New to This Mommy’s Heart? Check out my story from the beginning here – My PPCM Story
**Warning – Post Contains Graphic Images**
Courage, dear heart.
-C.S. Lewis
Primary graft dysfunction occurs when the left ventricle, right ventricle or both dysfunction within 24 hours of the heart transplant surgery and no obvious cause can be determined. About 10-15% of heart transplant patients experience primary graft dysfunction. There is usually a 50% chance the heart will start working again with no longterm consequences. If the heart doesn’t recover, the patient must be re-listed for transplant.
You didn’t think this surgery would be easy, did you? Haven’t you recognized the reoccurring theme throughout this story.
On the 10th, the day after my surgery, there were several tests to check the heart’s function but there were no significant improvements. Discussions began about putting me back on the transplant list as a 1A. I could not get another total artificial heart so my only options were for this heart to recover or to be retransplanted.
The UWMC staff was so good to my family during this horrible time in our lives. In my husband’s notes, he describes the floor as being very somber after my transplant. My family received many condolences and the nurses brought in food multiple times since they didn’t want to leave my side. I was so lucky to be in their care.
The time after the transplant was the worst for my family. All of the setbacks in my health were leaving them disheartened and not as optimistic about what the future held.

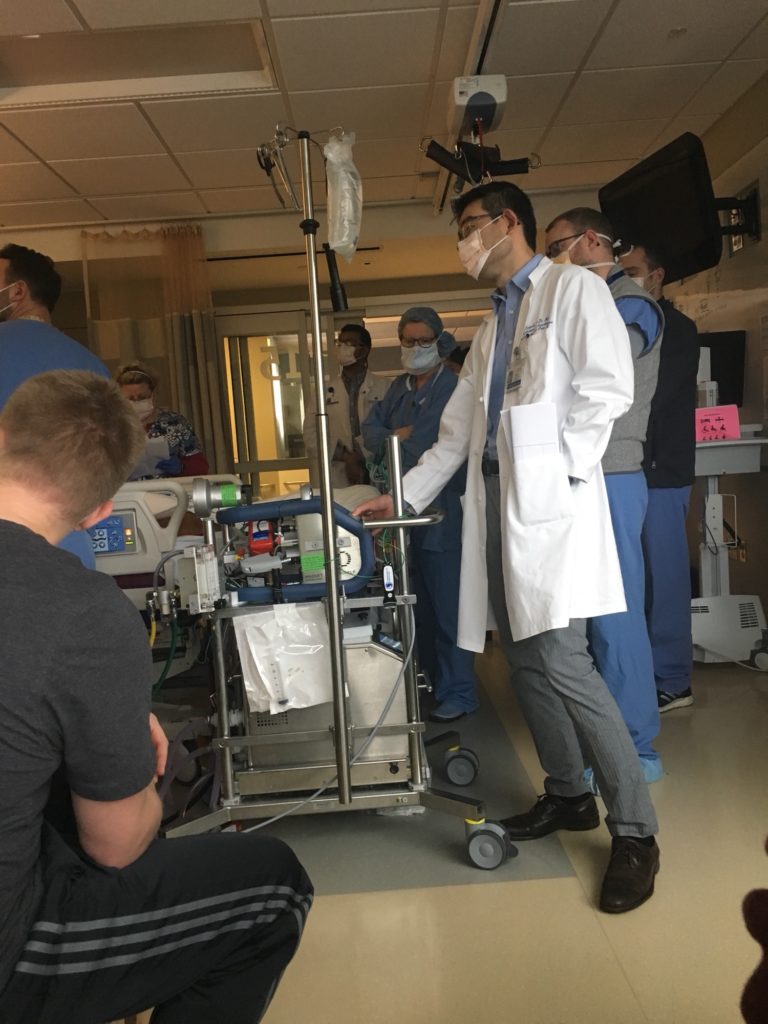
On the 11th, my husband’s family arrived, along with two of his friends from high school. That day they ran more tests to check my heart’s function. Luckily, there were some improvements. My ejection fraction and pulmonary artery pressure were basically normal, so my left ventricle was looking like it could support me off of ECMO. Unfortunately, there was no change with my right ventricle which was still not working well at all.


**GRAPHIC IMAGES AHEAD**


When on ECMO, one of the risks is bleeding. Just like the first time I was on ECMO, I was extremely oozy. I had to receive 3 more units of blood (up to 34 units total for my hospitalization).

On January 12th, I was taken into surgery for a washout. After a f
When they had first started the procedure, the right side of the heart still wasn’t looking good. However, once the wound vac was removed, the right side went back to near normal function. My heart was working so well that they were able to decannulate me from the ECMO. My chest was left open to wait for more swelling to go down but things finally seemed to be heading in the right direction.
I guess the day this happened, we had quite a large group in the waiting room. There was my family, my husband’s family and several of our friends there as well. I’m told there were many tears of joy and relief that I was doing better. ECMO is scary and having to get another transplant was not ideal. I was going to get to keep my heart. Who would have thought I would come out on the positive side of 50/50 odds?
On the 13th, I remained stable throughout. The primary issues at this point were my blood pressure being too high and the amount of fluid I had retained. They were managing my blood pressure by frequently adding and adjusting medications. I was given aggressive diuresis to combat m
They had been cautious with my medications up to this point but on the 13th they finally gave me ATG and tacrolimus.
Medical Terminology
- ATG – anti-thymocyte globulin also known as “Rabbit.” This is an infusion of rabbit antibodies against human T cells. It is used after transplants to reduce the chance of acute rejection.
- Tacrolimus – immunosuppress
e nt drug used to prevent rejection. This is one of the medications I will take for life.
Since I hadn’t had a bowel movement in over a week, my nurse focused on that and diuresis overnight. I ended up having 5-6 bowel movements over the course of the night totaling about 1.5 liters. By the morning I was down several liters in total despite all of my IV infusions.
Have I mentioned what great, amazing, awesome, fantastic angels on Earth nurses are? Another post for another day, but their jobs are so hard physically and emotionally. It takes such a special person to take on that role.
Another TTE was done on the 14th to check my heart function. It showed that, besides being very dry, my left ventricle was normal. My right ventricle still had moderate dysfunction but that is not uncommon following a heart transplant.

On the 15th, I went back in for another surgery. The surgery went well and was thankfully uneventful. They were able to finally close my chest and later that day they were able to extubate me. To be safe, they kept me on a high dose of oxygen overnight but I was swallowing my secretions and talking by the end of the night.
I get weepy when I read this part from my husband’s notes:
When she could finally start to talk she said she loved me…I missed talking to her so much.
Service Unavailable
The server is temporarily unable to service your request due to maintenance downtime or capacity problems. Please try again later.
Additionally, a 503 Service Unavailable error was encountered while trying to use an ErrorDocument to handle the request.

