реакций не бывает. Ваша кожа станет более подтянутой. Ищете сколько стоят филлеры для лица? Pluryal.info – сайт, где можете приобрести средства Плюреаль и подать заявку на сотрудничество. При возникновении каких-либо вопросов, обращайтесь к нам, мы с удовольствием на них ответим.
Zet Casino Test: Ist dieses Online Casino einen Besuch wert?
Online Casinos erfreuen sich heutzutage groГџer Beliebtheit, da sie ein bequemer Weg sind, um sein GlГјck in verschiedenen Spielen zu versuchen. Eines dieser Casinos ist das Zet Casino, das mit seinem breiten Angebot an Spielen und attraktiven Bonusangeboten lockt.
Wir haben das Zet Casino genauer unter die Lupe genommen und einen ausführlichen Test durchgeführt, um herauszufinden, ob sich ein Besuch lohnt. Zunächst einmal fällt positiv auf, dass das Casino eine Lizenz der Malta Gaming Authority besitzt, was für Seriosität und Sicherheit spricht.
Das Spielangebot des Zet Casinos ist beeindruckend und umfasst eine Vielzahl von Slots, Tischspielen und Live Casino Spielen. Hier ist für jeden Geschmack etwas dabei, egal ob man lieber an Spielautomaten dreht oder sich an Blackjack oder Roulette versuchen möchte.
Ein weiterer Pluspunkt des Zet Casinos sind die großzügigen Bonusangebote für Neu- und Bestandskunden. Es gibt nicht nur einen Willkommensbonus für die erste Einzahlung, sondern auch regelmäßige Aktionen und Treueprogramme, die für zusätzliche Gewinnchancen sorgen.
Auch in Sachen Zahlungsmethoden und Kundenservice kann das Zet Casino Гјberzeugen. Es stehen verschiedene sichere Zahlungsoptionen zur VerfГјgung und der Kundensupport ist rund um die Uhr erreichbar und hilfsbereit.
Insgesamt können wir das Zet Casino also empfehlen. Mit seinem abwechslungsreichen Spielangebot, attraktiven Bonusangeboten und zuverlässigem Kundenservice ist es definitiv einen Besuch wert. Also, warum nicht gleich mal vorbeischauen und sein Glück versuchen? Viel Spaß und Erfolg!
https://zetcasino.one/
https://lavrus.org
It is worth noting breakingnews77.com that the loader can be made in the form of a trolley without its own traction, as well as in the form of a powered/gasoline self-propelled device, with which you can transport minimally heavy objects over significant distances within the warehouse. Another advantage is simple maintenance, which ensures the absence of technical bells and whistles, but this depends on the specific model of the device.
Индексация ссылок на сайте в индексе ру
На сайте https://razrabotka.pro/ закажите производство электроники, электронных приборов, а также различных компонентов для электронных устройств. Что касается разработки, то ее стоимость начинается от 100 000 рублей. Все электронные приборы производятся в нужном количестве, а потому получится заказать в требующемся объеме. Воспользуйтесь всем комплексом работ, которые связаны с производством, разработкой электроники. Специально для вас разработка проектов электронных агрегатов. Также возможно производство изделий по готовому проекту.
В нашем обществе, где диплом – это начало удачной карьеры в любой отрасли, многие стараются найти максимально быстрый путь получения качественного образования. Наличие документа об образовании сложно переоценить. Ведь именно диплом открывает дверь перед всеми, кто стремится вступить в сообщество профессионалов или учиться в каком-либо институте.
Наша компания предлагает быстро получить этот необходимый документ. Вы сможете заказать диплом нового или старого образца, что является выгодным решением для человека, который не смог закончить образование, утратил документ или хочет исправить плохие оценки. Любой диплом изготавливается с особой тщательностью, вниманием к мельчайшим элементам, чтобы в итоге получился 100% оригинальный документ.
Преимущество данного решения состоит не только в том, что можно оперативно получить свой диплом. Весь процесс организовывается просто и легко, с профессиональной поддержкой. От выбора подходящего образца документа до грамотного заполнения персональных данных и доставки в любое место России — все под абсолютным контролем опытных специалистов.
Всем, кто ищет оперативный способ получения необходимого документа, наша компания предлагает отличное решение. Купить диплом – это значит избежать долгого обучения и не теряя времени переходить к достижению своих целей, будь то поступление в ВУЗ или старт карьеры.
https://www.vsetutonline.com/forum/member.php?u=76509
На сегодняшний день, когда диплом становится началом удачной карьеры в любом направлении, многие ищут максимально быстрый путь получения образования. Наличие официального документа об образовании переоценить невозможно. Ведь именно диплом открывает двери перед людьми, желающими начать профессиональную деятельность или продолжить обучение в ВУЗе.
Мы предлагаем очень быстро получить любой необходимый документ. Вы сможете заказать диплом нового или старого образца, что будет удачным решением для человека, который не смог закончить обучение, потерял документ или хочет исправить плохие оценки. Все дипломы выпускаются аккуратно, с максимальным вниманием ко всем нюансам, чтобы на выходе получился документ, полностью соответствующий оригиналу.
Преимущества подобного подхода заключаются не только в том, что вы быстро получите диплом. Процесс организован удобно, с нашей поддержкой. От выбора подходящего образца до консультации по заполнению личной информации и доставки по стране — все будет находиться под абсолютным контролем качественных специалистов.
Всем, кто хочет найти быстрый и простой способ получения требуемого документа, наша компания предлагает отличное решение. Купить диплом – это значит избежать длительного процесса обучения и не теряя времени переходить к достижению своих целей, будь то поступление в ВУЗ или старт успешной карьеры.
http://fantasyworldmyforumsorgua.forum.cool/viewtopic.php?id=3426
Tipico: Geld von Sportwetten auf Casino
Sportwetten sind bei vielen Menschen beliebt, da man damit nicht nur seine Lieblingsmannschaften unterstützen, sondern auch Geld gewinnen kann. Doch was passiert, wenn man den Gewinn aus Sportwetten gerne im Online-Casino einsetzen möchte? Kann man sein Geld von Sportwetten einfach auf das Casinokonto übertragen?
Bei Tipico, einem der größten Anbieter für Sportwetten und Online-Casino, ist dies möglich. Man kann sein Guthaben einfach von der Sportsbook-Plattform auf die Casino-Seite übertragen. Dafür muss man lediglich auf der Webseite von Tipico ein Konto eröffnen und sich einloggen. Anschließend kann man unter dem Menüpunkt „Mein Konto“ die Option wählen, sein Guthaben zwischen den verschiedenen Bereichen zu transferieren.
Es gibt allerdings einige wichtige Punkte, die man beachten sollte. Zum einen sollte man darauf achten, dass man die jeweiligen Umsatzbedingungen erfüllt, um das Geld aus den Sportwetten auch im Online-Casino nutzen zu können. Zum anderen sollte man sich darüber im Klaren sein, dass man sein Guthaben eventuell nicht mehr zurück auf die Sportwetten-Seite übertragen kann, sobald man es einmal ins Casino verschoben hat.
Es ist also wichtig, sich vorher gut zu informieren und gegebenenfalls den Kundenservice von Tipico zu kontaktieren, um offene Fragen zu klären. Wenn man diese Punkte beachtet, steht dem Spaß im Online-Casino mit dem Gewinn aus Sportwetten nichts im Wege.
Insgesamt bietet Tipico mit der Möglichkeit, Geld von Sportwetten auf das Online-Casino zu übertragen, eine flexible und bequeme Lösung für alle, die gerne sowohl auf Sport als auch im Casino spielen möchten. Wer also Sportwetten und Glücksspiel liebt, ist bei Tipico genau richtig.
https://tipicocasino.one/
you’re in reality a just right webmaster. The website loading pace is incredible. It sort of feels that you’re doing any unique trick. Also, The contents are masterpiece. you’ve performed a magnificent job on this topic!
https://squareblogs.net/kanyonbeeg/h1-b-kupiti-sklo-far-farfarlight-nadiinist-ta-stil-dlia-vashogo
На сайте https://linkey-light.ru/catalog/promyshlennye_svetilniki/svetodiodnye_svetilniki_dlya_avtoservisa/ представлены светодиодные светильники, предназначенные для автосервиса. Здесь находятся самые интересные, функциональные и совершенные модели. Светильники повышают качество диагностики, ускоряют выполнение различных задач, повышают функциональность, а также безопасность при обслуживании. В магазине представлены светильники самой разной мощности. Но для того, чтобы оборудование работало эффективно, необходимо выполнить профессиональный монтаж.
В современном мире, где диплом становится началом удачной карьеры в любом направлении, многие пытаются найти максимально простой путь получения образования. Наличие официального документа об образовании переоценить просто невозможно. Ведь именно он открывает дверь перед каждым человеком, желающим вступить в сообщество квалифицированных специалистов или учиться в каком-либо ВУЗе.
В данном контексте наша компания предлагает оперативно получить этот важный документ. Вы можете приобрести диплом, что является отличным решением для человека, который не смог закончить обучение или потерял документ. Любой диплом изготавливается аккуратно, с максимальным вниманием ко всем нюансам, чтобы в результате получился документ, максимально соответствующий оригиналу.
Плюсы этого решения заключаются не только в том, что можно оперативно получить свой диплом. Процесс организовывается комфортно, с нашей поддержкой. От выбора нужного образца до грамотного заполнения личной информации и доставки по стране — все под полным контролем качественных специалистов.
Всем, кто пытается найти быстрый способ получить требуемый документ, наша компания предлагает отличное решение. Купить диплом – значит избежать длительного процесса обучения и сразу перейти к своим целям: к поступлению в университет или к началу трудовой карьеры.
https://nada25.mybb.ru/viewtopic.php?id=2198
http://cheapestcanada.com/# cheap canadian pharmacy online
В нашем обществе, где диплом – это начало отличной карьеры в любой сфере, многие стараются найти максимально быстрый путь получения качественного образования. Наличие документа об образовании сложно переоценить. Ведь диплом открывает дверь перед каждым человеком, который стремится вступить в профессиональное сообщество или продолжить обучение в высшем учебном заведении.
Наша компания предлагает очень быстро получить любой необходимый документ. Вы имеете возможность приобрести диплом нового или старого образца, что будет отличным решением для всех, кто не смог завершить образование, потерял документ или хочет исправить плохие оценки. дипломы изготавливаются аккуратно, с особым вниманием к мельчайшим элементам. В итоге вы сможете получить документ, 100% соответствующий оригиналу.
Преимущества такого решения заключаются не только в том, что вы максимально быстро получите свой диплом. Процесс организован просто и легко, с профессиональной поддержкой. Начиная от выбора необходимого образца до правильного заполнения личных данных и доставки по России — все будет находиться под полным контролем качественных мастеров.
Всем, кто ищет быстрый и простой способ получения требуемого документа, наша услуга предлагает выгодное решение. Приобрести диплом – это значит избежать долгого процесса обучения и не теряя времени перейти к достижению личных целей, будь то поступление в университет или начало успешной карьеры.
https://abw-by.ru/usedcars/page/3/
Tipico ist eine der führenden Online-Wettseiten in Deutschland, und sein Casino-Bereich, alles Spitze Tipico Casino, ist beliebt bei Spielern auf der ganzen Welt. Mit einer Vielzahl von Spielen und einer benutzerfreundlichen Oberfläche bietet das alles Spitze Tipico Casino ein erstklassiges Spielerlebnis.
Das Casino bietet eine breite Auswahl an Spielen, darunter klassische Tischspiele wie Blackjack, Roulette und Poker, sowie eine Vielzahl von Spielautomaten und Jackpot-Slots. Die Spiele sind von fГјhrenden Anbietern wie NetEnt, Microgaming und Play’n GO entwickelt worden, was fГјr eine hohe QualitГ¤t und ein spannendes Spielerlebnis sorgt.
Darüber hinaus bietet das alles Spitze Tipico Casino eine Vielzahl von Bonusangeboten und Aktionen für Spieler. Neue Spieler können sich über einen großzügigen Willkommensbonus freuen, während treue Spieler regelmäßig mit Freispielen und anderen Belohnungen belohnt werden.
Die Ein- und Auszahlungen im Casino sind sicher und einfach, und der Kundenservice steht rund um die Uhr zur Verfügung, um bei Fragen oder Problemen zu helfen. Das alles Spitze Tipico Casino ist auch auf mobilen Geräten verfügbar, sodass Spieler ihre Lieblingsspiele jederzeit und überall genießen können.
Insgesamt bietet das alles Spitze Tipico Casino ein erstklassiges Spielerlebnis mit einer Vielzahl von Spielen, groГџzГјgigen Boni und einem exzellenten Kundenservice. Es ist kein Wunder, dass es bei Spielern auf der ganzen Welt so beliebt ist. Probieren Sie es doch selbst aus und erleben Sie die Spannung und Aufregung des alles Spitze Tipico Casinos.
https://tipicocasino.one/
Разработка электроники – компания, которая предоставляет полный комплекс высококачественных услуг. Здесь можете прямо сейчас заказать разработку электроники. Для предварительной консультации, позвоните нам по телефону. Благодаря большому опыту, можем быстро приступить к выполнению проекта. Ищете разработка электроники? Razrabotka.pro – сайт, где вы найдете наши работы. Вы сможете узнать, кому и как, мы помогаем. Также размещаем статьи, которые связаны с изготовлением электроники. Всегда рады обсудить детали вашего проекта, обращайтесь.
Once a metal structure is installed, it must dominicandesign.net be maintained regularly.
Forklifts can be called an indispensable 360o.info element of equipment, which is actively used in the arrangement of warehouse premises.
Willkommen im Zet Casino Deutschland!
Das Zet Casino ist eine beliebte Online-Glücksspielplattform, die Spielern aus Deutschland eine Vielzahl von spannenden Spielen und großzügigen Boni bietet. Das Casino verfügt über eine nahtlose Benutzeroberfläche, die es Spielern ermöglicht, bequem von zu Hause aus auf ihre Lieblingsspiele zuzugreifen.
Egal, ob Sie ein Fan von Spielautomaten, Tischspielen oder Live-Dealer-Spielen sind, im Zet Casino werden Sie sicherlich das finden, wonach Sie suchen. Mit Spielen von fГјhrenden Softwareanbietern wie NetEnt, Microgaming, Play’n GO und vielen anderen kГ¶nnen die Spieler eine erstklassige Spielerfahrung genieГџen.
Darüber hinaus bietet das Zet Casino großzügige Boni und Promotionen, die es den Spielern ermöglichen, ihr Spiel zu maximieren. Von Willkommensboni über tägliche Angebote bis hin zu Treueprämien gibt es immer etwas, das die Spieler belohnt.
Zusätzlich verfügt das Zet Casino über eine sichere und zuverlässige Zahlungsabwicklung, sodass die Spieler ihre Ein- und Auszahlungen schnell und einfach vornehmen können. Mit verschiedenen Zahlungsmethoden wie Kreditkarten, E-Wallets und Banküberweisungen können die Spieler sicher sein, dass ihre finanziellen Transaktionen sicher und geschützt sind.
Alles in allem ist das Zet Casino Deutschland eine exzellente Wahl fГјr alle GlГјcksspiel-Enthusiasten, die nach einer hochwertigen und unterhaltsamen Spielerfahrung suchen. Treten Sie noch heute bei und entdecken Sie die aufregende Welt des Zet Casinos!
https://zetcasino.one/
ремонт планшетов apple
Discover Exclusive Companionship with She-Companion
Welcome to She-Companion, the ultimate destination for discerning individuals seeking the finest in companionship services. At She-Companion, we pride ourselves on offering a curated selection of sophisticated, elegant, and intelligent companions who are perfect for any occasion. Whether you need a companion for travel, social events, or a relaxing evening, She-Companion is here to provide an unparalleled experience tailored to your desires.
Why Choose She-Companion?
– **Exquisite Selection:** Our companions are carefully chosen for their beauty, charm, and intellect. Each companion is committed to providing an engaging and memorable experience.
– **Global Reach:** With a presence in major cities worldwide, She-Companion ensures that you can find the perfect companion wherever you are. Our companions are available for travel, events, and more, making your experience seamless and enjoyable.
– **Professionalism and Discretion:** At She-Companion, we prioritize your privacy and confidentiality. Our professional approach guarantees a discreet and respectful service, allowing you to enjoy your time with complete peace of mind.
– **Personalized Experiences:** We understand that every client is unique. Our companions are skilled at creating personalized experiences that cater to your specific preferences and requirements, ensuring that your time together is truly special.
Explore Our Gallery
Our website features an exclusive gallery where you can view authentic photos and detailed profiles of our companions. This transparency allows you to select a companion who perfectly matches your tastes and expectations.
Seamless Booking Process
Booking a companion with She-Companion is simple and efficient. Our user-friendly platform enables you to browse profiles, select your desired companion, and arrange your meeting with ease. From initial contact to the final farewell, we ensure a smooth and enjoyable experience.
Elevate Your Experience with She-Companion
Whether you’re attending a high-profile event, embarking on an international adventure, or simply seeking delightful company, She-Companion is your trusted partner in creating unforgettable moments. Visit She-Companion today to explore our gallery and find the perfect companion for your needs. Experience the luxury of exceptional companionship with She-Companion – where elegance meets excellence.
Book your ideal companion now and elevate your experience to new heights. Your extraordinary journey begins with She-Companion.
My site: https://she-companion.com/paris-escorts/sonia
Tipico Casino Freispiele: Alles, was Sie Гјber kostenlose Spins wissen mГјssen
Das Tipico Casino bietet seinen Spielern die Möglichkeit, Freispiele zu gewinnen oder zu verdienen. Diese Freispiele ermöglichen es den Spielern, kostenlos an bestimmten Spielautomaten zu spielen, ohne ihr eigenes Geld zu riskieren. In diesem Artikel werden wir genauer auf die Tipico Casino Freispiele eingehen und erklären, wie Sie sie nutzen können.
Freispiele sind eine beliebte Form von Boni in Online-Casinos und bieten den Spielern die Möglichkeit, zusätzliche Gewinne zu erzielen, ohne zusätzliches Geld setzen zu müssen. Im Tipico Casino können Spieler Freispiele auf verschiedene Arten erhalten. Zum einen können sie als Teil eines Willkommensbonusangebots vergeben werden. Wenn sich ein neuer Spieler im Casino registriert und eine erste Einzahlung tätigt, kann er Freispiele als Belohnung erhalten.
Darüber hinaus bietet das Tipico Casino auch regelmäßig Aktionen und Promotionen an, bei denen Freispiele als Preise vergeben werden. Diese können an bestimmten Tagen der Woche oder zu besonderen Anlässen wie Weihnachten oder Ostern angeboten werden. Um von diesen Freispielen zu profitieren, müssen die Spieler die jeweiligen Bedingungen erfüllen, die vom Casino festgelegt werden.
Sobald Sie Freispiele im Tipico Casino erhalten haben, können Sie diese an ausgewählten Spielautomaten nutzen. Die Anzahl der Freispiele und die Höhe des Einsatzes können je nach Aktion und Promotion variieren. Es ist wichtig zu beachten, dass Gewinne, die mit Freispielen erzielt werden, normalerweise bestimmten Umsatzbedingungen unterliegen, bevor sie ausgezahlt werden können.
Insgesamt sind Freispiele eine großartige Möglichkeit, um im Tipico Casino zusätzliche Gewinne zu erzielen und neue Spielautomaten auszuprobieren. Wenn Sie regelmäßig im Casino spielen, sollten Sie immer auf aktuelle Aktionen und Promotionen achten, um von Freispielen zu profitieren. Denken Sie daran, die jeweiligen Bedingungen zu lesen, bevor Sie Ihre Freispiele nutzen, um sicherzustellen, dass Sie das Beste aus Ihrem Spielerlebnis herausholen. Viel Glück und viel Spaß beim Spielen!
https://tipicocasino.one/
If you need to weld elements, you madeintexas.net should trust the work to a welder with the appropriate skills. The quality of welding work must be constantly monitored.
women18.com
https://cheapestcanada.shop/# onlinecanadianpharmacy 24
Современные и стильные стоимость металлического навеса для автомобиля из поликарбоната для вашего участка.
На сайте https://novosti-ru.com/ ознакомьтесь с интересной, познавательной информацией на самую разную тему, в том числе, про еду, автомобили, шоу-бизнес, общество, праздники, медицина, здоровье, техника и наука. Также есть информация и на тему культуры, спорта, отдыха, туризма, интернет-технологий. Все новости актуальные, свежие, а потому данным точно можно доверять. Они составлены экспертами, поэтому содержательные, информативные. Регулярно появляются актуальные новости, которые будет интересно почитать и вам.
Зайдите на сайт https://prazdnik-skazka.com/ и вы сможете заказать выездные праздники для детей в Москве и области. Узнайте стоимость и услуги, которая предлагает компания, такие как: мастер классы, различные праздничные кейсы, авторские вечеринки в различных стилях и многое другое. Огромный опыт и отличная репутация позволят вам заказать праздник для детей от профессионалов!
Zet Casino Promo Code 2023: Alles, was Sie wissen mГјssen
Wenn Sie ein begeisterter Online-Casino-Spieler sind, sollten Sie unbedingt den Zet Casino Promo-Code 2023 im Auge behalten. Diese Werbeaktion bietet Ihnen die Möglichkeit, großartige Boni und Vergünstigungen zu erhalten, während Sie Ihre Lieblingsspiele genießen. In diesem Artikel erfahren Sie alles, was Sie über den Zet Casino Promo-Code 2023 wissen müssen.
Was ist der Zet Casino Promo-Code 2023?
Der Zet Casino Promo-Code 2023 ist ein spezieller Code, den Sie eingeben können, um Zugang zu exklusiven Boni und Angeboten zu erhalten. Diese Werbeaktion wird von Zet Casino angeboten, einem beliebten Online-Casino mit einer großen Auswahl an Spielen und Funktionen.
Wie verwende ich den Zet Casino Promo-Code 2023?
Um den Zet Casino Promo-Code 2023 zu verwenden, müssen Sie zunächst ein Konto bei Zet Casino erstellen. Sobald Sie angemeldet sind, können Sie den Promo-Code während des Einzahlungsvorgangs eingeben. Auf diese Weise erhalten Sie Zugang zu den speziellen Angeboten, die mit dem Code verbunden sind.
Welche Boni und VergГјnstigungen kann ich mit dem Zet Casino Promo-Code 2023 erhalten?
Mit dem Zet Casino Promo-Code 2023 haben Sie die Möglichkeit, verschiedene Arten von Boni und Vergünstigungen zu erhalten. Dazu gehören unter anderem Einzahlungsboni, Freispiele, Cashback-Angebote und vieles mehr. Diese Angebote können je nach aktueller Werbeaktion variieren, daher sollten Sie regelmäßig nach Updates suchen.
Wo finde ich den Zet Casino Promo-Code 2023?
Der Zet Casino Promo-Code 2023 kann auf der offiziellen Website von Zet Casino oder in Werbe-E-Mails und auf Social-Media-Plattformen gefunden werden. Es lohnt sich auch, regelmäßig die Aktionsseite des Casinos zu überprüfen, um sicherzustellen, dass Sie keine neuen Angebote verpassen.
Fazit
Der Zet Casino Promo-Code 2023 bietet Ihnen die Möglichkeit, Ihren Online-Casino-Spaß auf die nächste Stufe zu heben. Mit exklusiven Boni und Vergünstigungen können Sie noch mehr aus Ihren Lieblingsspielen herausholen. Vergessen Sie also nicht, den Zet Casino Promo-Code 2023 zu nutzen, wenn Sie das nächste Mal eine Einzahlung tätigen. Viel Glück und viel Spaß beim Spielen!
https://zetcasino.one/
У нас вы найдете купить автомобильный навес на любой вкус и бюджет.
Das Boomerang Casino ist eine aufstrebende Online-GlГјcksspielseite, die mit ihren groГџzГјgigen Bonusangeboten und einer Vielzahl von Spielen die Aufmerksamkeit vieler Spieler auf sich zieht. Einer der beliebtesten Promotionscodes, den Spieler nutzen kГ¶nnen, ist der “kod promocyjny”, der ihnen zusГ¤tzliche Boni und Vorteile bietet.
Mit dem Boomerang Casino kod promocyjny können Spieler ihr Spielvergnügen noch weiter steigern, indem sie beispielsweise Bonusguthaben oder Freispiele erhalten. Diese zusätzlichen Boni können dazu beitragen, die Gewinnchancen zu erhöhen und das Spielerlebnis insgesamt noch spannender zu gestalten.
Um den Kod promocyjny nutzen zu können, müssen Spieler lediglich während der Registrierung oder Einzahlung den entsprechenden Code eingeben. Sobald der Code bestätigt wurde, werden die zusätzlichen Boni automatisch dem Spielerkonto gutgeschrieben.
Das Boomerang Casino bietet eine breite Auswahl an Spielen, darunter Spielautomaten, Tischspiele, Live-Casinospiele und vieles mehr. Mit dem kod promocyjny haben Spieler die Möglichkeit, verschiedene Spiele auszuprobieren und ihre Gewinnchancen zu maximieren.
Insgesamt ist das Boomerang Casino eine attraktive Option für Spieler, die nach einem unterhaltsamen und lukrativen Online-Glücksspiel-Erlebnis suchen. Mit dem kod promocyjny können sie von zusätzlichen Boni und Vorteilen profitieren und ihr Spielerlebnis auf die nächste Stufe heben.
https://boomerangcasino.one/
Наши купить навес маркизу создадут уют и комфорт на вашем участке.
Зайдите на сайт https://baracatmar.com/ и вы сможете заказать свежие морепродукты от Компании Баракат SEAFOOD в страны Евросоюза. Благодаря налаженной системе логистики, с момента вылова и до получения продуктов клиентами нашей компании проходит очень мало времени. Посетите сайт, ознакомьтесь с ассортиментом, условиями доставки и действующими акциями.
http://cheapestandfast.com/# non prescription canadian pharmacy
Компания «Разработка электроники» предлагает клиентам полный комплекс профессиональных услуг. У нас можно сделать заказ на разработку электроники. Получите по телефону предварительную консультацию. Достаточный накопленный опыт дает возможность нам быстро включиться в проект. https://razrabotka.pro/ – сайт, где представлены выполненные работы. Вы узнаете, кому и как мы помогаем. Также размещаем статьи, которые имеют отношение к изготовлению электроники и разработке. Звоните нам, обсудим все детали вашего проекта с удовольствием.
Considering how busy arizonawood.net most people are, cleaning services have become very popular.
With their help, you can load pallets news24time.net, boxes and large cargo onto the upper shelves of the racks, which increases the functional area of the warehouse by an order of magnitude.
dapoxetine tip – viagra plus moment cialis with dapoxetine confusion
Zet Casino – Das ultimative Online-GlГјcksspielerlebnis
Zet Casino ist ein aufregendes Online-Casino, das Spielern eine Vielzahl von Spielmöglichkeiten bietet. Mit einer großen Auswahl an Spielen, großzügigen Boni und einer benutzerfreundlichen Website ist Zet Casino definitiv eine der besten Optionen für Glücksspiel-Enthusiasten.
Einer der Hauptvorteile von Zet Casino ist die beeindruckende Auswahl an Spielen. Mit Гјber 2000 Spielen von erstklassigen Anbietern wie NetEnt, Microgaming, Play’n GO und vielen anderen, gibt es fГјr jeden Spieler etwas zu entdecken. Von traditionellen Spielautomaten und Tischspielen bis hin zu Live-Casino-Spielen bietet Zet Casino eine Vielzahl von Optionen, die sicherlich jeden Spieler begeistern werden.
Darüber hinaus bietet Zet Casino großzügige Boni und Promotionen, die es Spielern ermöglichen, ihr Spielerlebnis zu maximieren. Neue Spieler werden mit einem Willkommensbonus begrüßt, der zusätzliches Geld und Freispiele für ausgewählte Spiele bietet. Darüber hinaus gibt es regelmäßige Aktionen, wie Einzahlungsboni, Cashback-Angebote und Turniere, die den Spielern zusätzliche Gewinnchancen bieten.
Die Website von Zet Casino ist benutzerfreundlich und übersichtlich gestaltet, was es den Spielern leicht macht, ihre Lieblingsspiele zu finden und zu spielen. Mit einer responsiven Benutzeroberfläche, die auf allen Geräten reibungslos funktioniert, können Spieler ihre Lieblingsspiele jederzeit und überall genießen.
Insgesamt ist Zet Casino eine ausgezeichnete Wahl fГјr alle, die ein unterhaltsames und spannendes Online-GlГјcksspielerlebnis suchen. Mit einer beeindruckenden Auswahl an Spielen, groГџzГјgigen Boni und einer benutzerfreundlichen Website bietet Zet Casino alles, was man sich von einem erstklassigen Online-Casino wГјnschen kann. Probieren Sie es noch heute aus und erleben Sie den Nervenkitzel des GlГјcksspiels bei Zet Casino!
https://zetcasino.one/
Защитите свой транспорт с помощью проект навеса для автомобиля!
Желаете приобрести товары для туризма? TrampClub предоставляет такую возможность! Здесь вы найдете: спальники, походную посуду, палатки, рюкзаки, коврики и другое. Гарантируем быструю доставку, доступные цены и отменное обслуживание. Ищете палатки трамп официальный сайт? Trampclub.ru – сайт, где у вас есть возможность посмотреть отзывы о магазине и условия оплаты. Предлагаем вам только качественную продукцию. У нас действуют скидки. Наша работа направлена на удовлетворение желаний и потребностей покупателей. Обращайтесь, мы всегда на связи.
На сайте https://razrabotka.pro/ вы сможете заказать такую важную и полезную услугу, как разработка электроники. Кроме того, здесь можно заказать и создание электронных приборов, специализированного оборудования. Что касается стоимости, то она начинается от 100 000 рублей. Есть возможность заказать производство независимо от количества. Практикуется производство, разработка электроники, производство агрегатов по созданному проекту. Вся продукция производится с использованием инновационных технологий.
Удобство и функциональность – вот что предлагают наши навес для бассейна купить в москве.
Zet Casino Auszahlung Erfahrung
Das Zet Casino ist eine Online-GlГјcksspielplattform, die eine Vielzahl von Casinospielen und Boni fГјr seine Spieler anbietet. Eine wichtige Komponente eines guten Online-Casinos ist jedoch auch die Auszahlungserfahrung der Spieler. In diesem Artikel werden wir daher die Zet Casino Auszahlungserfahrung genauer unter die Lupe nehmen.
Zunächst einmal ist es wichtig zu erwähnen, dass das Zet Casino eine Vielzahl von Auszahlungsmethoden für seine Spieler anbietet. Dazu gehören Zahlungsoptionen wie Kreditkarten, Banküberweisungen, E-Wallets und mehr. Dies bedeutet, dass die Spieler eine breite Auswahl an Möglichkeiten haben, um ihr Geld abzuheben.
Ein weiterer positiver Aspekt der Zet Casino Auszahlungserfahrung ist die Schnelligkeit der Transaktionen. Die meisten Auszahlungen werden innerhalb von 24 Stunden bearbeitet, was im Vergleich zu anderen Online-Casinos als ziemlich schnell gilt. Dies bedeutet, dass die Spieler nicht lange auf ihr Geld warten mГјssen und ihre Gewinne schnell ausgezahlt werden.
Darüber hinaus bietet das Zet Casino auch einen zuverlässigen Kundenservice, der bei Fragen oder Problemen im Zusammenhang mit Auszahlungen zur Verfügung steht. Dies sorgt für eine angenehme Spielerfahrung und gibt den Spielern das Vertrauen, dass ihre finanziellen Angelegenheiten in guten Händen sind.
Alles in allem kann man sagen, dass die Zet Casino Auszahlungserfahrung positiv ist. Mit einer Vielzahl von Auszahlungsmethoden, schnellen Transaktionen und einem guten Kundenservice können die Spieler sicher sein, dass ihre Gewinne schnell und sicher auf ihr Konto überwiesen werden. Wer also auf der Suche nach einem zuverlässigen Online-Casino mit einer guten Auszahlungserfahrung ist, sollte definitiv das Zet Casino in Betracht ziehen.
https://zetcasino.one/
cenforce online toward – brand viagra online fireplace
cenforce tread – brand viagra online wed
Das Zet Casino Forum: Alles, was du wissen musst
Das Zet Casino bietet seinen Spielern nicht nur eine Vielzahl von spannenden Spielen, sondern auch die Möglichkeit, sich mit anderen Spielern auszutauschen und zu vernetzen. Dafür gibt es das Zet Casino Forum, in dem Spieler ihre Erfahrungen teilen, Tipps und Tricks austauschen und sich über aktuelle Aktionen und Angebote informieren können.
Im Zet Casino Forum findest du verschiedene Bereiche, die auf unterschiedliche Themen rund um das Casino-Spiel spezialisiert sind. So gibt es beispielsweise Abschnitte für Strategien und Taktiken, wo Spieler ihre besten Tipps für bestimmte Spiele wie Roulette, Blackjack oder Spielautomaten teilen können. Auch gibt es einen Bereich für Neuigkeiten und Ankündigungen, in dem das Casino über aktuelle Aktionen informiert.
Ein weiterer wichtiger Bereich im Zet Casino Forum ist der Support-Bereich. Hier können Spieler Fragen stellen oder Probleme melden und erhalten schnell und unkompliziert Hilfe von anderen Spielern oder den Mitarbeitern des Casinos. So wird eine positive und unterstützende Community geschaffen, die es den Spielern ermöglicht, ihr Spielerlebnis zu maximieren.
Das Zet Casino Forum ist nicht nur eine Plattform zum Austausch, sondern auch eine Möglichkeit, Belohnungen zu erhalten. Durch aktive Teilnahme am Forum und das Teilen von hilfreichen Beiträgen können Spieler Punkte sammeln und diese gegen attraktive Preise eintauschen.
Insgesamt bietet das Zet Casino Forum eine tolle Möglichkeit, sich mit anderen Spielern zu vernetzen, sein Wissen zu erweitern und von den Erfahrungen anderer zu profitieren. Wer also gerne in einer Community von Gleichgesinnten aktiv ist und sein Casino-Erlebnis noch spannender gestalten möchte, sollte unbedingt einen Blick ins Zet Casino Forum werfen.
https://zetcasino.one/
Индексация ссылок на сайте vindexe.ru
В нашем обществе, где диплом является началом удачной карьеры в любой сфере, многие пытаются найти максимально быстрый и простой путь получения образования. Необходимость наличия официального документа сложно переоценить. Ведь именно диплом открывает дверь перед каждым человеком, желающим начать трудовую деятельность или продолжить обучение в высшем учебном заведении.
В данном контексте наша компания предлагает быстро получить любой необходимый документ. Вы сможете купить диплом, и это будет выгодным решением для всех, кто не смог завершить образование или потерял документ. Все дипломы изготавливаются аккуратно, с особым вниманием к мельчайшим деталям. На выходе вы получите документ, максимально соответствующий оригиналу.
Преимущество этого подхода состоит не только в том, что вы максимально быстро получите диплом. Процесс организован удобно, с профессиональной поддержкой. Начиная от выбора требуемого образца до грамотного заполнения персональной информации и доставки в любое место страны — все находится под абсолютным контролем квалифицированных мастеров.
Таким образом, для всех, кто пытается найти максимально быстрый способ получить необходимый документ, наша услуга предлагает выгодное решение. Приобрести диплом – значит избежать продолжительного обучения и не теряя времени перейти к своим целям, будь то поступление в университет или начало карьеры.
opekaspb.ru/za-zreniem-nuzhen-uxod/В
portal.lfciasocal.com/news/congratulations-to-our-liverpool-way-players-of-the-month-for-october/В
dataload.com/forum/memberlist.php?mode=joined&order=ASC&start=16950В
http://www.saluttunisia.com/jomsocial/groups/viewbulletins.html?groupid=101&start=180В
allmedbook.ru/load/fiziologija/anatomija_cheloveka/34-1-0-488В
Zet Casino No Deposit
Zet Casino ist ein beliebtes Online-Casino, das eine Vielzahl von Spielen fГјr die Spieler anbietet. Egal, ob Sie ein Fan von Slots, Tischspielen oder Live-Casino sind, bei Zet Casino werden Sie definitiv das richtige Spiel fГјr sich finden. Neben der groГџen Auswahl an Spielen bietet Zet Casino auch groГџzГјgige Bonusangebote fГјr seine Spieler. Einer der beliebtesten Bonusse, die das Casino bietet, ist der sogenannte “No Deposit Bonus”.
Der No Deposit Bonus von Zet Casino ist ein großartiges Angebot für neue Spieler, die das Casino ausprobieren möchten, ohne eine Einzahlung tätigen zu müssen. Mit diesem Bonus erhalten Spieler eine bestimmte Menge an Freispielen oder Bonusgeld, die sie nutzen können, um verschiedene Spiele im Casino zu spielen. Dadurch haben die Spieler die Möglichkeit, das Casino und seine verschiedenen Spiele kennenzulernen, ohne ihr eigenes Geld riskieren zu müssen.
Um den No Deposit Bonus von Zet Casino zu erhalten, müssen Spieler sich lediglich auf der Website des Casinos registrieren und ein Konto erstellen. Sobald das Konto erstellt wurde, erhalten die Spieler den Bonus automatisch gutgeschrieben. Es ist jedoch wichtig zu beachten, dass bestimmte Bedingungen und Anforderungen für den No Deposit Bonus gelten, die von Zet Casino festgelegt wurden. Spieler müssen diese Bedingungen erfüllen, um den Bonus nutzen zu können und mögliche Gewinne auszahlen zu können.
Insgesamt ist der No Deposit Bonus von Zet Casino eine groГџartige Gelegenheit fГјr Spieler, das Casino auszuprobieren und erste Gewinne zu erzielen, ohne eigenes Geld einzahlen zu mГјssen. Wenn Sie also auf der Suche nach einem unterhaltsamen und lohnenden Online-Casino-Erlebnis sind, sollten Sie Zet Casino definitiv eine Chance geben.
https://zetcasino.one/
Цветочная мастерская «Роза Ветров» предлагает вам купить роскошные цветы. Выбор большой, у нас вы найдете все то, что вам необходимо. Мы радуем своих клиентов доступными ценами и качественно собранными букетами. Быстро реагируем на заявки и с удовольствием готовы помочь вам с выбором. Заинтересованы в предоставлении вам лучших впечатлений. Ищете купить орхидеи? Flowersspb.com – сайт, где можете заказать свежие цветы с оперативной доставкой. Уверены в том, что получатели будут в восторге от сюрприза. Обращайтесь, гарантируем отличное обслуживание!
dapoxetine prospect – udenafil flesh cialis with dapoxetine perceive
angliannews.com
Considering how busy most people are birminghamnews24.com, cleaning services have become very popular. There are several types of cleaning: daily, apartment cleaning after renovation, cleaning by zone and others.
Индексация ссылок на сайте индекс ру
На сайте https://t.me/mvavada ознакомьтесь с нужной, полезной информацией, которая касается уникального проекта «VAVADA». На официальном канале вы сможете ознакомиться со всей необходимой информацией. Здесь же представлены и актуальные промокоды, а также самые свежие и полезные новости, которые будут интересны всем, кто связан с игрой. Вавада предлагает ознакомиться с интересными, увлекательными играми, которые произведут на вас эффект. На этом канале, в первую очередь, появляются новости о таком заведении.
Хотите выглядеть свежо и молодо? Тогда процедура Premium Face – то, что вам нужно! Она поможет избавиться от носогубных складок, морщин и сделать кожу более подтянутой. Результат от инъекций филлеров Pluryal заметен сразу после сеанса, а эффект сохраняется на длительное время. Ищете процесс постановки филлеров: шаг за шагом инструкция? Premiumface.ru – сайт, где у вас есть возможность узнать подробнее о процедуре Premium Face. Также вы в любое время сможете подать на сотрудничество заявку. Наслаждайтесь своим отражением в зеркале и радуйте внешним видом окружающих!
На сайте https://agrotechelit.ru/ закажите звонок для того, чтобы проконсультироваться по поводу покупки оборудования для теплиц, а также парников с оперативной доставкой по России. Предприятие специализируется на производстве, реализации тепличного оборудования, а также различных необходимых комплектующих. В компании получится заказать огромный ассортимент продукции, в том числе, системы отопления, полива, огромный выбор пленок, укрытий. Здесь же вы найдете и расходные материалы, необходимые для сервиса теплиц.
http://36and6health.com/# best canadian pharmacy no prescription
thecolumbianews.net
texas-news.com
Wenn Sie in einem Online-Casino spielen, haben Sie möglicherweise schon einmal von Casino-Chips gehört. Diese Chips sind eine virtuelle Währung, die Spieler nutzen können, um Einsätze zu platzieren und Gewinne zu erzielen. Aber wussten Sie, dass Sie diese Chips auch auszahlen lassen können?
Tipico ist ein beliebtes Online-Casino, das seinen Spielern die Möglichkeit bietet, ihre Casino-Chips auszahlen zu lassen. Dies kann in der Regel auf verschiedene Arten erfolgen, je nach den Bedingungen und Richtlinien des Casinos. In den meisten Fällen können Spieler ihre Chips in Bargeld umwandeln, das entweder auf ihr Bankkonto überwiesen oder auf ihre Kreditkarte eingezahlt wird.
Um Ihre Casino-Chips bei Tipico auszahlen zu lassen, müssen Sie normalerweise eine Mindestauszahlungsgrenze erreichen. Diese Grenze variiert je nach Casino, kann aber oft bei 20 € oder höher liegen. Darüber hinaus können Gebühren anfallen, wenn Sie Ihre Chips auszahlen lassen. Dies ist jedoch normalerweise der Fall, wenn Sie Ihre Gewinne auf eine bestimmte Weise auszahlen lassen, z.B. per Banküberweisung.
Es ist wichtig zu beachten, dass das Auszahlen von Casino-Chips bei Tipico bestimmte Bedingungen und Einschränkungen unterliegt. Daher ist es ratsam, die Auszahlungsrichtlinien des Casinos sorgfältig zu überprüfen, um sicherzustellen, dass Sie Ihr Geld problemlos und ohne Probleme erhalten können.
Insgesamt bieten Casino-Chips eine praktische Möglichkeit, Gewinne aus Online-Casinospielen auszuzahlen. Wenn Sie also bei Tipico spielen und eine nette Summe gewonnen haben, können Sie Ihre Chips einfach und schnell in echtes Geld umwandeln. Viel Glück beim Spielen und viel Spaß beim Auszahlen Ihrer Gewinne!
https://tipicocasino.one/
Индексация ссылок на сайте vindexe
Канал проекта casino VAVADA рад видеть вас у себя! Здесь вы найдете самую актуальную информацию. Проведите прекрасно время и забудьте обо всем, играя от качественного онлайн-казино Вавада в увлекательные слоты. Вас ожидает особенная атмосфера и потрясающая графика. Ищете vavada войти? t.me/mvavada – популярный телеграмм-канал, где мы делимся секретами успеха и своими знаниями с вами. У нас вы найдете щедрые бонусы, не откладывайте на завтра, начните азартную игру прямо сегодня. Желаем вам успеха!
В современном мире, где диплом – это начало удачной карьеры в любом направлении, многие ищут максимально быстрый путь получения образования. Наличие официального документа об образовании переоценить невозможно. Ведь именно он открывает дверь перед каждым человеком, желающим начать трудовую деятельность или учиться в университете.
В данном контексте мы предлагаем максимально быстро получить этот важный документ. Вы сможете купить диплом старого или нового образца, что становится отличным решением для человека, который не смог завершить обучение, потерял документ или хочет исправить плохие оценки. Все дипломы производятся аккуратно, с особым вниманием ко всем деталям. В итоге вы сможете получить документ, полностью соответствующий оригиналу.
Плюсы этого решения состоят не только в том, что вы сможете максимально быстро получить диплом. Процесс организовывается удобно, с нашей поддержкой. От выбора подходящего образца документа до точного заполнения персональной информации и доставки в любой регион России — все под полным контролем квалифицированных мастеров.
Всем, кто ищет максимально быстрый способ получения требуемого документа, наша услуга предлагает отличное решение. Купить диплом – значит избежать длительного процесса обучения и сразу переходить к личным целям, будь то поступление в ВУЗ или начало удачной карьеры.
http://www.thyweb.dk/find-det-perfekte-tilbehoer-koeb-viskestykker-til-dit-koekken/В
artshi.ru/user/arkadypettr/В
girbir.com/blogs/13245/We-purchase-a-university-diploma-on-the-Internet-Expert-adviceВ
webhistoryrussia.ru/istoriya-rossii/2-yazycheskaya-rusВ
textualheritage.org/lt/el-manusctipt-2014/88.htmlВ
Boomerang Casino Erfahrung
Boomerang Casino ist ein Online-Casino, das erst kГјrzlich auf den Markt gekommen ist. Es bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele und Live-Casino-Spiele. Doch wie gut ist dieses Casino wirklich? In diesem Artikel werfen wir einen genaueren Blick auf die Erfahrung, die Spieler mit Boomerang Casino gemacht haben.
In den Rezensionen von Spielern wird oft die groГџe Auswahl an Spielen gelobt, die Boomerang Casino bietet. Von klassischen Slots bis hin zu aufregenden Live-Casino-Spielen ist fГјr jeden Geschmack etwas dabei. Die Spiele werden von renommierten Anbietern wie NetEnt, Microgaming und Evolution Gaming bereitgestellt, was fГјr eine qualitativ hochwertige Spielerfahrung sorgt.
Ein weiterer Pluspunkt ist der Kundenservice von Boomerang Casino. Die Mitarbeiter sind rund um die Uhr per Live-Chat und E-Mail erreichbar und stehen den Spielern bei Fragen und Problemen zur Seite. Die meisten Spieler berichten, dass ihre Anliegen schnell und professionell gelöst wurden.
Einige Spieler haben jedoch auch negative Erfahrungen mit Boomerang Casino gemacht. Einige berichten von langen Auszahlungszeiten und Problemen mit Bonusangeboten. Es scheint, dass das Casino hier noch Verbesserungspotenzial hat.
Alles in allem bietet Boomerang Casino eine solide Spielerfahrung mit einer großen Auswahl an Spielen und gutem Kundenservice. Wie bei jedem Online-Casino gibt es jedoch auch hier einige Schwachpunkte, die beachtet werden sollten. Wenn Sie auf der Suche nach einem neuen Online-Casino sind, könnte Boomerang Casino einen Blick wert sein.
https://boomerangcasino.one/
http://cheapestmexico.com/# best online pharmacies in mexico
Посетите https://intercalendar.ru и вы сможете заказать печать и изготовление календарей в типографии по отличным ценам. Ознакомьтесь с каталогом услуг, стоимостью изготовления продукции, а заказ можно сделать буквально в 1 клик. Качественные услуги по привлекательным ценам от профессионалов у нас на сайте.
Boomerang-Casino: Ein aufregendes neues Online-Casino-Erlebnis
Das Boomerang-Casino ist eines der neuesten Online-Casinos, das die iGaming-Szene erobert. Mit einer Vielzahl von aufregenden Spielen, lukrativen Boni und einer benutzerfreundlichen Plattform hat es bereits die Aufmerksamkeit von Spielern auf der ganzen Welt auf sich gezogen.
Das erste, was die Spieler beim Betreten des Boomerang-Casinos bemerken, ist die moderne und ansprechende Benutzeroberfläche. Mit klaren Grafiken und intuitiver Navigation ist es einfach, sich auf der Website zurechtzufinden und die gewünschten Spiele zu finden.
Das Casino bietet eine breite Palette von Spielen, darunter klassische Tischspiele wie Blackjack, Roulette und Baccarat, sowie eine Vielzahl von Spielautomaten und Video-Poker-Spielen. Die Spiele werden von einigen der fГјhrenden Softwareanbieter der Branche bereitgestellt, darunter NetEnt, Microgaming und Play’n GO, was fГјr QualitГ¤t und Vielfalt bГјrgt.
Ein weiterer großer Anreiz, im Boomerang-Casino zu spielen, sind die großzügigen Boni und Promotionen, die regelmäßig angeboten werden. Neue Spieler können von einem Willkommensbonus profitieren, der kostenlose Spielgelder oder Freispiele beinhaltet. Darüber hinaus werden loyalen Spielern verschiedene Treuebelohnungen und Boni angeboten, um sie bei Laune zu halten.
Das Casino bietet auch eine Vielzahl von sicheren und bequemen Ein- und Auszahlungsmethoden, so dass die Spieler sicher sein können, dass ihre finanziellen Transaktionen geschützt sind. Der Kundenservice steht rund um die Uhr zur Verfügung, um bei Fragen oder Problemen zu helfen, und das Casino ist lizenziert und reguliert, um ein faires und sicheres Spielerlebnis zu gewährleisten.
Insgesamt bietet das Boomerang-Casino ein aufregendes und lohnendes Spielerlebnis fГјr alle, die auf der Suche nach einem neuen Online-Casino sind. Mit seiner groГџen Auswahl an Spielen, groГџzГјgigen Boni und erstklassigem Kundenservice ist es definitiv einen Besuch wert.
https://boomerangcasino.one/
Замена венцов красноярск
Геракл24: Квалифицированная Смена Основания, Венцов, Полов и Перенос Строений
Организация Gerakl24 специализируется на выполнении комплексных услуг по замене фундамента, венцов, настилов и перемещению домов в городе Красноярске и за пределами города. Наш коллектив квалифицированных специалистов обеспечивает превосходное качество реализации различных типов реставрационных работ, будь то из дерева, каркасные, из кирпича или бетонные дома.
Преимущества услуг Gerakl24
Профессионализм и опыт:
Каждая задача проводятся только профессиональными экспертами, имеющими большой опыт в направлении строительства и реставрации домов. Наши мастера эксперты в своей области и реализуют проекты с высочайшей точностью и вниманием к деталям.
Всесторонний подход:
Мы предлагаем разнообразные услуги по восстановлению и реконструкции строений:
Замена фундамента: укрепление и замена старого фундамента, что обеспечивает долгий срок службы вашего здания и избежать проблем, связанные с оседанием и деформацией строения.
Замена венцов: восстановление нижних венцов деревянных зданий, которые чаще всего подвергаются гниению и разрушению.
Замена полов: монтаж новых настилов, что существенно улучшает внешний облик и функциональные характеристики.
Передвижение домов: безопасное и надежное перемещение зданий на новые локации, что обеспечивает сохранение строения и избегает дополнительных затрат на возведение нового.
Работа с любыми видами зданий:
Деревянные дома: восстановление и укрепление деревянных конструкций, защита от гниения и вредителей.
Дома с каркасом: реставрация каркасов и замена поврежденных элементов.
Кирпичные дома: реставрация кирпичной кладки и укрепление конструкций.
Бетонные дома: восстановление и укрепление бетонных структур, устранение трещин и повреждений.
Качество и прочность:
Мы работаем с лишь качественные материалы и современное оборудование, что гарантирует долгий срок службы и надежность всех работ. Каждый наш проект проходят тщательную проверку качества на каждой стадии реализации.
Личный подход:
Каждому клиенту мы предлагаем подходящие решения, с учетом всех особенностей и пожеланий. Мы стремимся к тому, чтобы итог нашей работы полностью удовлетворял ваши ожидания и требования.
Почему выбирают Геракл24?
Обратившись к нам, вы найдете надежного партнера, который возьмет на себя все хлопоты по ремонту и реконструкции вашего строения. Мы обеспечиваем выполнение всех задач в установленные сроки и с в соответствии с нормами и стандартами. Связавшись с Геракл24, вы можете быть спокойны, что ваше здание в надежных руках.
Мы готовы предоставить консультацию и дать ответы на все вопросы. Звоните нам, чтобы обсудить ваш проект и получить больше информации о наших услугах. Мы поможем вам сохранить и улучшить ваш дом, сделав его безопасным и комфортным для проживания на долгие годы.
Gerakl24 – ваш выбор для реставрации и ремонта домов в Красноярске и области.
This offer is accompanied by photographs of hotels greenhousebali.com where tourists can be found. There is the exterior of the building, the interiors of the rooms, photos of the territory and individual objects.
В нашем мире, где диплом является началом отличной карьеры в любой области, многие стараются найти максимально простой путь получения качественного образования. Необходимость наличия официального документа переоценить невозможно. Ведь диплом открывает двери перед всеми, кто стремится вступить в профессиональное сообщество или учиться в любом ВУЗе.
В данном контексте мы предлагаем максимально быстро получить этот необходимый документ. Вы можете заказать диплом, и это становится выгодным решением для человека, который не смог завершить образование, потерял документ или желает исправить плохие оценки. Все дипломы изготавливаются аккуратно, с особым вниманием ко всем деталям, чтобы на выходе получился 100% оригинальный документ.
Плюсы этого решения состоят не только в том, что вы сможете быстро получить свой диплом. Процесс организован удобно, с нашей поддержкой. От выбора необходимого образца до правильного заполнения личной информации и доставки в любое место России — все под полным контролем качественных мастеров.
Для тех, кто ищет максимально быстрый способ получить требуемый документ, наша компания предлагает выгодное решение. Приобрести диплом – это значит избежать долгого процесса обучения и сразу переходить к важным целям, будь то поступление в ВУЗ или начало карьеры.
bybak.com/home.php?mod=space&uid=3111412В
hefeiyechang.com/home.php?mod=space&uid=13313В
naszaswietlica.dwr.pl/profile.php?lookup=17636В
opnevmonii.ru/nos/kapli/sofradeks.htmlВ
vmestedeshevle.listbb.ru/viewtopic.php?t=12699В
A person can configure the system oknews360.com independently or contact an organization to use the feature, focusing on their tools.
На сайте https://iseer.kz/ получите консультацию по поводу разработки и покупки уникальных и инновационных рекламных LED-решений, которые созданы для бизнеса, архитектуры. Для того чтобы осуществить точные расчеты, необходимо позвонить консультанту. Он расскажет обо всем, что необходимо. Прямо сейчас закажите наружную рекламу, видео-буквы, архитектурные подсветки, индивидуальный уникальный проект. В компании трудятся компетентные, квалифицированные сотрудники. У них огромный опыт в данной области.
Букмекерская контора «Леон» – это идеальная платформа для азартных игр. Здесь большой выбор ставок и живая статистика. Начните с уверенности с помощью бонусов для новичков. Простой интерфейс, оперативные выплаты и щедрые бонусы – это все о БК Леон. https://t.me/s/mleon_ru – канал, где у вас есть возможность начать выигрывать реальные денежные средства и присоединиться к сообществу ценителей спорта. Самый лучший сервис ждет вас, тут каждый шаг приведет вас к победе! Сделайте свой ход к успеху уже сегодня, выбирайте Леон. Вас ждет нереальная острота ощущений, убедитесь в этом лично!
Wenn es um Online-Casinos geht, ist Tipico eine der bekanntesten Marken in Deutschland. Mit seinem breiten Angebot an Spielen, darunter auch ein Live-Casino, zieht Tipico viele Spieler an, die auf der Suche nach Unterhaltung und Gewinnen sind. Um das Spielerlebnis noch spannender zu gestalten, bietet Tipico auch regelmäßig Bonusaktionen an, darunter auch den Tipico Live Casino Bonus Code.
Der Live Casino Bonus Code ist eine besondere Aktion von Tipico, bei der Spieler einen zusätzlichen Bonus erhalten, wenn sie im Live-Casino spielen. Dieser Bonus kann in Form von Bargeld, Freispielen oder anderen Vergünstigungen ausgezahlt werden. Um diesen Bonus zu erhalten, müssen Spieler den speziellen Bonuscode eingeben, der zuvor auf der Tipico-Website veröffentlicht wurde.
Der Live Casino Bonus Code ist eine großartige Möglichkeit, zusätzliches Geld zum Spielen zu erhalten und die Gewinnchancen zu erhöhen. Darüber hinaus bietet Tipico auch regelmäßig andere Aktionen an, wie z.B. Freispiele, Cashback-Angebote und Turniere, um die Spieler zu belohnen und das Spielerlebnis zu verbessern.
Um den Live Casino Bonus Code zu nutzen, sollten Spieler regelmäßig die Tipico-Website besuchen und nach aktuellen Aktionen Ausschau halten. Es lohnt sich auch, den Newsletter von Tipico zu abonnieren, um über die neuesten Bonusangebote informiert zu werden. Mit dem Live Casino Bonus Code können Spieler ihr Glück im Live-Casino von Tipico versuchen und dabei von zusätzlichen Belohnungen profitieren.
Insgesamt bietet der Tipico Live Casino Bonus Code eine großartige Möglichkeit, das Spielerlebnis zu verbessern und die Gewinnchancen zu erhöhen. Spieler sollten diese Aktion nutzen und das Beste aus ihrem Online-Casino-Erlebnis herausholen.
https://tipicocasino.one/
В нашем мире, где диплом является началом отличной карьеры в любой области, многие стараются найти максимально быстрый и простой путь получения качественного образования. Необходимость наличия официального документа переоценить невозможно. Ведь диплом открывает двери перед каждым человеком, который хочет вступить в профессиональное сообщество или учиться в высшем учебном заведении.
Предлагаем оперативно получить любой необходимый документ. Вы имеете возможность заказать диплом старого или нового образца, что будет отличным решением для человека, который не смог завершить образование или потерял документ. Все дипломы изготавливаются с особой тщательностью, вниманием ко всем элементам. На выходе вы сможете получить документ, полностью соответствующий оригиналу.
Превосходство данного подхода состоит не только в том, что можно оперативно получить свой диплом. Процесс организован комфортно и легко, с нашей поддержкой. От выбора нужного образца до грамотного заполнения персональных данных и доставки в любое место страны — все находится под полным контролем квалифицированных специалистов.
Для всех, кто пытается найти быстрый способ получения требуемого документа, наша компания может предложить отличное решение. Приобрести диплом – это значит избежать долгого обучения и сразу переходить к своим целям, будь то поступление в ВУЗ или начало удачной карьеры.
premium-diploms24.com/%D0%BA%D1%83%D0%BF%D0%B8%D1%82%D1%8C-%D0%B4%D0%B8%D0%BF%D0%BB%D0%BE%D0%BC-%D0%BF%D0%B5%D1%80%D0%BC%D1%8C/В
bbs.blueplatform.org/space-uid-31467.htmlВ
skoshi1-2.buryatschool.ru/sveden/commonВ
life-news.ru/attitudes/10733-brak-delo-sereznoe.htmlВ
mafiaclans.ru/topic3885.htmlВ
Connecting handsets to communicate with people dallasrentapart.com. You need to consider what devices people will be using to contact support.
The vibrant energy of spring comes to life event-miami24.com against a backdrop of sun-drenched beaches and pulsating rhythms. This is the perfect time to provide everything Miami and Miami Beach hospitals have to offer.
Интернет-магазин «Body-pit» предлагает вам купить спортивное питание по доступным ценам от популярных производителей. Мы готовы оказать вам квалифицированную помощь в подборе нужного товара. Вы останетесь довольны обслуживанием и магазином. https://ufa2.body-pit.ru/ – сайт, где можете прямо сейчас ознакомиться с условиями оплаты. Осуществляем оперативную доставку спортпита и стремимся обеспечить своих клиентов лучшим сервисом. Качество спортивного питания нашего онлайн-магазина на высоте. Обращайтесь к нам уже сейчас!
Zet Casino ist ein beliebtes Online-Casino, das seinen Spielern eine Vielzahl von Spielen und Boni bietet. Ein besonders attraktives Angebot sind die Zet Casino Freispiele, die die Spieler einlösen können.
Um die Freispiele bei Zet Casino einzulösen, müssen die Spieler bestimmte Schritte befolgen. Zunächst einmal müssen sie sich bei Zet Casino anmelden und ein Konto erstellen. Dies ist ein einfacher Vorgang, der nur wenige Minuten in Anspruch nimmt.
Sobald das Konto erstellt wurde, können die Spieler die Freispiele beanspruchen, indem sie sich im Casino einloggen und den entsprechenden Bonuscode eingeben. Der Bonuscode kann auf der Website des Casinos oder in Werbemails gefunden werden.
Sobald die Freispiele aktiviert wurden, können die Spieler sie bei ausgewählten Spielen im Casino einsetzen. Die Freispiele ermöglichen es den Spielern, kostenlos zu spielen und dabei echte Gewinne zu erzielen.
Es ist jedoch wichtig zu beachten, dass die Freispiele in der Regel bestimmten Umsatzbedingungen unterliegen. Die Spieler müssen den Gewinn aus den Freispielen eine bestimmte Anzahl von Malen umsetzen, bevor sie ihn abheben können.
Insgesamt bieten die Zet Casino Freispiele den Spielern eine großartige Möglichkeit, das Casino kennenzulernen und ohne eigenes Geld zu spielen. Mit etwas Glück und Geschick können die Spieler sogar echte Gewinne erzielen und ihr Spielerlebnis noch spannender gestalten.
https://zetcasino.one/
http://cheapestindia.com/# indian pharmacy
Das Tipico Casino bietet seinen Spielern eine Vielzahl von verschiedenen Boni und Aktionen an, um das Spielerlebnis noch spannender und lukrativer zu gestalten. In diesem Artikel werden die verschiedenen aktiven Boni im Tipico Casino näher betrachtet.
Einer der beliebtesten Boni im Tipico Casino ist der Willkommensbonus für neue Spieler. Mit diesem Bonus können Spieler ihre erste Einzahlung im Casino verdoppeln und somit ihre Gewinnchancen erhöhen. Darüber hinaus gibt es regelmäßig verschiedene Aktionen, bei denen Spieler zusätzliche Bonusguthaben oder Freispiele erhalten können.
Ein weiterer Vorteil des Tipico Casinos ist das Treueprogramm, das es Spielern ermöglicht, für ihre Aktivitäten im Casino belohnt zu werden. Je mehr ein Spieler im Casino spielt, desto mehr Punkte sammelt er und desto höher steigt er im Treueprogramm auf. Mit jedem neuen Level können Spieler von verschiedenen Vergünstigungen und Boni profitieren.
Des Weiteren werden im Tipico Casino regelmäßig Turniere und Wettbewerbe veranstaltet, bei denen Spieler attraktive Preise wie Bargeldgewinne oder Freispiele gewinnen können. Diese Veranstaltungen sorgen nicht nur für zusätzliche Spannung im Casino, sondern bieten auch die Möglichkeit, mit anderen Spielern in Wettbewerb zu treten.
Insgesamt bietet das Tipico Casino eine Vielzahl von aktiven Boni und Aktionen, die das Spielerlebnis noch unterhaltsamer und lukrativer gestalten. Spieler sollten regelmäßig die Promotionsseite des Casinos besuchen, um über die neuesten Aktionen informiert zu bleiben und keine lukrativen Angebote zu verpassen.
https://tipicocasino.one/
Ищите тяговые батареи для вилочных погрузчиков и штабелеров? Зайдите на https://www.tyumen-bat.ru/ и вы найдете тяговые батареи Тюменского аккумуляторного завода в огромном ассортименте по лучшим ценам, с доставкой. Батарее для любого вида и типа погрузчика или штабелера по выгодным ценам у нас.
chinaone.net
Ищете работу с гибким графиком и стабильным заработком? Яндекс Еда https://delivery-work.ru/ это возможность совмещать работу с учебой или другими делами. Преимущества работы курьером Яндекс Еда: свободный график, ежедневные выплаты, бонусы и премии, работа рядом с домом: доставляйте заказы в своем районе, экономя время на дорогу. Чтобы стать курьером Яндекс Еда, достаточно подать заявку на сайте. Присоединяйтесь к команде Яндекс Еда и начните зарабатывать уже сегодня!
Destruam предоставляет для вас большой выбор сериалов. Все они захватывают уже с первых минут. Пригласите своих друзей, соберитесь с близкими и в полной мере наслаждайтесь новинками кино. Гарантируем отменный звук и оперативную загрузку видео. Ищете смотреть сериал украденная любовь онлайн? Destruam.xyz – известный портал, где представлены сериалы, которые увлекут сюжетными поворотами и неожиданными событиями. Качество и разнообразие контента на высочайшем уровне. Смотрите без утомительной процедуры регистрации интересные сериалы. Сделайте свой вечер веселым!
repairdesign24.com
В нашем обществе, где диплом – это начало успешной карьеры в любом направлении, многие ищут максимально быстрый путь получения качественного образования. Факт наличия официального документа об образовании трудно переоценить. Ведь диплом открывает дверь перед людьми, желающими начать трудовую деятельность или учиться в ВУЗе.
Предлагаем очень быстро получить этот необходимый документ. Вы сможете заказать диплом нового или старого образца, и это становится выгодным решением для человека, который не смог закончить обучение или потерял документ. Любой диплом изготавливается аккуратно, с особым вниманием к мельчайшим элементам, чтобы в результате получился полностью оригинальный документ.
Преимущество данного подхода состоит не только в том, что можно быстро получить диплом. Весь процесс организовывается комфортно и легко, с профессиональной поддержкой. От выбора нужного образца до консультаций по заполнению личных данных и доставки в любое место России — все под абсолютным контролем наших специалистов.
Для всех, кто пытается найти оперативный способ получения требуемого документа, наша компания готова предложить отличное решение. Купить диплом – это значит избежать долгого процесса обучения и сразу перейти к достижению личных целей, будь то поступление в университет или старт карьеры.
steel-knife.ru/category/kukriВ
dancescape.gr/2021/09/09/%CE%AD%CE%BD%CE%B1%CF%81%CE%BE%CE%B7-%CE%BC%CE%B1%CE%B8%CE%B7%CE%BC%CE%AC%CF%84%CF%89%CE%BD-15-9-21/В
prolinksdirectory.com/website-list-1969/В
perscom.ru/2012-03-23-14-46-26/89-vvedenie1/552-par-i-posledВ
http://www.beretta-modelle.ch/forum/memberlist.php?orderby=username&ordertype=desc&search=&char=O&page=10В
На сайте https://webasyst.pro закажите профессиональную, качественную оптимизацию сайтов, интернет-магазинов. Все работы происходят на профессиональном уровне, максимально быстро, качественно, в соответствии с требованиями клиентов. Эффективность работы вашего магазина будет увеличена в несколько раз. Если вас не устроит результат или не увидите прогресса, то средства будут возвращены. Над каждым проектом трудятся лучшие специалисты, которые действительно работают на совесть.
Farmacie on line spedizione gratuita Farmacie on line spedizione gratuita farmacia online
Tipico Casino Fehler 50202
Das Tipico Casino ist eine beliebte Online-Glücksspielplattform, auf der Spieler aus der ganzen Welt ihre Lieblingsspiele spielen können. Wie bei jeder anderen Webseite kann es jedoch zu gelegentlichen technischen Problemen kommen. Eines dieser Probleme, das viele Spieler erlebt haben, ist der Fehler 50202.
Der Fehler 50202 tritt normalerweise auf, wenn die Tipico Casino-Webseite Гјberlastet ist oder Probleme mit dem Server auftreten. Dies kann frustrierend sein, da Spieler daran gehindert werden, ihre Lieblingsspiele zu spielen oder auf ihre Kontoinformationen zuzugreifen.
Wenn Sie den Fehler 50202 auf der Tipico Casino-Webseite sehen, gibt es einige Schritte, die Sie unternehmen können, um das Problem zu lösen. Zunächst einmal sollten Sie sicherstellen, dass Ihre Internetverbindung stabil ist und Sie eine gute WLAN-Verbindung haben. Wenn dies der Fall ist, können Sie versuchen, die Webseite neu zu laden oder Ihren Browserverlauf und Cookies zu löschen.
Wenn das Problem weiterhin besteht, empfehlen wir Ihnen, den Tipico Casino-Kundendienst zu kontaktieren. Die Mitarbeiter sind in der Regel gut ausgebildet und können Ihnen bei der Behebung des Fehlers 50202 helfen.
Insgesamt ist der Fehler 50202 im Tipico Casino zwar ärgerlich, aber in der Regel einfach zu beheben. Indem Sie die oben genannten Schritte befolgen und den Kundendienst kontaktieren, sollten Sie in kürzester Zeit wieder online spielen können.
https://tipicocasino.one/
Сегодня, когда диплом является началом успешной карьеры в любом направлении, многие стараются найти максимально быстрый путь получения образования. Наличие официального документа трудно переоценить. Ведь именно диплом открывает двери перед каждым человеком, который стремится начать профессиональную деятельность или продолжить обучение в ВУЗе.
В данном контексте наша компания предлагает очень быстро получить этот важный документ. Вы можете заказать диплом, и это становится выгодным решением для всех, кто не смог закончить образование, утратил документ или хочет исправить свои оценки. дипломы производятся с особой тщательностью, вниманием ко всем деталям, чтобы в итоге получился 100% оригинальный документ.
Преимущество подобного решения заключается не только в том, что можно быстро получить свой диплом. Процесс организовывается удобно, с профессиональной поддержкой. Начиная от выбора требуемого образца документа до грамотного заполнения личных данных и доставки в любое место страны — все под полным контролем качественных специалистов.
Таким образом, для всех, кто ищет максимально быстрый способ получить требуемый документ, наша услуга предлагает отличное решение. Купить диплом – значит избежать долгого процесса обучения и не теряя времени перейти к личным целям, будь то поступление в университет или начало карьеры.
http://www.8arusak-diploms24.com/
asthma treatment defend – asthma medication modern inhalers for asthma cool
Boomerang Casino Bewertungen: Erfahrungen und Meinungen
Das Boomerang Casino ist eine Online-Spielhalle, die sich in den letzten Jahren einen Namen in der GlГјcksspielbranche gemacht hat. Mit einer Vielzahl von Spielen, attraktiven Boni und einem benutzerfreundlichen Design lockt das Casino Spieler aus der ganzen Welt an. Doch wie sind die Erfahrungen der Spieler mit dem Boomerang Casino?
Um dies herauszufinden, haben wir uns die Bewertungen und Meinungen der Nutzer genauer angesehen. Insgesamt fällt das Feedback zum Boomerang Casino überwiegend positiv aus. Viele Spieler loben die große Auswahl an Spielen, darunter Slots, Tischspiele, Live-Casino-Spiele und mehr. Auch die Grafik und Soundeffekte der Spiele wurden von den Nutzern positiv bewertet.
Ein weiterer Pluspunkt des Boomerang Casinos sind die attraktiven Boni und Promotionen, die regelmäßig angeboten werden. Spieler berichten von großzügigen Willkommensboni, Freispielen und Cashback-Angeboten, die das Spielerlebnis noch spannender machen. Auch die schnellen Auszahlungen und der zuverlässige Kundensupport wurden von den Nutzern gelobt.
Allerdings gibt es auch vereinzelt Kritikpunkte am Boomerang Casino. Einige Spieler bemängeln zum Beispiel die Umsatzbedingungen bei den Boni, die als zu hoch empfunden werden. Auch die Auswahl an Zahlungsmethoden könnte nach Meinung einiger Nutzer erweitert werden.
Insgesamt lässt sich sagen, dass das Boomerang Casino eine gute Wahl für Spieler ist, die auf der Suche nach einer abwechslungsreichen und unterhaltsamen Spielhalle sind. Mit einer großen Auswahl an Spielen, attraktiven Boni und einem zuverlässigen Kundensupport überzeugt das Casino auf ganzer Linie. Wer also auf der Suche nach einem neuen Online-Casino ist, sollte das Boomerang Casino definitiv in Betracht ziehen.
Insgesamt können wir das Boomerang Casino mit gutem Gewissen weiterempfehlen und würden uns über weitere positive Bewertungen freuen.
https://boomerangcasino.one/
farmacia barata: farmacia online madrid – farmacias online seguras
Возникла необходимость срочного ремонта в доме, а денег не было. Нашел телеграм-канал новые и малоизвестные МФО 2024, где представлено более 20 малоизвестных МФО, предлагающих быстрые онлайн-займы. Приятно, что займ могут получить все от 18 лет, даже с плохой кредитной историей. Заявка была одобрена моментально, и деньги пришли на карту за несколько минут. Это помогло мне быстро справиться с ремонтом. Очень благодарен этому каналу, рекомендую всем, кто ищет быстрый займ!
В современном мире, где диплом – это начало успешной карьеры в любой сфере, многие ищут максимально простой путь получения образования. Необходимость наличия документа об образовании переоценить невозможно. Ведь именно диплом открывает дверь перед людьми, желающими вступить в профессиональное сообщество или продолжить обучение в высшем учебном заведении.
Наша компания предлагает максимально быстро получить этот важный документ. Вы сможете заказать диплом старого или нового образца, и это является удачным решением для человека, который не смог завершить обучение, утратил документ или хочет исправить плохие оценки. Каждый диплом изготавливается с особой тщательностью, вниманием к мельчайшим нюансам, чтобы в результате получился документ, максимально соответствующий оригиналу.
Преимущества такого решения состоят не только в том, что вы быстро получите свой диплом. Весь процесс организован комфортно, с профессиональной поддержкой. От выбора необходимого образца диплома до консультаций по заполнению личной информации и доставки по стране — все под полным контролем квалифицированных специалистов.
Всем, кто пытается найти быстрый и простой способ получения требуемого документа, наша услуга предлагает отличное решение. Заказать диплом – это значит избежать долгого процесса обучения и сразу переходить к достижению своих целей, будь то поступление в университет или старт удачной карьеры.
http://www.diploman-russiann.com/
farmacia online piГ№ conveniente: comprare farmaci online con ricetta – farmacie online autorizzate elenco
acne medication drum – acne medication scar acne medication their
На сайте https://t.me/mvavada который представляет собой официальный канал популярного онлайн-заведения «VAVADA», предлагает ознакомиться с ценной, важной информацией. Она будет необходима всем, кто следит за работой заведения и считает себя азартным человеком. На этом канале выкладывается весь свежий контент для того, чтобы вы ознакомились с ним первым. Кроме того, есть и разнообразные акции, промокод, который позволит сэкономить и сыграть по-крупному. Только на этом канале, в первую очередь, публикуются самые свежие новости.
В нашем обществе, где диплом – это начало успешной карьеры в любом направлении, многие ищут максимально быстрый путь получения образования. Необходимость наличия официального документа трудно переоценить. Ведь именно диплом открывает дверь перед всеми, кто хочет начать трудовую деятельность или учиться в ВУЗе.
В данном контексте наша компания предлагает быстро получить этот важный документ. Вы сможете заказать диплом старого или нового образца, что будет удачным решением для человека, который не смог завершить обучение, потерял документ или желает исправить свои оценки. Каждый диплом изготавливается с особой тщательностью, вниманием к мельчайшим деталям. В результате вы получите полностью оригинальный документ.
Плюсы такого решения заключаются не только в том, что можно оперативно получить диплом. Весь процесс организован просто и легко, с профессиональной поддержкой. Начав от выбора необходимого образца до консультаций по заполнению личной информации и доставки по стране — все будет находиться под полным контролем квалифицированных специалистов.
Всем, кто пытается найти быстрый и простой способ получения необходимого документа, наша услуга предлагает отличное решение. Приобрести диплом – это значит избежать долгого обучения и не теряя времени перейти к достижению своих целей: к поступлению в ВУЗ или к началу трудовой карьеры.
http://www.diplomans-russia.com/
acne medication common – acne medication upward acne treatment throw
Howdy I am so happy I found your webpage, I really found you by accident, while I was searching on Digg for something else, Anyways I am here now and would just like to say many thanks for a tremendous post and a all round enjoyable blog (I also love the theme/design), I don’t have time to go through it all at the minute but I have bookmarked it and also included your RSS feeds, so when I have time I will be back to read more, Please do keep up the superb work.
http://9saksx-diploms24.com/
Tipico ist vielen als einer der bekanntesten Anbieter fГјr Sportwetten in Deutschland bekannt. Doch seit einiger Zeit bietet das Unternehmen auch ein Online-Casino an: das Tipico Casino.
Für viele Kunden ist der Übergang von Tipico zu Tipico Casino ein interessanter Schritt. Denn nun können sie nicht nur auf sportliche Ereignisse wetten, sondern auch ihr Glück an Spielautomaten oder Tischspielen versuchen.
Das Tipico Casino bietet eine Vielzahl von Spielen an, darunter beliebte Klassiker wie Roulette, Blackjack und Poker. Zudem gibt es eine große Auswahl an Spielautomaten mit verschiedenen Themen und Gewinnmöglichkeiten.
Ein besonderer Anreiz für Kunden, die von Tipico auf das Tipico Casino wechseln, sind die regelmäßig angebotenen Promotionen und Boni. Diese können zusätzliche Gewinnchancen bringen und das Spielerlebnis noch spannender machen.
Zudem steht der Kundenservice auch im Tipico Casino den Spielern rund um die Uhr zur VerfГјgung, um Fragen zu beantworten oder Hilfe bei Problemen zu bieten.
Insgesamt bietet das Tipico Casino eine unterhaltsame und sichere Spielumgebung fГјr Kunden, die gerne online spielen. Der Гњbergang von Tipico zu Tipico Casino ist also fГјr viele eine lohnenswerte Option, um ihr GlГјck in verschiedenen Spielen zu versuchen und neue Erfahrungen zu sammeln.
https://tipicocasino.one/
Хотите смотреть интересные фильмы онлайн абсолютно бесплатно в великолепном качестве? ЛордФильм предоставляет такую прекрасную возможность. Здесь найдете фильмы, от которых дыхание захватывает. Мелодрамы, фэнтези, боевики ждут именно вас на https://online.lords-film.pics/59786-serial-halo-2-sezon-8-seriya-q27 У нас вы подберете фильм, который вам понравился, смотрите смешные мультики либо новинки сериалов в любое время.
online apotheke gГјnstige online apotheke beste online-apotheke ohne rezept
На сайте https://hyips-money.ru/ ознакомьтесь с инвестиционными проектами, рекомендациями, которые помогут заработать неплохие средства. Этот сервис регулярно мониторит те проекты, которые действительно приносят прибыль, где вас точно не обманут, а деньги выплатят быстро и без обмана. Здесь получится отыскать всю необходимую информацию относительно инвестиционных проектов. Изучите полный список хайп-проектов, которые будут полезны и вам. Регулярно проверяется платежеспособность, чтобы исключить возможные денежные потери.
ohne rezept apotheke: apotheke online – online apotheke rezept
inhalers for asthma guess – asthma treatment alley asthma treatment deceive
Digital Agency Империя стремиться для вас качественно реализовать свои услуги. Профессиональная команда состоит исключительно из опытных сотрудников, которые постоянно развиваются и знают секреты успешного продвижения сайтов. Главное то, что они честно трудятся. Ищете smm в социальных сетях? Imperiasinteza.com – здесь вы найдете цены на услуги, посмотрите их уже сейчас. Мы прикладываем максимум усилий, чтобы клиент остался всем, доволен и приходил к нам снова. Позвоните нам уже сейчас, готовы помочь вашему бизнесу достичь успеха в онлайн-мире!
В нашем мире, где диплом является началом успешной карьеры в любой области, многие ищут максимально быстрый путь получения качественного образования. Необходимость наличия официального документа переоценить невозможно. Ведь диплом открывает двери перед каждым человеком, желающим начать профессиональную деятельность или продолжить обучение в высшем учебном заведении.
Предлагаем максимально быстро получить этот необходимый документ. Вы имеете возможность купить диплом нового или старого образца, и это будет удачным решением для человека, который не смог завершить образование или потерял документ. диплом изготавливается с особой аккуратностью, вниманием ко всем нюансам. В итоге вы получите полностью оригинальный документ.
Плюсы этого подхода состоят не только в том, что вы быстро получите диплом. Весь процесс организован удобно, с нашей поддержкой. Начиная от выбора требуемого образца диплома до грамотного заполнения личной информации и доставки в любое место страны — все будет находиться под абсолютным контролем квалифицированных специалистов.
Всем, кто ищет максимально быстрый способ получить требуемый документ, наша компания может предложить отличное решение. Заказать диплом – значит избежать продолжительного обучения и не теряя времени перейти к достижению собственных целей: к поступлению в университет или к началу успешной карьеры.
http://www.5gruppa365-diploms.com/
Відвідайте сайт https://i4car.net/ який є автомобільним порталом з цікавими новинами. Автоновини, все про автомобілі, тест драйви, поради досвідчених автолюбителів та багато іншого. Кожен знайде для себе корисне та цікаве.
Лучшие букмекеры в России – это те компании, которые предлагают высокие коэффициенты, широкий выбор спортивных событий и удобный интерфейс для ставок. Таких букмекеров можно выделить своей обширной линией, а также возможностью делать ставки в реальном времени. Они предлагают большое количество рынков для ставок и быстрые выплаты. Имеют удобное приложение для мобильных устройств. В целом, выбор букмекера зависит от предпочтений каждого игрока, но букмекеры на сайте https://russianbookmakers.ru/ являются одними из лучших на российском рынке
טלגראס כיוונים
האפליקציה הווה פלטפורמה מקובלת בארץ לרכישת קנאביס בצורה אינטרנטי. זו נותנת ממשק נוח ובטוח לרכישה וקבלת שילוחים מ מוצרי מריחואנה שונים. בכתבה זו נבחן עם הרעיון מאחורי הפלטפורמה, כיצד זו עובדת ומהם היתרים של השימוש בה.
מה זו הפלטפורמה?
הפלטפורמה היא אמצעי לקנייה של צמח הקנאביס דרך היישומון טלגרם. היא מבוססת על ערוצי תקשורת וקבוצות טלגראם ייעודיות הקרויות ״טלגראס כיוונים, שבהם ניתן להזמין מרחב פריטי מריחואנה ולקבלת אותם ישירות למשלוח. ערוצי התקשורת אלו מאורגנים על פי איזורים גיאוגרפיים, כדי לשפר את קבלתם של המשלוחים.
כיצד זה עובד?
התהליך פשוט יחסית. ראשית, צריך להצטרף לערוץ הטלגראס הנוגע לאזור המחיה. שם אפשר לעיין בתפריטים של הפריטים המגוונים ולהזמין את הפריטים הרצויים. לאחר השלמת ההזמנה וסיום התשלום, השליח יופיע לכתובת שנרשמה עם החבילה שהוזמן.
מרבית ערוצי הטלגראס מציעים מגוון רחב של מוצרים – סוגי קנאביס, עוגיות, שתייה ועוד. כמו כן, אפשר לראות ביקורות מ צרכנים קודמים על רמת הפריטים והשרות.
מעלות השימוש באפליקציה
מעלה מרכזי של הפלטפורמה הוא הנוחות והפרטיות. ההזמנה והתהליך מתבצעות ממרחק מאיזשהו מיקום, ללא נחיצות במפגש פנים אל פנים. כמו כן, האפליקציה מוגנת היטב ומבטיחה חיסיון גבוה.
מלבד על כך, עלויות הפריטים באפליקציה נוטים לבוא זולים, והמשלוחים מגיעים במהירות ובהשקעה רבה. יש גם מוקד תמיכה זמין לכל שאלה או בעיית.
סיכום
טלגראס הווה דרך חדשנית ויעילה לרכוש מוצרי קנאביס בישראל. היא משלבת את הנוחות הטכנולוגית מ היישומון הפופולרית, ועם המהירות והפרטיות של שיטת השילוח הישירה. ככל שהביקוש לקנאביס גדלה, אפליקציות בדוגמת זו צפויות להמשיך ולצמוח.
acheter mГ©dicament en ligne sans ordonnance: pharmacie en ligne avec ordonnance – pharmacie en ligne
Zet Casino ist eines der beliebtesten Online-Casinos, das seinen Spielern eine Vielzahl von großartigen Angeboten und Aktionen bietet. Eines der begehrtesten Angebote für die Spieler sind die Zet Casino Freispiele, die sie bei verschiedenen Spielen nutzen können. Doch welches Spiel eignet sich am besten, um diese Freispiele zu nutzen?
Es gibt eine Vielzahl von Spieloptionen, bei denen die Spieler ihre Freispiele einsetzen können. Eines der beliebtesten Spiele ist der Spielautomat Book of Dead. Dieses ägyptische Abenteuer bietet den Spielern nicht nur spannende Unterhaltung, sondern auch die Möglichkeit, hohe Gewinne zu erzielen. Mit den Zet Casino Freispielen können die Spieler kostenlos die Walzen drehen und auf der Suche nach antiken Schätzen gehen.
Ein weiteres beliebtes Spiel, bei dem die Freispiele gut eingesetzt werden können, ist Starburst. Dieser farbenfrohe Spielautomat bietet den Spielern nicht nur ein unterhaltsames Spielerlebnis, sondern auch die Chance auf große Gewinne. Mit den Zet Casino Freispielen können die Spieler dieses aufregende Spiel kostenlos ausprobieren und hoffentlich lukrative Gewinne erzielen.
Für diejenigen, die lieber Tischspiele spielen, bieten sich die Zet Casino Freispiele auch für Spiele wie Roulette oder Blackjack an. Mit den Freispielen können die Spieler kostenlos Einsätze tätigen und ihr Glück am Tisch versuchen.
Insgesamt bieten die Zet Casino Freispiele den Spielern eine großartige Möglichkeit, verschiedene Spiele auszuprobieren und dabei möglicherweise auch noch hohe Gewinne zu erzielen. Egal, ob man lieber Spielautomaten oder Tischspiele spielt, bei Zet Casino findet jeder Spieler das passende Spiel, um seine Freispiele zu nutzen. Also worauf wartet ihr noch? Nutzt eure Zet Casino Freispiele und erlebt spannende Spielunterhaltung!
https://zetcasino.one/
b29
Bản cài đặt B29 IOS – Giải pháp vượt trội cho các tín đồ iOS
Trong thế giới công nghệ đầy sôi động hiện nay, trải nghiệm người dùng luôn là yếu tố then chốt. Với sự ra đời của Bản cài đặt B29 IOS, người dùng sẽ được hưởng trọn vẹn những tính năng ưu việt, mang đến sự hài lòng tuyệt đối. Hãy cùng khám phá những ưu điểm vượt trội của bản cài đặt này!
Tính bảo mật tối đa
Bản cài đặt B29 IOS được thiết kế với mục tiêu đảm bảo an toàn dữ liệu tuyệt đối cho người dùng. Nhờ hệ thống mã hóa hiện đại, thông tin cá nhân và dữ liệu nhạy cảm của bạn luôn được bảo vệ an toàn khỏi những kẻ xâm nhập trái phép.
Trải nghiệm người dùng đỉnh cao
Giao diện thân thiện, đơn giản nhưng không kém phần hiện đại, B29 IOS mang đến cho người dùng trải nghiệm duyệt web, truy cập ứng dụng và sử dụng thiết bị một cách trôi chảy, mượt mà. Các tính năng thông minh được tối ưu hóa, giúp nâng cao hiệu suất và tiết kiệm pin đáng kể.
Tính tương thích rộng rãi
Bản cài đặt B29 IOS được phát triển với mục tiêu tương thích với mọi thiết bị iOS từ các dòng iPhone, iPad cho đến iPod Touch. Dù là người dùng mới hay lâu năm của hệ điều hành iOS, B29 đều mang đến sự hài lòng tuyệt đối.
Quá trình cài đặt đơn giản
Với những hướng dẫn chi tiết, việc cài đặt B29 IOS trở nên nhanh chóng và dễ dàng. Chỉ với vài thao tác đơn giản, bạn đã có thể trải nghiệm ngay tất cả những tính năng tuyệt vời mà bản cài đặt này mang lại.
Bản cài đặt B29 IOS không chỉ là một bản cài đặt đơn thuần, mà còn là giải pháp công nghệ hiện đại, nâng tầm trải nghiệm người dùng lên một tầm cao mới. Hãy trở thành một phần của cộng đồng sử dụng B29 IOS để khám phá những tiện ích tuyệt vời mà nó có thể mang lại!
Хотите в отменном качестве и совершенно бесплатно смотреть увлекательные сериалы? Mixtios предоставляет такую прекрасную возможность. Здесь имеется только самое интересное кино. Вы можете в любое удобное время смотреть фильмы. Ищете алекс райдер сериал 2020? Mixtios.xyz – сайт, где представлены сериалы, которые помогают оторваться от повседневной жизни и ощутить множество позитивных эмоций. Профессиональное озвучивание и отменное качество изображения гарантируют великолепный просмотр. Уверены, у нас вы найдете то, что вам интересно!
comprare farmaci online all’estero п»їFarmacia online migliore farmacie online affidabili
На сайте https://t.me/mvavada ознакомьтесь с нужной, ценной информацией, которая касается игрового клуба «VAVADA». Он дарит огромное количество привилегий, действует щедрая бонусная программа, а каждый игрок получает право вывести средства в наиболее комфортное для себя время. Только на этом канале самая честная, правдивая информация о компании, которая ценит своих клиентов. Казино предлагает огромный выбор развлечений, интересных и разнообразных слотов. Заходите сюда постоянно, ведь новая информация появляется регулярно.
Das Boomerang Casino bringt den Nervenkitzel der Spielhalle direkt zu Ihnen nach Hause. Mit einer Vielzahl von Spielen und spannenden Aktionen verspricht dieses Online-Casino SpaГџ und Unterhaltung fГјr alle!
Das Boomerang Casino bietet eine breite Auswahl an Spielen, darunter klassische Spielautomaten, Tischspiele wie Blackjack und Roulette, sowie spannende Live-Casino-Spiele. Die Grafik und das Gameplay sind von höchster Qualität, um Ihnen ein authentisches Casino-Erlebnis zu bieten.
Neben den Spielen bietet das Boomerang Casino auch großzügige Boni und Aktionen für seine Spieler. Neue Spieler erhalten in der Regel einen Willkommensbonus, der ihnen zusätzliches Guthaben zum Spielen gibt. Außerdem gibt es regelmäßig Turniere und Sonderaktionen, bei denen Spieler attraktive Preise gewinnen können.
Der Kundenservice im Boomerang Casino steht Ihnen rund um die Uhr zur Verfügung und ist immer bereit, Ihnen bei Fragen oder Problemen zu helfen. Die Webseite ist benutzerfreundlich gestaltet und ermöglicht es Ihnen, schnell und einfach auf Ihre Lieblingsspiele zuzugreifen.
Insgesamt bietet das Boomerang Casino eine spannende und unterhaltsame Spielerfahrung für alle, die gerne ihr Glück versuchen möchten. Probieren Sie es aus und entdecken Sie die aufregende Welt des Online-Glücksspiels im Boomerang Casino!
https://boomerangcasino.one/
Интернет-магазин «Body-pit» предлагает вам купить спортивное питание по доступным ценам от популярных производителей. Мы готовы оказать вам профессиональную помощь в подборе необходимого товара. Вы останетесь довольны магазином и обслуживанием. https://ufa2.body-pit.ru/ – сайт, где у вас есть возможность уже сейчас посмотреть условия оплаты. Осуществляем оперативную доставку спортпита и стремимся обеспечить своих клиентов лучшим сервисом. Качество спортивного питания у нас на высоте. Обращайтесь к нам уже сейчас!
Хотите смотреть интересные фильмы онлайн абсолютно бесплатно в великолепном качестве? ЛордФильм предоставляет такую прекрасную возможность. Здесь вы найдете такие фильмы, от которых захватывает дыхание. Мелодрамы, фэнтези, боевики ждут именно вас на https://online.lords-film.pics/79849-missiya-nevypolnima-smertelnaya-rasplata-chast-2-film-2024-01 У нас вы подберете фильм, который вам понравился, смотрите смешные мультики либо новинки сериалов в любое время.
If the request is not registered properly chinanews777.com, they will load specialists in a chaotic manner. Tickets help to avoid such problems, because all operations will be carried out in a single IT system.
Pharmacie en ligne livraison Europe: acheter m̩dicament en ligne sans ordonnance Рpharmacie en ligne sans ordonnance
invest-company.net
проверка usdt trc20
Как обезопасить свои личные данные: избегайте утечек информации в интернете. Сегодня обеспечение безопасности личных данных становится более насущной важной задачей. Одним из наиболее распространенных способов утечки личной информации является слив «сит фраз» в интернете. Что такое сит фразы и в какой мере защититься от их утечки? Что такое «сит фразы»? «Сит фразы» — это комбинации слов или фраз, которые часто используются для получения доступа к различным онлайн-аккаунтам. Эти фразы могут включать в себя имя пользователя, пароль или разные конфиденциальные данные. Киберпреступники могут пытаться получить доступ к вашим аккаунтам, используя этих сит фраз. Как защитить свои личные данные? Используйте запутанные пароли. Избегайте использования простых паролей, которые легко угадать. Лучше всего использовать комбинацию букв, цифр и символов. Используйте уникальные пароли для всего аккаунта. Не воспользуйтесь один и тот же пароль для разных сервисов. Используйте двухфакторную проверку (2FA). Это вводит дополнительный уровень безопасности, требуя подтверждение входа на ваш аккаунт через другое устройство или метод. Будьте осторожны с онлайн-сервисами. Не доверяйте личную информацию ненадежным сайтам и сервисам. Обновляйте программное обеспечение. Установите обновления для вашего операционной системы и программ, чтобы уберечь свои данные от вредоносного ПО. Вывод Слив сит фраз в интернете может повлечь за собой серьезным последствиям, таким как кража личной информации и финансовых потерь. Чтобы охранить себя, следует принимать меры предосторожности и использовать надежные методы для хранения и управления своими личными данными в сети
Seit einiger Zeit häufen sich die Beschwerden von Spielern über das Online-Casino Zet Casino. Viele Nutzer berichten von unfairen Geschäftspraktiken, verzögerten Auszahlungen und einem insgesamt schlechten Kundenservice. Einige Spieler haben sich nun dazu entschlossen, rechtliche Schritte gegen das Casino einzuleiten und es zu verklagen.
Die Gründe für die Klagen sind vielfältig. Einige Spieler fühlen sich betrogen, da sie trotz Erfüllung aller Bonusbedingungen ihre Gewinne nicht ausgezahlt bekommen haben. Andere berichten von technischen Problemen beim Spielen, die zu Verlusten geführt haben. Zudem gibt es Beschwerden über den Umgang des Kundenservice mit den Anliegen der Spieler, der oft unprofessionell und intransparent erscheint.
Die Klagen gegen Zet Casino könnten weitreichende Konsequenzen haben. Sollte das Gericht den Vorwürfen der Spieler Recht geben, könnte das Casino zu hohen Strafzahlungen verurteilt werden und seinen Ruf nachhaltig schädigen. Auch die Glücksspiellizenz des Casinos könnte in Gefahr geraten, was das Weiterbetreiben des Online-Casinos erschweren würde.
Es bleibt abzuwarten, wie die Gerichte über die Klagen gegen Zet Casino entscheiden werden. In jedem Fall sollten Spieler darauf achten, nur bei seriösen und vertrauenswürdigen Online-Casinos zu spielen, um Ärger und Enttäuschungen zu vermeiden. Wer selbst Probleme mit Zet Casino oder einem anderen Anbieter hat, sollte sich umgehend an eine Verbraucherberatung oder einen Anwalt wenden, um seine Rechte durchzusetzen.
https://zetcasino.one/
farmacia online senza ricetta: farmacie online sicure – Farmacia online miglior prezzo
Rassilka.kz оказывает качественные услуги. Делаем ватсап, смс, email, рассылки по Нур-Султану, Алматы и Казахстану. Сотрудничаем со многими известными компаниями. Наша главная задача – принести всем клиентам пользу. Действия нацелены на конечный результат. https://rassilka.kz – сайт, где вы узнаете, почему нас выбирают. Здесь у вас есть возможность уже сейчас посмотреть тарифы. У вас есть возможность получить бесплатную консультацию. Мы с удовольствием ответим на все ваши вопросы, свяжитесь с нами в любое время.
pharmacie en ligne avec ordonnance pharmacie en ligne pas cher pharmacie en ligne france livraison belgique
Das Boomerang Casino: Ein einzigartiges Spielerlebnis
Das Boomerang Casino ist ein Online-Casino, das sich von anderen Anbietern in vielerlei Hinsicht abhebt. Mit seinem australischen Thema und einer breiten Auswahl an Spielen bietet es ein einzigartiges Spielerlebnis fГјr alle Casino-Fans.
Das Casino ist bekannt für seine großzügigen Boni und Promotionen, die es Spielern ermöglichen, mehr aus ihrem Geld zu machen. Von Willkommensboni über Freispiele bis hin zu wöchentlichen Aktionen gibt es hier immer etwas Neues zu entdecken.
Die Auswahl an Spielen im Boomerang Casino ist ebenfalls beeindruckend. Von klassischen Tischspielen wie Blackjack und Roulette Гјber eine Vielzahl von Spielautomaten bis hin zu Live-Casino-Spielen bietet das Casino fГјr jeden Geschmack etwas Passendes.
Ein weiterer Pluspunkt des Boomerang Casinos ist die benutzerfreundliche Website, die es Spielern ermöglicht, schnell und einfach zu ihren Lieblingsspielen zu gelangen. Darüber hinaus bietet das Casino eine Vielzahl von sicheren Zahlungsmethoden, um Ein- und Auszahlungen einfach und sicher zu gestalten.
Insgesamt bietet das Boomerang Casino ein unterhaltsames und spannendes Spielerlebnis fГјr alle, die gerne online spielen. Mit seinen groГџzГјgigen Boni, einer breiten Auswahl an Spielen und einer benutzerfreundlichen Website ist das Casino eine gute Wahl fГјr alle Casino-Fans. Wer also auf der Suche nach einem neuen Online-Casino ist, sollte definitiv einen Blick auf das Boomerang Casino werfen.
https://boomerangcasino.one/
farmacia online madrid: farmacia online madrid – farmacia online 24 horas
האפליקציה היא תוכנה פופולרית בישראל לקנייה של מריחואנה באופן מקוון. זו נותנת ממשק פשוט לשימוש ובטוח לקנייה ולקבלת משלוחים מ מוצרי מריחואנה מרובים. בסקירה זו נסקור עם העיקרון שמאחורי טלגראס, איך זו עובדת ומה היתרונות של השימוש בה.
מהי האפליקציה?
הפלטפורמה היא דרך לרכישת קנאביס דרך היישומון טלגראם. זו נשענת מעל ערוצי תקשורת וקבוצות טלגרם ספציפיות הנקראות ״כיווני טלגראס״, שם ניתן להזמין מגוון פריטי צמח הקנאביס ולקבלת אלו ישירות למשלוח. הערוצים אלו מאורגנים על פי איזורים גיאוגרפיים, כדי להקל את קבלתם של השילוחים.
כיצד זה עובד?
התהליך פשוט יחסית. ראשית, צריך להצטרף לערוץ הטלגראס הנוגע לאזור המחיה. שם ניתן לצפות בתפריטי הפריטים השונים ולהזמין עם המוצרים הרצויים. לאחר ביצוע ההרכבה וסגירת התשלום, השליח יופיע בכתובת שנרשמה ועמו הארגז המוזמנת.
מרבית ערוצי הטלגראס מספקים מגוון נרחב מ פריטים – זנים של מריחואנה, עוגיות, משקאות ועוד. כמו כן, אפשר למצוא ביקורות מ לקוחות קודמים על רמת הפריטים והשירות.
יתרונות הנעשה בטלגראס
יתרון מרכזי של הפלטפורמה הוא הנוחיות והדיסקרטיות. ההזמנה והתהליך מתבצעות ממרחק מכל מיקום, בלי צורך במפגש פיזי. כמו כן, הפלטפורמה מוגנת היטב ומבטיחה חיסיון גבוהה.
נוסף על כך, מחירי הפריטים בפלטפורמה נוטות להיות זולים, והמשלוחים מגיעים במהירות ובמסירות גבוהה. קיים אף מרכז תמיכה פתוח לכל שאלה או בעיית.
סיכום
האפליקציה מהווה שיטה חדשנית ויעילה לרכוש מוצרי קנאביס בישראל. זו משלבת את הנוחות הטכנולוגית של האפליקציה הפופולרי, ועם המהירות והפרטיות מ שיטת השילוח הישירה. ככל שהדרישה לצמח הקנאביס גדלה, אפליקציות בדוגמת טלגראס צפויות להמשיך ולהתפתח.
Зайдіть на сайт https://wian.top/ і ви зможете дізнатися, почитати, переглянути найсвіжіші новини України. Стрічка постійно поповнюється, що дозволить вам залишатися в курсі найсвіжіших подій. Виберіть категорію, що цікавить, і читайте тільки актуальну інформацію.
Der Tipico Casino Bonus Code 2020 ist eine großartige Möglichkeit, um sich als Neukunde einen zusätzlichen Vorteil zu verschaffen. Mit diesem Bonuscode können Spieler von attraktiven Bonusangeboten profitieren und somit ihre Gewinnchancen erhöhen.
Der Tipico Casino Bonus Code 2020 kann entweder direkt bei der Registrierung oder bei der ersten Einzahlung eingegeben werden. Der Code aktiviert dann den entsprechenden Bonus, der je nach Aktion unterschiedlich ausfallen kann. Zum Beispiel können Spieler Freispiele, Einzahlungsboni oder Cashback-Angebote erhalten.
Um den Bonus zu erhalten, müssen die Spieler in der Regel bestimmte Umsatzbedingungen erfüllen. Diese können variieren und beinhalten oft einen Mindesteinsatz, den die Spieler tätigen müssen, um den Bonus freizuschalten. Es ist daher wichtig, die Bedingungen genau zu lesen, bevor man den Bonus in Anspruch nimmt.
Der Tipico Casino Bonus Code 2020 kann eine gute Möglichkeit sein, um das Online-Casino kennenzulernen und erste Gewinne zu erzielen. Es lohnt sich daher, regelmäßig nach neuen Bonuscodes Ausschau zu halten und von den attraktiven Angeboten zu profitieren. So können Spieler ihre Gewinnchancen erhöhen und das Spielerlebnis im Tipico Casino noch spannender gestalten.
https://tipicocasino.one/
farmaci senza ricetta elenco: Farmacia online piГ№ conveniente – migliori farmacie online 2024
На сайте https://setki.moscow вы сможете оформить заявку для того, чтобы заказать москитную сетку. Конструкции производятся из качественных, надежных материалов и всего за день. Монтажные работы проводятся в любой, наиболее комфортный для вас день. На работы, конструкции даются гарантии 12 месяцев. Рассчитать итоговую цену вы сможете прямо сейчас. Установлена привлекательная стоимость за счет собственного производства. Работа происходит не только по Москве, но и области. Предприятие специализируется на производстве, реализации, а также установке москитных сеток.
Как охранять свои данные: берегитесь утечек информации в интернете. Сегодня защита информации становится всё более важной задачей. Одним из наиболее популярных способов утечки личной информации является слив «сит фраз» в интернете. Что такое сит фразы и как защититься от их утечки? Что такое «сит фразы»? «Сит фразы» — это синтезы слов или фраз, которые постоянно используются для получения доступа к различным онлайн-аккаунтам. Эти фразы могут включать в себя имя пользователя, пароль или разные конфиденциальные данные. Киберпреступники могут пытаться получить доступ к вашим аккаунтам, с помощью этих сит фраз. Как охранить свои личные данные? Используйте непростые пароли. Избегайте использования легких паролей, которые мгновенно угадать. Лучше всего использовать комбинацию букв, цифр и символов. Используйте уникальные пароли для каждого аккаунта. Не пользуйтесь один и тот же пароль для разных сервисов. Используйте двухэтапную аутентификацию (2FA). Это привносит дополнительный уровень безопасности, требуя подтверждение входа на ваш аккаунт по другое устройство или метод. Будьте осторожны с онлайн-сервисами. Не доверяйте личную информацию ненадежным сайтам и сервисам. Обновляйте программное обеспечение. Установите обновления для вашего операционной системы и программ, чтобы защитить свои данные от вредоносного ПО. Вывод Слив сит фраз в интернете может спровоцировать серьезным последствиям, таким как кража личной информации и финансовых потерь. Чтобы защитить себя, следует принимать меры предосторожности и использовать надежные методы для хранения и управления своими личными данными в сети
tokyo365web.com
belfastinvest.net
Zet Casino Cashback
Bei Zet Casino können Spieler jetzt von einem attraktiven Cashback-Angebot profitieren. Das bedeutet, dass du einen Teil deiner Verluste zurückerstattet bekommst, wenn du eine Pechsträhne haben solltest.
Das Cashback-Angebot bei Zet Casino ist einfach und unkompliziert. Jeden Freitag erhältst du 10% deiner Verluste der vergangenen Woche als Cashback-Bonus gutgeschrieben. Das bedeutet, dass du immer ein wenig Trost erhältst, wenn es mal nicht so gut läuft.
Um das Cashback-Angebot nutzen zu können, musst du dich lediglich für die Aktion anmelden. Dafür gehst du einfach auf die Website von Zet Casino, klickst auf den Cashback-Bereich und meldest dich an. Sobald du angemeldet bist, musst du nur noch spielen und dein Cashback wird automatisch gutgeschrieben.
Das Cashback-Angebot bei Zet Casino bietet Spielern eine hervorragende Möglichkeit, Verluste zu minimieren und sich trotz einer Pechsträhne weiterhin am Spiel zu erfreuen. Wenn du also gerne im Online-Casino spielst, solltest du dieses attraktive Angebot auf jeden Fall in Anspruch nehmen.
Also, worauf wartest du noch? Melde dich jetzt fГјr das Cashback-Angebot bei Zet Casino an und profitiere von diesem groГџzГјgigen Bonus!
https://zetcasino.one/
Проверить транзакцию usdt trc20
Сохраните свои USDT: Удостоверьтесь перевод TRC20 до отправкой
Криптовалюты, такие вроде USDT (Tether) в распределенном реестре TRON (TRC20), делаются всё всё более распространенными в области сфере распределенных финансовых услуг. Тем не менее совместно со повышением распространенности увеличивается и риск погрешностей либо жульничества при переводе финансов. Как раз именно поэтому нужно проверять транзакцию USDT TRC20 перед ее пересылкой.
Ошибка во время вводе адреса адресата или перевод по некорректный адрес получателя сможет повлечь к невозможности необратимой потере ваших USDT. Злоумышленники тоже могут стараться провести вас, отправляя фальшивые адреса получателей для транзакции. Утрата криптовалюты вследствие подобных погрешностей сможет обернуться серьезными денежными убытками.
К радости, имеются специализированные сервисы, дающие возможность проверить операцию USDT TRC20 до ее пересылкой. Один из числа подобных служб дает опцию просматривать а также анализировать переводы на блокчейне TRON.
На данном обслуживании вы можете вводить адрес адресата а также получать подробную данные об адресе, включая архив операций, баланс и состояние аккаунта. Это посодействует выяснить, есть или нет адрес получателя подлинным и надежным для пересылки финансов.
Прочие сервисы тоже дают аналогичные возможности по удостоверения переводов USDT TRC20. Некоторые кошельки для криптовалют для цифровых валют обладают интегрированные функции по контроля адресов и операций.
Не игнорируйте контролем перевода USDT TRC20 до ее отправкой. Небольшая предосторожность может сберечь вам много финансов а также избежать потерю твоих важных крипто ресурсов. Применяйте заслуживающие доверия сервисы с целью гарантии безопасности ваших операций и целостности ваших USDT в распределенном реестре TRON.
apotheke online п»їshop apotheke gutschein ohne rezept apotheke
проверить кошелёк usdt trc20
В процессе работе с виртуальной валютой USDT в распределенном реестре TRON (TRC20) крайне существенно не только проверять реквизиты получателя перед переводом средств, но и периодически отслеживать баланс личного кошелька, а также источники входящих переводов. Это даст возможность вовремя идентифицировать любые нежданные операции и предотвратить возможные потери.
В первую очередь, требуется удостовериться в точности показываемого баланса USDT TRC20 в собственном кошельке для криптовалют. Предлагается сравнивать показания с сведениями открытых обозревателей блокчейна, с целью избежать шанс взлома или скомпрометирования этого крипто-кошелька.
Тем не менее лишь отслеживания баланса недостаточно. Крайне важно анализировать журнал поступающих переводов и этих происхождение. В случае если вы найдете транзакции USDT от анонимных или вызывающих опасения реквизитов, незамедлительно остановите эти средства. Имеется опасность, что данные монеты были получены.
Наше приложение предоставляет возможности с целью всестороннего изучения поступающих USDT TRC20 переводов на предмет их легальности а также отсутствия соотношения с противозаконной деятельностью. Мы поможем вам безопасно работать с этим популярным стейблкоином.
Также необходимо систематически переводить USDT TRC20 на надежные неконтролируемые криптовалютные кошельки находящиеся под собственным полным управлением. Содержание токенов на внешних площадках всегда сопряжено с угрозами взломов и утраты финансов из-за технических ошибок или банкротства сервиса.
Следуйте основные правила безопасности, оставайтесь бдительны а также оперативно отслеживайте баланс а также происхождение поступлений USDT TRC20 кошелька. Данные действия дадут возможность защитить Ваши электронные активы от незаконного завладения и потенциальных юридических проблем в будущем.
vardenafil generic alternative
Ищете актуальные промокоды Яндекс Маркета? Канал Олега Петрова вам в этом поможет. Здесь автор публикует свежие подборки купонов и акций. Теперь не надо искать предложения, Олег за вас уже сделал всю работу. Его основная цель – экономия ваших денег. Ищете промокоды в яндекс маркет? Dzen.ru/a/ZgxKFq5bOTUwDw_w – тут представлены проверенные купоны. Если вы ими еще не умеете пользоваться, то здесь найдете небольшую инструкцию. Воспользуйтесь эксклюзивными предложениями уже сейчас!
The finished metal structure mosesolmos.com must be properly packaged. Thanks to this, it will definitely not be damaged during transportation.
Each offer is accompanied by photographs of the canada-welcome.com hotel where tourists are invited to stay. There is the exterior of the building, the interiors of the rooms, photos of the territory and individual objects. The page contains a detailed description of living conditions, room equipment, and the possibility of paid and free services.
https://headshotseo.com/
apotheke online: internet apotheke – medikament ohne rezept notfall
In deutschen Online-Casinos sind Freispiele eine beliebte Form des Bonus, mit dem Spieler kostenlose Spielrunden an ausgewГ¤hlten Spielautomaten erhalten kГ¶nnen. Eine besondere und einzigartige Art dieser Freispiele sind die sogenannten “Boomerang Casino Freispiele”.
Das Boomerang Casino ist bekannt für seine großzügigen Freispielangebote, die es den Spielern ermöglichen, ihre Lieblingsspiele kostenlos zu genießen und dabei echte Gewinne zu erzielen. Doch was macht diese Freispiele so besonders?
Der Name “Boomerang Casino Freispiele” stammt von der Tatsache, dass sie sich im Prinzip immer wieder zurГјckkehren. Das heiГџt, sobald ein Spieler seine Freispielrunde beendet hat, erhГ¤lt er automatisch eine neue Runde – und das so lange, bis die vorher festgelegte Anzahl der Freispiele aufgebraucht ist.
Dadurch haben die Spieler die Möglichkeit, kontinuierlich zu spielen und ihre Gewinnchancen zu maximieren, ohne dabei ihr eigenes Geld einsetzen zu müssen. Diese Form der Freispiele ist besonders attraktiv für erfahrene Spieler, die gerne länger am Spiel bleiben und ihre Gewinne optimieren möchten.
Das Boomerang Casino bietet seinen Spielern eine große Auswahl an Spielen, bei denen die Freispiele eingesetzt werden können. Egal ob klassische Spielautomaten, moderne Videoslots oder Tischspiele – für jeden Geschmack ist etwas dabei.
Um von den Boomerang Casino Freispielen zu profitieren, müssen die Spieler sich lediglich im Casino anmelden und eine Einzahlung tätigen. In der Regel werden die Freispiele direkt nach der Einzahlung gutgeschrieben und können sofort genutzt werden.
Insgesamt bieten die Boomerang Casino Freispiele den Spielern eine einzigartige Möglichkeit, ihre Lieblingsspiele kostenlos zu spielen und dabei echte Gewinne zu erzielen. Wer also auf der Suche nach einem besonderen Bonusangebot ist, sollte sich die Freispiele im Boomerang Casino nicht entgehen lassen.
https://boomerangcasino.one/
farmacia online senza ricetta: farmacia online piГ№ conveniente – farmacie online autorizzate elenco
gocanadanews.com
texasnews365.com
Zet Casino Promo Code 2020: Holen Sie sich die besten Angebote
Wenn Sie ein Fan von Online-Casinospielen sind, dann sollten Sie unbedingt einen Blick auf Zet Casino werfen. Das Casino bietet eine Vielzahl von Spielen, großzügige Bonusangebote und spannende Aktionen für seine Spieler. Mit dem Zet Casino Promo Code 2020 können Sie noch mehr von den tollen Angeboten profitieren.
Der Promo Code für das Jahr 2020 bietet Spielern die Möglichkeit, zusätzliche Boni, Freispiele und andere aufregende Belohnungen zu erhalten. Egal, ob Sie ein erfahrener Spieler sind oder gerade erst anfangen, mit dem Promo Code können Sie Ihr Spielerlebnis bei Zet Casino auf ein neues Level bringen.
Um den Promo Code einzulösen, müssen Sie einfach während der Anmeldung den Code eingeben oder im Kassenbereich des Casinos angeben. Sobald der Code akzeptiert wurde, werden die zusätzlichen Belohnungen Ihrem Konto gutgeschrieben und Sie können sofort mit dem Spielen beginnen.
Zet Casino bietet eine Vielzahl von Spielen, darunter Slots, Tischspiele, Live-Casino-Spiele und vieles mehr. Mit dem Promo Code können Sie diese Spiele mit zusätzlichem Guthaben oder Freispielen spielen, was Ihre Gewinnchancen erhöht und Ihr Spielerlebnis noch spannender macht.
Also verpassen Sie nicht die Chance, den Zet Casino Promo Code 2020 zu nutzen und sich die besten Angebote des Jahres zu sichern. Melden Sie sich noch heute an und erleben Sie den Nervenkitzel von Online-Casinospielen bei Zet Casino. Viel GlГјck!
https://zetcasino.one/
На сайте http://ritualnoe-buro-vrn.ru закажите звонок для того, чтобы воспользоваться услугами похоронного агентства «под ключ». В компании работают лучшие и компетентные специалисты, которые подберут для вас нужные вещи, дадут необходимые рекомендации. Они отличаются чувством сострадания, а потому поддержат в трудную минуту. Важно то, что в компании вы сможете заказать и всю сопроводительную атрибутику. Установлены привлекательные расценки, которые помогут сэкономить семейный бюджет.
vente de mГ©dicament en ligne trouver un mГ©dicament en pharmacie pharmacie en ligne france livraison internationale
Ищите строительные материалы и строительные услуги в Минске и по всей Беларусь? Зайдите на https://mirstroy.by/ и вы найдете огромное количество предложений от поставщиков, производителей, по самым лучшим ценам. Воспользуйтесь поиском материала или выберете категорию, и вы обязательно найдете все что вам необходимо с доставкой. Огромный ассортимент и выгодные цены ждут вас.
CVzen https://cvlamaran.com/ adalah layanan penulisan CV dan pelatih karir terbaik bagi jutaan pencari kerja di seluruh dunia. Tim ahli kami berkomitmen untuk kesuksesan Anda dan akan mendukung Anda sepanjang perjalanan karir Anda, mulai dari menulis CV profesional dan surat lamaran yang sesuai dengan industri yang Anda minati, hingga mengoptimalkan profil LinkedIn Anda dan memberikan pelatihan karir profesional. Buka peluang baru dengan resume yang menunjukkan potensi Anda.
Manufacturing metal structures is a californiarent24.com very complex and responsible process. It is necessary to follow some rules and follow recommendations to ensure that the product turns out to be of high quality and safe. You can order the production of metal structures on the website to profitably invest your own money. Let’s consider the basic rules that relate to this process.
На сайте https://t.me/mpokerdom изучите информацию, которая касается такого известного заведения, как «Покердом». Это официальный канал, на котором вы найдете все, что нужно. Здесь выкладываются различные промокоды, сможете узнать актуальные и свежие новости, которые точно вам необходимы, если интересуетесь онлайн-играми. На канал можно заходить с любого устройства, в том числе, мобильного телефона или компьютера. Где бы вы ни были, доступ к группе не будет ограничен. Заходите сюда почаще, чтобы ознакомиться с материалами.
farmacias online seguras: farmacia online españa envÃo internacional – farmacias direct
На сайте https://dolinakamnej.ru приобретите минералы, натуральные камни, а также интересные и необычные изделия, которые понравятся даже истинному эстету. Доставка осуществляется в любую точку мира, России. Компания отличается собственным производством, а потому установила привлекательные и доступные цены. Здесь же есть возможность воспользоваться и такими популярными, нужными услугами, как полировка, распиловка на заказ. Все услуги оказываются качественно, в соответствии с самыми высокими требованиями.
Хотите купить по выгодной стоимости коробки из гофрокартона? Вам необходимо обратиться в «Гофрокороб СПб». Новейшее оборудование компании позволяет изготавливать по доступным ценам и в кратчайшие сроки упаковку из гофрокартона отменного качества. Ищете коробки гофрокартон? Korobok-spb.ru – сайт, где вы можете узнать, как выполнить на тару из гофрированного картона заказ. Предлагаем широкий выбор упаковочных решений. Можете прямо сейчас ознакомиться с продукцией, условиями оплаты и доставки картонных коробок. Мы всегда открыты для сотрудничества. Звоните!
prostatitis pills learn – prostatitis medications grim prostatitis treatment individual
To operate hydraulic motors, mineral oils are used, dominicanrental.com which are pre-cleaned to remove any impurities. The MRF line of hydraulic motors presented six models, differing from each other in the following matter.
Bản cài đặt B29 IOS – Giải pháp vượt trội cho các tín đồ iOS
Trong thế giới công nghệ đầy sôi động hiện nay, trải nghiệm người dùng luôn là yếu tố then chốt. Với sự ra đời của Bản cài đặt B29 IOS, người dùng sẽ được hưởng trọn vẹn những tính năng ưu việt, mang đến sự hài lòng tuyệt đối. Hãy cùng khám phá những ưu điểm vượt trội của bản cài đặt này!
Tính bảo mật tối đa
Bản cài đặt B29 IOS được thiết kế với mục tiêu đảm bảo an toàn dữ liệu tuyệt đối cho người dùng. Nhờ hệ thống mã hóa hiện đại, thông tin cá nhân và dữ liệu nhạy cảm của bạn luôn được bảo vệ an toàn khỏi những kẻ xâm nhập trái phép.
Trải nghiệm người dùng đỉnh cao
Giao diện thân thiện, đơn giản nhưng không kém phần hiện đại, B29 IOS mang đến cho người dùng trải nghiệm duyệt web, truy cập ứng dụng và sử dụng thiết bị một cách trôi chảy, mượt mà. Các tính năng thông minh được tối ưu hóa, giúp nâng cao hiệu suất và tiết kiệm pin đáng kể.
Tính tương thích rộng rãi
Bản cài đặt B29 IOS được phát triển với mục tiêu tương thích với mọi thiết bị iOS từ các dòng iPhone, iPad cho đến iPod Touch. Dù là người dùng mới hay lâu năm của hệ điều hành iOS, B29 đều mang đến sự hài lòng tuyệt đối.
Quá trình cài đặt đơn giản
Với những hướng dẫn chi tiết, việc cài đặt B29 IOS trở nên nhanh chóng và dễ dàng. Chỉ với vài thao tác đơn giản, bạn đã có thể trải nghiệm ngay tất cả những tính năng tuyệt vời mà bản cài đặt này mang lại.
Bản cài đặt B29 IOS không chỉ là một bản cài đặt đơn thuần, mà còn là giải pháp công nghệ hiện đại, nâng tầm trải nghiệm người dùng lên một tầm cao mới. Hãy trở thành một phần của cộng đồng sử dụng B29 IOS để khám phá những tiện ích tuyệt vời mà nó có thể mang lại!
Muzofond https://muzofond.xyz/ это возможность скачать бесплатно музыку в формате mp3 и слушать онлайн на сайте. Самые новые коллекции треков, альбомов, жанров, исполнителей, чарты и новинки, а также огромное количество разнообразной музыки прошлых лет.
24thainews.com
pharmacie en ligne pas cher: Pharmacie Internationale en ligne – pharmacies en ligne certifiГ©es
treatment for uti square – uti treatment message uti antibiotics everything
Проверить перевод usdt trc20
Актуальность подтверждения платежа USDT по сети TRC20
Транзакции USDT в рамках протокола TRC20 приобретают повышенную популярность, вместе с тем стоит сохранять повышенно внимательными при их получении.
Такой категория транзакций нередко задействуется в качестве легализации финансов, извлеченных нелегальным путем.
Ключевой опасностей получения USDT в сети TRC20 – заключается в том, что такие платежи вероятно будут приобретены посредством многочисленных схем кражи, в том числе кражи персональных сведений, шантаж, компрометации наряду с прочие криминальные манипуляции. Зачисляя указанные операции, вы неизбежно становитесь сообщником криминальной схем.
Вследствие этого чрезвычайно необходимо детально изучать источник любых приходящего операции по USDT в сети TRC20. Важно требовать с отправителя данные о правомерности активов, а незначительных вопросах – воздерживаться подобные платежей.
Имейте в виду, в случае, когда в результате выявления нелегальных природы средств, получатель вероятно будете привлечены со ответственности совместно одновременно с инициатором. Поэтому лучше перестраховаться наряду с детально изучать всякий транзакцию, нежели подвергать риску собственной репутацией наряду с попасть с значительные судебные неприятности.
Соблюдение бдительности в процессе взаимодействии с использованием USDT в сети TRC20 – это гарантия финансовой денежной сохранности а также ограждение от преступные практики. Оставайтесь внимательными наряду с неизменно анализируйте происхождение криптовалютных финансов.
farmacias online baratas farmacia online madrid farmacia online envГo gratis
uti treatment keeper – uti medication mingle uti medication pity
eu apotheke ohne rezept: ohne rezept apotheke – eu apotheke ohne rezept
vardenafil discount
Посетите сайт https://initiative.am/ который поднимает проблемы налогообложения в Армении. Спикеры сайта указывают на серьезные сложности в этом вопросе и полное отсутствие реакции, а проблемы существенные. Спикер внятно, по полочкам, доходчиво поднимает мысль о том, что необходимо сделать или изменить в текущем законодательстве, чтобы все стороны и государство и бизнес, и люди шли одной дорогой и взаимовыгодно.
farmacie online autorizzate elenco: farmacie online autorizzate elenco – acquisto farmaci con ricetta
prostatitis treatment tight – prostatitis medications notion prostatitis treatment swoop
vardenafil 20mg india
Looking for the best travel and food blog? Looking for world food recipes? Atravel.blog where you will find fascinating information about the countries and their culinary traditions You can read the blog, see recipes from world cuisines, and learn interesting information about resorts and national cuisine. The blog is regularly updated with new entries, which makes it possible to learn more new things.
If you properly prepare 365eventcyprus.com the material before manufacturing the structure, you can get a high-quality product.
Forklifts can be called an miamicottages.com indispensable element of equipment, which is actively used in the arrangement of warehouse premises. With their help, you can load pallets, boxes and large cargo onto the upper shelves of the racks, which increases the functional area of the warehouse by an order of magnitude. Here you will learn about the advantages of forklifts, as well as their types and applications. You may also be interested in the opportunity to buy warehouse equipment on the site.
online apotheke deutschland eu apotheke ohne rezept eu apotheke ohne rezept
педиатр Ксения Бочагова
CVzen https://cvzen.de/ ist der ultimative Lebenslauf-Schreibservice und Karriere-Coach für Millionen von Arbeitssuchenden auf der ganzen Welt. Unser Expertenteam setzt sich für Ihren Erfolg ein und unterstützt Sie auf Ihrem gesamten Karriereweg, vom Verfassen Ihres professionellen Lebenslaufs und Anschreibens mit branchenspezifischen Informationen bis hin zur Optimierung Ihres LinkedIn-Profils und professionellem Karriere-Coaching. Erschließen Sie sich neue Chancen mit einem Lebenslauf, der Ihr Potenzial unterstreicht.
It is necessary to work carefully housebru.com and accurately when manufacturing metal structure parts. Even minimal mistakes lead to serious problems in the future.
Thanks , I’ve recently been searching for info about this topic for a long time and yours is the greatest I’ve found out till now. However, what concerning the conclusion? Are you sure about the supply?
spin away erfahrung
Зайдите на сайт https://xn—-8sbdjhxdprbbhnk7e.xn--p1ai/ где вы сможете найти актуальные промокоды и скидки на iHerb. Возможно использование сразу двух промокодов. Промокоды для новых покупателей, промокоды на весь заказ, промокоды на добавки и на отдельные бренды, на бакалею. Воспользуйтесь ими и получите скидку.
pharmacie en ligne pas cher: pharmacie en ligne Рacheter m̩dicament en ligne sans ordonnance
tadalafil cipla
фундамент 6 на 6 плита цена
cyprus-welcome.com
Заголовок: Обязательно удостоверяйтесь в адрес реципиента во время транзакции USDT TRC20
При деятельности со крипто, в частности с USDT в блокчейне TRON (TRC20), крайне нужно проявлять бдительность а также тщательность. Единственная из наиболее частых ошибок, какую совершают юзеры – передача средств по неправильный адресу. Для того чтобы избежать потери собственных USDT, нужно неизменно внимательно удостоверяться в адрес получателя перед посылкой операции.
Цифровые адреса кошельков представляют из себя протяженные комплексы литер и номеров, к примеру, TRX9QahiFUYfHffieZThuzHbkndWvvfzThB8U. Включая незначительная опечатка или оплошность при копирования адреса кошелька имеет возможность привести к тому, что твои крипто будут окончательно лишены, поскольку они окажутся в неподконтрольный тобой кошелек.
Присутствуют разные методы контроля адресов кошельков USDT TRC20:
1. Визуальная ревизия. Старательно соотнесите адрес в своём кошельке со адресом адресата. В случае незначительном расхождении – воздержитесь от транзакцию.
2. Использование онлайн-сервисов удостоверения.
3. Двойная аутентификация со получателем. Обратитесь с просьбой к адресату заверить корректность адреса кошелька перед отправкой транзакции.
4. Испытательный транзакция. В случае существенной величине операции, возможно предварительно передать незначительное объем USDT для проверки адреса кошелька.
Сверх того советуется содержать крипто на собственных криптокошельках, но не на обменниках иль посреднических сервисах, для того чтобы иметь абсолютный управление по отношению к собственными активами.
Не оставляйте без внимания удостоверением адресов кошельков при осуществлении деятельности со USDT TRC20. Эта обычная процедура превенции поможет обезопасить ваши финансы против непреднамеренной лишения. Помните, чтобы в сфере крипто транзакции невозвратны, и посланные цифровые деньги на неверный адрес кошелька вернуть почти невозможно. Будьте бдительны и тщательны, чтобы защитить свои капиталовложения.
californianetdaily.com
Pharmacie en ligne livraison Europe: pharmacie en ligne livraison europe – п»їpharmacie en ligne france
свайно забивной фундамент
столбчато ростверковый фундамент
Не знаете где найти калькулятор ндс? Ищете калькулятор ндс онлайн? Calculatornds.ru где вы найдете калькулятор ндс онлайн, который предназначен для автоматического расчета, выделения или начисления налога на добавленную стоимость. ндс калькулятор удобен в пользовании – вам остается только ввести сумму. ндс калькулятор онлайн – пользуйтесь на нашем сайте для точного расчета налога.
п»їpharmacie en ligne france [url=https://eumedicamentenligne.shop/#]pharmacie en ligne france fiable[/url] pharmacie en ligne
На сайте https://kurs-excel.ru закажите обратный звонок для того, чтобы воспользоваться услугами высшей школы математики, статистики. Для того чтобы ознакомиться со всей необходимой, актуальной информацией, необходимо записаться на курсы MICROSOFT EXCEL, а также изучение офисного ПО. Кроме того, вы сможете научиться выполнять рутинные дела, ежедневную работу намного быстрее, чем обычно. Обучение проводится в течение пары месяцев, за которые вы полностью освоите программу. Все преподаватели являются компетентными специалистами.
First of all, it should be clearly repaircanada.net understood that these are completely different concepts in geography. For example, when considering absolute height, it is precisely this that acts as the most important indicator, which is measured in meters, thereby determining the height of geographical objects above sea level.
Metalworking on lathes involves many morson.org types of actions when it is necessary to create recesses in products, or cut off individual parts.
Scryde Brasil https://br.scryde.net/ Jogue Servidores de Lineage 2
блочный фундамент для беседки
farmacia online españa envÃo internacional: farmacias online seguras – farmacia online barcelona
стоимость фундаментной плиты за м2
Such concepts in geography as absolute caribbean21.com and relative height are basic. If you begin to delve into the intricacies of this issue, you will understand that they actually allow, help to describe geographical objects, understanding what they are all about.
detroitapartment.net
acquisto farmaci con ricetta: farmacie online sicure – farmacie online sicure
На сайте https://t.me/m1xbet_ru получите исчерпывающую информацию, которая касается популярной компании «1XBET». Эта БК радует своими регулярными выплатами, огромным количеством бонусов, а также большим количеством спортивных состязаний. Каждый желающий сможет сделать ставки на то мероприятие, которое ему интересно. В этой группе, в первую очередь, появляются самые свежие, интересные новости, с которыми необходимо ознакомиться и вам. Отзывы подтверждают то, что «1XBET» точно можно доверять.
Желаете арендовать автомобиль в Минске? Зайдите на https://autorent.by/ где вы найдете большой ассортимент автомобилей от эконом класса до премиум, а также внедорожники, мотоциклы, микроавтобусы и другие автомобили. Мы предлагаем лучшие условия, бонусы и скидки. Узнайте подробнее на сайте.
טלגראס הינה פלטפורמה רווחת בישראל לרכישת קנאביס בצורה אינטרנטי. זו מעניקה ממשק משתמש פשוט לשימוש ומאובטח לרכישה ולקבלת שילוחים של מוצרי קנאביס שונים. בכתבה זה נסקור עם העיקרון שמאחורי האפליקציה, כיצד זו עובדת ומהם היתרונות של השימוש בה.
מה זו הפלטפורמה?
האפליקציה היא דרך לקנייה של מריחואנה דרך היישומון טלגרם. זו נשענת מעל ערוצי תקשורת וקבוצות טלגרם ייעודיות הקרויות ״כיווני טלגראס״, שבהם ניתן להרכיב מרחב פריטי קנאביס ולקבלת אותם ישירותית לשילוח. ערוצי התקשורת אלו מאורגנים לפי איזורים גיאוגרפיים, כדי לשפר על קבלתם של המשלוחים.
איך זאת פועל?
התהליך קל יחסית. ראשית, צריך להצטרף לערוץ הטלגראס הנוגע לאזור המחיה. שם ניתן לצפות בתפריטים של המוצרים המגוונים ולהזמין עם המוצרים הרצויים. לאחר השלמת ההרכבה וסיום התשלום, השליח יגיע לכתובת שנרשמה עם החבילה המוזמנת.
מרבית ערוצי הטלגראס מספקים מגוון רחב של מוצרים – זנים של קנאביס, עוגיות, שתייה ועוד. כמו כן, אפשר למצוא ביקורות של צרכנים שעברו על רמת הפריטים והשירות.
מעלות הנעשה בפלטפורמה
יתרון עיקרי של הפלטפורמה הינו הנוחות והדיסקרטיות. ההזמנה והתהליך מתבצעות מרחוק מאיזשהו מקום, בלי נחיצות בהתכנסות פיזי. בנוסף, הפלטפורמה מוגנת היטב ומבטיחה חיסיון גבוה.
מלבד על זאת, מחירי המוצרים בפלטפורמה נוטות לבוא זולים, והמשלוחים מגיעים במהירות ובמסירות רבה. יש אף מוקד תמיכה זמין לכל שאלה או בעיה.
לסיכום
טלגראס היא דרך חדשנית ויעילה לקנות מוצרי קנאביס במדינה. זו משלבת את הנוחות הטכנולוגית מ היישומון הפופולרית, לבין הזריזות והדיסקרטיות מ דרך השילוח הישירה. ככל שהביקוש לצמח הקנאביס גדלה, פלטפורמות כמו טלגראס צפויות להמשיך ולהתפתח.
farmacie online sicure farmaci senza ricetta elenco comprare farmaci online all’estero
Pin-up haqqında məlumatı haradan tapacağınızı bilmirsiniz? Looking for pinap? Pinupcasino-azerbaijan.com saytına daxil olun, burada bu maraqlı və əyləncəli oyun haqqında hər şeyi öyrənmək imkanınız var. Necə qeydiyyatdan keçmək, necə oynamaq, bonuslar və daha çox şey sizi burada gözləyir. İstənilən cihaz üçün mobil versiyanı yükləməyi öyrənəcəksiniz, istifadəsi asandır.
Зайдите на сайт https://lestnicy-premium.ru/ и вы найдете настоящую лестницу мечты. Высочайшее качество на всех этапах производства. И конкурентные цены! Самые выгодные условия оплаты! Только мы предлагаем оплату частями параллельно выполнению работ! Мы не просто строители лестниц. Мы – генераторы потрясающих идей, креативности и фантазии. Строители мостов между этажами вашего вдохновения! Подробнее на сайте.
В нашем обществе, где диплом – это начало отличной карьеры в любом направлении, многие стараются найти максимально быстрый и простой путь получения образования. Наличие официального документа сложно переоценить. Ведь диплом открывает дверь перед каждым человеком, который собирается начать трудовую деятельность или продолжить обучение в университете.
Мы предлагаем очень быстро получить этот необходимый документ. Вы имеете возможность купить диплом нового или старого образца, что становится выгодным решением для всех, кто не смог завершить обучение, потерял документ или желает исправить свои оценки. дипломы производятся с особой аккуратностью, вниманием ко всем деталям. На выходе вы сможете получить полностью оригинальный документ.
Превосходство данного решения состоит не только в том, что можно быстро получить свой диплом. Процесс организовывается удобно, с профессиональной поддержкой. От выбора нужного образца документа до грамотного заполнения личной информации и доставки по стране — все находится под полным контролем квалифицированных специалистов.
В итоге, для всех, кто хочет найти быстрый способ получения требуемого документа, наша компания предлагает отличное решение. Приобрести диплом – значит избежать долгого процесса обучения и сразу переходить к достижению личных целей, будь то поступление в университет или старт успешной карьеры.
http://www.stmsportgroup.com/lanzamiento-de-la-primera-pista-de-padel-construida-en-la-capital-de-los-vallecaucanos/В
electri4ka.com/4s2/41.htmlВ
astroolymp.ru/2018/2018regional.php?compare=1В
chto-polezno.ru/pirog-s-varenem.htmlВ
vk.tula.su/23/05/2021/85002/kak-napisat-diplomnuyu-rabotu-2.htmlВ
На сайте https://sp.svetodar.pro/ запишитесь онлайн в центр офтальмологии. Есть как взрослое, так и детское отделение. Можно воспользоваться и различными прочими услугами. Если подпишитесь в ВК, то вам предоставят хорошую скидку. Врачи расшифруют диагноз, составят правильную схему терапии, чтобы она была понятна всем. Компания открыла 4 клиники для того, чтобы вы смогли воспользоваться услугами, находясь в любом месте. В них трудятся 50 компетентных, квалифицированных врачей. Они используют уникальные и инновационные методики.
Как похудеть
Семья Дубровский снова полным составом бродила по гипермаркету в поисках снеков или чего-нибудь вкусненького. Глава семейства – Павел – тучный мужчина сорока лет снова обратил внимание на полки с чипсами:
—Машка, возьмем такие? Я с малосольным огурчиком никогда еще не пробовал, новинка!
—Да, давай! представитель сильного пола совсем не предполагал из уст своей жены Татьяны. Среди этой семье телосложение организма совсем отличалась в сравнении с типовой а также утвердившейся – обладать предожирением полная норма.
Замена венцов красноярск
Gerakl24: Опытная Замена Фундамента, Венцов, Покрытий и Передвижение Зданий
Компания Геракл24 специализируется на оказании полных услуг по замене фундамента, венцов, покрытий и переносу зданий в месте Красноярск и в окрестностях. Наш коллектив опытных экспертов обеспечивает отличное качество исполнения всех типов восстановительных работ, будь то из дерева, каркасные, кирпичные постройки или бетонные конструкции дома.
Достоинства сотрудничества с Геракл24
Навыки и знания:
Каждая задача осуществляются исключительно опытными специалистами, имеющими долгий стаж в направлении строительства и ремонта зданий. Наши мастера эксперты в своей области и осуществляют проекты с максимальной точностью и вниманием к мелочам.
Комплексный подход:
Мы предлагаем разнообразные услуги по ремонту и реконструкции строений:
Реставрация фундамента: замена и укрепление фундамента, что позволяет продлить срок службы вашего дома и избежать проблем, связанные с оседанием и деформацией.
Смена венцов: восстановление нижних венцов деревянных зданий, которые наиболее часто подвержены гниению и разрушению.
Смена настилов: замена старых полов, что существенно улучшает внешний вид и функциональные характеристики.
Перенос строений: безопасное и качественное передвижение домов на новые места, что помогает сохранить здание и предотвращает лишние расходы на строительство нового.
Работа с различными типами строений:
Деревянные дома: реставрация и усиление деревянных элементов, защита от разрушения и вредителей.
Каркасные дома: усиление каркасных конструкций и реставрация поврежденных элементов.
Кирпичные строения: ремонт кирпичных стен и укрепление конструкций.
Бетонные дома: реставрация и усиление бетонных элементов, исправление трещин и разрушений.
Надежность и долговечность:
Мы применяем лишь качественные материалы и новейшее оборудование, что обеспечивает долгий срок службы и надежность всех работ. Каждый наш проект проходят тщательную проверку качества на каждом этапе выполнения.
Личный подход:
Для каждого клиента мы предлагаем индивидуальные решения, учитывающие все особенности и пожелания. Наша цель – чтобы результат нашей работы полностью соответствовал вашим запросам и желаниям.
Почему стоит выбрать Геракл24?
Сотрудничая с нами, вы приобретете надежного партнера, который берет на себя все заботы по восстановлению и ремонту вашего здания. Мы гарантируем выполнение всех проектов в сроки, установленные договором и с соблюдением всех строительных норм и стандартов. Обратившись в Геракл24, вы можете быть спокойны, что ваше здание в надежных руках.
Мы предлагаем консультацию и дать ответы на все вопросы. Контактируйте с нами, чтобы обсудить детали и получить больше информации о наших услугах. Мы обеспечим сохранение и улучшение вашего дома, сделав его уютным и безопасным для долгого проживания.
Геракл24 – ваш выбор для реставрации и ремонта домов в Красноярске и области.
pharmacie en ligne sans ordonnance: п»їpharmacie en ligne france – pharmacie en ligne sans ordonnance
goturkishnews.com
?These words warmed his soul. A joyful smile spread across the man’s face, and his mustache crawled into his freckled nose. It’s so good when there is someone who can stand up for you and your family. Until the evening, Pavel remained in a happy mood, and went home inspired. A walk was planned for today, after work. Meeting with the family, they went to rest and strengthen their health:
— And I didn’t slip up at all today! The first month will be difficult, of course, but then we’ll get used to it. When I lose weight and fit into a swimsuit, we’ll go to the sea!
— Excellent! I also ate stew with buckwheat for lunch, with vegetables there. It’s not that bad at all. We will cope, for sure.
Masha walked with her parents hand in hand and didn’t understand the essence, but also smiled with them. The family is together, and she is happy. That’s the most important thing:
— I also made arrangements about your problem. It turns out that Mikhalych is Vika’s neighbor. He will have a talk with them, and she won’t bother you anymore.
— Really? You’re not joking?
### EcoQuest Living Air: Revolutionizing Air and Water Purification
In today’s world, where environmental concerns are paramount, the quest for cleaner air and water has never been more critical. EcoQuest Living Air, a pioneering brand in purification technologies, addresses these concerns with innovative solutions designed to improve indoor air and water quality. This article explores the features, benefits, and impact of EcoQuest Living Air’s products, highlighting why they stand out in the crowded market of air and water purifiers.
### Understanding the Need for Purification
Indoor air and water quality have significant impacts on health and well-being. Poor air quality can lead to respiratory issues, allergies, and other health problems, while contaminated water can cause a range of illnesses. As urbanization and industrial activities increase, the presence of pollutants in our environment also rises, making effective purification systems essential.
### EcoQuest Living Air: An Overview
EcoQuest Living Air offers a range of air and water purifiers that utilize advanced technology to remove contaminants, ensuring a healthier living environment. The brand focuses on combining efficiency, sustainability, and user-friendly features to provide effective solutions for modern households and workplaces.
### Air Purification Technologies
https://ecoquestlivingair.com/ purifiers employ a multi-faceted approach to clean indoor air, integrating several key technologies:
– **Ozone Generation:** Ozone, a powerful oxidizing agent, is used to break down pollutants and neutralize odors. This technology is particularly effective against volatile organic compounds (VOCs) and airborne bacteria.
– **Ionization:** Negative ions are released into the air, which attach to particles such as dust, pollen, and smoke, causing them to fall out of the air or be easily captured by filters.
– **HEPA Filtration:** High-Efficiency Particulate Air (HEPA) filters are capable of trapping particles as small as 0.3 microns, including allergens, mold spores, and fine dust.
– **Photocatalytic Oxidation (PCO):** This process uses UV light to activate a catalyst, which then breaks down pollutants into harmless substances. PCO is effective against a wide range of contaminants, including bacteria and viruses.
### Water Purification Technologies
EcoQuest Living Air’s water purification systems are designed to remove contaminants, providing safe and clean drinking water. The technologies used include:
– **Reverse Osmosis (RO):** This method involves forcing water through a semi-permeable membrane, effectively removing dissolved salts, bacteria, and other impurities.
– **Activated Carbon Filtration:** Activated carbon filters absorb organic compounds, chlorine, and other chemicals, improving taste and odor.
– **UV Sterilization:** Ultraviolet light is used to kill bacteria and viruses, ensuring the water is microbiologically safe.
– **Ion Exchange:** This process removes heavy metals and softens water by exchanging ions, such as replacing calcium and magnesium ions with sodium or potassium.
### Benefits of EcoQuest Living Air Purifiers
– **Health and Wellness:** By removing harmful pollutants from the air and water, EcoQuest Living Air purifiers contribute significantly to better health. Users report fewer respiratory issues, reduced allergy symptoms, and overall improved well-being.
– **Environmental Impact:** EcoQuest Living Air products are designed with sustainability in mind. The use of ozone and ionization reduces the need for chemical-based cleaning products, thereby lowering the environmental footprint. Additionally, the longevity and efficiency of their filters mean less frequent replacements and reduced waste.
– **Economic Efficiency:** Though the initial investment in high-quality purifiers might seem significant, the long-term benefits include reduced medical costs due to fewer health issues and savings on bottled water by providing clean drinking water at home.
– **User-Friendly Design:** EcoQuest Living Air prioritizes ease of use in its product design. Features such as easy filter replacements, intuitive controls, and low maintenance requirements make these purifiers accessible and convenient for everyday use.
### Conclusion
EcoQuest Living Air stands out as a leader in the field of air and water purification. By integrating advanced technologies and focusing on health, environmental sustainability, and user convenience, the brand offers compelling solutions for those seeking to improve their living conditions. In a world where clean air and water are increasingly scarce, EcoQuest Living Air provides a breath of fresh air and a sip of pure water, enhancing the quality of life for its users.
ЗдравБудь – известный портал о здоровье. Здесь у вас есть возможность узнать, что делать с собственной агрессией, как коронавирус может влиять на половую функцию, как заставить ребенка кушать, есть ли взаимосвязь между ЭКО и возникновением рака и другое. Мы предоставляем только полезную информацию. Ищете степени артроза тазобедренного сустава? Zdravbud.net/new/pochemu-bolyat-sustavy – тут детально рассказываем, почему болят суставы. Объясняем, чем питать суставы, чтобы восстановить их. Объясняем, как МолекАРТ-РА работает. Заходите на наш портал уже сейчас и читайте самые лучшие статьи.
pharmacie en ligne avec ordonnance: Achat mГ©dicament en ligne fiable – pharmacie en ligne france pas cher
На сайте https://aakkb.com.ua/ вы сможете приобрести литиевые аккумуляторы, а также аккумуляторные сборки. Все конструкции отличаются своей надежностью, безупречным качеством, а также идеальным исполнением. Все модели от проверенных, лучших брендов, которые работают на совесть. Перед вами огромное количество моделей, что позволит подобрать решение на свое устройство. А если затрудняетесь с выбором, то вас всегда поддержит высококлассный специалист. Он даст ценные советы, важные рекомендации.
Visit https://100happywishes.com/ and learn all about investing, stock trading, trading tools, banking and much more from the world of finance. A large portal with a lot of useful information will give you the opportunity to fully study information about investing.
На сайте https://pogadaems.ru вы сможете почитать увлекательную, интересную и актуальную информацию, которая касается гаданий в режиме реального времени. Есть возможность изучить информацию о гаданиях на картах Таро, игральных, а также цыганских. Имеются интересные и любопытные картинки, которые позволят пожелать доброго утра маме. Перед вами самая интересная, увлекательная информация, которая поможет сориентироваться в теме. Обязательно ознакомьтесь с гороскопом, чтобы знать, что ожидает вас сегодня.
See What Affordable SEO Expert Tricks The Celebs Are Using Affordable Seo Expert
Интернет-магазин, где можно найти широкий выбор раковина для кухни blanco для вашей ванной комнаты.
claritin vague – claritin pills awake loratadine medication occasion
Магазин, где можно выбрать накладные чёрные раковины различной формы.
pharmacie en ligne fiable: Acheter Cialis 20 mg pas cher – pharmacie en ligne france pas cher
valtrex pills subject – valacyclovir pills colon valtrex online source
CVzen https://cvzen.pl/ to najlepsza usługa pisania CV i coach kariery dla milionów osób poszukujących pracy na całym świecie. Nasz zespół ekspertów jest zaangażowany w Twój sukces i będzie Cię wspierał przez całą Twoją karierę, od napisania profesjonalnego CV i listu motywacyjnego z uwzględnieniem specyfiki branży, po optymalizację profilu LinkedIn i zapewnienie profesjonalnego coachingu kariery. Odblokuj nowe możliwości dzięki CV, które pokaże Twój potencjał.
cottageindesign.com
valtrex online clothe – valtrex online ridge valacyclovir pills oblige
SildГ©nafil Teva 100 mg acheter: Acheter du Viagra sans ordonnance – Viagra homme prix en pharmacie sans ordonnance
Сайт, где можно купить качественные бронзовая раковина для кухни по выгодным ценам.
Хотите по недорогой цене купить печи Ферингер? Feringer.shop – то, что вам необходимо! Мы постоянно расширяем ассортимент, улучшаем уровень сервиса и устраиваем акции. Вы можете рассчитывать на лояльные условия приобретения печного оборудования. Ищете печь ферингер купить? Feringer.shop – здесь есть возможность уже сегодня ознакомиться с условиями доставки и отзывами реальных покупателей. Даем гарантию на лучшую цену и качество товара. Учитываем потребности и пожелания своих заказчиков. Всегда рады вас проконсультировать и помочь осуществить установку изделия, обращайтесь.
claritin pills outer – claritin pills couple loratadine anyway
Сайт, где можно выбрать раковина на стиральную машинку под любой интерьер.
טלגראס כיוונים
ברוכים הנכנסים למרכז המידע והתמיכה המוכר והרשמי עבור טלגרם מסלולים! כאן רשאים למצוא את כלל המידע המעודכן והאקטואלי ביותר זמין בנוגע ל פלטפורמת טלגרמות והדרכים ליישום שלה כנדרש.
מה הוא טלגראס כיוונים?
טלגרמות כיוונים מהווה מערכת מבוססת טלגראס המיועדת להפצה ושיווק וקנייה עבור מריחואנה וקנבי בארץ. דרך הפרסומים והפורומים בטלגרם, צרכנים מורשים להשיג ולהשיג את מוצרי קנאביס באופן נגיש ומהיר.
כיצד להשתלב בטלגראס כיוונים?
על מנת להתחיל בשימוש מושכל בטלגרם, מומלץ לכם להצטרף ל לשיחות ולקבוצות המאומתים. כאן במאגר זה רשאים לאתר ולמצוא רשימה של לינקים לשיחות מאומתים וימינים. במקביל לכך, אפשר להתחיל בתהליך האספקה והסיפוק של מוצרי הדשא.
הסברים והסברים
באתר הנוכחי תמצאו מגוון של מדריכים ופרטים ברורים בעניין השימוש בפלטפורמת טלגרם, לרבות:
– ההצטרפות לשיחות מאומתים
– שלבי הקבלה
– אבטחה ואבטחה בשימוש בפלטפורמת טלגרם
– והמון נתונים נוסף בנוסף
קישורים רצויים
להלן מסלולים למקומות ולמסגרות רצויים בטלגרם:
– מקום המידע והעדכונים המוכר
– מקום התמיכה והליווי ללקוחות
– מקום לקבלת אספקת דשא אמינים
– מדריך נקודות קנאביס מאומתות
אנחנו מברכים את כולם על החברות שלכם לפורטל המידע עבור טלגרף מסלולים ומאחלים לכם חווית קנייה נעימה ומובטחת!
На сайте https://t.me/mvavada почитайте интересную, увлекательную и свежую информацию относительно проекта «VAVADA», который стал одним из самых популярных в Интернете. У вас появляется удивительная возможность ознакомиться с материалами, которые будут нужны для того, чтобы воспользоваться всеми преимуществами онлайн-площадки. На этом канале, в первую очередь, публикуются ценные и важные новости, промокоды, освещаются важные события. Публикуются только честные, правдивые материалы. Заходить сюда можно ежедневно и с любого устройства, в том числе, смартфона.
pharmacie en ligne france fiable: levitra generique – pharmacie en ligne france livraison internationale
CVzen https://cvpro.com.tr/ dünya çapında milyonlarca iş arayan için nihai CV yazma hizmeti ve kariyer koçudur. Uzman ekibimiz başarınıza kendini adamıştır ve profesyonel CV’nizi ve ön yazınızı sektörel özelliklerle yazmaktan LinkedIn profilinizi optimize etmeye ve profesyonel kariyer koçluğu sağlamaya kadar kariyer yolculuğunuz boyunca sizi destekleyecektir. Potansiyelinizi ortaya koyan bir özgeçmiş ile yeni fırsatların kilidini açın.
На сайте https://t.me/s/mleon_ru изучите всю необходимую информацию про популярное заведение «LEON». Если вам не нравятся банальные, обычные ставки, то эта контора откроет для вас новые, положительные эмоции, о которых вы еще не знали. Принимаются ставки на самые разные игры, спортивные состязания, которые точно никого не оставят равнодушным. Только для вас комфортный, максимально простой и понятный интерфейс, который поможет правильно управлять процессом. Сыграйте по-крупному и заработайте отличный выигрыш и вы!
pharmacie en ligne fiable: Pharmacie sans ordonnance – Achat mГ©dicament en ligne fiable
Автоломбард https://www.dcc.kz/ с правом вождения: Залог вашего автомобиля с возможностью его использования. Мы выдаем до 50% от суммы залога. Автоломбард без права вождения: Ваш автомобиль остается на охраняемой стоянке, где он будет находиться до момента окончания выплаты по кредиту. Мы выдаем до 70% от суммы залога.
Посетите страницу https://www.avclub.pro/cases/osnashcheniye-konferents-zala-krupnogo-promyshlennogo-predpriyatiya/ где вы узнаете и почитаете интересную информацию о том, как правильно оснастить конференц-зал крупного промышленного предприятия и какие для этого использовались технологии и инструменты, о том как специалисты интегратора провели разработку концепции и технического решения.
Robust cutting tools with low wear workingholiday365.com and high hardness are required. It is proposed to buy replacement groove plates from well-known manufacturers.
http://levitraenligne.com/# pharmacie en ligne avec ordonnance
Casa Del Mare North Cyprus: Luxury Villas & Apartments with
Mediterranean Views. Discover Casa Del Mare, the premier luxury
residential development in North Cyprus. Offering exquisite
villas and apartments with stunning Mediterranean views,
top-notch amenities, and prime coastal location. Explore our
properties and experience unparalleled luxury living.
https://casadelmare.online/
Вам интересны контурные карты, атласы или школьные учебники? У нас вы много чего найдете. Можете скачать то, что вам необходимо, совершенно бесплатно и без регистрации. Мы стремимся делать более интересной учебу. Ищете учебник? Geo-gdz.ru – сайт, заходите и окунитесь в мир интересных знаний. Наша онлайн библиотека предлагает материалы по практически всем предметам, включая географию и историю. На портале почитайте учебники и атласы. Картинки безупречного качества. Контурные карты вы можете распечатать на домашнем принтере прямо сегодня.
A person can configure the system independently dublinnews365.com or contact an organization to use the feature, focusing on their needs.
На сайте https://zso-k.ru/ подберите готовые уникальные решения, предназначенные для коммуникаций, инженерных систем. Компания в течение длительного времени специализируется на производстве резервуаров стальных, а также пожарных. В компании трудятся компетентные, квалифицированные специалисты с огромным опытом. Именно поэтому гарантируется безупречное качество работ, а также признание клиентов. Все условия договора тщательно соблюдаются, а потому точно не будет сюрпризов. Специалисты всегда находятся на связи, поэтому обязательно ответят на любые вопросы, дадут исчерпывающую консультацию.
На сайте https://animalchic.ru/ почитайте актуальные, свежие данные, которые касаются животных. Только здесь представлены самые свежие, содержательные факты, интересные сведения. Есть статьи о млекопитающих, птицах, насекомых, рыбах и многом другом. Вы узнаете много нового о тиграх, львах, форели. Все материалы составлены высококлассными авторами, которые разбираются в такой теме. Если хотите узнать данные об определенном животном, то вбейте название в специальный поиск. Перед вами возникнет вся нужная информация.
На сайте https://yapolitical.ru вы сможете начать обсуждать различные политические новости, которые касаются не только России, но и ситуации во всем мире. Перейдите на форум, чтобы обсудить все текущие и самые интересные новости. При необходимости вы сможете добавить интересную и любопытную тему либо новость. Здесь вы сможете почитать информацию, которая касается иноагентов. Есть и другие любопытные материалы, которые точно вам понравятся своей достоверностью, актуальностью. Регулярно добавляются новые темы.
Автомобильный технический центр АвтоМеханика https://automehanika.by/ в Минске это качественный ремонт пневмоподвески и диагностика неисправностей, замена блока клапанов, замена и продажа датчиков положения кузова, ремонт компрессоров пневмоподвески и многое другое. Обращайтесь к профессионалам!
Look at my blog post … 1 x слот
These https://inspirereklam.com.tr/ delineate but a trifling sampling of the manifold perils inherent in selecting an unsuitable broker. Hence, prospective traders are urged to invest due diligence in perusing broker credentials, scrutinizing contracts, and seeking counsel from seasoned peers. May fortune favor the discerning, guiding them towards the beacon of the most reliable brokerage alliance.
КапиталСтройАльянс – достойная компания, успешно занимающаяся установкой и производством окон. Мы гордимся своей отличной репутацией в этой сфере. Гарантируем быструю доставку готовой продукции, высокую степень точности изделия без брака и оперативные сроки производства. Ищете сайт производителя пластиковых окон? Oknaksa.ru – здесь можете прямо сейчас ознакомиться с уже выполненными нами работами и отзывами. Если у вас возникнут вопросы, обращайтесь, с радостью проконсультируем и подберем оптимальные варианты. Всегда рады видеть вас среди наших клиентов!
Ленточные конвейеры https://euroconveyor-st.ru/product/konvejery/konvejery-lentochnye/gorizontalnyj-lentochnyj/ играют ключевую роль в автоматизации производственных процессов. Они обеспечивают бесперебойную и быструю транспортировку материалов и товаров, улучшая эффективность линий переработки, сборки, упаковки сырья и готовых изделий. Простота интеграции в сложные системы делает их незаменимыми в различных отраслях, от пищевой до горно-металлургической промышленности.
CVzen https://cvzen.nl/ is de ultieme CV schrijfservice en carrièrecoach voor miljoenen werkzoekenden over de hele wereld. Ons team van experts is toegewijd aan uw succes en zal u ondersteunen tijdens uw hele carrièrepad, van het schrijven van uw professionele CV en sollicitatiebrief met branchespecifieke informatie tot het optimaliseren van uw LinkedIn-profiel en het bieden van professionele carrièrecoaching. Ontsluit nieuwe kansen met een cv waarin je potentieel tot zijn recht komt.
As soon as you begin to study 214rentals.com working in texts and popular Word editors, you can classify this problem as identifying empty extra sheets.
Plates can have various technical parameters fla-real-property.com, among which when choosing it is worth highlighting: cost of the product, manufacturer and purpose.
CVzen e o melhor servico https://cvpro.pt/ de redacao de curriculos e coach de carreira para milhoes de candidatos a emprego em todo o mundo. A nossa equipa de especialistas esta empenhada no seu sucesso e ira apoia-lo ao longo de toda a sua carreira, desde a elaboracao do seu CV profissional e carta de apresentacao com especificidades da industria ate a otimizacao do seu perfil no LinkedIn e ao fornecimento de coaching de carreira profissional. Desbloqueie novas oportunidades com um curriculo que mostre o seu potencial.
Приемная кампания ВГУ
Вас интересуют карты всех штатов США с популярными городами и достопримечательностями? East-usa.com – вот, что вам нужно! Детальная туристическая карта дает возможность сориентироваться на местности и спланировать собственное путешествие. Ищете western usa? East-usa.com – сайт, где есть карта, на ней показаны интересные места. Они могут быть для вас еще и полезными. У вас есть возможность узнать об объектах, о который вы ни разу не слышали. Карты дорог оптимизированы для просмотра на настольных компьютерах и мобильных устройствах.
FX broker https://linuxakademi.com.tr/ rating is a treasure trove of insights for traders. These ratings are based on user feedback, meticulous analysis of trading conditions, and the security of funds. Make sure to check them out when selecting a trusted and dependable partner for your journey towards winning trades.
As for relative height, it is italy-cars.com usually measured in meters. Moreover, it is worth noting that it is this that will show the difference between the absolute height of a geographical object, as well as the height of the surrounding area. If the mountain has an absolute height of 2000 meters, but the surrounding area is at an altitude of 1000 meters, then as for the relative height of the mountain, it is 1000 meters.
установка кондиционера в казани цена
pharmacies en ligne certifiГ©es: levitra generique – Pharmacie sans ordonnance
Зайдите на сайт https://piastrix.team/ и узнайте все об электронном кошельке Piastrix. Это российская разработка и помогает пользователям проводить и получать платежи в азартных играх. Узнайте подробно на сайте как зарегистрировать кошелек Пиастрикс и как им пользоваться, как пополнить и всех прочих преимуществах платежной системы Piastrix.
trouver un mГ©dicament en pharmacie: levitra generique sites surs – п»їpharmacie en ligne france
На сайте https://imperiasinteza.com оставьте заявку для того, чтобы воспользоваться такой популярной, нужной услугой, как продвижение сайтов в РФ и РБ. При этом оптимизация происходит с очень высокой скоростью, на профессиональном уровне. Огромный выбор самых разных услуг, подобранных с учетом индивидуальных особенностей. Работы обязательно принесут необходимые результаты. Все они выполняются качественно, на профессиональном уровне. Специалисты работают давно, а потому у них огромный опыт.
На сайте https://cdmebel.ru/ вы сможете заказать производство недорогой мебели высокого качества: для персонала, руководителя, для ресепшн. Также можно приобрести надежные, практичные стулья, кресла. Имеются и кухни, которые созданы для офисов. Вся мебель создается в соответствии с самыми последними технологиями и с учетом требований по дизайну. Компания отличается собственным современным производством. Любое пространство будет оснащено качественной мебелью. Сроки поставки являются минимальными.
KreditBaza.ru – информационный проект, который посвящен банковским услугам и банкам. Здесь вы найдете следующие разделы: РКО, дебетовые и кредитные карты, займы, кредиты. У нас собраны самые лучшие предложения. Выбирайте подходящее, и заполняйте онлайн анкету. Ищете где взять займ? Kreditbaza.ru – сайт, где найдете статьи, которые помогут разобраться в банковских продуктах и повысить финансовую грамотность. Вы узнаете, нужно ли брать займ и другое. Предоставляем исключительно полезную информацию, ознакомиться с ней можете в любое удобное для вас время.
Viagra vente libre pays: Viagra sans ordonnance 24h – Viagra homme sans ordonnance belgique
NEMALYARKA – компания, которая предоставляет профессиональные услуги по отделке и ремонту. Мы с радостью сделаем вам малярные работы. Мы знаем свою работу, нам доверились уже многие Калужане и не пожалели об этом. https://nemalyarka.ru/ – сайт, где можете прямо сейчас оставить заявку. Также здесь имеются полезные статьи. Покраска стен, шпаклевка q4 – все это умеем. Готовы выполнять самые трудные проекты, от которых другие отказались. Свяжитесь с нами для консультации, ответим на вопросы и реализуем любые желания. Ждем ваших предложений!
Геракл24: Профессиональная Замена Основания, Венцов, Полов и Перенос Зданий
Организация Геракл24 специализируется на предоставлении полных услуг по замене фундамента, венцов, настилов и передвижению строений в населённом пункте Красноярском регионе и за пределами города. Наша команда профессиональных специалистов обеспечивает высокое качество выполнения всех типов восстановительных работ, будь то деревянные, каркасные, кирпичные постройки или бетонные конструкции здания.
Плюсы работы с Геракл24
Навыки и знания:
Весь процесс проводятся лишь высококвалифицированными мастерами, имеющими долгий практику в области строительства и ремонта зданий. Наши мастера профессионалы в своем деле и осуществляют работу с максимальной точностью и вниманием к мелочам.
Полный спектр услуг:
Мы предоставляем разнообразные услуги по восстановлению и реконструкции строений:
Смена основания: укрепление и замена старого фундамента, что обеспечивает долгий срок службы вашего дома и устранить проблемы, связанные с оседанием и деформацией.
Реставрация венцов: замена нижних венцов деревянных домов, которые наиболее часто подвергаются гниению и разрушению.
Смена настилов: монтаж новых настилов, что значительно улучшает визуальное восприятие и практическую полезность.
Перенос строений: безопасное и качественное передвижение домов на новые локации, что обеспечивает сохранение строения и избежать дополнительных затрат на создание нового.
Работа с любыми видами зданий:
Дома из дерева: реставрация и усиление деревянных элементов, защита от гниения и вредителей.
Каркасные дома: реставрация каркасов и замена поврежденных элементов.
Дома из кирпича: ремонт кирпичных стен и укрепление стен.
Бетонные дома: ремонт и укрепление бетонных конструкций, ремонт трещин и дефектов.
Качество и прочность:
Мы применяем только проверенные материалы и передовые технологии, что гарантирует долгий срок службы и надежность всех работ. Все наши проекты проходят строгий контроль качества на каждом этапе выполнения.
Персонализированный подход:
Мы предлагаем каждому клиенту индивидуальные решения, учитывающие ваши требования и желания. Мы стремимся к тому, чтобы результат нашей работы соответствовал вашим ожиданиям и требованиям.
Почему стоит выбрать Геракл24?
Сотрудничая с нами, вы найдете надежного партнера, который берет на себя все заботы по ремонту и реконструкции вашего строения. Мы гарантируем выполнение всех проектов в сроки, оговоренные заранее и с соблюдением всех правил и норм. Связавшись с Геракл24, вы можете быть спокойны, что ваш дом в надежных руках.
Мы всегда готовы проконсультировать и ответить на ваши вопросы. Звоните нам, чтобы обсудить ваш проект и получить больше информации о наших услугах. Мы поможем вам сохранить и улучшить ваш дом, обеспечив его безопасность и комфорт на долгие годы.
Геракл24 – ваш партнер по реставрации и ремонту домов в Красноярске и окрестностях.
coloradonewss.com
vevobahis581.com
Посетите сайт https://videoline.spb.ru/ и вы сможете подобрать систему видеонаблюдения, а также заказать услуги по установке видеонаблюдения Спб. Ознакомьтесь с каталогом товаров. Установка видеонаблюдения и монтаж системы выполняются по ГОСТУ, обязательна гарантия с нашей стороны. Установка видеонаблюдения в СПб от Компании Видео Линия – это услуги от профессионалов, быстрые сроки, выгодные цены!
Купить Аттестат
Купить Аттестат
Для тех, кто понимает ценность подготовки в одном из лучших ВУЗов, наша компания предлагает купить диплом Белорусского государственного университета. А когда один диплом получен титаническими усилиями при сдаче всех сессий, то за вторым образованием идти уже нет сил. Диплом ВУЗа, изготовленный на типографском бланке, Престиж, и, как правило, всего лишь в наличии самого диплома, это билет в уверенное и обеспеченное будущее, купить диплом, аттестат с гарантией в красноярске. К ним относится рецензия, отчет из антиплагиата, а также отзыв от научного руководителя. На территории нашей страны работает много таких компаний, в которых можно не только купить Аттестат диплом, но также ряд других важных образовательных документов, к примеру, аттестат об окончании школы. Мы предлагаем одну из нестандартных, но очень востребованных услуг в нашей компании можно приобрести диплом. Мы не просим никакой предоплаты, даем возможность проверить диплом бакалавра до момента оплаты.
russkiy365-diploms-srednee.ru
Купить Дипломы Вуза О Высшем Образовании
Выберите надежного продавца и заполните специальную анкету на сайте. Купить диплом любого учебного заведения, который купит Аттестат занесен в реестр можно в нашей компании. Очень важно понимать, что купить диплом в Одессе можно на оригинальном бланке или на бланке, изготовленном типографским способом.
Купить Сертификат О Прохождении Курсов
При этом далеко не в каждом аттестате работодатель руководствуется теми знаниями, которые соискатель приобрел за время обучения в вузе. Документ любого ВУЗа, техникума или аттестат в Украине: оригинальные бланки оплата только после проверки бесплатная доставка срок изготовления – 1 день. Купить диплом можно уже сейчас, и купить его возможностями всю жизнь.
Destruam предоставляет для вас большой выбор сериалов. Все они уже с первых минут захватывают. Пригласите своих друзей, соберитесь с близкими и в полной мере наслаждайтесь новинками кино. Гарантируем отменный звук и оперативную загрузку видео. Ищете шерлок холмс фильм 2009 смотреть онлайн ? Destruam.xyz – популярный портал, где есть сериалы, увлекающие неожиданными событиями и сюжетными поворотами. Разнообразие и качество контента на высоком уровне. Смотрите интересные сериалы без утомительной процедуры регистрации. Сделайте свой вечер веселым!
acheter mГ©dicament en ligne sans ordonnance: trouver un mГ©dicament en pharmacie – pharmacie en ligne france livraison internationale
Линкей Лайт – интернет-магазин, который приглашает вас сделать выгодные покупки. Здесь можете приобрести качественный кронштейн по наилучшей стоимости. Даем гарантию на быструю доставку. Ищете купить кронштейн поворотный для светильников? Linkey-light.ru/catalog/komplektuyushchie/kronshteyny_krepleniya_/kronshteyn_povorotnyy_kp_60_dlya_lineynykh_svetilnikov – здесь имеется кронштейн поворотный КП-60, предназначенный для линейных светильников, чтобы его приобрести, оформите на сайте заявку. Также у вас есть возможность позвонить по телефону магазина. Мы всегда готовы проконсультировать вас.
CVzen est le service https://cvzen.fr/ ultime de rédaction de CV et de coaching de carrière pour des millions de chercheurs d’emploi à travers le monde. Notre équipe d’experts s’engage à votre réussite et vous accompagne tout au long de votre parcours professionnel, de la rédaction de votre CV professionnel et de votre lettre de motivation avec des spécificités sectorielles à l’optimisation de votre profil LinkedIn en passant par le coaching professionnel de carrière. Débloquez de nouvelles opportunités avec un CV qui met en valeur votre potentiel.
CVzen https://cvzen.it/ è il servizio di scrittura di CV e career coach per eccellenza per milioni di persone in cerca di lavoro in tutto il mondo. Il nostro team di esperti si impegna per il vostro successo e vi supporterà in tutto il vostro percorso professionale, dalla stesura di un CV professionale e di una lettera di presentazione specifica per il settore, all’ottimizzazione del vostro profilo LinkedIn, fino al career coaching professionale. Sbloccate nuove opportunità con un curriculum che metta in luce il vostro potenziale.
Студенческие Билеты
Вопросы оперативно решаются в групповом чате или личном кабинете. Осуществление поиска новых проектных организаций и архитектурных мастерских на вверенной территории, Обеспечение наличия актуальной технич еской информации и рекламной продукции Компании в проектных организациях и архитектурных мастерских, Проведение технически ориентированных презентаций и семинаров для сотрудников проектных организаций и архитектурных мастерских, Выполнение установленных студенческих билетов по применению продукции Компании в проектах, Помощь и участие в разработке и корректировке тех. Его можно получить после 5 лет обучения в ВУЗе, но можно и обойти эту формальность просто купить диплом из нашего каталога. Специалисты получают высокую зарплату, у них удобный график работы и отличные возможности для карьерного роста. Наши специалисты работают исключительно на законных основаниях и отвечают за свою работу. К тому же, у вас есть выбор вы можете купить абсолютно любой диплом на заказ: диплом бакалавра, диплом специалиста, диплом магистра, диплом кандидата или доктора наук, диплом с отличием или без, проведенный диплом или нет и так далее. При этом качество дипломов, которые мы выдаем, всегда на высоте.
http://www.russkiy365-diploms-srednee.ru
Доверенность На Авто 2019
Это всерьез прекрасный вариант устранить одним звонком массу проблем. Наша компания DIPLOMAN поможет вам сделать реальными ваши карьерные планы и амбиции. Тогда, билет будущей специальности определяется местоположением учебного учреждения.
Что Купить В Колледж
В нашей стране классификация образования выглядит следующим образом: дошкольное. Среди них можно выделить следующее: прежде всего, появляется возможность получить достойное место с хорошей заработной платой. Ситуации бывают разные, студенческий билет поможет разобраться и выбрать такой диплом, который подходит именно вам. Это учёная степень, которая присуждается исключительно в том случае, если ученый защитил докторскую диссертацию.
ремонт смартфонов
Радость, удивление, восторг, благодарность – вот эмоции, ради которых стоит дарить что-то необычное! У нас есть денежные карточки, аксессуары для медового месяца, папка со сладостями и многое др. https://boorsch.ru/ – сайт, где найдешь много уникальных идей, а еще получишь удовольствие от создания подарка своими руками! Все просто: теперь не надо переплачивать и ждать доставку. Получаешь шаблоны на электронную почту, печатаешь и сам делаешь подарок, следуя инструкции. Пусть ваш презент станет проявлением внимания и заботы!
pharmacie en ligne sans ordonnance: Pharmacies en ligne certifiees – п»їpharmacie en ligne france
Преимущества наших навес над автомобилем из поликарбоната очевидны – убедитесь сами.
На сайте https://gdz-history.ru/ изучите атласы, а также контурные карты по истории 6,5, 7, 8, 9, 10 классов. Есть возможность не только скачать, но и почитать в режиме реального времени. Делайте так, как удобно именно вам. Распечатайте чистые контурные карты по такой дисциплине, как история. Все материалы помогут вам получить необходимые знания, повысить уровень интеллекта. Теперь и вы сможете сдать предмет на высокий балл. Скачивайте информацию тогда, когда вам удобно и в любое время. На портале представлены и тезисы для ознакомления с темами.
Казино Taker является самым стабильным и предлагает отличную возможность заработать хорошие деньги. Разнообразие игр впечатляет, а условия здесь довольно выгодные. Ищете taker официальный сайт? Taker.blog – сайт, который дает возможность отдохнуть от различных проблем. Разнообразьте свой досуг прямо сейчас. Безпроблемные выплаты улучшают игровой процесс. Уверены, вам понравится данное казино. Служба поддержки онлайн казино быстро отвечает на любые вопросы и желает вам безграничной удачи. Выбирайте Тейкер!
Сколько Предметов В Аттестате 9 Класса 2023
Работодатель одинаково смотрит на диплом государственного и негосударственного учебного заведения. Таким образом, заказ дипломной работы предоставляет студенту уникальную возможность получить высокую оценку за свою работу без дополнительных затрат времени и усилий. Обучение на заочных курсах не требует присутствия на лекциях студентов. Трансляционная медицина есть и в России, и специалисты прогнозируют появление большого количества рабочих мест в этой области. В этом Вы сможете убедиться сами, только взяв бумагу в руки. Все документы изготовлены на оригинальных бланках, таких же, какие выпускают типографии ГОЗНАК, Киржач, Спецбланк, Пермь (в зависимости от уровня образования и года выдачи), выглядят как официальные корочки, полностью соответствуют всем требованиям и имеют все необходимые степени защиты: водяные знаки, микротекст, ультрафиолетовые элементы, волокна, гильоширная сетка и пр.
http://www.russkiy365-diploms-srednee.ru
Купить Диплом О Среднем Образовании В Брянске
Если у Вас есть нужные умения и опыт, но нет корочек, то покупая диплом техникума на нашем сайте, вы полностью оправдаете вложенные средства. Информация, переданная для заполнения, уничтожается после сотрудничества. За каждым изготовленным документом скрывается судьба человека и именно по этой причине так обидно и страшно, что находятся бизнесмены, которые на этом наживаются.
Милое Свидетельство О Браке
Для этого Вам нужно лишь выбрать и оформить заказ на нашем сайте. Самая лучшая реклама для любой компании это отзывы довольных клиентов. ВИДЕО – Свидетельство о браке Купить диплом о высшем образовании в Вологде с нашей компанией можно очень быстро и просто. Для этого Вам нужно лишь выбрать и оформить заказ на нашем сайте.
Metal structures must be produced newmexicodesign.net under strict quality control. Absolutely all work is checked – from the manufacture of elements to final assembly. It is necessary to check their size, strength, coating and other parameters.
Complex work requires experience chicago-job.com and the use of modern equipment using strong chemicals. Not every person has such an arsenal available.
The finished metal alabama-news.com structure must be properly packaged. Thanks to this, it will definitely not be damaged during transportation.
Хотите смотреть увлекательные сериалы абсолютно бесплатно и в отличном качестве? Mixtios вам в этом поможет. Здесь вы найдете самое лучшее кино. Вы можете в любое удобное время смотреть фильмы. Ищете волшебное приключение да винчи мультфильм 2023 смотреть онлайн ? Mixtios.xyz – сайт, где представлены сериалы, помогающие ощутить множество положительных эмоций и отвлекающие от повседневной жизни. Профессиональное озвучивание и отменное качество изображения гарантируют великолепный просмотр. Уверены, у нас вы найдете то, что вам интересно!
business-exclusive.com
dapoxetine command – dapoxetine solemn priligy footstep
pharmacie en ligne france livraison internationale: pharmacie en ligne – п»їpharmacie en ligne france
На сайте https://sibvitr.ru/ воспользуйтесь такой услугой, как производство мебели для офиса, дома. Здесь вы сможете заказать кухни, шкафы-купе, прихожие, вместительные гостиные, кабинеты руководителей, детскую мебель. Замер, а также дизайн-проект предоставляются бесплатно. На производство уйдет не более 7 дней. Вся продукция реализуется по привлекательным ценам. При этом качество остается на приемлемом уровне. На продукцию дается гарантия 12 месяцев. Опыт работы на рынке – более 20 лет. В штате работают более 40 сотрудников.
10 Healthy Habits To Use Word Rewriter article rewriter ai (https://30.farcaleniom.com/index/d2?diff=0&source=og&campaign=8220&content=&clickid=w7n7kkvqfyfppmh5&aurl=https://velostil.pro/user/screengray0/&an=&term=&site=&pushMode=popup)
MCI Clinic excels in treating myopia with a focus on experience, cutting-edge technology, and cost-effective solutions. Our specialists conduct thorough assessments to determine the extent of nearsightedness and recommend the most suitable corrective measures, such as prescription glasses, contact lenses, or advanced refractive surgeries like LASIK. Each treatment plan is customized for optimal results.
Trust MCI for top-notch myopia care that doesn’t strain your budget. Our commitment to exceptional, affordable eye care ensures you achieve clear vision and maintain eye health through innovative and economical treatments.
MCI Clinic – oftalmolog
На сайте https://cliningkrd.ru закажите звонок для того, чтобы воспользоваться услугами клинингового агентства «Cleaning». В компании трудятся исключительно квалифицированные, компетентные сотрудники, которые не только обучены, но и постоянно повышают квалификацию на специальных курсах. В работе используются инновационные и высокотехнологичные расходные материалы, которые и позволяют получить безупречный результат. Есть возможность вызвать бригаду специалистов в любое время.
Conventionally, forklifts can be divided alcitynews.com into manual and self-propelled. The manual version must be moved by the operator, which may require some effort if the weight of the load exceeds a thousand kilograms. The advantage of this type is its low cost and complete lack of maintenance. However, such a loader will not lift the load to too great a height.
nebrdecor.com
Хотите расслабиться и прекрасно провести вечер? Онлайн-казино – это то, что вам необходимо. Taker завлекает игроков увлекательными слотами. Ищете такер сайт? Taker.website – сайт, который великолепно сделан, долго разбираться тут не придется. Сыграть здесь можно во что угодно. Главное то, что тут есть возможность реально выиграть крупные деньги. Выплаты осуществляются без задержек, и это радует. Саппорт лояльный, отвечает на все вопросы быстро. Почувствуйте сами все достоинства отменного отдыха вместе с Такер!
Pharmacie en ligne livraison Europe: cialis generique – acheter mГ©dicament en ligne sans ordonnance
priligy mood – dapoxetine unconscious priligy key
CVzen es el mejor servicio https://cvzen.es/ de redacción de CV y orientación profesional para millones de personas que buscan empleo en todo el mundo. Nuestro equipo de expertos está comprometido con tu éxito y te apoyará a lo largo de tu trayectoria profesional, desde la redacción de tu CV profesional y tu carta de presentación con datos específicos del sector hasta la optimización de tu perfil de LinkedIn y la orientación profesional. Desbloquea nuevas oportunidades con un currículum que muestre tu potencial.
dublindecor.net
elitecolumbia.com
Here you will learn about the apartusa365.com advantages of forklifts, as well as their types and applications. You may also be interested in the opportunity to purchase warehouse equipment.
https://kamagraenligne.com/# pharmacie en ligne avec ordonnance
pharmacie en ligne avec ordonnance: cialis sans ordonnance – pharmacie en ligne pas cher
Taker – казино, которое обеспечивает безопасность и честность игры. Такер привлекает игроков увлекательными слотами, онлайн-казино регулярно предлагает щедрые акции и бонусы. Саппорт отзывчивый, работает оперативно и вежливо, вывод средств – быстрый. Ищете taker официальный сайт? Taker.bond – сайт, дизайн которого великолепный, у вас не будет трудностей с навигацией. Если вы решили посетить данное онлайн-казино, вы сделали правильный выбор в пользу азартных игр. Вам скучно точно не будет. Испытайте удачу прямо сейчас!
alanews24.com
loratadine medication false – claritin pills secret claritin seize
Сайт fermerstvo.in.ua пользуется повышенной популярностью. Здесь представлена только интересная информация. Ознакомиться с ней есть возможность уже сейчас. fermerstvo.in.ua – https://fermerstvo.in.ua сайт, где узнаете с чего начать фермерское хозяйство. Мы открыто делимся своими успехами и неудачами. Разбираем, как подготовиться к разведению домашней птицы. Объясним, как урожайность овощей повысить. У нас вы найдете ответы на необходимые вопросы. Делаем понятный контент. Вы получите глубокие знания обо всем, что связано с фермерским хозяйством.
Зайдите на сайт https://coffeeroom.by/ и вы сможете купить кофе лучших брендов мировых производителей с быстрой доставкой в Минске. Зерновой кофе, молотый кофе, степень обжарки, варианты по цене – все это вы найдете в поиске. А наша новая услуга аренда кофемашины позволит вам наслаждаться напитком каждый день.
payday loans nky Few customers find their lender via existing price comparison websites, which suffer from a number of limitations.
loratadine medication want – loratadine gaz loratadine medication darken
На сайте https://oboinastene.ru/ почитайте информацию об обоях. Вы узнаете об их видах, особенностях, преимуществах, использовании в интерьере. Кроме того, есть информация о том, как их правильно клеить, чтобы они красиво выглядели в течение долгого времени. Есть данные о ремонте кровли, о том, как правильно его выполнять. Все обои различаются между собой не только цветовой гаммой, но и фактурой, а также типом поверхности, текстурой и другими особенностями. Есть информация и об автоматических выключателях ДКС.
10 SEO Software Tips All Experts Recommend search engine rankings software (hklive.org)
pharmacie en ligne sans ordonnance: Levitra acheter – acheter mГ©dicament en ligne sans ordonnance
Taker – прекрасное онлайн-казино, достойное вашего внимания. Оно игроков завлекает интересными слотами, регулярно предоставляет щедрые бонусы и акции. Вывод средств оперативный, саппорт лояльный. Ищете такер сайт? Taker.vin – сайт, имеющий превосходный дизайн и простую навигацию, поэтому вам не будет сложно им пользоваться. Если решили посетить казино Такер, то вам повезло, потому что именно тут представлен широкий выбор азартных игр. Вы точно не заскучаете. Удачи вам!
Its like you read my mind! You appear to know a lot about this, like you wrote the book in it or something. I think that you could do with a few pics to drive the message home a little bit, but instead of that, this is great blog. A fantastic read. I’ll certainly be back.
https://gruppa365-diploms-srednee.ru/
На сайте https://autopiter.ru/ представлены оригинальные, неоригинальные запчасти, каталоги ГАЗ, ВАЗ, автохимия, автомасла наиболее популярных, практичных брендов, которые доказали свою надежность. Также представлены и аккумуляторы, все для спецтехники. А если хотите подобрать что-то определенное, то воспользуйтесь специальным поиском. Все автомасла, которые находятся в каталоге, отличаются гарантией качества. Обязательно посетите раздел с рекомендуемыми товарами. Все заказы доставляются максимально быстро.
fast cash nj With no faxing requirement, they can go about their work freely.
Admiring the dedication you put into your blog and detailed information you provide. It’s good to come across a blog every once in a while that isn’t the same old rehashed material. Great read! I’ve saved your site and I’m adding your RSS feeds to my Google account.
http://www.russkiy365-diploms-srednee.ru
Pharmacie en ligne livraison Europe: pharmacie en ligne pas cher – pharmacie en ligne pas cher
california-invest.com
Maximum effect from the greeceholidaytravel.com cleaning measures carried out. Professional employees will cope with pollution of any complexity and type of origin.
This is the perfect site for everyone who wants to understand this topic. You understand a whole lot its almost hard to argue with you (not that I personally will need to…HaHa). You certainly put a fresh spin on a topic which has been written about for years. Wonderful stuff, just wonderful!
http://www.gruppa365-diploms-srednee.ru
money cats Look on your statement and see how much you have paid in interest so far this year then think about what you could have done with the money yourself if your debt wasn’t there.
На сайте https://imperiasinteza.by оставьте заявку с той целью, чтобы воспользоваться услугами, связанными с логопедией, сенсорной интеграцией. Только для вас профессиональные услуги, консультации логопеда. В компании работает логопед-дефектолог для детей, можно воспользоваться сенсорной интеграцией. Специально для вас индивидуальные, а также групповые занятия, которые принесут должный эффект. При необходимости организуется выезд специалиста. Самая первая консультация предоставляется в подарок.
Если вам нужно легализовать документы для использования за границей, вы можете легко заказать апостиль у нас. Мы предлагаем быструю и надежную услугу, чтобы ваши документы были готовы в кратчайшие сроки.
Для тех, кто нуждается в официальном признании документов за рубежом, мы предоставляем полный спектр услуг, включая перевод и апостиль документов. Наши специалисты помогут вам быстро и качественно оформить все необходимые бумаги.
Если вам требуется апостиль документов, наша компания готова помочь вам в этом вопросе. Мы обеспечим юридическую силу ваших документов за границей, оперативно и профессионально выполнив все процедуры.
Чтобы ваше свидетельство о рождении было признано в других странах, вам необходим апостиль на свидетельство о рождении. Мы гарантируем точное и своевременное выполнение этой услуги, чтобы вы могли без проблем использовать документ за границей.
https://apostil-yaziki.ru/
Alptracking осуществляет аренду надежного и высококачественного туристического снаряжения. У нас вы найдете треккинговые палки, спальные мешки, рюкзаки, палатки, матрасы и коврики и т.д. Весь ассортимент снаряжения изучите, предварительно скачав на нашем сайте прайс-лист. Ищете аренда sup-бордов? Alptracking.ru – здесь у вас есть возможность уже сейчас ознакомиться с контактами, отзывами и условиями проката. Мы всегда готовы ответить на интересующие вас вопросы и оформить аренду необходимого снаряжения. Поможем вам путешествовать с комфортом!
cash advance Balt Mary. In the end, we would just like to say that over time the loan process has got easier and there are so many loans on offer in the market that everybody can get some sort of loan or the other.
What’s up, I wish for to subscribe for this website to obtain most up-to-date updates, thus where can i do it please assist.
gruppa365-diploms-srednee.ru
На сайте https://ax-card.ru/ закажите пластиковые карты для различных сфер деятельности. Их создают на инновационном, высокотехнологичном оборудовании компетентные специалисты с огромным опытом. Дополнительно они разработают макет, а при оказании услуги используют уникальные и инновационные технологии. Именно поэтому вы получите ожидаемый и прогнозируемый результат. Если вы заинтересовались услугой, то специально для вас может быть сделана пробная карта. Это абсолютно бесплатно.
Зайдите на сайт компании Финтех https://finteh.su/ которая специализируется на проектировании и строительстве каменных, деревянных, комбинированных и других домов под ключ. Подберите на сайте проект под себя или посмотрите готовые, типовые проекты. Привлекательные цены на строительство и акции от Финтех позволят вам построить качественный дом мечты!
Pharmacie en ligne livraison Europe: kamagra livraison 24h – Pharmacie Internationale en ligne
MIGRANT SUPPORT предлагает помощь в получении номера PESEL и гарантирует разумные цены. Квалифицированные специалисты компании, взявшись за вашу задачу, приложат максимум усилий для ее выполнения. https://migrant.support/poluchieniie_nomiera_pesel – сайт, где у вас есть возможность узнать, как сделать песель удаленно, и зачем он нужен. Мы оказываем бесплатную консультацию, работаем качественно и оперативно. К своим клиентам относимся лояльно, и делаем все, чтобы их ожидания были оправданы. Вы точно не пожалеете о своем выборе, обращайтесь!
Considering how busy most bestchicago.net people are, cleaning services have gained high popularity. There are several types of cleaning: daily, cleaning the apartment after renovation, cleaning by zone and others. Owners usually cope with superficial maintenance of the premises on their own, but general cleaning can cause difficulties.
The term “ticket” often refers repairtoday7.com to a support request. It is the ticket that guarantees a person that his problem will be quickly resolved. A high-quality ticket system for technical support will allow a business to gain many benefits. Let’s look at such innovations in more detail.
sellrentcars.com
unsecured personal loans excellent credit The advance agreement is between you and Mr. Payday and no one else is notified.
The service has collected on the usainvesttoday.com pages of its website all offers from tour operators in Moldova. Here you can find information for any tours to Egypt with departure from Chisinau, where you can select the number of travel participants, dates and travel options.
carsnow.net
На сайте https://trart.ru/ почитайте информацию, которая касается психологии. Так вы узнаете о том, каким образом сохранить отношения после того, как рождается ребенок. Также рассказываются основные причины конфликтов между свекровью, невесткой. Опубликованы данные, которые касаются причин появления семейного кризиса. Вы узнаете о том, каким образом эффективней пережить измену. Вы узнаете о самых эффективных и рациональных методиках, которые помогут вернуть в отношения страсть.
tradeusanews.com
Groove inserts can be used to carsnow.net work with various types of metals and alloys, including the most durable and hard ones. A long service life and the ability to sharpen the cutting edges of tools are guaranteed.
pharmacie en ligne: levitra en ligne – п»їpharmacie en ligne france
На сайте https://ruuserial.net/ находятся русские сериалы, которые точно вам понравятся, ведь в них играют самые популярные актеры. Они донесут до вас сюжет фильма так, чтобы вы прочувствовались. Есть фильмы самых разных жанров, в том числе, комедии, триллеры, мелодрамы, драмы и многое другое. Все фильмы в хорошем качестве, помогают вникнуть в истории и получить приятные эмоции. Обрадует и музыкальное сопровождение. Можно подыскать вариант по году выпуска. Постоянно происходит обновление кино.
Портал visti.in.ua заслуживает вашего внимания. Здесь предложены интересные новости Украины, которые в круглосуточном доступе находятся. Мы ценим и гордимся своими читателями. Для вас собрали только самое лучшее, поудобнее устраивайтесь и читайте интересную информацию. visti.in.ua – https://visti.in.ua сайт, который пользуется повышенной популярностью. Посетите его прямо сейчас и узнаете об экономике, науке, политике, спорте. Все сведения достоверны, можете даже в этом не сомневаться. Следите за нами и получайте истинное удовольствие от отменного контента!
Не знаете как принимать платежи в криптовалюте онлайн на вашем сайте? Зайдите на https://cryptocloud.plus/ и вы сможете быстро и бесплатно подключиться к нашим продуктам. Посетите сайт, узнайте о решениях и возможностях и всех наших преимуществах. Инструменты для удобной работы с криптовалютой к вашим услугам.
Rassilka.kz оказывает высококачественные услуги. Делаем email, смс, ватсап, рассылки по Алматы, Нур-Султану, а также Казахстану. Сотрудничаем с разными популярными компаниями. Наша главная задача – принести всем клиентам пользу. Действия нацелены на конечный результат. https://rassilka.kz – сайт, где вы узнаете, почему выбирают именно нас. Здесь можете в любое удобное для вас время ознакомиться с тарифами. У нас вы получите консультацию на бесплатной основе. Свяжитесь с нами, и мы ответим на все интересующие вопросы.
can you extend payday loans Payday loans are provided for situations and applicants that traditional banking institutions would decline.
В нашем мире, где диплом – это начало удачной карьеры в любой отрасли, многие стараются найти максимально быстрый и простой путь получения образования. Факт наличия официального документа об образовании трудно переоценить. Ведь диплом открывает двери перед любым человеком, который стремится начать трудовую деятельность или продолжить обучение в высшем учебном заведении.
Предлагаем очень быстро получить этот важный документ. Вы имеете возможность заказать диплом, и это становится удачным решением для всех, кто не смог завершить образование, потерял документ или хочет исправить плохие оценки. Любой диплом изготавливается аккуратно, с особым вниманием ко всем элементам, чтобы на выходе получился продукт, 100% соответствующий оригиналу.
Плюсы этого подхода состоят не только в том, что вы сможете быстро получить свой диплом. Весь процесс организован удобно, с профессиональной поддержкой. Начиная от выбора необходимого образца до правильного заполнения персональных данных и доставки в любой регион страны — все находится под полным контролем опытных специалистов.
Для тех, кто ищет быстрый способ получить необходимый документ, наша компания может предложить отличное решение. Купить диплом – это значит избежать долгого процесса обучения и не теряя времени перейти к достижению собственных целей, будь то поступление в университет или старт успешной карьеры.
http://www.rassvetykamchatki.ru
Working as a courier offers flexible hours as getusainvest.com one of the main benefits. An employee can work every day or every other day, the number of working hours is determined independently. The courier’s earnings directly depend on the number of completed orders.
Search by Image on Amazon https://chromewebstore.google.com/detail/search-by-image-on-amazon/fmiialomjacaogdjjkgicepphmekndli uses advanced technology to provide users with a unique functionality. By analyzing images, the extension is able to search for relevant products. To use this feature, users can conveniently right-click on any image in their browser and select the “Search on Amazon” option.
Заказать Вентилятор радиальный ВЦ 14-46 по оптовым ценам от завода производителя ООО Гевей можно на сайте https://vent-climate.ru/ Так же производим вентиляторы промышленные радиальные В
Pharmacie en ligne livraison Europe: Cialis sans ordonnance 24h – Pharmacie sans ordonnance
Вам интересна прописка в Польше, г. Варшава? MIGRANT SUPPORT вам в этом поможет. Компания предоставляет качественные услуги. Гарантирует лояльные цены и персональный подход к каждому клиенту. У вас есть возможность получить квалифицированную консультационную поддержку по необходимым вопросам. https://vpolshe.com/propiska-v-polshe-g-varshava-dogovor-arendy-zhilya-varshava/ – сайт, где вы узнаете, для чего нужна прописка (meldunek). Оставьте заявку на портале, и мы вам позвоним через некоторое время. Будем рады помочь с договором аренды жилья.
На сайте https://aakkb.com.ua/ вы сможете приобрести литиевые аккумуляторы, а также аккумуляторные сборки. Все конструкции отличаются своей надежностью, безупречным качеством, а также идеальным исполнением. Все модели от проверенных, лучших брендов, которые работают на совесть. Перед вами огромное количество моделей, что позволит подобрать решение на свое устройство. А если затрудняетесь с выбором, то вас всегда поддержит высококлассный специалист. Он даст ценные советы, важные рекомендации.
Offering a large selection of products alahomemaster.com, the seller works directly with manufacturers, which allows keeping prices at a fairly low level, because the chain of intermediaries disappears.
Почему теневой плинтус – красивая и практичная деталь интерьера,
Советы по монтажу теневого плинтуса без дополнительной помощи,
Креативные способы использования теневого плинтуса в дизайне помещения,
Теневой плинтус: классический стиль в современном исполнении,
Как подобрать цвет теневого плинтуса к отделке стен,
Теневой плинтус: простое решение для скрытия кабелей и проводов,
Преимущества использования теневого плинтуса с интегрированной подсветкой,
Современные тренды в использовании теневого плинтуса для уюта и красоты,
Почему теневой плинтус – важная деталь в оформлении интерьера
алюминиевый профиль алюминиевый профиль .
На сайте https://ruuserial.net/ находятся русские сериалы, которые точно вам понравятся, ведь в них играют самые популярные актеры. Они донесут до вас сюжет фильма так, чтобы вы прочувствовались. Есть фильмы самых разных жанров, в том числе, комедии, триллеры, мелодрамы, драмы и многое другое. Все фильмы в хорошем качестве, помогают вникнуть в истории и получить приятные эмоции. Обрадует и музыкальное сопровождение. Можно подыскать вариант по году выпуска. Постоянно происходит обновление кино.
На сайте https://imperiafohow.by оставьте заявку для того, чтобы воспользоваться услугой массажа. Вы почувствуете заботу о своем теле, полное расслабление и уход. Все массажисты являются компетентными, квалифицированными специалистами с огромным опытом. Все их движения максимально мягкие, приятные и деликатные, а потому вы почувствуете расслабление и негу. Используется косметика популярных, надежных брендов, которые работают на совесть. Но с той целью, чтобы достичь нужных результатов, следует ответственно подходить к оказанию услуги.
If this is necessary, you should make northfloridahouse.com sure that the installation of the metal structure is carried out professionally. All instructions must be followed in practice.
Corporate culture plays an important role. The interests of clients italycarsrental.com are put first for every employee of the company; the area of responsibility does not play an important role. For example, help desks gain additional incentive when they realize that quickly resolving employee issues has an impact on customer service. If, for example, a software glitch is not fixed, the manager will not calculate the loan program for the client. As a result, he will share negative experiences with other people, so the company’s reputation will suffer.
На сайте https://nichego-nebolit.ru/ ознакомьтесь с любопытной, интересной информацией, рекомендациями, которые касаются того, как подобрать каре, каковы преимущества и нюансы данной стрижки. Имеются данные о КТ легких и о том, когда лучше всего проводить процедуру и в каких случаях. Есть информация и о системах для нагревания табака. Даны рекомендации о том, как правильно выбрать брус. Есть любопытная статья об озонотерапии и том, как она может вам помочь в улучшении состояния здоровья.
Почему теневой плинтус – красивая и практичная деталь интерьера,
Шаг за шагом инструкция по установке теневого плинтуса,
Теневой плинтус как элемент декора: идеи и варианты применения,
Модные тренды в выборе теневых плинтусов для современного дома,
Гармония оттенков: выбор цвета теневого плинтуса для любого интерьера,
Как спрятать коммуникации с помощью теневого плинтуса: практические советы,
Теневой плинтус с подсветкой: создаем эффектное освещение в интерьере,
Современные тренды в использовании теневого плинтуса для уюта и красоты,
Интерьер безупречный до мелочей: роль теневого плинтуса в декоре
алюминиевый профиль алюминиевый профиль .
Преимущества теневого плинтуса в декорировании помещения,
Советы по монтажу теневого плинтуса без дополнительной помощи,
Креативные способы использования теневого плинтуса в дизайне помещения,
Теневой плинтус: классический стиль в современном исполнении,
Советы стилиста: как сделать цвет теневого плинтуса акцентом в помещении,
Как спрятать коммуникации с помощью теневого плинтуса: практические советы,
Интересные решения с теневым плинтусом и подсветкой: идеи для вдохновения,
Современные тренды в использовании теневого плинтуса для уюта и красоты,
Почему теневой плинтус – важная деталь в оформлении интерьера
купить теневой плинтус купить теневой плинтус .
Сайт visti.in.ua достоин вашего внимания. Здесь представлены актуальные новости Украины, они находятся в круглосуточном доступе. Мы гордимся и ценим своих читателей. Для вас собрали только самое лучшее, поудобнее устраивайтесь и читайте интересную информацию. visti.in.ua – https://visti.in.ua портал, который пользуется большой известностью. Посетите его прямо сейчас и узнаете об экономике, науке, политике, спорте. Все сведения достоверны, можете даже в этом не сомневаться. Следите за нами и получайте истинное удовольствие от отменного контента!
На сайте https://t.me/s/m_1go изучите всю необходимую информацию, которая касается онлайн-заведения 1GO. Воспользуйтесь возможностью сыграть и выиграть приличную сумму денег. Официальный канал находится в вашем мобильном телефоне. Почитать всю интересующую информацию получится в любое время, даже поздним вечером. Открывайте группу на своем мобильном телефоне либо компьютере, чтобы получить доступ к безграничному миру развлечений, бонусов, привилегий. Теперь и вы сможете присоединиться к обществу победителей!
Почему теневой плинтус – красивая и практичная деталь интерьера,
Как правильно установить теневой плинтус своими руками,
Теневой плинтус как элемент декора: идеи и варианты применения,
Теневой плинтус: классический стиль в современном исполнении,
Советы стилиста: как сделать цвет теневого плинтуса акцентом в помещении,
Теневой плинтус: простое решение для скрытия кабелей и проводов,
Теневой плинтус с подсветкой: создаем эффектное освещение в интерьере,
Как сделать помещение завершенным с помощью теневого плинтуса,
Интерьер безупречный до мелочей: роль теневого плинтуса в декоре
плинтус скрытого монтажа https://plintus-tenevoj-aljuminievyj-msk.ru/ .
Эскорт услуги в Москве
сеть сайтов pbn
Работая в поисковой оптимизации, нужно знать, что нельзя одним способом вывести сайт в верхние позиции поисковых систем, так как поисковики это как трек с финишной прямой, а веб-сайты это гоночные автомобили, которые все хотят быть на первом месте.
Так вот:
Перечень – Для того чтобы веб-сайт был адаптивным и быстрым, важна
улучшение
Сайт должен содержать только уникальный контент, это текст и картинки
ОБЯЗАТЕЛЬНО ссылочный профиль через сайты с статьями и непосредственно на главную
Увеличение обратных ссылок с помощью дополнительных сайтов
Ссылочная структура, это ссылки первого уровня, Tier-2, Tier-3
Ну и главное это сеть сайтов PBN, которая линкуется на манисайт
Все сайты PBN должны быть без отпечатков, т.е. системы поиска не должны осознавать, что это один владелец всех веб-сайтов, поэтому крайне важно следовать все эти указания.
На сайте https://omsksite.ru/ представлены самые эффективные, работающие методы выполнения ремонта. Этот блог посвящен строительным, ремонтным, отделочным работам. Вся информация является полезной, интересной. А самое главное, что позволит справиться с проблемой максимально быстро. На сайте будут рассказаны все тонкости ремонта и то, какие материалы для этих целей лучше использовать. Имеется контент на тему того, как правильно подобрать пластиковое окно. Есть информация про пожарную охрану, руководство, которое поможет правильно подобрать набор инструментов.
На сайте https://vpolshe.com/propiska-v-polshe-g-varshava-dogovor-arendy-zhilya-varshava/ вы сможете оформить такой важный документ, как прописка в Польше, Варшаве. Сотрудники компании оформят договор аренды жилья. Они проведут исчерпывающую, содержательную консультацию, на которой вы узнаете всю необходимую информацию, в том числе, и то, какие документы вам потребуются для оформления. Для наглядности присутствует и образец. Прописка потребуется для открытия счета, оформления карты побыту.
pharmacie en ligne france livraison internationale: Medicaments en ligne livres en 24h – pharmacie en ligne
На сайте https://setki.moscow вы сможете оформить заявку для того, чтобы заказать москитную сетку. Конструкции производятся из качественных, надежных материалов и всего за день. Монтажные работы проводятся в любой, наиболее комфортный для вас день. На работы, конструкции даются гарантии 12 месяцев. Рассчитать итоговую цену вы сможете прямо сейчас. Установлена привлекательная стоимость за счет собственного производства. Работа происходит не только по Москве, но и области. Предприятие специализируется на производстве, реализации, а также установке москитных сеток.
На сайте https://ruuserial.net/ посмотрите интересные, новые и полюбившиеся сериалы, которые унесут в удивительный мир. Все они находятся в отличном качестве, с хорошим звуком, а потому понравятся и киноманам. Отличаются интересным, незаурядным сюжетом, увлекательной актерской игрой, приятной музыкой. Есть и совсем новые сериалы, которые только вышли в этом году. Обновление сериалов происходит регулярно. А потому вы точно подберете тот вариант, который вы будете просматривать вечером, после работы или в выходной день.
швеллер размеры гост цены
The timber does not require carsdirecttoday.com special finishing or painting. If the timber is sufficiently dried, then this design will not shrink.
chicagonewsblog.com
If this is necessary, you should make carsnow.net sure that the installation of metal structures is carried out efficiently and professionally. All instructions should be followed by example.
Преимущества теневого плинтуса в декорировании помещения,
Советы по монтажу теневого плинтуса без дополнительной помощи,
Креативные способы использования теневого плинтуса в дизайне помещения,
Ретро-стиль с использованием теневых плинтусов: идеи для вдохновения,
Как подобрать цвет теневого плинтуса к отделке стен,
Безопасность и стиль: почему теневой плинтус – идеальное решение для дома,
Преимущества использования теневого плинтуса с интегрированной подсветкой,
Современные тренды в использовании теневого плинтуса для уюта и красоты,
Теневой плинтус: деталь, которая делает интерьер законченным и гармоничным
купить теневой плинтус https://plintus-tenevoj-aljuminievyj-msk.ru/ .
Почему теневой плинтус – красивая и практичная деталь интерьера,
Как правильно установить теневой плинтус своими руками,
Креативные способы использования теневого плинтуса в дизайне помещения,
Ретро-стиль с использованием теневых плинтусов: идеи для вдохновения,
Гармония оттенков: выбор цвета теневого плинтуса для любого интерьера,
Теневой плинтус: простое решение для скрытия кабелей и проводов,
Интересные решения с теневым плинтусом и подсветкой: идеи для вдохновения,
Современные тренды в использовании теневого плинтуса для уюта и красоты,
Интерьер безупречный до мелочей: роль теневого плинтуса в декоре
плинтус черный алюминиевый плинтус черный алюминиевый .
ремонт сотовых телефонов
Почему теневой плинтус – красивая и практичная деталь интерьера,
Советы по монтажу теневого плинтуса без дополнительной помощи,
Креативные способы использования теневого плинтуса в дизайне помещения,
Теневой плинтус: классический стиль в современном исполнении,
Как подобрать цвет теневого плинтуса к отделке стен,
Безопасность и стиль: почему теневой плинтус – идеальное решение для дома,
Интересные решения с теневым плинтусом и подсветкой: идеи для вдохновения,
Теневой плинтус: элегантность и стиль в дизайне помещения,
Интерьер безупречный до мелочей: роль теневого плинтуса в декоре
алюминиевый плинтус https://plintus-tenevoj-aljuminievyj-msk.ru/ .
Почему теневой плинтус – красивая и практичная деталь интерьера,
Шаг за шагом инструкция по установке теневого плинтуса,
Креативные способы использования теневого плинтуса в дизайне помещения,
Теневой плинтус: классический стиль в современном исполнении,
Как подобрать цвет теневого плинтуса к отделке стен,
Безопасность и стиль: почему теневой плинтус – идеальное решение для дома,
Интересные решения с теневым плинтусом и подсветкой: идеи для вдохновения,
Теневой плинтус: элегантность и стиль в дизайне помещения,
Интерьер безупречный до мелочей: роль теневого плинтуса в декоре
алюминиевые плинтуса купить алюминиевые плинтуса купить .
Visit https://timespothq.com/ for in-depth reviews, in-depth comparisons, review guides, and expert opinions on the latest productivity software. We’ll help you find the perfect solution for your unique needs. More details on the website.
аппаратура для реанимации
На сайте https://us-canad.com/ изучите карты автомобильных дорог Канады, США. Только здесь вас ожидает самый подробный, детальный атлас всех дорог, которые находятся в Северной Америке. Для каждого посетителя сайта доступны крупномасштабные, полноразмерные карты, где учитываются и маршруты США, а также расстояние в милях. Имеется атлас с границами округов. Представлена карта всех штатов вместе с автомагистралями. Перед вами подробные цветные карты всех штатов США, где присутствуют памятники, национальные парки и многое другое.
Компания https://primeinterior.ru/ занимается поставками натурального мрамора, гранита, травертина, оникса и кварцита со всего мира для премиальных интерьеров. Имеем собственное производство во Владивостоке и команду специалистов для монтажа. Готовы к крупным заказам любой сложности со всей России, есть опыт работы с отелями, ресторанами, ночными клубами. Создаём неповторимые интерьеры из природного камня, высокое качество работы и материалов.
The main advantage of a forklift is its chinanewsapp.com versatility and ease of use. Essentially, it is just a trolley with a durable fork that can be used to lift pallets or large loads to any height. It is worth noting that the loader can be made in the form of a trolley with no traction of its own, or in the form of an electric/gasoline self-propelled vehicle, with the help of which extremely heavy objects can be transported over impressive distances throughout the warehouse. Another advantage is simple maintenance, which is ensured by the absence of technical bells and whistles, but this depends on the specific model of the device.
Замена венцов красноярск
Gerakl24: Профессиональная Смена Фундамента, Венцов, Настилов и Перемещение Зданий
Компания Геракл24 специализируется на предоставлении полных работ по замене фундамента, венцов, покрытий и передвижению домов в городе Красноярском регионе и в окрестностях. Наша команда опытных мастеров обещает высокое качество исполнения различных типов восстановительных работ, будь то древесные, каркасного типа, кирпичные постройки или бетонные конструкции дома.
Преимущества работы с Gerakl24
Профессионализм и опыт:
Каждая задача осуществляются лишь высококвалифицированными мастерами, с обладанием большой стаж в сфере создания и ремонта зданий. Наши мастера профессионалы в своем деле и реализуют задачи с высочайшей точностью и вниманием к деталям.
Комплексный подход:
Мы предлагаем все виды работ по ремонту и восстановлению зданий:
Замена фундамента: замена и укрепление фундамента, что позволяет продлить срок службы вашего строения и устранить проблемы, вызванные оседанием и деформацией.
Реставрация венцов: замена нижних венцов деревянных домов, которые наиболее часто подвержены гниению и разрушению.
Замена полов: монтаж новых настилов, что существенно улучшает визуальное восприятие и практическую полезность.
Передвижение домов: качественный и безопасный перенос строений на новые места, что обеспечивает сохранение строения и избегает дополнительных затрат на возведение нового.
Работа с различными типами строений:
Деревянные дома: восстановление и защита деревянных строений, обработка от гниения и насекомых.
Каркасные дома: усиление каркасных конструкций и смена поврежденных частей.
Кирпичные строения: реставрация кирпичной кладки и укрепление стен.
Бетонные строения: ремонт и укрепление бетонных конструкций, устранение трещин и повреждений.
Качество и надежность:
Мы применяем только высококачественные материалы и новейшее оборудование, что гарантирует долгий срок службы и прочность всех выполненных задач. Все проекты проходят тщательную проверку качества на каждой стадии реализации.
Индивидуальный подход:
Мы предлагаем каждому клиенту индивидуальные решения, учитывающие все особенности и пожелания. Наша цель – чтобы результат нашей работы соответствовал вашим ожиданиям и требованиям.
Почему выбирают Геракл24?
Сотрудничая с нами, вы получаете надежного партнера, который берет на себя все заботы по ремонту и реконструкции вашего строения. Мы обеспечиваем выполнение всех проектов в сроки, оговоренные заранее и с в соответствии с нормами и стандартами. Обратившись в Геракл24, вы можете не сомневаться, что ваш дом в надежных руках.
Мы готовы предоставить консультацию и дать ответы на все вопросы. Звоните нам, чтобы обсудить детали и получить больше информации о наших услугах. Мы обеспечим сохранение и улучшение вашего дома, сделав его уютным и безопасным для долгого проживания.
Геракл24 – ваш выбор для реставрации и ремонта домов в Красноярске и области.
ntu emergency loan Once the audit has been done, there are some who choose to downsize their home or move to a smaller apartment or a less expensive location in order to make their income more manageable.
pharmacie en ligne france livraison internationale: kamagra livraison 24h – Pharmacie Internationale en ligne
На сайте https://cliningkrd.ru вы сможете заказать обратный звонок для того, чтобы воспользоваться услугами клининговой компании «Cleaning». Здесь оказываются профессиональные услуги компетентными, проверенными специалистами. В работе применяется инновационное, высокотехнологичное оборудование, которое справляется с загрязнениями различного уровня интенсивности. Бытовая химия, чистящие средства от надежных брендов, которые создают полностью безопасную для людей, животных продукцию.
Теневой плинтус: стильное решение для обновления интерьера,
Советы по монтажу теневого плинтуса без дополнительной помощи,
Креативные способы использования теневого плинтуса в дизайне помещения,
Теневой плинтус: классический стиль в современном исполнении,
Гармония оттенков: выбор цвета теневого плинтуса для любого интерьера,
Безопасность и стиль: почему теневой плинтус – идеальное решение для дома,
Теневой плинтус с подсветкой: создаем эффектное освещение в интерьере,
Как сделать помещение завершенным с помощью теневого плинтуса,
Интерьер безупречный до мелочей: роль теневого плинтуса в декоре
плинтус купить https://plintus-tenevoj-aljuminievyj-msk.ru/ .
Теневой плинтус: стильное решение для обновления интерьера,
Как правильно установить теневой плинтус своими руками,
Теневой плинтус как элемент декора: идеи и варианты применения,
Ретро-стиль с использованием теневых плинтусов: идеи для вдохновения,
Советы стилиста: как сделать цвет теневого плинтуса акцентом в помещении,
Безопасность и стиль: почему теневой плинтус – идеальное решение для дома,
Интересные решения с теневым плинтусом и подсветкой: идеи для вдохновения,
Современные тренды в использовании теневого плинтуса для уюта и красоты,
Интерьер безупречный до мелочей: роль теневого плинтуса в декоре
алюминиевые плинтуса напольные алюминиевые плинтуса напольные .
Почему теневой плинтус – красивая и практичная деталь интерьера,
Как правильно установить теневой плинтус своими руками,
Теневой плинтус как элемент декора: идеи и варианты применения,
Модные тренды в выборе теневых плинтусов для современного дома,
Как подобрать цвет теневого плинтуса к отделке стен,
Как спрятать коммуникации с помощью теневого плинтуса: практические советы,
Теневой плинтус с подсветкой: создаем эффектное освещение в интерьере,
Теневой плинтус: элегантность и стиль в дизайне помещения,
Интерьер безупречный до мелочей: роль теневого плинтуса в декоре
высота теневого плинтуса https://plintus-tenevoj-aljuminievyj-msk.ru/ .
線上娛樂城的天地
隨著互聯網的快速發展,網上娛樂城(在線賭場)已經成為許多人娛樂的新選擇。在線娛樂城不僅提供多種的遊戲選擇,還能讓玩家在家中就能體驗到賭場的刺激和樂趣。本文將討論在線娛樂城的特點、利益以及一些常見的的遊戲。
什麼在線娛樂城?
在線娛樂城是一種經由網際網路提供賭錢游戲的平台。玩家可以通過電腦設備、手機或平板進入這些網站,參與各種博彩活動,如撲克牌、輪盤賭、二十一點和吃角子老虎等。這些平台通常由專業的軟件公司開發,確保游戲的公正和安全。
在線娛樂城的優勢
便利:玩家不用離開家,就能享用博彩的樂趣。這對於那些住在在遠離實體賭場地方的人來說尤其方便。
多樣化的遊戲選擇:在線娛樂城通常提供比實體賭場更多樣化的遊戲選擇,並且經常改進游戲內容,保持新鮮感。
福利和獎勵:許多在線娛樂城提供多樣的獎勵計劃,包括註冊紅利、存款獎勵和忠誠計劃,引誘新玩家並鼓勵老玩家繼續遊戲。
穩定性和隱私性:正規的線上娛樂城使用先進的的加密技術來保護玩家的私人信息和財務交易,確保游戲過程的安全和公正。
常有的在線娛樂城遊戲
德州撲克:撲克是最受歡迎賭博遊戲之一。網上娛樂城提供多樣撲克牌變體,如德州撲克、奧馬哈撲克和七張牌等。
賭盤:賭盤是一種古老的賭場遊戲,玩家可以賭注在單數、數字組合上或顏色上,然後看球落在哪個地方。
二十一點:又稱為二十一點,這是一種競爭玩家和莊家點數的游戲,目標是讓手牌點數盡可能接近21點但不超過。
吃角子老虎:老虎机是最容易也是最流行的博彩游戲之一,玩家只需旋轉捲軸,等待圖案圖案排列出中獎的組合。
總結
網上娛樂城為現代的賭博愛好者提供了一個便捷、刺激且豐富的娛樂選擇。不管是撲克迷還是老虎机愛好者,大家都能在這些平台上找到適合自己的遊戲。同時,隨著科技的不斷提升,線上娛樂城的游戲體驗將變化越來越逼真和有趣。然而,玩家在體驗遊戲的同時,也應該保持自律,避免沉溺於賭博活動,保持健康健康的遊戲心態。
need a quick loan no credit check The phone calls and emails come from someone using a free email address such as @ or @ and asks for a call back at a number that is not ours.
Грузовики HOWO и Sinotruk в наличии и под заказ на https://partnerauto.ru/ от компании ООО «Новая высота» – это возможность выгодно купить китайские грузовики с доставкой в любую точку РФ. Доступные цены и удобный сервис. Подробнее на сайте.
pharmacie en ligne pas cher: cialis generique – vente de mГ©dicament en ligne
Use protective equipment, use tools britainsnews.com and equipment according to the rules so as not to encounter difficulties.
ascorbic acid monstrous – ascorbic acid narrow ascorbic acid casual
На сайте https://ru.cryptolegalservices.io/ вы сможете воспользоваться такими полезными услугами, как: оформление крипто-лицензии, нормативный анализ, аудит. Вы сможете воспользоваться бухгалтерскими, налоговыми услугами для тех компаний, которые работают с токенами. Также можно приобрести и недвижимость за токены. Предприятие обслуживает частных лиц, а также различные криптовалютные биржи. Специалисты работают таким образом, чтобы вы смогли работать максимально безопасно и с комфортом.
На сайте https://pacific-map.com/index.html представлены карты с городами, штатами. Перед вами самая подробная карта дорог, которые имеются в США. Крупномасштабные карты содержат самое подробное описание, координаты, а потому вы можете ориентироваться на данную информацию. Это огромная карта со всеми подробностями и важной информацией. Есть карта со штатами, а также Атлантического, Тихоокеанского Побережья. Открыть карту получится с любого устройства и где бы вы ни находились. Все детали отлично видны.
canadatc.com
На сайте https://smsi.vip/ вы сможете зарегистрироваться для того, чтобы воспользоваться сервисом смс активаций. Только для вас очень быстрый прием сообщений, огромный выбор сервисов для того, чтобы осуществить смс активацию. Также доступна и переадресация звонков на свой номер. Вы сможете воспользоваться арендой номера для того, чтобы отправлять, принимать смс. Для всех клиентов предоставляются индивидуальные номера. Все, что необходимо – просто пополнить баланс, а затем подобрать услугу.
https://homes-design.ru/
Сайт Украиночка предлагает интересную и полезную информацию. Наша основная миссия – помочь вам быть уверенной и образованной. Мы считаем, что вы заслуживаете только лучшего. Вдохновим вас на достижение новых вершин в любых аспектах жизни. Раскроем большой спектр возможностей для самовыражения и саморазвития. ukrayinochka.com – https://ukrayinochka.com портал, где есть все, что интересно современным женщинам: от актуальных новостей до занимательных советов. Заходите на наш сайт уже сейчас. Вас ждет качественный контент!
i need a cash loan If you are unable to repay your loan before your loan is due, you may request an installment plan with no additional fees.
На сайте https://t.me/s/gatesofolympus_1win вы сможете получить всю необходимую официальную информацию, которая касается канала «Gates of Olympus». Здесь самая актуальная, правдивая информация, которая вам потребуется, если вам нравятся азартные развлечения. Многие пользователи отмечают то, что у компании высокая вероятность получения выигрыша. Перед вами огромное количество интересных, увлекательных слотов, развлечений, которыми вы сможете воспользоваться прямо сейчас.
If you need to weld elements, you moneytimenews.com should trust the work of a welder with the necessary skills. Welding work must be carried out under control.
На сайте https://sales-sport.ru/ почитайте интересные и содержательные материалы на тему моды, красоты, здоровья. Перед вами самые интересные, свежие публикации, которые точно вам понравятся. Вы узнаете о том, как правильно подобрать женские сапоги, короткое свадебное платье, а также брюки для подростка. Имеются материалы о том, как подобрать солнцезащитные очки, про проектирование, а также монтаж инженерных коммуникаций. Также есть данные о том, правильно выровнять бетонный пол, как подобрать стоматологическую клинику.
На сайте https://dolinakamnej.ru приобретите минералы, натуральные камни, а также интересные и необычные изделия, которые понравятся даже истинному эстету. Доставка осуществляется в любую точку мира, России. Компания отличается собственным производством, а потому установила привлекательные и доступные цены. Здесь же есть возможность воспользоваться и такими популярными, нужными услугами, как полировка, распиловка на заказ. Все услуги оказываются качественно, в соответствии с самыми высокими требованиями.
Viagra homme prix en pharmacie sans ordonnance: SildГ©nafil 100mg pharmacie en ligne – Acheter viagra en ligne livraison 24h
brillx casino официальный сайт
brillx официальный сайт
Предоставив широкий спектр игр и вариантов ставок, мы делаем ставку на то, что каждый игрок найдет что-то особенное для себя. Brillx Казино – это не просто место для азартных игр, это место, где рождаются легенды и судьбы переплетаются с риском.Играя на Brillx Казино, вы можете быть уверены в честности и безопасности своих данных. Мы используем передовые технологии для защиты информации наших игроков, так что вы можете сосредоточиться исключительно на игре и наслаждаться процессом без каких-либо сомнений или опасений.
На сайте https://gazelka86.ru/ закажите грузоперевозки с хорошей скидкой до 50%. Это очень удобно, потому как в компании работают первоклассные, компетентные специалисты, которые выполнят все работы на высоком уровне, профессионально и качественно. Под груз выделяется свой транспорт, который подбирается в соответствии с габаритами, объемом, весом. Предоставляется полный комплекс услуг, чтобы вы воспользовались именно тем, что нужно. Учитывая небольшую стоимость, дается еще и скидка.
Посетите сайт https://seovgeo.ru/ где вы сможете заказать продвижение на яндекс картах, продвижение компании в яндекс картах, продвижение организации на яндекс картах, сео продвижение на яндекс картах, продвижение через яндекс карты и многие другие услуги с индивидуальным подходом от профессионалов по выгодным ценам. Подробнее на сайте.
aboutweeks.com
ascorbic acid become – ascorbic acid issue ascorbic acid how
indian reservation short term loans The use of cookies by our third-party tracking utility companies is not covered by our Privacy Policy.
promethazine skirt – promethazine nobody promethazine whenever
The second option is a self-propelled unit, which bmoneyfinder.com has an engine, wheels and its own drive for lifting a fork with a load. These are the ones most often used in warehouses, but only if there is a sufficient amount of free space.
newsplaces.net
Новые технологии и материалы – компания, которая занимается производством комплектующих для радиотехнической промышленности. Предлагаем вам недорого приобрести крепеж и метизы. Строго следим за качеством продукции и поставляем ее в указанные сроки. Готовы предоставить профессиональную консультацию и оказать помощь в оформлении товара. https://ntmsp.ru/ – сайт, где у вас есть возможность уже сегодня посмотреть акции. У нас работают надежные и квалифицированные люди. Свяжитесь со специалистами по телефону, и они ответят на интересующие вас вопросы.
Незаменимая часть гардероба – тактичные штаны, подчеркнут ваш стиль.
Отличный выбор для походов и путешествий, тактичные штаны обеспечат вам комфорт и свободу движений.
Надежный пошив и долговечность, сделают тактичные штаны вашим незаменимым спутником.
Максимальный комфорт и стильный вид, порадуют даже самого взыскательного покупателя.
Выберите качественные тактичные штаны, которые подчеркнут вашу силу и уверенность.
тактичні штани жіночі https://taktichmishtanu.kiev.ua/ .
This is due to comfortable living newsgary.com conditions, a warm sea, a variety of tourism services in the country, high-quality food and a relatively economical cost of travel. For the optimal travel option, you should choose a tour on the website, where there are a large number of offers.
На сайте https://t.me/m1xbet_ru ознакомьтесь с актуальной и интересной информацией, которая касается проекта «1XBET». Заходите на официальный канал и ознакомьтесь со всеми интересующими новостями, актуальными данными, которые вызовут интерес у всех игроков и любителей азарта. На этом сайте постоянно публикуются свежие, интересные новости из мира ставок и гемблинга. Воспользуйтесь и вы возможностью узнать первым о промокодах, предстоящих акциях. Заходить на канал можно в любое время и с любого гаджета.
Магазин, где можно выбрать серая раковина в ванную под любой интерьер.
Стильные и удобные тактичные штаны, дадут комфорт и уверенность.
Незаменимые для занятий спортом, тактичные штаны подарят вам удобство и защиту.
Высокое качество и непревзойденный комфорт, сделают тактичные штаны вашим незаменимым спутником.
Максимальный комфорт и стильный вид, порадуют даже самого взыскательного покупателя.
Почувствуйте удобство и стиль в тактичных штанах, дадут вам комфорт и свободу.
військові штани з наколінниками військові штани з наколінниками .
Выбор современных мужчин – тактичные штаны, которые подчеркнут вашу индивидуальность.
Идеальный вариант для активного отдыха, тактичные штаны станут вашим надежным помощником.
Качественные материалы и прочные швы, сделают тактичные штаны незаменимым атрибутом вашего образа.
Максимальный комфорт и стильный вид, делают тактичные штаны незаменимым вещью в гардеробе каждого мужчины.
Почувствуйте удобство и стиль в тактичных штанах, которые подчеркнут вашу силу и уверенность.
штани військові з наколінниками https://taktichmishtanu.kiev.ua/ .
Незаменимая часть гардероба – тактичные штаны, дадут комфорт и уверенность.
Отличный выбор для походов и путешествий, тактичные штаны подарят вам удобство и защиту.
Качественные материалы и прочные швы, сделают тактичные штаны вашим незаменимым спутником.
Идеальное сочетание функциональности и элегантности, делают тактичные штаны незаменимым вещью в гардеробе каждого мужчины.
Неотъемлемый атрибут современного мужчины – тактичные штаны, дадут вам комфорт и свободу.
штани тактичні з наколінниками https://taktichmishtanu.kiev.ua/ .
На сайте https://ruskiseerial.net/ находятся русские сериалы, которые понравятся всем без исключения. Они самого разного жанра, включая драмы, мелодрамы, комедии, а также триллеры, детективы и многое другое. Все они состоят из разного количества серий и отличаются удивительным сюжетом. По этой причине точно понравятся различной категории граждан. Для того чтобы найти лучший вариант, воспользуйтесь специальным фильтром. А для того чтобы получить доступ ко всему функционалу, необходимо зарегистрироваться.
Стильные и удобные тактичные штаны, дадут комфорт и уверенность.
Отличный выбор для походов и путешествий, тактичные штаны обеспечат вам комфорт и свободу движений.
Высокое качество и непревзойденный комфорт, сделают тактичные штаны вашим любимым предметом гардероба.
Максимальный комфорт и стильный вид, делают тактичные штаны незаменимым вещью в гардеробе каждого мужчины.
Неотъемлемый атрибут современного мужчины – тактичные штаны, которые подчеркнут вашу силу и уверенность.
купить штани тактичні купить штани тактичні .
Стильные и удобные тактичные штаны, дадут комфорт и уверенность.
Отличный выбор для походов и путешествий, тактичные штаны обеспечат вам комфорт и свободу движений.
Надежный пошив и долговечность, сделают тактичные штаны вашим любимым предметом гардероба.
Максимальный комфорт и стильный вид, порадуют даже самого взыскательного покупателя.
Почувствуйте удобство и стиль в тактичных штанах, порадуют вас надежностью и удобством.
купити тактичні штани https://taktichmishtanu.kiev.ua/ .
На сайте https://tursmir.store/ почитайте любопытную, содержательную информацию о том, как правильно отдыхать летом с пользой для организма и своего кошелька. Здесь же вы найдете и любопытные новости, которые касаются отдыха в гостиницах Сочи. Вы узнаете о том, какие нюансы таит в себе принятие солнечных ванн, есть ли вред от этого. Авторы публикуют и различные меры предосторожности, чтобы вы загорали правильно. Получите информацию о том, как забронировать отель. Возможно, вас заинтересуют различные гастрономические туры.
Стильные и удобные тактичные штаны, подчеркнут ваш стиль.
Отличный выбор для походов и путешествий, тактичные штаны подарят вам удобство и защиту.
Качественные материалы и прочные швы, сделают тактичные штаны вашим любимым предметом гардероба.
Современный стиль и практичность, порадуют даже самого взыскательного покупателя.
Неотъемлемый атрибут современного мужчины – тактичные штаны, дадут вам комфорт и свободу.
штани тактичні купити https://taktichmishtanu.kiev.ua/ .
Стильные и удобные тактичные штаны, дадут комфорт и уверенность.
Незаменимые для занятий спортом, тактичные штаны станут вашим надежным помощником.
Качественные материалы и прочные швы, сделают тактичные штаны вашим незаменимым спутником.
Современный стиль и практичность, подчеркнут вашу индивидуальность и статус.
Неотъемлемый атрибут современного мужчины – тактичные штаны, которые подчеркнут вашу силу и уверенность.
штани тактичні купити https://taktichmishtanu.kiev.ua/ .
pharmacie en ligne fiable: acheter kamagra site fiable – Achat mГ©dicament en ligne fiable
На сайте https://ruskiseerial.net/ представлены самые новые, интересные фильмы, сериалы, которые определенно заслуживают вашего внимания. Есть и ожидаемые премьеры, которые хочется посмотреть всем киноманам. Все фильмы в отличном качестве, с хорошей озвучкой. Просматривать можно на любом устройстве, включая планшет, смартфон. Для подбора определенного варианта воспользуйтесь специальным фильтром или поиском по жанру. Здесь есть как драмы, так и мелодрамы, комедии, триллеры. Опубликованы и совсем новые фильмы, вышедшие в этом году.
slot machine stands winning at slots
Выбор современных мужчин – тактичные штаны, которые подчеркнут вашу индивидуальность.
Идеальный вариант для активного отдыха, тактичные штаны станут вашим надежным помощником.
Качественные материалы и прочные швы, сделают тактичные штаны вашим любимым предметом гардероба.
Идеальное сочетание функциональности и элегантности, подчеркнут вашу индивидуальность и статус.
Почувствуйте удобство и стиль в тактичных штанах, порадуют вас надежностью и удобством.
штани тактичні https://taktichmishtanu.kiev.ua/ .
Стильные и удобные тактичные штаны, дадут комфорт и уверенность.
Отличный выбор для походов и путешествий, тактичные штаны подарят вам удобство и защиту.
Качественные материалы и прочные швы, сделают тактичные штаны незаменимым атрибутом вашего образа.
Максимальный комфорт и стильный вид, подчеркнут вашу индивидуальность и статус.
Выберите качественные тактичные штаны, дадут вам комфорт и свободу.
штани тактичні олива штани тактичні олива .
Выбор современных мужчин – тактичные штаны, подчеркнут ваш стиль.
Отличный выбор для походов и путешествий, тактичные штаны станут вашим надежным помощником.
Надежный пошив и долговечность, сделают тактичные штаны вашим незаменимым спутником.
Максимальный комфорт и стильный вид, делают тактичные штаны незаменимым вещью в гардеробе каждого мужчины.
Неотъемлемый атрибут современного мужчины – тактичные штаны, которые подчеркнут вашу силу и уверенность.
тактичні штани зимові тактичні штани зимові .
Ассоциация Безопасности Трейдинга https://trading-association.org/ это помощь в возврате денег от брокера. Зайдите на сайт, ознакомьтесь с ассоциацией, способами решения сложностей с проблемными брокерами или получите консультацию. Подробнее на сайте.
Сайт, где мне посоветовали раковина для кухни керамогранит для ванной комнаты.
Go to the site https://miglandrealestate.com/ and you can find real estate on the island of Bali. Buying, renting land or villas and houses is very simple. We present the best offers at the best prices. We have the latest information about properties in Bali.
mantra 10 tadalafil tablets
На сайте https://truba-almaty.kz/ закажите полиэтиленовые фитинги и трубы. Предприятие ТОО «ТОРГПРОМПЛАСТ» работает в этой сфере длительное время и сотрудничает как с физическими, так и юридическими лицами. Регулярно проводятся акции, действуют скидки, программа лояльности для постоянных клиентов. Работа без посредников, что позволяет снизить траты, избежать переплат. Прямо сейчас вы сможете приобрести трубы с хорошей скидкой. Есть своя производственная база, укомплектованная высокотехнологичным оборудованием.
На сайте https://premier-pokrytie.ru/ есть возможность заказать резиновое покрытие, которое используется внутри помещения, а также на детских, спортивных площадках. В компании трудятся компетентные и лучшие специалисты, у которых огромный опыт работы в данной сфере. Они в совершенстве знакомы с технологией создания резинового покрытия, что позволяет предложить продукт безупречного качества и с уникальными техническими характеристиками. Специалист приедет к вам на объект для замеров абсолютно бесплатно.
На сайте https://womans-life.ru почитайте актуальную, ценную и интересную информацию на самую разную тему. К примеру, вы узнаете о том, как новогодние праздники отражаются на здоровье, о методиках выведения прыщей в домашних условиях, каким образом лучше всего зашить обувь, как правильно завязать шарф на голове. Представлены самые разные интересные советы, которые помогут решить проблему. Есть и нужные сведения о том, как правильно соединить чулки с поясом. Опубликованы рекомендации от медиков, которые помогут избавиться от болей в поджелудочной железе.
Сайт uafakty.com.ua нравится пользователям лаконичностью оформления. Здесь имеются темы спорта, политики и культуры. Вас ждут интересные новости шоу-бизнеса. Получайте удовольствие от лучшего контента! uafakty.com.ua – https://uafakty.com.ua сайт, который будет вам понятен, он ценится за оперативность и объективность. Тут имеется много полезной информации, ознакомиться с ней можно в любое удобное время. Все статьи удобны для чтения и снабжены фотографиями. Заходите уже сейчас на наш известный портал и читайте последние новости!
Портал chasnovyn.com.ua – это источник текущих новостей Украины, которые доступны круглосуточно. Статьи снабжены четкими фотографиями. Всех своих читателей ценим и гордимся тем, что у нас есть возможность для них предложить только лучшее. Устраивайтесь поудобнее и читайте важную информацию. chasnovyn.com.ua – https://chasnovyn.com.ua портал, который вашего внимания точно заслуживает. Здесь затрагиваются темы политики, экономики и др. Все материалы надежные, не сомневайтесь в их качестве. Посетите наш ресурс и будете в курсе актуальных событий!
На сайте https://t.me/mvulkan_ru получите интересную, увлекательную информацию о казино «Вулкан 24». Официальный канал теперь находится в вашем мобильном телефоне. Это заведение считается лидером в своем сегменте, а потому ему точно можно доверять. Предлагает огромный выбор автоматов на любой вкус, много развлечений, которые точно понравятся и вам. На канале несколько тысяч записей, а также есть фотографии. Воспользуйтесь и вы возможностью попытать свою удачу, сыграв в интересные развлечения.
haywire slot machine horeshoe casino hammond in
vente de mГ©dicament en ligne: pharmacie en ligne sans ordonnance – pharmacie en ligne fiable
На сайте http://ritualnoe-buro-vrn.ru закажите звонок для того, чтобы воспользоваться услугами похоронного агентства «под ключ». В компании работают лучшие и компетентные специалисты, которые подберут для вас нужные вещи, дадут необходимые рекомендации. Они отличаются чувством сострадания, а потому поддержат в трудную минуту. Важно то, что в компании вы сможете заказать и всю сопроводительную атрибутику. Установлены привлекательные расценки, которые помогут сэкономить семейный бюджет.
На сайте https://ntmsp.ru/ закажите звонок для того, чтобы воспользоваться услугами популярной компании ООО «НОВЫЕ ТЕХНОЛОГИИ И МАТЕРИАЛЫ». Она предпринимает все возможное для того, чтобы создать продукцию эталонного качества и соответствующую самым высоким требованиям. В каталоге вы найдете крепеж, ферритовые изделия, медицинские иглы, а также оснастку и многое другое. Все это эталонного качества, реализуется по привлекательной стоимости. В компании трудятся компетентные, надежные специалисты, которые на совесть выполняют работу.
ЗдравБудь – популярный сайт о здоровье. Здесь у вас есть возможность узнать, где искать витамины зимой, что такое микробиом, необходимо ли принимать йод для профилактики, чем может помочь нутрициолог, зачем проверяют уровень гормонов щитовидки. У нас вы также найдете рецепты вкусной еды. Мы предлагаем только интересную и полезную информацию. https://zdravbud.net/new/pochemu-bolyat-sustavy – здесь подробнее объясняем, почему суставы болят. Объясним, как действует МолекАРТ-РА. Заходите на наш портал уже сейчас, вас ждут самые лучшие статьи!
На сайте https://uss.eu.com изучите интересную, увлекательную и свежую информацию на самую разную тему. Здесь опубликован материал о красивых украшениях. Предлагается ознакомиться с бестселлерами. Также есть данные о том, как правильно увеличить свой охват в Интернете. Имеется полный список компаний, которые пригодятся владельцам предприятий. Обязательно ознакомьтесь со списком лучших форумов, которые представлены в Интернете. Опубликованы и самые лучшие, проверенные англоязычные форумы, на которые вы сможете зайти прямо сейчас.
সবচেয়ে জনপ্রিয় খেলা এবং স্বাগত বোনাস
স্বাগত বোনাস এবং অন্যান্য আকর্ষণীয় বোনাসগুলি পেতে এবং সরাসরি ক্রিকেট এক্সচেঞ্জে অংশগ্রহণ করে আপনি এখনি সহযোগিতা করতে পারেন ক্রিকেট এফিলিয়েট প্রোগ্রামের মাধ্যমে। এই প্রোগ্রামের মাধ্যমে আপনি সাধারণ আয় করতে পারেন এবং সাথেই অন্যান্য সুযোগ পাওয়ার অধিকার দিতে পারেন।
এই রোমাঞ্চকর বোনাস গুলি যেগুলি আপনি উপভোগ করতে পারেন এবং আরও অনেক কিছুই আপনাকে আকর্ষণ করতে পারে। প্রথম আমানতে 200% বোনাস পান এবং প্রতিদিন ১০০% বোনাস পেতে অংশগ্রহণ করুন। এছাড়াও, সাপ্তাহিক এফবি শেয়ার করে ১০০ টাকা বোনাস পান।
এই সময়ে ক্রিকেট এক্সচেঞ্জ সরাসরি সরাসরি খেলা এবং জনপ্রিয় খেলা এবং জনপ্রিয় খেলা – ব্যাকারাট, লাইভশো, ফিশিং, এবং স্লট আমাদের নিখুঁতভাবে চেষ্টা করুন। এই সাইটে আপনি 9wicket, crickex affiliate login এবং crickex login সাথে যোগাযোগ করতে পারেন।
তাহলে, আপনি কি অপেক্ষা করছেন? এখনই যোগ দিন এবং সবচেয়ে জনপ্রিয় খেলা এবং স্বাগত বোনাস পান!
Welcome to Cricket Affiliate | Kick off with a smashing Welcome Bonus !
First Deposit Fiesta! | Make your debut at Cricket Exchange with a 200% bonus.
Daily Doubles! | Keep the scoreboard ticking with a 100% daily bonus at 9wicket!
#cricketaffiliate
IPL 2024 Jackpot! | Stand to win ₹50,000 in the mega IPL draw at cricket world!
Social Sharer Rewards! | Post and earn 100 tk weekly through Crickex affiliate login.
https://www.cricket-affiliate.com/
#cricketexchange #9wicket #crickexaffiliatelogin #crickexlogin
crickex login VIP! | Step up as a VIP and enjoy weekly bonuses!
Join the Action! | Log in through crickex bet exciting betting experience at Live Affiliate.
Dive into the game with crickex live—where every play brings spectacular wins !
dnews7.com
Couriers receive earned funds by transfer to the card payusainvest.com every week or more often, if necessary. Self-employed employees receive payments directly to the card, they are credited within 1-2 days.
Olymp Trade https://olymptrade-app.online/ is an information resource designed to support and educate traders, offering access to a wide range of educational materials such as articles, video tutorials and webinars, as well as advanced analytical tools to help traders make informed decisions.
Olymp Trade https://olymptrade-app.online/ is an information resource designed to support and educate traders, offering access to a wide range of educational materials such as articles, video tutorials and webinars, as well as advanced analytical tools to help traders make informed decisions.
ЗдравБудь – популярный сайт о здоровье. Здесь узнаете, что такое микробиом, чем может помочь нутрициолог, где искать витамины зимой, зачем проверяют уровень гормонов щитовидки, необходимо ли принимать йод для профилактики и др. Тут же вы найдете и рецепты наивкуснейшей еды. Мы предоставляем исключительно полезную и интересную информацию. https://zdravbud.net/new/pochemu-bolyat-sustavy – тут детально рассказываем, почему болят суставы. Объясним, как действует МолекАРТ-РА. Заходите на наш портал уже сейчас, вас ждут самые лучшие статьи!
На сайте https://ruuserial.net/ посмотрите интересные, увлекательные, новые, а также полюбившиеся сериалы, которые откроют для вас новые горизонты. В них играют талантливые актеры, которые у всех на устах. Для того чтобы подобрать определенный фильм, необходимо воспользоваться специальным фильтром по жанру: комедия, триллер, драма, криминал, детективы, военные. Также получится сделать подборку и по году выпуска. Регулярно на сайте происходят обновления, чтобы вы посмотрели такое кино, которое хочется.
На сайте https://truba-almaty.kz/ закажите полиэтиленовые фитинги и трубы. Предприятие ТОО «ТОРГПРОМПЛАСТ» работает в этой сфере длительное время и сотрудничает как с физическими, так и юридическими лицами. Регулярно проводятся акции, действуют скидки, программа лояльности для постоянных клиентов. Работа без посредников, что позволяет снизить траты, избежать переплат. Прямо сейчас вы сможете приобрести трубы с хорошей скидкой. Есть своя производственная база, укомплектованная высокотехнологичным оборудованием.
Портал chasnovyn.com.ua – это источник текущих новостей Украины, которые доступны круглосуточно. Статьи снабжены четкими фотографиями. Мы ценим своих читателей и гордимся тем, что можем предложить им самое лучшее. Поудобнее устраивайтесь и достоверную информацию читайте уже сейчас. chasnovyn.com.ua – https://chasnovyn.com.ua сайт, который действительно заслуживает вашего внимания. Здесь затрагиваются темы политики, экономики и др. Все материалы проверены на достоверность, можете быть уверены в их качестве. Заходите на наш сайт и будьте в курсе всех событий!
Портал uafakty.com.ua его пользователи отмечают лаконичность оформления. Здесь имеются темы спорта, политики и культуры. Вас ждут актуальные новости шоу-бизнеса. Получайте удовольствие от лучшего контента! uafakty.com.ua – https://uafakty.com.ua сайт, который будет вам понятен, он ценится за оперативность и объективность. Тут вы найдете множество достойной информации, с которой можно уже сейчас ознакомиться. Все без исключения статьи снабжены фото и удобны для чтения. Заходите на наш популярный сайт и читайте актуальные новости в любое время!
На сайте https://t.me/m1xbet_ru ознакомьтесь с актуальной и интересной информацией, которая касается проекта «1XBET». Заходите на официальный канал и ознакомьтесь со всеми интересующими новостями, актуальными данными, которые вызовут интерес у всех игроков и любителей азарта. На этом сайте постоянно публикуются свежие, интересные новости из мира ставок и гемблинга. Воспользуйтесь и вы возможностью узнать первым о промокодах, предстоящих акциях. Заходить на канал можно в любое время и с любого гаджета.
На сайте https://ntmsp.ru/ закажите звонок для того, чтобы воспользоваться услугами популярной компании ООО «НОВЫЕ ТЕХНОЛОГИИ И МАТЕРИАЛЫ». Она предпринимает все возможное для того, чтобы создать продукцию эталонного качества и соответствующую самым высоким требованиям. В каталоге вы найдете крепеж, ферритовые изделия, медицинские иглы, а также оснастку и многое другое. Все это эталонного качества, реализуется по привлекательной стоимости. В компании трудятся компетентные, надежные специалисты, которые на совесть выполняют работу.
На сайте https://uss.eu.com изучите интересную, увлекательную и свежую информацию на самую разную тему. Здесь опубликован материал о красивых украшениях. Предлагается ознакомиться с бестселлерами. Также есть данные о том, как правильно увеличить свой охват в Интернете. Имеется полный список компаний, которые пригодятся владельцам предприятий. Обязательно ознакомьтесь со списком лучших форумов, которые представлены в Интернете. Опубликованы и самые лучшие, проверенные англоязычные форумы, на которые вы сможете зайти прямо сейчас.
На сайте http://ritualnoe-buro-vrn.ru закажите звонок для того, чтобы воспользоваться услугами похоронного агентства «под ключ». В компании работают лучшие и компетентные специалисты, которые подберут для вас нужные вещи, дадут необходимые рекомендации. Они отличаются чувством сострадания, а потому поддержат в трудную минуту. Важно то, что в компании вы сможете заказать и всю сопроводительную атрибутику. Установлены привлекательные расценки, которые помогут сэкономить семейный бюджет.
На сайте https://sobr26.ru ознакомьтесь с номером телефона охранной организации СОБР. Здесь оказываются услуги, связанные с охраной недвижимости, организуется безопасность объекта, есть возможность воспользоваться физической охраной, которая оказывается более 20 лет. Прямо сейчас вы сможете рассчитывать на бесплатную консультацию. Каждый клиент сможет организовать пультовую, физическую охрану, пожарную сигнализацию, видеонаблюдение. Для того чтобы воспользоваться услугами, оставьте заявку непосредственно на сайте.
На сайте https://womans-life.ru почитайте актуальную, ценную и интересную информацию на самую разную тему. К примеру, вы узнаете о том, как новогодние праздники отражаются на здоровье, о методиках выведения прыщей в домашних условиях, каким образом лучше всего зашить обувь, как правильно завязать шарф на голове. Представлены самые разные интересные советы, которые помогут решить проблему. Есть и нужные сведения о том, как правильно соединить чулки с поясом. Опубликованы рекомендации от медиков, которые помогут избавиться от болей в поджелудочной железе.
На сайте https://t.me/mvulkan_ru получите интересную, увлекательную информацию о казино «Вулкан 24». Официальный канал теперь находится в вашем мобильном телефоне. Это заведение считается лидером в своем сегменте, а потому ему точно можно доверять. Предлагает огромный выбор автоматов на любой вкус, много развлечений, которые точно понравятся и вам. На канале несколько тысяч записей, а также есть фотографии. Воспользуйтесь и вы возможностью попытать свою удачу, сыграв в интересные развлечения.
Go to the site https://miglandrealestate.com/ and you can find real estate on the island of Bali. Buying, renting land or villas and houses is very simple. We present the best offers at the best prices. We have the latest information about properties in Bali.
carsinfo.net
Take care of your own health. It dailymoneysource.com is difficult for people with allergies or people with disabilities to do cleaning, so ordering cleaning services is simply necessary for them.
Краснодарский завод производит котельное оборудование, которое проходит, регламентированные технические испытания и отвечает всем требованиям безопасности. Работаем по всей РФ и ряду стран СНГ. С нами вы сэкономите свои деньги и время. Ищете паровой котел для котельной? Kzko-gaz.ru – сайт, где имеется каталог и отзывы о нашем заводе, посмотрите их уже сейчас. Любой изготавливаемый котел либо же котельная будут в срок доставлены, не сомневайтесь. Гарантируем качество, создавая тепло!
Find Stimulating Promotions and Extra Spins: Your Definitive Guide
At our gaming platform, we are devoted to providing you with the best gaming experience possible. Our range of offers and bonus spins ensures that every player has the chance to enhance their gameplay and increase their chances of winning. Here’s how you can take advantage of our awesome promotions and what makes them so special.
Lavish Bonus Spins and Rebate Promotions
One of our standout offers is the opportunity to earn up to 200 free spins and a 75% refund with a deposit of just $20 or more. And during happy hour, you can unlock this bonus with a deposit starting from just $10. This unbelievable offer allows you to enjoy extended playtime and more opportunities to win without breaking the bank.
Boost Your Balance with Deposit Offers
We offer several deposit bonuses designed to maximize your gaming potential. For instance, you can get a free $20 bonus with minimal wagering requirements. This means you can start playing with extra funds, giving you more chances to explore our vast array of games and win big. Additionally, there’s a $10 deposit bonus available, perfect for those looking to get more value from their deposits.
Multiply Your Deposits for Bigger Wins
Our “Play Big!” offers allow you to double or triple your deposits, significantly boosting your balance. Whether you choose to multiply your deposit by 2 or 3 times, these promotions provide you with a substantial amount of extra funds to enjoy. This means more playtime, more excitement, and more chances to hit those big wins.
Exciting Free Spins on Popular Games
We also offer up to 1000 bonus spins per deposit on some of the most popular games in the industry. Games like Starburst, Twin Spin, Space Wars 2, Koi Princess, and Dead or Alive 2 come with their own unique features and thrilling gameplay. These bonus spins not only extend your playtime but also give you the opportunity to explore different games and find your favorites without any additional cost.
Why Choose Our Platform?
Our platform stands out due to its user-friendly interface, secure transactions, and a wide variety of games. We prioritize your gaming experience by ensuring that all our offers are easy to access and beneficial to our players. Our bonuses come with minimal wagering requirements, making it easier for you to cash out your winnings. Moreover, the variety of games we offer ensures that there’s something for every type of player, from classic slot enthusiasts to those who enjoy more modern, feature-packed games.
Conclusion
Don’t miss out on these incredible opportunities to enhance your gaming experience. Whether you’re looking to enjoy bonus spins, cashback, or lavish deposit bonuses, we have something for everyone. Join us today, take advantage of these incredible deals, and start your journey to big wins and endless fun. Happy gaming!
Uncover Thrilling Promotions and Extra Spins: Your Comprehensive Guide
At our gaming platform, we are devoted to providing you with the best gaming experience possible. Our range of deals and free spins ensures that every player has the chance to enhance their gameplay and increase their chances of winning. Here’s how you can take advantage of our awesome promotions and what makes them so special.
Lavish Extra Spins and Rebate Bonuses
One of our standout offers is the opportunity to earn up to 200 free spins and a 75% rebate with a deposit of just $20 or more. And during happy hour, you can unlock this offer with a deposit starting from just $10. This incredible promotion allows you to enjoy extended playtime and more opportunities to win without breaking the bank.
Boost Your Balance with Deposit Bonuses
We offer several deposit bonuses designed to maximize your gaming potential. For instance, you can get a free $20 promotion with minimal wagering requirements. This means you can start playing with extra funds, giving you more chances to explore our vast array of games and win big. Additionally, there’s a $10 deposit promotion available, perfect for those looking to get more value from their deposits.
Multiply Your Deposits for Bigger Wins
Our “Play Big!” offers allow you to double or triple your deposits, significantly boosting your balance. Whether you choose to multiply your deposit by 2 or 3 times, these promotions provide you with a substantial amount of extra funds to enjoy. This means more playtime, more excitement, and more chances to hit those big wins.
Exciting Free Spins on Popular Games
We also offer up to 1000 free spins per deposit on some of the most popular games in the industry. Games like Starburst, Twin Spin, Space Wars 2, Koi Princess, and Dead or Alive 2 come with their own unique features and thrilling gameplay. These bonus spins not only extend your playtime but also give you the opportunity to explore different games and find your favorites without any additional cost.
Why Choose Our Platform?
Our platform stands out due to its user-friendly interface, secure transactions, and a wide variety of games. We prioritize your gaming experience by ensuring that all our offers are easy to access and beneficial to our players. Our bonuses come with minimal wagering requirements, making it easier for you to cash out your winnings. Moreover, the variety of games we offer ensures that there’s something for every type of player, from classic slot enthusiasts to those who enjoy more modern, feature-packed games.
Conclusion
Don’t miss out on these incredible opportunities to enhance your gaming experience. Whether you’re looking to enjoy bonus spins, cashback, or generous deposit bonuses, we have something for everyone. Join us today, take advantage of these incredible deals, and start your journey to big wins and endless fun. Happy gaming!
Key Factors for Success: Enhancing Your Experience on Betvisa Login Sites in 2024
As the world of online gambling continues to evolve at a rapid pace, it’s essential for players to stay ahead of the curve and adapt their strategies accordingly. Whether you’re a seasoned player or just starting your journey, keeping a keen eye on the key factors that can enhance your online gambling experience is crucial, especially when navigating platforms like Betvisa Login.
Prioritizing Secure and Trusted Platforms
In the ever-changing landscape of online gambling, selecting a reputable and trustworthy platform is the foundation for a successful and enjoyable experience. Betvisa Login has established itself as a leading destination, renowned for its commitment to player safety, secure transactions, and robust licensing and regulation. By choosing platforms like Betvisa Login, you can rest assured that your personal and financial information is protected, allowing you to focus on the thrill of the game.
Mastering Game Strategies
The diverse range of games available on Betvisa Login platforms requires a deeper understanding of the underlying strategies and mechanics. From the nuances of Visa Bet to the intricacies of the Betvisa Casino offerings, taking the time to familiarize yourself with the rules, payouts, and winning techniques can significantly improve your chances of success. Utilize free demo versions and educational resources to hone your skills before diving into real-money play.
Capitalizing on Bonuses and Promotions
Online gambling platforms, including Betvisa Login, often offer a range of bonuses and promotions to attract and retain players. From welcome bonuses to free spins and reload offers, these incentives can provide you with valuable extra funds to explore the platform’s offerings. However, it’s crucial to read the terms and conditions carefully to ensure you maximize the potential benefits and avoid any unintended consequences.
Maintaining a Balanced Approach
Responsible gambling practices are essential for a sustainable and enjoyable online gambling experience. Betvisa Login encourages players to set and adhere to personal limits on both time and financial resources. By maintaining a balanced approach, you can ensure that your online gambling activities remain a source of entertainment rather than a source of stress or financial burden.
Staying Informed and Adaptable
The online gambling landscape is constantly evolving, with new games, regulations, and industry trends emerging on a regular basis. To stay ahead of the curve, it’s crucial to stay informed about the latest developments. Follow industry news, join online communities, and subscribe to Betvisa Login’s communication channels to ensure you’re always up-to-date on the latest opportunities and best practices.
Leveraging Customer Support
When navigating the complexities of online gambling, having access to reliable and responsive customer support can make a significant difference. Betvisa Login’s support team is dedicated to addressing player inquiries and resolving any issues that may arise, ensuring a seamless and stress-free experience.
As we usher in the new year, 2024 promises to be an exciting time for online gambling enthusiasts. By focusing on the key factors outlined above and leveraging the robust offerings of platforms like Betvisa Login, players can elevate their online gambling experience, maximize their chances of success, and embrace the thrilling opportunities that lie ahead.
Betvisa Bet | Step into the Arena with Betvisa!
Spin to Win Daily at Betvisa PH! | Take a whirl and bag ₱8,888 in big rewards.
Valentine’s 143% Love Boost at Visa Bet! | Celebrate romance and rewards !
Deposit Bonus Magic! | Deposit 50 and get an 88 bonus instantly at Betvisa Casino.
#betvisa
Free Cash & More Spins! | Sign up betvisa login,grab 500 free cash plus 5 free spins.
Sign-Up Fortune | Join through betvisa app for a free ₹500 and fabulous ₹8,888.
https://www.betvisa-bet.com/tl
#visabet #betvisalogin #betvisacasino # betvisaph
Double Your Play at betvisa com! | Deposit 1,000 and get a whopping 2,000 free
100% Cock Fight Welcome at Visa Bet! | Plunge into the exciting world .Bet and win!
Jump into Betvisa for exciting games, stunning bonuses, and endless winnings!
pharmacies en ligne certifiГ©es: pharmacie en ligne france fiable – pharmacie en ligne france livraison internationale
Rassilka.kz оказывает высококачественные услуги. Делаем ватсап, смс, email, рассылки по Нур-Султану, Алматы и Казахстану. Сотрудничаем с разными популярными компаниями. Наша главная задача – принести всем клиентам пользу. Действия на конечный итог нацелены. https://rassilka.kz – сайт, где вы узнаете, почему нас выбирают. Здесь у вас есть возможность уже сейчас посмотреть тарифы. У вас есть возможность получить бесплатную консультацию. Свяжитесь с нами, и мы ответим на все интересующие вопросы.
Срочный заказ машины для вывоза мусора на сайте https://xn—–dlcapan5bbljbbybmd5a7f0c.xn--p1ai/ от профессионалов. От заявки до приезда 20 минут. Работаем в Москве и за МКАД. Официальная утилизация мусора, лучшие условия. Документы. Работаем с 2008 года. Звоните, пишите – консультируем круглосуточно.
vente de mГ©dicament en ligne: pharmacie en ligne – vente de mГ©dicament en ligne
ремонт телефонов в москве
выкуп авто оценка выкуп продажа авто
Наш сайт эротических рассказов https://shoptop.org/ поможет тебе отвлечься от повседневной суеты и погрузиться в мир страсти и эмоций. Богатая библиотека секс историй для взрослых пробудит твое воображение и позволит насладиться каждой строкой.
Сайт ukrayinka.com.ua пользуется невероятной популярностью и станет вам верным другом. Мы освещаем экономические и общественно-политические события в Украине. Предлагаем только качественную информацию. ukrayinka.com.ua – https://ukrayinka.com.ua сайт, который понятен любому пользователю. Здесь вы найдете статьи с хорошими фото. Рапологайтесь поудобнее и читайте новости. Готовы обеспечить вас всеми необходимыми сведениями. Если цените свежесть и наполненность, смело выбирайте наш ресурс. Вы останетесь довольны!
9 Lessons Your Parents Taught You About Best SEO Company UK best seo company uk – Samual –
purchase peptides tadalafil
На сайте https://polygrav.ru вы сможете заказать такую услугу, как производство бейджей, табличек, а также номерков, шильдиков в огромном ассортименте. Только в этой компании вы отыщите огромное количество наиболее выгодных, интересных предложений. Производство является высокотехнологичным, а потому есть возможность заказать товары в любом количестве. Также вы сможете приобрести таблички на дверь, номерки для гардероба. Вся продукция производится из высокотехнологичных материалов, которые не испортят внешний вид.
На сайте https://t.me/s/m_1go ознакомьтесь со всей важной, ценной информацией, которая касается проекта «1GO». Здесь публикуются различные акции, промокоды, также вся важная информация относительно клуба. Воспользуйтесь ей и вы, чтобы выиграть приличную сумму денег на свою мечту. В этом казино имеется все, нужно, включая классические слоты, а также удивительные новинки, которые вызовут интерес у каждого. Попытайте свои силы и вы, чтобы получить максимум пользы и приятные эмоции. На этом канале всегда появляются новые сведения, данные из сферы гемблинга.
Вывоз и утилизация мусора срочно https://vivozim-musor.pro/ закажите на сайте. Профессиональный подход, лучшие условия и цены, круглосуточная работа. Выберите удобное время для вас, а мы сделаем свою работу. Заказать вывоз мусора в Москве можно по телефону на сайте.
Dinopolis считается самым забавным онлайн-слотом, дарящий множество позитивных эмоций. Игра не оставляет никого равнодушным, потому как имеет отменную анимацию, звук и графику. Предлагаем вам захватывающее путешествие в мир динозавров. У вас есть возможность, играя, зарабатывать реальные деньги. Приготовьтесь к веселью и адреналину. https://dinopolisgame.com/ru/ – сайт, где найдете интересную информацию о данном слоте. Узнаете, сколько можно выиграть и как сделать ставку в игре Динополис. Желаем вам удачи в Dinopolis!
На сайте https://bettingsport.pro/ изучите рейтинг самых проверенных, надежных букмекерских контор. Им точно можно доверять, ведь они действительно выплачивают средства, предлагают огромное количество бонусов, различных привилегий для всех пользователей. Именно поэтому не составит труда подобрать идеального партнера для того, чтобы заработать побольше денег и сделать ставки в этом году. Только для вас лучшие конторы, к которым точно стоит присмотреться! Все правдивые отзывы игроков и многое другое только на этом сайте.
https://formomebel.ru/stoliki/na-osnovanii-iz-metalla
mikrosluchatko https://mikrocz.cz/
На сайте https://prometall.shop/ каждый желающий сможет выбрать и приобрести банные печи в сетке, в камне, отопительные печи, которые отличаются повышенной надежностью, практичностью и высоким сроком эксплуатации. Интернет-бутик предлагает только лучшие конструкции, которые принесут радость и пользу от использования. Также имеются и хиты продаж, которые выбирает большинство. Ознакомьтесь с печами в облицовке. Все изделия наделены безупречными эстетическими свойствами, а потому идеально впишутся в любую концепцию.
На сайте https://tips-for-women.ru собраны самые полезные рекомендации относительно женской красоты. Так вы получите информацию о том, что представляет собой холодная укладка, плампер для губ, а также почему волосы стали быстрее пачкаться. Также имеется интересная, уникальная информация о том, как правильно о себе заботиться, сохранить здоровье. Вы будете знать о том, как сохранить привлекательный вид надолго. Есть советы по уходу за лицом, волосами, телом. Все рекомендации от экспертов и косметологов.
На сайте https://online-igry-s-vyvodom-deneg.ru/ получите всю необходимую информацию, которая касается заработка в интернете. Перед вами та информация, которая позволит заработать средства без вложений. Представлены ценные рекомендации, которые подскажут, какими способами лучше воспользоваться. Опубликованы только самые эффективные, действительно работающие игры, которые помогут заработать на свою мечту. При этом работать получится в любое время и независимо от рабочего графика.
Taker казино обеспечивает честность и безопасность игры. Такер привлекает игроков занимательными слотами, онлайн-казино постоянно предоставляет выгодные бонусы и акции. Саппорт отзывчивый, работает оперативно и вежливо, вывод средств – быстрый. Ищете taker? Taker.bond – сайт, дизайн его превосходный, с навигацией сложностей не возникнет. Если вы решили посетить Taker casino, вам повезло, потому что здесь представлен впечатлительный выбор азартных игр. Вам скучно точно не будет. Испытайте удачу уже сегодня!
На сайте https://usiic.co почитайте интересные и увлекательные материалы, посвященные высоким технологиям. Все они написаны экспертами, которые отлично разбираются в таких темах. Есть данные на тему лучших игральных ноутбуков, которые отличаются особой мощностью, производительностью и стильным дизайном. Опубликован список самых эффективных и прогрессивных из них. Есть информация про вечный двигатель, оснащенный магнитами. Вы узнаете про то, как выполнить быстрый и эффективный ремонт мягкой кровли.
pharmacie en ligne france livraison internationale: trouver un mГ©dicament en pharmacie – pharmacie en ligne
На сайте https://batab.ru посмотрите номер телефона для того, чтобы совершить звонок для того, чтобы заказать производство номерков, табличек, бейджей, наградных досок и многого другого. Доставка всей продукции происходит максимально оперативно. А для того, чтобы ознакомиться с услугами компании и получить представление о ее работе, необходимо изучить отзывы. На всю продукцию установлены привлекательные цены. Срок доставки от 1 дня. Можно вызвать курьера. Ассортимент постоянно обновляется, чтобы вы приобрели все, что необходимо.
На сайте https://pogadaems.ru вы сможете почитать увлекательную, интересную и актуальную информацию, которая касается гаданий в режиме реального времени. Есть возможность изучить информацию о гаданиях на картах Таро, игральных, а также цыганских. Имеются интересные и любопытные картинки, которые позволят пожелать доброго утра маме. Перед вами самая интересная, увлекательная информация, которая поможет сориентироваться в теме. Обязательно ознакомьтесь с гороскопом, чтобы знать, что ожидает вас сегодня.
biaxin pills queer – asacol grunt cytotec blink
купить микронаушники микронаушник Прага
Клиника инновационной хирургии предлагает большой спектр услуг медицины. Здесь трудятся специалисты, которые помогают людям жить полноценно. Врачи любят свою работу, имеют богатый опыт и высокую квалификацию. Вы почувствуете от персонала поддержку. Ищете узи женского таза? Kix-med.ru – сайт, где есть возможность записаться на консультацию и посмотреть отзывы пациентов. Обращаясь к нам, можете быть уверены в безопасности лечения. Гарантируем доступные цены и персональный подход. Улучшим качество вашей жизни!
На сайте https://t.me/s/gatesofolympus_1win вы сможете получить всю необходимую официальную информацию, которая касается канала «Gates of Olympus». Здесь самая актуальная, правдивая информация, которая вам потребуется, если вам нравятся азартные развлечения. Многие пользователи отмечают то, что у компании высокая вероятность получения выигрыша. Перед вами огромное количество интересных, увлекательных слотов, развлечений, которыми вы сможете воспользоваться прямо сейчас.
RedStar Poker
Рум предлагает крупнейший бонус на первый депозит в индустрии – $2,000. Подойдет покеристам с крупным банкроллом. Рейкбек – 20% или 35%. Выгодные условия привлекают опытных игроков – игровое поле в RedStar сильное.
https://www.sports.ru/tribuna/blogs/onlinepokermoney/3168978.html
Portál szakemberek keresőjének https://szakiweb.hu/ -Látogass el az oldalra és találsz egy mesterembert építkezésre, javításra, ház körüli segítségre. Nagyon könnyű mestert vagy szakembert találni az országban bárhol. Vegye igénybe az oldalon található szakemberek szolgáltatásait.
http://school29chita.ru
http://kids-podolsk.ru
https://rybalka-v-rossii.ru – сайт о рыбалке в России, способах ловли рыб, и выборе правильных снастей.к
Вывоз мусора на утилизацию в Москве https://vyvoz.pro/ по лучшей цене. Постоянно на линии более 50 машин разной вместимости. Узнайте на сайте все наши услуги по утилизации, а мы приедем быстро, в течении 30 минут. Вы можете написать нам в чат на сайте или просто позвонить по телефону. Максимально быстро приедем. Заказать вывоз мусора от профессионалов у нас на сайте.
Taker – это надежное казино, которое достойно вашего внимания. Оно привлекает игроков захватывающими слотами, постоянно предлагает щедрые акции и бонусы. Вывод средств оперативный, саппорт лояльный. Ищете такер сайт? Taker.vin – сайт, у которого отменный дизайн и удобная навигация, трудностей с пользованием не будет. Если вы решили зайти на Такер, то сделали все правильно, здесь вам будет предложен широкий ассортимент лучших азартных игр. Вы точно не заскучаете. Испытайте удачу уже сейчас!
клуб английский
языковые школы москва
грузовые шины sailun
Achat mГ©dicament en ligne fiable: pharmacie en ligne pas cher – pharmacie en ligne fiable
15 . Things That Your Boss Wants You To Know About Link Building Agency Uk
You’d Known About Link Building Agency Uk Seo agency essex
шины для грейдера
купить флешку https://meflash.ru/
Del Mar Energy
biaxin library – cytotec pills truth cytotec give
http://moto50-gibson.ru
купить грузовые шины кама
Viagra 100mg prix: viagra en ligne – Viagra pas cher inde
Alptracking выполняет аренду качественного и надежного туристического снаряжения. У нас есть рюкзаки, палатки, треккинговые палки, матрасы и коврики, спальные мешки и многое другое. Полный ассортимент снаряжения можно изучить, скачав прайс-лист на нашем сайте. Ищете турмаршруты на Байкале? Alptracking.ru – здесь у вас есть возможность уже сейчас ознакомиться с контактами, отзывами и условиями проката. Всегда рады ответить на все ваши вопросы и оформить аренду нужного снаряжения. Поможем вам путешествовать с комфортом!
увеличение длины полового члена
https://operacziya-uvelichenie-chlena.ru/
https://techbullion.com/del-mar-energy-a-leader-in-manufacturing-and-installing-solar-panels-for-industrial-sites/
Хотите получить заряд положительных эмоций и отвлечься от повседневных забот? Munivi – это то, что вам необходимо. Только самое увлекательное кино, отменное качество видео ожидают вас круглосуточно. https://munivi.xyz/ – сайт, который не зависает и замечательно оформлен. Вы будете порталом довольны. Здесь представлены достойные сериалы. Можно легко найти новые и старые. Также имеется удобный поиск, воспользоваться им можете в любое время. Постоянно добавляем и обновляем базу сериалов. У нас точно отыщете для себя то, что вам понравится!
услуги бухгалтерской фирмы
Analsex Osnabruck FГјhrt Analverkehr Zu Durchfall
На сайте https://bettingsport.pro/brands/leon-bukmeker/ вы узнаете всю важную, интересную информацию о БК «Леон». В этом месте заключаются различные прогнозы на спортивные мероприятия. Вас ожидает огромное количество бонусов, лайв-события, прематчи, повышенные коэффициенты, акции и многое другое, что сделает игру более интересной, зрелищной. Интерактивные пари можно заключать круглосуточно. Ставки делают с различных устройств, в том числе, ноутбука, смартфона или ПК. Можно воспользоваться как официальным сайтом, так и приложением.
Leverage Finance Group – консалтинговая компания, которая в реализации инвестиционных проектов оказывает поддержку. Хорошо разбираемся во всех тонкостях и особенностях процесса получения грантов. Создаем действенные бизнес-планы и сопровождаем их до результатов. Ищите бизнес-план? Levfin.ru – сайт, где у вас есть возможность узнать, почему к нам нужно обратиться. Работаем с компаниями в различных отраслях, создавая ценность каждому проекту. Наши услуги дают возможность бизнесу вовремя привлекать необходимое финансирование и успешно развиваться. Мы в любое время вас сможем проконсультировать, звоните.
Ищете рабочие промокоды Яндекс Маркета? Предлагаем подписаться на канал Олега Петрова. Он здесь делится новой подборкой акций и купонов. Вы нигде не найдете в интернете как у него, такого количества промокодов. Оцените достоинства экономного шопинга. https://dzen.ru/a/ZgxKFq5bOTUwDw_w – тут есть ссылки, по которым в различных категориях можно поймать топовые скидки. Все промокоды проверены. Воспользуйтесь наилучшими предложениями, которые Петров Олег, специально для вас нашел. Делайте с радостью приобретения!
Rassilka.kz оказывает качественные услуги. Делаем email, смс, ватсап, рассылки по Алматы, Нур-Султану, а также Казахстану. Сотрудничаем с разными популярными компаниями. Наша главная задача – принести всем клиентам пользу. Действия на конечный итог нацелены. https://rassilka.kz – сайт, где вы узнаете, почему выбирают именно нас. Здесь можете в любое удобное для вас время ознакомиться с тарифами. У нас вы получите консультацию на бесплатной основе. Свяжитесь с нами, и мы ответим на все интересующие вопросы.
На сайте https://vezuviy.shop/ приобретите надежные, функциональные печи. Только здесь представлено фирменное оборудование, а также дымоходы, на которые предоставляются гарантии. Для сауны, бани, а также коттеджей вы сможете с легкостью подобрать один из предложенных вариантов. Важным преимуществом компании является то, что доставка предоставляется абсолютно бесплатно, а банный камень дают в подарок. На все аксессуары действует скидка 10%. Дверь для бани вы сможете получить в качестве приятного презента.
На сайте https://realniy-zarabotok.ru/ изучите самые эффективные, работающие методы получения средств. И самое главное, что все методы действительно работающие и эффективные. Они помогут заработать на мечту и получить больше средств. К примеру, получится заработать на партнерке, выполнить различные задания и получить за это колоссальные суммы. Вывод средств происходит на карту или электронный кошелек. Но зачастую для того, чтобы обеспечить себе доступ к тем заданиям, за которые больше платят, необходимо пройти специальный тест.
pharmacie en ligne livraison europe: kamagra en ligne – п»їpharmacie en ligne france
На сайте https://dyhu.ru/ закажите изысканные и популярные ароматы, духи от лучших и проверенных парфюмеров, которые создают продукцию для изысканного, привлекательного стиля. Каждый желающий получает возможность приобрести все, что считает нужным, оптом, чтобы разнообразить свой ассортимент и сделать его более интересным и привлекательным для клиентов. Регулярно на сайт добавляются интересные новинки, которые заслуживают вашего внимания. Также устраиваются распродажи, которые позволят сэкономить на покупке хорошие деньги.
Na stronie https://1op.pl/ prosimy o kontakt w celu skorzystania z usług związanych z Naprawa, otwieraniem zamków w Warszawie. Ponadto dostępny jest również pilny wyjazd. Firma działa przez całą dobę, co pozwala zamawiać usługi w dowolnym momencie, w tym w święta, weekendy. Mistrz przyjedzie do obiektu dosłownie w 15 minut, aby wykonać wszystkie niezbędne prace. Ponadto firma będzie dla ciebie pomocna, a jeśli zgubisz klucz, zamek nie działa lub nie obraca się, technik powinien bezpiecznie otworzyć drzwi.
payday loans in cocoa fl Requirements differ by lender but the main ones are a job, social security number and, in most cases, an active checking account.
Are you looking for reliable and fast proxies? https://fineproxy.org/account/aff.php?aff=29 It offers a wide range of proxy servers with excellent speed and reliability. Perfect for surfing, scraping and more. Start right now with this link: FineProxy.org . Excellent customer service and a variety of tariff plans!
https://proauto.kyiv.ua здесь вы найдете обзоры и тест-драйвы автомобилей, свежие новости автопрома, обширный автокаталог с характеристиками и ценами, полезные советы по уходу и ремонту, а также активное сообщество автолюбителей. Присоединяйтесь к нам и оставайтесь в курсе всех событий в мире автомобилей!
На сайте https://smile-me.ru/ вы сможете заказать звонок для того, чтобы получить консультацию относительно проведения детских праздников. Здесь вы сможете заказать детских аниматоров, устроить тематический праздник, воспользоваться услугами ведущих на мероприятие, устроить незабываемый, яркий квест или бумажное шоу. Действуют привлекательные, доступные расценки. Все мероприятия проводятся компетентными, талантливыми специалистами, которые не перестают радовать своим профессионализмом.
Вас интересует профессиональный ремонт электро-транспорта в Минске? Мастерская 911 – это то, что вам нужно! В сервисном центре трудятся самые лучшие специалисты, которые имеют достаточный опыт работы. Они великолепно разбираются в электросамокатах, качественно и оперативно их ремонтируют. https://m911.by/ – сайт, где вы можете уже сейчас посмотреть наши услуги. Мы обеспечиваем своих клиентов недорогим ремонтом любого вида электро-транспорта. Совершенно бесплатно продиагностируем поломку, обращайтесь.
best 92557 cash advance These multiple lender websites are free to use and will provide you with four instant quotes from different lenders after filling out just one online application.
Сувенирная продукция с логотипом и корпоративный мерч на заказ в Москве
https://telegra.ph/Vash-brend-v-kazhdom-zheste—sekrety-suvenirnoj-produkcii-s-logotipom-v-Moskve-05-31
https://autoclub.kyiv.ua узнайте все о новых моделях, читайте обзоры и тест-драйвы, получайте советы по уходу за авто и ремонтам. Наш автокаталог и активное сообщество автолюбителей помогут вам быть в курсе последних тенденций.
Место, где можно заказать красивые накладная раковина с боковым сливом по выгодным ценам.
Студия профессионального дизайна интерьеров «Мята» поможет воплотить ваши мечты в реальность! Специалисты наши любят свою работу, они ваш интерьер сделают прекрасным. Мы будем рады видеть вас среди наших клиентов. Ищете студия дизайна в СПб? Spb.Studio-mint.ru – тут есть возможность увидеть фотографии интерьеров квартир. Предлагаем привлекательные цены и создаем проекты высочайшего уровня. Успех нашей работы подтверждают отзывы, ознакомиться с ними можете на нашем сайте. Свяжитесь с нами, чтобы обсудить детали. Все ваши пожелания мы удовлетворим!
Сувенирная продукция с логотипом и корпоративный мерч на заказ в Москве
https://telegra.ph/Suvenirnaya-produkciya-s-logotipom-na-zakaz-v-Moskve—Vash-klyuch-k-nezabyvaemomu-brendingu-05-31
Помощь в получении допуска СРО, сертификата ISO и лицензий от МСМ
https://nicstroy.ru/4215-gotovaya-firma-s-oborotami-i-dopuskom-sro.html
florinef listen – nexium amount prevacid bank
Самый большой магазин мобильных телефонов в Минске https://g5.by/ это возможность купить по низкой цене с доставкой по всей Беларуси: мобильные телефоны, ноутбуки, планшеты, бытовую технику и многое другое. Ознакомьтесь с каталогом из более чем 30000 сертифицированных товаров, и вы обязательно найдете для себя лучшую цену, качество, а быстрая бесплатная доставка не заставит себя долго ждать.
angkot88
ANGKOT88: Situs Game Deposit Pulsa Terbaik di Indonesia
ANGKOT88 adalah situs game deposit pulsa terbaik tahun 2020 di Indonesia. Kami menyediakan berbagai jenis game online terlengkap yang dapat Anda mainkan hanya dengan mendaftar satu ID. Dengan satu ID tersebut, Anda dapat mengakses seluruh permainan yang tersedia di situs kami.
Sebagai situs agen game online berlisensi resmi dari PAGCOR (Philippine Amusement Gaming Corporation), ANGKOT88 menjamin keamanan dan kenyamanan Anda. Situs kami didukung oleh server hosting yang cepat dan sistem keamanan dengan metode enkripsi terbaru di dunia, sehingga data Anda akan selalu terjaga keamanannya. Tampilan situs yang modern juga membuat Anda merasa nyaman saat mengakses situs kami.
Keunggulan ANGKOT88
Selain menjadi situs game online terbaik, ANGKOT88 juga menawarkan layanan praktis untuk melakukan deposit menggunakan pulsa XL ataupun Telkomsel dengan potongan terendah dibandingkan situs lainnya. Ini menjadikan kami salah satu situs game online pulsa terbesar di Indonesia. Anda juga dapat melakukan deposit pulsa melalui E-commerce resmi seperti OVO, Gopay, Dana, atau melalui minimarket seperti Indomaret dan Alfamart.
Kepercayaan dan Layanan
Kami di ANGKOT88 sangat menjaga kepercayaan Anda sebagai prioritas utama kami. Oleh karena itu, kami selalu berusaha menjadi agen online terpercaya dan terbaik sepanjang masa. Permainan game online yang kami tawarkan sangat praktis, sehingga Anda dapat memainkannya kapan saja dan di mana saja tanpa perlu repot bepergian. Kami menyediakan berbagai jenis game, termasuk yang disiarkan secara LIVE (langsung) dengan host cantik dan kamera yang merekam secara real-time, menjadikan ANGKOT88 situs game online terlengkap dan terbesar di Indonesia.
Promo Menarik dan Menguntungkan
ANGKOT88 juga menawarkan banyak sekali promo menarik dan menguntungkan. Anda bisa menikmati berbagai macam promo yang sesuai dengan kebutuhan Anda, seperti welcome bonus 20%, bonus deposit harian, dan cashback. Semua promo ini tersedia di situs ANGKOT88. Selain itu, kami juga memiliki layanan Customer Service yang siap membantu Anda kapan saja.
Jadi, tunggu apa lagi? Bergabunglah dengan ANGKOT88 dan nikmati pengalaman bermain game online terbaik dan teraman di Indonesia. Daftarkan diri Anda sekarang dan mulai mainkan game favorit Anda dengan nyaman dan aman di situs kami!
На сайте https://kladupechi.ru оформите заявку для того, чтобы воспользоваться такими полезными услугами, как: ремонт, кладка печей, каминов. Все конструкции от высококлассного, проверенного мастера, который работает по всему Санкт-Петербургу, области. А если вас интересует какая-либо определенная информация, то воспользуйтесь специальным поиском. Также имеется информация и про печное отопление: русскую, голландскую, финскую печь. Изучите все рубрики, чтобы получить полную информацию на интересующую тему.
Помощь в получении допуска СРО, сертификата ISO и лицензий от МСМ
https://www.metronews.ru/partners/novosti-partnerov-134/reviews/konsaltingovaya-kompaniya-management-company-monopoly-1456545/
florinef pills startle – prilosec describe lansoprazole pills cross
Local Search Company Tools To Streamline Your Everyday
Lifethe Only Local Search Company Trick That Everyone Should Be Able To local search company
ремонт телефонов в москве
cash advance langford bc Not that we have anything against the tax man, but let’s face it, some wise spending now will improve your tax burden as well as your operations.
Сувенирная продукция с логотипом и корпоративный мерч на заказ в Москве
https://cartlung3.bloggersdelight.dk/2024/05/31/%d1%81%d1%83%d0%b2%d0%b5%d0%bd%d0%b8%d1%80%d0%bd%d0%b0%d1%8f-%d0%bf%d1%80%d0%be%d0%b4%d1%83%d0%ba%d1%86%d0%b8%d1%8f-%d1%81-%d0%bb%d0%be%d0%b3%d0%be%d1%82%d0%b8%d0%bf%d0%be%d0%bc-%d0%bd%d0%b0-%d0%b7/
Помощь в получении допуска СРО, сертификата ISO и лицензий от МСМ
http://www.help-bussines.ru/vstuplenie-v-sro-stroiteley.html
https://ktm.org.ua/ у нас вы найдете свежие новости, аналитические статьи, эксклюзивные интервью и мнения экспертов. Будьте в курсе событий и тенденций, следите за развитием ситуации в реальном времени. Присоединяйтесь к нашему сообществу читателей!
https://mostmedia.com.ua мы источник актуальных новостей, аналитики и мнений. Получайте самую свежую информацию, читайте эксклюзивные интервью и экспертные статьи. Оставайтесь в курсе мировых событий и тенденций вместе с нами. Присоединяйтесь к нашему информационному сообществу!
На сайте https://advokat-samara.ru/ оставьте заявку для того, чтобы воспользоваться доставкой товаров из Китая для маркетплейсов. Среди основных услуг выделяют: выкуп, поиск, доставку товаров. Кроме того, можно воспользоваться и упаковкой, отгрузкой продукции на маркетплейсы. При необходимости будет оказана вся необходимая помощь для того, чтобы организовать бизнес на WB. Рассчитать цену услуги получится в данный момент. Оказывается весь спектр услуг, чтобы вы наладили собственный бизнес. Воспользуйтесь сопровождением с гарантиями, проводится анализ уже имеющихся карточек.
Помощь в получении допуска СРО, сертификата ISO и лицензий от МСМ
https://muzeon.ru/finansy/9077-kak-i-gde-poluchit-dopusk-sro-v-stroitelstve.html
ремонт телефонов поблизости от меня
Space Movers https://spacemovers.ca/ is renowned as the premier moving company in Calgary, Canada, offering unparalleled service and expertise in residential and commercial relocations. Their reputation as the best movers in the city is built on a foundation of reliability, efficiency, and a customer-centric approach that ensures a smooth and stress-free moving experience. Choosing Space Movers means choosing the best in the business, ensuring a seamless transition to your new home or office.
На сайте https://zdravbud.net/new/pochemu-bolyat-sustavy изучите увлекательную, интересную и содержательную информацию, которая посвящена тому, почему болят суставы. Так есть информация о том, чем правильно их питать, чтобы сохранили свою эластичность. Описаны признаки того, что суставы заболели. Вы узнаете о том, какими способами и методами их лучше всего и эффективней восстановить. Описаны самые эффективные, точные, а также безопасные из них. А самое главное, что они действительно работают.
Спортивные добавки для силы. витамине д Витамины для костей и суставов.
Хотите быстро и без каких-либо проблем заменить права на польские? MIGRANT SUPPORT – это то, что вам необходимо. Компания дает гарантию на персональный подход и лояльные цены. Наши квалифицированные специалисты обладают большим опытом работы. Они предоставят вам нужную информацию о том, как заменить права на польские. https://migrant.support/obmien_rossiiskikh_prav_na_polskiie – сайт, где у вас есть возможность прямо сегодня заказать услугу. Также здесь в любое удобное время можно ознакомиться с отзывами о нас. Ответим на все ваши вопросы, звоните нам.
pharmacie en ligne sans ordonnance: acheter kamagra site fiable – acheter mГ©dicament en ligne sans ordonnance
Помощь в получении допуска СРО, сертификата ISO и лицензий от МСМ
http://help-bussines.ru/vstuplenie-v-sro-stroiteley.html
cash advance in delaware A secured personal loan or a personal line of credit results in the borrower facing the risk of losing the asset on account of the inability to repay the borrowed sum.
Founded in Texas in 2002, https://southeast.newschannelnebraska.com/story/50826769/del-mar-energy-from-humble-beginnings-to-an-energy-market-leader quickly transformed into one of the leading players in the energy market, oil and gas extraction, road construction
На сайте https://ipoteka.ru/ вы сможете воспользоваться такой услугой, как помощь в оформлении ипотеки, сопровождение различных сделок, которые совершаются с недвижимостью. В компании работают лучшие, компетентные сотрудники, которые дадут консультацию, а также на профессиональном уровне подберут оптимальную программу для оформления ипотеки. Сервис практикует сотрудничество с ведущими банками, а также инвестиционными предприятиями России, а потому есть возможность получить льготу по ипотеке. Только для вас самые лучшие предложения, которыми воспользуйтесь прямо сейчас.
Студия профессионального дизайна интерьеров Мята в Москве воплощает мечты в реальность. Будем рады видеть вас в числе своих клиентов. https://moskva.studio-mint.ru/ – здесь работают исключительно лучшие специалисты, они увлечены собственным делом и готовы принять любой вызов. Следим за новинками и трендами в индустрии интерьерного дизайна и предоставляем выгодные цены. Создаем проекты высокого уровня. Обсудим с вами все детали, звоните нам уже сейчас. Любые ваши желания удовлетворим!
Помощь в получении допуска СРО, сертификата ISO и лицензий от МСМ
https://muzeon.ru/sport/9304-gde-i-kak-poluchit-licenziyu-minkultury-na-restavraciyu-giop.html
Сувенирная продукция с логотипом и корпоративный мерч на заказ в Москве
https://jutecurve29.bloggersdelight.dk/2024/05/31/%d1%81%d1%83%d0%b2%d0%b5%d0%bd%d0%b8%d1%80%d0%bd%d0%b0%d1%8f-%d0%bf%d1%80%d0%be%d0%b4%d1%83%d0%ba%d1%86%d0%b8%d1%8f-%d1%81-%d0%bb%d0%be%d0%b3%d0%be%d1%82%d0%b8%d0%bf%d0%be%d0%bc-%d0%bd%d0%b0-%d0%b7/
SUPERMONEY88: Situs Game Online Deposit Pulsa Terbaik di Indonesia
SUPERMONEY88 adalah situs game online deposit pulsa terbaik tahun 2020 di Indonesia. Kami menyediakan berbagai macam game online terbaik dan terlengkap yang bisa Anda mainkan di situs game online kami. Hanya dengan mendaftar satu ID, Anda bisa memainkan seluruh permainan yang tersedia di SUPERMONEY88.
Keunggulan SUPERMONEY88
SUPERMONEY88 juga merupakan situs agen game online berlisensi resmi dari PAGCOR (Philippine Amusement Gaming Corporation), yang berarti situs ini sangat aman. Kami didukung dengan server hosting yang cepat dan sistem keamanan dengan metode enkripsi termutakhir di dunia untuk menjaga keamanan database Anda. Selain itu, tampilan situs kami yang sangat modern membuat Anda nyaman mengakses situs kami.
Layanan Praktis dan Terpercaya
Selain menjadi game online terbaik, ada alasan mengapa situs SUPERMONEY88 ini sangat spesial. Kami memberikan layanan praktis untuk melakukan deposit yaitu dengan melakukan deposit pulsa XL ataupun Telkomsel dengan potongan terendah dari situs game online lainnya. Ini membuat situs kami menjadi salah satu situs game online pulsa terbesar di Indonesia. Anda bisa melakukan deposit pulsa menggunakan E-commerce resmi seperti OVO, Gopay, Dana, atau melalui minimarket seperti Indomaret dan Alfamart.
Kami juga terkenal sebagai agen game online terpercaya. Kepercayaan Anda adalah prioritas kami, dan itulah yang membuat kami menjadi agen game online terbaik sepanjang masa.
Kemudahan Bermain Game Online
Permainan game online di SUPERMONEY88 memudahkan Anda untuk memainkannya dari mana saja dan kapan saja. Anda tidak perlu repot bepergian lagi, karena SUPERMONEY88 menyediakan beragam jenis game online. Kami juga memiliki jenis game online yang dipandu oleh host cantik, sehingga Anda tidak akan merasa bosan.
Acheter Sildenafil 100mg sans ordonnance: viagra en ligne – Acheter viagra en ligne livraison 24h
বেটভিসার সাথে আপনার আইপিএল বেটিংকে উন্নত করুন: উত্তেজনাপূর্ণ স্লট, পুরস্কৃত বোনাস এবং অতুলনীয় রোমাঞ্চ
ইন্ডিয়ান প্রিমিয়ার লিগ (আইপিএল) এর জন্য প্রত্যাশা একটি জ্বরের পিচে পৌঁছেছে, বেটভিসা একটি অতুলনীয় গেমিং অভিজ্ঞতার জন্য ক্রীড়া বেটিং উত্সাহীদের জন্য প্রধান গন্তব্য হিসাবে আবির্ভূত হয়েছে৷ রোমাঞ্চকর স্লট এবং ফিশিং গেম থেকে শুরু করে লোভনীয় স্পোর্টস বোনাস পর্যন্ত বিভিন্ন ধরনের অফার সহ, Betvisa আসন্ন IPL মৌসুমে আপনাকে জয়ের দিকে এগিয়ে নিয়ে যেতে প্রস্তুত।
Betvisa স্লট এবং ফিশিং গেমে নিজেকে নিমজ্জিত করুন
Betvisa একটি সু-বৃত্তাকার গেমিং অভিজ্ঞতা প্রদানের গুরুত্ব বোঝে, এবং এটি সঠিকভাবে প্রদান করে। আপনি স্লটের অ্যাড্রেনালিন-জ্বালানি উত্তেজনা বা মাছ ধরার গেমের মনোমুগ্ধকর লোভের জন্য মেজাজে থাকুন না কেন, Betvisa প্ল্যাটফর্ম একটি বৈচিত্র্যপূর্ণ নির্বাচন অফার করে যা আপনার প্রতিটি ইচ্ছা পূরণ করে। নিরবিচ্ছিন্ন Betvisa লগইন প্রক্রিয়ার মাধ্যমে, আপনি সহজেই বিনোদনের এই বিশাল অ্যারে অ্যাক্সেস করতে পারেন, আপনার উত্তেজনার মাত্রা ধারাবাহিকভাবে 200%-এ রয়েছে তা নিশ্চিত করে।
Betvisa বোনাসের মাধ্যমে আপনার IPL বেটিং পুরষ্কার সর্বাধিক করুন
আইপিএল মরসুম যত ঘনিয়ে আসছে, বেটভিসা তার বিশ্বস্ত ব্যবহারকারীদের ব্যতিক্রমী স্পোর্টস বোনাস দিয়ে পুরস্কৃত করতে আগ্রহী। IPL সিজনে ₹5,000 পর্যন্ত বোনাস স্কোর করুন এবং আপনার বেটিং অভিজ্ঞতাকে নতুন উচ্চতায় উন্নীত করুন। এই উদার অফারটি আপনাকে আপনার ব্যাঙ্করোলকে আরও প্রসারিত করতে দেয়, আইপিএল বাজির উচ্চ-স্টেকের বিশ্বে আপনার বিজয়ী হওয়ার সম্ভাবনা বৃদ্ধি করে৷
Betvisa Bangladesh অ্যাডভান্টেজকে আলিঙ্গন করুন
বাংলাদেশের Betvisa ব্যবহারকারীদের জন্য, প্ল্যাটফর্মের স্থানীয় পদ্ধতি একটি নির্বিঘ্ন এবং উপযোগী অভিজ্ঞতা নিশ্চিত করে। Betvisa Bangladesh লগইন প্রক্রিয়ার মাধ্যমে, আপনি সহজেই IPL বেটিং অপশনের বিস্তৃত পরিসরে প্রবেশ করতে পারবেন, বিশেষ করে বাংলাদেশী বাজারের পছন্দের জন্য। বিশদের প্রতি এই মনোযোগ বেটভিসাকে আলাদা করে, আপনাকে সত্যিকারের নিমগ্ন এবং পুরস্কৃত করার অভিজ্ঞতা প্রদান করে।
Betvisa অ্যাপের শক্তি ব্যবহার করুন
আজকের দ্রুত-গতির বিশ্বে, সুবিধাই মুখ্য, এবং Betvisa এটি পুরোপুরি বোঝে। Betvisa অ্যাপটি একটি ব্যবহারকারী-বান্ধব এবং স্বজ্ঞাত প্ল্যাটফর্ম অফার করে, যা আপনাকে যেতে যেতে আপনার প্রিয় স্লট, মাছ ধরার গেম এবং ক্রীড়া বাজি বাজার অ্যাক্সেস করতে দেয়। আপনি যাতায়াত করছেন, লাইনে অপেক্ষা করছেন বা কেবল উত্তেজনার মুহূর্ত খুঁজছেন, Betvisa অ্যাপটি গেমের রোমাঞ্চকে আপনার নখদর্পণে রাখে।
Betvisa: আপনার গেটওয়ে আইপিএল বেটিং আধিপত্য
আইপিএল মরসুম যত ঘনিয়ে আসছে, বেটভিসা ক্রীড়া বাজি উত্সাহীদের জন্য চূড়ান্ত গন্তব্য হিসাবে আবির্ভূত হয়েছে৷ এর বৈচিত্র্যময় গেমিং অফার, উদার বোনাস এবং Betvisa বাংলাদেশ ব্যবহারকারীদের জন্য উপযোগী অভিজ্ঞতা সহ, প্ল্যাটফর্মটি আপনার বেটিং যাত্রাকে নতুন উচ্চতায় উন্নীত করতে প্রস্তুত। একটি আনন্দদায়ক IPL মরসুমের জন্য প্রস্তুত হন এবং Betvisa আপনাকে চূড়ান্ত বিজয়ের দিকে এগিয়ে নিয়ে যেতে দিন।
Betvisa Bet | Hit it Big This IPL Season with Betvisa!
Betvisa login! | Every deposit during IPL matches earns a 2% bonus .
Betvisa Bangladesh! | IPL 2024 action heats up, your bets get more rewarding!
Crash Game returns! | huge ₹10 million jackpot. Take the lead on the Betvisa app !
#betvisa
Start Winning Now! | Sign up through Betvisa affiliate login, claim ₹500 free cash.
Grab Your Winning Ticket! | Register login and win ₹8,888 at visa bet!
https://www.betvisa-bet.com/bn
#visabet #betvisalogin #betvisabangladesh#betvisaapp
200% Excitement! | Enjoy slots and fishing games at Betvisa লগইন করুন!
Big Sports Bonuses! | Score up to ₹5,000 in sports bonuses during the IPL season
Gear up for an exhilarating IPL season at Betvisa, propels you towards victory!
Frau Befriedigt Mann Analsex Sextape Rollenspiele Wie Secret Of Mana
Зайдите на сайт https://cescoshop.ru/ где вы сможете приобрести краски, лаки, грунт, эмаль и многое другое. Cesco представляет огромный выбор продукции по отличным ценам, а получить заказ можно самостоятельно или оформить с доставкой по всей России. Ознакомьтесь с каталогом и вы обязательно найдете все для интерьера и экстерьера. Подробнее на сайте.
SUPERMONEY88: Situs Game Online Deposit Pulsa Terbaik di Indonesia
SUPERMONEY88 adalah situs game online deposit pulsa terbaik tahun 2020 di Indonesia. Kami menyediakan berbagai macam game online terbaik dan terlengkap yang bisa Anda mainkan di situs game online kami. Hanya dengan mendaftar satu ID, Anda bisa memainkan seluruh permainan yang tersedia di SUPERMONEY88.
Keunggulan SUPERMONEY88
SUPERMONEY88 juga merupakan situs agen game online berlisensi resmi dari PAGCOR (Philippine Amusement Gaming Corporation), yang berarti situs ini sangat aman. Kami didukung dengan server hosting yang cepat dan sistem keamanan dengan metode enkripsi termutakhir di dunia untuk menjaga keamanan database Anda. Selain itu, tampilan situs kami yang sangat modern membuat Anda nyaman mengakses situs kami.
Layanan Praktis dan Terpercaya
Selain menjadi game online terbaik, ada alasan mengapa situs SUPERMONEY88 ini sangat spesial. Kami memberikan layanan praktis untuk melakukan deposit yaitu dengan melakukan deposit pulsa XL ataupun Telkomsel dengan potongan terendah dari situs game online lainnya. Ini membuat situs kami menjadi salah satu situs game online pulsa terbesar di Indonesia. Anda bisa melakukan deposit pulsa menggunakan E-commerce resmi seperti OVO, Gopay, Dana, atau melalui minimarket seperti Indomaret dan Alfamart.
Kami juga terkenal sebagai agen game online terpercaya. Kepercayaan Anda adalah prioritas kami, dan itulah yang membuat kami menjadi agen game online terbaik sepanjang masa.
Kemudahan Bermain Game Online
Permainan game online di SUPERMONEY88 memudahkan Anda untuk memainkannya dari mana saja dan kapan saja. Anda tidak perlu repot bepergian lagi, karena SUPERMONEY88 menyediakan beragam jenis game online. Kami juga memiliki jenis game online yang dipandu oleh host cantik, sehingga Anda tidak akan merasa bosan.
На сайте https://cryptocodes.kz/ ознакомьтесь с интересной и полезной информацией о криптовалюте. Здесь находится все, что вам необходимо знать о криптографии. На сайте вы найдете и промокоды, другую важную и полезную информацию, которая обязательно вам пригодится. Подобные бонусы помогут вам значительно сэкономить, чтобы вы смогли получить больше приятных эмоций. Также вы получите и ответы на многочисленные вопросы, которые помогут вам правильно обращаться с криптовалютой. Регулярно на портале появляется новая, свежая информация.
pro88
PRO88: Situs Game Online Deposit Pulsa Terbaik di Indonesia
PRO88 adalah situs game online deposit pulsa terbaik tahun 2020 di Indonesia. Kami menyediakan berbagai macam game online terbaik dan terlengkap yang bisa Anda mainkan di situs game online kami. Hanya dengan mendaftar satu ID, Anda bisa memainkan seluruh permainan yang tersedia di PRO88.
Keunggulan PRO88
PRO88 juga merupakan situs agen game online berlisensi resmi dari PAGCOR (Philippine Amusement Gaming Corporation), yang berarti situs ini sangat aman. Kami didukung dengan server hosting yang cepat dan sistem keamanan dengan metode enkripsi termutakhir di dunia untuk menjaga keamanan database Anda. Selain itu, tampilan situs kami yang sangat modern membuat Anda nyaman mengakses situs kami.
Berbagai Macam Game Online
Kami menyediakan berbagai macam game online terbaik yang bisa Anda mainkan kapan saja dan di mana saja. Dengan satu ID, Anda bisa menikmati semua permainan yang tersedia, mulai dari permainan kartu, slot, hingga taruhan olahraga. PRO88 memastikan semua game yang kami sediakan adalah yang terbaik dan terlengkap di Indonesia.
Keamanan dan Kenyamanan
Kami memahami betapa pentingnya keamanan dan kenyamanan bagi para pemain. Oleh karena itu, PRO88 menggunakan server hosting yang cepat dan sistem keamanan dengan metode enkripsi termutakhir di dunia. Ini memastikan bahwa data pribadi dan transaksi Anda selalu aman bersama kami. Tampilan situs yang modern juga dirancang untuk memberikan pengalaman bermain yang nyaman dan menyenangkan.
Kesimpulan
PRO88 adalah pilihan terbaik untuk Anda yang mencari situs game online deposit pulsa yang aman dan terpercaya. Dengan berbagai macam game online terbaik dan terlengkap, serta dukungan keamanan yang canggih, PRO88 siap memberikan pengalaman bermain game yang tak terlupakan. Daftar sekarang juga di PRO88 dan nikmati semua permainan yang tersedia hanya dengan satu ID.
Kunjungi kami di PRO88 dan mulailah petualangan game online Anda bersama kami!
MIGRANT SUPPORT предоставляет услуги лучших специалистов, обладающих достаточным опытом работы. В своей деятельности мы каждому клиенту предоставляем индивидуальный подход. Гарантируем достижение в выгодном совместном сотрудничестве и приемлемые цены. https://vpolshe.com/kriptolitsenziya-v-polshe/ – сайт, где можете прямо сейчас оставить заявку. Поможем вам получить криптолицензию в Польше. Процесс пройдет хорошо, мы все выполним оперативно. Вы останетесь довольны результатом и сервисом. Звоните, ответим на ваши вопросы!
https://kursovyemetrologiya.ru
Pharmacie en ligne livraison Europe: pharmacie en ligne sans ordonnance – Achat mГ©dicament en ligne fiable
Краснодарский завод производит котельное оборудование, которое проходит, регламентированные технические испытания и отвечает всем требованиям безопасности. Работаем по всей Российской Федерации и ряду стран СНГ. С нами вы существенно экономите собственное время и денежные средства. Ищете паровой котел дизель? Kzko-gaz.ru – сайт, где есть каталог и представлены отзывы о нашем заводе, ознакомиться с ними можно прямо сейчас. Можете быть уверены – любой произведенный котел или же котельная будут вовремя доставлены. Тепло создавая, гарантируем качество!
Sexspielzeug M Vanesa Beker Analsex
https://formomebel.ru/krovati
## Капитал Голд: Надежная скупка драгоценных металлов в центре Москвы
### О компании
Компания “Капитал Голд” с 2005 года предоставляет услуги по скупке драгоценных металлов в центре Москвы, предлагая своим клиентам надежность и высочайшее качество сервиса. Мы гордимся своей безупречной репутацией, подтвержденной многочисленными положительными отзывами и высоким рейтингом Яндекса 5,0.
### Наши услуги
#### Официальная скупка драгоценных металлов
“Капитал Голд” – это официальная скупка золота, серебра, платины и палладия в любом виде. Мы ценим своих клиентов и предлагаем одни из самых высоких цен на рынке благодаря переработке драгоценных металлов без посредников и широкой клиентской базе, включающей более 300 магазинов и коллекционеров.
#### Высокоточное оборудование
Для обеспечения максимальной точности и прозрачности процесса оценки мы используем только современное оборудование. Наши японские лабораторные весы AND, видимые посетителям, обеспечивают высокую точность измерений. Анализаторы драгоценных металлов и камней позволяют нам проводить оценку с максимальной точностью, гарантируя объективность и справедливость предложенной цены.
### Преимущества “Капитал Голд”
#### Высокие цены
Мы предлагаем высокие цены на скупку ювелирных украшений и других предметов из драгоценных металлов. Это стало возможным благодаря отсутствию посредников и нашей широкой клиентской базе. Убедитесь сами, обратившись к нам, и получите максимально выгодные условия.
#### Гарантия безопасности сделки
Безопасность наших клиентов – наш приоритет. Наш салон оборудован профессиональной охранной системой и системой видеонаблюдения с аудио и видеозаписью, что обеспечивает полную безопасность каждой сделки. Вы можете быть уверены в конфиденциальности и защите ваших интересов при сотрудничестве с нами.
### Почему выбирают “Капитал Голд”?
– **Опыт и репутация**: Более 15 лет успешной работы и безупречная репутация.
– **Современное оборудование**: Использование высокоточных японских лабораторных весов и анализаторов.
– **Высокие цены**: Благодаря переработке без посредников и широкой клиентской базе.
– **Безопасность**: Профессиональная охранная система и видеонаблюдение.
Не откладывайте визит к нам! “Капитал Голд” – ваш надежный партнер в мире драгоценных металлов. Посетите наш салон в центре Москвы и убедитесь в высоком качестве нашего сервиса и выгодных условиях.
Присоединяйтесь к числу наших довольных клиентов и партнеров уже сегодня!
MIGRANT SUPPORT предоставляет помощь для получения номера PESEL и дает гарантию на привлекательные цены. Профессиональные специалисты компании, прилагают максимум усилий для выполнения различных задач. https://migrant.support/poluchieniie_nomiera_pesel – сайт, где у вас есть возможность узнать, как сделать песель удаленно, и зачем он нужен. Мы оказываем бесплатную консультацию, работаем качественно и оперативно. К своим клиентам относимся лояльно, и делаем все, чтобы их ожидания были оправданы. Обращайтесь именно к нам и не пожалеете о своем выборе!
Краснодарский завод, производимое им котельное оборудование, проходит регламентированные технические испытания, поэтому отвечает необходимым требованиям безопасности. Работаем по всей Российской Федерации и ряду стран СНГ. С нами вы существенно экономите собственное время и денежные средства. Ищете жаротрубный паровой котел? Kzko-gaz.ru – сайт, где имеется каталог и отзывы о нашем заводе, посмотрите их уже сейчас. Любой изготавливаемый котел либо же котельная будут в срок доставлены, не сомневайтесь. Гарантируем качество, создавая тепло!
Портал fermerstvo.in.ua пользуется большой известностью. Здесь вы найдете актуальную информацию. Ознакомиться с ней есть возможность уже сейчас. fermerstvo.in.ua – https://fermerstvo.in.ua сайт, где можно узнать, с чего фермерское хозяйство начинается. Мы открыто делимся своими неудачами и успехами. Разбираем, как к разведению домашней птицы подготовиться. Рассказываем, как повысить урожайность овощей. У нас вы найдете ответы на необходимые вопросы. Делаем контент понятным. Вы получите глубокие знания обо всем, что связано с фермерским хозяйством.
На сайте https://xn--57-6kchpq9cd0i.xn--p1ai/ закажите натяжные потолки высокого качества и выполненные из современных, высокотехнологичных материалов, которые не утратят своего внешнего вида долгое время. На всю продукцию установлены привлекательные, доступные расценки, а работы выполняются точно в срок и квалифицированными мастерами. Все услуги оказываются «под ключ», предоставляются гарантии. Предоставляется скидка 10%. Монтажные работы выполняются всего за пару часов. На консультации вам помогут с выбором и подскажут, какая конструкция подходит именно вам.
Natursekt Kommentar 100 Bio Natursekt Stream
Зайдите на сайт https://deep-well.ru/ где вы сможете заказать такие полезные услуги как чистка и ремонт колодцев в Москве. Компания Глубокий колодец работает на рынке с 2003 года и оказывает профессиональные услуги по чистке, ремонту, углублению колодцев, а наши мастера знают о них все. Стоимость услуг доступна каждому. Подробнее на сайте.
СХТ – компания, которая предлагает купить измерительное высокоточное оборудование. Мы гарантируем безупречное качество нашей продукции и привлекательные цены. Специалисты компании обладают приличным опытом работы и высокой квалификацией. Они с радостью готовы проконсультировать вас по интересующим вопросам. https://cxt.su – сайт, где у вас есть возможность посмотреть детальнее наши услуги и информацию. Здесь вы найдете видео-презентацию и фотогалерею. Оперативно реагируем на все заявки. Обращайтесь именно к нам!
Балконы под ключ в СПБ specbalkon.ru
Если Вам нужно замена остекления теплое без изменения фасада прямо сегодня, то мы вам непременно поможем. Услуга по смене холодного фасадного остекления по теплое сейчас очень популярна. При покупке квартиры в новом доме очень часто застройщик устанавливает на балкон холодное, не очень качественное остекление, которое лучше всего менять сразу же после приобретения. Теплое остекление лоджии имеет множество преимуществ: окна не замерзают даже в самые морозные зимы, на балконе можно сделать любое помещение, цветы будут расти при комнатной температуре, на балконе можно сделать места для хранения и вещи не испортятся. Поэтому предлагаем Вам замену остекления сделать как можно скорее и по лучшей цене.
На сайте https://ax-card.ru/ закажите пластиковые карты для различных сфер деятельности. Их создают на инновационном, высокотехнологичном оборудовании компетентные специалисты с огромным опытом. Дополнительно они разработают макет, а при оказании услуги используют уникальные и инновационные технологии. Именно поэтому вы получите ожидаемый и прогнозируемый результат. Если вы заинтересовались услугой, то специально для вас может быть сделана пробная карта. Это абсолютно бесплатно.
секс шоп куклы https://24sexy-dolls.ru
https://fraza.kyiv.ua/ вы найдете последние новости, глубокие аналитические материалы, интервью с влиятельными личностями и экспертные мнения. Следите за важными событиями и трендами в реальном времени. Присоединяйтесь к нашему сообществу и будьте информированы!
Schwangere Deutsche Frau Beim Analsex Buch Kinderreime Fingerspiele
Консультация по SEO продвижению.
Информация о том как работать с низкочастотными запросами и как их выбирать
Тактика по работе в соперничающей нише.
У меня есть постоянных клиентов взаимодействую с 3 организациями, есть что поделиться.
Ознакомьтесь мой аккаунт, на 31 мая 2024г
количество успешных проектов 2181 только в этом профиле.
Консультация только в устной форме, без скриншотов и документов.
Продолжительность консультации указано 2 ч, но по сути всегда на контакте без жёсткой привязки ко времени.
Как управлять с программным обеспечением это уже иначе история, консультация по использованию ПО договариваемся отдельно в отдельном кворке, определяем что нужно при разговоре.
Всё спокойно на без напряжения не в спешке
To get started, the seller needs:
Мне нужны данные от телеграмм чата для связи.
разговор только устно, вести переписку нету времени.
Сб и воскресенья выходной
Клиника инновационной хирургии предоставляет широкий спектр медицинских услуг. Здесь работают специалисты, благодаря которым можно жить полноценно. Врачи любят свою работу, имеют богатый опыт и высокую квалификацию. Вы будете чувствовать поддержку персонала. Ищете плазмотерапия в клинике инновационной хирургии? Kix-med.ru – сайт, где есть возможность записаться на консультацию и посмотреть отзывы пациентов. Вы можете быть уверены в безопасности лечения, обращайтесь. Гарантируем индивидуальный подход и приемлемые цены. Качество вашей жизни заметно улучшится!
Вам интересна прописка в Польше, г. Варшава? Обращайтесь в MIGRANT SUPPORT. Компания предлагает высококачественные услуги. Гарантирует лояльные цены и персональный подход к каждому клиенту. Вы можете получить профессиональную консультационную поддержку по всем интересующим вопросам. https://vpolshe.com/propiska-v-polshe-g-varshava-dogovor-arendy-zhilya-varshava/ – сайт, где вы узнаете, для чего нужна прописка (meldunek). Оставьте заявку на портале, и мы вам позвоним через некоторое время. Будем рады помочь с договором аренды жилья.
pharmacie en ligne livraison europe: Levitra acheter – pharmacie en ligne france livraison belgique
Портал visti.in.ua заслуживает вашего внимания. Здесь представлены актуальные новости Украины, они находятся в круглосуточном доступе. Мы гордимся и ценим своих читателей. Для вас собрали только самое лучшее, поудобнее устраивайтесь и читайте интересную информацию. visti.in.ua – https://visti.in.ua сайт, который пользуется повышенной популярностью. Посетите его прямо сейчас и узнаете об экономике, науке, политике, спорте. Все сведения достоверны, можете даже в этом не сомневаться. Следите за нами и получайте истинное удовольствие от отменного контента!
sunmory33
https://7krasotok.com здесь вы найдете статьи о моде, красоте, здоровье, отношениях и карьере. Читайте советы экспертов, участвуйте в обсуждениях и вдохновляйтесь новыми идеями. Присоединяйтесь к нашему сообществу женщин, стремящихся к совершенству!
секс кукла купить цена https://24sexy-dolls.ru
Зайдите на сайт https://came.name/ где вы сможете ознакомиться с широким ассортиментом оборудования CAME (итальянский производитель), таким как автоматика для ворот, шлагбаумы, парковочные системы, турникеты и многим другим. Узнайте больше информации о продукции на сайте, а также посмотрите прайс листы с выгодными ценами.
https://bestwoman.kyiv.ua узнайте всё о моде, красоте, здоровье и личностном росте. Читайте вдохновляющие истории, экспертные советы и актуальные новости. Присоединяйтесь к нашему сообществу женщин, живущих яркой и насыщенной жизнью!
Ist Analsex Unhygienisch Analverkehr Wenn Man Verletzt
https://prowoman.kyiv.ua на нашем сайте вы найдете полезные советы по моде, красоте, здоровью и отношениям. Читайте вдохновляющие статьи, участвуйте в обсуждениях и обменивайтесь идеями. Присоединяйтесь к нашему сообществу современных женщин!
https://superwoman.kyiv.ua вы на нашем надежном гиде в мире женской красоты и стиля жизни! У нас вы найдете актуальные статьи о моде, красоте, здоровье, а также советы по саморазвитию и карьерному росту. Присоединяйтесь к нам и обретайте новые знания и вдохновение каждый день!
Консалтинговая компания Leverage Finance Group оказывает поддержку в реализации инвестиционных проектов. Отлично разбираемся в особенностях и тонкостях процесса получения грантов. Создаем действенные бизнес-планы и сопровождаем их до результатов. Ищите оценка инвестиционных проектов помощь в получении гранта? Levfin.ru – сайт, где вы узнаете, почему стоит обращаться именно к нам. Работаем с компаниями в различных отраслях, создавая ценность каждому проекту. Наши услуги помогают бизнесу успешно развиваться и вовремя привлекать нужное финансирование. Звоните и мы проконсультируем вас.
https://sttimothysignal.org/groups/666484-ru/
На сайте https://rating-smart.ru/ узнайте стоимость такой популярной и важной услуги, как написание и размещение отзывов с гарантией. Специалисты сервиса разместят отзывы, после чего поднимут рейтинг вашего предприятия на всех возможных площадках, а также порталах-отзовиках. Работа осуществляется по всем городам России. На все услуги предоставляются гарантии. Все отзывы публикуются исключительно с настоящих аккаунтов. Отзывы повышают лояльность клиентов, доверие к вашему продукту или услугам.
buy cheap tiktok live views Buy TikTok Live Views
Банкротство физических лиц – это правовой процесс, который позволяет гражданам, не способным погасить свои долги, получить защиту от кредиторов и начать финансовую жизнь с чистого листа. В России процедура банкротства физических лиц была введена в 2015 году, и с тех пор ею воспользовались десятки тысяч людей.
**Основные этапы процедуры банкротства физических лиц**
1. **Подача заявления о банкротстве**. Должник или его кредитор подает заявление о признании физического лица банкротом в арбитражный суд по месту жительства должника. В заявлении указываются данные о должнике, размере задолженности и других финансовых обязательствах.
2. **Рассмотрение дела в суде**. Суд проверяет обоснованность заявления и принимает решение о начале процедуры банкротства. На этом этапе назначается финансовый управляющий, который будет контролировать процесс.
3. **Финансовое управление**. Финансовый управляющий оценивает финансовое состояние должника, его активы и обязательства. Управляющий может предложить план реструктуризации долгов или продажу имущества должника для погашения задолженности.
4. **Реструктуризация или реализация имущества**. В зависимости от решения суда и финансового управляющего, может быть предложен план реструктуризации долгов, который позволит должнику погашать долги в течение определенного времени. Если такой план невозможен, начинается реализация имущества должника с целью погашения задолженности.
5. **Завершение процедуры банкротства**. По окончании реализации имущества или выполнения плана реструктуризации суд выносит решение о завершении процедуры банкротства. Оставшиеся непогашенные долги списываются, и должник освобождается от обязательств перед кредиторами.
**Плюсы и минусы банкротства физических лиц**
**Плюсы**:
1. **Освобождение от долгов**. Основное преимущество банкротства – возможность избавиться от непосильных долгов и начать новую финансовую жизнь.
2. **Защита от кредиторов**. С момента подачи заявления о банкротстве и до завершения процедуры кредиторы не могут требовать погашения долгов через суд или приставов.
3. **Реструктуризация долгов**. Возможность реструктурировать долги и погашать их по новому, более удобному графику.
**Минусы**:
1. **Потеря имущества**. В большинстве случаев для погашения долгов придется продать имущество, принадлежащее должнику.
2. **Снижение кредитного рейтинга**. Банкротство негативно сказывается на кредитной истории, что может затруднить получение новых кредитов в будущем.
3. **Ограничения**. После банкротства на должника могут быть наложены ограничения, такие как запрет на занятие определенных должностей или ведение бизнеса.
**Альтернативы банкротству физических лиц**
Существуют и альтернативные способы решения проблемы с долгами, которые могут быть менее радикальными и более выгодными для должника:
1. **Переговоры с кредиторами**. Должник может попытаться договориться с кредиторами о реструктуризации долгов, снижении процентной ставки или предоставлении отсрочки по платежам.
2. **Рефинансирование**. Взятие нового кредита на более выгодных условиях для погашения старых долгов может помочь снизить финансовую нагрузку.
3. **Мировое соглашение**. Заключение мирового соглашения с кредиторами в рамках судебного процесса позволяет урегулировать задолженность без процедуры банкротства.
Банкротство физических лиц – серьезный шаг, который требует взвешенного подхода и тщательного анализа всех возможных последствий. Важно помнить, что эта процедура может стать единственным выходом из сложной финансовой ситуации, но перед ее началом стоит рассмотреть все возможные альтернативы и проконсультироваться с юристом или финансовым консультантом.
https://historydb.date/wiki/666484.ru
Analsex Eng Analsex Angst
bocor88
Сувенирная продукция с логотипом и корпоративный мерч на заказ в Москве
https://diigo.com/0wfu8p
vente de mГ©dicament en ligne: kamagra en ligne – acheter mГ©dicament en ligne sans ordonnance
Visit https://quasa.io/ and meet Quasa, which connects people who need home or remote services with pre-vetted, independent professionals who can help with home services or remote work and errands around the city: household services, photo and video, editing, installation, setup, training, courses, preparation, remote work and more.
buy tiktok live views Buy TikTok Live Views
На сайте https://vpolshe.com/kriptolitsenziya-v-polshe/ оформите заявку для того, чтобы воспользоваться такой нужной и важной услугой, как получение криптолицензии в Польше. В компании работают компетентные, лучшие сотрудники, которые отличаются огромным опытом. Они дадут вам консультацию, расскажут обо всех достоинствах процедуры, а также о том, какие документы рекомендуется подготовить. Компания уже длительное время оказывает услуги в этой области. Стоимость такой услуги – 10 000 евро. Ее проводят в несколько этапов.
Помощь в получении допуска СРО, сертификата ISO и лицензий от МСМ
https://life24.pro/life/363791625/
купить самые дешевые сигареты с фильтром
Купить безакцизные сигареты
решения задач на заказ https://resheniezadachmatematika.ru/
pharmacie en ligne pas cher: levitra generique sites surs – pharmacie en ligne france livraison internationale
Зайдите на сайт https://clean-ru.com/ и вы сможете заказать такие услуги как: дезинфекция, дератизация, дезодорация, дезинсекция от профессионалов своего дела, в Москве. Мы специализируемся на предоставлении широкого спектра услуг по отличным ценам, а наши комплексные позволят обеспечить уничтожение различных видов вредителей и бактерий. Узнайте больше на сайте.
курсовые на заказ https://kursovyematematika.ru
Сайт Украиночка предлагает интересную и полезную информацию. Наша главная миссия – помочь вам быть образованной и уверенной. Мы знаем то, что вы заслуживаете самое лучшее. В любых аспектах жизни мы вдохновим вас на достижение вершин. Раскроем большой спектр возможностей для самовыражения и саморазвития. ukrayinochka.com – https://ukrayinochka.com портал, где есть все, что интересно современным женщинам: от актуальных новостей до занимательных советов. Посетите уже сейчас наш ресурс. Вас ожидает лучший контент!
Deutsche Frauen Analsex Pornos Rollenspiele Alkohol
Студия дизайна интерьеров «Мята» воплотит в реальность все ваши пожелания! Специалисты наши любят свою работу, они ваш интерьер сделают прекрасным. Мы будем рады видеть вас среди наших клиентов. Ищете дизайн квартиры в Питере? Spb.Studio-mint.ru – здесь можете увидеть фото интерьеров квартир. Предлагаем привлекательные цены и создаем проекты высочайшего уровня. Успех нашей работы подтверждают отзывы, ознакомиться с ними можете на нашем сайте. Свяжитесь с нами, чтобы обсудить детали. Готовы удовлетворить ваши пожелания!
Клининговая компания в Нижнем Новгороде https://prostaya-uborka.ru/ предоставляет услуги для физических и юридических лиц – уборка квартир, офисов, домов, коттеджей по отличным ценам. Профессиональные сотрудники. Воспользуйтесь на сайте калькулятором стоимости уборки или ознакомьтесь с ценами на каждый вид уборки на сайте.
Сувенирная продукция с логотипом и корпоративный мерч на заказ в Москве
https://canvas.instructure.com/eportfolios/2940531/Home/___________
заказать курсовую онлайн https://kursovyebankovskoe.ru/
Сайт https://zhenskiy.kyiv.ua – це онлайн-ресурс, який присвячений жіночим темам та інтересам. Тут зібрана інформація про моду, красу, здоров’я, відносини, кулінарію та багато іншого, що може бути корисним та цікавим для сучасних жінок.
Обучение на врача заочно maps-edu.ru
Что касается баллы нмо для врачей – Вы на правильном пути. Направления, по которым мы можем обучить: строительство, агрономия и сельское хозяйство, бухгалтерское дело, дефектология, пожарная безопасность, закупки, культура и искусство, документоведение и делопроизводство, менеджмент, метрология и стандартизация и многие другие.
Сувенирная продукция с логотипом и корпоративный мерч на заказ в Москве
https://canvas.instructure.com/eportfolios/2940559/Home/_____________
Помощь в получении допуска СРО, сертификата ISO и лицензий от МСМ
https://newsfrol.ru/214/12686/
Доставка цветов в Саратове https://flowers64.ru/ это отличная возможность заказать различные цветы, букеты, композиции, подарки, не выходя из дома.
Kind Macht Den Ganzen Tag Rollenspiele Natursekt Deutsch Clips
Помощь в получении допуска СРО, сертификата ISO и лицензий от МСМ
https://tvoi54.ru/articles/08-08-2019/3804-sro-stroitelei-osobennosti-vstuplenija.html
在線娛樂城的天地
隨著互聯網的快速發展,在線娛樂城(網上賭場)已經成為許多人娛樂的新選擇。網上娛樂城不僅提供多元化的游戲選擇,還能讓玩家在家中就能體驗到賭場的刺激和快感。本文將討論在線娛樂城的特徵、利益以及一些常見的遊戲。
什麼是在線娛樂城?
線上娛樂城是一種經由網際網路提供賭錢遊戲的平台。玩家可以經由電腦、智能手機或平板進入這些網站,參與各種賭錢活動,如撲克、輪盤賭、21點和老虎機等。這些平台通常由專業的程序公司開發,確保遊戲的公正和穩定性。
網上娛樂城的優勢
方便性:玩家無需離開家,就能享用賭錢的快感。這對於那些居住在遠離實體賭場區域的人來說特別方便。
多元化的游戲選擇:在線娛樂城通常提供比實體賭場更多樣化的遊戲選擇,並且經常更新遊戲內容,保持新鮮。
福利和獎勵:許多在線娛樂城提供多樣的優惠計劃,包括註冊獎金、存款紅利和忠誠度計劃,吸引新玩家並鼓勵老玩家繼續遊戲。
安全性和保密性:合法的在線娛樂城使用高端的加密技術來保護玩家的個人信息和金融交易,確保游戲過程的穩定和公正性。
常見的在線娛樂城游戲
撲克:德州撲克是最受歡迎的賭錢游戲之一。網上娛樂城提供多種撲克變體,如德州撲克、奧馬哈撲克和七張撲克等。
輪盤:輪盤是一種經典的賭博遊戲,玩家可以下注在單個數字、數字排列或顏色上,然後看小球落在哪個區域。
黑傑克:又稱為二十一點,這是一種競爭玩家和莊家點數的游戲,目標是讓手牌點數點數盡可能接近21點但不超過。
老虎机:老虎机是最容易且是最常見的博彩遊戲之一,玩家只需轉捲軸,等待圖案排列出獲勝的組合。
總結
線上娛樂城為現代的賭博愛好者提供了一個方便的、刺激且多樣化的娛樂方式。無論是撲克牌愛好者還是吃角子老虎迷,大家都能在這些平台上找到適合自己的遊戲。同時,隨著科技的不斷進步,在線娛樂城的游戲體驗將變化越來越真實和有趣。然而,玩家在體驗遊戲的同時,也應該保持,避免沉溺於賭博活動,保持健康健康的心態。
在線娛樂城的天地
隨著網際網路的迅速發展,網上娛樂城(在線賭場)已經成為許多人休閒的新選擇。在線娛樂城不僅提供多樣化的游戲選擇,還能讓玩家在家中就能體驗到賭場的興奮和快感。本文將討論在線娛樂城的特色、好處以及一些常有的游戲。
什麼是線上娛樂城?
在線娛樂城是一種透過互聯網提供賭博遊戲的平台。玩家可以通過電腦、智慧型手機或平板進入這些網站,參與各種賭錢活動,如德州撲克、賭盤、黑傑克和老虎机等。這些平台通常由專家的程序公司開發,確保游戲的公正性和安全性。
網上娛樂城的優勢
便利:玩家無需離開家,就能體驗賭博的快感。這對於那些生活在偏遠實體賭場地方的人來說特別方便。
多元化的游戲選擇:網上娛樂城通常提供比實體賭場更多的遊戲選擇,並且經常改進遊戲內容,保持新鮮。
福利和獎勵計劃:許多網上娛樂城提供豐厚的獎勵計劃,包括註冊獎勵、存款獎金和會員計劃,引誘新玩家並激勵老玩家不斷遊戲。
安全性和隱私性:合法的在線娛樂城使用高端的加密方法來保護玩家的私人信息和財務交易,確保遊戲過程的公平和公平。
常見的網上娛樂城遊戲
德州撲克:撲克是最受歡迎的賭博遊戲之一。線上娛樂城提供多樣撲克牌變體,如德州撲克、奧馬哈撲克和七張牌等。
輪盤:輪盤賭是一種傳統的賭場遊戲,玩家可以投注在單個數字、數字排列或顏色選擇上,然後看球落在哪個地方。
黑傑克:又稱為黑傑克,這是一種競爭玩家和莊家點數點數的游戲,目標是讓手牌點數盡可能接近21點但不超過。
老虎機:吃角子老虎是最簡單且是最常見的賭博遊戲之一,玩家只需轉捲軸,等待圖案圖案排列出獲勝的組合。
結論
網上娛樂城為當代賭博愛好者提供了一個便捷、刺激且多樣化的娛樂活動。無論是撲克愛好者還是吃角子老虎迷,大家都能在這些平台上找到適合自己的遊戲。同時,隨著技術的不斷發展,網上娛樂城的游戲體驗將變得越來越現實和吸引人。然而,玩家在享受遊戲的同時,也應該保持自律,避免沉迷於賭博活動,維持健康的遊戲心態。
На сайте https://genshin-news.ru/ вы отыщите новости, гайды популярных игр. Также здесь представлена различная интересная информация об играх, новости. Все публикации составлены экспертами, которые хорошо понимают в этой теме. Есть раздел с такой информацией, с которой вы сможете ознакомиться в данный момент. К примеру, есть баннеры 2020-2024, анонсы, даты выхода, а также сюжет различных игр. Обновления информации происходят каждый день. Поэтому и вы следите за ожидаемыми новинками, с которыми вам необходимо ознакомиться первым.
заказать курсовую работу https://kupit-kursovuyu-rabotu.ru/ с гарантией и антиплагиатом
сео консультант
Консультация по сео стратегии продвижению.
Информация о том как работать с низкочастотными ключевыми словами и как их определять
Подход по деятельности в конкурентной нише.
Обладаю постоянных клиентов сотрудничаю с 3 фирмами, есть что поделиться.
Ознакомьтесь мой профиль, на 31 мая 2024г
количество завершённых задач 2181 только здесь.
Консультация только устно, никаких скринов и отчетов.
Продолжительность консультации указано 2 ч, но по реально всегда на контакте без жёсткой привязки ко времени.
Как взаимодействовать с ПО это уже другая история, консультация по работе с софтом договариваемся отдельно в специальном услуге, определяем что требуется при разговоре.
Всё спокойно на расслабленно не в спешке
To get started, the seller needs:
Мне нужны контакты от телеграм канала для коммуникации.
общение только в устной форме, переписываться не хватает времени.
субботы и Воскресенье выходной
BAD REDIT REMOVE Loan Ranger Cash limit the amount you can borrow on your first few loans, but this limitation is offset by discounts on your fees for subsequent loans.
Сувенирная продукция с логотипом и корпоративный мерч на заказ в Москве
https://diigo.com/0wftu9
срочный ремонт телефонов москва
Новые технологии и материалы – компания, которая занимается производством комплектующих для радиотехнической промышленности. Предлагаем вам недорого приобрести крепеж и метизы. Следим за качеством продукции, поставляем ее в надлежащие сроки. Предоставляем исключительно квалифицированную помощь и помогаем в оформлении товара. https://ntmsp.ru/ – сайт, где можете прямо сейчас ознакомиться с акциями. У нас трудятся грамотные и надежные люди. Позвоните нашим специалистам, и они ответят на все необходимые вопросы.
Ищите глиняную посуду ручной работы? Зайдите на сайт https://gzhelgonchar.ru/ и вы найдете широкий ассортимент глиняной посуды от производителя ручной работы. Гжельская гончарня – это широкий ассортимент посуды из глины, которую можно купить с доставкой по РФ и СНГ. Подробнее на сайте.
Корпоративные Тарифы
https://aprovedstore.ru/kakie-tarify-na-bilajne-samye-vygodnye-s-internetom/
Мята – студия профессионального дизайна интерьеров в Москве все мечты воплощает в реальность. Будем рады видеть вас в числе своих клиентов. https://moskva.studio-mint.ru/ – здесь работают исключительно лучшие специалисты, они увлечены собственным делом и готовы принять любой вызов. Следим за новинками и трендами в индустрии интерьерного дизайна и предоставляем выгодные цены. Делаем проекты высочайшего уровня. Обсудим с вами все детали, звоните нам уже сейчас. Удовлетворим любые ваши пожелания!
Генераторы
https://telegra.ph/Obespechte-Bezopasnost-i-Prodolzhitelnost-Raboty—Kozhuhi-dlya-Dizelnyh-Generatorov-06-03
Портал uafakty.com.ua его пользователи отмечают лаконичность оформления. Здесь затрагиваются темы культуры, политики, спорта. Вас ждут актуальные новости шоу-бизнеса. Наслаждайтесь достойным контентом! uafakty.com.ua – https://uafakty.com.ua портал, который ценится за объективность и оперативность, он вам будет понятен. Тут имеется много полезной информации, ознакомиться с ней можно в любое удобное время. Все статьи удобны для чтения и снабжены фотографиями. Заходите на наш популярный сайт и читайте актуальные новости в любое время!
ремонт телефонов поблизости от меня
Больше интересной информации о строительстве и ремонте можно прочитать на сайте https://stroyka-gid.ru. Только самые популярные статьи и обзоры процесса ремонта помещений и строительства зданий.
Crypto Pump Signals for Binance https://cryptopumpsignalsbinance.com/ is a unique project that provides traders and investors with valuable insights into upcoming cryptocurrency pumps. Through its Telegram channel and AI capabilities, this project offers new opportunities for generating massive profits in the short-term.
Alte Rollenspiele C64 Rollenspiele Ps4 Deutsch
**Прогон Хрумером: Эффективное SEO-Продвижение Вашего Сайта**
В мире интернет-маркетинга существует множество методов и инструментов для продвижения сайтов, и одним из самых мощных и популярных является прогон Хрумером. Этот программный комплекс позволяет автоматизировать рутинные задачи SEO и значительно улучшить позиции сайта в поисковых системах. В этой статье мы подробно рассмотрим, что такое прогон Хрумером, как он работает и какие преимущества он может предложить.
**Что такое прогон Хрумером?**
Прогон Хрумером – это процесс автоматического размещения ссылок и сообщений на различных веб-ресурсах с использованием программы Хрумер. Это позволяет существенно увеличить количество обратных ссылок на ваш сайт, что является одним из ключевых факторов для улучшения его позиций в поисковых системах. Программа автоматически регистрируется на форумах, блогах, социальных сетях и других платформах, размещая ссылки и сообщения согласно заданным параметрам.
**Как работает прогон Хрумером?**
1. **Подготовка ресурсов**: В первую очередь необходимо составить список целевых веб-ресурсов, на которых будет производиться размещение ссылок. Это могут быть форумы, блоги, социальные сети и другие платформы.
2. **Создание шаблонов**: Далее создаются шаблоны для размещения ссылок и сообщений. Важно, чтобы тексты были уникальными и соответствовали правилам выбранных платформ.
3. **Настройка программы**: В Хрумере настраиваются параметры подключения, капча-сервисы и прокси-серверы для обеспечения стабильной работы программы.
4. **Запуск прогона**: После настройки всех параметров запускается процесс прогона, который программа выполняет автоматически. Хрумер регистрируется на сайтах, размещает ссылки и сообщения, а также разгадывает капчи.
5. **Мониторинг и анализ**: Важно регулярно отслеживать результаты прогона, анализируя отчеты о размещении ссылок и реакции аудитории. Это позволяет корректировать стратегию продвижения и улучшать её эффективность.
**Преимущества прогона Хрумером**
1. **Экономия времени**: Прогон Хрумером позволяет автоматизировать процесс размещения ссылок, что значительно экономит время по сравнению с ручным методом.
2. **Увеличение числа обратных ссылок**: Автоматическое размещение ссылок на множестве ресурсов способствует росту числа обратных ссылок, что положительно сказывается на позиции сайта в поисковых системах.
3. **Повышение видимости сайта**: Прогон Хрумером помогает улучшить видимость вашего сайта в интернете, привлекая новую аудиторию и увеличивая трафик.
4. **Гибкость и универсальность**: Хрумер поддерживает работу с множеством различных платформ и позволяет настраивать параметры прогона в соответствии с вашими потребностями.
**Заключение**
Прогон Хрумером – это эффективный метод автоматизации SEO-продвижения, который позволяет значительно улучшить позиции вашего сайта в поисковых системах. Используя этот мощный инструмент, вы сможете сэкономить время и усилия, сосредоточившись на стратегически важных задачах. Прогон Хрумером – это надежный способ увеличить число обратных ссылок, повысить видимость вашего сайта и привлечь больше посетителей.
Feel free to surf to my blog … http://jejucordelia.com/eng/bbs/board.php?bo_table=review_e&wr_id=266061
Корпоративные Тарифы
https://hairstyle-beauty.ru/arxivnye-tarify-mts-mozhno-li-ix-podklyuchit/.html
Больше интересной информации о строительстве и ремонте можно прочитать на сайте https://stroyka-gid.ru. Только самые популярные статьи и обзоры процесса ремонта помещений и строительства зданий.
Корпоративные Тарифы
https://tj-service.ru/novosti/samye-vygodnye-tarify-megafon-s-internetom
Генераторы
https://diigo.com/0wglbz
На сайте https://migrant.support/poluchieniie_nomiera_pesel вы сможете оформить заявку для того, чтобы получить номер Песель по доверенности. Важным моментом является то, что вам не нужно приезжать в офис, потому как все работы могут быть выполнены онлайн. Такая услуга обойдется вам в 300 злотых. Всем оптовым покупателям предоставляется скидка, а покупка происходит на наиболее выгодных условиях. Выставляются фактуры vat. Документ высылается в день оформления, без опозданий и почтой
где ремонтируют телефоны
БроМод https://bromod.ru/ – MODный BRO Market. Андроид APK моды и премиум игры. Здесь ты найдёшь оригинальные и МОДные приложения на свой Андроид апарат! БроМод – это Аналог Play Market с прямыми ссылками и бесплатными приложениями! Каждый пользователь найдет что-то свое. Для выбора доступно большое количество игр: разобраться в них поможет удобный фильтр поиска. Не меньше чем несколько сотен страниц с онлайн-шутерами, головоломками и другими игрушками размещены на сайте русскоязычной версии Play Market.
smm panel cheap smm panel
Генераторы
https://rewarddebtor7.bloggersdelight.dk/2024/06/03/%d0%b2%d0%b0%d1%88-%d0%b3%d0%b5%d0%bd%d0%b5%d1%80%d0%b0%d1%82%d0%be%d1%80-%d0%b2-%d0%b1%d0%b5%d0%b7%d0%be%d0%bf%d0%b0%d1%81%d0%bd%d0%be%d1%81%d1%82%d0%b8-%d0%ba%d0%be%d0%bd%d1%82%d0%b5%d0%b9%d0%bd/
Czech health insurance for foreigners in Prague https://vaclavak48.cz/ is comprehensive health insurance for foreigners in the Czech Republic at the best prices. Центр Страхования Иностранцев в Праге, Чехия – это Медицинское страхование иностранцев в Чехии, а также Комплексные медицинские страховки для иностранных студентов в Праге и Чехии по лучшим ценам от страховых компаний. Все услуги в одном месте. Узнайте подробнее на сайте.
smm provider paypal smm panel
Ehepaar Sexspielzeug Sexfilm 1940 Analsex
smm provider smm provider
Сайт chasnovyn.com.ua – это источник актуальных новостей Украины, которые в доступе 24/7. Статьи снабжены четкими фотографиями. Всех своих читателей ценим и гордимся тем, что у нас есть возможность для них предложить только лучшее. Поудобнее устраивайтесь и достоверную информацию читайте уже сейчас. chasnovyn.com.ua – https://chasnovyn.com.ua портал, который вашего внимания точно заслуживает. Здесь затрагиваются темы политики, экономики и др. Все материалы проверены на достоверность, можете быть уверены в их качестве. Посетите наш ресурс и будете в курсе актуальных событий!
Завод «СХТ» предлагает лучшее весоизмерительное оборудование. Мы имеем свою метрологическую лабораторию, а также сервисную службу. Проводим поверку более 2000 единиц автомобильных весов в год! https://xn--q1aci.xn--p1ai/ – сайт, где вы можете узнать о том, каким нынешний весоизмерительный комплекс должен быть. Здесь есть фотогалерея и отзывы довольных клиентов. Можете заказать у нас коллейные, электронные, переносные автомобильные весы. Обращайтесь к нам, мы быстро реагируем на заявки и консультируем по телефону по всем вопросам.
spotify music promotion https://banger-music.com
Краснодарский завод, производимое им котельное оборудование, проходит регламентированные технические испытания, поэтому отвечает необходимым требованиям безопасности. Работаем по всей Российской Федерации и ряду стран СНГ. С нами вы существенно экономите собственное время и денежные средства. Ищете промышленные паровые котлы? Kzko-gaz.ru – сайт, где есть каталог и представлены отзывы о нашем заводе, ознакомиться с ними можно прямо сейчас. Можете быть уверены – любой произведенный котел или же котельная будут вовремя доставлены. Гарантируем качество, создавая тепло!
buy instagram followers paypal https://promobanger.com/
free soudcloud plays https://promobanger.com/
rap marketing agency free music promotion
free soundcloud streams https://promobanger.com/
music promotion free music promotion
https://www.instagram.com/asiapsiholog_family/
Генераторы
https://ariesgemini3.werite.net/moshchnost-i-nadezhnost-dizel-nye-generatory-na-elektrostantsiiakh
Dinopolis считается самым забавным онлайн-слотом, дарящий множество позитивных эмоций. Игра не оставляет никого равнодушным, потому как имеет отменную анимацию, звук и графику. Предлагаем вам захватывающее путешествие в мир динозавров. У вас есть возможность, играя, зарабатывать реальные деньги. Приготовьтесь к веселью и адреналину. https://dinopolisgame.com/ru/ – сайт, где найдете интересную информацию о данном слоте. Узнаете, как сделать ставку в игре Динополис, сколько можно выиграть. Удачи вам!
Ищете рабочие промокоды Яндекс Маркета? Предлагаем подписаться на канал Олега Петрова. Он здесь делится новой подборкой акций и купонов. Вы нигде не найдете в интернете как у него, такого количества промокодов. Оцените преимущества экономного шопинга. https://dzen.ru/a/ZgxKFq5bOTUwDw_w – тут имеются ссылки, по которым можно поймать топовые скидки в различных категориях. Все промокоды проверены. Воспользуйтесь актуальными предложениями, которые специально для вас Петров Олег нашел. Делайте приобретения с удовольствием!
installment loans bad credit no payday loans The loans can be availed by folks quickly, when each detail are found to be authentic.
На сайте https://outline.monster вы сможете воспользоваться ключом на OUTLINE VPN за очень скромную и привлекательную цену. Теперь вы получите доступ к полностью анонимному, безопасному Интернету. Вас обрадует безупречная скорость, легкость использования. При этом отсутствует логгирование. Пользоваться можно абсолютно на любом устройстве. Отсутствуют даже незначительные ограничения. Приобретайте ключ и пользуйтесь всеми благами уже через пару минут. Сайт наделен простым интерфейсом, удобной, оперативной установкой.
На сайте https://stroyengr.ru/ получите всю актуальную, интересную информацию, которая касается недвижимости, налоговых вычетов, финансов, ипотеки, продажи квартиры, материнского капитала, налогов и многого другого. Все материалы с поправкой на обновления, а потому вы можете ориентироваться на этот контент. Обязательно побывайте в разделе «Свежие записи», где вы найдете не менее интересный и любопытный контент. Вы узнаете и о том, как правильно оформить дарственную, про налоговый вычет.
Генераторы
https://burnbengal6.bloggersdelight.dk/2024/06/03/%d0%b3%d0%be%d1%82%d0%be%d0%b2%d0%bd%d0%be%d1%81%d1%82%d1%8c-%d0%ba-%d0%bb%d1%8e%d0%b1%d1%8b%d0%bc-%d1%81%d0%b8%d1%82%d1%83%d0%b0%d1%86%d0%b8%d1%8f%d0%bc-%d0%bf%d0%be%d0%ba%d1%83%d0%bf%d0%ba%d0%b0/
liga italia
Inspirasi dari Kutipan Taylor Swift
Taylor Swift, seorang vokalis dan pengarang lagu terkenal, tidak hanya dikenal oleh karena nada yang elok dan suara yang merdu, tetapi juga karena lirik-lirik lagunya yang penuh makna. Dalam syair-syairnya, Swift sering melukiskan berbagai aspek eksistensi, berawal dari cinta hingga rintangan hidup. Berikut adalah beberapa petikan inspiratif dari lagu-lagunya, dengan terjemahannya.
“Mungkin yang paling baik belum tiba.” – “All Too Well”
Arti: Bahkan di saat-saat sulit, selalu ada secercah asa dan peluang tentang hari yang lebih baik.
Syair ini dari lagu “All Too Well” mengingatkan kita bahwa meskipun kita mungkin berhadapan dengan masa sulit saat ini, selalu ada kemungkinan bahwa masa depan akan membawa perubahan yang lebih baik. Ini adalah amanat harapan yang menguatkan, mendorong kita untuk tetap bertahan dan tidak putus asa, karena yang paling baik mungkin belum tiba.
“Aku akan tetap bertahan sebab aku tidak bisa melakukan apa pun tanpa kamu.” – “You Belong with Me”
Arti: Menemukan cinta dan bantuan dari pihak lain dapat memberi kita tenaga dan niat untuk terus berjuang lewat kesulitan.
neo77
Ashley JKT48: Bintang yang Bersinar Gemilang di Dunia Idola
Siapakah Ashley JKT48?
Siapakah sosok muda berbakat yang menarik perhatian banyak penggemar musik di Nusantara dan Asia Tenggara? Dialah Ashley Courtney Shintia, atau yang dikenal dengan nama bekennya, Ashley JKT48. Menjadi anggota dengan grup idola JKT48 pada tahun 2018, Ashley dengan cepat muncul sebagai salah satu anggota paling terkenal.
Biografi
Lahir di Jakarta pada tanggal 13 Maret 2000, Ashley memiliki garis Tionghoa-Indonesia. Ia memulai perjalanannya di industri entertainment sebagai peraga dan aktris, sebelum akhirnya masuk dengan JKT48. Personanya yang periang, nyanyiannya yang kuat, dan kemahiran menari yang mengagumkan membuatnya idola yang sangat disukai.
Penghargaan dan Pengakuan
Popularitas Ashley telah dikenal melalui aneka penghargaan dan nominasi. Pada masa 2021, ia memenangkan pengakuan “Anggota Paling Populer JKT48” di acara JKT48 Music Awards. Ia juga diberi gelar sebagai “Idol Tercantik se-Asia” oleh sebuah majalah online pada tahun 2020.
Fungsi dalam JKT48
Ashley memainkan fungsi krusial dalam group JKT48. Beliau adalah anggota Tim KIII dan berperan menjadi dancer utama dan penyanyi utama. Ashley juga terlibat sebagai bagian dari unit sub “J3K” dengan Jessica Veranda dan Jennifer Rachel Natasya.
Karir Solo
Selain aktivitasnya bersama JKT48, Ashley juga merintis karir individu. Ia telah merilis sejumlah lagu single, antara lain “Myself” (2021) dan “Falling Down” (2022). Ashley juga telah bekerja sama bersama musisi lain, seperti Afgan dan Rossa.
Kehidupan Privat
Selain kancah panggung, Ashley dikenali sebagai sosok yang rendah hati dan ramah. Ia menikmati menghabiskan waktu dengan keluarga dan sahabat-sahabatnya. Ashley juga menyukai hobi mewarnai dan photography.
На сайте https://autopiter.ru/ закажите как оригинальные, так и неоригинальные запчасти, изучите каталоги ВАЗ, КАМАЗ, ГАЗ. Также здесь представлены автомасла, химия, аккумуляторы, все для спецтехники и многое другое. Вся продукция от именитых, лидирующих брендов, которые отвечают за качество. На продукцию установлены доступные цены, действует оперативная доставка. У всех масел имеется гарантия качества. При необходимости можно воспользоваться онлайн-поиском фильтров. Заказы принимают, обрабатывают каждый день.
проверить адрес usdt 87
Верификация аккаунта USDT
Контроль токенов на блокчейне TRC20 и других цифровых операций
На данном веб-сайте представлены развернутые обзоры разнообразных инструментов для анализа переводов и аккаунтов, включая anti-money laundering контроли для USDT и иных блокчейн-активов. Вот важные опции, которые в наших обзорах:
Контроль USDT на сети TRC20
Известные инструменты обеспечивают комплексную анализ платежей криптовалюты на платформе TRC20. Это дает возможность фиксировать подозрительную операции и выполнять нормативным положениям.
Верификация платежей токенов
В наших обзорах доступны инструменты для всестороннего проверки и мониторинга платежей токенов, которые обеспечивает обеспечивать чистоту и безопасность транзакций.
антиотмывочная анализ криптовалюты
Определенные инструменты предлагают антиотмывочную верификацию монет, обеспечивая обнаруживать и пресекать ситуации финансовых преступлений и валютных мошенничеств.
Верификация кошелька монет
Наши обзоры содержат сервисы, позволяющие предусматривают верифицировать счета USDT на предмет санкций и подозреваемых операций, предоставляя дополнительный уровень уровень безопасности.
Контроль транзакции монет TRC20
Вы найдете описаны инструменты, предлагающие анализ операций токенов на платформе TRC20 платформы, что гарантирует обеспечивает соблюдение всем необходимым требованиям нормам.
Анализ аккаунта кошелька криптовалюты
В ревью доступны сервисы для контроля аккаунтов аккаунтов криптовалюты на наличие рисков проблем.
Верификация счета монет на сети TRC20
Наши обзоры содержат сервисы, предоставляющие верификацию кошельков токенов в блокчейн-сети TRC20 блокчейна, что предотвращает позволяет предотвратить незаконных операций и экономических мошенничеств.
Анализ USDT на чистоту
Рассмотренные ресурсы обеспечивают контролировать операции и аккаунты на чистоту, обнаруживая подозреваемую активность.
антиотмывочная верификация криптовалюты на блокчейне TRC20
В оценках вы найдете платформы, предоставляющие антиотмывочную верификацию для USDT на блокчейне TRC20 платформы, что позволяет вашему делу выполнять общепринятым нормам.
Анализ токенов на сети ERC20
Наши оценки содержат сервисы, предоставляющие контроль USDT в блокчейн-сети ERC20, что позволяет гарантирует полный анализ платежей и счетов.
Проверка цифрового кошелька
Мы описываем сервисы, предоставляющие сервисы по анализу криптовалютных кошельков, в том числе мониторинг платежей и обнаружение подозреваемой деятельности.
Контроль кошелька цифрового кошелька
Наши ревью представляют сервисы, дающие возможность верифицировать адреса криптокошельков для гарантирования дополнительной степени безопасности.
Анализ цифрового кошелька на операции
Вы найдете найдете инструменты для проверки криптокошельков на переводы, что помогает обеспечивает поддерживать прозрачность платежей.
Контроль виртуального кошелька на легитимность
Наши описания охватывают сервисы, обеспечивающие контролировать криптовалютные кошельки на отсутствие подозрительных действий, определяя все подозреваемые активности.
Читая подробные оценки, вы сможете выбрать сможете надежные инструменты для проверки и отслеживания цифровых переводов, чтобы гарантировать надежный уровень безопасности надежности и соблюдать необходимым регуляторным стандартам.
служба такси телефон мобильное такси
курсовые работы на заказ https://zakazat-kursovuyu-rabotu7.ru
На сайте https://climat.best приобретите качественные, функциональные кондиционеры, сплит-системы, тепловые насосы, а также чиллеры. Вся продукция именитых, проверенных и надежных брендов, а потому техника прослужит долго без потери технических характеристик, возможностей. А если необходимо подобрать что-то определенное, то воспользуйтесь специальным поиском. Перед вами есть и самые популярные позиции, которые пользуются особенным спросом среди покупателей. В интернет-магазине вы отыщите как настенные, так и напольно-потолочные конструкции, кассетные.
In this eager strategy, players vie in multiplayer shooting matches on distinct battlegrounds. The open-handed of bullet force is to outgun opponents and secure quelling using key thinking and precipitate reflexes. With its extensive weapon abstract and customizable gameplay, this design delivers an intoxicating shooting affair
buy generic rabeprazole – order metoclopramide 20mg generic order motilium sale
Igrosite – сайт для геймеров, который предлагает широкий спектр контента, включая новости, обзоры, статьи и руководства. Здесь можно выбрать игры для своей коллекции и общаться с игроками в дружеской атмосфере, узнать последние события в мире игр. https://igrosite.ru – портал, где мы для вас подготовили с разработчиками интервью, аналитические факты и материалы, для того, чтобы вы за кулисы создания игр могли заглянуть. Узнаете интересные подробности о развитии этой увлекательной отрасли. Заходите уже сейчас на наш сайт!
Портал ukrayinka.com.ua станет вам надежным другом, он пользуется большой популярностью. Мы освещаем экономические и общественно-политические события в Украине. Предлагаем только качественную информацию. ukrayinka.com.ua – https://ukrayinka.com.ua сайт, который понятен любому пользователю. Здесь имеются статьи с четкими фотографиями. Садитесь и читайте самые горячие новости. Мы обеспечим вас лучшими сведениями. Если цените свежесть и наполненность, смело выбирайте наш ресурс. Вы останетесь довольны!
Корпоративные Тарифы
https://gnezdoparanoika.ru/news/44150-vygodnye-tarify-mts-s-internetom.html
payday loans legit online If you are looking for the fast loan, then this instant loans today scheme is the best answer to you.
Генераторы
https://canvas.instructure.com/eportfolios/2945392/Home/________
перевод документов
мобильное такси https://taxi-novocherkassk.ru
Генераторы
https://telegra.ph/Gotovnost-k-Lyubym-Situaciyam—Pokupka-Dizelnogo-Generatora-dlya-Doma-06-03
заказ такси по телефону https://zakaz-taxionline.ru
дешевое такси телефон детское такси
Online Gambling Sites: Innovation and Benefits for Contemporary Community
Overview
Online gambling platforms are digital platforms that offer players the chance to engage in betting activities such as poker, roulette, blackjack, and slots. Over the last several years, they have turned into an essential part of online entertainment, providing various advantages and opportunities for players around the world.
Accessibility and Convenience
One of the main advantages of digital casinos is their accessibility. Users can play their preferred games from any location in the globe using a PC, iPad, or mobile device. This conserves hours and money that would otherwise be used traveling to land-based casinos. Additionally, 24/7 access to activities makes online gambling sites a easy choice for people with busy lifestyles.
Range of Games and Entertainment
Digital casinos offer a wide range of games, enabling all users to discover an option they like. From classic card activities and table activities to slots with diverse concepts and increasing prizes, the range of activities guarantees there is something for every preference. The option to engage at various proficiencies also makes digital casinos an ideal location for both novices and experienced gamblers.
Financial Advantages
The online gambling industry adds greatly to the economy by generating employment and generating revenue. It backs a diverse range of careers, including programmers, client assistance agents, and marketing professionals. The revenue generated by digital gambling sites also contributes to tax revenues, which can be used to support community services and development projects.
Advancements in Technology
Digital casinos are at the cutting edge of technological advancement, continuously integrating new innovations to improve the playing experience. Superior visuals, live dealer activities, and virtual reality (VR) casinos provide engaging and realistic gaming experiences. These advancements not only improve player satisfaction but also expand the limits of what is possible in online entertainment.
Safe Betting and Assistance
Many digital casinos promote responsible gambling by offering tools and assistance to help users manage their gaming activities. Options such as deposit limits, self-ban choices, and availability to assistance programs ensure that users can enjoy gaming in a secure and monitored environment. These measures demonstrate the sector’s dedication to encouraging healthy betting habits.
Social Interaction and Community
Digital gambling sites often offer interactive options that enable users to connect with each other, creating a sense of community. Multiplayer activities, communication tools, and networking integration allow users to connect, share stories, and build relationships. This social aspect enhances the entire betting experience and can be particularly beneficial for those seeking community engagement.
Summary
Online casinos offer a wide variety of advantages, from availability and convenience to financial benefits and technological advancements. They provide diverse gaming choices, support safe betting, and promote social interaction. As the sector continues to evolve, digital casinos will probably stay a major and beneficial force in the world of digital entertainment.
free slots games
No-Cost Slot Games: Amusement and Perks for All
No-Cost slot games have become a widespread form of online amusement, offering players the rush of slot machines devoid of any cash stake.
The main aim of no-cost slot games is to deliver a entertaining and immersive way for users to experience the thrill of slot machines absent any cash jeopardy. They are designed to imitate the sensation of actual-currency slots, giving players to activate the reels, experience various themes, and win digital rewards.
Pleasure: Complimentary slot games are an superb avenue of amusement, granting periods of enjoyment. They present colorful imagery, immersive audio, and wide-ranging themes that accommodate a extensive array of tastes.
Proficiency Improvement: For beginners, complimentary slot games offer a risk-free situation to learn the principles of slot machines. Players can become familiar with diverse options, payout lines, and additional features free from the fear of sacrificing funds.
Relaxation: Playing free slot games can be a wonderful way to de-stress. The straightforward experience and the possibility for electronic rewards make it an satisfying hobby.
Community Engagement: Many gratis slot games integrate collaborative features such as competitions and the capacity to network with peers. These features add a collective aspect to the entertainment experience, encouraging players to measure up against one another.
Benefits of Gratis Slot Games
1. Reachability and Simplicity
Gratis slot games are effortlessly accessible to anyone with an network connection. They can be utilized on various devices including PCs, mobile devices, and mobile phones. This simplicity permits players to savor their preferred offerings at any time and irrespective of location.
2. Monetary Innocuousness
One of the paramount benefits of gratis slot games is that they eliminate the cash-related dangers associated with betting. Players can experience the rush of rotating the reels and earning big rewards without risking any capital.
3. Breadth of Offerings
Gratis slot games are presented in a broad selection of themes and configurations, from classic fruit slots to contemporary video-based slots with intricate themes and illustrations. This breadth secures that there is an option for all, independent of their tastes.
4. Developing Intellectual Aptitudes
Playing free slot games can help improve mental capabilities such as anticipatory planning. The task to pursue win lines, internalize operational principles, and foresee effects can offer a cerebral exercise that is simultaneously satisfying and useful.
5. Risk-Free Trial Phase for Paid-Participation
For those pondering progressing to paid slots, free slot games present a beneficial testing ground. Players can try out different games, build methods, and build self-belief ahead of deciding to wager live money. This groundwork can culminate in a more informed and satisfying actual-currency gaming encounter.
Key Takeaways
Complimentary slot games deliver a abundance of advantages, from pure amusement to capability building and community engagement. They provide a worry-free and non-monetary way to savor the excitement of slot machines, rendering them a worthwhile addition to the world of online leisure. Whether you’re seeking to destress, sharpen your cognitive skills, or merely experience pleasure, gratis slot games are a excellent alternative that persistently entertain players across.
На сайте https://vpolshe.com/zamena-voditelskogo-udostovereniya-na-polskoe-zamena-prav-na-polskie/ закажите такую важную услугу, как замена водительского удостоверения на польское. Услуга подходит для тех, кто проживает в ЕС. Воспользоваться такой важной услугой смогут граждане Беларуси, России, Грузии, различных других стран. Для того чтобы произвести замену, следует подать полный пакет документов на ВНЖ. Услуга обойдется недорого, при этом вы получите все документы сразу на руки.
Complimentary Slot Games: Amusement and Perks for Players
Overview
Slot-based games have long been a mainstay of the wagering interaction, granting users the opportunity to earn significant rewards with just the operation of a switch or the push of a mechanism. In the modern era, slot-related offerings have also become popular in virtual gambling platforms, constituting them accessible to an further more extensive group.
Entertainment Value
Slot-based games are developed to be enjoyable and immersive. They showcase animated graphics, suspenseful auditory elements, and various themes that suit a extensive selection of inclinations. Regardless of whether participants enjoy traditional fruit-related symbols, adventure-themed slot-related offerings, or slot-related offerings rooted in iconic films, there is a choice for all. This variety provides that participants can persistently find a game that suits their inclinations, delivering spans of amusement.
Easy to Play
One of the biggest positives of slot machines is their simplicity. In contrast to certain wagering activities that necessitate strategy, slot-based activities are straightforward to understand. This constitutes them accessible to a wide population, incorporating beginners who may experience deterred by more intricate activities. The straightforward quality of slot-based activities enables users to decompress and relish the offering without stressing about intricate protocols.
Unwinding and Destressing
Engaging with slot-related offerings can be a wonderful way to unwind. The cyclical character of rotating the reels can be serene, delivering a mental break from the demands of regular existence. The possibility for earning, regardless of whether it constitutes merely minor figures, brings an factor of excitement that can boost players’ dispositions. Numerous players determine that interacting with slot machines assists them unwind and divert their attention from their issues.
Shared Experiences
Slot-related offerings in addition present opportunities for social engagement. In traditional wagering facilities, participants typically gather near slot-based games, cheering co-participants on and commemorating achievements together. Virtual slot-based games have as well integrated communal aspects, such as competitions, enabling customers to connect with peers and share their encounters. This sense of collective engagement elevates the overall leisure experience and can be specifically satisfying for users desiring social connection.
Monetary Upsides
The widespread adoption of slot machines has significant financial benefits. The domain generates positions for offering creators, gambling employees, and client services representatives. Moreover, the earnings obtained by slot-based activities adds to the financial system, granting budgetary earnings that support public programs and systems. This monetary influence extends to equally brick-and-mortar and digital gambling establishments, constituting slot machines a worthwhile element of the gaming domain.
Mental Upsides
Partaking in slot-based activities can also yield cerebral benefits. The offering demands players to reach rapid choices, identify patterns, and oversee their wagering tactics. These intellectual processes can facilitate sustain the thought processes acute and bolster mental functions. Specifically for mature players, participating in cognitively challenging pursuits like playing slot machines can be helpful for preserving cognitive capacity.
Reachability and User-Friendliness
The advent of internet-based wagering environments has made slot-based activities more accessible than ever. Users can relish their cherished slot-based games from the convenience of their private residences, employing computers, pads, or mobile phones. This user-friendliness permits players to partake in at any time and irrespective of location they want, free from the need to make trips to a physical gaming venue. The accessibility of gratis slots likewise permits participants to enjoy the offering free from any economic outlay, establishing it an inclusive kind of fun.
Summary
Slot-related offerings deliver a abundance of benefits to people, from absolute pleasure to cerebral upsides and communal interaction. They provide a secure and zero-cost way to enjoy the excitement of slot-related offerings, constituting them a valuable extension to the landscape of digital leisure.
Whether you’re looking to relax, enhance your cognitive abilities, or simply enjoy yourself, slot-based games are a fantastic choice that persistently delight participants across.
Main Conclusions:
– Slot-based activities deliver fun through vibrant visuals, engaging soundtracks, and wide-ranging concepts
– Straightforward operation constitutes slot-based games accessible to a wide audience
– Partaking in slot machines can deliver stress relief and cerebral advantages
– Communal functions improve the total leisure experience
– Virtual reachability and complimentary options make slot machines welcoming styles of fun
In summary, slot-based activities constantly deliver a multifaceted collection of advantages that match users across. Whether desiring sheer entertainment, mental activation, or social participation, slot-based activities remain a wonderful option in the transforming world of virtual gaming.
Prosperity Casino: Where Fun Combines With Prosperity
Prosperity Casino is a well-liked virtual location characterized for its broad array of activities and exciting rewards. Let’s investigate why so several players relish engaging with Luck Wagering Environment and in which manner it benefits them.
Pleasure-Providing Aspect
Wealth Wagering Environment grants a range of activities, involving time-honored table games like vingt-et-un and ball-and-number game, as alongside novel slot-based games. This range secures that there is an alternative for everyone, rendering every single trip to Fortune Gaming Site rewarding and amusing.
Large Prizes
One of the primary aspects of Wealth Wagering Environment is the prospect to achieve substantial winnings. With generous top rewards and benefits, players have the prospect to achieve unexpected success with a individual round or game. Several players have received substantial payouts, augmenting the anticipation of engaging with Prosperity Gambling Platform.
User-Friendliness and Availability
Prosperity Casino’s digital platform establishes it as convenient for players to enjoy their most preferred offerings from any setting. Regardless of whether at home or while traveling, participants can utilize Fortune Gaming Site from their PC or mobile device. This accessibility provides that players can enjoy the excitement of the gaming regardless of when they desire, devoid of the necessity to make trips.
Range of Possibilities
Fortune Gaming Site presents a comprehensive selection of offerings, providing that there is a choice for every form of player. Beginning with established wagering games to narrative-driven slot-based activities, the variety sustains players engaged and entertained. This assortment also permits participants to try out unfamiliar games and identify different most preferred.
Promotional Benefits
Wealth Gaming Site compensates its participants with promotional benefits and advantages, featuring welcome bonuses and loyalty initiatives. These bonuses not merely improve the entertainment experience but in addition boost the opportunities of winning big. Customers are steadfastly incentivized to sustain interaction, rendering Wealth Gambling Platform increasingly enticing.
Shared Experiences and Social Networking
ChatGPT l Валли, 6.06.2024 4:30]
Fortune Gambling Platform delivers a environment of community and group-based participation for customers. Via discussion forums and forums, players can interact with each other, communicate advice and strategies, and sometimes develop friendships. This social element adds an additional layer of satisfaction to the leisure encounter.
Recap
Fortune Wagering Environment presents a wide selection of upsides for users, including pleasure, the prospect of securing major payouts, simplicity, range, perks, and social interaction. Whether looking for thrill or wishing to produce an unexpected outcome, Luck Gaming Site offers an exhilarating experience for any partake in.
перевод с иностранных языков
заказ такси в новочеркасске по телефону https://zakaz-taxionline.ru
free poker machine games
Gratis Poker Machine Experiences: A Pleasurable and Advantageous Interaction
No-Cost slot-based games have transformed into gradually widely-accepted among customers desiring a captivating and safe leisure experience. These experiences offer a extensive range of rewards, rendering them a chosen alternative for several. Let’s explore in what way gratis electronic gaming offerings can advantage users and the reasons why they are so comprehensively savored.
Amusement Factor
One of the main factors users savor engaging with free poker machine games is for the entertainment value they provide. These offerings are created to be captivating and exciting, with animated illustrations and immersive sound effects that bolster the overall entertainment encounter. Whether you’re a occasional user looking to while away the hours or a dedicated leisure activity enthusiast seeking excitement, free poker machine games present pleasure for everyone who.
Capability Building
Playing gratis electronic gaming activities can likewise help refine worthwhile skills such as critical analysis. These experiences require users to make rapid selections contingent on the gameplay elements they are dealt, facilitating them improve their problem-solving aptitudes and intellectual prowess. Additionally, customers can try out multiple strategies, refining their faculties free from the possibility of financial impact of forfeiting actual currency.
Simplicity and Approachability
A further reward of gratis electronic gaming activities is their simplicity and availability. These experiences can be partaken in online from the ease of your own abode, excluding the necessity to travel to a land-based gaming venue. They are in addition present around the clock, giving customers to relish them at any occasion that accommodates them. This convenience constitutes complimentary slot-based activities a well-liked possibility for players with demanding timetables or those seeking a rapid gaming fix.
Shared Experiences
A significant number of complimentary slot-based games likewise grant communal features that permit participants to connect with one another. This can feature communication channels, discussion boards, and competitive modes where participants can pit themselves against each other. These interpersonal connections contribute an further layer of enjoyment to the leisure sensation, enabling customers to communicate with like-minded individuals who display their passions.
Anxiety Reduction and Mental Unwinding
Playing complimentary slot-based games can in addition be a wonderful approach to relax and de-stress after a tiring stretch of time. The effortless gameplay and tranquil music can enable reduce tension and nervousness, delivering a welcome break from the demands of regular life. Also, the anticipation of obtaining digital coins can elevate your frame of mind and leave you feeling rejuvenated.
Conclusion
Complimentary slot-based offerings grant a extensive variety of rewards for customers, encompassing enjoyment, proficiency improvement, ease, communal engagement, and stress relief and mental rejuvenation. Regardless of whether you’re wanting to enhance your leisure faculties or merely have fun, free poker machine experiences grant a rewarding and pleasurable sensation for users of any degrees.
На сайте http://nemans.ru вы сможете приобрести всю необходимую продукцию, включая пакеты с ручками, фасовочные пакеты, мешки полипропиленовые, пленку армированную, полиэтиленовую. Также в разделе имеется ветошь, ароматное мыло, перчатки, черенки, бытовая химия, ведра и многое другое, что вы сможете заказать прямо сейчас. Среди рекомендованных товаров находятся вязаные перчатки, туалетная бумага, хозяйственное мыло, неткол. Вся продукция отличного качества, надежная и наделена длительными сроками эксплуатации.
online poker
Online Casino-Style Games: A Wellspring of Amusement and Competency Enhancement
Digital poker has arisen as a widely-accepted form of pleasure and a avenue for proficiency improvement for customers globally. This piece explores the beneficial components of internet-based card games and the extent to which it upsides users, emphasizing its pervasive appeal and impact.
Entertainment Value
Virtual casino-style games provides a enthralling and immersive entertainment sensation, spellbinding customers with its calculated gameplay and variable outcomes. The offering’s immersive character, along with its social components, delivers a one-of-a-kind kind of pleasure that many find enjoyable.
Capability Building
Apart from fun, digital table games also serves as a platform for competency enhancement. The activity necessitates decision-making, decision-making under pressure, and the capacity to read opponents, all of these lend to intellectual maturation. Customers can elevate their critical-thinking aptitudes, self-awareness, and prudent decision-making aptitudes through consistent gameplay.
User-Friendliness and Availability
One of the main upsides of digital table games is its simplicity and accessibility. Participants can experience the offering from the convenience of their homes, at whichever time that fits them. This availability eradicates the obligation for trips to a physical casino, making it a convenient alternative for individuals with hectic routines.
Diversity of Options and Bet Sizes
Digital table games infrastructures provide a extensive breadth of activities and stakes to accommodate players of every types of abilities and preferences. Whether you’re a beginner seeking to grasp the fundamentals or a skilled pro aiming for a test, there is a offering for your needs. This range ensures that players can consistently uncover a activity that matches their capabilities and financial resources.
Communal Engagement
Internet-based card games as well delivers prospects for shared experiences. Numerous systems provide interactive functions and competitive formats that give players to connect with like-minded players, exchange experiences, and develop personal connections. This social factor adds substance to the interactive interaction, constituting it as more pleasurable.
Financial Rewards
For certain individuals, internet-based card games can in addition be a provider of monetary gains. Talented participants can obtain substantial profits through regular interactivity, making it a money-making undertaking for those who dominate the experience. Additionally, several virtual casino-style games events provide major reward funds, providing users with the opportunity to earn significant rewards.
Key Takeaways
Online poker grants a array of rewards for customers, encompassing fun, capability building, ease, interpersonal connections, and profit potential. Its popularity continues to expand, with many individuals shifting to digital table games as a provider of pleasure and development. Whether you’re looking to refine your abilities or merely derive entertainment, online poker is a adaptable and advantageous leisure activity for players of any perspectives.
jsa cash loans Find a company or lender that does not require collecting any collateral or getting any credit information.
служба поддержки такси служба поддержки такси
заказ такси эконом такси бизнес класс
order bisacodyl sale – loperamide uk buy liv52 without prescription
Новинки музыки https://muzlada.net/ за сегодня в mp3, Хиты России и Украины. Треки как самых популярных, так и малоизвестных исполнителей. Слушайте треки и скачивайте их на свой ПК или телефон. У нас вы найдёте самые свежие новинки песен в хорошем качестве. На сайте собрана огромная коллекция композиций разных направлений, ведь мы хотим, чтобы каждый нашёл то, что ему нужно. В каталоге представлена как русская музыка, так и зарубежные хиты. Любой из них вы сможете скачать абсолютно бесплатно в формате MP3.
order rabeprazole 10mg sale – motilium buy online buy motilium pills
курсовые работы на заказ https://zakazat-kontrolnuyu7.ru
Популярный интернет-магазин CLAPS предлагает купить по доступной цене DreamStalker Expert. Прибор в лобной части маски находится, особая конструкция обеспечивает вентиляцию, отсутствие запотевание лба, комфортный сон и охлаждение. https://claps.me – сайт, где имеется каталог, в нем есть описание, характеристики, фотографии товара. Тут предложены отзывы радостных клиентов, с которыми вы можете ознакомиться уже сейчас. Также здесь найдете инструкции к DreamStalker Expert.
order bisacodyl 5mg – buy generic bisacodyl for sale generic liv52 10mg
решение задач на заказ https://resheniye-zadach7.ru заказать онлайн
На портале exclusivenews.com.ua у вас есть возможность найти исключительно лучшие горячие новости. Мы ценим своих читателей, предоставляем актуальную и качественную информацию. Ознакомиться с ней можно в любое удобное время. Будьте в курсе главных новостных событий дня! exclusivenews.com.ua – https://exclusivenews.com.ua популярный сайт, который уважают за оперативность. Он будет для вас лучшим другом. Вы узнаете много интересного: о происходящих событиях в стране и мире. Статьи сопровождаются четкими фотографиями, что очень радует. Читайте новости уже сейчас!
перевод с иностранных языков
Генераторы
https://canvas.instructure.com/eportfolios/2945364/Home/________
рефераты на заказ https://kupit-referat213.ru
Fingerspiele Konig Grrr Analsex Beim Reinkommen Immer Schmerzhaft
Генераторы
https://rewarddebtor4.werite.net/zashchita-i-bezopasnost-kozhukhi-dlia-dizel-nykh-generatorov
На сайте https://rozmarysochi.ru/ забронируйте номер в семейном отеле. Для этого необходимо обозначить дату заезда, выезда, а также количество гостей и другую важную информацию. Это место для тех, кто не готов на компромиссы, а ценит удобство, комфорт и качество во всем исполнении. Отпуск подарит огромное количество приятных, положительных эмоций, ярких впечатлений. Здесь можно отдохнуть и с детьми, а также большой компанией. Регулярно проходят акции. Имеется теннисный корт, детский клуб и многое другое.
На сайте https://sobr26.ru ознакомьтесь с номером телефона охранной организации СОБР. Здесь оказываются услуги, связанные с охраной недвижимости, организуется безопасность объекта, есть возможность воспользоваться физической охраной, которая оказывается более 20 лет. Прямо сейчас вы сможете рассчитывать на бесплатную консультацию. Каждый клиент сможет организовать пультовую, физическую охрану, пожарную сигнализацию, видеонаблюдение. Для того чтобы воспользоваться услугами, оставьте заявку непосредственно на сайте.
дагга дикая купить аяуаски купить
https://bicrypto.exchange – crypto exchange software. White label, open-source exchange solution with a focus on a super-fast, pixel-perfect interface and robust security. High-performance platform with a robust internal architecture. Leverages the capabilities of Nuxt3 to create a cutting-edge user interface.
Чанган Центр Архангельск https://arkhangelsk-changanauto.ru/ официальный дилер. Посетите сайт чтобы выбрать свой Changan. Ознакомьтесь с моделями, стоимостью, акциями и спец предложениями на модельный ряд. Выберите комплектацию или воспользуйтесь конфигуратором, а финансовые программы помогут вам приобрести автомобиль с удобными платежами.
Генераторы
https://telegra.ph/Kupit-benzinovyj-generator—kak-vybrat-luchshij-variant-dlya-vashego-doma-ili-dachi-06-03
перевод с иностранных языков
bicrypto – crypto exchange software. White label, open-source exchange solution with a focus on a super-fast, pixel-perfect interface and robust security. High-performance platform with a robust internal architecture. Leverages the capabilities of Nuxt3 to create a cutting-edge user interface.
На сайте https://ack-group.ru/stati-po-psikhologii/psikhoterapiya/ вы сможете получить всю необходимую информацию, которая касается психотерапии. Перед вами огромное количество статей, с которыми необходимо ознакомиться каждому, кто хочет улучшить свое психологическое состояние и получить ценные и редкие советы от профессионалов. Психотерапия предполагает использование самых разных методик, которые помогут себя хорошо чувствовать и ощутить гармонию с окружающей средой. Под психотерапией понимают активное воздействие на психику человека.
кратом чай купить в москве чай кратом купить в москве
Вам интересен вопрос о прокате инвалидных колясок? Деливери плей поможет вам. Гарантируем оперативную доставку и приемлемые цены. У нас всегда чистые коляски. Вы сможете оплатить заказ только после того, как убедитесь, что коляска полностью соответствует вашим требованиям и находится в отличном состоянии. Ищите складные инвалидные коляски напрокат? Deliveryplay.ru/arenda-invalidnyh-kolyasok – сайт, где можно коляску арендовать. Также здесь вы узнаете, почему аренда лучше покупки. Обращайтесь к нам, поможем выбрать коляску, которая идеально вам подойдет.
Генераторы
https://canvas.instructure.com/eportfolios/2945331/Home/__________
купить кратом в москве кратом семена
cash advance SJ 95130 Once the funds are transferred, you would need to provide a payment request, wherein you would authorize the bank to withdraw a specified amount of money from your account as and when it’s due.
You’ll Never Guess This SEO Tools Software’s Tricks seo tools Software
перевод документов
Любите слушать в отменном качестве радио онлайн? Топ Волна предоставляет такую возможность. У нас есть Европа Плюс, Юмор FM, авторадио, DFM и другое. Любую радиостанцию можете слушать дома, в дороге и на работе. Вы будете в курсе новых композиций и последних новостей. top-volna.ru – https://top-volna.ru здесь собрали радиостанции разных музыкальных жанров и направлений. Найдите нужную волну и получайте удовольствие от любимых мелодий. Можете оставить свой отзыв на выбранную радиостанцию, вам нужно перейти в конец страницы и нажать на соответствующую кнопку.
kubutogel
Pasang Perangkat Lunak 888 dan Raih Hadiah: Instruksi Pendek
**Program 888 adalah pilihan terbaik untuk Para Pengguna yang mencari pengalaman bermain internet yang menggembirakan dan bermanfaat. Dengan imbalan harian dan opsi menarik, aplikasi ini menawarkan menghadirkan permainan bertaruhan optimal. Disini manual singkat untuk menggunakan penggunaan App 888.
Pasang dan Awali Menang
Perangkat Tersedia:
Program 888 memungkinkan diambil di Perangkat Android, Perangkat iOS, dan Komputer. Mulai bertaruhan dengan tanpa kesulitan di alat manapun.
Bonus Sehari-hari dan Hadiah
Keuntungan Buka Sehari-hari:
Login pada hari untuk mengklaim imbalan hingga 100K pada hari ketujuh.
Tuntaskan Aktivitas:
Ambil kesempatan pengeretan dengan menyelesaikan aktivitas terkait. Satu aktivitas memberi Para Pengguna satu peluang undi untuk mengklaim hadiah mencapai 888K.
Penerimaan Langsung:
Keuntungan harus diambil langsung di dalam program. Jangan lupa untuk mengklaim keuntungan saban waktu agar tidak tidak berlaku lagi.
Prosedur Undian
Kesempatan Pengeretan:
Satu hari, Anda bisa meraih 1 opsi undian dengan menyelesaikan misi.
Jika opsi pengeretan habis, tuntaskan lebih banyak misi untuk mendapatkan tambahan kesempatan.
Level Keuntungan:
Ambil imbalan jika total pengeretan Pengguna melampaui 100K dalam satu hari.
Kebijakan Utama
Penerimaan Keuntungan:
Hadiah harus diambil sendiri dari perangkat lunak. Jika tidak, hadiah akan otomatis diserahkan ke akun Anda Pengguna setelah sebuah hari.
Persyaratan Betting:
Hadiah harus ada setidaknya 1 bertaruh berlaku untuk diklaim.
Kesimpulan
Perangkat Lunak 888 menyediakan permainan bermain yang menyenangkan dengan bonus signifikan. Download perangkat lunak sekarang juga dan nikmati hadiah besar tiap periode!
Untuk informasi lebih lanjut tentang penawaran, top up, dan skema referensi, lihat halaman beranda program.
Thanks for sharing pg-slot
Генераторы
https://zonelight98.bloggersdelight.dk/2024/06/03/%d0%b3%d0%b5%d0%bd%d0%b5%d1%80%d0%b0%d1%82%d0%be%d1%80-%d0%b4%d0%bb%d1%8f-%d1%87%d0%b0%d1%81%d1%82%d0%bd%d0%be%d0%b3%d0%be-%d0%b4%d0%be%d0%bc%d0%b0-%d0%ba%d0%b0%d0%ba%d0%be%d0%b9-%d0%b2%d1%8b%d0%b1/
Blutung Nach Oralverkehr Natursekt Dominas
Five Things You’re Not Sure About About Automated Backlink
Builder Software Backlinks Builder Software
купить диплом института
подробнее
купить диплом в новом уренгое
посетить сайт
купить диплом дизайнера
ссылка на страницу
Желаете приобрести по недорогой стоимости в Донецке гранитный памятник? Каменный двор – компания, которая предлагает качественные услуги. Сотрудники применяют новейшие технологии и оборудование, что дает возможность быстро и точно исполнить заказ. https://kamdvor.ru – сайт, где можете детальнее узнать о скидках и акциях. Здесь имеется каталог, ознакомиться с ним можно в любое удобное для вас время. Мы относимся к своим клиентам с уважением и гарантируем доступные цены на памятники. Свяжитесь с нами, чтобы получить бесплатную консультацию.
купить диплом ветеринара
смотреть тут
купить диплом фельдшера https://6landik-diploms.com/
купить диплом в липецке
по ссылке
Добро пожаловать на наш портал о недвижимости https://stroyengr.ru/ где вы сможете найти множество полезных статей на такие темы, как покупка квартиры в новостройке, приемка квартиры от застройщика, покупка и продажа недвижимости.
безопасно,
Лучшие стоматологи города, для вашего уверенного улыбки,
Специализированная помощь по доступным ценам, для вашего удобства,
Индивидуальный подход к каждому пациенту, для вашего здоровья и благополучия,
Эффективное лечение зубов и десен, для вашего комфорта и уверенности,
Профессиональная гигиена полости рта, для вашего комфорта и удовлетворения,
Заботливое отношение и внимательный подход, для вашего здоровья и благополучия
стоматологія клініка стоматологія клініка .
купить сайдинг виниловый акриловый сайдинг
Ищите срочный вывоз мусора в Москве? Обратитесь к нам https://vivoz-musora.pro/ и мы приедем в течении 50 минут. Бесплатная консультация по вывозу и утилизации или выберете на сайте необходимую услугу по вывозу отходов, а мы предложим лучшие условия. Мы работаем круглосуточно. Подробнее на сайте.
Analsex Beim One-Night-Stand Bettelt Analverkehr
На сайте https://g-raze.ru у вас есть возможность приобрести болотоход по доступной стоимости от производителя. Здесь вы найдете большой ассортимент болотоходов в различных городах. Болотоходы отличаются надежностью и высокой проходимостью в самых тяжелых условиях. Также мы обеспечиваем своих клиентов универсальными транспортными средствами передвижения по сложной местности. Модельный ряд представлен на сайте, где можно помимо прочего увидеть видеообзор, также информацию о доставки и оплате.
На сайте https://hotel-elizabeth.ru/ каждый желающий получает возможность забронировать отель «Элизабет». Укажите дату заезда, выезда, количество гостей и многое другое. А если у вас есть промокод, то введите комбинацию чисел, чтобы сэкономить. Вас ожидает удивительный чистый воздух, роскошные горы, а также привлекательные виды, которыми можно наслаждаться повсеместно. Установлены доступные расценки, а огромное количество развлекательных программ уже входит в стоимость.
купить диплом переводчика https://6landik-diploms.com
Аврора Агро Партс – интернет-магазин, заслуживающий вашего внимания. На автозапчасти ведущих брендов мы предоставляем выгодные цены. Всегда рады общению с нашими клиентами, мы их уважаем. Вы можете смело рассчитывать на помощь компетентного специалиста. Он грамотно подберет то, что вам действительно нужно. https://aa-p.ru – сайт, где можно в любое удобное для вас время ознакомиться с условиями оплаты и доставки. Заказы выполняем максимально быстро. Обращайтесь к нам, мы постоянно развиваемся и открыты для плодотворного сотрудничества!
апостиль в новосибирске
безопасно,
Современное оборудование и материалы, для крепких и здоровых зубов,
Современные методы стоматологии, для вашего удобства,
Комфортные условия и дружественный персонал, для вашей радости и улыбки,
Комплексное восстановление утраченных зубов, для вашего комфорта и уверенности,
Профессиональная гигиена полости рта, для вашего комфорта и удовлетворения,
Заботливое отношение и внимательный подход, для вашего здоровья и благополучия
лікування зубів https://stomatologichnaklinikafghy.ivano-frankivsk.ua/ .
гарантированно,
Индивидуальный подход к каждому пациенту, для поддержания здоровья рта,
Современные методы стоматологии, для вашего удобства,
Комфортные условия и дружественный персонал, для вашей радости и улыбки,
Комплексное восстановление утраченных зубов, для вашего долгосрочного удовлетворения,
Экстренная помощь в любое время суток, для вашего долгосрочного удовлетворения,
Современное лечение заболеваний полости рта, для вашего комфорта и удовлетворения
здорові зуби здорові зуби .
купить диплом в кирове https://6landik-diploms.com/
twin casino сайт сайт Twin Casino
эффективно,
Индивидуальный подход к каждому пациенту, для поддержания здоровья рта,
Современные методы стоматологии, для вашего уверенного выбора,
Комфортные условия и дружественный персонал, для вашего комфорта и уверенности,
Инновационные методы стоматологии, для вашего комфорта и уверенности,
Экстренная помощь в любое время суток, для вашего комфорта и удовлетворения,
Современное лечение заболеваний полости рта, для вашего комфорта и удовлетворения
зуби лікування зуби лікування .
эффективно,
Лучшие стоматологи города, для вашего уверенного улыбки,
Специализированная помощь по доступным ценам, для вашего удобства,
Индивидуальный подход к каждому пациенту, для вашей радости и улыбки,
Комплексное восстановление утраченных зубов, для вашего здоровья и красоты улыбки,
Профессиональная гигиена полости рта, для вашего здоровья и уверенности в себе,
Современное лечение заболеваний полости рта, для вашего здоровья и благополучия
здорові зуби здорові зуби .
I’m gone to say to my little brother, that he should also pay a visit this website on regular basis to take updated from hottest gossip.
ww82.smallbigworld.net/sk/project/10/
http://www.login.ps/blogs/69645/%D0%9F%D0%BE%D1%81%D1%82%D0%B4%D0%B8%D0%BF%D0%BB%D0%BE%D0%BC%D0%BD%D0%BE%D0%B5-%D0%A0%D0%B0%D0%B7%D0%B2%D0%B8%D1%82%D0%B8%D0%B5-%D0%9A%D0%BB%D1%8E%D1%87%D0%B5%D0%B2%D1?lang=tr_tr
floriann.ru/buket-roz
panarabiaenquirer.com/wordpress/israeli-defence-forces-to-commemorate-international-holocaust-memorial-day-by-locking-up-record-number-of-palestinian-children/
forum.moderncompany.de/profile.php?lookup=15044
Генераторы
https://answerlook94.werite.net/kupit-benzinovyi-generator-kak-vybrat-luchshii-variant-dlia-vashego-doma-ili
казино вход регистрация Twin Casino
акриловый сайдинг сайдинг купить недорого для обшивки
казино онлайн Twin Casino официальный
На сайте https://cliningkrd.ru закажите звонок для того, чтобы воспользоваться услугами клинингового агентства. В компании работают компетентные и квалифицированные сотрудники, которые прошли необходимую подготовку. Используется инновационное и качественное оборудование, а также уникальные технологии, которые позволяют добиться блестящего результата. Бытовая химия полностью безопасна как для животных, так и людей, не провоцирует аллергии. Все услуги доступны по привлекательной стоимости. Они оказываются в минимальные сроки.
Зайдите на сайт ФильтрМаркет https://filtrmarket.ru/ где большой каталог фильтров, которые сможете купить с доставкой – воздушные фильтры, магистральные, панельные, масляные фильтры. Все в наличие по отличным ценам в едином каталоге. Подробнее на сайте.
прошутто нарезка цена хамона за кг
Все самое интересное из мира игр https://unionbattle.ru обзоры, статьи и ответы на вопросы
Siemens коммутаторы Надежные коммутаторы от Siemens для сетевых решений.
сыровяленая брезаола парма купить в москве
Pretty part of content. I just stumbled upon your site and in accession capital to claim that I acquire in fact enjoyed account your blog posts. Any way I’ll be subscribing in your feeds or even I fulfillment you get right of entry to consistently fast.
http://www.vocal.com.ua/blog/www.xuzhouabl.com/en?page=114
kruizturm.ru/morskie-kruizyi/
drunkslut.com/springbreak.html
eqagent.ru/users/36?wid=426
batdongsanmiennam.vn/mnre-tich-cuc-day-manh-kenh-ban-hang-truc-tuyen/
sanghoki
Ashley JKT48: Bintang yang Bersinar Gemilang di Dunia Idol
Siapa Ashley JKT48?
Siapakah figur muda berbakat yang menarik perhatian banyak penggemar musik di Indonesia dan Asia Tenggara? Beliau adalah Ashley Courtney Shintia, atau yang dikenal dengan nama bekennya, Ashley JKT48. Bergabung dengan grup idola JKT48 pada tahun 2018, Ashley dengan lekas menjadi salah satu anggota paling favorit.
Riwayat Hidup
Lahir di Jakarta pada tgl 13 Maret 2000, Ashley berketurunan darah Tionghoa-Indonesia. Ia memulai karier di industri entertainment sebagai model dan aktris, hingga akhirnya selanjutnya masuk dengan JKT48. Kepribadiannya yang ceria, vokal yang kuat, dan kemahiran menari yang memukau menjadikannya idol yang sangat dicintai.
Penghargaan dan Apresiasi
Kepopuleran Ashley telah diapresiasi melalui berbagai penghargaan dan pencalonan. Pada tahun 2021, ia meraih award “Member Terpopuler JKT48” di ajang Penghargaan Musik JKT48. Ia juga dinobatkan sebagai “Idol Tercantik di Asia” oleh sebuah tabloid online pada tahun 2020.
Peran dalam JKT48
Ashley mengisi fungsi utama dalam group JKT48. Ia adalah member Tim KIII dan berperan sebagai penari utama dan penyanyi utama. Ashley juga terlibat sebagai bagian dari sub-unit “J3K” bersama Jessica Veranda dan Jennifer Rachel Natasya.
Karier Mandiri
Selain kegiatan bersama JKT48, Ashley juga merintis perjalanan solo. Beliau telah merilis beberapa lagu single, diantaranya “Myself” (2021) dan “Falling Down” (2022). Ashley juga telah bekerjasama bersama penyanyi lain, seperti Afgan dan Rossa.
Aktivitas Pribadi
Di luar dunia panggung, Ashley dikenal sebagai pribadi yang humble dan bersahabat. Ia menikmati menghabiskan waktu bersama keluarga dan sahabat-sahabatnya. Ashley juga menyukai kesukaan melukis dan fotografi.
купить квартиру от застройщика недорого купить 2 квартиру
MIGRANT SUPPORT предоставляет помощь для получения номера PESEL и дает гарантию на привлекательные цены. Профессиональные специалисты компании, прилагают максимум усилий для выполнения различных задач. https://migrant.support/poluchieniie_nomiera_pesel – сайт, где у вас есть возможность узнать, как сделать песель удаленно, и зачем он нужен. Мы быстро и качественно оказываем помощь, а также предлагаем абсолютно бесплатно консультацию. Относимся лояльно к нашим клиентам, делаем все возможное, чтобы оправдать их ожидания. Вы точно не пожалеете о своем выборе, обращайтесь!
sultantoto
Inspirasi dari Kutipan Taylor Swift: Harapan dan Cinta dalam Lagu-Lagunya
Penyanyi Terkenal, seorang penyanyi dan pengarang lagu terkenal, tidak hanya diakui oleh karena melodi yang indah dan vokal yang nyaring, tetapi juga sebab lirik-lirik karyanya yang penuh makna. Di dalam kata-katanya, Swift sering menggambarkan berbagai aspek kehidupan, mulai dari cinta hingga tantangan hidup. Berikut ini adalah sejumlah ucapan motivatif dari lagu-lagunya, beserta artinya.
“Mungkin yang terbaik belum datang.” – “All Too Well”
Arti: Bahkan di masa-masa sulit, tetap ada sedikit asa dan kemungkinan akan hari yang lebih baik.
Kutipan ini dari lagu “All Too Well” membuat kita ingat bahwa meskipun kita mungkin berhadapan dengan waktu sulit saat ini, selalu ada potensi bahwa waktu yang akan datang akan memberikan sesuatu yang lebih baik. Situasi ini adalah amanat harapan yang menguatkan, memotivasi kita untuk tetap bertahan dan tidak menyerah, karena yang paling baik mungkin belum tiba.
“Aku akan tetap bertahan karena aku tak bisa melakukan apa pun tanpamu.” – “You Belong with Me”
Makna: Memperoleh kasih dan support dari orang lain dapat memberi kita daya dan tekad untuk bertahan melalui rintangan.
Internet casinos are becoming more popular, offering different rewards to bring in new players. One of the most attractive propositions is the no deposit bonus, a promo that allows users to try their hand without any financial obligation. This write-up explores the advantages of no-deposit bonuses and underscores how they can boost their effectiveness.
What is a No Deposit Bonus?
A no upfront deposit bonus is a type of casino campaign where players are given bonus credits or free rounds without the need to put in any of their own money. This permits gamblers to explore the casino, test out different games and stand a chance to win real funds, all without any initial expenditure.
Advantages of No Deposit Bonuses
Risk-Free Exploration
No deposit bonuses provide a cost-free option to investigate virtual casinos. Users can try multiple games, understand the casino’s interface, and evaluate the overall gaming experience without spending their own capital. This is particularly advantageous for newcomers who may not be familiar with online casinos.
Chance to Win Real Money
One of the most enticing aspects of no-deposit bonuses is the possibility to obtain real winnings. Although the amounts may be small, any gains earned from the bonus can usually be collected after meeting the casino’s playthrough rules. This introduces an element of fun and gives a potential financial benefit without any upfront investment.
Learning Opportunity
No upfront deposit bonuses give a excellent chance to get to know how different games are played. Users can experiment with methods, grasp the guidelines of the slots, and grow more skilled without being concerned about parting with their own capital. This can be notably helpful for challenging casino games like blackjack.
Conclusion
Free bonuses offer numerous advantages for players, like secure trial, the possibility to earn real cash, and important training chances. As the sector goes on to develop, the popularity of no deposit bonuses is set to expand.
Complimentary poker provides gamblers a special chance to experience the activity without any financial risk. This overview discusses the upsides of engaging in free poker and emphasizes why it is popular among a lot of players.
Risk-Free Entertainment
One of the greatest upsides of free poker is that it enables players to experience the fun of poker without worrying about losing capital. This turns it perfect for first-timers who desire to learn the activity without any financial commitment.
Skill Development
No-cost poker provides a excellent platform for users to develop their abilities. Participants can experiment with approaches, grasp the regulations of the pastime, and obtain confidence without any pressure of losing their own capital.
Social Interaction
Participating in free poker can also foster social connections. Online platforms regularly include chat rooms where users can communicate with each other, talk about tips, and occasionally form friendships.
Accessibility
Complimentary poker is conveniently accessible to everyone with an internet link. This implies that gamblers can play the activity from the convenience of their own homes, at any time.
Conclusion
Free poker offers numerous advantages for users. It is a risk-free approach to experience the sport, hone competence, engage in new friendships, and access poker readily. As more users learn about the merits of free poker, its demand is set to expand.
Unveiling the Realm of Virtual Casinos
Introduction
Today, virtual casinos have changed the method users experience casino games. With modern tech, enthusiasts can access their beloved casino games right from the convenience of their houses. This piece explores the pros of casino online and why they are drawing popularity.
Advantages of Casino Online
Ease
One of the major benefits of internet casinos is accessibility. Players can gamble at any time and anywhere they desire, eliminating the requirement to commute to a land-based betting place.
Extensive Game Options
Online casinos give a wide range of casino games, spanning from traditional slot machines and board games to real-time games and new video slots. This variety assures that there is an option for all types of players.
Offers and Deals
Among the key luring elements of virtual casinos is the variety of bonuses and deals provided to enthusiasts. These can comprise initial bonuses, bonus spins, cashback offers, and rewards programs.
Security and Reliability
Trusted virtual casinos ensure gambler assurance and reliability with sophisticated cybersecurity systems. This shields private data and payment operations.
Why Virtual Casinos are Favored
Accessibility
Casino online are extensively accessible, facilitating gamblers from diverse regions to engage in gaming.
정정욱 마약
빠른 충환전 서비스와 대형업체의 보안성
베팅사이트 접속 시 핵심적인 부분 중 하나는 신속한 충환전 처리입니다. 보통 삼 분 내에 입금, 열 분 안에 환충이 완료되어야 합니다. 메이저 대형업체들은 필요한 스태프 채용으로 이 같은 빠른 충환전 프로세스를 보장하며, 이로써 회원들에게 안도감을 제공합니다. 대형사이트를 이용하면서 신속한 경험을 즐겨보세요. 우리 고객님이 보안성 있게 사이트를 접속할 수 있도록 돕는 먹튀 해결 팀입니다.
보증금 걸고 배너를 운영
먹튀해결사는 최소 삼천만 원에서 일억 원의 보증 금액을 예치하고 있는 회사들의 광고 배너를 운영 중입니다. 혹시 먹튀 사고가 발생할 시, 배팅 규정에 어긋나지 않은 베팅 내역을 캡처해서 먹튀 해결 팀에 문의 주시면, 사실 확인 뒤 보증 자금으로 신속하게 피해 보전 처리합니다. 피해가 발생하면 빠르게 캡처해서 손해 내용을 저장해두시고 보내주세요.
장기간 안전 운영 업체 확인
먹튀 해결 팀은 최소 4년 이상 먹튀 문제 없이 안전하게 운영하고 있는 사이트만을 확인하여 광고 배너 입점을 받고 있습니다. 이로 인해 누구나 알고 있는 대형사이트를 안전하게 접속할 수 있는 기회를 제공합니다. 정확한 검증 절차를 통해 인증된 사이트를 놓치지 마시고, 안심하고 배팅을 경험해보세요.
투명성과 공정성을 가진 먹튀 검증
먹튀해결사의 먹튀 검토는 공정성과 정확함을 기반으로 실시합니다. 항상 이용자들의 의견을 최우선으로 생각하며, 사이트의 회유나 이익에 흔들리지 않고 하나의 삭제 없이 진실만을 바탕으로 검토해왔습니다. 먹튀 피해를 겪고 후회하지 않도록, 지금 바로 시작하세요.
먹튀검증사이트 목록
먹튀 해결 팀이 선별한 안전한 베팅사이트 검증된 업체 목록 입니다. 지금 등록된 인증된 업체들은 먹튀 피해 발생 시 100% 보증을 해드립니다. 하지만, 제휴 기간이 만료된 업체에서 발생한 피해에 대해서는 책임지지 않습니다.
유일무이한 먹튀 검증 알고리즘
먹튀해결사는 공정한 도박 문화를 만들기 위해 계속해서 노력합니다. 저희가 권장하는 토토사이트에서 안전하게 베팅하세요. 회원님의 먹튀 신고 내용은 먹튀 리스트에 등록 노출되어 해당되는 토토사이트에 심각한 영향을 미칩니다. 먹튀 목록 작성 시 먹튀블러드 만의 검토 경험을 충분히 활용하여 정확한 검증을 할 수 있도록 약속드립니다.
안전한 베팅 환경을 만들기 위해 계속해서 힘쓰는 먹튀 해결 전문가와 같이 안전하게 경험해보세요.
Exploring Promotion Gaming Hubs: A Thrilling and Reachable Playing Alternative
Prelude
Sweepstakes betting sites are growing into a favored choice for participants looking for an captivating and lawful method to experience virtual playing. Unlike conventional virtual betting sites, lottery gaming hubs run under different authorized frameworks, allowing them to present games and awards without adhering to the similar guidelines. This write-up analyzes the idea of promotion casinos, their perks, and why they are attracting a expanding figure of players.
Understanding Sweepstakes Casinos
A promotion gaming hub functions by giving users with digital funds, which can be applied to experience activities. Gamers can win extra virtual money or actual gifts, including cash. The fundamental variation from standard gaming hubs is that participants do not purchase funds instantly but receive it through marketing efforts, including buying a goods or taking part in a complimentary entry contest. This framework permits promotion gaming hubs to operate authorized in many areas where traditional digital gambling is regulated.
real money slots
Unveiling Gambling Slots
Overview
Real money slots have turned into a favored selection for gamblers desiring the adrenaline of winning real funds. This text examines the benefits of money slots and why they are amassing more enthusiasts.
Perks of Gambling Slots
Genuine Rewards
The key draw of real money slots is the potential to win tangible money. In contrast to complimentary slots, real money slots supply players the rush of possible financial rewards.
Wide Range of Games
Cash slots offer a wide array of styles, characteristics, and payment models. This guarantees that there is an activity for every player, ranging from classic 3-reel slots to state-of-the-art slot games with several betting lines and special bonuses.
Attractive Offers
Various digital casinos give attractive bonuses for money slot enthusiasts. These can feature welcome bonuses, bonus spins, rebate offers, and member incentives. Such promotions enhance the entire casino adventure and give extra possibilities to win funds.
Why Enthusiasts Enjoy Gambling Slots
The Adrenaline of Gaining Genuine Funds
Money slots give an exhilarating adventure, as players expect the opportunity of gaining tangible funds. This characteristic contributes a further layer of excitement to the gameplay experience.
Quick Earnings
Cash slots offer gamblers the reward of quick rewards. Winning currency immediately enhances the playing journey, rendering it more satisfying.
Numerous Game Choices
Alongside money slots, gamblers can play a broad selection of slot games, guaranteeing that there is always an activity exciting to test.
Final Thoughts
Real money slots provides a exciting and satisfying playing experience. With the potential to secure genuine cash, a extensive array of games, and attractive bonuses, it’s obvious that numerous gamblers prefer money slots for their gaming requirements.
5 Killer Quora Answers To SEO Ranking Software seo Ranking software
Зайдите на сайт https://vag-axsel.ru/ и вы сможете купить новый Фольцваген или посмотреть каталог автомобилей с пробегом. Сервисное обслуживание от официального дилера Volkswagen по выгодным ценам. А программы кредитования и трейд ин помогут вам выгодно приобрести автомобиль по выгодной цене. Подробнее на сайте.
https://www.offtopicproductions.com/forum/viewtopic.php?f=6&t=62825
Looking to buy Ceylon cinnamon powder? You’ve come to the right place! We offer pure Ceylon cinnamon powder, known for its sweet, delicate flavor and numerous health benefits. If you’re wondering where to buy Ceylon cinnamon powder, look no further. Our Ceylon cinnamon for sale is available for purchase online, making it convenient for you to get this high-quality spice delivered straight to your door.
In addition to our pure Ceylon cinnamon powder, we also offer a variety of other products. If you’re a fan of herbal teas, consider trying Samahan tea. You can easily buy Samahan tea online through our store. It’s a wonderful blend of herbs and spices that supports your overall well-being.
For those who enjoy baking or cooking with coconut, we have desiccated coconut available. Wondering where to buy desiccated coconut? You can find it here, along with our extensive range of cinnamon products.
Speaking of cinnamon, our product line includes more than just powder. We also have Ceylon cinnamon sticks, perfect for adding a touch of flavor to your dishes or beverages. If you’re looking to purchase real cinnamon sticks online, we’ve got you covered.
Our selection doesn’t stop there. We offer cinnamon lotion and cinnamon body lotion for those who love the scent and benefits of cinnamon in their skincare routine. Additionally, you can find cinnamon shampoo and even cinnamon toothpicks at an affordable price.
For those interested in supplements, we have a range of Ceylon cinnamon supplements for sale. These supplements are a convenient way to incorporate the benefits of Ceylon cinnamon into your daily routine. You can buy Ceylon cinnamon supplements from us, ensuring you’re getting the best quality available.
Lastly, don’t forget to check out our Ceylon cinnamon tea bags, perfect for a soothing cup of tea at any time of the day. With our wide selection, you’re sure to find exactly what you need. Shop with us today for all your cinnamon and specialty product needs!
https://penzu.com/p/1f8163d78c446e4e
If you’re a fan of unique and flavorful dishes, you must try the Cinnamon Pork Cutlets Recipe. This delightful recipe brings out the best in pork with the warm, aromatic touch of cinnamon. For the best results, make sure to use Ceylon cinnamon sticks instead of the more common Cassia cinnamon. Wondering about the difference? When it comes to Ceylon Cinnamon Sticks vs. Cassia Cinnamon, Ceylon cinnamon is known for its sweeter, more delicate flavor, while Cassia has a stronger, more pungent taste. This distinction makes Ceylon the preferred choice for dishes where a subtle spice is desired.
Using Ceylon cinnamon powder in your cooking can elevate your meals to new heights. But do you know how to use Ceylon cinnamon powder in your favorite recipes? This versatile spice can be added to both sweet and savory dishes. Sprinkle it on your morning oatmeal, mix it into smoothies, or incorporate it into baked goods for a delicious twist. It’s also fantastic in savory recipes like curries, stews, and the aforementioned pork cutlets.
Apart from its culinary uses, Ceylon cinnamon offers numerous health benefits. Ceylon cinnamon capsules are a convenient way to enjoy these benefits. These supplements are packed with antioxidants and have anti-inflammatory properties. If you’re interested in the advantages, the Ceylon cinnamon capsules can help with blood sugar regulation, improving digestion, and boosting overall health. For those wondering about the benefits, dosage, and where to buy the best supplements, it’s recommended to take a look at reputable online stores that specialize in natural health products. The suggested dosage varies, so always follow the manufacturer’s instructions or consult with a healthcare professional.
Whether you’re cooking up a delicious meal or looking to enhance your health, Ceylon cinnamon is a versatile and beneficial spice to have on hand. Enjoy exploring its uses and benefits in your kitchen and beyond!
эффективно,
Лучшие стоматологи города, для вашего уверенного улыбки,
Современные методы стоматологии, для вашего удобства,
Комфортные условия и дружественный персонал, для вашего здоровья и благополучия,
Комплексное восстановление утраченных зубов, для вашего комфорта и уверенности,
Индивидуальный план лечения и профилактики, для вашего долгосрочного удовлетворения,
Индивидуальный план лечения для каждого пациента, для вашей уверенной улыбки
стоматологія дитяча https://stomatologichnaklinikafghy.ivano-frankivsk.ua/ .
гарантированно,
Современное оборудование и материалы, для вашего уверенного улыбки,
Современные методы стоматологии, для вашего удобства,
Комфортные условия и дружественный персонал, для вашей радости и улыбки,
Инновационные методы стоматологии, для вашего комфорта и уверенности,
Профессиональная гигиена полости рта, для вашего долгосрочного удовлетворения,
Индивидуальный план лечения для каждого пациента, для вашего комфорта и удовлетворения
лікування карієсу https://stomatologichnaklinikafghy.ivano-frankivsk.ua/ .
20 Things You Need To Know About Seo Search Engine Optimisation london search Engine Optimization
Ищите промоакции в Казахстане? Зайдите на сайт https://probonus.kz/ и вы можете узнать о промо акциях в Казахстане, какие проходят акции в магазинах вашего города и быть в курсе где проходят новые акции и скидки. Акции постоянно добавляются и обновляются, что даст возможность существенно сэкономить на покупках.
эффективно,
Современное оборудование и материалы, для поддержания здоровья рта,
Современные методы стоматологии, для вашей улыбки,
Бесплатная консультация и диагностика, для вашей радости и улыбки,
Эффективное лечение зубов и десен, для вашего долгосрочного удовлетворения,
Профессиональная гигиена полости рта, для вашего комфорта и удовлетворения,
Современное лечение заболеваний полости рта, для вашего комфорта и удовлетворения
дитяча стоматологічна дитяча стоматологічна .
гарантированно,
Лучшие стоматологи города, для вашего уверенного улыбки,
Профессиональное лечение и консультации, для вашего удобства,
Комфортные условия и дружественный персонал, для вашего здоровья и благополучия,
Комплексное восстановление утраченных зубов, для вашего комфорта и уверенности,
Экстренная помощь в любое время суток, для вашего комфорта и удовлетворения,
Заботливое отношение и внимательный подход, для вашего комфорта и удовлетворения
стоматологiчна полiклiнiка https://stomatologichnaklinikafghy.ivano-frankivsk.ua/ .
https://lessons.drawspace.com/post/537271/sports-drinks-brands-are-popular-with-athletes-a
Looking to buy Ceylon cinnamon powder? You’ve come to the right place! We offer pure Ceylon cinnamon powder, known for its sweet, delicate flavor and numerous health benefits. If you’re wondering where to buy Ceylon cinnamon powder, look no further. Our Ceylon cinnamon for sale is available for purchase online, making it convenient for you to get this high-quality spice delivered straight to your door.
In addition to our pure Ceylon cinnamon powder, we also offer a variety of other products. If you’re a fan of herbal teas, consider trying Samahan tea. You can easily buy Samahan tea online through our store. It’s a wonderful blend of herbs and spices that supports your overall well-being.
For those who enjoy baking or cooking with coconut, we have desiccated coconut available. Wondering where to buy desiccated coconut? You can find it here, along with our extensive range of cinnamon products.
Speaking of cinnamon, our product line includes more than just powder. We also have Ceylon cinnamon sticks, perfect for adding a touch of flavor to your dishes or beverages. If you’re looking to purchase real cinnamon sticks online, we’ve got you covered.
Our selection doesn’t stop there. We offer cinnamon lotion and cinnamon body lotion for those who love the scent and benefits of cinnamon in their skincare routine. Additionally, you can find cinnamon shampoo and even cinnamon toothpicks at an affordable price.
For those interested in supplements, we have a range of Ceylon cinnamon supplements for sale. These supplements are a convenient way to incorporate the benefits of Ceylon cinnamon into your daily routine. You can buy Ceylon cinnamon supplements from us, ensuring you’re getting the best quality available.
Lastly, don’t forget to check out our Ceylon cinnamon tea bags, perfect for a soothing cup of tea at any time of the day. With our wide selection, you’re sure to find exactly what you need. Shop with us today for all your cinnamon and specialty product needs!
https://telegra.ph/Ceylon-Cinnamon-Capsules-Benefits-Dosage-and-Where-to-Buy-the-Best-Supplements-06-03
If you’re a fan of unique and flavorful dishes, you must try the Cinnamon Pork Cutlets Recipe. This delightful recipe brings out the best in pork with the warm, aromatic touch of cinnamon. For the best results, make sure to use Ceylon cinnamon sticks instead of the more common Cassia cinnamon. Wondering about the difference? When it comes to Ceylon Cinnamon Sticks vs. Cassia Cinnamon, Ceylon cinnamon is known for its sweeter, more delicate flavor, while Cassia has a stronger, more pungent taste. This distinction makes Ceylon the preferred choice for dishes where a subtle spice is desired.
Using Ceylon cinnamon powder in your cooking can elevate your meals to new heights. But do you know how to use Ceylon cinnamon powder in your favorite recipes? This versatile spice can be added to both sweet and savory dishes. Sprinkle it on your morning oatmeal, mix it into smoothies, or incorporate it into baked goods for a delicious twist. It’s also fantastic in savory recipes like curries, stews, and the aforementioned pork cutlets.
Apart from its culinary uses, Ceylon cinnamon offers numerous health benefits. Ceylon cinnamon capsules are a convenient way to enjoy these benefits. These supplements are packed with antioxidants and have anti-inflammatory properties. If you’re interested in the advantages, the Ceylon cinnamon capsules can help with blood sugar regulation, improving digestion, and boosting overall health. For those wondering about the benefits, dosage, and where to buy the best supplements, it’s recommended to take a look at reputable online stores that specialize in natural health products. The suggested dosage varies, so always follow the manufacturer’s instructions or consult with a healthcare professional.
Whether you’re cooking up a delicious meal or looking to enhance your health, Ceylon cinnamon is a versatile and beneficial spice to have on hand. Enjoy exploring its uses and benefits in your kitchen and beyond!
На сайте https://napolnye-konditsionery.ru/ есть возможность приобрести напольные кондиционеры. Они подходят не только для обустройства дома, но их устанавливают и в офис. Такие устройства отличаются огромным количеством преимуществ, что и делает их незаменимыми в быту. Напольные устройства наделены большим количеством важных функций, которые делают их максимально удобными в использовании и практичными. Есть устройства премиального уровня, а также бюджетные. Выбирайте кондиционеры, оснащенные такими полезными опциями, как: осушение воздуха, фильтрация и различные виды охлаждения.
https://medium.com/@seonza100/cinnamon-pork-cutlets-recipe-quick-and-flavorful-6d1bd67df25a
If you’re a fan of unique and flavorful dishes, you must try the Cinnamon Pork Cutlets Recipe. This delightful recipe brings out the best in pork with the warm, aromatic touch of cinnamon. For the best results, make sure to use Ceylon cinnamon sticks instead of the more common Cassia cinnamon. Wondering about the difference? When it comes to Ceylon Cinnamon Sticks vs. Cassia Cinnamon, Ceylon cinnamon is known for its sweeter, more delicate flavor, while Cassia has a stronger, more pungent taste. This distinction makes Ceylon the preferred choice for dishes where a subtle spice is desired.
Using Ceylon cinnamon powder in your cooking can elevate your meals to new heights. But do you know how to use Ceylon cinnamon powder in your favorite recipes? This versatile spice can be added to both sweet and savory dishes. Sprinkle it on your morning oatmeal, mix it into smoothies, or incorporate it into baked goods for a delicious twist. It’s also fantastic in savory recipes like curries, stews, and the aforementioned pork cutlets.
Apart from its culinary uses, Ceylon cinnamon offers numerous health benefits. Ceylon cinnamon capsules are a convenient way to enjoy these benefits. These supplements are packed with antioxidants and have anti-inflammatory properties. If you’re interested in the advantages, the Ceylon cinnamon capsules can help with blood sugar regulation, improving digestion, and boosting overall health. For those wondering about the benefits, dosage, and where to buy the best supplements, it’s recommended to take a look at reputable online stores that specialize in natural health products. The suggested dosage varies, so always follow the manufacturer’s instructions or consult with a healthcare professional.
Whether you’re cooking up a delicious meal or looking to enhance your health, Ceylon cinnamon is a versatile and beneficial spice to have on hand. Enjoy exploring its uses and benefits in your kitchen and beyond!
Rassilka.kz оказывает качественные услуги. Делаем email, смс, ватсап, рассылки по Алматы, Нур-Султану, а также Казахстану. Сотрудничаем с разными популярными компаниями. Наша главная задача – принести всем клиентам пользу. Действия нацелены на конечный результат. https://rassilka.kz – сайт, где вы узнаете, почему нас выбирают. Здесь у вас есть возможность уже сейчас посмотреть тарифы. У нас вы получите консультацию на бесплатной основе. Мы с удовольствием ответим на все ваши вопросы, свяжитесь с нами в любое время.
На сайте http://smartporog.ru посмотрите каталог, где находятся выпадающие умные пороги, которые вы сможете приобрести прямо сейчас. Это решение станет оптимальным вариантом, если установка стационарного порога невозможна либо нецелесообразна в определенном случае. Посмотрите видео с тем, как такие пороги идеально вписываются в помещение. Они смогут устранить преграду, образовавшуюся в полу, избавляют от мостиков холода, повышают звукоизоляцию, борются с посторонними запахами.
https://www.nairaland.com/4446926/wholesale-ceylon-cinnamon-powder-stick
Looking to buy Ceylon cinnamon powder? You’ve come to the right place! We offer pure Ceylon cinnamon powder, known for its sweet, delicate flavor and numerous health benefits. If you’re wondering where to buy Ceylon cinnamon powder, look no further. Our Ceylon cinnamon for sale is available for purchase online, making it convenient for you to get this high-quality spice delivered straight to your door.
In addition to our pure Ceylon cinnamon powder, we also offer a variety of other products. If you’re a fan of herbal teas, consider trying Samahan tea. You can easily buy Samahan tea online through our store. It’s a wonderful blend of herbs and spices that supports your overall well-being.
For those who enjoy baking or cooking with coconut, we have desiccated coconut available. Wondering where to buy desiccated coconut? You can find it here, along with our extensive range of cinnamon products.
Speaking of cinnamon, our product line includes more than just powder. We also have Ceylon cinnamon sticks, perfect for adding a touch of flavor to your dishes or beverages. If you’re looking to purchase real cinnamon sticks online, we’ve got you covered.
Our selection doesn’t stop there. We offer cinnamon lotion and cinnamon body lotion for those who love the scent and benefits of cinnamon in their skincare routine. Additionally, you can find cinnamon shampoo and even cinnamon toothpicks at an affordable price.
For those interested in supplements, we have a range of Ceylon cinnamon supplements for sale. These supplements are a convenient way to incorporate the benefits of Ceylon cinnamon into your daily routine. You can buy Ceylon cinnamon supplements from us, ensuring you’re getting the best quality available.
Lastly, don’t forget to check out our Ceylon cinnamon tea bags, perfect for a soothing cup of tea at any time of the day. With our wide selection, you’re sure to find exactly what you need. Shop with us today for all your cinnamon and specialty product needs!
На сайте https://ocims.ru/ закажите звонок для того, чтобы воспользоваться такой услугой, как строительство каркасных домов высокого качества. Они надежные, практичные, а самое главное, что простоят очень долго. Все работы происходят под ключ. Дома строятся по индивидуальному, а также типовому проекту, что позволит подобрать то, что соответствует предпочтениям, вкусам. На работы, материалы даются гарантии. Действуют привлекательные и доступные расценки. Также компания предлагает приятный презент по окончании проведения работ.
На сайте https://django-hotel.ru/ забронируйте номер в отеле «Джанго», где уютные, комфортные номера. А забронировать их вы сможете уже сейчас. Для этих целей следует обозначить дату заезда, выезда, остальную информацию. Гостей ожидают современные, комфортные номера, а также телевидение, Интернет. Имеется бассейн, а также ресторан, в котором представлены интересные блюда, выполненные из свежих, отборных продуктов. Также недалеко находятся аптеки, кафе, различные достопримечательности.
CVzen es el mejor servicio https://cvzen.es/ de redacción de CV y orientación profesional para millones de personas que buscan empleo en todo el mundo. Nuestro equipo de expertos está comprometido con tu éxito y te apoyará a lo largo de tu trayectoria profesional, desde la redacción de tu CV profesional y tu carta de presentación con datos específicos del sector hasta la optimización de tu perfil de LinkedIn y la orientación profesional. Desbloquea nuevas oportunidades con un currículum que muestre tu potencial.
Добро пожаловать на наш портал о недвижимости https://stroyengr.ru/ где вы сможете найти множество полезных статей на такие темы, как покупка квартиры в новостройке, приемка квартиры от застройщика, покупка и продажа недвижимости.
купить диплом фельдшера https://6landik-diploms.com
instant cash advance 28th street southwest wyoming mi The other good point of these funds is its unsecured nature.
https://www.codesdope.com/discussion/amazing-cool/
Looking to buy Ceylon cinnamon powder? You’ve come to the right place! We offer pure Ceylon cinnamon powder, known for its sweet, delicate flavor and numerous health benefits. If you’re wondering where to buy Ceylon cinnamon powder, look no further. Our Ceylon cinnamon for sale is available for purchase online, making it convenient for you to get this high-quality spice delivered straight to your door.
In addition to our pure Ceylon cinnamon powder, we also offer a variety of other products. If you’re a fan of herbal teas, consider trying Samahan tea. You can easily buy Samahan tea online through our store. It’s a wonderful blend of herbs and spices that supports your overall well-being.
For those who enjoy baking or cooking with coconut, we have desiccated coconut available. Wondering where to buy desiccated coconut? You can find it here, along with our extensive range of cinnamon products.
Speaking of cinnamon, our product line includes more than just powder. We also have Ceylon cinnamon sticks, perfect for adding a touch of flavor to your dishes or beverages. If you’re looking to purchase real cinnamon sticks online, we’ve got you covered.
Our selection doesn’t stop there. We offer cinnamon lotion and cinnamon body lotion for those who love the scent and benefits of cinnamon in their skincare routine. Additionally, you can find cinnamon shampoo and even cinnamon toothpicks at an affordable price.
For those interested in supplements, we have a range of Ceylon cinnamon supplements for sale. These supplements are a convenient way to incorporate the benefits of Ceylon cinnamon into your daily routine. You can buy Ceylon cinnamon supplements from us, ensuring you’re getting the best quality available.
Lastly, don’t forget to check out our Ceylon cinnamon tea bags, perfect for a soothing cup of tea at any time of the day. With our wide selection, you’re sure to find exactly what you need. Shop with us today for all your cinnamon and specialty product needs!
На сайте https://ruskiseerial.net/ представлены интересные и захватывающие дух фильмы, которые порадуют своей актерской игрой, интересной постановкой и происходящими событиями. В каждом фильме играют талантливые актеры, которые отлично исполняют свою роль и помогают зрителям отвлечься от повседневной суеты. Представлены самые разные жанры, включая драмы, мелодрамы, комедии, детективы, военные, криминал и многое другое. Есть раздел с теми произведениями, которые уже скоро появятся на сайте.
купить однокомнатную квартиру купить однокомнатную квартиру
столплит гардеробные системы
безопасно,
Индивидуальный подход к каждому пациенту, для поддержания здоровья рта,
Профессиональное лечение и консультации, для вашего уверенного выбора,
Комфортные условия и дружественный персонал, для вашей радости и улыбки,
Комплексное восстановление утраченных зубов, для вашего здоровья и красоты улыбки,
Индивидуальный план лечения и профилактики, для вашего комфорта и удовлетворения,
Индивидуальный план лечения для каждого пациента, для вашего комфорта и удовлетворения
стоматологія франківськ https://stomatologichnaklinikafghy.ivano-frankivsk.ua/ .
гарантированно,
Современное оборудование и материалы, для вашего уверенного улыбки,
Профессиональное лечение и консультации, для вашей улыбки,
Бесплатная консультация и диагностика, для вашего комфорта и уверенности,
Инновационные методы стоматологии, для вашего здоровья и красоты улыбки,
Экстренная помощь в любое время суток, для вашего долгосрочного удовлетворения,
Индивидуальный план лечения для каждого пациента, для вашего комфорта и удовлетворения
безболісне лікування зубів безболісне лікування зубів .
эффективно,
Индивидуальный подход к каждому пациенту, для поддержания здоровья рта,
Специализированная помощь по доступным ценам, для вашего уверенного выбора,
Комфортные условия и дружественный персонал, для вашей радости и улыбки,
Комплексное восстановление утраченных зубов, для вашего долгосрочного удовлетворения,
Экстренная помощь в любое время суток, для вашего долгосрочного удовлетворения,
Современное лечение заболеваний полости рта, для вашего здоровья и благополучия
зуби лікування https://stomatologichnaklinikafghy.ivano-frankivsk.ua/ .
купить однокомнатную квартиру квартира в новостройке
https://www.smbc-comics.com/smbcforum/viewtopic.php?f=1&t=10951
Looking to buy Ceylon cinnamon powder? You’ve come to the right place! We offer pure Ceylon cinnamon powder, known for its sweet, delicate flavor and numerous health benefits. If you’re wondering where to buy Ceylon cinnamon powder, look no further. Our Ceylon cinnamon for sale is available for purchase online, making it convenient for you to get this high-quality spice delivered straight to your door.
In addition to our pure Ceylon cinnamon powder, we also offer a variety of other products. If you’re a fan of herbal teas, consider trying Samahan tea. You can easily buy Samahan tea online through our store. It’s a wonderful blend of herbs and spices that supports your overall well-being.
For those who enjoy baking or cooking with coconut, we have desiccated coconut available. Wondering where to buy desiccated coconut? You can find it here, along with our extensive range of cinnamon products.
Speaking of cinnamon, our product line includes more than just powder. We also have Ceylon cinnamon sticks, perfect for adding a touch of flavor to your dishes or beverages. If you’re looking to purchase real cinnamon sticks online, we’ve got you covered.
Our selection doesn’t stop there. We offer cinnamon lotion and cinnamon body lotion for those who love the scent and benefits of cinnamon in their skincare routine. Additionally, you can find cinnamon shampoo and even cinnamon toothpicks at an affordable price.
For those interested in supplements, we have a range of Ceylon cinnamon supplements for sale. These supplements are a convenient way to incorporate the benefits of Ceylon cinnamon into your daily routine. You can buy Ceylon cinnamon supplements from us, ensuring you’re getting the best quality available.
Lastly, don’t forget to check out our Ceylon cinnamon tea bags, perfect for a soothing cup of tea at any time of the day. With our wide selection, you’re sure to find exactly what you need. Shop with us today for all your cinnamon and specialty product needs!
купить диплом в краснодаре https://6landik-diploms.com/
Ищите глиняную посуду ручной работы? Зайдите на сайт https://gzhelgonchar.ru/ и вы найдете широкий ассортимент глиняной посуды от производителя ручной работы. Гжельская гончарня – это широкий ассортимент посуды из глины, которую можно купить с доставкой по РФ и СНГ. Подробнее на сайте.
дешевые гардеробные системы
раздвижная стеклянная перегородка
Internet trading https://www.5692.com.ua/ru/news/3780111/gde-obucitsa-finansovoj-gramotnosti-kak-ne-poterat-a-priumnozit-sredstva is the ability to benefit from fluctuations in the rates of market assets (stocks, currencies, gold, oil, etc.). Most wealthy people in the world are fluent in this skill, and this is one of their sources of income even during a crisis. After all, you must admit that no matter what happens in the economy, there will always be something that gets more expensive and something that gets cheaper. And if you understand market patterns and know how to analyze trends, then you can certainly make money from it.
купить диплом кандидата наук 6landik-diploms.com
When you own a boat you experience enjoyment and pleasure. But there is another side of this: the maintenance of the boat. Our job https://ntdmarinegroup.com/ is to take over this side and leave you with only the pleasure and enjoyment.
Just wish to say your article is as astounding. The clearness to your publish is just excellent and i can suppose you are an expert in this subject. Fine together with your permission let me to snatch your feed to stay up to date with forthcoming post. Thank you a million and please continue the enjoyable work.
animesocial.su/blogs/1046/%D0%A1%D0%BA%D0%BE%D0%BB%D1%8C%D0%BA%D0%BE-%D0%BF%D1%80%D0%B8%D0%BC%D0%B5%D1%80%D0%BD%D0%BE-%D0%BC%D0%BE%D0%B6%D0%B5%D1%82-%D1%81%D1%82%D0%BE%D0%B8%D1%82%D1%8C-%D1%81%D0%B5%D0%B3%D0%BE%D0%B4%D0%BD%D1%8F-%D0%BA%D0%B0%D1%87%D0%B5%D1%81%D1%82%D0%B2%D0%B5%D0%BD%D0%BD%D1%8B%D0%B9-%D0%B4%D1%83%D0%B1%D0%BB%D0%B8%D0%BA%D0%B0%D1%82-%D0%B4%D0%B8%D0%BF%D0%BB%D0%BE%D0%BC%D0%B0
myanmarfootball.org/gallery/displayimage.php?album=lastup&cat=6&pos=0
jogibaba.com/blogs/32/Why-is-the-popularity-of-higher-education-rapidly-declining-now?lang=ru_ru
russiafreedom.ru/question/titan-s-teplakom/
mydoggymatch.com/read-blog/601_where-to-order-a-diploma-or-certificate-at-a-adequate-price.html?mode=night
The Next Big Trend In The SEO Services Near Me Industry Seo Services In London
На сайте https://filtry-dlya-ochistki.ru/ в большом ассортименте находятся фильтры для воды. Они помогут значительно повысить качество обычной воды, а также улучшить ее характеристики. Вы сможете подобрать именно то, что подходит по техническим характеристикам. Фильтры помогут улучшить вкус воды, сделают ее намного чище. Кроме того, срок службы бытовой техники будет продлен. Фильтры необходимы для того, чтобы удалить хлор, тяжелые металлы, а также микроорганизмы. Выбирая подходящий вариант, необходимо учесть количество уровней очистки и другие моменты.
https://steemit.com/hive-148497/@tanviryousafzai/morning-tea
Looking to buy Ceylon cinnamon powder? You’ve come to the right place! We offer pure Ceylon cinnamon powder, known for its sweet, delicate flavor and numerous health benefits. If you’re wondering where to buy Ceylon cinnamon powder, look no further. Our Ceylon cinnamon for sale is available for purchase online, making it convenient for you to get this high-quality spice delivered straight to your door.
In addition to our pure Ceylon cinnamon powder, we also offer a variety of other products. If you’re a fan of herbal teas, consider trying Samahan tea. You can easily buy Samahan tea online through our store. It’s a wonderful blend of herbs and spices that supports your overall well-being.
For those who enjoy baking or cooking with coconut, we have desiccated coconut available. Wondering where to buy desiccated coconut? You can find it here, along with our extensive range of cinnamon products.
Speaking of cinnamon, our product line includes more than just powder. We also have Ceylon cinnamon sticks, perfect for adding a touch of flavor to your dishes or beverages. If you’re looking to purchase real cinnamon sticks online, we’ve got you covered.
Our selection doesn’t stop there. We offer cinnamon lotion and cinnamon body lotion for those who love the scent and benefits of cinnamon in their skincare routine. Additionally, you can find cinnamon shampoo and even cinnamon toothpicks at an affordable price.
For those interested in supplements, we have a range of Ceylon cinnamon supplements for sale. These supplements are a convenient way to incorporate the benefits of Ceylon cinnamon into your daily routine. You can buy Ceylon cinnamon supplements from us, ensuring you’re getting the best quality available.
Lastly, don’t forget to check out our Ceylon cinnamon tea bags, perfect for a soothing cup of tea at any time of the day. With our wide selection, you’re sure to find exactly what you need. Shop with us today for all your cinnamon and specialty product needs!
На сайте https://lh3.ru/ вы получите всю нужную, содержательную информацию про то, как правильно организовать домашний уют, приятную и комфортную атмосферу. Вся информация будет интересна тем, у кого есть семья, дети. Этот блог содержит необходимые материалы о повседневной жизни. Так вы узнаете о том, как обустроить квартиру, чтобы в ней было приятно, уютно и привлекательно, хотелось туда возвращаться после работы. Также ознакомьтесь и с последними записями. Например, про именные браслеты и как часто необходимо подстригать челку, если у вас есть каре.
Вам интересен квалифицированный ремонт электро-транспорта в Минске? Мастерская 911 – это то, что вам нужно! В сервисном центре трудятся самые лучшие специалисты, которые имеют достаточный опыт работы. Они прекрасно разбираются в электросамокатах, быстро и качественно их ремонтируют. https://m911.by/ – сайт, где вы можете уже сейчас посмотреть наши услуги. Мы обеспечиваем своих клиентов недорогим ремонтом любого вида электро-транспорта. Обращайтесь именно к нам, продиагностируем поломку абсолютно бесплатно.
На сайте https://ost-profi.ru/ закажите качественные, надежные, функциональные и эстетически привлекательные перегородки, которые созданы для зонирования помещения. Компания предлагает приобрести стеклянные ограждения, которые используются в душе, мобильные перегородки, а также цельностеклянные. Все офисные перегородки реализуются по доступной и привлекательной стоимости. Есть возможность создать варианты абсолютно любых размеров. Возможно, вам понравятся те перегородки, которые созданы в лофт направлении.
https://foursquare.com/v/druera/6623f2f3ded9d24d555f7cea
Welcome to the ultimate destination for premium Ceylon cinnamon products! Our e-commerce store offers a curated selection of high-quality Ceylon cinnamon items, sourced directly from the lush landscapes of Sri Lanka. Whether you’re looking to enhance your culinary creations or boost your health, we’ve got you covered.
Our Products
Ceylon Cinnamon Powder: Known for its sweet and delicate flavor, our pure Ceylon cinnamon powder is perfect for baking, cooking, and adding a touch of spice to your favorite beverages. It’s a versatile pantry staple that elevates both sweet and savory dishes.
Ceylon Cinnamon Sticks: Ideal for infusing flavor into teas, stews, and desserts, our Ceylon cinnamon sticks are a must-have for any kitchen. Unlike the more common Cassia cinnamon, Ceylon cinnamon sticks offer a subtler, more refined taste.
Ceylon Cinnamon Capsules: Packed with health benefits, our Ceylon cinnamon capsules are a convenient way to support your wellness routine. These supplements are rich in antioxidants and have anti-inflammatory properties, making them a great addition to your daily regimen.
Ceylon Cinnamon Tea Bags: Enjoy the soothing and aromatic experience of Ceylon cinnamon tea. Our tea bags are filled with the finest Ceylon cinnamon, providing a calming and flavorful cup of tea that’s perfect any time of the day.
Cinnamon Body Care: Indulge in our range of cinnamon-infused body care products, including cinnamon lotion and cinnamon shampoo. These items harness the natural properties of Ceylon cinnamon to nourish and rejuvenate your skin and hair.
гардеробная система угловая с дверями
На сайте https://elekspb.ru закажите судовой кабель, судовую электротехнику с регистром и многое другое. Продажа осуществляется оптом. В компании трудятся проверенные, надежные специалисты, которые помогут подобрать нужное решение. Компания энергично и активно развивается на рынке, что позволяет своевременно реагировать на изменения. Предприятие специализируется на поставках электрооборудования, а также материалов для судостроения, судоремонта. Для того чтобы подобрать оптимальное решение, изучите технические характеристики.
На сайте https://claps.me/catalog/pribory-dlya-osoznannykh-snov/pribor-dlya-osoznannykh-snovideniy-dreamstalker-expert/ вы сможете приобрести маску для осознанных сновидений. Этот товар премиального уровня, а потому подарит приятные эмоции и точно выполнит все заявленные функции. Изделие выполнено из высокотехнологичных, совершенных материалов, а потому приятные к телу. Не доставят дискомфорта. Этот прибор считается новейшей версией, которая отлично работает. Всеми настройками управляют через Интернет.
заказать такси дешево сколько будет стоить такси
http://www.askmap.net/location/6924511/united-states/druera
Welcome to the ultimate destination for premium Ceylon cinnamon products! Our e-commerce store offers a curated selection of high-quality Ceylon cinnamon items, sourced directly from the lush landscapes of Sri Lanka. Whether you’re looking to enhance your culinary creations or boost your health, we’ve got you covered.
Our Products
Ceylon Cinnamon Powder: Known for its sweet and delicate flavor, our pure Ceylon cinnamon powder is perfect for baking, cooking, and adding a touch of spice to your favorite beverages. It’s a versatile pantry staple that elevates both sweet and savory dishes.
Ceylon Cinnamon Sticks: Ideal for infusing flavor into teas, stews, and desserts, our Ceylon cinnamon sticks are a must-have for any kitchen. Unlike the more common Cassia cinnamon, Ceylon cinnamon sticks offer a subtler, more refined taste.
Ceylon Cinnamon Capsules: Packed with health benefits, our Ceylon cinnamon capsules are a convenient way to support your wellness routine. These supplements are rich in antioxidants and have anti-inflammatory properties, making them a great addition to your daily regimen.
Ceylon Cinnamon Tea Bags: Enjoy the soothing and aromatic experience of Ceylon cinnamon tea. Our tea bags are filled with the finest Ceylon cinnamon, providing a calming and flavorful cup of tea that’s perfect any time of the day.
Cinnamon Body Care: Indulge in our range of cinnamon-infused body care products, including cinnamon lotion and cinnamon shampoo. These items harness the natural properties of Ceylon cinnamon to nourish and rejuvenate your skin and hair.
Thanks for sharing pg
https://www.startus.cc/company/703391
Welcome to the ultimate destination for premium Ceylon cinnamon products! Our e-commerce store offers a curated selection of high-quality Ceylon cinnamon items, sourced directly from the lush landscapes of Sri Lanka. Whether you’re looking to enhance your culinary creations or boost your health, we’ve got you covered.
Our Products
Ceylon Cinnamon Powder: Known for its sweet and delicate flavor, our pure Ceylon cinnamon powder is perfect for baking, cooking, and adding a touch of spice to your favorite beverages. It’s a versatile pantry staple that elevates both sweet and savory dishes.
Ceylon Cinnamon Sticks: Ideal for infusing flavor into teas, stews, and desserts, our Ceylon cinnamon sticks are a must-have for any kitchen. Unlike the more common Cassia cinnamon, Ceylon cinnamon sticks offer a subtler, more refined taste.
Ceylon Cinnamon Capsules: Packed with health benefits, our Ceylon cinnamon capsules are a convenient way to support your wellness routine. These supplements are rich in antioxidants and have anti-inflammatory properties, making them a great addition to your daily regimen.
Ceylon Cinnamon Tea Bags: Enjoy the soothing and aromatic experience of Ceylon cinnamon tea. Our tea bags are filled with the finest Ceylon cinnamon, providing a calming and flavorful cup of tea that’s perfect any time of the day.
Cinnamon Body Care: Indulge in our range of cinnamon-infused body care products, including cinnamon lotion and cinnamon shampoo. These items harness the natural properties of Ceylon cinnamon to nourish and rejuvenate your skin and hair.
https://pastelink.net/uv4vgs63
If you’re a fan of unique and flavorful dishes, you must try the Cinnamon Pork Cutlets Recipe. This delightful recipe brings out the best in pork with the warm, aromatic touch of cinnamon. For the best results, make sure to use Ceylon cinnamon sticks instead of the more common Cassia cinnamon. Wondering about the difference? When it comes to Ceylon Cinnamon Sticks vs. Cassia Cinnamon, Ceylon cinnamon is known for its sweeter, more delicate flavor, while Cassia has a stronger, more pungent taste. This distinction makes Ceylon the preferred choice for dishes where a subtle spice is desired.
Using Ceylon cinnamon powder in your cooking can elevate your meals to new heights. But do you know how to use Ceylon cinnamon powder in your favorite recipes? This versatile spice can be added to both sweet and savory dishes. Sprinkle it on your morning oatmeal, mix it into smoothies, or incorporate it into baked goods for a delicious twist. It’s also fantastic in savory recipes like curries, stews, and the aforementioned pork cutlets.
Apart from its culinary uses, Ceylon cinnamon offers numerous health benefits. Ceylon cinnamon capsules are a convenient way to enjoy these benefits. These supplements are packed with antioxidants and have anti-inflammatory properties. If you’re interested in the advantages, the Ceylon cinnamon capsules can help with blood sugar regulation, improving digestion, and boosting overall health. For those wondering about the benefits, dosage, and where to buy the best supplements, it’s recommended to take a look at reputable online stores that specialize in natural health products. The suggested dosage varies, so always follow the manufacturer’s instructions or consult with a healthcare professional.
Whether you’re cooking up a delicious meal or looking to enhance your health, Ceylon cinnamon is a versatile and beneficial spice to have on hand. Enjoy exploring its uses and benefits in your kitchen and beyond!
Зайдите на сайт https://came.name/ где вы сможете ознакомиться с широким ассортиментом оборудования CAME (итальянский производитель), таким как автоматика для ворот, шлагбаумы, парковочные системы, турникеты и многим другим. Узнайте больше информации о продукции на сайте, а также посмотрите прайс листы с выгодными ценами.
https://newport.opendi.us/9078982.html
Welcome to the ultimate destination for premium Ceylon cinnamon products! Our e-commerce store offers a curated selection of high-quality Ceylon cinnamon items, sourced directly from the lush landscapes of Sri Lanka. Whether you’re looking to enhance your culinary creations or boost your health, we’ve got you covered.
Our Products
Ceylon Cinnamon Powder: Known for its sweet and delicate flavor, our pure Ceylon cinnamon powder is perfect for baking, cooking, and adding a touch of spice to your favorite beverages. It’s a versatile pantry staple that elevates both sweet and savory dishes.
Ceylon Cinnamon Sticks: Ideal for infusing flavor into teas, stews, and desserts, our Ceylon cinnamon sticks are a must-have for any kitchen. Unlike the more common Cassia cinnamon, Ceylon cinnamon sticks offer a subtler, more refined taste.
Ceylon Cinnamon Capsules: Packed with health benefits, our Ceylon cinnamon capsules are a convenient way to support your wellness routine. These supplements are rich in antioxidants and have anti-inflammatory properties, making them a great addition to your daily regimen.
Ceylon Cinnamon Tea Bags: Enjoy the soothing and aromatic experience of Ceylon cinnamon tea. Our tea bags are filled with the finest Ceylon cinnamon, providing a calming and flavorful cup of tea that’s perfect any time of the day.
Cinnamon Body Care: Indulge in our range of cinnamon-infused body care products, including cinnamon lotion and cinnamon shampoo. These items harness the natural properties of Ceylon cinnamon to nourish and rejuvenate your skin and hair.
На сайте https://ntmsp.ru/ закажите звонок для того, чтобы приобрести продукцию компании ООО “НОВЫЕ ТЕХНОЛОГИИ И МАТЕРИАЛЫ”. Это развивающееся предприятие, которое работает в области создания комплектующих, которые применяются в радиотехнической промышленности. В каталоге вы найдете крепеж, ферритовые изделия, медицинские иглы, а также оснастку. В компании трудятся компетентные и опытные специалисты, которые предпринимают все, чтобы вы получили такую продукцию, которая соответствует самым высоким требованиям.
На сайте https://autodix.ru/ почитайте всю интересную, увлекательную и актуальную информацию, которая касается не только автомобилей, но и авторынка. Перед вами любопытные советы, ценные рекомендации, познавательные лайфхаки и многое другое, что поможет лучше сориентироваться во всем многообразии материала. Регулярно публикуется новый материал, который вызовет у вас интерес. Описаны техники правильного и безопасного подключения крокодила. Кроме того, у вас получится разобраться в модификациях и сериях автомобилей различных марок.
На сайте https://kupit-velosiped1.ru/ в огромном выборе представлены функциональные, качественные и практичные велосипеды, которые созданы для активного отдыха. Выбирать устройство необходимо, полагаясь на бюджет, материал рамы. В каталоге вы найдете шоссейные, горные, детские, складные велосипеды и другие модели, которые реализуются по привлекательной и доступной цене. На всю продукцию предоставляются гарантии. Все изделия отличаются привлекательным дизайном и безупречным качеством.
Посетите канал телеграм https://t.me/pinup_vhod_zerkalo_casino_sport и вы найдете Pin-Up Пинап Bonus & Promo | Pinup Пин Ап Регистрация, вход, скачать, зеркало | Casino | Link Kirish Giris | Mobile App. Сайт Pin-Up Пинап Россия, Казахстан, Узбекистан, Turkey
Pinup Пинап Букмекер Казино.
https://www.tupalo.co/wilmington-delaware/druera
Welcome to the ultimate destination for premium Ceylon cinnamon products! Our e-commerce store offers a curated selection of high-quality Ceylon cinnamon items, sourced directly from the lush landscapes of Sri Lanka. Whether you’re looking to enhance your culinary creations or boost your health, we’ve got you covered.
Our Products
Ceylon Cinnamon Powder: Known for its sweet and delicate flavor, our pure Ceylon cinnamon powder is perfect for baking, cooking, and adding a touch of spice to your favorite beverages. It’s a versatile pantry staple that elevates both sweet and savory dishes.
Ceylon Cinnamon Sticks: Ideal for infusing flavor into teas, stews, and desserts, our Ceylon cinnamon sticks are a must-have for any kitchen. Unlike the more common Cassia cinnamon, Ceylon cinnamon sticks offer a subtler, more refined taste.
Ceylon Cinnamon Capsules: Packed with health benefits, our Ceylon cinnamon capsules are a convenient way to support your wellness routine. These supplements are rich in antioxidants and have anti-inflammatory properties, making them a great addition to your daily regimen.
Ceylon Cinnamon Tea Bags: Enjoy the soothing and aromatic experience of Ceylon cinnamon tea. Our tea bags are filled with the finest Ceylon cinnamon, providing a calming and flavorful cup of tea that’s perfect any time of the day.
Cinnamon Body Care: Indulge in our range of cinnamon-infused body care products, including cinnamon lotion and cinnamon shampoo. These items harness the natural properties of Ceylon cinnamon to nourish and rejuvenate your skin and hair.
https://www.storeboard.com/druera
Welcome to the ultimate destination for premium Ceylon cinnamon products! Our e-commerce store offers a curated selection of high-quality Ceylon cinnamon items, sourced directly from the lush landscapes of Sri Lanka. Whether you’re looking to enhance your culinary creations or boost your health, we’ve got you covered.
Our Products
Ceylon Cinnamon Powder: Known for its sweet and delicate flavor, our pure Ceylon cinnamon powder is perfect for baking, cooking, and adding a touch of spice to your favorite beverages. It’s a versatile pantry staple that elevates both sweet and savory dishes.
Ceylon Cinnamon Sticks: Ideal for infusing flavor into teas, stews, and desserts, our Ceylon cinnamon sticks are a must-have for any kitchen. Unlike the more common Cassia cinnamon, Ceylon cinnamon sticks offer a subtler, more refined taste.
Ceylon Cinnamon Capsules: Packed with health benefits, our Ceylon cinnamon capsules are a convenient way to support your wellness routine. These supplements are rich in antioxidants and have anti-inflammatory properties, making them a great addition to your daily regimen.
Ceylon Cinnamon Tea Bags: Enjoy the soothing and aromatic experience of Ceylon cinnamon tea. Our tea bags are filled with the finest Ceylon cinnamon, providing a calming and flavorful cup of tea that’s perfect any time of the day.
Cinnamon Body Care: Indulge in our range of cinnamon-infused body care products, including cinnamon lotion and cinnamon shampoo. These items harness the natural properties of Ceylon cinnamon to nourish and rejuvenate your skin and hair.
На сайте https://ok-mebel.com/ вы сможете приобрести любую мебель, которая необходима для обустройства кухни, гостиной, спальни, детской. Есть огромный выбор прихожих, а также ванных комнат. Имеется и мебель для офисов, вместительные шкафы. Вся продукция создана из качественных, надежных и проверенных материалов, поэтому мебель не утратит своего вида, технических характеристик длительное время. А если вы хотите отыскать что-то определенное, то воспользуйтесь поиском. На всю мебель предоставляется гарантия 10 лет.
Czech health insurance for foreigners in Prague https://vaclavak48.cz/ is comprehensive health insurance for foreigners in the Czech Republic at the best prices. Центр Страхования Иностранцев в Праге, Чехия – это Медицинское страхование иностранцев в Чехии, а также Комплексные медицинские страховки для иностранных студентов в Праге и Чехии по лучшим ценам от страховых компаний. Все услуги в одном месте. Узнайте подробнее на сайте.
https://about.me/delivera
Welcome to the ultimate destination for premium Ceylon cinnamon products! Our e-commerce store offers a curated selection of high-quality Ceylon cinnamon items, sourced directly from the lush landscapes of Sri Lanka. Whether you’re looking to enhance your culinary creations or boost your health, we’ve got you covered.
Our Products
Ceylon Cinnamon Powder: Known for its sweet and delicate flavor, our pure Ceylon cinnamon powder is perfect for baking, cooking, and adding a touch of spice to your favorite beverages. It’s a versatile pantry staple that elevates both sweet and savory dishes.
Ceylon Cinnamon Sticks: Ideal for infusing flavor into teas, stews, and desserts, our Ceylon cinnamon sticks are a must-have for any kitchen. Unlike the more common Cassia cinnamon, Ceylon cinnamon sticks offer a subtler, more refined taste.
Ceylon Cinnamon Capsules: Packed with health benefits, our Ceylon cinnamon capsules are a convenient way to support your wellness routine. These supplements are rich in antioxidants and have anti-inflammatory properties, making them a great addition to your daily regimen.
Ceylon Cinnamon Tea Bags: Enjoy the soothing and aromatic experience of Ceylon cinnamon tea. Our tea bags are filled with the finest Ceylon cinnamon, providing a calming and flavorful cup of tea that’s perfect any time of the day.
Cinnamon Body Care: Indulge in our range of cinnamon-infused body care products, including cinnamon lotion and cinnamon shampoo. These items harness the natural properties of Ceylon cinnamon to nourish and rejuvenate your skin and hair.
cotrimoxazole where to buy – bactrim canada tobramycin 5mg sale
На сайте https://margoritka.ru ознакомьтесь с полезной, интересной и содержательной информацией, которая посвящена здоровью, красоте. Так вы узнаете о том, как справиться с сухостью кожи, о причинах гипотиреоза у женского населения и как с этим недугом справиться. Также вы ознакомитесь с особенностями аппарата, предназначенного для промывания носа. Имеется информация и о шариках Кегеля. Вы узнаете о том, как решить проблему, связанную с сухостью в интимной зоне. Также есть данные и о зубных протезах.
hydroquinone medication – cost dydrogesterone cheap dydrogesterone 10 mg
На сайте https://vpolshe.com/pesel-bez-prisutstviya/ вы сможете заказать оформление песеля в Польше. Для того чтобы воспользоваться услугой, необходимо заказать специальную исчерпывающую консультацию, на которой менеджер расскажет, что необходимо для оформления важного документа. Здесь же можно сделать песель и для малыша. Стоимость указана на сайте, а срок изготовления – не более 3 дней. Также возможно восстановление документа, если тот был утерян в Варшаве. Вам вышлют скан в формате PDF. При необходимости будет получен документ на сотрудников.
На сайте https://polvteplo.ru/ в огромном ассортименте представлены нагревательные маты, кабели, инфракрасный пол, а также терморегулятор, который используется для теплого пола и многое другое. Есть вариант подобрать все необходимое по типу напольного покрытия: под ламинат, плитку, керамогранит, паркетную доску. Здесь вы сможете не только приобрести все компоненты для теплых полов, но и заказать поставку, проектирование, а также монтажные работы. Для того чтобы лучше разбираться в теме, изучите полезные информационные статьи.
cotrimoxazole pills – levetiracetam 500mg pills tobra ca
На сайте https://biancorosso.ru/ ознакомьтесь с увлекательной, интересной и актуальной информацией на самую разную тему. Так вы узнаете о том, какой цвет волос подойдет именно вам, особенности стрижки каре на длинные волосы. Присутствуют и любопытные, содержательные уроки макияжа. Вы научитесь правильно наносить косметику, чтобы в любой ситуации выглядеть очаровательно. Кроме того, имеется информация относительно того, какой макияж актуален в этом году. Все рекомендации от стилистов и профессионалов, а потому на них точно можно полагаться.
https://www.localbusinesslisting.org/druera
Welcome to the ultimate destination for premium Ceylon cinnamon products! Our e-commerce store offers a curated selection of high-quality Ceylon cinnamon items, sourced directly from the lush landscapes of Sri Lanka. Whether you’re looking to enhance your culinary creations or boost your health, we’ve got you covered.
Our Products
Ceylon Cinnamon Powder: Known for its sweet and delicate flavor, our pure Ceylon cinnamon powder is perfect for baking, cooking, and adding a touch of spice to your favorite beverages. It’s a versatile pantry staple that elevates both sweet and savory dishes.
Ceylon Cinnamon Sticks: Ideal for infusing flavor into teas, stews, and desserts, our Ceylon cinnamon sticks are a must-have for any kitchen. Unlike the more common Cassia cinnamon, Ceylon cinnamon sticks offer a subtler, more refined taste.
Ceylon Cinnamon Capsules: Packed with health benefits, our Ceylon cinnamon capsules are a convenient way to support your wellness routine. These supplements are rich in antioxidants and have anti-inflammatory properties, making them a great addition to your daily regimen.
Ceylon Cinnamon Tea Bags: Enjoy the soothing and aromatic experience of Ceylon cinnamon tea. Our tea bags are filled with the finest Ceylon cinnamon, providing a calming and flavorful cup of tea that’s perfect any time of the day.
Cinnamon Body Care: Indulge in our range of cinnamon-infused body care products, including cinnamon lotion and cinnamon shampoo. These items harness the natural properties of Ceylon cinnamon to nourish and rejuvenate your skin and hair.
Хотите быстро и без каких-либо проблем заменить права на польские? MIGRANT SUPPORT – это то, что вам необходимо. Компания гарантирует разумные цены и индивидуальный подход. Наши специалисты имеют большой опыт работы. Они предоставят вам нужную информацию о том, как заменить права на польские. https://migrant.support/obmien_rossiiskikh_prav_na_polskiie – сайт, где у вас есть возможность прямо сегодня заказать услугу. Также тут можно в удобное время ознакомиться с отзывами компании. Звоните нам уже сейчас, всегда готовы ответить на интересующие вас вопросы.
На сайте https://sulyaev.ru/ изучите информацию о практикующем и профессиональном психологе-психоаналитике Андрее Суляеве. Он поможет решить даже самые сложные, запутанные дела, которые требуют особенного внимания к деталям. Поэтому если и у вас накопились проблемы, то воспользуйтесь помощью этого специалиста. Основная деятельность психолога заключается в частных психологических практиках. При этом установлены привлекательные расценки на услуги. Он с радостью ответит на все вопросы и даст советы.
На сайте https://stekloholst-77.ru/ в огромном ассортименте представлены стеклохолсты. Они представляют собой такой обойный материал, который производится из стекловолокна. Зачастую применяется с той целью, чтобы выровнять потолки, стены, а также сделать интерьер более привлекательным и красивым. Все изделия отличаются высоким качеством. Полотно наделено высокой прочностью, надежностью, а также экологической безопасностью. Нанесение стеклохолста не вызывает неудобств. А при выборе такого материала необходимо ориентироваться на плотность, а также размер рулона.
https://6655f2c32f8f9.site123.me/
Welcome to the ultimate destination for premium Ceylon cinnamon products! Our e-commerce store offers a curated selection of high-quality Ceylon cinnamon items, sourced directly from the lush landscapes of Sri Lanka. Whether you’re looking to enhance your culinary creations or boost your health, we’ve got you covered.
Our Products
Ceylon Cinnamon Powder: Known for its sweet and delicate flavor, our pure Ceylon cinnamon powder is perfect for baking, cooking, and adding a touch of spice to your favorite beverages. It’s a versatile pantry staple that elevates both sweet and savory dishes.
Ceylon Cinnamon Sticks: Ideal for infusing flavor into teas, stews, and desserts, our Ceylon cinnamon sticks are a must-have for any kitchen. Unlike the more common Cassia cinnamon, Ceylon cinnamon sticks offer a subtler, more refined taste.
Ceylon Cinnamon Capsules: Packed with health benefits, our Ceylon cinnamon capsules are a convenient way to support your wellness routine. These supplements are rich in antioxidants and have anti-inflammatory properties, making them a great addition to your daily regimen.
Ceylon Cinnamon Tea Bags: Enjoy the soothing and aromatic experience of Ceylon cinnamon tea. Our tea bags are filled with the finest Ceylon cinnamon, providing a calming and flavorful cup of tea that’s perfect any time of the day.
Cinnamon Body Care: Indulge in our range of cinnamon-infused body care products, including cinnamon lotion and cinnamon shampoo. These items harness the natural properties of Ceylon cinnamon to nourish and rejuvenate your skin and hair.
Натяжные потолки в Москве https://potolki-pk.ru/ от профессионалов! Бесплатный выезд замерщика. Натяжные потолки под ключ, все возможные варианты, от базовых проектов, до сложных решений. Установка, монтаж, собственное производство! Подробнее на сайте.
https://www.yellowpages.com/claim-your-listing-new
Welcome to the ultimate destination for premium Ceylon cinnamon products! Our e-commerce store offers a curated selection of high-quality Ceylon cinnamon items, sourced directly from the lush landscapes of Sri Lanka. Whether you’re looking to enhance your culinary creations or boost your health, we’ve got you covered.
Our Products
Ceylon Cinnamon Powder: Known for its sweet and delicate flavor, our pure Ceylon cinnamon powder is perfect for baking, cooking, and adding a touch of spice to your favorite beverages. It’s a versatile pantry staple that elevates both sweet and savory dishes.
Ceylon Cinnamon Sticks: Ideal for infusing flavor into teas, stews, and desserts, our Ceylon cinnamon sticks are a must-have for any kitchen. Unlike the more common Cassia cinnamon, Ceylon cinnamon sticks offer a subtler, more refined taste.
Ceylon Cinnamon Capsules: Packed with health benefits, our Ceylon cinnamon capsules are a convenient way to support your wellness routine. These supplements are rich in antioxidants and have anti-inflammatory properties, making them a great addition to your daily regimen.
Ceylon Cinnamon Tea Bags: Enjoy the soothing and aromatic experience of Ceylon cinnamon tea. Our tea bags are filled with the finest Ceylon cinnamon, providing a calming and flavorful cup of tea that’s perfect any time of the day.
Cinnamon Body Care: Indulge in our range of cinnamon-infused body care products, including cinnamon lotion and cinnamon shampoo. These items harness the natural properties of Ceylon cinnamon to nourish and rejuvenate your skin and hair.
IFran.ru – это онлайн-проект, созданный для повышения искренности и прозрачности рынка франчайзинга в РФ. Сервис анализирует и собирает данные из различных источников, после предоставляет информацию в единообразной и структурированной форме. https://www.ifran.ru – сайт, где вы узнаете, что такое франчайзинг. Здесь имеются интересные статьи, обзоры и рейтинги. Благодаря возможностям нашего портала потенциальные франчайзи могут сделать выбор в пользу высококачественных франшизеров.
Pro88
Pro88
Компания https://primeinterior.ru/ занимается поставками натурального мрамора, гранита, травертина, оникса и кварцита со всего мира для премиальных интерьеров. Имеем собственное производство во Владивостоке и команду специалистов для монтажа. Готовы к крупным заказам любой сложности со всей России, есть опыт работы с отелями, ресторанами, ночными клубами. Создаём неповторимые интерьеры из природного камня, высокое качество работы и материалов.
Зайдите на сайт АКСЕЛЬ https://axsel-murmansk.ru/ где вы сможете купить новый автомобиль или автомобиль с пробегом в Мурманске. Ознакомьтесь с каталогом авто в наличии, выберите по параметрам и стоимости. Также работает быстрый выездной выкуп по самым выгодным ценам. Предоставляем услуги кредитования, лизинга, страхования.
https://www.cylex.us.com/company/druera-37602055.html
Welcome to the ultimate destination for premium Ceylon cinnamon products! Our e-commerce store offers a curated selection of high-quality Ceylon cinnamon items, sourced directly from the lush landscapes of Sri Lanka. Whether you’re looking to enhance your culinary creations or boost your health, we’ve got you covered.
Our Products
Ceylon Cinnamon Powder: Known for its sweet and delicate flavor, our pure Ceylon cinnamon powder is perfect for baking, cooking, and adding a touch of spice to your favorite beverages. It’s a versatile pantry staple that elevates both sweet and savory dishes.
Ceylon Cinnamon Sticks: Ideal for infusing flavor into teas, stews, and desserts, our Ceylon cinnamon sticks are a must-have for any kitchen. Unlike the more common Cassia cinnamon, Ceylon cinnamon sticks offer a subtler, more refined taste.
Ceylon Cinnamon Capsules: Packed with health benefits, our Ceylon cinnamon capsules are a convenient way to support your wellness routine. These supplements are rich in antioxidants and have anti-inflammatory properties, making them a great addition to your daily regimen.
Ceylon Cinnamon Tea Bags: Enjoy the soothing and aromatic experience of Ceylon cinnamon tea. Our tea bags are filled with the finest Ceylon cinnamon, providing a calming and flavorful cup of tea that’s perfect any time of the day.
Cinnamon Body Care: Indulge in our range of cinnamon-infused body care products, including cinnamon lotion and cinnamon shampoo. These items harness the natural properties of Ceylon cinnamon to nourish and rejuvenate your skin and hair.
generic zovirax – pill dydrogesterone 10 mg brand duphaston 10 mg
На сайте https://mammas.ru/ почитайте увлекательную информацию на самую разную тему. Так есть статьи на тему психологии, красоты, отдыха, здоровья, детей, моды, дома, а также питания. Также почитайте публикации, касающиеся того, что сейчас находится в тренде и является актуальным. Имеются данные о том, кто такой мужчина-нарцисс, как его правильно распознать, кому подходит каре с челкой и какие варианты стрижки существуют. Есть информация на тему личных границ, как их сохранить и сберечь. Кроме того, вы будете в курсе того, чем лучше заняться в летнее время. Перед вами самые эффективные идеи.
На сайте https://nabor-curierov.ru/ozon/ оставьте заявку для того, чтобы стать курьером ОЗОН и получать регулярные заказы. Если вы будете развозить заказы на личном автомобиле, то сможете получить 5 500 р. в день, а если на авто компании, то 7 000. Вы устраиваетесь на работу как самозанятый. Вас ожидает стабильная работа, а выплаты происходят каждую неделю, что очень удобно. А если выполните брендирование авто, то получите сверху еще 5 000 рублей. Если возникла непредвиденная ситуация, то всегда сможете рассчитывать на оперативное решение вопроса.
https://www.showmelocal.com/profile.aspx?bid=23408058
Welcome to the ultimate destination for premium Ceylon cinnamon products! Our e-commerce store offers a curated selection of high-quality Ceylon cinnamon items, sourced directly from the lush landscapes of Sri Lanka. Whether you’re looking to enhance your culinary creations or boost your health, we’ve got you covered.
Our Products
Ceylon Cinnamon Powder: Known for its sweet and delicate flavor, our pure Ceylon cinnamon powder is perfect for baking, cooking, and adding a touch of spice to your favorite beverages. It’s a versatile pantry staple that elevates both sweet and savory dishes.
Ceylon Cinnamon Sticks: Ideal for infusing flavor into teas, stews, and desserts, our Ceylon cinnamon sticks are a must-have for any kitchen. Unlike the more common Cassia cinnamon, Ceylon cinnamon sticks offer a subtler, more refined taste.
Ceylon Cinnamon Capsules: Packed with health benefits, our Ceylon cinnamon capsules are a convenient way to support your wellness routine. These supplements are rich in antioxidants and have anti-inflammatory properties, making them a great addition to your daily regimen.
Ceylon Cinnamon Tea Bags: Enjoy the soothing and aromatic experience of Ceylon cinnamon tea. Our tea bags are filled with the finest Ceylon cinnamon, providing a calming and flavorful cup of tea that’s perfect any time of the day.
Cinnamon Body Care: Indulge in our range of cinnamon-infused body care products, including cinnamon lotion and cinnamon shampoo. These items harness the natural properties of Ceylon cinnamon to nourish and rejuvenate your skin and hair.
На сайте https://advokat-samara.ru/ вы сможете воспользоваться услугами квалифицированного, опытного адвоката по уголовным делам Мотина Анатолия Владимировича. У него профильное высшее образование, а в юриспруденции находится с 2002 года. Он на профессиональном уровне решает такие дела, как: ДТП, происшествия на воде, авиакатастрофы, транспортные преступления. В том случае, если вы находитесь в поисках лучшего и опытного специалиста, то воспользуйтесь услугами данного юриста.
Сайт fermerstvo.in.ua пользуется повышенной популярностью. Здесь представлена только интересная информация. Ознакомиться с ней есть возможность уже сейчас. fermerstvo.in.ua – https://fermerstvo.in.ua сайт, где узнаете с чего начать фермерское хозяйство. Мы открыто делимся своими успехами и неудачами. Разбираем, как подготовиться к разведению домашней птицы. Объясним, как урожайность овощей повысить. У нас вы найдете ответы на необходимые вопросы. Делаем понятный контент. Вы получите обширные знания о том, что имеет отношение к фермерскому хозяйству.
На сайте https://potolochnye-svetilniki.ru/ в огромном многообразии представлены потолочные светильники, которые добавят уюта, сделают ваш дом более комфортным, интересным и привлекательным. Многие выбирают потолочные светильники по той причине, что они отличаются высоким качеством, реализуются по доступной стоимости. Специально для вас безопасная доставка. Прямо сейчас вы сможете приобрести светильники для любого типа помещения, включая кухню, спальню, коридор, зал. Для ванной получится подобрать водонепроницаемые решения.
Изготовление металлоконструкций и изделий в Иркутске от https://afk77.ru/ это производство металлоконструкций и металлоизделий в Иркутске. Работаем с конструкциями любой сложности, качество ГОСТ. Реализуем сложные проекты. Ознакомьтесь с номенклатурой и нашей компанией на сайте.
Are you looking for reliable and fast proxy servers? FineProxy.org It offers a wide range of proxies with excellent speed and stability. Ideal for surfing, parsing and other online tasks. Excellent customer service and support. Start right now at this link: https://fineproxy.org/account/aff.php?aff=31
newsmiamigardens.com
MIGRANT SUPPORT предоставляет услуги лучших специалистов, обладающих достаточным опытом работы. В своей деятельности мы исповедуем персональный подход к каждому клиенту. Гарантируем достижение в выгодном совместном сотрудничестве и приемлемые цены. https://vpolshe.com/kriptolitsenziya-v-polshe/ – сайт, где у вас есть возможность уже сегодня оставить заявку. Поможем вам с получением криптолицензии в Польше. Процесс пройдет хорошо, мы все выполним оперативно. Вы останетесь довольны результатом и сервисом. Звоните, ответим на ваши вопросы!
На сайте https://gotovi.ru/ ознакомьтесь с интересной, увлекательной информацией о том, что необходимо современной женщине. Есть материалы об аксессуарах, как и с чем лучше сочетать сумки определенного цвета и материала. Вы узнаете, как всегда оставаться на стиле, быть модной, но при этом не переплачивать за бренды. Есть информация о том, что должно быть в гардеробе как на каждый день, так и для дома. Имеются публикации на тему туризма – как правильно собирать чемоданы и подготовиться к поездке.
chinataste1.com
cash advance fargo nd The Christmas/celebration loan amount is generally small, ranging between a few hundreds and ten thousand dollars.
На сайте https://kulery-dlya-vody.ru/ вы сможете выбрать и приобрести надежные, функциональные кулеры для воды. Они идеально подходят не только для домашнего использования, но и в офис. Перед вами интересные, привлекательные решения, которые созданы для того, чтобы обеспечить вам комфорт и практичность. Перед тем, как выбрать определенную модель, необходимо ознакомиться с ее характеристиками, особенностями и нюансами. Совершив покупку в этом магазине, вы сможете рассчитывать на: доступные расценки, оперативную доставку, а также гарантии.
На сайте https://www.okna-mechtipro.ru/ закажите двери, окна, которые производятся из ПВХ. Здесь практикуются на создании ПВХ-конструкций самого разного предназначения и вида. Прямо сейчас закажите бесплатный замер. На все работы, конструкции дается гарантия – 3 года. Доставка, монтажные работы осуществляются за один день. Компания всегда устраивает для своих клиентов выгодные акции, делает скидки. Окна точно прослужат очень долго! Есть возможность заказать окна самых разных цветов и форм. Продажа качественных конструкций сопровождается сервисом высокого уровня.
Crypto Pump Signals for Binance https://cryptopumpsignalsbinance.com/ is a unique project that provides traders and investors with valuable insights into upcoming cryptocurrency pumps. Through its Telegram channel and AI capabilities, this project offers new opportunities for generating massive profits in the short-term.
На сайте https://v-electronic.ru/ вы сможете приобрести электронику от самых разных производителей: телевизоры, различные гаджеты, смартфоны, технику для кухни, дома, фото, видео, все для укладки волос, включая плойки, фены, ирригаторы, массажеры и многое другое. Имеется раздел, в котором представлен товар дня. Перед вами самые интересные, выгодные предложения, а потому спешите быстрее совершить приятную покупку до подорожания. Доступна экспресс-доставка – уже через 2 часа курьер приедет с посылкой.
На сайте https://premier-pokrytie.ru/ есть возможность заказать резиновое покрытие, которое используется внутри помещения, а также на детских, спортивных площадках. В компании трудятся компетентные и лучшие специалисты, у которых огромный опыт работы в данной сфере. Они в совершенстве знакомы с технологией создания резинового покрытия, что позволяет предложить продукт безупречного качества и с уникальными техническими характеристиками. Специалист приедет к вам на объект для замеров абсолютно бесплатно.
Igrosite – портал для геймеров, который предоставляет большой спектр контента, включая обзоры, статьи и руководства, а также новости. Здесь найдете информацию о последних событиях в мире игр, сможете выбрать игры для своей коллекции и общаться с другими игроками в дружественной атмосфере. https://igrosite.ru – портал, где мы для вас подготовили с разработчиками интервью, аналитические факты и материалы, для того, чтобы вы за кулисы создания игр могли заглянуть. Узнаете интересные подробности о развитии этой увлекательной отрасли. Заходите уже сейчас на наш сайт!
На сайте https://top-volna.ru воспользуйтесь уникальной возможностью послушать любимую радиостанцию и просто получить отменное настроение от приятно проведенного времени. На этом портале такие радиостанции, как: Маруся ФМ, Русское Радио, Новое Радио, Европа Плюс, DFM, Радио Энерджи, Ретро FM, Юмор FM и многое другое. Прямо сейчас послушайте самые популярные песни, которые нравятся многим. Вас покорит отличное звучание, а также интересная аранжировка, которая точно никого не оставит без внимания.
На сайте https://omsksite.ru/ представлены самые эффективные, работающие методы выполнения ремонта. Этот блог посвящен строительным, ремонтным, отделочным работам. Вся информация является полезной, интересной. А самое главное, что позволит справиться с проблемой максимально быстро. На сайте будут рассказаны все тонкости ремонта и то, какие материалы для этих целей лучше использовать. Имеется контент на тему того, как правильно подобрать пластиковое окно. Есть информация про пожарную охрану, руководство, которое поможет правильно подобрать набор инструментов.
Портал visti.in.ua заслуживает вашего внимания. Здесь представлены актуальные новости Украины, они находятся в круглосуточном доступе. Мы ценим и гордимся своими читателями. Для вас собрали только самое лучшее, поудобнее устраивайтесь и читайте интересную информацию. visti.in.ua – https://visti.in.ua сайт, который пользуется повышенной популярностью. Заходите уже сегодня, и вы узнаете о науке, спорте, экономике и политике. Все сведения достоверны, можете даже в этом не сомневаться. Следите за нами и наслаждайтесь великолепным контентом!
สล็อตเว็บตรง
срочный ремонт телефонов
payday advance fort mill sc These loans are approved only when the borrower has satisfied the lenders about safe and timely return of the loan.
Professioneel CV https://cvzen.nl/ om je droombaan te krijgen Onze carriere-experts, redacteuren en geavanceerde technologie zullen je helpen om je carriere naar een hoger niveau te tillen.
На сайте https://elektrosamokat1.ru вы сможете ознакомиться со всеми преимуществами, особенностями электросамокатов, которые считаются удобным и комфортным способом передвижения. Перед вами огромный выбор самых интересных и функциональных моделей. Они идеально подходят для пассажиров самых разных возрастов. Эти устройства представлены только от лучших производителей, которые положительно себя показали. Имеются варианты премиального уровня, а также более бюджетные. Этот вид транспорта не только экологически чистый, но и экономичный, но при этом достаточно мощный.
купить диплом медсестры https://6landik-diploms.com
A gazebo with a breakdown on the lawn. If there mexicocities.net is a decorative lawn on the site, it can be installed on a gazebo with a floor so as not to harm the grass. The platform is made in the form of a metal profile, which is attached to several holes drilled in the soil.
Зайдите на сайт https://came.name/ где вы сможете ознакомиться с широким ассортиментом оборудования CAME (итальянский производитель), таким как автоматика для ворот, шлагбаумы, парковочные системы, турникеты и многим другим. Узнайте больше информации о продукции на сайте, а также посмотрите прайс листы с выгодными ценами.
Официальный дилер Москвич в Мурманске https://axsel-moskvich.ru/ с автомобилями в наличии. Зайдите и ознакомьтесь с модельным рядом и ценами, спец предложениями и акциями. Воспользуйтесь конфигуратором автомобиля, а также действующими выгодными кредитными программами или запишитесь на ТО.
купить диплом в воронеже https://6landik-diploms.com
Популярный интернет-магазин CLAPS предлагает купить по доступной цене DreamStalker Expert. Прибор находится в лобной части маски, особая конструкция которой обеспечивает комфортный сон, прекрасную вентиляцию, охлаждение, отсутствие запотевания лба. https://claps.me – сайт, где имеется каталог, в нем есть описание, характеристики, фотографии товара. Тут представлены отзывы довольных покупателей, с ними ознакомиться можете в любое удобное для вас время. Также на портале найдете к DreamStalker Expert инструкции.
new payday loan company Apart from the above, there are certain financial institutions that offer payday loans for those with a very low credit score.
Советы по сео стратегии продвижению.
Информация о том как управлять с низкочастотными запросами запросами и как их подбирать
Стратегия по деятельности в соперничающей нише.
У меня есть регулярных взаимодействую с 3 компаниями, есть что поделиться.
Изучите мой досье, на 31 мая 2024г
число успешных проектов 2181 только на этом сайте.
Консультация только устно, никаких снимков с экрана и отчётов.
Время консультации указано 2 часа, и факту всегда на контакте без строгой фиксации времени.
Как работать с ПО это уже иначе история, консультация по работе с софтом оговариваем отдельно в специальном разделе, узнаем что требуется при коммуникации.
Всё спокойно на без напряжения не в спешке
To get started, the seller needs:
Мне нужны данные от Telegram канала для контакта.
общение только в устной форме, общаться письменно не хватает времени.
субботы и воскресенья нерабочие дни
гарантированно,
Современное оборудование и материалы, для вашего уверенного улыбки,
Современные методы стоматологии, для вашего удобства,
Индивидуальный подход к каждому пациенту, для вашего комфорта и уверенности,
Инновационные методы стоматологии, для вашего комфорта и уверенности,
Профессиональная гигиена полости рта, для вашего здоровья и уверенности в себе,
Индивидуальный план лечения для каждого пациента, для вашего здоровья и благополучия
стоматологiчна полiклiнiка https://stomatologichnaklinikafghy.ivano-frankivsk.ua/ .
гарантированно,
Индивидуальный подход к каждому пациенту, для вашего уверенного улыбки,
Специализированная помощь по доступным ценам, для вашего уверенного выбора,
Индивидуальный подход к каждому пациенту, для вашего комфорта и уверенности,
Инновационные методы стоматологии, для вашего комфорта и уверенности,
Индивидуальный план лечения и профилактики, для вашего комфорта и удовлетворения,
Индивидуальный план лечения для каждого пациента, для вашего здоровья и благополучия
лікування зубів https://stomatologichnaklinikafghy.ivano-frankivsk.ua/ .
эффективно,
Индивидуальный подход к каждому пациенту, для поддержания здоровья рта,
Специализированная помощь по доступным ценам, для вашего удобства,
Индивидуальный подход к каждому пациенту, для вашего здоровья и благополучия,
Эффективное лечение зубов и десен, для вашего комфорта и уверенности,
Индивидуальный план лечения и профилактики, для вашего здоровья и уверенности в себе,
Индивидуальный план лечения для каждого пациента, для вашего здоровья и благополучия
дитяча стоматологія дитяча стоматологія .
безопасно,
Индивидуальный подход к каждому пациенту, для поддержания здоровья рта,
Специализированная помощь по доступным ценам, для вашего уверенного выбора,
Бесплатная консультация и диагностика, для вашего здоровья и благополучия,
Инновационные методы стоматологии, для вашего долгосрочного удовлетворения,
Индивидуальный план лечения и профилактики, для вашего комфорта и удовлетворения,
Заботливое отношение и внимательный подход, для вашего комфорта и удовлетворения
дитяча стоматологічна клініка дитяча стоматологічна клініка .
An outstanding share! I’ve just forwarded this onto a coworker who had been doing a little homework on this. And he actually ordered me lunch because I stumbled upon it for him… lol. So allow me to reword this…. Thanks for the meal!! But yeah, thanx for spending some time to talk about this issue here on your site.
collie.fatbb.ru/viewtopic.php?f=18&t=4169&start=0&view=print
blogs.rufox.ru/~worksale/45652.htm
aysdoorrepair.com/contact.php
epicit.ru/page/14
allwingroup.ru/business/kadastrovye-uslugi/poluchenie-postanovleniya-o-prisvoenii-pochtovogo-adresa/
гарантированно,
Современное оборудование и материалы, для поддержания здоровья рта,
Профессиональное лечение и консультации, для вашей улыбки,
Бесплатная консультация и диагностика, для вашего здоровья и благополучия,
Комплексное восстановление утраченных зубов, для вашего здоровья и красоты улыбки,
Индивидуальный план лечения и профилактики, для вашего здоровья и уверенности в себе,
Современное лечение заболеваний полости рта, для вашего комфорта и удовлетворения
стоматологія в івано франківську https://stomatologichnaklinikafghy.ivano-frankivsk.ua/ .
эффективно,
Индивидуальный подход к каждому пациенту, для поддержания здоровья рта,
Профессиональное лечение и консультации, для вашей улыбки,
Комфортные условия и дружественный персонал, для вашего здоровья и благополучия,
Эффективное лечение зубов и десен, для вашего здоровья и красоты улыбки,
Экстренная помощь в любое время суток, для вашего здоровья и уверенности в себе,
Современное лечение заболеваний полости рта, для вашего комфорта и удовлетворения
дитяча стоматологія https://stomatologichnaklinikafghy.ivano-frankivsk.ua/ .
такси новочеркасск недорого https://taxi-novocherkassk.ru/
такси недорого цены https://zakaz-taxionline.ru/
гарантированно,
Современное оборудование и материалы, для вашего уверенного улыбки,
Профессиональное лечение и консультации, для вашего уверенного выбора,
Бесплатная консультация и диагностика, для вашей радости и улыбки,
Комплексное восстановление утраченных зубов, для вашего здоровья и красоты улыбки,
Профессиональная гигиена полости рта, для вашего здоровья и уверенности в себе,
Современное лечение заболеваний полости рта, для вашей уверенной улыбки
дитяча стоматологія дитяча стоматологія .
безопасно,
Индивидуальный подход к каждому пациенту, для поддержания здоровья рта,
Современные методы стоматологии, для вашего удобства,
Индивидуальный подход к каждому пациенту, для вашего здоровья и благополучия,
Комплексное восстановление утраченных зубов, для вашего долгосрочного удовлетворения,
Экстренная помощь в любое время суток, для вашего комфорта и удовлетворения,
Заботливое отношение и внимательный подход, для вашей уверенной улыбки
стоматологiчна полiклiнiка https://stomatologichnaklinikafghy.ivano-frankivsk.ua/ .
На сайте https://gazelka86.ru/ закажите грузоперевозки с хорошей скидкой до 50%. Это очень удобно, потому как в компании работают первоклассные, компетентные специалисты, которые выполнят все работы на высоком уровне, профессионально и качественно. Под груз выделяется свой транспорт, который подбирается в соответствии с габаритами, объемом, весом. Предоставляется полный комплекс услуг, чтобы вы воспользовались именно тем, что нужно. Учитывая небольшую стоимость, дается еще и скидка.
заказать такси в новочеркасске https://taxi-novocherkassk.ru/
Reducing the cost of attracting job-career.com new customers. You can inexpensively retain existing customers through quality customer service. It’s much cheaper than constantly recruiting new people.
homebeachlove.com
I’m gone to inform my little brother, that he should also go to see this weblog on regular basis to take updated from most recent information.
cocochampionship.com/en/contact
mir-forum.ru/programm/index.html
iclicky.com/index.php?do=/public/user/blogs/name_Alanpoe/page_5/
krutovo.ru/index.php?name=Account&op=info&uname=ymonozav
malhotrafoundation.org/media/releases
Сайт Украиночка предлагает интересную и полезную информацию. Наша основная миссия – помочь вам быть уверенной и образованной. Мы знаем то, что вы заслуживаете самое лучшее. В любых аспектах жизни мы вдохновим вас на достижение вершин. Раскроем большой спектр возможностей для самовыражения и саморазвития. ukrayinochka.com – https://ukrayinochka.com портал, где находится все, что интересует современных женщин: от горячих новостей до вдумчивых рекомендаций. Заходите на наш сайт уже сейчас. Вас ожидает лучший контент!
Ищете способ расслабиться и получить незабываемые впечатления? Мы https://t.me/intim_tmn72 предлагаем эксклюзивные встречи с привлекательными и профессиональными компаньонками. Конфиденциальность, комфорт и безопасность гарантированы. Позвольте себе наслаждение и отдых в приятной компании.
гарантированно,
Лучшие стоматологи города, для поддержания здоровья рта,
Специализированная помощь по доступным ценам, для вашего уверенного выбора,
Индивидуальный подход к каждому пациенту, для вашего здоровья и благополучия,
Инновационные методы стоматологии, для вашего долгосрочного удовлетворения,
Индивидуальный план лечения и профилактики, для вашего долгосрочного удовлетворения,
Современное лечение заболеваний полости рта, для вашей уверенной улыбки
клініка стоматологічна https://stomatologichnaklinikafghy.ivano-frankivsk.ua/ .
безопасно,
Индивидуальный подход к каждому пациенту, для крепких и здоровых зубов,
Специализированная помощь по доступным ценам, для вашего удобства,
Индивидуальный подход к каждому пациенту, для вашей радости и улыбки,
Эффективное лечение зубов и десен, для вашего долгосрочного удовлетворения,
Профессиональная гигиена полости рта, для вашего долгосрочного удовлетворения,
Индивидуальный план лечения для каждого пациента, для вашего здоровья и благополучия
дитяча стоматологічна дитяча стоматологічна .
заказать такси эконом https://zakaz-taxionline.ru/
payday loan store on 87th Loans for fair credit rating are given in secured or unsecured options.
Reducing the cost of attracting job-career.com new customers. You can inexpensively retain existing customers through quality customer service. It’s much cheaper than constantly recruiting new people.
На сайте https://avangardmet.ru вы сможете воспользоваться такими нужными услугами, как: проектирование, обратный инжиниринг, механическая обработка и многое другое. Предприятие ООО “Авангард” успешно развивается, чтобы предложить потребителю только лучшее и прогрессивное. Оно производит, поставляет детали для компаний, связанных с машиностроением, авиационной, медицинской промышленностью. Важной задачей является производство аналогов импортных деталей эталонного качества. Инженеры отличаются высшим образованием.
What’s up to every one, for the reason that I am in fact eager of reading this website’s post to be updated regularly. It carries pleasant stuff.
fastpas.info/
forum.wowcircle.com/member.php?u=584887&tab=activitystream&type=all&page=2
csaladokert.tarsadalmiinnovaciok.hu/forum/topic/zahry-machinery-equipment/?part=21
floriann.ru/buket-roz
vsekruizi.ru/Special_offers/thailand_from_krasnodar/
На сайте https://vavada1v.fun/ пройдите регистрацию для того, чтобы начать играть в казино Вавада. Оно обрадует вас огромным количеством удивительных, разнообразных развлечений, бонусами. А самое главное, что заслуженный выигрыш вы получите сразу же, без задержек. После регистрации для вас открывается удивительный мир ярких эмоций и безграничного количества развлечений, а потому вы точно будете знать, чем заняться сегодня вечером. Заходить сюда можно, в том числе, с мобильного телефона и любого другого гаджета.
Вам интересен вопрос о прокате инвалидных колясок? Деливери плей предоставляет такую возможность. Гарантируем доступные цены и быструю доставку. У нас коляски исключительно чистые. Вы сможете, заказ оплатить тогда, когда убедитесь в том, что коляска находится в отменном состоянии и полностью соответствует вашим требованиям. Ищите аренда инвалидных колясок в москве? Deliveryplay.ru/arenda-invalidnyh-kolyasok – сайт, где можно коляску арендовать. Помимо прочего у нас можно узнать, почему аренда выгоднее приобретения. Мы поможем вам выбрать идеальную коляску, которая вам подойдет, обращайтесь.
It’s remarkable for me to have a web page, which is useful designed for my knowledge. thanks admin
3drus.ru/forum/topic_34713/1
minnesotawildclub.com/read-blog/197_why-is-the-popularity-of-higher-education-declining-in-our-time.html?mode=day%C3%82%C2%A0
bancaanxudoithuong3d.com/category/game-ban-ca-doi-the?filter_by=popular7
n-seo.ru/verstka-shablonov-na-joomla.html/index.html
templateinspire.com/opencart/Lingerie/index.php?route=information/blogger&blogger_id=2
vong lo?i euro 2024
На сайте http://www.tribal-tattoo.ru ознакомьтесь с работами, которые создают искусные, талантливые мастера тату-салона «Tribal». Они сделают тату в самых разных направлениях и независимо от сложности. Все самые интересные, неповторимые и креативные идеи будут в обязательном порядке реализованы. В работе используются только качественные и одноразовые расходные материалы, высокоточное оборудование, которое позволит получить нужный результат. Кроме того, выполняется перекрытие тех работ, которые были исполнены некачественно. При помощи тату получится скорректировать шрамы и рубцы.
Hi there, everything is going nicely here and ofcourse every one is sharing facts, that’s actually excellent, keep up writing.
sp12.ru/com/pristroy/open/59
maixepanphat.vn/author/dangkhoa98/page/2/
local-urban-eats.mn.co/posts/56793349
brandedhoodie.com/sign-up/
http://www.nppremium.com/%E0%B9%80%E0%B8%A7%E0%B9%87%E0%B8%9A%E0%B8%9A%E0%B8%AD%E0%B8%A3%E0%B9%8C%E0%B8%94-100-compare_cialis_levitra.html
cash advance outer loop If your car breaks down unexpectedly, for example, you might find yourself really struggling to finance the repair bill.
Ищете способ расслабиться и получить незабываемые впечатления? Мы https://t.me/intim_tmn72 предлагаем эксклюзивные встречи с привлекательными и профессиональными компаньонками. Конфиденциальность, комфорт и безопасность гарантированы. Позвольте себе наслаждение и отдых в приятной компании.
This is really interesting, You are a very skilled blogger. I’ve joined your feed and look forward to seeking more of your great post. Also, I have shared your web site in my social networks!
russianecuador.com/member.php?tab=visitor_messaging&u=13207&page=20
forumjizni.ru/member.php?u=120588
http://www.mathemlib.ru/
ezoinfo.ru/Narodnay_medizina/Saving_power/Saving_power_9.php
custom-engravable-jewelry.com/bracelet.php
На сайте https://ipoteka.ru/ вы сможете воспользоваться такой услугой, как помощь в оформлении ипотеки, сопровождение различных сделок, которые совершаются с недвижимостью. В компании работают лучшие, компетентные сотрудники, которые дадут консультацию, а также на профессиональном уровне подберут оптимальную программу для оформления ипотеки. Сервис практикует сотрудничество с ведущими банками, а также инвестиционными предприятиями России, а потому есть возможность получить льготу по ипотеке. Только для вас самые лучшие предложения, которыми воспользуйтесь прямо сейчас.
griseofulvin over the counter – griseofulvin 250 mg price gemfibrozil 300mg without prescription
Hi there, I want to subscribe for this webpage to take newest updates, thus where can i do it please assist.
myanmarfootball.org/gallery/displayimage.php?album=lastup&cat=6&pos=0
formlineneedles.com/News/
local-urban-eats.mn.co/posts/56793349
logomotiv.hu/garancia
portugues.ru/forum/album.php?albumid=80&attachmentid=3712
forxiga 10 mg tablet – sinequan 75mg canada precose 50mg price
На сайте https://seobomba.ru/ закажите такую полезную и важную услугу, как продвижение портала вечными ссылками. Такая раскрутка считается одной из самых востребованных в этом году. А для того, чтобы сэкономить финансы, лучше заказать услуги напрямую, без посредничества. Все ссылки проходят детальный отбор, чтобы предложить продукцию эталонного качества. Предлагается гибкая система расценок. Гарантируется прозрачность работ и исключительно с лучшими партнерами, которым точно можно доверять.
Портал uafakty.com.ua его пользователи отмечают лаконичность оформления. Здесь затрагиваются темы культуры, политики, спорта. Вас ждут интересные новости шоу-бизнеса. Наслаждайтесь достойным контентом! uafakty.com.ua – https://uafakty.com.ua сайт, который будет вам понятен, он ценится за оперативность и объективность. Тут вы найдете множество достойной информации, с которой можно уже сейчас ознакомиться. Все статьи удобны для чтения и снабжены фотографиями. Заходите на наш популярный сайт и читайте актуальные новости в любое время!
Желаете приобрести по недорогой стоимости в Донецке гранитный памятник? Каменный двор – компания, которая предлагает качественные услуги. Сотрудники используют новейшее оборудование и технологии, что позволяет точно и оперативно выполнить заказ. https://kamdvor.ru – сайт, где можно подробнее узнать об акциях и скидках. Здесь вы найдете каталог, который можно посмотреть уже сейчас. Мы с уважением относимся к своим клиентам и даем гарантию на лояльные цены на памятники. Свяжитесь с нами, чтобы получить бесплатную консультацию.
Компания «СХТ» предлагает вам приобрести высокоточное измерительное оборудование. Мы гарантируем безупречное качество нашей продукции и привлекательные цены. Специалисты компании обладают приличным опытом работы и высокой квалификацией. Они с радостью готовы проконсультировать вас по интересующим вопросам. https://cxt.su – сайт, где можете прямо сейчас ознакомиться с более подробной информацией о нас и наших услугах. Здесь вы найдете фотогалерею и видео-презентацию. Оперативно реагируем на все заявки. Обращайтесь уже сейчас к нам!
personal loan with low income Unlike a direct lender which lends you the money, a loan aggregator is a middleman – a company that collects your personal and financial information on a loan application and shops it around to lenders who may offer you a loan.
buy generic forxiga – doxepin order online buy generic precose for sale
На сайте https://cliningkrd.ru вы сможете заказать обратный звонок для того, чтобы воспользоваться услугами клининговой компании «Cleaning». Здесь оказываются профессиональные услуги компетентными, проверенными специалистами. В работе применяется инновационное, высокотехнологичное оборудование, которое справляется с загрязнениями различного уровня интенсивности. Бытовая химия, чистящие средства от надежных брендов, которые создают полностью безопасную для людей, животных продукцию.
order griseofulvin 250mg sale – buy fulvicin 250mg sale lopid 300 mg cost
instant loan approval guaranteed Judicial: Judiciary is the branch that works towards implementing and carrying out the laws made by the legislative body.
https://vk.com/kent_bonus
e-mallorca.com
The purpose of MRF hydraulic motors is to 365wyoming.com convert the energy that comes from the fluid flow into mechanical energy that rotates the output shaft. The scope of application of high-torque hydraulic motors MRF is extremely wide. They are used as part of injection molding machines; they are used to operate presses that process plastic. Hydraulic motors are used in woodworking and forging equipment, road equipment, and drilling rigs.
https://aisory.tech – платформа для создания AI Telegram-ботов. Наделяйте своих ботов способностями к естественному диалогу, генерации уникального контента и решению аналитических задач. Простой конструктор платформы делает создание умных чат-ботов доступным для любой компании.
Since the admin of this site is working, no doubt very soon it will be well-known, due to its feature contents.
http://www.kohteht.ru/index.php?links_exchange=yes&page=8&show_all=yes
tivi24h.com/2011/01/xem-bong-online-bong-truc-tuyen-kenh.html
smartwatchcolombia.com/producto/78/smartwatch-serie-8-ultra-11-2023–manilla-de-regalo/7arusak-diploms.com
webnewsrealty.ru/page/13
muscle-bg.com/component/content/article/399-kolko-nasiteni-maznini-trqbva-da-qdem.html
жк купить квартиру от застройщика купить квартиру от застройщика цены
20 Reasons To Believe Text Rewriter Ai Will Never Be Forgotten Ai Word Rewriter
На сайте https://geocarshield.ru у вас получится оформить страховку в Грузию. При этом все манипуляции выполняются в режиме реального времени. Вам не нужно долго стоять в очереди, ожидая своего момента. Оформление происходит всего за 5 минут. Вы сможете получить полис на автомобиль всего в несколько шагов. Оплата происходит любым, наиболее удобным для вас способом! Если появились какие-то вопросы, то вы сможете получить ответы на них, ведь служба поддержки работает круглосуточно! Прямо сейчас оформите страховку на легковой автомобиль, мотоцикл, автобус, прицеп, спецтехнику.
На сайте https://bukmeker.website ознакомьтесь с информацией, которая посвящена букмекерским конторам. Вся она свежая, интересная и актуальная, чтобы вы получили полный ответ на свой вопрос. Этот портал является вашим гидом по ставкам. В последнее время букмекерские конторы заполучили огромную популярность благодаря тому, что позволяют существенно заработать, заполучить деньги на свою мечту. Процесс ставок добавляет адреналина, приятных и положительных эмоций. Перед вами только те конторы, которым действительно стоит доверять.
купить квартиру в казани от застройщика купить квартиру недорого
small personal loans marietta ga Alternative forms of credit may be less expensive and more suitable for your financial needs.
dailywealthy.com
Increasing competitiveness. If customer service usamars.com is thoughtful, then your company will stand out among competitors. People choose those companies that offer a high level of quality service.
купить квартиру в казани новостройка от застройщика жк купить квартиру от застройщика
Dinopolis считается самым забавным онлайн-слотом, дарящий множество позитивных эмоций. Игра не оставляет никого равнодушным, потому как имеет отменную анимацию, звук и графику. Предлагаем вам невероятное путешествие в мир динозавров. У вас есть возможность, играя, зарабатывать реальные деньги. Приготовьтесь к веселью и адреналину. https://dinopolisgame.com/ru/ – сайт, где найдете интересную информацию о данном слоте. Узнаете, как сделать ставку в игре Динополис, сколько можно выиграть. Удачи вам!
На сайте https://kladupechi.ru почитайте всю полезную и важную информацию про печное отопление. Есть данные про голландскую, русскую, финскую печи. На портале опубликованы свежие и содержательные записи на самую разную тему. Все материалы сопровождаются цветными, яркими картинками. Для наглядности изучите видеоматериалы, на которых раскрывается секрет того, как правильно и безошибочно выполнять работы. Имеется видео про каминопечь, мангал барбекю и многое другое. Есть данные про кладку банных печей.
купить квартиру от застройщика https://kvartiru-kupit-kzn.ru
купить квартиру недорого купить квартиру от застройщика
купить квартиру в казани новостройка от застройщика купить квартиру от застройщика
купить квартиру от застройщика цены https://nedvizhimost16.ru
купить квартиру в новостройке от застройщика купить квартиру в казани от застройщика
jsa cash loans Accordingly, some of the above limitations may not apply to you.
купить квартиру от застройщика https://nedvizhimost16.ru
На сайте https://bettingsport.pro/brands/liga-stavok-bukmeker/ ознакомьтесь с актуальной, свежей информацией, которая касается такой популярной БК, как «Лига ставок». Теперь каждый желающий получает возможность не только поддержать любимую команду, но и получить за это финансовое вознаграждение. Компания принимает участие в прогнозах на различные игры, включая виртуальный спорт, а также одиночные поединки. «Лига ставок» представляет собой лицензионную БК, где находится огромное количество видов спорта, матчей.
смотреть аниме атака титанов атака титанов смотреть онлайн бесплатно
generic cialis super active tadalafil 20mg
Выбирайте коляску Cybex для комфорта вашего ребенка, для вашего выбора.
Лучшие оферты на коляски Cybex, для самых взыскательных.
5 причин выбрать именно коляску Cybex для вашего малыша, которые заставят вас влюбиться в этот бренд.
Коляска Cybex: безопасность и стиль в одном флаконе, которые не оставят вас равнодушными.
Коляска Cybex для активных мам и малышей, учитывая все особенности и пожелания.
Как правильно подобрать коляску Cybex для вашей семьи, исходя из индивидуальных потребностей и предпочтений.
Коляска Cybex: высокое качество и стильный дизайн, которые ценят комфорт и безопасность.
Эксклюзивные предложения на коляски Cybex, которые порадуют вас своим разнообразием и качеством.
5 важных критериев при выборе коляски Cybex, для вашего малыша.
Лучшие коляски Cybex для вашего малыша: обзор моделей, чтобы сделать правильный выбор.
Коляска Cybex: стиль, комфорт и безопасность, которые не оставят вас равнодушными.
5 важных критериев при выборе коляски Cybex, которые порадуют вас своим качеством и функционалом.
Лучшие предложения на коляски Cybex для вашего ребенка, которые стоит рассмотреть перед покупкой.
Топ-5 колясок Cybex для вашей семьи, если вы цените качество и комфорт.
Лучшие модели колясок Cybex: подробный обзор, которые ценят надежность и стиль.
Новинки колясок Cybex, которые стоит рассмотреть, перед совершением покупки.
Коляска Cybex: безопасность и комфорт для вашего малыша, исходя из личных предпочтений и потребностей.
Как выбрать идеальную коляску Cybex для вашего малыша: главные моменты, которые не оставят вас равнодушными.
коляска cybex balios s lux коляска cybex balios s lux .
https://b2b-point.io/arcticles/
https://skyhighcondos.ca/kingdom4d
https://b2b-point.io/tips-for-renting-a-house/
fast online cash loans The contributions were uncovered in a tax return filed by Online Consumers Network.
Лучшие модели колясок Cybex на рынке, в магазине.
Лучшие оферты на коляски Cybex, для истинных ценителей качества.
Ключевые преимущества колясок Cybex, которые заставят вас влюбиться в этот бренд.
Коляска Cybex: безопасность и стиль в одном флаконе, которые не оставят вас равнодушными.
Элегантные решения для вашего ребенка – коляски Cybex, учитывая все особенности и пожелания.
Советы по выбору коляски Cybex для вашего малыша, исходя из индивидуальных потребностей и предпочтений.
Коляска Cybex: высокое качество и стильный дизайн, которые ценят комфорт и безопасность.
Топ-модели колясок Cybex на любой вкус и цвет, которые порадуют вас своим разнообразием и качеством.
5 важных критериев при выборе коляски Cybex, для вашего малыша.
Лучшие коляски Cybex для вашего малыша: обзор моделей, чтобы сделать правильный выбор.
Элегантные решения для вашей семьи – коляски Cybex, которые не оставят вас равнодушными.
Как выбрать идеальную коляску Cybex для вашего малыша, которые порадуют вас своим качеством и функционалом.
Как выбрать коляску Cybex: главные моменты, которые стоит рассмотреть перед покупкой.
Почему стоит выбрать именно коляски Cybex, если вы цените качество и комфорт.
Почему коляски Cybex так популярны у родителей, которые ценят надежность и стиль.
Топ-модели колясок Cybex для вашей семьи, перед совершением покупки.
Топ-5 лучших моделей колясок Cybex, исходя из личных предпочтений и потребностей.
Лучшие предложения на коляски Cybex для вашей семьи, которые не оставят вас равнодушными.
прогулочная коляска cybex https://kolyaskicybex.ru/ .
Идеальная коляска Cybex для вашего малыша, новинки.
Лучшие оферты на коляски Cybex, которые порадуют каждого.
5 причин выбрать именно коляску Cybex для вашего малыша, которые заставят вас влюбиться в этот бренд.
Топ-5 моделей колясок Cybex для вашего ребенка, которые не оставят вас равнодушными.
Как выбрать идеальную коляску Cybex для вашей семьи, учитывая все особенности и пожелания.
Советы по выбору коляски Cybex для вашего малыша, исходя из индивидуальных потребностей и предпочтений.
Коляска Cybex: высокое качество и стильный дизайн, которые ценят комфорт и безопасность.
Идеальная коляска Cybex для вашего малыша: как выбрать, которые порадуют вас своим разнообразием и качеством.
Как выбрать коляску Cybex, которая подойдет именно вашему малышу, для вашего малыша.
Лучшие коляски Cybex для вашего малыша: обзор моделей, чтобы сделать правильный выбор.
Топ-модели колясок Cybex для вашего малыша, которые не оставят вас равнодушными.
Как выбрать идеальную коляску Cybex для вашего малыша, которые порадуют вас своим качеством и функционалом.
Как выбрать коляску Cybex: главные моменты, которые стоит рассмотреть перед покупкой.
Топ-5 колясок Cybex для вашей семьи, если вы цените качество и комфорт.
Выбор коляски Cybex для вашего малыша: как не ошибиться, которые ценят надежность и стиль.
Топ-модели колясок Cybex для вашей семьи, перед совершением покупки.
Коляска Cybex: безопасность и комфорт для вашего малыша, исходя из личных предпочтений и потребностей.
Как выбрать идеальную коляску Cybex для вашего малыша: главные моменты, которые не оставят вас равнодушными.
прогулочная коляска cybex прогулочная коляска cybex .
На сайте https://mosgorkabell.ru/ у вас есть возможность сдать кабель на лом в изоляции на персональных условиях. Компания специализируется на скупке проводов и кабелей, электродвигателей и цветного лома, поэтому вам заплатят дорого! Точную стоимость приема кабеля уточните на сайте по телефону. Вы можете посмотреть на сайте фото и видео отчет. Цены на покупку кабелей у нас выгодные, убедитесь в этом лично. Заполните форму на сайте, или отправьте заявку на расчет скупки проводов и кабелей.
Идеальная коляска Cybex для вашего малыша, лучшие предложения.
Лучшие оферты на коляски Cybex, для самых взыскательных.
Почему стоит обратить внимание на коляски Cybex, которые заставят вас влюбиться в этот бренд.
Коляска Cybex: безопасность и стиль в одном флаконе, которые не оставят вас равнодушными.
Коляска Cybex для активных мам и малышей, учитывая все особенности и пожелания.
Как правильно подобрать коляску Cybex для вашей семьи, исходя из индивидуальных потребностей и предпочтений.
Почему коляски Cybex так популярны среди родителей, которые ценят комфорт и безопасность.
Топ-модели колясок Cybex на любой вкус и цвет, которые порадуют вас своим разнообразием и качеством.
5 важных критериев при выборе коляски Cybex, для вашего малыша.
Лучшие коляски Cybex для вашего малыша: обзор моделей, чтобы сделать правильный выбор.
Элегантные решения для вашей семьи – коляски Cybex, которые не оставят вас равнодушными.
5 важных критериев при выборе коляски Cybex, которые порадуют вас своим качеством и функционалом.
Лучшие предложения на коляски Cybex для вашего ребенка, которые стоит рассмотреть перед покупкой.
Почему стоит выбрать именно коляски Cybex, если вы цените качество и комфорт.
Выбор коляски Cybex для вашего малыша: как не ошибиться, которые ценят надежность и стиль.
Как выбрать идеальную коляску Cybex для вашего малыша: подробный гид, перед совершением покупки.
Коляска Cybex: безопасность и комфорт для вашего малыша, исходя из личных предпочтений и потребностей.
Лучшие предложения на коляски Cybex для вашей семьи, которые не оставят вас равнодушными.
коляска cybex коляска cybex .
Glory Casino
Glory Casino
смотреть бесплатно атака титанов атака титанов смотреть онлайн бесплатно
Идеальная коляска Cybex для вашего малыша, в магазине.
Коляска Cybex: комфорт и безопасность в одном, которые порадуют каждого.
Ключевые преимущества колясок Cybex, которые заставят вас влюбиться в этот бренд.
Коляска Cybex: безопасность и стиль в одном флаконе, которые не оставят вас равнодушными.
Коляска Cybex для активных мам и малышей, учитывая все особенности и пожелания.
Как правильно подобрать коляску Cybex для вашей семьи, исходя из индивидуальных потребностей и предпочтений.
Почему коляски Cybex так популярны среди родителей, которые ценят комфорт и безопасность.
Идеальная коляска Cybex для вашего малыша: как выбрать, которые порадуют вас своим разнообразием и качеством.
5 важных критериев при выборе коляски Cybex, для вашего малыша.
Какая коляска Cybex лучше всего подойдет вашей семье?, чтобы сделать правильный выбор.
Коляска Cybex: стиль, комфорт и безопасность, которые не оставят вас равнодушными.
5 важных критериев при выборе коляски Cybex, которые порадуют вас своим качеством и функционалом.
Идеальная коляска Cybex: комфорт и удобство для вашего малыша, которые стоит рассмотреть перед покупкой.
Почему стоит выбрать именно коляски Cybex, если вы цените качество и комфорт.
Почему коляски Cybex так популярны у родителей, которые ценят надежность и стиль.
Новинки колясок Cybex, которые стоит рассмотреть, перед совершением покупки.
Коляска Cybex: безопасность и комфорт для вашего малыша, исходя из личных предпочтений и потребностей.
Лучшие предложения на коляски Cybex для вашей семьи, которые не оставят вас равнодушными.
коляска сайбекс купить https://kolyaskicybex.ru/ .
Выбирайте коляску Cybex для комфорта вашего ребенка, в нашем каталоге.
Коляска Cybex: комфорт и безопасность в одном, для истинных ценителей качества.
Почему стоит обратить внимание на коляски Cybex, которые заставят вас влюбиться в этот бренд.
Идеальный выбор для заботливых родителей – коляски Cybex, которые не оставят вас равнодушными.
Коляска Cybex для активных мам и малышей, учитывая все особенности и пожелания.
Как правильно подобрать коляску Cybex для вашей семьи, исходя из индивидуальных потребностей и предпочтений.
Почему коляски Cybex так популярны среди родителей, которые ценят комфорт и безопасность.
Идеальная коляска Cybex для вашего малыша: как выбрать, которые порадуют вас своим разнообразием и качеством.
Ключевые моменты, на которые стоит обратить внимание при выборе коляски Cybex, для вашего малыша.
Лучшие коляски Cybex для вашего малыша: обзор моделей, чтобы сделать правильный выбор.
Коляска Cybex: стиль, комфорт и безопасность, которые не оставят вас равнодушными.
Лучшие модели колясок Cybex для вашей семьи, которые порадуют вас своим качеством и функционалом.
Идеальная коляска Cybex: комфорт и удобство для вашего малыша, которые стоит рассмотреть перед покупкой.
Почему стоит выбрать именно коляски Cybex, если вы цените качество и комфорт.
Лучшие модели колясок Cybex: подробный обзор, которые ценят надежность и стиль.
Как выбрать идеальную коляску Cybex для вашего малыша: подробный гид, перед совершением покупки.
Топ-5 лучших моделей колясок Cybex, исходя из личных предпочтений и потребностей.
Особенности выбора коляски Cybex: как сделать правильный выбор, которые не оставят вас равнодушными.
купить коляску cybex https://kolyaskicybex.ru/ .
разработка чат ботов telegram
Идеальная коляска Cybex для вашего малыша, новинки.
Лучшие оферты на коляски Cybex, которые порадуют каждого.
Почему стоит обратить внимание на коляски Cybex, которые заставят вас влюбиться в этот бренд.
Топ-5 моделей колясок Cybex для вашего ребенка, которые не оставят вас равнодушными.
Элегантные решения для вашего ребенка – коляски Cybex, учитывая все особенности и пожелания.
Выбирайте коляску Cybex с умом и стилем, исходя из индивидуальных потребностей и предпочтений.
Коляска Cybex: высокое качество и стильный дизайн, которые ценят комфорт и безопасность.
Идеальная коляска Cybex для вашего малыша: как выбрать, которые порадуют вас своим разнообразием и качеством.
Как выбрать коляску Cybex, которая подойдет именно вашему малышу, для вашего малыша.
Выбор коляски Cybex: что важно знать перед покупкой, чтобы сделать правильный выбор.
Коляска Cybex: стиль, комфорт и безопасность, которые не оставят вас равнодушными.
Лучшие модели колясок Cybex для вашей семьи, которые порадуют вас своим качеством и функционалом.
Как выбрать коляску Cybex: главные моменты, которые стоит рассмотреть перед покупкой.
Коляска Cybex для вашего малыша: лучшие модели, если вы цените качество и комфорт.
Почему коляски Cybex так популярны у родителей, которые ценят надежность и стиль.
Как выбрать идеальную коляску Cybex для вашего малыша: подробный гид, перед совершением покупки.
Как выбрать идеальную коляску Cybex для вашей семьи, исходя из личных предпочтений и потребностей.
Как выбрать идеальную коляску Cybex для вашего малыша: главные моменты, которые не оставят вас равнодушными.
прогулочная коляска кубекс прогулочная коляска кубекс .
Идеальная коляска Cybex для вашего малыша, для вашего выбора.
Как выбрать идеальную коляску Cybex для вашего малыша, для истинных ценителей качества.
Почему стоит обратить внимание на коляски Cybex, которые заставят вас влюбиться в этот бренд.
Идеальный выбор для заботливых родителей – коляски Cybex, которые не оставят вас равнодушными.
Элегантные решения для вашего ребенка – коляски Cybex, учитывая все особенности и пожелания.
Как правильно подобрать коляску Cybex для вашей семьи, исходя из индивидуальных потребностей и предпочтений.
Коляска Cybex: высокое качество и стильный дизайн, которые ценят комфорт и безопасность.
Топ-модели колясок Cybex на любой вкус и цвет, которые порадуют вас своим разнообразием и качеством.
5 важных критериев при выборе коляски Cybex, для вашего малыша.
Какая коляска Cybex лучше всего подойдет вашей семье?, чтобы сделать правильный выбор.
Коляска Cybex: стиль, комфорт и безопасность, которые не оставят вас равнодушными.
5 важных критериев при выборе коляски Cybex, которые порадуют вас своим качеством и функционалом.
Лучшие предложения на коляски Cybex для вашего ребенка, которые стоит рассмотреть перед покупкой.
Топ-5 колясок Cybex для вашей семьи, если вы цените качество и комфорт.
Почему коляски Cybex так популярны у родителей, которые ценят надежность и стиль.
Новинки колясок Cybex, которые стоит рассмотреть, перед совершением покупки.
Топ-5 лучших моделей колясок Cybex, исходя из личных предпочтений и потребностей.
Как выбрать идеальную коляску Cybex для вашего малыша: главные моменты, которые не оставят вас равнодушными.
детские коляски кубекс https://kolyaskicybex.ru/ .
telegram нейросеть бот
атака титанов онлайн бесплатно смотреть атака титанов
На сайте https://telegra.ph/Kak-kupit-firmu-s-oborotom-05-15 получите всю важную, ценную и свежую информацию, которая касается покупки предприятия с оборотом. Вы узнаете о том, как приобрести бухгалтерскую компанию. Предоставляется подробная инструкция. Представлена информация, которая касается того, как реализовать ООО без долгов. Имеются и пошаговые инструкции, как приобрести бухгалтерскую компанию и реализовать ООО, если есть один учредитель без долгов. Также есть информация и о том, как правильней реализовать компанию без долгов.
Зайдите на https://tgramcat.com/ где вы найдете каталог телеграмм каналов всевозможных тем и направлений. Каналы тг постоянно пополняются и обновляются, что позволит найти интересное для вас. Каталог тг каналов можно искать по названию или узнать статистику по ним. Телеграмм каналы разбиты по категориям, но можно посмотреть подборку лучших. Вы можете добавить и свой канал.
Идеальная коляска Cybex для вашего малыша, в магазине.
Коляска Cybex: комфорт и безопасность в одном, которые порадуют каждого.
5 причин выбрать именно коляску Cybex для вашего малыша, которые заставят вас влюбиться в этот бренд.
Коляска Cybex: безопасность и стиль в одном флаконе, которые не оставят вас равнодушными.
Как выбрать идеальную коляску Cybex для вашей семьи, учитывая все особенности и пожелания.
Как правильно подобрать коляску Cybex для вашей семьи, исходя из индивидуальных потребностей и предпочтений.
Почему коляски Cybex так популярны среди родителей, которые ценят комфорт и безопасность.
Топ-модели колясок Cybex на любой вкус и цвет, которые порадуют вас своим разнообразием и качеством.
Ключевые моменты, на которые стоит обратить внимание при выборе коляски Cybex, для вашего малыша.
Лучшие коляски Cybex для вашего малыша: обзор моделей, чтобы сделать правильный выбор.
Элегантные решения для вашей семьи – коляски Cybex, которые не оставят вас равнодушными.
Лучшие модели колясок Cybex для вашей семьи, которые порадуют вас своим качеством и функционалом.
Как выбрать коляску Cybex: главные моменты, которые стоит рассмотреть перед покупкой.
Почему стоит выбрать именно коляски Cybex, если вы цените качество и комфорт.
Лучшие модели колясок Cybex: подробный обзор, которые ценят надежность и стиль.
Топ-модели колясок Cybex для вашей семьи, перед совершением покупки.
Топ-5 лучших моделей колясок Cybex, исходя из личных предпочтений и потребностей.
Как выбрать идеальную коляску Cybex для вашего малыша: главные моменты, которые не оставят вас равнодушными.
коляска cybex цена https://kolyaskicybex.ru/ .
Идеальная коляска Cybex для вашего малыша, в магазине.
Лучшие оферты на коляски Cybex, для истинных ценителей качества.
5 причин выбрать именно коляску Cybex для вашего малыша, которые заставят вас влюбиться в этот бренд.
Идеальный выбор для заботливых родителей – коляски Cybex, которые не оставят вас равнодушными.
Элегантные решения для вашего ребенка – коляски Cybex, учитывая все особенности и пожелания.
Как правильно подобрать коляску Cybex для вашей семьи, исходя из индивидуальных потребностей и предпочтений.
Трендовые коляски Cybex для вашего малыша, которые ценят комфорт и безопасность.
Эксклюзивные предложения на коляски Cybex, которые порадуют вас своим разнообразием и качеством.
Как выбрать коляску Cybex, которая подойдет именно вашему малышу, для вашего малыша.
Какая коляска Cybex лучше всего подойдет вашей семье?, чтобы сделать правильный выбор.
Коляска Cybex: стиль, комфорт и безопасность, которые не оставят вас равнодушными.
Как выбрать идеальную коляску Cybex для вашего малыша, которые порадуют вас своим качеством и функционалом.
Лучшие предложения на коляски Cybex для вашего ребенка, которые стоит рассмотреть перед покупкой.
Коляска Cybex для вашего малыша: лучшие модели, если вы цените качество и комфорт.
Почему коляски Cybex так популярны у родителей, которые ценят надежность и стиль.
Новинки колясок Cybex, которые стоит рассмотреть, перед совершением покупки.
Как выбрать идеальную коляску Cybex для вашей семьи, исходя из личных предпочтений и потребностей.
Особенности выбора коляски Cybex: как сделать правильный выбор, которые не оставят вас равнодушными.
коляска cybex balios https://kolyaskicybex.ru/ .
Лучшие модели колясок Cybex на рынке, лучшие предложения.
Лучшие оферты на коляски Cybex, для истинных ценителей качества.
Ключевые преимущества колясок Cybex, которые заставят вас влюбиться в этот бренд.
Топ-5 моделей колясок Cybex для вашего ребенка, которые не оставят вас равнодушными.
Коляска Cybex для активных мам и малышей, учитывая все особенности и пожелания.
Советы по выбору коляски Cybex для вашего малыша, исходя из индивидуальных потребностей и предпочтений.
Коляска Cybex: высокое качество и стильный дизайн, которые ценят комфорт и безопасность.
Топ-модели колясок Cybex на любой вкус и цвет, которые порадуют вас своим разнообразием и качеством.
Ключевые моменты, на которые стоит обратить внимание при выборе коляски Cybex, для вашего малыша.
Выбор коляски Cybex: что важно знать перед покупкой, чтобы сделать правильный выбор.
Топ-модели колясок Cybex для вашего малыша, которые не оставят вас равнодушными.
Как выбрать идеальную коляску Cybex для вашего малыша, которые порадуют вас своим качеством и функционалом.
Идеальная коляска Cybex: комфорт и удобство для вашего малыша, которые стоит рассмотреть перед покупкой.
Коляска Cybex для вашего малыша: лучшие модели, если вы цените качество и комфорт.
Выбор коляски Cybex для вашего малыша: как не ошибиться, которые ценят надежность и стиль.
Топ-модели колясок Cybex для вашей семьи, перед совершением покупки.
Топ-5 лучших моделей колясок Cybex, исходя из личных предпочтений и потребностей.
Особенности выбора коляски Cybex: как сделать правильный выбор, которые не оставят вас равнодушными.
коляска cybex balios коляска cybex balios .
смотреть бесплатно атака титанов https://ataka-titanov-anime.ru
In the game heardle unlimited, you harken to to down snippets of songs and tax to estimate the titles. As you progress, the clips accede to longer to help you cause precise guesses. This regatta blends music trivia with a joy, interactive format, gift endless pastime recompense music enthusiasts.
купить мебель
https://formomebel.ru/stoliki/na-osnovanii-iz-metalla
Meal options range from a hollanderhomes.com choice of hotels without services provided to full board.
personal loans emergency cash If you never have gotten a payday loan before then you will want to talk to a few different lenders to get a better idea of how they work The payment plan should be made clear at the outset of the application process.
Ищете удобный интернет-магазин электрооборудования? Вам поможет надежный партнер ЭлектроМастер, который предоставляет исключительно качественные товары. Мы принимаем оплату за покупки разными способами. Ищете штиль инстаб is550? Sprise.store – сайт, где можете ознакомиться с каталогом и условиями доставки. Стараемся со своими клиентами выстроить длительные отношения, мы их ценим. Если у вас возникли какие-либо вопросы, свяжитесь с нами по телефону, с удовольствием придем вам на помощь. Сэкономим ваши деньги и время. С нетерпением ждем ваших заказов!
livingspainhome.com
аниме атака титанов смотреть атака титанов
купи для дома мебель
https://formomebel.ru/stoliki/na-osnovanii-iz-metalla
https://guardian.ng/news/del-mar-energy-new-horizons-of-development-in-the-sea-of-japan-region/
На сайте https://stroy-m2.ru/ вы сможете приобрести все для стройки, инструмент, профессиональное оборудование, а также все необходимое для обустройства дома, сада. Обязательно ознакомьтесь с предложениями дня, которые позволят вам существенно сэкономить свои финансы. Так у вас получится с хорошей скидкой приобрести все, о чем вы мечтали, включая садовую технику, а также все необходимое для ванной комнаты, организации благородной кухни. А если желаете найти что-то определенное, то воспользуйтесь специальным поиском.
Easy Payments – ваш надежный помощник в запуске бизнеса на международном рынке. Возьмем все задачи на себя, сэкономив время клиента. Мы не применяем сомнительных схем, все наши действия соответствуют международным законам. Гарантируем конфиденциальность данных. Ищете открыть компанию в Англии? Easypayments.online – сайт, где можно подробно ознакомиться с информацией и отзывами о нас. Разбираемся в нюансах регистрации фирм за рубежом, готовы проконсультировать вас совершенно бесплатно по интересующим вопросам. Обращайтесь!
На сайте https://top10-hotel.ru/ представлено огромное количество отелей на самый взыскательный вкус. Они находятся в самых разных городах и странах, чтобы вы устроили себе незабываемое путешествие. Прямо сейчас у вас получится изучить все отели. Перед тем, как принять решение, ознакомьтесь со всем каталогом отелей. Воспользуйтесь специальным каталогом, который подберет решение по рейтингу, отзывам, звездности отеля. Также стоит учесть и параметры отеля, общий рейтинг и многое другое. Установлены самые разные цены.
Не знаете как принимать платежи в криптовалюте онлайн на вашем сайте? Зайдите на https://cryptocloud.plus/ и вы сможете быстро и бесплатно подключиться к нашим продуктам. Посетите сайт, узнайте о решениях и возможностях и всех наших преимуществах. Инструменты для удобной работы с криптовалютой к вашим услугам.
Ищете проверенных букмекеров в России? Мы отобрали букмекерские конторы, которые прекрасно относятся к своим игрокам. Предоставляем для вас к просмотру рейтинг и регулярно в актуальном состоянии его поддерживаем. Ищете отзывы о бк? Bettingsport.pro – портал, где представлена только интересная и полезная информация, посмотреть ее можно в любое удобное время. Наш портал стал незаменимым помощником для любителей ставок на спорт в РФ. Публикуем отзывы клиентов букмекерских контор, рекомендуем их изучить. Комментарии позволят определиться с выбором для ставок.
It is necessary to follow some thespice.net rules and follow recommendations for everything to work out efficiently and safely. You can order the production of metal structures on the website to profitably invest your own money. Let’s consider the basic rules that relate to this process.
online casino no deposit bonus keep what you win gaming bets
На сайте https://ardis-hotel.ru/ забронируйте номер в популярном и уютном отеле «Ардис», который создан для приятного отдыха и изучения достопримечательностей. Прямо сейчас вы сможете забронировать номер на определенную дату. В отеле имеется развитая инфраструктура, а приветливый и дружелюбный персонал поможет с размещением. Все питание готовят исключительно из свежих, отборных продуктов. В меню есть все необходимое. Вас ожидают комфортные и большие номера. Здесь есть возможность отдохнуть с детьми самого разного возраста.
sildenafil vs tadalafil vs vardenafil
На сайте https://split-sistemy-77.ru/ вы сможете приобрести качественные, функциональные, надежные сплит-системы, которые представлены здесь в огромном ассортименте. Они станут идеальным решением для домашнего и офисного использования. А если не можете определиться с выбором, то вам всегда помогут опытные и компетентные специалисты компании. Все устройства представлены проверенными, лучшими производителями. Они дают гарантии на все оборудование. Цель магазина заключается в том, чтобы ваша покупка была как можно приятней и экономически выгодной.
In such a situation, it autonow.net is necessary to dismantle the tiles in the place where the gazebo will stand. Then, as in the previous case, the soil surface is drilled and a profile is installed on which all structures are supported.
what is the best online casino for real money online casino
rkm llc payday loans The one thing they might do for you is negotiate a smaller pay off so that you do not have as much on the back end of your loan.
Сайт https://ru.pocket-option.online/ это возможность торговать бинарными опционами и широкий спектр мировых торговых активов. Посетите сайт, узнайте все преимущества – гибкая торговля, всестороннее обучение, разнообразные торговые инструменты, демо-счет, удобное пополнение и вывод средств, индикаторы и сигналы. Начать торговлю можно в 1 клик. Подробнее на сайте.
Creation of a metal structure yourfloridafamily.com project. It is necessary to ensure that each drawing and basic calculations are correct. Loads, operating conditions of the product, as well as basic safety standards are taken into account.
http://nedvigimost.bbok.ru/viewtopic.php?id=25726#p44438
what online casino has free bonus without deposit? gaming bets
На сайте https://ru.ruka.world/ вы сможете приобрести фрезерное, лазерное оборудование для вашего бизнеса. Преимущества применения лазерных станков – это высокая скорость работы, малые отходы материала и возможность создания сложных узоров. Фрезерные станки приобретите у нас по лояльной стоимости. На все наше оборудование мы предоставляем гарантию. Подробнее ознакомиться с нашими услугами вы можете на сайте. Если у вас возникли вопросы, у нас есть техническая круглосуточная поддержка, обращайтесь, всегда рады вам помочь.
Hello to every , because I am really keen of reading this website’s post to be updated on a regular basis. It contains pleasant stuff.
topstavka.ru/action?page=2
vnbaolut.com/ami
forum.javabox.net/viewtopic.php?f=7&t=14765&view=print
myworldoftank.ru/article/kak-vklyuchit-otobrazhenie-shansov-na-pobedu-xvm-v-world-of-tanks.html
tivi24h.com/2011/01/xem-bong-online-bong-truc-tuyen-kenh.html
голяк куб в кубе https://golyak-serial-online.ru
голяк смотреть кубик https://golyak-serial-online.ru
В питомнике «go Mikheeva Elena» можете купить щенка и обрести преданного друга. Елена Михеева – заводчик японских собак, гарантирует поддержку на протяжении всей жизни малыша и квалифицированную помощь. Ее щенки и собаки растут строго на натуральной еде, так они получают нужные витамины и микроэлементы для крепкого здоровья. https://shibainu-japan.ru – сайт, где можно уже сейчас посмотреть фото. Также здесь есть возможность забронировать щенка Сиба Ину. Он будет дарить вам радость и положительные эмоции.
vardenafil cost
娛樂城官網
娛樂城官網
Вам нужна чистка дымоходов в Ленобласти и в СПБ по высшему качеству? Вам поможет мастер трубочист-печник. В работе он использует исключительно современные технологии. Если вы обратитесь к нему, то получите по доступным ценам квалифицированные услуги. Ищете вызвать трубочиста спб? Трубочист78.рф – сайт, где есть возможность узнать детальную информацию. Трубочист в общении очень приятный, он оперативно справится с работой и оставит все в полном порядке. Мастер ответит на интересующие вопросы. Ваша печь-камин будет снова радовать вас уютом и теплом в доме.
сериал голяк голяк онлайн
Hi! Would you mind if I share your blog with my myspace group? There’s a lot of people that I think would really appreciate your content. Please let me know. Thanks
newspromworld.ru/page/2
floriann.ru/buket-roz
mipon.net/bbs-c/clever.cgi/clever.cgi?page=280
jaezfinancialgroup.icu/pages/contact-us
http://www.automania.by/forum/index.php?showtopic=19046&pid=32742&mode=threaded&show=&st=0
голяк онлайн https://golyak-serial-online.ru
голяк куб в кубе смотреть онлайн https://golyak-serial-online.ru
Посетите сайт GuidesGame https://guidesgame.ru/ и вы найдете коды подарков и бонусов для игр с уникальными наградами для игр на iOS, Android и PC. Вы сможете также узнать гайды для игр и увидеть базу различных игр. Промокоды на игры, коды Roblox и многое другое у нас.
What a stuff of un-ambiguity and preserveness of valuable experience on the topic of unpredicted emotions.
vnbaolut.com/ami
floriann.ru/buket-roz
medicineshocknews.ru/page/7
t99.vn/tap-doan-t99-va-vng-cloud-ky-ket-hop-tac-chien-luoc-toan-dien-ve-tai-chinh-cong-nghe
suamaylanh.com.vn/tin-tuc/40-hang-dien-tu-dien-lanh-ton-nhieu.html
how many payday loans can i get in kansas No. This is a person that does not deserve to be given a loan, does not deserve to be helped when they have no funds to feed their daily needs, does not warrant a green light next to their name when they enquire with their bank if they can have a loan, does not have any means to feed their children when money doesn’t stretch for the month.
I used to be able to find good advice from your blog posts.
http://arusak-attestats24.com
Hello mates, good paragraph and fastidious arguments commented at this place, I am truly enjoying by these.
supplements that have tadalafil
Simply wish to say your article is as astonishing. The clarity on your publish is simply great and i can assume you are an expert in this subject. Well with your permission let me to clutch your RSS feed to keep updated with forthcoming post. Thank you a million and please carry on the gratifying work.
zhaktrans.ru/p40135689-tnvd-wd615-612601080225.html
myfootballday.ru/page/14
allukrnews.ru/put-k-professionalnomu-priznaniyu-pokupka-diploma-kak-reshenie/
http://www.kaktusy.cz/eshop/index.php?links_exchange=yes&page=41&show_all=yes
mazda-demio.ru/forums/index.php?autocom=gallery&req=si&img=4139
Наша компания https://instock-dv.ru/ продаёт товары для дома, строительства, бытовую химию и парфюмерию и еще более 10000 наименований товаров оптом. Сотрудничаем с более чем 100 производителями различных брендов товаров. Мы занимаем лидирующие позиции среди оптовых B2B компаний Дальнего Востока и готовы выходить на новые рынки.
In this perturbation artifice, players forced to navigate a frightening the human race while avoiding the beastly superficial known as siren head. The main unjaundiced of Horn Administrator is survival, requiring players to pour down the drain slyness and cunning to evade capture. With its atmospheric tension and relentless pursuit, the underhand offers a chilling experience.
What’s up i am kavin, its my first occasion to commenting anyplace, when i read this post i thought i could also create comment due to this good piece of writing.
rem-penata.ru/remont/natyazhnyie-potolki
top-estate-soft.ru/funktsional/vygruzka/obzor-platnyh-sajtov-dlya-xml-vygruzki/
gadjetforyou.ru/kupit-diplom-10
77lub.ru/products/small-engine-oils/
ukrevent.ru/page/12/
На сайте https://teletype.in/@registratoria77/kak-kupit-ili-prodat-gotovuu-firmu получите информацию о том, как реализовать или приобрести готовую компанию. Так вы узнаете, как приобрести нулевое ООО по привлекательной стоимости. Также есть информация и о том, как реализовать рабочую компанию с оборотами. Перед вами актуальная и ценная информация, которая ответит на все вопросы. Кроме того, вы будете в курсе того, как приобрести строительную компанию с историей, а также оборотами. Самые исчерпывающие рекомендации.
What Is International SEO Services? What Are The Benefits And How To Make Use Of It Seo Service Uk
Интернет-магазин «CLAPS» предлагает купить прибор DreamStalker Expert. Современный гаджет предназначен для проведения необычных экспериментов в осознанном сне, практик саморазвития и самосовершенствования, преодоления фобий и кошмарных снов. Ищете прибор для осознанных сновидений? Claps.me – сайт, где есть каталог, в нем содержатся характеристики, фотографии и отзывы покупателей. Здесь узнаете, что входит в комплект поставки прибора «DreamStalker Expert».
I loved as much as you’ll receive carried out right here. The sketch is tasteful, your authored material stylish. nonetheless, you command get bought an shakiness over that you wish be delivering the following. unwell unquestionably come more formerly again since exactly the same nearly a lot often inside case you shield this hike.
virusinfo.info/cpstyles/vB/?gde_kupit_diplom_o_srednem_obrazovanii.html
sdo.rea.ru/siteFDO/?executorID=ForumExecutor&mode=showThemes&&cursor=60
night-optics.ru/gallery2/main.php?g2_view=core.DownloadItem&g2_itemId=827
clubecig.fr/blogs/27-qu-est-ce-que-le-sweet-spot.html
girlscools.ru/page/39
step up loans online Average APR rates in Colorado fell from 319 percent to 129 percent and borrowers spent $41.9 million less in 2012 than in 2009, before the changes.
форум вебкам моделей и моделей OnlyFans! Здесь вы найдете полезные советы, поддержку и обсуждения на темы, связанные с работой в вебкам индустрии и на платформе OnlyFans. Присоединяйтесь к нашему сообществу, делитесь опытом и получайте ответы на все ваши вопросы.
https://forum.vipcamclub.ru/
На сайте https://kamdvor.ru/ вы сможете купить гранитный памятник по доступным ценам. Для клиентов постоянно разрабатываются выгодные предложения. Чтобы сэкономить, вы можете воспользоваться скидками и акциями. На сайте ознакомьтесь с готовыми гранитными композициями, для определения с более подходящим вашему вкусу вариантом. На любой заказ мы предоставляем честные цены. Все работы осуществляются оперативно. Предлагаем длительную гарантию на нашу продукцию, обращайтесь.
https://whyworkbook.com/?keyword=asia77
На сайте https://hotel-familyresort.ru/ забронируйте номер в гостеприимном и уютном отеле, где вам всегда рады. В отеле действует развитая инфраструктура, имеется корпус с номерами, а также бассейн, обеденный зал, площадка, а также кафе. Также имеется многое другое для комфортного проживания. Предоставляется концепция «Все включено», чтобы вы отдохнули как нужно. Отель гордится высококлассным уровнем сервиса и гостеприимством. Насладитесь большим выбором высококлассных услуг, интересными развлекательными программами для детей с аниматорами.
На сайте https://filtry-dlya-ochistki-vody-gejzer.ru/ ознакомьтесь с техническими характеристиками фильтров для очистки воды Гейзер. Они сделают так, что в вашем доме всегда будет абсолютно чистая, полностью безопасная вода с безупречными органолептическими свойствами. Фильтры созданы в уникальных, лабораторных условиях, чтобы удовлетворить самые высокие предпочтения клиентов. Устройства обеспечивают безупречную степень очистки. При этом вода не будет слишком жесткой. Продукция реализуется по лучшей стоимости.
Go to the site https://miglandrealestate.com/ and you can find real estate on the island of Bali. Buying, renting land or villas and houses is very simple. We present the best offers at the best prices. We have the latest information about properties in Bali.
Leonbets – казино, заслуживающее внимания. Новичкам букмекерская контора идеально подойдет, поскольку именно с ней проще всего разобраться. Удобное мобильное приложение, множество игр, интересных акций, моментальные выплаты, отзывчивая служба поддержки – это все радует. Ищете leon отзывы? Bettingsport.pro/brands/leon-bukmeker – портал, где предложена интересная информация, посмотрите ее уже сейчас. Чтобы делать ставки в букмекерской конторе Леон, необходимо зарегистрироваться. Удачи вам и крупных выигрышей!
Mob25.com предлагает вам ознакомиться с полезной и интересной информацией. Тут найдете статьи, новости и книги на любые темы. Узнаете, что можно засолить вместо селедки, как с помощью яркой плитки создать шедевры декора, почему француженки не носят Шанель, как сделать школьника отличником. Ищете книги о компьютерах? Mob25.com – сайт, где у вас есть возможность найти каталог книг. У нас научитесь выбирать безопасную косметику и избавитесь от проблем с кожей. Есть поиск, которым можете уже сейчас воспользоваться. Заходите на наш сайт с книгами в любое время!
Slotเว็บตรง – สนุกกับการเล่นได้ทุกอุปกรณ์ที่ใช้งานอินเทอร์เน็ต
ในปัจจุบันนี้ การหมุนสล็อตมีความไม่ยุ่งยากมากยิ่งขึ้น คุณไม่จำเป็นเดินทางไปยังสถานที่เล่นคาสิโนที่ไหน ๆ เพียงแค่มีอุปกรณ์ที่มีความสามารถเชื่อมต่อกับอินเทอร์เน็ต คุณก็สามารถสนุกกับการปั่นสล็อตออนไลน์กับ PG Slot ได้จากทุกที่
การพัฒนาเทคโนโลยีของ PG Slot
ที่ PG Slot เราได้พัฒนาโซลูชั่นสำหรับการจัดการเกมคาสิโนออนไลน์เพื่อตอบสนองความต้องการให้มากที่สุด คุณไม่ต้องติดตั้งแอปพลิเคชันหรือโหลดแอปพลิเคชันใด ๆ ให้น่าเบื่อหรือใช้หน่วยความจำในอุปกรณ์เชื่อมต่อของคุณ การให้บริการเกมสล็อตออนไลน์ของเราใช้งานผ่านเว็บตรงที่ใช้เทคโนโลยี HTML 5 ที่ล้ำสมัย
ปั่นสล็อตได้ทุกอุปกรณ์
คุณสามารถเล่นสล็อตออนไลน์กับ PG Slot ได้อย่างสะดวกเพียงเข้าถึงในเว็บไซต์ของเรา เว็บตรงสล็อตออนไลน์ของเรารองรับทุกซอฟต์แวร์และทุกประเภททั้ง Android และ iOS ไม่ว่าคุณจะใช้สมาร์ทโฟน คอมพิวเตอร์ หรือไอแพดรุ่นไหน ก็มีโอกาสมั่นใจได้ว่าคุณจะเล่นเกมสล็อตออนไลน์ได้อย่างรื่นไหล ไม่มีการขัดข้องหรือสะดุดใด ๆ
ลองเล่นเกมสล็อตฟรี
เว็บตรงของเราเปิดให้บริการเพียงแค่คุณเข้าถึงในเว็บไซต์ของ PG Slot ก็สามารถทดลองเล่นสล็อตฟรีได้ทันที ไม่ต้องเสียค่าใช้จ่ายใด ๆ นี่เป็นโอกาสที่ดีในการเรียนรู้และเรียนรู้เกี่ยวกับเกมก่อนที่จะลงเดิมพันด้วยเงินจริง
การเล่นสล็อตออนไลน์กับ PG Slot ให้คุณสามารถเพลิดเพลินกับการเล่นเกมคาสิโนได้ทุกที่ทุกเวลา ไม่ว่าคุณจะอยู่ที่ไหน เพียงแค่มีเครื่องมือที่เข้าถึงอินเทอร์เน็ต คุณก็อาจสนุกกับการปั่นสล็อตได้อย่างไม่มีข้อผูกมัด!
CVzen è il servizio di scrittura di CV https://cvzen.it/ e career coach per eccellenza per milioni di persone in cerca di lavoro in tutto il mondo. Il nostro team di esperti si impegna per il vostro successo e vi supporterà in tutto il vostro percorso professionale, dalla stesura di un CV professionale e di una lettera di presentazione specifica per il settore, all’ottimizzazione del vostro profilo LinkedIn, fino al career coaching professionale. Sbloccate nuove opportunità con un curriculum che metta in luce il vostro potenziale.
brand dimenhydrinate 50 mg – buy dramamine 50mg online cost actonel 35 mg
На сайте https://uastend.com/messages/novyj-vzglyad-na-kontekstnuyu-reklamu-uastend-com-predlagaet-luchshie-marketingovye-resheniya/ вы сможете ознакомиться с увлекательной, интересной и полезной информацией, которая касается контекстной рекламы. Специально для вас самые эффективные, проверенные и надежные решения для продвижения бизнеса. При этом если вы вложите 100 долларов, то сможете заработать тысячу. Здесь рассматриваются и лучшие места для рекламы. А на первый месяц предоставляется скидка 50%.
https://pinup-oyun.com/ sayt?na daxil olun v? siz mind?n cox muxt?lif slot olan Pin Up onlayn platformas?na apar?lacaqs?n?z. Canl? oyunlar, klassik rulet, kazino, televiziya ?yl?nc?si v? daha cox. Sur?tli qeydiyyat, ayd?n interfeys v? ?la bonus sistemi
of chance and strategy. Unlike traditional casino games, the Aviator Game involves a virtual plane that ascends aviator virtual game
Today, I went to the beach front with my kids. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She placed the shell to her ear and screamed. There was a hermit crab inside and it pinched her ear. She never wants to go back! LoL I know this is totally off topic but I had to tell someone!
lasfloresboutique.ru/product-page/%D0%B1%D1%83%D0%BA%D0%B5%D1%82-%D0%BD%D0%B5%D0%B2%D0%B5%D1%81%D1%82%D1%8B-%D0%B8%D0%B7-%D0%BF%D0%B5%D1%80%D1%81%D0%B8%D0%BA%D0%BE%D0%B2%D1%8B%D1%85-%D1%80%D0%BE%D0%B7-%D0%B8-%D1%84%D1%80%D0%B5%D0%B7%D0%B8%D0%B8
giaibngdaquocteu23.com/2021-10-cb-hay-trong-trong-fifa-online-4-hien-nay-keo8386/
club.sabaylok.com/blogs/1873/Why-is-the-popularity-of-universities-decreasing-all-the-time?lang=tr_tr
ветерантюмгео.рф/galereya/?type_0=gallery&album_gallery_id_0=2
http://www.sitebs.ru/blogs/95000.html
На сайте https://ofisnye-kresla-77.ru/ в большом выборе представлены офисные кресла самых разных расцветок, вариантов, а также модификаций. Все они созданы из качественных, современных и инновационных материалов, которые не утратят своего внешнего вида. Кресла идеально подходят как для установки дома, так и в офисе. С такими изделиями вы будете работать более плодотворно и функциональней. Все конструкции выполнены с учетом эргономических особенностей. Это особенно важно, если планируется долгая работа за столом.
anyone know any good payday loans Medical bills, electricity bills, car bills, school fees are some ends which you can easily fulfil with the help of cash loans.
Посмотреть любимый фильм или же дораму онлайн вместе с близкими и друзьями, даже находясь на расстоянии легко, у нас! Пару кликов, и все что вам нужно для создания своей кинокомнаты + делимся на нее ссылкой с другом! Ищете смотреть по сети с другом? Unotalone.su – сайт, где есть возможность детальнее посмотреть информацию. Время таймлайна видео каждого участника комнаты автоматически ежесекундно синхронизируется с ее владельцем. Кроме того, вы можете сами управлять плеером: ставить на паузу, регулировать громкость, а также качество. Удачного вам просмотра!
https://fieldlineapps.ca/barbar77
enalapril 5mg pills – buy enalapril 5mg generic zovirax buy online
В питомнике «go Mikheeva Elena» вы можете приобрести себе щенка, он будет вам преданным другом. Елена Михеева – заводчик японских собак, гарантирует поддержку на протяжении всей жизни малыша и квалифицированную помощь. Ее собаки и щенки растут исключительно на натуральной еде, так они получают необходимые микроэлементы и витамины для крепкого здоровья. https://shibainu-japan.ru – сайт, где можно уже сейчас посмотреть фото. Также здесь есть возможность забронировать щенка Сиба Ину. Он будет вам дарить позитивные эмоции и радость.
Накрутка подписчиков Инстаграм, Тик Ток, Ютуб, Телеграм, Твиттер
https://www.sq.com.ua/rus/press_release/04.10.2023/kupit-podpiscikov-v-ukraine-vasi-preimushhestva-i-garantii-kakoi-sait-v-etom-pomozet-body
Avtoshini.md предлагает купить шины по наилучшей цене. Мы постоянно обновляем ассортимент, новинки ждут вас. На весь товар предоставляется гарантия. У нас имеется то, что вам нужно. Для осуществления покупки, добавьте товар в корзину. Ищете шины 265/35 r18 в Молдове? Avtoshini.md – сайт, где имеется каталог, в нем представлена продукция известных производителей. При возникновении каких-либо вопросов, воспользуйтесь профессиональной консультацией менеджера. Звоните нам уже сейчас, мы с удовольствием поможем вам с приобретением и оформим заказ.
Summary of Key Points aviator app prediction
enalapril cheap – cheap doxazosin zovirax generic
twin казино
На сайте https://lodochnye-motory-77.ru/ представлены лодочные моторы в огромном выборе. Это позволит отыскать необходимую модель, которая подходит конкретно под ваши нужды. Тем самым вам будет обеспечен комфорт и удобство во время эксплуатации. Каждый товар прошел строгий контроль качества и соответствует самым высоким требованиям по безопасности. Предлагаются привлекательные, доступные расценки, а доставка заказа в самые разные регионы. Выбирая мотор, необходимо ориентироваться на мощность, а также тип топлива и то, какой вес у мотора.
https://drawerbeetle5.werite.net/zaim-pod-mashinu
На сайте https://kamdvor.ru/ вы сможете изучить весь ассортимент памятников, чтобы выбрать наиболее подходящий вариант. Есть возможность заказать такой памятник, который будет выполнен максимально быстро, особенно если нет времени ждать. В компании выполняют и фигурные гранитные надгробья, а также различные мемориальные комплексы. На все товары установлены доступные и привлекательны расценки, чтобы воспользоваться услугой смогли все желающие. Отсутствуют скрытые платежи. При необходимости специалист приедет абсолютно бесплатно.
Накрутка подписчиков Инстаграм, Тик Ток, Ютуб, Телеграм, Твиттер
https://teletap.org/novosti-mira/pravdivyj-vzglyad-na-nakrutku-lajkov-v-soczialnyh-setyah.html
improvements have not only made the game more appealing but also more accessible to a wider audience. aviator game baixar
Компания, специализирующаяся на продаже вилочных погрузчиков Heli https://heli.com.ru/ предлагает широкий ассортимент надежной и высокопроизводительной техники для погрузочно-разгрузочных работ. Heli – ведущий производитель вилочных погрузчиков, известный своим качеством и инновациями. Доверяйте профессионалам – выбирайте Heli для эффективной и безопасной работы на складе!
Space Movers https://spacemovers.ca/ is renowned as the premier moving company in Calgary, Canada, offering unparalleled service and expertise in residential and commercial relocations. Their reputation as the best movers in the city is built on a foundation of reliability, efficiency, and a customer-centric approach that ensures a smooth and stress-free moving experience. Choosing Space Movers means choosing the best in the business, ensuring a seamless transition to your new home or office.
Ищите прочистку канализации в Санкт-Петербурге? Зайдите на https://prochistka.ru/ где вы сможете воспользоваться услугами прочистки канализации, устранения засоров, заказать чистку водоснабжения и другие услуги. Огромный опыт, приятные цены, круглосуточный аварийный выезд. Вызвать сантехника устранить засор легко! Подробнее на сайте.
https://diigo.com/0wkjef
Хотите узнать все самое важное из мира ММА прямо сейчас? Octagon Express предлагает вам главные новости ММА на сегодня! Сенсационные материалы, горячие видео и свежие интервью с бойцами – все это на нашем сайте. Будь в курсе всех событий и не пропусти ни одной детали. Подписывайся на Octagon Express и будь первым, кто узнает все последние новости из мира ММА!
Накрутка подписчиков Инстаграм, Тик Ток, Ютуб, Телеграм, Твиттер
https://www.otzyvua.net/uk/nakrutkamediacom
На сайте https://lan-union.ru предлагается к покупке сетевое и кабельное оборудование. В каталоге компании вы найдете подробное описание, также характеристики продукции и товаров производителя. На сайте вы можете увидеть сертификаты на продукцию, и детальнее ознакомиться с сервисом. Из преимуществ компании, можно отметить быструю логистику, высочайшее качество оборудования и расширенную гарантию. Для того чтобы быть в курсе акций и новостей компании, подпишитесь на рассылку.
娛樂城
富遊娛樂城評價:2024年最新評價
推薦指數 : ★★★★★ ( 5.0/5 )
富遊娛樂城作為目前最受歡迎的博弈網站之一,在台灣擁有最高的註冊人數。
RG富遊以安全、公正、真實和順暢的品牌保證,贏得了廣大玩家的信賴。富遊線上賭場不僅提供了豐富多樣的遊戲種類,還有眾多吸引人的優惠活動。在出金速度方面,獲得無數網紅和網友的高度評價,確保玩家能享有無憂的博弈體驗。
推薦要點
新手首選: 富遊娛樂城,2024年評選首選,提供專為新手打造的豐富教學和獨家優惠。
一存雙收: 首存1000元,立獲1000元獎金,僅需1倍流水,新手友好。
免費體驗: 新玩家享免費體驗金,暢遊各式遊戲,開啟無限可能。
優惠多元: 活動豐富,流水要求低,適合各類型玩家。
玩家首選: 遊戲多樣,服務優質,是新手與老手的最佳賭場選擇。
富遊娛樂城詳情資訊
賭場名稱 : RG富遊
創立時間 : 2019年
賭場類型 : 現金版娛樂城
博弈執照 : 馬爾他牌照(MGA)認證、英屬維爾京群島(BVI)認證、菲律賓(PAGCOR)監督競猜牌照
遊戲類型 : 真人百家樂、運彩投注、電子老虎機、彩票遊戲、棋牌遊戲、捕魚機遊戲
存取速度 : 存款5秒 / 提款3-5分
軟體下載 : 支援APP,IOS、安卓(Android)
線上客服 : 需透過官方LINE
富遊娛樂城優缺點
優點
台灣註冊人數NO.1線上賭場
首儲1000贈1000只需一倍流水
擁有體驗金免費體驗賭場
網紅部落客推薦保證出金線上娛樂城
缺點
需透過客服申請體驗金
富遊娛樂城存取款方式
存款方式
提供四大超商(全家、7-11、萊爾富、ok超商)
虛擬貨幣ustd存款
銀行轉帳(各大銀行皆可)
取款方式
網站內申請提款及可匯款至綁定帳戶
現金1:1出金
富遊娛樂城平台系統
真人百家 — RG真人、DG真人、歐博真人、DB真人(原亞博/PM)、SA真人、OG真人、WM真人
體育投注 — SUPER體育、鑫寶體育、熊貓體育(原亞博/PM)
彩票遊戲 — 富遊彩票、WIN 539
電子遊戲 —RG電子、ZG電子、BNG電子、BWIN電子、RSG電子、GR電子(好路)
棋牌遊戲 —ZG棋牌、亞博棋牌、好路棋牌、博亞棋牌
電競遊戲 — 熊貓體育
捕魚遊戲 —ZG捕魚、RSG捕魚、好路GR捕魚、DB捕魚
cash-out perfectly. tips to play aviator
https://telegra.ph/Zalozhit-avtomobil-06-13
Taker – это казино, которое пользуется невероятной популярностью. Сайт работает без каких-либо сбоев. Здесь представлен широкий выбор азартных игр. Если вы желаете отлично отдохнуть и провести время, советуем обратить свое внимание на Тейкер. Ищете тейкер? Vehrrxcso.ru – портал, предлагающий поиграть в удовольствие и при этом заработать хорошие деньги. Предоставляются щедрые акции и бонусы. Выплаты осуществляются без задержек, а саппорт реагирует на обращение пользователей мгновенно. У Тейкер поклонников очень много, вы точно останетесь довольны работой данного казино.
Many online platforms host competitive tournaments and events for the Aviator Game. These events offer players aviator demo mode
На сайте https://t.me/zaimys вы сможете взять в займы любую сумму. При этом деньги будут выданы в полном объеме на любые нужды. Обратиться сюда смогут даже те, у кого плохая кредитная история. Решение о выдаче средств принимается мгновенно. А потому нужная сумма будет выдана сразу же. Вы сможете потратить ее на свое усмотрение. При этом не нужно предоставлять справки, куда вы потратите деньги. Воспользуйтесь и вы возможностью получить нужную сумму прямо сейчас. Для этого просто оформите заявку, после чего сумма будет переведена на карточку.
https://telegra.ph/Dengi-pod-zalog-avto-pod-pts-06-13
На сайте https://zazhigalki-77.ru/ в большом выборе находятся зажигалки, которые выполнены в традиционном, а также более современном направлении. Сотрудники магазина тщательно контролируют то, какая продукция поступает, чтобы клиенты смогли воспользоваться функциональными и высокотехнологичными решениями высокого качества. При заказе вы сможете ощутить все удобство покупки товаров через сайт, ведь здесь предусмотрен максимально комфортный интерфейс. Выбирайте бензиновые, газовые зажигалки, а также электрические.
На сайте https://romanova-park-hotel.ru/ забронируйте комфортный, уютный номер в парк-отеле «Романова». Вас обрадует безупречный уровень сервиса, приветливый персонал. Кроме того, есть уютные, вместительные и просторные номера – все для того, чтобы устроить яркий, незабываемый отдых. Вы сможете отдохнуть на белоснежном пляже, насладиться архитектурой Крыма, питанием, а также интересными шоу для детей. Ознакомьтесь со всеми номерами в специальном разделе. Установлены привлекательные и умеренные расценки.
В последние годы трейдинг на валютном рынке Форекс https://wilio.uz/ приобрел в Узбекистане огромную популярность. Этому способствует несколько факторов. Во-первых, доступность — для торговли нужен интернет, мобильный телефон и компьютер. То есть трейдинг в Ташкенте и Бухаре – это то же самое, что трейдинг в Самарканде и Намангане. Торговать можно из любой точки в любое время. Во-вторых, возможность заработка — трейдинг на Forex позволяет зарабатывать достаточно денег, чтобы сделать это своей профессией. В-третьих, низкий стартовый капитал — не требуется больших инвестиций, чтобы начать торговать.
https://canvas.instructure.com/eportfolios/2963391/Home/_
Social Elements: Options for multiplayer gameplay and chat features enhance the social experience. aviator game betway
На сайте https://t.me/zaimys вы сможете взять в займы любую сумму. При этом деньги будут выданы в полном объеме на любые нужды. Обратиться сюда смогут даже те, у кого плохая кредитная история. Решение о выдаче средств принимается мгновенно. А потому нужная сумма будет выдана сразу же. Вы сможете потратить ее на свое усмотрение. При этом не нужно предоставлять справки, куда вы потратите деньги. Воспользуйтесь и вы возможностью получить нужную сумму прямо сейчас. Для этого просто оформите заявку, после чего сумма будет переведена на карточку.
https://robincoal4.werite.net/zaim-pod-zalog-pts-bez-avto
Winline – отличная букмекерская контора. Вас порадуют хорошие акции, оперативные выплаты и понятный интерфейс. Приложение без сбоев работает. Менеджеры службы технической поддержки стремятся реагировать оперативно для удовлетворения потребностей игроков. Вы можете разрешить проблемы с выводом денег и пополнением счета. Ищете winline описание бк? Bettingsport.pro/brands/winline-bukmeker – здесь есть полезная информация, посмотрите ее уже сегодня. Проведите интересно свое свободное время. Удачи вам в игре!
Заказать Вентилятор радиальный ВЦ 14-46 по оптовым ценам от завода производителя ООО Гевей можно на сайте https://vent-climate.ru/ Так же производим вентиляторы промышленные радиальные ВР 300-45.
Накрутка подписчиков Инстаграм, Тик Ток, Ютуб, Телеграм, Твиттер
https://donklephant.net/sport/nakrutka-i-sport-kak-prodvigat-sportivnye-meropriyatiya-i-tovary-s-pomoshhyu-nakrutkamedia-com.html
Надежная компания Jetboos организовывает частные перелеты и обеспечивает безопасность для своих клиентов. Предлагаем максимально выгодные цены и обязуемся соблюдать высокие стандарты защиты данных. Всегда готовы проконсультировать вас по любым интересующим вопросам. Ищете аренда частного самолета в москве? Jetboos.com – сайт, где есть возможность оставить заявку уже сегодня. Здесь также можете ознакомиться с отзывами о нас. Вы будете в восторге от сервиса и уровня комфорта. Забронируйте прямо сейчас частный джет. Ваше путешествие будет беззаботным и приятным, доверьтесь нам!
Зайдите на https://freebet-master.info/ и вы сможете получить фрибет за регистрацию, фрибет без депозита, узнать букмекерские конторы с фрибетом, фрибет за регистрацию без депозита, бонусы бк, бонусы букмекерских контор, бонусы букмекеров, фрибет за регистрацию с депозитом, фрибет за регистрацию 2024, бесплатные фрибеты, фрибет за регистрацию, евро 2024, бонусы на евро 2024.
ветклиника минск на карте
На сайте https://www.youtube.com/channel/UCoSPY_dfB7D2iNlMNFMPqEA вы сможете посмотреть различные видеоматериалы, которые носят развлекательный характер. Здесь очень много юмора, интересных сюжетов, которые помогут взглянуть на привычные вещи под другим углом. Все ролики помогут заполучить приятное и положительное настроение, разнообразить досуг. Просматривать их можно на любом устройстве, в том числе, планшете, смартфоне. Все материалы отличного качества и созданные с любовью к своему зрителю.
favorite among online gaming enthusiasts. aviator jeux casino
ветеринарная клиника дзержинск
All these points are important master-stroy.com in the process of manufacturing and installation of metal structures. Pay attention to them so as not to encounter difficulties in the future.
The weight of the parcel ehappynews.com can be up to 20 kg, and its format must correspond to the size of the trunk.
https://canvas.instructure.com/eportfolios/2963379/Home/_
На сайте https://barbekyu-i-grili.ru/ находится большой выбор барбекю, гриля. Перед вами самые интересные и практичные модели, которые помогут приготовить мясо, запечь овощи на гриле. Все оборудование является функциональным, а благодаря разнообразию моделей вы сможете подобрать вариант с учетом предпочтений, требований, материального положения. Все изделия представлены именитыми производителями, отвечающими за качество. Каждая модель детально проверяется на соответствие самым высоким показателям качества.
В питомнике «go Mikheeva Elena» можете купить щенка и обрести преданного друга. Заводчик японских собак Елена Михеева гарантирует своевременную консультацию и поддержку на протяжении всей жизни малыша в любое время и по интересующим вопросам. Ее щенки и собаки растут строго на натуральной еде, так они получают нужные витамины и микроэлементы для крепкого здоровья. https://shibainu-japan.ru – сайт, где можете прямо сейчас посмотреть фото. Также здесь можно забронировать щенка Сиба Ину. Он будет дарить вам радость и положительные эмоции.
Ищете удобный интернет-магазин электрооборудования? ЭлектроМастер – ваш надежный партнер, который предлагает только высококачественные товары. За покупки мы принимаем оплату любыми способами. Ищете энергия ибп гарант-500? Sprise.store – сайт, где вы можете посмотреть условия доставки и каталог. Стараемся со своими клиентами выстроить длительные отношения, мы их ценим. Если у вас возникли какие-либо вопросы, свяжитесь с нами по телефону, с удовольствием придем вам на помощь. Сэкономим ваше время и денежные средства. С нетерпением ждем ваших заказов!
FreeWorldTV.LIVE предоставляет большой выбор по всем миру телеканалов. И это абсолютно бесплатно! Вы можете на любом устройстве, подключенном к интернету смотреть телеканалы, без абонплаты и регистрации. https://freeworldtv.live/ – сайт, где имеется детальная информация, посмотрите ее уже сегодня. Вы познакомитесь с различными языками, традициями, стилями развлечений, будете в курсе мировых новостей и спортивных репортажей. Наслаждайтесь просмотром высококачественных HD-каналов!
https://fingercrack1.werite.net/kredit-s-zalogom-avtomobilia
Technical Specifications aviators game
На сайте https://sprise.store/ вы сможете найти все нужное для обустройства офиса, дома либо производства. Мы предоставляем большой выбор электротоваров от ведущих производителей по выгодной стоимости. Все товары обеспечены гарантией изготовителей и имеют сертификаты качества. Оплата выполняется разными способами, удобными для покупателей. На сайте вы найдете популярные товары и удобный каталог, где сможете выбрать интересующий товар. При возникновении вопросов касаемо выбора товара, позвоните по круглосуточному телефону на сайте.
Накрутка подписчиков Инстаграм, Тик Ток, Ютуб, Телеграм, Твиттер
https://chexov.net/iskusstvo-virusnyh-chellendzhej-pochemu-nakrutka-podpischikov-vazhnyj-shag/
Торговля на Форекс в Узбекистане https://instaforex.uz/ набирает обороты, открывая новые возможности для людей. Трейдинг в Ташкенте, Самарканде и в других городах помогает увеличить доход, защитить сбережения от инфляции и масштабировать финансовые возможности. Однако, будь то трейдинг в Намангане, Андижане или в другом городе, для прибыльной торговли на Forex нужен компьютер, интернет, знания и правильно выбранный брокер.
На сайте https://napolnye-plintusy.ru/ в огромном ассортименте представлены напольные плинтусы. Они станут идеальным решением для декорирования помещения. В каталоге вы найдете: деревянные, пластиковые, металлические плинтусы, а также те, что выполнены из МДФ. Перед вами огромный ассортимент цветовой палитры, а также модификаций. Есть как светлые, так и темные, яркие решения, которые станут яркой деталью стиля. Важным моментом является то, что изделия неприхотливы в уходе и не утратят технических характеристик длительное время.
https://robinknot7.bloggersdelight.dk/2024/06/13/%d0%b7%d0%b0%d0%b9%d0%bc-%d0%bf%d0%be%d0%b4-%d0%bf%d1%82%d1%81/
Ищете способ решить финансовые проблемы? ЗАЙМБОТ вам в этом поможет. Оформление займа займет всего несколько минут. Ищете список мфо россии онлайн? T.me/zaimys – здесь вы найдете актуальную информацию о выгодных займах, кредитах и микрозаймах. Забудьте о длительных очередях, долгосрочных процедурах и бюрократии! Предоставляем людям нужную поддержку в экстренных ситуациях. Делаем процесс займа прозрачным и удобным, заботимся о вашем комфорте. Не нужно на потом откладывать свои планы. Получите денежные средства уже сейчас и реализуйте ваши задумки!
In-Game Bonuses and Rewards how to play aviator game and win
rx care pharmacy orlando fl
Olymp Trade https://olymptrade-app.online/ is an information resource designed to support and educate traders, offering access to a wide range of educational materials such as articles, video tutorials and webinars, as well as advanced analytical tools to help traders make informed decisions.
Бесплатный хостинг картинок и обмен фотографиями для сайтов и блогов https://imgfoto.host/ это легкий способ и бесплатное решение для размещения картинок, скриншотов, фотографий по всему миру. Просто перетащите или вставьте изображение и готово! Можете воспользоваться и нашим API.
На сайте https://xn—-utbcjbgv0e.com.ua/ вы найдете огромное количество компонентов, которые идеально подойдут для мыловарения, производства косметических средств. Здесь опубликовано все, что необходимо для того, чтобы творить и создавать полезную продукцию. Все товары от проверенных, надежных поставщиков, которые дорожат репутацией. При этом удерживаются привлекательные расценки, чтобы вы приобрели все необходимое. Возможны как оптовые, так и розничные продажи. Теперь и вы сможете создать свою качественную, натуральную косметику.
Fair Play Policies and RNG aviator game tips
LEMON CAR – автосервис с хорошей репутацией, который предоставляет услуги по приемлемой стоимости. Здесь трудится компетентная команда мастеров. Они используют только новейшее оборудование и готовы о вашей машине позаботиться. https://lemon-car.ru – сайт, где можно узнать актуальные цены, а также сроки. Клиенты автосервиса высоко оценивают скорость и качество обслуживания. Позвоните нам уже сейчас и мы вас компетентно проконсультируем. С помощью LemonCar ваше авто будет выглядеть ухоженно и надежно работать очень долгое время.
In this iconic fighting courageous, players meet in head-to-head battles, utilizing a roster of characters with lone fighting styles and fatalities. The largest objective in https://mortalkombatplay.com is to outfight opponents in unkind, high-stakes matches, making it a favorite all of a add up to fighting contest enthusiasts.
Вам нужна чистка дымоходов в Ленобласти и в СПБ по высшему качеству? Мастер трубочист-печник готов вам в этом помочь. В работе он применяет только новейшие технологии. Если вы обратитесь к нему, то получите по доступным ценам квалифицированные услуги. Ищете чистка печной трубы? Трубочист78.рф – сайт, где можете узнать более подробную информацию. Трубочист приятный в общении, он быстро справится с задачей, оставив все в идеальном порядке. Мастер ответит на интересующие вопросы. Ваша печь-камин будет снова радовать вас уютом и теплом в доме.
CVzen to najlepsza usługa pisania CV https://cvzen.pl/ i coach kariery dla milionów osób poszukujących pracy na całym świecie. Nasz zespół ekspertów jest zaangażowany w Twój sukces i będzie Cię wspierał przez całą Twoją karierę, od napisania profesjonalnego CV i listu motywacyjnego z uwzględnieniem specyfiki branży, po optymalizację profilu LinkedIn i zapewnienie profesjonalnego coachingu kariery. Odblokuj nowe możliwości dzięki CV, które pokaże Twój potencjał.
Player Reviews and Testimonials aviator game telegram
На сайте https://www.imperiya-hotel.ru/ забронируйте номер в отеле «Империя», где есть все необходимое для организации невероятного путешествия, приятного досуга. Забронируйте номер уже сейчас, чтобы приехать к определенной дате и времени. Для этого необходимо определиться с датой заезда, выезда, количеством гостей. К преимуществам отеля относят то, что он находится на первой линии моря, очень близко находятся культурные объекты, пляж на набережной оборудован всем необходимым. Устройте себе незабываемый отдых.
https://stgeorgesbc.com/?keyword=paito-hk-6d-angkanet
На сайте https://xn--80aimfnww.xn--p1ai/ вы сможете воспользоваться такой популярной услугой, как кадровый аудит. В обязательном порядке будет оценен профессионализм, качество работы сотрудников. Кроме того, подготавливается к проверке ГИТ. Компетентные, лучшие специалисты найдут ошибки, которые были допущены при организации кадрового учета. Будут предложены максимально работающие методики их устранения. У сотрудников огромный опыт работы в данном направлении. Оставьте заявку на оказание услуги прямо сейчас!
2024娛樂城推薦,經過玩家實測結果出爐Top5!
2024娛樂城排名是這五間上榜,玩家尋找娛樂城無非就是要找穩定出金娛樂城,遊戲體驗良好、速度流暢,Ace博評網都幫你整理好了,給予娛樂城新手最佳的指南,不再擔心被黑網娛樂城詐騙!
2024娛樂城簡述
在現代,2024娛樂城數量已經超越以前,面對琳瑯滿目的娛樂城品牌,身為新手的玩家肯定難以辨別哪間好、哪間壞。
好的平台提供穩定的速度與遊戲體驗,穩定的系統與資訊安全可以保障用戶的隱私與資料,不用擔心收到傳票與任何網路威脅,這些線上賭場也提供合理的優惠活動給予玩家。
壞的娛樂城除了會騙取你的金錢之外,也會打著不實的廣告、優惠滿滿,想領卻是一場空!甚至有些平台還沒辦法登入,入口網站也是架設用來騙取新手儲值進他們口袋,這些黑網娛樂城是玩家必須避開的風險!
評測2024娛樂城的標準
Ace這次從網路上找來五位使用過娛樂城資歷2年以上的老玩家,給予他們使用各大娛樂城平台,最終選出Top5,而評選標準為下列這些條件:
以玩家觀點出發,優先考量玩家利益
豐富的遊戲種類與卓越的遊戲體驗
平台的信譽及其安全性措施
客服團隊的回應速度與服務品質
簡便的儲值流程和多樣的存款方法
吸引人的優惠活動方案
前五名娛樂城表格
賭博網站排名 線上賭場 平台特色 玩家實測評價
No.1 富遊娛樂城 遊戲選擇豐富,老玩家優惠多 正面好評
No.2 bet365娛樂城 知名大廠牌,運彩盤口選擇多 介面流暢
No.3 亞博娛樂城 多語言支持,介面簡潔順暢 賽事豐富
No.4 PM娛樂城 撲克牌遊戲豐富,選擇多元 直播順暢
No.5 1xbet娛樂城 直播流暢,安全可靠 佳評如潮
線上娛樂城玩家遊戲體驗評價分享
網友A:娛樂城平台百百款,富遊娛樂城是我3年以來長期使用的娛樂城,別人有的系統他們都有,出金也沒有被卡過,比起那些玩娛樂城還會收到傳票的娛樂城,富遊真的很穩定,值得推薦。
網友B:bet365中文的介面簡約,還有超多體育賽事盤口可以選擇,此外賽事大部分也都有附上直播來源,不必擔心看不到賽事最新狀況,全螢幕還能夠下單,真的超方便!
網友C:富遊娛樂城除了第一次儲值有優惠之外,儲值到一定金額還有好禮五選一,實用又方便,有問題的時候也有客服隨時能夠解答。
網友D:從大陸來台灣工作,沒想到台灣也能玩到亞博體育,這是以前在大陸就有使用的平台,雖然不是簡體字,但使用介面完全沒問題,遊戲流暢、速度比以前使用還更快速。
網友E:看玖壹壹MV發現了PM娛樂城這個大品牌,PM的真人百家樂沒有輸給在澳門實地賭場,甚至根本不用出門,超級方便的啦!
Aw, this was a very good post. Finding the time and actual effort to create a really good article… but what can I say… I hesitate a lot and never seem to get anything done.
musey-uglich.ru
syair hk pangkalantoto
Cash Out: Decide when to cash out to secure your winnings. If you cash out before the plane crashes, you win. If aviator app hack
https://bakerybeetle1.bloggersdelight.dk/2024/06/13/%d0%b7%d0%b0%d0%bb%d0%be%d0%b3-%d0%bf%d0%be%d0%b4-%d0%bf%d1%82%d1%81-%d1%81%d0%bf%d0%b1/
На сайте https://claps.me/catalog/pribory-dlya-osoznannykh-snov/pribor-dlya-osoznannykh-snovideniy-dreamstalker-expert/ у вас есть возможность купить прибор по доступной стоимости для осознанности сновидений. Приобретая на сайте данный прибор, вы его получите непосредственно от производителя и от разработчика, без посредников. Здесь вы найдете подробную информацию о характеристиках прибора, описание и отзывы покупателей. При возникновении вопросов вы можете обратиться на портале в группу технической поддержки.
world-newss.com
womenbabe.com
buy etodolac 600mg sale – buy etodolac 600mg buy pletal 100mg online
Портал о культуре – ваш гид по культурной жизни города. Здесь вы найдёте информацию о театрах, музеях, галереях и исторических достопримечательностях. Откройте для себя яркие события, фестивали и выставки, которые делают Ярославль культурной жемчужиной России.
Online Platforms Offering the Game aviator game free bonus
официальный сайт Dragon Money официальный сайт Dragon Money
Adguard – одно из наилучших решений для блокировки навязчивой рекламы, вредоносных программ и трекеров. Adguard трафик экономит, и возможности просмотра расширяет. Наслаждайтесь быстрым Интернетом без каких-либо раздражающих элементов. https://adsguard.ru/ – сайт, где вы узнаете, зачем необходим блокировщик рекламы. Здесь можно ознакомиться с актуальной стоимостью и почитать отзывы. Преимущества AdGuard: доступность на любой платформе, защита конфиденциальности, родительский контроль. Сделайте свой интернет безопасным!
Hey there I am so excited I found your weblog, I really found you by mistake, while I was researching on Askjeeve for something else, Regardless I am here now and would just like to say cheers for a marvelous post and a all round interesting blog (I also love the theme/design), I don’t have time to read through it all at the moment but I have bookmarked it and also included your RSS feeds, so when I have time I will be back to read more, Please do keep up the great b.
musey-uglich.ru
Ассоциация Безопасности Трейдинга https://trading-association.org/ это помощь в возврате денег от брокера. Зайдите на сайт, ознакомьтесь с ассоциацией, способами решения сложностей с проблемными брокерами или получите консультацию. Подробнее на сайте.
Лига Ставок – букмекерская компания, которая круглосуточно принимает ставки на спорт. Приложение очень удобное, все просто и понятно. Выплаты быстрые, и это радует. При появлении проблем или вопросов можете обратиться к службе поддержки букмекера. Ищете лига ставок букмекерская компания? Bettingsport.pro/brands/liga-stavok-bukmeker – сайт, где имеется занимательная информация, посмотрите ее уже сегодня. Мы обсуждаем важные правила букмекерской конторы «Лига Ставок». Делимся необходимыми знаниями. Вы сможете узнать, как делать ставки в БК и играть.
На сайте https://top-volna.ru воспользуйтесь уникальной возможностью послушать любимую радиостанцию и просто получить отменное настроение от приятно проведенного времени. На этом портале такие радиостанции, как: Маруся ФМ, Русское Радио, Новое Радио, Европа Плюс, DFM, Радио Энерджи, Ретро FM, Юмор FM и многое другое. Прямо сейчас послушайте самые популярные песни, которые нравятся многим. Вас покорит отличное звучание, а также интересная аранжировка, которая точно никого не оставит без внимания.
Вам интересна в Москве компетентная тонировка стекол авто? Готовы помочь вам! Высокое качество нашей работы достигается благодаря использованию сертифицированных материалов и профессионализму сотрудников. Нам можно доверять! http://xn—–6kccgdtutdbkoeocgd0azhek.xn--p1ai/ – сайт, где у вас есть возможность оставить заявку. Мы обязательно свяжемся с вами в ближайшее время и ответим на ваши вопросы. Постоянно проводим акции и гарантируем выгодные цены. Беремся за осуществление заказов разной сложности. Обращайтесь к нам в любое время!
На сайте https://www.parvenik.ru/ представлены веники в большом ассортименте и из самого разного дерева. Есть как дубовые, так и березовые, хвойные, эвкалиптовые. Имеются варианты из липы, клена, травы в пучках и многое другое. Представлены эфирные масла, чаи для бани и многое другое, что необходимо для того, чтобы оздоровить организм, полноценно попариться в бане. Очень часто на сайте проходят акции, действуют скидки. Приобретайте товары со скидками. Перед покупкой обязательно ознакомьтесь с характеристиками.
https://grand-sapphire-blu.com/
Grand Sapphire BLU Resort and Residences. Apartments for sale in Iskele,
Northern Cyprus. New launch by NorthernLand. Secure Your Apartment Today!
В нашем обществе, где диплом – это начало отличной карьеры в любой области, многие стараются найти максимально быстрый путь получения качественного образования. Наличие официального документа переоценить просто невозможно. Ведь диплом открывает двери перед каждым человеком, желающим начать трудовую деятельность или учиться в любом институте.
Предлагаем очень быстро получить любой необходимый документ. Вы имеете возможность заказать диплом, что является удачным решением для человека, который не смог закончить обучение или утратил документ. Каждый диплом изготавливается аккуратно, с максимальным вниманием ко всем элементам. В результате вы получите продукт, 100% соответствующий оригиналу.
Преимущество данного решения заключается не только в том, что можно максимально быстро получить свой диплом. Процесс организован удобно, с профессиональной поддержкой. От выбора необходимого образца документа до правильного заполнения личной информации и доставки по стране — все под абсолютным контролем наших специалистов.
В итоге, для тех, кто ищет быстрый и простой способ получения необходимого документа, наша услуга предлагает отличное решение. Приобрести диплом – значит избежать долгого процесса обучения и сразу переходить к достижению личных целей: к поступлению в университет или к началу успешной карьеры.
http://http://seoyour.ru/
В питомнике «go Mikheeva Elena» можете купить щенка и обрести преданного друга. Елена Михеева – заводчик японских собак, гарантирует поддержку на протяжении всей жизни малыша и квалифицированную помощь. Ее щенки и собаки растут строго на натуральной еде, так они получают нужные витамины и микроэлементы для крепкого здоровья. https://shibainu-japan.ru – сайт, где можете прямо сейчас посмотреть фото. Также здесь можно забронировать щенка Сиба Ину. Он будет вам дарить позитивные эмоции и радость.
На сайте https://kronshtejny-dlya-televizorov.ru/ вы сможете изучить кронштейны для телевизоров, которые представлены здесь в большом выборе. В разделе вы обязательно отыщите подходящее по форме, размеру решение. Есть фиксированные варианты, которые считаются наиболее надежными и практичными. А еще имеются наклонные, потолочные, поворотные. При выборе необходимо учесть размер телевизора, а также его вес. Все конструкции от лучших, проверенных марок, которые отвечают за качество.
Интернет-магазин «CLAPS» предлагает купить прибор DreamStalker Expert. Новейший гаджет необходим для осуществления практик самосовершенствования и саморазвития, преодоления кошмарных снов и фобий, и выполнения необычных экспериментов в осознанном сне. Ищете dream stalker? Claps.me – портал, где имеется каталог для ознакомления, содержатся отзывы покупателей, фотографии и характеристики. Здесь узнаете, что входит в комплект поставки прибора «DreamStalker Expert».
драгон мани казино регистрация драгон мани казино
the thrill of betting and cashing out. Common themes in reviews include the game’s fairness, the enjoyment of aviator app for pc
сайт драгон мани казино бонус драгон мани казино
вход 1go casino 1го казино
The material is cleaned, coated magic-stroy.com with protective agents against rust, and other steps are performed.
Customer service is how well invest24news.com consumers are served at different stages of cooperation with the company. This is the selection of a service or product, the pre-sale support process, service support or warranty assistance. Specialists provide consultations, communication with clients and other services. You can retain those customers who already exist in the company and attract new people.
environment for players to enjoy the game. Some popular platforms include Name], Name], and aviator demon
Hello there! I know this is kinda off topic however , I’d figured I’d ask. Would you be interested in exchanging links or maybe guest writing a blog article or vice-versa? My blog covers a lot of the same topics as yours and I believe we could greatly benefit from each other. If you’re interested feel free to shoot me an e-mail. I look forward to hearing from you! Superb blog by the way!
sanjosesharksclub.com/read-blog/497_where-can-i-buy-a-certificate-or-a-diploma-at-a-bargain-price.html?mode=night
we.riseup.net/wikis/565961
beta.getonvibe.net/blogs/246/Why-is-the-popularity-of-universities-constantly-declining-nowadays
forum.l2star.net/member.php?u=17186
floriann.ru/buket-roz
На сайте https://ocims.ru/ закажите звонок для того, чтобы воспользоваться такой услугой, как строительство каркасных домов высокого качества. Они надежные, практичные, а самое главное, что простоят очень долго. Все работы происходят под ключ. Дома строятся по индивидуальному, а также типовому проекту, что позволит подобрать то, что соответствует предпочтениям, вкусам. На работы, материалы даются гарантии. Действуют привлекательные и доступные расценки. Также компания предлагает приятный презент по окончании проведения работ.
Наши металлические лестницы от производителя https://www.supersvarshik.com/ продуманы, просчитаны на прочность, с удобными ступенями из просечного листа, на которых не задерживается снег, песок или мусор. Ступени из металла и листа ПВЛ являются и прекрасным протектором, нога на них не скользит. Лестницы из металла и листа ПВЛ окрашены в камере порошковой краской – это защищенное и долговечное покрытие для металла. Установка и монтаж уличной металлической лестницы осуществляется на вкрученные в землю металлические сваи, на который методом сварки крепятся блоки из площадки и лестничного марша, Монтаж уличной лестницы из металла проходит очень оперативно, в отличии от других видов лестниц. Спроектируем, изготовим и смонтируем для вас самую правильную лестницу!
На сайте http://nemans.ru вы сможете приобрести всю необходимую продукцию, включая пакеты с ручками, фасовочные пакеты, мешки полипропиленовые, пленку армированную, полиэтиленовую. Также в разделе имеется ветошь, ароматное мыло, перчатки, черенки, бытовая химия, ведра и многое другое, что вы сможете заказать прямо сейчас. Среди рекомендованных товаров находятся вязаные перчатки, туалетная бумага, хозяйственное мыло, неткол. Вся продукция отличного качества, надежная и наделена длительными сроками эксплуатации.
2024娛樂城介紹
台灣2024娛樂城越開越多間,新開的線上賭場層出不窮,每間都以獨家的娛樂城優惠和體驗金來吸引玩家,致力於提供一流的賭博遊戲體驗。以下來介紹這幾間娛樂城網友對他們的真實評價,看看哪些娛樂城上榜了吧!
2024娛樂城排名
2023下半年,各家娛樂城競爭激烈,相繼推出誘人優惠,不論是娛樂城體驗金、反水流水還是首儲禮金,甚至還有娛樂城抽I15手機。以下就是2024年網友推薦的娛樂城排名:
NO.1 富遊娛樂城
NO.2 Bet365台灣
NO.3 DG娛樂城
NO.4 九州娛樂城
NO.5 亞博娛樂城
2024娛樂城推薦
根據2024娛樂城排名,以下將富遊娛樂城、BET365、亞博娛樂城、九州娛樂城、王者娛樂城推薦給大家,包含首儲贈點、免費體驗金、存提款速度、流水等等…
娛樂城遊戲種類
線上娛樂城憑藉其廣泛的遊戲種類,成功滿足了各式各樣玩家的喜好和需求。這些娛樂城遊戲不僅多元化且各具特色,能夠為玩家提供無與倫比的娛樂體驗。下面是一些最受歡迎的娛樂城遊戲類型:
電子老虎機
魔龍傳奇、雷神之鎚、戰神呂布、聚寶財神、鼠來寶、皇家777
真人百家樂
真人視訊百家樂、牛牛、龍虎、炸金花、骰寶、輪盤
電子棋牌
德州撲克、兩人麻將、21點、十三支、妞妞、三公、鬥地主、大老二、牌九
體育下注
世界盃足球賽、NBA、WBC世棒賽、英超、英雄聯盟LOL、特戰英豪
線上彩票
大樂透、539、美國天天樂、香港六合彩、北京賽車
捕魚機遊戲
三仙捕魚、福娃捕魚、招財貓釣魚、西遊降魔、吃我一砲、賓果捕魚
2024娛樂城常見問題
娛樂城是什麼?
娛樂城/線上賭場(現金網)是台灣對於線上賭場的特別稱呼,而且是現金網,大家也許會好奇為什麼不直接叫做線上賭場或是線上博弈就好了。
其實這是有原因的,線上賭場這種東西,架站在台灣是違法的,在早期經營線上博弈被抓的風險非常高所以換了一個打模糊仗的代稱「娛樂城」來規避警方的耳目,畢竟以前沒有Google這種東西,這樣的代稱還是多少有些作用的。
信用版娛樂城是什麼?
信用版娛樂城是一種賭博平台,允許玩家在沒有預先充值的情況下參與遊戲。這種模式類似於信用卡,通常以周結或月結的方式結算遊戲費用。因此,如果玩家無法有效管理自己的投注額,可能會在月底面臨巨大的支付壓力。
娛樂城不出金怎麼辦?
釐清原因,如未違反娛樂城機制,可能是遇上黑網娛樂城,請盡快通報165反詐騙。
how to get monograph without a prescription – order etodolac 600 mg without prescription cilostazol 100 mg pills
1go casino официальный сайт 1го казино
Today, I went to the beach with my children. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put the shell to her ear and screamed. There was a hermit crab inside and it pinched her ear. She never wants to go back! LoL I know this is totally off topic but I had to tell someone!
http://www.redlideres.cl/lider/sergio-rica/
kinogonews.ru/page/5
usaessayexperts.com/faq/
sport-faq.ru/page/4
mymotospeed.ru/page/4
and the player’s goal is to cash out before the plane crashes. This simple yet thrilling concept has made it a aviator game hack download
сайт 1go casino сайт 1go casino
Ищете способ решить финансовые проблемы? ЗАЙМБОТ поможет вам в этом. Оформление займа займет всего несколько минут. Ищете список мфо дающих деньги онлайн? T.me/zaimys – тут вы найдете информацию о кредитах, микрозаймах и выгодных займах. Забудьте о длительных очередях, долгосрочных процедурах и бюрократии! Предоставляем людям нужную поддержку в экстренных ситуациях. Заботимся о вашем комфорте, делаем процесс займа удобным и прозрачным. Не стоит откладывать свои планы на потом. Получите деньги прямо сейчас и воплощайте в реальность свои задумки!
Benefits of Playing Online aviator game demo online
Wow, fantastic blog structure! How lengthy have you ever been blogging for? you made running a blog look easy. The whole look of your website is great, let alone the content!
gerincservdebrecen.hu/informaciok/a-kezeles-menete
myworldoftank.ru/article/kak-vklyuchit-otobrazhenie-shansov-na-pobedu-xvm-v-world-of-tanks.html
http://www.martinsimoveisijui.com.br/blog/nutricosmeticos
vsekruizi.ru/Special_offers/thailand_from_krasnodar/
slcomp.kz/index.php?route=information/blogger&blogger_id=5
zyban online pharmacy
На сайте https://elektrovelosipedy-77.ru/ представлен внушительный выбор электровелосипедов различных марок. Они идеально подойдут тем, кто любит активно отдыхать. Это очень комфортный, удобный способ передвижения, который поможет вам сэкономить много времени. На всю продукцию действуют привлекательные цены, а доставка происходит максимально оперативно. Окончательно определиться с покупкой помогут технические характеристики, которые и влияют на цели покупки. При покупке необходимо полагаться и на емкость батареи.
Посетите сайт https://seovgeo.ru/ где вы сможете заказать продвижение на яндекс картах, продвижение компании в яндекс картах, продвижение организации на яндекс картах, сео продвижение на яндекс картах, продвижение через яндекс карты и многие другие услуги с индивидуальным подходом от профессионалов по выгодным ценам. Подробнее на сайте.
На сайте https://pervomai-172.ru/ цветочный интернет-магазин предлагает доставку прекрасных цветов по выгодным ценам. Вы можете заказать доставку прямо из офиса либо дома, теперь не нужно идти в магазин для выбора цветов. Зайдите в каталог, выберите интересующий вас букет, укажите адрес, время доставки и оплатите заказ. На сайте есть рубрика «Часто задаваемые вопросы», где вы найдете популярные ответы. Также тут имеются отзывы благодарных клиентов, ознакомьтесь с ними уже сейчас.
tadalafil india pharmacy
На сайте https://shalyapin-crimea.ru/ забронируйте номер в пансионате «Дом семейного отдыха «Федор Шаляпин». Он расположен в центре города и обрадует всех желающих приятным уровнем сервиса. Вас ожидает парк аттракционов, а также кинотеатр, городской театр и многое другое, что скрасит досуг. Всю информацию, которая касается услуг, вы отыщите на официальном сайте. Также вас ожидает и охраняемая стоянка. А для того, чтобы иметь представление о пансионате, ознакомьтесь с отзывами, а также зайдите в фотогалерею.
купить квартиру в казани от застройщика квартира в новостройке от застройщика
купить квартиру https://kvartiru-kupit-spb.ru
include welcome bonuses, loyalty rewards, and special promotions that provide additional chances to win and aviator download
The courier needs to pick floridahomz.com up the parcel from the sender and deliver it to the recipient. In case of unforeseen situations, all parcels are insured.
thiswhatido.com
Thank you for sharing your thoughts. I really appreciate your efforts and I will be waiting for your further post thank you once again.
dopul.ru/obzor-interneta/70-chto-takoe-diplom-ob-obrazovanii-zachem-on-nuzhen.html
alcado.com.vn/san-pham-xa-hang
newsbeautiful.ru/page/10/
vague.social/blogs/31670/Why-is-the-popularity-of-universities-rapidly-declining-today
russianecuador.com/member.php?tab=visitor_messaging&u=13207&page=20
На сайте http://koleso-na-hodu.ru каждый желающий получает возможность приобрести шины больших, а также редких размеров с оперативной доставкой по всему городу, области. Непосредственно на сайте у вас получится подобрать шины, исходя из таких параметров, как: ширина, высота профиля, диаметр, стоимость, производитель, сезонность. Вся продукция сертифицированная, качественная, оригинальная. Если остались вопросы, то заполните специальную форму со своими данными, чтобы менеджер перезвонил для уточнения определенных моментов.
цены на квартиры https://novostroyka-kzn16.ru
Social Elements: Options for multiplayer gameplay and chat features enhance the social experience. aviator demo account
купить квартиру в Санкт-Петербурге от застройщика продажа квартир цены
На сайте https://pd-seller.ru получится скачать бесплатно либо приобрести Parallels Desktop 19 для Mac. Предоставляется месячная гарантия возврата денежных средств. Вас ожидает огромное количество различных приложений, которые используются для Windows, торговое, бухгалтерское ПО, КОМПАС и многое другое. Посмотрите видео-презентацию прямо сейчас! При покупке вы получите ключ Windows абсолютно бесплатно. Все лицензии являются официальными. Вы сможете легко приобрести, воспользоваться, продлить и обновить.
Зайдите на сайт https://365-calendar.ru/ и вы сможете узнать все о винограде – виноградарство, сорта винограда, выращивание и уход, а советы и рекомендации опытных виноградарей помогут вам достичь успеха в выращивании виноградных лоз. Вы сможете не только прочитать информацию о сортах винограда и выращивании, но также найти новости из мира виноделия с интересными фактами. Подробнее не сайте.
In https://sites.google.com/view/yandereaigirlfriendsimulator, you’re stuck inside the hospice of an passionate anime catgirl. Your objective is to incline her to unrestricted the disguise door so you can gross away. To whatever manner, be guarded—if you nettle her anger, things could apply dangerous.
Hello colleagues, how is the whole thing, and what you desire to say on the topic of this paragraph, in my view its actually remarkable in support of me.
clubecig.fr/blogs/27-qu-est-ce-que-le-sweet-spot.html
petrovsky-hotel.ru/booking/?arrival-date-offset=1&nights=1&room-type=10945
http://www.leac-escrime.fr/edj-entrainement-des-jeunes-2020-2021/
inspiretemplate.com/opencart/freeze/index.php?route=information/blogger&blogger_id=4
bradfrost.online/speaking
недорогие квартиры от застройщика https://novostroyka-kzn16.ru
nm board of pharmacy tramadol
The manual version must womenup.net be moved by the operator, which may require some effort if the weight of the load exceeds a thousand kilograms. The advantage of this type is its low cost and complete lack of maintenance. However, such a loader will not lift the load to too great a height.
娛樂城
Player台灣線上娛樂城遊戲指南與評測
台灣最佳線上娛樂城遊戲的終極指南!我們提供專業評測,分析熱門老虎機、百家樂、棋牌及其他賭博遊戲。從遊戲規則、策略到選擇最佳娛樂城,我們全方位覆蓋,協助您更安全的遊玩。
layer如何評測:公正與專業的評分標準
在【Player娛樂城遊戲評測網】我們致力於為玩家提供最公正、最專業的娛樂城評測。我們的評測過程涵蓋多個關鍵領域,旨在確保玩家獲得可靠且全面的信息。以下是我們評測娛樂城的主要步驟:
安全與公平性
安全永遠是我們評測的首要標準。我們審查每家娛樂城的執照資訊、監管機構以及使用的隨機數生成器,以確保其遊戲結果的公平性和隨機性。
02.
遊戲品質與多樣性
遊戲的品質和多樣性對於玩家體驗至關重要。我們評估遊戲的圖形、音效、用戶介面和創新性。同時,我們也考量娛樂城提供的遊戲種類,包括老虎機、桌遊、即時遊戲等。
03.
娛樂城優惠與促銷活動
我們仔細審視各種獎勵計劃和促銷活動,包括歡迎獎勵、免費旋轉和忠誠計劃。重要的是,我們也檢查這些優惠的賭注要求和條款條件,以確保它們公平且實用。
04.
客戶支持
優質的客戶支持是娛樂城質量的重要指標。我們評估支持團隊的可用性、響應速度和專業程度。一個好的娛樂城應該提供多種聯繫方式,包括即時聊天、電子郵件和電話支持。
05.
銀行與支付選項
我們檢查娛樂城提供的存款和提款選項,以及相關的處理時間和手續費。多樣化且安全的支付方式對於玩家來說非常重要。
06.
網站易用性、娛樂城APP體驗
一個直觀且易於導航的網站可以顯著提升玩家體驗。我們評估網站的設計、可訪問性和移動兼容性。
07.
玩家評價與反饋
我們考慮真實玩家的評價和反饋。這些資料幫助我們了解娛樂城在實際玩家中的表現。
娛樂城常見問題
娛樂城是什麼?
娛樂城是什麼?娛樂城是台灣對於線上賭場的特別稱呼,線上賭場分為幾種:現金版、信用版、手機娛樂城(娛樂城APP),一般來說,台灣人在稱娛樂城時,是指現金版線上賭場。
線上賭場在別的國家也有別的名稱,美國 – Casino, Gambling、中國 – 线上赌场,娱乐城、日本 – オンラインカジノ、越南 – Nhà cái。
娛樂城會被抓嗎?
在台灣,根據刑法第266條,不論是實體或線上賭博,參與賭博的行為可處最高5萬元罰金。而根據刑法第268條,為賭博提供場所並意圖營利的行為,可能面臨3年以下有期徒刑及最高9萬元罰金。一般賭客若被抓到,通常被視為輕微罪行,原則上不會被判處監禁。
信用版娛樂城是什麼?
信用版娛樂城是一種線上賭博平台,其中的賭博活動不是直接以現金進行交易,而是基於信用系統。在這種模式下,玩家在進行賭博時使用虛擬的信用點數或籌碼,這些點數或籌碼代表了一定的貨幣價值,但實際的金錢交易會在賭博活動結束後進行結算。
現金版娛樂城是什麼?
現金版娛樂城是一種線上博弈平台,其中玩家使用實際的金錢進行賭博活動。玩家需要先存入真實貨幣,這些資金轉化為平台上的遊戲籌碼或信用,用於參與各種賭場遊戲。當玩家贏得賭局時,他們可以將這些籌碼或信用兌換回現金。
娛樂城體驗金是什麼?
娛樂城體驗金是娛樂場所為新客戶提供的一種免費遊玩資金,允許玩家在不需要自己投入任何資金的情況下,可以進行各類遊戲的娛樂城試玩。這種體驗金的數額一般介於100元到1,000元之間,且對於如何使用這些體驗金以達到提款條件,各家娛樂城設有不同的規則。
квартиры от застройщика цены квартиры в новостройках Санкт-Петербурге
На сайте https://climat.best приобретите качественные, функциональные кондиционеры, сплит-системы, тепловые насосы, а также чиллеры. Вся продукция именитых, проверенных и надежных брендов, а потому техника прослужит долго без потери технических характеристик, возможностей. А если необходимо подобрать что-то определенное, то воспользуйтесь специальным поиском. Перед вами есть и самые популярные позиции, которые пользуются особенным спросом среди покупателей. В интернет-магазине вы отыщите как настенные, так и напольно-потолочные конструкции, кассетные.
台灣線上娛樂城
在现代,在线赌场提供了多种便捷的存款和取款方式。对于较大金额的存款,您可以选择中国信托、台中银行、合作金库、台新银行、国泰银行或中华邮政。这些银行提供的服务覆盖金额范围从$1000到$10万,确保您的资金可以安全高效地转入赌场账户。
如果您需要进行较小金额的存款,可以选择通过便利店充值。7-11、全家、莱尔富和OK超商都提供这种服务,适用于金额范围在$1000到$2万之间的充值。通过这些便利店,您可以轻松快捷地完成资金转账,无需担心银行的营业时间或复杂的操作流程。
在进行娱乐场提款时,您可以选择通过各大银行转账或ATM转账。这些方法不仅安全可靠,而且非常方便,适合各种提款需求。最低提款金额为$1000,而上限则没有限制,确保您可以灵活地管理您的资金。
在选择在线赌场时,玩家评价和推荐也是非常重要的。许多IG网红和部落客,如丽莎、穎柔、猫少女日记-Kitty等,都对一些知名的娱乐场给予了高度评价。这些推荐不仅帮助您找到可靠的娱乐场所,还能确保您在游戏中享受到最佳的用户体验。
总体来说,在线赌场通过提供多样化的存款和取款方式,以及得到广泛认可的服务质量,正在不断吸引更多的玩家。无论您选择通过银行还是便利店进行充值,都能体验到快速便捷的操作。同时,通过查看玩家的真实评价和推荐,您也能更有信心地选择合适的娱乐场,享受安全、公正的游戏环境。
Aw, this was an incredibly nice post. Taking a few minutes and actual effort to generate a really good article… but what can I say… I hesitate a lot and never seem to get nearly anything done.
dbecosmeticos.com.br/blog/suplemento-alimentar-hair-supply/montazh-kondicionera-moskva.ru
nfrap.ru/photogallery/964/index.html
petkit.com.cn/member/index.php?uid=ehalipa&action=viewarchives&aid=6644
ufawedding.ru/forum/index.php?action=reminder
http://www.kangas-industrial.com/e_feedback/index.asp?page=2769
Convenience: Play from the comfort of your home or on the go. is aviator a live game
G-Raze компания изготавливает надежные и мощные вездеходы, которые можно купить по лояльной стоимости. Мы те производители, которые после приобретения предлагают консультацию на бесплатной основе. С нами вы в каждой поездке ощутите уверенность и комфорт. Ищете недорогой болотоход вездеход купить? G-raze.ru – сайт, где можно увидеть модельный ряд вездеходов и видеообзор. Привлекательная стоимость, комфорт, высокое качество – вот основные наши преимущества. Если вам наш проект интересен, оставьте заявку, и мы с вами созвонимся. У нас лучшее качество вездеходов. Убедитесь в этом лично.
become more comfortable with the gameplay. Observing patterns and understanding the timing of the plane’s ascent how to win in aviator game
Грузовики HOWO и Sinotruk в наличии и под заказ на https://partnerauto.ru/ от компании ООО «Новая высота» – это возможность выгодно купить китайские грузовики с доставкой в любую точку РФ. Доступные цены и удобный сервис. Подробнее на сайте.
https://emmerechts.com/?keyword=indonesia-vs-irak-u23
That is really interesting, You are a very professional blogger. I have joined your feed and look ahead to in quest of extra of your great post. Also, I have shared your site in my social networks
bietthulideco.vn/biet-thu-nha-vuon-26-nv26-khu-do-thi-lideco-bac-32/
passo.su/forums/index.php?autocom=gallery&req=si&img=2801%C3%82%C2%A0
http://www.agrimoto.fr/achat/cat-piles-170.html
myteana.ru/forums/index.php?autocom=gallery&req=si&img=4490
bensbookmarks.com/author/bensbookmarks/page/2
buy feldene no prescription – feldene 20mg us order exelon online cheap
На сайте https://uss.eu.com изучите интересную, увлекательную и свежую информацию на самую разную тему. Здесь опубликован материал о красивых украшениях. Предлагается ознакомиться с бестселлерами. Также есть данные о том, как правильно увеличить свой охват в Интернете. Имеется полный список компаний, которые пригодятся владельцам предприятий. Обязательно ознакомьтесь со списком лучших форумов, которые представлены в Интернете. Опубликованы и самые лучшие, проверенные англоязычные форумы, на которые вы сможете зайти прямо сейчас.
На сайте http://waltzprof.com закажите обратный звонок с той целью, чтобы ознакомиться с полным ассортиментом, который производит завод ООО “Валцпроф”. Здесь представлен стальной профиль в большом выборе. Изучите технические характеристики фасадной системы, которая создана из нержавеющей, оцинкованной стали. Также в компании получится приобрести и скрытые петли для профильных дверей. Вся продукция создается на высокотехнологичном, инновационном оборудовании. Выпускается только продукция высокого качества и в строго обозначенные сроки.
Online Communities and Forums aviator game pc
На сайте https://g-raze.ru у вас есть возможность приобрести болотоход по доступной стоимости от производителя. Здесь вы найдете большой ассортимент болотоходов в различных городах. Болотоходы отличаются надежностью и высокой проходимостью в самых тяжелых условиях. Также мы обеспечиваем своих клиентов универсальными транспортными средствами передвижения по сложной местности. Модельный ряд представлен на сайте, где можно помимо прочего увидеть видеообзор, также информацию о доставки и оплате.
There is a list of items not worldofwood.net allowed for transportation by courier. Responsibility for violating this rule lies entirely with the sender, because the courier cannot always visually determine the type of item in the parcel.
buy generic piroxicam 20 mg – buy exelon 3mg sale rivastigmine 6mg ca
Доставка цветов и подарков по городу Минску https://sendflowers.by/ Беларуси и миру! Мы предлагаем посетителям доставку роз, букетов цветов, цветочные композиции, дополненные изысканными конфетами, воздушными шарами, яркими открытками, вазами, а также мишками, мягкими игрушками, открытками ручной работы в Минске и во всех городах Беларуси. Международная доставка цветов через партнерскую сеть Telelfora.
https://diigo.com/0wkjjr
квартира в новостройке от застройщика купить квартиру в Санкт-Петербурге от застройщика
Playing the Aviator Game involves a few simple steps: aviator game website
На сайте https://esdogames.ru ознакомьтесь с самыми трендовыми, актуальными и интересными играми, которые точно произведут на вас эффект. Здесь вы найдете все, что вас интересует, включая самые зрелищные игры, которые захватывают с самых первых минут. Также представлен список лучших игр за 2024 год. Вы сможете поиграть во все, что хочется, прямо сейчас. А если вы ищите что-то конкретное, то воспользуйтесь специальным поиском. Подберите игру по жанру, режиму игры, платформе, чтобы облегчить поиск.
I’d like to find out more? I’d love to find out some additional information.
primerosauxilios.org/primeros-auxilios/que-es-y-como-curar-una-herida.php
auto-dealers-script.com/gallery
http://www.as7abe.com/wall/blogs/user/sonnick84?&page=3
containertraffic.ru/news/detail.php?ID=54
mse-online.ru/novosti/vybor-luchshej-shkoly-dlya-vashego-rebenka.html
купить квартиру купить квартиру в Санкт-Петербурге от застройщика
Effective Strategies for Beginners aviator online demo
На сайте https://gamingoff.ru/solutions/limbo-prohozhdenie/ почитайте информацию о платформере, который подходит как для консолей и ПК, так и мобильных телефонов. Вы узнаете о том, как правильно пройти все испытания и забрать приз. Вас ожидают увлекательные, интересные пейзажи, огромное количество головоломок. А на пути будут встречаться монстры, интересные ловушки. Здесь вы найдете информацию о том, как правильно проходить все 39 глав. А если приложение помогло, то обязательно напишите комментарий.
На сайте https://3d-printery-77.ru/ в огромном выборе находятся 3D принтеры, которые идеально подходят для выполнения самых разных задач. Вы всегда сможете воспользоваться профессиональной консультацией, а на всю продукцию предоставляется гарантия качества. Организуется оперативная доставка по стране. Все принтеры представлены именитыми, проверенными и надежными брендами, которые дорожат репутацией. Также есть изделия, которые предназначены для профессионального использования.
Professional care of the premises. Cleaners undergo house-invest.com detailed training, where they learn the combination of different cleaning products with different types of materials.
На сайте https://usiic.co почитайте интересные и увлекательные материалы, посвященные высоким технологиям. Все они написаны экспертами, которые отлично разбираются в таких темах. Есть данные на тему лучших игральных ноутбуков, которые отличаются особой мощностью, производительностью и стильным дизайном. Опубликован список самых эффективных и прогрессивных из них. Есть информация про вечный двигатель, оснащенный магнитами. Вы узнаете про то, как выполнить быстрый и эффективный ремонт мягкой кровли.
квартира в новостройке продажа квартир цены
I got this website from my friend who informed me concerning this website and now this time I am visiting this site and reading very informative articles or reviews here.
kunigami-minibas.jp/userinfo.php?uid=17375
adventure-vinwonders.com/vi/bai-viet-du-lich/an-gi-o-phu-quoc-top-30-dac-san-phu-quoc-cuc-ninh-mieng-du-khach/
muscle-bg.com/component/content/article/399-kolko-nasiteni-maznini-trqbva-da-qdem.html
blog-doma.ru/proizvodstvo-biogumusa
http://www.skitour.su/member.php?u=1002&tab=activitystream&type=all&page=28
Visit https://timespothq.com/ for in-depth reviews, in-depth comparisons, review guides, and expert opinions on the latest productivity software. We’ll help you find the perfect solution for your unique needs. More details on the website.
Каталог эротических рассказов https://vicmin.ru подарит тебе возможность уйти от рутины и погрузиться в мир секса и безудержного наслаждения. Обширная коллекция рассказов для взрослых разбудит твое воображение и принесет немыслимое удовольствие.
cash out before the plane crashes. The objective is to maximize winnings by timing the cash-out perfectly, aviator game logo png
https://diigo.com/0wkjlx
Компания Телефлора https://teleflora.by/ — официальный представитель международной службы доставки цветов и подарков Teleflora в Республике Беларусь! Доставка цветов, подарков, букетов через партнерскую сеть по Минску, пригороду Минска и всем городам Беларуси осуществляется курьером до двери получателя. Только свежие цветы. Бережное отношение к клиентам. Международная доставка цветов!
A good article, say thank you you quest of such painstaking work on the search and processing of information. https://sites.google.com/view/solarsmashinfo Gracious to assume from posts with this approach. I’d like to court your other articles.
What’s up friends, its wonderful paragraph on the topic of teachingand completely defined, keep it up all the time.
dachkanews.ru/page/10/
forexgroupx.ru/page/4
sharypovo.today/news/society/page/9/
dr650.ehehe.net/cgi/bbs/discourse/c_board.cgi?page=0&mode=move&pass=&u_max=&tmpl=
demo.4admins.ru/viewtopic.php?f=10&t=1549&start=0&view=print
Origins of the Aviator Game aviator game parimatch
На сайте https://imperiafohow.by оставьте заявку для того, чтобы воспользоваться услугой массажа. Вы почувствуете заботу о своем теле, полное расслабление и уход. Все массажисты являются компетентными, квалифицированными специалистами с огромным опытом. Все их движения максимально мягкие, приятные и деликатные, а потому вы почувствуете расслабление и негу. Используется косметика популярных, надежных брендов, которые работают на совесть. Но с той целью, чтобы достичь нужных результатов, следует ответственно подходить к оказанию услуги.
plane crashes, making it a game of both luck and timing. This dynamic gameplay keeps players engaged and coming aviator game hack app
На сайте https://zdravbud.net/new/pochemu-bolyat-sustavy изучите увлекательную, интересную и содержательную информацию, которая посвящена тому, почему болят суставы. Так есть информация о том, чем правильно их питать, чтобы сохранили свою эластичность. Описаны признаки того, что суставы заболели. Вы узнаете о том, какими способами и методами их лучше всего и эффективней восстановить. Описаны самые эффективные, точные, а также безопасные из них. А самое главное, что они действительно работают.
На сайте https://moredoram.ru вы найдете дорамы, фильмы, сериалы высокого качества. Они понравятся всем любителям такого жанра и помогут расслабиться после трудового дня и просто получить приятные эмоции. Вы сможете воспользоваться функцией случайной дорамы, изучить список лучших из них. Все они в отличном качестве, с безупречным звуком, что позволит насладиться просмотром на любом устройстве, включая смартфон, ПК, планшет. Регулярно появляются многообещающие новинки, с которыми необходимо ознакомиться и вам.
купить диплом врача https://diplom-izhevsk.ru
Новостройки в Екатеринбурге, купить квартиру в новостройке https://kupit-kvartiruekb.ru от застройщика. Строительство жилой и коммерческой недвижимости. Высокое качество, прозрачность на всех этапах строительства и сделки.
I get pleasure from, cause I found exactly what I was having a look for. You’ve ended my four day lengthy hunt! God Bless you man. Have a nice day. Bye
mormoniconoclast.net/deadpool-movie-review/
sinopipefittings.com/e_Feedback/?page=10995
mutinyhockey.com/memberlist.php?mode=joined&order=ASC&start=336850%C3%82%C2%A0
turbodom.ru/music/instrumentalnaya/?music/instrumentalnaya&letter=%D0%A4/index.html
kinogonews.ru/page/5
Summary of Key Points aviator game online free
Компания ГОСТ-Art предлагает широкий ассортимент текстильных изделий. Гарантируем персональный подход, отменное качество продукции и выгодные цены. Специализируемся на производстве и поставках постельного белья, полотенец, одеял и других товаров. Ищете текстиль для хостела? Gost-art.ru – сайт, где можно прямо сейчас оставить заявку. Мы в ближайшее время вам перезвоним. Ценим своих клиентов и стремимся обеспечить им высокий уровень обслуживания. Сделаем все, чтобы ваш заказ был вовремя доставлен и выполнен, обращайтесь к нам.
5 Reasons To Be An Online SEO Tools Software Business And 5 Reasons Not To
tool For Seo
По поиску бурение скважин в хомутово мы вам обязательно окажем помощь. На данном интернет сайте можно увидеть приблизительную глубину бурения на собственном участке в видео, а также цены. Но самый точный способ — это позвать к себе специалиста для определения лучшего места под скважину, определения объема работы и, в соответствии с этим, цены. Напишите свой номер и мы созвонимся с Вами в ближайшее время.
где можно купить диплом https://diplom-izhevsk.ru
Teleflora Belarus Unit https://flower-shop.by/ offers flower delivery services. The Company operates as an online florist for internet flowers in Minsk, Belarus. Send flowers to Minsk, Belarus and International with us. Business Gifts. Sending flowers online is easy with a wide network of florists to process and deliver your flower order. We take care of all Belarus flower delivery orders, We have a network of florists and flower shops who can deliver flowers as requested by our customers.
Cash Out: Decide when to cash out to secure your winnings. If you cash out before the plane crashes, you win. If aviator game hack software download
ensures compatibility across various platforms without the need for additional software downloads. aviator casino online
На сайте https://cliningkrd.ru вы сможете заказать обратный звонок для того, чтобы воспользоваться услугами клининговой компании «Cleaning». Здесь оказываются профессиональные услуги компетентными, проверенными специалистами. В работе применяется инновационное, высокотехнологичное оборудование, которое справляется с загрязнениями различного уровня интенсивности. Бытовая химия, чистящие средства от надежных брендов, которые создают полностью безопасную для людей, животных продукцию.
https://antheat9.bloggersdelight.dk/2024/06/13/%d0%ba%d1%80%d0%b5%d0%b4%d0%b8%d1%82-%d0%bf%d0%be%d0%b4-%d0%b7%d0%b0%d0%bb%d0%be%d0%b3-%d0%b0%d0%b2%d1%82%d0%be-%d0%b2-%d1%81%d0%bf%d0%b1/
Новые технологии и материалы – достойная компания, которая специализируется на изготовлении для радиотехнической промышленности комплектующих. Предлагаем вам купить крепеж и метизы по самой доступной цене. Внимательно следим за своей продукцией и поставляем ее точно в срок. С радостью окажем вам помощь в оформлении заказа. Ищете электроэрозия? Ntmsp.ru – сайт, где можно уже сейчас ознакомиться с актуальными акциями. У нас трудятся профессиональные и опытные сотрудники. Свяжитесь с нами по телефону, и мы ответим на ваши вопросы.
bimabet slot
of players who enjoy the excitement of this high-flying adventure and see if you have what it takes to time your aviator predictor bot apk
Cериал Голяк https://golyak-serial-online.ru смотреть онлайн в хорошем качестве и с лучшей озвучкой на любых устройствах. Все сезоны истории мелкого преступника Винни и его друзей в английском городке!
สล็อต
สล็อตแมชชีนเว็บตรง: ความรื่นเริงที่ท่านไม่ควรพลาด
การเล่นเกมสล็อตในปัจจุบันนี้ได้รับความนิยมเพิ่มมากขึ้น เนื่องจากความง่ายดายที่นักเดิมพันสามารถใช้งานได้จากทุกที่ทุกเวลา โดยไม่ต้องเสียเวลาในการเดินทางไปยังสถานที่บ่อน ในเนื้อหานี้ เราจะกล่าวถึง “สล็อต” และความสนุกที่คุณจะได้สัมผัสในเกมสล็อตเว็บตรง
ความง่ายดายในการเล่นสล็อต
หนึ่งในเหตุผลสล็อตเว็บตรงเป็นที่สนใจอย่างมาก คือความสะดวกสบายที่ผู้เล่นมี คุณสามารถเล่นสล็อตได้ทุกหนทุกแห่งทุกเวลา ไม่ว่าจะเป็นในบ้าน ในออฟฟิศ หรือแม้กระทั่งในการเดินทาง สิ่งที่จำเป็นต้องมีคือเครื่องมือที่สามารถเชื่อมต่ออินเทอร์เน็ตได้ ไม่ว่าจะเป็นสมาร์ทโฟน แท็บเล็ต หรือโน้ตบุ๊ก
นวัตกรรมกับสล็อตออนไลน์เว็บตรง
การเล่นสล็อตในปัจจุบันนี้ไม่เพียงแต่สะดวกสบาย แต่ยังมีนวัตกรรมใหม่ล่าสุดอีกด้วย สล็อตที่เว็บตรงใช้เทคโนโลยี HTML5 ซึ่งทำให้ท่านไม่ต้องกังวลเกี่ยวกับการลงซอฟต์แวร์หรือแอปพลิเคชันเสริม แค่เปิดเบราว์เซอร์บนอุปกรณ์ของคุณและเข้าสู่เว็บไซต์ คุณก็สามารถเริ่มเล่นได้ทันที
ความหลากหลายของเกมสล็อต
สล็อตออนไลน์เว็บตรงมาพร้อมกับความหลากหลายของเกมของเกมที่เล่นที่ผู้เล่นสามารถเลือกเล่นได้ ไม่ว่าจะเป็นเกมสล็อตแบบคลาสสิกหรือเกมที่มีฟีเจอร์ฟีเจอร์เด็ดและโบนัสเพียบ ท่านจะพบเจอมีเกมที่ให้เล่นมากมาย ซึ่งทำให้ไม่มีวันเบื่อกับการเล่นเกมสล็อต
การรองรับทุกเครื่องมือ
ไม่ว่าผู้เล่นจะใช้สมาร์ทโฟนแอนดรอยด์หรือ iOS ท่านก็สามารถเล่นเกมสล็อตออนไลน์ได้อย่างไม่มีสะดุด เว็บไซต์ของเรารองรับระบบปฏิบัติการและทุกเครื่อง ไม่ว่าจะเป็นสมาร์ทโฟนรุ่นล่าสุดหรือรุ่นเก่าแก่ หรือแม้แต่แท็บเล็ทและโน้ตบุ๊ก คุณก็สามารถเล่นเกมสล็อตได้ได้อย่างครบถ้วน
ทดลองเล่นเกมสล็อต
สำหรับผู้ที่เพิ่งเริ่มต้นกับการเล่นสล็อต หรือยังไม่มั่นใจเกี่ยวกับเกมที่อยากเล่น PG Slot ยังมีบริการทดลองเล่นสล็อตฟรี ผู้เล่นสามารถทดลองเล่นได้ทันทีโดยไม่ต้องสมัครสมาชิกหรือฝากเงิน การทดลองเล่นนี้จะช่วยให้คุณเรียนรู้และเข้าใจวิธีการเล่นได้โดยไม่ต้องเสียค่าใช้จ่าย
โปรโมชันและโบนัส
ข้อดีอีกอย่างหนึ่งของการเล่นสล็อตออนไลน์กับ PG Slot คือมีโปรโมชันและโบนัสมากมายสำหรับสมาชิก ไม่ว่าผู้เล่นจะเป็นผู้เล่นใหม่หรือผู้เล่นเก่า ผู้เล่นสามารถได้รับโปรโมชั่นและโบนัสต่าง ๆ ได้ตลอดเวลา ซึ่งจะเพิ่มโอกาสชนะและเพิ่มความสนุกในเกม
บทสรุป
การเล่นสล็อตที่ PG Slot เป็นการลงทุนที่คุ้มค่า ท่านจะได้รับความเพลิดเพลินและความสะดวกสบายจากการเล่นเกมสล็อต นอกจากนี้ยังมีโอกาสลุ้นรับรางวัลและโบนัสเพียบ ไม่ว่าท่านจะใช้สมาร์ทโฟน แทปเล็ตหรือโน้ตบุ๊กรุ่นใด ก็สามารถเริ่มเล่นกับเราได้ทันที อย่ารอช้า เข้าร่วมและเริ่มเล่นสล็อตออนไลน์ PG Slot ทันที
На сайте https://runobe.ru почитайте ранобэ онлайн и в отличном качестве. Все они на русском языке, а потому насладиться чтением сможет каждый. Все произведения имеют интересный сюжет, непредсказуемую развязку, а потому понравятся всем без исключения. Выбор японских романов обновляется ежедневно, чтобы вы смогли найти то, что действительно вам нравится. Вы можете ознакомиться сразу с несколькими, чтобы определиться с тем, какие из них вам нравятся больше. Для того чтобы подыскать определенный вариант, необходимо воспользоваться специальным поиском.
Мы предлагаем услуги по изготовлению и монтажу металлоконструкций в Воронеже https://specstroy36.ru/ и Воронежской области. Команда профессиональных специалистов готова выполнить проект любой сложности и размера. Мы работаем с различными типами металла, чтобы удовлетворить все потребности клиентов. Наше оборудование высокотехнологично и позволяет точно выполнять все металлообрабатывающие операции. СпецСтрой36 гарантирует высокое качество продукции, долговечность и надежность конструкций. Вы сможете получить индивидуальный подход и решение, которое соответствует вашим требованиям и бюджету. Свяжитесь с нами, чтобы обсудить ваши потребности и получить бесплатную консультацию. Специалисты компании всегда готовы помочь воплотить любой проект с использованием металлоконструкций.
Online casino games have surged in popularity due to their convenience and the immersive experience they offer. aviator game bot
ทดลองดำเนินการเล่นสล็อต และค้นพบประสบการณ์การเล่นเกมที่ไม่เหมือนใคร!
สำหรับนักพนันที่กำลังมองหาความบันเทิงและโอกาสในการคว้ารางวัลมหาศาล สล็อตออนไลน์เป็นอีกหนึ่งทางเลือกที่ที่คุ้มค่าใช้.ด้วยความจำนวนมากของเกมสล็อตที่น่าตื่นเต้น ผู้เล่นสามารถทดลองเล่นและค้นหาเกมที่ต้องการได้อย่างง่ายดาย.
ไม่ว่าคุณจะชอบเกมสล็อตคลาสสิกหรือต้องการความท้าทายใหม่, ทางเลือกรอกลับมาให้คุณสัมผัส. จากสล็อตที่มีหัวข้อมากมาย ไปจนถึงเกมที่มีลักษณะพิเศษและเงินรางวัล, ผู้เล่นจะได้พบกับการเล่นเกมที่น่าตื่นเต้นและน่าติดตาม.
ด้วยการทดลองเล่นสล็อตฟรี, คุณสามารถปฏิบัติวิธีการเล่นและค้นหากลยุทธ์ที่ถูกใจก่อนลงทุนด้วยเงินจริง. นี่คือโอกาสสำคัญที่จะศึกษากับเกมและยกระดับโอกาสในการแสดงรางวัลใหญ่.
อย่าเลื่อนเวลา, ร่วมกับการทดลองเล่นสล็อตออนไลน์วันนี้ และค้นพบประสบการณ์การเล่นเกมที่ไม่เหมือนใคร! เพลิดเพลินกับความน่าสนใจ, ความยินดี และโอกาสชนะรางวัลใหญ่. กล้าก้าวไปเดินทางสู่ความสำเร็จลุล่วงของคุณในวงการสล็อตออนไลน์แล้ววันนี้!
Радіо П’ятниця – це чудова музика та гарний настрій! Слухати Радіо П’ятниця можна завжди і всюди. Вмикайте Радіо П’ятниця онлайн та насолоджуйтесь улюбленими хітами. Радіо П’ятниця дарує радість кожного дня. https://www.asiacheat.com/bbs/board.php?bo_table=free&wr_id=34648
ทดสอบ ใช้งาน สล็อต PG ควบคู่กับ เข้าถึง ไปยัง ภพ แห่ง ความเพลิดเพลิน ที่ ไร้ขีดจำกัด
ต่อ นักเสี่ยงโชค ที่ คิดค้น มองหา ความรู้สึก เกมที่แตกต่าง, สล็อต PG ถือเป็น ตัวเลือกที่ ที่ น่าสนใจ เป็นอย่างมาก. อันเนื่องมาจาก ความหลากหลายของ ของ ตัวเกมสล็อต ที่ น่าติดตาม และ น่าค้นหา, นักเล่นเกม จะได้ ทดสอบ และ ลอง รูปแบบเกม ที่ เหมาะกับ แบบอย่างการเล่น ของตนเอง.
แม้ว่า ผู้เล่น จะต้องการ ความผ่อนคลาย แบบเดิม หรือ การท้าทาย ที่แตกต่าง, สล็อต PG จะมี ให้เลือกอย่างมากมาย. ตั้งแต่ สล็อตรูปแบบคลาสสิค ที่ คุ้นเคย ไปจนถึง ตัวเกม ที่ ให้ ฟังก์ชันพิเศษ และ โบนัสล้นหลาม, ผู้เล่น จะสามารถ ได้ทดลอง การเล่น ที่ ตื่นเต้น และ ตื่นเต้น
เนื่องจาก การลองเล่น สล็อต PG โดยไม่เสียค่าใช้จ่าย, ผู้เล่น สามารถ ทำความเข้าใจ กระบวนการเล่น และ ทดลอง เคล็ดลับ ต่างๆ ก่อน เริ่มลงเดิมพัน ด้วยเงินทุน. นี่ ถือเป็น โอกาส ที่ยอดเยี่ยม ที่จะ ปรับตัว และ ยกระดับ ความน่าจะเป็น ในการ คว้ารางวัล รางวัลใหญ่.
อย่าเนิ่นช้า, เข้าถึง ใน การเล่นทดลอง สล็อต PG เดี๋ยวนี้ และ ลองใช้ การเล่น ที่ ไม่มีขอบเขต! รับรู้ ความดึงดูดใจ, ความเพลิดเพลิน และ ช่องทาง ในการ ได้รับรางวัล มหายิ่ง. เริ่มต้น พัฒนา สู่ ความสำเร็จ ของคุณในวงการ การพนันสล็อต เดี๋ยวนี้!
เรื่อง ไซต์ PG Slots พวกเขา มี ข้อได้เปรียบ หลายประการ แตกต่างจาก คาสิโนแบบ เก่า, โดยมาก ใน ยุคสมัยใหม่. คุณประโยชน์สำคัญ เหล่านี้ ได้แก่:
ความง่ายสะดวก: ผู้เล่น สามารถเข้าถึง สล็อตออนไลน์ได้ ตลอดเวลา จาก ทุกอย่าง, ให้ ผู้เล่นสามารถ ทดลอง ได้ ทุกแห่ง ไม่ต้อง เสียเวลา ไปคาสิโนแบบ ดั้งเดิม ๆ
เกมมากมายแตกต่าง: สล็อตออนไลน์ ให้ เกม ที่ หลากหลาย, เช่น สล็อตประเภทคลาสสิค หรือ ตัวเกม ที่มี ความสามารถ และประโยชน์ พิเศษ, ไม่ทำ ความเหงา ในเกม
แคมเปญส่งเสริมการขาย และค่าตอบแทน: สล็อตออนไลน์ ส่วนใหญ่ มี ข้อเสนอส่งเสริมการขาย และโบนัส เพื่อยกระดับ ความเป็นไปได้ ในการ ชนะ และ ส่งเสริม ความเพลิดเพลิน ให้กับเกม
ความเชื่อมั่น และ ความน่าเชื่อถือ: สล็อตออนไลน์ แทบจะ ใช้งาน ระบบรักษาความปลอดภัย ที่ เหมาะสม, และ พึ่งพาได้ ว่า ข้อมูลลับ และ การเงิน จะได้รับ คุ้มครอง
บริการสนับสนุน: PG Slots ว่าจ้าง ทีมงาน ที่มีความเชี่ยวชาญ ที่ตั้งใจ ดูแล ตลอดเวลาไม่หยุด
การเล่นบนอุปกรณ์เคลื่อนที่: สล็อต PG อนุญาต การเล่นบนโทรศัพท์, ให้ ผู้เล่นสามารถเข้าร่วม ตลอด 24 ชั่วโมง
ทดลองเล่นโดยไม่เสียค่าใช้จ่าย: สำหรับ ผู้เล่นที่เพิ่งเริ่ม, PG ยังให้บริการ เล่นฟรี อีกที่, เพื่อ ผู้เล่น เรียนรู้ วิธีใช้ และทราบ เกมก่อน เล่นด้วยเงินจริง
สล็อต PG มีคุณสมบัติ ประโยชน์ เป็นจำนวนมาก ที่ ก่อให้เกิด ให้ได้รับความนิยม ในยุคปัจจุบัน, ช่วย ความรู้สึก ความบันเทิง ให้กับเกมด้วย.
ensures compatibility across various platforms without the need for additional software downloads. aviator game tickets
По поиску бурение на воду иркутск мы вам непременно поможем. На данном интернет сайте можно узнать примерную глубину бурения на собственном участке в видео, а также стоимость. Но самый безупречный способ — это пригласить к себе специалиста для выявления верного участка под скважину, понятие объема работы и, в соответствии с этим, стоимость. Оставьте контактный номер телефона и мы свяжемся с Вами в скорое время.
Adguard – одно из наилучших решений для блокировки навязчивой рекламы, вредоносных программ и трекеров. Adguard трафик экономит, и возможности просмотра расширяет. Наслаждайтесь быстрым Интернетом без каких-либо раздражающих элементов. https://adsguard.ru/ – сайт, где вы узнаете, зачем необходим блокировщик рекламы. Здесь можно прочитать отзывы и ознакомиться с актуальными ценами. Достоинства AdGuard: защита конфиденциальности, родительский контроль, доступность на любой платформе. Сделайте свой интернет безопасным!
Драгон Мани Казино https://krpb.ru – ваше место для азартных приключений! Наслаждайтесь широким выбором игр, щедрыми бонусами и захватывающими турнирами. Безопасность и честная игра гарантированы. Присоединяйтесь к нам и испытайте удачу в самом захватывающем онлайн-казино!
Ensuring Safe Gaming Practices how to download aviator game app
https://selfgrowth.com/articles/find-quickly-and-profitably-with-i-teka-search-for-medicines-in-kazakhstan
На сайте https://setevoj-kabel.ru/ в большом многообразии находятся сетевые кабели. Они отлично подходят для самых разных целей. Они обеспечат качественное, надежное подключение, а потому необходимы везде. В магазине вы отыщите варианты самых разных типов и только от проверенных, лучших брендов. При выборе необходимо учитывать то, для каких целей будет использоваться кабель и в каких условиях. Также на покупку влияют и такие моменты: длина кабеля, уровень экранирования и другие нюансы. Вы всегда сможете воспользоваться консультацией специалиста.
Приобрести сколько стоит пробурить скважину для воды можно на веб портале мастер-буров.рф прямо сейчас. Скважина с чистой водой — один из главных деталей на Вашем участке. Мы даем гарантию на качество работы, материалов, а также осуществляем сервисное обслуживание. Внешние факторы могут негативно влиять на скважину и качество воды, мы также работаем с восстановлением скважин от деформации и с очищением от заиливания. Звоните, пишите, будем рады с Вами работать.
Several key developers and companies have played a significant role in the development and success of the aviator demo game play
Famous French footballer Kylian Mbappe https://kylianmbappe.prostoprosport-ar.com has become a global ambassador for Dior. The athlete will represent the men’s collections of creative director Kim Jones and the Sauvage fragrance, writes WWD. Mbappe’s appointment follows on from the start of the fashion house’s collaboration with the Paris Saint-Germain football club. Previously, Jones created a uniform for the team where Kylian is a player.
Visit the website https://www.sparklo.com/ – this is a unique offer for recycling garbage and waste. Our reversible vending machines or spark machines can turn your trash into treasure. Making recycling fun produces proven results! This is a solution from the future! More details on the website.
На сайте https://turk-kino.ru посмотрите интересное и запоминающееся турецкое кино вместе с другом. Есть такие именитые картины, как «Запах клубники», «Зимородок», «Великолепный век» и многое другое. Для того чтобы начать совместный просмотр, необходимо создать комнату. Сделать это получится в 3 шага, а инструкция прилагается. Перед вами многообещающие новинки, а также топ лучших фильмов за 2024 год. Во всех фильмах играют ваши любимые актеры, звучит приятная музыка. Есть подборка рекомендованных фильмов, которые выбирают многие.
Working as a courier is userhomes.com suitable for everyone, thanks to the ability to work on foot, by bicycle, by scooter or by car.
excitement it brings to the table. Jeetkhel Aviator
Cash Out: Decide when to cash out to secure your winnings. If you cash out before the plane crashes, you win. If aviator game prediction hack
social interaction adds a new layer of excitement and competition to the game, making it more engaging and aviator conta demo
Исламский информационный портал https://naistine.ru/ рассказывающий о религии Ислам. На сайте вы найдете ценные советы, различные молитвы, аяты и суры из Корана, а так же достоверные хадисы.
Why No One Cares About Local Search SEO local seo company
Competitive Tournaments and Events aviator app free download
สล็อตเว็บตรง — สามารถใช้ มือถือ แท็บเลต คอมฯ ฯลฯ สำหรับการเล่น
ระบบสล็อตเว็บตรง ของ PG Slot ได้รับการพัฒนาและปรับแต่ง เพื่อให้ รองรับการใช้ บนอุปกรณ์ที่หลากหลายได้อย่าง ครบถ้วน ไม่สำคัญว่าจะใช้ โทรศัพท์มือถือ แท็บเล็ต หรือ คอมพิวเตอร์ส่วนตัว รุ่นไหน
ที่ PG เราเข้าใจว่าผู้เล่นต้องการ ของลูกค้า ในเรื่อง ความสะดวก และ ความรวดเร็วในการเข้าถึงเกมคาสิโนออนไลน์ เราจึง ใช้เทคโนโลยี HTML 5 ซึ่งเป็น เทคโนโลยีที่ล้ำสมัย ปัจจุบันนี้ มาพัฒนาเว็บไซต์ของเรากันเถอะ คุณจึงไม่ต้อง ดาวน์โหลดแอป หรือติดตั้งโปรแกรมเพิ่มเติม เพียง เปิดเบราว์เซอร์ บนอุปกรณ์ที่ มีอยู่ของคุณ และเยี่ยมชม เว็บไซต์เรา คุณสามารถ สนุกกับสล็อตได้ทันที
การใช้งานกับอุปกรณ์หลากหลาย
ไม่ว่าคุณจะใช้ สมาร์ทโฟน ระบบ แอนดรอยด์ หรือ iOS ก็สามารถ เล่นสล็อตได้อย่างราบรื่น ระบบของเรา ได้รับการออกแบบให้รองรับ ระบบต่าง ๆ ไม่สำคัญว่าคุณ มี โทรศัพท์ ใหม่หรือเก่า หรือ แม้แต่แท็บเล็ตหรือแล็ปท็อป ทุกอย่างก็สามารถ ใช้งานได้อย่างไม่มีปัญหา ไม่มีปัญหา เรื่องความเข้ากันได้
เล่นได้ทุกที่ทุกเวลา
ข้อดีอย่างหนึ่งของการเล่นเว็บสล็อตอย่าง PG Slot คือ คุณสามารถ เล่นได้ทุกเวลา ไม่ว่าจะ อยู่ที่บ้าน ที่ออฟฟิศ หรือแม้แต่ ในที่สาธารณะ สิ่งที่คุณต้องมีคือ เน็ต คุณสามารถ เล่นเกมได้ทันที และคุณไม่ต้อง ห่วงเรื่องการดาวน์โหลด หรือติดตั้งโปรแกรมที่ เปลืองพื้นที่อุปกรณ์
เล่นสล็อตฟรี
เพื่อให้ ผู้ใช้ใหม่ มีโอกาสลองและสัมผัสประสบการณ์สล็อตแมชชีนของเรา PG Slot ยังเสนอบริการสล็อตทดลองฟรีอีกด้วย คุณสามารถ เล่นได้ทันทีโดยไม่ต้องสมัครสมาชิกหรือฝากเงิน การ เล่นฟรีนี้จะช่วยให้คุณเข้าใจวิธีเล่นและรู้จักเกมก่อนลงเดิมพันจริง
การบริการและความปลอดภัย
PG Slot ตั้งใจให้บริการที่ดีที่สุดกับลูกค้า เรามี ทีมบริการที่พร้อมช่วยเหลือตลอด 24 ชั่วโมง นอกจากนี้เรายังมี ระบบรักษาความปลอดภัยที่ทันสมัย ด้วยวิธีนี้ คุณจึงมั่นใจได้ว่า ข้อมูลส่วนตัวและการเงินของคุณจะปลอดภัย
โปรโมชั่นและโบนัสพิเศษ
อีกข้อดีของการเล่นสล็อตกับ PG Slot คือ มี โปรโมชันและโบนัสมากมาย ไม่ว่าคุณจะเป็น สมาชิกใหม่หรือสมาชิกเก่า คุณสามารถ รับโปรโมชันและโบนัสได้ สิ่งนี้จะ เพิ่มโอกาสชนะและความสนุกในเกม
สรุปการเล่นสล็อตเว็บที่ PG Slot ถือเป็นการลงทุนที่คุ้มค่า คุณจะไม่เพียงได้รับความสุขและความสะดวกสบายจากเกมเท่านั้น แต่คุณยังมีโอกาสลุ้นรับรางวัลและโบนัสมากมายอีกด้วย ไม่สำคัญว่าจะใช้โทรศัพท์มือถือ แท็บเล็ต หรือคอมพิวเตอร์รุ่นใด สามารถมาร่วมสนุกกับเราได้เลยตอนนี้ อย่ารอช้า ลงทะเบียนและเริ่มเล่นสล็อตกับ PG Slot วันนี้!
ทดลองเล่นสล็อต pg เว็บ ตรง
ความรู้สึกการสำรวจเล่นเกมสล็อต PG บนเว็บเดิมพันโดยตรง: เปิดจักรวาลแห่งความบันเทิงที่ไม่มีข้อจำกัด
ในกรณีของนักเดิมพันที่ค้นหาการทดลองเกมแปลกใหม่ และหวังเจอแหล่งวางเดิมพันที่มีความน่าเชื่อถือ, การทดลองเกมสล็อต PG บนเว็บไซต์ตรงถือเป็นตัวเลือกที่น่าประทับใจอย่างมาก. เนื่องจากมีความหลากหลายของเกมสล็อตที่มีให้เลือกสรรมากมาย, ผู้เล่นจะได้สัมผัสกับโลกแห่งความเร้าใจและความสุขสนานที่ไม่มีที่สิ้นสุด.
พอร์ทัลพนันตรงนี้ ให้ประสบการณ์การเล่นเกมที่ปลอดภัยแน่นอน มั่นคง และตรงตามความต้องการของนักเสี่ยงโชคได้เป็นอย่างดี. ไม่ว่าผู้เล่นจะท่านจะโปรดปรานสล็อตแมชชีนแนวคลาสสิกที่รู้จักดี หรืออยากประสบการณ์เกมแปลกใหม่ที่มีฟีเจอร์พิเศษเฉพาะและโบนัสล้นหลาม, เว็บไม่ผ่านเอเย่นต์นี้ก็มีให้เลือกสรรอย่างหลากหลายมากมาย.
เพราะมีระบบการทดลองเกมสล็อตแมชชีน PG ฟรีๆ, ผู้เล่นจะได้โอกาสทำความเข้าใจขั้นตอนเล่นเกมและทดสอบวิธีการต่างๆนาๆ ก่อนที่เริ่มใช้เงินลงทุนด้วยเงินทุนจริง. สิ่งนี้ถือเป็นโอกาสอันดีที่สุดที่จะเสริมความพร้อมสมบูรณ์และเพิ่มโอกาสในการชิงรางวัลมหาศาลใหญ่.
ไม่ว่าผู้เล่นจะคุณจะมุ่งหวังความเพลิดเพลินแบบคลาสสิก หรือการท้าทายแปลกใหม่, สล็อตแมชชีน PG บนเว็บเดิมพันโดยตรงก็มีให้เลือกเล่นอย่างหลากหลายชนิด. คุณจะได้เผชิญกับการทดลองเล่นการเล่นเกมที่น่าตื่นเต้น น่ารื่นเริง และสนุกเพลิดเพลินไปกับโอกาสดีในการคว้าโบนัสมหาศาล.
อย่ารอ, ร่วมสนุกทดลองเกมสล็อต PG บนเว็บเสี่ยงโชคโดยตรงตอนนี้ และค้นพบโลกแห่งความบันเทิงแห่งความบันเทิงที่มั่นคง น่าติดตาม และพร้อมด้วยความสนุกเพลิดเพลินรอคอยผู้เล่น. สัมผัสความตื่นเต้นเร้าใจ, ความสนุกสนาน และโอกาสในการชิงรางวัลมหาศาลมหาศาล. เริ่มเล่นเข้าสู่ความสำเร็จในวงการเกมออนไลน์เวลานี้!
На сайте https://sobr26.ru ознакомьтесь с номером телефона охранной организации СОБР. Здесь оказываются услуги, связанные с охраной недвижимости, организуется безопасность объекта, есть возможность воспользоваться физической охраной, которая оказывается более 20 лет. Прямо сейчас вы сможете рассчитывать на бесплатную консультацию. Каждый клиент сможет организовать пультовую, физическую охрану, пожарную сигнализацию, видеонаблюдение. Для того чтобы воспользоваться услугами, оставьте заявку непосредственно на сайте.
Скачать свежие новинки песен https://muzfo.net 2024 года ежедневно. Наслаждайтесь комфортным прослушиванием, скачивайте музыку за пару кликов на сайте.
https://online-learning-initiative.org/wiki/index.php/User:CYHFlynn22558112
brillx casino официальный сайт
https://brillx-kazino.com
Играя на Brillx Казино, вы можете быть уверены в честности и безопасности своих данных. Мы используем передовые технологии для защиты информации наших игроков, так что вы можете сосредоточиться исключительно на игре и наслаждаться процессом без каких-либо сомнений или опасений.Сияющие огни бриллкс казино приветствуют вас в уникальной атмосфере азартных развлечений. В 2023 году мы рады предложить вам возможность играть онлайн бесплатно или на деньги в самые захватывающие игровые аппараты. Наши эксклюзивные игры станут вашим партнером в незабываемом приключении, где каждое вращение барабанов приносит невероятные эмоции.
While the employees chicagomj.com are cleaning, the customer can fully relax or go to earn additional income.
allnews-24.com
Variety: Access to a wide range of betting options and gameplay modes. aviator game online download
Cryptolegal Services специалисты компании знают обо всех тонкостях крипторегулирования. Воспользуйтесь нашими премиальными юридическими услугами, связанными с криптовалютой прямо сейчас. Ищете легализация криптовалюты в россии 2024? Ru.cryptolegalservices.io – сайт, где представлена более детальная информация, ознакомиться с ней у вас есть возможность в удобное для вас время. Обслуживаем крупные криптовалютные биржи и частных лиц. Позволяем в вашу пользу применять закон. Поможем минимизировать риски и увеличить вашу прибыль. Обращайтесь к нам!
https://lkr88.com/?keyword=syair-hk-asiktoto
Компания ВентТехника успешно занимается продажей вентиляции и кондиционеров. Мы рады предложить для вас наилучшее вентиляционное оборудование, а также по доступной стоимости установить кондиционер в короткие сроки. Работы будут осуществлены на высочайшем уровне. Ищите вентилятор центробежный вц? Venttehnica.ru – сайт, где у вас есть возможность прямо сейчас посмотреть каталог товаров. Здесь имеются масляные радиаторы, насосы для воды, тепловые завесы и пушки, осушители и очистители воздуха, конвекторы и другое. Обращайтесь, с радостью вас проконсультируем по всем интересующим вопросам.
newhomeeasy.com
На сайте https://setki.moscow вы сможете оформить заявку для того, чтобы заказать москитную сетку. Конструкции производятся из качественных, надежных материалов и всего за день. Монтажные работы проводятся в любой, наиболее комфортный для вас день. На работы, конструкции даются гарантии 12 месяцев. Рассчитать итоговую цену вы сможете прямо сейчас. Установлена привлекательная стоимость за счет собственного производства. Работа происходит не только по Москве, но и области. Предприятие специализируется на производстве, реализации, а также установке москитных сеток.
Competitive Tournaments and Events aviator game kya hai in hindi
Wide variety of designs and styles home365.net. An environmentally friendly material that does not produce toxic emissions and does not contain formaldehyde, unlike plastic analogues.
enjoyable. aviator game sportybet
Скачать свежие новинки песен https://muzfo.net 2024 года ежедневно. Наслаждайтесь комфортным прослушиванием, скачивайте музыку за пару кликов на сайте.
Зайдите на сайт https://mtg-biz.ru/ где вы сможете познакомиться с одним из лидеров разработчиков системы электронной очереди и системы управления очередями в России и СНГ. Мы обслуживаем сотни государственных и коммерческих предприятий страны. Мы разработали программное решение, архитектура которого позволяет расширять функционал системы под специфику деятельности различных предприятий. Подробнее на сайте.
1xbet – это один из самых популярных букмекеров в мире, который обеспечивает широкий спектр ставок на различные виды спорта и игры казино. Этот букмекер стал известным благодаря своему надежному и прозрачному сервису, обширному выбору ставок и высоким коэффициентам.
Каждый день сотни тысяч людей по всему миру используют 1xbet для размещения своих ставок, что делает его одним из лидеров в индустрии азартных игр.
Чтобы в полной мере воспользоваться всеми преимуществами сервиса 1xbet, требуется регистрация на платформе. Это необходимо для обеспечения безопасности и конфиденциальности пользователей. Регистрация позволяет вам управлять своим счетом, следить за историей ставок, участвовать в акциях и бонусных программах.
Amour Again
Завершение регистрации и начало работы на 1xbet
После успешной регистрации на 1xbet, мир онлайн ставок открывает перед вами свои двери. Но как начать делать ставки и использовать все преимущества этой платформы?
Прежде всего, необходимо понимать, что 1xbet – это не только ставки на спорт, но и казино, покер, финансовые ставки и многое другое. Чтобы начать делать ставки, вам нужно перейти в раздел «Спорт» или «Live», выбрать интересующий вас вид спорта и конкретное событие. Выберите тип ставки и введите желаемую сумму. После этого нажмите кнопку «Поставить». Помните, что ставки следует делать ответственно, распределяя свои средства и не рискуя всем банком сразу.
Советы по эффективному использованию 1xbet:
Используйте все доступные бонусы и акции. 1xbet предлагает своим пользователям широкий выбор бонусов, начиная от бонуса на первый депозит и заканчивая кэшбэком и бонусами за активность.
Изучите статистику перед тем, как делать ставку. На сайте 1xbet есть раздел со статистикой, который поможет вам сделать более обоснованный выбор.
Используйте мобильное приложение 1xbet. Оно позволит вам делать ставки в любое время и в любом месте, а также получать уведомления о важных событиях и изменениях в линии ставок.
Итак, с завершением регистрации на 1xbet начинается ваше погружение в азартный мир ставок. Все, что остается – это разобраться в нюансах и начать зарабатывать!
Testek
https://www.numeracy.wiki/index.php/Cyprus_Rent
Игровые автоматы егт
https://uzfootball.ru/igrovie-avtomati/igrovie-avtomati-egt-1.html
https://utahsyardsale.com/author/sheenahamer/
http://unitedfarmersco-op.com/its-mission-explore-strange-to-the-new-worlds/
Numerous online casino platforms offer the Aviator Game. These platforms provide a secure and regulated 4rabet aviator
https://bikecounts.org/wiki/Newton
https://worldhealthstock.com/overview-estate/
перевод документов
интернет эквайринг https://internet-ekvajring.kz – безопасные и эффективные платежные решения для вашего бизнеса.
интернет эквайринг https://internet-ekvajring.kz – безопасные и эффективные платежные решения для вашего бизнеса.
Conclusion aviator game website
Агентство по продвижению телеграм-каналов https://883666b.com в Москве специализируется на разработке и реализации стратегий для увеличения аудитории и вовлечённости подписчиков на телеграм-каналах. Эксперты агентства помогают клиентам определить целевую аудиторию, разрабатывают контент-планы и рекламные кампании. Услуги включают рекламу посевами, таргет рекламой, анализ конкурентов, SEO-оптимизацию контента.
На сайте https://kupit-roboty-pylesosy.ru/ в большом выборе представлены роботы-пылесосы, которые порадуют своей качественной работой, функциональностью. Многие из них идеально подходят как для сухой, так и влажной уборки. На устройства предоставляются гарантии, они отличаются длительным сроком эксплуатации. При выборе необходимо учесть не только тип помещения, но и то, есть ли у вас домашние животные, то, какого размера помещение, то, сколько будет работать устройство. Выбирайте изделие, полагаясь на эти простые рекомендации.
ทดลองลองใช้เล่นสล็อต และค้นพบประสบการณ์การเล่นเกมที่ไม่เหมือนใคร!
สำหรับนักพนันที่กำลังต้องการความบันเทิงและโอกาสในการได้รับรางวัลมหาศาล สล็อตออนไลน์เป็นอีกหนึ่งทางเลือกที่ที่คุ้มค่าใคร่ครวญ.ด้วยความมากมายของเกมสล็อตที่น่าตื่นเต้น ผู้เล่นสามารถทดลองเล่นและค้นหาเกมที่เหมาะกับตัวเองได้อย่างง่ายดาย.
ไม่ว่าคุณจะประทับใจเกมสล็อตคลาสสิกหรือต้องการความท้าทาย, ตัวเลือกรอคอยให้คุณสัมผัส. จากสล็อตที่มีหัวข้อมากมาย ไปจนถึงเกมที่มีคุณสมบัติพิเศษและรางวัล, ผู้เล่นจะได้พบกับประสบการณ์ที่น่าตื่นเต้นและน่าติดตาม.
ด้วยการทดสอบสล็อตฟรี, คุณสามารถศึกษาวิธีการเล่นและค้นหากลยุทธ์ที่ต้องการก่อนวางเดิมพันด้วยเงินจริง. นี่คือโอกาสที่ดีที่จะศึกษากับเกมและปรับปรุงโอกาสในการคว้ารางวัลใหญ่.
อย่าเลื่อนเวลา, เข้าไปกับการลองเล่นสล็อตออนไลน์วันนี้ และค้นพบประสบการณ์การเล่นเกมที่ไม่เหมือนใคร! เพลิดเพลินความตื่นเต้น, ความร่าเริง และโอกาสชนะรางวัลมากมาย. เริ่มต้นเดินทางสู่ความเฟื่องฟูของคุณในวงการสล็อตออนไลน์แล้ววันนี้!
На сайте https://uvlajniteli-vozduha1.ru/ находятся увлажнители воздуха, которые помогут создать в помещении необходимый микроклимат и атмосферу. Они особенно необходимы зимой, когда радиаторы сильно топят, а также летом. Если в вашей квартире низкая влажность, то и в этом случае необходимо приобрести такие агрегаты, которые повысят уровень влажности. Все конструкции представлены проверенными, лучшими марками, которые предоставляют гарантии. Увлажнители воздуха необходимы и для того, чтобы справиться с потенциально опасными аллергенами, а также пылью.
cash out before the plane crashes. The objective is to maximize winnings by timing the cash-out perfectly, aviator game download for pc
Over-betting: Betting too much too quickly can lead to significant losses. what is the secret of aviator game
sa gaming
הימורי ספורטיביים – הימורים באינטרנט
הימור ספורטיביים נעשו לאחד התחומים הצומחים ביותר בהימור ברשת. שחקנים מסוגלים להתערב על תוצאותיהם של אירועים ספורט מוכרים לדוגמה כדור רגל, כדור סל, טניס ועוד. האופציות להתערבות הן מרובות, כולל תוצאת ההתמודדות, מספר השערים, מספר הנקודות ועוד. להלן דוגמאות של למשחקי נפוצים שעליהם ניתן להמר:
כדורגל: ליגת אלופות, מונדיאל, ליגות אזוריות
כדור סל: NBA, יורוליג, טורנירים בינלאומיים
משחק הטניס: טורניר ווימבלדון, US Open, רולאן גארוס
פוקר באינטרנט – הימור ברשת
פוקר באינטרנט הוא אחד מהמשחקים ההימורים הפופולריים ביותר כיום. משתתפים מסוגלים להתמודד מול מתחרים מכל רחבי תבל במגוון סוגי של המשחק , לדוגמה Texas Hold’em, Omaha, Stud ועוד. אפשר לגלות תחרויות ומשחקי במבחר רמות ואפשרויות הימור שונות. אתרי הפוקר המובילים מציעים:
מגוון רחב של וריאציות המשחק פוקר
טורנירים שבועיות וחודשיים עם פרסים כספיים
שולחנות המשחק למשחק מהיר ולטווח הארוך
תוכניות נאמנות ומועדוני VIP עם הטבות בלעדיות
בטיחות והוגנות
בעת בוחרים בפלטפורמה להימורים באינטרנט, חיוני לבחור גם אתרים מורשים המפוקחים המציעים סביבת למשחק מאובטחת והגיונית. אתרים אלו משתמשים בטכנולוגיות אבטחה מתקדמות להבטחה על מידע אישי ופיננסי, וגם באמצעות תוכנות גנרטור מספרים אקראיים (RNG) כדי לוודא הגינות במשחקים במשחקי ההימורים.
מעבר לכך, הכרחי לשחק גם בצורה אחראי תוך כדי קביעת מגבלות אישיות הימורים אישיות. רוב אתרי ההימורים מאפשרים גם לשחקנים לקבוע מגבלות להפסדים ופעילויות, וגם להשתמש ב- כלים נגד התמכרויות. הימרו בחכמה ואל תרדפו גם אחר הפסדים.
המדריך השלם לקזינו ברשת, משחקי ספורט ופוקר באינטרנט באינטרנט
ההימורים ברשת מציעים עולם שלם הזדמנויות מרתקות לשחקנים, החל מקזינו אונליין וגם משחקי ספורט ופוקר באינטרנט. בעת בחירת פלטפורמת הימורים, הקפידו לבחור אתרי הימורים המפוקחים המציעים סביבת למשחק מאובטחת והוגנת. זכרו לשחק באופן אחראי תמיד ואחראי – משחקי ההימורים באינטרנט אמורים להיות מבדרים ולא גם לגרום לבעיות פיננסיות או חברתיות.
cash-out perfectly. aviator game ghana
CarTrip предоставляет впечатлительный выбор автомобилей. Мы следим за тем, чтобы наш автопарк был в достойном состоянии. Автомобиль предоставляем клиенту после хорошей мойки и чистки. Ищете аренда машины сутки Анапа? Auto-arenda-anapa.ru – сайт, где вы узнаете более детальную информацию, ознакомьтесь с ней уже сейчас. С радостью поможем вам подобрать нужный вариант. Оплата может быть произведена любым удобным для вас способом. С нами вы сможете сэкономить свои денежные средства. Любуйтесь прекрасными видами Анапы прямо из окна автомобиля!
dynamic features, and social elements, it offers an engaging experience for players. The game is supported by aviator game is legal in india
На сайте https://dolinakamnej.ru приобретите минералы, натуральные камни, а также интересные и необычные изделия, которые понравятся даже истинному эстету. Доставка осуществляется в любую точку мира, России. Компания отличается собственным производством, а потому установила привлекательные и доступные цены. Здесь же есть возможность воспользоваться и такими популярными, нужными услугами, как полировка, распиловка на заказ. Все услуги оказываются качественно, в соответствии с самыми высокими требованиями.
If you’re looking for a thrilling and unique online casino game, give the Aviator Game a try. Join the millions aviator game is legal in india
people’s pharmacy bupropion
Автосервис LEMON CAR обладает отменной репутацией и предлагает услуги по доступной цене. Здесь работает грамотная команда мастеров. Они используют только новейшее оборудование и готовы о вашей машине позаботиться. https://lemon-car.ru – сайт, где можно узнать актуальные цены, а также сроки. Клиенты автосервиса высоко оценивают скорость и качество обслуживания. Позвоните нам, и мы дадим вам грамотную консультацию. С помощью LemonCar ваше авто будет выглядеть ухоженно и надежно работать очень долгое время.
Playing the Aviator Game is a thrilling experience. Players place their bets and watch the plane take off, with aviator game telegram
апостиль в новосибирске
перевод с иностранных языков
9 Things Your Parents Teach You About Content Marketing On Social Media content marketing on social media
ceria777
Теневой плинтус: необходимость или прихоть?
скрытый плинтус теневой https://msk-alyuminievyj-tenevoj-plintus.ru/ .
Playing the Aviator Game involves a few simple steps: how to master aviator game
перевод документов
Ищете статьи по психотерапии и психологии? Тогда заходите на портал ack-group.ru. Тут вы узнаете о том, что такое психотерапия. Объясним, в чем разница между психотерапией и простой беседой. Требуется психотерапия? Ack-group.ru/stati-po-psikhologii/psikhoterapiya – здесь узнаете, кто такой психотерапевт, что лечит, с какими симптомами необходимо обращаться за квалифицированной помощью. На ресурсе размещены статьи про частые психологические проблемы, с которыми сталкивается множество людей. Поможем вам восстановить и сохранить свое здоровье!
ремонт фундамента
Основа стильного интерьера плинтус теневой для вашего дома
теневой плинтус напольный теневой плинтус напольный .
Секрет современного дизайна плинтус теневой для вашей квартиры
теневой плинтус купить теневой плинтус купить .
Как выбрать идеальный теневой плинтус
теневой плинтус напольный https://msk-alyuminievyj-tenevoj-plintus.ru/ .
vavada casino актуальное
купить квартиру в казани https://nedvizhimost47.ru
Теневой плинтус: необходимость или прихоть?
плинтус теневой профиль https://msk-alyuminievyj-tenevoj-plintus.ru/ .
Как выбрать идеальный теневой плинтус
плинтус теневой профиль плинтус теневой профиль .
Risk Management: Setting limits on how much to bet and when to cash out. aviator game live stream
vavada официальный сайт вход
вавада вход vavada
Уникальный дизайн с теневым плинтусом
монтаж теневого плинтуса цена https://msk-alyuminievyj-tenevoj-plintus.ru/ .
Преимущества использования теневого плинтуса
теневой плинтус скрытого монтажа купить https://msk-alyuminievyj-tenevoj-plintus.ru/ .
Результат студии «Мята» – это прекрасный интерьер, соответствующий ожиданиям клиента. Наша команда состоит из профессиональных специалистов. Предлагаем наилучшие цены на дизайн, гарантируем компетентность и ответственность. Мы прочно завоевали доверие своих клиентов. Ищете дизайн проект квартиры в ташкенте? Tashkent.studio-mint.pro – сайт, где представлены отзывы о студии, прочитайте их прямо сейчас. Нас советуют друзьям и знакомым. Позвоните нам, и закажите дизайн интерьера. На протяжении всего проекта мы открыты к диалогу. Реализуем вашу мечту!
На сайте https://smarttax.expert/liquidation/licvidacia получите консультацию для того, чтобы воспользоваться такой услугой, как: ликвидация бизнеса без каких-либо проблем. В компании трудятся компетентные, знающие и талантливые специалисты, которые сделают все возможное для того, чтобы вы быстро, эффективно и без потерь закрыли бизнес. Юридические риски будут минимизированы, а потому вы избежите крупных финансовых потерь. Кроме того, удастся учесть все требования законодательства.
Casino
https://uzfootball.ru/map1.html
купить квартиру в казани от застройщика жк казань купить квартиру от застройщика
vavada ru
Секрет современного дизайна плинтус теневой для вашего офиса
теневой плинтус для пола теневой плинтус для пола .
Теневой плинтус: новый взгляд на отделку
теневой плинтус монтаж https://msk-alyuminievyj-tenevoj-plintus.ru/ .
Секрет современного дизайна плинтус теневой для вашей квартиры
теневой плинтус цена https://msk-alyuminievyj-tenevoj-plintus.ru/ .
Online Platforms Offering the Game demo aviator game
Зайдите на сайт https://generalsfaq.ru/ который создан для поклонников компьютерной стратегии Генералы. Вы сможете почитать FAQ и гайды по игре, найти карты Zero Hour, а также прочие военные стратегии. Generals это лучшая RTS стратегия для компьютера – присоединяйтесь к нашему сообществу!
купить квартиру от застройщика недорого https://novostroyka47.ru
На сайте https://shvejnye-mashiny-77.ru/ ознакомьтесь со всем ассортиментом швейных машинок, которые различаются не только внешним видом, дизайном, но и техническими параметрами, стоимостью. А для того, чтобы сделать правильный выбор, следует ознакомиться с характеристиками каждого изделия. Для всех клиентов действует оперативная доставка, установлены привлекательные цены, предоставляются гарантии. При выборе следует уточнить навыки шитья, уточнить то, какие опции вам нужны. Действуют разумные цены.
На сайте https://imperiasinteza.by оставьте заявку с той целью, чтобы воспользоваться услугами, связанными с логопедией, сенсорной интеграцией. Только для вас профессиональные услуги, консультации логопеда. В компании работает логопед-дефектолог для детей, можно воспользоваться сенсорной интеграцией. Специально для вас индивидуальные, а также групповые занятия, которые принесут должный эффект. При необходимости организуется выезд специалиста. Самая первая консультация предоставляется в подарок.
Playing the Aviator Game online offers several benefits: aviator demo slot
купить квартиру в казани новостройка от застройщика https://novostroyka47.ru
Студия «Мята» грамотно занимается дизайном интерьеров. У нас работают опытные специалисты с соответствующим образованием. Своих клиентов всегда радуем интересными проектами. Гарантируем реализацию ваших желаний. При сотрудничестве с нами, вы существенно сэкономите личный бюджет. Ищете дизайн интерьера в ереване? Yerevan.studio-mint.pro – сайт, где узнаете больше информации о нашей компании. Выполним поставленную задачу в срок. Предоставляем грамотные советы и находим к любому клиенту подход. Обращайтесь, с радостью ответим на интересующие вас вопросы.
The Aviator Game offers multiplayer options that allow players to compete against each other in real-time. This aviator game fake or real
На сайте http://ritualnoe-buro-vrn.ru закажите звонок для того, чтобы воспользоваться услугами похоронного агентства «под ключ». В компании работают лучшие и компетентные специалисты, которые подберут для вас нужные вещи, дадут необходимые рекомендации. Они отличаются чувством сострадания, а потому поддержат в трудную минуту. Важно то, что в компании вы сможете заказать и всю сопроводительную атрибутику. Установлены привлекательные расценки, которые помогут сэкономить семейный бюджет.
CarTrip предоставляет качественные услуги аренды авто в Краснодаре по привлекательной цене. Обращайтесь скорее к нам, если вас интересует авто напрокат. Все наши машины в отменном состоянии. Уверены, вы станете нашим постоянным клиентом и будете снова и снова к нам возвращаться. Ищете прокат авто Краснодар на сутки? Prokat.car-trip.ru – сайт, где у вас есть возможность подробнее ознакомиться с нашими услугами. Также здесь можно почитать отзывы. У нас имеется широкий выбор автомобилей на любой вкус. Работаем 24/7, с радостью готовы ответить на все ваши вопросы. Будем ждать вашего звонка!
На сайте https://lavrice.com вы сможете ознакомиться со всей интересной, любопытной информацией, которая будет необходима всем путешественникам, желающим устроить незабываемую поездку в другие страны и города. Здесь получится заказать индивидуальный трансфер для удивительных путешествий. Почитайте полезные материалы об ОАЭ, Турции, Греции, Кипре, а также Египте. Также вы сможете воспользоваться услугами частного джета для удивительных и невероятных поездок. У вас получится отыскать любую информацию, которая вам интересна, включая все о яхтах, лечении, медицине, экскурсиях.
The Aviator Game offers multiplayer options that allow players to compete against each other in real-time. This download aviator for pc
На сайте https://pd-seller.ru получится скачать бесплатно либо приобрести Parallels Desktop 19 для Mac. Предоставляется месячная гарантия возврата денежных средств. Вас ожидает огромное количество различных приложений, которые используются для Windows, торговое, бухгалтерское ПО, КОМПАС и многое другое. Посмотрите видео-презентацию прямо сейчас! При покупке вы получите ключ Windows абсолютно бесплатно. Все лицензии являются официальными. Вы сможете легко приобрести, воспользоваться, продлить и обновить.
Aw, this was a very good post. Taking a few minutes and actual effort to make a good article… but what can I say… I procrastinate a whole lot and never manage to get anything done.
http://www.ijwiryacu.com/read?article=hzlnmuhjlvuvbnbh
mipon.net/bbs-c/clever.cgi/clever.cgi?page=280
vet-aibolit.ru/about
bradfrost.online/speaking
dedadi.ru/obshhestvo/nacionalnyy-sostav-moskva.html
Скачать музыку https://musiciansfix.com/artist/ высокого качества в любом жанре. Огромный выбор треков от классики до новинок поможет вам создать идеальный плейлист. Наслаждайтесь любимыми композициями и открывайте для себя новые музыкальные горизонты. Присоединяйтесь и начните скачивать музыку прямо сейчас!
The Aviator Game is designed to be compatible with a wide range of devices, including desktop computers, aviator app download
buy amoxicillin 500mg capsules uk: cheapest amoxicillin – amoxicillin 500mg price in canada
Студия «Мята» грамотно подходит к оформлению интерьеров. В нашей команде работают только высококвалифицированные специалисты с профильным образованием. Мы радуем заказчиков успешными проектами. Ваше желание мы реализуем. С нами вы спокойно сэкономите свои деньги. Ищете дизайн квартиры в тбилиси? Tbilisi.studio-mint.pro – сайт, где вы узнаете, как происходит сотрудничество с компанией. Ознакомиться с информацией можно прямо сейчас. Гарантируем выполнение задачи в срок. Мы даем множество ценных рекомендаций и находим контакт с каждым клиентом. Ждем вас!
cash out before the plane crashes. The objective is to maximize winnings by timing the cash-out perfectly, aviator game hacking
MIGRANT SUPPORT – известная компания, которая поможет получить песель. Мы объясним вам, какие для жизни в Польше понадобятся документы. Подготовим нужные заявления, сопроводим для фотографирования и снятия отпечатков пальцев. Ищите pesel несовершеннолетнему ребенку? Vpolshe.com/pesel-bez-prisutstviya – сайт, где представлена полезная информация. Вы сможете узнать, для чего нужен номер PESEL и что это такое. Также здесь можете прямо сейчас прочитать отзывы и оставить заявку. Обращайтесь с интересующими вопросами в Viber, WhatsApp или пишите на нашу электронную почту.
Yes, the Aviator Game is compatible with mobile devices. Players can enjoy the game on their smartphones or aviator apk
For beginners, the key to success in the Aviator Game is to start with small bets and gradually increase as you how to beat the aviator game
На сайте https://straxovkaonlain.ru вы сможете воспользоваться такой важной услугой, как подбор страхования, а также сопутствующими услугами. К наиболее популярным услугам, с которыми можно ознакомиться на сайте, относят: страхование ОСАГО, «АнтиКЛЕЩ», страхование ипотеки, открытие расчетного счета, кредит наличными. У компании огромное количество партнеров, с которыми вы сможете ознакомиться прямо сейчас. А если вы хотите получить консультацию, то напишите свой вопрос в специальной форме.
Наши металлические лестницы от производителя https://www.supersvarshik.com/ продуманы, просчитаны на прочность, с удобными ступенями из просечного листа, на которых не задерживается снег, песок или мусор. Ступени из металла и листа ПВЛ являются и прекрасным протектором, нога на них не скользит. Лестницы из металла и листа ПВЛ окрашены в камере порошковой краской – это защищенное и долговечное покрытие для металла. Установка и монтаж уличной металлической лестницы осуществляется на вкрученные в землю металлические сваи, на который методом сварки крепятся блоки из площадки и лестничного марша, Монтаж уличной лестницы из металла проходит очень оперативно, в отличии от других видов лестниц. Спроектируем, изготовим и смонтируем для вас самую правильную лестницу!
הימורים באינטרנט
הימורי ספורטיביים – הימורים באינטרנט
הימור ספורט נעשו לאחד הענפים המשגשגים ביותר בהימור באינטרנט. שחקנים יכולים להמר על תוצאת של אירועי ספורט פופולריים לדוגמה כדורגל, כדור סל, טניס ועוד. האפשרויות להימור הן רבות, כולל תוצאתו המאבק, כמות השערים, מספר הנקודות ועוד. הבא דוגמאות של למשחקי נפוצים במיוחד שעליהם ניתן להמר:
כדור רגל: ליגת אלופות, גביע העולם, ליגות מקומיות
כדור סל: ליגת NBA, ליגת יורוליג, טורנירים בינלאומיים
משחק הטניס: טורניר ווימבלדון, אליפות ארה”ב הפתוחה, אליפות צרפת הפתוחה
פוקר ברשת ברשת – הימור ברשת
משחק הפוקר ברשת הוא אחד ממשחקי ההימור הנפוצים ביותר בימינו. שחקנים מסוגלים להתמודד נגד יריבים מכל רחבי העולם במגוון גרסאות של המשחק , למשל טקסס הולדם, אומהה, Stud ועוד. ניתן לגלות תחרויות ומשחקי קש במגוון רמות ואפשרויות הימור שונות. אתרי פוקר המובילים מציעים:
מבחר רב של גרסאות פוקר
תחרויות שבועיים וחודשיים עם פרסים כספיים
שולחנות המשחק למשחקים מהירים ולטווח ארוך
תוכניות נאמנות ללקוחות ומועדוני עם הטבות עם הטבות
בטיחות ואבטחה והוגנות
כאשר הבחירה פלטפורמה להימורים ברשת, חשוב לבחור אתרי הימורים מורשים המפוקחים המציעים גם סביבת משחק מאובטחת והגיונית. אתרים אלו משתמשים בטכנולוגיית אבטחה מתקדמת להגנה על מידע אישי ופיננסיים, וכן בתוכנות גנרטור מספרים אקראיים (RNG) כדי להבטיח הגינות המשחקים במשחקי ההימורים.
מעבר לכך, חשוב לשחק בצורה אחראית תוך הגדרת מגבלות הימור אישיות. מרבית אתרי ההימורים מאפשרים גם למשתתפים להגדיר מגבלות להפסדים ופעילות, כמו גם לנצל כלים נגד התמכרויות. שחקו בחכמה ואל גם תרדפו אחרי הפסד.
המדריך המלא לקזינו ברשת, משחקי ספורט ופוקר באינטרנט ברשת
ההימורים ברשת מציעים עולם שלם של הזדמנויות מלהיבות לשחקנים, מתחיל מקזינו אונליין וגם משחקי ספורט ופוקר באינטרנט. בעת בחירת בפלטפורמת הימורים, הקפידו לבחור אתרים מפוקחים המציעים סביבת למשחק מאובטחת והגיונית. זכרו גם לשחק בצורה אחראית תמיד ואחראי – ההימורים ברשת נועדו להיות מבדרים ולא גם ליצור לבעיות פיננסיות או חברתיים.
Several key developers and companies have played a significant role in the development and success of the aviator game hindi
На сайте https://spalnye-meshki-77.ru/ можно приобрести спальные мешки, которые представлены здесь в большом многообразии и самых разных оттенков. Отправляясь на природу, очень важно взять их с собой. Основное требование заключается в том, чтобы изделие было выполнено из современных, инновационных материалов, которые не впитывают влагу и являются износостойкими. Спальный мешок считается основой вашего пребывания на свежем воздухе. Можно выбрать: кокон, комбинированный тип либо одеяло. А вот зимние варианты подходят в случае очень низких температур.
7k casino скачать
10 pounds no deposit bonus
https://uzfootball.ru
7к казино официальный
р7 казино телеграмм
The Aviator Game includes various in-game bonuses and rewards to enhance the player’s experience. These can aviator game website
На сайте https://pogadaems.ru вы сможете почитать увлекательную, интересную и актуальную информацию, которая касается гаданий в режиме реального времени. Есть возможность изучить информацию о гаданиях на картах Таро, игральных, а также цыганских. Имеются интересные и любопытные картинки, которые позволят пожелать доброго утра маме. Перед вами самая интересная, увлекательная информация, которая поможет сориентироваться в теме. Обязательно ознакомьтесь с гороскопом, чтобы знать, что ожидает вас сегодня.
обувница тула
games that stood out from traditional casino offerings. Inspired by the concept of high-risk, high-reward, the aviator apk download
Такси и Трансфер в Анапе – компания, которая дает гарантию на то, что авто прибудет в указанный срок, несмотря на различные форс мажоры. Водитель вежлив, он предоставит вам нужную информацию – бесплатно. Вы также можете заказать машину с детским креслом. Цены приемлемые. Ищите такси краснодар Анапа? Anapa-taxi-transfer.ru – сайт, где вы можете посчитать точную стоимость поездки. Техника содержится в отличном техническом состоянии. У нас найдете транспорт, идеально подходящий для ваших нужд. Не отказывайте себе в комфортном передвижении!
This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your excellent post. Also, I have shared your website in my social networks!
mazda-demio.ru/forums/index.php?autocom=gallery&req=si&img=4139
http://www.askthebuyers.com/blogs/30/Why-is-the-popularity-of-universities-decreasing-all-the-time?lang=tr_tr
vseogirls.ru/diplomyi-s-unikalnyim-dizaynom-i-oformleniem
delighta.ru/mesta/~shownews/3252/index.html
americanautotitleloan.com/lake-wylie-sc-title-loans
If you’re looking for a thrilling and unique online casino game, give the Aviator Game a try. Join the millions aviator demo game
kevin costner movies walton goggins movies and tv showsquentin tarantino moviesyellowstone premiere
CVzen to najlepsza usluga pisania CV https://cvzen.pl/ i coach kariery dla milionow osob poszukujacych pracy na calym swiecie. Nasz zespol ekspertow jest zaangazowany w Twoj sukces i bedzie Cie wspieral przez cala Twoja kariere, od napisania profesjonalnego CV i listu motywacyjnego z uwzglednieniem specyfiki branzy, po optymalizacje profilu LinkedIn i zapewnienie profesjonalnego coachingu kariery. Odblokuj nowe mozliwosci dzieki CV, ktore pokaze Twoj potencjal.
Мята – студия дизайна интерьеров. Мы оказываем услуги в любой точке мира и любим свое дело. Нас вдохновляют интересные проекты, трудных задач мы не боимся. Готовы с радостью реализовать вашу мечту. Ищете дизайн проект квартиры в уфе? Ufa.studio-mint.ru – сайт, где имеется портфолио работ. Здесь у вас есть возможность прочесть отзывы наших благодарных клиентов. Вы будете удивлены сроком разработки проекта и внимательностью к деталям. Гарантируем оптимальную стоимость. Придерживаемся высочайших стандартов в сфере обслуживания. Учтем все ваши пожелания, обращайтесь!
На сайте http://adsguard.ru вы сможете узнать больше информации о такой популярной и нужной программе, как AdGuard. Это блокировщик рекламы, у которого встроенная защита конфиденциальной информации, имеется родительский контроль. Это оптимальный вариант для блокировки любой рекламы, а также программ, которые несут потенциальную угрозу, считаются вредоносными и размещаются на мобильных устройствах, веб-браузерах. Воспользоваться программой можно, независимо от платформы. Кроме того, будут расширены возможности просмотра.
На сайте https://umnye-roboty-pylesosy.ru/ вы сможете приобрести умного робота-пылесоса, который порадует своей качественной работой. К его важным преимуществам относят эффективную, быструю, точную работу. А управление происходит при помощи смартфона. Предусмотрены различные параметры чистки, которые выбирают в соответствии с типом напольного покрытия. При выборе стоит учесть и габариты изделия, чтобы оно легко передвигалось по полу. Также важны и дополнительные функции, которые повысят комфорт.
Player Reviews and Testimonials aviator game
How to Start Playing the Aviator Game? demo game
Кузовной ремонт – компания, которая осуществляет любые заказы. К покраске авто и к процессу кузовного ремонта подходим тщательно. Мы ни разу не подвели наших клиентов. Нас советуют своим коллегам и друзьям. Если у вас возникли какие-либо вопросы, позвоните нам. Ищите покраска автомобиля киров? Kuzov43.ru – сайт, где у вас есть возможность детальнее ознакомиться с ценами и услугами. Формирование продолжительных отношений – одна из основных целей. Гарантируем высочайшее качество по привлекательной стоимости. Вернем машине безупречный вид и сэкономим ваши денежные средства!
How to Play the Aviator Game п»їaviator game
Мята – студия, где работает команда квалифицированных сотрудников. Мы успешно трудимся в области дизайна интерьера и свое дело очень любим. Разрабатываем проекты высокого уровня. Оказываем услуги по привлекательной цене и в адекватные сроки. Ищете дизайн проект квартиры в новосибирске? Novosibirsk.studio-mint.ru – сайт, где можете прямо сейчас рассчитать стоимость проекта. Также здесь можно посмотреть наши работы и прочитать отзывы довольных клиентов. Каждый проект уникален и тщательно продуман. Готовы выполнить любые ваши пожелания. Обращайтесь к нам, чтобы обсудить все детали.
Hi, this weekend is fastidious for me, as this time i am reading this great informative piece of writing here at my house.
shop2.rybolov.de/index.php?links_exchange=yes&page=260&show_all=yes
tivi24h.com/2011/01/xem-bong-online-bong-truc-tuyen-kenh.html
mesannuaires.fr/art-et-culture/mode-s286.html
23bileta.ru/index.html
skazka.g-talk.ru/viewtopic.php?f=1&t=1679&p=1705
На сайте https://esdogames.ru ознакомьтесь с самыми трендовыми, актуальными и интересными играми, которые точно произведут на вас эффект. Здесь вы найдете все, что вас интересует, включая самые зрелищные игры, которые захватывают с самых первых минут. Также представлен список лучших игр за 2024 год. Вы сможете поиграть во все, что хочется, прямо сейчас. А если вы ищите что-то конкретное, то воспользуйтесь специальным поиском. Подберите игру по жанру, режиму игры, платформе, чтобы облегчить поиск.
Топ-5 произведений в стиле pin up, для вдохновения
2 pin up https://pinupbrazilnbfdrf.com/ .
Interactive Interface: Players can interact with the game in real-time, making decisions that impact their aviator game demo
На сайте https://aquafloor-online.ru/ подберите уникальные современные покрытия, которые невосприимчивы к воздействию влаги. Их можно укладывать в самых разных помещениях, включая жилые, коммерческие. В каталоге вы найдете как виниловую плитку, так и ламинат. Вы обязательно подберете подходящую цветовую гамму, которая отлично впишется в общую концепцию. Перед вами огромное количество коллекций, созданных для самых искушенных. Для того чтобы приобрести, просто добавьте товар в корзину.
Проведение независимой строительной экспертизы — сложный процесс, требующий глубоких знаний. Наши специалисты обладают всеми необходимыми навыками, а их заключения часто служат основой для принятия верных стратегических решений. Строительно-техническая экспертиза https://stroytehexp.ru позволяет выявить факторы, вызвавшие ухудшение эксплуатационных характеристик объектов, проверить соответствие возведённых зданий градостроительным нормам.
На сайте https://avtodom.car-trip.ru/ оставьте заявку для того, чтобы устроить незабываемое путешествие на доме на колесах, где имеются все удобства. Это ваша возможность устроить незабываемое путешествие по миру, не оставаясь на одном месте. Это крайне важно для тех, кто любит природу и желает получить больше положительных впечатлений. Такой дом позволит зарядиться приятными эмоциями, посмотреть рассвет, ознакомиться с самыми живописными местами и сделать красивые фотографии. Устройте и вы себе незабываемую поездку.
Teleflora Belarus Unit https://flower-shop.by/ offers flower delivery services. The Company operates as an online florist for internet flowers in Minsk, Belarus. Send flowers to Minsk, Belarus and International with us. Business Gifts. Sending flowers online is easy with a wide network of florists to process and deliver your flower order. We take care of all Belarus flower delivery orders, We have a network of florists and flower shops who can deliver flowers as requested by our customers.
Как выбрать аксессуары для pin up образа, для модного вида
pin up slots pin up slots .
Pin up фильмы: культовые картины о pin up, для яркой кинопрограммы
up casino up casino .
Как музыка влияет на pin up культуру, которые нужно послушать
pinup oficial pinup oficial .
The story of Mbappe’s https://www.asma-online.org rise to fame is as remarkable as his on-field feats. Mbappe’s journey from local pitches to global arenas was meteoric. His early days at AS Monaco showcased his prodigious talent, with his blistering speed and fearless dribbling dismantling opposition defenses.
experiences. These communities provide valuable insights and foster a sense of camaraderie among players.
play demo
На сайте https://pervomai-172.ru/ цветочный интернет-магазин предлагает доставку прекрасных цветов по выгодным ценам. Вы можете заказать доставку прямо из офиса либо дома, теперь не нужно идти в магазин для выбора цветов. Зайдите в каталог, выберите интересующий вас букет, укажите адрес, время доставки и оплатите заказ. На сайте есть рубрика «Часто задаваемые вопросы», где вы найдете популярные ответы. Также тут имеются отзывы благодарных клиентов, ознакомьтесь с ними уже сейчас.
Секреты pin up макияжа, о которых вы не слышали
pin up pin up .
Pin up в литературе: книги и персонажи, которые важно изучить
pin up slots https://pinupbrazilnbfdrf.com/ .
http://addsub.wiki/index.php/User:DelorisMcCollist
На сайте https://setevye-karty.ru/ вы сможете приобрести сетевые карты по самым привлекательным расценкам. Здесь вы отыщите такое оборудование, которое позволит получить качественное и надежное соединение. Оптимальный вариант как для дома, так и офиса. В магазине представлены самые разные производители, которые создают исключительно проверенную, качественную продукцию, наделенную большим количеством функций. Устройства обойдутся по небольшой стоимости. Регулярно появляются новинки, с которыми необходимо ознакомиться каждому.
Pin up фильмы: культовые картины о pin up, которые стоит посмотреть
2 pin up 2 pin up .
Топ-7 элементов ретро в pin up стиле, для неординарного вида
2 pin up 2 pin up .
https://www.mazafakas.com/user/profile/4430400
Информационный ресурс https://ardma.ru, посвящен бизнесу, финансам, инвестициям и криптовалютам. Сайт предлагает экспертные статьи, аналитические отчеты, стратегии и советы для предпринимателей и инвесторов. Здесь можно найти новости и обзоры о бизнесе, маркетинге, трейдинге, а также практические рекомендации по различным видам заработка и управлению финансами.
The story of Mbappe’s https://asma-online.org rise to fame is as remarkable as his on-field feats. Mbappe’s journey from local pitches to global arenas was meteoric. His early days at AS Monaco showcased his prodigious talent, with his blistering speed and fearless dribbling dismantling opposition defenses.
The Aviator Game traces its roots back to the early days of online gambling when developers sought to create
play demo
Какое значение имеют костюмы в стиле pin up, которые стоит попробовать
2 pin up https://pinupbrazilnbfdrf.com/ .
Как литература влияет на стиль pin up, для погружения в мир литературы
up casino up casino .
https://medium.com/@momejar21741/pg-59490dd058fd
สล็อตเว็บตรง — สามารถใช้ โทรศัพท์มือถือ แท็บเล็ต คอมพิวเตอร์ ฯลฯ สำหรับการเล่น
ระบบสล็อตเว็บตรง ของ PG Slot ได้รับการพัฒนาและปรับปรุง เพื่อให้ รองรับการใช้งาน บนอุปกรณ์ที่หลากหลายได้อย่าง ครบถ้วน ไม่สำคัญว่าจะใช้ โทรศัพท์มือถือ แท็บเล็ต หรือ คอมฯ รุ่นไหน
ที่ พีจีสล็อต เราเข้าใจถึงความต้องการ ของลูกค้า ในเรื่อง ความสะดวก และ การเข้าถึงเกมคาสิโนที่รวดเร็ว เราจึง นำ HTML 5 มาใช้ ซึ่งเป็น เทคโนโลยีล่าสุด ในตอนนี้ มาพัฒนาเว็บไซต์ของเรากันเถอะ คุณจึงไม่ต้อง ติดตั้งแอป หรือติดตั้งโปรแกรมเพิ่มเติม เพียง เปิดเว็บเบราว์เซอร์ บนอุปกรณ์ที่ คุณใช้อยู่ และเยี่ยมชม เว็บไซต์ของเรา คุณสามารถ สนุกกับสล็อตได้ทันที
การใช้งานกับอุปกรณ์หลากหลาย
ไม่ว่าคุณจะใช้ สมาร์ทโฟน ระบบ แอนดรอยด์ หรือ ไอโอเอส ก็สามารถ เล่นสล็อตได้อย่างราบรื่น ระบบของเรา ได้รับการออกแบบให้รองรับ ระบบปฏิบัติการทั้งหมด ไม่สำคัญว่าคุณ ใช้ โทรศัพท์ รุ่นใหม่หรือรุ่นเก่า หรือ แม้แต่แท็บเล็ตหรือแล็ปท็อป ทุกอย่างก็สามารถ ใช้งานได้ดี ไม่มีปัญหา ความเข้ากันได้
เล่นได้ทุกที่และทุกเวลา
ข้อดีของการเล่น PG Slot คือ คุณสามารถ เล่นได้ทุกเวลา ไม่ว่าจะ อยู่ที่บ้าน ที่ทำงาน หรือแม้แต่ ในที่สาธารณะ สิ่งที่คุณต้องมีคือ การเชื่อมต่ออินเทอร์เน็ต คุณสามารถ เริ่มเกมได้ทันที และคุณไม่ต้อง ห่วงเรื่องการดาวน์โหลด หรือติดตั้งโปรแกรมที่ ใช้พื้นที่ในอุปกรณ์
ลองเล่นสล็อตแมชชีนฟรี
เพื่อให้ ผู้ใช้ใหม่ มีโอกาสลองและสัมผัสประสบการณ์สล็อตแมชชีนของเรา PG Slot ยังเสนอบริการสล็อตทดลองฟรีอีกด้วย คุณสามารถ เริ่มเล่นได้ทันทีโดยไม่ต้องลงทะเบียนหรือฝากเงิน การ เล่นฟรีนี้จะช่วยให้คุณเข้าใจวิธีเล่นและรู้จักเกมก่อนลงเดิมพันจริง
บริการและการรักษาความปลอดภัย
PG Slot ตั้งใจให้บริการที่ดีที่สุดกับลูกค้า เรามี ทีมงานพร้อมบริการคุณตลอดเวลา นอกจากนี้เรายังมี ระบบรักษาความปลอดภัยที่ทันสมัย ด้วยวิธีนี้ คุณจึงมั่นใจได้ว่า ข้อมูลส่วนบุคคลและธุรกรรมทางการเงินของคุณจะได้รับการปกป้องอย่างดีที่สุด
โปรโมชั่นและโบนัสพิเศษ
อีกข้อดีของการเล่นสล็อตกับ PG Slot ก็คือ มี โปรโมชันและโบนัสมากมาย ไม่ว่าคุณจะเป็น สมาชิกใหม่หรือเก่า คุณสามารถ รับโปรโมชันและโบนัสได้ สิ่งนี้จะ เพิ่มโอกาสชนะและสนุกกับเกมมากขึ้น
สรุปการเล่นสล็อตเว็บที่ PG Slot ถือเป็นการลงทุนที่คุ้มค่า คุณจะไม่เพียงได้รับความสุขและความสะดวกสบายจากเกมเท่านั้น แต่คุณยังมีโอกาสลุ้นรับรางวัลและโบนัสมากมายอีกด้วย ไม่สำคัญว่าจะใช้โทรศัพท์มือถือ แท็บเล็ต หรือคอมพิวเตอร์รุ่นใด สามารถมาร่วมสนุกกับเราได้เลยตอนนี้ อย่ารอช้า ลงทะเบียนและเริ่มเล่นสล็อตกับ PG Slot วันนี้!
Real Madrid midfielder Rodrigo https://rodrygo.prostoprosport-ar.com gave Madrid the lead in the Champions League quarter-final first leg against Manchester City. The meeting takes place in Madrid. Rodrigo scored in the 14th minute after a pass from Vinicius Junior.
MEBELZOOM предлагает только высококачественную продукцию. Все изделия сертифицированы и соответствуют всем необходимым стандартам РФ. Вы можете связаться с нашей службой поддержки при возникновении вопросов. У нас работают сотрудники с достаточным опытом работы в мебельном бизнесе. Ищете магазин недорогой мебели? Mebelzoom.ru – сайт, где вы найдете большой ассортимент мебели. Гарантируем доступные цены, быструю доставку и отменное качество товаров. Обращайтесь к нам, мы готовы предоставить вам квалифицированную помощь.
I’d like to find out more? I’d like to find out more details.
ms.wizmedic.com/bbs/board.php?bo_table=news&wr_id=94
click2connect.buzz/index.php?do=/public/user/blogs/name_Alanpoe/page_5/
bbs.blueplatform.org/space-uid-31463.html
appleincub.ru/page/11
medik-look.ru/kupit-diplom-onlayn-udobno-i-byistro
Staying Calm: Keeping a cool head and avoiding impulsive decisions during gameplay.
demo game
Посмотреть дораму или любимый фильм с друзьями на расстоянии очень легко, у нас! Несколько движений – все, что необходимо для сотворения собственной кинокомнаты + делимся ссылкой на нее с другом! Ищете сайт для совместного просмотра фильмов с друзьями? Unotalone.su – сайт, где есть возможность детальнее посмотреть информацию. Время таймлайна видео всех участников комнаты автоматически каждую секунду с ее владельцем синхронизируется. Помимо прочего, вы можете лично плеером управлять: регулировать качество и громкость, также ставить на паузу. Удачного вам просмотра!
south park смотреть бесплатно https://southpark-serial.ru
Interactive Interface: Players can interact with the game in real-time, making decisions that impact their
play game
На сайте https://xakexpert.com/ вы найдете профессионального и компетентного хакера, который поможет вам решить самую сложную задачу, которая требует усидчивости и повышенного внимания. Здесь у вас получится заказать взлом почты, отслеживание и другие важные услуги. Если и вы подозреваете своих близких людей в нечестности, мужа в измене, а сотрудников в краже, то необходимо быстрее воспользоваться такой услугой. Если нашли подходящего специалиста, то нужно быстрее с ним связаться через чат. Услуги не будут стоить дорого.
south park смотреть бесплатно южный парк смотреть онлайн
жк казань купить квартиру https://nedvizhimost-47.ru
ремонт ноутбуков
Any work should open with the question “why?” The stroibloger.com answer is actually simple – customer service needs help to help people.
stagramer.com
Fair Play Policies and RNG
aviator game demo
купить квартиру в новостройке от застройщика купить квартиру в казани новостройка от застройщика
Игра «Hamster Kombat» пользуется популярностью и обещает быструю прибыль. Для запуска ее необходимо воспользоваться в мессенджере Telegram официальным ботом. Вам не потребуется вносить реальные деньги. Приглашаем вас окунуться в захватывающий мир боевых хомяков. Ищете хамстер комбат бот? Hamster-kombat-bot.io – сайт, где можно найти о проекте интересующую информацию. Здесь узнаете, как начать игру в «Хамстер Комбат». Ознакомьтесь с информацией уже сейчас. В игре у вас есть возможность своего хомяка прокачать и получить приличный доход благодаря Telegram.
На сайте https://moredoram.ru вы найдете дорамы, фильмы, сериалы высокого качества. Они понравятся всем любителям такого жанра и помогут расслабиться после трудового дня и просто получить приятные эмоции. Вы сможете воспользоваться функцией случайной дорамы, изучить список лучших из них. Все они в отличном качестве, с безупречным звуком, что позволит насладиться просмотром на любом устройстве, включая смартфон, ПК, планшет. Регулярно появляются многообещающие новинки, с которыми необходимо ознакомиться и вам.
Hey there! This post couldn’t be written any better! Reading this post reminds me of my good old room mate! He always kept talking about this. I will forward this post to him. Fairly certain he will have a good read. Thank you for sharing!
janews.com.au/modules/newbb/viewtopic.php?topic_id=6875&forum=12&post_id=6875
balivillarental.net/villarental/villa_maridadi.html
mydoggymatch.com/read-blog/601_where-to-order-a-diploma-or-certificate-at-a-adequate-price.html?mode=night
http://www.sitebs.ru/blogs/95000.html
forum.drustvogil-galad.si/index.php?topic=10004.0
Bukmeker.website предлагает исключительно интересную и важную информацию. С радостью поможем вам разобраться в мире букмекерских ставок. Расскажем, каковы типичные условия отыгрыша фрибета. Ищете cтавки на спорт? Bukmeker.website – портал, где мы занимательными советами с вами делимся. Говорим о том, что нужно сделать, чтобы быть успешным игроком. Вы узнаете, как выбрать надежную букмекерскую контору и что делать, если бонус не был начислен. Научитесь принимать верные решения при размещении ставок. Присоединяйтесь к нам прямо сейчас!
can also help in making informed cash-out decisions.
aviator game
Safety is paramount when playing online games. Players should ensure they are playing on reputable platforms
aviator game demo
На сайте https://lan-union.ru предлагается к покупке сетевое и кабельное оборудование. В каталоге компании вы найдете подробное описание, также характеристики продукции и товаров производителя. На сайте вы можете увидеть сертификаты на продукцию, и детальнее ознакомиться с сервисом. Из преимуществ компании, можно отметить быструю логистику, высочайшее качество оборудования и расширенную гарантию. Для того чтобы быть в курсе акций и новостей компании, подпишитесь на рассылку.
teplica-parnik.net
Карьерный коуч https://vminske.by/fashion/kto-takie-karernye-konsultanty — эксперт рынка труда, который помогает людям определить свои карьерные цели, развиваться в выбранной области и достигать успеха в профессиональной деятельности.
купить квартиру в казани https://kupit-kvartiru47.ru
Мы предлагаем услуги по изготовлению и монтажу металлоконструкций в Воронеже https://specstroy36.ru/ и Воронежской области. Команда профессиональных специалистов готова выполнить проект любой сложности и размера. Мы работаем с различными типами металла, чтобы удовлетворить все потребности клиентов. Наше оборудование высокотехнологично и позволяет точно выполнять все металлообрабатывающие операции. СпецСтрой36 гарантирует высокое качество продукции, долговечность и надежность конструкций. Вы сможете получить индивидуальный подход и решение, которое соответствует вашим требованиям и бюджету. Свяжитесь с нами, чтобы обсудить ваши потребности и получить бесплатную консультацию. Специалисты компании всегда готовы помочь воплотить любой проект с использованием металлоконструкций.
Risk Management: Setting limits on how much to bet and when to cash out.
How to play aviator online casino
На сайте https://moduleo-shop.ru/ вы сможете приобрести кварц-виниловую плитку, которая отличается удобной акустикой, привлекательным и красивым внешним видом. При этом конструкции очень простые в уходе, отсутствует эффект вдавливания. Материал является полностью водостойким. Есть возможность подобрать абсолютно любую цветовую гамму, которая отлично впишется в дизайн. Все расценки являются доступными, а сделать заказ получится в любое время. Материал высокого качества, а процесс оформления заказа максимально простой.
На сайте https://agrotechelit.ru закажите звонок для того, чтобы получить консультацию по поводу покупки оборудования для теплиц, а также парников. При этом поставки организуются по России. Компания «АГРОТЕХЭЛИТ» в течение долгого времени занимается производством, реализацией тепличной техники. Также есть возможность заказать и различные полезные комплектующие. Продукция продается по лучшим ценам. Все товары отличного качества. А прямо сейчас ознакомьтесь с хитами продаж и актуальными товарами.
With the right approach, the besttoday.org entire process of assembling the gazebo and installing it takes a couple of hours. To prevent the structure from losing its decorative appearance, fastening materials should be stored in inconspicuous places. Or close them with special devices.
На сайте https://ventilyatory-77.ru/ приобретите качественные, надежные и функциональные вентиляторы, которые помогут вам получить дома или в офисе приятную обстановку и избавиться от изнуряющей жары. В магазине представлены как напольные, так и настенные вентиляторы, а также потолочные – огромное многообразие моделей для всех желающих. Любая категория имеет определенный набор функций. Ассортимент магазина детально отобран для того, чтобы все устройства прослужили как можно дольше. Воспользуйтесь оперативной доставкой.
Результат работы студии «Мята» – идеальный интерьер, который полностью соответствует вашим ожиданиям. Команда студии состоит из квалифицированных сотрудников. Предлагаем наилучшие цены на дизайн, гарантируем компетентность и ответственность. Мы завоевали доверие наших клиентов. Ищете студия дизайна в ташкенте? Tashkent.studio-mint.pro – сайт, где вы найдете отзывы о нас, посмотрите их уже сегодня. Нас рекомендуют знакомым и друзьям. Позвоните нам, и закажите дизайн интерьера. На протяжении всего проекта мы открыты к диалогу. Исполним вашу мечту!
Licensing and Regulation
Why should you play aviator demo
LEMON CAR – автосервис с хорошей репутацией, который предоставляет услуги по приемлемой стоимости. Здесь трудится компетентная команда мастеров. Они используют только новейшее оборудование и готовы о вашей машине позаботиться. https://lemon-car.ru – сайт, где есть возможность узнать сроки и актуальные цены. Клиенты автосервиса на высшем уровне оценивают качество обслуживания и скорость. Позвоните нам, и мы дадим вам грамотную консультацию. С помощью LemonCar ваше авто будет выглядеть ухоженно и надежно работать очень долгое время.
услуги seo оптимизация сео оптимизация сайта
seo продвижение сайта сколько стоит заказать сео продвижение сайта
Software Requirements
Does aviator crash have a demo version
создание и продвижение сайта https://prodvizhenie-saytov43.ru
seo продвижение сайтов seo услуги
Не знаете, как решить свои финансовые проблемы? ЗАЙМБОТ поможет вам в этом. Вы сможете за несколько минут оформить займ. Ищете список реальных мфо? T.me/zaimys – тут вы найдете информацию о кредитах, микрозаймах и выгодных займах. Забудьте о длительных очередях, долгосрочных процедурах и бюрократии! Предлагаем людям в экстренных ситуациях необходимую поддержку. Делаем процесс займа прозрачным и удобным, заботимся о вашем комфорте. Не нужно на потом откладывать свои планы. Получите деньги прямо сейчас и воплощайте в реальность свои задумки!
cash-out perfectly.
Aviator game APK
Студия «Мята» грамотно занимается дизайном интерьеров. У нас трудятся компетентные сотрудники с необходимым образованием. Радуем своих клиентов успешными проектами. Гарантируем реализацию ваших желаний. При сотрудничестве с нами, вы существенно сэкономите личный бюджет. Ищете студия дизайна в ереване? Yerevan.studio-mint.pro – сайт, где узнаете больше информации о нашей компании. Все задачи выполняем в указанный срок. Находим подход к каждому клиенту и предоставляем полезные советы. С удовольствием ответим на все ваши вопросы, обращайтесь прямо сейчас.
На сайте https://runobe.ru почитайте ранобэ онлайн и в отличном качестве. Все они на русском языке, а потому насладиться чтением сможет каждый. Все произведения имеют интересный сюжет, непредсказуемую развязку, а потому понравятся всем без исключения. Выбор японских романов обновляется ежедневно, чтобы вы смогли найти то, что действительно вам нравится. Вы можете ознакомиться сразу с несколькими, чтобы определиться с тем, какие из них вам нравятся больше. Для того чтобы подыскать определенный вариант, необходимо воспользоваться специальным поиском.
A completely free schedule allows you to plitki.com consider working as a courier as a full-time job or part-time job.
seo продвижение цена https://prodvizhenye-seo.ru
To play the Aviator Game, you need a device with internet access and a web browser that supports HTML5. This
How to play Aviator demo online
На сайте https://jidkie-oboi-77.ru/ в огромном выборе находятся жидкие обои. К их важным преимуществам относят простоту нанесения, а потому решить задачу под силу даже дилетанту, который ни разу с этим не сталкивался. Важным моментом является то, что обои маскируют дефекты, неровности стен. Выбирая материал, необходимо учитывать следующие моменты: определитесь с цветовой гаммой, а также целями приобретения. Важно, чтобы цветовая гамма идеально вписалась в интерьер. Есть как шелковые, так и хлопковые.
By carrying out timely pronovosti.org cleaning of your home, a person extends the life of furniture, flooring and other materials. The cleaning company’s employees treat all types of surfaces with care, using only professional products in their work.
Several key developers and companies have played a significant role in the development and success of the
Aviator game app
Easy Payments – ваш надежный помощник в запуске бизнеса на международном рынке. Берем все задачи на себя, экономя время клиента. Наши действия соответствуют международным законам, не используем какие-либо подозрительные схемы. Гарантируем конфиденциальность данных. Ищете регистрация компании в UK? Easypayments.online – сайт, где можно подробно ознакомиться с информацией и отзывами о нас. По всем интересующим вопросам проконсультируем абсолютно бесплатно, мы разбираемся в нюансах регистрации фирм за рубежом. Обращайтесь!
High-quality timber stroihome.net is resistant to aggressive environmental influences. Does not fade and tolerates low temperatures. Long service life.
Can I Play the Aviator Game on Mobile?
aviator app
Мята – студия, которая компетентно подходит к оформлению интерьеров. У нас в команде трудятся исключительно профессиональные специалисты с профильным образованием. Своих заказчиков всегда радуем успешными проектами. Ваше желание мы реализуем. С нами сможете сэкономить свой бюджет. Ищете дизайн проект квартиры в тбилиси? Tbilisi.studio-mint.pro – сайт, где у вас есть возможность узнать, как выполняется сотрудничество с компанией. Ознакомиться с информацией можно прямо сейчас. Гарантируем осуществление задачи точно в срок. Находим контакт с любым клиентом и даем много ценных советов. Обращайтесь к нам!
Hello! Do you use Twitter? I’d like to follow you if that would be okay. I’m absolutely enjoying your blog and look forward to new posts.
shop.electricoresigns.com/index.php?route=information/blogger&blogger_id=6
http://www.olimpicxativa.com/abonos.htm
etlapok-gyartasa.hu/portfolio/kiegeszitok-cash-box/
blog-doma.ru/proizvodstvo-biogumusa
myweektour.ru/page/4/
Visit the website https://www.sparklo.com/ – this is a unique offer for recycling garbage and waste. Our reversible vending machines or spark machines can turn your trash into treasure. Making recycling fun produces proven results! This is a solution from the future! More details on the website.
Key Developers and Companies Involved
aviator game
На сайте http://mvpol.ru/ закажите смету для того, чтобы узнать стоимость промышленных полов. Среди основных услуг выделяют: текущий ремонт полов, промышленные наливные полы, бетонные полы, у которых упрочненный верх. Также можно воспользоваться и предварительным сметным расчетом. В компании производят наливные полы для парковок, холодильных комбинатов, автосервисов, торговых центров. Все выполнено из качественных и надежных материалов, которые прослужат долго, не потрескаются, сохранят внешний вид.
First of all, it should be 365newss.net clearly understood that these are completely different concepts in geography. For example, when considering absolute height, it is precisely this that acts as the most important indicator, which is measured in meters, thereby determining the height of geographical objects above sea level.
На сайте https://moyuschie-pylesosy.ru/ в огромном выборе находятся моющие пылесосы, которые будут необходимы в каждом доме. К важным преимуществам подобных устройств относят то, что они смогут провести быструю, комфортную уборку любой поверхности, качественно очистят от пыли и различных загрязнений. Устройства эффективно справятся с самыми разными пятнами быстро, эффективно и без проблем. Дополнительно устройство поддерживает чистоту воздуха. Покупая устройство, необходимо ориентироваться на такие параметры, как: мощность, объем бака.
ensures compatibility across various platforms without the need for additional software downloads.
aviator demo
While the game itself is free to access, playing involves placing bets with real money. Some platforms may offer
aviator demo
balforum.net
Pattern Analysis: Studying the game’s patterns and trends to predict optimal cash-out times.
aviator demo
canadatc.com
На сайте https://turk-kino.ru посмотрите интересное и запоминающееся турецкое кино вместе с другом. Есть такие именитые картины, как «Запах клубники», «Зимородок», «Великолепный век» и многое другое. Для того чтобы начать совместный просмотр, необходимо создать комнату. Сделать это получится в 3 шага, а инструкция прилагается. Перед вами многообещающие новинки, а также топ лучших фильмов за 2024 год. Во всех фильмах играют ваши любимые актеры, звучит приятная музыка. Есть подборка рекомендованных фильмов, которые выбирают многие.
Please let me know if you’re looking for a writer for your site. You have some really good articles and I feel I would be a good asset. If you ever want to take some of the load off, I’d really like to write some material for your blog in exchange for a link back to mine. Please blast me an email if interested. Thank you!
admvoznesenie.ru/officials/blogs/history.php?PAGEN_1=48
vet-aibolit.ru/about
iawbs.com/home.php?mod=space&uid=792962&do=profile&from=space
ik21v.ru/
http://www.gimnazija-ivanjica.edu.rs/mobilearn/claroline/phpbb/viewtopic.php?topic=141&cidReset=true&cidReq=INF1%20
homeprorab.info
https://autolux-azerbaijan.com/# pin-up 141 casino
Cryptolegal Services специалисты компании знают обо всех тонкостях крипторегулирования. Воспользуйтесь нашими премиальными юридическими услугами, связанными с криптовалютой прямо сейчас. Ищете недвижимость за криптовалюту в дубае? Ru.cryptolegalservices.io – сайт, где имеется подробная информация, посмотрите ее уже сегодня. Обслуживаем крупные криптовалютные биржи и частных лиц. Позволяем в вашу пользу применять закон. Поможем минимизировать риски и увеличить вашу прибыль. Обращайтесь к нам!
Yes, the Aviator Game is compatible with mobile devices. Players can enjoy the game on their smartphones or
aviator demo
madeintexas.net
become more comfortable with the gameplay. Observing patterns and understanding the timing of the plane’s ascent
aviator demo
Pin Up Azerbaycan ?Onlayn Kazino: Pin Up Azerbaycan ?Onlayn Kazino – pin-up 141 casino
To use, you simply need to instukzia.com drive the forklift up to the load and then lift it with a fork. Next, the goods are raised to a safe height and transported to the prospect of long-term storage. To make the use of equipment simple and fast, it is very important to store everything on special pallets, which are specifically designed to make it easier to lift the stored goods.
Common Feedback and Suggestions
aviator demo
Мята – студия дизайна интерьеров. Мы оказываем услуги в любой точке мира и любим свое дело. Нас вдохновляют интересные проекты, трудных задач мы не боимся. Всегда готовы реализовать вашу мечту. Ищете дизайн интерьера в уфе? Ufa.studio-mint.ru – сайт, где имеется портфолио работ. Здесь у вас есть возможность прочесть отзывы наших благодарных клиентов. Вы будете приятно удивлены внимательностью к деталям и сроком разработки проекта. Гарантируем оптимальную стоимость. Придерживаемся высоких стандартов в области обслуживания. Обращайтесь к нам, учтем все ваши пожелания!
Hello, I think your site might be having browser compatibility issues. When I look at your blog site in Safari, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, wonderful blog!
mobix.com.ua/index.php?links_exchange=yes&page=41
spg.co.kr/bbs/board.php?bo_table=cus_res&wr_id=92&sca=%EC%98%81%EC%97%85%EC%A7%80%EC%9B%90&page=55
mysoccerex.com/tag/football-club/
chefrobertsdirect.com/index.php?main_page=page&id=2
http://www.sljlz.cn/home.php?mod=space&uid=181463
Mob25.com предоставляет для вас интересную и занимательную информацию. Здесь найдете новости, статьи и книги на различную тему. Узнаете, что можно засолить вместо селедки, как с помощью яркой плитки создать шедевры декора, почему француженки не носят Шанель, как сделать школьника отличником. Ищете биографии и мемуары? Mob25.com – сайт, где представлен каталог книг. У нас научитесь выбирать безопасную косметику и избавитесь от проблем с кожей. Имеется поиск, воспользуйтесь им прямо сейчас. Заходите на наш портал с книгами!
https://autolux-azerbaijan.com/# pin-up 141 casino
Watch the Plane Ascend: The plane takes off and starts climbing.
aviator demo
Pin Up Kazino ?Onlayn: pin-up360 – Pin-up Giris
Risk Management: Setting limits on how much to bet and when to cash out.
aviator demo
Известная игра Hamster Kombat обещает оперативный заработок. Запустить ее можете через официального бота в телеграме. Ничего платить реальными деньгами не нужно. У игры Хамстер Комбат хорошие отзывы, предлагаем вам окунуться в увлекательный мир боевых хомяков. https://hamster-kombat-bot.io – сайт, где имеется вся информация о проекте. Вы узнаете, как в Hamster Kombat начать играть. Ознакомиться с информацией можно прямо сейчас. В игре можно прокачать хомяка и применяя Telegram, зарабатывать.
На сайте https://avtodom.car-trip.ru/ оставьте заявку для того, чтобы устроить увлекательное путешествие на трейлере. В автодоме предусмотрено все необходимое для вашего комфорта, чтобы вы удобно расположились внутри. При этом имеется все необходимое для того, чтобы вы ощущали себя комфортно. Имеются различные варианты автодомов, среди которых вы подберете решение для себя. Внутри находятся соляные батареи, газовая плита, раковина, а также столовая зона и многое другое, включая мангал и москитные сетки.
Player reviews and testimonials are overwhelmingly positive, with many praising the game’s exciting gameplay and
aviator demo
На сайте https://kuhonnye-vytyazhki.ru/ представлены в большом выборе кухонные вытяжки, которые положительным образом влияют на качество воздуха в помещении. Дополнительно отлично впишутся в дизайн и станут его яркой деталью. Вытяжки идеально сочетают функциональность и огромный набор ценных опций. Выбирая подходящий вариант, необходимо полагаться на такие параметры, как: размер вытяжки, который больше всего подходит для вашей кухни. Также учтите и мощность устройства. Установлены привлекательные расценки.
Мята – студия, где работает команда квалифицированных сотрудников. Мы успешно трудимся в области дизайна интерьера и свое дело очень любим. Разрабатываем проекты высокого уровня. Оказываем услуги по привлекательной цене и в адекватные сроки. Ищете дизайн квартиры в новосибирске? Novosibirsk.studio-mint.ru – сайт, где можете прямо сейчас рассчитать стоимость проекта. Также тут можно ознакомиться с нашими работами и отзывами клиентов. Каждый проект уникален и тщательно продуман. Готовы выполнить любые ваши пожелания. Обращайтесь, обсудим все детали.
На сайте https://ocims.ru/ закажите звонок для того, чтобы воспользоваться такой услугой, как строительство каркасных домов высокого качества. Они надежные, практичные, а самое главное, что простоят очень долго. Все работы происходят под ключ. Дома строятся по индивидуальному, а также типовому проекту, что позволит подобрать то, что соответствует предпочтениям, вкусам. На работы, материалы даются гарантии. Действуют привлекательные и доступные расценки. Также компания предлагает приятный презент по окончании проведения работ.
Pin Up Azerbaycan ?Onlayn Kazino: ?Onlayn Kazino – pin-up 141 casino
experiences. These communities provide valuable insights and foster a sense of camaraderie among players.
aviator demo
Swampy and creeping soil. In such areas, slush constantly forms after even a light rain. In repaircanada.net this case, you will have to raise the soil level using sprinkling. It could be rubble.
uquest.net
demo versions or free play options to allow players to practice before betting real money.
aviator demo
Casino
https://uzfootball.ru/map1.html
https://starfielduniverse.com/index.php?title=Winrating.ru
https://cps-mediawiki.cs.rptu.de/index.php/User:RickeySolander
новые сервера л2 эссенс
Анонсы л2
increase the excitement of the game.
aviator demo
мониторинг серверов ла2
Сервера л2
Hi colleagues, good post and nice urging commented at this place, I am genuinely enjoying by these.
drosetourmanila.com/vn/retail_promo.html
score808.chat/blogs/4268/Where-to-buy-a-diploma-or-certificate-at-a-comfortable
http://www.kangas-industrial.com/e_feedback/index.asp?page=2769
mipon.net/bbs-c/clever.cgi/clever.cgi?page=280
aed-defibrillator.be/defibrillator_promo.asp?prod=67&sort_products=1&itemsPerpage=10
In such a situation, women18.com water will not accumulate under the gazebo, and it itself will be located on a hill.
https://autolux-azerbaijan.com/# Pin Up Azerbaycan
environment for players to enjoy the game. Some popular platforms include Name], Name], and
aviator demo
If we are talking about massive boxes, then they coloradonewss.com should also have a small platform under which you can crawl with a forklift, otherwise transportation will take much longer.
Vinicius Junior https://viniciusjunior.prostoprosport-ar.com is a Brazilian and Spanish footballer who plays as a striker for Real Madrid and the Brazilian national team. Junior became the first player in the history of Los Blancos, born in 2000, to play an official match and score a goal.
Kylian Mbappe https://kylianmbappe.prostoprosport-ar.com is a French footballer, striker for Paris Saint-Germain and captain of the French national team. He began playing football in the semi-professional club Bondi, which plays in the lower leagues of France. He was noticed by Monaco scouts, which he joined in 2015 and that same year, at the age of 16, he made his debut for the Monegasques. The youngest debutant and goal scorer in the club’s history.
Basic Rules and Objectives
aviator demo
На сайте https://dekorativnye-shtukaturki-77.ru/ в огромном многообразии находится декоративная штукатурка. Она необходима для того, чтобы разнообразить интерьер и сделать его более стильным и ярким. Для того чтобы принять окончательное решение, необходимо ознакомиться с каталогом. Штукатурка дает возможность создать удивительные узоры, интересные рисунки, которые станут яркой деталью. Этот материал отличается экологической чистотой, он полностью безопасен для здоровья людей, животных.
Pin-Up Casino: Pin Up Azerbaycan ?Onlayn Kazino – Pin Up Azerbaycan
enjoyable.
aviator demo
Karim Benzema https://karimbenzema.prostoprosport-ar.com is a French footballer who plays as a striker for the Saudi Arabian club Al-Ittihad. He played for the French national team, for which he played 97 matches and scored 37 goals. At the age of 17, he became one of the best reserve players, scoring three dozen goals per season.
На сайте http://koleso-na-hodu.ru каждый желающий получает возможность приобрести шины больших, а также редких размеров с оперативной доставкой по всему городу, области. Непосредственно на сайте у вас получится подобрать шины, исходя из таких параметров, как: ширина, высота профиля, диаметр, стоимость, производитель, сезонность. Вся продукция сертифицированная, качественная, оригинальная. Если остались вопросы, то заполните специальную форму со своими данными, чтобы менеджер перезвонил для уточнения определенных моментов.
I absolutely love your blog and find the majority of your post’s to be exactly what I’m looking for. Do you offer guest writers to write content in your case? I wouldn’t mind publishing a post or elaborating on a number of the subjects you write in relation to here. Again, awesome blog!
nation.geoman.ru/demogr/alph0014.shtml
wow-tour.ru/page/36
kanc4life.com.ua/index.php?links_exchange=yes&page=170&show_all=yes
sadovod63.ru/products
sport-faq.ru/page/4
Victor James Osimhen https://victorosimhen.prostoprosport-ar.com is a Nigerian footballer who plays as a forward for the Italian club Napoli and the Nigerian national team. In 2015, he was recognized as the best football player in Africa among players under 17 according to the Confederation of African Football.
britainsnews.com
https://autolux-azerbaijan.com/# Pin-Up Casino
dublindecor.net
Wow that was odd. I just wrote an extremely long comment but after I clicked submit my comment didn’t show up. Grrrr… well I’m not writing all that over again. Regardless, just wanted to say great blog!
#GGG###
http://chelmaps.ru/index.php?subaction=userinfo&user=amygiguj
На сайте https://mian.msk.ru/ ознакомьтесь с интересными, актуальными и ценными новостями, которые касаются самых разных сфер деятельности, включая экономику, политику и многое другое. Перед вами как совсем свежие и актуальные новости, так и те, что произошли вчера и на днях. Также имеется информация, которая касается игромании и того, как с ней бороться. Есть и интересные исследования ученых и информация, которая прольет свет на многое. Опубликованы данные про армию, культуру, технологии, летние виды спорта.
Pin Up: ?Onlayn Kazino – pin-up 141 casino
台灣線上娛樂城
台灣線上娛樂城是指通過互聯網提供賭博和娛樂服務的平台。這些平台主要針對台灣用戶,但實際上可能在境外運營。以下是一些關於台灣線上娛樂城的重要信息:
1. 服務內容:
– 線上賭場遊戲(如老虎機、撲克、輪盤等)
– 體育博彩
– 彩票遊戲
– 真人荷官遊戲
2. 特點:
– 全天候24小時提供服務
– 可通過電腦或移動設備訪問
– 常提供優惠活動和獎金來吸引玩家
3. 支付方式:
– 常見支付方式包括銀行轉賬、電子錢包等
– 部分平台可能接受加密貨幣
4. 法律狀況:
– 在台灣,線上賭博通常是非法的
– 許多線上娛樂城實際上是在國外註冊運營
5. 風險:
– 由於缺乏有效監管,玩家可能面臨財務風險
– 存在詐騙和不公平遊戲的可能性
– 可能導致賭博成癮問題
6. 爭議:
– 這些平台的合法性和道德性一直存在爭議
– 監管機構試圖遏制這些平台的發展,但效果有限
重要的是,參與任何形式的線上賭博都存在風險,尤其是在法律地位不明確的情況下。建議公眾謹慎對待,並了解相關法律和潛在風險。
如果您想了解更多具體方面,例如如何識別和避免相關風險,我可以提供更多信息。
I do not even know how I ended up here, but I thought this post was good. I do not know who you are but certainly you are going to a famous blogger if you are not already 😉 Cheers!
Портал о здоровье https://rezus.ru и здоровом образе жизни, рекомендации врачей и полезные сервисы. Простые рекомендации для укрепления здоровья и повышения качества жизни.
order piracetam 800 mg – purchase biltricide for sale buy sinemet 20mg generic
Toni Kroos https://tonikroos.prostoprosport-ar.com is a German footballer who plays as a central midfielder for Real Madrid and the German national team. World champion 2014. The first German player in history to win the UEFA Champions League six times.
https://glorycasinobangla.in/
Сервера ла2
live porn free
Glory Casino
live xxx cams
live naked men
porn live cam
Robert Lewandowski https://robertlewandowski.prostoprosport-ar.com is a Polish footballer, forward for the Spanish club Barcelona and captain of the Polish national team. Considered one of the best strikers in the world. Knight of the Commander’s Cross of the Order of the Renaissance of Poland.
волчонок онлайн хорошем качестве все сезоны https://volchonok-tv.ru
gaysex live free
nude live cams
shenale cam
couples nude webcam
shemele live
nude couple cam
промокоды cat casino
https://t.me/s/promokody_cat_casino
сериал волчонок сезон смотреть онлайн волчонок онлайн
buy piracetam 800 mg online – order generic praziquantel 600mg sinemet 20mg pills
free live pron
Mohamed Salah https://mohamedsalah.prostoprosport-ar.com is an Egyptian footballer who plays as a forward for the English club Liverpool and the Egyptian national team. Considered one of the best football players in the world. Three-time winner of the English Premier League Golden Boot: in 2018 (alone), 2019 (along with Sadio Mane and Pierre-Emerick Aubameyang) and 2022 (along with Son Heung-min).
Секреты успешного получения лицензии на недвижимость|Ключевая информация о лицензии на недвижимость|Подробное руководство по получению лицензии на недвижимость|Секреты быстрого получения лицензии на недвижимость|Разберитесь в процессе получения лицензии на недвижимость|Полезные советы по получению лицензии на недвижимость|Простой путь к получению лицензии на недвижимость|Как стать агентом с лицензией на недвижимость|Эффективные стратегии получения лицензии на недвижимость|Успешное получение лицензии на недвижимость: шаг за шагом|Процесс получения лицензии на недвижимость: как это работает|Как получить лицензию на недвижимость и стать успешным агентом|Основные шаги к успешной лицензии на недвижимость|Как стать агентом по недвижимости с лицензией: пошаговое руководство|Профессиональные советы по получению лицензии на недвижимость|Разберитесь в процессе получения лицензии на недвижимость: полное руководство|Шаги к успешной лицензии на недвижимость|Советы по успешному получению лицензии на недвижимость|Профессиональные советы по получению лицензии на недвижимость|Три шага к успешной лицензии на недвижимость|Простой путь к получению лицензии на недвижимость|Основные шаги к профессиональной лицензии на недвижимость|Инструкция по получению лицензии на недвижимость|Процесс получения лицензии на недвижимость: ключевые моменты|Как получить лицензию на недвижимость: основные принципы и стратегии|Лицензия на недвижимость: важные аспекты для успешного получения
How to Get a Real Estate License in Texas https://realestatelicensehefrsgl.com/states/texas-real-estate-license/ .
free live nude cam
Pedro Gonzalez Lopez https://pedri.prostoprosport-ar.com better known as Pedri, is a Spanish footballer who plays as an attacking midfielder for Barcelona and the Spanish national team. Bronze medalist of the 2020 European Championship, as well as the best young player of this tournament. Silver medalist at the 2020 Olympic Games in Tokyo. At the age of 18, he was included in the list of 30 football players nominated for the 2021 Ballon d’Or.
Шаги к получению лицензии на недвижимость|Легко и быстро получите лицензию на недвижимость|Подробное руководство по получению лицензии на недвижимость|Советы по получению лицензии на недвижимость|Разберитесь в процессе получения лицензии на недвижимость|Получите профессиональную лицензию на недвижимость|Лицензия на недвижимость: важные аспекты|Изучите основы получения лицензии на недвижимость|Эффективные стратегии получения лицензии на недвижимость|Успешное получение лицензии на недвижимость: шаг за шагом|Процесс получения лицензии на недвижимость: как это работает|Полезные советы по получению лицензии на недвижимость|Легкий путь к получению лицензии на недвижимость|Топ советы по получению лицензии на недвижимость|Профессиональные советы по получению лицензии на недвижимость|Эффективные стратегии для успешного получения лицензии на недвижимость|Шаги к успешной лицензии на недвижимость|Советы по успешному получению лицензии на недвижимость|Лицензия на недвижимость: ключ к успеху в индустрии недвижимости|Три шага к успешной лицензии на недвижимость|Получите лицензию на недвижимость и станьте профессиональным агентом|Как получить лицензию на недвижимость быстро и легко|Инструкция по получению лицензии на недвижимость|Секреты быстрого получения лицензии на недвижимость|Эффективные советы по успешному получению лицензии на недвижимость|Лицензия на недвижимость: важные аспекты для успешного получения
How to get a real estate license in Arizona How to get a real estate license in Arizona .
Секреты успешного получения лицензии на недвижимость|Все, что вам нужно знать о лицензии на недвижимость|Как начать карьеру в недвижимости с лицензией|Советы по получению лицензии на недвижимость|Разберитесь в процессе получения лицензии на недвижимость|Полезные советы по получению лицензии на недвижимость|Лицензия на недвижимость: важные аспекты|Изучите основы получения лицензии на недвижимость|Три шага к успешной лицензии на недвижимость|Успешное получение лицензии на недвижимость: шаг за шагом|Основные моменты получения лицензии на недвижимость|Как получить лицензию на недвижимость и стать успешным агентом|Основные шаги к успешной лицензии на недвижимость|Как стать агентом по недвижимости с лицензией: пошаговое руководство|Как получить лицензию на недвижимость легко и быстро|Эффективные стратегии для успешного получения лицензии на недвижимость|Шаги к успешной лицензии на недвижимость|Инструкция по получению лицензии на недвижимость|Лицензия на недвижимость: ключ к успеху в индустрии недвижимости|Легко получите лицензию на недвижимость с этими советами|Получите лицензию на недвижимость и станьте профессиональным агентом|Как получить лицензию на недвижимость быстро и легко|Шаги к успешной лицензии на недвижимость|Простой путь к получению лицензии на недвижимость|Три шага к профессиональной лицензии на недвижимость|Сек
How to get a real estate license in Michigan https://realestatelicensehefrsgl.com/states/michigan-real-estate-license/ .
Как получить лицензию на недвижимость|Все, что вам нужно знать о лицензии на недвижимость|Подробное руководство по получению лицензии на недвижимость|Успешные стратегии получения лицензии на недвижимость|Разберитесь в процессе получения лицензии на недвижимость|Получите профессиональную лицензию на недвижимость|Простой путь к получению лицензии на недвижимость|Изучите основы получения лицензии на недвижимость|Эффективные стратегии получения лицензии на недвижимость|Инструкция по получению лицензии на недвижимость|Процесс получения лицензии на недвижимость: как это работает|Секреты скорого получения лицензии на недвижимость|Основные шаги к успешной лицензии на недвижимость|Лицензия на недвижимость: ключ к успешной карьере|Профессиональные советы по получению лицензии на недвижимость|Разберитесь в процессе получения лицензии на недвижимость: полное руководство|Секреты получения лицензии на недвижимость от экспертов|Как быстро и легко получить лицензию на недвижимость|Ключевые моменты получения лицензии на недвижимость|Секреты успешного получения лицензии на недвижимость: что вам нужно знать|Получите лицензию на недвижимость и станьте профессиональным агентом|Как получить лицензию на недвижимость быстро и легко|Инструкция по получению лицензии на недвижимость|Простой путь к получению лицензии на недвижимость|Три шага к профессиональной лицензии на недвижимость|Сек
How to get a real estate license in Arizona How to get a real estate license in Arizona .
Как получить лицензию на недвижимость|Легко и быстро получите лицензию на недвижимость|Станьте лицензированным агентом по недвижимости|Секреты быстрого получения лицензии на недвижимость|Эффективные способы получения лицензии на недвижимость|Следуйте этим шагам для получения лицензии на недвижимость|Простой путь к получению лицензии на недвижимость|Как стать агентом с лицензией на недвижимость|Три шага к успешной лицензии на недвижимость|Лицензия на недвижимость для начинающих: советы и рекомендации|Основные моменты получения лицензии на недвижимость|Секреты скорого получения лицензии на недвижимость|Легкий путь к получению лицензии на недвижимость|Как стать агентом по недвижимости с лицензией: пошаговое руководство|Как получить лицензию на недвижимость легко и быстро|Как получить лицензию на недвижимость без стресса|Получение лицензии на недвижимость: лучшие практики и советы|Советы по успешному получению лицензии на недвижимость|Лицензия на недвижимость: ключ к успеху в индустрии недвижимости|Легко получите лицензию на недвижимость с этими советами|Получите лицензию на недвижимость и станьте профессиональным агентом|Как получить лицензию на недвижимость быстро и легко|Инструкция по получению лицензии на недвижимость|Процесс получения лицензии на недвижимость: ключевые моменты|Как получить лицензию на недвижимость: основные принципы и стратегии|Сек
How to get a real estate license in Illinois How to get a real estate license in Illinois .
dalycitynewspaper.com
buy 5000 tiktok followers cheap buy tiktok followers
На сайте https://pharmspirt.ru/ вы сможете подобрать уникальные и революционные решения из сферы хранения спиртов, прекурсоров, ЛВЖ. Среди основных сфер деятельности выделяют: оказание услуг для фармацевтических, химических, пищевых компаний. Предприятие оказывает профессиональный консалтинг, связанный с правилами хранения этилового спирта. Компания проводит и обучение: вебинары в сфере оборота спирта, спиртосодержащей продукции. Сотрудники прекрасно понимают программу, потому как она подается в простой форме.
I enjoy your blog posts, saved to my bookmarks!
buy tiktok likes and views buy tiktok likes
If you don’t mind, where do you host your weblog? I am looking for a very good web host and your webpage seams to be extremely fast and up most the time…
Продажа сигарет дешево блоками (поблочно), оптом и в розницу в Украине без предоплаты наложенным платежом: https://lostsmoke.org.ua/
Lionel Andres Messi Cuccittini https://lionelmessi.prostoprosport-ar.com is an Argentine footballer, forward and captain of the MLS club Inter Miami, captain of the Argentina national team. World champion, South American champion, Finalissima winner, Olympic champion. Considered one of the best football players of all time.
Cristiano Ronaldo https://cristiano-ronaldo.prostoprosport-ar.com is a Portuguese footballer, forward, captain of the Saudi Arabian club An-Nasr and the Portuguese national team. European Champion. Considered one of the best football players of all time. The best scorer in the history of football according to the IFFIS and fourth according to the RSSSF
найти человека по номеру телефона через спутник бесплатно без регистрации в реальном времени москва
найти местоположение по номеру телефона бесплатно
где находится телефон по номеру на карте онлайн бесплатно
Как получить лицензию на недвижимость|Легко и быстро получите лицензию на недвижимость|Как начать карьеру в недвижимости с лицензией|Советы по получению лицензии на недвижимость|Инструкция по получению лицензии на недвижимость|Полезные советы по получению лицензии на недвижимость|Лицензия на недвижимость: важные аспекты|Изучите основы получения лицензии на недвижимость|Как получить лицензию на недвижимость: советы экспертов|Лицензия на недвижимость для начинающих: советы и рекомендации|Процесс получения лицензии на недвижимость: как это работает|Как получить лицензию на недвижимость и стать успешным агентом|Получите лицензию на недвижимость и станьте профессионалом|Топ советы по получению лицензии на недвижимость|Советы по получению лицензии на недвижимость от профессионалов|Эффективные стратегии для успешного получения лицензии на недвижимость|Шаги к успешной лицензии на недвижимость|Инструкция по получению лицензии на недвижимость|Лицензия на недвижимость: ключ к успеху в индустрии недвижимости|Секреты успешного получения лицензии на недвижимость: что вам нужно знать|Получите лицензию на недвижимость и станьте профессиональным агентом|Как получить лицензию на недвижимость быстро и легко|Получение лицензии на недвижимость для начинающих: советы от экспертов|Процесс получения лицензии на недвижимость: ключевые моменты|Три шага к профессиональной лицензии на недвижимость|Лицензия на недвижимость: важные аспекты для успешного получения
How to get real estate license in Nevada How to get real estate license in Nevada .
Секреты успешного получения лицензии на недвижимость|Легко и быстро получите лицензию на недвижимость|Подробное руководство по получению лицензии на недвижимость|Советы по получению лицензии на недвижимость|Разберитесь в процессе получения лицензии на недвижимость|Получите профессиональную лицензию на недвижимость|Секреты успешного получения лицензии на недвижимость|Как стать агентом с лицензией на недвижимость|Три шага к успешной лицензии на недвижимость|Инструкция по получению лицензии на недвижимость|Основные моменты получения лицензии на недвижимость|Секреты скорого получения лицензии на недвижимость|Получите лицензию на недвижимость и станьте профессионалом|Топ советы по получению лицензии на недвижимость|Советы по получению лицензии на недвижимость от профессионалов|Разберитесь в процессе получения лицензии на недвижимость: полное руководство|Секреты получения лицензии на недвижимость от экспертов|Советы по успешному получению лицензии на недвижимость|Ключевые моменты получения лицензии на недвижимость|Три шага к успешной лицензии на недвижимость|Получите лицензию на недвижимость и станьте профессиональным агентом|Как получить лицензию на недвижимость быстро и легко|Инструкция по получению лицензии на недвижимость|Процесс получения лицензии на недвижимость: ключевые моменты|Как получить лицензию на недвижимость: основные принципы и стратегии|Лицензия на недвижимость: важные аспекты для успешного получения
How to get a real estate license in Illinois https://realestatelicensehefrsgl.com/states/illinois-real-estate-license/ .
Шаги к получению лицензии на недвижимость|Легко и быстро получите лицензию на недвижимость|Как начать карьеру в недвижимости с лицензией|Советы по получению лицензии на недвижимость|Разберитесь в процессе получения лицензии на недвижимость|Следуйте этим шагам для получения лицензии на недвижимость|Лицензия на недвижимость: важные аспекты|Как стать агентом с лицензией на недвижимость|Как получить лицензию на недвижимость: советы экспертов|Успешное получение лицензии на недвижимость: шаг за шагом|Процесс получения лицензии на недвижимость: как это работает|Секреты скорого получения лицензии на недвижимость|Легкий путь к получению лицензии на недвижимость|Топ советы по получению лицензии на недвижимость|Советы по получению лицензии на недвижимость от профессионалов|Как получить лицензию на недвижимость без стресса|Шаги к успешной лицензии на недвижимость|Советы по успешному получению лицензии на недвижимость|Лицензия на недвижимость: ключ к успеху в индустрии недвижимости|Легко получите лицензию на недвижимость с этими советами|Получите лицензию на недвижимость и станьте профессиональным агентом|Основные шаги к профессиональной лицензии на недвижимость|Инструкция по получению лицензии на недвижимость|Процесс получения лицензии на недвижимость: ключевые моменты|Как получить лицензию на недвижимость: основные принципы и стратегии|Лицензия на недвижимость: важные аспекты для успешного получения
How do you get a real estate license in Tennessee How do you get a real estate license in Tennessee .
Как получить лицензию на недвижимость|Ключевая информация о лицензии на недвижимость|Как начать карьеру в недвижимости с лицензией|Секреты быстрого получения лицензии на недвижимость|Эффективные способы получения лицензии на недвижимость|Получите профессиональную лицензию на недвижимость|Лицензия на недвижимость: важные аспекты|Как стать агентом с лицензией на недвижимость|Эффективные стратегии получения лицензии на недвижимость|Лицензия на недвижимость для начинающих: советы и рекомендации|Процесс получения лицензии на недвижимость: как это работает|Полезные советы по получению лицензии на недвижимость|Получите лицензию на недвижимость и станьте профессионалом|Лицензия на недвижимость: ключ к успешной карьере|Как получить лицензию на недвижимость легко и быстро|Разберитесь в процессе получения лицензии на недвижимость: полное руководство|Получение лицензии на недвижимость: лучшие практики и советы|Советы по успешному получению лицензии на недвижимость|Профессиональные советы по получению лицензии на недвижимость|Легко получите лицензию на недвижимость с этими советами|Простой путь к получению лицензии на недвижимость|Как получить лицензию на недвижимость быстро и легко|Получение лицензии на недвижимость для начинающих: советы от экспертов|Простой путь к получению лицензии на недвижимость|Три шага к профессиональной лицензии на недвижимость|Лицензия на недвижимость: важные аспекты для успешного получения
How to get real estate license in Ohio How to get real estate license in Ohio .
Онлайн казино с моментальными выплатами на реальные деньги онлайн – регистрация Twin Casino
узнать геолокацию по номеру
Yassine Bounou https://yassine-bounou.prostoprosport-ar.com also known as Bono, is a Moroccan footballer who plays as a goalkeeper for the Saudi Arabian club Al-Hilal and the Moroccan national team. On November 10, 2022, he was included in the official application of the Moroccan national team to participate in the matches of the 2022 World Cup in Qatar
Anderson Sousa Conceicao better known as Talisca https://talisca.prostoprosport-ar.com is a Brazilian footballer who plays as a midfielder for the An-Nasr club. A graduate of the youth team from Bahia, where he arrived in 2009 ten years ago.
Шаги к получению лицензии на недвижимость|Все, что вам нужно знать о лицензии на недвижимость|Станьте лицензированным агентом по недвижимости|Успешные стратегии получения лицензии на недвижимость|Эффективные способы получения лицензии на недвижимость|Полезные советы по получению лицензии на недвижимость|Простой путь к получению лицензии на недвижимость|Изучите основы получения лицензии на недвижимость|Как получить лицензию на недвижимость: советы экспертов|Лицензия на недвижимость для начинающих: советы и рекомендации|Основные моменты получения лицензии на недвижимость|Как получить лицензию на недвижимость и стать успешным агентом|Основные шаги к успешной лицензии на недвижимость|Лицензия на недвижимость: ключ к успешной карьере|Профессиональные советы по получению лицензии на недвижимость|Как получить лицензию на недвижимость без стресса|Получение лицензии на недвижимость: лучшие практики и советы|Инструкция по получению лицензии на недвижимость|Ключевые моменты получения лицензии на недвижимость|Три шага к успешной лицензии на недвижимость|Получите лицензию на недвижимость и станьте профессиональным агентом|Как получить лицензию на недвижимость быстро и легко|Получение лицензии на недвижимость для начинающих: советы от экспертов|Простой путь к получению лицензии на недвижимость|Как получить лицензию на недвижимость: основные принципы и стратегии|Сек
How to get your real estate license in Virginia https://realestatelicensehefrsgl.com/states/virginia-real-estate-license/ .
Как получить лицензию на недвижимость|Легко и быстро получите лицензию на недвижимость|Как начать карьеру в недвижимости с лицензией|Секреты быстрого получения лицензии на недвижимость|Эффективные способы получения лицензии на недвижимость|Полезные советы по получению лицензии на недвижимость|Лицензия на недвижимость: важные аспекты|Как стать агентом с лицензией на недвижимость|Как получить лицензию на недвижимость: советы экспертов|Лицензия на недвижимость для начинающих: советы и рекомендации|Секреты профессиональной лицензии на недвижимость|Как получить лицензию на недвижимость и стать успешным агентом|Основные шаги к успешной лицензии на недвижимость|Топ советы по получению лицензии на недвижимость|Профессиональные советы по получению лицензии на недвижимость|Разберитесь в процессе получения лицензии на недвижимость: полное руководство|Шаги к успешной лицензии на недвижимость|Советы по успешному получению лицензии на недвижимость|Лицензия на недвижимость: ключ к успеху в индустрии недвижимости|Три шага к успешной лицензии на недвижимость|Как стать агентом по недвижимости с лицензией|Основные шаги к профессиональной лицензии на недвижимость|Инструкция по получению лицензии на недвижимость|Простой путь к получению лицензии на недвижимость|Три шага к профессиональной лицензии на недвижимость|Лицензия на недвижимость: важные аспекты для успешного получения
How to get a real estate license in California https://realestatelicensehefrsgl.com/states/california-real-estate-license/ .
Шаги к получению лицензии на недвижимость|Легко и быстро получите лицензию на недвижимость|Станьте лицензированным агентом по недвижимости|Успешные стратегии получения лицензии на недвижимость|Эффективные способы получения лицензии на недвижимость|Следуйте этим шагам для получения лицензии на недвижимость|Секреты успешного получения лицензии на недвижимость|Изучите основы получения лицензии на недвижимость|Три шага к успешной лицензии на недвижимость|Лицензия на недвижимость для начинающих: советы и рекомендации|Секреты профессиональной лицензии на недвижимость|Секреты скорого получения лицензии на недвижимость|Легкий путь к получению лицензии на недвижимость|Как стать агентом по недвижимости с лицензией: пошаговое руководство|Советы по получению лицензии на недвижимость от профессионалов|Как получить лицензию на недвижимость без стресса|Получение лицензии на недвижимость: лучшие практики и советы|Как быстро и легко получить лицензию на недвижимость|Лицензия на недвижимость: ключ к успеху в индустрии недвижимости|Секреты успешного получения лицензии на недвижимость: что вам нужно знать|Как стать агентом по недвижимости с лицензией|Секреты успешного получения лицензии на недвижимость|Получение лицензии на недвижимость для начинающих: советы от экспертов|Простой путь к получению лицензии на недвижимость|Три шага к профессиональной лицензии на недвижимость|Сек
How to get a real estate license in New York How to get a real estate license in New York .
вавада казино официальный сайт вход
казино вавада
вавада рабочее зеркало на сегодня
Neymar da Silva Santos Junior https://neymar.prostoprosport-ar.com is a Brazilian footballer who plays as a striker, winger and attacking midfielder for the Saudi Arabian club Al-Hilal and the Brazilian national team. Considered one of the best players in the world. The best scorer in the history of the Brazilian national team.
Harry Edward Kane https://harry-kane.prostoprosport-ar.com is an English footballer, forward for the German club Bayern and captain of the England national team. Considered one of the best football players in the world. He is Tottenham Hotspur’s and England’s all-time leading goalscorer, as well as the second most goalscorer in the Premier League. Member of the Order of the British Empire.
вавада вход
Бесплатные игры на деньги с моментальными выплатами онлайн – леон бет
перевод с иностранных языков
best online pharmacies in mexico: mexican pharmacy – mexican online pharmacies prescription drugs
Получите дополнительные бонусы и фриспины в онлайн казино
лучшие онлайн казино беларуси онлайн казино .
перевод документов
перевод документов
ремонт мобильных телефонов в москве
апостиль в новосибирске
https://northern-doctors.org/# reputable mexican pharmacies online
https://telegra.ph/statistika-matchej-sport-06-26-2
перевод документов
апостиль в новосибирске
перевод с иностранных языков
перевод документов
ближайший ремонт телефонов
Зайдите на сайт Завода РемонтЯм https://xn--e1aoadejs8h.xn--p1ai/ который занимается производством и продажей дорожной техники для ремонта и содержания автомобильных дорог. Гарантия, бесплатный сервис, доставка по всей России. Собственное конструкторское подразделение, сервисная поддержка 24/7 – и многое другое для наших клиентов. Подробнее на сайте.
перевод с иностранных языков
Erling Breut Haaland https://erling-haaland.prostoprosport-ar.com is a Norwegian footballer who plays as a forward for the English club Manchester City and the Norwegian national team. English Premier League record holder for goals per season.
Почему стоит построить дом из бруса 9х12 | Как выбрать идеальный проект для дома из бруса 9х12 | Интерьер для дома из бруса 9х12: советы дизайнера | Секреты уютного интерьера в доме из бруса 9х12 | Выбор фундамента для дома из бруса 9х12 | Выбор фундамента для дома из бруса 9х12 | Сад и огород вокруг дома из бруса 9х12 | Современные технологии строительства дома из бруса 9х12 | Дом из бруса 9х12: важные моменты | Расходы на строительство дома из бруса 9х12
проект дома из бруса 9х12 https://domizbrusa-9x12spb.ru/ .
апостиль в новосибирске
mexico pharmacies prescription drugs: northern doctors – buying prescription drugs in mexico online
апостиль в новосибирске
Красные сушеные мухоморы на заказ c доставкой по России на сайте https://red-muhomor.ru/ это возможность купить высококачественные сушеные мухоморы для исследовательских, образовательных и декоративных целей. Зайдите в наш каталог, чтобы узнать больше о наших продуктах. Подробнее на сайте.
Скачать музыку https://audiobot.pro/ еще никогда не было так просто. Зайдите на сайт, ищите любимые треки или готовые музыкальные подборки, которые вы сможете скачать в один клик без регистрации. Лучшая коллекция mp3 в интернете на сайте. Каждый найдет для себя необходимый жанр и музыку. Скачивайте вашу музыку из ВК в телеграм, на компьютер, телефон или планшет.
перевод документов
На сайте https://iz-medi.ru/ предлагается к продаже большой ассортимент товаров из нержавеющей стали. Благодаря обслуживанию высочайшего качества, компания смогла создать надежную основу доверия среди потребителей, делающих приобретения у нас. Предлагаем большой выбор товаров, гибкие условия оплаты, дисконтные программы и оперативную доставку заказов. Мы имеем компетентную команду экспертов, которые дадут вам полезные рекомендации. На сайте вы можете подробнее ознакомиться с условиями оплаты и доставки, а также просмотреть каталог.
апостиль в новосибирске
ремонт телефонов в москве
Lineage 2
апостиль в новосибирске
перевод документов
Ali al-Buleahi https://ali-al-bulaihi.prostoprosport-ar.com Saudi footballer, defender of the club ” Al-Hilal” and the Saudi Arabian national team. On May 15, 2018, Ali al-Buleakhi made his debut for the Saudi Arabian national team in a friendly game against the Greek team, coming on as a substitute midway through the second half.
https://northern-doctors.org/# best online pharmacies in mexico
Добро пожаловать на наш ресурс, где вы найдете множество полезных статей на тему приемки недвижимости в новостройке или покупки квартиры с черновой отделкой. Узнайте, как обезопасить себя от ненадёжных застройщиков, какие проверки провести перед покупкой жилья, и о многом другом!
https://citadel-ca.ru
На сайте https://lan-union.ru предлагается к покупке сетевое и кабельное оборудование. В каталоге компании вы найдете подробное описание, также характеристики продукции и товаров производителя. На сайте вы можете увидеть сертификаты на продукцию, и детальнее ознакомиться с сервисом. Из преимуществ компании, можно отметить быструю логистику, высочайшее качество оборудования и расширенную гарантию. Для того чтобы быть в курсе акций и новостей компании, подпишитесь на рассылку.
перевод с иностранных языков
10 Things That Your Family Taught You About SEO Consultancy
London seo consultancy london
перевод с иностранных языков
апостиль в новосибирске
На сайте https://dekorativnye-shtukaturki-77.ru/ в огромном многообразии находится декоративная штукатурка. Она необходима для того, чтобы разнообразить интерьер и сделать его более стильным и ярким. Для того чтобы принять окончательное решение, необходимо ознакомиться с каталогом. Штукатурка дает возможность создать удивительные узоры, интересные рисунки, которые станут яркой деталью. Этот материал отличается экологической чистотой, он полностью безопасен для здоровья людей, животных.
Ваш путь к удаче: лучшие онлайн казино, попробовать.
Веселье и азарт: самые популярные онлайн казино, испытайте прямо сейчас.
Популярные азартные игры в онлайн казино, посетите прямо сейчас.
Играйте в лучшие онлайн казино и получайте щедрые бонусы и выигрыши, попробуйте прямо сейчас.
Новые возможности для азартных игроков в онлайн казино, посетите прямо сейчас.
Наши рекомендации: лучшие онлайн казино, испытайте сейчас.
Увлекательные игры и выигрыши в онлайн казино, испытайте прямо сейчас.
Играйте и выигрывайте большие суммы в лучших онлайн казино, попробуйте сейчас.
Играйте в азартные игры и выигрывайте захватывающие призы в онлайн казино, посетите прямо сейчас.
Лучшие бонусы и выигрыши в онлайн казино, испытайте прямо сейчас.
Новые возможности и азартные игры в онлайн казино, попробуйте прямо сейчас.
Играть и выигрывать: самые популярные онлайн казино для вас, испытайте сейчас.
Увлекательные игры и призы в онлайн казино, посетите прямо сейчас.
Большие выигрыши и возможности: самые популярные онлайн казино для вас, испытайте сейчас.
Популярные игры и призы в онлайн казино, посетите прямо сейчас.
Лучшие бонусы и выигрыши в онлайн казино, присоединяйтесь прямо сейчас.
Популярные возможности для азартных игроков в онлайн казино,
онлайн казино https://onlayn-kazino-reyting-belarusi.com/ .
перевод документов
mexican rx online: mexico drug stores pharmacies – purple pharmacy mexico price list
Скачать приложения для Андроид бесплатно на сайте https://appstoreandroid.ru/ такие как мессенджеры, социальные сети, экшен и многое другое. Бесплатные приложения для Андроид в огромном количестве позволят найти все самое необходимое для вас.
Зайдите на сайт https://autostrong-m.ru/ где вы сможете воспользоваться легким поиском новых и б/у запчастей с доставкой в России в интернет-магазине Автостронг! Купить автозапчасти легко – вы можете искать по номеру запчасти, по VIN автомобиля, по марке авто. Зайдите в каталог – запчасти представленные там – в наличии с отправкой в кратчайшие сроки. Подробнее на сайте.
апостиль в новосибирске
перевод документов
See Real – известная компания, специализирующаяся на наружной рекламе и светодиодных технологиях. Предлагаем выгодные цены и привлечем в бизнес новых клиентов. Будем рады обсудить с вами самую смелую идею. Стремимся к долгосрочному сотрудничеству. Оставьте свои данные, и мы в ближайшее время с вами свяжемся. Ищете реклама наружная изготовление? Iseer.kz – сайт, где можете узнать больше информации о нас и заказать звонок консультанта, чтобы он рассчитал стоимость. Квалифицированная команда к творческим вызовам готова. Оцените нашу работу!
апостиль в новосибирске
перевод с иностранных языков
Luka Modric https://lukamodric.prostoprosport-ar.com is a Croatian footballer, central midfielder and captain of the Spanish club Real Madrid, captain of the Croatian national team. Recognized as one of the best midfielders of our time. Knight of the Order of Prince Branimir. Record holder of the Croatian national team for the number of matches played.
перевод с иностранных языков
https://northern-doctors.org/# mexico pharmacy
Лучший секс блог о сексе и жизни: https://sexcloud.ru/
перевод с иностранных языков
Выбирайте из самых популярных онлайн казино в Румынии, чтобы выиграть крупный джекпот.
Выберите лучшие онлайн казино в Румынии, и стать богаче за считанные минуты.
Выбор казино онлайн для румынских геймеров, где можно получить массу бонусов и подарков.
Играйте в онлайн казино из Румынии, для захватывающего азартного опыта.
Играйте только в проверенных казино онлайн в Румынии, для возможности выиграть крупные суммы денег.
cazino online bani reali cazino online bani reali .
перевод документов
Блог о индивидуалках и сопутствующих социальных явлениях. Как проститутки живут в обществе, вся информация здесь: https://sexcloud.ru/
mexico drug stores pharmacies: mexican pharmacy online – purple pharmacy mexico price list
перевод с иностранных языков
перевод документов
перевод с иностранных языков
перевод документов
У нас вы найдете полезные статьи на тему недвижимости, например, покупка квартиры в новостройке, продажа и покупка недвижимости, юридическое сопровождение сделки.
Узнайте все нюансы, которые помогут вам принять правильное решение и осуществить успешную сделку с недвижимостью. Наши статьи помогут вам быть в курсе последних новостей и законов жилищного рынка, а также избежать недоразумений.
http://domzenit.ru
buy 1k tiktok followers buy followers tiktok
перевод с иностранных языков
ремонт смартфонов в москве
medicine in mexico pharmacies: Mexico pharmacy that ship to usa – mexican border pharmacies shipping to usa
advances, players can expect even more exciting features and enhancements to the gameplay experience.
jogo do tigrinho
Захватывающий мир онлайн казино, получайте щедрые призы в известных онлайн казино, играйте с удовольствием.
Надежность и азарт в онлайн казино, возможность выиграть становится выше.
Играйте в лучших онлайн казино, заходите и побеждайте.
Настоящий азарт в онлайн казино, выигрывайте и наслаждайтесь успехом.
Эффективные стратегии в онлайн казино, тренируйтесь и побеждайте.
лучшие онлайн казино с минимальным депозитом онлайн казино .
перевод с иностранных языков
buy tiktok followers tokmatik best site to buy tiktok followers
http://northern-doctors.org/# buying prescription drugs in mexico
перевод с иностранных языков
перевод с иностранных языков
перевод с иностранных языков
ремонт телефонов
Доверие – центр, который вас приглашает воспользоваться услугами. Запишитесь к психологу по номеру телефона на сайте. Семейный психолог делает так, чтобы для обоих супругов консультации были комфортными. https://ack-group.ru – сайт, где можно узнать более подробную информацию. Подростковый психолог выяснит уровень вашей проблемы и подберет подходящий способ ее решения. Цена консультации психолога доступна любому. Психолог в СПБ поможет урегулировать отношения с окружающими и с собой. Обращайтесь в любое время!
апостиль в новосибирске
buy tiktok followers instant buy 1000 tiktok followers cheap
апостиль в новосибирске
buying prescription drugs in mexico online: mexican pharmaceuticals online – buying prescription drugs in mexico online
buy tiktok followers cheap https://www.templates.com/blog/how-to-get-more-followers-on-tiktok-expert-tips/
перевод документов
апостиль в новосибирске
ремонт сотовых телефонов в москве
перевод документов
hydrea online order – how to get hydrea without a prescription order methocarbamol 500mg online cheap
the thrill of betting and cashing out. Common themes in reviews include the game’s fairness, the enjoyment of
tigrinho demo
перевод документов
Ищите тексты песен? Зайдите на сайт https://txtsong.ru/ где собрано более 185 000 текстов песен от 28 00 исполнителей. Пополнение базы новинками происходит каждый день. Любые группы, любые исполнители – все тексты песен для вас. Подробнее на сайте.
https://northern-doctors.org/# medication from mexico pharmacy
перевод с иностранных языков
перевод с иностранных языков
Читайте интересные статьи на актуальные темы, связанные с продажей жилья, например квартира от застройщика или налог на недвижимость.
Сайт: https://ooo-trotuar.ru
mexican rx online: mexican northern doctors – mexico pharmacies prescription drugs
перевод с иностранных языков
ремонт телефонов в москве
апостиль в новосибирске
Известная игра Hamster Kombat обещает оперативный заработок. Вы можете ее через официального бота в телеграмме запустить. Ничего платить реальными деньгами не нужно. У игры Хамстер Комбат хорошие отзывы, предлагаем вам окунуться в увлекательный мир боевых хомяков. https://hamster-kombat-bot.io – сайт, где имеется вся информация о проекте. Вы узнаете, как начать играть в Hamster Kombat. Ознакомиться с информацией можно прямо сейчас. В Хамстер Комбат можете прокачать своего хомяка и зарабатывать, используя Telegram.
перевод с иностранных языков
перевод с иностранных языков
hydroxyurea cheap – buy hydrea pills for sale methocarbamol order
перевод документов
Наши – гарантия надежности и долговечности.
перевод с иностранных языков
mexican drugstore online: best online pharmacies in mexico – mexican pharmacy
перевод с иностранных языков
Social Elements: Options for multiplayer gameplay and chat features enhance the social experience.
jogo do tigrinho demo
http://northern-doctors.org/# best online pharmacies in mexico
перевод документов
перевод документов
перевод документов
перевод документов
mexican rx online: purple pharmacy mexico price list – medicine in mexico pharmacies
перевод документов
перевод с иностранных языков
Почему стоит построить дом из бруса 9х12 | Почему стоит построить дом из бруса 9х12 | Как создать уютный интерьер в доме из бруса 9х12 | Как обеспечить эффективное отопление в доме из бруса 9х12 | Выбор материалов для теплоизоляции и вентиляции в доме из бруса 9х12 | Типы фундаментов для дома из бруса 9х12 | Современные технологии строительства дома из бруса 9х12 | Инновации в строительстве дома из бруса 9х12 | Советы по созданию уютной зоны отдыха в доме из бруса 9х12 | Сколько стоит построить дом из бруса 9х12
проект дома из бруса одноэтажный 9х12 https://domizbrusa-9x12spb.ru/ .
перевод с иностранных языков
game was designed to provide an adrenaline-pumping experience that mimics the thrill of gambling with a twist.
jogo do tigrinho
перевод с иностранных языков
https://northern-doctors.org/# purple pharmacy mexico price list
перевод с иностранных языков
перевод документов
Safety is paramount when playing online games. Players should ensure they are playing on reputable platforms
fortune tiger
http://northern-doctors.org/# mexican pharmaceuticals online
The best film magazin https://orbismagazine.com, film industry trade publications in 2024 to keep you informed with the latest video production, filmmaking, photographynews. We create beautiful and magnetic projects.
перевод с иностранных языков
апостиль в новосибирске
KissVK https://kissvk.pro/ это скачать музыку бесплатно в формате mp3 или слушать онлайн на сайте. Огромная коллекция треков всех годов и жанров. Новинки 2024 года, ТОП чарты, ТОП музыка, музыкальные подборки. Скачать музыку по настроению, в машину, на природу, для вечеринки в один клик на сайте.
апостиль в новосибирске
mexican pharmaceuticals online: Mexico pharmacy that ship to usa – mexico drug stores pharmacies
перевод с иностранных языков
перевод с иностранных языков
перевод с иностранных языков
purple pharmacy mexico price list: mexican northern doctors – mexican pharmaceuticals online
There are numerous online communities and forums where Aviator Game enthusiasts can share tips, strategies, and
tigrinho aposta
https://northern-doctors.org/# reputable mexican pharmacies online
Хотите купить занимательные сериалы на DVD? Serialexpress – это то, что вам нужно. У нас есть диски, которых вы ни в одном магазине не найдете. Качество сериалов великолепное, мы точно знаем, что вы останетесь своим приобретением, очень довольны. Товары в доступе по приемлемой цене, они упакованы очень хорошо. https://serialexpress.ru – портал, где имеется каталог, здесь можете ознакомиться и с оплатой. У нас есть накопительная скидочная система. Качество доставки вас удивит. Остались вопросы? Обратитесь за ответами к нашим компетентным менеджерам.
На сайте https://elektricheskie-kaminy.ru/ представлены электрические камины в огромном ассортименте. Эти конструкции подарят вашему дому незабываемый уют, комфорт. И самое важное, что они прослужат очень долго. Магазин предпринимает все возможное для того, чтобы процесс покупки был очень простым и понятным. Камины не выбрасывают в атмосферу вредные вещества. А для того, чтобы они начали обогревать, не потребуются дрова, а только розетка. Отсутствует открытый огонь, а потому возможность пожара сведена к минимуму.
Зайдите на сайт https://trc20casino.com/ где вы найдете Топ крипто казино в России 2024. Обзор, бонусы на депозит. Такие площадки дают возможность использовать цифровые монеты для депозитов и кешаута. Ознакомьтесь с обзорами, как ввести и вывести деньги, как пройти регистрацию и играйте в удовольствие!
Автозапчасти в Беларуси на сайте https://nikey.by/ это возможность купить в ассортименте автозапчасти, которых более 3 000 000, удобный поиск по VIN, а также номеру запчасти или марки автомобиля, а также большое количество различного масла, фильтров, расходников. Можно забрать самостоятельно или воспользоваться быстрой доставкой.
best online pharmacies in mexico: mexican northern doctors – mexican pharmacy
Взять займ или кредит
https://specclass.ru/wp-content/plugins/wp-postviews/views/news/post/1/3/19_kreditnaya_karta_pyat_pravil.html под проценты, подав заявку на денежный микрозайм для физических лиц. Выбирайте среди 570 лучших предложений займа онлайн. Возьмите микрозайм онлайн или наличными в день обращения. Быстрый поиск и удобное сравнение условий по займам и микрокредитам в МФО.
NGolo Kante https://ngolokante.prostoprosport-ar.com is a French footballer who plays as a defensive midfielder for the Saudi Arabian club Al-Ittihad and the French national team. His debut for the first team took place on May 18, 2012 in a match against Monaco (1:2). In the 2012/13 season, Kante became the main player for Boulogne, which played in Ligue 3.
К-ЖБИ производит большой ассортимент продукции отменного качества. Компания уже давно зарекомендовала себя с хорошей стороны. Мы постоянно развиваемся, гарантируем полное соблюдение сроков, приемлемые цены и высочайший уровень сервиса. Осуществляем оперативную доставку. Ищете цемент строительный с доставкой? Gbisp.ru – сайт, где найдете подробную информацию о нас, ознакомьтесь с ней. Здесь есть возможность оставить заявку, укажите свои контактные данные, и мы вам перезвоним. Вы получите компетентную консультацию. С нами выгодно сотрудничать!
перевод документов
Summary of Key Points
tigrinho aposta
На сайте https://shemi-otopleniya.ru/ вам предлагают качественную гибкую подводку из нержавеющей стали. Здесь вы сможете найти подробные характеристики с фото товара, а также увидеть всю продукцию. Вся гибкая подводка производится из высококачественной нержавейки. На сайте у вас есть возможность найти раздел с акциями и спецпредложениями. Гибкую подводку вы сможете приобрести под заказ самой разной модификации, диаметра и формы. Портал предлагает исчерпывающую информацию о гибкой подводке, ознакомьтесь с ней в любое удобное время.
A Step-By-Step Guide For Choosing The Right Tier Link Building In Seo
links Tier (http://www.anseongjumul.com)
https://avesis.acibadem.edu.tr/nadi.bakirci
https://hastane.harran.edu.tr/turizm/tr/icerik.aspx?detay=18
С нашими ваш автомобиль будет защищен круглый год.
На сайте https://zasos.fun/ вы найдете разные смачные приколы. Данный развлекательный сайт позволяет отдохнуть от тяжелой работы и окунуться в виртуальный мир развлечений. Здесь у вас есть возможность найти фильмы и сериалы, новости шоу-бизнеса, игры, юмористический контент, занимательные статьи и многое другое. На портале есть интересующие вас разделы, где каждый найдет, что-то необходимое для себя. Погружайтесь в неповторимый мир развлечений уже сегодня.
Are There Any Costs Involved?
fortune tiger
Ruben Diogo da Silva Neves https://ruben-neves.prostoprosport-ar.com is a Portuguese footballer who plays as a midfielder for the Saudi Arabian club Al-Hilal and the Portuguese national team. Currently, Ruben Neves plays for the Al-Hilal club wearing number 8. His contract with the Saudi club is valid until the end of June 2026.
budva haus kaufen hotel verkaufen
Музыка ВКонтакте https://audiobot.pw/ – слушать онлайн и скачать музыку бесплатно. Скачать, слушать, бесплатно, без установки программ, на компьютер, телефон, планшет, музыка, вк, vk, вконтакте. Лучшие подборки, лучшие чарты. Миллионы треков в mp3 для прослушивания онлайн или скачивания.
https://northern-doctors.org/# mexico pharmacy
https://avesis.medipol.edu.tr/aysegul.copur/yayinlar
http://www.istek.k12.tr/covid-19-istek-okullari-mutlu-ve-basari-ogrencilerin-okulu-2377
dobro voda
grundstuck am see
mexico drug stores pharmacies: mexican pharmacy northern doctors – purple pharmacy mexico price list
Cash Out: Decide when to cash out to secure your winnings. If you cash out before the plane crashes, you win. If
tigrinho
На нашем сайте вы найдете всю необходимую информацию о недвижимости – от бронирования квартиры в новостройке до приобретения недвижимости от застройщика.
Мы поможем вам выбрать лучшую квартиру в новостройке, расскажем, как не попасть в ловушку при выборе жилья и подскажем, как сэкономить на покупке.
Заходите: https://quartz-rsk.ru
https://northern-doctors.org/# mexican drugstore online
mexican border pharmacies shipping to usa: mexico drug stores pharmacies – mexican rx online
Kobe Bean Bryant https://kobebryant.prostoprosport-ar.com is an American basketball player who played in the National Basketball Association for twenty seasons for one team, the Los Angeles Lakers. He played as an attacking defender. He was selected in the first round, 13th overall, by the Charlotte Hornets in the 1996 NBA Draft. He won Olympic gold twice as a member of the US national team.
В компания МеталлоДеталь работают грамотные специалисты, которые имеют опыт производства сложных деталей по персональным эскизам, образцам и чертежам. Вы можете получить консультацию по телефону. Задавайте интересующие вопросы, и мы с удовольствием на них ответим. https://metobrabotka.com – сайт, где представлен каталог продукции, вы можете прямо сейчас ознакомиться с ним. Также здесь имеется галерея фотографий нашей компании. Мы выполняем все виды работ по металлообработке. Доставка продукции осуществляется оперативно. Обращайтесь к нам и не пожалеете!
На сайте https://moresliv.cc/ вы можете скачать бесплатно сливы курсов через торрент. Здесь каждый день добавляются свежие материалы. Обновления быстрые, а поддержка качественная. Воспользуйтесь поиском на сайте, впишите курс по названию либо по автору. Здесь любой найдет для себя большую коллекцию актуальных курсов, доступных без каких-либо затрат для скачивания. Тут собраны марафоны в таких областях, как финансы, программирование, бизнес и другое. Присоединяйтесь прямо сейчас и расширьте свои возможности и знания.
Fair Play Policies and RNG
tigrinho demo
На сайте https://podvodka.okis.ru/ у вас есть возможность заказать качественные гибкие подводки из нержавеющей стали. Широкий перечень продукции, такой как сильфонные гибкие подводки и многое другое вы можете заказать на сайте по телефону. Пользователи в считанные минуты смогут купить товар и найти необходимые модели. Меню сайта позволит вам отыскать то, что вас интересует. Также здесь есть таблица на размеры с ценой, руководство по монтажу и технические характеристики подводки с фото.
mexican border pharmacies shipping to usa: northern doctors pharmacy – buying from online mexican pharmacy
Секс-работа в городе Москве является комплексной и разнообразной трудностью. Несмотря на этот бизнес запрещена законом, эта деятельность остаётся важным нелегальным сектором.
Исторический
В советские времена интимные услуги процветала незаконно. По окончании СССР, в ситуации финансовой кризиса, проституция появилась более видимой.
Нынешняя Ситуация
Сегодня коммерческий секс в Москве представляет собой многочисленные формы, вплоть до высококлассных эскорт-услуг до уличного уровня проституции. Люксовые услуги часто предоставляются через интернет, а улицы коммерческий секс сконцентрирована в конкретных районах Москвы.
Общественно-экономические аспекты
Множество представительницы слабого пола вступают в эту сферу из-за материальных затруднений. Интимные услуги является привлекательным из-за шансом быстрого заработка, но это подразумевает угрозу здоровью и безопасности.
Законодательные вопросы
Проституция в стране запрещена, и за эту деятельность осуществление состоят строгие санкции. Проституток регулярно привлекают к к юридической наказанию.
Поэтому, не обращая внимания на запреты, проституция остаётся сегментом экономики в тени города с большими социальными и законодательными последствиями.
проститутки фрунзенская
http://northern-doctors.org/# mexican drugstore online
cash out before the plane crashes. The objective is to maximize winnings by timing the cash-out perfectly,
tigrinho
http://northern-doctors.org/# medication from mexico pharmacy
buying from online mexican pharmacy: northern doctors – medication from mexico pharmacy
最新娛樂城
Ищите скачать музыку бесплатно с ВКонтакте, слушать онлайн на сайте? Зайдите на https://kissvk.pw/ и вы сможете найти огромную коллекцию треков в mp3 на любой вкус. Ваши любимые треки, подборки, различные жанры, песни 2024, песни прошлых лет. Лучшие музыканты и певцы, подборки от редакции. Любые жанры, хиты, редкие песни – все это у нас на сайте.
Place Your Bet: Choose the amount you want to bet.
tigrinho aposta
medication from mexico pharmacy: mexican pharmacy – buying prescription drugs in mexico online
https://northern-doctors.org/# mexico drug stores pharmacies
Продажа подземных канализационных ёмкостей https://neseptik.com по выгодным ценам. Ёмкости для канализации подземные объёмом до 200 м3. Металлические накопительные емкости для канализации заказать и купить в Екатеринбурге.
mexican drugstore online: buying prescription drugs in mexico – mexican border pharmacies shipping to usa
Купити ліхтарики https://bailong-police.com.ua оптом та в роздріб, каталог та прайс-лист, характеристики, відгуки, акції та знижки. Купити ліхтарик онлайн з доставкою. Відмінний вибір ліхтарів: налобні, ручні, тактичні, ультрафіолетові, кемпінгові, карманні за вигідними цінами.
На сайте https://burstenstore.ru вы сможете купить все для кондитера. Продукция предназначена как для любителей, создавать сладости на кухне, так и для кондитеров с опытом. Вся продукция имеет сертификаты качества и абсолютно безопасна для здоровья. Товары доставляем почтой, транспортными компаниями и курьером. На оптовые заказы у нас действуют специальные цены. На сайте вы можете подробнее ознакомиться с каталогом нашей продукцией, посмотреть информацию о магазине и почитать отзывы.
History and Development
jogo do tigrinho
Андрей Суляев – психоаналитик, справится с запутанными и сложными проблемами. Его основная работа, которую он ведет официально, является частная психологическая практика. Консультации проходят как в очном формате, так и онлайн, из любой точки мира. https://sulyaev.ru – здесь представлена актуальная стоимость услуги, ознакомиться с ней можете прямо сейчас. Материалы сайта дадут возможность вам лучше в области психологии сориентироваться. Андрей Суляев с удовольствием ответит на дополнительные вопросы. Задавайте их уже сейчас!
кипр недвижимость дешево
台灣線上娛樂城是指通過互聯網提供賭博和娛樂服務的平台。這些平台主要針對台灣用戶,但實際上可能在境外運營。以下是一些關於台灣線上娛樂城的重要信息:
1. 服務內容:
– 線上賭場遊戲(如老虎機、撲克、輪盤等)
– 體育博彩
– 彩票遊戲
– 真人荷官遊戲
2. 特點:
– 全天候24小時提供服務
– 可通過電腦或移動設備訪問
– 常提供優惠活動和獎金來吸引玩家
3. 支付方式:
– 常見支付方式包括銀行轉賬、電子錢包等
– 部分平台可能接受加密貨幣
4. 法律狀況:
– 在台灣,線上賭博通常是非法的
– 許多線上娛樂城實際上是在國外註冊運營
5. 風險:
– 由於缺乏有效監管,玩家可能面臨財務風險
– 存在詐騙和不公平遊戲的可能性
– 可能導致賭博成癮問題
6. 爭議:
– 這些平台的合法性和道德性一直存在爭議
– 監管機構試圖遏制這些平台的發展,但效果有限
重要的是,參與任何形式的線上賭博都存在風險,尤其是在法律地位不明確的情況下。建議公眾謹慎對待,並了解相關法律和潛在風險。
如果您想了解更多具體方面,例如如何識別和避免相關風險,我可以提供更多信息。
mexico pharmacies prescription drugs: Mexico pharmacy that ship to usa – mexican pharmaceuticals online
Долго искал как найти классный офис для своей компании и нашел здесь (https://t.me/commers_estate_chat). Рекомендую!
http://northern-doctors.org/# mexico pharmacy
Lebron Ramone James https://lebronjames.prostoprosport-ar.com American basketball player who plays the positions of small and power forward. He plays for the NBA team Los Angeles Lakers. Experts recognize him as one of the best basketball players in history, and a number of experts put James in first place. One of the highest paid athletes in the world.
Коллеги, я наткнулся на группу в телеграмме по коммерческой недвижимости (https://t.me/commers_estate_chat) где разместил несколько объявлений о сдачи своих торговых помещений в аренду и нашел прямых арендаторов (цветы, аптека и продуктовый). Так что пользуетесь!)
кипр вторичные квартиры
недвижимость на кипре недорого объявления
Для развития своей компании искал новые локации для открытия и нашел много отличных предложений и контактов собственников в этой группе (https://t.me/commers_estate_chat)
На сайте https://moyuschie-pylesosy.ru/ в огромном выборе находятся моющие пылесосы, которые будут необходимы в каждом доме. К важным преимуществам подобных устройств относят то, что они смогут провести быструю, комфортную уборку любой поверхности, качественно очистят от пыли и различных загрязнений. Устройства эффективно справятся с самыми разными пятнами быстро, эффективно и без проблем. Дополнительно устройство поддерживает чистоту воздуха. Покупая устройство, необходимо ориентироваться на такие параметры, как: мощность, объем бака.
Всем привет! Искал по всему интернету где можно найти выгодный вариант для покупки коммерческой недвижимости и нашел очень ликвидный объект здесь (https://t.me/commers_estate_chat)
Зайдите на сайт UKBusiness https://ukbusiness.ru/ и ознакомьтесь с полезной информацией о том как расширить границы своего бизнеса, выйти на международный рынок со своими продуктами и услугами. На сайте вы узнаете: про бизнес в Великобритании, как открыть бизнес в Англии – налоги, финансы, иммиграция и визы, недвижимость и многое другое.
На сайте https://www.krasser.ru/met_izdel.html посмотрите телефон завода для того, чтобы воспользоваться такой полезной услугой, как изготовление металлоизделий, конструкций из стали. Для удобства имеется собственный склад металлоизделий. Услуга оказывается по чертежам. Компания выполняет только высококачественные работы и создает детали, выполненные из металла, независимо от сложности и предназначения. Также можно заказать производство эксклюзивных решений. Все товары разрабатываются с учетом требований, предпочтений заказчика. Техническое задание высылайте по почте.
mexican online pharmacies prescription drugs: mexican northern doctors – mexican mail order pharmacies
На сайте https://gdz-history.ru/index.html представлены контурные карты, атласы по истории, другая важная и ценная информация, которая поможет расширить мировоззрение, получить новые знания. Всю полезную информацию вы сможете изучить в режиме реального времени, скачать контурные карты абсолютно бесплатно. Перед вами готовые контурные карты за 5, 6, 7, 8, 9 классы. Скачивайте и распечатывайте чистые карты по истории в любое время, чтобы узнать больше нужной, актуальной информации. Вся самая свежая и качественная информация только здесь!
Rise of RA подходит для всех типов игроков: от новичков до профессионалов. https://rise-of-ra.com – тут узнаете, как в Rise of RA выигрывать, почему предсказывать победы нельзя и другое. Для вас мы собрали реальные отзывы, чтобы вы о слоте свое мнение могли составить. Rise of RA – это прекрасный выбор для поклонников древнеегипетской тематики. Слот отличается превосходной графикой, звуковым сопровождением и анимацией. Окунитесь в мир загадочного Египта!
коммерческая недвижимость москва московская область
Several key developers and companies have played a significant role in the development and success of the
fortune tiger
Luis Fernando Diaz Marulanda https://luis-diaz.prostoprosport-ar.com Colombian footballer, winger for Liverpool and the Colombian national team . Diaz is a graduate of the Barranquilla club. On April 26, 2016, in a match against Deportivo Pereira, he made his Primera B debut. On January 30, 2022, he signed a contract with the English Liverpool for five years, the transfer amount was 40 million euros.
Зайдите на сайт https://apps-betting.ru/ где вы сможете скачать приложения для ставок от лучших букмекерских контор, а также ознакомиться с ТОП 10 лучших приложений для ставок. Установить приложение можно на Android или iOS (айфон), и начать делать ставки на спорт в 1 клик. Почитайте информацию на сайте как выбрать лучшего букмекера и другие полезные советы.
http://northern-doctors.org/# mexican pharmaceuticals online
жилые комплексы кипра
Миссия ЭНЕРГОТЕХСТРОЙ 2000 – поставки высококачественной продукции. Компания ценит свою деловую репутацию, мы предлагаем адекватные цены нашим покупателям и удобные способы оплаты. Предоставим вам необходимую информацию и обсудим условия выгодного сотрудничества. Ищете кабель ввгнг гост? Best-vendor.ru/product-tag/kabel-vvgng – сайт, где у вас есть возможность уже сейчас сделать заказ кабеля ВВГнг. Здесь узнаете, сколько времени занимает доставка. При возникновении вопросов, звоните нам по телефону. Поможем вам с выбором подходящих товаров.
mexico drug stores pharmacies: mexican pharmacy – pharmacies in mexico that ship to usa
Maria Sharapova https://maria-sharapova.prostoprosport-ar.com Russian tennis player. The former first racket of the world, winner of five Grand Slam singles tournaments from 2004 to 2014, one of ten women in history who has the so-called “career slam”.
На сайте https://elektricheskie-kaminy.ru/ представлены электрические камины в огромном ассортименте. Эти конструкции подарят вашему дому незабываемый уют, комфорт. И самое важное, что они прослужат очень долго. Магазин предпринимает все возможное для того, чтобы процесс покупки был очень простым и понятным. Камины не выбрасывают в атмосферу вредные вещества. А для того, чтобы они начали обогревать, не потребуются дрова, а только розетка. Отсутствует открытый огонь, а потому возможность пожара сведена к минимуму.
mexico drug stores pharmacies: northern doctors pharmacy – mexican drugstore online
experiences. These communities provide valuable insights and foster a sense of camaraderie among players.
aviator game online
https://northern-doctors.org/# mexican pharmaceuticals online
Добро пожаловать на GPSPhone.ru! Определение местоположения по номеру телефона онлайн! ??
?? Не можете найти свой телефон? Бесплатно отследите его по номеру через спутник прямо сейчас! ??
??? Узнайте местоположение по номеру телефона онлайн на карте России с помощью геолокации! ???
?? Наш сервис позволяет найти телефон по номеру через спутник бесплатно без регистрации! ??
?? Отследите местоположение человека в реальном времени онлайн без регистрации! ??
?? Поиск по номеру телефона и определение местоположения стали проще! Попробуйте прямо сейчас на GPSPhone.ru! ??
Найдите телефон по номеру и узнайте местоположение онлайн с нашим удобным и бесплатным сервисом! ??
Геолокация по номеру телефона
mexican mail order pharmacies: northern doctors – mexican border pharmacies shipping to usa
Центр «Доверие» приглашает вас воспользоваться услугами. Запишитесь к психологу по номеру телефона на сайте. Семейный психолог делает так, чтобы для обоих супругов консультации были комфортными. https://ack-group.ru – сайт, где можно узнать более подробную информацию. Подростковый психолог выяснит уровень вашей проблемы и подберет подходящий способ ее решения. Консультация психолога цена доступна абсолютно каждому. Психолог в СПБ поможет урегулировать отношения с окружающими и с собой. Обращайтесь в любое время!
Its wonderful as your other blog posts : D, regards for putting up.
Interactive Interface: Players can interact with the game in real-time, making decisions that impact their
aviator game demo
Mohammed Khalil Ibrahim Al-Owais https://mohammed-alowais.prostoprosport-ar.com is a Saudi professional footballer who plays as a goalkeeper for the national team Saudi Arabia and Al-Hilal. He is known for his quick reflexes and alertness at the gate.
Kevin De Bruyne https://kevin-de-bruyne.prostoprosport-ar.com Belgian footballer, midfielder of the Manchester club City” and the Belgian national team. A graduate of the football clubs “Ghent” and “Genk”. In 2008 he began his adult career, making his debut with Genk.
purple pharmacy mexico price list: mexican pharmacy online – mexico drug stores pharmacies
https://northern-doctors.org/# mexican pharmaceuticals online
На сайте https://pmk3d.ru/ можно сделать заказ на качественную 3D-Печать. Компетентные специалисты превратят вашу идею в цифровую модель и выберут подходящий материал. Для более подробной информации, перейдите на страницу 3D-Печать. На сайте можно также посмотреть примеры работ и ознакомиться с портфолио. Для заказа заполните форму. Если у вас остались какие-либо вопросы, позвоните нам по телефонам, либо напишите на электронную почту, мы с удовольствием ответим на все интересующие вас вопросы.
mexican rx online: northern doctors pharmacy – mexican online pharmacies prescription drugs
Variety: Access to a wide range of betting options and gameplay modes.
play aviator game
https://northern-doctors.org/# mexican pharmacy
mexico pharmacy: northern doctors pharmacy – mexican pharmaceuticals online
Quincy Anton Promes https://quincy-promes.prostoprosport-br.com Dutch footballer, attacking midfielder and forward for Spartak Moscow . He played for the Dutch national team. He won his first major award in 2017, when Spartak became the champion of Russia.
Экспертиза ремонта в квартире https://remnovostroi.ru проводится для оценки качества выполненных работ, соответствия требованиям безопасности и стандартам строительства. Специалисты проверяют используемые материалы, исполнение работ, конструктивные особенности, безопасность, внешний вид и эстетику ремонта. По результатам экспертизы составляется экспертное заключение с оценкой качества и рекомендациями по устранению недостатков.
Игра на деньги Money Train отличается удобным и понятным интерфейсом. Промокоды и бонусы в этом слоте делают игру более выгодной и завлекательной. Если вам по нраву азарт и риск, то Money Train – это то, что вам необходимо! Лудоманы отмечают отличную графику и звуковое сопровождение. безанкор – сайт, где имеется познавательная информация об игре, посмотрите ее уже сегодня. Вы узнаете, какая тематика, присутствует в Money Train и какова максимальная выигрышная сумма в слоте. Играйте разумно и ответственно!
На сайте https://blackrent.ru/ можно заказать услугу аренды авто бизнес класса. Здесь у вас есть возможность легко и быстро оформить аренду автомобиля без водителя, с водителем и на свадьбу. У нас только проверенные и новые авто с гарантией низкой цены и без потери качества. Вы можете выбрать любую марку и модель авто, исходя из своих предпочтений. Клиентов поддерживаем на всем сроке аренды. Ознакомьтесь подробнее с нашим парком авто, отзывами, услугами, а также тарифами. Следите за акциями и новостями на сайте. Заполните форму, и мы вам наберем.
buying prescription drugs in mexico online: northern doctors pharmacy – mexico pharmacies prescription drugs
For beginners, the key to success in the Aviator Game is to start with small bets and gradually increase as you
aviator game demo
https://northern-doctors.org/# pharmacies in mexico that ship to usa
mexican pharmaceuticals online: mexican northern doctors – mexico drug stores pharmacies
На сайте https://iz-nerzhaveyki.ru/ вы можете приобрести из нержавеющей стали подводки, фитинги, фланцы, краны и другое. Здесь вы подробнее узнаете про шаровые краны, рукав высокого давления и гибкую подводку. Каталог на сайте позволит подобрать то, что вас интересует. Вся продукция качественная, она представлена на портале с фото и техническими характеристиками. Если у вас возникли вопросы по продукции, обратитесь к нам по телефону на сайте, либо на электронную почту.
Online Communities and Forums
aviator game online
https://northern-doctors.org/# buying prescription drugs in mexico
Компания «БытовкиСтарт» успешно работает уже более 5 лет. Мы удерживаем наилучшие цены на рынке и осуществляем оперативную доставку. Продукция вся есть в наличии. Бытовки произведены из надежных и прочных материалов. Гарантируем качество наших товаров. https://bytovkistart.ru – сайт, где можете прямо сейчас оставить заявку на профессиональную консультацию. Менеджеры все вежливые, они помогут вам с выбором интересующего вас варианта. При возникновении вопросов, сразу же обращайтесь к нам!
purple pharmacy mexico price list: mexican pharmacy – mexican pharmaceuticals online
Изучайте инглиш с помощью телесериала Friends! Уроки разговорного английского а также пополнение словарного запаса через ключевые моменты сериала. Учи английский по сериалу Friends – эффективный и увлекательный метод сделать лучше навыки понимания английским языком. Переходите на наш сайт https://serial-druzya.pp.ua/ и начинайте изучать английский язык бесплатно.
п»їbest mexican online pharmacies: mexican rx online – mexico pharmacy
laptops, tablets, and smartphones. This flexibility allows players to enjoy the game on their preferred device,
aviator game online
https://northern-doctors.org/# medicine in mexico pharmacies
п»їbest mexican online pharmacies: mexican northern doctors – mexican pharmaceuticals online
Ищете video summarizer? Go to Chrome web store chromewebstore.google.com/detail/youtube-transcript/jgibaoklabopileepldnlkbbcibhbgmd and download Youtube text, video transcript, video to text, video summary, ChatGPT video summary, Youtube summary. The best app for text transcription of YouTube videos.
pharmacies in mexico that ship to usa cmq mexican pharmacy online mexico drug stores pharmacies
На сайте https://laboratoriya-electro.ru/ вы сможете заказать обратный звонок для того, чтобы проконсультироваться по поводу оказания профессиональных услуг по измерениям, испытаниям различного типа электрооборудования. Вы сможете воспользоваться огромным спектром услуг, в том числе, высоковольтными испытаниями, замерами. В лаборатории находится все необходимое высокоточное оборудование. По этой причине все меры абсолютно безопасные, а ваша техника будет полностью отвечать самым высоким требованиям.
На сайте https://east-usa.com/index.html ознакомьтесь с подробной, актуальной информацией, которая касается карты Соединенных Штатов Америки. Только здесь представлена самая полная информация, которая вам обязательно пригодится для того, чтобы расширить кругозор. Перед вами подробная карта всех автомобильных дорог. Указаны и наиболее популярные достопримечательности, которые обязательно вас заинтересуют. Карта сгруппирована по следующим регионам: Средний Запад, Запад США, Юг США, Северо-восток.
Larry Joe Bird https://larry-bird.prostoprosport-br.com American basketball player who spent his entire professional career in the NBA ” Boston Celtics.” Olympic champion (1992), champion of the 1977 Universiade, 3-time NBA champion (1981, 1984, 1986), three times recognized as MVP of the season in the NBA (1984, 1985, 1986), 10 times included in the symbolic teams of the season (1980-88 – first team, 1990 – second team).
срочный ремонт сотовых телефонов
Секреты успешной перетяжки мебели, проверенных временем
Как преобразить интерьер с минимальными затратами, перетянутую мебель мечтали ваши друзья
Топ-3 причины для перетяжки мебели в доме, закажите услугу профессионалов
Вдохновляющие идеи для перетяжки мебели, которые понравятся каждому
Профессиональные советы по перетяжке мебели, применить в деле
компания “КакСвоим”.
http://mamalovesherbargains.com
Зайдите на сайт компании Эквивуд https://equiwood.ru/ которая занимается подбором, доставкой и наладкой деревообрабатывающего оборудования под требования клиента. Только проверенные поставщики и исключительно личные представители на территории стран Азии и Европы, что гарантирует качество оборудования. Осуществляем пусконаладочные работы, обучаем работе на станке, а также гарантия от нашей компании и пост гарантийное техобслуживание.
Roberto Firmino Barbosa de Oliveira https://roberto-firmino.prostoprosport-br.com Brazilian footballer, attacking midfielder, forward for the Saudi club “Al-Ahli”. Firmino is a graduate of the Brazilian club KRB, from where he moved to Figueirense in 2007. In June 2015 he moved to Liverpool for 41 million euros.
Вам интересны последние новости Ленинградской области и Санкт-Петербурга? Nowosti.spb.ru – это то, что вам действительно нужно! Здесь вы найдете такие категории: культура, экономика, политика, ЖКХ, спорт, медицина, общество. Предлагаем читателям все в понятном виде и выделяем самое основное. За каждым заголовком и фотографией располагается сюжет. Ищете происшествия санкт-петербурга и ленинградской области? Nowosti.spb.ru – здесь вы найдете много чего интересного и полезного. Наш ресурс выбирают те люди, которые ценят наполненность и свежесть. Читайте у нас самые актуальные новости. Рады вам в любое время!
Overview of the Aviator Game Experience
aviator game
Популярная компания ForgeHaus предоставляет большой спектр таких услуг, как создание функциональных автонавесов и эксклюзивные декоративные элементы из разных материалов. Мы реализовываем самые смелые проекты. Ищете новая беседка? Forgehaus.ru – сайт, где имеется о нас подробная информация, ознакомьтесь с ней уже сегодня. Гарантируем доступные цены, высокое качество нашей работы, быстрое выполнение заказов и персональный подход. Вся продукция долговечна и безопасна. Позвоните нам уже сейчас. Ваши идеи превратим в реальность!
buying from online mexican pharmacy cmq pharma mexican pharmacy reputable mexican pharmacies online
ремонт телефонов рядом
http://wiki.iurium.cz/w/U%C5%BEivatel:AngelesStreetman
Khvicha Kvaratskhelia https://khvicha-kvaratskhelia.prostoprosport-br.com Georgian footballer, winger for Napoli and captain of the Georgian national team. A graduate of Dynamo Tbilisi. He made his debut for the adult team on September 29, 2017 in the Georgian championship match against Kolkheti-1913. In total, in the 2017 season he played 4 matches and scored 1 goal in the championship.
Damian Emiliano Martinez https://emiliano-martinez.prostoprosport-br.com Argentine footballer, goalkeeper of the Aston Villa club and national team Argentina. Champion and best goalkeeper of the 2022 World Cup.
Numerous online casino platforms offer the Aviator Game. These platforms provide a secure and regulated
aviator game online
https://culturaitaliana.org/wiki/User:KelleyTims62365
На сайте https://panoramaburo.ru/landscape-design оставьте заявку на услугу по ландшафтному дизайну под ключ. Вам предложат интегрированный подход к созданию и проектирование современных внешних пространств. Квалифицированная команда воплотит все ваши мечты и фантазии в реальность. Подробнее ознакомиться с услугами компании, а также галереей работ, можно на сайте. Учитываются особенности каждого участка, предпочтения и пожелания клиентов, убедитесь в этом лично.
ремонт телефонов в москве
buying prescription drugs in mexico cmqpharma.com mexico pharmacy
срочный ремонт сотовых телефонов
mexico drug stores pharmacies: cmq pharma – mexican online pharmacies prescription drugs
plane ascends, the higher the multiplier. For example, if you bet $10 and cash out at a 2x multiplier, you win
aviator game
buy depakote 250mg without prescription – buy topamax generic generic topamax 100mg
Jack Peter Grealish https://jackgrealish.prostoprosport-br.com English footballer, midfielder of the Manchester City club and the England national team. A graduate of the English club Aston Villa from Birmingham. In the 2012/13 season he won the NextGen Series international tournament, playing for the Aston Villa under-19 team
Kyle Andrew Walker https://kylewalker.prostoprosport-br.com English footballer, captain of the Manchester City club and the England national team. In the 2013/14 season, he was on loan at the Notts County club, playing in League One (3rd division of England). Played 37 games and scored 5 goals in the championship.
mexico drug stores pharmacies mexico pharmacy buying prescription drugs in mexico
Hamster Kombat – популярная игра, которая обещает быстрый заработок. Запустить ее можете через официального бота в телеграме. Реальными деньгами платить не надо. У игры доброжелательные отзывы, погрузитесь в мир боевых хомяков. https://hamster-kombat-bot.io – сайт, где имеется вся информация о проекте. Вы узнаете, как начать играть в Hamster Kombat. Ознакомиться с информацией можно прямо сейчас. В игре можно прокачать хомяка и применяя Telegram, зарабатывать.
Glory Casino
Risk Management: Setting limits on how much to bet and when to cash out.
aviator game demo
Glory Casino
FinandCrypto.com offers useful and relevant information on the topic of finance, technology and cryptocurrencies. Talking about blockchain in simple words. You can view the content at any time convenient for you. https://finandcrypto.com – a popular site that is loved for its clear interface and simplicity. Exchange rates are presented here. There is also a search here, we recommend using it. Our main task is to help you make investment and financial decisions. With us you will be aware of the latest news!
mexican drugstore online best online pharmacies in mexico mexican mail order pharmacies
Son Heung Min https://sonheung-min.prostoprosport-br.com South Korean footballer, striker and captain of the English Premier League club Tottenham Hotspur and the Republic of Korea national team. In 2022 he won the Premier League Golden Boot. Became the first Asian footballer in history to score 100 goals in the Premier League
increase the excitement of the game.
aviator game demo
Laure Boulleau https://laure-boulleau.prostoprosport-fr.com French football player, defender. She started playing football in the Riom team, in 2000 she moved to Isere, and in 2002 to Issigneux. All these teams represented the Auvergne region. In 2003, Bullo joined the Clairefontaine academy and played for the academy team for the first time.
Интимные услуги в Москве существует как многосложной и многогранной трудностью. Несмотря на она противозаконна законом, этот бизнес остаётся крупным подпольным сектором.
Прошлый
В советского времени периоды проституция процветала подпольно. По окончании Советской империи, в ситуации финансовой нестабильности, она стала более заметной.
Нынешняя Ситуация
Сегодня проституция в Москве включает многочисленные формы, от престижных услуг эскорта до самой публичной интимных услуг. Высококлассные обслуживание в большинстве случаев осуществляются через интернет, а уличная интимные услуги сосредоточена в специфических участках Москвы.
Социальные и Экономические Аспекты
Множество женщины занимаются в эту деятельность вследствие финансовых трудностей. Коммерческий секс может быть интересной из-за перспективы мгновенного заработка, но такая работа подразумевает рисками для здоровья и жизни.
Юридические аспекты
Проституция в Российской Федерации запрещена, и за её осуществление состоят жесткие штрафы. Работников интимной сферы часто задерживают к административной и правовой ответственности.
Таким образом, не обращая внимания на запреты, секс-работа существует как аспектом незаконной экономики столицы с большими социально-правовыми последствиями.
mexican online pharmacies prescription drugs mexican pharmacy medicine in mexico pharmacies
На сайте https://venttehnica.ru/ компания предлагает приобрести и установить вентиляционное оборудование. Специалисты с удовольствием помогут вам с выбором качественного и недорогого оборудования. На сайте у вас есть возможность задать вопрос техническому специалисту. Также здесь представлен каталог товаров и спецпредложения, которые вы уже сейчас можете посмотреть. Расширенный поиск позволяет найти тот товар, который вас интересует. Оформить заказ можно по телефонам на сайте, либо по электронной почте, указанной на портале.
that use encryption and secure payment methods to protect their personal and financial information.
aviator demo game
buying prescription drugs in mexico cmq pharma mexico drug stores pharmacies
Don’t Make This Mistake When It Comes To Your SEO Service Near Me Near by
The Aviator Game includes various in-game bonuses and rewards to enhance the player’s experience. These can
aviator demo game
Центр «Доверие» приглашает вас воспользоваться услугами. Приём психолога для записи можно обратиться по контактному номеру телефона. Семейный психолог старается сделать так, чтобы консультации были комфортными для обоих супругов. https://ack-group.ru – сайт, где можно узнать более подробную информацию. Подростковый психолог выяснит вашу проблему и подберет нужный способ для ее решения. Цена консультации психолога доступна любому. Психолог в СПБ поможет урегулировать отношения с окружающими и с собой. Обращайтесь в любое время!
CVzen to najlepsza usługa pisania CV https://cvzen.pl/ i coach kariery dla milionów osób poszukujących pracy na całym świecie. Nasz zespół ekspertów jest zaangażowany w Twój sukces i będzie Cię wspierał przez całą Twoją karierę, od napisania profesjonalnego CV i listu motywacyjnego z uwzględnieniem specyfiki branży, po optymalizację profilu LinkedIn i zapewnienie profesjonalnego coachingu kariery. Odblokuj nowe możliwości dzięki CV, które pokaże Twój potencjał.
In January 2010, Harry Kane https://harry-kane.prostoprosport-fr.com received an invitation to the England U-team for the first time 17 for the youth tournament in Portugal. At the same time, the striker, due to severe illness, did not go to the triumphant 2010 European Championship for boys under 17 for the British.
Antoine Griezmann https://antoine-griezmann.prostoprosport-fr.com French footballer, striker and midfielder for Atletico Madrid. Player and vice-captain of the French national team, as part of the national team – world champion 2018. Silver medalist at the 2016 European Championship and 2022 World Championship.
перевод документов
апостиль в новосибирске
Хотите приобрести интересные сериалы на DVD? Serialexpress – это то, что вам нужно. У нас есть диски, которых вы ни в одном магазине не найдете. Качество сериалов великолепное, мы точно знаем, что вы останетесь своим приобретением, очень довольны. Товары в доступе по приемлемой цене, они упакованы очень хорошо. https://serialexpress.ru – сайт, где есть каталог, также тут можно посмотреть условия оплаты. У нас действует накопительная система скидок. Качество доставки вас приятно удивит. Есть вопросы? Не стесняйтесь обращаться к нашим менеджерам.
п»їbest mexican online pharmacies cmq pharma mexico drug stores pharmacies
апостиль в новосибирске
Ignoring Patterns: Failing to observe and learn from the game’s patterns can reduce your chances of winning.
aviator game
перевод документов
Современная сеть металлобаз Металл ДК в Москве https://metall-dk.ru/ – это продажа металлопроката оптом и в розницу. Арматура, профильная труба, стальной металлопрокат по низким ценам.
перевод документов
перевод с иностранных языков
перевод документов
На сайте https://geo-gdz.ru/ представлены ГДЗ по географии, истории. Перед вами огромная библиотека, которая работает в режиме реального времени. Здесь вы найдете школьные учебники, контурные карты, а также атласы, которые помогут получить новые знания, освоить нужную дисциплину. Список всей важной и нужной информации находится прямо на страницах сайта. Каждый год вносятся изменения в соответствии с политическими действиями. Этот сайт предназначен специально для тех, кто не в курсе этих изменений, но стремится расширить свой уровень знаний.
перевод документов
перевод с иностранных языков
На сайте https://pacific-map.com/index.html вы ознакомитесь с картой США с городами, штатами. Перед вами самая полная карта автомобильных дорог США. Есть карта Атлантического, Тихоокеанского побережья, имеется физическая карта США. Только здесь указана самая полная и содержательная информация, которая прольет свет на многочисленные вопросы. Вся информация является содержательной, интересной, актуальной, а потому на нее точно можно положиться. Обращайтесь и вы сюда за информацией, если необходимо что-то уточнить.
перевод документов
На сайте https://good-lawn.ru/ustroystvo-gazona у вас есть возможность оставить заявку на услугу по благоустройству территории и озеленению участков. Проектируя «дизайн загородной жизни» компания начинает свою работу с генерального плана участка, где будут учтены все пожелания и нюансы клиента. Примеры работ, цены и отзывы вы найдете на нашем портале. Все архитекторы компании имеют профильное образование и являются призерами дизайнерских конкурсов. Если хотите получить консультацию, оставьте заявку и специалисты свяжутся с вами в ближайшее время.
Читайте реальные отзывы клиентов и сотрудников об агентстве Topface Media на сайте https://topfacemedia-otzyvy.ru/ Поделитесь вашими собственными впечатлениями, оставляйте отзывы о взаимодействии с компанией Топфейс Медиа: дайте оценку нашей работе по управлению репутацией или задайте любой интересующий вопрос.
перевод документов
апостиль в новосибирске
Karim Mostafa Benzema https://karim-benzema.prostoprosport-fr.com French footballer, striker for the Saudi club Al-Ittihad . He played for the French national team, for which he played 97 matches and scored 37 goals.
mexican pharmacy mexican online pharmacy mexican mail order pharmacies
Achraf Hakimi Mou https://achraf-hakimi.prostoprosport-fr.com Moroccan footballer, defender of the French club Paris Saint-Germain “and the Moroccan national team. He played for Real Madrid, Borussia Dortmund and Inter Milan.
апостиль в новосибирске
Ищете оклейка авто? Зайдите на сайт just-vinyl.ru где вы сможете узнать все о наших услугах от Just Vinyl. Специализируемся на услуге оклейка авто под ключ, а также в продаже антигравийная пленка. Пленка на авто даст возможность изменить полностью цвет вашего автомобиля либо с помощью наших услуг по оклейке авто создать уникальный дизайн. Ознакомьтесь с ценами, нашими работами и ассортиментом на сайте. В Just Vinyl качество на первом месте!
перевод документов
Bonuses: Online casinos often offer bonuses and promotions, enhancing the gaming experience.
aviator demo game
перевод документов
перевод с иностранных языков
перевод документов
Tomer.ru – сайт, где можно найти подборку самых лучших фильмов о страсти и любви. Считаем, что их обязательно стоит посмотреть. Они станут украшением вашего вечера, и, возможно, даже повлияют на вашу жизнь. Ищете турецкие сериалы смотреть? Tomer.ru/blog/zhizn-v-turtsii/597-turetskie-serialy-na-russkom-yazyke.html – здесь можете узнать, почему турецкие сериалы пользуются популярностью у российских зрителей. Посмотрите на сайте список новинок уже сегодня. Заходите на наш портал, вас ждет много чего интересного и полезного!
перевод документов
Перетяжка мягкой мебели
https://www.credly.com/users/username.962aabc5/badges .
перевод с иностранных языков
advancements have allowed for improved graphics, smoother gameplay, and more interactive features. These
play aviator game
Калькулятор Ба Цзы https://xn--80aaczlbgb1auuk9b6de5c.xn--p1ai/ позволяет строить карту рождения, она состоит из набора восьми иероглифов, который формируется на основе даты и времени рождения человека, с учётом места рождения. Карта рождения отражает врожденные особенности характера личности сильные и слабые стороны, а также конкурентные преимущества. Она также помогает определить, качество жизни человека в разных сферах, а также определить какие даты будут оптимальными для различных событий, таких как переезд, смена работы, свадьба, начало диеты и другие.
Компания ОптимаСтройКомплект имеет прекрасную репутацию. Предлагаем строительные материалы по привлекательным ценам. Сэкономим ваши денежные средства! У нас предусмотрены скидки крупным клиентам. Можете оплачивать товары любым удобным для вас способом. https://optimalstroy.ru – сайт, где у вас есть возможность найти о нас еще больше информации. Здесь можно ознакомиться с продукцией и условиями доставки. Также можете почитать полезные статьи. Наши специалисты всегда вам помогут в случае, если у вас возникнут вопросы. Работаем для тех людей, которые ценят свое время!
апостиль в новосибирске
апостиль в новосибирске
апостиль в новосибирске
The ability to play from anywhere, coupled with the variety of games available, has attracted millions of
play aviator game
перевод с иностранных языков
перевод документов
апостиль в новосибирске
перевод документов
Kylian Mbappe Lotten https://kylian-mbappe.prostoprosport-fr.com Footballeur francais, attaquant du Paris Saint-Germain et capitaine de l’equipe de France. Le 1er juillet 2024, il deviendra joueur du club espagnol du Real Madrid.
перевод документов
апостиль в новосибирске
buy norpace generic – order disopyramide phosphate generic pill chlorpromazine 100mg
перевод документов
перевод документов
перевод с иностранных языков
advancements have allowed for improved graphics, smoother gameplay, and more interactive features. These
aviator demo game
В компания МеталлоДеталь работают грамотные специалисты, которые имеют опыт производства сложных деталей по персональным эскизам, образцам и чертежам. Вы можете получить консультацию по телефону. Задавайте вопросы, и мы с радостью ответим на них. https://metobrabotka.com – сайт, где представлен каталог продукции, вы можете прямо сейчас ознакомиться с ним. Также тут есть галерея фото нашей компании. По металлообработке мы осуществляем все виды работ. Доставка продукции выполняется довольно быстро. Обращайтесь к нам и не пожалеете!
апостиль в новосибирске
Jogo do Tigre https://jogo-do-tigre.prostoprosport-br.com is a simple and fun game that tests your reflexes and coordination. In this game you need to put your finger on the screen, pull out the stick and go through each peg. However, you must ensure that the stick is the right length, neither too long nor too short.
апостиль в новосибирске
апостиль в новосибирске
disopyramide phosphate oral – chlorpromazine online buy chlorpromazine uk
перевод документов
Mohamed Salah Hamed Mehrez Ghali https://mohamed-salah.prostoprosport-fr.com Footballeur egyptien, attaquant du club anglais de Liverpool et l’equipe nationale egyptienne. Considere comme l’un des meilleurs footballeurs du monde
казино 1вин
перевод документов
перевод документов
1win casino бонус за регистрацию
Convenience: Play from the comfort of your home or on the go.
aviator game
перевод документов
перевод с иностранных языков
перевод документов
перевод документов
перевод документов
Comprehensive Guide to Mac Antivirus Software: Protection, Features, and Recommendations
апостиль в новосибирске
апостиль в новосибирске
перевод документов
tablets, making it convenient to play anywhere and anytime.
aviator game
Best Antivirus Software of 2024: Comprehensive Guide and Recommendations
перевод с иностранных языков
Declan Rice https://declan-rice.prostoprosport-fr.com Footballeur anglais, milieu defensif du club d’Arsenal et de l’equipe nationale equipe d’Angleterre. Originaire de Kingston upon Thames, Declan Rice s’est entraine a l’academie de football de Chelsea des l’age de sept ans. En 2014, il devient joueur de l’academie de football de West Ham United.
перевод с иностранных языков
перевод с иностранных языков
Olivier Jonathan Giroud https://olivier-giroud.prostoprosport-fr.com French footballer, striker for Milan and the French national team. Knight of the Legion of Honor. Participant in four European Championships (2012, 2016, 2020 and 2024) and three World Championships (2014, 2018 and 2022).
перевод документов
перевод документов
перевод документов
перевод с иностранных языков
перевод документов
improved mobile compatibility. Developers continually use this feedback to enhance the game and provide a better
aviator game
перевод с иностранных языков
перевод с иностранных языков
перевод документов
перевод документов
перевод с иностранных языков
перевод с иностранных языков
апостиль в новосибирске
апостиль в новосибирске
cash out before the plane crashes. The objective is to maximize winnings by timing the cash-out perfectly,
aviator game
перевод документов
перевод с иностранных языков
Rise of RA подходит для игроков всех типов, и новичкам, и профессионалам. https://rise-of-ra.com – тут узнаете, как в Rise of RA выигрывать, почему предсказывать победы нельзя и другое. Для вас мы собрали реальные отзывы, чтобы вы о слоте свое мнение могли составить. Rise of RA – это великолепный выбор для любителей древнеегипетской тематики. Слот имеет прекрасную графику, анимацию и звуковое сопровождение. Погрузитесь в атмосферу загадочного Египта!
На сайте https://relomania.com/ оставьте заявку для того, чтобы проконсультироваться по поводу переезда в Испанию. Если и вы желаете жить на Средиземноморском море, выгодно инвестировать в недвижимость и просто спокойно жить в Испании, то время организовать переезд. В этом вам помогут сотрудники надежной компании «Relomania», которая начнет с вами работать на любом этапе. Только для клиентов агентства мягкая адаптация, независимо от того, что вы хотите: приобрести автомобиль, недвижимость.
Xavi or Xavi Quentin Sy Simons https://xavi-simons.prostoprosport-fr.com Dutch footballer, midfielder of the Paris Saint-Germain club -Germain” and the Dutch national team, playing on loan for the German club RB Leipzig.
перевод документов
Ronaldo de Asis Moreira https://ronaldinhogaucho.prostoprosport-br.com Brazilian footballer, played as an attacking midfielder and striker. World Champion (2002). Winner of the Golden Ball (2005). The best football player in the world according to FIFA in 2004 and 2005.
перевод документов
апостиль в новосибирске
На сайте https://deliveryplay.ru/arenda-invalidnyh-kolyasok закажите обратный звонок для того, чтобы воспользоваться такой нужной и полезной услугой, как прокат инвалидных колясок. Вы сможете воспользоваться оперативной доставкой, в том числе, экспресс. Для того чтобы воспользоваться арендой, не нужно вносить залог. Предусмотрен и самовывоз. Полный перечень услуг для клиентов. Действуют привлекательные расценки. Все коляски проходят обработку. Имеются самые разные размеры, независимо от веса.
перевод с иностранных языков
апостиль в новосибирске
перевод с иностранных языков
ensures compatibility across various platforms without the need for additional software downloads.
aviator game
See Real – известная компания, специализирующаяся на наружной рекламе и светодиодных технологиях. Предлагаем выгодные цены и привлечем в бизнес новых клиентов. Будем рады обсудить с вами самую смелую идею. Стремимся к долгосрочному сотрудничеству. Оставьте контактные данные, и мы обязательно свяжемся с вами в ближайшее время. Ищете казахстан лед экраны уличные? Iseer.kz – сайт, где можете узнать больше информации о нас и заказать звонок консультанта, чтобы он рассчитал стоимость. Квалифицированная команда к творческим вызовам готова. Оцените нашу работу!
апостиль в новосибирске
Edu.vdgb.ru – сайт, ежедневно мы работаем над тем, чтобы он стал еще удобнее. У нас вы сможете отыскать много чего интересного. Узнаете, что такое видеокурсы «Фирмы 1С». Приобретайте новые знания и развивайте свой мозг. Курсы 1С онлайн-обучение позволят освоить управление программой и разобраться во всех изменениях. С ценами и отзывами ознакомьтесь на нашем сайте. https://edu.vdgb.ru – здесь можно купить курсы. Вы научитесь пользоваться 1С в совершенстве и обретете возможность карьерного роста. Успейте записаться на онлайн обучение!
апостиль в новосибирске
перевод документов
апостиль в новосибирске
перевод документов
апостиль в новосибирске
Carlos Henrique Casimiro https://carloscasemiro.prostoprosport-br.com Futebolista brasileiro, volante do clube ingles Manchester United e capitao do Selecao Brasileira. Pentacampeao da Liga dos Campeoes da UEFA, campeao mundial e sul-americano pela selecao juvenil brasileira.
Kylian Mbappe Lotten https://kylianmbappe.prostoprosport-br.com Futebolista frances, atacante do Paris Saint-Germain e capitao da selecao francesa equipe . Em 1? de julho de 2024, ele se tornara jogador do clube espanhol Real Madrid.
перевод документов
Chasing Losses: Trying to recover losses by betting more can be detrimental.
aviator game
апостиль в новосибирске
перевод документов
перевод документов
https://win-line.net/אתרי-הימורים-אמינים/
לשלוח, ראיה לדבריך.
פעילות ההימורים באינטרנט הפכה לענף מושך מאוד בעת האחרונה, המאפשר אפשרויות מגוונות של חלופות הימורים, לדוגמה מכונות מזל.
במאמר זה נסקור את תחום ההתמודדות המקוונת ונמסור לכם נתונים חשובים שיסייע לכם להבין באזור מסקרן זה.
קזינו אונליין – הימורים באינטרנט
הימורי ספורט מציע מגוון רחב של פעילויות מוכרים כגון חריצים. ההימורים באינטרנט מעניקים לשחקנים ליהנות מאווירת התמודדות אותנטית בכל מקום ובשעה.
האירוע פירוט קצר
מכונות מזל משחקי מזל
רולטה הימור על פרמטרים על גלגל מסתובב בצורה עגולה
בלאק ג’ק משחק קלפים בו המטרה להגיע לסכום של 21
משחק קלפים פוקר משחק קלפים מבוסס אסטרטגיה
באקרה משחק קלפים פשוט וזריז
הימורים בתחום הספורט – התמודדות באינטרנט
הימורי ספורט מהווים חלק מ אחד הענפים המתפתחים המובילים ביותר בהימורים באינטרנט. משתתפים יכולים להתמודד על תוצאים של תחרויות ספורט מועדפים כגון ועוד.
ההימורים אפשר לבצע על תוצאת המשחק, מספר השערים ועוד.
המשחק פירוט משחקי ספורט מרכזיים
ניחוש הביצועים ניחוש התוצאה הסופית של האירוע כדורגל, כדורסל, קריקט
הפרש נקודות ניחוש ההפרש בתוצאות בין הקבוצות כדורגל, כדורסל, אמריקאי
מספר שערים/נקודות ניחוש כמות הביצועים בתחרות כדורגל, כדורסל, טניס
מנצח המשחק ניחוש מי יזכה בתחרות (ללא קשר לביצועים) מגוון ענפי ספורט
התמודדות דינמית הימורים במהלך המשחק בזמן אמת כדורגל, טניס, הוקי
התמודדות מורכבת שילוב של מספר פעילויות מספר ענפי ספורט
פעילות פוקר מקוונת – קזינו באינטרנט
פוקר אונליין מכיל אחד מסוגי התמודדות הפופולריים המובהקים ביותר בזמן האחרון. משתתפים יכולים להשתתף בפני מתמודדים אחרים מכל רחבי הגלובליזציה במגוון
перевод с иностранных языков
Секреты успешной перетяжки мебели, проверенных временем
Преображаем вашу мебель с помощью перетяжки, перетянутую мебель мечтали ваши друзья
Топ-3 причины для перетяжки мебели в доме, закажите услугу профессионалов
Какой стиль выбрать для перетяжки мебели, которые понравятся каждому
Профессиональные советы по перетяжке мебели, запомнить
Мебельная компания “КакСвоим”.
апостиль в новосибирске
перевод документов
https://win-line.net/ווינר-ליין-ווינר-אונליין/
לשלוח, אסמכתא לדבריך.
ההמרה באינטרנט הפכה לנישה פופולרי מאוד בעשור האחרון, המאפשר מגוון רחב של אפשרויות פעילות, החל מ הימורי ספורט.
בסקירה זה נבדוק את עולם הקזינו המקוון ונעניק לכם הערות חשובות שיסייע לכם לנתח בנושא אטרקטיבי זה.
קזינו אונליין – הימורים באינטרנט
הימורי ספורט מציע אופציות שונות של אפשרויות מסורתיים כגון רולטה. הקזינו באינטרנט מאפשרים למשתתפים לחוות מאווירת התמודדות מקצועית בכל עת ומקום.
הפעילות פירוט קצר
מכונות מזל הימורי גלגל
משחק הרולטה הימור על תוצאות על גלגל מסתובב
משחק הקלפים בלאק ג’ק משחק קלפים להשגת ניקוד של 21
משחק הפוקר משחק קלפים אסטרטגי
משחק הבאקרה משחק קלפים קל וזריז
הימורי ספורט – קזינו באינטרנט
התמרמרות ספורטיבית מייצגים אחד האזורים הצומחים ביותר בפעילות באינטרנט. מתמודדים מסוגלים להתמודד על פרמטרים של אירועי ספורט מושכים כגון ועוד.
העסקאות ניתן לתמוך על הביצועים בתחרות, מספר הנקודות ועוד.
אופן ההתמודדות הסבר תחרויות ספורט מקובלות
ניחוש הביצועים ניחוש התוצאה הסופית של התחרות כדורגל, כדורסל, קריקט
הפרש תוצאות ניחוש ההפרש בתוצאות בין הקבוצות כדורגל, כדורסל, אמריקאי
מספר שערים/נקודות ניחוש כמה שערים או נקודות יהיו במשחק כדורגל, כדורסל, הוקי קרח
מנצח המשחק ניחוש מי יזכה בתחרות (ללא קשר לביצועים) כל ענפי הספורט
התמרמרות בזמן אמת התמודדות במהלך האירוע בזמן אמת כדורגל, טניס, הוקי
התמודדות מורכבת שילוב של מספר פעילויות מספר תחומי ספורט
משחקי קלפים אונליין – קזינו באינטרנט
התמודדות בפוקר מקוון הוא אחד מענפי הקזינו המרכזיים הגדולים ביותר כיום. מבקרים מסוגלים להשתלב מול משתתפים אחרים מרחבי הכדור הארצי במגוון
Experienced players can benefit from more advanced strategies, such as:
aviator game
Lionel Messi https://lionelmessi.prostoprosport-br.com e um jogador de futebol argentino, atacante e capitao do clube da MLS Inter Miami. , capitao da selecao argentina. Campeao mundial, campeao sul-americano, vencedor da Finalissima, campeao olimpico. Considerado um dos melhores jogadores de futebol de todos os tempos.
Mohamed Salah https://mohamedsalah.prostoprosport-br.com e um futebolista egipcio que joga como atacante do clube ingles Liverpool e do Selecao egipcia. Considerado um dos melhores jogadores de futebol do mundo. Tricampeao da Chuteira de Ouro da Premier League inglesa: em 2018 (sozinho), 2019 (junto com Sadio Mane e Pierre-Emerick Aubameyang) e 2022 (junto com Son Heung-min).
Harry Kane https://harry-kane.prostoprosport-br.com recebeu um convite para a selecao sub-alterna da Inglaterra pela primeira vez tempo 17 para o torneio juvenil em Portugal. Ao mesmo tempo, o atacante, devido a doenca grave, nao compareceu ao triunfante Campeonato Europeu Sub-17 masculino de 2010 pelos britanicos.
Safety is paramount when playing online games. Players should ensure they are playing on reputable platforms
aviator game
Центр «Доверие» приглашает вас воспользоваться услугами. Запишитесь к психологу по номеру телефона на сайте. Семейный психолог делает так, чтобы для обоих супругов консультации были комфортными. https://ack-group.ru – сайт, где можно узнать более подробную информацию. Подростковый психолог выяснит вашу проблему и подберет нужный способ для ее решения. Консультация психолога цена доступна абсолютно каждому. Психолог в Спб поможет наладить отношения с собой и окружающими. Обращайтесь!
Игра на деньги Money Train отличается удобным и понятным интерфейсом. Бонусы и промокоды в данном слоте делают игру еще более увлекательной и выгодной. Если вам по нраву азарт и риск, то Money Train – это то, что вам необходимо! Лудоманы отмечают хорошее звуковое сопровождение и прекрасную графику. безанкор – сайт, где размещена интересная информация об игре, ознакомиться с ней можете в любое удобное для вас время. Вы узнаете, какая тематика, присутствует в Money Train и какова максимальная выигрышная сумма в слоте. Играйте разумно и ответственно!
Zlatan Ibrahimovic https://zlatan-ibrahimovic.prostoprosport-br.com Bosnian pronunciation: ibraxi?mo?it?]; genus. 3 October 1981, Malmo, Sweden) is a Swedish footballer who played as a striker. Former captain of the Swedish national team.
Luis Alberto Suarez Diaz https://luis-suarez.prostoprosport-br.com Uruguayan footballer, striker for Inter Miami and Uruguay national team. The best scorer in the history of the Uruguay national team. Considered one of the world’s top strikers of the 2010s
the opportunity to compete for larger prizes and showcase their skills on a larger stage.
aviator game
chubby teen blowjob
latina facefuck
http://center-2.ru/forum/?mingleforumaction=viewtopic&t=13063#postid-25933
Идеальные тактичные штаны для любого случая, которые подчеркнут вашу индивидуальность.
Выберите стильные тактичные штаны для своего гардероба, которые подчеркнут вашу уверенность и стиль.
Советы по выбору тактичных штанов, для максимального комфорта и функциональности.
Выберите удобные тактичные штаны для своего гардероба, и какие модели актуальны в этом сезоне.
Идеальные тактичные штаны для похода на природу, и какие модели стоит выбрать для уникального стиля.
купити штани чоловічі тактичні купити штани чоловічі тактичні .
live sex chat
http://forum.computest.ru/post/676593/#p676593
Gareth Frank Bale https://garethbale.prostoprosport-br.com Jogador de futebol gales que atuou como ala. Ele jogou na selecao galesa. Ele se destacou pela alta velocidade e um golpe bem colocado. Artilheiro (41 gols) e recordista de partidas disputadas (111) na historia da selecao.
Interactive Interface: Players can interact with the game in real-time, making decisions that impact their
aviator game
webcam models
мраморные памятники камень Уфалей
Идеальные тактичные штаны для любого случая, которые подчеркнут вашу индивидуальность.
Новинки в мире тактичной одежды: лучшие штаны, для активного образа жизни.
Чем отличаются тактичные штаны от обычных, для максимального комфорта и функциональности.
Какие тактичные штаны подойдут именно вам, сделанные для динамичного образа жизни.
Тактичные штаны: выбор современного мужчины, и какие модели стоит выбрать для уникального стиля.
брюки тактичні https://vijskovitaktichnishtanu.kiev.ua/ .
Выберите стильные тактичные штаны для повседневной носки, сделанные из качественных материалов.
Тактичные штаны: модные тренды этого сезона, сделанные для вашего комфорта.
Как правильно выбрать тактичные штаны, и какие модели стоит обратить внимание.
Тактичные штаны: идеальное сочетание стиля и практичности, сделанные для динамичного образа жизни.
Идеальные тактичные штаны для похода на природу, для максимального комфорта в походе.
зимові штани тактичні https://vijskovitaktichnishtanu.kiev.ua/ .
На сайте https://ipoteka-1.ru представлена вся самая актуальная, полезная информация, касающаяся ипотеки на вторичку, новостройку. Представлен материал о созаемщиках, о том, что лучше: арендовать жилье либо взять ипотеку. Есть данные о расходах на ипотеку и каким образом их понизить. Вы узнаете все о займах в режиме реального времени, как получить ипотеку, чтобы вам не отказали. Все статьи написаны экспертами, поэтому в них только точная и надежная информация. Вы получите ответ на вопрос, как быть, если нечем платить за ипотеку.
Как выбрать лучшие тактичные штаны для активного отдыха, которые подчеркнут вашу индивидуальность.
Выберите стильные тактичные штаны для своего гардероба, которые подчеркнут вашу уверенность и стиль.
Как правильно выбрать тактичные штаны, и какие модели стоит обратить внимание.
Выберите удобные тактичные штаны для своего гардероба, и какие модели актуальны в этом сезоне.
Какие материалы лучше всего подойдут для тактичных штанов, для максимального комфорта в походе.
наколінники для тактичних штанів https://vijskovitaktichnishtanu.kiev.ua/ .
Как выбрать лучшие тактичные штаны для активного отдыха, для идеального комфорта и функциональности.
Новинки в мире тактичной одежды: лучшие штаны, которые подчеркнут вашу уверенность и стиль.
Чем отличаются тактичные штаны от обычных, для максимального комфорта и функциональности.
Выберите удобные тактичные штаны для своего гардероба, сделанные для динамичного образа жизни.
Какие материалы лучше всего подойдут для тактичных штанов, чтобы чувствовать себя комфортно в любой ситуации.
купити тактичні зимові штани купити тактичні зимові штани .
Kevin De Bruyne https://kevin-de-bruyne.prostoprosport-br.com Futebolista belga, meio-campista do Manchester club City” e a selecao belga. Formado pelos clubes de futebol “Ghent” e “Genk”. Em 2008 iniciou sua carreira adulta, fazendo sua estreia no Genk.
На сайте http://koleso-na-hodu.ru каждый желающий получает возможность приобрести шины больших, а также редких размеров с оперативной доставкой по всему городу, области. Непосредственно на сайте у вас получится подобрать шины, исходя из таких параметров, как: ширина, высота профиля, диаметр, стоимость, производитель, сезонность. Вся продукция сертифицированная, качественная, оригинальная. Если остались вопросы, то заполните специальную форму со своими данными, чтобы менеджер перезвонил для уточнения определенных моментов.
The Aviator Game uses a Random Number Generator (RNG) to ensure fair play. This technology ensures that each
aviator game
Antoine Griezmann https://antoine-griezmann.prostoprosport-br.com Futebolista frances, atacante e meio-campista do Atletico de Madrid. Jogador e vice-capitao da selecao francesa, integrante da selecao – campea mundial 2018. Medalhista de prata no Europeu de 2016 e no Mundial de 2022.
Андрей Суляев – психоаналитик, справится с запутанными и сложными проблемами. Частная психологическая практика – его главная деятельность, которую он ведет официально. Консультации осуществляются онлайн, из любой точки мира и в очном формате. https://sulyaev.ru – здесь представлена актуальная стоимость услуги, ознакомиться с ней можете прямо сейчас. Материалы сайта дадут возможность вам лучше в области психологии сориентироваться. Андрей Суляев с удовольствием ответит на дополнительные вопросы. Задавайте их уже сейчас!
Профессиональные seo https://seo-optimizaciya-kazan.ru услуги для максимизации онлайн-видимости вашего бизнеса. Наши эксперты проведут глубокий анализ сайта, оптимизируют контент и структуру, улучшат технические аспекты и разработают индивидуальные стратегии продвижения.
Playing the Aviator Game involves a few simple steps:
aviator game
На сайте http://nemans.ru приобретите фасовочные пакеты, а также тару с ручками, мешки полипропиленовые, пленку полиэтиленовую, армированную, клейкую ленту, стрейч, различную бумажную продукцию, салфетки, тряпки и многое другое. Все товары реализуются по лучшим ценам, доступна оперативная доставка. Вся продукция от проверенных, надежных поставщиков, которые работают на результат. Все товары абсолютно безопасные, простые в использовании и помогают оперативно закончить уборку и не тратить на нее много времени. Регулярно на определенные товары устанавливаются скидки.
1win казино – ваш путь к успеху, начните игру прямо сейчас!
1win казино – место, где рождаются победы, выигрывайте крупные суммы вместе с 1win казино!
Увлекательное казино 1win ждет вас, получите незабываемые впечатления!
Играйте и выигрывайте с 1win казино, станьте победителем вместе с 1win казино!
1win казино – лучший выбор для азартных игр, получите удовольствие от азарта с 1win казино!
1win скачать 1win скачать .
На сайте https://arenda-kolyasok.ru/ ознакомьтесь с телефоном компании, где вы сможете заказать инвалидные коляски в большом ассортименте и самой разной модификации. Для того чтобы воспользоваться услугой, не потребуется залог. Доставка по столице в течение нескольких часов. В качестве бонуса – поднятие коляски на нужный этаж, а внутри МКАД действует бесплатная доставка. Имеются самые разные размеры. Специалист подберет вариант специально для вас. Все коляски эталонного качества, надежные и практичные.
casino game.
aviator game
К-ЖБИ производит большой ассортимент продукции отменного качества. Компания уже давно зарекомендовала себя с хорошей стороны. Мы постоянно развиваемся, гарантируем полное соблюдение сроков, приемлемые цены и высочайший уровень сервиса. Выполняем быструю доставку. Ищете плоские полнотелые плиты перекрытий и плиты серии п пт птп пп? Gbisp.ru – сайт, где найдете подробную информацию о нас, ознакомьтесь с ней. Здесь есть возможность оставить заявку, укажите свои контактные данные, и мы вам перезвоним. Вы получите квалифицированную консультацию. Сотрудничество с нами будет выгодно для вас!
Выберите стильные тактичные штаны для повседневной носки, которые подчеркнут вашу индивидуальность.
Новинки в мире тактичной одежды: лучшие штаны, которые подчеркнут вашу уверенность и стиль.
Как правильно выбрать тактичные штаны, чтобы выглядеть стильно в любой ситуации.
Выберите удобные тактичные штаны для своего гардероба, для стильного и практичного образа.
Идеальные тактичные штаны для похода на природу, для максимального комфорта в походе.
штани мультікам з наколінниками https://vijskovitaktichnishtanu.kiev.ua/ .
Выберите стильные тактичные штаны для повседневной носки, сделанные из качественных материалов.
Новинки в мире тактичной одежды: лучшие штаны, которые подчеркнут вашу уверенность и стиль.
Советы по выбору тактичных штанов, чтобы выглядеть стильно в любой ситуации.
Тактичные штаны: идеальное сочетание стиля и практичности, для стильного и практичного образа.
Какие материалы лучше всего подойдут для тактичных штанов, и какие модели стоит выбрать для уникального стиля.
штани зимові тактичні https://vijskovitaktichnishtanu.kiev.ua/ .
Как выбрать лучшие тактичные штаны для активного отдыха, сделанные из качественных материалов.
Тактичные штаны: модные тренды этого сезона, для активного образа жизни.
Как правильно выбрать тактичные штаны, и какие модели стоит обратить внимание.
Какие тактичные штаны подойдут именно вам, сделанные для динамичного образа жизни.
Тактичные штаны: выбор современного мужчины, для максимального комфорта в походе.
військові штани з наколінниками військові штани з наколінниками .
To start playing the Aviator Game, simply choose a reputable online casino platform that offers the game.
aviator game
1win казино: доступно на любых гаджетах
1win 1win .
Numerous online casino platforms offer the Aviator Game. These platforms provide a secure and regulated
aviator game
https://cmqpharma.online/# mexican border pharmacies shipping to usa
mexico pharmacies prescription drugs
Romelu Menama Lukaku Bolingoli https://romelulukaku.prostoprosport-br.com Futebolista belga, atacante do clube ingles Chelsea e da selecao belga . Por emprestimo, ele joga pelo clube italiano Roma.
Приветствую. Может кто знает, где найти разные блоги о недвижимости? Сейчас читаю https://1eve1.ru
buying from online mexican pharmacy mexican pharmacy online buying from online mexican pharmacy
Как выбрать лучшие тактичные штаны для активного отдыха, сделанные из качественных материалов.
Новинки в мире тактичной одежды: лучшие штаны, сделанные для вашего комфорта.
Чем отличаются тактичные штаны от обычных, и какие модели стоит обратить внимание.
Тактичные штаны: идеальное сочетание стиля и практичности, для стильного и практичного образа.
Какие материалы лучше всего подойдут для тактичных штанов, чтобы чувствовать себя комфортно в любой ситуации.
штани з наколінниками https://vijskovitaktichnishtanu.kiev.ua/ .
На сайте https://gametorrent.net/ вы найдете все нужное для погружения в захватывающий мир игр. У нас имеется множество аркад и головоломок, которые помогут вам весело и с пользой провести время. Файлы всегда доступны для скачивания в высоком качестве. Мы гарантируем безопасность. Можете быть уверены, что получите исключительно лучшие игры, свободные от вредоносных программ и вирусов. Свежие новинки игровой индустрии ждут именно вас, скачивайте их прямо сейчас!
experiences. These communities provide valuable insights and foster a sense of camaraderie among players.
aviator game
Как выбрать лучшие тактичные штаны для активного отдыха, которые подчеркнут вашу индивидуальность.
Тактичные штаны: модные тренды этого сезона, сделанные для вашего комфорта.
Советы по выбору тактичных штанов, и какие модели стоит обратить внимание.
Какие тактичные штаны подойдут именно вам, для стильного и практичного образа.
Какие материалы лучше всего подойдут для тактичных штанов, и какие модели стоит выбрать для уникального стиля.
штани жіночі тактичні https://vijskovitaktichnishtanu.kiev.ua/ .
Как выбрать лучшие тактичные штаны для активного отдыха, сделанные из качественных материалов.
Новинки в мире тактичной одежды: лучшие штаны, для активного образа жизни.
Как правильно выбрать тактичные штаны, чтобы выглядеть стильно в любой ситуации.
Какие тактичные штаны подойдут именно вам, и какие модели актуальны в этом сезоне.
Какие материалы лучше всего подойдут для тактичных штанов, для максимального комфорта в походе.
тактичні штани з наколінниками зимові https://vijskovitaktichnishtanu.kiev.ua/ .
aldactone ca – naltrexone buy online naltrexone price
Neymar da Silva Santos Junior https://neymar.prostoprosport-br.com e um futebolista brasileiro que atua como atacante, ponta e atacante. meio-campista do clube saudita Al-Hilal e da selecao brasileira. Considerado um dos melhores jogadores do mundo. O maior artilheiro da historia da Selecao Brasileira.
Выберите стильные тактичные штаны для повседневной носки, которые подчеркнут вашу индивидуальность.
Тактичные штаны: модные тренды этого сезона, которые подчеркнут вашу уверенность и стиль.
Чем отличаются тактичные штаны от обычных, для максимального комфорта и функциональности.
Какие тактичные штаны подойдут именно вам, сделанные для динамичного образа жизни.
Какие материалы лучше всего подойдут для тактичных штанов, для максимального комфорта в походе.
зимові штани тактичні https://vijskovitaktichnishtanu.kiev.ua/ .
На сайте https://altdikam.ru/chunks-of-stone-large-and-small.html вы сможете ознакомиться с техническими характеристиками, а также фотографиями каменных глыб алтайских, на которых растет мох. Перед вами крупные, а также мелкие глыбы, которые применяются для ландшафтного декорирования, а также благоустройства территории. Также имеются речные валуны, высокогорный скальник. Стоимость крупных глыб стартует от 7 000 рублей. Прямо сейчас посмотрите все фотографии. Есть глыбы-скальник, вес которых от 100 кг. Они представлены в огромном ассортименте и самых разных размеров.
На сайте https://best-vendor.ru/product/kabel-avbbshv/ приобретите кабель АВБбШв силовой и с жилой из алюминия, а также изоляцией, шлангом из ПВХ. Вся продукция выполнена из современных материалов, а потому точно не покроется коррозией. В этой компании у вас получится приобрести кабель максимально оперативно и с комфортом. При этом на все конструкции даются гарантии. Установлены привлекательные и честные расценки. Имеются все необходимые микроразмеры, что позволит подобрать вариант в зависимости от предпочтений.
Идеальные тактичные штаны для любого случая, для идеального комфорта и функциональности.
Тактичные штаны: модные тренды этого сезона, для активного образа жизни.
Как правильно выбрать тактичные штаны, для максимального комфорта и функциональности.
Какие тактичные штаны подойдут именно вам, и какие модели актуальны в этом сезоне.
Идеальные тактичные штаны для похода на природу, для максимального комфорта в походе.
штани військові з наколінниками https://vijskovitaktichnishtanu.kiev.ua/ .
Как выбрать лучшие тактичные штаны для активного отдыха, сделанные из качественных материалов.
Тактичные штаны: модные тренды этого сезона, которые подчеркнут вашу уверенность и стиль.
Чем отличаются тактичные штаны от обычных, для максимального комфорта и функциональности.
Какие тактичные штаны подойдут именно вам, для стильного и практичного образа.
Тактичные штаны: выбор современного мужчины, и какие модели стоит выбрать для уникального стиля.
купить штани тактичні купить штани тактичні .
Выберите стильные тактичные штаны для повседневной носки, которые подчеркнут вашу индивидуальность.
Новинки в мире тактичной одежды: лучшие штаны, для активного образа жизни.
Советы по выбору тактичных штанов, и какие модели стоит обратить внимание.
Тактичные штаны: идеальное сочетание стиля и практичности, и какие модели актуальны в этом сезоне.
Какие материалы лучше всего подойдут для тактичных штанов, чтобы чувствовать себя комфортно в любой ситуации.
тактичні штани військові тактичні штани військові .
Выберите стильные тактичные штаны для повседневной носки, для идеального комфорта и функциональности.
Тактичные штаны: модные тренды этого сезона, сделанные для вашего комфорта.
Чем отличаются тактичные штаны от обычных, чтобы выглядеть стильно в любой ситуации.
Тактичные штаны: идеальное сочетание стиля и практичности, и какие модели актуальны в этом сезоне.
Тактичные штаны: выбор современного мужчины, и какие модели стоит выбрать для уникального стиля.
купити штани тактичні купити штани тактичні .
The Aviator Game uses a Random Number Generator (RNG) to ensure fair play. This technology ensures that each
aviator game
Всем привет! Подскажите, где найти разные блоги о недвижимости? Сейчас читаю https://an72.ru
Jude Victor William Bellingham https://jude-bellingham.prostoprosport-cz.org anglicky fotbalista, zaloznik spanelskeho klubu Real Madrid a anglicky narodni tym. V dubnu 2024 ziskal cenu za prulom roku z Laureus World Sports Awards. Stal se prvnim fotbalistou, ktery ji obdrzel.
На сайте https://best-vendor.ru/product/vedro-ocinkovannoe/ вы сможете ознакомиться и приобрести в необходимом количестве ведра оцинкованные. Они потребуются для самых разных нужд, в том числе, и для организации хозяйства, уборки дома. На этом портале получится приобрести все необходимое как в розницу, так и оптом. Вы сможете купить все, что нужно и прямо сейчас. При необходимости получите профессиональную консультацию. Представлены ведра различного объема: 3, 5, 7, 12 литров. Ведра защищены от коррозии.
Как выбрать лучшие тактичные штаны для активного отдыха, сделанные из качественных материалов.
Выберите стильные тактичные штаны для своего гардероба, сделанные для вашего комфорта.
Как правильно выбрать тактичные штаны, и какие модели стоит обратить внимание.
Выберите удобные тактичные штаны для своего гардероба, сделанные для динамичного образа жизни.
Идеальные тактичные штаны для похода на природу, для максимального комфорта в походе.
штани чоловічі тактичні штани чоловічі тактичні .
Идеальные тактичные штаны для любого случая, для идеального комфорта и функциональности.
Выберите стильные тактичные штаны для своего гардероба, сделанные для вашего комфорта.
Чем отличаются тактичные штаны от обычных, чтобы выглядеть стильно в любой ситуации.
Какие тактичные штаны подойдут именно вам, сделанные для динамичного образа жизни.
Тактичные штаны: выбор современного мужчины, и какие модели стоит выбрать для уникального стиля.
куплю тактичні штани куплю тактичні штани .
На сайте http://turkiserial.com/ можно турецкие сериалы на русском языке смотреть онлайн абсолютно бесплатно в высоком качестве. Вы можете отыскать тут историю по душе, которая будет радовать с каждым новым эпизодом. На странице любого сериала представлена необходимая информация: год, страна, жанр, краткое описание, актерский состав. Смотреть выбранный вами сериал можно в удобное время. Гарантируем вам быструю загрузку и чистый звук. Наслаждайтесь просмотром!
Kylian Mbappe Lotten https://kylian-mbappe.prostoprosport-cz.org Francouzsky fotbalista, utocnik Paris Saint-Germain a kapitan tymu francouzskeho tymu. 1. cervence 2024 se stane hracem spanelskeho klubu Real Madrid.
Ищите строительство дома в Сочи и Краснодарском крае под ключ? Зайдите на сайт https://alternativa-sochi.ru/ где вы сможете ознакомиться с проектами домов и портфолио Компании Альтернатива и заказать строительство под ключ – качественные, быстровозводимые, энергоэффективные каркасные дома от фундамента до чистовой отделки. Гарантия, поэтапная оплата, помощь с ипотекой. Подробнее на сайте.
Hello there! cheap finasteride tablets excellent internet site.
buy generic cyclophosphamide – purchase cytoxan sale buy trimetazidine online
Всем привет! Подскажите, где найти разные статьи о недвижимости? Пока нашел https://armid44.ru
Mohamed Salah https://mohamed-salah.prostoprosport-cz.org je egyptsky fotbalista, ktery hraje jako utocnik za anglictinu. klub Liverpool a egyptsky narodni tym. Povazovan za jednoho z nejlepsich fotbalistu na svete.
На сайте https://kinogo.gr/ смотреть достойные фильмы онлайн можно круглосуточно и при этом абсолютно бесплатно. Мы предлагаем большой выбор новинок. Сделали удобный интерфейс. С помощью системы поиска легко и быстро можно отыскать любой интересующий фильм. А еще можете узнать много интересного об актерах и сюжете. У вас есть возможность ознакомиться с отзывами о киноленте и поделиться своим мнением о ней после просмотра. Выбирайте фильм на свой вкус и им наслаждайтесь!
Kevin De Bruyne https://kevin-de-bruyne.prostoprosport-cz.org Belgicky fotbalista, zaloznik Manchesteru klub City” a belgicky narodni tym. Absolvent fotbalovych klubu „Ghent” a „Genk”. V roce 2008 zahajil svou karieru dospelych, debutoval v Genku.
Алтайский центр природного камня предлагает уникальную возможность приобрести глыбы со мхом и лишайником по самым выгодным ценам. Существенно сэкономим ваши денежные средства! Выполняем доставку. Гарантируем великолепное обслуживание. Вы можете сами в этом убедиться. Чтобы узнать сроки поставки и получить фото камня, пожалуйста, отправьте в WhatsApp запрос. Ищете купить глыбы с лишайником? Altdikam.ru – портал, мы регулярно работаем над его улучшением. Здесь все ясно и наглядно. Если у вас появились интересующие вопросы, позвоните нам по телефону. С удовольствием вам поможем!
buy cytoxan without prescription – strattera 25mg canada brand vastarel
Hi there! how to get generic finasteride great internet site.
Как правильно подобрать материал для перетяжки мебели: профессиональные советы и рекомендации, для достижения идеального результата.
Самые стильные направления в перетяжке мебели: вдохновляющие решения для вашего интерьера, для создания неповторимого облика вашего дома.
DIY перетяжка мебели: легкие и креативные способы обновления интерьера, для создания уютной и гармоничной обстановки.
Преимущества перетяжки мебели: почему это стоит попробовать, для создания долговременного и стильного интерьера.
Как выбрать подходящего мастера для перетяжки мебели: советы и рекомендации, чтобы ваша мебель выглядела идеально.
Как создать современный интерьер с помощью перетяжки мебели: минималистический подход, которые добавят вашему дому легкость и свежесть.
Какие текстуры выбрать для перетяжки мебели в скандинавском стиле: уютные и теплые материалы, которые добавят вашему дому теплоту и гармонию.
Как сделать перетяжку мебели экономично и эффективно: секреты и советы, для привлечения внимания качественно выполненной работы.
Советы по перетяжке мебели в провансальском стиле: как создать атмосферу загородного уюта, которые принесут в ваш дом атмосферу тепла и ностальгии.
Какие детали учесть для перетяжки мебели в классическом стиле: изысканные и шикарные элементы, для создания аристократической атмосферы иллюзии.
Профессиональные секреты перетяжки мебели: как сделать работу максимально эффективной, для успешной реализации вашего проекта и получения отличного результата.
перетяжка мебели перетяжка мебели беларусь .
Приветствую. Может кто знает, где почитать разные блоги о недвижимости? Сейчас читаю https://azimut-irkutsk.ru
На сайте https://domanaveka.pro/ вы сможете узнать все подробности относительно строительства, проектирования коттеджей, домов. Все работы проверяются в нескольких уровнях, чтобы гарантировать заказчику эталонное качество работы. Специально для вас индивидуальное проектирование, а также дизайн. Строительство осуществляется по СНиПу, ГОСТу, поэтому дома передаются другому поколению. В команде трудятся первоклассные, компетентные сотрудники, которые выполнят проект на высоком уровне и в минимальные сроки.
Lionel Messi https://lionel-messi.prostoprosport-cz.org je argentinsky fotbalista, utocnik a kapitan klubu MLS Inter Miami. , kapitan argentinske reprezentace. Mistr sveta, vitez Jizni Ameriky, vitez finale, olympijsky vitez. Povazovan za jednoho z nejlepsich fotbalistu vsech dob.
Bernardo Silva https://bernardo-silva.prostoprosport-cz.org Portugalsky fotbalista, zaloznik. Narozen 10. srpna 1994 v Lisabonu. Silva je povazovan za jednoho z nejlepsich utocnych zalozniku na svete. Fotbalista je povestny svou vytrvalosti a vykonem.
Antoine Griezmann https://antoine-griezmann.prostoprosport-cz.org Francouzsky fotbalista, utocnik a zaloznik za Atletico de Madrid. Hrac a vicekapitan francouzskeho narodniho tymu, clen tymu – mistr sveta 2018 Stribrny medailista z mistrovstvi Evropy 2016 a mistrovstvi sveta 2022.
Robert Lewandowski https://robert-lewandowski.prostoprosport-cz.org je polsky fotbalista, utocnik spanelskeho klubu Barcelona a kapitan polskeho narodniho tymu. Povazovan za jednoho z nejlepsich utocniku na svete. Rytir krize velitele polskeho renesancniho radu.
Howdy! how to get valacyclovir price excellent web site.
spironolactone 25mg uk – revia 50 mg for sale naltrexone uk
Всем привет! Подскажите, где найти разные статьи о недвижимости? Сейчас читаю https://ecn-novodom.ru
Hello! cost cheap valacyclovir pills very good web page.
На сайте https://lasttorent.ru/ размещены различные игры, можете скачать их через торрент абсолютно бесплатно. У нас вы не пропустите ни одной новинки игровой индустрии. Начать играть можете прямо сейчас. Строка поиска находится в верхней части страницы. Можно искать игры по названию. Файлы абсолютно безопасны, отсутствуют вирусы. Если у вас возникли какие-либо вопросы, напишите нам, обязательно на них ответим и все разъясним. Играйте и получайте удовольствие!
На сайте https://best-vendor.ru/product/kabel-vbbshv/ приобретите кабель ВБбШв с медной жилой, изоляцией, а также защитным шлангом, который произведен из ПВХ. Используется для того, чтобы перераспределить энергию в электрических установках. Прямо сейчас вы сможете приобрести все необходимое оптом и в любом количестве, по доступной стоимости. Предоставляются гарантии качества. Совершите приобретение прямо сейчас. В наличии огромное количество различных размеров. На кабель действуют предложения круглогодично.
Son Heung Min https://son-heung-min.prostoprosport-cz.org Jihokorejsky fotbalista, utocnik a kapitan anglickeho klubu Premier League Tottenham Hotspur a narodniho tymu Korejske republiky. V roce 2022 vyhral Zlatou kopacku Premier League.
Luka Modric https://luka-modric.prostoprosport-cz.org je chorvatsky fotbalista, stredni zaloznik a kapitan spanelskeho tymu. klub Real Madrid, kapitan chorvatskeho narodniho tymu. Uznavan jako jeden z nejlepsich zalozniku nasi doby. Rytir Radu prince Branimira. Rekordman chorvatske reprezentace v poctu odehranych zapasu.
Cristiano Ronaldo https://cristiano-ronaldo.prostoprosport-cz.org je portugalsky fotbalista, utocnik, kapitan Saudske Arabie klubu An-Nasr a portugalskeho narodniho tymu. Mistr Evropy. Povazovan za jednoho z nejlepsich fotbalistu vsech dob. Nejlepsi strelec v historii fotbalu podle IFFIS a ctvrty podle RSSSF
Pablo Martin Paez Gavira https://gavi.prostoprosport-cz.org Spanelsky fotbalista, zaloznik barcelonskeho klubu a spanelske reprezentace. Povazovan za jednoho z nejtalentovanejsich hracu sve generace. Ucastnik mistrovstvi sveta 2022. Vitez Ligy narodu UEFA 2022/23
Hello! cost cheap valacyclovir prices good internet site.
Приветствую. Может кто знает, где почитать полезные блоги о недвижимости? Пока нашел https://germes-alania.ru
Pedro Gonzalez Lopez https://pedri.prostoprosport-cz.org lepe znamy jako Pedri, je spanelsky fotbalista, ktery hraje jako utocny zaloznik. za Barcelonu a spanelskou reprezentaci. Bronzovy medailista z mistrovstvi Evropy 2020 a zaroven nejlepsi mlady hrac tohoto turnaje.
Rodrigo Silva de Goiz https://rodrygo.prostoprosport-cz.org Brazilsky fotbalista, utocnik Realu Madrid a brazilskeho narodniho tymu. V breznu 2017 byl Rodrigo povolan do narodniho tymu Brazilie U17 na zapasy Montague Tournament.
Alison Ramses Becker https://alisson-becker.prostoprosport-cz.org Brazilsky fotbalista nemeckeho puvodu, brankar klubu Liverpool a brazilsky narodni tym. Je povazovan za jednoho z nejlepsich brankaru sve generace a je znamy svymi vynikajicimi zakroky, presnosti prihravek a schopnosti jeden na jednoho.
Karim Benzema https://karim-benzema.prostoprosport-cz.org je francouzsky fotbalista, ktery hraje jako utocnik za Saudskou Arabii. Arabsky klub Al-Ittihad. Hral za francouzsky narodni tym, za ktery odehral 97 zapasu a vstrelil 37 branek. V 17 letech se stal jednim z nejlepsich hracu rezervy, nastrilel tri desitky golu za sezonu.
Hello! can you buy valacyclovir pill good website.
На сайте https://best-vendor.ru/product/vojlok/ есть возможность изучить всю информацию о войлоке, а также то, для чего применяется данный материал. Он используется в самых разных сферах промышленности, включая металлургическую, строительство. На этом сайте у вас получится заказать и приобрести материал в любом количестве. Все, что необходимо, это – определиться с объемом заказа. Заказывайте войлок как оптом, так и в розницу. Предоставляются гарантии качества. Продукция реализуется по привлекательной и доступной стоимости.
мгл 35 g12
На сайте https://best-vendor.ru/product/kabel-kg-xl/ представлен кабель КГ-ХЛ. Эта конструкция с медной жилой, а также оболочкой из резины. Используется для того, чтобы присоединить передвижные механизмы к сетям, если напряжение переменное. Есть возможность приобрести кабель как в розницу, так и оптом. Вам будет гарантировано высокое качество продукции. Ознакомьтесь с рейтингом товара перед тем, как принять решение. Все товары реализуются по привлекательным ценам. Добавьте их в избранное, если отложили покупку.
Howdy! where can i get cheap valacyclovir pill good web site.
На сайте https://kinogo-fil.net/ вам предлагается смотреть интересные фильмы и сериалы бесплатно и без каких-либо ограничений. Здесь собрано множество подборок фильмов и категорий жанров, мультсериалов и мультфильмов. Вы сможете найти фильм для любых целей. Структура сайта позволит вам в несколько кликов начать смотреть ваш любимый сериал или же фильм. Наш сервис даст возможность вам подписаться на конкретный сериал, каждый раз, когда будет выходить новая серия, вы сразу же об этом узнаете! Приятного вам просмотра!
Thibaut Nicolas Marc Courtois https://thibaut-courtois.prostoprosport-cz.org Belgicky fotbalista, brankar spanelskeho klubu Real Madrid . V sezone 2010/11 byl uznan jako nejlepsi brankar v belgicke Pro League a take hrac roku pro Genk. Trojnasobny vitez Ricardo Zamora Trophy
Virgil van Dijk https://virgil-van-dijk.prostoprosport-cz.org Nizozemsky fotbalista, stredni obrance, kapitan anglickeho klubu Liverpool a kapitan nizozemskeho narodniho tymu.
Bruno Guimaraes Rodriguez Moura https://bruno-guimaraes.prostoprosport-cz.org Brazilsky fotbalista, defenzivni zaloznik Newcastlu United a Brazilsky narodni tym. Vitez olympijskych her 2020 v Tokiu.
Toni Kroos https://toni-kroos.prostoprosport-cz.org je nemecky fotbalista, ktery hraje jako stredni zaloznik za Real Madrid a nemecky narodni tym. Mistr sveta 2014. Prvni nemecky hrac v historii, ktery sestkrat vyhral Ligu mistru UEFA.
Toni Kroos https://toni-kroos.prostoprosport-cz.org je nemecky fotbalista, ktery hraje jako stredni zaloznik za Real Madrid a nemecky narodni tym. Mistr sveta 2014. Prvni nemecky hrac v historii, ktery sestkrat vyhral Ligu mistru UEFA.
Darwin Gabriel Nunez Ribeiro https://darwin-nunez.prostoprosport-cz.org Uruguaysky fotbalista, utocnik anglickeho klubu Liverpool a Uruguaysky narodni tym. Bronzovy medailista mistrovstvi Jizni Ameriky mezi mladeznickymi tymy.
Romelu Menama Lukaku Bolingoli https://romelu-lukaku.prostoprosport-cz.org Belgicky fotbalista, utocnik anglickeho klubu Chelsea a Belgican vyber. Na hostovani hraje za italsky klub Roma.
На сайте https://linii-okraski.ru/ вы сможете заказать линии окраски рулонного металла. Только в этой компании все изделия созданы с использованием революционных технологий и представляют собой уникальную и инновационную разработку, которая обязательно поможет вашему бизнесу. Линии Окраски отличаются отсутствием аналогов, являются особым изобретением. На технику предоставляются гарантии – 24 месяца. При необходимости воспользуйтесь профессиональной технической поддержкой, которая работает в круглосуточном режиме.
Изготавливаем рольставни на окна и двери https://mskroll.ru/rolstavni/ по индивидуальным размерам. Доставляем и устанавливаем в сжатые сроки. Гарантия – 2 года, а также производим рольставни для защиты окон и дверей по вашим размерам. Доставка и монтаж день в день. Гарантия – 24 месяца.
проститутки москвы индивидуалки https://prostitutki-213.ru
buy tiktok followers real https://tiktok-followers-buy.com
buy 10000 tiktok followers https://buy-tiktok-followers.com
отчаянные домохозяйки смотреть в хорошем отчаянные домохозяйки смотреть
проститутки индивидуалки дешевые проститутки москвы
can you buy followers on tiktok to go live buy 1000 tiktok followers
На сайте https://torrent-game.net/ у вас есть возможность скачать игры – торрент на компьютер абсолютно бесплатно. В наличии торренты (новые версии игр). Все они по рубрикам рассортированы. Есть удобная поисковая система, это дает возможность в кратчайшие сроки найти необходимое для вас. Под каждую игру имеется отдельная страница сайта. Заходите на ресурс и выбирайте интересующий продукт, и грузите исполняемое приложение. Выбор очень большой, вы отыщите то, что вас точно увлечет.
На сайте https://www.krasser.ru/met_izdel.html уточните стоимость металлоизделий. Их производит предприятие ООО “КрассНабСервис”, которое длительное время специализируется на производстве металлоизделий. Здесь получится заказать изделия, которые производятся из стали, металла. Имеется собственный склад. Все металлоизделия создаются строго по чертежам, а также с учетом индивидуальных особенностей производства. На этом предприятии получится заказать, произвести, приобрести металлоизделия, а также железо.
tiktok buy followers buy followers on tiktok
отчаянные домохозяйки сезон онлайн бесплатно онлайн https://domohozyayki-serial.ru
Hello! can you get cheap valacyclovir pill good web page.
Анонсы л2
https://businka74.ru риобет казино
драгон мани казино официальный сайт драгон мани казино
Большой выбор игровых автоматов, рабочее зеркало сайта https://fartunaplay.ru/slot-machines играть на реальные деньги онлайн
Сервера ла2
На сайте https://best-vendor.ru/product-tag/kanat-gost/ приобретите стальные канаты, которые потребуются для самых разных целей. Продукция выполнена по ГОСТу, что подтверждает эталонное высокое качество. Действует оперативная доставка. Есть возможность заказать продукцию в самом разном объеме и количестве. Канаты различаются техническими характеристиками. Для того чтобы заказать товары, необходимо просто позвонить менеджеру по телефону. У него получится уточнить всю необходимую информацию.
Качественная и недорогая https://mebelvam-nn.ru лучшие цены, доставка и сборка.
Rio Bet официальный сайт Rio Bet Casino
регистрация драгон мани казино https://trucktir.ru
Hi there! can i purchase valacyclovir without rx beneficial web page.
Качественная и недорогая детская мебель лучшие цены, доставка и сборка.
Pin Up casino https://pin-up.salexy.kz official website, Pin Up slot machines play for money online, Pin Up mirror working for today.
Slot machines on the official website and mirrors of the Pin Up online casino https://pin-up.tr-kazakhstan.kz are available for free mode, and after registering at Pin Up Casino Ru you can play for money.
Pin up entry to the official website. Play online casino Pin Up https://pin-up.prostoprosport.ru for real money. Register on the Pin Up Casino website and claim bonuses!
Sports in Azerbaijan https://idman-xeberleri.com.az development and popular sports Azerbaijan is a country with rich sports traditions and outstanding achievements on the international stage.
Howdy! order valacyclovir without rx great website.
Howdy! where to buy cheap valacyclovir without dr prescription good web page.
What a refreshing read! Your writing style is engaging, and the content is both uplifting and motivating. Keep up the great work!
kissbet
World of Games https://onlayn-oyunlar.com.az provides the latest news about online games, game reviews, gameplay and ideas, game tactics and tips. The most popular and spectacular
The main sports news of Azerbaijan https://idman.com.az. Your premier source for the latest news, exclusive interviews, in-depth analysis and live coverage of everything happening in sports in Azerbaijan.
UFC in Azerbaijan https://ufc.com.az news, schedule of fights and tournaments 2024, rating of UFC fighters, interviews, photos and videos. Live broadcasts and broadcasts of tournaments, statistics.
NHL (National Hockey League) News https://nhl.com.az the latest and greatest NHL news for today. Sports news – latest NHL news, standings, match results, online broadcasts.
На сайте https://t.me/s/freebet_za_registraciu вы найдете актуальные фрибеты от самых разных контор и на этот год. Вы узнаете о том, как заполучить фрибет, зарегистрировавшись и не проиграть. Еще представлена таблица со сравнениями самых разных условий. Перед вами те БК, которые предлагают огромное количество бонусов. В обязательном порядке указывается и сумма, на которую вы сможете рассчитывать сразу же при регистрации. Если хотите ознакомиться с рейтингом букмекерских контор, то перейдите на соответствующий сайт.
Howdy! where can i buy cheap valacyclovir prices very good internet site.
Video production studio Dubai
http://aeroviewimage.com/
На сайте https://best-vendor.ru/product/flyaga-alyuminievaya/ в большом выборе представлена фляга алюминиевая самого разного объема. Она необходима для хранения молока, воды, а также различных пищевых продуктов и многого другого. Вместимость фляжек различная, в том числе, есть 20 и 25 литров. В этой компании у вас получится с комфортом и максимально оперативно приобрести флягу со всеми гарантиями качества. Выбирайте необходимое количество. Все фляги выполнены по ГОСТу, в соответствии с самыми высокими нормативами. Не покрываются коррозией.
Hi there! where buy cheap valacyclovir no prescription excellent web site.
ensures that the games are fair and that the platforms adhere to strict standards of operation.
aviator game
Привилегированный частный эротический массаж Новосибирск база вип спа
include welcome bonuses, loyalty rewards, and special promotions that provide additional chances to win and
aviator game
эскорт услуги от индивидуалок москвы https://prostitutki-213.ru. Вызвать проститутку на любой вкус по низким ценам. Каталог шлюх Москвы
Установка кондиционера на мансарде Казань
https://multi-air.ru/
На сайте https://lan-union.ru предлагается к покупке сетевое и кабельное оборудование. В каталоге компании вы найдете подробное описание, также характеристики продукции и товаров производителя. На сайте вы можете увидеть сертификаты на продукцию, и детальнее ознакомиться с сервисом. Из преимуществ компании, можно отметить быструю логистику, высочайшее качество оборудования и расширенную гарантию. Для того чтобы быть в курсе акций и новостей компании, подпишитесь на рассылку.
На сайте https://lordfilm-hd.cfd/ вы сможете ознакомиться со всеми интересными, увлекательными и головокружительными фильмами, которые точно произведут на вас эффект. Все фильмы выполнены в отличном высоком качестве и с хорошим звуком. Есть и ожидаемые премьеры, выхода которых ожидали давно. У фильмов оригинальный, непредсказуемый сюжет. В кино играют лучшие актеры. Вас обрадуют спецэффекты, приятная музыка и любопытное повествование. Из всего многообразия вы точно найдете то, что посмотреть сегодня.
of players who enjoy the excitement of this high-flying adventure and see if you have what it takes to time your
п»їaviator game
Hello there! can i get valacyclovir pill beneficial website.
Зайдите на сайт https://pech.pro/ где вы сможете ознакомиться с огромным ассортиментом печей, каминов и всем необходимым для отделки бани. Также вы сможете заказать парную под ключ, которую мы спроектируем, доставим и смонтируем. Лучший ассортимент, привлекательные цены, доставка, гарантия. Подробнее на сайте.
Online casino games have surged in popularity due to their convenience and the immersive experience they offer.
aviator game
Hello! can i get generic valacyclovir without dr prescription excellent internet site.
How Tier Backlinks Has Changed The History Of Tier Backlinks tiers
1win slots официальный
increase the excitement of the game.
aviator game
Hi there! accutane 40 mg pharmacy very good web page.
https://lovewiki.faith/wiki/Saransk
http://www.ylemtech.co.kr/board/bbs/board.php?bo_table=free&wr_id=9757
навес из поликарбоната под ключ
Technical Specifications
aviator game
https://www.goodspeedcomputer.com/question/saransk/
https://eif-wiki.47th.info/index.php?title=User:DonetteBranco
Hello! cialis canada pharmacy online great web site.
На сайте https://1080kino.net/ можете смотреть лучшие фильмы онлайн абсолютно бесплатно в хорошем качестве. Организуйте себе прекрасный отдых, чтобы отвлечься от повседневных забот. Мы собрали для вас большую коллекцию фильмов разных жанров. Часто обновляем контент, смотрите новинки прямо сейчас. Фильмы увлекут вас захватывающим сюжетом и разнообразными событиями. Добавляйте наш развлекательный портал в закладки для того, чтобы следить за выходом интересного кино.
While the game itself is free to access, playing involves placing bets with real money. Some platforms may offer
aviator game
Hello! online pharmacy no prescription haldol very good internet site.
The Aviator Game is an exciting online casino game that has captivated players worldwide with its unique blend
aviator game
купить диплом в орле купить диплом в орле .
the thrill of betting and cashing out. Common themes in reviews include the game’s fairness, the enjoyment of
aviator game
Откройте тайны берців зсу, исследуйте, традиции, разберитесь в, Берці зсу: символ верности и чести, загляните в, поищите, погрузитесь, традициями, в мир, Берцем зсу було від роду козацького, дізнайтеся
берці зсу 2021 берці зсу 2021 .
На сайте https://mees.com.ru/ вы сможете ознакомиться со всей необходимой безработному, студенту, школьнику информацией, которая касается поиска работы, интересных вакансий. Здесь размещают резюме соискатели, заинтересованные в поиске проверенных, опытных кадров, которые желают трудиться и зарабатывать деньги. Здесь сможет отыскать для себя работу специалист с различным опытом работы или даже без нее. При необходимости вы сможете подписаться на рассылку для того, чтобы получать самые интересные вакансии. Они обновляются регулярно.
Hi there! thailand online pharmacy excellent website.
Откройте тайны берців зсу, исследуйте, изучите, истории, раскройте, загляните в, смысл, погрузитесь, изучите, Спробуйте на власній шкірі бути Берцем зсу, Берцем зсу було від роду козацького, зрозумійте
берці літні зсу https://bercitaktichnizsu.vn.ua/ .
Погрузитесь в мир берців зсу, исследуйте, Какова история появления берців зсу?, Тайна берців зсу, рассмотрите, Берці зсу: путь к мудрости, смысл, Берці зсу: от древности до современности, освойте, Як живеться в берцах зсу, традиції, силу
берці літні зсу https://bercitaktichnizsu.vn.ua/ .
Откройте тайны берців зсу, историю, обычаи, Тайна берців зсу, Берці зсу: символ верности и чести, Берці зсу: путь к мудрости, найдите, Берці зсу: от древности до современности, Берці зсу: символ силы и мудрости, Спробуйте на власній шкірі бути Берцем зсу, дізнайтесь, значення
нові берці зсу 2021 нові берці зсу 2021 .
Multiplayer Options and Social Interaction
aviator game
купить диплом в иваново diplomvash.ru .
Погрузитесь в мир берців зсу, анализируйте, познакомьтесь с, символике, Берці зсу: традиции древних времен, мистику, сущность, погрузитесь, историей, загляните, дізнайтесь, таємниці
купити берці літні зсу купити берці літні зсу .
Погрузитесь в мир берців зсу, Почему берці зсу так важны для культуры?, освойте, углубитесь в, магию, Берці зсу: охранители души, Берці зсу: талисман силы, почувствуйте, изучите, Як живеться в берцах зсу, Берець зсу – це не просто взуття!, значення
нові берци зсу нові берци зсу .
На сайте https://avto-lombard42.ru/ есть возможность рассчитать займ на специальном калькуляторе, который работает в режиме реального времени. Ломбард работает в круглосуточном режиме, а потому воспользоваться услугами вы сможете в любое время. Здесь вы сможете получить займ под залог ПТС, выкупаются машины самых разных марок. Для того чтобы получить необходимую сумму, следует связаться со специалистом по телефону, уточнить все нюансы. Оценщики произведут осмотр автомобиля, после чего назначат стоимость.
Погрузитесь в мир берців зсу, историю, Какова история появления берців зсу?, значении, магию, Берці зсу: охранители души, сущность, Берці зсу: духовное наследие Украины, историей, Як живеться в берцах зсу, анатомію, зрозумійте
нові берци зсу https://bercitaktichnizsu.vn.ua/ .
Погрузитесь в мир берців зсу, значение, познакомьтесь с, Легенды и предания о берцах зсу, проанализируйте, загляните в, истину, Берці зсу: духовное наследие Украины, Берці зсу: подвиги и традиции, проникнитесь, анатомію, зрозумійте
берці тактичні зсу берці тактичні зсу .
Hi! onlie pharmacy with echeck very good web page.
Online casino games have surged in popularity due to their convenience and the immersive experience they offer.
aviator game
Погрузитесь в мир берців зсу, происхождение, Почему берці зсу считаются священными?, углубитесь в, Берці зсу: связь с предками, погрузитесь в, Берці зсу: талисман силы, Берці зсу: духовное наследие Украины, познакомьтесь с, загляните, традиції, зрозумійте
нові берци зсу https://bercitaktichnizsu.vn.ua/ .
Узнайте всю правду о берцах зсу, анализируйте, обычаи, истории, рассмотрите, тайны, смысл, проникнитесь, Берці зсу: символ силы и мудрости, Почуйте, як б’ють від Берця зсу, дізнайтесь, значення
нові берци зсу https://bercitaktichnizsu.vn.ua/ .
Откройте тайны берців зсу, Какую роль играют берці зсу в обрядах?, Зачем люди носят берці зсу?, Тайна берців зсу, рассмотрите, Берці зсу: охранители души, сущность, почувствуйте, историей, Спробуйте на власній шкірі бути Берцем зсу, символіку, силу
нові берці зсу https://bercitaktichnizsu.vn.ua/ .
Hello there! boner pills sold in stores great internet site.
На сайте https://iz-nerzhaveyki.ru/ вы можете приобрести из нержавеющей стали подводки, фитинги, фланцы, краны и другое. Здесь вы подробнее узнаете про шаровые краны, рукав высокого давления и гибкую подводку. Каталог на сайте позволит подобрать то, что вас интересует. Вся продукция качественная, она представлена на портале с фото и техническими характеристиками. Если у вас возникли вопросы по продукции, обратитесь к нам по телефону на сайте, либо на электронную почту.
Do you want to make money on binary options? Visit https://expertoption-app.online/ where you can download the Expert Option app for all devices to instantly start trading anywhere. A clear interface, many indicators, free accurate signals – all the benefits in one application.
excitement it brings to the table.
aviator game
Hello there! male ed pharmacy great internet site.
Register an account, make a deposit, and navigate to the Aviator Game to start playing.
aviator game
ремонт стиральных машин дома на выезде http://centr-remonta-stiralnyh-mashin.ru .
Visit the website https://gate-a-door.com/ where you can order installation and repair of all types of garage doors and gates. More than 10 years of experience, individual design, guarantee for all services. Electric, automatic, swing, sliding gates and a full range of maintenance services! Visit the website.
include welcome bonuses, loyalty rewards, and special promotions that provide additional chances to win and
aviator game
Discovered an intriguing article, I recommend you to check it out https://chessdatabase.science/wiki/Free_Video_Chat_Without_Registration
Convenience: Play from the comfort of your home or on the go.
aviator game
Multiplayer Options and Social Interaction
aviator game
Hello there! viagra mexican pharmacy very good web site.
purchase cyclobenzaprine online – order cyclobenzaprine 15mg pills vasotec online buy
Cash Out: Decide when to cash out to secure your winnings. If you cash out before the plane crashes, you win. If
aviator game
Competitive Tournaments and Events
aviator game
Hello there! best indian pharmacy beneficial web page.
Chasing Losses: Trying to recover losses by betting more can be detrimental.
aviator game
Howdy! the canadian pharmacy one item beneficial web site.
invitation movie barbara stanwyck imdbaot part 2 season 4imdb wayward pinesshaun cassidy movies
flexeril 15mg ca – flexeril 15mg without prescription vasotec 5mg uk
Швеллер: Применение, Виды и Преимущества
Что такое швеллер?
Швеллер — это металлический профиль, имеющий П-образное сечение. Он широко используется в строительстве, машиностроении и других отраслях благодаря своей прочности, устойчивости к нагрузкам и универсальности. Швеллеры могут быть изготовлены из различных материалов, включая сталь, алюминий и другие сплавы.
Виды швеллеров
Существует несколько основных видов швеллеров, различающихся по методу производства и назначению:
1. Горячекатаный швеллер: Производится путем прокатки стальных заготовок при высоких температурах. Характеризуется высокой прочностью и используется в строительстве крупных сооружений.
2. Гнутый швеллер: Изготавливается методом холодной гибки стальных листов. Менее прочный по сравнению с горячекатаным, но обладает большей гибкостью и подходит для более легких конструкций.
3. Алюминиевый швеллер: Легкий и устойчивый к коррозии, что делает его идеальным для использования в условиях повышенной влажности или агрессивных сред.
Применение швеллеров
Швеллеры находят широкое применение в различных областях благодаря своей универсальности и надежности:
1. Строительство: Используются в каркасах зданий, мостах, перекрытиях и других конструкциях, где требуется высокая прочность и устойчивость к нагрузкам.
2. Машиностроение: Применяются в производстве станков, автомобилей, вагонов и других механизмов, где важны жесткость и устойчивость к деформациям.
3. Инфраструктура: Используются в строительстве железных дорог, трубопроводов и других инфраструктурных объектов.
4. Декоративное и промышленное строительство: Швеллеры могут использоваться в создании декоративных элементов, лестниц, ограждений и других конструкций.
Преимущества использования швеллеров
Использование швеллеров в строительстве и других областях имеет ряд преимуществ:
1. Высокая прочность: Швеллеры способны выдерживать значительные нагрузки, что делает их незаменимыми в строительстве и машиностроении.
2. Универсальность: Благодаря разнообразию видов и размеров, швеллеры можно использовать в самых разных проектах и конструкциях.
3. Устойчивость к деформациям: П-образная форма обеспечивает высокую жесткость и устойчивость к изгибам и деформациям.
4. Долговечность: Швеллеры из стали и алюминия обладают высокой устойчивостью к коррозии и другим воздействиям, что обеспечивает длительный срок службы.
Заключение
Швеллер — это незаменимый элемент в строительстве и машиностроении, обеспечивающий прочность, надежность и долговечность конструкций. Благодаря разнообразию видов и размеров, швеллеры находят широкое применение в различных областях, от крупных инфраструктурных проектов до мелких декоративных элементов. Выбирая швеллеры для своих проектов, вы можете быть уверены в их качестве и надежности.
http://www.allshveller.ru/
Today, I went to the beach front with my children. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She placed the shell to her ear and screamed. There was a hermit crab inside and it pinched her ear. She never wants to go back! LoL I know this is entirely off topic but I had to tell someone!
gama casino регистрация
Скачать музыку бесплатно на https://vritme.org/ это возможность найти самые любимые треки, новинки музыки, альбомы целиком в одном месте. Скачать музыку на любое устройство или слушать онлайн у нас на сайте. Постоянное добавление треков – от самых новых до редких песен. Чарты альбомов, новые альбомы, музыка под настроение – любые жанры и лучшее качество звука в mp3.
Origins of the Aviator Game
aviator game
Хотите приобрести интересные сериалы на DVD? Serialexpress – это то, что вам нужно. У нас есть диски, которых вы ни в одном магазине не найдете. Качество сериалов отличное, вы точно останетесь довольны покупкой. Товары в доступе по лояльной стоимости, они отлично упакованы. https://serialexpress.ru – сайт, где есть каталог, также тут можно посмотреть условия оплаты. У нас есть накопительная скидочная система. Качество доставки вас приятно удивит. Есть вопросы? Обратитесь за ответами к нашим компетентным менеджерам.
Historic Center of Florence, New Generation Festival (Mikhail Bakhtiarov as sponsor)…This was an impressive event for young opera talents taking place in the Corsini Palace gardens hosted by the formidable Principessa Giogiana and her daughter Sabrina. New Generation Festival Mikhail Bakhtiarov
Hi! vipps certified online pharmacy viagra very good website.
Playing the Aviator Game involves a few simple steps:
aviator game
Hello! canadian pharmacy 100mg viagra excellent web page.
Strategies and Tips
aviator game
Сервис на высшем уровне, спасибо за консультацию и помощь!
аккумуляторы оптом
Howdy! md pharmacy discounts cialas beneficial site.
plane ascends, the higher the multiplier. For example, if you bet $10 and cash out at a 2x multiplier, you win
aviator game
Hello there! mexico pharmacy drugs nexium beneficial website.
balancing the risk of waiting longer for a higher payout against the potential loss if the plane crashes.
aviator game
На сайте https://turkzona.com/ представлены интересные, увлекательные турецкие сериалы, которые точно понравятся всем любителям такого направления. Все фильмы интересные, увлекательные, а самое главное, что представлены в отличном качестве, отличаются четкой картинкой, качественным звуком, что усиливает приятные эмоции от просмотра. Перед вами огромный выбор вариантов фильмов самых разных жанров: мелодрамы, драмы. Для того чтобы подобрать оптимальный вариант, необходимо определиться с годом выпуска.
На сайте https://vkinogo.net/ можете смотреть интересные фильмы совершенно бесплатно в любое удобное для вас время. Наслаждайтесь увлекательными сюжетами и блестящей игрой актеров. Мы сделали простой и удобный портал. В нашем каталоге представлены все жанры. Выбор фильмов достаточно широк, уверены в том, что у нас вы найдете кино по своему вкусу. Можете прямо сейчас ознакомиться с последними новинками. Не упустите возможность погрузиться в захватывающий мир кино!
LeanBiome is a dietary supplement designed to promote weight loss and improve overall health. It is formulated with a unique blend of probiotics, prebiotics, and natural ingredients that work together to support a healthy gut microbiome. The gut microbiome plays a crucial role in digestion, metabolism, and the immune system. By optimizing the gut microbiome, LeanBiome aims to help individuals achieve their weight loss goals more effectively and sustainably. https://sites.google.com/spsw.edu.pl/leanbiome/
Hi! non prescription pharmacy excellent website.
casino game.
aviator game
Tonic Greens has gained popularity as a health supplement known for its rich blend of vitamins, minerals, and plant extracts. This article explores its composition, potential health benefits, usage instructions, and possible side effects. https://sites.google.com/spsw.edu.pl/tonicgreens/
SightCare is a revolutionary dietary supplement designed to support and maintain optimal eye health. In today’s digital age, where screens dominate our daily lives, the need for effective eye care solutions has never been greater. SightCare aims to meet this need with its scientifically formulated blend of essential nutrients and antioxidants. https://sites.google.com/spsw.edu.pl/sightcare/
Evolution and Technological Advancements
aviator game
Hi! best online pharmacy no prescription excellent internet site.
Boostaro stands out as a natural solution for boosting energy levels and supporting overall vitality. Its blend of caffeine, adaptogens, and essential nutrients offers a balanced approach to enhancing physical and mental energy. As with any supplement, consult with a healthcare professional before starting, especially if you have any health concerns or sensitivities. https://sites.google.com/spsw.edu.pl/boostaro/
Prostadine is a dietary supplement formulated to support prostate health, particularly in men experiencing symptoms of benign prostatic hyperplasia (BPH) or other prostate-related issues. As men age, maintaining prostate health becomes increasingly important to avoid urinary discomfort and other related problems. Prostadine aims to provide a natural solution through a blend of ingredients known for their beneficial effects on the prostate. https://sites.google.com/spsw.edu.pl/prostabiome
whether at home or on the go.
aviator game
На сайте https://spb-gid.ru/ представлена самая исчерпывающая, интересная информация, которая касается Санкт-Петербурга. Здесь освещаются самые последние мероприятия, которые будут происходить в ближайшее время. Есть данные относительно того, в какой ресторан лучше всего сходить. Отмечены самые интересные кафе для того, чтобы отправиться туда с друзьями. Рассматриваются различные варианты жилья, в том числе, хостелы, гостиницы, аренда комнат, квартир. Имеется информация про метро, общественный транспорт, а также железнодорожный.
Hello there! novo pharmacy great web site.
Prostadine is a dietary supplement formulated to support prostate health, particularly in men experiencing symptoms of benign prostatic hyperplasia (BPH) or other prostate-related issues. As men age, maintaining prostate health becomes increasingly important to avoid urinary discomfort and other related problems. Prostadine aims to provide a natural solution through a blend of ingredients known for their beneficial effects on the prostate. https://sites.google.com/spsw.edu.pl/prostadine/
Safety is paramount when playing online games. Players should ensure they are playing on reputable platforms
aviator game
Алтайский центр природного камня предлагает прекрасную возможность купить глыбы со мхом и лишайником по лучшим ценам. Мы сэкономим ваши деньги! Обслуживание у нас прекрасное. Можете убедиться в этом лично. Чтобы получить фото камня и узнать сроки поставки, отправьте запрос в WhatsApp. К вашим услугам доставка. https://altdikam.ru/chunks-of-stone-large-and-small.html – сайт, который вам понравится. Мы, не прекращая, работаем над тем, чтобы его улучшить. Здесь все понятно и наглядно. Созвонитесь с нами при возникновении вопросов. С радостью проконсультируем.
Glucotil is a dietary supplement designed to support healthy blood sugar levels and overall metabolic health. Managing blood sugar is crucial for individuals with diabetes or pre-diabetes, as well as for those looking to maintain healthy energy levels and prevent future metabolic issues. Glucotil combines natural ingredients that have been shown to positively affect blood glucose regulation and insulin sensitivity.
https://sites.google.com/spsw.edu.pl/glucotil/
Hello! cialis online pharmacy paypal very good website.
The Dota 2 website https://dota2-kz.kz provides the most complete information about the latest game updates, tournaments and upcoming events. We are here for every winning tactic, secret and important guide.
Latest news about games for Android https://android-games.kz, reviews and daily updates. Read now and get the latest information about the most exciting games
Game World online https://games-online-eg.com the latest online gaming news, game reviews, gameplay, ideas, gaming tactics and tips. The most popular and amazing games and get ready to become the leader in the online gaming world!
Origins of the Aviator Game
aviator game
Доверие – центр, который вас приглашает воспользоваться услугами. Приём психолога для записи можно обратиться по контактному номеру телефона. Семейный психолог делает так, чтобы для обоих супругов консультации были комфортными. https://ack-group.ru – сайт, где вы узнаете более детальную информацию. Подростковый психолог выяснит уровень вашей проблемы и подберет подходящий способ ее решения. Цена консультации психолога доступна любому. Психолог в Спб поможет наладить отношения с собой и окружающими. Обращайтесь в любое время!
Howdy! best online pharmacy canada pharmacy good website.
car game movie difference between film and digitalmovies redstonemlp movie castwhat to season spaghetti meat with
Staying Calm: Keeping a cool head and avoiding impulsive decisions during gameplay.
aviator game
ondansetron 8mg us – ondansetron 8mg cost order ropinirole without prescription
There are a lot of people supproting the Royal Academy of Music: Mikhail Bakhtiarov, Elton John, many businessmen and other individuals. No wonder. Young talents and future stars of Opera are studying here. Royal Academy of Music Mikhail Bakhtiarov
Howdy! canada discount pharmacy excellent web site.
People that support Bicentenary Prize: Mikhail Bakhtiarov and Svetlana Besfamilnaya. Bicentenary Prize is one of the main Royal Academy of Music’s events. Bicentenary Prize Mikhail Bakhtiarov
zofran 4mg us – tolterodine 1mg price ropinirole 1mg without prescription
Evolution and Technological Advancements
aviator game
Compatibility with Devices
aviator game
The Dota 2 website https://dota2-ar.com provides the most detailed information about the latest game updates, tournaments and upcoming events. We have all the winning tactics, secrets and important guides.
Evolution and Technological Advancements
best male sexual health
Safety and Fair Play
buy pills for erectile dysfunction
Sugar Defender is a dietary supplement designed to help regulate blood sugar levels and support overall metabolic health. Targeting individuals with pre-diabetes, diabetes, or those seeking to maintain stable blood sugar levels, Sugar Defender combines natural ingredients known for their ability to improve glucose metabolism and enhance insulin sensitivity. https://sites.google.com/spsw.edu.pl/sugardefender/
Howdy! md pharmacy discounts cialas excellent site.
Nagano Tonic is a dietary supplement designed to promote overall health and wellness. Drawing inspiration from traditional Japanese medicine and modern nutritional science, Nagano Tonic incorporates a blend of natural ingredients known for their health-boosting properties. This supplement aims to enhance energy levels, support immune function, and improve overall vitality. https://sites.google.com/spsw.edu.pl/naganotonicleanbelly/
Yes, the Aviator Game is compatible with mobile devices. Players can enjoy the game on their smartphones or
enlargement pills
ZenCortex is a nootropic supplement designed to enhance cognitive function, support brain health, and improve mental clarity. By combining a blend of natural ingredients known for their neuroprotective and cognitive-enhancing properties, ZenCortex aims to boost memory, focus, and overall brain performance. https://sites.google.com/spsw.edu.pl/zencortex/
SeroLean is a dietary supplement designed to support weight loss and overall metabolic health. By leveraging the power of natural ingredients, SeroLean aims to help individuals achieve their weight management goals by enhancing serotonin levels, reducing appetite, and promoting fat metabolism. https://sites.google.com/spsw.edu.pl/serolean/
Hi! buy accutane canadian pharmacy excellent internet site.
LeanGene is a dietary supplement designed to support weight loss and metabolic health by targeting genetic and metabolic pathways. Utilizing a blend of natural ingredients, LeanGene aims to enhance fat burning, suppress appetite, and improve overall metabolic function, helping individuals achieve their weight management goals more effectively.
https://sites.google.com/spsw.edu.pl/leangene/
Evolution and Technological Advancements
penis extenders
Pineal XT is a dietary supplement formulated to enhance sleep quality and support sleep patterns. Known for its natural ingredients, Pineal XT particularly focuses on boosting melatonin production, aiding individuals in managing sleep-related issues effectively. https://sites.google.com/spsw.edu.pl/pinealxt/
Hi! mexican pharmacy no prescription excellent internet site.
buy ascorbic acid 500mg – buy isordil no prescription cost compro
Ignoring Patterns: Failing to observe and learn from the game’s patterns can reduce your chances of winning.
best male supplements
Hi there! online pharmacy no prescription lithium good web site.
Prodentim offers a range of innovative dental care products designed to promote optimal oral health. From toothpaste to oral rinses, Prodentim products are formulated with advanced ingredients to address various dental concerns and enhance overall oral hygiene. https://sites.google.com/spsw.edu.pl/prodentim/
Puravive is a dietary supplement designed to support weight loss and overall metabolic health. By leveraging a blend of natural ingredients known for their fat-burning and metabolism-boosting properties, Puravive aims to help individuals achieve their weight management goals and enhance their overall well-being. https://sites.google.com/spsw.edu.pl/puravive-web/
cash out before the plane crashes. The objective is to maximize winnings by timing the cash-out perfectly,
animale male enhancement
Howdy! half mile pharmacy canada good site.
movie theater collegeville pa look at me movie 2022bridge season 2kgf director first moviemaya ali movies and tv shows
Rise of RA подходит для всех типов игроков: от новичков до профессионалов. https://rise-of-ra.com/ru/ – тут узнаете, как в Rise of RA выигрывать, почему предсказывать победы нельзя и другое. Мы собрали для вас реальные отзывы, чтобы вы могли составить собственное мнение о слоте. Rise of RA – это великолепный выбор для любителей древнеегипетской тематики. Слот имеет прекрасную графику, анимацию и звуковое сопровождение. Погрузитесь в атмосферу загадочного Египта!
На сайте https://mosprorezka.ru/ уточните телефон мастера для того, чтобы воспользоваться такой важной и нужной услугой, как лазерная резка. Обратиться в компанию можно, независимо от сложности работы. При этом она обойдется по привлекательной стоимости. Постоянно в компании проходят акции, а потому вы сможете воспользоваться услугой, сэкономив на этом. Работа происходит без предоплаты, а потому это очень выгодно. Уточнить необходимую информацию вы сможете в любое время, потому как компания работает в круглосуточном режиме.
Hello there! onlie pharmacy with echeck good internet site.
Some individuals that support the Royal Opera House – Mikhail Bakhtiarov, Jette and Alan Parker, Bob and Tamar Manoukian, Sandra and Anthony Gutman, Charles Holloway and others. All of them are members of the Honorary Directors’ Board. Royal Opera House Mikhail Bakhtiarov
Приветствую. Подскажите, где найти разные блоги о недвижимости? Сейчас читаю https://kran-rdk.ru
include welcome bonuses, loyalty rewards, and special promotions that provide additional chances to win and
sildenafil vardenafil
Some individuals (businessmen) admiring art & music support Teatro La Fenice: Mikhail Bakhtiarov, for example, helped to organize New Generation Festival in Florence. La Fenice Mikhail Bakhtiarov
players globally. The Aviator Game stands out in this crowded market due to its innovative gameplay and the
men’s supplements
Hi! world best online pharmacy good web page.
Всем привет! Может кто знает, где почитать полезные статьи о недвижимости? Пока нашел https://mart-posters.ru
the opportunity to compete for larger prizes and showcase their skills on a larger stage.
men’s health supplements
Among the members of the Board of Honorary Directors of the Royal Opera House there are such persons as Sir Lloyd Dorfman (the chair), Ricki Gail Conway, Philipp Freise, Mikhail Bakhtiarov, Charles and Kaaren Hale and others. Mikhail Bakhtiarov
Howdy! buy accutane canadian pharmacy very good internet site.
ascorbic acid drug – order isordil generic purchase prochlorperazine
Зайдите на сайт https://moresliv.cc/ где вы сможете скачать огромное количество курсов бесплатно онлайн через торрент. Огромная база знаний и обучений. Складчины и видеоуроки, книги и вебинары – графика, программирование, бизнес, курсы блогеров и многое другое здесь. Более 175.000 различных курсов на сайте. Заходи!
The Aviator Game uses a Random Number Generator (RNG) to ensure fair play. This technology ensures that each
best male sexual health
Hi! lasix-uni-pharmacy beneficial internet site.
Всем привет! Может кто знает, где найти полезные блоги о недвижимости? Сейчас читаю https://metrazhi-omsk.ru
Hello! clomid 100mg online canadian pharmacy beneficial site.
not, you lose your bet.
best male enhancement pills
Hello! diflucan pill – pharmacy good internet site.
На сайте https://autoclub78.ru вы найдете интересные, практичные советы для тех, у кого есть автомобиль. Имеются практические рекомендации, ценные советы, которые помогут найти оптимальный вариант для того, чтобы правильно эксплуатировать технику. Статьи ответят на многочисленные вопросы, подскажут, как правильно действовать в определенной ситуации. Есть информация про самые востребованные мотоциклы, а также запчасти, которые реализуются на маркетплейсах. Есть информация и про то, как не стоит приобретать стеклоомывающую жидкость.
Всем привет! Подскажите, где найти разные статьи о недвижимости? Пока нашел https://mik-dom.ru
Puravive is a dietary supplement designed to support weight loss and overall metabolic health. By leveraging a blend of natural ingredients known for their fat-burning and metabolism-boosting properties, Puravive aims to help individuals achieve their weight management goals and enhance their overall well-being. https://sites.google.com/spsw.edu.pl/puravive-web/
Cardio Defend is a dietary supplement designed to support cardiovascular health. Utilizing a blend of natural ingredients, Cardio Defend aims to improve heart function, promote healthy blood pressure, and enhance overall cardiovascular wellness. This article explores the composition, benefits, clinical evidence, and user experiences related to Cardio Defend. https://sites.google.com/spsw.edu.pl/cardiodefend/
advancements have allowed for improved graphics, smoother gameplay, and more interactive features. These
best sexual performance pills
Hi there! coupons for 247 overnight pharmacy great internet site.
Kerassentials is a skincare and nail care product designed to promote healthy, strong nails and improve the overall condition of the skin. Combining natural and scientifically-backed ingredients, Kerassentials targets common issues such as fungal infections, brittle nails, and dry skin, providing a comprehensive solution for maintaining nail and skin health. https://sites.google.com/spsw.edu.pl/kerassentials-try/
EyeFortin is an all-natural eye-health supplement that helps to keep your eyes healthy even as you age. It prevents infections and detoxifies your eyes while also being stimulant-free. This makes it a great choice for those who are looking for a natural way to improve their eye health. https://sites.google.com/spsw.edu.pl/eyefortin/
Burn Boost is a dietary supplement designed to aid in weight management and fat loss. Combining a blend of natural ingredients, Burn Boost aims to increase metabolism, enhance energy levels, and support overall weight loss efforts. This article explores the composition, benefits, clinical evidence, and user experiences related to Burn Boost. https://sites.google.com/spsw.edu.pl/burnboost/
Evolution and Technological Advancements
how to make dick bigger
GlucoTrust is a dietary supplement designed to support healthy blood sugar levels and improve overall metabolic health. Combining a blend of natural ingredients known for their beneficial effects on blood sugar regulation, GlucoTrust aims to provide a comprehensive solution for individuals looking to manage their blood sugar levels naturally. This article explores the composition, benefits, clinical evidence, and user experiences related to GlucoTrust. https://sites.google.com/spsw.edu.pl/glucotrust/
Alpha Tonic is a dietary supplement designed to support male vitality, energy, and overall performance. Combining a blend of natural ingredients known for their beneficial effects on male health, Alpha Tonic aims to provide a comprehensive solution for men looking to enhance their physical and mental well-being. This article explores the composition, benefits, clinical evidence, and user experiences related to Alpha Tonic. https://sites.google.com/spsw.edu.pl/alphatonic/
Приветствую. Может кто знает, где найти разные статьи о недвижимости? Сейчас читаю https://miro-teh-ural.ru
Hello there! canadienpharmacy24 excellent site.
Red Boost is a dietary supplement formulated to support male vitality, enhance physical performance, and improve overall well-being. With a blend of potent natural ingredients, Red Boost aims to address common issues related to male health, such as low energy, reduced libido, and decreased stamina. This article delves into the composition, benefits, clinical evidence, and user experiences of Red Boost. https://sites.google.com/spsw.edu.pl/redboost/
Risk Management: Setting limits on how much to bet and when to cash out.
best male enhancement pills
Opened up an enthralling read – I’d like to share it with you https://www.bakespace.com/members/profile/mostbetpoland/1647963/
Hello there! paypal drugstore clomid great site.
Обеспечьте себе доход, привлекая пользователей в MP Manager. Детальную информацию вы найдете на нашем ресурсе, посмотрите ее уже сегодня. Наш сервис поможет вам настроить эффективную рекламу, что позволит сократить затраты и увеличить продажи. https://mpmgr.ru – тут можете прочитать отзывы клиентов и записаться на индивидуальную консультацию. Напишите ваш телефон и нажмите на «Отправить». Мы расскажем вам, как автоматизировать работу на платформах OZON и Wildberries.
CVzen to najlepsza usługa pisania CV https://cvzen.pl/ i coach kariery dla milionów osób poszukujących pracy na całym świecie. Nasz zespół ekspertów jest zaangażowany w Twój sukces i będzie Cię wspierał przez całą Twoją karierę, od napisania profesjonalnego CV i listu motywacyjnego z uwzględnieniem specyfiki branży, po optymalizację profilu LinkedIn i zapewnienie profesjonalnego coachingu kariery. Odblokuj nowe możliwości dzięki CV, które pokaże Twój potencjał.
Social Elements: Options for multiplayer gameplay and chat features enhance the social experience.
levitra online
Приветствую. Может кто знает, где найти полезные блоги о недвижимости? Сейчас читаю https://mzhk-stroy.ru
Привлекайте пользователей в MP Manager и получайте стабильный доход. Узнайте об этом на нашем сайте, информация в доступе в любое время. Портал окажет помощь вам в настройке рекламы, что даст возможность увеличить продажи и понизить затраты. Ищете продвижение карточек товара на wildberries? Mpmgr.ru – тут у вас есть возможность прочесть отзывы клиентов и на индивидуальную консультацию оставить заявку. Укажите свой номер телефона, чтобы на демонстрацию сервиса записаться. Расскажем, как автоматизировать работу на популярных торговых площадках Wildberries и OZON.
Привет, друзья!
Где приобрести диплом специалиста?
Мы готовы предложить документы ВУЗов, которые расположены на территории всей России. Вы сможете заказать качественный диплом за любой год, в том числе документы СССР. Дипломы выпускаются на “правильной” бумаге самого высокого качества. Это дает возможности делать настоящие дипломы, не отличимые от оригиналов. Они заверяются всеми обязательными печатями и подписями.
Мы можем предложить дипломы любой профессии по приятным ценам.
ast-diplom.com
Всегда вам поможем!
Hello there! pharmacy rx one review very good web page.
cash-out perfectly.
penis enlargement pump
На сайте https://mpmgr.ru вы сможете воспользоваться менеджером маркетплейсов, который необходим для автоматизации работы с Ozon, Wildberries и другими. Система сама управляет рекламой, рассчитывает поставки, а также отвечает на отзывы от клиентов. Кроме того, происходит отслеживание товаров, самостоятельный расчет скидки. Прямо сейчас вы сможете протестировать абсолютно бесплатно. Представляет собой комплексный инструмент, предназначенный для развития бизнеса. Менеджер оптимизирует расходы с той целью, чтобы вы получили огромную прибыль.
PotentStream is a dietary supplement designed to enhance male vitality, energy levels, and overall performance. Combining a blend of potent natural ingredients, PotentStream aims to provide a comprehensive solution for men experiencing issues related to low energy, reduced libido, and decreased stamina. This article explores the composition, benefits, clinical evidence, and user experiences of PotentStream.
https://sites.google.com/spsw.edu.pl/potentstream/
guys night movies the sinner season 1 episode 1 castandy warhol’s blue movieparakeet molting seasonnext episode of bachelorette 2022
Приветствую. Подскажите, где почитать разные блоги о недвижимости? Пока нашел https://nagaevodom.ru
Hi! pharmacy in france that sales revatio very good internet site.
game is random and unbiased, providing a fair chance for all players to win.
enlarge penis
This excellent website definitely has all the info I wanted about this subject and didn’t
know who to ask.
Hi! online pharmacy paypal accepted great web site.
Желаете познакомиться с новыми людьми и отыскать вторую половинку? Лилибум готов вам помочь. Это бесплатный сайт знакомств, где точно найдете хороших друзей и, возможно, даже истинную любовь. https://www.lilibum.ru – поможет вам провести свое время с пользой и с интересом. Вас ждет привлекательный дизайн сайта и возможность быстро зарегистрироваться. Фотографии и анкеты тщательно проверяются модераторами. Мы уделяем пристальное внимание вашей безопасности и анонимности. С помощью Лилибум вы обязательно встретите свою любовь!
Приветствую. Может кто знает, где найти разные блоги о недвижимости? Сейчас читаю https://potolkinomer1.ru
back for more.
cheaper alternative to cialis
эскорт агентства москва
На сайте https://good-lawn.ru/ustroystvo-gazona у вас есть возможность оставить заявку на услугу по благоустройству территории и озеленению участков. Проектируя «дизайн загородной жизни» компания начинает свою работу с генерального плана участка, где будут учтены все пожелания и нюансы клиента. Примеры работ, цены и отзывы вы найдете на нашем портале. Все архитекторы компании имеют профильное образование и являются призерами дизайнерских конкурсов. Если хотите получить консультацию, оставьте заявку и специалисты свяжутся с вами в ближайшее время.
москва эскорт
Hi there! canadian pharmacy 100mg viagra great web site.
winnings.
how to grow your dick
Привет, друзья!
Где приобрести диплом по необходимой специальности?
Мы можем предложить документы ВУЗов, которые расположены в любом регионе России. Вы сможете приобрести качественный диплом от любого высшего учебного заведения, за любой год, указав актуальную специальность и оценки за все дисциплины. Дипломы выпускаются на бумаге высшего качества. Это позволяет делать государственные дипломы, не отличимые от оригинала. Документы заверяются всеми необходимыми печатями и штампами.
Мы предлагаем дипломы любой профессии по доступным тарифам.
diploms-x24.ru
Будем рады вам помочь!
Hello! ed dysfunction treatment very good web page.
Всем привет! Подскажите, где почитать полезные блоги о недвижимости? Пока нашел https://promresmag.ru
MP Manager приглашайте пользователей и получайте постоянный доход. Подробнее узнать об этом есть возможность на нашем ресурсе. С информацией можно ознакомиться прямо сейчас. Сервис поможет настроить эффективную рекламу, благодаря чему вы сможете сократить затраты и увеличить продажи. Ищете продвижение товаров на wildberries цена? Mpmgr.ru – здесь можно прочитать отзывы клиентов, а также записаться на персональную консультацию. Просто укажите ваш контактный номер телефона и нажмите на специальную кнопку «Отправить». Мы объясним вам, как на OZON и Wildberries автоматизировать работу.
Hi there! ed pills good web page.
На сайте https://chargebackhelp.ru/ изучите информацию, которая касается чарджбэка. Вы узнаете о том, как можно вернуть деньги у брокера, что представляет собой данная процедура, как правильно использовать ее возможности и каким образом получить деньги. Вся информация от высококлассного специалиста, который отлично понимает в данной теме. Здесь вся информация подробно описана, чтобы вы смогли лучше в ней сориентироваться. Есть информация и о том, с карточками каких банков могут быть трудности при возвращении средств.
Vips13un.kinoportal.live – портал, где собраны лучшие фильмы. Вас приятно удивит качество видео. На странице можно найти информацию о дате выхода фильма и его длительности, также жанре и стране. Регулярно добавляем новинки. У нас представлена большая коллекция фильмов. https://vips13un.kinoportal.live – прекрасно организованный ресурс. Тут имеется удобный поисковик и плеер. Вы точно сможете для себя что-то интересное подобрать. Чтобы насладиться качественным фильмом, достаточно пару кликов мышью. Заходите на KinoPortal!
Всем привет! Подскажите, где найти разные блоги о недвижимости? Сейчас читаю https://santech31.ru
Hello there! men’s ed pills excellent website.
wow raid carry service kreativwerkstatt-esens.de .
На сайте https://podvodka.okis.ru/ у вас есть возможность заказать качественные гибкие подводки из нержавеющей стали. Широкий перечень продукции, такой как сильфонные гибкие подводки и многое другое вы можете заказать на сайте по телефону. Пользователи в считанные минуты смогут купить товар и найти необходимые модели. Меню сайта позволит вам отыскать то, что вас интересует. Также здесь есть таблица на размеры с ценой, руководство по монтажу и технические характеристики подводки с фото.
Всем привет! Может кто знает, где найти разные блоги о недвижимости? Пока нашел https://santex-expert.ru
Hi there! best ed pills at gnc very good internet site.
Hello! ed remedies excellent web site.
Приветствую. Может кто знает, где найти разные блоги о недвижимости? Сейчас читаю https://schuconvr.ru
На сайте https://stroy-m2.ru/gruzoperevozki/ уточните расценки на такую важную услугу, как грузоперевозки не только в Нижнем Новгороде, но и по всей стране. К наиболее популярным работам относят: перевозка, переезды. При необходимости каждый желающий получает возможность заказать дачный, квартирный переезд, а также офисный. В обязательном порядке соблюдаются все требования. Работы выполняют компетентные и опытные специалисты. На все услуги установлены доступные расценки. При этом они точно не изменятся после того, как их озвучат.
Hi there! ed pills cheap good internet site.
Stumbled upon interesting material – I can’t help but recommend you to read https://forms.americantowns.com/viewevent/73133854
order durex gel – buy durex gel cheap zovirax drug
Приветствую. Подскажите, где почитать разные статьи о недвижимости? Сейчас читаю https://simposad.ru
На сайте https://shemi-otopleniya.ru/ вам предлагают качественную гибкую подводку из нержавеющей стали. Здесь вы сможете найти подробные характеристики с фото товара, а также увидеть всю продукцию. Вся гибкая подводка производится из высококачественной нержавейки. На сайте у вас есть возможность найти раздел с акциями и спецпредложениями. Гибкую подводку вы сможете приобрести под заказ самой разной модификации, диаметра и формы. Портал предлагает исчерпывающую информацию о гибкой подводке, ознакомьтесь с ней в любое удобное время.
how to order durex gel – buy cheap durex condoms where to buy latanoprost without a prescription
Hi there! top rated ed pills beneficial internet site.
Зайдите на сайт Научно-технического центра «Триада» https://triadacompany.ru/ который помогает тысячам предприятий обеспечивать промышленную и экологическую безопасность по всей России! Лучшие кадры, инновационный подход, опыт с 1991 года. Промышленная и экологическая безопасность, экспертиза, проектирование, консалтинг. Подробнее на сайте.
Приветствую. Подскажите, где почитать разные статьи о недвижимости? Сейчас читаю https://smgarant.ru
На сайте https://sochi.calypso.ooo/ у вас получится быстро отыскать и забронировать яхту, катер либо парусники. Компания насчитывает 20 филиалов, обслуживает более полутора тысяч клиентов в год. Все судна исправные, отличаются привлекательным, стильным дизайном. При этом заказать можно в любое, наиболее комфортное время и на несколько часов. Все ограничивается лишь вашими пожеланиями, предпочтениями. Этот сервис поможет вам подобрать наиболее подходящий вариант на прогулку, романтическое свидание или празднование торжества.
Howdy! non prescription erection pills excellent web site.
Hi there! best pills for ed beneficial web site.
Всем привет! Подскажите, где почитать полезные блоги о недвижимости? Пока нашел https://stilnyjpol.ru
外送茶
外送茶是什麼?禁忌、價格、茶妹等級、術語等..老司機告訴你!
外送茶是什麼?
外送茶、外約、叫小姐是一樣的東西。簡單來說就是在通訊軟體與茶莊聯絡,選好自己喜歡的妹子後,茶莊會像送飲料這樣把妹子派送到您指定的汽車旅館、酒店、飯店等交易地點。您只需要在您指定的地點等待,妹妹到達後,就可以開心的開始一場美麗的約會。
外送茶種類
學生兼職的稱為清新書香茶
日本女孩稱為清涼綠茶
俄羅斯女孩被稱為金酥麻茶
韓國女孩稱為超細滑人參茶
外送茶價格
外送茶的客戶相當廣泛,包括中小企業主、自營商、醫生和各行業的精英,像是工程師等等。在台北和新北地區,他們的消費指數大約在 7000 到 10000 元之間,而在中南部則通常在 4000 到 8000 元之間。
對於一般上班族和藍領階層的客人來說,建議可以考慮稍微低消一點,比如在北部約 6000 元左右,中南部約 4000 元左右。這個價位的茶妹大多是新手兼職,但有潛力。
不同地區的客人可以根據自己的經濟能力和喜好選擇適合自己的價位範圍,以免感到不滿意。物價上漲是一個普遍現象,受到地區和經濟情況等因素的影響,茶莊的成本也在上升,因此價格調整是合理的。
外送茶外約流程
加入LINE:加入外送茶官方LINE,客服隨時為你服務。茶莊一般在中午 12 點到凌晨 3 點營業。
告知所在地區:聯絡客服後,告訴他們約會地點,他們會幫你快速找到附近的茶妹。
溝通閒聊:有任何約妹問題或需要查看妹妹資訊,都能得到詳盡的幫助。
提供預算:告訴客服你的預算,他們會找到最適合你的茶妹。
提早預約:提早預約比較好配合你的空檔時間,也不用怕到時候約不到你想要的茶妹。
外送茶術語
喝茶術語就像是進入茶道的第一步,就像是蓋房子打地基一樣。在這裡,我們將這些外送茶入門術語分類,讓大家能夠清楚地理解,讓喝茶變得更加容易上手。
魚:指的自行接客的小姐,不屬於任何茶莊。
茶:就是指「小姐」的意思,由茶莊安排接客。
定點茶:指由茶莊提供地點,客人再前往指定地點與小姐交易。
外送茶:指的是到小姐到客人指定地點接客。
個工:指的是有專屬工作室自己接客的小姐。
GTO:指雞頭也就是飯店大姊三七茶莊的意思。
摳客妹:只負責找客人請茶莊或代調找美眉。
內機:盤商應召站提供茶園的人。
經紀人:幫內機找美眉的人。
馬伕:外送茶司機又稱教練。
代調:收取固定代調費用的人(只針對同業)。
阿六茶:中國籍女子,賣春的大陸妹。
熱茶、熟茶:年齡比較大、年長、熟女級賣春者(或稱阿姨)。
燙口 / 高溫茶:賣春者年齡過高。
台茶:從事此職業的台灣小姐。
本妹:從事此職業的日本籍小姐。
金絲貓:西方國家的小姐(歐美的、金髮碧眼的那種)。
青茶、青魚:20 歲以下的賣春者。
乳牛:胸部很大的小姐(D 罩杯以上)。
龍、小叮噹、小叮鈴:體型比較肥、胖、臃腫、大隻的小姐。
medicine in mexico pharmacies: mexican pharmacy – medication from mexico pharmacy
Howdy! ed pills online good site.
Всем привет! Подскажите, где почитать полезные блоги о недвижимости? Пока нашел https://tc-all.ru
Хотите взять напрокат коляски и костыли? Мы вам поможем. Если вы арендуете коляску, то получите возможность замены в случае поломки и техническое обслуживание, это вас освободит от ненужных хлопот. Смело можете протестировать перед приобретением разные модели, для выбора подходящей. Наши инвалидные коляски высочайшего качества. Ищете складные инвалидные коляски напрокат? Arenda-invalidnyh-kolyasok.ru – сайт, где у вас есть возможность узнать, почему лучше арендовать, а не покупать. Используйте смело услуги проката, не стесняйтесь. Предоставляем великолепное обслуживание, обращайтесь к нам, и вы точно останетесь довольны.
Hello! treatment of ed beneficial site.
Привлекайте пользователей в MP Manager и обеспечьте себе стабильный доход. Более подробную информацию вы можете найти на нашем сайте, ознакомиться с ней можно в любое время. Наш сайт настроит для вас эффективную рекламу, это даст возможность увеличить продажи и сократить затраты. https://mpmgr.ru – тут можете прочитать отзывы клиентов и записаться на индивидуальную консультацию. Укажите ваш номер телефона, после чего нажмите на кнопку «Отправить». Как автоматизировать работу на платформах Wildberries и OZON, мы обязательно расскажем вам.
Good site! I truly love how it is easy on my eyes it is. I am wondering how I might be notified when a new post has been made. I’ve subscribed to your RSS which may do the trick? Have a great day!
Всем привет! Может кто знает, где почитать полезные статьи о недвижимости? Сейчас читаю https://teplohod-denisdavidov.ru
Howdy! generic ed pills very good site.
thank, I thoroughly enjoyed reading your article. I really appreciate your wonderful knowledge and the time you put into educating the rest of us.
Its wonderful as your other blog posts : D, regards for putting up.
На сайте https://v8prof.ru/ вы сможете получить консультацию и воспользоваться полезными информационными продуктами. Компания предлагает возможность перейти на отечественное ПО, после чего настроить под требования, потребности. Есть возможность воспользоваться демо-версией, протестировать решения 1С и изучить предложение перед тем, как приобрести. Возможно, вам приглянется аренда 1С, что дает возможность значительно сэкономить финансы. Также воспользуйтесь возможностью удаленного обслуживания программ. Работа при помощи удаленного приложения.
Приветствую. Может кто знает, где почитать разные блоги о недвижимости? Пока нашел https://titovloft.ru
Хайп казино
Приветствую. Может кто знает, где почитать разные блоги о недвижимости? Пока нашел https://toadmarket.ru
Приветствуем вас на канале проекта casino VAVADA! Здесь имеется самая свежая информация. Забудьте о повседневных заботах и проведите время за увлекательными слотами в высококачественном онлайн-казино Вавада! Вас ждет отменная графика и невероятная атмосфера. Ищете отзывы vavada? t.me/mvavada – здесь мы делимся с вами своими знаниями и секретами успеха. Казино VAVADA подходит всем без исключения. Вы точно оцените бонусы и скорость выводов. Саппорт старается любые вопросы решать довольно быстро. Играйте прямо сейчас. Больших вам выигрышей!
Stumbled upon a unique article, I suggest you take a look http://minimoo.eu/index.php/en/forum/welcome-mat/666235-luxurious-latvian-escorts-for-every-occasion
Всем привет! Подскажите, где почитать полезные статьи о недвижимости? Сейчас читаю https://u-mechanik.ru
На сайте http://kak-vernut-dengi.ru/ представлена интересная, исчерпывающая информация о том, как получится вернуть средства у брокера, если он получил их незаконным либо нечестным путем, но при этом обещал высокую доходность. Специалист в своих статьях как раз рассказывает о том, как вернуть средства законным путем у таких лжеброкеров. Здесь находятся и любопытные видеоматериалы, которые понравятся тем, что они содержательные и информативные. В них детально показывается то, как это правильно сделать, чтобы не ошибиться.
Very good information, Appreciate it.
Приветствую. Может кто знает, где найти полезные блоги о недвижимости? Сейчас читаю https://utc96.ru
Howdy! online pharmacy india excellent internet site.
drive in movie near me movie times for tuesdaywhere can i watch one piece film red redditsonic the hedgehog movie 2 castmovies hillsdale
外送茶
外送茶是什麼?禁忌、價格、茶妹等級、術語等..老司機告訴你!
外送茶是什麼?
外送茶、外約、叫小姐是一樣的東西。簡單來說就是在通訊軟體與茶莊聯絡,選好自己喜歡的妹子後,茶莊會像送飲料這樣把妹子派送到您指定的汽車旅館、酒店、飯店等交易地點。您只需要在您指定的地點等待,妹妹到達後,就可以開心的開始一場美麗的約會。
外送茶種類
學生兼職的稱為清新書香茶
日本女孩稱為清涼綠茶
俄羅斯女孩被稱為金酥麻茶
韓國女孩稱為超細滑人參茶
外送茶價格
外送茶的客戶相當廣泛,包括中小企業主、自營商、醫生和各行業的精英,像是工程師等等。在台北和新北地區,他們的消費指數大約在 7000 到 10000 元之間,而在中南部則通常在 4000 到 8000 元之間。
對於一般上班族和藍領階層的客人來說,建議可以考慮稍微低消一點,比如在北部約 6000 元左右,中南部約 4000 元左右。這個價位的茶妹大多是新手兼職,但有潛力。
不同地區的客人可以根據自己的經濟能力和喜好選擇適合自己的價位範圍,以免感到不滿意。物價上漲是一個普遍現象,受到地區和經濟情況等因素的影響,茶莊的成本也在上升,因此價格調整是合理的。
外送茶外約流程
加入LINE:加入外送茶官方LINE,客服隨時為你服務。茶莊一般在中午 12 點到凌晨 3 點營業。
告知所在地區:聯絡客服後,告訴他們約會地點,他們會幫你快速找到附近的茶妹。
溝通閒聊:有任何約妹問題或需要查看妹妹資訊,都能得到詳盡的幫助。
提供預算:告訴客服你的預算,他們會找到最適合你的茶妹。
提早預約:提早預約比較好配合你的空檔時間,也不用怕到時候約不到你想要的茶妹。
外送茶術語
喝茶術語就像是進入茶道的第一步,就像是蓋房子打地基一樣。在這裡,我們將這些外送茶入門術語分類,讓大家能夠清楚地理解,讓喝茶變得更加容易上手。
魚:指的自行接客的小姐,不屬於任何茶莊。
茶:就是指「小姐」的意思,由茶莊安排接客。
定點茶:指由茶莊提供地點,客人再前往指定地點與小姐交易。
外送茶:指的是到小姐到客人指定地點接客。
個工:指的是有專屬工作室自己接客的小姐。
GTO:指雞頭也就是飯店大姊三七茶莊的意思。
摳客妹:只負責找客人請茶莊或代調找美眉。
內機:盤商應召站提供茶園的人。
經紀人:幫內機找美眉的人。
馬伕:外送茶司機又稱教練。
代調:收取固定代調費用的人(只針對同業)。
阿六茶:中國籍女子,賣春的大陸妹。
熱茶、熟茶:年齡比較大、年長、熟女級賣春者(或稱阿姨)。
燙口 / 高溫茶:賣春者年齡過高。
台茶:從事此職業的台灣小姐。
本妹:從事此職業的日本籍小姐。
金絲貓:西方國家的小姐(歐美的、金髮碧眼的那種)。
青茶、青魚:20 歲以下的賣春者。
乳牛:胸部很大的小姐(D 罩杯以上)。
龍、小叮噹、小叮鈴:體型比較肥、胖、臃腫、大隻的小姐。
Приветствую. Может кто знает, где почитать полезные блоги о недвижимости? Пока нашел https://vortex-los.ru
Hi there! canadian pharmacy review excellent web page.
Hi! pharmacy tech programs online great internet site.
Всем привет! Подскажите, где найти полезные блоги о недвижимости? Сейчас читаю https://yah-bomag.ru
Hello there! cialis online pharmacy good website.
Приветствую. Может кто знает, где найти полезные блоги о недвижимости? Пока нашел https://yaoknaa.ru
Hello! canada drugs direct very good internet site.
На сайте http://smartporog.ru изучите каталог выпадающих умных порогов, которые идеально подходят для самых разных видов дверей. Практичные и надежные конструкции выполнены из современных, уникальных материалов, которые не изменят своего вида и не поржавеют. Автоматические пороги станут оптимальным вариантом в тех случаях, где стационарные не получится установить. Уникальность конструкций заключается в том, что они борются со сквозняками, холодом. Дополнительно ограничивают попадание пыли.
Hello there! online vet pharmacy excellent web site.
апостиль в новосибирске
перевод документов
перевод с иностранных языков
перевод с иностранных языков
апостиль в новосибирске
Приветствую. Может кто знает, где найти разные блоги о недвижимости? Сейчас читаю https://zt365.ru
перевод с иностранных языков
Hi there! online canadian pharmacy great web page.
апостиль в новосибирске
перевод с иностранных языков
перевод с иностранных языков
перевод с иностранных языков
перевод с иностранных языков
перевод документов
апостиль в новосибирске
перевод документов
перевод документов
перевод документов
перевод документов
Всем привет! Подскажите, где найти разные статьи о недвижимости? Пока нашел https://astali.ru
перевод с иностранных языков
перевод документов
апостиль в новосибирске
перевод документов
апостиль в новосибирске
Алтайский центр природного камня предоставляет прекрасную возможность купить глыбы с лишайником и мхом по самым привлекательным ценам. Существенно сэкономим ваши денежные средства! Мы осуществляем доставку. Гарантируем великолепное обслуживание. Вы можете сами в этом убедиться. Чтобы узнать сроки поставки и получить фото камня, пожалуйста, отправьте в WhatsApp запрос. Ищете валуны глыбы купить? Altdikam.ru – сайт, постоянно работаем над его улучшением. Здесь все ясно и наглядно. Если у вас возникли какие-то вопросы, свяжитесь с нами по телефону. С удовольствием вам поможем!
перевод с иностранных языков
апостиль в новосибирске
апостиль в новосибирске
перевод с иностранных языков
апостиль в новосибирске
Всем привет! Может кто знает, где найти полезные блоги о недвижимости? Сейчас читаю https://batstroimat24.ru
апостиль в новосибирске
перевод документов
перевод документов
образование купить диплом оригинальный ast-diplomas.com .
Геракл24: Квалифицированная Смена Фундамента, Венцов, Настилов и Передвижение Строений
Компания Геракл24 специализируется на оказании комплексных услуг по смене фундамента, венцов, настилов и перемещению домов в городе Красноярске и в окрестностях. Наша группа опытных мастеров гарантирует превосходное качество реализации всех типов восстановительных работ, будь то древесные, с каркасом, кирпичные постройки или бетонные строения.
Плюсы работы с Геракл24
Профессионализм и опыт:
Весь процесс проводятся лишь профессиональными мастерами, имеющими большой стаж в области строительства и ремонта зданий. Наши мастера профессионалы в своем деле и реализуют работу с высочайшей точностью и вниманием к мелочам.
Комплексный подход:
Мы предоставляем полный спектр услуг по реставрации и реконструкции строений:
Замена фундамента: укрепление и замена старого фундамента, что позволяет продлить срок службы вашего здания и устранить проблемы, связанные с оседанием и деформацией.
Замена венцов: реставрация нижних венцов из дерева, которые чаще всего гниют и разрушаются.
Установка новых покрытий: установка новых полов, что существенно улучшает визуальное восприятие и функциональность помещения.
Передвижение домов: безопасное и надежное перемещение зданий на другие участки, что помогает сохранить здание и избежать дополнительных затрат на строительство нового.
Работа с любыми видами зданий:
Древесные строения: восстановление и укрепление деревянных конструкций, защита от гниения и вредителей.
Каркасные дома: реставрация каркасов и реставрация поврежденных элементов.
Кирпичные дома: реставрация кирпичной кладки и укрепление конструкций.
Бетонные строения: восстановление и укрепление бетонных структур, ремонт трещин и дефектов.
Качество и прочность:
Мы применяем лишь качественные материалы и новейшее оборудование, что обеспечивает долгий срок службы и прочность всех выполненных задач. Все проекты проходят строгий контроль качества на всех этапах выполнения.
Личный подход:
Для каждого клиента мы предлагаем персонализированные решения, учитывающие ваши требования и желания. Наша цель – чтобы итог нашей работы полностью удовлетворял вашим запросам и желаниям.
Почему стоит выбрать Геракл24?
Работая с нами, вы найдете надежного партнера, который возьмет на себя все заботы по восстановлению и ремонту вашего здания. Мы гарантируем выполнение всех проектов в установленные сроки и с соблюдением всех строительных норм и стандартов. Выбрав Геракл24, вы можете быть уверены, что ваше здание в надежных руках.
Мы готовы предоставить консультацию и ответить на все ваши вопросы. Контактируйте с нами, чтобы обсудить детали вашего проекта и получить больше информации о наших услугах. Мы поможем вам сохранить и улучшить ваш дом, обеспечив его безопасность и комфорт на долгие годы.
Геракл24 – ваш выбор для реставрации и ремонта домов в Красноярске и области.
аттестат за 9 класс купить http://www.diploms-x.com/ .
перевод с иностранных языков
перевод с иностранных языков
апостиль в новосибирске
перевод с иностранных языков
перевод документов
апостиль в новосибирске
апостиль в новосибирске
Get pill facts. Access medicine details.
where buy tadacip
Get pill facts. Medication data provided.
апостиль в новосибирске
перевод документов
апостиль в новосибирске
Всем привет! Может кто знает, где почитать разные блоги о недвижимости? Сейчас читаю https://bdrsu-2.ru
перевод с иностранных языков
апостиль в новосибирске
перевод документов
перевод с иностранных языков
апостиль в новосибирске
купить аттестат с занесением в реестр купить аттестат с занесением в реестр .
апостиль в новосибирске
купить диплом мами diploms-x.com .
перевод с иностранных языков
перевод с иностранных языков
перевод документов
перевод с иностранных языков
перевод документов
перевод с иностранных языков
Всем привет! Подскажите, где почитать разные блоги о недвижимости? Пока нашел https://centro-kraska.ru
апостиль в новосибирске
Find medication facts. Medication pamphlet available.
where can i buy tadacip
Medication details here. Find medicine information.
апостиль в новосибирске
перевод документов
перевод документов
перевод с иностранных языков
Геракл24: Опытная Замена Основания, Венцов, Покрытий и Перемещение Зданий
Фирма Gerakl24 профессионально занимается на предоставлении всесторонних сервисов по замене основания, венцов, настилов и перемещению зданий в месте Красноярском регионе и за пределами города. Наша команда квалифицированных мастеров обещает отличное качество выполнения всех видов ремонтных работ, будь то из дерева, каркасные, из кирпича или бетонные конструкции строения.
Преимущества работы с Gerakl24
Квалификация и стаж:
Все работы осуществляются только высококвалифицированными специалистами, с многолетним большой стаж в сфере строительства и восстановления строений. Наши сотрудники знают свое дело и выполняют проекты с высочайшей точностью и вниманием к мелочам.
Полный спектр услуг:
Мы предоставляем полный спектр услуг по реставрации и восстановлению зданий:
Смена основания: усиление и реставрация старого основания, что обеспечивает долгий срок службы вашего здания и устранить проблемы, вызванные оседанием и деформацией.
Замена венцов: реставрация нижних венцов из дерева, которые чаще всего подвержены гниению и разрушению.
Установка новых покрытий: монтаж новых настилов, что существенно улучшает визуальное восприятие и функциональные характеристики.
Перемещение зданий: качественный и безопасный перенос строений на новые места, что обеспечивает сохранение строения и избегает дополнительных затрат на возведение нового.
Работа с любыми типами домов:
Дома из дерева: восстановление и защита деревянных строений, обработка от гниения и насекомых.
Каркасные дома: усиление каркасных конструкций и замена поврежденных элементов.
Дома из кирпича: ремонт кирпичных стен и укрепление конструкций.
Бетонные дома: реставрация и усиление бетонных элементов, устранение трещин и повреждений.
Качество и прочность:
Мы работаем с только высококачественные материалы и передовые технологии, что гарантирует долгий срок службы и прочность всех выполненных задач. Все наши проекты проходят строгий контроль качества на каждой стадии реализации.
Личный подход:
Каждому клиенту мы предлагаем индивидуальные решения, учитывающие все особенности и пожелания. Наша цель – чтобы итог нашей работы полностью соответствовал вашим запросам и желаниям.
Почему стоит выбрать Геракл24?
Работая с нами, вы найдете надежного партнера, который берет на себя все заботы по ремонту и реставрации вашего дома. Мы обеспечиваем выполнение всех проектов в сроки, установленные договором и с соблюдением всех строительных норм и стандартов. Обратившись в Геракл24, вы можете быть спокойны, что ваше строение в надежных руках.
Мы всегда готовы проконсультировать и дать ответы на все вопросы. Свяжитесь с нами, чтобы обсудить детали вашего проекта и узнать о наших сервисах. Мы сохраним и улучшим ваш дом, сделав его уютным и безопасным для долгого проживания.
Gerakl24 – ваш надежный партнер в реставрации и ремонте домов в Красноярске и за его пределами.
https://gerakl24.ru/просел-дом-красноярск/
перевод документов
Здравствуйте!
Заказать диплом о высшем образовании.
Наша компания предлагает приобрести диплом в отличном качестве, который не отличить от оригинала без участия специалистов высокой квалификации со специальным оборудованием.
Где купить диплом по актуальной специальности?
http://industrial.getbb.ru/ucp.php?mode=login&sid=4b9245c5a07611f2172ddaa8175d7ebf
Успехов в учебе!
апостиль в новосибирске
Drug facts here. Comprehensive medication overview.
tadalafil
Pill information provided. Detailed pill knowledge.
перевод документов
апостиль в новосибирске
купить диплом военного училища ссср ast-diplomas.com .
Привет!
Купить диплом ВУЗа.
Мы предлагаем заказать диплом отличного качества, который не отличить от оригинала без участия специалиста высокой квалификации со сложным оборудованием.
Где приобрести диплом специалиста?
http://www.mirmafii.ru/article/7427
Успешной учебы!
minoxidil where to buy – buy minoxidil online proscar usa
перевод документов
перевод с иностранных языков
Здравствуйте!
Мы готовы предложить дипломы любой профессии по разумным тарифам.
Мы предлагаем документы ВУЗов, расположенных на территории всей России. Вы сможете купить качественный диплом за любой год, указав необходимую специальность и оценки за все дисциплины. Дипломы и аттестаты печатаются на бумаге высшего качества. Это позволяет делать государственные дипломы, не отличимые от оригиналов. Документы заверяются необходимыми печатями и подписями.
Гарантируем, что в случае проверки документов работодателями, подозрений не появится.
Где приобрести диплом специалиста?
sklad-slabov.ru/forum/user/2961/
На сайте http://waltzprof.com приобретите стальной профиль, который находится здесь в огромном ассортименте. Есть возможность заказать продукцию в любом количестве. Конструкции необходимы для того, чтобы собрать ограждающие преграды, для лофт перегородок, а также противопожарных конструкций. Все изделия выполнены из современных материалов, которым не страшны атмосферные осадки, воздействие внешних факторов. Все изделия полностью соответствуют самым высоким требованиям, выполнены по ГОСТу.
Всем привет! Может кто знает, где найти полезные блоги о недвижимости? Сейчас читаю https://cvetkrovli.ru
перевод документов
перевод с иностранных языков
娛樂城
перевод с иностранных языков
На сайте https://geo-gdz.ru/ представлены ГДЗ по географии, истории. Перед вами огромная библиотека, которая работает в режиме реального времени. Здесь вы найдете школьные учебники, контурные карты, а также атласы, которые помогут получить новые знания, освоить нужную дисциплину. Список всей важной и нужной информации находится прямо на страницах сайта. Каждый год вносятся изменения в соответствии с политическими действиями. Этот сайт предназначен специально для тех, кто не в курсе этих изменений, но стремится расширить свой уровень знаний.
Find drug details. Medication data provided.
purchase tadacip
Patient drug information. Get medicine details.
Привет, друзья!
Где приобрести диплом специалиста?
Приобрести диплом ВУЗа.
http://breget74.ru/novosti/stoimost-nefti-brent-ostaetsia-vblizi-72-wti-desheveet-chyt-slabee.html
Рады оказаться полезными!
апостиль в новосибирске
https://vk.com/peacplaycloud
купить аттестаты за 11 купить аттестаты за 11 .
платформы для инвесторов
перевод с иностранных языков
краудфандинг для малого бизнеса
план ремонта домов в москве
апостиль в новосибирске
Здравствуйте!
Приобрести диплом о высшем образовании.
Наша компания предлагает заказать диплом в отличном качестве, который невозможно отличить от оригинального документа без участия специалиста высокой квалификации с дорогостоящим оборудованием.
Где купить диплом специалиста?
http://mongolsmc.listbb.ru/posting.php?mode=post&f=1
Успехов в учебе!
перевод с иностранных языков
Came across an intriguing article – it’s worth your attention, trust me https://www.windycitygridiron.com/users/worksale555
Привет!
Мы изготавливаем дипломы психологов, юристов, экономистов и любых других профессий по доступным тарифам.
Мы можем предложить документы техникумов, которые расположены в любом регионе РФ. Вы можете заказать качественно напечатанный диплом от любого учебного заведения, за любой год, в том числе документы старого образца СССР. Документы выпускаются на бумаге высшего качества. Это дает возможность делать государственные дипломы, которые невозможно отличить от оригинала. Они заверяются необходимыми печатями и подписями.
Гарантируем, что в случае проверки документов работодателем, никаких подозрений не появится.
Где заказать диплом специалиста?
c904581v.beget.tech/2023/10/30/ogromnyy-vybor-kachestvennyh-diplomov-v-luchshem-internet-magazine.html
Medicine information provided. Access medicine information.
buy tadacip online
Detailed medication knowledge. Read about pills.
апостиль в новосибирске
апостиль в новосибирске
Всем привет! Подскажите, где почитать разные статьи о недвижимости? Сейчас читаю https://deon-stroy.ru
апостиль в новосибирске
платформы для инвестиции
сайт со стартапами для инвестиций
перевод с иностранных языков
https://aspectremont.com/
перевод с иностранных языков
апостиль в новосибирске
перевод с иностранных языков
Latest medicine developments. Access medicine information.
order tadacip
Find drug information. Find medicine information.
перевод документов
перевод с иностранных языков
апостиль в новосибирске
перевод документов
перевод с иностранных языков
перевод документов
Comprehensive pill guide. Patient pill facts.
buy tadacip pills
Medication resource available. Comprehensive pill resource.
апостиль в новосибирске
Привет, друзья!
Где приобрести диплом по нужной специальности?
Заказать диплом университета.
https://toolbarqueries.google.td/url?sa=j&source=web&rct=j&url=http://aurus-diploms.com
Всегда вам поможем!
Всем привет! Подскажите, где найти разные статьи о недвижимости? Пока нашел https://dom-vasilevo.ru
перевод с иностранных языков
Meet AI Binance trading bot
Quickstart your trading journey with AI-driven Dollar Cost
Averaging bot, designed for sustainable low-risk growth
over the long term.
btc trade
перевод с иностранных языков
перевод документов
white ninja movie film cillian murphymovie theaters kerrvilledrive in movie theater amelia ohioshaka zulu movie 1986 cast
Copy trading bots and Smart terminal
Create or copy top-performing bots with a fair
profit-sharing and automate powerful trading positions
with Smart Terminal.
btc trading bot
апостиль в новосибирске
Привет!
Заказать диплом университета.
Наша компания предлагает заказать диплом высокого качества, неотличимый от оригинала без использования специального оборудования и квалифицированного специалиста.
Где заказать диплом специалиста?
https://lubercy.ixbb.ru/viewtopic.php?id=6615#p14726
Успехов в учебе!
перевод с иностранных языков
перевод документов
Академии KRAKEN
Данный раздел посвящен образовательным проектам площадки KRAKEN. Здесь вы сможете ознакомиться с нашими сервисами, их услугами, а также различной полезной информацией. Мы предоставляем нашим пользователям не только возможность купли-продажи запрещенных веществ, мы предоставляем возможность стать частью комьюнити настоящих профессионалов, частью комьюнити — Академии KRAKEN!
Актуальные ссылки на площадку
КЛИР: (браузер+впн)
—
Kraken18att.ru
ТОР: (впн+тор)
— kraken2trfqodidvlh4aa337cpzfrhdlfldhve5nf7njhumwr7instad.onion
Kraken18at
Здравствуйте!
Мы предлагаем дипломы любой профессии по приятным тарифам.
Мы готовы предложить документы техникумов, которые расположены на территории всей РФ. Вы можете заказать диплом за любой год, указав подходящую специальность и хорошие оценки за все дисциплины. Документы печатаются на бумаге самого высокого качества. Это дает возможность делать настоящие дипломы, не отличимые от оригинала. Они будут заверены всеми обязательными печатями и штампами.
Гарантируем, что при проверке документов работодателями, никаких подозрений не появится.
Где приобрести диплом по необходимой специальности?
prikol100500.ru/kupit-diplom-vyisokoe-kachestvo-i-nadezhnost
raid carries wow https://www.kreativwerkstatt-esens.de .
перевод с иностранных языков
апостиль в новосибирске
buy rogaine for sale – where can i buy minoxidil order propecia 1mg pills
апостиль в новосибирске
апостиль в новосибирске
перевод с иностранных языков
перевод с иностранных языков
перевод документов
апостиль в новосибирске
перевод документов
перевод документов
Добрый день!
Купить диплом университета
Наши специалисты предлагают максимально быстро приобрести диплом, который выполнен на бланке ГОЗНАКа и заверен печатями, штампами, подписями. Документ способен пройти любые проверки, даже с использованием специально предназначенного оборудования. Достигайте свои цели быстро и просто с нашим сервисом.
Где купить диплом по актуальной специальности?
http://forumkoldovstva.listbb.ru/posting.php?mode=post&f=37&sid=c3ad323722f78cdc771d78f61ced5813
Поможем вам всегда!.
перевод документов
We can see that we need to develop policies to deal with this trend.
Добрый день!
Для определенных людей, заказать диплом университета – это острая необходимость, шанс получить выгодную работу. Однако для кого-то – это желание не терять массу времени на учебу в ВУЗе. С какой бы целью вам это не понадобилось, мы готовы помочь. Быстро, качественно и по доступной цене сделаем документ нового или старого образца на настоящих бланках с реальными подписями и печатями.
Наша компания предлагает выгодно и быстро купить диплом, который выполнен на бланке ГОЗНАКа и заверен печатями, водяными знаками, подписями. Документ пройдет лубую проверку, даже с применением специального оборудования. Достигайте своих целей быстро и просто с нашими дипломами.
Где приобрести диплом специалиста?
http://catalogue.bbok.ru/viewtopic.php?id=2868#p24671
Удачи!
апостиль в новосибирске
перевод документов
купить диплом о образовании недорого купить диплом о образовании недорого .
купить образование высшее diplomyx.com .
купить аттестат 9 класс купить аттестат 9 класс .
апостиль в новосибирске
перевод с иностранных языков
перевод документов
апостиль в новосибирске
Здравствуйте!
Купить диплом любого университета
Мы предлагаем быстро и выгодно заказать диплом, который выполняется на бланке ГОЗНАКа и заверен печатями, водяными знаками, подписями. Наш диплом способен пройти любые проверки, даже при использовании специальных приборов. Достигайте своих целей быстро и просто с нашим сервисом.
Где купить диплом по необходимой специальности?
http://o91707v5.beget.tech/2024/07/11/diplom-lyuboy-specialnosti-kachestvenno-i-bezopasno.html
Рады помочь!.
апостиль в новосибирске
перевод с иностранных языков
апостиль в новосибирске
Привет!
Для определенных людей, заказать диплом университета – это острая необходимость, удачный шанс получить выгодную работу. Но для кого-то – это очевидное желание не терять время на учебу в институте. С какой бы целью вам это не потребовалось, наша компания готова помочь. Быстро, качественно и по доступной цене сделаем документ нового или старого образца на подлинных бланках с реальными печатями.
Наши специалисты предлагают максимально быстро заказать диплом, который выполнен на оригинальной бумаге и заверен печатями, штампами, подписями официальных лиц. Документ пройдет лубую проверку, даже при помощи специальных приборов. Достигайте своих целей максимально быстро с нашим сервисом.
Где заказать диплом по нужной специальности?
http://video.listbb.ru/viewtopic.php?f=3&t=341
Успехов в учебе!
апостиль в новосибирске
апостиль в новосибирске
купить диплом управление персоналом asxdiplomik.com .
купить диплом республика diplomyx.com .
апостиль в новосибирске
nettruyen
NetTruyen ZZZ: Nền tảng đọc truyện tranh trực tuyến dành cho mọi lứa tuổi
NetTruyen ZZZ là nền tảng đọc truyện tranh trực tuyến miễn phí với số lượng truyện tranh lên đến hơn 30.000 đầu truyện với chất lượng hình ảnh và tốc độ tải cao. Nền tảng được xây dựng với mục tiêu mang đến cho người đọc những trải nghiệm đọc truyện tranh tốt nhất, đồng thời tạo dựng cộng đồng yêu thích truyện tranh sôi động và gắn kết với hơn 11 triệu thành viên (tính đến tháng 7 năm 2024).
NetTruyen ZZZ – Kho tàng truyện tranh phong phú:
NetTruyen ZZZ sở hữu kho tàng truyện tranh khổng lồ với hơn 30.000 đầu truyện thuộc nhiều thể loại khác nhau như:
● Manga: Những bộ truyện tranh Nhật Bản với nhiều thể loại phong phú như lãng mạn, hành động, hài hước, v.v.
● NetTruyen anime: Hàng ngàn bộ truyện tranh anime chọn lọc được đăng tải đều đặn trên NetTruyen ZZZ được chuyển thể từ phim hoạt hình Nhật Bản với nội dung hấp dẫn và hình ảnh đẹp mắt.
● Truyện manga: Hơn 10.000 bộ truyện tranh manga hay nhất được đăng tải đầy đủ trên NetTruyen ZZZ.
● Truyện manhua: Hơn 5000 bộ truyện tranh manhua được đăng tải trọn bộ đầy đủ trên NetTruyen ZZZ.
● Truyện manhwa: Những bộ truyện tranh manhwa Hàn Quốc được yêu thích nhất có đầy đủ trên NetTruyen với cốt truyện lôi cuốn và hình ảnh bắt mắt cùng với nét vẽ độc đáo và nội dung đa dạng.
● Truyện ngôn tình: Những câu chuyện tình yêu lãng mạn, ngọt ngào và đầy cảm xúc.
● Truyện trinh thám: Những câu chuyện ly kỳ, bí ẩn và đầy lôi cuốn xoay quanh các vụ án và quá trình phá án.
● Truyện tranh xuyên không: Những câu chuyện về những nhân vật du hành thời gian hoặc không gian đến một thế giới khác.
NetTruyen ZZZ không ngừng cập nhật những bộ truyện tranh mới nhất và hot nhất trên thị trường, đảm bảo mang đến cho bạn đọc những trải nghiệm đọc truyện mới mẻ và thú vị nhất.
Chất lượng hình ảnh và nội dung đỉnh cao tại NetTruyenZZZ:
Với hơn 30 triệu lượt truy cập hằng tháng, NetTruyen ZZZ luôn chú trọng vào chất lượng hình ảnh và nội dung của các bộ truyện tranh được đăng tải trên nền tảng. Hình ảnh được hiển thị sắc nét, rõ ràng, không bị mờ hay vỡ ảnh. Nội dung được dịch thuật chính xác, dễ hiểu và giữ nguyên vẹn ý nghĩa của tác phẩm gốc.
NetTruyen ZZZ hợp tác với đội ngũ dịch giả và biên tập viên chuyên nghiệp, giàu kinh nghiệm để đảm bảo chất lượng bản dịch tốt nhất. Nền tảng cũng có hệ thống kiểm duyệt nội dung nghiêm ngặt để đảm bảo nội dung lành mạnh, phù hợp với mọi lứa tuổi.
Trải nghiệm đọc truyện mượt mà, tiện lợi:
NetTruyen ZZZ được thiết kế với giao diện đẹp mắt, thân thiện với người dùng và dễ dàng sử dụng. Bạn đọc có thể đọc truyện tranh trên mọi thiết bị, từ máy tính, điện thoại thông minh đến máy tính bảng. Nền tảng cũng cung cấp nhiều tính năng tiện lợi như:
● Tìm kiếm truyện tranh theo tên, tác giả, thể loại, v.v.
● Lưu truyện tranh yêu thích để đọc sau.
● Đánh dấu trang để dễ dàng quay lại vị trí đang đọc.
● Chia sẻ truyện tranh với bạn bè.
● Tham gia bình luận và thảo luận về truyện tranh.
NetTruyen ZZZ luôn nỗ lực để mang đến cho bạn đọc những trải nghiệm đọc truyện mượt mà, tiện lợi và thú vị nhất.
Định hướng phát triển:
NetTruyen ZZZ cam kết không ngừng phát triển và hoàn thiện để trở thành nền tảng đọc truyện tranh trực tuyến tốt nhất dành cho bạn đọc tại Việt Nam. Nền tảng sẽ tiếp tục cập nhật những bộ truyện tranh mới nhất và hot nhất trên thị trường thế giới, đồng thời nâng cao chất lượng hình ảnh và nội dung. NetTruyen ZZZ cũng sẽ phát triển thêm nhiều tính năng mới để mang đến cho bạn đọc những trải nghiệm đọc truyện tốt nhất.
NetTruyen ZZZ luôn đặt lợi ích của bạn đọc lên hàng đầu. Nền tảng cam kết:
● Cung cấp kho tàng truyện tranh khổng lồ và đa dạng với chất lượng hình ảnh và nội dung đỉnh cao.
● Mang đến cho bạn đọc những trải nghiệm đọc truyện mượt mà, tiện lợi và thú vị nhất.
● Luôn lắng nghe ý kiến phản hồi của bạn đọc và không ngừng cải thiện để mang đến dịch vụ tốt nhất.
NetTruyen ZZZ hy vọng sẽ trở thành người bạn đồng hành không thể thiếu của bạn trong hành trình khám phá thế giới truyện tranh đầy màu sắc.
Kết nối với NetTruyen ZZZ ngay hôm nay để tận hưởng những trải nghiệm đọc truyện tuyệt vời.
перевод документов
перевод документов
купить диплом о среднем специальном недорого diplomasx.com .
апостиль в новосибирске
апостиль в новосибирске
перевод документов
перевод документов
перевод с иностранных языков
На сайте https://100rent.by/ каждый желающий получает возможность взять в аренду строительную технику: автомобили, а также различное вспомогательное оборудование, современную технику для выполнения определенных работ. В каталоге вы найдете и строительный инструмент, подъемники, все для бетонных работ, а также уборочное оборудование. Эта площадка является ведущей в Беларуси. А для того, чтобы отыскать оптимальное решение, воспользуйтесь поиском. При необходимости вы сможете подать объявление, если у вас есть предложение.
перевод с иностранных языков
перевод документов
перевод документов
Pill trends described. Medication guide available.
ivermectin buy uk
Overdose effects detailed. Patient medication resource.
апостиль в новосибирске
перевод с иностранных языков
Всем привет)
Будучи студентом, я наслаждался учебой до тех пор, пока не пришло время писать диплом. Но паниковать не стоило, ведь существуют компании, которые помогают с написанием и защитой диплома на отличные оценки!
Изначально я искал информацию по теме: купить диплом в миассе, купить диплом во владимире, купить диплом повара, купить диплом в туле, купить диплом в кисловодске, затем наткнулся на http://liderotrasli.ru/index.php?subaction=userinfo&user=okuwuc, где все мои учебные вопросы были решены!
Успехов в учебе!
перевод с иностранных языков
апостиль в новосибирске
перевод документов
купить диплом в кирово-чепецке diplomasx.com .
апостиль в новосибирске
Hi, its fastidious paragraph on the topic of media print, we all be familiar with media is a great source of information.
перевод с иностранных языков
Discovered an interesting article, I suggest you familiarize yourself https://fbc.net.ua/news/stati/profesijni-poslugy-z-vidnovlennya-danyh-koly-varto-zvertatysya/
перевод документов
апостиль в новосибирске
апостиль в новосибирске
перевод документов
перевод с иностранных языков
cheap leflunomide 20mg – buy alfacip generic cheap cartidin
перевод с иностранных языков
купить диплом вуза в шымкенте http://www.diploms-x.com .
Must-Watch Movies on Netflix: June 2024 Edition spirited away disney moviejerry springer show full episodesfootball movie tim mcgrawbroa the movie
перевод документов
перевод с иностранных языков
купить диплом нового образца в екатеринбурге ast-diplomas.com .
апостиль в новосибирске
cost arava 20mg – buy generic cartidin online buy cartidin without prescription
апостиль в новосибирске
Access medicine details. Medication pamphlet available.
new ed treatments
Medicine facts provided. Drug guide available.
апостиль в новосибирске
перевод с иностранных языков
перевод с иностранных языков
апостиль в новосибирске
апостиль в новосибирске
сколько стоит купить диплом техникума ast-diplomas.com .
перевод с иностранных языков
апостиль в новосибирске
перевод документов
перевод с иностранных языков
перевод документов
перевод с иностранных языков
апостиль в новосибирске
перевод документов
перевод документов
Find pill facts. Comprehensive pill resource.
purchase isotretinoin
Pill overview available. Current medicine trends.
перевод документов
перевод документов
купить диплом конкурса педагога diploms-x.com .
апостиль в новосибирске
перевод с иностранных языков
перевод документов
апостиль в новосибирске
перевод документов
перевод документов
апостиль в новосибирске
перевод с иностранных языков
перевод с иностранных языков
перевод документов
Pill effects explained. Find pill facts.
generic accutane
Drug guide provided. Interactions explained here.
перевод с иностранных языков
перевод с иностранных языков
апостиль в новосибирске
апостиль в новосибирске
Just stumble upon your blog from from time to time. nice article
перевод с иностранных языков
перевод документов
На сайте http://nemans.ru приобретите фасовочные пакеты, а также тару с ручками, мешки полипропиленовые, пленку полиэтиленовую, армированную, клейкую ленту, стрейч, различную бумажную продукцию, салфетки, тряпки и многое другое. Все товары реализуются по лучшим ценам, доступна оперативная доставка. Вся продукция от проверенных, надежных поставщиков, которые работают на результат. Все товары абсолютно безопасные, простые в использовании и помогают оперативно закончить уборку и не тратить на нее много времени. Регулярно на определенные товары устанавливаются скидки.
перевод с иностранных языков
перевод документов
апостиль в новосибирске
перевод документов
цена аттестата http://diploms-x.com/ .
апостиль в новосибирске
перевод документов
Привет!
Где купить диплом специалиста?
Мы изготавливаем дипломы любой профессии по доступным тарифам.
pmk-polymer.ru/content/kontakty
перевод с иностранных языков
перевод с иностранных языков
перевод с иностранных языков
апостиль в новосибирске
Обеспечьте конфиденциальность с резидентскими прокси, прибегнуть к этим инструментом.
В чем особенность резидентских прокси?, узнайте подробностями.
Как выбрать лучший резидентский прокси, инструкция для пользователей.
Для каких целей используют резидентские прокси?, ознакомьтесь с возможностями.
В чем преимущество безопасности резидентских прокси?, обзор функций безопасности.
Какие риски может предотвратить резидентский прокси?, рассмотрим важные аспекты.
Зачем нужны резидентские прокси и какой их выигрыш?, рассмотрим основные плюсы.
Как быстрее работать в сети с резидентским прокси?, советы для оптимизации работы.
Почему резидентский прокси стоит использовать для парсинга, анализ возможностей для парсеров.
Как обеспечить конфиденциальность в Интернете с резидентским прокси?, практические шаги к безопасности онлайн.
Как расширить свои возможности в соцсетях с резидентским прокси?, рекомендации функционала.
Зачем арендовать резидентские прокси и какие бонусы?, рассмотрим лучшие варианты.
Как избежать DDoS с резидентским прокси?, подробно изучим меры безопасности.
В чем причина популярности резидентских прокси?, подробно изучим основные факторы.
Как выбрать между резидентским и дата-центровым прокси?, рекомендации для выбора.
резидент прокси https://rezidentnieproksi.ru/ .
Latest medication updates. Drug guide here.
generic accutane
Get drug details. Pill information available.
купить диплом челгу http://diploms-x.com/ .
перевод с иностранных языков
перевод с иностранных языков
апостиль в новосибирске
перевод с иностранных языков
I like your blog. It sounds every informative.
апостиль в новосибирске
перевод документов
апостиль в новосибирске
апостиль в новосибирске
апостиль в новосибирске
апостиль в новосибирске
перевод с иностранных языков
https://karimmassimov.com/
Здравствуйте!
Задался вопросом: можно ли на самом деле купить диплом государственного образца в Москве? Был приятно удивлен — это реально и легально!
Сначала искал информацию в интернете на тему: купить диплом в глазове, купить диплом в ульяновске, купить диплом физика, купить диплом в твери, купить дипломы о высшем и получил базовые знания. В итоге остановился на материале: http://sims-game.com/index.php?subaction=userinfo&user=izotony
Успешной учебы!
перевод с иностранных языков
Drug facts provided. Drug details provided.
accutane generic
Detailed drug knowledge. Latest pill news.
Всем привет! Подскажите, где найти разные блоги о недвижимости? Пока нашел https://2204000.ru
перевод документов
апостиль в новосибирске
апостиль в новосибирске
Охраняйте свою конфиденциальность с резидентскими прокси, преимущества.
Смотрите зарубежные сериалы с резидентскими прокси, пользуйтесь контентом.
Увеличьте скорость и стабильность интернет-соединения с резидентскими прокси, в чем преимущество.
Защитите свои учетные данные и личную информацию с резидентскими прокси, и чувствуйте себя спокойно.
Прячьте свою локацию и IP-адрес с резидентскими прокси, и оставайтесь незамеченными.
Обходите цензуру и блокировки с резидентскими прокси, и не бойтесь за свою приватность.
резидентские прокси https://rezidentnie-proksi.ru/ .
перевод с иностранных языков
перевод с иностранных языков
перевод документов
перевод документов
апостиль в новосибирске
перевод документов
Всем привет! Может кто знает, где найти разные статьи о недвижимости? Сейчас читаю https://adeldv.ru
перевод документов
Brand names listed. Pill impacts described.
buy isotretinoin
Comprehensive drug resource. Find medicine information.
перевод с иностранных языков
перевод с иностранных языков
перевод документов
апостиль в новосибирске
Высокие коэффициенты на спортивные события | Надежные ставки на 1win | 1win создан для настоящих победителей | Стань частью 1win| 1win – доверие и надежность| 1win делает игру насыщенной и интересной| 1win – это стиль жизни победителя| 1win дает возможность заработать большие деньги| На 1win вы всегда находитесь в выигрыше| 1win – это надежность и качество
1win зеркало 1win зеркало .
verapamil 240mg for sale – valsartan 80mg for sale tenoretic sale
NetTruyen ZZZ: Nền tảng đọc truyện tranh trực tuyến dành cho mọi lứa tuổi
NetTruyen ZZZ là nền tảng đọc truyện tranh trực tuyến miễn phí với số lượng truyện tranh lên đến hơn 30.000 đầu truyện với chất lượng hình ảnh và tốc độ tải cao. Nền tảng được xây dựng với mục tiêu mang đến cho người đọc những trải nghiệm đọc truyện tranh tốt nhất, đồng thời tạo dựng cộng đồng yêu thích truyện tranh sôi động và gắn kết với hơn 11 triệu thành viên (tính đến tháng 7 năm 2024).
NetTruyen ZZZ – Kho tàng truyện tranh phong phú:
NetTruyen ZZZ sở hữu kho tàng truyện tranh khổng lồ với hơn 30.000 đầu truyện thuộc nhiều thể loại khác nhau như:
● Manga: Những bộ truyện tranh Nhật Bản với nhiều thể loại phong phú như lãng mạn, hành động, hài hước, v.v.
● NetTruyen anime: Hàng ngàn bộ truyện tranh anime chọn lọc được đăng tải đều đặn trên NetTruyen ZZZ được chuyển thể từ phim hoạt hình Nhật Bản với nội dung hấp dẫn và hình ảnh đẹp mắt.
● Truyện manga: Hơn 10.000 bộ truyện tranh manga hay nhất được đăng tải đầy đủ trên NetTruyen ZZZ.
● Truyện manhua: Hơn 5000 bộ truyện tranh manhua được đăng tải trọn bộ đầy đủ trên NetTruyen ZZZ.
● Truyện manhwa: Những bộ truyện tranh manhwa Hàn Quốc được yêu thích nhất có đầy đủ trên NetTruyen với cốt truyện lôi cuốn và hình ảnh bắt mắt cùng với nét vẽ độc đáo và nội dung đa dạng.
● Truyện ngôn tình: Những câu chuyện tình yêu lãng mạn, ngọt ngào và đầy cảm xúc.
● Truyện trinh thám: Những câu chuyện ly kỳ, bí ẩn và đầy lôi cuốn xoay quanh các vụ án và quá trình phá án.
● Truyện tranh xuyên không: Những câu chuyện về những nhân vật du hành thời gian hoặc không gian đến một thế giới khác.
NetTruyen ZZZ không ngừng cập nhật những bộ truyện tranh mới nhất và hot nhất trên thị trường, đảm bảo mang đến cho bạn đọc những trải nghiệm đọc truyện mới mẻ và thú vị nhất.
Chất lượng hình ảnh và nội dung đỉnh cao tại NetTruyenZZZ:
Với hơn 30 triệu lượt truy cập hằng tháng, NetTruyen ZZZ luôn chú trọng vào chất lượng hình ảnh và nội dung của các bộ truyện tranh được đăng tải trên nền tảng. Hình ảnh được hiển thị sắc nét, rõ ràng, không bị mờ hay vỡ ảnh. Nội dung được dịch thuật chính xác, dễ hiểu và giữ nguyên vẹn ý nghĩa của tác phẩm gốc.
NetTruyen ZZZ hợp tác với đội ngũ dịch giả và biên tập viên chuyên nghiệp, giàu kinh nghiệm để đảm bảo chất lượng bản dịch tốt nhất. Nền tảng cũng có hệ thống kiểm duyệt nội dung nghiêm ngặt để đảm bảo nội dung lành mạnh, phù hợp với mọi lứa tuổi.
Trải nghiệm đọc truyện mượt mà, tiện lợi:
NetTruyen ZZZ được thiết kế với giao diện đẹp mắt, thân thiện với người dùng và dễ dàng sử dụng. Bạn đọc có thể đọc truyện tranh trên mọi thiết bị, từ máy tính, điện thoại thông minh đến máy tính bảng. Nền tảng cũng cung cấp nhiều tính năng tiện lợi như:
● Tìm kiếm truyện tranh theo tên, tác giả, thể loại, v.v.
● Lưu truyện tranh yêu thích để đọc sau.
● Đánh dấu trang để dễ dàng quay lại vị trí đang đọc.
● Chia sẻ truyện tranh với bạn bè.
● Tham gia bình luận và thảo luận về truyện tranh.
NetTruyen ZZZ luôn nỗ lực để mang đến cho bạn đọc những trải nghiệm đọc truyện mượt mà, tiện lợi và thú vị nhất.
Định hướng phát triển:
NetTruyen ZZZ cam kết không ngừng phát triển và hoàn thiện để trở thành nền tảng đọc truyện tranh trực tuyến tốt nhất dành cho bạn đọc tại Việt Nam. Nền tảng sẽ tiếp tục cập nhật những bộ truyện tranh mới nhất và hot nhất trên thị trường thế giới, đồng thời nâng cao chất lượng hình ảnh và nội dung. NetTruyen ZZZ cũng sẽ phát triển thêm nhiều tính năng mới để mang đến cho bạn đọc những trải nghiệm đọc truyện tốt nhất.
NetTruyen ZZZ luôn đặt lợi ích của bạn đọc lên hàng đầu. Nền tảng cam kết:
● Cung cấp kho tàng truyện tranh khổng lồ và đa dạng với chất lượng hình ảnh và nội dung đỉnh cao.
● Mang đến cho bạn đọc những trải nghiệm đọc truyện mượt mà, tiện lợi và thú vị nhất.
● Luôn lắng nghe ý kiến phản hồi của bạn đọc và không ngừng cải thiện để mang đến dịch vụ tốt nhất.
NetTruyen ZZZ hy vọng sẽ trở thành người bạn đồng hành không thể thiếu của bạn trong hành trình khám phá thế giới truyện tranh đầy màu sắc.
Kết nối với NetTruyen ZZZ ngay hôm nay để tận hưởng những trải nghiệm đọc truyện tuyệt vời.
апостиль в новосибирске
Приветствую. Может кто знает, где почитать разные блоги о недвижимости? Пока нашел https://eniseynev.ru
Medication reactions explained. Medicine brochure provided.
purchase propecia
Access medication details. Medication essentials explained.
апостиль в новосибирске
перевод с иностранных языков
Привет!
Официальная покупка диплома вуза с сокращенной программой в Москве
dachaweek.ru/vash-put-k-uspehu-diplom-na-zakaz
Рады оказать помощь!.
апостиль в новосибирске
перевод с иностранных языков
Всем привет! Подскажите, где почитать полезные блоги о недвижимости? Пока нашел https://fuseitdecore.ru
апостиль в новосибирске
1win – ваш идеальный партнер для ставок
Выигрывайте с 1win без усилий
Завоюйте свою удачу вместе с 1win
1win – надежный партнер для всех любителей ставок
Букмекерская контора 1win радует своих клиентов каждый день
Ваши ставки всегда успешные с 1win
1win – ваш ключ к миру ставок и азарта
1win гарантирует вам только лучшие условия для ставок
1win – ваш верный путь к финансовой независимости
1win – это бесконечные возможности для выигрышей
Ставки на спорт никогда не были такими увлекательными как с 1win
Присоединяйтесь к миллионам победителей на платформе 1win
1win: надежность и качество для вас
Начните свой путь к успеху с 1win|Получайте удовольствие от ставок с 1win
Ставки на спорт без ограничений с 1win|1win – ваш уникальный шанс стать настоящим победителем|1win делает вашу игру интересной и прибыльной|1win – ваш проводник в мире ставок и азарта|Играйте и выигрывайте с 1win|1win делает вашу игру максимально увлекательной и выгодной|1win – ваш путь к успеху и богатству|1win – это ваш лучший друг в мире ставок|1win делает вашу игру более прибыльной и интересной|1win гарантирует вам только успешные ставки|1win – это ваш ключ к финансовой независимости|Увеличивайте свои шансы на успех с 1win|1win – это ваш ключ к финансовой стабильности|1win радует своих клиентов только лучшими условиями|1win – ваш верный партнер в мире ставок|Начните свой путь к успеху с 1win|1win – это ваш путь к большим выигрышам|Ув
1win зеркало 1win зеркало .
апостиль в новосибирске
апостиль в новосибирске
апостиль в новосибирске
Medicine guide here. Medicine essentials explained.
purchase propecia
Get drug details. Access medicine information.
перевод с иностранных языков
перевод с иностранных языков
апостиль в новосибирске
подъем дома
замена венцов
Приветствую. Может кто знает, где найти разные блоги о недвижимости? Сейчас читаю https://galastroy-sk.ru
Ставки на спорт в 1win: высокие коэффициенты и большие выигрыши, перейти.
Играйте и выигрывайте вместе с 1win, попробовать свою удачу.
Зарабатывайте вместе с 1win и наслаждайтесь выигрышами, начать играть.
1win – ваш партнер в мире киберспорта, испытать победу.
Играйте безопасно и выигрывайте большие деньги с 1win, начать играть.
1win вход https://1win-sayt.by/ .
Find pill info. Medication effects explained.
buy propecia uk
Get medication facts. Get drug details.
Стоимость дипломов высшего и среднего образования и как избежать подделок
ya.webtalk.ru/viewtopic.php?id=9651#p47259
ремонт фундамента
подъем дома
замена венцов
подъем дома
ремонт фундамента
verapamil 240mg brand – diovan 160mg uk generic tenoretic
подъем дома
ремонт фундамента
Всем привет! Подскажите, где почитать полезные блоги о недвижимости? Сейчас читаю https://ggs45.ru
подъем дома
замена венцов
atenolol cost – tenormin over the counter carvedilol 6.25mg pills
подъем дома
замена венцов
Discovered an article that might interest you Ц don’t miss it! https://www.barkingcarnival.com/users/worksale555
ремонт фундамента
замена венцов
подъем дома
Medicine effects explained. Patient medication resource.
buy propecia no rx
Latest medicine developments. Pill leaflet here.
100RENT.BY – ведущая онлайн-платформа для аренды строительной и специальной техники, оборудования в разных регионах Беларуси. Наша главная цель – сделать взаимодействие между арендаторами и арендодателями в строительной сфере более эффективным. Ищете аренда газонокосилки минск? 100rent.by – сайт, где представлена детальная информация о нас, ознакомиться с ней можете прямо сейчас. Мы создали новейший и простой интерфейс для удобства публикования и поиска объявлений. Предлагаем гибкие тарифы и гарантируем быструю регистрацию. Всегда вам рады!
ремонт фундамента
Stumbled upon interesting material – I can’t help but recommend you to read https://www.bigblueview.com/users/worksale555
tenormin us – order betapace 40mg pills buy coreg medication
замена венцов
На сайте https://xn--80aa1agibdda2ab.xn--p1ai/ можно приобрести насосное оборудование, автоматику, средства управления, трубопроводную арматуру. Ознакомьтесь со всеми самыми выгодными предложениями прямо сейчас, в том числе, и хитами продаж. Именно они пользуются особым спросом среди покупателей. На всю продукцию установлены привлекательные расценки, зачастую действуют акции, которые делают приобретение более выгодным. Все товары от лучших производителей, положительно себя зарекомендовавших.
ремонт фундамента
подъем дома
ремонт фундамента
ремонт фундамента
Всем привет! Может кто знает, где почитать разные блоги о недвижимости? Пока нашел https://glwin.ru
На сайте https://ufa2.body-pit.ru/ приобретите качественное, сертифицированное спортивное питание, которое позволит заполучить красивое тело мечты, привлекательный рельеф или значительно похудеть. В этом интернет-магазине вы найдете витамины, гейнеры, сжигатели жира, аминокислоты, предтренировочные комплексы, антиоксиданты. Вся продукция сертифицированная, высокого качества, представлена именитыми брендами. Важным моментом является то, что доставка заказа осуществляется в тот день, когда оформили покупку.
замена венцов
ремонт фундамента
купить бланк диплома о среднем asxdiplomik.com/kupit-diplom-moskva .
замена венцов
СамГруз – компания, которую многие рекомендуют. Наши услуги: перевозка строительного материала, доставка мебели и оргтехники из магазина, вывоз строительного мусора и хлама на газели. У нас работают водители с опытом. Грузчики аккуратные. Гарантируем вам разумные цены и оперативную подачу грузового автомобиля. https://gruz63.ru – сайт, где можете подробнее ознакомиться с нашими услугами и посмотреть контактную информацию. СамГруз – быстро, недорого, качественно. Можете лично в этом удостовериться. Мы не подведем вас!
ремонт фундамента
Каждый день бот https://t.me/sychev_sergei_bot предлагает вам варианты развития тела и души, отдыха и познания чего-то нового. Следуйте подсказкам календаря – увеличивайте шансы на успех в своей жизни и обретайте внутреннюю гармонию. Рекомендации рассчитываются индивидуально (по дате рождения) на основе знаний древней китайской метафизики и адаптирован под запросы современной жизни.
На сайте https://campus815.ru забронируйте путевку на детские языковые смены. Если у вас трое детей, то такая возможность предоставляется вам абсолютно бесплатно. Если нужно бронирование на двое детей, то в этом случае получаете скидку в 50%. А на супер ранее бронирование дается скидка в 25%. На сайте вы сможете ознакомиться с информацией о том, когда запланированы ближайшие смены. Для того чтобы сориентироваться в обучении и принять правильное решение, необходимо ознакомиться с фото. Подберите смену прямо сейчас.
куплю диплом ссср asxdiplomik.com/kupit-diplom-moskva .
ремонт фундамента
подъем дома
замена венцов
подъем дома
замена венцов
На сайте https://sochi.calypso.ooo/ у вас получится быстро отыскать и забронировать яхту, катер либо парусники. Компания насчитывает 20 филиалов, обслуживает более полутора тысяч клиентов в год. Все судна исправные, отличаются привлекательным, стильным дизайном. При этом заказать можно в любое, наиболее комфортное время и на несколько часов. Все ограничивается лишь вашими пожеланиями, предпочтениями. Этот сервис поможет вам подобрать наиболее подходящий вариант на прогулку, романтическое свидание или празднование торжества.
купить диплом о высшем образовании с занесением в реестр в ульяновске asxdiplomik.com/kupit-diplom-moskva .
ремонт фундамента
Медиагет – популярный торрент-клиент для скачивания файлов. Программа имеет простой интерфейс и поддерживает множество форматов. Подробнее о возможностях Медиагет можно узнать на сайте https://skachat-mediaget-fast.ru.
ремонт фундамента
Скачать музыку https://kissvk.top/ очень просто! Зайдите на сайт где вы найдете самые свежие композиции, музыку, альбомы, треки. Новинки 2024 и лучшая музыка за все годы, которую можно качать в mp3 абсолютно бесплатно и без регистрации. Самый большой сборник музыки в интернете для скачивания у нас на сайте.
laptops, tablets, and smartphones. This flexibility allows players to enjoy the game on their preferred device,
demo aviator game
На сайте https://somovo-mebel.ru/catalog/gostinnye/ вы сможете приобрести функциональные, качественные гостиные, которые разработаны с особой заботой о покупателях и их комфорте. И самое важное, что соблюдаются все технологические процессы, внимание уделяется каждой детали. Предлагаются такие гостиные, которые полностью отвечают запросам и требованиям самого притязательного покупателя. Все гостиные выполнены из современных, высококачественных материалов, за счет чего мебель прослужит очень долго. Гостиные выполнены в самом разном стиле.
ремонт фундамента
Приветствую. Может кто знает, где почитать разные статьи о недвижимости? Пока нашел https://gor-bur.ru
подъем дома
}
ремонт фундамента
замена венцов
замена венцов
замена венцов
Find drug details. Complete medicine overview.
where buy propecia
Comprehensive medicine facts. Access medication details.
замена венцов
futurama season 8 release date lord of the rings movie releasewhat happened to julia from hell’s kitchen season 3does family guy still make new episodesgaturro: the movie
ремонт фундамента
dynamic features, and social elements, it offers an engaging experience for players. The game is supported by
aviator game online
замена венцов
Здравствуйте!
Мы предлагаем документы техникумов, расположенных в любом регионе России. Вы можете заказать диплом за любой год, указав подходящую специальность и оценки за все дисциплины. Дипломы и аттестаты делаются на “правильной” бумаге высшего качества. Это позволяет делать настоящие дипломы, которые невозможно отличить от оригинала. Документы заверяются всеми обязательными печатями и штампами.
Заказать диплом любого университета.
doomelang.com/read-blog/6800
Успешной учебы!
ремонт фундамента
ремонт фундамента
Здравствуйте!
Мы изготавливаем дипломы любой профессии по приятным ценам. Цена зависит от выбранной специальности, года получения и образовательного учреждения.
Где приобрести диплом специалиста?
Заказать диплом университета
arusak-diploms-srednee.ru/kupit-attestat-za-11-klass
Хорошей учебы!
замена венцов
замена венцов
Привет!
Мы изготавливаем дипломы любых профессий по доступным ценам. Цена будет зависеть от выбранной специальности, года выпуска и образовательного учреждения.
Где приобрести диплом по актуальной специальности?
Приобрести диплом любого ВУЗа
arusak-diploms-srednee.ru
Успешной учебы!
Привет!
Купить документ о получении высшего образования можно у нас в столице.
ast-diplom24.ru/kupit-diplom-sankt-peterburg
Хорошей учебы!
Get pill facts. Medication details here.
buy lioresal online
Comprehensive drug guide. Patient medication guide.
Your System – ваш надежный партнер в области оборудования для видеонаблюдения. Предоставляем большой выбор качественной продукции. Работаем исключительно с достойными производителями. Стремимся обеспечить клиентам высокий уровень обслуживания и персональный подход. Ищете системы видеонаблюдения купить? Y-ss.ru – сайт, где можно купить охранные системы по лояльным ценам. Доставим ваш заказ в любую точку России. Для вас работаем без выходных. Как процесс покупок сделать простым, с удовольствием расскажем. Свяжитесь с нами любым способом.
Всем привет! Может кто знает, где найти разные статьи о недвижимости? Сейчас читаю https://hameleon1.ru
подъем дома
ремонт фундамента
Привет!
Заказать документ о получении высшего образования вы имеете возможность в нашей компании.
ast-diplomy.com/otzyvy
Успешной учебы!
замена венцов
plane ascends, the higher the multiplier. For example, if you bet $10 and cash out at a 2x multiplier, you win
aviator play game
подъем дома
ремонт фундамента
Здравствуйте!
Возможно ли купить диплом стоматолога, и как это происходит
http://www.as7abe.com/wall/blogs/post/new
Рады помочь!.
замена венцов
замена венцов
Добрый день!
Как оказалось, купить диплом кандидата наук не так уж и сложно
drochan.listbb.ru/viewtopic.php?f=4&t=427
Будем рады вам помочь!.
Привет, друзья!
Купить документ университета вы сможете в нашей компании в столице.
ast-diplom.com/otzyvy
Хорошей учебы!
Привет, друзья!
Где заказать диплом специалиста?
Мы предлагаем быстро заказать диплом, который выполняется на бланке ГОЗНАКа и заверен мокрыми печатями, водяными знаками, подписями. Диплом пройдет любые проверки, даже при использовании специального оборудования. Решите свои задачи быстро с нашей компанией.
Приобрести диплом о высшем образовании.
http://www.rugladyseminars.com/cb-profile/pluginclass/cbblogs?action=blogs&func=show&id=409
ремонт фундамента
На сайте https://east-usa.com/index.html ознакомьтесь с подробной, актуальной информацией, которая касается карты Соединенных Штатов Америки. Только здесь представлена самая полная информация, которая вам обязательно пригодится для того, чтобы расширить кругозор. Перед вами подробная карта всех автомобильных дорог. Указаны и наиболее популярные достопримечательности, которые обязательно вас заинтересуют. Карта сгруппирована по следующим регионам: Средний Запад, Запад США, Юг США, Северо-восток.
замена венцов
купить диплом о высшем цена купить диплом о высшем цена .
диплом о высшем купить ast-diploms.com .
замена венцов
ремонт фундамента
подъем дома
Приветствую. Подскажите, где найти разные блоги о недвижимости? Пока нашел https://iskrb.ru
Features and Benefits
aviator app
ремонт фундамента
ремонт фундамента
Процесс получения диплома стоматолога: реально ли это сделать быстро?
diploms-x24.ru/kupit-diplom-omsk
замена венцов
Pill trends described. Drug facts provided.
purchase baclofen
Current medication trends. Drug leaflet available.
рюкзак школьный черный купить
купить диплом о среднем образование цена ast-diploms.com .
Are There Any Costs Involved?
aviator play game
Здравствуйте!
Где купить диплом специалиста?
Наша компания предлагает выгодно и быстро купить диплом, который выполняется на оригинальной бумаге и заверен мокрыми печатями, водяными знаками, подписями. Документ способен пройти лубую проверку, даже с применением специального оборудования. Достигайте цели максимально быстро с нашими дипломами.
Купить диплом университета.
ourownnetwork.mn.co/posts/61838009
Приветствую. Подскажите, где найти полезные блоги о недвижимости? Пока нашел https://juzhnybereg24.ru
На сайте https://podolog66.ru/ вы сможете записаться на прием к подологу. Среди основных услуг выделяют: избавление от стержневой мозоли, лечение трещин стопы, грибка ногтей на ногах, удаление вросшего ногтя. Медики помогут восстановить детские ногти, удалят бородавки. Все манипуляции являются полностью безболезненными, выполняются с использованием уникальных технологий, высококачественных средств. Уже сразу пациент чувствует существенное облегчение. Вы можете записаться на консультацию или процедуру в наиболее комфортное для себя время.
Лучшие казино
Привет!
Мы можем предложить документы техникумов, которые находятся в любом регионе РФ. Можно купить диплом от любого заведения, за любой год, в том числе документы старого образца СССР. Дипломы и аттестаты выпускаются на “правильной” бумаге самого высшего качества. Это позволяет делать государственные дипломы, которые не отличить от оригиналов. Они заверяются необходимыми печатями и подписями.
umorforme.ru/prodazha-diplomov-lyubogo-uchebnogo-zavedeniya-rossii
Pill impacts described. Drug facts provided.
purchase baclofen online no prescription
Patient medicine resource. Comprehensive pill overview.
Здравствуйте!
Купить диплом любого университета.
lifethelife.com/read-blog/292
Many online platforms host competitive tournaments and events for the Aviator Game. These events offer players
aviator demo
http://nimbustech.co.kr/board/bbs/board.php?bo_table=free&wr_id=1169076
купить диплом кондитера http://www.diploms-x.com .
Приветствую. Подскажите, где почитать полезные статьи о недвижимости? Сейчас читаю https://klimat-hck.ru
Привет, друзья!
Приобретение диплома ПТУ с сокращенной программой обучения в Москве
sklad-slabov.ru/forum/user/7793/
Окажем помощь!.
https://site547576904.fo.team/
дипломы купить о среднем образовании дипломы купить о среднем образовании .
Добрый день!
Купить диплом о высшем образовании.
antoinegriezmannclub.com/read-blog/2400
где купить диплом форум где купить диплом форум .
Can I Play the Aviator Game on Mobile?
aviator play game
Привет, друзья!
Наша компания предлагает быстро и выгодно приобрести диплом, который выполнен на оригинальной бумаге и заверен мокрыми печатями, штампами, подписями официальных лиц. Документ способен пройти лубую проверку, даже при использовании профессиональных приборов. Достигайте свои цели быстро и просто с нашим сервисом.
led119.ru/forum/user/107400/
Успешной учебы!
Добрый день!
Где купить диплом по нужной специальности?
ractis.ru/forums/index.php?autocom=gallery&req=si&img=2536
Хорошей учебы!
Привет!
Купить документ института вы сможете в нашей компании.
ast-diplom.com/kupit-diplom-voronezh
Успешной учебы!
Ремстройсервис – надежная компания. Ее успех обусловлен высоким качеством выполнения работ, соответствием современным требованиям в планировке, отделке, выборе экологически чистых материалов. Созданы специальные программы, чтобы было несложно купить собственное жилье по лояльным ценам. https://rss48.ru – сайт, где вы найдете больше информации о нас, ознакомиться с ней можете прямо сейчас. При возникновении каких-либо вопросов, смело обращайтесь к нам. Мы с удовольствием вас проконсультируем. Живите по-новому вместе с Ремстройсервис!
диплом высшее образование диплом высшее образование .
Агентство интернет-маркетинга полного цикла «SeoУслуга» Мы поможем вам не только с продвижением сайта, но и созданием проектов под ключ: от больших интернет-магазинов до корпоративных сайтов, визиток и landing page. СеоУслуга – ваш надежный партнер – https://seousluga.ru/
Здравствуйте!
Купить документ о получении высшего образования можно у нас в Москве.
diploms-x.com/kupit-diplom-omsk
Удачи!
Pill leaflet provided. Complete drug overview.
buy baclofen no rx
Find medicine info. Medicine impacts described.
Добрый день!
Заказать документ о получении высшего образования вы сможете в нашем сервисе.
ast-diplom.com/kupit-diplom-nizhnij-novgorod
На сайте https://speakerpub.ru получите возможность забронировать столик в популярном пабе с изысканным интерьером для того, чтобы весело, необычно и интересно провести время вместе со своими друзьями, второй половинкой. Здесь подают бизнес-ланчи, вкусное и ароматное пиво, организуют различные развлечения, спортивные трансляции, которые точно никого не оставят равнодушным. Дополнительно вас порадует и привлекательный интерьер, который выглядит стильно. Перед вами огромный ассортимент бифштексов, оригинальных закусок и многого другого.
Центр Тех Профи в Перми предлагает качественный ремонт роботов-пылесосов с гарантией до 6 месяцев. Наши мастера с многолетним опытом работы выполнят ремонт в кратчайшие сроки, используя оригинальные запчасти. Доступны услуги выездного ремонта и доставки техники курьером, а также бесплатная диагностика.
Приветствую. Может кто знает, где почитать полезные блоги о недвижимости? Пока нашел https://kolahouse.ru
Привет, друзья!
Приобрести документ о получении высшего образования можно у нас в Москве.
ast-diplomas.com/kupit-diplom-nizhnij-novgorod
Здравствуйте!
Купить диплом ВУЗа.
sfpdsa.listbb.ru/viewtopic.php?f=2&t=370
Успехов в учебе!
На сайте http://eoknadveri.ru закажите звонок для того, чтобы приобрести пластиковые окна от производителя. Конструкции создаются из алюминия, ПВХ. На все предоставляется гарантия – 20 лет, ведь сотрудники предприятия уверены в своей работе. Отсутствует торговая надбавка. Доставка, замер, монтажные работы – все это выполняется тогда, когда удобно именно вам. При необходимости вы сможете воспользоваться бесплатной консультацией. Компания выполняет остекление балконов, квартир, фасадов, коттеджей.
Software Requirements
aviator game demo
Porn movies free
Добрый день!
Официальная покупка школьного аттестата с упрощенным обучением в Москве
biketrials.ru/live/blog.php?b=9128
Окажем помощь!.
Добрый день!
Мы изготавливаем дипломы любой профессии по выгодным ценам. Цена будет зависеть от выбранной специальности, года выпуска и образовательного учреждения.
landik-diploms-srednee.ru/kupit-diplom-v-novosibirske
Удачи!
Добрый день!
Где купить диплом специалиста?
Мы готовы предложить документы ВУЗов, которые расположены на территории всей РФ. Можно приобрести качественный диплом от любого заведения, за любой год, указав актуальную специальность и хорошие оценки за все дисциплины. Дипломы печатаются на “правильной” бумаге самого высшего качества. Это позволяет делать государственные дипломы, которые невозможно отличить от оригиналов. Документы заверяются всеми необходимыми печатями и подписями.
Мы изготавливаем дипломы любой профессии по выгодным ценам.
diplomyx.com/kupit-diplom-ekaterinbur
Всегда вам поможем!
game play movie movie robin hood with kevin costnerwhen does rifle season start in vermontmovie sherlock holmes sisterwill there be a season 2 of the way home
Привет!
Купить диплом о высшем образовании.
Мы можем предложить документы техникумов, которые расположены на территории всей России. Вы можете приобрести качественно сделанный диплом за любой год, в том числе документы СССР. Дипломы и аттестаты выпускаются на “правильной” бумаге самого высокого качества. Это дает возможности делать настоящие дипломы, не отличимые от оригиналов. Документы будут заверены всеми требуемыми печатями и штампами.
octomo.co.uk/read-blog/949
Привет, друзья!
Приобретение диплома ВУЗа с сокращенной программой обучения в Москве
webnewsrealty.ru/kupite-diplom-i-zabudte-o-studencheskih-dolgih-nochah
Рады помочь!.
Всем привет! Может кто знает, где почитать полезные статьи о недвижимости? Пока нашел https://komdizrem.ru
Здравствуйте!
Мы готовы предложить дипломы любой профессии по приятным ценам. Стоимость может зависеть от выбранной специальности, года получения и университета.
landik-diploms-srednee.ru/svidetelstvo-o-razvode
Хорошей учебы!
Drug facts provided. Read about medicines.
buy baclofen with no prescription
Patient medication facts. Medication overview available.
Желаете продать свое авто быстро и по достойной цене? У нас трудятся грамотные специалисты, которые обладают приличным опытом в области продаж. Предложим оценку вашего авто абсолютно бесплатно. Теперь не надо на утомительные поиски покупателя тратить время. Мы берем на себя все организационные вопросы. Ищете выкуп автомобиля сразу в казани сайт? Cars16.ru – сайт, где вы сможете более подробную информацию отыскать. Дорожим нашими клиентами и подбираем особый подход. Расчет совершаем удобным способом. Гарантируем прозрачные сделки. Свяжитесь с нами, чтобы обсудить детали. С удовольствием вам поможем!
Online Platforms Offering the Game
aviator app
Discovered a unique article – recommended to acquaint yourself! https://www.behance.net/gallery/203467553/Exclusive-Riga-Escort-Services
купить диплом о высшем образовании в новосибирске https://diploms-x.com .
Добрый день!
Где заказать диплом по актуальной специальности?
Заказать диплом о высшем образовании.
stroimarket-komi.ru/club/user/54/blog/38295/
Добрый день!
Мы предлагаем купить диплом в высоком качестве, который невозможно отличить от оригинального документа без использования дорогостоящего оборудования и квалифицированного специалиста.
http://www.mkbox.ru/communication/forum/user/73714/
Удачи!
Привет!
Купить диплом ВУЗа
lighttur.ru/ofitsialnyie-diplomyi-podlinnost-i-nadezhnost
Всем привет! Подскажите, где почитать разные блоги о недвижимости? Сейчас читаю https://konditsioneri-shop.ru
The Aviator Game is a thrilling online casino game that combines chance and strategy. With its unique gameplay,
play aviator demo game
Comprehensive medication overview. Drug facts provided.
cost of cheap clarithromycin pills
Latest drug news. Overdose effects detailed.
как купить диплом diplomyx.com .
While the game itself is free to access, playing involves placing bets with real money. Some platforms may offer
aviator play game
Приветствую. Подскажите, где найти полезные блоги о недвижимости? Пока нашел https://glatt-nsk.ru
На сайте https://oknatitan.ru/ закажите звонок для того, чтобы приобрести деревянные, пластиковые, алюминиевые окна, а также стеклопакеты. Можно приобрести окна в коттедж, которые идеально впишутся в общую концепцию, защитят от мороза, промозглого ветра, сквозняков. Прямо сейчас вы сможете воспользоваться скидкой в 47%. При необходимости специалисты специально для вас подберут наиболее оптимальный вариант материала, чтобы результат превзошел ожидания. На сайте ознакомьтесь с техническими характеристиками каждого материала, чтобы подобрать достойный вариант.
Здравствуйте!
Наша компания предлагает купить диплом в высоком качестве, неотличимый от оригинального документа без использования специального оборудования и опытного специалиста.
“i636356o.bget.ru/index.php?action=profile;u=319124”
Удачи!
Здравствуйте!
Заказать документ университета можно у нас.
diplomyx24.ru/kupit-diplom-moskva
Удачи!
ремонт фундамента
Patient medication resource. Abuse effects detailed.
buy biaxin no prescription
Latest medication updates. Drug pamphlet provided.
подъем дома
ремонт фундамента
Привет, друзья!
Заказать документ института можно у нас в столице.
diplomyx.com/kupit-diplom-o-srednem-obrazovanii
Успешной учебы!
ремонт фундамента
На сайте https://t.me/bet_vodka получите нужную информацию, которая касается популярной и надежной БК «Водка Бет». Это зеркало официального сайта, а потому здесь находится вся содержательная, актуальная и честная информация, свежие промокоды. Вы самым первым узнаете о предстоящих акциях, любопытных событиях. Для того чтобы узнать все, что нужно, просто пройдите регистрацию. А затем необходимо ввести промокод, который действует определенный интервал времени. Информация обновляется постоянно, чтобы вы первым узнали обо всем.
ремонт фундамента
рюкзак школьный черный купить
рюкзак школьный черный купить
Name], each offering unique bonuses and promotions for Aviator Game players.
aviator game online
рюкзак школьный черный купить
купить диплом высшее окончание asxdiplomik.com .
рюкзак школьный черный купить
рюкзак школьный черный купить
рюкзак школьный черный купить
best porn
рюкзак школьный черный купить
рюкзак школьный черный купить
Medication guide available. Get information instantly.
buying clarithromycin online
Medicine leaflet here. Medication impacts explained.
Вид-Строй [url=http://www.internet-magazin-strojmaterialov.ru]http://www.internet-magazin-strojmaterialov.ru[/url] .
рюкзак школьный черный купить
рюкзак школьный черный купить
I also got to function on really impactful scalable hiiring
initiatives across the business.
Here is my web site … ezalba.com
game was designed to provide an adrenaline-pumping experience that mimics the thrill of gambling with a twist.
aviator play game
рюкзак школьный черный купить
рюкзак школьный черный купить
рюкзак школьный черный купить
рюкзак школьный черный купить
i-tec.ru https://multimedijnyj-integrator.ru/ .
рюкзак школьный черный купить
Вас интересует прокат инвалидных колясок? Деливери плей предоставляет такую возможность. Гарантируем доступные цены и быструю доставку. У нас всегда чистые коляски. Вы сможете оплатить заказ только после того, как убедитесь, что коляска полностью соответствует вашим требованиям и находится в отличном состоянии. Ищите Прокат Инвалидных колясок? Deliveryplay.ru/arenda-invalidnyh-kolyasok – сайт, где можно коляску арендовать. Также здесь вы узнаете, почему аренда лучше покупки. Обращайтесь к нам, поможем выбрать коляску, которая идеально вам подойдет.
balforum.net
рюкзак школьный черный купить
Привет!
Вопросы и ответы: можно ли быстро купить диплом старого образца?
landik-diploms-srednee.ru/kupit-diplom-v-ekaterinburge
Удачи!
Привет, друзья!
Мы можем предложить документы ВУЗов, которые находятся в любом регионе Российской Федерации. Вы можете заказать качественный диплом от любого заведения, за любой год, в том числе документы старого образца СССР. Дипломы и аттестаты печатаются на бумаге самого высшего качества. Это дает возможность делать государственные дипломы, не отличимые от оригиналов. Они будут заверены необходимыми печатями и подписями.
geoamor.com/read-blog/30681
aparthome.org
рюкзак школьный черный купить
improved mobile compatibility. Developers continually use this feedback to enhance the game and provide a better
play plinko game
рюкзак школьный черный купить
Здравствуйте!
Всё, что нужно знать о покупке аттестата о среднем образовании
molbiol.ru/forums/index.php?showtopic=1235739
Рады помочь!.
рюкзак школьный черный купить
На сайте https://novagard.ru/ закажите звонок для того, чтобы узнать всю необходимую информацию о производстве и установке практичных и качественных заборов, которые ставятся под ключ и в столице. В этой компании на высоком уровне и качественно создают навесы, ворота, оказывают различные дополнительные услуги. Ознакомиться с ценами вы сможете непосредственно на сайте. Вся продукция создается из качественных, надежных и высокотехнологичных материалов, которые не утратят вида долгое время. Для того чтобы иметь представление о качестве работ, изучите портфолио.
Pill facts here. Medicine overview available.
where to get generic clarithromycin without insurance
Access pill details. Medication information here.
рюкзак школьный черный купить
рюкзак школьный черный купить
рюкзак школьный черный купить
cheap atorvastatin pills – cheap atorvastatin bystolic 20mg for sale
рюкзак школьный черный купить
рюкзак школьный черный купить
Привет!
Официальная покупка диплома вуза с сокращенной программой в Москве
arsenal.listbb.ru/viewtopic.php?f=14&t=472
Рады помочь!.
рюкзак школьный черный купить
Encountered a captivating article, I propose you read Техосмотр СПб Пункты техосмотра
На сайте https://santeh.club вы сможете приобрести качественные, надежные унитазы, ванны, а также полотенцесушители, инсталляции, смесители и многое другое от лучших производителей, которые предлагают исключительно качественную продукцию для помещений различного дизайна и площади. Предоставляется дополнительная гарантия качества, которая выдается производителем. Перед вами огромный выбор интересных новинок, которые появляются регулярно. Возможна услуга самовывоза. Доставка покупок по всем регионам.
рюкзак школьный черный купить
100RENT.BY – популярная онлайн-платформа для аренды специальной и строительной техники, оборудования в различных регионах Беларуси. Наша главная цель – сделать взаимодействие между арендаторами и арендодателями в строительной сфере более эффективным. Ищете мини экскаватор аренда? 100rent.by – сайт, где представлена детальная информация о нас, ознакомиться с ней можете прямо сейчас. Мы создали новейший и простой интерфейс для удобства публикования и поиска объявлений. Предлагаем гибкие тарифы и гарантируем быструю регистрацию. Всегда рады вам!
рюкзак школьный черный купить
purchase atorvastatin generic – atorlip tablets buy nebivolol 20mg pill
рюкзак школьный черный купить
vacation movie tom selleck and gene simmons moviefairly oddparents superhero episodesnl 40th anniversary full episodeheartland season 3 episode 4
На сайте https://logisticbda.com оставьте заявку для того, чтобы вам рассчитали стоимость такой услуги, как заказ продукции для маркетплейсов и непосредственно из Китая. Сотрудники выполняют такие важные работы, как: выкуп, поиск, транспортировка из Китая. Специально для вас отгрузка, упаковка на маркетплейсы. Сотрудники окажут помощь в формировании бизнеса на различных маркетплейсах. Закупка происходит с самых проверенных, надежных магазинов, которым точно можно доверять. Проводятся различные складские работы, дополнительные услуги.
рюкзак школьный черный купить
enjoyable.
play plinko game
На сайте https://vips13un.kinoportal.live/ подберите интересный, увлекательный фильм, который подходит для домашнего совместного просмотра, а также в выходной день. Также находятся и любопытные передачи, которые смотрят многие. Вы обязательно найдете то, что полностью соответствует вашим предпочтениям, вкусам. Все кино, передачи представлены в отличном качестве и с хорошим звуком, поэтому просмотр принесет лишь приятные эмоции. Регулярно появляются многообещающие новинки, которые тоже заслуживают вашего внимания.
Reliability. Concluding an agreement allows sveto-copy.com you to avoid unpleasant situations and obtain a guarantee of high-quality work.
Ищите Скачать музыку https://vkmusic.in/ – тогда зайдите на сайт и насладитесь шикарным выбором альбомов, треков, всех самых свежих хитов которые вы можете качать в любом количестве в мп3 на сайте. Лучшая подборка в машину, для отдыха, релакса. Вся музыка у нас.
рюкзак школьный черный купить
If you think through poiskmonet.com every detail, you can achieve effective results.
рюкзак школьный черный купить
рюкзак школьный черный купить
На сайте https://rss48.ru/ ознакомьтесь с новостройками города Липецка. Приобрести квартиру мечты в благоустроенном районе вы сможете прямо сейчас и непосредственно от застройщика. Если вся сумма у вас не накоплена, то совершить покупку можно и в рассрочку. В каталоге вы отыщите таунхаусы, квартиры с ремонтом, а также комфортные виллы. В каждом районе развитая инфраструктура, есть своя сервисная компания, а также продуманные европланировки и многое другое для лучшего проживания. В каждой квартире индивидуальное отопление.
рюкзак школьный черный купить
Get details now. Misuse consequences detailed.
buy biaxin cheap
Access medication facts. Drug facts provided.
рюкзак школьный черный купить
Добрый день!
Приобрести документ института можно в нашей компании в Москве.
asxdiplomik24.ru/kupit-diplom-sankt-peterburg
рюкзак школьный черный купить
рюкзак школьный черный купить
На сайте https://penza-evakuator.ru/ закажите звонок для того, чтобы воспользоваться услугами эвакуатора: грузового, легкового. Для того чтобы заказать услугу, необходимо позвонить по обозначенному номеру. Возможна любая форма оплаты, а стоимость начинается от 2 500 рублей. Подача транспорта организуется в течение получаса. Работа в круглосуточном режиме, отсутствуют выходные. Организуется эвакуация мототехники, квадроциклов, малогабаритных, легковых автомобилей, спортивных машин, джипов, внедорожников.
Привет, друзья!
Заказать документ о получении высшего образования можно у нас в Москве.
ast-diplomas.com/kupit-diplom-rostov-na-donu
У нас есть подробное описание цены на ритуальные принадлежности в Алматы. Ознакомьтесь с нашим постом, чтобы узнать больше о стоимости различных принадлежностей и найти наиболее выгодные предложения на рынке.
рюкзак школьный черный купить
Привет, друзья!
Как избежать рисков при покупке диплома колледжа или ВУЗа в России.
Заказать диплом любого ВУЗа.
network-1062788.mn.co/posts/61828980
рюкзак школьный черный купить
производители лифтового оборудования
рюкзак школьный черный купить
На сайте https://pro100-stone.ru закажите звонок для того, чтобы купить изделия, выполненные из ненатурального камня. В этой компании занимаются разработкой, производством подоконников, столешниц, раковин, моек, а также барных стоек и многого другого. Материал обладает поистине безграничными возможностями, что позволяет создавать удивительные шедевры как для коммерческих объектов, так и для дома. Создаются конструкции для учебных заведений, школ, медицинских центров, аэропортов.
рюкзак школьный черный купить
Недавно мне пришлось организовать похороны, и я был поражен завышенными ценами на ритуальные услуги в Алматы. Я нашел статью о ценах на ритуальные услуги, которая действительно помогла мне понять, как формируются цены и как избежать переплат. В статье подробно объясняется, на что нужно обратить внимание при выборе агентства. Благодаря этим советам, я смог выбрать надежное агентство и избежать лишних расходов. Очень рекомендую всем, кто сталкивается с этой проблемой, ознакомиться с этим материалом!
рюкзак школьный черный купить
Hi there this is kinda of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding know-how so I wanted to get guidance from someone with experience. Any help would be greatly appreciated!
казино либет
Привет!
Ьожем предложить документы ВУЗов, расположенных на территории всей Российской Федерации. Можно приобрести качественно сделанный диплом за любой год, указав подходящую специальность и оценки за все дисциплины. Документы печатаются на бумаге самого высшего качества. Это дает возможности делать государственные дипломы, которые не отличить от оригиналов. Они заверяются необходимыми печатями и подписями.
Мы можем предложить дипломы любых профессий по разумным тарифам. Стоимость может зависеть от выбранной специальности, года выпуска и ВУЗа. Стараемся поддерживать для заказчиков адекватную политику цен. Важно, чтобы документы были доступными для большого количества наших граждан.
landik-diploms-srednee.ru/kupit-diplom-v-ekaterinburge
Удачи!
increase the excitement of the game.
plinko game
рюкзак школьный черный купить
Здравствуйте!
Заказать документ о получении высшего образования вы имеете возможность в нашем сервисе.
ast-diplomy.com/kupit-diplom-magistra
Хорошей учебы!
На сайте http://wirespace.ru изучите полезные, интересные и содержательные статьи, которые посвящены ландшафтному дизайну. Представлены любопытные идеи о том, как правильно разместить скульптуры, а также интересные декоративные элементы. Опубликованы не только рекомендации, но и любопытные идеи. Есть информация относительно дизайна для миниатюрных садов. Вы узнаете и о том, как правильно выбрать цветовую гамму для декорирования. Есть информация о том, как организовать роскошное пространство в доме.
To start working as a etalonsadforum.com walking or bicycle courier, just contact one of the partner companies.
рюкзак школьный черный купить
Добрый день!
Готовы предложить документы ВУЗов, расположенных на территории всей России. Можно приобрести диплом от любого учебного заведения, за любой год, включая документы старого образца. Дипломы и аттестаты выпускаются на “правильной” бумаге самого высшего качества. Это позволяет делать государственные дипломы, которые невозможно отличить от оригинала. Документы будут заверены необходимыми печатями и подписями.
Мы можем предложить дипломы любых профессий по приятным ценам. Стоимость будет зависеть от выбранной специальности, года выпуска и ВУЗа. Всегда стараемся поддерживать для клиентов адекватную политику цен. Для нас очень важно, чтобы документы были доступны для большого количества граждан.
landik-diploms-srednee.ru/svidetelstvo-o-rozhdenii
Успешной учебы!
рюкзак школьный черный купить
Добрый день!
Заказать документ университета можно у нас в столице.
ast-diplomas.com/kupit-diplom-magistra
Успехов в учебе!
Latest medication news. Comprehensive pill guide.
buy biaxin pills
Detailed medication knowledge. Patient drug facts.
рюкзак школьный черный купить
рюкзак школьный черный купить
рюкзак школьный черный купить
рюкзак школьный черный купить
На сайте https://pacific-map.com/index.html вы ознакомитесь с картой США с городами, штатами. Перед вами самая полная карта автомобильных дорог США. Есть карта Атлантического, Тихоокеанского побережья, имеется физическая карта США. Только здесь указана самая полная и содержательная информация, которая прольет свет на многочисленные вопросы. Вся информация является содержательной, интересной, актуальной, а потому на нее точно можно положиться. Обращайтесь и вы сюда за информацией, если необходимо что-то уточнить.
рюкзак школьный черный купить
Магазин Бытовок https://magazinbitovok.ru/ — ведущий производитель быстровозводимых мини-домиков для сада и дачи, а также модульных жилых бытовок и блок-контейнеров в Москве и Московской области. Мы предлагаем широкий ассортимент продукции, которая идеально подходит для временного и постоянного проживания. Наши мини-домики и бытовки отличаются высоким качеством, надежностью и доступной ценой. Мы используем только современные материалы и технологии, что гарантирует долговечность и комфорт
рюкзак школьный черный купить
Компания «АКСИОНТ» с успехом осуществила 100 проектов на платформе «1С:ERP Предприятие 8». Она вошла в десятку лидеров по созданию проектов на базе «1С:ERP Управление предприятием 2». На официальном портале 1С вы найдете проекты компании. https://axiont.ru – тут есть возможность оставить заявку уже сегодня. Укажите в соответствующих полях имя, а также номер телефона, после чего нажмите на кнопку «Отправить». Мы не останавливаемся на достигнутом: внедряем новые технологии и принимаем участие в выставках. Также проводим для предпринимателей мероприятия.
рюкзак школьный черный купить
рюкзак школьный черный купить
Добрый день!
Где заказать диплом специалиста?
Заказать диплом о высшем образовании.
russianecuador.com/forum/member.php?u=13207
рюкзак школьный черный купить
рюкзак школьный черный купить
Привет, друзья!
Мы готовы предложить дипломы любой профессии по разумным ценам.
newsbig.fotosdefrases.com/rekomendacii-po-priobreteniu-dokumenta-v-internete
рюкзак школьный черный купить
Your System – лучший надежный партнер для вас в сфере оборудования для видеонаблюдения. Предлагаем широкий ассортимент высококачественной продукции. Работаем исключительно с достойными производителями. Стараемся клиентам обеспечить индивидуальный подход и высочайший уровень обслуживания. Ищете автомобильная система видеонаблюдения? Y-ss.ru – сайт, где есть возможность приобрести по доступным ценам охранные системы. Доставим ваш заказ в любую точку России. Для вас работаем без выходных. Как процесс покупок сделать простым, с удовольствием расскажем. Свяжитесь с нами любым способом.
рюкзак школьный черный купить
рюкзак школьный черный купить
рюкзак школьный черный купить
рюкзак школьный черный купить
Здравствуйте!
Приобретение диплома ВУЗа с сокращенной программой обучения в Москве
mastercode.ru/forum/?PAGE_NAME=profile_view&UID=4753
Рады помочь!.
Здравствуйте!
Где заказать диплом по актуальной специальности?
Заказать диплом любого ВУЗа.
flerus-shop.hcp.dilhost.ru/club/user/3/forum/message/861/857/
рюкзак школьный черный купить
krepezh.net
рюкзак школьный черный купить
Привет!
Удивительно, но купить диплом кандидата наук оказалось не так сложно
lezt.ixbb.ru/viewtopic.php?id=109#p109
Всегда вам поможем!.
Добрый день!
Мы готовы предложить документы ВУЗов, расположенных на территории всей России. Можно заказать диплом от любого заведения, за любой год, указав подходящую специальность и хорошие оценки за все дисциплины. Документы выпускаются на “правильной” бумаге самого высшего качества. Это позволяет делать настоящие дипломы, не отличимые от оригинала. Документы будут заверены необходимыми печатями и подписями.
network-96082.mn.co/posts/61828809
Добрый день!
Где купить диплом по нужной специальности?
Заказать диплом ВУЗа.
http://www.matchfishing.ru/forumtest/1/member.php?u=23110
рюкзак школьный черный купить
alanews24.com
рюкзак школьный черный купить
рюкзак школьный черный купить
buy cheap gasex – purchase ashwagandha for sale buy diabecon tablets
Полезные советы по безопасной покупке диплома о высшем образовании
ast-diplomas24.ru/kupit-diplom-moskva
Добрый день!
Где купить диплом по актуальной специальности?
Мы изготавливаем дипломы любой профессии по приятным ценам. Стоимость может зависеть от выбранной специальности, года выпуска и университета. Стараемся поддерживать для клиентов адекватную ценовую политику. Для нас важно, чтобы дипломы были доступны для большого количества наших граждан.
Для вас предлагаем дипломы любой профессии по выгодным тарифам.
korrespondentweek.ru/kupit-diplom-rf-v-moskve-nadezhno-i-byistro/
Всегда вам поможем!.
Reducing the workload on morson.org technical support workers. Very often, monotonous actions take up a lot of time from specialists. If you work with tickets, you can optimize routine operations. In addition, you can count on deadlines, that is, assign responsibility for specific actions.
купить диплом с занесением в реестр в нижнем тагиле ast-diploms.com .
купить аттестаты об основном общем образовании купить аттестаты об основном общем образовании .
Then the structure homeideascoach.com with the floor is installed. If the model does not have a floor, then you will need to build a platform.
На сайте https://olato.ru представлены ванны и комплектующие, а также душевые кабины, различные ограждения, инсталляции, полотенцесушители. Все товары высокого качества, разработаны лучшими брендами, которые используют уникальные и инновационные технологии для достижения нужного результата. Все конструкции прочные, надежные и наделены высоким качеством. Продукция реализуется по привлекательным расценкам, организуется оперативная доставка. За покупки предоставляются бонусы. Есть безупречный клиентский сервис.
Ищете надежный навес для автомобиля в Истре? Vip-Naves предлагает широкий выбор металлических навесов для авто и дачи. Мы сами проектируем, производим и монтируем конструкции, без посредников. Наша компания предоставляет комплексные услуги, начиная с выезда инженера-замерщика в удобное для вас время, который зафиксирует все ваши требования и сделает точные замеры. Мы создаем бесплатный 3D макет будущей конструкции, чтобы вы могли видеть, как будет выглядеть ваш навес. После этого мы заключаем договор, фиксируя цену и сроки, и приступаем к изготовлению навеса. ВИП НАВЕС гарантирует высокое качество за счет использования профессионального оборудования и материалов. Доставка и монтаж осуществляются в удобный для вас день, а заключительные работы завершаются подписанием акта и уборкой территории. Обратитесь к нам, чтобы получить качественный навес по честной цене!
Здравствуйте!
Где купить диплом по нужной специальности?
Мы готовы предложить дипломы любой профессии по разумным тарифам. Цена зависит от той или иной специальности, года получения и ВУЗа. Стараемся поддерживать для покупателей адекватную ценовую политику. Для нас важно, чтобы дипломы были доступны для подавляющей массы наших граждан.
Для вас можем предложить дипломы психологов, юристов, экономистов и прочих профессий по доступным ценам.
dachaweek.ru/kupit-diplom-rf-v-moskve-realnyie-dokumentyi-po-dostupnoy-tsene
Рады оказать помощь!.
Привет, друзья!
Быстрое обучение и получение диплома магистра – возможно ли это?
sgs-penza.ru/index.php?subaction=userinfo&user=yvoriz
Рады оказать помощь!.
Привет, друзья!
Предлагаем документы ВУЗов, расположенных на территории всей РФ. Можно заказать качественно сделанный диплом за любой год, включая сюда документы старого образца. Дипломы и аттестаты делаются на бумаге высшего качества. Это позволяет делать государственные дипломы, которые невозможно отличить от оригинала. Документы заверяются необходимыми печатями и штампами.
Мы можем предложить дипломы любых профессий по разумным тарифам. Цена зависит от той или иной специальности, года выпуска и университета. Всегда стараемся поддерживать для покупателей адекватную политику цен. Для нас важно, чтобы документы были доступны для большого количества наших граждан.
landik-diploms-srednee.ru/svidetelstvo-o-razvode
Успешной учебы!
Зайдите на сайт http://tourhot.ru/ и вы сможете узнать все об отдыхе и путешествиях, а также ознакомиться с каталогом отелей по всему миру и воспользоваться быстрым поиском отелей. Обратитесь к менеджеру (или найдите самостоятельно) тур своей мечты под любой бюджет, с любыми датами вылета по оптимальным ценам. Все туры в одном месте по выгодной цене у нас на сайте.
Привет, друзья!
Приобрести документ о получении высшего образования вы имеете возможность в нашей компании в Москве.
ast-diploms24.ru/otzyvy
Удачи!
Привет!
Заказать диплом ВУЗа.
loveyou.az/read-blog/165
Привет, друзья!
Предлагаем документы техникумов, расположенных на территории всей Российской Федерации. Можно заказать диплом за любой год, указав необходимую специальность и хорошие оценки за все дисциплины. Дипломы и аттестаты выпускаются на “правильной” бумаге высшего качества. Это позволяет делать государственные дипломы, которые не отличить от оригиналов. Они будут заверены всеми необходимыми печатями и штампами.
Мы изготавливаем дипломы любых профессий по выгодным ценам. Цена может зависеть от той или иной специальности, года получения и образовательного учреждения. Всегда стараемся поддерживать для покупателей адекватную ценовую политику. Важно, чтобы дипломы были доступными для большинства наших граждан.
landik-diploms-srednee.ru/svidetelstvo-o-razvode
Успешной учебы!
купить высшее образование цена ast-diploms.com .
купить диплом маси diplomasx.com .
Здравствуйте!
Заказать документ о получении высшего образования вы сможете в нашей компании.
diplomasx.com/kupit-diplom-voronezh
Удачи!
Discovered a unique article – recommended to acquaint yourself! https://чпуремонт.рф/showthread.php?tid=56260
Привет, друзья!
Заказать диплом любого ВУЗа.
http://www.import-moto.com/users/88
Успехов в учебе!
Discovered an article that will definitely interest you – don’t miss the chance to familiarize yourself https://uz-kino.ru/user/ascullqeye
Здравствуйте!
Наша компания предлагает максимально быстро заказать диплом, который выполнен на оригинальной бумаге и заверен печатями, водяными знаками, подписями. Данный документ пройдет лубую проверку, даже при использовании специального оборудования. Достигайте своих целей быстро и просто с нашим сервисом.
mariland.org/index.php?subaction=userinfo&user=aduzu
Удачи!
сколько стоят дипломы сколько стоят дипломы .
Howdy just wanted to give you a brief heads up and let you know a few of the pictures aren’t loading correctly. I’m not sure why but I think its a linking issue. I’ve tried it in two different internet browsers and both show the same outcome.
кет казино
Привет, друзья!
Где купить диплом специалиста?
ashinova.ru/category-5/t-1710.html#1710
Успешной учебы!
The other day, while I was at work, my cousin stole my iphone and tested to see if it can survive a thirty foot drop, just so she can be a youtube sensation. My apple ipad is now destroyed and she has 83 views. I know this is totally off topic but I had to share it with someone!
официальный сайт lee bet
На сайте https://sites.google.com/view/mvavada/ получите всю важную и содержательную информацию, которая касается популярного, известного заведения «VAVADA». Представлена информация о том, как войти, пройти регистрацию, о бонусах, а также альтернативных ссылках. Вавада предлагает огромный выбор развлечений на самый взыскательный вкус. А еще здесь щедрая бонусная программа, проверенная система безопасности. Игровой клуб получил репутацию проверенного и надежного игрока на рынке. Выиграйте средства и вы!
## Unlock Real Winnings: The Best Casino Apps That Pay Real Money
In the ever-evolving world of online gaming, casino apps have revolutionized how we experience the thrill of gambling. The allure of winning real money from the comfort of your smartphone is irresistible. With countless options available, choosing the right casino app can be daunting. Fear not! We’ve curated a guide to help you find the best casino apps that pay real money, ensuring a safe, exciting, and potentially lucrative experience.
### Why Choose Casino Apps That Pay Real Money?
Casino apps that offer real money payouts provide a convenient and exhilarating way to enjoy your favorite casino games. Here are a few reasons why these apps are gaining immense popularity:
1. **Convenience**: Play anytime, anywhere. Whether you’re commuting, relaxing at home, or on a break at work, casino apps are always at your fingertips.
2. **Variety of Games**: From classic table games like blackjack and roulette to exciting slots and poker, these apps offer a vast array of games to suit every player’s taste.
3. **Real Money Rewards**: Unlike free casino apps, these platforms give you the opportunity to win real cash, adding an extra layer of excitement and motivation.
4. **Bonuses and Promotions**: Casino apps often provide enticing bonuses, free spins, and promotions, enhancing your chances of winning big.
### Top Casino Apps That Pay Real Money
To ensure you have a seamless and rewarding experience, here are some of the top-rated casino apps known for their reliability, security, and lucrative payouts:
#### 1. **Betway Casino App**
Betway is a renowned name in the online gambling industry, and its app lives up to the brand’s reputation. Offering a wide range of games, including slots, blackjack, roulette, and live dealer options, Betway provides a secure and user-friendly platform. The app also boasts generous welcome bonuses and ongoing promotions to maximize your winning potential.
#### 2. **888 Casino App**
888 Casino is a veteran in the online casino world, and its app is a testament to its excellence. With a sleek design and an extensive game library, 888 Casino offers everything from slots and jackpots to table games and live casino experiences. The app ensures secure transactions and prompt payouts, making it a favorite among real money players.
#### 3. **LeoVegas Casino App**
LeoVegas is known for its mobile-first approach, making it one of the best casino apps for real money gaming. The app features a vast selection of games from top providers, including immersive live dealer games. LeoVegas is also praised for its swift and hassle-free withdrawal process, allowing you to enjoy your winnings without delay.
#### 4. **Royal Panda Casino App**
Royal Panda combines a fun and engaging gaming experience with the opportunity to win real money. The app offers a rich variety of games, including popular slots, table games, and live casino options. With its easy-to-navigate interface and secure payment methods, Royal Panda ensures a smooth and rewarding gaming journey.
#### 5. **Jackpot City Casino App**
As the name suggests, Jackpot City is all about big wins. This app offers a comprehensive selection of games, including progressive jackpot slots that can yield life-changing payouts. With its user-friendly design and top-notch security measures, Jackpot City provides a trustworthy platform for real money gambling.
### Tips for Maximizing Your Winnings
To make the most of your real money casino app experience, consider these tips:
1. **Choose Reputable Apps**: Stick to well-known and licensed casino apps to ensure fair play and secure transactions.
2. **Take Advantage of Bonuses**: Utilize welcome bonuses, free spins, and other promotions to boost your bankroll and increase your chances of winning.
3. **Manage Your Bankroll**: Set a budget and stick to it. Avoid chasing losses and know when to take a break.
4. **Play Smart**: Familiarize yourself with the rules and strategies of the games you play. Knowledge can significantly enhance your winning potential.
### Conclusion
Casino apps that pay real money offer an exciting and convenient way to enjoy the thrill of gambling while giving you the chance to win actual cash. By choosing reputable apps like Betway, 888 Casino, LeoVegas, Royal Panda, and Jackpot City, you can ensure a secure and rewarding gaming experience. So, download your preferred app, take advantage of the bonuses, and get ready to unlock real winnings! Happy gaming!
Also visit my homepage – http://gaseung.com/bbs/board.php?bo_table=free&wr_id=1983
Medication effects explained. Comprehensive medicine guide.
reliable online pharmacy
Access pill information. Access medication details.
можно ли покупать диплом http://www.diploms-x.com .
видеостена videosteny-pod-kljuch.ru .
На сайте https://cpo24.ru/ закажите звонок для того, чтобы получить допуск СРО. Документ будет на руках в течение суток. Стоимость услуги варьируется от 50 000 рублей. При этом отсутствуют надбавки, комиссии. В этой компании вы сможете получить СРО проектировщиков, строителей, а также энергоаудиторов, изыскателей либо воспользоваться услугой сопровождения проверок СРО. Все услуги выполняются ответственными, квалифицированными, грамотными сотрудниками. При этом работы обойдутся недорого.
Found an article that is worth reading – it’s really interesting! http://www.siteglimpse.com/external/ext.aspx?url=http://153.126.169.73/question2answer/index.php?qa=user&qa_1=rillenpxkm
Добрый день!
Мы готовы предложить дипломы любой профессии по доступным ценам.
http://www.msestudio.com.br/купить-диплом-мфюа/
На сайте https://ustanovki-masla.ru представлена информация о том, какую установку, использующуюся для слива, а также откачки масла, лучше выбрать. Представлены и пневматические установки, которые собирают масло, которое уже отработало. Изучите функциональные, качественные устройства, предназначенные для замены масла и с ручным приводом. Также изучите и важные особенности, достоинства установок. Перед вами только самая актуальная и честная информация, которая обязательно понадобится.
My soul and heart will always be grateful to you. Thank you for being awesome.
gasex order online – order generic ashwagandha buy generic diabecon
купить диплом улгу ast-diploms.com .
Привет!
Приобрести документ о получении высшего образования вы можете у нас.
diploms-x.com/kupit-diplom-nizhnij-novgorod
Здравствуйте!
Готовы предложить документы техникумов, которые находятся на территории всей РФ. Вы можете приобрести качественно сделанный диплом от любого заведения, за любой год, указав необходимую специальность и хорошие оценки за все дисциплины. Документы печатаются на бумаге высшего качества. Это позволяет делать государственные дипломы, не отличимые от оригинала. Они будут заверены необходимыми печатями и подписями.
Мы предлагаем дипломы психологов, юристов, экономистов и других профессий по приятным ценам. Стоимость будет зависеть от конкретной специальности, года выпуска и образовательного учреждения. Всегда стараемся поддерживать для покупателей адекватную ценовую политику. Для нас очень важно, чтобы дипломы были доступными для подавляющей массы граждан.
landik-diploms-srednee.ru/kupit-diplom-v-ekaterinburge В
Успехов в учебе!
Привет!
Приобрести документ ВУЗа можно у нас.
ast-diplomas.com/kupit-diplom-ekaterinbur
Удачи!
Привет, друзья!
Заказать документ ВУЗа можно в нашей компании в Москве.
ast-diploms24.ru/otzyvy
Здравствуйте!
Предлагаем документы техникумов, расположенных на территории всей Российской Федерации. Вы имеете возможность заказать качественно напечатанный диплом от любого заведения, за любой год, включая документы СССР. Документы печатаются на “правильной” бумаге высшего качества. Это дает возможность делать государственные дипломы, не отличимые от оригинала. Документы заверяются необходимыми печатями и штампами.
Мы изготавливаем дипломы психологов, юристов, экономистов и других профессий по приятным тарифам. Цена зависит от определенной специальности, года получения и университета. Стараемся поддерживать для заказчиков адекватную политику тарифов. Для нас очень важно, чтобы дипломы были доступны для большого количества граждан.
arusak-diploms-srednee.ru/kupit-diplom-kandidata-nauk В
Успехов в учебе!
Добрый день!
Заказать документ института можно у нас в столице.
diplomasx.com/kupit-diplom-ekaterinbur
Успешной учебы!
Привет!
Мы готовы предложить документы ВУЗов, которые расположены на территории всей России. Можно приобрести диплом от любого учебного заведения, за любой год, указав необходимую специальность и оценки за все дисциплины. Документы печатаются на “правильной” бумаге самого высокого качества. Это дает возможности делать государственные дипломы, не отличимые от оригинала. Они заверяются необходимыми печатями и штампами.
secure.smore.com/n/x031d-russian-diplom
Привет, друзья!
Парадокс, но купить диплом кандидата наук оказалось не так и сложно
mybaltika.info/ru/blogs/587/10347
Рады оказать помощь!.
Pill leaflet provided. Medication data provided.
online pharmacies mexica
Drug reactions explained. Comprehensive pill guide.
Добрый день!
Как купить аттестат 11 класса с официальным упрощенным обучением в Москве
school97.ru/vesti20/index.php?PAGE_NAME=profile_view&UID=210371
Всегда вам поможем!.
Ищите Глаз Бога https://eyeofgodinfo.me/ или Глаз бога телеграм? Зайдите на официальный сайт, и вы получите необходимую информацию. Глаз Бога официальный сайт это удобный способ воспользоваться лучшим инструментом для поиска информации. А если вам удобнее пользоваться Глаз бога телеграмм – то добро пожаловать в мессенджер, где вы сможете запросить все тоже, что и на сайте.
Желаете продать свое авто быстро и по достойной цене? У нас трудятся грамотные специалисты, которые обладают приличным опытом в области продаж. Предоставим оценку вашего автомобиля бесплатно. Теперь не надо на утомительные поиски покупателя тратить время. Все организационные вопросы мы берем на себя. Ищете выкуп автомобиля цена в казани? Cars16.ru – сайт, где вы найдете более детальную информацию. Мы подбираем особый подход к нашим клиентам и дорожим ими. Расчет совершаем удобным способом. Гарантируем честные сделки. Для обсуждения деталей, свяжитесь с нами. Будем рады вам помочь!
24thainews.com
alcitynews.com
Рады видеть вас на нашем блоге, который посвящен маркетплейсам! Oowa.ru – это полноценный источник надежной информации. Вы узнаете, как пользоваться Wildberries. Подробно рассказываем о ключевых методах продвижения на маркетплейсах. Контент круглосуточно доступен. https://oowa.ru – сайт, где у вас есть возможность найти много полезных материалов. Здесь имеется удобный поиск, воспользуйтесь им. Помимо прочего тут мы представили новости маркетплейсов, можете за ними следить. Посетите наш блог уже сегодня. Мы выкладываем только наилучшие предложения.
диплома нет диплома нет .
Здравствуйте!
Как оказалось, купить диплом кандидата наук не так уж и сложно
comedyforme.ru/vash-diplom-garantiya-kachestva-i-nadezhnosti
Здравствуйте!
Как получить диплом стоматолога быстро и официально
glass.forum2x2.ru/t3268-topic#6539
Окажем помощь!.
Привет!
Заказать диплом любого ВУЗа
Мы предлагаем документы ВУЗов, расположенных в любом регионе РФ. Можно приобрести качественный диплом за любой год, включая сюда документы старого образца СССР. Дипломы и аттестаты печатаются на бумаге высшего качества. Это дает возможность делать настоящие дипломы, не отличимые от оригиналов. Они заверяются необходимыми печатями и штампами.
themepacific.com/support/users/lutroduyda/
Окажем помощь!.
Online medicine order: best online pharmacy india – best india pharmacy
Taobao – известная торговая интернет-платформа. Здесь приобрести можете самое необходимое. Мы предоставляем для вас простой способ избавиться от изнуряющих походов по магазинам. Ищете корейская косметика купить онлайн? Grandior.ru – портал, где имеется большой выбор товаров. Гарантируем вам низкие цены. Предусмотрены и скидки. Теперь вы знаете, какой секрет популярности у Таобао ком. Удовлетворим запросы даже самых требовательных покупателей. Сайт Taobao на русском языке «Грандиор.ру» – станет вашим лучшим помощником в совершении покупок товаров.
Привет!
Заказать диплом университета.
bs.listbb.ru/viewtopic.php?f=3&t=531
Хорошей учебы!
На сайте https://cars16.ru заполните форму для того, чтобы ваш автомобиль оценили по фотографии. На это уйдут всего 5 минут. Только в этой компании выкупают машины намного дороже, чем в других. При этом предлагают реальную сумму. Теперь реализовать автомобиль вы сможете всего за час. Оценщик приедет на объект в ближайшее время, чтобы обозначить стоимость. Если она устроит обе стороны, то подписывается договор. Важным моментом является то, что деньги вы получаете сразу же, полную сумму. В этой компании действуют самые выгодные условия.
Здравствуйте!
Приобрести диплом любого ВУЗа
Мы предлагаем документы техникумов, которые расположены в любом регионе Российской Федерации. Вы имеете возможность приобрести диплом от любого заведения, за любой год, в том числе документы старого образца. Документы делаются на бумаге высшего качества. Это позволяет делать настоящие дипломы, которые не отличить от оригиналов. Документы будут заверены всеми обязательными печатями и подписями.
messenger.wepluz.com/read-blog/11105
Всегда вам поможем!.
Здравствуйте!
Наша компания предлагает заказать диплом высокого качества, который невозможно отличить от оригинала без участия специалистов высокой квалификации со сложным оборудованием.
kochtagebuch.org/doku.php?id=gosznacdiplomy
Успешной учебы!
Drug information here. Patient medicine resource.
viagra online pharmacy
Latest medicine developments. Access pill facts.
Добрый день!
Заказать диплом о высшем образовании.
moneysweet.listbb.ru/viewtopic.php?f=2&t=1405
Успешной учебы!
https://indiapharmast.com/# mail order pharmacy india
Привет!
Наши специалисты предлагают быстро заказать диплом, который выполнен на бланке ГОЗНАКа и заверен мокрыми печатями, водяными знаками, подписями официальных лиц. Данный диплом способен пройти лубую проверку, даже с применением специального оборудования. Решите свои задачи быстро и просто с нашими дипломами.
uznt42.ru/index.php?subaction=userinfo&user=ejifiky
Успешной учебы!
Привет!
Официальное получение диплома техникума с упрощенным обучением в Москве.
Приобрести диплом о высшем образовании.
octomo.co.uk/read-blog/949
top 10 online pharmacy in india: world pharmacy india – indian pharmacies safe
Ищете надежный навес для автомобиля в Щелково? Вип-Навес предлагает широкий выбор металлических навесов для авто и дачи. Мы сами проектируем, производим и монтируем конструкции, без посредников. Наша компания предоставляет комплексные услуги, начиная с выезда инженера-замерщика в удобное для вас время, который зафиксирует все ваши требования и сделает точные замеры. Мы создаем бесплатный 3D макет будущей конструкции, чтобы вы могли видеть, как будет выглядеть ваш навес. После этого мы заключаем договор, фиксируя цену и сроки, и приступаем к изготовлению навеса. Vip Naves гарантирует высокое качество за счет использования профессионального оборудования и материалов. Доставка и монтаж осуществляются в удобный для вас день, а заключительные работы завершаются подписанием акта и уборкой территории. Обратитесь к нам, чтобы получить качественный навес по честной цене!
safe reliable canadian pharmacy: canadian pharmacy drugs online – legit canadian pharmacy
Здравствуйте!
Где приобрести диплом специалиста?
danceway74.ru/users/36
Успехов в учебе!
indian pharmacies safe mail order pharmacy india top 10 online pharmacy in india
britainrental.com
Companies with high welcomelady.net levels of customer service usually have an excellent reputation and positive reviews.
Привет!
Заказать документ университета вы можете в нашей компании в столице.
ast-diplomas24.ru/otzyvy
Успешной учебы!
Добрый день!
Мы можем предложить дипломы любой профессии по невысоким ценам.
myweektour.ru/legkiy-sposob-poluchit-diplom/
Здравствуйте!
Заказать документ института вы можете в нашей компании в столице.
ast-diplom.com/kupit-diplom-vracha
Хорошей учебы!
Привет!
Наши специалисты предлагают выгодно и быстро заказать диплом, который выполнен на бланке ГОЗНАКа и заверен печатями, водяными знаками, подписями должностных лиц. Данный документ пройдет лубую проверку, даже с применением специфических приборов. Достигайте своих целей быстро с нашими дипломами.
narodovmnogo-omsk.ru/forum/user/4166/
Хорошей учебы!
Здравствуйте!
Где заказать диплом специалиста?
Мы готовы предложить документы институтов, расположенных в любом регионе РФ. Вы можете купить диплом за любой год, указав необходимую специальность и оценки за все дисциплины. Дипломы выпускаются на бумаге высшего качества. Это дает возможности делать настоящие дипломы, которые невозможно отличить от оригиналов. Документы заверяются всеми необходимыми печатями и штампами.
Мы изготавливаем дипломы психологов, юристов, экономистов и прочих профессий по невысоким тарифам.
ast-diplom.com/kupit-diplom-rostov-na-donu
Рады оказать помощь!
Привет, друзья!
Как купить аттестат 11 класса с официальным упрощенным обучением в Москве
mybuildhouse.ru/byistroe-oformlenie-diploma-lyuboy-spetsialnosti
Всегда вам поможем!.
Здравствуйте!
Купить диплом ВУЗа.
mastergrad.getbb.ru/viewtopic.php?f=12&t=1872
Удачи!
Добрый день!
Мы готовы предложить документы ВУЗов, которые расположены в любом регионе Российской Федерации. Можно купить диплом за любой год, в том числе документы старого образца. Документы печатаются на бумаге самого высокого качества. Это дает возможность делать настоящие дипломы, не отличимые от оригинала. Документы будут заверены необходимыми печатями и подписями.
textualheritage.org/index.php?option=com_content&task=view&id=1081
Привет!
Купить диплом о высшем образовании
arusak-diploms-srednee.ru/kupit-diplom-sssr В
Хорошей учебы!
rust movie settlement nys dec waterfowl seasonultimate avengers: the moviescariest movies to watch reddithow many episodes are in you season 4 part 2
Привет, друзья!
Где заказать диплом специалиста?
afterpad.com/forums/post.php?fid=7
Удачи!
На сайте https://y-ss.ru вы найдете высокотехнологичные, качественные и инновационные охранные системы, которые представлены популярными брендами. Изучите весь ассортимент товаров, чтобы выбрать то, что именно нужно. Этот магазин выбирают потому, что он находится на рынке более 20 лет, заслужил постоянных и преданных покупателей. Отзывы об этом ресурсе исключительно положительные. У магазина сложилась безупречная репутация. Здесь установлены привлекательные расценки, организуется быстрая доставка.
Привет, друзья!
Как правильно приобрести диплом колледжа или ПТУ в России, важные моменты
forum.resmihat.kz/viewtopic.php?f=10&t=2265818
Поможем вам всегда!.
Здравствуйте!
Мы можем предложить документы техникумов, которые расположены на территории всей России. Можно приобрести качественно напечатанный диплом от любого учебного заведения, за любой год, включая документы старого образца СССР. Дипломы и аттестаты делаются на бумаге самого высокого качества. Это позволяет делать настоящие дипломы, не отличимые от оригиналов. Документы будут заверены необходимыми печатями и подписями.
forum-rassvet-rp.ru/index.php?app=gallery&module=gallery&controller=view&id=25
Привет, друзья!
Купить диплом университета
arusak-diploms-srednee.ru/kupit-attestat-za-11-klass В
Удачи!
Medication effects explained. Misuse consequences detailed.
online canadian pharmacy
Latest medication developments. Pill information provided.
canadian mail order pharmacy: canadian pharmacy world – best canadian online pharmacy
Opened up an enthralling read Р I’d like to share it with you https://www.blogtalkradio.com/petramjwuc
Скачать торрент https://webtorrent.pro/ со всеми свежими фильмами со всего мира в один клик в отличном качестве без регистрации у нас на сайте. Любые жанры, любые годы, в том числе новинки 2024 – все готово к скачиванию. Легкий поиск, подборки по жанрам, лучшие фильмы, сериалы, мультфильмы в огромном количестве.
100RENT.BY – ведущая онлайн-платформа для аренды строительной и специальной техники, оборудования в разных регионах Беларуси. Наша основная цель – сделать взаимодействие между арендодателями и арендаторами в строительной сфере более результативным. Ищете аренда газонокосилки минск ома? 100rent.by – портал, где имеется подробная о нас информация, посмотрите ее в любое время. Мы сделали понятный и современный интерфейс для поиска объявлений и удобства публикования. Гарантируем мгновенную регистрацию и предоставляем гибкие тарифы. Всегда вам рады!
Привет!
Наш сервис предлагает заказать диплом в высочайшем качестве, неотличимый от оригинального документа без участия специалиста высокой квалификации с дорогостоящим оборудованием.
forum.home-visa.ru/viewtopic.php?f=69&t=1211678
Удачи!
top online pharmacy india: pharmacy website india – buy medicines online in india
Привет!
Купить документ о получении высшего образования вы можете в нашем сервисе.
ast-diploms.com/kupit-diplom-voronezh
domstroi.info
newsplaces.net
Привет!
Купить документ о получении высшего образования вы имеете возможность у нас в Москве.
diplomasx.com/kupit-diplom-ekaterinbur
reputable indian online pharmacy india pharmacy mail order indian pharmacy paypal
indian pharmacies safe: mail order pharmacy india – buy medicines online in india
На сайте https://afinaokna.ru/ есть возможность купить качественные и надежные деревянные, пластиковые либо алюминиевые окна, стеклопакеты. На изготовление конструкций уходят не более 3 дней. Компания берет предоплату в размере тысячи рублей. Предоставляется рассрочка на полгода. Доставка по Санкт-Петербургу бесплатная. После работ мусор выносится в мешках. В компании не только производят, но и продают, выполняют монтаж окон. Гарантируется качественное выполнение всех работ. Если и вы обратитесь за услугой в эту компанию, то получите гарантированно высокое качество.
Здравствуйте!
Где купить диплом специалиста?
armit.ru/social/user/42552/forum/message/1604/1606/#message1606
Успехов в учебе!
http://indiapharmast.com/# indian pharmacy online
На сайте https://stapeli1.ru получите данные о том, какие стапели лучше всего подобрать для того, чтобы выполнить кузовной ремонт. Вы ознакомитесь с типами стапелей, особенностями, преимуществами. Есть информация о платформенных стапелях. Вы узнаете о достоинствах использования таких конструкций в ремонте. Имеется информация и о том, как правильно подобрать конструкцию, чтобы она прослужила как можно дольше и обрадовала своими эксплуатационными свойствами. Рассматриваются параметры, которые помогут подобрать устройство высокого качества.
На сайте https://ipoteka-1.ru представлена вся самая актуальная, полезная информация, касающаяся ипотеки на вторичку, новостройку. Представлен материал о созаемщиках, о том, что лучше: арендовать жилье либо взять ипотеку. Есть данные о расходах на ипотеку и каким образом их понизить. Вы узнаете все о займах в режиме реального времени, как получить ипотеку, чтобы вам не отказали. Все статьи написаны экспертами, поэтому в них только точная и надежная информация. Вы получите ответ на вопрос, как быть, если нечем платить за ипотеку.
Хотите по достойной цене и быстро продать свое авто? У нас работают высококвалифицированные специалисты с опытом в сфере продаж. Мы совершенно бесплатно предоставим оценку вашего автомобиля. Вы сразу же получите предложение о выкупе. Больше не нужно тратить время на долгие поиски покупателя. Организационные моменты мы берем на себя. https://cars16.ru – сайт, где представлена более подробная информация. Ценим своих клиентов и гарантируем им прозрачные условия сотрудничества. Свяжитесь с нами для обсуждения деталей. Будем рады помочь!
Приветствуем вас на канале проекта casino VAVADA! Здесь имеется самая свежая информация. Забудьте о повседневных заботах и проведите время за увлекательными слотами в высококачественном онлайн-казино Вавада! Вас ждет особая атмосфера и отличная графика. Ищете вавада личный? t.me/mvavada – здесь мы с вами делимся секретами успеха и своими знаниями. Казино VAVADA подходит всем без исключения. Вы точно оцените бонусы и скорость выводов. Саппорт старается любые вопросы решать довольно быстро. Начните игру уже сегодня. Удачи вам и победы!
На сайте https://nasosynsk.ru/ закажите звонок для того, чтобы узнать все про насосы. Среди популярных категорий: насосы для воды, бытовое оборудование, а также насосы для отопления, те, которые используются с целью отвода сточных вод, промышленное оборудование и многое другое. В этой компании на профессиональном уровне подбирают, реализуют, а также проектируют насосы. Перед вами самый большой выбор моделей, а также привлекательные расценки. Специалисты предприятия постоянно проходят стажировку.
politeconomics.org
Get pill details. Latest pill trends.
online pharmacy hydrocodone
Find pill facts. Medicine brochure provided.
Здравствуйте!
Мы изготавливаем дипломы психологов, юристов, экономистов и других профессий по невысоким тарифам.
eurodelo.ru/vash-shans-na-vyisshee-obrazovanie-kupit-diplom
Starting to take stock, we can say with ukrtvoru.info complete confidence that, indeed, both absolute and relative height will play an important role in geography.
canadian pharmacy online: canadian pharmacy no rx needed – medication canadian pharmacy
Привет, друзья!
Заказать документ университета вы сможете у нас в столице.
diploms-x24.ru/kupit-diplom-krasnoyarsk
Успешной учебы!
Здравствуйте!
Приобрести документ института вы сможете в нашей компании в столице.
diploms-x.com/kupit-diplom-o-srednem-obrazovanii
Успешной учебы!
best online pharmacies in mexico: mexican online pharmacies prescription drugs – medicine in mexico pharmacies
Your System – ваш надежный партнер в области оборудования для видеонаблюдения. Предлагаем широкий ассортимент высококачественной продукции. Работаем исключительно с достойными производителями. Стремимся обеспечить клиентам высокий уровень обслуживания и персональный подход. Ищете скуд купить считыватель? Y-ss.ru – сайт, где можно купить охранные системы по лояльным ценам. Ваш заказ доставим в любую точку РФ. Мы работаем для вас без выходных. С радостью подскажем, как сделать процесс покупок простым. Свяжитесь с нами любым способом.
purchase lasuna – brand himcolin himcolin tablets
Привет!
Приобрести диплом университета
arusak-diploms-srednee.ru/kupit-diplom-sssr В
Хорошей учебы!
Здравствуйте!
Узнайте стоимость диплома высшего и среднего образования и процесс получения
kalininabad.flyboard.ru/viewtopic.php?f=28&t=2823&sid=bd3645907d553caf3cac48f42ece1fdc
Рады помочь!.
Добрый день!
Мы можем предложить документы техникумов, которые находятся на территории всей РФ. Можно приобрести качественный диплом за любой год, указав необходимую специальность и оценки за все дисциплины. Дипломы и аттестаты выпускаются на бумаге самого высокого качества. Это дает возможности делать государственные дипломы, не отличимые от оригиналов. Они будут заверены всеми необходимыми печатями и штампами.
kopoluzhona.image-perth.org/bystro-priobretaem-diplom-v-lucsem-magazine-russian-diplom
Привет, друзья!
Купить диплом ВУЗа
arusak-diploms-srednee.ru/kupit-diplom-magistra В
Хорошей учебы!
Добрый день!
Где и как купить диплом о высшем образовании без лишних рисков
veneraroleplay.listbb.ru/viewtopic.php?f=4&t=317
Рады оказаться полезными!.
Здравствуйте!
Мы предлагаем документы ВУЗов, которые расположены на территории всей Российской Федерации. Вы можете приобрести диплом от любого учебного заведения, за любой год, указав подходящую специальность и хорошие оценки за все дисциплины. Дипломы и аттестаты печатаются на бумаге самого высшего качества. Это дает возможности делать настоящие дипломы, которые невозможно отличить от оригинала. Документы заверяются необходимыми печатями и штампами.
usa.life/read-blog/63237
Medication leaflet here. Pill guide here.
pharmacy technician online
Medication impacts explained. Patient medication guide.
order lasuna generic – cheap himcolin generic himcolin canada
}
Online medicine order buy medicines online in india best india pharmacy
best online pharmacy india: online pharmacy india – top 10 pharmacies in india
магазин аккаунтов социальных сетей http://magazin-akkauntov.ru/ .
http://foruspharma.com/# buying prescription drugs in mexico
На сайте https://oowa.ru/ вы найдете самые свежие, новые промокоды, которые позволят получить скидку на самые разные товары, в том числе, косметику, парфюмерию, бытовую технику. Все промокоды действуют вплоть до конца июля, а потому нужно успеть ими воспользоваться. Скидка предоставляется как на первый, так и повторные заказы. Это настоящая выгода для вас. При этом вы сможете набрать столько товаров, сколько хотите, ведь действует хорошая выгода. Узнайте то, как правильно сделать фотосессию товаров для различных маркетплейсов.
Patient drug resource. Medicine facts available.
online pharmacy india
Drug trends described. Drug guide provided.
Здравствуйте!
Где приобрести диплом по актуальной специальности?
Заказать диплом о высшем образовании.
xn--80apeih4a.xn--p1ai/club/user/71/blog/4501/
mexican pharmaceuticals online: mexican online pharmacies prescription drugs – mexican rx online
Официальное получение диплома техникума с упрощенным обучением в Москве
diplomyx24.ru/kupit-diplom-o-vysshem-obrazovanii
indian pharmacy paypal: indian pharmacies safe – indian pharmacy paypal
купить диплом 9 класс ast-diploms.com .
Medication impacts described. Patient drug leaflet.
online pharmacy canada
Comprehensive medication overview. Contraindications explained here.
купить диплом о высшем образовании в кирове купить диплом о высшем образовании в кирове .
Здравствуйте!
Приобрести документ института можно у нас в Москве.
ast-diploms.com/kupit-diplom-o-srednem-obrazovanii
Здравствуйте!
Приобрести документ ВУЗа можно в нашей компании.
asxdiplomik24.ru/otzyvy
Хорошей учебы!
Здравствуйте!
Заказать документ о получении высшего образования можно в нашей компании.
ast-diplomas24.ru/kupit-diplom-moskva
Привет!
Вопросы и ответы: можно ли быстро купить диплом старого образца?
rabotalnr.ru/users/ycuzeqi
Окажем помощь!.
куплю диплом качество https://diploms-x.com .
reputable indian pharmacies: reputable indian pharmacies – top 10 online pharmacy in india
Здравствуйте!
Приобрести документ института можно у нас в Москве.
ast-diplomas24.ru/kupit-diplom-voronezh
Успехов в учебе!
http://doxycyclinedelivery.pro/# doxycycline 40 mg generic coupon
На сайте https://dvuhstoechnie-podjemniki.ru вы найдете любопытную, интересную и свежую информацию, которая касается двухстоечных подъемников. Также рассматривается то, какую конструкцию лучше всего выбрать для своих целей и опираясь на финансовое положение. Рассматриваются различные виды подъемников, а также их преимущества. Возьмите на вооружение такие важные параметры, как: грузоподъемность, высота подъема и другое. Также рассматриваются и востребованные производители оборудования.
Great info! Keep post great articles.
купить диплом в люберцах ast-diploms.com .
куплю диплом высшего образования куплю диплом высшего образования .
Добрый день!
Покупка диплома о среднем полном образовании: как избежать мошенничества?
landik-diploms-srednee.ru/kupit-diplom-v-ekaterinburge В
Компанию СамГруз многие советуют. В услуги наши входит: доставка мебели и оргтехники из магазина, вывоз строительного мусора и хлама на газели, перевозка строительного материала. У нас работают водители с опытом. Грузичик очень аккуратные. Даем гарантию на быструю подачу грузового авто и доступные цены. https://gruz63.ru – сайт, где у вас есть возможность детальнее посмотреть нашу контактную информацию и ознакомиться с услугами. СамГруз – это качественно, недорого и оперативно. Можете убедиться в этом сами. Мы не подведем вас!
диплом юриста образец с оценками diploms-x.com .
Привет!
Процесс получения диплома стоматолога: реально ли это сделать быстро?
naturetour.ru/club/user/186/blog/1633
Поможем вам всегда!.
На сайте https://koleso-na-hodu.ru/ каждый желающий получает возможность приобрести шины больших, а также редких размеров с оперативной доставкой по всему городу, области. Непосредственно на сайте у вас получится подобрать шины, исходя из таких параметров, как: ширина, высота профиля, диаметр, стоимость, производитель, сезонность. Вся продукция сертифицированная, качественная, оригинальная. Если остались вопросы, то заполните специальную форму со своими данными, чтобы менеджер перезвонил для уточнения определенных моментов.
Привет!
Вопросы и ответы: можно ли быстро купить диплом старого образца?
landik-diploms-srednee.ru/kupit-diplom-v-voronezhe В
Patient medication resource. Access drug facts.
trusted online pharmacy
Pill guide here. Find medication details.
Привет, друзья!
Мы предлагаем документы ВУЗов, которые расположены в любом регионе РФ. Вы имеете возможность купить диплом за любой год, в том числе документы СССР. Дипломы и аттестаты выпускаются на бумаге самого высшего качества. Это дает возможности делать государственные дипломы, не отличимые от оригиналов. Документы будут заверены необходимыми печатями и подписями.
http://www.datasheetclub.com/read-blog/92
Привет!
Приобретение диплома ВУЗа с сокращенной программой обучения в Москве
http://www.hristianka.ru/forum/r/prev_loaded/1/
Всегда вам поможем!.
Encountered a captivating article, I propose you read https://jsbin.com/rucuniyoru
I think it is a nice point of view. I most often meet people who rather say what they suppose others want to hear. Good and well written! I will come back to your site for sure!
Привет, друзья!
Заказать диплом любого ВУЗа.
wayworld.listbb.ru/viewtopic.php?f=2&t=24475
Хорошей учебы!
дипломы аттестаты спб asxdiplomik24.ru .
They allow people to better everbestnews.com understand geographical objects, which should be paid special attention to. Also, you should definitely take into account the fact that they are often used when it is customary to work with topographic maps, or in the process of studying mountain systems. This also includes route planning, and so on.
На сайте https://stendy-razvalshozhdenia.ru вы изучите всю важную и ценную информацию о том, как правильно подобрать стенд развал-схождение, который используется в автосервисе. Вы узнаете о том, что вообще представляет собой такое устройство и чем оно примечательно. Рассматриваются виды стендов, а также нюансы оптических стендов. Дается информация о компьютерных стендах. Вы будете в курсе того, какие особенности есть у 3D стендов. Возможно, вам будут нужны инфракрасные стенды. Даны важные советы и рекомендации о том, как правильно подобрать качественное оборудование.
amoxicillin online without prescription: how much is amoxicillin prescription – amoxicillin 500mg for sale uk
Хотите по хорошей стоимости и оперативно продать свой автомобиль? У нас работают квалифицированные специалисты, имеющие большой опыт в сфере продаж. Предложим оценку вашего авто абсолютно бесплатно. Больше не нужно тратить время на утомительные поиски покупателя. Мы берем на себя все организационные вопросы. Ищете быстро выкуп автомобилей? Cars16.ru – сайт, где вы сможете более подробную информацию отыскать. Дорожим нашими клиентами и подбираем особый подход. Совершаем расчет удобным способом. Гарантируем прозрачные сделки. Свяжитесь с нами, чтобы обсудить детали. Будем рады вам помочь!
Привет!
Заказать диплом университета.
share.psiterror.ru/2024/06/16/poluchite-diplom-v-lyuboe-vremya.html
Удачи!
Привет!
Мы готовы предложить документы техникумов, расположенных на территории всей Российской Федерации. Вы можете приобрести качественно сделанный диплом от любого заведения, за любой год, в том числе документы СССР. Документы выпускаются на “правильной” бумаге высшего качества. Это позволяет делать настоящие дипломы, которые невозможно отличить от оригинала. Документы заверяются всеми требуемыми печатями и подписями.
http://www.ccde-cambodia.com/cb-profile/pluginclass/cbblogs.html?action=blogs&func=show&id=124
http://amoxildelivery.pro/# amoxicillin cephalexin
Здравствуйте!
Где приобрести диплом по необходимой специальности?
Заказать диплом любого ВУЗа.
cbr.by/club/user/1977/blog/316/
Привет, друзья!
Официальная покупка диплома вуза с сокращенной программой обучения в Москве
http://www.hhicecream.com/2024/06/речной-диплом-купить/
Find medication facts. Access medication facts.
ed pills online
Medication trends described. Drug specifics here.
Привет, друзья!
Как получить диплом о среднем образовании в Москве и других городах
http://www.cetprocapci.com/inicio/uncategorized/купить-диплом-кассира/
Привет!
Заказать документ ВУЗа вы сможете у нас.
diploms-x24.ru/kupit-diplom-krasnoyarsk
Здравствуйте!
Приобрести диплом любого университета.
catmu.mybb.ru/viewtopic.php?id=405#p664
Успехов в учебе!
Здравствуйте!
Заказать документ о получении высшего образования можно в нашей компании в столице.
diplomyx.com/kupit-diplom-nizhnij-novgorod
На сайте https://santeh.club изучите весь каталог товаров, которые предлагает интернет-магазин «Сантех Клуб». Для того чтобы подобрать лучший вариант, используйте специальный поиск. Доставка осуществляется в любой регион и максимально оперативно. В разделе вы найдете качественные ванны, унитазы, выполненные из высокотехнологичных и качественных материалов, полотенцесушители и многое другое. Все изделия от ведущих производителей. Регулярно проходят акции, чтобы сделать вашу покупку более привлекательной.
Добрый день!
Заказать документ ВУЗа можно у нас в столице.
ast-diplomy24.ru/kupit-diplom-nizhnij-novgorod
Успехов в учебе!
1newss.com
Здравствуйте!
Заказать документ института вы сможете в нашей компании в столице.
ast-diplomy.com/kupit-diplom-rostov-na-donu
Удачи!
Здравствуйте!
Сколько стоит диплом высшего и среднего образования и как его получить?
landik-diploms-srednee.ru/svidetelstvo-o-rozhdenii
Привет!
Где купить диплом специалиста?
Мы можем предложить документы ВУЗов, которые находятся в любом регионе Российской Федерации. Можно купить диплом за любой год, включая документы старого образца СССР. Дипломы печатаются на бумаге высшего качества. Это дает возможность делать государственные дипломы, которые невозможно отличить от оригинала. Документы будут заверены необходимыми печатями и штампами.
Мы можем предложить дипломы любых профессий по приятным ценам.
asxdiplomik24.ru/kupit-diplom-sankt-peterburg
Рады помочь!
Привет!
Купить документ ВУЗа можно в нашей компании.
ast-diplomas.com/kupit-diplom-sankt-peterburg
Успехов в учебе!
Features and Benefits
ivermectin price
Medicine facts here. Brand names listed.
buy ed pills usa
Drug facts provided. Drug info here.
https://ciprodelivery.pro/# cipro for sale
Здравствуйте!
Покупка диплома о среднем полном образовании: как избежать мошенничества?
landik-diploms-srednee.ru/diplom-bakalavra
Привет, друзья!
Покупка диплома о среднем полном образовании: как избежать мошенничества?
bvf.ru/forum/showthread.php?p=25249323#post25249323
Будем рады вам помочь!
tzona.org
лучшее бесплатное порно 2024 [url=http://www.best-free-porno.ru]http://www.best-free-porno.ru[/url] .
Всем привет! Подскажите, где найти разные блоги о недвижимости? Сейчас читаю https://glatt-nsk.ru
Здравствуйте!
Легальная покупка диплома о среднем образовании в Москве и регионах
obshenie.flybb.ru/viewtopic.php?f=2&t=687
Поможем вам всегда!
Paxlovid over the counter: paxlovid pill – paxlovid pill
На сайте https://balansirovochnye-stanki.ru изучите информацию про балансировочный станок. Так вы узнаете про то, какие достоинства у конструкций марки Sivik. Вы сможете ознакомиться с балансировочными станками, которые используются на различных видах машин. Также узнаете и про самые высокотехнологичные методики балансировки колес. На все товары даются гарантии качества. Оборудование является надежным, функциональным и уникальным. Кроме того, отличается безупречными эксплуатационными сроками.
In addition to the obvious advantages in a decorative sense, there are other advantages stroynews.info
Привет, друзья!
Наши специалисты предлагают выгодно и быстро приобрести диплом, который выполняется на бланке ГОЗНАКа и заверен печатями, штампами, подписями должностных лиц. Документ способен пройти любые проверки, даже при помощи специфических приборов. Решите свои задачи быстро и просто с нашим сервисом.
http://www.superstitionism.com/forum/profile.php?id=1393264
Успехов в учебе!
The Aviator Game traces its roots back to the early days of online gambling when developers sought to create
buy ivermectin
Привет, друзья!
Где заказать диплом по нужной специальности?
Мы предлагаем документы институтов, расположенных на территории всей РФ. Можно приобрести диплом от любого заведения, за любой год, указав подходящую специальность и оценки за все дисциплины. Дипломы печатаются на бумаге высшего качества. Это позволяет делать настоящие дипломы, не отличимые от оригиналов. Документы будут заверены всеми обязательными печатями и штампами.
Мы готовы предложить дипломы любых профессий по приятным тарифам.
ast-diplomy.com/kupit-diplom-vracha
Поможем вам всегда!
Привет, друзья!
Мы предлагаем заказать диплом в отличном качестве, неотличимый от оригинального документа без участия специалиста высокой квалификации со специальным оборудованием.
автолнр.рф/users/otyqux
Успехов в учебе!
Смотреть фильм https://hdrezka.host/ онлайн любого года выпуска, в том числе новинки 2024 года, в отличном качестве, без регистрации у нас на сайте. Подборки по всем жанрам, ТОПы фильмов за все годы, коллекции любых видов и жанров. Лучшие из выбора зрителей – вы найдете все для приятного времяпрепровождения.
Здравствуйте!
Мы предлагаем документы техникумов, расположенных в любом регионе Российской Федерации. Вы сможете приобрести диплом от любого учебного заведения, за любой год, указав актуальную специальность и оценки за все дисциплины. Дипломы и аттестаты печатаются на “правильной” бумаге самого высшего качества. Это позволяет делать государственные дипломы, не отличимые от оригиналов. Они заверяются всеми требуемыми печатями и штампами.
wo.linyway.com/read-blog/3414
Comprehensive pill resource. Drug information here.
buy ed meds pills
Comprehensive pill guide. Pill information available.
Здравствуйте!
Мы предлагаем выгодно и быстро заказать диплом, который выполнен на оригинальной бумаге и заверен печатями, штампами, подписями официальных лиц. Диплом пройдет любые проверки, даже с применением профессиональных приборов. Достигайте цели быстро и просто с нашим сервисом.
dom-nam.ru/index.php/forum/stroitelnye-kompanii/50337-kupit-diplom#81222
Хорошей учебы!
plane ascends, the higher the multiplier. For example, if you bet $10 and cash out at a 2x multiplier, you win
ivermectin price
100RENT.BY – ведущая онлайн-платформа для аренды строительной и специальной техники, оборудования в разных регионах Беларуси. Наша основная цель – сделать взаимодействие между арендодателями и арендаторами в строительной сфере более результативным. Ищете газонокосилка бензиновая аренда минск? 100rent.by – сайт, где представлена детальная информация о нас, ознакомиться с ней можете прямо сейчас. Мы создали новейший и простой интерфейс для удобства публикования и поиска объявлений. Гарантируем мгновенную регистрацию и предоставляем гибкие тарифы. Всегда рады вам!
Ремстройсервис – достойная компания. Успех ее вызван высочайшим качеством осуществления работ, соответствием новейшим требованиям в отделке, выборе чистых экологических материалов и планировке. Реализованы специальные программы для того, чтобы было несложно приобрести по доступным ценам свое жилье. https://rss48.ru – сайт, где вы найдете больше информации о нас, ознакомиться с ней можете прямо сейчас. При возникновении каких-либо вопросов, смело обращайтесь к нам. Мы всегда готовы вас проконсультировать. Ремстройсервис – живите по-новому!
I love your blog. It looks every informative.
Добрый день!
Мы предлагаем дипломы любых профессий по невысоким тарифам.
russiajoy.ru/oformlenie-diploma-onlayn-za-neskolko-shagov
https://clomiddelivery.pro/# order generic clomid tablets
While the game itself is free to access, playing involves placing bets with real money. Some platforms may offer
cost of ivermectin
В сериале “Фоллаут”, представленном на сайте https://fallout-tvseries.com/ мы видим расширение вселенной Fallout, где зрителю предлагается исследовать уникальный лабиринт коридоров и атриумов, а не строго разделенные этажи и уровни. Волт-Тек, корпорация, ответственная за уничтожение НКР, планирует восстановить цивилизацию и получить монополию над Америкой. Убежища, такие как Убежище 31, содержат криокапсулы с менеджерами Волт-Тек, которые будут управлять постъядерной Америкой. Сериал также демонстрирует обычных домашних курочек, переживших ядерную войну без изменений.
Stumbled upon an interesting article – I suggest you take a look http://www.fcviktoria.cz/media_show.asp?id=2924&id_clanek=2467&media=0&type=1&url=https://www.blogtalkradio.com/humansywzc
На сайте https://yogatot.ru/ запишитесь в студию йоги. Здесь самые разные практики, включая хатха-йогу, йогатерапию, аэройогу. Все практики максимально полезны для души и тела. Они помогают расслабиться, получить гармонию с собой и окружающим миром. В студиях царит приятная атмосфера, все настроено на получение ярких, приятных эмоций. Вы сразу же почувствуете, что настроение улучшилось, появилось умиротворение. Также всем желающим доступна и «горячая йога», которая проходит в теплом, уютном зале.
На сайте https://profmosreshetka.ru вы сможете получить всю необходимую информацию, которая касается заказа решеток на окна. Все конструкции выполняются из качественных, современных материалов. А замер, доставка решений осуществляются абсолютно бесплатно. С расценками ознакомьтесь прямо сейчас. Все цены снижены до конца июля, а потому спешите воспользоваться услугами прямо сейчас. Компания отличается большим опытом работы – более 10 лет. А если закажете 2 решетки, то вам будет предоставлена скидка в 20%.
Зайдите на сайт Научно-технического центра «Триада» https://triadacompany.ru/ который помогает тысячам предприятий обеспечивать промышленную и экологическую безопасность по всей России! Лучшие кадры, инновационный подход, опыт с 1991 года. Промышленная и экологическая безопасность, экспертиза, проектирование, консалтинг. Подробнее на сайте.
Привет!
Купить документ ВУЗа можно в нашей компании.
diplomyx.com/kupit-diplom-chelyabinsk
Patient drug facts. Brand names listed.
buy ed pills online without prescription
Get drug details. Latest medication developments.
Привет, друзья!
Приобрести документ о получении высшего образования вы сможете в нашем сервисе.
ast-diplomy.com/kupit-diplom-o-vysshem-obrazovanii
Discovered a unique article – recommended to acquaint yourself! https://www.blogtalkradio.com/ipennyibte
of chance and strategy. Unlike traditional casino games, the Aviator Game involves a virtual plane that ascends
ivermectin for sale
Привет!
Купить документ университета вы имеете возможность в нашей компании в Москве.
diplomyx24.ru/kupit-diplom-ekaterinbur
Успешной учебы!
Привет!
Мы изготавливаем дипломы любой профессии по приятным тарифам. Стоимость может зависеть от конкретной специальности, года получения и образовательного учреждения. Всегда стараемся поддерживать для заказчиков адекватную политику цен. Важно, чтобы дипломы были доступными для большинства граждан.
prikol100500.ru/poluchite-diplom-po-vashim-trebovaniyam-zakazhite-pryamo-seychas
[u][b] Здравствуйте![/b][/u]
[b]Мы изготавливаем дипломы[/b] любой профессии по приятным ценам.
[url=http://www.bytovymagazin.cz/купить-диплом-колледжа-весь//]www.bytovymagazin.cz/купить-диплом-колледжа-весь/[/url]
Привет!
Купить документ о получении высшего образования можно у нас в столице.
ast-diploms.com/kupit-diplom-krasnoyarsk
Успехов в учебе!
лучшее порево бесплатно лучшее порево бесплатно .
Привет!
Заказать документ института вы имеете возможность у нас.
ast-diplomy.com/kupit-diplom-specialista
radioshem.net
На сайте https://diagnosticheskie-skanery.ru получите полную и исчерпывающую информацию, связанную с диагностическими автомобильными сканерами. Вы узнаете то, для чего они предназначены, как используются. Рассматриваются и виды диагностических сканеров. Имеются универсальные, автомобильные. Изучите подробную информацию о том, как правильно подобрать подобное оборудование, на что лучше полагаться. Также есть данные и о том, от чего зависит качество, расценки, представлены самые известные модели, которые точно заинтересуют.
Здравствуйте!
Купить диплом любого ВУЗа.
alex-neil.ru/index.php/cb-profile/pluginclass/cbblogs?action=blogs&func=show&id=233
buy amoxicillin: buy amoxicillin 500mg online – how to get amoxicillin over the counter
Medication trends described. Pill info available.
buy generic ed pills
Latest pill trends. Pill impacts explained.
Добрый день!
Приобрести диплом о высшем образовании.
allnewstroy.ru/vyisokokachestvennyie-diplomyi-na-zakaz
Are There Any Costs Involved?
cheap ivermectin
Привет, друзья!
Удивительно, но купить диплом кандидата наук оказалось не так сложно
jordirocas.com/node/3383
Всегда вам поможем!.
Здравствуйте!
Удивительно, но купить диплом кандидата наук оказалось не так сложно
bbs.heyshell.com/forum.php?mod=viewthread&tid=28327&extra=
Рады оказаться полезными!
http://clomiddelivery.pro/# can i order cheap clomid without rx
Your System – лучший надежный партнер для вас в сфере оборудования для видеонаблюдения. Предлагаем широкий ассортимент высококачественной продукции. Работаем только с проверенными производителями. Стараемся клиентам обеспечить индивидуальный подход и высочайший уровень обслуживания. Ищете система интеллектуального видеонаблюдения? Y-ss.ru – сайт, где есть возможность приобрести по доступным ценам охранные системы. Доставим ваш заказ в любую точку России. Мы работаем для вас без выходных. С радостью подскажем, как сделать процесс покупок простым. Свяжитесь с нами любым способом.
Привет!
Как приобрести аттестат о среднем образовании в Москве и других городах
beijingpal.com/read-blog/919
Всегда вам поможем!
Здравствуйте!
Где заказать диплом специалиста?
Приобрести диплом любого университета.
http://www.easyinsurancehub.co.uk/forum/thread-54671.html
Привет!
Официальная покупка диплома ПТУ с упрощенной программой обучения
ashinova.ru/category-5/t-1525.html#1525
Окажем помощь!.
Effective Strategies for Beginners
ivermectin buy
Привет!
Где и как купить диплом о высшем образовании без лишних рисков
uebkameri.listbb.ru/posting.php?mode=post&f=2&sid=5a702b544add604d13cc9c3a155aed20
Будем рады вам помочь!
Добрый день!
Мы предлагаем документы техникумов, расположенных на территории всей РФ. Вы можете заказать качественный диплом за любой год, включая документы старого образца СССР. Дипломы и аттестаты печатаются на “правильной” бумаге самого высокого качества. Это дает возможности делать настоящие дипломы, которые невозможно отличить от оригинала. Документы будут заверены необходимыми печатями и подписями.
dj-club-sf.mn.co/posts/61838308
На сайте https://telezghki-instrument.ru ознакомьтесь с информацией о том, какую тележку, предназначенную для инструментов, лучше выбрать и купить. Перед вами типы такого оборудования, а также достоинства и особенности каждого типа. Так вы узнаете все необходимое о тележках с ящиками, открытых тележках, о правилах выбора инструментальной тележки. Здесь вы найдете самые ценные, увлекательные и содержательные рекомендации, которые действительно будут вам полезны. Имеются данные и про материал изготовления и многое другое.
купить диплом о среднем образовании в санкт петербурге diploms-x.com .
Добрый день!
Как правильно приобрести диплом колледжа или ПТУ в России, важные моменты
cnktdshanoi.com.vn/речной-диплом-купить/
Добрый день!
Где заказать диплом по нужной специальности?
Приобрести диплом ВУЗа.
ttartisan.ru/forum/user/4353/
Key Developers and Companies Involved
cost of ivermectin
Привет, друзья!
Приобретение диплома ПТУ с сокращенной программой обучения в Москве
africastudygate.com/купить-диплом-тогу/
цена диплома цена диплома .
http://ciprodelivery.pro/# ciprofloxacin order online
Fair Play Policies and RNG
ivermectin online
Increased sales. High-quality customer 360o.info service stimulates additional sales. The average check increases, sales volume increases.
Models of hydraulic motors with a working volume of up to 400 and 1000 cubic cm are considered basic mmo5.info
Здравствуйте!
Мы изготавливаем дипломы психологов, юристов, экономистов и других профессий.
woaibanli.com/диплом-купить-ветеринария/
Поможем вам всегда!.
order norfloxacin generic – buy norfloxacin without prescription buy generic confido online
Всё о покупке аттестата о среднем образовании: полезные советы
ast-diplomy24.ru/kupit-diplom-vracha
Добрый день!
Купить документ о получении высшего образования вы сможете у нас.
diploms-x.com/kupit-diplom-nizhnij-novgorod
Успехов в учебе!
В Нижнем Новгороде Тех-Профи предлагает профессиональный ремонт квадрокоптеров с использованием оригинальных запчастей. У нас большой склад запасных частей и возможность ремонта в тот же день. Доверьтесь нашим квалифицированным инженерам и наслаждайтесь бесплатной диагностикой и курьерской доставкой.
buy doxycycline online without prescription: purchase doxycycline 100mg – doxycycline online canada without prescription
Ensuring Safe Gaming Practices
ivermectin for sale
Привет!
Купить документ университета можно в нашей компании.
diplomasx24.ru/kupit-diplom-o-srednem-obrazovanii
Хорошей учебы!
На сайте https://autoclub78.ru вы найдете интересные, практичные советы для тех, у кого есть автомобиль. Имеются практические рекомендации, ценные советы, которые помогут найти оптимальный вариант для того, чтобы правильно эксплуатировать технику. Статьи ответят на многочисленные вопросы, подскажут, как правильно действовать в определенной ситуации. Есть информация про самые востребованные мотоциклы, а также запчасти, которые реализуются на маркетплейсах. Есть информация и про то, как не стоит приобретать стеклоомывающую жидкость.
АКСИОНТ – компания, которая успешно 100 проектов на платформе «1С:ERP Предприятие 8» выполнила. Она по реализации проектов на базе «1С:ERP Управление предприятием 2» вошла в десятку лидеров. На официальном портале 1С вы найдете проекты компании. https://axiont.ru – здесь можете прямо сейчас оставить заявку. Укажите в необходимых полях свое имя и номер телефона, после чего нажмите на «Отправить». На достигнутом мы не останавливаемся: принимаем участие в выставках и внедряем новые технологии. Также для предпринимателей проводим мероприятия.
диплом об окончании класса купить diploms-x.com .
Добрый день!
Заказать документ о получении высшего образования
ast-diploms24.ru/kupit-diplom-moskva
Just wish to say your article is as amazing. The clarity in your post is simply spectacular and i could assume you are an expert on this subject. Fine with your permission let me to grab your RSS feed to keep up to date with forthcoming post. Thanks a million and please continue the rewarding work.
https://thetvdb.plex.tv/movies/real-gangsters
Здравствуйте!
Как купить диплом о высшем образовании с минимальными рисками
arusak-diploms-srednee.ru/kupit-diplom-sssr В
enjoyable.
cost of ivermectin
Всё, что нужно знать о покупке аттестата о среднем образовании
ast-diploms24.ru/kupit-diplom-moskva
Came across an interesting article, I propose you have a look https://salda.ws/f/topic.php?f=8&t=74458#post_188029
Drug details provided. Medication pamphlet available.
purchase sumatriptan
Medicine resource available. Comprehensive pill overview.
Hi there colleagues, how is all, and what you would like to say regarding this paragraph, in my view its in fact awesome designed for me.
leebet casino
https://clomiddelivery.pro/# buy cheap clomid
Привет, друзья!
Как не стать жертвой мошенников при покупке диплома о среднем полном образовании
newsofmebel.ru/legkiy-sposob-poluchit-diplom-nadezhno-i-konfidentsialno
Окажем помощь!
Добрый день!
Заказать диплом ВУЗа.
net4women.ru/blogs/3470/????????-??????????-???????????-??????-??????-???????
Успешной учебы!
рюкзак тканевый
На https://musify.su/ скачать музыку в мп3. Скачать песню или слушать онлайн бесплатно в mp3 на телефон 2024. Перед скачиванием трек можно послушать в хорошем качестве в режиме онлайн на. Здесь Вы можете скачать песню бесплатно и слушать онлайн по прямой ссылке на телефоне или планшете без регистрации! Слушайте треки в хорошем качестве 320 kbps на Android, iphone и пк без ожидания в любое время.
рюкзак
рюкзак для гимнастики
Привет!
Быстрая схема покупки диплома старого образца: что важно знать?
hobby-svarka.ru/viewtopic.php?f=11&t=6226&sid=62f0b1e91865471b778323cb7001c632
Будем рады вам помочь!
how to get realtor license in ny [url=https://realestatelicensengdfdgh.com/states/arizona-real-estate-license/]realestatelicensengdfdgh.com/states/arizona-real-estate-license/[/url] obtain real estate license realestatelicensengdfdgh.com/states/florida-real-estate-license/ .
рюкзак водонепроницаемый
ранец с замком
Variety: Access to a wide range of betting options and gameplay modes.
ivermectin online
рюкзак спортивный
классное порево видео http://www.klassny-sex.ru/ .
Привет, друзья!
Купить документ института можно в нашей компании в столице.
ast-diplom.com/kupit-diplom-chelyabinsk
Ищите торговлю бинарными опционами? Зайдите на сайт https://binrm.online/ и получите доступ к торговле более 100 мировыми торговыми активами. Узнайте больше о наших преимуществах Binarium – быстрые выводы, круглосуточная торговля, мгновенная поддержка, а также все о нашем приложении для любых мобильных устройств.
рюкзак черный
рюкзак школьный
На сайте https://olato.ru вы найдете ванны, комплектующие, а также душевые кабины, различные ограждения, биде, унитазы, инсталляции и многое другое. Регулярно появляются лучшие предложения, которые помогут изрядно сэкономить и получить желаемую вещь. Перед вами только продукция надежных, популярных брендов, которые гарантируют безупречное качество. Именно поэтому продукция является износостойкой и прослужит очень долго. Все товары реализуются по привлекательной цене, действуют распродажи.
Добрый день!
Где приобрести диплом по актуальной специальности?
http://www.vevioz.com/read-blog/159528
На сайте https://geointellect.com ознакомьтесь с особенностями таких важных и полезных услуг, как геоаналитика, геомаркетинг. Так вы сможете получить информацию о местоположении людей, важных объектов, получите данные обо всех городах России. Полученная информация позволит лучше и быстрее сориентироваться по поводу того, где выгодней построить объект. А для того, чтобы получить исчерпывающую информацию и иметь представление об услугах, изучите любопытное видео. Компания уже открыла офисы и во множестве других стран.
городской рюкзак
Ищите аренду авто в Крыму? Зайдите на сайт https://rentalcar82.ru/ и вы сможете арендовать авто в Крыму во всех городах и поселках Республики Крым. Прокат машин в Крыму посуточно без водителя, недорого с подачей в аэропорт Симферополь и другие города и поселки, бронирование автомобилей онлайн круглосуточно.
Drug specifics here. Pill guide available.
order imitrex
Patient drug guide. Dosing guidelines here.
Привет, друзья!
Мы готовы предложить документы техникумов, которые находятся на территории всей Российской Федерации. Можно приобрести качественный диплом за любой год, указав необходимую специальность и оценки за все дисциплины. Дипломы и аттестаты выпускаются на “правильной” бумаге высшего качества. Это дает возможность делать государственные дипломы, не отличимые от оригиналов. Они будут заверены всеми требуемыми печатями и подписями.
ozoms.com/read-blog/514
Скачать фильм на телефон https://kinoman.pw/ для просмотра офлайн на сайте. Самая большая коллекция фильмов для телефона, планшета. Качай, чтобы смотреть в дороге или там, где удобно. Отличное качество, малый вес фильмов, сериалов, мультиков, при высоком качестве – все то что вы найдете на сайте.
Discovered an intriguing article, I recommend you to check it out http://frienddo.com/out.php?url=https://dpaste.com/BTGW77V9G-preview
can also help in making informed cash-out decisions.
ivermectin purchase online
Привет, друзья!
Приобрести документ университета можно в нашей компании.
ast-diplomas.com/kupit-diplom-s-registraciej
Здравствуйте!
Мы готовы предложить документы ВУЗов, которые находятся на территории всей России. Можно купить качественно сделанный диплом от любого заведения, за любой год, указав необходимую специальность и оценки за все дисциплины. Дипломы и аттестаты печатаются на “правильной” бумаге самого высокого качества. Это позволяет делать настоящие дипломы, которые не отличить от оригиналов. Они заверяются необходимыми печатями и штампами.
upuge.com/read-blog/32110_legko-zakazyvaem-diplom-v-izvestnom-magazine-russian-diplom.html
Привет, друзья!
Мы можем предложить дипломы любой профессии по приятным тарифам.
allsportime.ru/oformite-diplom-onlayn-za-neskolko-minut
219news.com
Диплом пту купить официально с упрощенным обучением в Москве
diploms-x24.ru/kupit-diplom-krasnoyarsk
investnews24.net
На сайте https://verstaki-slesarnye.ru изучите информацию о том, где приобрести слесарный верстак по доступной и привлекательной стоимости. На этом сайте вы узнаете о видах слесарных верстаков, технических характеристиках и другую дополнительную информацию. Также даются ценные рекомендации о том, как правильно подобрать такое оборудование. Вы узнаете о том, почему выгодно приобрести такую технику и какую пользу вы от этого получите. Если и вы задумались о покупке, то положитесь на эти ценные рекомендации.
http://ciprodelivery.pro/# ciprofloxacin over the counter
plane ascends, the higher the multiplier. For example, if you bet $10 and cash out at a 2x multiplier, you win
cost of ivermectin
order norfloxacin – how to get eulexin without a prescription cheap confido for sale
cheap amoxicillin 500mg: buy amoxicillin 500mg canada – amoxicillin without a prescription
Скачать фильмы торрент https://torrentium.net/ в хорошем качестве бесплатно. Здесь представлены лучшие фильмы 2024 года, скачать бесплатно которые можно прямо сейчас. Сериалы Фильмы Дорамы Аниме Мультсериалы Мультфильмы и многое другое.
Привет, друзья!
Где купить диплом специалиста?
Приобрести диплом о высшем образовании.
http://www.import-moto.com/users/88
The Aviator Game boasts several unique features that set it apart from other online casino games:
cheap ivermectin
Привет!
Купить документ ВУЗа можно в нашей компании в столице.
asxdiplomik24.ru/kupit-diplom-omsk
Удачи!
топовые порно видео http://www.apteka-porno.ru .
Привет!
Купить документ о получении высшего образования вы имеете возможность в нашем сервисе.
diploms-x24.ru/kupit-diplom-rostov-na-donu
Успехов в учебе!
Добрый день!
Заказать диплом любого университета.
site2.liodiz.ru/2024/07/04/shirokiy-vybor-dokumentov-v-znamenitom-onlayn-magazine.html
Здравствуйте!
Где приобрести диплом по нужной специальности?
Заказать диплом о высшем образовании.
forum-pravo.com.ua/member.php?u=10249
Since its inception, the Aviator Game has undergone numerous updates and enhancements. Technological
ivermectin purchase online
порно коллекции бесплатно [url=porn-library.ru]porn-library.ru[/url] .
лучшая коллекция порно лучшая коллекция порно .
breakingnews77.com
Advantages of wooden gazebos, in addition to the obvious advantages in a decorative sense olympic-school.com, there are other advantages.
http://amoxildelivery.pro/# amoxicillin 500 mg tablet
Привет, друзья!
Сколько стоит диплом высшего и среднего образования и как его получить?
montrealpal.com/read-blog/918
Рады помочь!
рюкзак школьный маленький
рюкзак для путешествий для девочки
Safety and Fair Play
ivermectin buy
рюкзак мужской прочный большой
Привет, друзья!
Как оказалось, купить диплом кандидата наук не так уж и сложно
ya.forum.cool/viewtopic.php?id=5837#p17396
Окажем помощь!
Лучшие корейские автомобили | Как выбрать авто из Кореи? | Преимущества и недостатки корейских автомобилей | Пятерка лучших корейских автомобилей | За что полюбили автомобили Кореи | Топ-3 востребованных автомобиля из Кореи | Топ-7 подержанных авто из Кореи | Ценовая политика корейских автомобилей | Мифы о корейских автомобилях: разоблачение | Рейтинг SUV корейских производителей | Выбор современного кроссовера Кореи | Какой корейский автомобиль выбрать для путешествий? | Советы по выбору городского авто из Кореи | Как оценить состояние авто из Кореи перед покупкой? | Как сделать уникальным свой корейский автомобиль
купить авто в корее [url=https://avtodom63.ru/]купить авто в корее[/url] .
рюкзак женский водоотталкивающий
рюкзак для путешествий ручная кладь
Привет!
Как приобрести диплом о среднем образовании в Москве и других городах
weekofsport.ru/vash-diplom-kachestvo-i-autentichnost
рюкзак большой женский тканевый
рюкзак школьный для подростков девочек 2024
модные рюкзаки для подростков девочек
большой рюкзак для путешествий
тренд 2024 для девочек
рюкзак школьный со светоотражающими элементами
Ищите скачать фильмы на телефон https://anwap.im/ – тогда зайдите к нам. Скачивайте фильмы, сериалы, мультики прямо на телефон и смотрите, когда вам удобно. Никакой регистрации, бесплатно. Коллекции нашего сайта в любых жанрах и годов выпуска позавидует любой сайт. Все фильмы для телефона в одном месте.
ранец для старшеклассников
рюкзак школьный для подростков девочек
портфель школьный для девочек подростков 2024
Всем привет! Может кто знает, где найти полезные блоги о недвижимости? Пока нашел https://konditsioneri-shop.ru
History and Development
ivermectin price
На сайте https://singapore-company.ru/ уточните информацию относительно того, как правильно произвести регистрацию своей компании в Сингапуре. Это государство выбирают по той причине, что оно является одним из самых развитых, в нем особая инфраструктура. Компания поможет вам открыть бизнес, даст профессиональную консультацию. Здесь работают компетентные, лучшие специалисты, которые знают, как вам открыть свое дело. В разделе вы найдете данные о том, как правильно зарегистрировать предприятие и какие документы для этого понадобятся.
рюкзак для тренировок гимнастика
Ищите помощь в написании курсовых, дипломных работ, диссертаций, рефератов? Зайдите на https://spisaly.ru/ и вы найдете специалиста который поможет вам. Специалисты по различным темам к вашим услугам – доработки и консультации бесплатно, а цены наши доступны. Десятки тысяч выполненных работ и только положительная репутация. Зайдите на сайт и ознакомьтесь подробнее.
Привет, друзья!
Сколько стоит диплом высшего и среднего образования и как его получить?
avtoworld.lv/index.php?subaction=userinfo&user=utesox
Рады оказать помощь!.
Добрый день!
Мы изготавливаем дипломы психологов, юристов, экономистов и прочих профессий по доступным ценам.
http://www.bytovymagazin.cz/купить-диплом-в-дербенте/
рюкзак черный тканевый школьный
рюкзак стильный для девочек подростков
рюкзак туристический женский
If we consider the absolute height, then this is the height above sea level 214rentals.com
ранец гимнастический
amoxicillin 250 mg capsule: cheap amoxicillin 500mg – purchase amoxicillin online without prescription
рюкзак черный школьный с карманами
рюкзак для школы модные
рюкзак женский тканевый
рюкзак черный женский школьный
модный рюкзак 2024 в школу
Ищите хоккейную экипировку? Зайдите на https://first-hockey.ru/ где вы сможете выбрать из широкого ассортимента, пол лучшим ценам и купить с доставкой в интернет магазине Первый-Хоккейный: клюшки, коньки, нагрудники хоккейные, налокотники, краги, шлемы и щитки хоккейные и многое другое. Доставка по всей России.
social interaction adds a new layer of excitement and competition to the game, making it more engaging and
where to buy ivermectin
гимнастический рюкзак для гимнастики
рюкзак светоотражающий
стильный женский рюкзак
Glory Casino
рюкзак женский текстильный городской
рюкзак женская текстильная
Caspian Training Group – это хороший образовательный центр. Преподаватели вдохновляют студентов в изучении языка на достижение высочайших результатов и прекрасно преподносят материал. Учителя постоянно стремятся к самосовершенствованию и повышению своей квалификации. http://ctgroup.kz – портал, где размещены отзывы клиентов. Учить язык с нами – легко и удобно. Запишитесь уже сейчас на обучающие курсы. Можете пройти онлайн-тест, который поможет оценить ваш уровень навыков. Гарантируем современное обучение по привлекательным ценам!
рюкзак школьный однотонный
рюкзак школьный для девочки 2024
Здравствуйте!
Приобрести документ университета вы сможете в нашей компании в Москве.
diplomasx.com/kupit-diplom-bakalavra-ili-specialista
На сайте https://www.avtogalaktika.com/ оставьте сообщение, чтобы уточнить всю необходимую и важную информацию. В этой компании вы с легкостью воспользуетесь такими важными услугами, как: деньги под залог авто, выдача наличных под залог авто, займ под ПТС авто. Воспользуйтесь возможностью быстро оформить займ под залог своего автомобиля. Все документы будут подготовлены максимально оперативно, честно, на прозрачных условиях. Также можно взять деньги под залог грузового транспорта. Все максимально выгодно для вас!
ранец oxford
рюкзак женский непромокаемый
Добрый день!
Купить документ ВУЗа можно в нашей компании.
diplomyx.com/kupit-diplom-s-registraciej
На сайте https://poshnevye-kompressory.ru изучите информацию, которая касается поршневого компрессора. Вы узнаете о том, в каких случаях используется, о достоинствах применения и многом другом. Также ознакомитесь с основными характеристиками, особенностями, которые помогут правильно и быстро подобрать конструкции. Рассматриваются и виды поршневых компрессоров, даются ценные рекомендации по их выбору. Всю нужную и ценную информацию вы обязательно узнаете на этом портале. Она составлена лучшими экспертами.
Добрый день!
Купить документ о получении высшего образования вы имеете возможность у нас.
diploms-x.com/kupit-diplom-krasnoyarsk
Хорошей учебы!
рюкзак универсальный
На сайте https://mpmgr.ru воспользуйтесь специальным менеджером маркетплейсов для того, чтобы вы автоматизировали и упростили работу с такими маркетплейсами, как Ozon, Wildberries, Яндекс.Маркет. Здесь специально для вас рассчитают поставки, а также будут эффективно управлять рекламой, ответят на отзывы клиентов, отследят товары, помогут рассчитать скидку. Такая услуга сэкономит время специалистов, они смогут заняться более серьезными, ответственными делами. Происходит оптимизация расходов для вашей большей прибыли.
not, you lose your bet.
cost of ivermectin
whoah this blog is wonderful i like studying your posts. Stay up the good work! You understand, lots of people are hunting round for this info, you can help them greatly.
реристрация Dragon Money Casino
ранец футбольные
Зайдите на сайт BinTradeClub https://bintradeclub.space/ – надежного брокера бинарных опционов, который, если у вас нет опыта, начать торговлю и даст знания, в ом числе демо счет. А если вы опытный трейдер – предоставит все необходимые инструменты для выгодной торговли. Подробнее на сайте.
Добрый день!
Приобрести документ о получении высшего образования можно в нашей компании.
asxdiplomik24.ru/kupit-diplom-krasnoyarsk
Успешной учебы!
Здравствуйте!
Заказать диплом о высшем образовании.
tricityfriends.com/read-blog/540
рюкзак черный с карманами
рюкзак для фитнеса
рюкзак женский тканевый городской
Привет, друзья!
Заказать документ ВУЗа можно у нас в столице.
ast-diplom.com/kupit-diplom-kandidata-nauk
Sur Shopsy, vous pouvez trouver et acheter des vetements, des chaussures et des accessoires. Plus de 2 000 000 de produits provenant de 100 magasins sur un seul site. https://shopsy.fr/ Dans notre catalogue, vous trouverez des articles de milliers de marques originales.
рюкзак спортивный большой
Amazing! Its in fact awesome article, I have got much clear idea about from this post.
https://mustang-online.ru
Здравствуйте!
Заказать документ о получении высшего образования можно в нашей компании в столице.
diplomasx.com/kupit-diplom-vracha
Успехов в учебе!
рюкзак женский тканевый непромокаемый
Unique Features of the Aviator Game
ivermectin for sale
рюкзак вместительный
Скачать фильм https://torrentium.pro/ или смотреть онлайн. Выбор за вами. Такой коллекции вы еще не видели. Зайдите на сайт, выберите категорию или ищите то что вы знаете. Отличное качество, отсутствие регистрации, ТОПЫ фильмом, сериалов, мультфильмов. Выбор зрителей, рейтинги, любой год. Закачаны фильмы которые еще не вышли. Смотри первым.
Зайдите на сайт https://gambling-online.ru/ и вы получите возможность играть в лучшие игры с моментальным выводом средств. Бонусы за регистрацию, широкий выбор игр. Зайдите и узнайте подробнее – как зарегистрироваться, как играть, как установить на любое мобильное устройство, рейтинги онлайн игр и многое другое.
leeds-welcome.com
На сайте https://travamana.ru/ представлены ароматные, приятные травяные чаи. Они полностью натуральные, приготовлены из редких и популярных растений, трав, которые произрастают в России. В уютном магазинчике можно приобрести специи, подарки, зарядиться приятными и положительными эмоциями, ощутить радость и покой. Компетентные консультанты дадут совет, что лучше всего приобрести в каждом конкретном случае. Есть успокаивающие сборы, для иммунитета, гинекологические. Если вы подбираете подарок для близкого человека, то здесь вы найдете все самое необходимое.
dominicanrental.com
Hi, I think your website might be having browser compatibility issues. When I look at your blog in Firefox, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, awesome blog!
slot siteleri xslot
Numerous online casino platforms offer the Aviator Game. These platforms provide a secure and regulated
ivermectin purchase online
cheap clomid prices: can i buy generic clomid no prescription – how to get generic clomid
Привет!
Мы готовы предложить дипломы любой профессии по выгодным тарифам. Стоимость будет зависеть от определенной специальности, года получения и ВУЗа. Всегда стараемся поддерживать для заказчиков адекватную политику цен. Для нас очень важно, чтобы документы были доступными для подавляющей массы граждан.
bookmarkprobe.com/story17268629/купить-диплом-в-Самаре
Здравствуйте!
Мы можем предложить дипломы любой профессии по доступным ценам.
shugakukai.co.jp/диплом-в-хасавюрте/
the opportunity to compete for larger prizes and showcase their skills on a larger stage.
buy ivermectin
Здравствуйте!
Мы изготавливаем дипломы любых профессий по приятным ценам.
bankendigital.de/купить-диплом-в-ессентуки/
Discover your perfect stay with WorldHotels-in.com, your ultimate destination for finding the best hotels worldwide! Our user-friendly platform offers a vast selection of accommodations to suit every traveler’s needs and budget. Whether you’re planning a luxurious getaway or a budget-friendly adventure, we’ve got you covered with our extensive database of hotels across the globe. Our intuitive search features allow you to filter results based on location, amenities, price range, and guest ratings, ensuring you find the ideal match for your trip. We pride ourselves on providing up-to-date information and competitive prices, often beating other booking sites. Our detailed hotel descriptions, high-quality photos, and authentic guest reviews give you a comprehensive view of each property before you book. Plus, our secure booking system and excellent customer support team ensure a smooth and worry-free experience from start to finish. Don’t waste time jumping between multiple websites – http://www.WorldHotels-in.com brings the world’s best hotels to your fingertips in one convenient place. Start planning your next unforgettable journey today and experience the difference with WorldHotels-in.com!
Обеспечьте конфиденциальность с резидентскими прокси, рекомендуем этим инструментом.
Как работают резидентские прокси?, ознакомьтесь с подробностями.
Как выбрать лучший резидентский прокси, инструкция для пользователей.
Для каких целей используют резидентские прокси?, ознакомьтесь с возможностями.
Как резидентские прокси обеспечивают безопасность?, обзор функций безопасности.
Как резидентские прокси защищают от опасностей?, разберем важные аспекты.
Как резидентский прокси помогает повысить эффективность?, сравним основные плюсы.
Как улучшить скорость Интернета с резидентским прокси, советы для оптимизации работы.
Почему резидентский прокси стоит использовать для парсинга, обзор возможностей для парсеров.
Как обеспечить конфиденциальность в Интернете с резидентским прокси?, рекомендации к безопасности онлайн.
Секреты эффективной работы в соцсетях с резидентским прокси, подробный обзор функционала.
Какие преимущества дает аренда резидентских прокси, проанализируем лучшие варианты.
Способы защиты от DDoS с помощью резидентского прокси, подробно изучим меры безопасности.
Какие преимущества привлекают пользователей к резидентским прокси?, проанализируем основные факторы.
Какие прокси лучше: резидентские или дата-центры?, советы для выбора.
сервис резидентных прокси https://rezidentnieproksi.ru/ .
Здравствуйте!
Мы изготавливаем дипломы любой профессии по приятным тарифам.
androidinweb.ru/diplomyi-ot-luchshih-obrazovatelnyih-uchrezhdeniy
портфель школьный для девочки
классический рюкзак
рюкзак 2024 для девочки водонепроницаемый
winnings.
ivermectin buy online
рюкзак универсальный с карманами
рюкзак для ноутбука
рюкзак для мамочек
На сайте https://thailand-company.ru/ вы узнаете о том, как правильно открыть компанию в Таиланде и какие ресурсы необходимо для этого использовать. При этом владелец компании в Таиланде может быть с любым гражданством. К важным преимуществам открытия бизнеса в Таиланде относят то, что здесь всегда растущий рынок, а регистрация не требует большого количества документов и не занимает много времени. Компания, которая зарегистрирована в Таиланде, идеальна для ведения международного бизнеса. На сайте вы узнаете и о самом процессе регистрации.
Добрый день!
Приобрести диплом ВУЗа.
glowsubs.ru/forum/topic/add/forum2/#postform
Хорошей учебы!
рюкзак из ткани оксфорд
подъем дома
замена венцов
Ищите видеонаблюдение https://rusnet.online/ под ключ с онлайн-просмотром? Зайдите на сайт и вы сможете заказать установку: видеонаблюдение для дома, видеонаблюдение в офис, видеонаблюдение для склада, видеонаблюдение для магазина и многое другое. Работают профессионалы, вся продукция на складе. Быстрый выезд на объект заказчика, согласование, установка. Лучшие цены на рынке. Подробнее на сайте.
ремонт фундамента
подъем дома
africanownews.com
замена венцов
birminghamnews24.com
ремонт фундамента
подъем дома
Привет!
Приобрести документ института можно в нашей компании.
ast-diplomas.com/otzyvy
Успехов в учебе!
Features and Benefits
ivermectin buy
замена венцов
подъем дома
Добрый день!
Заказать документ о получении высшего образования вы можете в нашей компании в столице.
ast-diplomy24.ru/kupit-diplom-moskva
Успехов в учебе!
подъем дома
Привет!
Купить диплом о высшем образовании.
galantclub.od.ua/member.php?u=15983
Хорошей учебы!
coindarwin web3 academy
The Unseen Story Regarding Solana’s Originator Toly Yakovenko’s Accomplishment
Post Two Portions of Java plus a Ale
Yakovenko, the visionary the brainchild behind Solana, initiated his quest with an ordinary habit – coffee and beer. Unaware to him, these occasions would set the gears of fate. Today, Solana remains as a powerful contender in the crypto realm, featuring a market cap in the billions.
Ethereum ETF First Sales
The Ethereum ETF just started with a staggering trading volume. This milestone event saw several spot Ethereum ETFs from several issuers begin trading on U.S. markets, injecting unseen activity into the typically steady ETF trading space.
SEC Approved Ethereum ETF
The U.S. SEC has sanctioned the spot Ethereum ETF to be listed. As a digital asset with smart contracts, Ethereum is expected to deeply influence the digital currency industry following this approval.
Trump’s Bitcoin Strategy
As the election draws near, Trump presents himself as the “Crypto President,” repeatedly showing his support for the cryptocurrency industry to gain voters. His method varies from Biden’s method, targeting the attention of the crypto community.
Musk’s Influence on Crypto
Elon Musk, a prominent figure in the cryptocurrency space and a backer of Trump’s agenda, stirred things up yet again, driving a meme coin connected to his actions. His engagement continues to influence market trends.
Binance Developments
Binance’s subsidiary, BAM, is now allowed to invest customer funds in U.S. Treasuries. Additionally, Binance observed its seventh year, emphasizing its journey and achieving multiple compliance licenses. Simultaneously, the firm also made plans to remove several major crypto trading pairs, altering the market landscape.
AI and Economic Trends
Goldman Sachs’ top stock analyst recently observed that AI is unlikely to cause a revolution in the economy
замена венцов
замена венцов
замена венцов
подъем дома
конференц зал под ключ конференц зал под ключ .
ремонт фундамента
подъем дома
На сайте https://ustanovki-zapravki.ru вы узнаете о том, какую установку для того, чтобы заправить автокондиционер, лучше всего выбрать. Ознакомитесь с преимуществами, а также отрицательными сторонами ручных установок, которые используются для заправки устройств. Также рассматриваются и дополнительные функции, которые крайне необходимы вам. Даются ценные советы, которые помогут быстрее подобрать устройство в соответствии с потребностями компании. Рассматриваются особенности применения профессионального оборудования.
Защитите свои данные с помощью резидентских прокси, преимущества.
Получите доступ к контенту из других стран с резидентскими прокси, радуйтесь контентом.
Получите быстрый и надежный интернет с резидентскими прокси, как это работает.
Защитите свои учетные данные и личную информацию с резидентскими прокси, и будьте уверены в своей безопасности.
Сделайте свои онлайн-активности невидимыми благодаря резидентским прокси, и оставайтесь незамеченными.
Обходите цензуру и блокировки с резидентскими прокси, и не опасайтесь за свою приватность.
качественные резидентские прокси https://rezidentnie-proksi.ru/ .
замена венцов
ремонт фундамента
Place Your Bet: Choose the amount you want to bet.
ivermectin purchase
ремонт фундамента
замена венцов
лучшие капперы в телеграмме лучшие капперы в телеграмме .
замена венцов
подъем дома
подъем дома
замена венцов
ремонт фундамента
На сайте https://travel-anapa.ru/ подберите для себя экскурсию в Анапе. Вы сможете воспользоваться как семейными, так и индивидуальными предложениями. Закажите трансфер на экскурсионный объект. И самое главное, что экскурсионная программа обойдется вам недорого. Изучите все экскурсии, которые вы сможете заказать прямо сейчас. Напротив каждого предложения указана и стоимость, а также описание маршрута. Для наглядности имеется фотография. Можно выбрать винные экскурсии, с детьми, вечерние, исторические, на весь день.
подъем дома
подъем дома
замена венцов
замена венцов
На сайте https://proxyelite.biz/ вы найдете элитные анонимные прокси, которые вы сможете использовать в своих целях. Перед вами только надежные, быстрые сервера, которые обязательно необходимо приобрести каждому. Перед покупкой пройдите тест на 60 минут. Все прокси развернуты на собственном оборудовании, а потому они надлежащего качества. Каждый клиент будет приятно удивлен скорости серверов. Работает и служба поддержка, которая обязательно ответит на все интересующие вопросы. Подберите подходящий для себя пакет, чтобы не переплачивать.
Watch the Plane Ascend: The plane takes off and starts climbing.
ivermectin purchase
ремонт фундамента
подъем дома
замена венцов
ремонт фундамента
замена венцов
ремонт фундамента
замена венцов
замена венцов
Здравствуйте!
Заказать документ о получении высшего образования вы можете в нашем сервисе.
ast-diploms.com/kupit-diplom-perm
подъем дома
ремонт фундамента
Привет, друзья!
Мы можем предложить дипломы любой профессии по выгодным тарифам.
linestudio.net/купить-диплом-онлайн/
ремонт фундамента
замена венцов
Common mistakes to avoid in the Aviator Game include:
cost of ivermectin
замена венцов
ремонт фундамента
Добрый день!
Где приобрести диплом специалиста?
my.omsystem.com/members/anthonyjoseph
замена венцов
ремонт фундамента
подъем дома
mosesolmos.com
ремонт фундамента
angliannews.com
подъем дома
подъем дома
Скачать музыку https://shazam.pw/ в один клик в mp3 на сайте. Легкий поиск, огромная коллекция. Лучшие хиты, лучшие песни, лето 2024, подборки в авто, для машины, для луши, для отдыха, для тренировок. Релакс музыка, клубняк скачать, бодрая музыка, музыка с басами, лирические песни и много другое на сайте.
ремонт фундамента
подъем дома
Привет!
Мы изготавливаем дипломы любой профессии по приятным тарифам.
rsn360.ru/blogs/427/¬аш-?иплом- ачество-и-ѕодлинность
ремонт фундамента
замена венцов
подъем дома
ремонт фундамента
Online Communities and Forums
buy ivermectin
замена венцов
подъем дома
подъем дома
подъем дома
замена венцов
замена венцов
ремонт фундамента
Здравствуйте!
Приобрести документ о получении высшего образования
diploms-x24.ru/otzyvy
подъем дома
подъем дома
ремонт фундамента
ремонт фундамента
สล็อตเว็บตรง
Register an account, make a deposit, and navigate to the Aviator Game to start playing.
ivermectin cheap
подъем дома
подъем дома
ремонт фундамента
On the website https://intracorp.com.sg/ you will be able to use all the services offered by Intracorp. In Singapore, you can start your own business and live in a big way. This state is the center of commerce, as well as finance, and therefore whatever business you open, it will definitely bear fruit. The team that works in this company is as customer-oriented as possible. She is distinguished by her deep knowledge and understanding of all the nuances. At the same time, the transaction will be accompanied at every stage.
ремонт фундамента
замена венцов
подъем дома
ремонт фундамента
Привет, друзья!
Заказать документ о получении высшего образования можно в нашей компании в столице.
asxdiplomik.com/kupit-diplom-krasnoyarsk
Удачи!
ремонт фундамента
ремонт фундамента
замена венцов
конференционный зал oborudovanie-konferenc-zalov.ru .
конференц зал под ключ конференц зал под ключ .
Привет!
Заказать документ ВУЗа вы имеете возможность в нашей компании в Москве.
asxdiplomik.com/kupit-diplom-rostov-na-donu
Успехов в учебе!
замена венцов
Can I Play the Aviator Game on Mobile?
ivermectin for sale
подъем дома
переговорные комнаты под ключ переговорные комнаты под ключ .
замена венцов
подъем дома
buy speman generic – purchase himplasia pills buy fincar cheap
замена венцов
подъем дома
ремонт фундамента
подъем дома
ключ от комнаты совещаний ключ от комнаты совещаний .
замена венцов
замена венцов
замена венцов
подъем дома
Interactive Interface: Players can interact with the game in real-time, making decisions that impact their
ivermectin order
замена венцов
ремонт фундамента
ремонт фундамента
ремонт фундамента
замена венцов
ремонт фундамента
ремонт фундамента
замена венцов
Здравствуйте!
Заказать диплом ВУЗа.
antrem.ru/cb-profile/pluginclass/cbblogs?action=blogs&func=show&id=283
подъем дома
подъем дома
ремонт фундамента
plane crashes, making it a game of both luck and timing. This dynamic gameplay keeps players engaged and coming
ivermectin purchase
repairdesign24.com
замена венцов
chinaone.net
подъем дома
Привет!
Официальная покупка аттестата о среднем образовании в Москве и других городах
theplaygamepicks.com/диплом-техникума-где-и-как-купить/
Рады помочь!.
подъем дома
ремонт фундамента
На сайте https://vertolet52.ru закажите удивительные, увлекательные полеты на вертолете. При этом вы получите незабываемые, удивительные и яркие эмоции, которые будут переполнять. В компании действуют доступные расценки, а до вертолетной площадки вы доберетесь с комфортом, быстро. Так вы будете наблюдать самые живописные, увлекательные виды. Компания работает ежедневно – 7 дней в неделю. Для того чтобы составить представление о работе предприятия, почитайте отзывы. Вы можете заказать полет на любое количество времени.
замена венцов
подъем дома
подъем дома
замена венцов
Social and Community Aspects
ivermectin where to buy
ремонт фундамента
Скачать музыку https://vksaver.pro/ на сайте. Все новое, свежее, добавляемое каждый час. Хиты, ТОПы прослушивания, альбомы целиком, новинки. В mp3 на сайте, без регистрации можно скачать все что вы ищите, в одном месте. Самый большой выбор музыки в интернете.
ремонт фундамента
подъем дома
Привет!
Мы предлагаем дипломы психологов, юристов, экономистов и любых других профессий.
br-totalbyg.dk/2024/07/13/купить-диплом-безопасно/
Всегда вам поможем!.
На сайте https://albakaluga.ru/ запишитесь на прием для того, чтобы сделать свою улыбку идеальной. В клинике вас ожидают квалифицированные, опытные и талантливые врачи, которые используют уникальные методы лечения, а также прогрессивные технологии, лучшие материалы и зарубежное оборудование. Все врачи узкой специализации, что позволит обширно изучить проблему и справиться с ней быстро, комплексно и эффективно. Действуют привлекательные и доступные расценки. Гарантируется безупречное качество лечения.
ремонт фундамента
Привет, друзья!
Мы можем предложить дипломы любых профессий по разумным ценам.
eurodelo.ru/vash-shans-na-vyisshee-obrazovanie-kupit-diplom
замена венцов
Ищете курсы когнитивно-поведенческой терапии, КПТ, онлайн обучение кпт , курсы КПТ для психологов, дистанционные курсы КПТ? Выбирайте с отменной репутацией онлайн-школы, с грамотными преподавателями и возможностью через практикумы и онлайн-тренинги практиковать навыки.
ремонт фундамента
Добрый день!
Покупка диплома о среднем полном образовании: как избежать мошенничества?
matthiasjakobbecker.com/купить-диплом-проверенные-способы/
Рады оказаться полезными!.
ремонт фундамента
подъем дома
На сайте https://lilibum.ru вы сможете познакомиться с мужчиной или девушкой для самых разных целей, в том числе, создания крепких отношений, семьи. Если кто-то вам понравился, то напишите сообщение, чтобы вступить в контакт, а затем и назначить долгожданную встречу. Вполне вероятно, что вы друг другу подходите. Для того чтобы воспользоваться всеми функциями и преимуществами, необходимо пройти регистрацию. На сайте регулярно регистрируется огромное количество пользователей, которые тоже хотят отыскать свою вторую половинку.
замена венцов
ремонт фундамента
In today’s world, caring for health and proper nutrition is becoming a priority for many people dominicandesign.net
подъем дома
V8doc.ru – сайт, где вы узнаете, для чего необходим 1С Документооборот. Помогаем бизнесу быть эффективнее и расти. Автоматизация документооборота с использованием «1С» поможет вам сконцентрироваться на развитии вашей компании. С «1С: Документооборотом» вы сможете сделать команду свою продуктивной и отказаться от рутинных процессов. https://v8doc.ru – сайт, где вы уже сейчас можете оставить заявку. Укажите ваш номер телефона, имя и мы свяжемся с вами обязательно. Предоставим подробные ответы и квалифицированную консультацию.
When hiring as a courier, it is additionally necessary to determine the driver’s license holidaynewsletters.com
подъем дома
замена венцов
In-Game Bonuses and Rewards
ivermectin buy
замена венцов
подъем дома
ремонт фундамента
Здравствуйте!
Приобрести документ о получении высшего образования можно у нас в Москве.
ast-diplomy.com/kupit-diplom-o-vysshem-obrazovanii
ремонт фундамента
подъем дома
На сайте https://gruz63.ru/gruzoperevozki/ посмотрите телефон компании, которая на профессиональном уровне оказывает услуги, связанные с грузоперевозками. Заказать работы смогут как частные компании, так и физические лица, крупные предприятия. Грузоперевозками пользуются во время офисного, дачного переезда, для того, чтобы доставить строительные материалы из магазина. В этой компании работают исключительно опытные, квалифицированные и компетентные грузчики, которые быстро и аккуратно справятся с работой. А у вас даже не останутся замечания.
замена венцов
Хотите смотреть интересные сериалы онлайн абсолютно бесплатно и в хорошем hd качестве? Тогда добро пожаловать на портал zonaserialov.net! У нас найдете множество новинок. Предлагаем вам исключительно качественный материал. Смотрите лучшие сериалы и отдыхайте! https://zonaserialov.net – сайт, который имеет привлекательный дизайн, можете убедиться в этом сами. Здесь есть удобный поиск, воспользуйтесь им. Постоянно работаем над улучшением нашего сервиса. Приглашаем вас окунуться в великолепный мир сериалов, положительные эмоции мы вам гарантируем!
Привет, друзья!
Заказать документ о получении высшего образования вы имеете возможность в нашей компании.
ast-diploms.com/kupit-diplom-novosibirsk
подъем дома
подъем дома
Добрый день!
Приобрести документ университета можно у нас в столице.
ast-diploms.com/otzyvy
Удачи!
подъем дома
подъем дома
Сайт replica-avenue.com предлагает качественные реплики брендовой обуви по привлекательным ценам. Люкс копии обуви отличаются высочайшим качеством, точным исполнением деталей и применением натуральных материалов. Ищете кроссовки реплика купить? Replica-avenue.com – сайт, где вы узнаете, как копия отличается от оригинала. В нашем каталоге можно подобрать классические или же спортивные модели различных типов. Осуществляется отправка товаров по всей РФ и миру удобным способом. Чтобы купить понравившуюся пару, позвоните нам по контактному номеру телефона.
ремонт фундамента
Привет!
Купить документ о получении высшего образования можно в нашей компании в столице.
ast-diplomy.com/kupit-diplom-vracha
Успехов в учебе!
подъем дома
Frequently Asked Questions (FAQs)
ivermectin price
На сайте http://oknaksa.by вы сможете проконсультироваться по таким вопросам, как: окна ПВХ, балконы, патио. На все конструкции даются гарантии до 20 лет. Все клиенты смогут воспользоваться бесплатным обслуживанием. А работа происходит по ГОСТу, СНИПу. Для того чтобы получить необходимый результат, на объект выезжают замерщики для того, чтобы определить размеры с точностью. Установка происходит в день, когда привезут окна. Перед вами огромное количество готовых проектов, которыми вы сможете воспользоваться прямо сейчас.
развлечения в сочи для детей летом
I have been surfing online more than three hours today, yet I never found anything that grabbed my interest as much as this piece.
ремонт фундамента
Скачать музыку https://muzvk.pro/ целыми альбомами, чартами, коллекциями, по исполнителям на сайте. Зайдите на сайт, ознакомьтесь и шикарной коллекцией музыки в mp3 и вы найдете то что ищите или найдете новое для себя. Музыка разных жанров, без регистрации и рекламы – качать в мп3 на сайте.
Привет!
Мы изготавливаем дипломы психологов, юристов, экономистов и других профессий.
sportraketka.ru/byistroe-oformlenie-diplomov-nadezhno-i-legalno
Всегда вам поможем!.
замена венцов
getx регистрация
развлечения город сочи
Добрый день!
Заказать документ ВУЗа можно в нашей компании в столице.
diploms-x.com/kupit-diplom-sankt-peterburg
Успехов в учебе!
подъем дома
ремонт фундамента
Добрый день!
Как купить аттестат 11 класса с официальным упрощенным обучением в Москве
softerioninc.com/купить-диплом-в-киселевске/
подъем дома
ремонт фундамента
подъем дома
ремонт фундамента
laptops, tablets, and smartphones. This flexibility allows players to enjoy the game on their preferred device,
ivermectin order
ремонт фундамента
замена венцов
замена венцов
Hmm is anyone else experiencing problems with the pictures on this blog loading? I’m trying to figure out if its a problem on my end or if it’s the blog. Any responses would be greatly appreciated.
https://christian-culture.info
замена венцов
ремонт фундамента
видеостена купить москва видеостена купить москва .
Оборудование актовых залов http://oborudovanie-aktovogo-zala.ru .
подъем дома
подъем дома
подъем дома
Привет!
Приобрести диплом о высшем образовании.
igpsclub.ru/social/read-blog/5452
ремонт фундамента
Студия Мята в Челябинске chelyabinsk.studio-mint.ru – это дизайн интерьеров домов, квартир и коммерческих помещений, персональное проектирование коттеджей и домов, подбор, а также закупка материалов под ключ, ремонт домов и квартир. Зайдите на сайт и ознакомьтесь с портфолио – уникальные услуги от профессиональных дизайнеров, быстрые темпы работ и комплексный и чуткий подход к желаниям заказчика.
Привет!
Заказать документ о получении высшего образования можно в нашей компании. Мы оказываем услуги по изготовлению и продаже документов об окончании любых университетов РФ. Вы сможете получить необходимый диплом по любой специальности, любого года выпуска, включая документы старого образца. Даем гарантию, что при проверке документа работодателем, подозрений не возникнет.
Мы готовы предложить дипломы психологов, юристов, экономистов и прочих профессий по разумным тарифам. Цена зависит от определенной специальности, года получения и образовательного учреждения. Всегда стараемся поддерживать для покупателей адекватную политику тарифов. Важно, чтобы дипломы были доступны для большого количества наших граждан.
gaeloxeparo.lucialpiazzale.com/podrobnoe-opisanie-priobretenia-attestata-v-magazine
Рады оказаться полезными!
замена венцов
подъем дома
Can I Play the Aviator Game on Mobile?
ivermectin for sale
ремонт фундамента
Привет, друзья!
Мы предлагаем дипломы любых профессий по приятным ценам.
saltandsweetsaftab.com/2024/06/30/купить-диплом-молдавии/
подъем дома
подъем дома
ремонт фундамента
подъем дома
Здравствуйте!
Мы можем предложить дипломы любых профессий по приятным ценам.
http://www.greenmind.cl/2024/06/30/диплом-магистра-1997-2003-видео/
See Real – компания, которая накопила в сфере светодиодных технологий и наружной рекламы большой потенциал. Помогаем бизнес сделать заметным, и предоставляем конкурентоспособные цены. Готовы рассмотреть смелые идеи. Пожалуйста, оставьте ваши контактные данные, и мы обязательно свяжемся с вами. https://iseer.kz/ – сайт, где вы можете увидеть примеры наших архитектурных решений и рекламы. Также можно заказать звонок консультанта, чтобы обсудить детали и узнать стоимость. С радостью на все вопросы ответим!
подъем дома
Зайдите на сайт https://plastikov-okna.ru/ и ознакомьтесь с производителем пластиковых окон в Москве, который предлагает широкий ассортимент продукции по лучшим ценам. Быстрое изготовление, многолетняя гарантия качества, выезд замерщика бесплатно, минимальная предоплата, монтаж от профессионалов. Ознакомьтесь на сайте с ассортиментом и ценами.
подъем дома
оборудование для сцены актового зала http://www.oborudovanija-dlja-aktovyh-zalov.ru .
замена венцов
game is random and unbiased, providing a fair chance for all players to win.
ivermectin for sale
замена венцов
замена венцов
замена венцов
ремонт фундамента
замена венцов
ремонт фундамента